User login
Statins Do Not Worsen Diabetes Microvascular Complications, May Be Protective
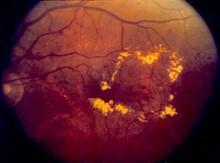
Contrary to expectations, statin use before the development of type II diabetes did not worsen microvascular complications such as retinopathy, neuropathy, and gangrene of the foot.
In fact, despite concerns that statins have been seen to increase glucose levels and the risk of diabetes development, they may provide a protective effect from these conditions in newly developed diabetic patients, according to an analysis of data from more than 60,000 individuals in the Danish Patient Registry.
"The cumulative incidences of diabetic retinopathy, diabetic neuropathy, and gangrene were reduced in statin users compared with non–statin users, but [the] risk of diabetic nephropathy was similar for all patients with diabetes," stated Dr. Sune F. Nielsen, Ph.D., and Dr. Børge G. Nordestgaard of the Herlev Hospital, Copenhagen University Hospital. However, they did find that statin use, as previously seen, did significantly increase the risk of developing diabetes in the first place. Their study was published online Sept. 10 in the Lancet Diabetes & Endocrinology (2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
The researchers performed a nested matched study of all men and women living in Denmark who were diagnosed with incident diabetes during 1996-2009 at age 40 years or older, and assessed their outcomes through use of the Danish Civil Registration System, the Danish Patient Registry, and the Danish Registry of Medicinal Product Statistics. After exclusions, 62,716 patients with diabetes were randomly selected for the study: 15,679 statin users and 47,037 non–statin users. The primary outcome was the incidence of diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and gangrene of the foot. The design "captured 100% of individuals in Denmark who had ever used a statin within the time frame of the study."
Follow-up was censored at date of death for 9,560 individuals. During 215,725 person-years of follow-up, diabetic retinopathy was recorded in 2,866 patients, diabetic neuropathy in 1,406, diabetic nephropathy in 1,248, and gangrene of the foot in 2,392.
Over a median follow-up of 2.7 years, statin users were significantly less likely to be diagnosed with diabetic neuropathy (hazard ratio, 0.66; 95% confidence interval, 0.57-0.75: P less than .0001) and diabetic retinopathy (HR, 0.60; 95% CI 0.54-0.66: P less than .0001) than were those who had not received statins. However, no difference was noted in the incidence of diabetic nephropathy (HR, 0.97; 95% CI, 0.85-1.10; P = .62).
In contrast, the researchers found that statin use significantly increased the risk of developing diabetes in people who did not have the disease when the study began. When they compared a random selection of 272,994 non–statin users with 90,998 statin users, the multivariable adjusted hazard ratio for the risk of developing diabetes was 1.17 (95% CI, 1.14-1.21). These results are similar to those seen in previous randomized studies of statin use.
"In conclusion, we found no evidence that statin use is associated with an increased risk of microvascular disease; this result is important and clinically reassuring on its own. Whether or not statins are protective against some forms of microvascular disease, a possibility raised by these data, and by which mechanism, will need to be addressed in studies similar to ours, or in Mendelian randomization studies," said Dr. Nielsen and Dr. Nordestgaard. "Ideally, however, this question should be addressed in the setting of a randomized controlled trial," they added.
Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
Pharmacoepidemiological studies need cautious interpretation and can be regarded only as hypothesis generating; Dr. Nielsen and Dr. Nordestgaard are appropriately circumspect.
The study has many strengths, such as its size, the quality and coverage of the national registry, and external validity – i.e., statin use was associated with an increased risk of diabetes, an effect size similar to that reported in randomized trials of statins. However, important weaknesses of the study include the absence of data on important predictors of microvascular disease – e.g., hemoglobin A1c, urine albumin, and blood pressure. For now, any benefit of statins on microvascular complications remains unproven.
Dr. David Preiss, of the University of Glasgow (Scotland), is cochair of the Scottish Lipid Forum, whose annual meeting is supported by grants from pharmaceutical companies including MSD, AstraZeneca, and Sanofi. The remarks are taken from his accompanying commentary (Lancet Diabetes Endocrinol. 2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
Pharmacoepidemiological studies need cautious interpretation and can be regarded only as hypothesis generating; Dr. Nielsen and Dr. Nordestgaard are appropriately circumspect.
The study has many strengths, such as its size, the quality and coverage of the national registry, and external validity – i.e., statin use was associated with an increased risk of diabetes, an effect size similar to that reported in randomized trials of statins. However, important weaknesses of the study include the absence of data on important predictors of microvascular disease – e.g., hemoglobin A1c, urine albumin, and blood pressure. For now, any benefit of statins on microvascular complications remains unproven.
Dr. David Preiss, of the University of Glasgow (Scotland), is cochair of the Scottish Lipid Forum, whose annual meeting is supported by grants from pharmaceutical companies including MSD, AstraZeneca, and Sanofi. The remarks are taken from his accompanying commentary (Lancet Diabetes Endocrinol. 2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
Pharmacoepidemiological studies need cautious interpretation and can be regarded only as hypothesis generating; Dr. Nielsen and Dr. Nordestgaard are appropriately circumspect.
The study has many strengths, such as its size, the quality and coverage of the national registry, and external validity – i.e., statin use was associated with an increased risk of diabetes, an effect size similar to that reported in randomized trials of statins. However, important weaknesses of the study include the absence of data on important predictors of microvascular disease – e.g., hemoglobin A1c, urine albumin, and blood pressure. For now, any benefit of statins on microvascular complications remains unproven.
Dr. David Preiss, of the University of Glasgow (Scotland), is cochair of the Scottish Lipid Forum, whose annual meeting is supported by grants from pharmaceutical companies including MSD, AstraZeneca, and Sanofi. The remarks are taken from his accompanying commentary (Lancet Diabetes Endocrinol. 2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
Contrary to expectations, statin use before the development of type II diabetes did not worsen microvascular complications such as retinopathy, neuropathy, and gangrene of the foot.
In fact, despite concerns that statins have been seen to increase glucose levels and the risk of diabetes development, they may provide a protective effect from these conditions in newly developed diabetic patients, according to an analysis of data from more than 60,000 individuals in the Danish Patient Registry.
"The cumulative incidences of diabetic retinopathy, diabetic neuropathy, and gangrene were reduced in statin users compared with non–statin users, but [the] risk of diabetic nephropathy was similar for all patients with diabetes," stated Dr. Sune F. Nielsen, Ph.D., and Dr. Børge G. Nordestgaard of the Herlev Hospital, Copenhagen University Hospital. However, they did find that statin use, as previously seen, did significantly increase the risk of developing diabetes in the first place. Their study was published online Sept. 10 in the Lancet Diabetes & Endocrinology (2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
The researchers performed a nested matched study of all men and women living in Denmark who were diagnosed with incident diabetes during 1996-2009 at age 40 years or older, and assessed their outcomes through use of the Danish Civil Registration System, the Danish Patient Registry, and the Danish Registry of Medicinal Product Statistics. After exclusions, 62,716 patients with diabetes were randomly selected for the study: 15,679 statin users and 47,037 non–statin users. The primary outcome was the incidence of diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and gangrene of the foot. The design "captured 100% of individuals in Denmark who had ever used a statin within the time frame of the study."
Follow-up was censored at date of death for 9,560 individuals. During 215,725 person-years of follow-up, diabetic retinopathy was recorded in 2,866 patients, diabetic neuropathy in 1,406, diabetic nephropathy in 1,248, and gangrene of the foot in 2,392.
Over a median follow-up of 2.7 years, statin users were significantly less likely to be diagnosed with diabetic neuropathy (hazard ratio, 0.66; 95% confidence interval, 0.57-0.75: P less than .0001) and diabetic retinopathy (HR, 0.60; 95% CI 0.54-0.66: P less than .0001) than were those who had not received statins. However, no difference was noted in the incidence of diabetic nephropathy (HR, 0.97; 95% CI, 0.85-1.10; P = .62).
In contrast, the researchers found that statin use significantly increased the risk of developing diabetes in people who did not have the disease when the study began. When they compared a random selection of 272,994 non–statin users with 90,998 statin users, the multivariable adjusted hazard ratio for the risk of developing diabetes was 1.17 (95% CI, 1.14-1.21). These results are similar to those seen in previous randomized studies of statin use.
"In conclusion, we found no evidence that statin use is associated with an increased risk of microvascular disease; this result is important and clinically reassuring on its own. Whether or not statins are protective against some forms of microvascular disease, a possibility raised by these data, and by which mechanism, will need to be addressed in studies similar to ours, or in Mendelian randomization studies," said Dr. Nielsen and Dr. Nordestgaard. "Ideally, however, this question should be addressed in the setting of a randomized controlled trial," they added.
Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
Contrary to expectations, statin use before the development of type II diabetes did not worsen microvascular complications such as retinopathy, neuropathy, and gangrene of the foot.
In fact, despite concerns that statins have been seen to increase glucose levels and the risk of diabetes development, they may provide a protective effect from these conditions in newly developed diabetic patients, according to an analysis of data from more than 60,000 individuals in the Danish Patient Registry.
"The cumulative incidences of diabetic retinopathy, diabetic neuropathy, and gangrene were reduced in statin users compared with non–statin users, but [the] risk of diabetic nephropathy was similar for all patients with diabetes," stated Dr. Sune F. Nielsen, Ph.D., and Dr. Børge G. Nordestgaard of the Herlev Hospital, Copenhagen University Hospital. However, they did find that statin use, as previously seen, did significantly increase the risk of developing diabetes in the first place. Their study was published online Sept. 10 in the Lancet Diabetes & Endocrinology (2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
The researchers performed a nested matched study of all men and women living in Denmark who were diagnosed with incident diabetes during 1996-2009 at age 40 years or older, and assessed their outcomes through use of the Danish Civil Registration System, the Danish Patient Registry, and the Danish Registry of Medicinal Product Statistics. After exclusions, 62,716 patients with diabetes were randomly selected for the study: 15,679 statin users and 47,037 non–statin users. The primary outcome was the incidence of diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and gangrene of the foot. The design "captured 100% of individuals in Denmark who had ever used a statin within the time frame of the study."
Follow-up was censored at date of death for 9,560 individuals. During 215,725 person-years of follow-up, diabetic retinopathy was recorded in 2,866 patients, diabetic neuropathy in 1,406, diabetic nephropathy in 1,248, and gangrene of the foot in 2,392.
Over a median follow-up of 2.7 years, statin users were significantly less likely to be diagnosed with diabetic neuropathy (hazard ratio, 0.66; 95% confidence interval, 0.57-0.75: P less than .0001) and diabetic retinopathy (HR, 0.60; 95% CI 0.54-0.66: P less than .0001) than were those who had not received statins. However, no difference was noted in the incidence of diabetic nephropathy (HR, 0.97; 95% CI, 0.85-1.10; P = .62).
In contrast, the researchers found that statin use significantly increased the risk of developing diabetes in people who did not have the disease when the study began. When they compared a random selection of 272,994 non–statin users with 90,998 statin users, the multivariable adjusted hazard ratio for the risk of developing diabetes was 1.17 (95% CI, 1.14-1.21). These results are similar to those seen in previous randomized studies of statin use.
"In conclusion, we found no evidence that statin use is associated with an increased risk of microvascular disease; this result is important and clinically reassuring on its own. Whether or not statins are protective against some forms of microvascular disease, a possibility raised by these data, and by which mechanism, will need to be addressed in studies similar to ours, or in Mendelian randomization studies," said Dr. Nielsen and Dr. Nordestgaard. "Ideally, however, this question should be addressed in the setting of a randomized controlled trial," they added.
Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
FROM THE LANCET DIABETES & ENDOCRINOLOGY
Statins do not worsen diabetes microvascular complications, may be protective
Contrary to expectations, statin use before the development of type II diabetes did not worsen microvascular complications such as retinopathy, neuropathy, and gangrene of the foot.
In fact, despite concerns that statins have been seen to increase glucose levels and the risk of diabetes development, they may provide a protective effect from these conditions in newly developed diabetic patients, according to an analysis of data from more than 60,000 individuals in the Danish Patient Registry.
"The cumulative incidences of diabetic retinopathy, diabetic neuropathy, and gangrene were reduced in statin users compared with non–statin users, but [the] risk of diabetic nephropathy was similar for all patients with diabetes," stated Dr. Sune F. Nielsen, Ph.D., and Dr. Børge G. Nordestgaard of the Herlev Hospital, Copenhagen University Hospital. However, they did find that statin use, as previously seen, did significantly increase the risk of developing diabetes in the first place. Their study was published online Sept. 10 in the Lancet Diabetes & Endocrinology (2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
The researchers performed a nested matched study of all men and women living in Denmark who were diagnosed with incident diabetes during 1996-2009 at age 40 years or older, and assessed their outcomes through use of the Danish Civil Registration System, the Danish Patient Registry, and the Danish Registry of Medicinal Product Statistics. After exclusions, 62,716 patients with diabetes were randomly selected for the study: 15,679 statin users and 47,037 non–statin users. The primary outcome was the incidence of diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and gangrene of the foot. The design "captured 100% of individuals in Denmark who had ever used a statin within the time frame of the study."
Follow-up was censored at date of death for 9,560 individuals. During 215,725 person-years of follow-up, diabetic retinopathy was recorded in 2,866 patients, diabetic neuropathy in 1,406, diabetic nephropathy in 1,248, and gangrene of the foot in 2,392.
Over a median follow-up of 2.7 years, statin users were significantly less likely to be diagnosed with diabetic neuropathy (hazard ratio, 0.66; 95% confidence interval, 0.57-0.75: P less than .0001) and diabetic retinopathy (HR, 0.60; 95% CI 0.54-0.66: P less than .0001) than were those who had not received statins. However, no difference was noted in the incidence of diabetic nephropathy (HR, 0.97; 95% CI, 0.85-1.10; P = .62).
In contrast, the researchers found that statin use significantly increased the risk of developing diabetes in people who did not have the disease when the study began. When they compared a random selection of 272,994 non–statin users with 90,998 statin users, the multivariable adjusted hazard ratio for the risk of developing diabetes was 1.17 (95% CI, 1.14-1.21). These results are similar to those seen in previous randomized studies of statin use.
"In conclusion, we found no evidence that statin use is associated with an increased risk of microvascular disease; this result is important and clinically reassuring on its own. Whether or not statins are protective against some forms of microvascular disease, a possibility raised by these data, and by which mechanism, will need to be addressed in studies similar to ours, or in Mendelian randomization studies," said Dr. Nielsen and Dr. Nordestgaard. "Ideally, however, this question should be addressed in the setting of a randomized controlled trial," they added.
Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
Pharmacoepidemiological studies need cautious interpretation and can be regarded only as hypothesis generating; Dr. Nielsen and Dr. Nordestgaard are appropriately circumspect.
The study has many strengths, such as its size, the quality and coverage of the national registry, and external validity – i.e., statin use was associated with an increased risk of diabetes, an effect size similar to that reported in randomized trials of statins. However, important weaknesses of the study include the absence of data on important predictors of microvascular disease – e.g., hemoglobin A1c, urine albumin, and blood pressure. For now, any benefit of statins on microvascular complications remains unproven.
Dr. David Preiss, of the University of Glasgow (Scotland), is cochair of the Scottish Lipid Forum, whose annual meeting is supported by grants from pharmaceutical companies including MSD, AstraZeneca, and Sanofi. The remarks are taken from his accompanying commentary (Lancet Diabetes Endocrinol. 2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
Pharmacoepidemiological studies need cautious interpretation and can be regarded only as hypothesis generating; Dr. Nielsen and Dr. Nordestgaard are appropriately circumspect.
The study has many strengths, such as its size, the quality and coverage of the national registry, and external validity – i.e., statin use was associated with an increased risk of diabetes, an effect size similar to that reported in randomized trials of statins. However, important weaknesses of the study include the absence of data on important predictors of microvascular disease – e.g., hemoglobin A1c, urine albumin, and blood pressure. For now, any benefit of statins on microvascular complications remains unproven.
Dr. David Preiss, of the University of Glasgow (Scotland), is cochair of the Scottish Lipid Forum, whose annual meeting is supported by grants from pharmaceutical companies including MSD, AstraZeneca, and Sanofi. The remarks are taken from his accompanying commentary (Lancet Diabetes Endocrinol. 2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
Pharmacoepidemiological studies need cautious interpretation and can be regarded only as hypothesis generating; Dr. Nielsen and Dr. Nordestgaard are appropriately circumspect.
The study has many strengths, such as its size, the quality and coverage of the national registry, and external validity – i.e., statin use was associated with an increased risk of diabetes, an effect size similar to that reported in randomized trials of statins. However, important weaknesses of the study include the absence of data on important predictors of microvascular disease – e.g., hemoglobin A1c, urine albumin, and blood pressure. For now, any benefit of statins on microvascular complications remains unproven.
Dr. David Preiss, of the University of Glasgow (Scotland), is cochair of the Scottish Lipid Forum, whose annual meeting is supported by grants from pharmaceutical companies including MSD, AstraZeneca, and Sanofi. The remarks are taken from his accompanying commentary (Lancet Diabetes Endocrinol. 2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
Contrary to expectations, statin use before the development of type II diabetes did not worsen microvascular complications such as retinopathy, neuropathy, and gangrene of the foot.
In fact, despite concerns that statins have been seen to increase glucose levels and the risk of diabetes development, they may provide a protective effect from these conditions in newly developed diabetic patients, according to an analysis of data from more than 60,000 individuals in the Danish Patient Registry.
"The cumulative incidences of diabetic retinopathy, diabetic neuropathy, and gangrene were reduced in statin users compared with non–statin users, but [the] risk of diabetic nephropathy was similar for all patients with diabetes," stated Dr. Sune F. Nielsen, Ph.D., and Dr. Børge G. Nordestgaard of the Herlev Hospital, Copenhagen University Hospital. However, they did find that statin use, as previously seen, did significantly increase the risk of developing diabetes in the first place. Their study was published online Sept. 10 in the Lancet Diabetes & Endocrinology (2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
The researchers performed a nested matched study of all men and women living in Denmark who were diagnosed with incident diabetes during 1996-2009 at age 40 years or older, and assessed their outcomes through use of the Danish Civil Registration System, the Danish Patient Registry, and the Danish Registry of Medicinal Product Statistics. After exclusions, 62,716 patients with diabetes were randomly selected for the study: 15,679 statin users and 47,037 non–statin users. The primary outcome was the incidence of diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and gangrene of the foot. The design "captured 100% of individuals in Denmark who had ever used a statin within the time frame of the study."
Follow-up was censored at date of death for 9,560 individuals. During 215,725 person-years of follow-up, diabetic retinopathy was recorded in 2,866 patients, diabetic neuropathy in 1,406, diabetic nephropathy in 1,248, and gangrene of the foot in 2,392.
Over a median follow-up of 2.7 years, statin users were significantly less likely to be diagnosed with diabetic neuropathy (hazard ratio, 0.66; 95% confidence interval, 0.57-0.75: P less than .0001) and diabetic retinopathy (HR, 0.60; 95% CI 0.54-0.66: P less than .0001) than were those who had not received statins. However, no difference was noted in the incidence of diabetic nephropathy (HR, 0.97; 95% CI, 0.85-1.10; P = .62).
In contrast, the researchers found that statin use significantly increased the risk of developing diabetes in people who did not have the disease when the study began. When they compared a random selection of 272,994 non–statin users with 90,998 statin users, the multivariable adjusted hazard ratio for the risk of developing diabetes was 1.17 (95% CI, 1.14-1.21). These results are similar to those seen in previous randomized studies of statin use.
"In conclusion, we found no evidence that statin use is associated with an increased risk of microvascular disease; this result is important and clinically reassuring on its own. Whether or not statins are protective against some forms of microvascular disease, a possibility raised by these data, and by which mechanism, will need to be addressed in studies similar to ours, or in Mendelian randomization studies," said Dr. Nielsen and Dr. Nordestgaard. "Ideally, however, this question should be addressed in the setting of a randomized controlled trial," they added.
Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
Contrary to expectations, statin use before the development of type II diabetes did not worsen microvascular complications such as retinopathy, neuropathy, and gangrene of the foot.
In fact, despite concerns that statins have been seen to increase glucose levels and the risk of diabetes development, they may provide a protective effect from these conditions in newly developed diabetic patients, according to an analysis of data from more than 60,000 individuals in the Danish Patient Registry.
"The cumulative incidences of diabetic retinopathy, diabetic neuropathy, and gangrene were reduced in statin users compared with non–statin users, but [the] risk of diabetic nephropathy was similar for all patients with diabetes," stated Dr. Sune F. Nielsen, Ph.D., and Dr. Børge G. Nordestgaard of the Herlev Hospital, Copenhagen University Hospital. However, they did find that statin use, as previously seen, did significantly increase the risk of developing diabetes in the first place. Their study was published online Sept. 10 in the Lancet Diabetes & Endocrinology (2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
The researchers performed a nested matched study of all men and women living in Denmark who were diagnosed with incident diabetes during 1996-2009 at age 40 years or older, and assessed their outcomes through use of the Danish Civil Registration System, the Danish Patient Registry, and the Danish Registry of Medicinal Product Statistics. After exclusions, 62,716 patients with diabetes were randomly selected for the study: 15,679 statin users and 47,037 non–statin users. The primary outcome was the incidence of diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and gangrene of the foot. The design "captured 100% of individuals in Denmark who had ever used a statin within the time frame of the study."
Follow-up was censored at date of death for 9,560 individuals. During 215,725 person-years of follow-up, diabetic retinopathy was recorded in 2,866 patients, diabetic neuropathy in 1,406, diabetic nephropathy in 1,248, and gangrene of the foot in 2,392.
Over a median follow-up of 2.7 years, statin users were significantly less likely to be diagnosed with diabetic neuropathy (hazard ratio, 0.66; 95% confidence interval, 0.57-0.75: P less than .0001) and diabetic retinopathy (HR, 0.60; 95% CI 0.54-0.66: P less than .0001) than were those who had not received statins. However, no difference was noted in the incidence of diabetic nephropathy (HR, 0.97; 95% CI, 0.85-1.10; P = .62).
In contrast, the researchers found that statin use significantly increased the risk of developing diabetes in people who did not have the disease when the study began. When they compared a random selection of 272,994 non–statin users with 90,998 statin users, the multivariable adjusted hazard ratio for the risk of developing diabetes was 1.17 (95% CI, 1.14-1.21). These results are similar to those seen in previous randomized studies of statin use.
"In conclusion, we found no evidence that statin use is associated with an increased risk of microvascular disease; this result is important and clinically reassuring on its own. Whether or not statins are protective against some forms of microvascular disease, a possibility raised by these data, and by which mechanism, will need to be addressed in studies similar to ours, or in Mendelian randomization studies," said Dr. Nielsen and Dr. Nordestgaard. "Ideally, however, this question should be addressed in the setting of a randomized controlled trial," they added.
Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
FROM THE LANCET DIABETES & ENDOCRINOLOGY
Key clinical point: Statins may protect against microvascular complications in diabetes patients.
Major finding: Statin users were significantly less likely to be diagnosed with diabetic neuropathy (HR, 0.66) and diabetic retinopathy (HR, 0.60) than non–statin users.
Data source: A registry study compared 62,716 patients with diabetes: 15,679 statin users and 47,037 non–statin users.
Disclosures: Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
Asymptomatic carotid stenosis tied to mental decline
BOSTON – Asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis, said Dr. Brajesh K. Lal, of the University of Maryland, Baltimore.
Dr. Lal presented results from the Asymptomatic Carotid Stenosis and Cognitive Function (ACCOF) study. "The key finding is that we've identified for the first time unequivocally that an asymptomatic carotid artery plaque in a patient that has never suffered a stroke before can result in cognitive impairment," Dr. Lal said at the Vascular Annual Meeting.
Vascular comorbidities, such as diabetes, hypertension, coronary disease, and hyperlipidemia, are well known to cause vascular cognitive impairment (VCI), and this new research indicates that ACS should be added to that list, according to Dr. Lal and his colleagues.
They assessed 129 patients, 69 with greater than or equal to 50% ACS and 60 controls with vascular co-morbidities without ACS. An overall index of cognitive function and five domain-specific scores were computed. Breath-holding index (BHI), an estimate of cerebrovascular reserve, was measured using transcranial Doppler. Patients were assigned to high vs. low BHI groups using a cut-off score of 0.69. They assessed differences among stenosis vs. control patients and stenosis patients with low vs. high BHIs.
The stenosis and control groups did not differ with respect to vascular risk factors, IQ, educational attainment, and depressive symptoms. The stenosis group performed worse on the overall composite cognitive score and the domain-specific scores for processing speed and learning/memory, all significant differences. Within the stenosis group, those with low BHI performed significantly worse on learning, and trended lower on processing speed and overall composite score.
"The ACCOF study results showed that asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis. The deficit is driven primarily by reduced processing speed and learning/memory, and is mild to moderate in severity. A likely mechanism for this impairment is reduced cerebrovascular reserve," said Dr. Lal. "These findings have the potential to impact decision making in the management of patients with ACS."
Dr. Lal and his colleagues showed that moderate (>50%) asymptomatic carotid stenosis (ACS) is associated with cognitive impairment. They claim that "these findings have the potential to impact decision making in the management of patients with ACS" and presumably to support more aggressive treatment of carotid plaque by either endarterectomy or stenting. While their findings suggest that the latter presumption may be the case, two other questions must be answered. The first is whether there is a cause and effect relationship and not just an association. The second and more important element that must be shown is that elimination of the plaque or restoration of luminal diameter to the stenotic carotid artery will reverse the decline. Until the latter is proven, it is hard to see how these findings alone can justify increasing the indications for more aggressive treatment. Hopefully in future work, Dr. Lal and his colleagues will address these two questions so that the therapeutic implications of his interesting findings can be fully realized.
Dr. Frank J. Veith is an associate medical editor for Vascular Specialist.
Dr. Lal and his colleagues showed that moderate (>50%) asymptomatic carotid stenosis (ACS) is associated with cognitive impairment. They claim that "these findings have the potential to impact decision making in the management of patients with ACS" and presumably to support more aggressive treatment of carotid plaque by either endarterectomy or stenting. While their findings suggest that the latter presumption may be the case, two other questions must be answered. The first is whether there is a cause and effect relationship and not just an association. The second and more important element that must be shown is that elimination of the plaque or restoration of luminal diameter to the stenotic carotid artery will reverse the decline. Until the latter is proven, it is hard to see how these findings alone can justify increasing the indications for more aggressive treatment. Hopefully in future work, Dr. Lal and his colleagues will address these two questions so that the therapeutic implications of his interesting findings can be fully realized.
Dr. Frank J. Veith is an associate medical editor for Vascular Specialist.
Dr. Lal and his colleagues showed that moderate (>50%) asymptomatic carotid stenosis (ACS) is associated with cognitive impairment. They claim that "these findings have the potential to impact decision making in the management of patients with ACS" and presumably to support more aggressive treatment of carotid plaque by either endarterectomy or stenting. While their findings suggest that the latter presumption may be the case, two other questions must be answered. The first is whether there is a cause and effect relationship and not just an association. The second and more important element that must be shown is that elimination of the plaque or restoration of luminal diameter to the stenotic carotid artery will reverse the decline. Until the latter is proven, it is hard to see how these findings alone can justify increasing the indications for more aggressive treatment. Hopefully in future work, Dr. Lal and his colleagues will address these two questions so that the therapeutic implications of his interesting findings can be fully realized.
Dr. Frank J. Veith is an associate medical editor for Vascular Specialist.
BOSTON – Asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis, said Dr. Brajesh K. Lal, of the University of Maryland, Baltimore.
Dr. Lal presented results from the Asymptomatic Carotid Stenosis and Cognitive Function (ACCOF) study. "The key finding is that we've identified for the first time unequivocally that an asymptomatic carotid artery plaque in a patient that has never suffered a stroke before can result in cognitive impairment," Dr. Lal said at the Vascular Annual Meeting.
Vascular comorbidities, such as diabetes, hypertension, coronary disease, and hyperlipidemia, are well known to cause vascular cognitive impairment (VCI), and this new research indicates that ACS should be added to that list, according to Dr. Lal and his colleagues.
They assessed 129 patients, 69 with greater than or equal to 50% ACS and 60 controls with vascular co-morbidities without ACS. An overall index of cognitive function and five domain-specific scores were computed. Breath-holding index (BHI), an estimate of cerebrovascular reserve, was measured using transcranial Doppler. Patients were assigned to high vs. low BHI groups using a cut-off score of 0.69. They assessed differences among stenosis vs. control patients and stenosis patients with low vs. high BHIs.
The stenosis and control groups did not differ with respect to vascular risk factors, IQ, educational attainment, and depressive symptoms. The stenosis group performed worse on the overall composite cognitive score and the domain-specific scores for processing speed and learning/memory, all significant differences. Within the stenosis group, those with low BHI performed significantly worse on learning, and trended lower on processing speed and overall composite score.
"The ACCOF study results showed that asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis. The deficit is driven primarily by reduced processing speed and learning/memory, and is mild to moderate in severity. A likely mechanism for this impairment is reduced cerebrovascular reserve," said Dr. Lal. "These findings have the potential to impact decision making in the management of patients with ACS."
BOSTON – Asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis, said Dr. Brajesh K. Lal, of the University of Maryland, Baltimore.
Dr. Lal presented results from the Asymptomatic Carotid Stenosis and Cognitive Function (ACCOF) study. "The key finding is that we've identified for the first time unequivocally that an asymptomatic carotid artery plaque in a patient that has never suffered a stroke before can result in cognitive impairment," Dr. Lal said at the Vascular Annual Meeting.
Vascular comorbidities, such as diabetes, hypertension, coronary disease, and hyperlipidemia, are well known to cause vascular cognitive impairment (VCI), and this new research indicates that ACS should be added to that list, according to Dr. Lal and his colleagues.
They assessed 129 patients, 69 with greater than or equal to 50% ACS and 60 controls with vascular co-morbidities without ACS. An overall index of cognitive function and five domain-specific scores were computed. Breath-holding index (BHI), an estimate of cerebrovascular reserve, was measured using transcranial Doppler. Patients were assigned to high vs. low BHI groups using a cut-off score of 0.69. They assessed differences among stenosis vs. control patients and stenosis patients with low vs. high BHIs.
The stenosis and control groups did not differ with respect to vascular risk factors, IQ, educational attainment, and depressive symptoms. The stenosis group performed worse on the overall composite cognitive score and the domain-specific scores for processing speed and learning/memory, all significant differences. Within the stenosis group, those with low BHI performed significantly worse on learning, and trended lower on processing speed and overall composite score.
"The ACCOF study results showed that asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis. The deficit is driven primarily by reduced processing speed and learning/memory, and is mild to moderate in severity. A likely mechanism for this impairment is reduced cerebrovascular reserve," said Dr. Lal. "These findings have the potential to impact decision making in the management of patients with ACS."
Crawford Forum: Are procedures overused?
BOSTON – This year’s F. Stanley Crawford Critical Issues Forum, titled "Appropriate Use of Vascular Surgery Procedures: Do We Have a Problem?," was a response to the question of whether vascular surgeons are performing too many procedures and if enough evidence exists to support the ones that are being done, according to Dr. Peter F. Lawrence, incoming president of the SVS. Dr. Lawrence, who organized this year’s session, discussed how the issue of overuse and appropriateness has become a common theme in the media, in public policy discussions, and among medical societies.
"In Vascular Specialist, our newspaper, both Drs. Frank Veith and Russell Samson have written editorials about the overuse of vascular procedures. Dr. Veith titled his topic ‘The Blacksnake Phenomenon’ and pointed out that not everything that we find and identify needs to be treated."
Dr. Lawrence chose and introduced five speakers charged with addressing the problem.
Dr. Robert M. Zwolak addressed the currently available data on vascular surgery procedures, focusing in particular on the Medicare procedural data derived from the Centers for Medicare & Medicaid Services. He pointed out several instances where the number of vascular procedures performed decreased tremendously over time, independent of reimbursement, including a remarkable 47% decrease in major amputations from 1996 to 2013. Open lower extremity bypass decreased, by 57%, to such a low level that it called into question the ability of the specialty to maintain excellence in performing the procedure. On the flip side, there was also a tremendous increase in certain procedures, including vein treatments, which grew more than 6,000% when reimbursement became available.
Dr. Michael D. Dake addressed the critical issue of optimizing multispecialty involvement in vascular procedures. In particular, he advocated a cooperative vs. adversarial approach. This included working together for common credentialing, institutional harmonization, and development of "care teams" for vascular diseases, such as already exist for transcatheter aortic valve replacement. He said SVS should take responsibility for promoting a "Big Tent approach" and become the overarching society dealing with all things vascular, including involvement in common credentialing and guidelines development.
Dr. Timothy Ferris discussed the various types of influence that hospital and physician practice organizations could have that impact appropriateness. In particular, he outlined a computer program that his own institution, Massachusetts General Hospital, Boston, developed that allows physicians to recognize and comply with guideline criteria generated through multispecialty consensus at the hospital. Within a few years, they found a tremendous increase in the number of procedures deemed appropriate. This information enabled them to influence insurance providers to waive the necessity of preauthorization, which often requires up to 30 people to fill out the paperwork.
Dr. Peter Gloviczki addressed the issue of practice guidelines as criteria for determining appropriateness. He reiterated their importance, but maintained that they were highly variable in their evidentiary basis, and that the quality of individual guidelines should always be considered so as to avoid a "herd mentality."
Dr. Samson topped off the forum with a discussion of the ethical issues related to frequency of procedures. He pointed out that personal integrity is critical and that the greatest potential risk of unethical behavior exists in outpatient centers. "The only time an intervention occurs is when a major complication sends a patient to a hospital or a negligent action results in a malpractice suit. As long as our government and insurers fail to determine what and where and who should be doing these procedures, I believe we will have unscrupulous doctors let loose on their unsuspecting prey." He said one of the ways to prevent this was to require that only board-certified and appropriately trained physicians be allowed to perform procedures.
BOSTON – This year’s F. Stanley Crawford Critical Issues Forum, titled "Appropriate Use of Vascular Surgery Procedures: Do We Have a Problem?," was a response to the question of whether vascular surgeons are performing too many procedures and if enough evidence exists to support the ones that are being done, according to Dr. Peter F. Lawrence, incoming president of the SVS. Dr. Lawrence, who organized this year’s session, discussed how the issue of overuse and appropriateness has become a common theme in the media, in public policy discussions, and among medical societies.
"In Vascular Specialist, our newspaper, both Drs. Frank Veith and Russell Samson have written editorials about the overuse of vascular procedures. Dr. Veith titled his topic ‘The Blacksnake Phenomenon’ and pointed out that not everything that we find and identify needs to be treated."
Dr. Lawrence chose and introduced five speakers charged with addressing the problem.
Dr. Robert M. Zwolak addressed the currently available data on vascular surgery procedures, focusing in particular on the Medicare procedural data derived from the Centers for Medicare & Medicaid Services. He pointed out several instances where the number of vascular procedures performed decreased tremendously over time, independent of reimbursement, including a remarkable 47% decrease in major amputations from 1996 to 2013. Open lower extremity bypass decreased, by 57%, to such a low level that it called into question the ability of the specialty to maintain excellence in performing the procedure. On the flip side, there was also a tremendous increase in certain procedures, including vein treatments, which grew more than 6,000% when reimbursement became available.
Dr. Michael D. Dake addressed the critical issue of optimizing multispecialty involvement in vascular procedures. In particular, he advocated a cooperative vs. adversarial approach. This included working together for common credentialing, institutional harmonization, and development of "care teams" for vascular diseases, such as already exist for transcatheter aortic valve replacement. He said SVS should take responsibility for promoting a "Big Tent approach" and become the overarching society dealing with all things vascular, including involvement in common credentialing and guidelines development.
Dr. Timothy Ferris discussed the various types of influence that hospital and physician practice organizations could have that impact appropriateness. In particular, he outlined a computer program that his own institution, Massachusetts General Hospital, Boston, developed that allows physicians to recognize and comply with guideline criteria generated through multispecialty consensus at the hospital. Within a few years, they found a tremendous increase in the number of procedures deemed appropriate. This information enabled them to influence insurance providers to waive the necessity of preauthorization, which often requires up to 30 people to fill out the paperwork.
Dr. Peter Gloviczki addressed the issue of practice guidelines as criteria for determining appropriateness. He reiterated their importance, but maintained that they were highly variable in their evidentiary basis, and that the quality of individual guidelines should always be considered so as to avoid a "herd mentality."
Dr. Samson topped off the forum with a discussion of the ethical issues related to frequency of procedures. He pointed out that personal integrity is critical and that the greatest potential risk of unethical behavior exists in outpatient centers. "The only time an intervention occurs is when a major complication sends a patient to a hospital or a negligent action results in a malpractice suit. As long as our government and insurers fail to determine what and where and who should be doing these procedures, I believe we will have unscrupulous doctors let loose on their unsuspecting prey." He said one of the ways to prevent this was to require that only board-certified and appropriately trained physicians be allowed to perform procedures.
BOSTON – This year’s F. Stanley Crawford Critical Issues Forum, titled "Appropriate Use of Vascular Surgery Procedures: Do We Have a Problem?," was a response to the question of whether vascular surgeons are performing too many procedures and if enough evidence exists to support the ones that are being done, according to Dr. Peter F. Lawrence, incoming president of the SVS. Dr. Lawrence, who organized this year’s session, discussed how the issue of overuse and appropriateness has become a common theme in the media, in public policy discussions, and among medical societies.
"In Vascular Specialist, our newspaper, both Drs. Frank Veith and Russell Samson have written editorials about the overuse of vascular procedures. Dr. Veith titled his topic ‘The Blacksnake Phenomenon’ and pointed out that not everything that we find and identify needs to be treated."
Dr. Lawrence chose and introduced five speakers charged with addressing the problem.
Dr. Robert M. Zwolak addressed the currently available data on vascular surgery procedures, focusing in particular on the Medicare procedural data derived from the Centers for Medicare & Medicaid Services. He pointed out several instances where the number of vascular procedures performed decreased tremendously over time, independent of reimbursement, including a remarkable 47% decrease in major amputations from 1996 to 2013. Open lower extremity bypass decreased, by 57%, to such a low level that it called into question the ability of the specialty to maintain excellence in performing the procedure. On the flip side, there was also a tremendous increase in certain procedures, including vein treatments, which grew more than 6,000% when reimbursement became available.
Dr. Michael D. Dake addressed the critical issue of optimizing multispecialty involvement in vascular procedures. In particular, he advocated a cooperative vs. adversarial approach. This included working together for common credentialing, institutional harmonization, and development of "care teams" for vascular diseases, such as already exist for transcatheter aortic valve replacement. He said SVS should take responsibility for promoting a "Big Tent approach" and become the overarching society dealing with all things vascular, including involvement in common credentialing and guidelines development.
Dr. Timothy Ferris discussed the various types of influence that hospital and physician practice organizations could have that impact appropriateness. In particular, he outlined a computer program that his own institution, Massachusetts General Hospital, Boston, developed that allows physicians to recognize and comply with guideline criteria generated through multispecialty consensus at the hospital. Within a few years, they found a tremendous increase in the number of procedures deemed appropriate. This information enabled them to influence insurance providers to waive the necessity of preauthorization, which often requires up to 30 people to fill out the paperwork.
Dr. Peter Gloviczki addressed the issue of practice guidelines as criteria for determining appropriateness. He reiterated their importance, but maintained that they were highly variable in their evidentiary basis, and that the quality of individual guidelines should always be considered so as to avoid a "herd mentality."
Dr. Samson topped off the forum with a discussion of the ethical issues related to frequency of procedures. He pointed out that personal integrity is critical and that the greatest potential risk of unethical behavior exists in outpatient centers. "The only time an intervention occurs is when a major complication sends a patient to a hospital or a negligent action results in a malpractice suit. As long as our government and insurers fail to determine what and where and who should be doing these procedures, I believe we will have unscrupulous doctors let loose on their unsuspecting prey." He said one of the ways to prevent this was to require that only board-certified and appropriately trained physicians be allowed to perform procedures.
Delayed revisions led to worse congenital outcomes
In previous studies on patients under 6 months of age undergoing a wide range of congenital cardiac operations, Dr. Meena Nathan and her colleagues at Boston Children’s Hospital found that immediate revisions of procedures intraoperatively that resulted in adequate anatomic correction of residual defects did not affect outcomes, but that delayed revisions of residual lesions resulted in worse patient outcomes.
Dr. Nathan presented the results of a larger prospective cohort of patients that she and her colleagues studied who were followed from index surgery to discharge from January 2011 to September 2013.
Patients were divided into four groups: a) intraoperative revisions of residual lesion, b) delayed postoperative revision of residual lesions during the same hospital stay, c) both intraoperative and delayed (BOTH) revision of residual lesions, d) and no revisions (neither intraoperative nor postoperative revision), Dr. Nathan said at the annual meeting of the American Association for Thoracic Surgery.
They used linear and logistic regression to compare the outcomes mortality, complications (excluding unplanned postoperative reinterventions) and postoperative hospital length of stay across the four groups (using patients who had intraoperative revisions only as reference group).
"We adjusted for baseline patient risk including age, prematurity, presence of extracardiac anomalies, and RACHS-1 risk category, each of which could contribute to the difference in outcomes," according to Dr. Nathan.
"In addition, to allow inclusion of all patients in the risk-adjusted analyses, we added two additional categories to the RACHS-1 categories: all patients less than 18 years of age with non–RACHS-1 categorizable procedures, and adults greater than 18 years who are not eligible for RACHS-1 risk adjustment," Dr. Nathan added.
A total of 2,427 patients were discharged after congenital cardiac operations during the time period studied.
As might be expected, on multivariable modeling, adjusting for other significant patient factors, the no-revisions group fared better than the other three groups. The intraoperative revision group had significantly lower postoperative length of stay and complication rates when compared to the delayed postoperative revision and the BOTH group, but they showed no significant differences in mortality compared to these two groups.
On subgroup analysis of the intraoperative revision group, 86% left the hospital with an optimal or adequate repair on discharge echocardiogram, Dr. Nathan added.
"We found that the intraoperative correction of residual lesions results in a shorter length of stay and lower complications when compared to those patients who underwent delayed postoperative revision of residual lesion," she concluded.
Dr. Nathan reported that she had no relevant disclosures.
In previous studies on patients under 6 months of age undergoing a wide range of congenital cardiac operations, Dr. Meena Nathan and her colleagues at Boston Children’s Hospital found that immediate revisions of procedures intraoperatively that resulted in adequate anatomic correction of residual defects did not affect outcomes, but that delayed revisions of residual lesions resulted in worse patient outcomes.
Dr. Nathan presented the results of a larger prospective cohort of patients that she and her colleagues studied who were followed from index surgery to discharge from January 2011 to September 2013.
Patients were divided into four groups: a) intraoperative revisions of residual lesion, b) delayed postoperative revision of residual lesions during the same hospital stay, c) both intraoperative and delayed (BOTH) revision of residual lesions, d) and no revisions (neither intraoperative nor postoperative revision), Dr. Nathan said at the annual meeting of the American Association for Thoracic Surgery.
They used linear and logistic regression to compare the outcomes mortality, complications (excluding unplanned postoperative reinterventions) and postoperative hospital length of stay across the four groups (using patients who had intraoperative revisions only as reference group).
"We adjusted for baseline patient risk including age, prematurity, presence of extracardiac anomalies, and RACHS-1 risk category, each of which could contribute to the difference in outcomes," according to Dr. Nathan.
"In addition, to allow inclusion of all patients in the risk-adjusted analyses, we added two additional categories to the RACHS-1 categories: all patients less than 18 years of age with non–RACHS-1 categorizable procedures, and adults greater than 18 years who are not eligible for RACHS-1 risk adjustment," Dr. Nathan added.
A total of 2,427 patients were discharged after congenital cardiac operations during the time period studied.
As might be expected, on multivariable modeling, adjusting for other significant patient factors, the no-revisions group fared better than the other three groups. The intraoperative revision group had significantly lower postoperative length of stay and complication rates when compared to the delayed postoperative revision and the BOTH group, but they showed no significant differences in mortality compared to these two groups.
On subgroup analysis of the intraoperative revision group, 86% left the hospital with an optimal or adequate repair on discharge echocardiogram, Dr. Nathan added.
"We found that the intraoperative correction of residual lesions results in a shorter length of stay and lower complications when compared to those patients who underwent delayed postoperative revision of residual lesion," she concluded.
Dr. Nathan reported that she had no relevant disclosures.
In previous studies on patients under 6 months of age undergoing a wide range of congenital cardiac operations, Dr. Meena Nathan and her colleagues at Boston Children’s Hospital found that immediate revisions of procedures intraoperatively that resulted in adequate anatomic correction of residual defects did not affect outcomes, but that delayed revisions of residual lesions resulted in worse patient outcomes.
Dr. Nathan presented the results of a larger prospective cohort of patients that she and her colleagues studied who were followed from index surgery to discharge from January 2011 to September 2013.
Patients were divided into four groups: a) intraoperative revisions of residual lesion, b) delayed postoperative revision of residual lesions during the same hospital stay, c) both intraoperative and delayed (BOTH) revision of residual lesions, d) and no revisions (neither intraoperative nor postoperative revision), Dr. Nathan said at the annual meeting of the American Association for Thoracic Surgery.
They used linear and logistic regression to compare the outcomes mortality, complications (excluding unplanned postoperative reinterventions) and postoperative hospital length of stay across the four groups (using patients who had intraoperative revisions only as reference group).
"We adjusted for baseline patient risk including age, prematurity, presence of extracardiac anomalies, and RACHS-1 risk category, each of which could contribute to the difference in outcomes," according to Dr. Nathan.
"In addition, to allow inclusion of all patients in the risk-adjusted analyses, we added two additional categories to the RACHS-1 categories: all patients less than 18 years of age with non–RACHS-1 categorizable procedures, and adults greater than 18 years who are not eligible for RACHS-1 risk adjustment," Dr. Nathan added.
A total of 2,427 patients were discharged after congenital cardiac operations during the time period studied.
As might be expected, on multivariable modeling, adjusting for other significant patient factors, the no-revisions group fared better than the other three groups. The intraoperative revision group had significantly lower postoperative length of stay and complication rates when compared to the delayed postoperative revision and the BOTH group, but they showed no significant differences in mortality compared to these two groups.
On subgroup analysis of the intraoperative revision group, 86% left the hospital with an optimal or adequate repair on discharge echocardiogram, Dr. Nathan added.
"We found that the intraoperative correction of residual lesions results in a shorter length of stay and lower complications when compared to those patients who underwent delayed postoperative revision of residual lesion," she concluded.
Dr. Nathan reported that she had no relevant disclosures.
Open repair of acute DeBakey type I dissection favorable
TORONTO - Placing a stent-graft in the descending thoracic aorta during surgical repair of the proximal aorta of patients with acute DeBakey type I dissection is becoming an increasingly popular approach. A suggested advantage of this approach is the avoidance of subsequent, high-risk operations to repair the descending and thoracoabdominal aortic segments in those patients whose chronic dissection causes later aneurysm formation.
Dr. Joseph S. Coselli presented a study that he and his colleagues at the Baylor College of Medicine undertook to better define the risks associated with these secondary operations that stenting is suggested to avoid. They found that the use of open repair showed excellent early survival and acceptable morbidity and the use of adjuncts to protect against ischemic complications was associated with improved early outcomes.
"We prospectively examined our contemporary experience with open distal aortic repair in patients with chronic DeBakey type I aortic dissection in 200 consecutive patients with open descending thoracic (n = 29) or thoracoabdominal (n = 171) aortic repairs. Data were collected between January 2005 and June 2013," said Dr. Coselli at the annual meeting of the American Association for Thoracic Surgery.
The median patient age was 57 years, and the median interval between initial proximal aortic repair and the subsequent distal operation was 4.8 years. In 30 patients (15%), repairs were prompted by the onset of acute symptoms; this included 10 patients (5%) who had a new acute DeBakey type III dissection superimposed on the chronic dissection. Forty-three repairs (22%) were emergent or urgent, and hypothermic circulatory arrest was necessary in 17 (9%).
Of the 171 thoracoabdominal aortic repairs, 145 (86%) were Crawford extent I or II; adjuncts used during thoracoabdominal procedures included cerebrospinal fluid drainage in 159 patients (93%), left heart bypass in 128 (75%), and cold renal perfusion in 123 (72%). The researchers used univariate and bivariate analyses to examine associations between potential risk factors and early death.
There were 14 early deaths (7%) and 35 late deaths, yielding an actuarial 6-year survival of 71%. Two patients (1%) developed permanent paraplegia, 4 (2%) had permanent paraparesis, 10 (5%) had strokes, and 9 (5%) had permanent renal failure necessitating dialysis. Greater age and the use of hypothermic circulatory arrest were significantly associated with early death. The use of left heart bypass and the use of cold renal perfusion were each significantly associated with early survival. There were no associations between early death and connective tissue disorders, emergent or urgent surgery, or extent of aortic repair, Dr. Coselli added.
"For our patients who survived DeBakey type I aortic dissection and subsequently develop distal aortic aneurysms, the use of open repair of the descending thoracic or thoracoabdominal aorta results in excellent early survival and acceptable morbidity. We found that the use of adjuncts to protect against ischemic complications is associated with improved early outcomes," Dr. Coselli stated.
In an interview, Dr. Coselli added that it is important to note that the disease process leading to late aneurysm after DeBakey type I dissection is likely much different than it is for the typically older cohort of distal aortic repairs for purely aneurysmal disease. The DeBakey I patients are about a decade or more younger and seem to have much less atherosclerotic disease. "We use the need for visceral endarterectomy as a marker for this," he said.
And, since older age is one of the best predictors of operative mortality and adverse event, the DeBakey I patients tend to do better than the typical older cohort undergoing open distal aortic repair. This is despite the fact that the vast majority of patients had an extensive history of prior aortic repair, including 35 repairs with prior open distal aortic repair or prior TEVAR (and naturally, extensive prior proximal aortic repair).
"The rate of permanent paraplegia was low, we speculated that the progressive nature of late distal aortic dilatation contributes to this low rate. Often DTA repair is followed by TAAA repair or vice versa. This is similar to the 'staged model' of distal aortic repair that Dr. Randall Griepp and Dr. C.D. Etz have published [Eur. J. Cardiothorac. Surg. 2008 34(3):605-14], possibly allowing for collateral circulation. This combined with our aggressive reattachment strategy for intercostal/lumbar arteries, may have contributed to this low rate," he added.
"Lastly, the reintervention rates for antegrade TEVAR and frozen elephant trunk tend to be high, and there is concern for an enhanced risk of paraplegia during these types of repairs. And with standard TEVAR, the rates of reintervention in patients with chronic dissection appear greater than those with only an aneurysm," Dr. Coselli concluded.
The authors of the study reported having no conflicts.
TORONTO - Placing a stent-graft in the descending thoracic aorta during surgical repair of the proximal aorta of patients with acute DeBakey type I dissection is becoming an increasingly popular approach. A suggested advantage of this approach is the avoidance of subsequent, high-risk operations to repair the descending and thoracoabdominal aortic segments in those patients whose chronic dissection causes later aneurysm formation.
Dr. Joseph S. Coselli presented a study that he and his colleagues at the Baylor College of Medicine undertook to better define the risks associated with these secondary operations that stenting is suggested to avoid. They found that the use of open repair showed excellent early survival and acceptable morbidity and the use of adjuncts to protect against ischemic complications was associated with improved early outcomes.
"We prospectively examined our contemporary experience with open distal aortic repair in patients with chronic DeBakey type I aortic dissection in 200 consecutive patients with open descending thoracic (n = 29) or thoracoabdominal (n = 171) aortic repairs. Data were collected between January 2005 and June 2013," said Dr. Coselli at the annual meeting of the American Association for Thoracic Surgery.
The median patient age was 57 years, and the median interval between initial proximal aortic repair and the subsequent distal operation was 4.8 years. In 30 patients (15%), repairs were prompted by the onset of acute symptoms; this included 10 patients (5%) who had a new acute DeBakey type III dissection superimposed on the chronic dissection. Forty-three repairs (22%) were emergent or urgent, and hypothermic circulatory arrest was necessary in 17 (9%).
Of the 171 thoracoabdominal aortic repairs, 145 (86%) were Crawford extent I or II; adjuncts used during thoracoabdominal procedures included cerebrospinal fluid drainage in 159 patients (93%), left heart bypass in 128 (75%), and cold renal perfusion in 123 (72%). The researchers used univariate and bivariate analyses to examine associations between potential risk factors and early death.
There were 14 early deaths (7%) and 35 late deaths, yielding an actuarial 6-year survival of 71%. Two patients (1%) developed permanent paraplegia, 4 (2%) had permanent paraparesis, 10 (5%) had strokes, and 9 (5%) had permanent renal failure necessitating dialysis. Greater age and the use of hypothermic circulatory arrest were significantly associated with early death. The use of left heart bypass and the use of cold renal perfusion were each significantly associated with early survival. There were no associations between early death and connective tissue disorders, emergent or urgent surgery, or extent of aortic repair, Dr. Coselli added.
"For our patients who survived DeBakey type I aortic dissection and subsequently develop distal aortic aneurysms, the use of open repair of the descending thoracic or thoracoabdominal aorta results in excellent early survival and acceptable morbidity. We found that the use of adjuncts to protect against ischemic complications is associated with improved early outcomes," Dr. Coselli stated.
In an interview, Dr. Coselli added that it is important to note that the disease process leading to late aneurysm after DeBakey type I dissection is likely much different than it is for the typically older cohort of distal aortic repairs for purely aneurysmal disease. The DeBakey I patients are about a decade or more younger and seem to have much less atherosclerotic disease. "We use the need for visceral endarterectomy as a marker for this," he said.
And, since older age is one of the best predictors of operative mortality and adverse event, the DeBakey I patients tend to do better than the typical older cohort undergoing open distal aortic repair. This is despite the fact that the vast majority of patients had an extensive history of prior aortic repair, including 35 repairs with prior open distal aortic repair or prior TEVAR (and naturally, extensive prior proximal aortic repair).
"The rate of permanent paraplegia was low, we speculated that the progressive nature of late distal aortic dilatation contributes to this low rate. Often DTA repair is followed by TAAA repair or vice versa. This is similar to the 'staged model' of distal aortic repair that Dr. Randall Griepp and Dr. C.D. Etz have published [Eur. J. Cardiothorac. Surg. 2008 34(3):605-14], possibly allowing for collateral circulation. This combined with our aggressive reattachment strategy for intercostal/lumbar arteries, may have contributed to this low rate," he added.
"Lastly, the reintervention rates for antegrade TEVAR and frozen elephant trunk tend to be high, and there is concern for an enhanced risk of paraplegia during these types of repairs. And with standard TEVAR, the rates of reintervention in patients with chronic dissection appear greater than those with only an aneurysm," Dr. Coselli concluded.
The authors of the study reported having no conflicts.
TORONTO - Placing a stent-graft in the descending thoracic aorta during surgical repair of the proximal aorta of patients with acute DeBakey type I dissection is becoming an increasingly popular approach. A suggested advantage of this approach is the avoidance of subsequent, high-risk operations to repair the descending and thoracoabdominal aortic segments in those patients whose chronic dissection causes later aneurysm formation.
Dr. Joseph S. Coselli presented a study that he and his colleagues at the Baylor College of Medicine undertook to better define the risks associated with these secondary operations that stenting is suggested to avoid. They found that the use of open repair showed excellent early survival and acceptable morbidity and the use of adjuncts to protect against ischemic complications was associated with improved early outcomes.
"We prospectively examined our contemporary experience with open distal aortic repair in patients with chronic DeBakey type I aortic dissection in 200 consecutive patients with open descending thoracic (n = 29) or thoracoabdominal (n = 171) aortic repairs. Data were collected between January 2005 and June 2013," said Dr. Coselli at the annual meeting of the American Association for Thoracic Surgery.
The median patient age was 57 years, and the median interval between initial proximal aortic repair and the subsequent distal operation was 4.8 years. In 30 patients (15%), repairs were prompted by the onset of acute symptoms; this included 10 patients (5%) who had a new acute DeBakey type III dissection superimposed on the chronic dissection. Forty-three repairs (22%) were emergent or urgent, and hypothermic circulatory arrest was necessary in 17 (9%).
Of the 171 thoracoabdominal aortic repairs, 145 (86%) were Crawford extent I or II; adjuncts used during thoracoabdominal procedures included cerebrospinal fluid drainage in 159 patients (93%), left heart bypass in 128 (75%), and cold renal perfusion in 123 (72%). The researchers used univariate and bivariate analyses to examine associations between potential risk factors and early death.
There were 14 early deaths (7%) and 35 late deaths, yielding an actuarial 6-year survival of 71%. Two patients (1%) developed permanent paraplegia, 4 (2%) had permanent paraparesis, 10 (5%) had strokes, and 9 (5%) had permanent renal failure necessitating dialysis. Greater age and the use of hypothermic circulatory arrest were significantly associated with early death. The use of left heart bypass and the use of cold renal perfusion were each significantly associated with early survival. There were no associations between early death and connective tissue disorders, emergent or urgent surgery, or extent of aortic repair, Dr. Coselli added.
"For our patients who survived DeBakey type I aortic dissection and subsequently develop distal aortic aneurysms, the use of open repair of the descending thoracic or thoracoabdominal aorta results in excellent early survival and acceptable morbidity. We found that the use of adjuncts to protect against ischemic complications is associated with improved early outcomes," Dr. Coselli stated.
In an interview, Dr. Coselli added that it is important to note that the disease process leading to late aneurysm after DeBakey type I dissection is likely much different than it is for the typically older cohort of distal aortic repairs for purely aneurysmal disease. The DeBakey I patients are about a decade or more younger and seem to have much less atherosclerotic disease. "We use the need for visceral endarterectomy as a marker for this," he said.
And, since older age is one of the best predictors of operative mortality and adverse event, the DeBakey I patients tend to do better than the typical older cohort undergoing open distal aortic repair. This is despite the fact that the vast majority of patients had an extensive history of prior aortic repair, including 35 repairs with prior open distal aortic repair or prior TEVAR (and naturally, extensive prior proximal aortic repair).
"The rate of permanent paraplegia was low, we speculated that the progressive nature of late distal aortic dilatation contributes to this low rate. Often DTA repair is followed by TAAA repair or vice versa. This is similar to the 'staged model' of distal aortic repair that Dr. Randall Griepp and Dr. C.D. Etz have published [Eur. J. Cardiothorac. Surg. 2008 34(3):605-14], possibly allowing for collateral circulation. This combined with our aggressive reattachment strategy for intercostal/lumbar arteries, may have contributed to this low rate," he added.
"Lastly, the reintervention rates for antegrade TEVAR and frozen elephant trunk tend to be high, and there is concern for an enhanced risk of paraplegia during these types of repairs. And with standard TEVAR, the rates of reintervention in patients with chronic dissection appear greater than those with only an aneurysm," Dr. Coselli concluded.
The authors of the study reported having no conflicts.
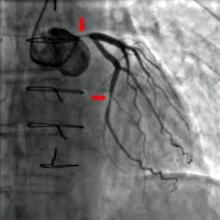
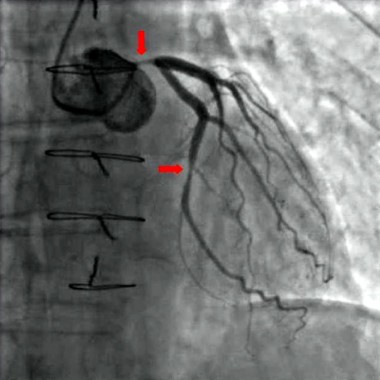
BITA improves CABG in diabetic patients
Diabetes has historically been associated with greater mortality and more and worse postoperative complications after coronary artery bypass grafting (CABG). Researchers continue to search for improved surgical techniques and other options to improve CABG outcomes in diabetic patients.
The use of bilateral internal thoracic artery (ITA) grafting and complete revascularization was found to improve the results of CABG in patients with diabetes, according to the results of an assessment of nearly 12,000 diabetic patients who underwent surgical revascularization, according to Dr. Sajjad Raza, a research fellow in cardiac surgery, who presented the results of a study that he and his colleagues performed at the Cleveland Clinic.
Patients who were operated upon from January 1972 to January 2011 were included in the study.
"Our research was designed to identify surgical revascularization techniques that can improve early and late results in patients with diabetes undergoing CABG," said Dr. Raza at the annual meeting of the American Association for Thoracic Surgery.
Surgical revascularization techniques investigated comprised single (71%) and bilateral (7.9%) ITA with or without other grafts vs. the use of saphenous vein grafting alone (SVG, 21%), as well as incomplete (18%) vs. complete revascularization, and the use of off- (5.0%) vs. on-pump CABG. The median follow-up was nearly 8 years, with total follow-up of more than 100,000 patient-years, according to Dr. Raza.
Multivariable analysis was performed to assess the effect of surgical techniques on early and late mortality.
After adjustment for patient characteristics, single ITA grafting with or without other grafts vs. SVG alone was associated with a 43% decrease in early mortality and 17% decrease in late mortality. The use of bilateral ITA grafting with or without other grafts led to a 60% decrease in early mortality and a 33% decrease in late mortality, with all hazard ratios being within their confidence intervals, and hence significant, said Dr.Raza.
In addition, bilateral ITA grafting was found to be significantly more effective than single ITA grafting in decreasing late mortality in patients with multisystem disease.
Incomplete revascularization was not found to be associated with increased early mortality, but was significantly associated with a 10% increase in late mortality The use of off-pump vs. on-pump CABG had no statistically significant effect on early and late mortality, Dr. Raza added.
"Overall, bilateral ITA grafting and complete revascularization improved results of CABG in diabetics. These surgical techniques should be used in diabetics undergoing CABG," Dr. Raza stated.
In an interview, commenting on the significance of the research, Dr. Raza added: "Diabetes is an emerging epidemic affecting nearly 382 million people worldwide. Because it is a risk factor for development of coronary artery disease, the number of diabetics undergoing coronary surgery has increased to nearly 50% of all patients undergoing surgical revascularization today.
"We know from the BARI2D and FREEDOM studies that for diabetics with multivessel coronary artery disease, CABG results in better outcomes than medical therapy or percutaneous coronary intervention. However, what remains unclear is which surgical revascularization techniques improve the outcomes of CABG in patients with diabetes. Our study helps to answer this important question," he concluded.
Dr. Raza reported having no relevant disclosures.
Diabetes has historically been associated with greater mortality and more and worse postoperative complications after coronary artery bypass grafting (CABG). Researchers continue to search for improved surgical techniques and other options to improve CABG outcomes in diabetic patients.
The use of bilateral internal thoracic artery (ITA) grafting and complete revascularization was found to improve the results of CABG in patients with diabetes, according to the results of an assessment of nearly 12,000 diabetic patients who underwent surgical revascularization, according to Dr. Sajjad Raza, a research fellow in cardiac surgery, who presented the results of a study that he and his colleagues performed at the Cleveland Clinic.
Patients who were operated upon from January 1972 to January 2011 were included in the study.
"Our research was designed to identify surgical revascularization techniques that can improve early and late results in patients with diabetes undergoing CABG," said Dr. Raza at the annual meeting of the American Association for Thoracic Surgery.
Surgical revascularization techniques investigated comprised single (71%) and bilateral (7.9%) ITA with or without other grafts vs. the use of saphenous vein grafting alone (SVG, 21%), as well as incomplete (18%) vs. complete revascularization, and the use of off- (5.0%) vs. on-pump CABG. The median follow-up was nearly 8 years, with total follow-up of more than 100,000 patient-years, according to Dr. Raza.
Multivariable analysis was performed to assess the effect of surgical techniques on early and late mortality.
After adjustment for patient characteristics, single ITA grafting with or without other grafts vs. SVG alone was associated with a 43% decrease in early mortality and 17% decrease in late mortality. The use of bilateral ITA grafting with or without other grafts led to a 60% decrease in early mortality and a 33% decrease in late mortality, with all hazard ratios being within their confidence intervals, and hence significant, said Dr.Raza.
In addition, bilateral ITA grafting was found to be significantly more effective than single ITA grafting in decreasing late mortality in patients with multisystem disease.
Incomplete revascularization was not found to be associated with increased early mortality, but was significantly associated with a 10% increase in late mortality The use of off-pump vs. on-pump CABG had no statistically significant effect on early and late mortality, Dr. Raza added.
"Overall, bilateral ITA grafting and complete revascularization improved results of CABG in diabetics. These surgical techniques should be used in diabetics undergoing CABG," Dr. Raza stated.
In an interview, commenting on the significance of the research, Dr. Raza added: "Diabetes is an emerging epidemic affecting nearly 382 million people worldwide. Because it is a risk factor for development of coronary artery disease, the number of diabetics undergoing coronary surgery has increased to nearly 50% of all patients undergoing surgical revascularization today.
"We know from the BARI2D and FREEDOM studies that for diabetics with multivessel coronary artery disease, CABG results in better outcomes than medical therapy or percutaneous coronary intervention. However, what remains unclear is which surgical revascularization techniques improve the outcomes of CABG in patients with diabetes. Our study helps to answer this important question," he concluded.
Dr. Raza reported having no relevant disclosures.
Diabetes has historically been associated with greater mortality and more and worse postoperative complications after coronary artery bypass grafting (CABG). Researchers continue to search for improved surgical techniques and other options to improve CABG outcomes in diabetic patients.
The use of bilateral internal thoracic artery (ITA) grafting and complete revascularization was found to improve the results of CABG in patients with diabetes, according to the results of an assessment of nearly 12,000 diabetic patients who underwent surgical revascularization, according to Dr. Sajjad Raza, a research fellow in cardiac surgery, who presented the results of a study that he and his colleagues performed at the Cleveland Clinic.
Patients who were operated upon from January 1972 to January 2011 were included in the study.
"Our research was designed to identify surgical revascularization techniques that can improve early and late results in patients with diabetes undergoing CABG," said Dr. Raza at the annual meeting of the American Association for Thoracic Surgery.
Surgical revascularization techniques investigated comprised single (71%) and bilateral (7.9%) ITA with or without other grafts vs. the use of saphenous vein grafting alone (SVG, 21%), as well as incomplete (18%) vs. complete revascularization, and the use of off- (5.0%) vs. on-pump CABG. The median follow-up was nearly 8 years, with total follow-up of more than 100,000 patient-years, according to Dr. Raza.
Multivariable analysis was performed to assess the effect of surgical techniques on early and late mortality.
After adjustment for patient characteristics, single ITA grafting with or without other grafts vs. SVG alone was associated with a 43% decrease in early mortality and 17% decrease in late mortality. The use of bilateral ITA grafting with or without other grafts led to a 60% decrease in early mortality and a 33% decrease in late mortality, with all hazard ratios being within their confidence intervals, and hence significant, said Dr.Raza.
In addition, bilateral ITA grafting was found to be significantly more effective than single ITA grafting in decreasing late mortality in patients with multisystem disease.
Incomplete revascularization was not found to be associated with increased early mortality, but was significantly associated with a 10% increase in late mortality The use of off-pump vs. on-pump CABG had no statistically significant effect on early and late mortality, Dr. Raza added.
"Overall, bilateral ITA grafting and complete revascularization improved results of CABG in diabetics. These surgical techniques should be used in diabetics undergoing CABG," Dr. Raza stated.
In an interview, commenting on the significance of the research, Dr. Raza added: "Diabetes is an emerging epidemic affecting nearly 382 million people worldwide. Because it is a risk factor for development of coronary artery disease, the number of diabetics undergoing coronary surgery has increased to nearly 50% of all patients undergoing surgical revascularization today.
"We know from the BARI2D and FREEDOM studies that for diabetics with multivessel coronary artery disease, CABG results in better outcomes than medical therapy or percutaneous coronary intervention. However, what remains unclear is which surgical revascularization techniques improve the outcomes of CABG in patients with diabetes. Our study helps to answer this important question," he concluded.
Dr. Raza reported having no relevant disclosures.
FDA: Remove IVC filters 29-54 days after implantation
Inferior vena cava filters for protection against pulmonary embolism begin to show more risk than benefit between 29 and 54 days after implantation and should be removed, according to an FDA Safety Communication: "Removing Retrievable Inferior Vena Cava Filters," issued this May by the U. S. Food and Drug Administration.
This communication was an update of an August 2010 statement directed toward "physicians who implant inferior vena cava filters and clinicians responsible for the ongoing care of patients with these devices." According to the update, it was issued to include information on recently published research and postmarket surveillance studies for these devices.
The FDA developed a quantitative decision analysis using data available in the literature to assess whether there was a time period during which the risk of having an IVC filter in place outweighed the benefits.
The decision analysis (Decision Analysis of Retrievable Inferior Vena Cava Filters in Patients without Pulmonary Embolism) was published in the Journal of Vascular Surgery: Venous and Lymphatic Disorders in October 2013 (1:376-84). The article PDF is available at the FDA site.
The mathematical model indicated that if the patient’s transient risk for pulmonary embolism had passed, the risk/benefit profile begins to favor removal of the IVC filter between 29 and 54 days after implantation, according to the FDA.
The FDA is requiring collection of additional clinical data for currently marketed IVC filters in the United States to address safety questions that remain unanswered for both permanent and retrievable filters.
The FDA gave manufacturers two options for data collection. The first was participation in the PRESERVE (Predicting the Safety and Effectiveness of Inferior Vena Cava Filters) study, an independent national clinical study to examine the use of IVC filters in the prevention of pulmonary embolism. Other manufacturers are conducting postmarket surveillance (522 studies).
The data gathered from the PRESERVE study and the 522 studies will help the FDA, manufacturers, and health care professionals assess the use and safety profile of these devices and understand evolving patterns of clinical use of IVC filters, according to the communication.
Inferior vena cava filters for protection against pulmonary embolism begin to show more risk than benefit between 29 and 54 days after implantation and should be removed, according to an FDA Safety Communication: "Removing Retrievable Inferior Vena Cava Filters," issued this May by the U. S. Food and Drug Administration.
This communication was an update of an August 2010 statement directed toward "physicians who implant inferior vena cava filters and clinicians responsible for the ongoing care of patients with these devices." According to the update, it was issued to include information on recently published research and postmarket surveillance studies for these devices.
The FDA developed a quantitative decision analysis using data available in the literature to assess whether there was a time period during which the risk of having an IVC filter in place outweighed the benefits.
The decision analysis (Decision Analysis of Retrievable Inferior Vena Cava Filters in Patients without Pulmonary Embolism) was published in the Journal of Vascular Surgery: Venous and Lymphatic Disorders in October 2013 (1:376-84). The article PDF is available at the FDA site.
The mathematical model indicated that if the patient’s transient risk for pulmonary embolism had passed, the risk/benefit profile begins to favor removal of the IVC filter between 29 and 54 days after implantation, according to the FDA.
The FDA is requiring collection of additional clinical data for currently marketed IVC filters in the United States to address safety questions that remain unanswered for both permanent and retrievable filters.
The FDA gave manufacturers two options for data collection. The first was participation in the PRESERVE (Predicting the Safety and Effectiveness of Inferior Vena Cava Filters) study, an independent national clinical study to examine the use of IVC filters in the prevention of pulmonary embolism. Other manufacturers are conducting postmarket surveillance (522 studies).
The data gathered from the PRESERVE study and the 522 studies will help the FDA, manufacturers, and health care professionals assess the use and safety profile of these devices and understand evolving patterns of clinical use of IVC filters, according to the communication.
Inferior vena cava filters for protection against pulmonary embolism begin to show more risk than benefit between 29 and 54 days after implantation and should be removed, according to an FDA Safety Communication: "Removing Retrievable Inferior Vena Cava Filters," issued this May by the U. S. Food and Drug Administration.
This communication was an update of an August 2010 statement directed toward "physicians who implant inferior vena cava filters and clinicians responsible for the ongoing care of patients with these devices." According to the update, it was issued to include information on recently published research and postmarket surveillance studies for these devices.
The FDA developed a quantitative decision analysis using data available in the literature to assess whether there was a time period during which the risk of having an IVC filter in place outweighed the benefits.
The decision analysis (Decision Analysis of Retrievable Inferior Vena Cava Filters in Patients without Pulmonary Embolism) was published in the Journal of Vascular Surgery: Venous and Lymphatic Disorders in October 2013 (1:376-84). The article PDF is available at the FDA site.
The mathematical model indicated that if the patient’s transient risk for pulmonary embolism had passed, the risk/benefit profile begins to favor removal of the IVC filter between 29 and 54 days after implantation, according to the FDA.
The FDA is requiring collection of additional clinical data for currently marketed IVC filters in the United States to address safety questions that remain unanswered for both permanent and retrievable filters.
The FDA gave manufacturers two options for data collection. The first was participation in the PRESERVE (Predicting the Safety and Effectiveness of Inferior Vena Cava Filters) study, an independent national clinical study to examine the use of IVC filters in the prevention of pulmonary embolism. Other manufacturers are conducting postmarket surveillance (522 studies).
The data gathered from the PRESERVE study and the 522 studies will help the FDA, manufacturers, and health care professionals assess the use and safety profile of these devices and understand evolving patterns of clinical use of IVC filters, according to the communication.
Angiography timing not a risk for acute kidney injury
Acute kidney injury is a serious adverse effect of cardiac surgery, and contrast-induced nephropathy from coronary angiography has been suggested as a potentially important component. However, the results of a retrospective study of more than 2,500 patients showed that acute kidney injury is significantly higher only in those patients who have combined cardiac surgery within 24 hours of catheterization.
The study by Dr. Giovanni Mariscalco of the Varese (Italy) University Hospital, and his colleagues assessed all consecutive patients undergoing cardiac surgery at the hospital between Jan. 1, 2005, and Dec. 31, 2011. The operations performed were isolated coronary artery bypass grafting (CABG), valve surgery with or without concomitant CABG, and proximal aortic procedures. After exclusion of patients who did not undergo cardiopulmonary bypass, a known major cause of acute kidney injury (AKI), and those who died during the procedure, a total of 2,504 patients remained. These patients had a mean age of 68.4 years; 67.3% were men, according to the report.
The primary endpoint was the effect of timing between cardiac catheterization and surgery on the development of AKI. Postoperative AKI was defined by the consensus RIFLE criteria (risk, injury, failure, loss of function, and end-stage renal disease), using the maximal change in serum creatinine and the estimated glomerular filtration rate during the first 7 days after surgery, compared with baseline.
The overall incidence of AKI after surgery was 9.2% (230/2,504 patients). A breakdown by procedure showed that AKI occurred in 7.7% of isolated CABG patients, 12.2% of isolated valve patients, 9.5% of combined-procedure patients, and 9.5% of the proximal aorta surgery patients (Int. J. Cardiol. 2014;173:46-54).
As has been seen in previous studies, AKI was associated with patient-specific pre- and perioperative variables, including increased patient age, added comorbidities, longer cardiopulmonary bypass (CPB) times, higher rates of combined procedures, and the use of intra-aortic balloon pumps.
Unadjusted analysis of the total cohort showed AKI was significantly associated with contrast exposure within 1 day of surgery. However, in multivariable analysis, the time interval between catheterization and surgery was not an independent predictor of postoperative AKI for the total cohort. In subgroup analysis, only the combined valve and CABG group of patients showed an independent association of contrast exposure within 1 day before surgery and AKI in both the prematched (odds ratio, 2.69; P = .004) and the postmatched (OR, 3.68; P = .014) groups.
"Avoiding surgery within 1 day after contrast exposure should be recommended for patients undergoing valve surgery with concomitant CABG only. For other types of cardiac operations, delaying cardiac surgery after contrast exposure seems not to be justified," the researchers concluded.
The study was supported by the Fondazione Cesare Bartorelli. The authors reported having no disclosures.
Acute kidney injury is a serious adverse effect of cardiac surgery, and contrast-induced nephropathy from coronary angiography has been suggested as a potentially important component. However, the results of a retrospective study of more than 2,500 patients showed that acute kidney injury is significantly higher only in those patients who have combined cardiac surgery within 24 hours of catheterization.
The study by Dr. Giovanni Mariscalco of the Varese (Italy) University Hospital, and his colleagues assessed all consecutive patients undergoing cardiac surgery at the hospital between Jan. 1, 2005, and Dec. 31, 2011. The operations performed were isolated coronary artery bypass grafting (CABG), valve surgery with or without concomitant CABG, and proximal aortic procedures. After exclusion of patients who did not undergo cardiopulmonary bypass, a known major cause of acute kidney injury (AKI), and those who died during the procedure, a total of 2,504 patients remained. These patients had a mean age of 68.4 years; 67.3% were men, according to the report.
The primary endpoint was the effect of timing between cardiac catheterization and surgery on the development of AKI. Postoperative AKI was defined by the consensus RIFLE criteria (risk, injury, failure, loss of function, and end-stage renal disease), using the maximal change in serum creatinine and the estimated glomerular filtration rate during the first 7 days after surgery, compared with baseline.
The overall incidence of AKI after surgery was 9.2% (230/2,504 patients). A breakdown by procedure showed that AKI occurred in 7.7% of isolated CABG patients, 12.2% of isolated valve patients, 9.5% of combined-procedure patients, and 9.5% of the proximal aorta surgery patients (Int. J. Cardiol. 2014;173:46-54).
As has been seen in previous studies, AKI was associated with patient-specific pre- and perioperative variables, including increased patient age, added comorbidities, longer cardiopulmonary bypass (CPB) times, higher rates of combined procedures, and the use of intra-aortic balloon pumps.
Unadjusted analysis of the total cohort showed AKI was significantly associated with contrast exposure within 1 day of surgery. However, in multivariable analysis, the time interval between catheterization and surgery was not an independent predictor of postoperative AKI for the total cohort. In subgroup analysis, only the combined valve and CABG group of patients showed an independent association of contrast exposure within 1 day before surgery and AKI in both the prematched (odds ratio, 2.69; P = .004) and the postmatched (OR, 3.68; P = .014) groups.
"Avoiding surgery within 1 day after contrast exposure should be recommended for patients undergoing valve surgery with concomitant CABG only. For other types of cardiac operations, delaying cardiac surgery after contrast exposure seems not to be justified," the researchers concluded.
The study was supported by the Fondazione Cesare Bartorelli. The authors reported having no disclosures.
Acute kidney injury is a serious adverse effect of cardiac surgery, and contrast-induced nephropathy from coronary angiography has been suggested as a potentially important component. However, the results of a retrospective study of more than 2,500 patients showed that acute kidney injury is significantly higher only in those patients who have combined cardiac surgery within 24 hours of catheterization.
The study by Dr. Giovanni Mariscalco of the Varese (Italy) University Hospital, and his colleagues assessed all consecutive patients undergoing cardiac surgery at the hospital between Jan. 1, 2005, and Dec. 31, 2011. The operations performed were isolated coronary artery bypass grafting (CABG), valve surgery with or without concomitant CABG, and proximal aortic procedures. After exclusion of patients who did not undergo cardiopulmonary bypass, a known major cause of acute kidney injury (AKI), and those who died during the procedure, a total of 2,504 patients remained. These patients had a mean age of 68.4 years; 67.3% were men, according to the report.
The primary endpoint was the effect of timing between cardiac catheterization and surgery on the development of AKI. Postoperative AKI was defined by the consensus RIFLE criteria (risk, injury, failure, loss of function, and end-stage renal disease), using the maximal change in serum creatinine and the estimated glomerular filtration rate during the first 7 days after surgery, compared with baseline.
The overall incidence of AKI after surgery was 9.2% (230/2,504 patients). A breakdown by procedure showed that AKI occurred in 7.7% of isolated CABG patients, 12.2% of isolated valve patients, 9.5% of combined-procedure patients, and 9.5% of the proximal aorta surgery patients (Int. J. Cardiol. 2014;173:46-54).
As has been seen in previous studies, AKI was associated with patient-specific pre- and perioperative variables, including increased patient age, added comorbidities, longer cardiopulmonary bypass (CPB) times, higher rates of combined procedures, and the use of intra-aortic balloon pumps.
Unadjusted analysis of the total cohort showed AKI was significantly associated with contrast exposure within 1 day of surgery. However, in multivariable analysis, the time interval between catheterization and surgery was not an independent predictor of postoperative AKI for the total cohort. In subgroup analysis, only the combined valve and CABG group of patients showed an independent association of contrast exposure within 1 day before surgery and AKI in both the prematched (odds ratio, 2.69; P = .004) and the postmatched (OR, 3.68; P = .014) groups.
"Avoiding surgery within 1 day after contrast exposure should be recommended for patients undergoing valve surgery with concomitant CABG only. For other types of cardiac operations, delaying cardiac surgery after contrast exposure seems not to be justified," the researchers concluded.
The study was supported by the Fondazione Cesare Bartorelli. The authors reported having no disclosures.
Major finding: Only combined surgery plus contrast within 1 day before surgery was significantly associated with AKI in the prematched (OR, 2.69) and postmatched (OR, 3.68) groups.
Data source: A single-institute, retrospective study of 2,504 cardiac surgery patients.
Disclosures: The study was supported by the Fondazione Cesare Bartorelli. The authors reported having no financial disclosures.
Attendings in 'simultaneous' ORs
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs. However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single institution review by Dr. Kenan W. Yount.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon-to-operating room.
In his presentation, Dr. Yount discussed the results of their review study, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two surgeries. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 operation types, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically [affect] operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also operations being scheduled in separate rooms must be done so with reasonable foresight."
As long as institutions are following these practices, he concluded, "It would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs. However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single institution review by Dr. Kenan W. Yount.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon-to-operating room.
In his presentation, Dr. Yount discussed the results of their review study, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two surgeries. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 operation types, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically [affect] operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also operations being scheduled in separate rooms must be done so with reasonable foresight."
As long as institutions are following these practices, he concluded, "It would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs. However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single institution review by Dr. Kenan W. Yount.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon-to-operating room.
In his presentation, Dr. Yount discussed the results of their review study, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two surgeries. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 operation types, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically [affect] operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also operations being scheduled in separate rooms must be done so with reasonable foresight."
As long as institutions are following these practices, he concluded, "It would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
Major finding: Running two rooms was not associated with any differences in operative duration, morbidity, or mortality in multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category.
Data source: The study reviewed 1,377 cardiac and 1682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two surgeries.
Disclosures: Dr. Yount had no disclosures.