User login
Patient outcomes not affected by attendings running ‘simultaneous’ ORs
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs.
However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single-institution review presented by Dr. Kenan W. Yount at the annual meeting of the American Association for Thoracic Surgery.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon to operating room.
In his presentation, Dr. Yount discussed the results of their review, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two operations. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates of postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 types of surgery, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically impact operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also, operations being scheduled in separate rooms must be done so with reasonable foresight." As long as institutions are following these practices, he concluded, "it would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs.
However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single-institution review presented by Dr. Kenan W. Yount at the annual meeting of the American Association for Thoracic Surgery.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon to operating room.
In his presentation, Dr. Yount discussed the results of their review, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two operations. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates of postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 types of surgery, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically impact operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also, operations being scheduled in separate rooms must be done so with reasonable foresight." As long as institutions are following these practices, he concluded, "it would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs.
However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single-institution review presented by Dr. Kenan W. Yount at the annual meeting of the American Association for Thoracic Surgery.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon to operating room.
In his presentation, Dr. Yount discussed the results of their review, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two operations. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates of postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 types of surgery, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically impact operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also, operations being scheduled in separate rooms must be done so with reasonable foresight." As long as institutions are following these practices, he concluded, "it would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
AT THE AATS ANNUAL MEETING
Major finding: Running two rooms was not associated with any differences in operative duration, morbidity, or mortality in multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category.
Data source: The study reviewed 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two operations.
Disclosures: Dr. Yount had no disclosures.
Triple therapy topped monotherapy in early rheumatoid arthritis
In arithmetic and newly diagnosed rheumatoid arthritis alike, three is greater than one.
Initial triple disease-modifying therapy with either of two glucocorticoid (GC) bridging therapies proved quicker in attaining treatment goals and required fewer treatment intensifications for patients with very early RA than did initial methotrexate monotherapy with oral GC therapy, according to the results of a randomized, comparative trial.
Several previous clinical trials concluded that initial combination therapy had better clinical efficacy than monotherapy. However, most rheumatologists have not incorporated this into daily practice, according to Dr. Pascal Hendrik Pieter de Jong of the University Medical Center, Rotterdam, the Netherlands, and his colleagues.
Previous combination-therapy studies have usually been disregarded, the researchers noted, because the trials were biased by the use of GCs. So, Dr. de Jong and his colleagues compared the benefits of the 1-year clinical efficacy of initial triple disease-modifying antirheumatic drugs to the benefits of initial methotrexate monotherapy unbiased by the use of GC therapy, either oral or intramuscular.
Primary outcomes of the study were the area under the curve of the Health Assessment Questionnaire (to assess functional ability) and Disease Activity Score (to assess disease state), and the proportion of patients with radiographic progression, the investigators reported online May 1 in Annals of the Rheumatic Diseases (Ann. Rheum. Dis. May 1, 2014 [doi: 10.1136/annrheumdis-2013-204788]).
The study population comprised the 281 patients with a high probability of progress to persistent arthritis (greater than 70%) who were in the Rotterdam Early Arthritis Cohort (tReach) trial. All patients were over age 18, with arthritis in one or more joints and symptom duration of less than 1 year; 68% of the patients were women.
Patients were randomized to one of three arms:
1) initial triple disease-modifying therapy (iTDT) of methotrexate plus sulfasalazine and hydroxychloroquine, with GCs administered intramuscularly,
2) iTDT with an oral GC tapering scheme, or
3) initial methotrexate monotherapy (iMM) with oral GCs similar to the second treatment arm.
Concurrent treatment with nonsteroidal anti-inflammatory drugs and intra-articular injections (maximum of two per 3 months) was allowed.
The largest difference in disease activity states between the treatment arms was seen after 3 months, although that effect gradually diminished to nonsignificance by 12 months. Similarly, there were no significant differences in functional ability at 12 months.
After 3 months, 40% fewer biological agents were prescribed in the iTDT group than in the iMM group, and that difference persisted over time. However, disease activity, functional ability, and radiographic progression were not different between the two treatments after 12 months, regardless of GC bridging therapies. Early initiation of biological agents in the iMM group might have prevented or delayed the radiographic progression, the researchers suggested.
There were no differences in serious adverse events seen in the treatment arms, but the proportion of patients with medication adjustments due to adverse events was significantly higher in the iTDT (65%), compared with the iMM group (45%). No differences were seen between the two GC bridging therapies. Gastrointestinal complaints (56%) and fatigue (36%) were the two most commonly reported adverse events.
"We found no differences in disease activity, functional ability, and radiographic progression after 12 months of treatment owing to our treat-to-target approach (intensifying treatment until the target is reached)," the investigators observed. "Therefore, it is not the endpoint, but progress towards the endpoint, which matters most."
In addition, delaying the implementation of biological agents with iTDT treatment resulted in "reducing costs enormously," according to the researchers, although the cost-utility analysis of the tREACH trial has to reconfirm this, they added.
"We think that future research should focus on developing a more personalized treatment approach, in which differentiation between patients who would thrive on iMM and those who need iTDT might be a first step," they said.
"Before choosing the initial treatment strategy, rheumatologists should be aware of the benefits and the risks, but additionally, known prognostic factors and the patient’s wish should be taken into account. One single intramuscular GC injection and a low-dose, oral GC tapering scheme would be sufficient as bridging therapy," the researchers concluded.
The research was supported by an unrestricted grant from Pfizer, which had no involvement in the study design, data collection, analysis, or publication of the results. Data management was sponsored by the Dutch Arthritis Foundation. The authors reported that they had no competing interests.
Initial triple disease-modifying therapy, glucocorticoid, early RA, methotrexate monotherapy with oral GC therapy, initial combination therapy, Dr. Pascal Hendrik Pieter de Jong, Health Assessment Questionnaire, Disease Activity Score, radiographic progression, Annals of the Rheumatic Diseases, Rotterdam Early Arthritis Cohort (tReach) trial,
In arithmetic and newly diagnosed rheumatoid arthritis alike, three is greater than one.
Initial triple disease-modifying therapy with either of two glucocorticoid (GC) bridging therapies proved quicker in attaining treatment goals and required fewer treatment intensifications for patients with very early RA than did initial methotrexate monotherapy with oral GC therapy, according to the results of a randomized, comparative trial.
Several previous clinical trials concluded that initial combination therapy had better clinical efficacy than monotherapy. However, most rheumatologists have not incorporated this into daily practice, according to Dr. Pascal Hendrik Pieter de Jong of the University Medical Center, Rotterdam, the Netherlands, and his colleagues.
Previous combination-therapy studies have usually been disregarded, the researchers noted, because the trials were biased by the use of GCs. So, Dr. de Jong and his colleagues compared the benefits of the 1-year clinical efficacy of initial triple disease-modifying antirheumatic drugs to the benefits of initial methotrexate monotherapy unbiased by the use of GC therapy, either oral or intramuscular.
Primary outcomes of the study were the area under the curve of the Health Assessment Questionnaire (to assess functional ability) and Disease Activity Score (to assess disease state), and the proportion of patients with radiographic progression, the investigators reported online May 1 in Annals of the Rheumatic Diseases (Ann. Rheum. Dis. May 1, 2014 [doi: 10.1136/annrheumdis-2013-204788]).
The study population comprised the 281 patients with a high probability of progress to persistent arthritis (greater than 70%) who were in the Rotterdam Early Arthritis Cohort (tReach) trial. All patients were over age 18, with arthritis in one or more joints and symptom duration of less than 1 year; 68% of the patients were women.
Patients were randomized to one of three arms:
1) initial triple disease-modifying therapy (iTDT) of methotrexate plus sulfasalazine and hydroxychloroquine, with GCs administered intramuscularly,
2) iTDT with an oral GC tapering scheme, or
3) initial methotrexate monotherapy (iMM) with oral GCs similar to the second treatment arm.
Concurrent treatment with nonsteroidal anti-inflammatory drugs and intra-articular injections (maximum of two per 3 months) was allowed.
The largest difference in disease activity states between the treatment arms was seen after 3 months, although that effect gradually diminished to nonsignificance by 12 months. Similarly, there were no significant differences in functional ability at 12 months.
After 3 months, 40% fewer biological agents were prescribed in the iTDT group than in the iMM group, and that difference persisted over time. However, disease activity, functional ability, and radiographic progression were not different between the two treatments after 12 months, regardless of GC bridging therapies. Early initiation of biological agents in the iMM group might have prevented or delayed the radiographic progression, the researchers suggested.
There were no differences in serious adverse events seen in the treatment arms, but the proportion of patients with medication adjustments due to adverse events was significantly higher in the iTDT (65%), compared with the iMM group (45%). No differences were seen between the two GC bridging therapies. Gastrointestinal complaints (56%) and fatigue (36%) were the two most commonly reported adverse events.
"We found no differences in disease activity, functional ability, and radiographic progression after 12 months of treatment owing to our treat-to-target approach (intensifying treatment until the target is reached)," the investigators observed. "Therefore, it is not the endpoint, but progress towards the endpoint, which matters most."
In addition, delaying the implementation of biological agents with iTDT treatment resulted in "reducing costs enormously," according to the researchers, although the cost-utility analysis of the tREACH trial has to reconfirm this, they added.
"We think that future research should focus on developing a more personalized treatment approach, in which differentiation between patients who would thrive on iMM and those who need iTDT might be a first step," they said.
"Before choosing the initial treatment strategy, rheumatologists should be aware of the benefits and the risks, but additionally, known prognostic factors and the patient’s wish should be taken into account. One single intramuscular GC injection and a low-dose, oral GC tapering scheme would be sufficient as bridging therapy," the researchers concluded.
The research was supported by an unrestricted grant from Pfizer, which had no involvement in the study design, data collection, analysis, or publication of the results. Data management was sponsored by the Dutch Arthritis Foundation. The authors reported that they had no competing interests.
In arithmetic and newly diagnosed rheumatoid arthritis alike, three is greater than one.
Initial triple disease-modifying therapy with either of two glucocorticoid (GC) bridging therapies proved quicker in attaining treatment goals and required fewer treatment intensifications for patients with very early RA than did initial methotrexate monotherapy with oral GC therapy, according to the results of a randomized, comparative trial.
Several previous clinical trials concluded that initial combination therapy had better clinical efficacy than monotherapy. However, most rheumatologists have not incorporated this into daily practice, according to Dr. Pascal Hendrik Pieter de Jong of the University Medical Center, Rotterdam, the Netherlands, and his colleagues.
Previous combination-therapy studies have usually been disregarded, the researchers noted, because the trials were biased by the use of GCs. So, Dr. de Jong and his colleagues compared the benefits of the 1-year clinical efficacy of initial triple disease-modifying antirheumatic drugs to the benefits of initial methotrexate monotherapy unbiased by the use of GC therapy, either oral or intramuscular.
Primary outcomes of the study were the area under the curve of the Health Assessment Questionnaire (to assess functional ability) and Disease Activity Score (to assess disease state), and the proportion of patients with radiographic progression, the investigators reported online May 1 in Annals of the Rheumatic Diseases (Ann. Rheum. Dis. May 1, 2014 [doi: 10.1136/annrheumdis-2013-204788]).
The study population comprised the 281 patients with a high probability of progress to persistent arthritis (greater than 70%) who were in the Rotterdam Early Arthritis Cohort (tReach) trial. All patients were over age 18, with arthritis in one or more joints and symptom duration of less than 1 year; 68% of the patients were women.
Patients were randomized to one of three arms:
1) initial triple disease-modifying therapy (iTDT) of methotrexate plus sulfasalazine and hydroxychloroquine, with GCs administered intramuscularly,
2) iTDT with an oral GC tapering scheme, or
3) initial methotrexate monotherapy (iMM) with oral GCs similar to the second treatment arm.
Concurrent treatment with nonsteroidal anti-inflammatory drugs and intra-articular injections (maximum of two per 3 months) was allowed.
The largest difference in disease activity states between the treatment arms was seen after 3 months, although that effect gradually diminished to nonsignificance by 12 months. Similarly, there were no significant differences in functional ability at 12 months.
After 3 months, 40% fewer biological agents were prescribed in the iTDT group than in the iMM group, and that difference persisted over time. However, disease activity, functional ability, and radiographic progression were not different between the two treatments after 12 months, regardless of GC bridging therapies. Early initiation of biological agents in the iMM group might have prevented or delayed the radiographic progression, the researchers suggested.
There were no differences in serious adverse events seen in the treatment arms, but the proportion of patients with medication adjustments due to adverse events was significantly higher in the iTDT (65%), compared with the iMM group (45%). No differences were seen between the two GC bridging therapies. Gastrointestinal complaints (56%) and fatigue (36%) were the two most commonly reported adverse events.
"We found no differences in disease activity, functional ability, and radiographic progression after 12 months of treatment owing to our treat-to-target approach (intensifying treatment until the target is reached)," the investigators observed. "Therefore, it is not the endpoint, but progress towards the endpoint, which matters most."
In addition, delaying the implementation of biological agents with iTDT treatment resulted in "reducing costs enormously," according to the researchers, although the cost-utility analysis of the tREACH trial has to reconfirm this, they added.
"We think that future research should focus on developing a more personalized treatment approach, in which differentiation between patients who would thrive on iMM and those who need iTDT might be a first step," they said.
"Before choosing the initial treatment strategy, rheumatologists should be aware of the benefits and the risks, but additionally, known prognostic factors and the patient’s wish should be taken into account. One single intramuscular GC injection and a low-dose, oral GC tapering scheme would be sufficient as bridging therapy," the researchers concluded.
The research was supported by an unrestricted grant from Pfizer, which had no involvement in the study design, data collection, analysis, or publication of the results. Data management was sponsored by the Dutch Arthritis Foundation. The authors reported that they had no competing interests.
Initial triple disease-modifying therapy, glucocorticoid, early RA, methotrexate monotherapy with oral GC therapy, initial combination therapy, Dr. Pascal Hendrik Pieter de Jong, Health Assessment Questionnaire, Disease Activity Score, radiographic progression, Annals of the Rheumatic Diseases, Rotterdam Early Arthritis Cohort (tReach) trial,
Initial triple disease-modifying therapy, glucocorticoid, early RA, methotrexate monotherapy with oral GC therapy, initial combination therapy, Dr. Pascal Hendrik Pieter de Jong, Health Assessment Questionnaire, Disease Activity Score, radiographic progression, Annals of the Rheumatic Diseases, Rotterdam Early Arthritis Cohort (tReach) trial,
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: Start patients with newly diagnosed rheumatoid arthritis on triple disease-modifying therapy rather than methotrexate monotherapy.
Major finding: Triple therapy resulted in 40% fewer treatment intensifications than did monotherapy, but it required more medication adjustments because of adverse events. No differences in radiographic progression were seen.
Data source: The report summarized 1-year data from the tREACH trial, a randomized, single-blinded, three-arm clinical efficacy study with 281 patients.
Disclosures: The research was supported by an unrestricted grant from Pfizer, which had no involvement in the study design, data collection, analysis, or publication of the results. Data management was sponsored by the Dutch Arthritis Foundation. The authors reported that they had no competing interests.
Tracking top research in the ATS late-breakers session
On Sunday morning at the American Thoracic Society 2014 International Conference in San Diego, the focus will be on late-breaking clinical trials with presentations of the latest research from basic studies to the best contemporary patient care in disciplines ranging from pulmonary to critical care to sleep medicine and beyond. This emphasis on basic, translational, and clinical science distinguishes the ATS International Conference from other meetings.
The complete listing of this year’s presentations and their abstracts is available online. Here are highlights of five of the exceptional presentations scheduled for Sunday morning’s Late Breaking Abstracts in Clinical Trials, which will be moderated by Dr. R. Graham Barr of Columbia University, New York; Dr. Klaus F. Rabe of the University of Kiel and Clinic Grosshansdorf, Germany; and Dr. Y. Michael Shim of the University of Virginia, Charlottesville.
ASPIRE trial results
Dr. George R. Washko Jr. of Brigham and Women’s Hospital, Boston, will discuss the results of the ASPIRE trial, a multicenter, randomized, controlled study evaluating AeriSeal System endoscopic lung volume reduction therapy for chronic obstructive pulmonary disease (COPD) with advanced emphysema. The study was initiated in September 2012, and was terminated prematurely on Nov. 13, 2013, after enrollment and randomization of less than one-third of the planned patients, for nonmedical and nonregulatory reasons. Although interim results from ASPIRE confirm prior findings that hydrogel-based lung volume reduction therapy can produce improvements in advanced emphysema patient outcomes, compared with optimized medical treatment, the treatment is associated with an increased risk of adverse events requiring hospitalization, according to the researchers.
The study compared AeriSeal Lung Sealant therapy plus medical treatment to medical treatment alone. At 90-day follow-up for available patients, there was a significant improvement in forced expiratory volume in 1 second (FEV1) in the treatment group vs. the control group.
Dr. Washko will discuss how, at the time of study termination, significantly more adverse events requiring hospitalizations occurred in patients in the treatment group (43%), as compared with the control patients (15%). The majority of these events were respiratory (39% treatment vs. 15% control). There were two deaths in the treatment group (one treatment-related) and none in the control group, according to Dr. Washko and his colleagues.
RODEO trial findings
Short-term treatment with rosuvastatin in stable COPD patients without known cardiovascular disease was associated with reduced systemic inflammation, but did not improve endothelial or pulmonary function, according to the results of the RODEO (Effect of Rosuvastatin Treatment in Stable COPD) trial, which will be presented by Dr. Anke Neukamm of Akershus University Hospital, Lørenskog, Norway.
Dr. Neukamm and her colleagues tested the hypotheses that statin therapy is associated with improved endothelial and pulmonary function and reduced systemic inflammation in patients with stable COPD. In their randomized, placebo-controlled, double-blind, parallel trial, stable COPD patients (n = 99) from two hospital outpatient clinics were assigned to receive rosuvastatin 10 mg or matching placebo once daily for 12 weeks.
She will present their data showing that rosuvastatin therapy was associated with a highly significant decrease in serum LDL cholesterol, but that in the intention-to-treat analysis, no significant between-group difference in change in endothelial or pulmonary function was observed.
ACROSS trial results
In adults with severe sepsis and detectable levels of plasma cell–free hemoglobin, treatment with acetaminophen reduced oxidative injury and improved renal function, according to the results of the randomized ACROSS (Acetaminophen for the Reduction of Oxidative Injury in Patients with Severe Sepsis) trial, which will be presented by Dr. David R. Janz, a clinical fellow at Vanderbilt University, Nashville, Tenn.
Dr. Janz will report on the phase II, randomized, double-blind, placebo-controlled trial that he and his colleagues performed, comparing acetaminophen 1 g by mouth every 6 hours for 3 days versus placebo in adults with severe sepsis admitted to the intensive care unit for less than 24 hours and who had detectable plasma cell–free hemoglobin, a potent oxidant.
They found that the acetaminophen group had significantly lower levels of plasma F2-isoprostanes on study day 2 and significantly lower levels of creatinine on study day 3, although there was no statistically significant difference in hospital mortality or adverse events between the acetaminophen and placebo groups.
Beta-blocker therapy in patients with i-PAH
Dr. J.S.J.A. Van Campen, of the Institute for Cardiovascular Research, VU Medical Center, Amsterdam, and colleagues performed a randomized, controlled clinical trial of beta-blocker therapy in patients with idiopathic pulmonary arterial hypertension (i-PAH) to specifically assess the clinical effectiveness of bisoprolol.
Dr. Van Campen will present their results showing that in patients with i-PAH, beta-blocker therapy is safe and is tolerated equally as in patients with left heart failure. A significant reduction of heart rate was achieved with the tolerated dose, and right ventricular ejection fraction and quality of life improved without a significant drop in exercise capacity
They studied 18 patients with optimally treated, stable i-PAH (9/9 New York Heart Association II/III ) who received bisoprolol in an escalating dose up to a maximum of 10 mg or four tablets of placebo. A physical examination and physiological evaluation were performed every 2 weeks; and an ECG, a 6-minute walking distance test, and a Minnesota quality of life questionnaire were administered every month. MRI and echocardiography of the heart, heart rate variability measurements, cardiopulmonary exercise testing, and PET scans were performed at baseline, at crossover, and at the end of the study.
Dr. Van Campen will discuss how there were no reported cases of syncope during the entire study period. One patient developed fluid retention after the start of bisoprolol despite oral diuretics and had to be treated with intravenous diuretics. Four other significant adverse events were reported but not associated with the study medication. Only 2 of 18 patients did not tolerate bisoprolol due to hypotension, bradycardia, or tiredness.
CPAP managed with web-messaging program
Dr. Dominic Munafo, a pulmonologist in San Diego, and his colleagues performed an unblinded, multicenter, prospective trial of patients with newly diagnosed obstructive sleep apnea to determine whether a web-based, automated messaging program for continuous positive airway pressure (CPAP) improved adherence of patients to the treatment regimen, compared with standard coaching care.
Dr. Munafo will discuss how there was no statistically significant difference between the web-messaging sleep group and the standard coaching group in Medicare adherence, mean hours of CPAP usage, CPAP efficacy, or improvement in score on the Epworth Sleepiness Scale. However, they did find that the use of the automated web-based follow-up program utilizing text messaging and e-mail was widely accepted and yielded excellent adherence at a substantially reduced coaching labor requirement when compared to the standard coaching group.
On Sunday morning at the American Thoracic Society 2014 International Conference in San Diego, the focus will be on late-breaking clinical trials with presentations of the latest research from basic studies to the best contemporary patient care in disciplines ranging from pulmonary to critical care to sleep medicine and beyond. This emphasis on basic, translational, and clinical science distinguishes the ATS International Conference from other meetings.
The complete listing of this year’s presentations and their abstracts is available online. Here are highlights of five of the exceptional presentations scheduled for Sunday morning’s Late Breaking Abstracts in Clinical Trials, which will be moderated by Dr. R. Graham Barr of Columbia University, New York; Dr. Klaus F. Rabe of the University of Kiel and Clinic Grosshansdorf, Germany; and Dr. Y. Michael Shim of the University of Virginia, Charlottesville.
ASPIRE trial results
Dr. George R. Washko Jr. of Brigham and Women’s Hospital, Boston, will discuss the results of the ASPIRE trial, a multicenter, randomized, controlled study evaluating AeriSeal System endoscopic lung volume reduction therapy for chronic obstructive pulmonary disease (COPD) with advanced emphysema. The study was initiated in September 2012, and was terminated prematurely on Nov. 13, 2013, after enrollment and randomization of less than one-third of the planned patients, for nonmedical and nonregulatory reasons. Although interim results from ASPIRE confirm prior findings that hydrogel-based lung volume reduction therapy can produce improvements in advanced emphysema patient outcomes, compared with optimized medical treatment, the treatment is associated with an increased risk of adverse events requiring hospitalization, according to the researchers.
The study compared AeriSeal Lung Sealant therapy plus medical treatment to medical treatment alone. At 90-day follow-up for available patients, there was a significant improvement in forced expiratory volume in 1 second (FEV1) in the treatment group vs. the control group.
Dr. Washko will discuss how, at the time of study termination, significantly more adverse events requiring hospitalizations occurred in patients in the treatment group (43%), as compared with the control patients (15%). The majority of these events were respiratory (39% treatment vs. 15% control). There were two deaths in the treatment group (one treatment-related) and none in the control group, according to Dr. Washko and his colleagues.
RODEO trial findings
Short-term treatment with rosuvastatin in stable COPD patients without known cardiovascular disease was associated with reduced systemic inflammation, but did not improve endothelial or pulmonary function, according to the results of the RODEO (Effect of Rosuvastatin Treatment in Stable COPD) trial, which will be presented by Dr. Anke Neukamm of Akershus University Hospital, Lørenskog, Norway.
Dr. Neukamm and her colleagues tested the hypotheses that statin therapy is associated with improved endothelial and pulmonary function and reduced systemic inflammation in patients with stable COPD. In their randomized, placebo-controlled, double-blind, parallel trial, stable COPD patients (n = 99) from two hospital outpatient clinics were assigned to receive rosuvastatin 10 mg or matching placebo once daily for 12 weeks.
She will present their data showing that rosuvastatin therapy was associated with a highly significant decrease in serum LDL cholesterol, but that in the intention-to-treat analysis, no significant between-group difference in change in endothelial or pulmonary function was observed.
ACROSS trial results
In adults with severe sepsis and detectable levels of plasma cell–free hemoglobin, treatment with acetaminophen reduced oxidative injury and improved renal function, according to the results of the randomized ACROSS (Acetaminophen for the Reduction of Oxidative Injury in Patients with Severe Sepsis) trial, which will be presented by Dr. David R. Janz, a clinical fellow at Vanderbilt University, Nashville, Tenn.
Dr. Janz will report on the phase II, randomized, double-blind, placebo-controlled trial that he and his colleagues performed, comparing acetaminophen 1 g by mouth every 6 hours for 3 days versus placebo in adults with severe sepsis admitted to the intensive care unit for less than 24 hours and who had detectable plasma cell–free hemoglobin, a potent oxidant.
They found that the acetaminophen group had significantly lower levels of plasma F2-isoprostanes on study day 2 and significantly lower levels of creatinine on study day 3, although there was no statistically significant difference in hospital mortality or adverse events between the acetaminophen and placebo groups.
Beta-blocker therapy in patients with i-PAH
Dr. J.S.J.A. Van Campen, of the Institute for Cardiovascular Research, VU Medical Center, Amsterdam, and colleagues performed a randomized, controlled clinical trial of beta-blocker therapy in patients with idiopathic pulmonary arterial hypertension (i-PAH) to specifically assess the clinical effectiveness of bisoprolol.
Dr. Van Campen will present their results showing that in patients with i-PAH, beta-blocker therapy is safe and is tolerated equally as in patients with left heart failure. A significant reduction of heart rate was achieved with the tolerated dose, and right ventricular ejection fraction and quality of life improved without a significant drop in exercise capacity
They studied 18 patients with optimally treated, stable i-PAH (9/9 New York Heart Association II/III ) who received bisoprolol in an escalating dose up to a maximum of 10 mg or four tablets of placebo. A physical examination and physiological evaluation were performed every 2 weeks; and an ECG, a 6-minute walking distance test, and a Minnesota quality of life questionnaire were administered every month. MRI and echocardiography of the heart, heart rate variability measurements, cardiopulmonary exercise testing, and PET scans were performed at baseline, at crossover, and at the end of the study.
Dr. Van Campen will discuss how there were no reported cases of syncope during the entire study period. One patient developed fluid retention after the start of bisoprolol despite oral diuretics and had to be treated with intravenous diuretics. Four other significant adverse events were reported but not associated with the study medication. Only 2 of 18 patients did not tolerate bisoprolol due to hypotension, bradycardia, or tiredness.
CPAP managed with web-messaging program
Dr. Dominic Munafo, a pulmonologist in San Diego, and his colleagues performed an unblinded, multicenter, prospective trial of patients with newly diagnosed obstructive sleep apnea to determine whether a web-based, automated messaging program for continuous positive airway pressure (CPAP) improved adherence of patients to the treatment regimen, compared with standard coaching care.
Dr. Munafo will discuss how there was no statistically significant difference between the web-messaging sleep group and the standard coaching group in Medicare adherence, mean hours of CPAP usage, CPAP efficacy, or improvement in score on the Epworth Sleepiness Scale. However, they did find that the use of the automated web-based follow-up program utilizing text messaging and e-mail was widely accepted and yielded excellent adherence at a substantially reduced coaching labor requirement when compared to the standard coaching group.
On Sunday morning at the American Thoracic Society 2014 International Conference in San Diego, the focus will be on late-breaking clinical trials with presentations of the latest research from basic studies to the best contemporary patient care in disciplines ranging from pulmonary to critical care to sleep medicine and beyond. This emphasis on basic, translational, and clinical science distinguishes the ATS International Conference from other meetings.
The complete listing of this year’s presentations and their abstracts is available online. Here are highlights of five of the exceptional presentations scheduled for Sunday morning’s Late Breaking Abstracts in Clinical Trials, which will be moderated by Dr. R. Graham Barr of Columbia University, New York; Dr. Klaus F. Rabe of the University of Kiel and Clinic Grosshansdorf, Germany; and Dr. Y. Michael Shim of the University of Virginia, Charlottesville.
ASPIRE trial results
Dr. George R. Washko Jr. of Brigham and Women’s Hospital, Boston, will discuss the results of the ASPIRE trial, a multicenter, randomized, controlled study evaluating AeriSeal System endoscopic lung volume reduction therapy for chronic obstructive pulmonary disease (COPD) with advanced emphysema. The study was initiated in September 2012, and was terminated prematurely on Nov. 13, 2013, after enrollment and randomization of less than one-third of the planned patients, for nonmedical and nonregulatory reasons. Although interim results from ASPIRE confirm prior findings that hydrogel-based lung volume reduction therapy can produce improvements in advanced emphysema patient outcomes, compared with optimized medical treatment, the treatment is associated with an increased risk of adverse events requiring hospitalization, according to the researchers.
The study compared AeriSeal Lung Sealant therapy plus medical treatment to medical treatment alone. At 90-day follow-up for available patients, there was a significant improvement in forced expiratory volume in 1 second (FEV1) in the treatment group vs. the control group.
Dr. Washko will discuss how, at the time of study termination, significantly more adverse events requiring hospitalizations occurred in patients in the treatment group (43%), as compared with the control patients (15%). The majority of these events were respiratory (39% treatment vs. 15% control). There were two deaths in the treatment group (one treatment-related) and none in the control group, according to Dr. Washko and his colleagues.
RODEO trial findings
Short-term treatment with rosuvastatin in stable COPD patients without known cardiovascular disease was associated with reduced systemic inflammation, but did not improve endothelial or pulmonary function, according to the results of the RODEO (Effect of Rosuvastatin Treatment in Stable COPD) trial, which will be presented by Dr. Anke Neukamm of Akershus University Hospital, Lørenskog, Norway.
Dr. Neukamm and her colleagues tested the hypotheses that statin therapy is associated with improved endothelial and pulmonary function and reduced systemic inflammation in patients with stable COPD. In their randomized, placebo-controlled, double-blind, parallel trial, stable COPD patients (n = 99) from two hospital outpatient clinics were assigned to receive rosuvastatin 10 mg or matching placebo once daily for 12 weeks.
She will present their data showing that rosuvastatin therapy was associated with a highly significant decrease in serum LDL cholesterol, but that in the intention-to-treat analysis, no significant between-group difference in change in endothelial or pulmonary function was observed.
ACROSS trial results
In adults with severe sepsis and detectable levels of plasma cell–free hemoglobin, treatment with acetaminophen reduced oxidative injury and improved renal function, according to the results of the randomized ACROSS (Acetaminophen for the Reduction of Oxidative Injury in Patients with Severe Sepsis) trial, which will be presented by Dr. David R. Janz, a clinical fellow at Vanderbilt University, Nashville, Tenn.
Dr. Janz will report on the phase II, randomized, double-blind, placebo-controlled trial that he and his colleagues performed, comparing acetaminophen 1 g by mouth every 6 hours for 3 days versus placebo in adults with severe sepsis admitted to the intensive care unit for less than 24 hours and who had detectable plasma cell–free hemoglobin, a potent oxidant.
They found that the acetaminophen group had significantly lower levels of plasma F2-isoprostanes on study day 2 and significantly lower levels of creatinine on study day 3, although there was no statistically significant difference in hospital mortality or adverse events between the acetaminophen and placebo groups.
Beta-blocker therapy in patients with i-PAH
Dr. J.S.J.A. Van Campen, of the Institute for Cardiovascular Research, VU Medical Center, Amsterdam, and colleagues performed a randomized, controlled clinical trial of beta-blocker therapy in patients with idiopathic pulmonary arterial hypertension (i-PAH) to specifically assess the clinical effectiveness of bisoprolol.
Dr. Van Campen will present their results showing that in patients with i-PAH, beta-blocker therapy is safe and is tolerated equally as in patients with left heart failure. A significant reduction of heart rate was achieved with the tolerated dose, and right ventricular ejection fraction and quality of life improved without a significant drop in exercise capacity
They studied 18 patients with optimally treated, stable i-PAH (9/9 New York Heart Association II/III ) who received bisoprolol in an escalating dose up to a maximum of 10 mg or four tablets of placebo. A physical examination and physiological evaluation were performed every 2 weeks; and an ECG, a 6-minute walking distance test, and a Minnesota quality of life questionnaire were administered every month. MRI and echocardiography of the heart, heart rate variability measurements, cardiopulmonary exercise testing, and PET scans were performed at baseline, at crossover, and at the end of the study.
Dr. Van Campen will discuss how there were no reported cases of syncope during the entire study period. One patient developed fluid retention after the start of bisoprolol despite oral diuretics and had to be treated with intravenous diuretics. Four other significant adverse events were reported but not associated with the study medication. Only 2 of 18 patients did not tolerate bisoprolol due to hypotension, bradycardia, or tiredness.
CPAP managed with web-messaging program
Dr. Dominic Munafo, a pulmonologist in San Diego, and his colleagues performed an unblinded, multicenter, prospective trial of patients with newly diagnosed obstructive sleep apnea to determine whether a web-based, automated messaging program for continuous positive airway pressure (CPAP) improved adherence of patients to the treatment regimen, compared with standard coaching care.
Dr. Munafo will discuss how there was no statistically significant difference between the web-messaging sleep group and the standard coaching group in Medicare adherence, mean hours of CPAP usage, CPAP efficacy, or improvement in score on the Epworth Sleepiness Scale. However, they did find that the use of the automated web-based follow-up program utilizing text messaging and e-mail was widely accepted and yielded excellent adherence at a substantially reduced coaching labor requirement when compared to the standard coaching group.
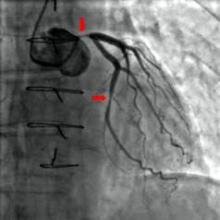
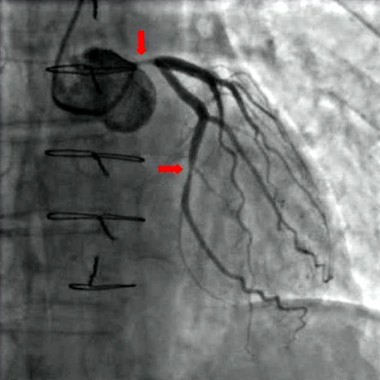
Angiography timing shown not a risk for AKI in most cardiac surgery
Acute kidney injury is a serious adverse effect of cardiac surgery, and contrast-induced nephropathy due to coronary angiography has been suggested as a potentially important component. However, the results of a retrospective study of more than 2,500 patients showed that acute kidney injury is significantly higher only in those patients who have combined cardiac surgery within 24 hours of catheterization.
The study by Dr. Giovanni Mariscalco of the Varese (Italy) University Hospital, and his colleagues assessed all consecutive patients undergoing cardiac surgery at the hospital between Jan. 1, 2005, and Dec. 31, 2011. The operations performed were isolated coronary artery bypass grafting (CABG), valve surgery with or without concomitant CABG, and proximal aortic procedures. After exclusion of patients who did not undergo cardiopulmonary bypass, a known major cause of acute kidney injury (AKI), and those who died during the procedure, a total of 2,504 patients remained. These patients had a mean age of 68.4 years and consisted mostly of men (67.3%), according to the report in the April issue of the International Journal of Cardiology.
The primary endpoint of the study was the effect of timing between cardiac catheterization and surgery on the development of AKI. Postoperative AKI was defined by the consensus RIFLE criteria (risk, injury, failure, loss of function, and end-stage renal disease), using the maximal change in serum creatinine and the estimated glomerular filtration rate during the first 7 days after surgery, compared with baseline values collected the day before surgery or immediately before surgery when cardiac catheterization was performed on the same day as the operation.
The researchers defined AKI as a 50% increase in the postoperative serum creatinine over baseline. Propensity analysis was used to match patients, who were then assessed both pre- and postmatch.
The overall incidence of AKI after surgery was 9.2% (230/2,504 patients). A breakdown by procedure showed that AKI occurred in 7.7% of isolated CABG patients, 12.2% of isolated valve patients, 9.5% of combined-procedure patients, and 9.5% of the proximal aorta surgery patients (Int. J. Cardiol. 2014;173:46-54).
As has been seen in previous studies, AKI was associated with patient-specific pre- and perioperative variables, including increased patient age, added comorbidities, longer cardiopulmonary bypass (CPB) times, higher rates of combined procedures, and the use of intra-aortic balloon pumps.
Unadjusted analysis of the total cohort showed AKI was significantly associated with contrast exposure within 1 day of surgery. However, in multivariable analysis, the time interval between catheterization and surgery as both a categorical and continuous variable was not an independent predictor of postoperative AKI for the total cohort. In subgroup analysis, only the combined valve and CABG group of patients showed an independent association of contrast exposure within 1 day before surgery and AKI in both the prematched (odds ratio, 2.69; P = .004) and the postmatched (OR, 3.68; P = .014) groups.
"Avoiding surgery within 1 day after contrast exposure should be recommended for patients undergoing valve surgery with concomitant CABG only. For other types of cardiac operations, delaying cardiac surgery after contrast exposure seems not to be justified," the researchers concluded.
Study limitations cited include its retrospective and single-institution nature and the statistical effect of different numbers of observations among the surgery groups. Patients affected with AKI also had higher rates of other postoperative complications, and AKI in some cases may have been the result of these rather than an independent event.
he study was supported by the Fondazione Cesare Bartorelli. The authors reported having no financial disclosures.
Acute kidney injury is a serious adverse effect of cardiac surgery, and contrast-induced nephropathy due to coronary angiography has been suggested as a potentially important component. However, the results of a retrospective study of more than 2,500 patients showed that acute kidney injury is significantly higher only in those patients who have combined cardiac surgery within 24 hours of catheterization.
The study by Dr. Giovanni Mariscalco of the Varese (Italy) University Hospital, and his colleagues assessed all consecutive patients undergoing cardiac surgery at the hospital between Jan. 1, 2005, and Dec. 31, 2011. The operations performed were isolated coronary artery bypass grafting (CABG), valve surgery with or without concomitant CABG, and proximal aortic procedures. After exclusion of patients who did not undergo cardiopulmonary bypass, a known major cause of acute kidney injury (AKI), and those who died during the procedure, a total of 2,504 patients remained. These patients had a mean age of 68.4 years and consisted mostly of men (67.3%), according to the report in the April issue of the International Journal of Cardiology.
The primary endpoint of the study was the effect of timing between cardiac catheterization and surgery on the development of AKI. Postoperative AKI was defined by the consensus RIFLE criteria (risk, injury, failure, loss of function, and end-stage renal disease), using the maximal change in serum creatinine and the estimated glomerular filtration rate during the first 7 days after surgery, compared with baseline values collected the day before surgery or immediately before surgery when cardiac catheterization was performed on the same day as the operation.
The researchers defined AKI as a 50% increase in the postoperative serum creatinine over baseline. Propensity analysis was used to match patients, who were then assessed both pre- and postmatch.
The overall incidence of AKI after surgery was 9.2% (230/2,504 patients). A breakdown by procedure showed that AKI occurred in 7.7% of isolated CABG patients, 12.2% of isolated valve patients, 9.5% of combined-procedure patients, and 9.5% of the proximal aorta surgery patients (Int. J. Cardiol. 2014;173:46-54).
As has been seen in previous studies, AKI was associated with patient-specific pre- and perioperative variables, including increased patient age, added comorbidities, longer cardiopulmonary bypass (CPB) times, higher rates of combined procedures, and the use of intra-aortic balloon pumps.
Unadjusted analysis of the total cohort showed AKI was significantly associated with contrast exposure within 1 day of surgery. However, in multivariable analysis, the time interval between catheterization and surgery as both a categorical and continuous variable was not an independent predictor of postoperative AKI for the total cohort. In subgroup analysis, only the combined valve and CABG group of patients showed an independent association of contrast exposure within 1 day before surgery and AKI in both the prematched (odds ratio, 2.69; P = .004) and the postmatched (OR, 3.68; P = .014) groups.
"Avoiding surgery within 1 day after contrast exposure should be recommended for patients undergoing valve surgery with concomitant CABG only. For other types of cardiac operations, delaying cardiac surgery after contrast exposure seems not to be justified," the researchers concluded.
Study limitations cited include its retrospective and single-institution nature and the statistical effect of different numbers of observations among the surgery groups. Patients affected with AKI also had higher rates of other postoperative complications, and AKI in some cases may have been the result of these rather than an independent event.
he study was supported by the Fondazione Cesare Bartorelli. The authors reported having no financial disclosures.
Acute kidney injury is a serious adverse effect of cardiac surgery, and contrast-induced nephropathy due to coronary angiography has been suggested as a potentially important component. However, the results of a retrospective study of more than 2,500 patients showed that acute kidney injury is significantly higher only in those patients who have combined cardiac surgery within 24 hours of catheterization.
The study by Dr. Giovanni Mariscalco of the Varese (Italy) University Hospital, and his colleagues assessed all consecutive patients undergoing cardiac surgery at the hospital between Jan. 1, 2005, and Dec. 31, 2011. The operations performed were isolated coronary artery bypass grafting (CABG), valve surgery with or without concomitant CABG, and proximal aortic procedures. After exclusion of patients who did not undergo cardiopulmonary bypass, a known major cause of acute kidney injury (AKI), and those who died during the procedure, a total of 2,504 patients remained. These patients had a mean age of 68.4 years and consisted mostly of men (67.3%), according to the report in the April issue of the International Journal of Cardiology.
The primary endpoint of the study was the effect of timing between cardiac catheterization and surgery on the development of AKI. Postoperative AKI was defined by the consensus RIFLE criteria (risk, injury, failure, loss of function, and end-stage renal disease), using the maximal change in serum creatinine and the estimated glomerular filtration rate during the first 7 days after surgery, compared with baseline values collected the day before surgery or immediately before surgery when cardiac catheterization was performed on the same day as the operation.
The researchers defined AKI as a 50% increase in the postoperative serum creatinine over baseline. Propensity analysis was used to match patients, who were then assessed both pre- and postmatch.
The overall incidence of AKI after surgery was 9.2% (230/2,504 patients). A breakdown by procedure showed that AKI occurred in 7.7% of isolated CABG patients, 12.2% of isolated valve patients, 9.5% of combined-procedure patients, and 9.5% of the proximal aorta surgery patients (Int. J. Cardiol. 2014;173:46-54).
As has been seen in previous studies, AKI was associated with patient-specific pre- and perioperative variables, including increased patient age, added comorbidities, longer cardiopulmonary bypass (CPB) times, higher rates of combined procedures, and the use of intra-aortic balloon pumps.
Unadjusted analysis of the total cohort showed AKI was significantly associated with contrast exposure within 1 day of surgery. However, in multivariable analysis, the time interval between catheterization and surgery as both a categorical and continuous variable was not an independent predictor of postoperative AKI for the total cohort. In subgroup analysis, only the combined valve and CABG group of patients showed an independent association of contrast exposure within 1 day before surgery and AKI in both the prematched (odds ratio, 2.69; P = .004) and the postmatched (OR, 3.68; P = .014) groups.
"Avoiding surgery within 1 day after contrast exposure should be recommended for patients undergoing valve surgery with concomitant CABG only. For other types of cardiac operations, delaying cardiac surgery after contrast exposure seems not to be justified," the researchers concluded.
Study limitations cited include its retrospective and single-institution nature and the statistical effect of different numbers of observations among the surgery groups. Patients affected with AKI also had higher rates of other postoperative complications, and AKI in some cases may have been the result of these rather than an independent event.
he study was supported by the Fondazione Cesare Bartorelli. The authors reported having no financial disclosures.
FROM THE INTERNATIONAL JOURNAL OF CARDIOLOGY
Major finding: Only combined surgery plus contrast within 1 day before surgery was significantly associated with AKI in the prematched (OR, 2.69) and postmatched (OR, 3.68) groups.
Data source: A single-institute, retrospective study of 2,504 cardiac surgery patients.
Disclosures: The study was supported by the Fondazione Cesare Bartorelli. The authors reported having no financial disclosures.
Post-LVAD acute kidney injury is predictor of all-cause mortality
Acute kidney injury is not only common after implantation of a left ventricular assist device, it is also an independent predictor of 30-day and 1-year all-cause mortality, according to a retrospective, single-institution study.
In addition, multivariate analysis showed that only diabetes was a significant predictor of post-LVAD implantation acute kidney injury (AKI), the investigators stated in the report published online Feb. 15 in the American Journal of Nephrology.
Dr. Abhijit Naik and Dr. Jay L. Koyner of the section of nephrology at the University of Chicago and their colleagues identified 168 patients who underwent LVAD implantation at the university. They excluded 11 patients because of previous end-stage renal disease and intraoperative mortality. The remaining cohort of 157 patients served as their study population, which was 78% men and 58% white and had a mean age of around 57 years (Am. J. Nephrol. 2014 Feb. 15 [doi:10.1159/000358495]).
The obtained demographic, biochemical, and clinical profiles from the national Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS), the Society of Thoracic Surgeons (STS) database, and the University of Chicago medical record (EMR). Baseline creatinine was defined as the listing of creatinine data obtained from the INTERMACS registry, or failing that, the last serum creatinine in the EMR prior to device implantation.
They defined the primary outcome of AKI as a 50% rise in serum creatinine over the preoperative baseline during the first 7 postoperative days. All-cause mortality was monitored over 1 year after implantation, with data reported at 30 and 365 days.
A total of 44 of 157 (28%) of patients developed AKI based on the study criteria. The only significant baseline differences between the patients with and without AKI were the presence of diabetes and cerebrovascular disease (CVD), each significantly higher in the patients who developed AKI.
Univariate analysis showed CVD and diabetes as significant predictors of developing AKI, but upon multivariate analysis, only diabetes retained significance (odds ratio, 2.27; P = .04).
As for mortality, only AKI (hazard ratio, 3.01; P = .03) and cardiopulmonary bypass time (HR, 1.01; P = .02) were significant predictors of 30-day mortality. Preoperative diabetes mellitus (HR, 1.9; P = .03) or postimplantation AKI (HR, 1.85; P = .03) were significant independent predictors of 1-year mortality. Higher preoperative body mass index was significantly and slightly protective (HR, 0.95; P = .03).
The authors stated that the strength of their study was that it is the largest cohort study of LVAD patients to employ a consensus definition of AKI; limitations were its single-center and retrospective nature and the use of database reviews.
As AKI is a common adverse outcome following traditional cardiac surgery, including coronary artery bypass grafting and/or valve replacement, more research is needed to tease out any differences unique to LVAD implantation, the investigators said.
"Given the high AKI rates and the mounting evidence linking AKI to mortality following VAD implantation, the use of biomarkers to identify patients at risk may have a role. Large prospective multicenter trials are needed to develop a risk stratification system to identify patients at risk for developing post-VAD implantation AKI," the researchers concluded.
Dr. Koyner was supported by a K23 grant from the National Institutes of Health. One of the coauthors reported research funding from Thoratec and another reported consulting fees from Thoratec and HeartWare. The other authors reported no disclosures.
Acute kidney injury is not only common after implantation of a left ventricular assist device, it is also an independent predictor of 30-day and 1-year all-cause mortality, according to a retrospective, single-institution study.
In addition, multivariate analysis showed that only diabetes was a significant predictor of post-LVAD implantation acute kidney injury (AKI), the investigators stated in the report published online Feb. 15 in the American Journal of Nephrology.
Dr. Abhijit Naik and Dr. Jay L. Koyner of the section of nephrology at the University of Chicago and their colleagues identified 168 patients who underwent LVAD implantation at the university. They excluded 11 patients because of previous end-stage renal disease and intraoperative mortality. The remaining cohort of 157 patients served as their study population, which was 78% men and 58% white and had a mean age of around 57 years (Am. J. Nephrol. 2014 Feb. 15 [doi:10.1159/000358495]).
The obtained demographic, biochemical, and clinical profiles from the national Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS), the Society of Thoracic Surgeons (STS) database, and the University of Chicago medical record (EMR). Baseline creatinine was defined as the listing of creatinine data obtained from the INTERMACS registry, or failing that, the last serum creatinine in the EMR prior to device implantation.
They defined the primary outcome of AKI as a 50% rise in serum creatinine over the preoperative baseline during the first 7 postoperative days. All-cause mortality was monitored over 1 year after implantation, with data reported at 30 and 365 days.
A total of 44 of 157 (28%) of patients developed AKI based on the study criteria. The only significant baseline differences between the patients with and without AKI were the presence of diabetes and cerebrovascular disease (CVD), each significantly higher in the patients who developed AKI.
Univariate analysis showed CVD and diabetes as significant predictors of developing AKI, but upon multivariate analysis, only diabetes retained significance (odds ratio, 2.27; P = .04).
As for mortality, only AKI (hazard ratio, 3.01; P = .03) and cardiopulmonary bypass time (HR, 1.01; P = .02) were significant predictors of 30-day mortality. Preoperative diabetes mellitus (HR, 1.9; P = .03) or postimplantation AKI (HR, 1.85; P = .03) were significant independent predictors of 1-year mortality. Higher preoperative body mass index was significantly and slightly protective (HR, 0.95; P = .03).
The authors stated that the strength of their study was that it is the largest cohort study of LVAD patients to employ a consensus definition of AKI; limitations were its single-center and retrospective nature and the use of database reviews.
As AKI is a common adverse outcome following traditional cardiac surgery, including coronary artery bypass grafting and/or valve replacement, more research is needed to tease out any differences unique to LVAD implantation, the investigators said.
"Given the high AKI rates and the mounting evidence linking AKI to mortality following VAD implantation, the use of biomarkers to identify patients at risk may have a role. Large prospective multicenter trials are needed to develop a risk stratification system to identify patients at risk for developing post-VAD implantation AKI," the researchers concluded.
Dr. Koyner was supported by a K23 grant from the National Institutes of Health. One of the coauthors reported research funding from Thoratec and another reported consulting fees from Thoratec and HeartWare. The other authors reported no disclosures.
Acute kidney injury is not only common after implantation of a left ventricular assist device, it is also an independent predictor of 30-day and 1-year all-cause mortality, according to a retrospective, single-institution study.
In addition, multivariate analysis showed that only diabetes was a significant predictor of post-LVAD implantation acute kidney injury (AKI), the investigators stated in the report published online Feb. 15 in the American Journal of Nephrology.
Dr. Abhijit Naik and Dr. Jay L. Koyner of the section of nephrology at the University of Chicago and their colleagues identified 168 patients who underwent LVAD implantation at the university. They excluded 11 patients because of previous end-stage renal disease and intraoperative mortality. The remaining cohort of 157 patients served as their study population, which was 78% men and 58% white and had a mean age of around 57 years (Am. J. Nephrol. 2014 Feb. 15 [doi:10.1159/000358495]).
The obtained demographic, biochemical, and clinical profiles from the national Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS), the Society of Thoracic Surgeons (STS) database, and the University of Chicago medical record (EMR). Baseline creatinine was defined as the listing of creatinine data obtained from the INTERMACS registry, or failing that, the last serum creatinine in the EMR prior to device implantation.
They defined the primary outcome of AKI as a 50% rise in serum creatinine over the preoperative baseline during the first 7 postoperative days. All-cause mortality was monitored over 1 year after implantation, with data reported at 30 and 365 days.
A total of 44 of 157 (28%) of patients developed AKI based on the study criteria. The only significant baseline differences between the patients with and without AKI were the presence of diabetes and cerebrovascular disease (CVD), each significantly higher in the patients who developed AKI.
Univariate analysis showed CVD and diabetes as significant predictors of developing AKI, but upon multivariate analysis, only diabetes retained significance (odds ratio, 2.27; P = .04).
As for mortality, only AKI (hazard ratio, 3.01; P = .03) and cardiopulmonary bypass time (HR, 1.01; P = .02) were significant predictors of 30-day mortality. Preoperative diabetes mellitus (HR, 1.9; P = .03) or postimplantation AKI (HR, 1.85; P = .03) were significant independent predictors of 1-year mortality. Higher preoperative body mass index was significantly and slightly protective (HR, 0.95; P = .03).
The authors stated that the strength of their study was that it is the largest cohort study of LVAD patients to employ a consensus definition of AKI; limitations were its single-center and retrospective nature and the use of database reviews.
As AKI is a common adverse outcome following traditional cardiac surgery, including coronary artery bypass grafting and/or valve replacement, more research is needed to tease out any differences unique to LVAD implantation, the investigators said.
"Given the high AKI rates and the mounting evidence linking AKI to mortality following VAD implantation, the use of biomarkers to identify patients at risk may have a role. Large prospective multicenter trials are needed to develop a risk stratification system to identify patients at risk for developing post-VAD implantation AKI," the researchers concluded.
Dr. Koyner was supported by a K23 grant from the National Institutes of Health. One of the coauthors reported research funding from Thoratec and another reported consulting fees from Thoratec and HeartWare. The other authors reported no disclosures.
FROM THE AMERICAN JOURNAL OF NEPHROLOGY
Major finding: Acute kidney injury was a significant predictor of 30-day mortality (hazard ratio, 3.01; P = .03) in patients who had implantation of a left ventricular assist device.
Data source: A retrospective, single-institution study using INTERMACS and STS databases with a sample of 168 patients who had undergone LVAD implantation.
Disclosures: Dr. Koyner was supported by a K23 grant from the National Institutes of Health. One of the coauthors reported research funding from Thoratec and another reported consulting fees from Thoratec and HeartWare. The other authors reported no disclosures.
Novel Watchman antistroke device backed as warfarin equivalent
GAITHERSBURG, MD – A Food and Drug Administration advisory panel has voted in favor of approving the Watchman Left Atrial Appendage Closure Device for patients with nonvalvular atrial fibrillation. One of the panelists described the device as "transformative technology," as it is the first device alternative to medical therapy for the prevention of stroke due to atrial fibrillation to be approved in the United States.
At a meeting on Dec. 11, the FDA Circulatory System Devices Panel of the Medical Devices Advisory Committee voted 13-1 to recommend approval of Boston Scientific’s Watchman Left Atrial Appendage Closure (LAAC) Therapy, a percutaneously delivered permanent cardiac implant placed in the left atrial appendage for the prevention of thromboembolism from the left atrial appendage. If approved, the indication will be for patients with nonvalvular atrial fibrillation who are eligible for warfarin therapy to reduce the risk of stroke and systemic embolism based on CHADS2 or CHA2DS2-VASc scores. In addition, the panel recommended and the company echoed that the final indication language should make clear that the therapy should be only for warfarin-eligible patients who had a significant reason not to remain on chronic anticoagulation therapy.
Dr. Rachel Neubrander of the FDA detailed how the device previously was reviewed by an FDA panel in 2009, and ultimately was not approved because of the agency’s and an advisory panel’s significant concerns about the design of the pivotal PROTECT-AF trial, which included low-risk patients with a CHADS2 score of 1 and also included patients indicated for chronic clopidogrel therapy.
In concert with the FDA, Boston Scientific developed the PREVAIL trial to address those concerns. PREVAIL enrolled only high-risk subjects with CHADS2 scores of at least 2 and those with a CHADS2 score of 1 who had additional stroke risk factors present and were recommended for warfarin therapy by ACC/AHA/ESC 2006 guidelines.
In addition, PREVAIL excluded subjects indicated for chronic clopidogrel therapy. Because 56% of primary safety events in the device group occurred on the day of the procedure in the PROTECT-AF trial, and there was evidence of a significant learning curve, PREVAIL was designed to require at least 20% of the subjects to be implanted at new investigational sites and at least 25% of the subjects to be implanted by new operators.
At the current meeting, the device was recommended for approval based upon the totality of the data obtained from both the PROTECT-AF and PREVAIL trials, and information from the Continued Access to PREVAIL (CAP2) registry, according to the majority of the panelists, who indicated that the data from the PREVAIL trial alone was premature for such a determination based upon the current lack of long-term data, compared with the PROTECT-AF trial.
The panel stated that it was impressed by the greatly reduced incidence of perioperative primary safety events in PREVAIL compared with PROTECT-AF, and the success of Boston Scientific’s training protocol to ensure that new operators performed as well as or better than experienced operators. The panel thus suggested that some definition of the site requirements and training requirements instituted by the company for the PREVAIL trial be included in the final label.
Of concern, PREVAIL failed to meet its primary endpoint of noninferiority compared with warfarin with regard to the composite 18-month rate of stroke, systemic embolism, and cardiovascular or unexplained death. This was attributed to the fact that the PREVAIL trial had accumulated 18-month data on fewer than 30% of the patients at the point of analysis. The great majority of the panel concluded that the trend of PREVAIL, when combined in a Bayesien analysis with 50% discounted data from the patients with CHADS2 scores of at least 2 in the PROTECT-AF trial, and taking into account the CAP registry, was acceptable. The lone dissenting panel member said that this lack of complete PREVAIL data and the fact that it technically did not meet its primary endpoint were his reasons for voting against approval.
The panel concluded that the Watchman device data supported the hypothesis of left atrial appendage thromboembolism as the major source of stroke due to atrial fibrillation and that the device was noninferior to warfarin in preventing such strokes once the initial perioperative period of 7 days was passed. They said that because there was a periprocedural primary adverse event risk, the device should not be considered as a substitute for warfarin in all patients, but only in those for whom warfarin compliance over the long term was a significant problem whether from patient lifestyle or medical reasons.
Of additional concern, the panel noted that there was no evidence that the Watchman device was superior to warfarin therapy with regard to the elimination of major bleeding events. During the open portion of the panel meeting, patients and their doctors nearly unanimously indicated their preference for the Watchman technology over warfarin because of their fear of and experience of frequent and significant bleeds while on anticoagulation. The panel suggested that, because of this apparent common misperception, the lack of bleeding benefit should be pointed out in the final indication language.
The panel agreed with FDA’s concern that a postmarketing study should be conducted if the device is approved, and that the study should be large enough to answer some of the concerns brought up in the meeting as to long-term results, including safety and efficacy in a broader population than that studied in the two trials, which was overwhelmingly white, and predominately male.
The FDA usually follows the recommendations of its advisory panels. Members of FDA panels have usually been cleared of conflicts related to the product under review; occasionally, a panelist is given a waiver, but not at this meeting.
The Watchman device has been approved in Europe since 2005.
Dr. Rachel Neubrander,
GAITHERSBURG, MD – A Food and Drug Administration advisory panel has voted in favor of approving the Watchman Left Atrial Appendage Closure Device for patients with nonvalvular atrial fibrillation. One of the panelists described the device as "transformative technology," as it is the first device alternative to medical therapy for the prevention of stroke due to atrial fibrillation to be approved in the United States.
At a meeting on Dec. 11, the FDA Circulatory System Devices Panel of the Medical Devices Advisory Committee voted 13-1 to recommend approval of Boston Scientific’s Watchman Left Atrial Appendage Closure (LAAC) Therapy, a percutaneously delivered permanent cardiac implant placed in the left atrial appendage for the prevention of thromboembolism from the left atrial appendage. If approved, the indication will be for patients with nonvalvular atrial fibrillation who are eligible for warfarin therapy to reduce the risk of stroke and systemic embolism based on CHADS2 or CHA2DS2-VASc scores. In addition, the panel recommended and the company echoed that the final indication language should make clear that the therapy should be only for warfarin-eligible patients who had a significant reason not to remain on chronic anticoagulation therapy.
Dr. Rachel Neubrander of the FDA detailed how the device previously was reviewed by an FDA panel in 2009, and ultimately was not approved because of the agency’s and an advisory panel’s significant concerns about the design of the pivotal PROTECT-AF trial, which included low-risk patients with a CHADS2 score of 1 and also included patients indicated for chronic clopidogrel therapy.
In concert with the FDA, Boston Scientific developed the PREVAIL trial to address those concerns. PREVAIL enrolled only high-risk subjects with CHADS2 scores of at least 2 and those with a CHADS2 score of 1 who had additional stroke risk factors present and were recommended for warfarin therapy by ACC/AHA/ESC 2006 guidelines.
In addition, PREVAIL excluded subjects indicated for chronic clopidogrel therapy. Because 56% of primary safety events in the device group occurred on the day of the procedure in the PROTECT-AF trial, and there was evidence of a significant learning curve, PREVAIL was designed to require at least 20% of the subjects to be implanted at new investigational sites and at least 25% of the subjects to be implanted by new operators.
At the current meeting, the device was recommended for approval based upon the totality of the data obtained from both the PROTECT-AF and PREVAIL trials, and information from the Continued Access to PREVAIL (CAP2) registry, according to the majority of the panelists, who indicated that the data from the PREVAIL trial alone was premature for such a determination based upon the current lack of long-term data, compared with the PROTECT-AF trial.
The panel stated that it was impressed by the greatly reduced incidence of perioperative primary safety events in PREVAIL compared with PROTECT-AF, and the success of Boston Scientific’s training protocol to ensure that new operators performed as well as or better than experienced operators. The panel thus suggested that some definition of the site requirements and training requirements instituted by the company for the PREVAIL trial be included in the final label.
Of concern, PREVAIL failed to meet its primary endpoint of noninferiority compared with warfarin with regard to the composite 18-month rate of stroke, systemic embolism, and cardiovascular or unexplained death. This was attributed to the fact that the PREVAIL trial had accumulated 18-month data on fewer than 30% of the patients at the point of analysis. The great majority of the panel concluded that the trend of PREVAIL, when combined in a Bayesien analysis with 50% discounted data from the patients with CHADS2 scores of at least 2 in the PROTECT-AF trial, and taking into account the CAP registry, was acceptable. The lone dissenting panel member said that this lack of complete PREVAIL data and the fact that it technically did not meet its primary endpoint were his reasons for voting against approval.
The panel concluded that the Watchman device data supported the hypothesis of left atrial appendage thromboembolism as the major source of stroke due to atrial fibrillation and that the device was noninferior to warfarin in preventing such strokes once the initial perioperative period of 7 days was passed. They said that because there was a periprocedural primary adverse event risk, the device should not be considered as a substitute for warfarin in all patients, but only in those for whom warfarin compliance over the long term was a significant problem whether from patient lifestyle or medical reasons.
Of additional concern, the panel noted that there was no evidence that the Watchman device was superior to warfarin therapy with regard to the elimination of major bleeding events. During the open portion of the panel meeting, patients and their doctors nearly unanimously indicated their preference for the Watchman technology over warfarin because of their fear of and experience of frequent and significant bleeds while on anticoagulation. The panel suggested that, because of this apparent common misperception, the lack of bleeding benefit should be pointed out in the final indication language.
The panel agreed with FDA’s concern that a postmarketing study should be conducted if the device is approved, and that the study should be large enough to answer some of the concerns brought up in the meeting as to long-term results, including safety and efficacy in a broader population than that studied in the two trials, which was overwhelmingly white, and predominately male.
The FDA usually follows the recommendations of its advisory panels. Members of FDA panels have usually been cleared of conflicts related to the product under review; occasionally, a panelist is given a waiver, but not at this meeting.
The Watchman device has been approved in Europe since 2005.
GAITHERSBURG, MD – A Food and Drug Administration advisory panel has voted in favor of approving the Watchman Left Atrial Appendage Closure Device for patients with nonvalvular atrial fibrillation. One of the panelists described the device as "transformative technology," as it is the first device alternative to medical therapy for the prevention of stroke due to atrial fibrillation to be approved in the United States.
At a meeting on Dec. 11, the FDA Circulatory System Devices Panel of the Medical Devices Advisory Committee voted 13-1 to recommend approval of Boston Scientific’s Watchman Left Atrial Appendage Closure (LAAC) Therapy, a percutaneously delivered permanent cardiac implant placed in the left atrial appendage for the prevention of thromboembolism from the left atrial appendage. If approved, the indication will be for patients with nonvalvular atrial fibrillation who are eligible for warfarin therapy to reduce the risk of stroke and systemic embolism based on CHADS2 or CHA2DS2-VASc scores. In addition, the panel recommended and the company echoed that the final indication language should make clear that the therapy should be only for warfarin-eligible patients who had a significant reason not to remain on chronic anticoagulation therapy.
Dr. Rachel Neubrander of the FDA detailed how the device previously was reviewed by an FDA panel in 2009, and ultimately was not approved because of the agency’s and an advisory panel’s significant concerns about the design of the pivotal PROTECT-AF trial, which included low-risk patients with a CHADS2 score of 1 and also included patients indicated for chronic clopidogrel therapy.
In concert with the FDA, Boston Scientific developed the PREVAIL trial to address those concerns. PREVAIL enrolled only high-risk subjects with CHADS2 scores of at least 2 and those with a CHADS2 score of 1 who had additional stroke risk factors present and were recommended for warfarin therapy by ACC/AHA/ESC 2006 guidelines.
In addition, PREVAIL excluded subjects indicated for chronic clopidogrel therapy. Because 56% of primary safety events in the device group occurred on the day of the procedure in the PROTECT-AF trial, and there was evidence of a significant learning curve, PREVAIL was designed to require at least 20% of the subjects to be implanted at new investigational sites and at least 25% of the subjects to be implanted by new operators.
At the current meeting, the device was recommended for approval based upon the totality of the data obtained from both the PROTECT-AF and PREVAIL trials, and information from the Continued Access to PREVAIL (CAP2) registry, according to the majority of the panelists, who indicated that the data from the PREVAIL trial alone was premature for such a determination based upon the current lack of long-term data, compared with the PROTECT-AF trial.
The panel stated that it was impressed by the greatly reduced incidence of perioperative primary safety events in PREVAIL compared with PROTECT-AF, and the success of Boston Scientific’s training protocol to ensure that new operators performed as well as or better than experienced operators. The panel thus suggested that some definition of the site requirements and training requirements instituted by the company for the PREVAIL trial be included in the final label.
Of concern, PREVAIL failed to meet its primary endpoint of noninferiority compared with warfarin with regard to the composite 18-month rate of stroke, systemic embolism, and cardiovascular or unexplained death. This was attributed to the fact that the PREVAIL trial had accumulated 18-month data on fewer than 30% of the patients at the point of analysis. The great majority of the panel concluded that the trend of PREVAIL, when combined in a Bayesien analysis with 50% discounted data from the patients with CHADS2 scores of at least 2 in the PROTECT-AF trial, and taking into account the CAP registry, was acceptable. The lone dissenting panel member said that this lack of complete PREVAIL data and the fact that it technically did not meet its primary endpoint were his reasons for voting against approval.
The panel concluded that the Watchman device data supported the hypothesis of left atrial appendage thromboembolism as the major source of stroke due to atrial fibrillation and that the device was noninferior to warfarin in preventing such strokes once the initial perioperative period of 7 days was passed. They said that because there was a periprocedural primary adverse event risk, the device should not be considered as a substitute for warfarin in all patients, but only in those for whom warfarin compliance over the long term was a significant problem whether from patient lifestyle or medical reasons.
Of additional concern, the panel noted that there was no evidence that the Watchman device was superior to warfarin therapy with regard to the elimination of major bleeding events. During the open portion of the panel meeting, patients and their doctors nearly unanimously indicated their preference for the Watchman technology over warfarin because of their fear of and experience of frequent and significant bleeds while on anticoagulation. The panel suggested that, because of this apparent common misperception, the lack of bleeding benefit should be pointed out in the final indication language.
The panel agreed with FDA’s concern that a postmarketing study should be conducted if the device is approved, and that the study should be large enough to answer some of the concerns brought up in the meeting as to long-term results, including safety and efficacy in a broader population than that studied in the two trials, which was overwhelmingly white, and predominately male.
The FDA usually follows the recommendations of its advisory panels. Members of FDA panels have usually been cleared of conflicts related to the product under review; occasionally, a panelist is given a waiver, but not at this meeting.
The Watchman device has been approved in Europe since 2005.
Dr. Rachel Neubrander,
Dr. Rachel Neubrander,
AT AN FDA ADVISORY COMMITTEE MEETING
Spouses surveyed report influence on CTS applicant decision making
A resident’s ability to balance work and personal life is dependent on multiple factors, with spousal or partner approval likely comprising one of the most important, according to a report published in the Journal of Surgical Education. The report details the results of an electronic survey sent to thoracic surgery spouses via contact with all thoracic surgery residents over 2 years at two training programs and all current thoracic surgery residents in 2010.
A total of 66 surveys were completed and returned (a response rate of 19%), with 86% of the respondents being women, and 82% being married for a mean of 4.3 years; 59% had children, and 64% were planning on having more children within 3 years.
Nearly 90%of the spouses responding reported that they want to travel to more of the interviews, and that they had some to complete influence on which training program to attend, according to Mr. Michael Bohl and Dr. Rishindra M. Reddy of the Section of Thoracic Surgery at the University of Michigan, Ann Arbor (J. Surg. Education 2013;70:640-6).
Nearly 80% of the respondents also reported that they wanted more information on salary and on housing, as well as access to faculty spouses. The top 3 factors in chosing a program they reported were: quality of fellowship, geographic location, and proximity to family.
Knowledge of the extent of influence and the desires of spouses with regard to CTStraining positions might allow targeting these needs at a point early enough in the process to help capture general surgery residents interested in but not committed to CTS residency, the researchers suggested.
"The results show numerous demographic and characteristic trends which, if further validated by definitive studies, would be applicable to all post-surgery residency training programs and may help CTS programs to be more competitive in attracting applicants and their families.
The authors had no relevant disclosures.
A resident’s ability to balance work and personal life is dependent on multiple factors, with spousal or partner approval likely comprising one of the most important, according to a report published in the Journal of Surgical Education. The report details the results of an electronic survey sent to thoracic surgery spouses via contact with all thoracic surgery residents over 2 years at two training programs and all current thoracic surgery residents in 2010.
A total of 66 surveys were completed and returned (a response rate of 19%), with 86% of the respondents being women, and 82% being married for a mean of 4.3 years; 59% had children, and 64% were planning on having more children within 3 years.
Nearly 90%of the spouses responding reported that they want to travel to more of the interviews, and that they had some to complete influence on which training program to attend, according to Mr. Michael Bohl and Dr. Rishindra M. Reddy of the Section of Thoracic Surgery at the University of Michigan, Ann Arbor (J. Surg. Education 2013;70:640-6).
Nearly 80% of the respondents also reported that they wanted more information on salary and on housing, as well as access to faculty spouses. The top 3 factors in chosing a program they reported were: quality of fellowship, geographic location, and proximity to family.
Knowledge of the extent of influence and the desires of spouses with regard to CTStraining positions might allow targeting these needs at a point early enough in the process to help capture general surgery residents interested in but not committed to CTS residency, the researchers suggested.
"The results show numerous demographic and characteristic trends which, if further validated by definitive studies, would be applicable to all post-surgery residency training programs and may help CTS programs to be more competitive in attracting applicants and their families.
The authors had no relevant disclosures.
A resident’s ability to balance work and personal life is dependent on multiple factors, with spousal or partner approval likely comprising one of the most important, according to a report published in the Journal of Surgical Education. The report details the results of an electronic survey sent to thoracic surgery spouses via contact with all thoracic surgery residents over 2 years at two training programs and all current thoracic surgery residents in 2010.
A total of 66 surveys were completed and returned (a response rate of 19%), with 86% of the respondents being women, and 82% being married for a mean of 4.3 years; 59% had children, and 64% were planning on having more children within 3 years.
Nearly 90%of the spouses responding reported that they want to travel to more of the interviews, and that they had some to complete influence on which training program to attend, according to Mr. Michael Bohl and Dr. Rishindra M. Reddy of the Section of Thoracic Surgery at the University of Michigan, Ann Arbor (J. Surg. Education 2013;70:640-6).
Nearly 80% of the respondents also reported that they wanted more information on salary and on housing, as well as access to faculty spouses. The top 3 factors in chosing a program they reported were: quality of fellowship, geographic location, and proximity to family.
Knowledge of the extent of influence and the desires of spouses with regard to CTStraining positions might allow targeting these needs at a point early enough in the process to help capture general surgery residents interested in but not committed to CTS residency, the researchers suggested.
"The results show numerous demographic and characteristic trends which, if further validated by definitive studies, would be applicable to all post-surgery residency training programs and may help CTS programs to be more competitive in attracting applicants and their families.
The authors had no relevant disclosures.
Fruits, but not vegetables, shown to lower AAA risk
The consumption of fruits, but not vegetables, was associated with a decreased risk of abdominal aortic aneurysm, especially the risk of rupture, according to results of a large database study of two prospective cohorts of Swedish men and women.
"The risk of AAA decreased with increasing consumption of fruit (P =.003), whereas no significant association was observed for vegetable consumption," wrote Dr. Otto Stackelberg and his colleagues at Uppsala (Sweden) University (Circulation 2013;128:795-802).
The study population in the final analysis of the two cohorts consisted of 36,109 women from the Swedish Mammography Cohort (established between 1987 and 1990) and 44,317 men from the Cohort of Swedish Men (established in 1997).
Both cohorts responded in 1997 to extensive questionnaires – identical except for sex-specific questions – that included 96 food-item questions accompanied by other lifestyle factors. Results were linked to the Swedish Inpatient Register and the Swedish National Cause of Death Register to follow outcomes of these patients.
National health coverage in Sweden has been nearly 100% since 1987. All cases of AAA were identified by clinical events, not by general screening. AAA repair was identified via the Nordic Classification of Surgical Procedures. To classify aneurysmal localization and rupture status of AAA repairs, the researchers linked the cohorts to the Swedish Registry for Vascular Surgery (founded in 1987, which accounted for 93.1% of all AAA repairs in Sweden).
Fruit and vegetable consumption was summed from results of the 96 food item questionnaire and converted to daily consumption categories ranging from never to greater than or equal to 3 times daily.
Covariates assessed included education, alcohol consumption, diet, physical activity, waist circumference, and smoking duration and amount. The study population was ethnically homogenous. History of cardiovascular disease, diabetes, hypertension, and hypercholesterolemia was obtained from the Swedish Inpatient Register, the Swedish National Diabetes Register, and the self-reported data from the questionnaire.
During 13 years of follow-up (1998-2010), the researchers found that there were 1,086 primary cases (899 in men; 83%) and 222 cases of ruptured AAA (181 in men; 82%). The mean age for nonruptured AAA was 74 years in men and 76 years in women. For ruptured AAA it was 76 and 78.5 years in men and women, respectively. Cox proportional hazard analysis was used to estimate hazard ratios.
Individuals in the highest quartile of fruit consumption (greater than 2 servings per day) had a 25% lower risk of AAA and a 43% lower risk of ruptured AAA, compared with those in the lowest quartiles of fruit consumption (less than 0.7 servings per day). No association was observed between vegetable consumption and AAA risk. There was no impact of smoking or sex of the individual on the fruit consumption–related AAA risk for both ruptured and nonruptured AAA.
Men and women with a high consumption of fruit and vegetables were more educated; consumed more fish, meat, and whole grains; and were more likely to be leaner and physically active, and less likely to be smokers, according to the researchers. In addition, high consumers of fruit consumed less alcohol, whereas the reverse was true of high consumers of vegetables.
"A diet high in fruits may help to prevent many vascular diseases, and this study provides evidence that a lower risk of AAA will be among the benefits," the researchers concluded.
The study was funded by grants from the Swedish Research Council and the Karolinska Institute. The authors reported they had no disclosures.
So I guess the old adage is correct ... "An apple a day keeps the doctor away," or should I say "An Apple A day keeps the AAA Away?"
Dr. Russell Samson is the Medical Editor of Vascular Specialist.
So I guess the old adage is correct ... "An apple a day keeps the doctor away," or should I say "An Apple A day keeps the AAA Away?"
Dr. Russell Samson is the Medical Editor of Vascular Specialist.
So I guess the old adage is correct ... "An apple a day keeps the doctor away," or should I say "An Apple A day keeps the AAA Away?"
Dr. Russell Samson is the Medical Editor of Vascular Specialist.
The consumption of fruits, but not vegetables, was associated with a decreased risk of abdominal aortic aneurysm, especially the risk of rupture, according to results of a large database study of two prospective cohorts of Swedish men and women.
"The risk of AAA decreased with increasing consumption of fruit (P =.003), whereas no significant association was observed for vegetable consumption," wrote Dr. Otto Stackelberg and his colleagues at Uppsala (Sweden) University (Circulation 2013;128:795-802).
The study population in the final analysis of the two cohorts consisted of 36,109 women from the Swedish Mammography Cohort (established between 1987 and 1990) and 44,317 men from the Cohort of Swedish Men (established in 1997).
Both cohorts responded in 1997 to extensive questionnaires – identical except for sex-specific questions – that included 96 food-item questions accompanied by other lifestyle factors. Results were linked to the Swedish Inpatient Register and the Swedish National Cause of Death Register to follow outcomes of these patients.
National health coverage in Sweden has been nearly 100% since 1987. All cases of AAA were identified by clinical events, not by general screening. AAA repair was identified via the Nordic Classification of Surgical Procedures. To classify aneurysmal localization and rupture status of AAA repairs, the researchers linked the cohorts to the Swedish Registry for Vascular Surgery (founded in 1987, which accounted for 93.1% of all AAA repairs in Sweden).
Fruit and vegetable consumption was summed from results of the 96 food item questionnaire and converted to daily consumption categories ranging from never to greater than or equal to 3 times daily.
Covariates assessed included education, alcohol consumption, diet, physical activity, waist circumference, and smoking duration and amount. The study population was ethnically homogenous. History of cardiovascular disease, diabetes, hypertension, and hypercholesterolemia was obtained from the Swedish Inpatient Register, the Swedish National Diabetes Register, and the self-reported data from the questionnaire.
During 13 years of follow-up (1998-2010), the researchers found that there were 1,086 primary cases (899 in men; 83%) and 222 cases of ruptured AAA (181 in men; 82%). The mean age for nonruptured AAA was 74 years in men and 76 years in women. For ruptured AAA it was 76 and 78.5 years in men and women, respectively. Cox proportional hazard analysis was used to estimate hazard ratios.
Individuals in the highest quartile of fruit consumption (greater than 2 servings per day) had a 25% lower risk of AAA and a 43% lower risk of ruptured AAA, compared with those in the lowest quartiles of fruit consumption (less than 0.7 servings per day). No association was observed between vegetable consumption and AAA risk. There was no impact of smoking or sex of the individual on the fruit consumption–related AAA risk for both ruptured and nonruptured AAA.
Men and women with a high consumption of fruit and vegetables were more educated; consumed more fish, meat, and whole grains; and were more likely to be leaner and physically active, and less likely to be smokers, according to the researchers. In addition, high consumers of fruit consumed less alcohol, whereas the reverse was true of high consumers of vegetables.
"A diet high in fruits may help to prevent many vascular diseases, and this study provides evidence that a lower risk of AAA will be among the benefits," the researchers concluded.
The study was funded by grants from the Swedish Research Council and the Karolinska Institute. The authors reported they had no disclosures.
The consumption of fruits, but not vegetables, was associated with a decreased risk of abdominal aortic aneurysm, especially the risk of rupture, according to results of a large database study of two prospective cohorts of Swedish men and women.
"The risk of AAA decreased with increasing consumption of fruit (P =.003), whereas no significant association was observed for vegetable consumption," wrote Dr. Otto Stackelberg and his colleagues at Uppsala (Sweden) University (Circulation 2013;128:795-802).
The study population in the final analysis of the two cohorts consisted of 36,109 women from the Swedish Mammography Cohort (established between 1987 and 1990) and 44,317 men from the Cohort of Swedish Men (established in 1997).
Both cohorts responded in 1997 to extensive questionnaires – identical except for sex-specific questions – that included 96 food-item questions accompanied by other lifestyle factors. Results were linked to the Swedish Inpatient Register and the Swedish National Cause of Death Register to follow outcomes of these patients.
National health coverage in Sweden has been nearly 100% since 1987. All cases of AAA were identified by clinical events, not by general screening. AAA repair was identified via the Nordic Classification of Surgical Procedures. To classify aneurysmal localization and rupture status of AAA repairs, the researchers linked the cohorts to the Swedish Registry for Vascular Surgery (founded in 1987, which accounted for 93.1% of all AAA repairs in Sweden).
Fruit and vegetable consumption was summed from results of the 96 food item questionnaire and converted to daily consumption categories ranging from never to greater than or equal to 3 times daily.
Covariates assessed included education, alcohol consumption, diet, physical activity, waist circumference, and smoking duration and amount. The study population was ethnically homogenous. History of cardiovascular disease, diabetes, hypertension, and hypercholesterolemia was obtained from the Swedish Inpatient Register, the Swedish National Diabetes Register, and the self-reported data from the questionnaire.
During 13 years of follow-up (1998-2010), the researchers found that there were 1,086 primary cases (899 in men; 83%) and 222 cases of ruptured AAA (181 in men; 82%). The mean age for nonruptured AAA was 74 years in men and 76 years in women. For ruptured AAA it was 76 and 78.5 years in men and women, respectively. Cox proportional hazard analysis was used to estimate hazard ratios.
Individuals in the highest quartile of fruit consumption (greater than 2 servings per day) had a 25% lower risk of AAA and a 43% lower risk of ruptured AAA, compared with those in the lowest quartiles of fruit consumption (less than 0.7 servings per day). No association was observed between vegetable consumption and AAA risk. There was no impact of smoking or sex of the individual on the fruit consumption–related AAA risk for both ruptured and nonruptured AAA.
Men and women with a high consumption of fruit and vegetables were more educated; consumed more fish, meat, and whole grains; and were more likely to be leaner and physically active, and less likely to be smokers, according to the researchers. In addition, high consumers of fruit consumed less alcohol, whereas the reverse was true of high consumers of vegetables.
"A diet high in fruits may help to prevent many vascular diseases, and this study provides evidence that a lower risk of AAA will be among the benefits," the researchers concluded.
The study was funded by grants from the Swedish Research Council and the Karolinska Institute. The authors reported they had no disclosures.
Researchers propose antiviral treatment options for MERS-CoV
In treating the emerging virus MERS-CoV, two antivirals already licensed to treat hepatitis C should be considered for early intervention therapy, according to researchers from the National Institute of Allergy and Infectious Diseases.
This research, based upon favorable results in a rhesus monkey model of Middle East respiratory syndrome coronavirus (MERS-CoV), comes at a time of great interest in the progression of the MERS-CoV outbreak, currently restricted to the Middle East. As of this writing, the World Health Organization reported that from September 2012 to date, WHO had been informed of a total of 114 laboratory-confirmed cases of infection with MERS-CoV with 54 deaths, including those of health care workers involved in treating infected individuals.
Dr. Darryl Falzarano and his colleagues at the National Institutes of Health’s (NIH’s) National Institute of Allergy and Infectious Diseases (NIAID) demonstrated that a combination of ribaravin and interferon alpha-2b stopped MERS-CoV replication in cell culture and improved clinical outcomes in infected monkeys, using a model system for the disease reported on earlier this year in the New England Journal of Medicine (2013;368:1560-2).
In a Sept. 8 release, the NIH announced publication of a letter in Nature Medicine detailing how treatment of rhesus macaques with the two antivirals 8 hours after inoculation with MERS-CoV affected the progression of disease as compared to untreated controls. Treated animals did not develop breathing abnormalities and had "no or very mild radiographic evidence of pneumonia. Moreover, treated animals showed lower levels of systemic (serum) and local (lung) proinflammatory markers, in addition to fewer viral genome copies, distinct gene expression, and less severe histopathological changes in the lungs," according to the researchers (Nat. Med. 2013 Sept. 8 [doi: 10.1038/nm.3362]).
The proposed intervention is similar to that found effective for the earlier, similarly behaving SARS (severe acute respiratory syndrome) virus. "The clinical experience from SARS suggests that a number of interventions, including ribavirin with and without corticosteroids, interferon-alfa with corticosteroids, ribavirin with lopinavir and ritonavir, and convalescent plasma may improve the outcome in patients but the data are not conclusive," wrote Dr. Hisham Momattin and his colleagues, who assessed therapeutic options for MERS-CoV in a systematic review of SARS therapy appearing in the International Journal of Infectious Diseases (2013;17:e792-e798).
"The high case fatality rate [currently seen] is likely related to the pattern of the disease, as we probably are seeing only the tip of the iceberg of critically ill and admitted patients. The high fatality rate is likely to decline as milder clinical cases emerge. Similar to SARS, common symptoms in patients with MERS-CoV include fever, cough, shortness of breath, and gastrointestinal symptoms. Most patients have had pneumonia, and the majority was reported to have multiple comorbid conditions," Dr. Momattin and his colleagues said. "The rapid deployment of effective therapeutics is a high priority, as there is currently no specific therapy or vaccine for MERS-CoV," they added.
Because the virus has been seen to be transmitted to and even kill health care workers in close contact with infected individuals, most authorities are recommending precautions in the treatment of patients suspected to have MERS-CoV.
In a recent overview, Dr. Jaffar Al-Tawfiq pointed out that the exact mode of transmission of the virus is not yet known, and addressed the advised containment protocol for hospital health care workers: "When caring for patients with suspected or confirmed cases of MERS-CoV, the following recommendations for infection control measures in hospital settings include: standard precautions; droplet precautions (wearing a medical mask when in close contact (within 1 m) and upon entering the room or cubicle of the patient); and performing hand hygiene in accordance with the World Health Organization’s (WHO’s) five moments of hand hygiene. Additional measures include wearing a particulate respirator when performing aerosol-generating procedures in addition to other precautions as outlined by WHO," (J. Infect. Public Health 2013;6:319-22).
Dr. Al-Tawfiq discussed a MERS-CoV outbreak in a health care setting where there was evidence of person-to-person transmission, and the outbreak was aborted by the implementation of basic infection control measures. He pointed out that the Centers for Disease Control and Prevention in the United States recommended placing the patient in an airborne-infection isolation room.
For those questioning the relevance of such dedicated research and investment of resources in narrowly focused emergent diseases, Dr. Hanan Balkhy, editor in chief of the Journal of Infection and Public Health, had an answer in her recent editorial (J. Infect. Public Health 2013;6:317-18). "Today the current viruses, whether the novel MERS-CoV or any of the emerging influenza viruses, do have the potential capacity to evolve into acquiring the ability to sustained human-to-human transmission. And therefore, we will continue to hope for the best and act as if it is the worst. In doing so, the infectious disease community will be criticized for being overstated in their policies and take the heat as they have in the past with similar scenarios, such as the H1N1 pandemic. I just hope people realize that hindsight is always 20/20."
Dr. Falzarano and his colleagues are part of a team that includes Dr. Vincent Munster, chief of the Virus Ecology Unit in NIAID’s Laboratory of Virology, who is leading the NIAID Rocky Mountain Laboratories team investigating the ecology and molecular biology of the new coronavirus.
The NIAID researchers and the authors of these reports disclosed no relevant conflicts.
In treating the emerging virus MERS-CoV, two antivirals already licensed to treat hepatitis C should be considered for early intervention therapy, according to researchers from the National Institute of Allergy and Infectious Diseases.
This research, based upon favorable results in a rhesus monkey model of Middle East respiratory syndrome coronavirus (MERS-CoV), comes at a time of great interest in the progression of the MERS-CoV outbreak, currently restricted to the Middle East. As of this writing, the World Health Organization reported that from September 2012 to date, WHO had been informed of a total of 114 laboratory-confirmed cases of infection with MERS-CoV with 54 deaths, including those of health care workers involved in treating infected individuals.
Dr. Darryl Falzarano and his colleagues at the National Institutes of Health’s (NIH’s) National Institute of Allergy and Infectious Diseases (NIAID) demonstrated that a combination of ribaravin and interferon alpha-2b stopped MERS-CoV replication in cell culture and improved clinical outcomes in infected monkeys, using a model system for the disease reported on earlier this year in the New England Journal of Medicine (2013;368:1560-2).
In a Sept. 8 release, the NIH announced publication of a letter in Nature Medicine detailing how treatment of rhesus macaques with the two antivirals 8 hours after inoculation with MERS-CoV affected the progression of disease as compared to untreated controls. Treated animals did not develop breathing abnormalities and had "no or very mild radiographic evidence of pneumonia. Moreover, treated animals showed lower levels of systemic (serum) and local (lung) proinflammatory markers, in addition to fewer viral genome copies, distinct gene expression, and less severe histopathological changes in the lungs," according to the researchers (Nat. Med. 2013 Sept. 8 [doi: 10.1038/nm.3362]).
The proposed intervention is similar to that found effective for the earlier, similarly behaving SARS (severe acute respiratory syndrome) virus. "The clinical experience from SARS suggests that a number of interventions, including ribavirin with and without corticosteroids, interferon-alfa with corticosteroids, ribavirin with lopinavir and ritonavir, and convalescent plasma may improve the outcome in patients but the data are not conclusive," wrote Dr. Hisham Momattin and his colleagues, who assessed therapeutic options for MERS-CoV in a systematic review of SARS therapy appearing in the International Journal of Infectious Diseases (2013;17:e792-e798).
"The high case fatality rate [currently seen] is likely related to the pattern of the disease, as we probably are seeing only the tip of the iceberg of critically ill and admitted patients. The high fatality rate is likely to decline as milder clinical cases emerge. Similar to SARS, common symptoms in patients with MERS-CoV include fever, cough, shortness of breath, and gastrointestinal symptoms. Most patients have had pneumonia, and the majority was reported to have multiple comorbid conditions," Dr. Momattin and his colleagues said. "The rapid deployment of effective therapeutics is a high priority, as there is currently no specific therapy or vaccine for MERS-CoV," they added.
Because the virus has been seen to be transmitted to and even kill health care workers in close contact with infected individuals, most authorities are recommending precautions in the treatment of patients suspected to have MERS-CoV.
In a recent overview, Dr. Jaffar Al-Tawfiq pointed out that the exact mode of transmission of the virus is not yet known, and addressed the advised containment protocol for hospital health care workers: "When caring for patients with suspected or confirmed cases of MERS-CoV, the following recommendations for infection control measures in hospital settings include: standard precautions; droplet precautions (wearing a medical mask when in close contact (within 1 m) and upon entering the room or cubicle of the patient); and performing hand hygiene in accordance with the World Health Organization’s (WHO’s) five moments of hand hygiene. Additional measures include wearing a particulate respirator when performing aerosol-generating procedures in addition to other precautions as outlined by WHO," (J. Infect. Public Health 2013;6:319-22).
Dr. Al-Tawfiq discussed a MERS-CoV outbreak in a health care setting where there was evidence of person-to-person transmission, and the outbreak was aborted by the implementation of basic infection control measures. He pointed out that the Centers for Disease Control and Prevention in the United States recommended placing the patient in an airborne-infection isolation room.
For those questioning the relevance of such dedicated research and investment of resources in narrowly focused emergent diseases, Dr. Hanan Balkhy, editor in chief of the Journal of Infection and Public Health, had an answer in her recent editorial (J. Infect. Public Health 2013;6:317-18). "Today the current viruses, whether the novel MERS-CoV or any of the emerging influenza viruses, do have the potential capacity to evolve into acquiring the ability to sustained human-to-human transmission. And therefore, we will continue to hope for the best and act as if it is the worst. In doing so, the infectious disease community will be criticized for being overstated in their policies and take the heat as they have in the past with similar scenarios, such as the H1N1 pandemic. I just hope people realize that hindsight is always 20/20."
Dr. Falzarano and his colleagues are part of a team that includes Dr. Vincent Munster, chief of the Virus Ecology Unit in NIAID’s Laboratory of Virology, who is leading the NIAID Rocky Mountain Laboratories team investigating the ecology and molecular biology of the new coronavirus.
The NIAID researchers and the authors of these reports disclosed no relevant conflicts.
In treating the emerging virus MERS-CoV, two antivirals already licensed to treat hepatitis C should be considered for early intervention therapy, according to researchers from the National Institute of Allergy and Infectious Diseases.
This research, based upon favorable results in a rhesus monkey model of Middle East respiratory syndrome coronavirus (MERS-CoV), comes at a time of great interest in the progression of the MERS-CoV outbreak, currently restricted to the Middle East. As of this writing, the World Health Organization reported that from September 2012 to date, WHO had been informed of a total of 114 laboratory-confirmed cases of infection with MERS-CoV with 54 deaths, including those of health care workers involved in treating infected individuals.
Dr. Darryl Falzarano and his colleagues at the National Institutes of Health’s (NIH’s) National Institute of Allergy and Infectious Diseases (NIAID) demonstrated that a combination of ribaravin and interferon alpha-2b stopped MERS-CoV replication in cell culture and improved clinical outcomes in infected monkeys, using a model system for the disease reported on earlier this year in the New England Journal of Medicine (2013;368:1560-2).
In a Sept. 8 release, the NIH announced publication of a letter in Nature Medicine detailing how treatment of rhesus macaques with the two antivirals 8 hours after inoculation with MERS-CoV affected the progression of disease as compared to untreated controls. Treated animals did not develop breathing abnormalities and had "no or very mild radiographic evidence of pneumonia. Moreover, treated animals showed lower levels of systemic (serum) and local (lung) proinflammatory markers, in addition to fewer viral genome copies, distinct gene expression, and less severe histopathological changes in the lungs," according to the researchers (Nat. Med. 2013 Sept. 8 [doi: 10.1038/nm.3362]).
The proposed intervention is similar to that found effective for the earlier, similarly behaving SARS (severe acute respiratory syndrome) virus. "The clinical experience from SARS suggests that a number of interventions, including ribavirin with and without corticosteroids, interferon-alfa with corticosteroids, ribavirin with lopinavir and ritonavir, and convalescent plasma may improve the outcome in patients but the data are not conclusive," wrote Dr. Hisham Momattin and his colleagues, who assessed therapeutic options for MERS-CoV in a systematic review of SARS therapy appearing in the International Journal of Infectious Diseases (2013;17:e792-e798).
"The high case fatality rate [currently seen] is likely related to the pattern of the disease, as we probably are seeing only the tip of the iceberg of critically ill and admitted patients. The high fatality rate is likely to decline as milder clinical cases emerge. Similar to SARS, common symptoms in patients with MERS-CoV include fever, cough, shortness of breath, and gastrointestinal symptoms. Most patients have had pneumonia, and the majority was reported to have multiple comorbid conditions," Dr. Momattin and his colleagues said. "The rapid deployment of effective therapeutics is a high priority, as there is currently no specific therapy or vaccine for MERS-CoV," they added.
Because the virus has been seen to be transmitted to and even kill health care workers in close contact with infected individuals, most authorities are recommending precautions in the treatment of patients suspected to have MERS-CoV.
In a recent overview, Dr. Jaffar Al-Tawfiq pointed out that the exact mode of transmission of the virus is not yet known, and addressed the advised containment protocol for hospital health care workers: "When caring for patients with suspected or confirmed cases of MERS-CoV, the following recommendations for infection control measures in hospital settings include: standard precautions; droplet precautions (wearing a medical mask when in close contact (within 1 m) and upon entering the room or cubicle of the patient); and performing hand hygiene in accordance with the World Health Organization’s (WHO’s) five moments of hand hygiene. Additional measures include wearing a particulate respirator when performing aerosol-generating procedures in addition to other precautions as outlined by WHO," (J. Infect. Public Health 2013;6:319-22).
Dr. Al-Tawfiq discussed a MERS-CoV outbreak in a health care setting where there was evidence of person-to-person transmission, and the outbreak was aborted by the implementation of basic infection control measures. He pointed out that the Centers for Disease Control and Prevention in the United States recommended placing the patient in an airborne-infection isolation room.
For those questioning the relevance of such dedicated research and investment of resources in narrowly focused emergent diseases, Dr. Hanan Balkhy, editor in chief of the Journal of Infection and Public Health, had an answer in her recent editorial (J. Infect. Public Health 2013;6:317-18). "Today the current viruses, whether the novel MERS-CoV or any of the emerging influenza viruses, do have the potential capacity to evolve into acquiring the ability to sustained human-to-human transmission. And therefore, we will continue to hope for the best and act as if it is the worst. In doing so, the infectious disease community will be criticized for being overstated in their policies and take the heat as they have in the past with similar scenarios, such as the H1N1 pandemic. I just hope people realize that hindsight is always 20/20."
Dr. Falzarano and his colleagues are part of a team that includes Dr. Vincent Munster, chief of the Virus Ecology Unit in NIAID’s Laboratory of Virology, who is leading the NIAID Rocky Mountain Laboratories team investigating the ecology and molecular biology of the new coronavirus.
The NIAID researchers and the authors of these reports disclosed no relevant conflicts.
Fruits, not vegetables, seen to lower AAA risk
The consumption of fruits, but not vegetables, was associated with a decreased risk of abdominal aortic aneurysm, especially the risk of rupture, according to results of a large database study of two prospective cohorts of Swedish men and women.
"The risk of AAA decreased with increasing consumption of fruit (P =.003), whereas no significant association was observed for vegetable consumption," wrote Dr. Otto Stackelberg and his colleagues at Uppsala (Sweden) University (Circulation 2013;128:795-802).
The study population in the final analysis consisted of 36,109 women from the Swedish Mammography Cohort (established between 1987 and 1990) and 44,317 men from the Cohort of Swedish Men (established in 1997).
Both cohorts responded in 1997 to extensive questionnaires – identical except for sex-specific questions – that included 96 food-item questions accompanied by other lifestyle factors. Results were linked to the Swedish Inpatient Register and the Swedish National Cause of Death register to follow outcomes of these patients.
National health coverage in Sweden has been nearly 100% since 1987. All cases of AAA were identified by clinical events, not by general screening. AAA repair was identified via the Nordic Classification of Surgical Procedures. To classify aneurysmal localization and rupture status of AAA repairs, the researchers linked the cohorts to the Swedish Registry for Vascular Surgery (founded in 1987, which accounted for 93.1% of all AAA repairs in Sweden).
Fruit and vegetable consumption was summed from results of the 96 food item questionnaire and converted to daily consumption categories ranging from never to greater than or equal to 3 times daily.
Covariates assessed included education, alcohol consumption, diet, physical activity, waist circumference, and smoking duration and amount. The study population was ethnically homogenous. History of cardiovascular disease, diabetes, hypertension, and hypercholesterolemia was obtained from the Swedish Inpatient Register, the Swedish National Diabetes Register, and the self-reported data from the questionnaire.
During 13 years of follow-up (1998-2010), the researchers found that there were 1,086 primary cases (899 in men; 83%) and 222 cases of ruptured AAA (181 in men; 82%). The mean age for nonruptured AAA was 74 years in men and 76 years in women. For ruptured AAA it was 76 and 78.5 years in men and women, respectively. Cox proportional hazard analysis was used to estimate hazard ratios.
Individuals in the highest quartile of fruit consumption (greater than 2 servings per day) had a 25% lower risk of AAA and a 43% lower risk of ruptured AAA, compared with those in the lowest quartiles of fruit consumption (less than 0.7 servings per day). No association was observed between vegetable consumption and AAA risk. There was no impact of smoking or sex of the individual on the fruit consumption–related AAA risk for both ruptured and nonruptured AAA.
Men and women with a high consumption of fruit and vegetables were more educated, consumed more fish, meat, and whole grains, and were more likely to be leaner and physically active, and less likely to be smokers, according to the researchers. In addition, high consumers of fruit consumed less alcohol, whereas the reverse was true of high consumers of vegetables.
"A diet high in fruits may help to prevent many vascular diseases, and this study provides evidence that a lower risk of AAA will be among the benefits," the researchers concluded.
The study was funded by grants from the Swedish Research Council and the Karolinska Institute. The authors reported they had no disclosures.
The consumption of fruits, but not vegetables, was associated with a decreased risk of abdominal aortic aneurysm, especially the risk of rupture, according to results of a large database study of two prospective cohorts of Swedish men and women.
"The risk of AAA decreased with increasing consumption of fruit (P =.003), whereas no significant association was observed for vegetable consumption," wrote Dr. Otto Stackelberg and his colleagues at Uppsala (Sweden) University (Circulation 2013;128:795-802).
The study population in the final analysis consisted of 36,109 women from the Swedish Mammography Cohort (established between 1987 and 1990) and 44,317 men from the Cohort of Swedish Men (established in 1997).
Both cohorts responded in 1997 to extensive questionnaires – identical except for sex-specific questions – that included 96 food-item questions accompanied by other lifestyle factors. Results were linked to the Swedish Inpatient Register and the Swedish National Cause of Death register to follow outcomes of these patients.
National health coverage in Sweden has been nearly 100% since 1987. All cases of AAA were identified by clinical events, not by general screening. AAA repair was identified via the Nordic Classification of Surgical Procedures. To classify aneurysmal localization and rupture status of AAA repairs, the researchers linked the cohorts to the Swedish Registry for Vascular Surgery (founded in 1987, which accounted for 93.1% of all AAA repairs in Sweden).
Fruit and vegetable consumption was summed from results of the 96 food item questionnaire and converted to daily consumption categories ranging from never to greater than or equal to 3 times daily.
Covariates assessed included education, alcohol consumption, diet, physical activity, waist circumference, and smoking duration and amount. The study population was ethnically homogenous. History of cardiovascular disease, diabetes, hypertension, and hypercholesterolemia was obtained from the Swedish Inpatient Register, the Swedish National Diabetes Register, and the self-reported data from the questionnaire.
During 13 years of follow-up (1998-2010), the researchers found that there were 1,086 primary cases (899 in men; 83%) and 222 cases of ruptured AAA (181 in men; 82%). The mean age for nonruptured AAA was 74 years in men and 76 years in women. For ruptured AAA it was 76 and 78.5 years in men and women, respectively. Cox proportional hazard analysis was used to estimate hazard ratios.
Individuals in the highest quartile of fruit consumption (greater than 2 servings per day) had a 25% lower risk of AAA and a 43% lower risk of ruptured AAA, compared with those in the lowest quartiles of fruit consumption (less than 0.7 servings per day). No association was observed between vegetable consumption and AAA risk. There was no impact of smoking or sex of the individual on the fruit consumption–related AAA risk for both ruptured and nonruptured AAA.
Men and women with a high consumption of fruit and vegetables were more educated, consumed more fish, meat, and whole grains, and were more likely to be leaner and physically active, and less likely to be smokers, according to the researchers. In addition, high consumers of fruit consumed less alcohol, whereas the reverse was true of high consumers of vegetables.
"A diet high in fruits may help to prevent many vascular diseases, and this study provides evidence that a lower risk of AAA will be among the benefits," the researchers concluded.
The study was funded by grants from the Swedish Research Council and the Karolinska Institute. The authors reported they had no disclosures.
The consumption of fruits, but not vegetables, was associated with a decreased risk of abdominal aortic aneurysm, especially the risk of rupture, according to results of a large database study of two prospective cohorts of Swedish men and women.
"The risk of AAA decreased with increasing consumption of fruit (P =.003), whereas no significant association was observed for vegetable consumption," wrote Dr. Otto Stackelberg and his colleagues at Uppsala (Sweden) University (Circulation 2013;128:795-802).
The study population in the final analysis consisted of 36,109 women from the Swedish Mammography Cohort (established between 1987 and 1990) and 44,317 men from the Cohort of Swedish Men (established in 1997).
Both cohorts responded in 1997 to extensive questionnaires – identical except for sex-specific questions – that included 96 food-item questions accompanied by other lifestyle factors. Results were linked to the Swedish Inpatient Register and the Swedish National Cause of Death register to follow outcomes of these patients.
National health coverage in Sweden has been nearly 100% since 1987. All cases of AAA were identified by clinical events, not by general screening. AAA repair was identified via the Nordic Classification of Surgical Procedures. To classify aneurysmal localization and rupture status of AAA repairs, the researchers linked the cohorts to the Swedish Registry for Vascular Surgery (founded in 1987, which accounted for 93.1% of all AAA repairs in Sweden).
Fruit and vegetable consumption was summed from results of the 96 food item questionnaire and converted to daily consumption categories ranging from never to greater than or equal to 3 times daily.
Covariates assessed included education, alcohol consumption, diet, physical activity, waist circumference, and smoking duration and amount. The study population was ethnically homogenous. History of cardiovascular disease, diabetes, hypertension, and hypercholesterolemia was obtained from the Swedish Inpatient Register, the Swedish National Diabetes Register, and the self-reported data from the questionnaire.
During 13 years of follow-up (1998-2010), the researchers found that there were 1,086 primary cases (899 in men; 83%) and 222 cases of ruptured AAA (181 in men; 82%). The mean age for nonruptured AAA was 74 years in men and 76 years in women. For ruptured AAA it was 76 and 78.5 years in men and women, respectively. Cox proportional hazard analysis was used to estimate hazard ratios.
Individuals in the highest quartile of fruit consumption (greater than 2 servings per day) had a 25% lower risk of AAA and a 43% lower risk of ruptured AAA, compared with those in the lowest quartiles of fruit consumption (less than 0.7 servings per day). No association was observed between vegetable consumption and AAA risk. There was no impact of smoking or sex of the individual on the fruit consumption–related AAA risk for both ruptured and nonruptured AAA.
Men and women with a high consumption of fruit and vegetables were more educated, consumed more fish, meat, and whole grains, and were more likely to be leaner and physically active, and less likely to be smokers, according to the researchers. In addition, high consumers of fruit consumed less alcohol, whereas the reverse was true of high consumers of vegetables.
"A diet high in fruits may help to prevent many vascular diseases, and this study provides evidence that a lower risk of AAA will be among the benefits," the researchers concluded.
The study was funded by grants from the Swedish Research Council and the Karolinska Institute. The authors reported they had no disclosures.
FROM CIRCULATION