User login
Biomarker may ID high-risk colon cancers
A biomarker for which a screening test is already available – lack of CDX2 expression – appears to identify the approximately 20% of stage II and 50% of stage III colon cancers that are at high risk of recurrence and would benefit from adjuvant chemotherapy, according to a report published online Jan. 21 in the New England Journal of Medicine.
Distinguishing the high-risk tumors from those unlikely to recur or progress would allow some patients to opt for adjuvant chemotherapy that has been shown to significantly raise the rates of overall and disease-free survival. At present, almost all patients with stage II colon cancer are treated using surgery alone, said Dr. Piero Dalerba of the Herbert Irving Comprehensive Cancer Center and the department of pathology and cell biology at Columbia University, New York, and his associates.
The investigators used a bioinformatics approach to search for biomarkers that would identify the most aggressive colon cancers: undifferentiated tumors characterized by immature, stem-like colonic epithelial cells and depleted of more mature cells. They focused on biomarkers for which clinical diagnostic tests are already available, to facilitate use in real-world clinical practice. Their search through 2,329 colon gene-expression array experiments found that when tumors do not express one particular protein, homeobox transcription factor CDX2, “a master regulator of intestinal development and oncogenesis” that is highly specifically expressed in intestinal epithelium, those tumors tend to have aggressive features such as advanced stage, vascular invasion, and BRAF mutation.
Survival outcomes were then compared in a discovery data set of 466 patients. The 5-year disease-free survival rate was significantly lower, at 41%, among the 32 patients who had CDX2-negative tumors than the 74% survival rate among the 434 patients with CDX2-positive tumors. The hazard ratio for disease recurrence among patients with CDX2-negative vs. CDX2-positive tumors was 2.73, Dr. Dalerba and his associates said (N Engl J Med. 2016 Jan 21. doi:10.1056/NEJMoa1506597).
The investigators confirmed these findings in a separate validation data set of 366 patients, of whom 48 had CDX2-negative and 318 had CDX2-positive tumors. Five-year disease-free survival (48% vs. 71%), overall survival (33% vs. 59%), and disease-specific survival (45% vs. 72%) were significantly lower with CDX2-negative tumors, and the HR for disease recurrence was 2.42.
To determine whether adjuvant chemotherapy would improve survival outcomes in patients with CDX2-negative tumors, the researchers assessed outcomes in an expanded dataset of 669 patients with stage II and 1,228 patients with stage III colon cancer. They confirmed that among patients with stage II CDX2-negative tumors, those who received adjuvant chemotherapy had a higher rate of disease-free survival (91%) than did those who didn’t receive adjuvant chemotherapy (56%). Similarly, among patients with stage III CDX2-negative tumors, those who received adjuvant chemotherapy had a higher rate of disease-free survival (74%) than those who did not receive adjuvant chemotherapy (37%).
This survival benefit was independent of many known risk factors, including tumor grade, they noted.
These results must be replicated in future prospective studies, because this study’s design was retrospective and exploratory, Dr. Dalerba and his associates added.
This work was supported by the National Comprehensive Cancer Network, the National Institutes of Health, Siebel Stem Cell Institute, the Thomas and Stacey Siebel Foundation, the Virginia and D.K. Ludwig Fund for Cancer Research, the California Institute for Regenerative Medicine, the U.S. Department of Defense, the Bladder Cancer Advocacy Network, and BD Biosciences. Dr. Dalerba reported ties to Quanticel Pharmaceuticals and Oncomed Pharmaceuticals, and his associates reported ties to numerous industry sources.
These study findings give clinicians the opportunity to move beyond the existing inadequate method of selecting patients for adjuvant chemotherapy. Although this was not a perfect or definitive study, since it was retrospective and the number of patients with CDX2-negative colon cancers was relatively small, it nevertheless entailed numerous rigorous data analyses.

|
Dr. C. Richard Boland |
Moreover, the results raise the important question of what mechanism might be silencing CDX2 in this subset of aggressive cancers. The answer could lead to the discovery of new approaches to treating the underlying problem.
C. Richard Boland, M.D., and Ajay Goel, Ph.D., are at the Center for Gastrointestinal Research and the Center for Epigenetics, Cancer Prevention, and Genomics at Baylor Research Institute, and at the Baylor Charles A. Sammons Cancer Center, all in Dallas. They reported having no relevant financial disclosures. Dr. Boland and Dr. Goel made these remarks in an editorial accompanying Dr. Dalerba’s report (N Engl J Med. 2016 Jan 21. doi:10.1056/NEJMe1514353).
These study findings give clinicians the opportunity to move beyond the existing inadequate method of selecting patients for adjuvant chemotherapy. Although this was not a perfect or definitive study, since it was retrospective and the number of patients with CDX2-negative colon cancers was relatively small, it nevertheless entailed numerous rigorous data analyses.

|
Dr. C. Richard Boland |
Moreover, the results raise the important question of what mechanism might be silencing CDX2 in this subset of aggressive cancers. The answer could lead to the discovery of new approaches to treating the underlying problem.
C. Richard Boland, M.D., and Ajay Goel, Ph.D., are at the Center for Gastrointestinal Research and the Center for Epigenetics, Cancer Prevention, and Genomics at Baylor Research Institute, and at the Baylor Charles A. Sammons Cancer Center, all in Dallas. They reported having no relevant financial disclosures. Dr. Boland and Dr. Goel made these remarks in an editorial accompanying Dr. Dalerba’s report (N Engl J Med. 2016 Jan 21. doi:10.1056/NEJMe1514353).
These study findings give clinicians the opportunity to move beyond the existing inadequate method of selecting patients for adjuvant chemotherapy. Although this was not a perfect or definitive study, since it was retrospective and the number of patients with CDX2-negative colon cancers was relatively small, it nevertheless entailed numerous rigorous data analyses.

|
Dr. C. Richard Boland |
Moreover, the results raise the important question of what mechanism might be silencing CDX2 in this subset of aggressive cancers. The answer could lead to the discovery of new approaches to treating the underlying problem.
C. Richard Boland, M.D., and Ajay Goel, Ph.D., are at the Center for Gastrointestinal Research and the Center for Epigenetics, Cancer Prevention, and Genomics at Baylor Research Institute, and at the Baylor Charles A. Sammons Cancer Center, all in Dallas. They reported having no relevant financial disclosures. Dr. Boland and Dr. Goel made these remarks in an editorial accompanying Dr. Dalerba’s report (N Engl J Med. 2016 Jan 21. doi:10.1056/NEJMe1514353).
A biomarker for which a screening test is already available – lack of CDX2 expression – appears to identify the approximately 20% of stage II and 50% of stage III colon cancers that are at high risk of recurrence and would benefit from adjuvant chemotherapy, according to a report published online Jan. 21 in the New England Journal of Medicine.
Distinguishing the high-risk tumors from those unlikely to recur or progress would allow some patients to opt for adjuvant chemotherapy that has been shown to significantly raise the rates of overall and disease-free survival. At present, almost all patients with stage II colon cancer are treated using surgery alone, said Dr. Piero Dalerba of the Herbert Irving Comprehensive Cancer Center and the department of pathology and cell biology at Columbia University, New York, and his associates.
The investigators used a bioinformatics approach to search for biomarkers that would identify the most aggressive colon cancers: undifferentiated tumors characterized by immature, stem-like colonic epithelial cells and depleted of more mature cells. They focused on biomarkers for which clinical diagnostic tests are already available, to facilitate use in real-world clinical practice. Their search through 2,329 colon gene-expression array experiments found that when tumors do not express one particular protein, homeobox transcription factor CDX2, “a master regulator of intestinal development and oncogenesis” that is highly specifically expressed in intestinal epithelium, those tumors tend to have aggressive features such as advanced stage, vascular invasion, and BRAF mutation.
Survival outcomes were then compared in a discovery data set of 466 patients. The 5-year disease-free survival rate was significantly lower, at 41%, among the 32 patients who had CDX2-negative tumors than the 74% survival rate among the 434 patients with CDX2-positive tumors. The hazard ratio for disease recurrence among patients with CDX2-negative vs. CDX2-positive tumors was 2.73, Dr. Dalerba and his associates said (N Engl J Med. 2016 Jan 21. doi:10.1056/NEJMoa1506597).
The investigators confirmed these findings in a separate validation data set of 366 patients, of whom 48 had CDX2-negative and 318 had CDX2-positive tumors. Five-year disease-free survival (48% vs. 71%), overall survival (33% vs. 59%), and disease-specific survival (45% vs. 72%) were significantly lower with CDX2-negative tumors, and the HR for disease recurrence was 2.42.
To determine whether adjuvant chemotherapy would improve survival outcomes in patients with CDX2-negative tumors, the researchers assessed outcomes in an expanded dataset of 669 patients with stage II and 1,228 patients with stage III colon cancer. They confirmed that among patients with stage II CDX2-negative tumors, those who received adjuvant chemotherapy had a higher rate of disease-free survival (91%) than did those who didn’t receive adjuvant chemotherapy (56%). Similarly, among patients with stage III CDX2-negative tumors, those who received adjuvant chemotherapy had a higher rate of disease-free survival (74%) than those who did not receive adjuvant chemotherapy (37%).
This survival benefit was independent of many known risk factors, including tumor grade, they noted.
These results must be replicated in future prospective studies, because this study’s design was retrospective and exploratory, Dr. Dalerba and his associates added.
This work was supported by the National Comprehensive Cancer Network, the National Institutes of Health, Siebel Stem Cell Institute, the Thomas and Stacey Siebel Foundation, the Virginia and D.K. Ludwig Fund for Cancer Research, the California Institute for Regenerative Medicine, the U.S. Department of Defense, the Bladder Cancer Advocacy Network, and BD Biosciences. Dr. Dalerba reported ties to Quanticel Pharmaceuticals and Oncomed Pharmaceuticals, and his associates reported ties to numerous industry sources.
A biomarker for which a screening test is already available – lack of CDX2 expression – appears to identify the approximately 20% of stage II and 50% of stage III colon cancers that are at high risk of recurrence and would benefit from adjuvant chemotherapy, according to a report published online Jan. 21 in the New England Journal of Medicine.
Distinguishing the high-risk tumors from those unlikely to recur or progress would allow some patients to opt for adjuvant chemotherapy that has been shown to significantly raise the rates of overall and disease-free survival. At present, almost all patients with stage II colon cancer are treated using surgery alone, said Dr. Piero Dalerba of the Herbert Irving Comprehensive Cancer Center and the department of pathology and cell biology at Columbia University, New York, and his associates.
The investigators used a bioinformatics approach to search for biomarkers that would identify the most aggressive colon cancers: undifferentiated tumors characterized by immature, stem-like colonic epithelial cells and depleted of more mature cells. They focused on biomarkers for which clinical diagnostic tests are already available, to facilitate use in real-world clinical practice. Their search through 2,329 colon gene-expression array experiments found that when tumors do not express one particular protein, homeobox transcription factor CDX2, “a master regulator of intestinal development and oncogenesis” that is highly specifically expressed in intestinal epithelium, those tumors tend to have aggressive features such as advanced stage, vascular invasion, and BRAF mutation.
Survival outcomes were then compared in a discovery data set of 466 patients. The 5-year disease-free survival rate was significantly lower, at 41%, among the 32 patients who had CDX2-negative tumors than the 74% survival rate among the 434 patients with CDX2-positive tumors. The hazard ratio for disease recurrence among patients with CDX2-negative vs. CDX2-positive tumors was 2.73, Dr. Dalerba and his associates said (N Engl J Med. 2016 Jan 21. doi:10.1056/NEJMoa1506597).
The investigators confirmed these findings in a separate validation data set of 366 patients, of whom 48 had CDX2-negative and 318 had CDX2-positive tumors. Five-year disease-free survival (48% vs. 71%), overall survival (33% vs. 59%), and disease-specific survival (45% vs. 72%) were significantly lower with CDX2-negative tumors, and the HR for disease recurrence was 2.42.
To determine whether adjuvant chemotherapy would improve survival outcomes in patients with CDX2-negative tumors, the researchers assessed outcomes in an expanded dataset of 669 patients with stage II and 1,228 patients with stage III colon cancer. They confirmed that among patients with stage II CDX2-negative tumors, those who received adjuvant chemotherapy had a higher rate of disease-free survival (91%) than did those who didn’t receive adjuvant chemotherapy (56%). Similarly, among patients with stage III CDX2-negative tumors, those who received adjuvant chemotherapy had a higher rate of disease-free survival (74%) than those who did not receive adjuvant chemotherapy (37%).
This survival benefit was independent of many known risk factors, including tumor grade, they noted.
These results must be replicated in future prospective studies, because this study’s design was retrospective and exploratory, Dr. Dalerba and his associates added.
This work was supported by the National Comprehensive Cancer Network, the National Institutes of Health, Siebel Stem Cell Institute, the Thomas and Stacey Siebel Foundation, the Virginia and D.K. Ludwig Fund for Cancer Research, the California Institute for Regenerative Medicine, the U.S. Department of Defense, the Bladder Cancer Advocacy Network, and BD Biosciences. Dr. Dalerba reported ties to Quanticel Pharmaceuticals and Oncomed Pharmaceuticals, and his associates reported ties to numerous industry sources.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: A biomarker for which a screening test is already available – lack of CDX2 expression – appears to identify which stage II and III colon cancers are high-risk and would benefit from adjuvant chemotherapy.
Major finding: Five-year disease-free survival rate was significantly lower (41%) in patients who had CDX2-negative tumors than in patients with CDX2-positive tumors (74%).
Data source: A series of analyses using data mining to identify (in a database of 466 patients) and validate (in databases of 366 and 1,897 patients) a biomarker for early colon cancers at high risk for recurrence/metastasis.
Disclosures: The National Comprehensive Cancer Network, the National Institutes of Health, Siebel Stem Cell Institute, the Thomas and Stacey Siebel Foundation, the Virginia and D.K. Ludwig Fund for Cancer Research, the California Institute for Regenerative Medicine, the U.S. Department of Defense, the Bladder Cancer Advocacy Network, and BD Biosciences supported the work. Dr. Dalerba reported ties to Quanticel Pharmaceuticals and Oncomed Pharmaceuticals, and his associates reported ties to numerous industry sources.
Eluxadoline improves symptoms of IBS with diarrhea
The new drug eluxadoline improved symptoms of irritable bowel syndrome (IBS) with diarrhea in two manufacturer-sponsored phase III clinical trials involving 2,427 patients, according to a report published online January 21 in the New England Journal of Medicine.
At present, treatment options for IBS with diarrhea are limited and are frequently ineffective. Eluxadoline is a peripherally acting agonist of three different opioid receptors which, in the enteric circuitry of the GI tract, act in regulating GI motility, secretion, and visceral sensation. The agent is thought to decrease visceral hypersensitivity without disrupting intestinal motility completely, said Dr. Anthony J. Lembo of Harvard University and Beth Israel Deaconess Medical Center, Boston, and his associates.
They assessed patient response to the drug in two randomized, double-blind, placebo-controlled trials conducted at hundreds of medical centers in the U.S., Canada, and the United Kingdom. Study participants received oral tablets of 75-mg eluxadoline, 100-mg eluxadoline, or matching placebos for 26 weeks, followed by either an additional 26 weeks of treatment solely for safety assessment in one study or an additional 4-week period of placebo withdrawal in the other.
The primary efficacy endpoint was the proportion of patients who reported a reduction of at least 30% in baseline scores for worst abdominal pain together with improvement on stool-consistency scores, on at least half the days of follow-up. This endpoint was reached in a significantly greater proportion of patients taking 75-mg eluxadoline (23.4%) or 100-mg eluxadoline (29.3%) than placebo (19.0%) in the first trial. Treatment responses were similar in the second trial (30.4% and 32.7% vs 20.2%, respectively).
Both doses of eluxadoline also improved secondary endpoints of stool consistency, frequency, and urgency, but did not reduce episodes of incontinence. Both doses also were superior to placebo in providing “adequate” relief of IBS symptoms, improving global symptom scores, and improving disease-related quality of life. Treatment responses were first observed within 1 week of initiating therapy and persisted throughout the 26-week assessment period, and the magnitude of benefit was comparable to that reported for alosetron and rifaximin, the investigators said (N Engl J Med. 2016 Jan 21. doi: 10.1056/NEJMoa1505180).
Regarding safety, no treatment-related trends were noted in serum chemical values or hematologic values over time. Isolated renal and metabolic events occurred, but “there was no pattern across study groups.” Serious adverse events occurred in more patients taking 75-mg (4.2%) or 100-mg (4.8%) eluxadoline, compared with those taking placebo (3.0%). Five patients taking the active drug developed pancreatitis (0.3%) and 8 (0.5%) developed acute abdominal pain in conjunction with abrupt increases in liver enzymes, which was deemed to stem from spasm of the sphincter of Oddi. Most of these events developed within 2 weeks of initiating treatment. No patients in the placebo groups developed these problems.
In addition, two patients taking the active drug reported feeling euphoria and two reported feeling drunk, while none of the patients in the placebo group reported such adverse events. The most common adverse events during the study were nausea, constipation, and abdominal pain. Rates of treatment discontinuation were higher among patients taking both doses of active drug than among those taking placebo.
IBS symptoms did not worsen appreciably during the withdrawal period or for 2 weeks of follow-up after treatment ended.
The new drug eluxadoline improved symptoms of irritable bowel syndrome (IBS) with diarrhea in two manufacturer-sponsored phase III clinical trials involving 2,427 patients, according to a report published online January 21 in the New England Journal of Medicine.
At present, treatment options for IBS with diarrhea are limited and are frequently ineffective. Eluxadoline is a peripherally acting agonist of three different opioid receptors which, in the enteric circuitry of the GI tract, act in regulating GI motility, secretion, and visceral sensation. The agent is thought to decrease visceral hypersensitivity without disrupting intestinal motility completely, said Dr. Anthony J. Lembo of Harvard University and Beth Israel Deaconess Medical Center, Boston, and his associates.
They assessed patient response to the drug in two randomized, double-blind, placebo-controlled trials conducted at hundreds of medical centers in the U.S., Canada, and the United Kingdom. Study participants received oral tablets of 75-mg eluxadoline, 100-mg eluxadoline, or matching placebos for 26 weeks, followed by either an additional 26 weeks of treatment solely for safety assessment in one study or an additional 4-week period of placebo withdrawal in the other.
The primary efficacy endpoint was the proportion of patients who reported a reduction of at least 30% in baseline scores for worst abdominal pain together with improvement on stool-consistency scores, on at least half the days of follow-up. This endpoint was reached in a significantly greater proportion of patients taking 75-mg eluxadoline (23.4%) or 100-mg eluxadoline (29.3%) than placebo (19.0%) in the first trial. Treatment responses were similar in the second trial (30.4% and 32.7% vs 20.2%, respectively).
Both doses of eluxadoline also improved secondary endpoints of stool consistency, frequency, and urgency, but did not reduce episodes of incontinence. Both doses also were superior to placebo in providing “adequate” relief of IBS symptoms, improving global symptom scores, and improving disease-related quality of life. Treatment responses were first observed within 1 week of initiating therapy and persisted throughout the 26-week assessment period, and the magnitude of benefit was comparable to that reported for alosetron and rifaximin, the investigators said (N Engl J Med. 2016 Jan 21. doi: 10.1056/NEJMoa1505180).
Regarding safety, no treatment-related trends were noted in serum chemical values or hematologic values over time. Isolated renal and metabolic events occurred, but “there was no pattern across study groups.” Serious adverse events occurred in more patients taking 75-mg (4.2%) or 100-mg (4.8%) eluxadoline, compared with those taking placebo (3.0%). Five patients taking the active drug developed pancreatitis (0.3%) and 8 (0.5%) developed acute abdominal pain in conjunction with abrupt increases in liver enzymes, which was deemed to stem from spasm of the sphincter of Oddi. Most of these events developed within 2 weeks of initiating treatment. No patients in the placebo groups developed these problems.
In addition, two patients taking the active drug reported feeling euphoria and two reported feeling drunk, while none of the patients in the placebo group reported such adverse events. The most common adverse events during the study were nausea, constipation, and abdominal pain. Rates of treatment discontinuation were higher among patients taking both doses of active drug than among those taking placebo.
IBS symptoms did not worsen appreciably during the withdrawal period or for 2 weeks of follow-up after treatment ended.
The new drug eluxadoline improved symptoms of irritable bowel syndrome (IBS) with diarrhea in two manufacturer-sponsored phase III clinical trials involving 2,427 patients, according to a report published online January 21 in the New England Journal of Medicine.
At present, treatment options for IBS with diarrhea are limited and are frequently ineffective. Eluxadoline is a peripherally acting agonist of three different opioid receptors which, in the enteric circuitry of the GI tract, act in regulating GI motility, secretion, and visceral sensation. The agent is thought to decrease visceral hypersensitivity without disrupting intestinal motility completely, said Dr. Anthony J. Lembo of Harvard University and Beth Israel Deaconess Medical Center, Boston, and his associates.
They assessed patient response to the drug in two randomized, double-blind, placebo-controlled trials conducted at hundreds of medical centers in the U.S., Canada, and the United Kingdom. Study participants received oral tablets of 75-mg eluxadoline, 100-mg eluxadoline, or matching placebos for 26 weeks, followed by either an additional 26 weeks of treatment solely for safety assessment in one study or an additional 4-week period of placebo withdrawal in the other.
The primary efficacy endpoint was the proportion of patients who reported a reduction of at least 30% in baseline scores for worst abdominal pain together with improvement on stool-consistency scores, on at least half the days of follow-up. This endpoint was reached in a significantly greater proportion of patients taking 75-mg eluxadoline (23.4%) or 100-mg eluxadoline (29.3%) than placebo (19.0%) in the first trial. Treatment responses were similar in the second trial (30.4% and 32.7% vs 20.2%, respectively).
Both doses of eluxadoline also improved secondary endpoints of stool consistency, frequency, and urgency, but did not reduce episodes of incontinence. Both doses also were superior to placebo in providing “adequate” relief of IBS symptoms, improving global symptom scores, and improving disease-related quality of life. Treatment responses were first observed within 1 week of initiating therapy and persisted throughout the 26-week assessment period, and the magnitude of benefit was comparable to that reported for alosetron and rifaximin, the investigators said (N Engl J Med. 2016 Jan 21. doi: 10.1056/NEJMoa1505180).
Regarding safety, no treatment-related trends were noted in serum chemical values or hematologic values over time. Isolated renal and metabolic events occurred, but “there was no pattern across study groups.” Serious adverse events occurred in more patients taking 75-mg (4.2%) or 100-mg (4.8%) eluxadoline, compared with those taking placebo (3.0%). Five patients taking the active drug developed pancreatitis (0.3%) and 8 (0.5%) developed acute abdominal pain in conjunction with abrupt increases in liver enzymes, which was deemed to stem from spasm of the sphincter of Oddi. Most of these events developed within 2 weeks of initiating treatment. No patients in the placebo groups developed these problems.
In addition, two patients taking the active drug reported feeling euphoria and two reported feeling drunk, while none of the patients in the placebo group reported such adverse events. The most common adverse events during the study were nausea, constipation, and abdominal pain. Rates of treatment discontinuation were higher among patients taking both doses of active drug than among those taking placebo.
IBS symptoms did not worsen appreciably during the withdrawal period or for 2 weeks of follow-up after treatment ended.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: The new drug eluxadoline improved symptoms of IBS with diarrhea in two manufacturer-sponsored phase III trials.
Major finding: The primary endpoint – a reduction of at least 30% in abdominal pain and improved stool-consistency scores – was reached in a significantly greater proportion of patients taking 75-mg eluxadoline (23.4%) or 100-mg eluxadoline (29.3%) than placebo (19.0%) in the first trial.
Data source: Two randomized double-blind placebo-controlled phase III trials involving 2,428 patients followed for up to 1 year.
Disclosures: These trials were sponsored by Furiex Pharmaceuticals, an affiliate of Allergan. Dr. Lembo reported being paid to serve on advisory boards for Allergan, Furiex, Prometheus Laboratories, Salix, Valeant, Forest Laboratories, Alkermes, AstraZeneca, and Ironwood; his associates reported ties to numerous industry sources.
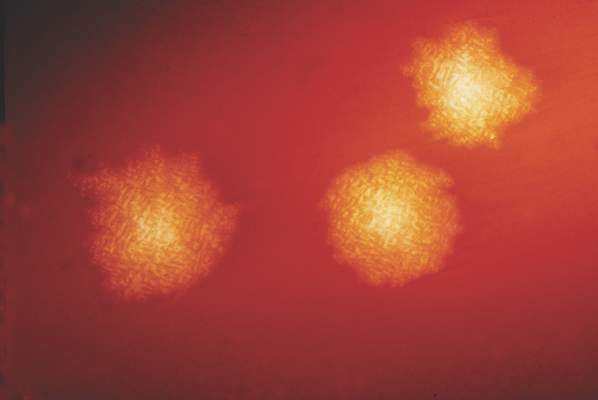
Sirolimus reduced posttransplant skin cancer risk
Sirolimus protects organ-transplant recipients against developing skin cancer, reducing their risk by 40%, according to a retrospective cohort study published in JAMA Dermatology on Jan. 20.
Recipients of solid organs are at three- to fourfold higher risk of developing cancer, compared with the general population, and the most common type they get is nonmelanoma skin cancer. The risk of developing cutaneous squamous cell carcinoma is 65-250 times higher in organ-transplant recipients. Drugs that reduce the growth and proliferation of tumor cells by inhibiting mTOR (mammalian target of rapamycin), including sirolimus, are believed to reduce this cancer risk, said Pritesh S. Karia of the department of dermatology, Brigham and Women’s Hospital and Harvard University, Boston, and his associates (JAMA Dermatol. 2016 Jan 20. doi: 10.1001/jamadermatol.2015.5548).
The investigators reviewed the electronic medical records of 329 patients (mean age, 56 years) who underwent organ transplantation at one of the two medical centers during a 9-year period and who then developed a cancer of any type. The study participants received renal (53.8%), heart (17.6%), lung (16.4%), liver (10.3%), or mixed-organ (1.8%) transplants. The most common index cancers they developed post transplant included cutaneous squamous cell carcinoma (31.9%), basal cell carcinoma (22.5%), and melanoma (2.7%).
Of the 329 patients, 97 (29.5%) then received sirolimus, while 232 (70.5%) did not. During a median follow-up of 38 months, 130 of these patients (39.5%) developed a second posttransplant cancer. The sirolimus-treated group showed a reduction in risk for cancer of any type, compared with the group that did not receive sirolimus (30.9% of 97 vs. 43.1% of 232).
Nearly all (88.5%) of the second posttransplant cancers that developed were skin cancers, and sirolimus reduced the risk of skin cancers by 40%. The 1-year, 3-year, and 5-year rates of skin cancer after an index posttransplant cancer were 9.3%, 20.6%, and 24.7% in the sirolimus group, compared with 17.7%, 31.0%, and 35.8%, respectively, in the untreated group, “thus demonstrating a lower risk for skin cancer with sirolimus treatment,” they said.
“Even for patients who have already had difficulty with skin cancer formation, mTOR inhibition appears to be of benefit. No difference in cancer outcomes was observable between sirolimus-treated and [untreated] groups because poor outcomes were rare,” Mr. Karia and his associates wrote.
These findings suggest that sirolimus chemoprevention should be considered for the subset of organ-transplant recipients who develop post-transplant cancer, they noted. The results also highlight the need for dermatologists and transplant physicians “to be aware of skin cancer history, coordinate regular posttransplant surveillance of skin cancers” in patients with organ transplant recipients, especially those with a history of skin cancer, and to communicate closely “as skin cancers form to consider reduction in immunosuppressive therapy or conversion to an mTOR-based regimen if skin cancer formation is of concern,” they added.
This study was supported by sirolimus manufacturer Novartis Pharmaceuticals. Mr. Karia and his associates reported having no relevant financial disclosures.
Sirolimus protects organ-transplant recipients against developing skin cancer, reducing their risk by 40%, according to a retrospective cohort study published in JAMA Dermatology on Jan. 20.
Recipients of solid organs are at three- to fourfold higher risk of developing cancer, compared with the general population, and the most common type they get is nonmelanoma skin cancer. The risk of developing cutaneous squamous cell carcinoma is 65-250 times higher in organ-transplant recipients. Drugs that reduce the growth and proliferation of tumor cells by inhibiting mTOR (mammalian target of rapamycin), including sirolimus, are believed to reduce this cancer risk, said Pritesh S. Karia of the department of dermatology, Brigham and Women’s Hospital and Harvard University, Boston, and his associates (JAMA Dermatol. 2016 Jan 20. doi: 10.1001/jamadermatol.2015.5548).
The investigators reviewed the electronic medical records of 329 patients (mean age, 56 years) who underwent organ transplantation at one of the two medical centers during a 9-year period and who then developed a cancer of any type. The study participants received renal (53.8%), heart (17.6%), lung (16.4%), liver (10.3%), or mixed-organ (1.8%) transplants. The most common index cancers they developed post transplant included cutaneous squamous cell carcinoma (31.9%), basal cell carcinoma (22.5%), and melanoma (2.7%).
Of the 329 patients, 97 (29.5%) then received sirolimus, while 232 (70.5%) did not. During a median follow-up of 38 months, 130 of these patients (39.5%) developed a second posttransplant cancer. The sirolimus-treated group showed a reduction in risk for cancer of any type, compared with the group that did not receive sirolimus (30.9% of 97 vs. 43.1% of 232).
Nearly all (88.5%) of the second posttransplant cancers that developed were skin cancers, and sirolimus reduced the risk of skin cancers by 40%. The 1-year, 3-year, and 5-year rates of skin cancer after an index posttransplant cancer were 9.3%, 20.6%, and 24.7% in the sirolimus group, compared with 17.7%, 31.0%, and 35.8%, respectively, in the untreated group, “thus demonstrating a lower risk for skin cancer with sirolimus treatment,” they said.
“Even for patients who have already had difficulty with skin cancer formation, mTOR inhibition appears to be of benefit. No difference in cancer outcomes was observable between sirolimus-treated and [untreated] groups because poor outcomes were rare,” Mr. Karia and his associates wrote.
These findings suggest that sirolimus chemoprevention should be considered for the subset of organ-transplant recipients who develop post-transplant cancer, they noted. The results also highlight the need for dermatologists and transplant physicians “to be aware of skin cancer history, coordinate regular posttransplant surveillance of skin cancers” in patients with organ transplant recipients, especially those with a history of skin cancer, and to communicate closely “as skin cancers form to consider reduction in immunosuppressive therapy or conversion to an mTOR-based regimen if skin cancer formation is of concern,” they added.
This study was supported by sirolimus manufacturer Novartis Pharmaceuticals. Mr. Karia and his associates reported having no relevant financial disclosures.
Sirolimus protects organ-transplant recipients against developing skin cancer, reducing their risk by 40%, according to a retrospective cohort study published in JAMA Dermatology on Jan. 20.
Recipients of solid organs are at three- to fourfold higher risk of developing cancer, compared with the general population, and the most common type they get is nonmelanoma skin cancer. The risk of developing cutaneous squamous cell carcinoma is 65-250 times higher in organ-transplant recipients. Drugs that reduce the growth and proliferation of tumor cells by inhibiting mTOR (mammalian target of rapamycin), including sirolimus, are believed to reduce this cancer risk, said Pritesh S. Karia of the department of dermatology, Brigham and Women’s Hospital and Harvard University, Boston, and his associates (JAMA Dermatol. 2016 Jan 20. doi: 10.1001/jamadermatol.2015.5548).
The investigators reviewed the electronic medical records of 329 patients (mean age, 56 years) who underwent organ transplantation at one of the two medical centers during a 9-year period and who then developed a cancer of any type. The study participants received renal (53.8%), heart (17.6%), lung (16.4%), liver (10.3%), or mixed-organ (1.8%) transplants. The most common index cancers they developed post transplant included cutaneous squamous cell carcinoma (31.9%), basal cell carcinoma (22.5%), and melanoma (2.7%).
Of the 329 patients, 97 (29.5%) then received sirolimus, while 232 (70.5%) did not. During a median follow-up of 38 months, 130 of these patients (39.5%) developed a second posttransplant cancer. The sirolimus-treated group showed a reduction in risk for cancer of any type, compared with the group that did not receive sirolimus (30.9% of 97 vs. 43.1% of 232).
Nearly all (88.5%) of the second posttransplant cancers that developed were skin cancers, and sirolimus reduced the risk of skin cancers by 40%. The 1-year, 3-year, and 5-year rates of skin cancer after an index posttransplant cancer were 9.3%, 20.6%, and 24.7% in the sirolimus group, compared with 17.7%, 31.0%, and 35.8%, respectively, in the untreated group, “thus demonstrating a lower risk for skin cancer with sirolimus treatment,” they said.
“Even for patients who have already had difficulty with skin cancer formation, mTOR inhibition appears to be of benefit. No difference in cancer outcomes was observable between sirolimus-treated and [untreated] groups because poor outcomes were rare,” Mr. Karia and his associates wrote.
These findings suggest that sirolimus chemoprevention should be considered for the subset of organ-transplant recipients who develop post-transplant cancer, they noted. The results also highlight the need for dermatologists and transplant physicians “to be aware of skin cancer history, coordinate regular posttransplant surveillance of skin cancers” in patients with organ transplant recipients, especially those with a history of skin cancer, and to communicate closely “as skin cancers form to consider reduction in immunosuppressive therapy or conversion to an mTOR-based regimen if skin cancer formation is of concern,” they added.
This study was supported by sirolimus manufacturer Novartis Pharmaceuticals. Mr. Karia and his associates reported having no relevant financial disclosures.
FROM JAMA DERMATOLOGY
Key clinical point: Sirolimus protects organ-transplant recipients against skin cancer.
Major finding: The 1-year, 3-year, and 5-year rates of skin cancer after an index posttransplant cancer were 9.3%, 20.6%, and 24.7% in the sirolimus group, compared with 17.7%, 31.0%, and 35.8% in the untreated group.
Data source: A retrospective cohort study of 329 organ-transplant recipients who had already developed one cancer likely related to their immunosuppressive therapy.
Disclosures: This study was supported by sirolimus manufacturer Novartis Pharmaceuticals. Mr. Karia and his associates reported having no relevant financial disclosures.
Adjuvant therapy extends survival in early SCLC
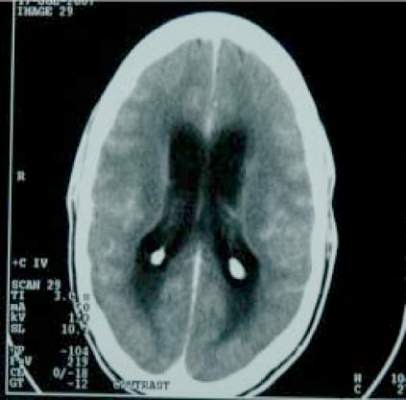
Surgical resection followed by adjuvant chemotherapy, with or without prophylactic cranial irradiation, extends overall survival beyond that achieved with surgery alone in early-stage small-cell lung cancer, according to a report published online Jan. 18 in Journal of Clinical Oncology.
National Comprehensive Cancer Network guidelines recommend surgery with adjuvant chemotherapy for patients with stage I SCLC, and also recommend prophylactic cranial irradiation. But these recommendations are based on “limited” data, and the roles of both adjuvant chemotherapy and irradiation for this patient population are “not yet well characterized,” said Dr. Chi-Fu Jeffrey Yang of Duke University Medical Center, Durham, N.C., and his associates.
In what they described as the first population-based study to assess adjuvant therapy in such patients, the investigators analyzed information in the National Cancer Database concerning 954 patients treated across the country during 2003-2011. A total of 566 patients (59.3%) received adjuvant chemotherapy and the remaining 388 did not. A total of 190 patients who received adjuvant chemotherapy also had prophylactic radiotherapy to the brain (99 patients), the lung (87 patients), or to an unrecorded site (4 patients).
The median follow-up for the entire cohort was 43 months. Overall median survival time was 55.6 months, and 5-year survival was 47.4%.
Compared with no adjuvant therapy, treatment with adjuvant chemotherapy, with or without radiotherapy, significantly extended both overall survival (66.0 months vs 42.1 months) and the 5-year overall survival rate (52.7% vs 40.4%) in the primary analysis of the study. After the data were adjusted to account for multiple confounding variables, the use of adjuvant chemotherapy alone and of adjuvant chemotherapy plus radiotherapy both were associated with improved survival, Dr. Yang and his associates said (J Clin Oncol. 2016 Jan. 18. doi:10.1200/jco.2015.63.8171).
In contrast, adjuvant chemotherapy with thoracic irradiation and thoracic irradiation alone were not associated with improved survival. However, it is possible that this study was affected by selection bias in that patients who received both chemotherapy and cranial irradiation may have been healthier than those who did not. The researchers attempted to control for possible bias in the multivariable analysis, but further assessment in prospective randomized clinical trials is warranted, they added.
Surgical resection followed by adjuvant chemotherapy, with or without prophylactic cranial irradiation, extends overall survival beyond that achieved with surgery alone in early-stage small-cell lung cancer, according to a report published online Jan. 18 in Journal of Clinical Oncology.
National Comprehensive Cancer Network guidelines recommend surgery with adjuvant chemotherapy for patients with stage I SCLC, and also recommend prophylactic cranial irradiation. But these recommendations are based on “limited” data, and the roles of both adjuvant chemotherapy and irradiation for this patient population are “not yet well characterized,” said Dr. Chi-Fu Jeffrey Yang of Duke University Medical Center, Durham, N.C., and his associates.
In what they described as the first population-based study to assess adjuvant therapy in such patients, the investigators analyzed information in the National Cancer Database concerning 954 patients treated across the country during 2003-2011. A total of 566 patients (59.3%) received adjuvant chemotherapy and the remaining 388 did not. A total of 190 patients who received adjuvant chemotherapy also had prophylactic radiotherapy to the brain (99 patients), the lung (87 patients), or to an unrecorded site (4 patients).
The median follow-up for the entire cohort was 43 months. Overall median survival time was 55.6 months, and 5-year survival was 47.4%.
Compared with no adjuvant therapy, treatment with adjuvant chemotherapy, with or without radiotherapy, significantly extended both overall survival (66.0 months vs 42.1 months) and the 5-year overall survival rate (52.7% vs 40.4%) in the primary analysis of the study. After the data were adjusted to account for multiple confounding variables, the use of adjuvant chemotherapy alone and of adjuvant chemotherapy plus radiotherapy both were associated with improved survival, Dr. Yang and his associates said (J Clin Oncol. 2016 Jan. 18. doi:10.1200/jco.2015.63.8171).
In contrast, adjuvant chemotherapy with thoracic irradiation and thoracic irradiation alone were not associated with improved survival. However, it is possible that this study was affected by selection bias in that patients who received both chemotherapy and cranial irradiation may have been healthier than those who did not. The researchers attempted to control for possible bias in the multivariable analysis, but further assessment in prospective randomized clinical trials is warranted, they added.
Surgical resection followed by adjuvant chemotherapy, with or without prophylactic cranial irradiation, extends overall survival beyond that achieved with surgery alone in early-stage small-cell lung cancer, according to a report published online Jan. 18 in Journal of Clinical Oncology.
National Comprehensive Cancer Network guidelines recommend surgery with adjuvant chemotherapy for patients with stage I SCLC, and also recommend prophylactic cranial irradiation. But these recommendations are based on “limited” data, and the roles of both adjuvant chemotherapy and irradiation for this patient population are “not yet well characterized,” said Dr. Chi-Fu Jeffrey Yang of Duke University Medical Center, Durham, N.C., and his associates.
In what they described as the first population-based study to assess adjuvant therapy in such patients, the investigators analyzed information in the National Cancer Database concerning 954 patients treated across the country during 2003-2011. A total of 566 patients (59.3%) received adjuvant chemotherapy and the remaining 388 did not. A total of 190 patients who received adjuvant chemotherapy also had prophylactic radiotherapy to the brain (99 patients), the lung (87 patients), or to an unrecorded site (4 patients).
The median follow-up for the entire cohort was 43 months. Overall median survival time was 55.6 months, and 5-year survival was 47.4%.
Compared with no adjuvant therapy, treatment with adjuvant chemotherapy, with or without radiotherapy, significantly extended both overall survival (66.0 months vs 42.1 months) and the 5-year overall survival rate (52.7% vs 40.4%) in the primary analysis of the study. After the data were adjusted to account for multiple confounding variables, the use of adjuvant chemotherapy alone and of adjuvant chemotherapy plus radiotherapy both were associated with improved survival, Dr. Yang and his associates said (J Clin Oncol. 2016 Jan. 18. doi:10.1200/jco.2015.63.8171).
In contrast, adjuvant chemotherapy with thoracic irradiation and thoracic irradiation alone were not associated with improved survival. However, it is possible that this study was affected by selection bias in that patients who received both chemotherapy and cranial irradiation may have been healthier than those who did not. The researchers attempted to control for possible bias in the multivariable analysis, but further assessment in prospective randomized clinical trials is warranted, they added.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Surgical resection followed by adjuvant chemotherapy, with or without prophylactic cranial irradiation, extends overall survival in early-stage small-cell lung cancer.
Major finding: Compared with no adjuvant therapy, treatment with adjuvant chemotherapy, with or without radiotherapy, significantly extended overall survival (66.0 months vs 42.1 months).
Data source: A retrospective analysis of information in the National Cancer Database concerning 954 patients treated during 2003-2011 and followed up for a median of 43 months.
Disclosures: The National Institutes of Health Cardiothoracic Surgical Trials Network and the American College of Surgeons Resident Research Scholarship supported the study. Dr. Yang had no financial relationships to disclose.
Adjuvant chemotherapy boosts survival for patients with locally advanced bladder cancer
Adjuvant chemotherapy improves survival in patients with locally advanced bladder cancer who did not receive the neoadjuvant chemotherapy that is currently advocated by some experts, according to a report published online Jan. 18 in Journal of Clinical Oncology.
Two large randomized clinical trials and one meta-analysis demonstrated a survival advantage for patients who received neoadjuvant cisplatin-based chemotherapy, but three subsequent trials attempting to confirm those results were unable to do so: all three were terminated early because of poor accrual of study participants. At present, 1%-15% of eligible U.S. patients with muscle-invasive bladder cancer receive neoadjuvant chemotherapy. Clinicians favor adjuvant chemotherapy instead, “likely because of theoretic concerns regarding delaying potentially curative surgery and the ability to base treatment decisions on more precise pathologic, rather than clinical, staging,” said Dr. Matthew D. Galsky of Tisch Cancer Institute, Mount Sinai, N.Y., and his associates.
To further examine this issue, they analyzed information in the National Cancer Database, a registry that collects deidentified patient-level data from more than 1,500 U.S. hospitals with accredited cancer programs, which represents approximately 70% of all newly diagnosed cases across the country. For this observational study, the investigators focused on 5,653 patients who underwent radical cystectomy for urothelial bladder cancer during a 3-year period and who were found to have pathologic T3-4 and/or nodal involvement at surgery. A total of 1,293 patients (23%) then received multiagent chemotherapy while the remainder received no chemotherapy. All the patients were followed for a median of 7 years.
Compared with patients who did not receive adjuvant chemotherapy, those who did tended to be younger, have a higher income, have fewer comorbidities, and have positive surgical margins. The data were adjusted to account for these and other differences between the two study groups by using propensity-score matching.
Five-year overall survival was 37.0% with adjuvant chemotherapy and 29.1% without it, a significant difference favoring the treatment. In a further analysis, chemotherapy was associated with improved overall survival with an HR of 0.70. This survival benefit was strong across all subgroups of patients regardless of patient age, performance status, lymph node status, and a variety of other factors, and it remained robust in sensitivity analyses, Dr. Galsky and his associates said (J Clin Oncol. 2016 Jan. 18. doi:10.1200/JCO.2015.64.1076).
These findings “provide important information for facilitating treatment decisions.” Neoadjuvant chemotherapy followed by cystectomy remains the preferred approach, but for patients who don’t receive that, postcystectomy chemotherapy may still improve survival, they said.
Galsky et al. provide compelling evidence to support adjuvant chemotherapy for advanced bladder cancer, and their data will likely make the recommendation for the treatment more emphatic.
However, there are a few caveats. The data do not provide specifics about the chemotherapy these patients received: Was it cisplatin based? What was the number of doses given, and what was the dose intensity? There also is no information about recurrences or subsequent salvage therapies in the control group. And although the investigators took great care to control for imbalances between the two study groups, the possibility that these factors may have affected the final outcomes cannot be ruled out completely.
Dr. Sumanta K. Pal is a medical oncologist at the City of Hope Comprehensive Cancer Center, Duarte, Calif. He reported ties to Novartis, Medivation, Astellas Pharma, Pfizer, Novartis, AVEO Pharmaceuticals, Myriad Pharmaceuticals, and Genentech. Dr. Pal and his associates made these remarks in an editorial (J Clin Oncol. 2016 Jan. 18. doi:10.1200/JCO.2015.65.4368).
Galsky et al. provide compelling evidence to support adjuvant chemotherapy for advanced bladder cancer, and their data will likely make the recommendation for the treatment more emphatic.
However, there are a few caveats. The data do not provide specifics about the chemotherapy these patients received: Was it cisplatin based? What was the number of doses given, and what was the dose intensity? There also is no information about recurrences or subsequent salvage therapies in the control group. And although the investigators took great care to control for imbalances between the two study groups, the possibility that these factors may have affected the final outcomes cannot be ruled out completely.
Dr. Sumanta K. Pal is a medical oncologist at the City of Hope Comprehensive Cancer Center, Duarte, Calif. He reported ties to Novartis, Medivation, Astellas Pharma, Pfizer, Novartis, AVEO Pharmaceuticals, Myriad Pharmaceuticals, and Genentech. Dr. Pal and his associates made these remarks in an editorial (J Clin Oncol. 2016 Jan. 18. doi:10.1200/JCO.2015.65.4368).
Galsky et al. provide compelling evidence to support adjuvant chemotherapy for advanced bladder cancer, and their data will likely make the recommendation for the treatment more emphatic.
However, there are a few caveats. The data do not provide specifics about the chemotherapy these patients received: Was it cisplatin based? What was the number of doses given, and what was the dose intensity? There also is no information about recurrences or subsequent salvage therapies in the control group. And although the investigators took great care to control for imbalances between the two study groups, the possibility that these factors may have affected the final outcomes cannot be ruled out completely.
Dr. Sumanta K. Pal is a medical oncologist at the City of Hope Comprehensive Cancer Center, Duarte, Calif. He reported ties to Novartis, Medivation, Astellas Pharma, Pfizer, Novartis, AVEO Pharmaceuticals, Myriad Pharmaceuticals, and Genentech. Dr. Pal and his associates made these remarks in an editorial (J Clin Oncol. 2016 Jan. 18. doi:10.1200/JCO.2015.65.4368).
Adjuvant chemotherapy improves survival in patients with locally advanced bladder cancer who did not receive the neoadjuvant chemotherapy that is currently advocated by some experts, according to a report published online Jan. 18 in Journal of Clinical Oncology.
Two large randomized clinical trials and one meta-analysis demonstrated a survival advantage for patients who received neoadjuvant cisplatin-based chemotherapy, but three subsequent trials attempting to confirm those results were unable to do so: all three were terminated early because of poor accrual of study participants. At present, 1%-15% of eligible U.S. patients with muscle-invasive bladder cancer receive neoadjuvant chemotherapy. Clinicians favor adjuvant chemotherapy instead, “likely because of theoretic concerns regarding delaying potentially curative surgery and the ability to base treatment decisions on more precise pathologic, rather than clinical, staging,” said Dr. Matthew D. Galsky of Tisch Cancer Institute, Mount Sinai, N.Y., and his associates.
To further examine this issue, they analyzed information in the National Cancer Database, a registry that collects deidentified patient-level data from more than 1,500 U.S. hospitals with accredited cancer programs, which represents approximately 70% of all newly diagnosed cases across the country. For this observational study, the investigators focused on 5,653 patients who underwent radical cystectomy for urothelial bladder cancer during a 3-year period and who were found to have pathologic T3-4 and/or nodal involvement at surgery. A total of 1,293 patients (23%) then received multiagent chemotherapy while the remainder received no chemotherapy. All the patients were followed for a median of 7 years.
Compared with patients who did not receive adjuvant chemotherapy, those who did tended to be younger, have a higher income, have fewer comorbidities, and have positive surgical margins. The data were adjusted to account for these and other differences between the two study groups by using propensity-score matching.
Five-year overall survival was 37.0% with adjuvant chemotherapy and 29.1% without it, a significant difference favoring the treatment. In a further analysis, chemotherapy was associated with improved overall survival with an HR of 0.70. This survival benefit was strong across all subgroups of patients regardless of patient age, performance status, lymph node status, and a variety of other factors, and it remained robust in sensitivity analyses, Dr. Galsky and his associates said (J Clin Oncol. 2016 Jan. 18. doi:10.1200/JCO.2015.64.1076).
These findings “provide important information for facilitating treatment decisions.” Neoadjuvant chemotherapy followed by cystectomy remains the preferred approach, but for patients who don’t receive that, postcystectomy chemotherapy may still improve survival, they said.
Adjuvant chemotherapy improves survival in patients with locally advanced bladder cancer who did not receive the neoadjuvant chemotherapy that is currently advocated by some experts, according to a report published online Jan. 18 in Journal of Clinical Oncology.
Two large randomized clinical trials and one meta-analysis demonstrated a survival advantage for patients who received neoadjuvant cisplatin-based chemotherapy, but three subsequent trials attempting to confirm those results were unable to do so: all three were terminated early because of poor accrual of study participants. At present, 1%-15% of eligible U.S. patients with muscle-invasive bladder cancer receive neoadjuvant chemotherapy. Clinicians favor adjuvant chemotherapy instead, “likely because of theoretic concerns regarding delaying potentially curative surgery and the ability to base treatment decisions on more precise pathologic, rather than clinical, staging,” said Dr. Matthew D. Galsky of Tisch Cancer Institute, Mount Sinai, N.Y., and his associates.
To further examine this issue, they analyzed information in the National Cancer Database, a registry that collects deidentified patient-level data from more than 1,500 U.S. hospitals with accredited cancer programs, which represents approximately 70% of all newly diagnosed cases across the country. For this observational study, the investigators focused on 5,653 patients who underwent radical cystectomy for urothelial bladder cancer during a 3-year period and who were found to have pathologic T3-4 and/or nodal involvement at surgery. A total of 1,293 patients (23%) then received multiagent chemotherapy while the remainder received no chemotherapy. All the patients were followed for a median of 7 years.
Compared with patients who did not receive adjuvant chemotherapy, those who did tended to be younger, have a higher income, have fewer comorbidities, and have positive surgical margins. The data were adjusted to account for these and other differences between the two study groups by using propensity-score matching.
Five-year overall survival was 37.0% with adjuvant chemotherapy and 29.1% without it, a significant difference favoring the treatment. In a further analysis, chemotherapy was associated with improved overall survival with an HR of 0.70. This survival benefit was strong across all subgroups of patients regardless of patient age, performance status, lymph node status, and a variety of other factors, and it remained robust in sensitivity analyses, Dr. Galsky and his associates said (J Clin Oncol. 2016 Jan. 18. doi:10.1200/JCO.2015.64.1076).
These findings “provide important information for facilitating treatment decisions.” Neoadjuvant chemotherapy followed by cystectomy remains the preferred approach, but for patients who don’t receive that, postcystectomy chemotherapy may still improve survival, they said.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Adjuvant chemotherapy improves survival in patients with locally advanced bladder cancer who did not receive the neoadjuvant chemotherapy that is currently advocated.
Major finding: Five-year overall survival was 37.0% with adjuvant chemotherapy and 29.1% without it.
Data source: A propensity-matched observational cohort study involving 5,653 cases in a national cancer database followed for approximately 7 years.
Disclosures: This study was supported by a Clinical and Translational Science KL2 Faculty Scholars Award. Dr. Galsky reported ties to Dual Therapeutics, BioMotive, Janssen Oncology, Dendreon, Merck, GlaxoSmithKline, Eli Lilly, Astellas Pharma, Genentech, Novartis, and Bristol-Myers Squibb.
Patient isolation key to containing in-hospital norovirus
Patient isolation in their own rooms is the most important factor in controlling outbreaks of norovirus within hospitals, according to a report in the Journal of Infectious Diseases.
Investigators surveyed six London hospitals for a 3-month period to gather data concerning norovirus outbreaks. They assessed two teaching hospitals with 230 and 780 beds, respectively; one specialist center with 160 beds; two district general hospitals with 284 and 650 beds, respectively; and one 100-bed community hospital. There were 20 norovirus outbreaks during the survey period involving 57 patients and 7 staff members, said Martina Cummins, a nurse consultant and deputy director, Infection Prevention and Control, Bart’s Health NHS Trust, Ilford (England) and Derren Ready, a clinical scientist at Public Health England, London.
The number of outbreaks varied markedly among the different hospitals. The smaller teaching hospital and the smaller district general hospital had zero outbreaks, while the specialist hospital and the community hospital had only one outbreak each involving only three and six patients, respectively. The larger teaching hospital had two outbreaks involving only four patients in total. In contrast, the larger district general hospital, which had an older infrastructure, had 16 separate outbreaks involving 44 patients, and it was the only facility in which staff members (7) also became ill.
The ability to control an outbreak of norovirus hinged on the availability of isolation rooms. All the hospitals with two or fewer outbreaks had easily available isolation rooms, while the hospital that had numerous outbreaks did not. The most severely affected hospital had large wards caring for up to 26 patients, with limited or no barriers between beds. The beds in these wards were closer together (within 2.3 meters) than those in all the other hospitals. In addition, this hospital had limited care facilities, including only two sinks per ward for staff members to use and only four shared toilets per ward, Ms. Cummins and Mr. Ready said (J Infect Dis. 2016;213[S1]:S12-S14. doi:10.1093/infdis/jiv529).
Norovirus outbreaks among patients can have a major impact on the affected departments, wards, or clinical areas, but those that extend to staff members can lead to severe staffing shortages that close down whole wards or even entire hospitals, they noted.
No sponsor or funding source was identified for this study. Ms. Cummins and Mr. Ready reported having no relevant financial disclosures.
Patient isolation in their own rooms is the most important factor in controlling outbreaks of norovirus within hospitals, according to a report in the Journal of Infectious Diseases.
Investigators surveyed six London hospitals for a 3-month period to gather data concerning norovirus outbreaks. They assessed two teaching hospitals with 230 and 780 beds, respectively; one specialist center with 160 beds; two district general hospitals with 284 and 650 beds, respectively; and one 100-bed community hospital. There were 20 norovirus outbreaks during the survey period involving 57 patients and 7 staff members, said Martina Cummins, a nurse consultant and deputy director, Infection Prevention and Control, Bart’s Health NHS Trust, Ilford (England) and Derren Ready, a clinical scientist at Public Health England, London.
The number of outbreaks varied markedly among the different hospitals. The smaller teaching hospital and the smaller district general hospital had zero outbreaks, while the specialist hospital and the community hospital had only one outbreak each involving only three and six patients, respectively. The larger teaching hospital had two outbreaks involving only four patients in total. In contrast, the larger district general hospital, which had an older infrastructure, had 16 separate outbreaks involving 44 patients, and it was the only facility in which staff members (7) also became ill.
The ability to control an outbreak of norovirus hinged on the availability of isolation rooms. All the hospitals with two or fewer outbreaks had easily available isolation rooms, while the hospital that had numerous outbreaks did not. The most severely affected hospital had large wards caring for up to 26 patients, with limited or no barriers between beds. The beds in these wards were closer together (within 2.3 meters) than those in all the other hospitals. In addition, this hospital had limited care facilities, including only two sinks per ward for staff members to use and only four shared toilets per ward, Ms. Cummins and Mr. Ready said (J Infect Dis. 2016;213[S1]:S12-S14. doi:10.1093/infdis/jiv529).
Norovirus outbreaks among patients can have a major impact on the affected departments, wards, or clinical areas, but those that extend to staff members can lead to severe staffing shortages that close down whole wards or even entire hospitals, they noted.
No sponsor or funding source was identified for this study. Ms. Cummins and Mr. Ready reported having no relevant financial disclosures.
Patient isolation in their own rooms is the most important factor in controlling outbreaks of norovirus within hospitals, according to a report in the Journal of Infectious Diseases.
Investigators surveyed six London hospitals for a 3-month period to gather data concerning norovirus outbreaks. They assessed two teaching hospitals with 230 and 780 beds, respectively; one specialist center with 160 beds; two district general hospitals with 284 and 650 beds, respectively; and one 100-bed community hospital. There were 20 norovirus outbreaks during the survey period involving 57 patients and 7 staff members, said Martina Cummins, a nurse consultant and deputy director, Infection Prevention and Control, Bart’s Health NHS Trust, Ilford (England) and Derren Ready, a clinical scientist at Public Health England, London.
The number of outbreaks varied markedly among the different hospitals. The smaller teaching hospital and the smaller district general hospital had zero outbreaks, while the specialist hospital and the community hospital had only one outbreak each involving only three and six patients, respectively. The larger teaching hospital had two outbreaks involving only four patients in total. In contrast, the larger district general hospital, which had an older infrastructure, had 16 separate outbreaks involving 44 patients, and it was the only facility in which staff members (7) also became ill.
The ability to control an outbreak of norovirus hinged on the availability of isolation rooms. All the hospitals with two or fewer outbreaks had easily available isolation rooms, while the hospital that had numerous outbreaks did not. The most severely affected hospital had large wards caring for up to 26 patients, with limited or no barriers between beds. The beds in these wards were closer together (within 2.3 meters) than those in all the other hospitals. In addition, this hospital had limited care facilities, including only two sinks per ward for staff members to use and only four shared toilets per ward, Ms. Cummins and Mr. Ready said (J Infect Dis. 2016;213[S1]:S12-S14. doi:10.1093/infdis/jiv529).
Norovirus outbreaks among patients can have a major impact on the affected departments, wards, or clinical areas, but those that extend to staff members can lead to severe staffing shortages that close down whole wards or even entire hospitals, they noted.
No sponsor or funding source was identified for this study. Ms. Cummins and Mr. Ready reported having no relevant financial disclosures.
FROM THE JOURNAL OF INFECTIOUS DISEASES
Key clinical point: Patient isolation is the key to containing norovirus outbreaks within hospitals.
Major finding: All five hospitals with two or fewer outbreaks had easily available isolation rooms, while the one hospital that had 16 outbreaks did not.
Data source: An enhanced surveillance study of six London hospitals that had 20 norovirus outbreaks involving 57 patients and 7 staff members during a 3-month period.
Disclosures: No sponsor or funding source was identified for this study. Ms. Cummins and Mr. Ready reported having no relevant financial disclosures.
Bronchoscopic nitinol coils improve severe emphysema
Bronchoscopically placed nitinol coils to reduce lung volume markedly improved quality of life and modestly improved walk distance and lung function in a preliminary study of patients with severe emphysema, which was published online Jan. 12 in JAMA.
The magnitude and severity of serious and nonserious adverse effects were far less than has been reported for more invasive lung volume reduction surgery in this patient population. However, the short-term financial costs of coil placement were substantial, said Dr. Gaetan Deslee of University of Reims (France) Hospital and his associates.
Nitinol coils are shape-memory devices delivered into subsegmental airways to reduce regional parenchymal volume, which increases expansion of adjacent nontargeted lung. This increases the nontargeted tissue’s elastic recoil and reestablishes small-airway tethering, which improves expiratory flow and reduces air trapping.
The investigators compared this procedure against usual care in 100 patients with severe emphysema who were treated and followed for 1 year at 10 university hospitals across France. Both groups underwent pretreatment pulmonary rehabilitation and received inhaled bronchodilators with or without inhaled corticosteroids and with or without supplemental oxygen at the discretion of their treating physicians. Then patients were randomly assigned – 50 to receive the coils and 50 to receive usual care.
The coils were inserted under general anesthesia, and approximately 10 coils were placed per targeted lobe. Most patients later underwent the procedure on the opposite side, so that 47 patients received bilateral and 3 received unilateral coils during 97 bronchoscopies. The mean procedure time was 54 minutes, and the treatment significantly decreased lung hyperinflation.
The primary efficacy endpoint, improvement in 6-minute walk test scores after 6 months, was evaluable for 44 patients in each study group. A total of 18 patients (36%) who underwent coil placement and 9 (18%) who received usual care improved their scores by at least 54 m, which was a significant difference, the investigators said (JAMA. 2016 Jan 12. doi: 10.1001/jama.2015.17821).
In addition, all secondary endpoints were significantly better after coil placement than after usual care at both 6 months and 12 months. This included forced expiratory volume in 1 second, forced vital capacity, residual volume, and residual volume/total lung capacity, scores on the Medical Research Council dyspnea scale, and scores on a measure of health-related quality of life.
A cost-benefit analysis at 1 year showed that the mean increase in expenditures was $47,908 per person in the coil group, compared with the usual-care group. The 1-year incremental cost-effectiveness ratio was $782,598 per quality-adjusted life year (QALY). Assuming that the quality of life gains would be maintained over 3 years and that the costs of follow-up care would be identically low in both study groups, this ratio would decrease to $270,000 per QALY at 3 years.
However, neither of these cost-effectiveness ratios would be considered economical enough to warrant adopting this technology in most countries, Dr. Deslee and his associates noted.
At least one serious adverse event developed in 52% of the coil group and in 38% of the usual-care group, and there were four deaths (8%) in the coil group and three deaths (6%) in the usual-care group. The most frequent adverse event was pneumonia, which resolved with medical care in all cases. “The mechanism involved in pneumonia may result from local airway irritation, subsegmental airway closure, tension-induced inflammation, or local ischemia rather than from an infectious mechanism,” the researchers said.
This study was limited in that coil placement was not compared with either a sham or control procedure, patients were not blinded to treatment assignment, the sample size was relatively small, and follow-up was short. Larger studies using more rigorous statistical methods are needed “to draw a definitive conclusion regarding the long-term efficacy of coil treatment,” they added.
The improvement in health-related quality of life scores in this study represents a mean response of approximately three times the established minimal clinically important difference. By comparison, trials of pharmacologic interventions rarely achieve even the minimal clinically important difference.
Despite the high cost-effectiveness ratio of more than $700,000 per QALY – when ratios of $50,000 to $100,000 per QALY are commonly deemed to be the maximal acceptable limit – clinicians shouldn’t hesitate to use this treatment if these findings are confirmed in larger trials. Bronchoscopically placed nitinol coils are largely palliative, but the response is meaningful and offers realistic hope to patients who have few other treatment choices.
Dr. Frank C. Sciurba, Dr. Divay Chandra, and Dr. Jessica Bon are all in the division of pulmonary, allergy, and critical care medicine at the University of Pittsburgh. Dr. Sciurba reported receiving grants from PneumRX, maker of the coils used in this study, and PulmonX. Dr. Sciurba, Dr. Chandra, and Dr. Bon made these remarks in an editorial accompanying Dr. Deslee’s report (JAMA 2016;315:139-41).
The improvement in health-related quality of life scores in this study represents a mean response of approximately three times the established minimal clinically important difference. By comparison, trials of pharmacologic interventions rarely achieve even the minimal clinically important difference.
Despite the high cost-effectiveness ratio of more than $700,000 per QALY – when ratios of $50,000 to $100,000 per QALY are commonly deemed to be the maximal acceptable limit – clinicians shouldn’t hesitate to use this treatment if these findings are confirmed in larger trials. Bronchoscopically placed nitinol coils are largely palliative, but the response is meaningful and offers realistic hope to patients who have few other treatment choices.
Dr. Frank C. Sciurba, Dr. Divay Chandra, and Dr. Jessica Bon are all in the division of pulmonary, allergy, and critical care medicine at the University of Pittsburgh. Dr. Sciurba reported receiving grants from PneumRX, maker of the coils used in this study, and PulmonX. Dr. Sciurba, Dr. Chandra, and Dr. Bon made these remarks in an editorial accompanying Dr. Deslee’s report (JAMA 2016;315:139-41).
The improvement in health-related quality of life scores in this study represents a mean response of approximately three times the established minimal clinically important difference. By comparison, trials of pharmacologic interventions rarely achieve even the minimal clinically important difference.
Despite the high cost-effectiveness ratio of more than $700,000 per QALY – when ratios of $50,000 to $100,000 per QALY are commonly deemed to be the maximal acceptable limit – clinicians shouldn’t hesitate to use this treatment if these findings are confirmed in larger trials. Bronchoscopically placed nitinol coils are largely palliative, but the response is meaningful and offers realistic hope to patients who have few other treatment choices.
Dr. Frank C. Sciurba, Dr. Divay Chandra, and Dr. Jessica Bon are all in the division of pulmonary, allergy, and critical care medicine at the University of Pittsburgh. Dr. Sciurba reported receiving grants from PneumRX, maker of the coils used in this study, and PulmonX. Dr. Sciurba, Dr. Chandra, and Dr. Bon made these remarks in an editorial accompanying Dr. Deslee’s report (JAMA 2016;315:139-41).
Bronchoscopically placed nitinol coils to reduce lung volume markedly improved quality of life and modestly improved walk distance and lung function in a preliminary study of patients with severe emphysema, which was published online Jan. 12 in JAMA.
The magnitude and severity of serious and nonserious adverse effects were far less than has been reported for more invasive lung volume reduction surgery in this patient population. However, the short-term financial costs of coil placement were substantial, said Dr. Gaetan Deslee of University of Reims (France) Hospital and his associates.
Nitinol coils are shape-memory devices delivered into subsegmental airways to reduce regional parenchymal volume, which increases expansion of adjacent nontargeted lung. This increases the nontargeted tissue’s elastic recoil and reestablishes small-airway tethering, which improves expiratory flow and reduces air trapping.
The investigators compared this procedure against usual care in 100 patients with severe emphysema who were treated and followed for 1 year at 10 university hospitals across France. Both groups underwent pretreatment pulmonary rehabilitation and received inhaled bronchodilators with or without inhaled corticosteroids and with or without supplemental oxygen at the discretion of their treating physicians. Then patients were randomly assigned – 50 to receive the coils and 50 to receive usual care.
The coils were inserted under general anesthesia, and approximately 10 coils were placed per targeted lobe. Most patients later underwent the procedure on the opposite side, so that 47 patients received bilateral and 3 received unilateral coils during 97 bronchoscopies. The mean procedure time was 54 minutes, and the treatment significantly decreased lung hyperinflation.
The primary efficacy endpoint, improvement in 6-minute walk test scores after 6 months, was evaluable for 44 patients in each study group. A total of 18 patients (36%) who underwent coil placement and 9 (18%) who received usual care improved their scores by at least 54 m, which was a significant difference, the investigators said (JAMA. 2016 Jan 12. doi: 10.1001/jama.2015.17821).
In addition, all secondary endpoints were significantly better after coil placement than after usual care at both 6 months and 12 months. This included forced expiratory volume in 1 second, forced vital capacity, residual volume, and residual volume/total lung capacity, scores on the Medical Research Council dyspnea scale, and scores on a measure of health-related quality of life.
A cost-benefit analysis at 1 year showed that the mean increase in expenditures was $47,908 per person in the coil group, compared with the usual-care group. The 1-year incremental cost-effectiveness ratio was $782,598 per quality-adjusted life year (QALY). Assuming that the quality of life gains would be maintained over 3 years and that the costs of follow-up care would be identically low in both study groups, this ratio would decrease to $270,000 per QALY at 3 years.
However, neither of these cost-effectiveness ratios would be considered economical enough to warrant adopting this technology in most countries, Dr. Deslee and his associates noted.
At least one serious adverse event developed in 52% of the coil group and in 38% of the usual-care group, and there were four deaths (8%) in the coil group and three deaths (6%) in the usual-care group. The most frequent adverse event was pneumonia, which resolved with medical care in all cases. “The mechanism involved in pneumonia may result from local airway irritation, subsegmental airway closure, tension-induced inflammation, or local ischemia rather than from an infectious mechanism,” the researchers said.
This study was limited in that coil placement was not compared with either a sham or control procedure, patients were not blinded to treatment assignment, the sample size was relatively small, and follow-up was short. Larger studies using more rigorous statistical methods are needed “to draw a definitive conclusion regarding the long-term efficacy of coil treatment,” they added.
Bronchoscopically placed nitinol coils to reduce lung volume markedly improved quality of life and modestly improved walk distance and lung function in a preliminary study of patients with severe emphysema, which was published online Jan. 12 in JAMA.
The magnitude and severity of serious and nonserious adverse effects were far less than has been reported for more invasive lung volume reduction surgery in this patient population. However, the short-term financial costs of coil placement were substantial, said Dr. Gaetan Deslee of University of Reims (France) Hospital and his associates.
Nitinol coils are shape-memory devices delivered into subsegmental airways to reduce regional parenchymal volume, which increases expansion of adjacent nontargeted lung. This increases the nontargeted tissue’s elastic recoil and reestablishes small-airway tethering, which improves expiratory flow and reduces air trapping.
The investigators compared this procedure against usual care in 100 patients with severe emphysema who were treated and followed for 1 year at 10 university hospitals across France. Both groups underwent pretreatment pulmonary rehabilitation and received inhaled bronchodilators with or without inhaled corticosteroids and with or without supplemental oxygen at the discretion of their treating physicians. Then patients were randomly assigned – 50 to receive the coils and 50 to receive usual care.
The coils were inserted under general anesthesia, and approximately 10 coils were placed per targeted lobe. Most patients later underwent the procedure on the opposite side, so that 47 patients received bilateral and 3 received unilateral coils during 97 bronchoscopies. The mean procedure time was 54 minutes, and the treatment significantly decreased lung hyperinflation.
The primary efficacy endpoint, improvement in 6-minute walk test scores after 6 months, was evaluable for 44 patients in each study group. A total of 18 patients (36%) who underwent coil placement and 9 (18%) who received usual care improved their scores by at least 54 m, which was a significant difference, the investigators said (JAMA. 2016 Jan 12. doi: 10.1001/jama.2015.17821).
In addition, all secondary endpoints were significantly better after coil placement than after usual care at both 6 months and 12 months. This included forced expiratory volume in 1 second, forced vital capacity, residual volume, and residual volume/total lung capacity, scores on the Medical Research Council dyspnea scale, and scores on a measure of health-related quality of life.
A cost-benefit analysis at 1 year showed that the mean increase in expenditures was $47,908 per person in the coil group, compared with the usual-care group. The 1-year incremental cost-effectiveness ratio was $782,598 per quality-adjusted life year (QALY). Assuming that the quality of life gains would be maintained over 3 years and that the costs of follow-up care would be identically low in both study groups, this ratio would decrease to $270,000 per QALY at 3 years.
However, neither of these cost-effectiveness ratios would be considered economical enough to warrant adopting this technology in most countries, Dr. Deslee and his associates noted.
At least one serious adverse event developed in 52% of the coil group and in 38% of the usual-care group, and there were four deaths (8%) in the coil group and three deaths (6%) in the usual-care group. The most frequent adverse event was pneumonia, which resolved with medical care in all cases. “The mechanism involved in pneumonia may result from local airway irritation, subsegmental airway closure, tension-induced inflammation, or local ischemia rather than from an infectious mechanism,” the researchers said.
This study was limited in that coil placement was not compared with either a sham or control procedure, patients were not blinded to treatment assignment, the sample size was relatively small, and follow-up was short. Larger studies using more rigorous statistical methods are needed “to draw a definitive conclusion regarding the long-term efficacy of coil treatment,” they added.
FROM JAMA
Key clinical point: Bronchoscopically placed nitinol coils to reduce lung volume markedly improved quality of life and modestly improved walk distance in severe emphysema.
Major finding: 36% of patients who underwent coil placement achieved an improvement of at least 54 m in the 6-minute walk test, compared with only 18% who received usual care.
Data source: A preliminary randomized trial involving 100 patients treated at 10 university hospitals in France and followed for 1 year.
Disclosures: This study was supported by the French Ministry of Health. Dr. Deslee reported ties to PneumRx, maker of the coils tested in this study; his associates reported ties to PneumRx, Novatech, GlaxoSmithKline, Boehringer Ingelheim, Novartis, AstraZeneca, and Pulmonix.
Tuberculous meningitis: Intensified anti-TB therapy not useful
Intensified antituberculosis therapy doesn’t appear to improve survival in adults with tuberculous meningitis, compared with standard treatment, according to a report published online Jan. 14 in the New England Journal of Medicine.
This result, from a 3-year randomized double-blind placebo controlled clinical trial involving 817 adults in Vietnam, contradicts findings from previous small studies which suggested that increasing the rifampin dose and adding a fluoroquinolone to the standard regimen might improve outcomes, said Dr. A. Dorothee Heemskerk of the Oxford University Clinical Research Unit, Ho Chi Minh City, Vietnam, and her associates.
Current guidelines recommend at least 2 months of therapy with four antituberculosis agents, followed by treatment with rifampin (10 mg/kg) and isoniazid for an additional 7-10 months. “However, these recommendations are based on data from pulmonary tuberculosis and do not take into account the differential ability of antituberculosis drugs to penetrate the brain,” the investigators noted.
The concentration of rifampin in cerebrospinal fluid reaches only 30% of that in the plasma, so it has been proposed that higher-dose rifampin (15 mg/kg) might be more effective for tuberculous meningitis. Fluoroquinolones such as levofloxacin were proposed because they are active against tuberculosis and achieve good penetration of the blood-brain barrier.
Dr. Heemskerk and her associates tested this hypothesis at two tertiary referral centers for severe cases of tuberculosis or infectious diseases in Vietnam. All the study participants received standard daily isoniazid (5 mg/kg), rifampin (10 mg/kg), pyrazinamide (25 mg/kg), and ethambutol (20 mg/kg) for 3 months, followed by the same doses of rifampin and isoniazid for an additional 6 months. Approximately half (408 patients in the intensive-therapy group) received additional rifampin (5 mg/kg) and levofloxacin (20 mg/kg), while the other half (409 patients in the control group) received matching placebos.
The median patient age was 35 years. Approximately 43% of patients were coinfected with HIV.
The primary outcome measure – death at 9-month follow-up – occurred in 113 of the intensive-therapy group and 114 of the control group, a nonsignificant difference (HR, 0.94). The intensified treatment was no better than was standard treatment in any subgroup of patients or in any secondary outcomes, including neurologic disability and time to a new neurologic event or death, the investigators said (N Engl J Med. 2016 Jan 14. doi:10.1056/NEJMoa1507062).
However, intensive therapy was associated with a higher frequency of seizures (23 vs. 11 patients), visual impairment (14 vs. 4 patients), allergic reactions (30 patients vs. 17 patients), jaundice (19 vs. 7 patients), grade 3 or 4 hyponatremia (112 patients vs. 81 patients), and adverse events leading to treatment interruptions (95 patients vs. 64 patients).
It is possible that raising the dose of rifampin by only 5 mg/kg may not have increased intracerebral drug concentrations “sufficiently to enhance bacterial killing. Recent data suggest that much higher doses (up to 35 mg/kg per day) may have an acceptable side-effect profile and may be necessary to significantly increase the killing of M. tuberculosis in pulmonary tuberculosis,” Dr. Heemskerk and her associates noted.
“Although the results of our study do not support a change in the currently recommended treatment regimens for tuberculous meningitis, enhanced antituberculosis treatment with higher doses of first-line drugs, including intravenous rifampin, or the newer antituberculosis drugs bedaquiline and delamanid, still require investigation,” they added.
Wellcome Trust and the Li Ka Shing Foundation supported the study. Dr. Heemskerk and her associates reported having no relevant financial disclosures.
These findings are disappointing and suggest that fluoroquinolones are not going to revolutionize the treatment of tuberculous meningitis, even though they may replace isoniazid because of their bactericidal activity. The 28% mortality and other measures of illness in both study groups were no better than those achieved by the standard therapy used in the 1950s.
It is also disappointing that three new drugs finally becoming available for this indication – bedaquiline, delamanid, and pretomanid – are highly protein bound and unlikely to freely penetrate the blood-brain barrier.
Dr. Peter R. Donald is at the Desmond Tutu TB Center and the department of pediatrics and child health at Stellenbosch University, Tygerberg (South Africa). He reported having no relevant financial disclosures. Dr. Donald made these remarks in an editorial accompanying Dr. Heemskerk’s report (New Engl J Med. 2016 Jan 14. doi:10.1056/NEJMe1511990).
These findings are disappointing and suggest that fluoroquinolones are not going to revolutionize the treatment of tuberculous meningitis, even though they may replace isoniazid because of their bactericidal activity. The 28% mortality and other measures of illness in both study groups were no better than those achieved by the standard therapy used in the 1950s.
It is also disappointing that three new drugs finally becoming available for this indication – bedaquiline, delamanid, and pretomanid – are highly protein bound and unlikely to freely penetrate the blood-brain barrier.
Dr. Peter R. Donald is at the Desmond Tutu TB Center and the department of pediatrics and child health at Stellenbosch University, Tygerberg (South Africa). He reported having no relevant financial disclosures. Dr. Donald made these remarks in an editorial accompanying Dr. Heemskerk’s report (New Engl J Med. 2016 Jan 14. doi:10.1056/NEJMe1511990).
These findings are disappointing and suggest that fluoroquinolones are not going to revolutionize the treatment of tuberculous meningitis, even though they may replace isoniazid because of their bactericidal activity. The 28% mortality and other measures of illness in both study groups were no better than those achieved by the standard therapy used in the 1950s.
It is also disappointing that three new drugs finally becoming available for this indication – bedaquiline, delamanid, and pretomanid – are highly protein bound and unlikely to freely penetrate the blood-brain barrier.
Dr. Peter R. Donald is at the Desmond Tutu TB Center and the department of pediatrics and child health at Stellenbosch University, Tygerberg (South Africa). He reported having no relevant financial disclosures. Dr. Donald made these remarks in an editorial accompanying Dr. Heemskerk’s report (New Engl J Med. 2016 Jan 14. doi:10.1056/NEJMe1511990).
Intensified antituberculosis therapy doesn’t appear to improve survival in adults with tuberculous meningitis, compared with standard treatment, according to a report published online Jan. 14 in the New England Journal of Medicine.
This result, from a 3-year randomized double-blind placebo controlled clinical trial involving 817 adults in Vietnam, contradicts findings from previous small studies which suggested that increasing the rifampin dose and adding a fluoroquinolone to the standard regimen might improve outcomes, said Dr. A. Dorothee Heemskerk of the Oxford University Clinical Research Unit, Ho Chi Minh City, Vietnam, and her associates.
Current guidelines recommend at least 2 months of therapy with four antituberculosis agents, followed by treatment with rifampin (10 mg/kg) and isoniazid for an additional 7-10 months. “However, these recommendations are based on data from pulmonary tuberculosis and do not take into account the differential ability of antituberculosis drugs to penetrate the brain,” the investigators noted.
The concentration of rifampin in cerebrospinal fluid reaches only 30% of that in the plasma, so it has been proposed that higher-dose rifampin (15 mg/kg) might be more effective for tuberculous meningitis. Fluoroquinolones such as levofloxacin were proposed because they are active against tuberculosis and achieve good penetration of the blood-brain barrier.
Dr. Heemskerk and her associates tested this hypothesis at two tertiary referral centers for severe cases of tuberculosis or infectious diseases in Vietnam. All the study participants received standard daily isoniazid (5 mg/kg), rifampin (10 mg/kg), pyrazinamide (25 mg/kg), and ethambutol (20 mg/kg) for 3 months, followed by the same doses of rifampin and isoniazid for an additional 6 months. Approximately half (408 patients in the intensive-therapy group) received additional rifampin (5 mg/kg) and levofloxacin (20 mg/kg), while the other half (409 patients in the control group) received matching placebos.
The median patient age was 35 years. Approximately 43% of patients were coinfected with HIV.
The primary outcome measure – death at 9-month follow-up – occurred in 113 of the intensive-therapy group and 114 of the control group, a nonsignificant difference (HR, 0.94). The intensified treatment was no better than was standard treatment in any subgroup of patients or in any secondary outcomes, including neurologic disability and time to a new neurologic event or death, the investigators said (N Engl J Med. 2016 Jan 14. doi:10.1056/NEJMoa1507062).
However, intensive therapy was associated with a higher frequency of seizures (23 vs. 11 patients), visual impairment (14 vs. 4 patients), allergic reactions (30 patients vs. 17 patients), jaundice (19 vs. 7 patients), grade 3 or 4 hyponatremia (112 patients vs. 81 patients), and adverse events leading to treatment interruptions (95 patients vs. 64 patients).
It is possible that raising the dose of rifampin by only 5 mg/kg may not have increased intracerebral drug concentrations “sufficiently to enhance bacterial killing. Recent data suggest that much higher doses (up to 35 mg/kg per day) may have an acceptable side-effect profile and may be necessary to significantly increase the killing of M. tuberculosis in pulmonary tuberculosis,” Dr. Heemskerk and her associates noted.
“Although the results of our study do not support a change in the currently recommended treatment regimens for tuberculous meningitis, enhanced antituberculosis treatment with higher doses of first-line drugs, including intravenous rifampin, or the newer antituberculosis drugs bedaquiline and delamanid, still require investigation,” they added.
Wellcome Trust and the Li Ka Shing Foundation supported the study. Dr. Heemskerk and her associates reported having no relevant financial disclosures.
Intensified antituberculosis therapy doesn’t appear to improve survival in adults with tuberculous meningitis, compared with standard treatment, according to a report published online Jan. 14 in the New England Journal of Medicine.
This result, from a 3-year randomized double-blind placebo controlled clinical trial involving 817 adults in Vietnam, contradicts findings from previous small studies which suggested that increasing the rifampin dose and adding a fluoroquinolone to the standard regimen might improve outcomes, said Dr. A. Dorothee Heemskerk of the Oxford University Clinical Research Unit, Ho Chi Minh City, Vietnam, and her associates.
Current guidelines recommend at least 2 months of therapy with four antituberculosis agents, followed by treatment with rifampin (10 mg/kg) and isoniazid for an additional 7-10 months. “However, these recommendations are based on data from pulmonary tuberculosis and do not take into account the differential ability of antituberculosis drugs to penetrate the brain,” the investigators noted.
The concentration of rifampin in cerebrospinal fluid reaches only 30% of that in the plasma, so it has been proposed that higher-dose rifampin (15 mg/kg) might be more effective for tuberculous meningitis. Fluoroquinolones such as levofloxacin were proposed because they are active against tuberculosis and achieve good penetration of the blood-brain barrier.
Dr. Heemskerk and her associates tested this hypothesis at two tertiary referral centers for severe cases of tuberculosis or infectious diseases in Vietnam. All the study participants received standard daily isoniazid (5 mg/kg), rifampin (10 mg/kg), pyrazinamide (25 mg/kg), and ethambutol (20 mg/kg) for 3 months, followed by the same doses of rifampin and isoniazid for an additional 6 months. Approximately half (408 patients in the intensive-therapy group) received additional rifampin (5 mg/kg) and levofloxacin (20 mg/kg), while the other half (409 patients in the control group) received matching placebos.
The median patient age was 35 years. Approximately 43% of patients were coinfected with HIV.
The primary outcome measure – death at 9-month follow-up – occurred in 113 of the intensive-therapy group and 114 of the control group, a nonsignificant difference (HR, 0.94). The intensified treatment was no better than was standard treatment in any subgroup of patients or in any secondary outcomes, including neurologic disability and time to a new neurologic event or death, the investigators said (N Engl J Med. 2016 Jan 14. doi:10.1056/NEJMoa1507062).
However, intensive therapy was associated with a higher frequency of seizures (23 vs. 11 patients), visual impairment (14 vs. 4 patients), allergic reactions (30 patients vs. 17 patients), jaundice (19 vs. 7 patients), grade 3 or 4 hyponatremia (112 patients vs. 81 patients), and adverse events leading to treatment interruptions (95 patients vs. 64 patients).
It is possible that raising the dose of rifampin by only 5 mg/kg may not have increased intracerebral drug concentrations “sufficiently to enhance bacterial killing. Recent data suggest that much higher doses (up to 35 mg/kg per day) may have an acceptable side-effect profile and may be necessary to significantly increase the killing of M. tuberculosis in pulmonary tuberculosis,” Dr. Heemskerk and her associates noted.
“Although the results of our study do not support a change in the currently recommended treatment regimens for tuberculous meningitis, enhanced antituberculosis treatment with higher doses of first-line drugs, including intravenous rifampin, or the newer antituberculosis drugs bedaquiline and delamanid, still require investigation,” they added.
Wellcome Trust and the Li Ka Shing Foundation supported the study. Dr. Heemskerk and her associates reported having no relevant financial disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Intensified anti-TB therapy doesn’t improve survival, compared with standard treatment, in adults with tuberculous meningitis.
Major finding: The primary outcome measure – death at 9-month follow-up – occurred in 113 of the intensive-therapy group and 114 of the control group, a nonsignificant difference (HR, 0.94).
Data source: A 3-year randomized double-blind placebo-controlled trial involving 817 Vietnamese adults followed for 9 months.
Disclosures: Wellcome Trust and the Li Ka Shing Foundation supported the study. Dr. Heemskerk and her associates reported having no relevant disclosures.
Frozen noninferior to fresh fecal microbiota transplantation
Fecal microbiota transplantation using frozen-then-thawed fecal material proved noninferior to that using fresh material for treating recurrent or refractory Clostridium difficile infection, according to a report published online Jan. 12 in JAMA.
Using frozen rather than fresh fecal material offers many advantages, such as allowing much more widespread and immediate accessibility of the treatment; reducing the number and frequency of donor screenings, which in turn would reduce costs; and ameliorating concern about potential transmission of pathogens from the donor to the recipient, since samples could be stored in quarantine until screening results are known, said Dr. Christine H. Lee of the department of pathology and molecular medicine, McMaster University, Hamilton (Ont.), and her associates.
They performed a 2-year randomized, double-blind noninferiority trial at six academic medical centers in Canada to compare frozen with fresh donor material in 232 adults with recurrent or refractory C. difficile infection. These study participants had “an extensive burden of comorbidity”: most had inflammatory bowel diseases and approximately 85% were immunocompromised, having undergone chronic hemodialysis or kidney transplantation, or having had metastatic solid tumors or hematologic malignancies. Half of the study subjects were inpatients, and approximately 75% were aged 65 years and older.
The patients were assigned to receive 50 mL of frozen-then-thawed FMT (114 participants) or fresh FMT (118 participants) by retention enema, delivered using 60-mL syringes. Those who didn’t improve by day 4 were given an additional FMT from the same donor. “Administration by enema is significantly less invasive than colonoscopy or nasojejunal/gastric administration and can be performed outside an acute care facility,” Dr. Lee and her associates noted.
The primary efficacy endpoint was clinical resolution, defined as no recurrence of C. difficile–related diarrhea at 13 weeks and no need for antibiotics. In the per-protocol population, 83.5% of the frozen FMT group and 85.1% of the fresh FMT group achieved this endpoint. In the intention-to-treat population, 75.0% of the frozen FMT group and 70.3% of the fresh FMT group achieved it. Both results demonstrate the noninferiority of frozen FMT, the investigators said (JAMA. 2016;315[2]:142-9. doi:10.1001/jama.201518098).
The proportion of adverse events and severe adverse events was deemed low and did not differ between the two study groups. The most common adverse events that may possibly have been related to treatment occurred in similar numbers of each group and included transient diarrhea, abdominal cramps, and nausea during the first 24 hours after transplantation and constipation and excess flatulence during the 13-week follow-up.
Even though this follow-up was longer than that in most clinical trials of FMT for C. difficile infection, which only tracked patients for 40 days, it is still insufficient to assess the long-term safety of the treatment. Ten-year follow-up of the participants in this trial is currently under way to examine any beneficial effects the treatment might exert on the metabolic syndrome, diabetes, or autoimmune disease, as well as any negative effects such as the development of autoimmune disorders or cancer.
The findings of Dr. Lee and her associates offer the best evidence to date supporting the use of frozen stool material in FMT, which would eliminate many of the logistical burdens associated with the treatment. For example, stool collection and processing would no longer have to be tied to the date and time of each individual transplantation.
These results also support the use of centralized stool banks, which would offer clinicians access to safe, screened stool material that could be shipped and stored frozen, then thawed for use as needed.
Dr. Preeti N. Malani and Dr. Krishna Rao are with the division of infectious diseases at the University of Michigan Health System, Ann Arbor. Dr. Malani is also an associate editor at JAMA and Dr. Rao is also with the Veterans Affairs Ann Arbor Healthcare System. Dr. Rao’s work is supported in part by the Claude D. Pepper Older Americans Independence Center. Dr. Malani and Dr. Rao reported having no relevant financial disclosures. They made these remarks in an editorial (JAMA. 2016;315[2]:137-8) accompanying Dr. Lee’s report.
The findings of Dr. Lee and her associates offer the best evidence to date supporting the use of frozen stool material in FMT, which would eliminate many of the logistical burdens associated with the treatment. For example, stool collection and processing would no longer have to be tied to the date and time of each individual transplantation.
These results also support the use of centralized stool banks, which would offer clinicians access to safe, screened stool material that could be shipped and stored frozen, then thawed for use as needed.
Dr. Preeti N. Malani and Dr. Krishna Rao are with the division of infectious diseases at the University of Michigan Health System, Ann Arbor. Dr. Malani is also an associate editor at JAMA and Dr. Rao is also with the Veterans Affairs Ann Arbor Healthcare System. Dr. Rao’s work is supported in part by the Claude D. Pepper Older Americans Independence Center. Dr. Malani and Dr. Rao reported having no relevant financial disclosures. They made these remarks in an editorial (JAMA. 2016;315[2]:137-8) accompanying Dr. Lee’s report.
The findings of Dr. Lee and her associates offer the best evidence to date supporting the use of frozen stool material in FMT, which would eliminate many of the logistical burdens associated with the treatment. For example, stool collection and processing would no longer have to be tied to the date and time of each individual transplantation.
These results also support the use of centralized stool banks, which would offer clinicians access to safe, screened stool material that could be shipped and stored frozen, then thawed for use as needed.
Dr. Preeti N. Malani and Dr. Krishna Rao are with the division of infectious diseases at the University of Michigan Health System, Ann Arbor. Dr. Malani is also an associate editor at JAMA and Dr. Rao is also with the Veterans Affairs Ann Arbor Healthcare System. Dr. Rao’s work is supported in part by the Claude D. Pepper Older Americans Independence Center. Dr. Malani and Dr. Rao reported having no relevant financial disclosures. They made these remarks in an editorial (JAMA. 2016;315[2]:137-8) accompanying Dr. Lee’s report.
Fecal microbiota transplantation using frozen-then-thawed fecal material proved noninferior to that using fresh material for treating recurrent or refractory Clostridium difficile infection, according to a report published online Jan. 12 in JAMA.
Using frozen rather than fresh fecal material offers many advantages, such as allowing much more widespread and immediate accessibility of the treatment; reducing the number and frequency of donor screenings, which in turn would reduce costs; and ameliorating concern about potential transmission of pathogens from the donor to the recipient, since samples could be stored in quarantine until screening results are known, said Dr. Christine H. Lee of the department of pathology and molecular medicine, McMaster University, Hamilton (Ont.), and her associates.
They performed a 2-year randomized, double-blind noninferiority trial at six academic medical centers in Canada to compare frozen with fresh donor material in 232 adults with recurrent or refractory C. difficile infection. These study participants had “an extensive burden of comorbidity”: most had inflammatory bowel diseases and approximately 85% were immunocompromised, having undergone chronic hemodialysis or kidney transplantation, or having had metastatic solid tumors or hematologic malignancies. Half of the study subjects were inpatients, and approximately 75% were aged 65 years and older.
The patients were assigned to receive 50 mL of frozen-then-thawed FMT (114 participants) or fresh FMT (118 participants) by retention enema, delivered using 60-mL syringes. Those who didn’t improve by day 4 were given an additional FMT from the same donor. “Administration by enema is significantly less invasive than colonoscopy or nasojejunal/gastric administration and can be performed outside an acute care facility,” Dr. Lee and her associates noted.
The primary efficacy endpoint was clinical resolution, defined as no recurrence of C. difficile–related diarrhea at 13 weeks and no need for antibiotics. In the per-protocol population, 83.5% of the frozen FMT group and 85.1% of the fresh FMT group achieved this endpoint. In the intention-to-treat population, 75.0% of the frozen FMT group and 70.3% of the fresh FMT group achieved it. Both results demonstrate the noninferiority of frozen FMT, the investigators said (JAMA. 2016;315[2]:142-9. doi:10.1001/jama.201518098).
The proportion of adverse events and severe adverse events was deemed low and did not differ between the two study groups. The most common adverse events that may possibly have been related to treatment occurred in similar numbers of each group and included transient diarrhea, abdominal cramps, and nausea during the first 24 hours after transplantation and constipation and excess flatulence during the 13-week follow-up.
Even though this follow-up was longer than that in most clinical trials of FMT for C. difficile infection, which only tracked patients for 40 days, it is still insufficient to assess the long-term safety of the treatment. Ten-year follow-up of the participants in this trial is currently under way to examine any beneficial effects the treatment might exert on the metabolic syndrome, diabetes, or autoimmune disease, as well as any negative effects such as the development of autoimmune disorders or cancer.
Fecal microbiota transplantation using frozen-then-thawed fecal material proved noninferior to that using fresh material for treating recurrent or refractory Clostridium difficile infection, according to a report published online Jan. 12 in JAMA.
Using frozen rather than fresh fecal material offers many advantages, such as allowing much more widespread and immediate accessibility of the treatment; reducing the number and frequency of donor screenings, which in turn would reduce costs; and ameliorating concern about potential transmission of pathogens from the donor to the recipient, since samples could be stored in quarantine until screening results are known, said Dr. Christine H. Lee of the department of pathology and molecular medicine, McMaster University, Hamilton (Ont.), and her associates.
They performed a 2-year randomized, double-blind noninferiority trial at six academic medical centers in Canada to compare frozen with fresh donor material in 232 adults with recurrent or refractory C. difficile infection. These study participants had “an extensive burden of comorbidity”: most had inflammatory bowel diseases and approximately 85% were immunocompromised, having undergone chronic hemodialysis or kidney transplantation, or having had metastatic solid tumors or hematologic malignancies. Half of the study subjects were inpatients, and approximately 75% were aged 65 years and older.
The patients were assigned to receive 50 mL of frozen-then-thawed FMT (114 participants) or fresh FMT (118 participants) by retention enema, delivered using 60-mL syringes. Those who didn’t improve by day 4 were given an additional FMT from the same donor. “Administration by enema is significantly less invasive than colonoscopy or nasojejunal/gastric administration and can be performed outside an acute care facility,” Dr. Lee and her associates noted.
The primary efficacy endpoint was clinical resolution, defined as no recurrence of C. difficile–related diarrhea at 13 weeks and no need for antibiotics. In the per-protocol population, 83.5% of the frozen FMT group and 85.1% of the fresh FMT group achieved this endpoint. In the intention-to-treat population, 75.0% of the frozen FMT group and 70.3% of the fresh FMT group achieved it. Both results demonstrate the noninferiority of frozen FMT, the investigators said (JAMA. 2016;315[2]:142-9. doi:10.1001/jama.201518098).
The proportion of adverse events and severe adverse events was deemed low and did not differ between the two study groups. The most common adverse events that may possibly have been related to treatment occurred in similar numbers of each group and included transient diarrhea, abdominal cramps, and nausea during the first 24 hours after transplantation and constipation and excess flatulence during the 13-week follow-up.
Even though this follow-up was longer than that in most clinical trials of FMT for C. difficile infection, which only tracked patients for 40 days, it is still insufficient to assess the long-term safety of the treatment. Ten-year follow-up of the participants in this trial is currently under way to examine any beneficial effects the treatment might exert on the metabolic syndrome, diabetes, or autoimmune disease, as well as any negative effects such as the development of autoimmune disorders or cancer.
FROM JAMA
Key clinical point: Fecal microbiota transplantation using frozen-then-thawed fecal material proved noninferior to using fresh material for recurrent/refractory Clostridium difficile infection.
Major finding: In the per-protocol population, 83.5% of the frozen FMT group and 85.1% of the fresh FMT group achieved clinical resolution.
Data source: A 2-year randomized, double-blind noninferiority trial involving 232 patients treated at six academic medical centers in Canada and followed for 13 weeks.
Disclosures: This study was funded by Physicians Services Inc., the Natural Sciences and Engineering Council, the National Science Foundation, and the gastrointestinal diseases research unit at Kingston (Ont.) General Hospital. Dr. Lee reported participating in clinical trials for ViroPharma, Actelion, Cubist, and Merck, and serving on the advisory boards of Rebiotix and Merck. Her associates reported numerous ties to industry sources.
Investigational maternal group B strep vaccine well tolerated
An investigational trivalent group B streptococcal vaccine given to pregnant women produced elevated antibody levels in their infants, indicating that the infants likely were protected by passive immunity, according to a report published online Jan. 11 in Obstetrics & Gynecology.
A maternally administered vaccine was proposed as possibly the most effective means of preventing group B strep disease “across the entire period of vulnerability in newborns.” In this phase II randomized study performed at two sites in Belgium and three in Canada, levels of GBS-specific antibodies were assessed in infants of 86 healthy women vaccinated at 24-35 weeks’ gestation.
A total of 51 women received active vaccine and 35 received a placebo injection in the 2-year trial, which was supported by Novartis Vaccines and Diagnostics, maker of this investigational vaccine, according to Dr. Gilbert G.G. Donders of Femicare Clinical Research for Women, Tienen, Belgium, and his associates.
Mean maternal antibody levels increased by 16-fold to 23-fold after vaccination. Levels of antibody transfer, as measured in cord blood samples or needlestick samples from the neonate at birth, ranged from 66% to 79% – which is comparable to levels seen after maternal immunization with other vaccines such as those against Haemophilus influenzae type b or meningococcal disease.
At 3 months of age, antibody levels in the infants had decreased to approximately 22%-25% of what they had been at birth, but this was still 5-8 times higher than antibody levels in the placebo group, the investigators reported (Obstet Gynecol. 2016;127:214-22. doi: 10.1097/AOG.0000000000001190).
Neither the mothers nor the infants showed any “concerning safety signals.” One-minute and 5-minute Apgar scores were similar between the two study groups, and the percentage of infants who achieved “normal” scores on developmental measures also was similar: 71%-96% at 5 months and 93%-100% at 7 months in both groups. One newborn developed perinatal asphyxia, “which was considered possibly related to vaccination because no other obvious cause was present,” the researchers noted.
In addition, there was a possibility that the investigational vaccine contained a compound that might interfere with the infant’s response to routine diphtheria immunization. But no such interference was detected when these responses were measured after the infants received their final diphtheria vaccination, according to the researchers.
Novartis Vaccines and Diagnostics, whose non-influenza human vaccine business was recently transferred to GlaxoSmithKline, sponsored the study. Dr. Donders received research fees for undertaking the trial, other coauthors received research funding from Novartis, and four coauthors were employed by Novartis at the time of the study.
An investigational trivalent group B streptococcal vaccine given to pregnant women produced elevated antibody levels in their infants, indicating that the infants likely were protected by passive immunity, according to a report published online Jan. 11 in Obstetrics & Gynecology.
A maternally administered vaccine was proposed as possibly the most effective means of preventing group B strep disease “across the entire period of vulnerability in newborns.” In this phase II randomized study performed at two sites in Belgium and three in Canada, levels of GBS-specific antibodies were assessed in infants of 86 healthy women vaccinated at 24-35 weeks’ gestation.
A total of 51 women received active vaccine and 35 received a placebo injection in the 2-year trial, which was supported by Novartis Vaccines and Diagnostics, maker of this investigational vaccine, according to Dr. Gilbert G.G. Donders of Femicare Clinical Research for Women, Tienen, Belgium, and his associates.
Mean maternal antibody levels increased by 16-fold to 23-fold after vaccination. Levels of antibody transfer, as measured in cord blood samples or needlestick samples from the neonate at birth, ranged from 66% to 79% – which is comparable to levels seen after maternal immunization with other vaccines such as those against Haemophilus influenzae type b or meningococcal disease.
At 3 months of age, antibody levels in the infants had decreased to approximately 22%-25% of what they had been at birth, but this was still 5-8 times higher than antibody levels in the placebo group, the investigators reported (Obstet Gynecol. 2016;127:214-22. doi: 10.1097/AOG.0000000000001190).
Neither the mothers nor the infants showed any “concerning safety signals.” One-minute and 5-minute Apgar scores were similar between the two study groups, and the percentage of infants who achieved “normal” scores on developmental measures also was similar: 71%-96% at 5 months and 93%-100% at 7 months in both groups. One newborn developed perinatal asphyxia, “which was considered possibly related to vaccination because no other obvious cause was present,” the researchers noted.
In addition, there was a possibility that the investigational vaccine contained a compound that might interfere with the infant’s response to routine diphtheria immunization. But no such interference was detected when these responses were measured after the infants received their final diphtheria vaccination, according to the researchers.
Novartis Vaccines and Diagnostics, whose non-influenza human vaccine business was recently transferred to GlaxoSmithKline, sponsored the study. Dr. Donders received research fees for undertaking the trial, other coauthors received research funding from Novartis, and four coauthors were employed by Novartis at the time of the study.
An investigational trivalent group B streptococcal vaccine given to pregnant women produced elevated antibody levels in their infants, indicating that the infants likely were protected by passive immunity, according to a report published online Jan. 11 in Obstetrics & Gynecology.
A maternally administered vaccine was proposed as possibly the most effective means of preventing group B strep disease “across the entire period of vulnerability in newborns.” In this phase II randomized study performed at two sites in Belgium and three in Canada, levels of GBS-specific antibodies were assessed in infants of 86 healthy women vaccinated at 24-35 weeks’ gestation.
A total of 51 women received active vaccine and 35 received a placebo injection in the 2-year trial, which was supported by Novartis Vaccines and Diagnostics, maker of this investigational vaccine, according to Dr. Gilbert G.G. Donders of Femicare Clinical Research for Women, Tienen, Belgium, and his associates.
Mean maternal antibody levels increased by 16-fold to 23-fold after vaccination. Levels of antibody transfer, as measured in cord blood samples or needlestick samples from the neonate at birth, ranged from 66% to 79% – which is comparable to levels seen after maternal immunization with other vaccines such as those against Haemophilus influenzae type b or meningococcal disease.
At 3 months of age, antibody levels in the infants had decreased to approximately 22%-25% of what they had been at birth, but this was still 5-8 times higher than antibody levels in the placebo group, the investigators reported (Obstet Gynecol. 2016;127:214-22. doi: 10.1097/AOG.0000000000001190).
Neither the mothers nor the infants showed any “concerning safety signals.” One-minute and 5-minute Apgar scores were similar between the two study groups, and the percentage of infants who achieved “normal” scores on developmental measures also was similar: 71%-96% at 5 months and 93%-100% at 7 months in both groups. One newborn developed perinatal asphyxia, “which was considered possibly related to vaccination because no other obvious cause was present,” the researchers noted.
In addition, there was a possibility that the investigational vaccine contained a compound that might interfere with the infant’s response to routine diphtheria immunization. But no such interference was detected when these responses were measured after the infants received their final diphtheria vaccination, according to the researchers.
Novartis Vaccines and Diagnostics, whose non-influenza human vaccine business was recently transferred to GlaxoSmithKline, sponsored the study. Dr. Donders received research fees for undertaking the trial, other coauthors received research funding from Novartis, and four coauthors were employed by Novartis at the time of the study.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: An investigational trivalent group B strep vaccine for pregnant women raised antibody levels in their infants, indicating that the infants likely were protected by passive immunity.
Major finding: Mean maternal antibody levels increased by 16-fold to 23-fold after vaccination, and levels of antibody transfer, as measured in cord blood samples or needlestick samples from the neonate at birth, ranged from 66% to 79%.
Data source: A manufacturer-sponsored phase II randomized placebo-controlled single-blinded study involving 86 healthy pregnant women in Belgium and Canada.
Disclosures: Novartis Vaccines and Diagnostics, whose non-influenza human vaccine business was recently transferred to GlaxoSmithKline, sponsored the study. Dr. Donders received research fees for undertaking the trial, other coauthors received research funding from Novartis, and four coauthors were employed by Novartis at the time of the study.