User login
M. Alexander Otto began his reporting career early in 1999 covering the pharmaceutical industry for a national pharmacists' magazine and freelancing for the Washington Post and other newspapers. He then joined BNA, now part of Bloomberg News, covering health law and the protection of people and animals in medical research. Alex next worked for the McClatchy Company. Based on his work, Alex won a year-long Knight Science Journalism Fellowship to MIT in 2008-2009. He joined the company shortly thereafter. Alex has a newspaper journalism degree from Syracuse (N.Y.) University and a master's degree in medical science -- a physician assistant degree -- from George Washington University. Alex is based in Seattle.
RCT confirms CT scan screening catches lung cancer early
CT scan screening of older people with heavy smoking histories – using lesion volume, not diameter, as a trigger for further work-up – reduced lung cancer deaths by about 30% in a randomized trial from the Netherlands and Belgium with almost 16,000 current and former smokers, investigators reported in the New England Journal of Medicine.
The Dutch-Belgian lung-cancer screening trial (Nederlands-Leuvens Longkanker Screenings Onderzoek [NELSON]) is “arguably the only adequately powered trial other than the” National Lung Screening Trial (NLST) in the United States to assess the role of CT scan screening among smokers, wrote University of London cancer epidemiologist Stephen Duffy, MSc, and University of Liverpool molecular oncology professor John Field, PhD, in an accompanying editorial.
NLST, which used lesion diameter, found an approximately 20% lower lung cancer mortality than screening with chest x-rays among 53,454 heavy smokers after a median follow-up of 6.5 years. The trial ultimately led the U.S. Preventive Services Task Force to recommend annual screening for people aged 55-80 years with a history of at least 30 pack-years.
European countries have considered similar programs but have hesitated “partly due to doubts fostered by the early publication of inconclusive results of a number of smaller trials in Europe. These doubts should be laid to rest,” Mr. Duffy and Dr. Field wrote.
“With the NELSON results, the efficacy of low-dose CT screening for lung cancer is confirmed. Our job is no longer to assess whether low-dose CT screening for lung cancer works; it does. Our job is to identify the target population in which it will be acceptable and cost effective,” they added.
The 15,789 NELSON participants (84% men, with a median age of 58 years and 38 pack-year history) were randomized about 1:1 to either low-dose CT scan screening at baseline and 1, 3, and 5.5 years, or to no screening.
At 10 years follow-up, there were 5.58 lung cancer cases and 2.5 deaths per 1,000 person-years in the screened group versus 4.91 cases and 3.3 deaths per 1,000 person-years among controls. Lung-cancer mortality was 24% lower among screened subjects overall, and 33% lower among screened women. The team estimated that screening prevented about 60 lung cancer deaths.
Using volume instead of diameter “resulted in low[er] referral rates” – 2.1% with a positive predictive value of 43.5% versus 24% with a positive predictive value of 3.8% in NLST – for additional work-up, explained investigators led by H.J. de Koning, MD, PhD, of the department of public health at Erasmus University Medical Center in Rotterdam, the Netherlands.
The upper limit of overdiagnosis risk – a major concern with any screening program – was 18.5% with NLST versus 8.9% with NELSON, they wrote.
In short: “Volume CT screening enabled a significant reduction of harms (e.g., false positive tests and unnecessary work-up procedures) without jeopardizing favorable outcomes,” the investigators wrote. Indeed, an ad hoc analysis suggested “more-favorable effects on lung-cancer mortality than in the NLST, despite lower referral rates for suspicious lesions” and the fact that NLST used annual screening.
“Recently,” Mr. Duffy and Dr. Field explained in their editorial, “the NELSON investigators evaluated both diameter and volume measurement to estimate lung-nodule size as an imaging biomarker for nodule management; this provided evidence that using mean or maximum axial diameter to assess nodule volume led to a substantial overestimation of nodule volume.” Direct measurement of volume “resulted in a substantial number of early-stage cancers identified at the time of diagnosis and avoided false positives from the overestimation incurred by management based on diameter.”
“The lung-nodule management system used in the NELSON trial has been advocated in the European position statement on lung-cancer screening. This will improve the acceptability of the intervention, because the rate of further investigation has been a major concern in lung cancer screening,” they wrote.
Baseline characteristics did not differ significantly between the screened and unscreened in NELSON, except for a slightly longer duration of smoking in the screened group.
The work was funded by the Netherlands Organization of Health Research and Development, among others. Mr. Duffy and Dr. de Koning didn’t report any disclosures. Dr. Field is an advisor for AstraZeneca, Epigenomics, and Nucleix, and has a research grant to his university from Janssen.
SOURCE: de Honing HJ et al. N Engl J Med. 2020 Jan 29. doi: 10.1056/NEJMoa1911793.
CT scan screening of older people with heavy smoking histories – using lesion volume, not diameter, as a trigger for further work-up – reduced lung cancer deaths by about 30% in a randomized trial from the Netherlands and Belgium with almost 16,000 current and former smokers, investigators reported in the New England Journal of Medicine.
The Dutch-Belgian lung-cancer screening trial (Nederlands-Leuvens Longkanker Screenings Onderzoek [NELSON]) is “arguably the only adequately powered trial other than the” National Lung Screening Trial (NLST) in the United States to assess the role of CT scan screening among smokers, wrote University of London cancer epidemiologist Stephen Duffy, MSc, and University of Liverpool molecular oncology professor John Field, PhD, in an accompanying editorial.
NLST, which used lesion diameter, found an approximately 20% lower lung cancer mortality than screening with chest x-rays among 53,454 heavy smokers after a median follow-up of 6.5 years. The trial ultimately led the U.S. Preventive Services Task Force to recommend annual screening for people aged 55-80 years with a history of at least 30 pack-years.
European countries have considered similar programs but have hesitated “partly due to doubts fostered by the early publication of inconclusive results of a number of smaller trials in Europe. These doubts should be laid to rest,” Mr. Duffy and Dr. Field wrote.
“With the NELSON results, the efficacy of low-dose CT screening for lung cancer is confirmed. Our job is no longer to assess whether low-dose CT screening for lung cancer works; it does. Our job is to identify the target population in which it will be acceptable and cost effective,” they added.
The 15,789 NELSON participants (84% men, with a median age of 58 years and 38 pack-year history) were randomized about 1:1 to either low-dose CT scan screening at baseline and 1, 3, and 5.5 years, or to no screening.
At 10 years follow-up, there were 5.58 lung cancer cases and 2.5 deaths per 1,000 person-years in the screened group versus 4.91 cases and 3.3 deaths per 1,000 person-years among controls. Lung-cancer mortality was 24% lower among screened subjects overall, and 33% lower among screened women. The team estimated that screening prevented about 60 lung cancer deaths.
Using volume instead of diameter “resulted in low[er] referral rates” – 2.1% with a positive predictive value of 43.5% versus 24% with a positive predictive value of 3.8% in NLST – for additional work-up, explained investigators led by H.J. de Koning, MD, PhD, of the department of public health at Erasmus University Medical Center in Rotterdam, the Netherlands.
The upper limit of overdiagnosis risk – a major concern with any screening program – was 18.5% with NLST versus 8.9% with NELSON, they wrote.
In short: “Volume CT screening enabled a significant reduction of harms (e.g., false positive tests and unnecessary work-up procedures) without jeopardizing favorable outcomes,” the investigators wrote. Indeed, an ad hoc analysis suggested “more-favorable effects on lung-cancer mortality than in the NLST, despite lower referral rates for suspicious lesions” and the fact that NLST used annual screening.
“Recently,” Mr. Duffy and Dr. Field explained in their editorial, “the NELSON investigators evaluated both diameter and volume measurement to estimate lung-nodule size as an imaging biomarker for nodule management; this provided evidence that using mean or maximum axial diameter to assess nodule volume led to a substantial overestimation of nodule volume.” Direct measurement of volume “resulted in a substantial number of early-stage cancers identified at the time of diagnosis and avoided false positives from the overestimation incurred by management based on diameter.”
“The lung-nodule management system used in the NELSON trial has been advocated in the European position statement on lung-cancer screening. This will improve the acceptability of the intervention, because the rate of further investigation has been a major concern in lung cancer screening,” they wrote.
Baseline characteristics did not differ significantly between the screened and unscreened in NELSON, except for a slightly longer duration of smoking in the screened group.
The work was funded by the Netherlands Organization of Health Research and Development, among others. Mr. Duffy and Dr. de Koning didn’t report any disclosures. Dr. Field is an advisor for AstraZeneca, Epigenomics, and Nucleix, and has a research grant to his university from Janssen.
SOURCE: de Honing HJ et al. N Engl J Med. 2020 Jan 29. doi: 10.1056/NEJMoa1911793.
CT scan screening of older people with heavy smoking histories – using lesion volume, not diameter, as a trigger for further work-up – reduced lung cancer deaths by about 30% in a randomized trial from the Netherlands and Belgium with almost 16,000 current and former smokers, investigators reported in the New England Journal of Medicine.
The Dutch-Belgian lung-cancer screening trial (Nederlands-Leuvens Longkanker Screenings Onderzoek [NELSON]) is “arguably the only adequately powered trial other than the” National Lung Screening Trial (NLST) in the United States to assess the role of CT scan screening among smokers, wrote University of London cancer epidemiologist Stephen Duffy, MSc, and University of Liverpool molecular oncology professor John Field, PhD, in an accompanying editorial.
NLST, which used lesion diameter, found an approximately 20% lower lung cancer mortality than screening with chest x-rays among 53,454 heavy smokers after a median follow-up of 6.5 years. The trial ultimately led the U.S. Preventive Services Task Force to recommend annual screening for people aged 55-80 years with a history of at least 30 pack-years.
European countries have considered similar programs but have hesitated “partly due to doubts fostered by the early publication of inconclusive results of a number of smaller trials in Europe. These doubts should be laid to rest,” Mr. Duffy and Dr. Field wrote.
“With the NELSON results, the efficacy of low-dose CT screening for lung cancer is confirmed. Our job is no longer to assess whether low-dose CT screening for lung cancer works; it does. Our job is to identify the target population in which it will be acceptable and cost effective,” they added.
The 15,789 NELSON participants (84% men, with a median age of 58 years and 38 pack-year history) were randomized about 1:1 to either low-dose CT scan screening at baseline and 1, 3, and 5.5 years, or to no screening.
At 10 years follow-up, there were 5.58 lung cancer cases and 2.5 deaths per 1,000 person-years in the screened group versus 4.91 cases and 3.3 deaths per 1,000 person-years among controls. Lung-cancer mortality was 24% lower among screened subjects overall, and 33% lower among screened women. The team estimated that screening prevented about 60 lung cancer deaths.
Using volume instead of diameter “resulted in low[er] referral rates” – 2.1% with a positive predictive value of 43.5% versus 24% with a positive predictive value of 3.8% in NLST – for additional work-up, explained investigators led by H.J. de Koning, MD, PhD, of the department of public health at Erasmus University Medical Center in Rotterdam, the Netherlands.
The upper limit of overdiagnosis risk – a major concern with any screening program – was 18.5% with NLST versus 8.9% with NELSON, they wrote.
In short: “Volume CT screening enabled a significant reduction of harms (e.g., false positive tests and unnecessary work-up procedures) without jeopardizing favorable outcomes,” the investigators wrote. Indeed, an ad hoc analysis suggested “more-favorable effects on lung-cancer mortality than in the NLST, despite lower referral rates for suspicious lesions” and the fact that NLST used annual screening.
“Recently,” Mr. Duffy and Dr. Field explained in their editorial, “the NELSON investigators evaluated both diameter and volume measurement to estimate lung-nodule size as an imaging biomarker for nodule management; this provided evidence that using mean or maximum axial diameter to assess nodule volume led to a substantial overestimation of nodule volume.” Direct measurement of volume “resulted in a substantial number of early-stage cancers identified at the time of diagnosis and avoided false positives from the overestimation incurred by management based on diameter.”
“The lung-nodule management system used in the NELSON trial has been advocated in the European position statement on lung-cancer screening. This will improve the acceptability of the intervention, because the rate of further investigation has been a major concern in lung cancer screening,” they wrote.
Baseline characteristics did not differ significantly between the screened and unscreened in NELSON, except for a slightly longer duration of smoking in the screened group.
The work was funded by the Netherlands Organization of Health Research and Development, among others. Mr. Duffy and Dr. de Koning didn’t report any disclosures. Dr. Field is an advisor for AstraZeneca, Epigenomics, and Nucleix, and has a research grant to his university from Janssen.
SOURCE: de Honing HJ et al. N Engl J Med. 2020 Jan 29. doi: 10.1056/NEJMoa1911793.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Serum keratin 18 promising as AAH biomarker
Outperforms MELD, ABIC
.
Standard biomarker scores – Model for End-stage Liver Disease (MELD), age, serum bilirubin, International Normalized Ratio, and serum creatinine (ABIC), as well as others – predict prognosis and severity of alcoholic liver disease, but they don’t reflect “the magnitude of cell death nor the form of cell death (apoptosis/necrosis), which may be important in distinguishing various forms of liver injury” and guiding therapy, explained investigators led by Vatsalya Vatsalya, MD, of the division of gastroenterology, hepatology, and nutrition at the University of Louisville (Ky.).
It’s important, for instance, to identify people with alcoholic cirrhosis but not active hepatitis, as they “would likely not benefit from anti-inflammatory agents such as steroids or [interleukin]-1 receptor antagonists, but would incur their side effects.” For those and other reasons, “new biomarkers are needed for diagnosing AAH, assessing the degree of hepatocyte death, and predicting mortality,” they said (Clin Gastroenterol Hepatol. 2019 Dec 4. doi: 10.1016/j.cgh.2019.11.050).
Keratin 18 – both the cleaved form (K18M30) and the uncleaved protein (K18M65) – have been suggested before as a marker for AAH, so the investigators took a closer look.
They analyzed serum from 57 people with severe AAH (MELD score above 20), 27 people with moderate AAH (MELD score 12-19), 34 with nonalcoholic steatohepatitis, 17 healthy controls, and 38 people with alcohol use disorder and either mild or no liver injury.
Overall, 51.9% of moderate AAH cases and 38.9% of severe cases had K18M65 levels between 641 and 2,000 IU/L; 25.9% of moderate and 61.1% of severe cases had K18M65 levels greater than 2,000 IU/L. All severe cases had levels above 641 IU/L. Serum levels of K18 also identified patients who died within 90 days with greater accuracy than did MELD, ABIC, and other scores, the investigators said.
The K18M65:ALT [alanine aminotransferase] ratio distinguished AAH from nonalcoholic steatohepatitis with a sensitivity of 0.971 and specificity of 0.829. Findings were similar for the K18M30:ALT ratio.
Levels of K18M65 and K18M30 increased significantly as liver disease worsened, as did the degree of necrosis as indicated by the K18M65:K18M30 ratio. Meanwhile, although k18 levels correlated with MELD scores, levels of ALT, aspartate aminotransferase (AST), and the ratio of AST:ALT did not.
“There is a stronger association between serum level of keratin 18 and amount of hepatocyte death and liver disease severity than for other biomarkers,” the team concluded.
Patients were in their mid 40s, on average, and there were more men than women.
The National Institutes of Health supported the work, and the investigators had no disclosures.
Outperforms MELD, ABIC
Outperforms MELD, ABIC
.
Standard biomarker scores – Model for End-stage Liver Disease (MELD), age, serum bilirubin, International Normalized Ratio, and serum creatinine (ABIC), as well as others – predict prognosis and severity of alcoholic liver disease, but they don’t reflect “the magnitude of cell death nor the form of cell death (apoptosis/necrosis), which may be important in distinguishing various forms of liver injury” and guiding therapy, explained investigators led by Vatsalya Vatsalya, MD, of the division of gastroenterology, hepatology, and nutrition at the University of Louisville (Ky.).
It’s important, for instance, to identify people with alcoholic cirrhosis but not active hepatitis, as they “would likely not benefit from anti-inflammatory agents such as steroids or [interleukin]-1 receptor antagonists, but would incur their side effects.” For those and other reasons, “new biomarkers are needed for diagnosing AAH, assessing the degree of hepatocyte death, and predicting mortality,” they said (Clin Gastroenterol Hepatol. 2019 Dec 4. doi: 10.1016/j.cgh.2019.11.050).
Keratin 18 – both the cleaved form (K18M30) and the uncleaved protein (K18M65) – have been suggested before as a marker for AAH, so the investigators took a closer look.
They analyzed serum from 57 people with severe AAH (MELD score above 20), 27 people with moderate AAH (MELD score 12-19), 34 with nonalcoholic steatohepatitis, 17 healthy controls, and 38 people with alcohol use disorder and either mild or no liver injury.
Overall, 51.9% of moderate AAH cases and 38.9% of severe cases had K18M65 levels between 641 and 2,000 IU/L; 25.9% of moderate and 61.1% of severe cases had K18M65 levels greater than 2,000 IU/L. All severe cases had levels above 641 IU/L. Serum levels of K18 also identified patients who died within 90 days with greater accuracy than did MELD, ABIC, and other scores, the investigators said.
The K18M65:ALT [alanine aminotransferase] ratio distinguished AAH from nonalcoholic steatohepatitis with a sensitivity of 0.971 and specificity of 0.829. Findings were similar for the K18M30:ALT ratio.
Levels of K18M65 and K18M30 increased significantly as liver disease worsened, as did the degree of necrosis as indicated by the K18M65:K18M30 ratio. Meanwhile, although k18 levels correlated with MELD scores, levels of ALT, aspartate aminotransferase (AST), and the ratio of AST:ALT did not.
“There is a stronger association between serum level of keratin 18 and amount of hepatocyte death and liver disease severity than for other biomarkers,” the team concluded.
Patients were in their mid 40s, on average, and there were more men than women.
The National Institutes of Health supported the work, and the investigators had no disclosures.
.
Standard biomarker scores – Model for End-stage Liver Disease (MELD), age, serum bilirubin, International Normalized Ratio, and serum creatinine (ABIC), as well as others – predict prognosis and severity of alcoholic liver disease, but they don’t reflect “the magnitude of cell death nor the form of cell death (apoptosis/necrosis), which may be important in distinguishing various forms of liver injury” and guiding therapy, explained investigators led by Vatsalya Vatsalya, MD, of the division of gastroenterology, hepatology, and nutrition at the University of Louisville (Ky.).
It’s important, for instance, to identify people with alcoholic cirrhosis but not active hepatitis, as they “would likely not benefit from anti-inflammatory agents such as steroids or [interleukin]-1 receptor antagonists, but would incur their side effects.” For those and other reasons, “new biomarkers are needed for diagnosing AAH, assessing the degree of hepatocyte death, and predicting mortality,” they said (Clin Gastroenterol Hepatol. 2019 Dec 4. doi: 10.1016/j.cgh.2019.11.050).
Keratin 18 – both the cleaved form (K18M30) and the uncleaved protein (K18M65) – have been suggested before as a marker for AAH, so the investigators took a closer look.
They analyzed serum from 57 people with severe AAH (MELD score above 20), 27 people with moderate AAH (MELD score 12-19), 34 with nonalcoholic steatohepatitis, 17 healthy controls, and 38 people with alcohol use disorder and either mild or no liver injury.
Overall, 51.9% of moderate AAH cases and 38.9% of severe cases had K18M65 levels between 641 and 2,000 IU/L; 25.9% of moderate and 61.1% of severe cases had K18M65 levels greater than 2,000 IU/L. All severe cases had levels above 641 IU/L. Serum levels of K18 also identified patients who died within 90 days with greater accuracy than did MELD, ABIC, and other scores, the investigators said.
The K18M65:ALT [alanine aminotransferase] ratio distinguished AAH from nonalcoholic steatohepatitis with a sensitivity of 0.971 and specificity of 0.829. Findings were similar for the K18M30:ALT ratio.
Levels of K18M65 and K18M30 increased significantly as liver disease worsened, as did the degree of necrosis as indicated by the K18M65:K18M30 ratio. Meanwhile, although k18 levels correlated with MELD scores, levels of ALT, aspartate aminotransferase (AST), and the ratio of AST:ALT did not.
“There is a stronger association between serum level of keratin 18 and amount of hepatocyte death and liver disease severity than for other biomarkers,” the team concluded.
Patients were in their mid 40s, on average, and there were more men than women.
The National Institutes of Health supported the work, and the investigators had no disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Wuhan virus: What clinicians need to know
As the Wuhan coronavirus story unfolds, , according to infectious disease experts.

“We are asking that of everyone with fever and respiratory symptoms who comes to our clinics, hospital, or emergency room. It’s a powerful screening tool,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn.
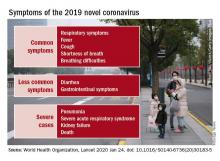
In addition to fever, common signs of infection include cough, shortness of breath, and breathing difficulties. Some patients have had diarrhea, vomiting, and other gastrointestinal symptoms. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure, and death. The incubation period appears to be up to 2 weeks, according to the World Health Organization (WHO).
If patients exhibit symptoms and either they or a close contact has returned from China recently, take standard airborne precautions and send specimens – a serum sample, oral and nasal pharyngeal swabs, and lower respiratory tract specimens if available – to the local health department, which will forward them to the Centers for Disease Control and Prevention (CDC) for testing. Turnaround time is 24-48 hours.
The 2019 Novel Coronavirus (2019-nCoV), identified as the cause of an outbreak of respiratory illness first detected in December in association with a live animal market in Wuhan, China, has been implicated in almost 2,000 cases and 56 deaths in that country. Cases have been reported in 13 countries besides China. Five cases of 2019-nCoV infection have been confirmed in the United States, all in people recently returned from Wuhan. As the virus spreads in China, however, it’s almost certain more cases will show up in the United States. Travel history is key, Dr. Schaffner and others said.
Plan and rehearse
The first step to prepare is to use the CDC’s Interim Guidance for Healthcare Professionals to make a written plan specific to your practice to respond to a potential case. The plan must include notifying the local health department, the CDC liaison for testing, and tracking down patient contacts.
“It’s not good enough to just download CDC’s guidance; use it to make your own local plan and know what to do 24/7,” said Daniel Lucey, MD, an infectious disease expert at Georgetown University Medical Center, Washington, D.C.
“Know who is on call at the health department on weekends and nights,” he said. Know where the patient is going to be isolated; figure out what to do if there’s more than one, and tests come back positive. Have masks on hand, and rehearse the response. “Make a coronavirus team, and absolutely have the nurses involved,” as well as other providers who may come into contact with a case, he added.
“You want to be able to do as well as your counterparts in Washington state and Chicago,” where the first two U.S. cases emerged. “They were prepared. They knew what to do,” Dr. Lucey said.
Those first two U.S. patients – a man in Everett, Wash., and a Chicago woman – developed symptoms after returning from Wuhan, a city of 11 million just over 400 miles inland from the port city of Shanghai. On Jan. 26 three more cases were confirmed by the CDC, two in California and one in Arizona, and each had recently traveled to Wuhan. All five patients remain hospitalized, and there’s no evidence they spread the infection further. There is also no evidence of human-to-human transmission of other cases exported from China to any other countries, according to the WHO.
WHO declined to declare a global health emergency – a Public Health Emergency of International Concern, in its parlance – on Jan. 23. The step would have triggered travel and trade restrictions in member states, including the United States. For now, at least, the group said it wasn’t warranted at this point.
Fatality rates
The focus right now is China. The outbreak has spread beyond Wuhan to other parts of the country, and there’s evidence of fourth-generation spread.
Transportation into and out of Wuhan and other cities has been curtailed, Lunar New Year festivals have been canceled, and the Shanghai Disneyland has been closed, among other measures taken by Chinese officials.
The government could be taking drastic measures in part to prevent the public criticism it took in the early 2000’s for the delayed response and lack of transparency during the global outbreak of another wildlife market coronavirus epidemic, severe acute respiratory syndrome (SARS). In a press conference Jan. 22, WHO officials commended the government’s containment efforts but did not say they recommended them.
According to WHO, serious cases in China have mostly been in people over 40 years old with significant comorbidities and have skewed towards men. Spread seems to be limited to family members, health care providers, and other close contacts, probably by respiratory droplets. If that pattern holds, WHO officials said, the outbreak is containable.
The fatality rate appears to be around 3%, a good deal lower than the 10% reported for SARS and much lower than the nearly 40% reported for Middle East respiratory syndrome (MERS), another recent coronavirus mutation from the animal trade.
The Wuhan virus fatality rate might drop as milder cases are detected and added to the denominator. “It definitely appears to be less severe than SARS and MERS,” said Amesh Adalja, MD, an infectious disease physician in Pittsburgh and emerging infectious disease researcher at Johns Hopkins University, Baltimore.
SARS: Lessons learned
In general, the world is much better equipped for coronavirus outbreaks than when SARS, in particular, emerged in 2003.
WHO officials in their press conference lauded China for it openness with the current outbreak, and for isolating and sequencing the virus immediately, which gave the world a diagnostic test in the first days of the outbreak, something that wasn’t available for SARS. China and other countries also are cooperating and working closely to contain the Wuhan virus.
“What we know today might change tomorrow, so we have to keep tuned in to new information, but we learned a lot from SARS,” Dr. Shaffner said. Overall, it’s likely “the impact on the United States of this new coronavirus is going to be trivial,” he predicted.
Dr. Lucey, however, recalled that the SARS outbreak in Toronto in 2003 started with one missed case. A woman returned asymptomatic from Hong Kong and spread the infection to her family members before she died. Her cause of death wasn’t immediately recognized, nor was the reason her family members were sick, since they hadn’t been to Hong Kong recently.
The infection ultimately spread to more than 200 people, about half of them health care workers. A few people died.
If a virus is sufficiently contagious, “it just takes one. You don’t want to be the one who misses that first patient,” Dr. Lucey said.
Currently, there are no antivirals or vaccines for coronaviruses; researchers are working on both, but for now, care is supportive.
This article was updated with new case numbers on 1/26/20.
As the Wuhan coronavirus story unfolds, , according to infectious disease experts.

“We are asking that of everyone with fever and respiratory symptoms who comes to our clinics, hospital, or emergency room. It’s a powerful screening tool,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn.
In addition to fever, common signs of infection include cough, shortness of breath, and breathing difficulties. Some patients have had diarrhea, vomiting, and other gastrointestinal symptoms. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure, and death. The incubation period appears to be up to 2 weeks, according to the World Health Organization (WHO).
If patients exhibit symptoms and either they or a close contact has returned from China recently, take standard airborne precautions and send specimens – a serum sample, oral and nasal pharyngeal swabs, and lower respiratory tract specimens if available – to the local health department, which will forward them to the Centers for Disease Control and Prevention (CDC) for testing. Turnaround time is 24-48 hours.
The 2019 Novel Coronavirus (2019-nCoV), identified as the cause of an outbreak of respiratory illness first detected in December in association with a live animal market in Wuhan, China, has been implicated in almost 2,000 cases and 56 deaths in that country. Cases have been reported in 13 countries besides China. Five cases of 2019-nCoV infection have been confirmed in the United States, all in people recently returned from Wuhan. As the virus spreads in China, however, it’s almost certain more cases will show up in the United States. Travel history is key, Dr. Schaffner and others said.
Plan and rehearse
The first step to prepare is to use the CDC’s Interim Guidance for Healthcare Professionals to make a written plan specific to your practice to respond to a potential case. The plan must include notifying the local health department, the CDC liaison for testing, and tracking down patient contacts.
“It’s not good enough to just download CDC’s guidance; use it to make your own local plan and know what to do 24/7,” said Daniel Lucey, MD, an infectious disease expert at Georgetown University Medical Center, Washington, D.C.
“Know who is on call at the health department on weekends and nights,” he said. Know where the patient is going to be isolated; figure out what to do if there’s more than one, and tests come back positive. Have masks on hand, and rehearse the response. “Make a coronavirus team, and absolutely have the nurses involved,” as well as other providers who may come into contact with a case, he added.
“You want to be able to do as well as your counterparts in Washington state and Chicago,” where the first two U.S. cases emerged. “They were prepared. They knew what to do,” Dr. Lucey said.
Those first two U.S. patients – a man in Everett, Wash., and a Chicago woman – developed symptoms after returning from Wuhan, a city of 11 million just over 400 miles inland from the port city of Shanghai. On Jan. 26 three more cases were confirmed by the CDC, two in California and one in Arizona, and each had recently traveled to Wuhan. All five patients remain hospitalized, and there’s no evidence they spread the infection further. There is also no evidence of human-to-human transmission of other cases exported from China to any other countries, according to the WHO.
WHO declined to declare a global health emergency – a Public Health Emergency of International Concern, in its parlance – on Jan. 23. The step would have triggered travel and trade restrictions in member states, including the United States. For now, at least, the group said it wasn’t warranted at this point.
Fatality rates
The focus right now is China. The outbreak has spread beyond Wuhan to other parts of the country, and there’s evidence of fourth-generation spread.
Transportation into and out of Wuhan and other cities has been curtailed, Lunar New Year festivals have been canceled, and the Shanghai Disneyland has been closed, among other measures taken by Chinese officials.
The government could be taking drastic measures in part to prevent the public criticism it took in the early 2000’s for the delayed response and lack of transparency during the global outbreak of another wildlife market coronavirus epidemic, severe acute respiratory syndrome (SARS). In a press conference Jan. 22, WHO officials commended the government’s containment efforts but did not say they recommended them.
According to WHO, serious cases in China have mostly been in people over 40 years old with significant comorbidities and have skewed towards men. Spread seems to be limited to family members, health care providers, and other close contacts, probably by respiratory droplets. If that pattern holds, WHO officials said, the outbreak is containable.
The fatality rate appears to be around 3%, a good deal lower than the 10% reported for SARS and much lower than the nearly 40% reported for Middle East respiratory syndrome (MERS), another recent coronavirus mutation from the animal trade.
The Wuhan virus fatality rate might drop as milder cases are detected and added to the denominator. “It definitely appears to be less severe than SARS and MERS,” said Amesh Adalja, MD, an infectious disease physician in Pittsburgh and emerging infectious disease researcher at Johns Hopkins University, Baltimore.
SARS: Lessons learned
In general, the world is much better equipped for coronavirus outbreaks than when SARS, in particular, emerged in 2003.
WHO officials in their press conference lauded China for it openness with the current outbreak, and for isolating and sequencing the virus immediately, which gave the world a diagnostic test in the first days of the outbreak, something that wasn’t available for SARS. China and other countries also are cooperating and working closely to contain the Wuhan virus.
“What we know today might change tomorrow, so we have to keep tuned in to new information, but we learned a lot from SARS,” Dr. Shaffner said. Overall, it’s likely “the impact on the United States of this new coronavirus is going to be trivial,” he predicted.
Dr. Lucey, however, recalled that the SARS outbreak in Toronto in 2003 started with one missed case. A woman returned asymptomatic from Hong Kong and spread the infection to her family members before she died. Her cause of death wasn’t immediately recognized, nor was the reason her family members were sick, since they hadn’t been to Hong Kong recently.
The infection ultimately spread to more than 200 people, about half of them health care workers. A few people died.
If a virus is sufficiently contagious, “it just takes one. You don’t want to be the one who misses that first patient,” Dr. Lucey said.
Currently, there are no antivirals or vaccines for coronaviruses; researchers are working on both, but for now, care is supportive.
This article was updated with new case numbers on 1/26/20.
As the Wuhan coronavirus story unfolds, , according to infectious disease experts.

“We are asking that of everyone with fever and respiratory symptoms who comes to our clinics, hospital, or emergency room. It’s a powerful screening tool,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn.
In addition to fever, common signs of infection include cough, shortness of breath, and breathing difficulties. Some patients have had diarrhea, vomiting, and other gastrointestinal symptoms. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure, and death. The incubation period appears to be up to 2 weeks, according to the World Health Organization (WHO).
If patients exhibit symptoms and either they or a close contact has returned from China recently, take standard airborne precautions and send specimens – a serum sample, oral and nasal pharyngeal swabs, and lower respiratory tract specimens if available – to the local health department, which will forward them to the Centers for Disease Control and Prevention (CDC) for testing. Turnaround time is 24-48 hours.
The 2019 Novel Coronavirus (2019-nCoV), identified as the cause of an outbreak of respiratory illness first detected in December in association with a live animal market in Wuhan, China, has been implicated in almost 2,000 cases and 56 deaths in that country. Cases have been reported in 13 countries besides China. Five cases of 2019-nCoV infection have been confirmed in the United States, all in people recently returned from Wuhan. As the virus spreads in China, however, it’s almost certain more cases will show up in the United States. Travel history is key, Dr. Schaffner and others said.
Plan and rehearse
The first step to prepare is to use the CDC’s Interim Guidance for Healthcare Professionals to make a written plan specific to your practice to respond to a potential case. The plan must include notifying the local health department, the CDC liaison for testing, and tracking down patient contacts.
“It’s not good enough to just download CDC’s guidance; use it to make your own local plan and know what to do 24/7,” said Daniel Lucey, MD, an infectious disease expert at Georgetown University Medical Center, Washington, D.C.
“Know who is on call at the health department on weekends and nights,” he said. Know where the patient is going to be isolated; figure out what to do if there’s more than one, and tests come back positive. Have masks on hand, and rehearse the response. “Make a coronavirus team, and absolutely have the nurses involved,” as well as other providers who may come into contact with a case, he added.
“You want to be able to do as well as your counterparts in Washington state and Chicago,” where the first two U.S. cases emerged. “They were prepared. They knew what to do,” Dr. Lucey said.
Those first two U.S. patients – a man in Everett, Wash., and a Chicago woman – developed symptoms after returning from Wuhan, a city of 11 million just over 400 miles inland from the port city of Shanghai. On Jan. 26 three more cases were confirmed by the CDC, two in California and one in Arizona, and each had recently traveled to Wuhan. All five patients remain hospitalized, and there’s no evidence they spread the infection further. There is also no evidence of human-to-human transmission of other cases exported from China to any other countries, according to the WHO.
WHO declined to declare a global health emergency – a Public Health Emergency of International Concern, in its parlance – on Jan. 23. The step would have triggered travel and trade restrictions in member states, including the United States. For now, at least, the group said it wasn’t warranted at this point.
Fatality rates
The focus right now is China. The outbreak has spread beyond Wuhan to other parts of the country, and there’s evidence of fourth-generation spread.
Transportation into and out of Wuhan and other cities has been curtailed, Lunar New Year festivals have been canceled, and the Shanghai Disneyland has been closed, among other measures taken by Chinese officials.
The government could be taking drastic measures in part to prevent the public criticism it took in the early 2000’s for the delayed response and lack of transparency during the global outbreak of another wildlife market coronavirus epidemic, severe acute respiratory syndrome (SARS). In a press conference Jan. 22, WHO officials commended the government’s containment efforts but did not say they recommended them.
According to WHO, serious cases in China have mostly been in people over 40 years old with significant comorbidities and have skewed towards men. Spread seems to be limited to family members, health care providers, and other close contacts, probably by respiratory droplets. If that pattern holds, WHO officials said, the outbreak is containable.
The fatality rate appears to be around 3%, a good deal lower than the 10% reported for SARS and much lower than the nearly 40% reported for Middle East respiratory syndrome (MERS), another recent coronavirus mutation from the animal trade.
The Wuhan virus fatality rate might drop as milder cases are detected and added to the denominator. “It definitely appears to be less severe than SARS and MERS,” said Amesh Adalja, MD, an infectious disease physician in Pittsburgh and emerging infectious disease researcher at Johns Hopkins University, Baltimore.
SARS: Lessons learned
In general, the world is much better equipped for coronavirus outbreaks than when SARS, in particular, emerged in 2003.
WHO officials in their press conference lauded China for it openness with the current outbreak, and for isolating and sequencing the virus immediately, which gave the world a diagnostic test in the first days of the outbreak, something that wasn’t available for SARS. China and other countries also are cooperating and working closely to contain the Wuhan virus.
“What we know today might change tomorrow, so we have to keep tuned in to new information, but we learned a lot from SARS,” Dr. Shaffner said. Overall, it’s likely “the impact on the United States of this new coronavirus is going to be trivial,” he predicted.
Dr. Lucey, however, recalled that the SARS outbreak in Toronto in 2003 started with one missed case. A woman returned asymptomatic from Hong Kong and spread the infection to her family members before she died. Her cause of death wasn’t immediately recognized, nor was the reason her family members were sick, since they hadn’t been to Hong Kong recently.
The infection ultimately spread to more than 200 people, about half of them health care workers. A few people died.
If a virus is sufficiently contagious, “it just takes one. You don’t want to be the one who misses that first patient,” Dr. Lucey said.
Currently, there are no antivirals or vaccines for coronaviruses; researchers are working on both, but for now, care is supportive.
This article was updated with new case numbers on 1/26/20.
Exogenous boosting against shingles not as robust as thought
Exposure to children with chickenpox reduces the incidence of shingles in adults 33% over 2 years, and 27% out to 20 years, according to British investigators.
Being exposed to children with illness due to varicella infection acts as an “exogenous booster” in adults who had chickenpox themselves as children, making shingles less likely, they explained in a BMJ article.
Although that’s good news, it’s been reported previously that exposure to children with chickenpox confers complete protection against shingles in adults for years afterward.
The finding matters in the United Kingdom because varicella vaccine is not part of the pediatric immunization schedule. The United States is the only country that mandates two shots as a requirement for children to attend school.
The United Kingdom, however, is reconsidering its policy. In the past, the exogenous booster idea has been one of the arguments used against mandating the vaccine for children; the concern is that preventing chickenpox in children – and subsequent reexposure to herpes zoster in adults – would kick off a costly wave of shingles in adults.
The study results “are themselves unable to justify for or against specific vaccination schedules, but they do suggest that revised mathematical models are required to estimate the impact of varicella vaccination, with the updated assumption that exogenous boosting is incomplete and only reduces the risk of zoster by about 30%,” noted the investigators, led by Harriet Forbes of the London School of Hygiene and Tropical Medicine.
The researchers identified 9,604 adults with a shingles diagnosis during 1997-2018 who at some point lived with a child who had chickenpox. Data came from the U.K. Clinical Practice Research Datalink, a general practice database.
They then looked at the incidence of shingles within 20 years of exposure to the sick child and compared it with the incidence before exposure and after 20 years, by which time the exogenous booster is thought to wear off. It was a self-controlled case series analysis, “a relatively novel epidemiological study design where individuals act as their own controls. Comparisons are made within individuals rather than between individuals as in a cohort or case control study,” Ms. Forbes and colleagues explained.
After adjustment for age, calendar time, and season, they found that in the 2 years after household exposure to a child with varicella, adults were 33% less likely to develop zoster (incidence ratio 0.67, 95% confidence interval 0.62-0.73), and 27% less likely from 10 to 20 years (IR 0.73, CI 0.62-0.87). The boosting effect appeared to be stronger in men.
“Exogenous boosting provides some protection from the risk of herpes zoster, but not complete immunity, as assumed by previous cost effectiveness estimates of varicella immunization,” the researchers said.
More than two-thirds of the adults with shingles were women, which fits with previous reports. Median age of exposure to a child with varicella was 38 years.
Ms. Forbes and colleagues noted that “the study design required patients with zoster to be living with a child with varicella, therefore the study cohort is younger than a general population with zoster. ... However, when we restricted our analysis to adults aged 50 and older at exposure to varicella, a similar pattern of association was observed, with no evidence of effect modification by age. This suggests that although the median age of our study cohort ... was low, the findings can be generalized to older people.”
There was no external funding for the work, and the lead investigator had no relevant financial disclosures. One investigator reported research grants from GSK and Merck, both makers of chickenpox and shingles vaccines.
SOURCE: Forbes H et al. BMJ. 2020 Jan 22;368:l6987.
Exposure to children with chickenpox reduces the incidence of shingles in adults 33% over 2 years, and 27% out to 20 years, according to British investigators.
Being exposed to children with illness due to varicella infection acts as an “exogenous booster” in adults who had chickenpox themselves as children, making shingles less likely, they explained in a BMJ article.
Although that’s good news, it’s been reported previously that exposure to children with chickenpox confers complete protection against shingles in adults for years afterward.
The finding matters in the United Kingdom because varicella vaccine is not part of the pediatric immunization schedule. The United States is the only country that mandates two shots as a requirement for children to attend school.
The United Kingdom, however, is reconsidering its policy. In the past, the exogenous booster idea has been one of the arguments used against mandating the vaccine for children; the concern is that preventing chickenpox in children – and subsequent reexposure to herpes zoster in adults – would kick off a costly wave of shingles in adults.
The study results “are themselves unable to justify for or against specific vaccination schedules, but they do suggest that revised mathematical models are required to estimate the impact of varicella vaccination, with the updated assumption that exogenous boosting is incomplete and only reduces the risk of zoster by about 30%,” noted the investigators, led by Harriet Forbes of the London School of Hygiene and Tropical Medicine.
The researchers identified 9,604 adults with a shingles diagnosis during 1997-2018 who at some point lived with a child who had chickenpox. Data came from the U.K. Clinical Practice Research Datalink, a general practice database.
They then looked at the incidence of shingles within 20 years of exposure to the sick child and compared it with the incidence before exposure and after 20 years, by which time the exogenous booster is thought to wear off. It was a self-controlled case series analysis, “a relatively novel epidemiological study design where individuals act as their own controls. Comparisons are made within individuals rather than between individuals as in a cohort or case control study,” Ms. Forbes and colleagues explained.
After adjustment for age, calendar time, and season, they found that in the 2 years after household exposure to a child with varicella, adults were 33% less likely to develop zoster (incidence ratio 0.67, 95% confidence interval 0.62-0.73), and 27% less likely from 10 to 20 years (IR 0.73, CI 0.62-0.87). The boosting effect appeared to be stronger in men.
“Exogenous boosting provides some protection from the risk of herpes zoster, but not complete immunity, as assumed by previous cost effectiveness estimates of varicella immunization,” the researchers said.
More than two-thirds of the adults with shingles were women, which fits with previous reports. Median age of exposure to a child with varicella was 38 years.
Ms. Forbes and colleagues noted that “the study design required patients with zoster to be living with a child with varicella, therefore the study cohort is younger than a general population with zoster. ... However, when we restricted our analysis to adults aged 50 and older at exposure to varicella, a similar pattern of association was observed, with no evidence of effect modification by age. This suggests that although the median age of our study cohort ... was low, the findings can be generalized to older people.”
There was no external funding for the work, and the lead investigator had no relevant financial disclosures. One investigator reported research grants from GSK and Merck, both makers of chickenpox and shingles vaccines.
SOURCE: Forbes H et al. BMJ. 2020 Jan 22;368:l6987.
Exposure to children with chickenpox reduces the incidence of shingles in adults 33% over 2 years, and 27% out to 20 years, according to British investigators.
Being exposed to children with illness due to varicella infection acts as an “exogenous booster” in adults who had chickenpox themselves as children, making shingles less likely, they explained in a BMJ article.
Although that’s good news, it’s been reported previously that exposure to children with chickenpox confers complete protection against shingles in adults for years afterward.
The finding matters in the United Kingdom because varicella vaccine is not part of the pediatric immunization schedule. The United States is the only country that mandates two shots as a requirement for children to attend school.
The United Kingdom, however, is reconsidering its policy. In the past, the exogenous booster idea has been one of the arguments used against mandating the vaccine for children; the concern is that preventing chickenpox in children – and subsequent reexposure to herpes zoster in adults – would kick off a costly wave of shingles in adults.
The study results “are themselves unable to justify for or against specific vaccination schedules, but they do suggest that revised mathematical models are required to estimate the impact of varicella vaccination, with the updated assumption that exogenous boosting is incomplete and only reduces the risk of zoster by about 30%,” noted the investigators, led by Harriet Forbes of the London School of Hygiene and Tropical Medicine.
The researchers identified 9,604 adults with a shingles diagnosis during 1997-2018 who at some point lived with a child who had chickenpox. Data came from the U.K. Clinical Practice Research Datalink, a general practice database.
They then looked at the incidence of shingles within 20 years of exposure to the sick child and compared it with the incidence before exposure and after 20 years, by which time the exogenous booster is thought to wear off. It was a self-controlled case series analysis, “a relatively novel epidemiological study design where individuals act as their own controls. Comparisons are made within individuals rather than between individuals as in a cohort or case control study,” Ms. Forbes and colleagues explained.
After adjustment for age, calendar time, and season, they found that in the 2 years after household exposure to a child with varicella, adults were 33% less likely to develop zoster (incidence ratio 0.67, 95% confidence interval 0.62-0.73), and 27% less likely from 10 to 20 years (IR 0.73, CI 0.62-0.87). The boosting effect appeared to be stronger in men.
“Exogenous boosting provides some protection from the risk of herpes zoster, but not complete immunity, as assumed by previous cost effectiveness estimates of varicella immunization,” the researchers said.
More than two-thirds of the adults with shingles were women, which fits with previous reports. Median age of exposure to a child with varicella was 38 years.
Ms. Forbes and colleagues noted that “the study design required patients with zoster to be living with a child with varicella, therefore the study cohort is younger than a general population with zoster. ... However, when we restricted our analysis to adults aged 50 and older at exposure to varicella, a similar pattern of association was observed, with no evidence of effect modification by age. This suggests that although the median age of our study cohort ... was low, the findings can be generalized to older people.”
There was no external funding for the work, and the lead investigator had no relevant financial disclosures. One investigator reported research grants from GSK and Merck, both makers of chickenpox and shingles vaccines.
SOURCE: Forbes H et al. BMJ. 2020 Jan 22;368:l6987.
FROM BMJ
Hippocampal sparing temporal lobectomy recommended for medically refractory epilepsy
BALTIMORE – according to a review from researchers at Thomas Jefferson University in Philadelphia.
Often, the hippocampus and other mesial structures are removed even if they appear normal. The concern is that even normal looking tissue could harbor epileptogenic elements and leaving them in tact could reduce postoperative seizure control, explained senior investigator and neurologist Michael Sperling, MD, director of the Jefferson Comprehensive Epilepsy Center.
He and his colleagues wanted to see if that was really true, so they compared outcomes in 21 patients who had mesial-sparing lobectomies with 19 patients who had the standard approach. Cases and controls were matched for age, preoperative seizure frequency, side of surgery, and other factors. None of the patients had MTS.
There was no significant difference in postoperative seizure recurrence between the two groups (P = .974). The standard procedure had a slight edge early on, but at 2.5 years, just over 60% of patients in both groups were seizure free. At 5 years, about 50% were seizure free, and almost 40% in both arms at 7.5 years.
About two-thirds of patients in each arm had pre- and postoperative verbal memory testing, with similar duration from surgery to postop evaluation. There was no change among the hippocampus-sparing patients, but a roughly one standard deviation drop in delayed recall and logical memory on the California Verbal Learning Test in the standard group.
Even so, it wasn’t enough to affect employment, which the investigators used as a surrogate for disability; postoperative employment was comparable in both groups. People mostly retained their jobs, and there was no difference in job loss. A few people in each arm actually found jobs after surgery.
The investigators concluded that “it is reasonable to recommend mesial temporal sparing procedure in patients with dominant neocortical temporal lobe epilepsy when the hippocampus appears normal in the MRI. However, as resecting the mesial temporal structures was not associated with a greater chance of becoming unemployed following the surgery, there appears to be no major contraindication to performing an [anterior temporal lobectomy] if clinically warranted.”
The results are reassuring. “My bias walking in was that” seizure recurrence would be worse after hippocampal-sparing surgery. “I was pleased to see that it was about the same. If you want to try to preserve verbal memory and the MRI is normal, you can get away with sparing the mesial temporal structures, and still get a good seizure outcome,” Dr. Sperling said at the annual meeting of the American Epilepsy Society, where the study was presented.
“But if you have to take the hippocampus for whatever reason, the functional consequence of a decline in verbal memory is not severe enough as to be disabling,” which is “one of the big concerns” with temporal lobectomy, he said.
The findings “will make us more likely to recommend mesial-sparing surgery, but at the same time” perhaps not be quite as worried about disability with the standard approach.
Temporal lobe epilepsy with normal mesial structures isn’t very common, which explains the small numbers in the series. It’s possible subtle difference in seizure control and employment outcomes would have been found with a larger series, “but obviously there were no major differences. I think the fundamental questions have been answered to my satisfaction,” Dr. Sperling said.
Overall, “it’s better to operate and try to cure people than to worry that you will make their memory worse when the consequences of having uncontrolled epilepsy is a higher death rate,” he said.
There were about equal numbers of men and women in the review; patients were in their early 30s, on average; and most had left-sided surgery. Just over half in each arm had preoperative tonic-clonic seizures. The mean duration of epilepsy was 14.9 years in the mesial-sparing group, and 8.6 years in the standard arm.
There was no funding for the review, and Dr. Sperling didn’t have any relevant disclosures.
SOURCE: Goldstein L et al. AES 2019. Abstract 1.339.
BALTIMORE – according to a review from researchers at Thomas Jefferson University in Philadelphia.
Often, the hippocampus and other mesial structures are removed even if they appear normal. The concern is that even normal looking tissue could harbor epileptogenic elements and leaving them in tact could reduce postoperative seizure control, explained senior investigator and neurologist Michael Sperling, MD, director of the Jefferson Comprehensive Epilepsy Center.
He and his colleagues wanted to see if that was really true, so they compared outcomes in 21 patients who had mesial-sparing lobectomies with 19 patients who had the standard approach. Cases and controls were matched for age, preoperative seizure frequency, side of surgery, and other factors. None of the patients had MTS.
There was no significant difference in postoperative seizure recurrence between the two groups (P = .974). The standard procedure had a slight edge early on, but at 2.5 years, just over 60% of patients in both groups were seizure free. At 5 years, about 50% were seizure free, and almost 40% in both arms at 7.5 years.
About two-thirds of patients in each arm had pre- and postoperative verbal memory testing, with similar duration from surgery to postop evaluation. There was no change among the hippocampus-sparing patients, but a roughly one standard deviation drop in delayed recall and logical memory on the California Verbal Learning Test in the standard group.
Even so, it wasn’t enough to affect employment, which the investigators used as a surrogate for disability; postoperative employment was comparable in both groups. People mostly retained their jobs, and there was no difference in job loss. A few people in each arm actually found jobs after surgery.
The investigators concluded that “it is reasonable to recommend mesial temporal sparing procedure in patients with dominant neocortical temporal lobe epilepsy when the hippocampus appears normal in the MRI. However, as resecting the mesial temporal structures was not associated with a greater chance of becoming unemployed following the surgery, there appears to be no major contraindication to performing an [anterior temporal lobectomy] if clinically warranted.”
The results are reassuring. “My bias walking in was that” seizure recurrence would be worse after hippocampal-sparing surgery. “I was pleased to see that it was about the same. If you want to try to preserve verbal memory and the MRI is normal, you can get away with sparing the mesial temporal structures, and still get a good seizure outcome,” Dr. Sperling said at the annual meeting of the American Epilepsy Society, where the study was presented.
“But if you have to take the hippocampus for whatever reason, the functional consequence of a decline in verbal memory is not severe enough as to be disabling,” which is “one of the big concerns” with temporal lobectomy, he said.
The findings “will make us more likely to recommend mesial-sparing surgery, but at the same time” perhaps not be quite as worried about disability with the standard approach.
Temporal lobe epilepsy with normal mesial structures isn’t very common, which explains the small numbers in the series. It’s possible subtle difference in seizure control and employment outcomes would have been found with a larger series, “but obviously there were no major differences. I think the fundamental questions have been answered to my satisfaction,” Dr. Sperling said.
Overall, “it’s better to operate and try to cure people than to worry that you will make their memory worse when the consequences of having uncontrolled epilepsy is a higher death rate,” he said.
There were about equal numbers of men and women in the review; patients were in their early 30s, on average; and most had left-sided surgery. Just over half in each arm had preoperative tonic-clonic seizures. The mean duration of epilepsy was 14.9 years in the mesial-sparing group, and 8.6 years in the standard arm.
There was no funding for the review, and Dr. Sperling didn’t have any relevant disclosures.
SOURCE: Goldstein L et al. AES 2019. Abstract 1.339.
BALTIMORE – according to a review from researchers at Thomas Jefferson University in Philadelphia.
Often, the hippocampus and other mesial structures are removed even if they appear normal. The concern is that even normal looking tissue could harbor epileptogenic elements and leaving them in tact could reduce postoperative seizure control, explained senior investigator and neurologist Michael Sperling, MD, director of the Jefferson Comprehensive Epilepsy Center.
He and his colleagues wanted to see if that was really true, so they compared outcomes in 21 patients who had mesial-sparing lobectomies with 19 patients who had the standard approach. Cases and controls were matched for age, preoperative seizure frequency, side of surgery, and other factors. None of the patients had MTS.
There was no significant difference in postoperative seizure recurrence between the two groups (P = .974). The standard procedure had a slight edge early on, but at 2.5 years, just over 60% of patients in both groups were seizure free. At 5 years, about 50% were seizure free, and almost 40% in both arms at 7.5 years.
About two-thirds of patients in each arm had pre- and postoperative verbal memory testing, with similar duration from surgery to postop evaluation. There was no change among the hippocampus-sparing patients, but a roughly one standard deviation drop in delayed recall and logical memory on the California Verbal Learning Test in the standard group.
Even so, it wasn’t enough to affect employment, which the investigators used as a surrogate for disability; postoperative employment was comparable in both groups. People mostly retained their jobs, and there was no difference in job loss. A few people in each arm actually found jobs after surgery.
The investigators concluded that “it is reasonable to recommend mesial temporal sparing procedure in patients with dominant neocortical temporal lobe epilepsy when the hippocampus appears normal in the MRI. However, as resecting the mesial temporal structures was not associated with a greater chance of becoming unemployed following the surgery, there appears to be no major contraindication to performing an [anterior temporal lobectomy] if clinically warranted.”
The results are reassuring. “My bias walking in was that” seizure recurrence would be worse after hippocampal-sparing surgery. “I was pleased to see that it was about the same. If you want to try to preserve verbal memory and the MRI is normal, you can get away with sparing the mesial temporal structures, and still get a good seizure outcome,” Dr. Sperling said at the annual meeting of the American Epilepsy Society, where the study was presented.
“But if you have to take the hippocampus for whatever reason, the functional consequence of a decline in verbal memory is not severe enough as to be disabling,” which is “one of the big concerns” with temporal lobectomy, he said.
The findings “will make us more likely to recommend mesial-sparing surgery, but at the same time” perhaps not be quite as worried about disability with the standard approach.
Temporal lobe epilepsy with normal mesial structures isn’t very common, which explains the small numbers in the series. It’s possible subtle difference in seizure control and employment outcomes would have been found with a larger series, “but obviously there were no major differences. I think the fundamental questions have been answered to my satisfaction,” Dr. Sperling said.
Overall, “it’s better to operate and try to cure people than to worry that you will make their memory worse when the consequences of having uncontrolled epilepsy is a higher death rate,” he said.
There were about equal numbers of men and women in the review; patients were in their early 30s, on average; and most had left-sided surgery. Just over half in each arm had preoperative tonic-clonic seizures. The mean duration of epilepsy was 14.9 years in the mesial-sparing group, and 8.6 years in the standard arm.
There was no funding for the review, and Dr. Sperling didn’t have any relevant disclosures.
SOURCE: Goldstein L et al. AES 2019. Abstract 1.339.
REPORTING FROM AES 2019
Cognitive screening of older physicians: What’s fair?
Cognitive screening of 141 clinicians 70 years or older at Yale New Haven (Conn.) Hospital identified 18 with cognitive deficits likely to impair their ability to practice medicine. Six retired and 12 agreed to limit their practice to closely proctored environments, according to a report in JAMA.
It was part of a program to screen all practitioners 70 years or older who apply for reappointment to the medical staff, and every 2 years thereafter, due to “concerns about the potentially compromised ability of older clinicians,” said the authors, Yale rheumatologist and geriatrician Leo M. Cooney Jr., MD, and Thomas Balcezak, MD, Yale New Haven’s chief medical officer.
Yale is not alone. Intermountain Healthcare, Stanford Hospitals and Clinics, Scripps Health Care, Penn Medicine, and the University of California, San Diego, are among the institutions with similar programs.
The move is being driven by the aging of the medical community. About 15% of U.S. physicians are over 65 years old, a tripling from 23,000 in 1980 to 73,000 in 2012-2016, and the number is growing, according to an editorial by Jeffrey L. Saver, MD, professor of neurology and senior associate vice president of neurology at the University of California, Los Angeles.
Given the trend, “it is not surprising that the issue of screening aging physicians for cognitive deficits has gained attention over the last decade,” Katrina Armstrong, MD, chair of the department of medicine at Massachusetts General Hospital, Boston, and Eileen E. Reynolds, MD, associate professor of medicine at Beth Israel Deaconess Medical Center, Boston, noted in a second editorial.
“Cognitive decline often accompanies aging, and the prevalence of dementia increases rapidly after age 70 years,” they said.
The data on whether older clinicians pose a risk to patients is limited and somewhat mixed. An analysis of 736,537 Medicare hospitalizations found no association between physician age and 30-day patient mortality among physicians 60 years or older with more than 201 admissions per year, but higher mortality among older physicians with lower volumes.
A meta-analysis of 62 studies showed that “older physicians have less factual knowledge, are less likely to adhere to appropriate standards of care, and may also have poorer patient outcomes.”
The new Yale data, meanwhile, suggests that “approximately 13% [18 of 141] of physicians and other clinicians older than 70 years should not be practicing independently,” Dr. Armstrong and Dr. Reynolds said in their editorial.
There is support for screening efforts. “As a profession that deals with human life, medical practitioners must obviously have the cognitive capacity to safely practice medicine. I applaud the approach taken by Yale New Haven Hospital in that cognitive abilities themselves, and not simply funds of knowledge, are assessed,” said Richard J. Caselli, MD, professor of neurology at the Mayo Clinic Arizona, Scottsdale, and a leader of the Alzheimer’s disease program there.
However, it’s not hard to imagine highly competent but older physicians taking umbrage at cognitive screening, and there’s been pushback. Stanford was considering a Yale-like approach but opted instead for peer review after opposition. Objections from the Utah Medical Association led Utah to enact a law banning age-based physician screening. In 2015, the American Medical Association issued a report calling for the development of guidelines and standards for assessing competency in aging physicians, but the AMA House of Delegates shelved it pending further study.
There are concerns about age discrimination, discounting the accumulated wisdom of long-practicing physicians, and misclassifying competent physicians, particularly those who provide quality care in rural and other underserved areas. Indeed, 8 of 14 clinicians who screened positive at Yale and underwent more extensive testing were allowed to recredential, “suggesting that the false-positive screening rate could be as high as 57%,” Dr. Armstrong and Dr. Reynolds noted.
The consensus seems to be that there probably is a need for some sort of screening, but it must be both sound and fair. Rather than a piecemeal institutional approach, perhaps there is “an important opportunity for other groups, including specialty boards and state licensing boards” to standardize the process, they said.
Among other things, assessments could focus less on test scores and more on the practice of medicine. For instance, fine motor skill/motor planning assessments for surgeons, and intermediate results could trigger a more extensive assessment of actual clinical performance, perhaps even direct observation, Dr. Saver said in his editorial.
As far as clinical performance goes, none of the 18 clinicians at Yale had previous performance problems. “Was this a failure of the system to report impaired physicians or were these physicians compensating sufficiently to avoid detection?” In either case, “cognitive testing should be a red flag that triggers other clinical assessments,” said Carl I. Cohen, MD, professor and director of the division of geriatric psychiatry at the State University of New York, Brooklyn.
The original plan at Yale was for neurologic and ophthalmologic examinations beginning at age 70, but ultimately it was decided to go with a battery of 16 tests to assess visual scanning and psychomotor efficiency, processing speed under pressure, concentration, and working memory, among other things. Testing takes about 50-90 minutes, and is graded by single neuropsychologist to ensure consistency. Results were compared with normative scores from both older and younger clinicians.
To prevent clinicians from preparing for it, Yale isn’t releasing its test battery.
Suboptimal performance triggered additional evaluations, including in-depth assessment of intellectual, memory, and executive function. Final reviews and recommendations were made by a committee that included a geriatrician, the clinician’s section or department chair, and current and past chief medical officers.
Among the 18 providers who demonstrated deficits impairing their ability to practice medicine, 5 were 70-74 years old; 4 were 75-79; and 9 were 80 years or older. Minor abnormalities were found in 34 other candidates (24.1%); they were allowed to recredential but were scheduled for rescreening at 1-year intervals, instead of every 2 years.
The mean age among the 141 screened clinicians was 74.3 years and ranged from 69 to 92 years; 86% were men. Applicants included 125 physicians (88.7%) as well as 5 advanced practice registered nurses; 4 dentists; 3 psychologists; 2 podiatrists; 1 physician associate; and 1 midwife.
The authors had no relevant disclosures.
SOURCE: Cooney L et al. JAMA. 2020 Jan 14;323(2):179-80.
Cognitive screening of 141 clinicians 70 years or older at Yale New Haven (Conn.) Hospital identified 18 with cognitive deficits likely to impair their ability to practice medicine. Six retired and 12 agreed to limit their practice to closely proctored environments, according to a report in JAMA.
It was part of a program to screen all practitioners 70 years or older who apply for reappointment to the medical staff, and every 2 years thereafter, due to “concerns about the potentially compromised ability of older clinicians,” said the authors, Yale rheumatologist and geriatrician Leo M. Cooney Jr., MD, and Thomas Balcezak, MD, Yale New Haven’s chief medical officer.
Yale is not alone. Intermountain Healthcare, Stanford Hospitals and Clinics, Scripps Health Care, Penn Medicine, and the University of California, San Diego, are among the institutions with similar programs.
The move is being driven by the aging of the medical community. About 15% of U.S. physicians are over 65 years old, a tripling from 23,000 in 1980 to 73,000 in 2012-2016, and the number is growing, according to an editorial by Jeffrey L. Saver, MD, professor of neurology and senior associate vice president of neurology at the University of California, Los Angeles.
Given the trend, “it is not surprising that the issue of screening aging physicians for cognitive deficits has gained attention over the last decade,” Katrina Armstrong, MD, chair of the department of medicine at Massachusetts General Hospital, Boston, and Eileen E. Reynolds, MD, associate professor of medicine at Beth Israel Deaconess Medical Center, Boston, noted in a second editorial.
“Cognitive decline often accompanies aging, and the prevalence of dementia increases rapidly after age 70 years,” they said.
The data on whether older clinicians pose a risk to patients is limited and somewhat mixed. An analysis of 736,537 Medicare hospitalizations found no association between physician age and 30-day patient mortality among physicians 60 years or older with more than 201 admissions per year, but higher mortality among older physicians with lower volumes.
A meta-analysis of 62 studies showed that “older physicians have less factual knowledge, are less likely to adhere to appropriate standards of care, and may also have poorer patient outcomes.”
The new Yale data, meanwhile, suggests that “approximately 13% [18 of 141] of physicians and other clinicians older than 70 years should not be practicing independently,” Dr. Armstrong and Dr. Reynolds said in their editorial.
There is support for screening efforts. “As a profession that deals with human life, medical practitioners must obviously have the cognitive capacity to safely practice medicine. I applaud the approach taken by Yale New Haven Hospital in that cognitive abilities themselves, and not simply funds of knowledge, are assessed,” said Richard J. Caselli, MD, professor of neurology at the Mayo Clinic Arizona, Scottsdale, and a leader of the Alzheimer’s disease program there.
However, it’s not hard to imagine highly competent but older physicians taking umbrage at cognitive screening, and there’s been pushback. Stanford was considering a Yale-like approach but opted instead for peer review after opposition. Objections from the Utah Medical Association led Utah to enact a law banning age-based physician screening. In 2015, the American Medical Association issued a report calling for the development of guidelines and standards for assessing competency in aging physicians, but the AMA House of Delegates shelved it pending further study.
There are concerns about age discrimination, discounting the accumulated wisdom of long-practicing physicians, and misclassifying competent physicians, particularly those who provide quality care in rural and other underserved areas. Indeed, 8 of 14 clinicians who screened positive at Yale and underwent more extensive testing were allowed to recredential, “suggesting that the false-positive screening rate could be as high as 57%,” Dr. Armstrong and Dr. Reynolds noted.
The consensus seems to be that there probably is a need for some sort of screening, but it must be both sound and fair. Rather than a piecemeal institutional approach, perhaps there is “an important opportunity for other groups, including specialty boards and state licensing boards” to standardize the process, they said.
Among other things, assessments could focus less on test scores and more on the practice of medicine. For instance, fine motor skill/motor planning assessments for surgeons, and intermediate results could trigger a more extensive assessment of actual clinical performance, perhaps even direct observation, Dr. Saver said in his editorial.
As far as clinical performance goes, none of the 18 clinicians at Yale had previous performance problems. “Was this a failure of the system to report impaired physicians or were these physicians compensating sufficiently to avoid detection?” In either case, “cognitive testing should be a red flag that triggers other clinical assessments,” said Carl I. Cohen, MD, professor and director of the division of geriatric psychiatry at the State University of New York, Brooklyn.
The original plan at Yale was for neurologic and ophthalmologic examinations beginning at age 70, but ultimately it was decided to go with a battery of 16 tests to assess visual scanning and psychomotor efficiency, processing speed under pressure, concentration, and working memory, among other things. Testing takes about 50-90 minutes, and is graded by single neuropsychologist to ensure consistency. Results were compared with normative scores from both older and younger clinicians.
To prevent clinicians from preparing for it, Yale isn’t releasing its test battery.
Suboptimal performance triggered additional evaluations, including in-depth assessment of intellectual, memory, and executive function. Final reviews and recommendations were made by a committee that included a geriatrician, the clinician’s section or department chair, and current and past chief medical officers.
Among the 18 providers who demonstrated deficits impairing their ability to practice medicine, 5 were 70-74 years old; 4 were 75-79; and 9 were 80 years or older. Minor abnormalities were found in 34 other candidates (24.1%); they were allowed to recredential but were scheduled for rescreening at 1-year intervals, instead of every 2 years.
The mean age among the 141 screened clinicians was 74.3 years and ranged from 69 to 92 years; 86% were men. Applicants included 125 physicians (88.7%) as well as 5 advanced practice registered nurses; 4 dentists; 3 psychologists; 2 podiatrists; 1 physician associate; and 1 midwife.
The authors had no relevant disclosures.
SOURCE: Cooney L et al. JAMA. 2020 Jan 14;323(2):179-80.
Cognitive screening of 141 clinicians 70 years or older at Yale New Haven (Conn.) Hospital identified 18 with cognitive deficits likely to impair their ability to practice medicine. Six retired and 12 agreed to limit their practice to closely proctored environments, according to a report in JAMA.
It was part of a program to screen all practitioners 70 years or older who apply for reappointment to the medical staff, and every 2 years thereafter, due to “concerns about the potentially compromised ability of older clinicians,” said the authors, Yale rheumatologist and geriatrician Leo M. Cooney Jr., MD, and Thomas Balcezak, MD, Yale New Haven’s chief medical officer.
Yale is not alone. Intermountain Healthcare, Stanford Hospitals and Clinics, Scripps Health Care, Penn Medicine, and the University of California, San Diego, are among the institutions with similar programs.
The move is being driven by the aging of the medical community. About 15% of U.S. physicians are over 65 years old, a tripling from 23,000 in 1980 to 73,000 in 2012-2016, and the number is growing, according to an editorial by Jeffrey L. Saver, MD, professor of neurology and senior associate vice president of neurology at the University of California, Los Angeles.
Given the trend, “it is not surprising that the issue of screening aging physicians for cognitive deficits has gained attention over the last decade,” Katrina Armstrong, MD, chair of the department of medicine at Massachusetts General Hospital, Boston, and Eileen E. Reynolds, MD, associate professor of medicine at Beth Israel Deaconess Medical Center, Boston, noted in a second editorial.
“Cognitive decline often accompanies aging, and the prevalence of dementia increases rapidly after age 70 years,” they said.
The data on whether older clinicians pose a risk to patients is limited and somewhat mixed. An analysis of 736,537 Medicare hospitalizations found no association between physician age and 30-day patient mortality among physicians 60 years or older with more than 201 admissions per year, but higher mortality among older physicians with lower volumes.
A meta-analysis of 62 studies showed that “older physicians have less factual knowledge, are less likely to adhere to appropriate standards of care, and may also have poorer patient outcomes.”
The new Yale data, meanwhile, suggests that “approximately 13% [18 of 141] of physicians and other clinicians older than 70 years should not be practicing independently,” Dr. Armstrong and Dr. Reynolds said in their editorial.
There is support for screening efforts. “As a profession that deals with human life, medical practitioners must obviously have the cognitive capacity to safely practice medicine. I applaud the approach taken by Yale New Haven Hospital in that cognitive abilities themselves, and not simply funds of knowledge, are assessed,” said Richard J. Caselli, MD, professor of neurology at the Mayo Clinic Arizona, Scottsdale, and a leader of the Alzheimer’s disease program there.
However, it’s not hard to imagine highly competent but older physicians taking umbrage at cognitive screening, and there’s been pushback. Stanford was considering a Yale-like approach but opted instead for peer review after opposition. Objections from the Utah Medical Association led Utah to enact a law banning age-based physician screening. In 2015, the American Medical Association issued a report calling for the development of guidelines and standards for assessing competency in aging physicians, but the AMA House of Delegates shelved it pending further study.
There are concerns about age discrimination, discounting the accumulated wisdom of long-practicing physicians, and misclassifying competent physicians, particularly those who provide quality care in rural and other underserved areas. Indeed, 8 of 14 clinicians who screened positive at Yale and underwent more extensive testing were allowed to recredential, “suggesting that the false-positive screening rate could be as high as 57%,” Dr. Armstrong and Dr. Reynolds noted.
The consensus seems to be that there probably is a need for some sort of screening, but it must be both sound and fair. Rather than a piecemeal institutional approach, perhaps there is “an important opportunity for other groups, including specialty boards and state licensing boards” to standardize the process, they said.
Among other things, assessments could focus less on test scores and more on the practice of medicine. For instance, fine motor skill/motor planning assessments for surgeons, and intermediate results could trigger a more extensive assessment of actual clinical performance, perhaps even direct observation, Dr. Saver said in his editorial.
As far as clinical performance goes, none of the 18 clinicians at Yale had previous performance problems. “Was this a failure of the system to report impaired physicians or were these physicians compensating sufficiently to avoid detection?” In either case, “cognitive testing should be a red flag that triggers other clinical assessments,” said Carl I. Cohen, MD, professor and director of the division of geriatric psychiatry at the State University of New York, Brooklyn.
The original plan at Yale was for neurologic and ophthalmologic examinations beginning at age 70, but ultimately it was decided to go with a battery of 16 tests to assess visual scanning and psychomotor efficiency, processing speed under pressure, concentration, and working memory, among other things. Testing takes about 50-90 minutes, and is graded by single neuropsychologist to ensure consistency. Results were compared with normative scores from both older and younger clinicians.
To prevent clinicians from preparing for it, Yale isn’t releasing its test battery.
Suboptimal performance triggered additional evaluations, including in-depth assessment of intellectual, memory, and executive function. Final reviews and recommendations were made by a committee that included a geriatrician, the clinician’s section or department chair, and current and past chief medical officers.
Among the 18 providers who demonstrated deficits impairing their ability to practice medicine, 5 were 70-74 years old; 4 were 75-79; and 9 were 80 years or older. Minor abnormalities were found in 34 other candidates (24.1%); they were allowed to recredential but were scheduled for rescreening at 1-year intervals, instead of every 2 years.
The mean age among the 141 screened clinicians was 74.3 years and ranged from 69 to 92 years; 86% were men. Applicants included 125 physicians (88.7%) as well as 5 advanced practice registered nurses; 4 dentists; 3 psychologists; 2 podiatrists; 1 physician associate; and 1 midwife.
The authors had no relevant disclosures.
SOURCE: Cooney L et al. JAMA. 2020 Jan 14;323(2):179-80.
FROM JAMA
Draft ACR Takayasu’s guidelines: Surgery is the last resort
ATLANTA – One of the goals in soon-to-be-published Takayasu’s arteritis guidelines from the American College of Rheumatology is to wean patients off high-dose steroids once they are in remission.
This recommendation is in opposition to another option – namely, switching these patients to low-dose glucocorticoids. The idea is to prevent long-term side effects, particularly in children. The guidelines also recommend against escalating immunotherapy for asymptomatic increases in inflammatory markers and generally recommend against surgery – stenting in most cases – unless there is threat to life, limb, or organ and also if limb pain is so severe it cramps quality of life and dose escalation doesn’t get the job done. If surgery is planned, patients should be on perioperative steroids if there’s active disease.
It’s draft guidance for now, but it’s probably what the final document will say when it’s published in 2020, according to a presentation at the annual meeting of the American College of Rheumatology by one of the authors, Anisha Dua, MD, an associate professor of rheumatology at Northwestern University, Chicago. She gave a sneak preview at the meeting.
In general, severe, active Takayasu’s calls for high-dose oral steroids in conjunction with a nonsteroid immunosuppressive, such as methotrexate, azathioprine, leflunomide, or mycophenolate mofetil. There’s evidence that dual therapy gives a more durable remission and also reduces the need for steroids.
When that approach doesn’t do the trick, the next step is a tumor necrosis factor (TNF) inhibitor. There’s evidence for infliximab, adalimumab, certolizumab, and etanercept. Dr. Dua noted, “We still can consider” tocilizumab, but it failed to meet its primary endpoint in a randomized trial, and evidence for other biologics is sparse or nonexistent. “TNF inhibitors are the first line” for refractory disease, Dr. Dua said.
The steroid taper comes after 6-12 months of remission. Given their toxicity, “our goal for steroids is zero,” especially in pediatric populations. Even in remission, patients should have a clinical assessment, including inflammatory markers, every 3-12 months.
A rise in C-reactive protein or erythrocyte sedimentation rate, with no new symptoms, might be a reason for more frequent monitoring, but it’s not a reason to escalate immunosuppression. That should be kept in reserve for new vascular lesions, rapid progression on an old one, or worsening of organ or limb ischemia.
“We recommend [escalation] over surgical intervention” because patients often develop collateral circulation that solves the problem; it also gives the disease time to quiet down should the patient eventually go into surgery. Immediate surgery is reserved for organ or life-threatening disease, Dr. Dua said.
“Takayasu’s is different from other vasculitides in the sense that patients often present with certain nonspecific constitutional symptoms,” and there’s not a lot of pathology or histology to work with, “so we do tend to rely on imaging a lot,” Dr. Dua said.
Angiography has fallen out of favor because it’s invasive and exposes patients to radiation, among other problems. The field has moved to noninvasive imaging such as color Doppler ultrasound, CT angiography, magnetic resonance angiography, and PET CT.
“We do recommend regularly scheduled, noninvasive imaging every 6-12 months, in addition to the routine clinical assessment,” except in children with inactive disease; the risk of sedation outweighs the imaging benefit, Dr. Dua said.
In patients with single-vessel cranial or cervical stenosis, without symptoms, “we recommend medical over surgical management because of the risk of surgery. Surgery can be considered for multivessel involvement,” she said.
She and her colleagues also recommend medical management for renal artery stenosis, including antihypertensives and immunotherapy escalation for active disease. Surgery is considered for refractory hypertension or worsening kidney function
Dr. Dua is a primary investigator and adviser for Chemocentryx and an adviser for Novartis and AbbVie.
ATLANTA – One of the goals in soon-to-be-published Takayasu’s arteritis guidelines from the American College of Rheumatology is to wean patients off high-dose steroids once they are in remission.
This recommendation is in opposition to another option – namely, switching these patients to low-dose glucocorticoids. The idea is to prevent long-term side effects, particularly in children. The guidelines also recommend against escalating immunotherapy for asymptomatic increases in inflammatory markers and generally recommend against surgery – stenting in most cases – unless there is threat to life, limb, or organ and also if limb pain is so severe it cramps quality of life and dose escalation doesn’t get the job done. If surgery is planned, patients should be on perioperative steroids if there’s active disease.
It’s draft guidance for now, but it’s probably what the final document will say when it’s published in 2020, according to a presentation at the annual meeting of the American College of Rheumatology by one of the authors, Anisha Dua, MD, an associate professor of rheumatology at Northwestern University, Chicago. She gave a sneak preview at the meeting.
In general, severe, active Takayasu’s calls for high-dose oral steroids in conjunction with a nonsteroid immunosuppressive, such as methotrexate, azathioprine, leflunomide, or mycophenolate mofetil. There’s evidence that dual therapy gives a more durable remission and also reduces the need for steroids.
When that approach doesn’t do the trick, the next step is a tumor necrosis factor (TNF) inhibitor. There’s evidence for infliximab, adalimumab, certolizumab, and etanercept. Dr. Dua noted, “We still can consider” tocilizumab, but it failed to meet its primary endpoint in a randomized trial, and evidence for other biologics is sparse or nonexistent. “TNF inhibitors are the first line” for refractory disease, Dr. Dua said.
The steroid taper comes after 6-12 months of remission. Given their toxicity, “our goal for steroids is zero,” especially in pediatric populations. Even in remission, patients should have a clinical assessment, including inflammatory markers, every 3-12 months.
A rise in C-reactive protein or erythrocyte sedimentation rate, with no new symptoms, might be a reason for more frequent monitoring, but it’s not a reason to escalate immunosuppression. That should be kept in reserve for new vascular lesions, rapid progression on an old one, or worsening of organ or limb ischemia.
“We recommend [escalation] over surgical intervention” because patients often develop collateral circulation that solves the problem; it also gives the disease time to quiet down should the patient eventually go into surgery. Immediate surgery is reserved for organ or life-threatening disease, Dr. Dua said.
“Takayasu’s is different from other vasculitides in the sense that patients often present with certain nonspecific constitutional symptoms,” and there’s not a lot of pathology or histology to work with, “so we do tend to rely on imaging a lot,” Dr. Dua said.
Angiography has fallen out of favor because it’s invasive and exposes patients to radiation, among other problems. The field has moved to noninvasive imaging such as color Doppler ultrasound, CT angiography, magnetic resonance angiography, and PET CT.
“We do recommend regularly scheduled, noninvasive imaging every 6-12 months, in addition to the routine clinical assessment,” except in children with inactive disease; the risk of sedation outweighs the imaging benefit, Dr. Dua said.
In patients with single-vessel cranial or cervical stenosis, without symptoms, “we recommend medical over surgical management because of the risk of surgery. Surgery can be considered for multivessel involvement,” she said.
She and her colleagues also recommend medical management for renal artery stenosis, including antihypertensives and immunotherapy escalation for active disease. Surgery is considered for refractory hypertension or worsening kidney function
Dr. Dua is a primary investigator and adviser for Chemocentryx and an adviser for Novartis and AbbVie.
ATLANTA – One of the goals in soon-to-be-published Takayasu’s arteritis guidelines from the American College of Rheumatology is to wean patients off high-dose steroids once they are in remission.
This recommendation is in opposition to another option – namely, switching these patients to low-dose glucocorticoids. The idea is to prevent long-term side effects, particularly in children. The guidelines also recommend against escalating immunotherapy for asymptomatic increases in inflammatory markers and generally recommend against surgery – stenting in most cases – unless there is threat to life, limb, or organ and also if limb pain is so severe it cramps quality of life and dose escalation doesn’t get the job done. If surgery is planned, patients should be on perioperative steroids if there’s active disease.
It’s draft guidance for now, but it’s probably what the final document will say when it’s published in 2020, according to a presentation at the annual meeting of the American College of Rheumatology by one of the authors, Anisha Dua, MD, an associate professor of rheumatology at Northwestern University, Chicago. She gave a sneak preview at the meeting.
In general, severe, active Takayasu’s calls for high-dose oral steroids in conjunction with a nonsteroid immunosuppressive, such as methotrexate, azathioprine, leflunomide, or mycophenolate mofetil. There’s evidence that dual therapy gives a more durable remission and also reduces the need for steroids.
When that approach doesn’t do the trick, the next step is a tumor necrosis factor (TNF) inhibitor. There’s evidence for infliximab, adalimumab, certolizumab, and etanercept. Dr. Dua noted, “We still can consider” tocilizumab, but it failed to meet its primary endpoint in a randomized trial, and evidence for other biologics is sparse or nonexistent. “TNF inhibitors are the first line” for refractory disease, Dr. Dua said.
The steroid taper comes after 6-12 months of remission. Given their toxicity, “our goal for steroids is zero,” especially in pediatric populations. Even in remission, patients should have a clinical assessment, including inflammatory markers, every 3-12 months.
A rise in C-reactive protein or erythrocyte sedimentation rate, with no new symptoms, might be a reason for more frequent monitoring, but it’s not a reason to escalate immunosuppression. That should be kept in reserve for new vascular lesions, rapid progression on an old one, or worsening of organ or limb ischemia.
“We recommend [escalation] over surgical intervention” because patients often develop collateral circulation that solves the problem; it also gives the disease time to quiet down should the patient eventually go into surgery. Immediate surgery is reserved for organ or life-threatening disease, Dr. Dua said.
“Takayasu’s is different from other vasculitides in the sense that patients often present with certain nonspecific constitutional symptoms,” and there’s not a lot of pathology or histology to work with, “so we do tend to rely on imaging a lot,” Dr. Dua said.
Angiography has fallen out of favor because it’s invasive and exposes patients to radiation, among other problems. The field has moved to noninvasive imaging such as color Doppler ultrasound, CT angiography, magnetic resonance angiography, and PET CT.
“We do recommend regularly scheduled, noninvasive imaging every 6-12 months, in addition to the routine clinical assessment,” except in children with inactive disease; the risk of sedation outweighs the imaging benefit, Dr. Dua said.
In patients with single-vessel cranial or cervical stenosis, without symptoms, “we recommend medical over surgical management because of the risk of surgery. Surgery can be considered for multivessel involvement,” she said.
She and her colleagues also recommend medical management for renal artery stenosis, including antihypertensives and immunotherapy escalation for active disease. Surgery is considered for refractory hypertension or worsening kidney function
Dr. Dua is a primary investigator and adviser for Chemocentryx and an adviser for Novartis and AbbVie.
REPORTING FROM ACR 2019
Prednisolone scores for hand OA
ATLANTA – Dutch investigators at the annual meeting of the American College of Rheumatology made a good case for 6 weeks of low-dose prednisolone to help people with hand osteoarthritis get over a particularly bad spell.
A total of 42 patients randomized to prednisolone 10 mg/day fell a mean of 21.5 mm at 6 weeks from a baseline visual analog hand pain score of 54 mm (out of a possible 100 mm), versus a drop of 5.2 mm from a baseline score of 53 mm among 46 randomized to placebo; the mean group difference was 16.5 mm. Patients taking prednisolone did better on function, quality of life, and physician global assessments, too.
“This trial provides evidence that local inflammation is a suitable target for drug treatment in hand OA. We think this study provides clinicians with a short-term treatment option for patients who have a flare of their disease,” said lead investigator Féline Kroon, MD, a rheumatologist at Leiden (the Netherlands) University Medical Center.
“The large beneficial effect size exceeded that of all available therapeutic options for hand osteoarthritis,” including NSAIDs, she and her team noted in the study write-up, which was published to coincide with the meeting (Lancet. 2019 Nov 30;394[10213]:1993-2001).
Many physicians already use short-course prednisolone for hand OA, but there was no clinical evidence that it helped until now. The study also adds weight to the idea that OA has an inflammatory component – an idea that has been building for a while, Dr. Kroon said.
Leiden investigators and others have previously shown that synovial inflammation is often present in hand OA and a main determinant of pain and radiographic progression.
The 92 patients in the Low-Dose Prednisolone in Patients with Painful Hand Osteoarthritis (HOPE) trial had to have at least four interphalangeal joints (IPJs) with osteoarthritic nodes, at least one IPJ with soft swelling or erythema, and at least one with a positive power Doppler signal or grade 2 or higher synovitis on ultrasound. They also had to have flared at least 20 mm on the pain scale with NSAID washout.
There were more responders in the prednisolone group at 6 weeks (72% versus 33%), and significantly greater improvement in synovial thickening. There was no difference in power Doppler score or synovitis score per joint on MRI, but bone marrow lesions appeared less severe with prednisolone.
All the between-group differences disappeared when prednisolone was tapered after 6 weeks.
Four patients discontinued the study because of an adverse event: a myocardial infarction in the prednisolone group, and, in the control arm, a bowel surgery, an infected leg hematoma, and a case of Lyme arthritis of the knee. Adverse events were otherwise mild and similar in both arms.
The mean age in the study was 64 years, and 79% of the subjects were women. Exclusion criteria included chronic inflammatory rheumatic diseases, psoriasis, use of immune-modulating drugs within 90 days of baseline, and predominantly thumb base pain instead of finger pain.
The approach “is for short course. Long-term steroids can have important side effects, like osteoporosis. We do not think this study should be used to encourage prolonged prescribing of glucocorticoids in patients with hand OA,” Dr. Kroon said.
Two previous trials of glucocorticoids for hand OA were inconclusive. A dose of prednisone 5 mg/day for 4 weeks did not separate from placebo in one, and the second showed pain improvements with a combination of prednisolone and dipyridamole versus placebo, but with more adverse events, particularly dipyridamole headaches.
The work was funded by the Dutch Arthritis Society. Dr. Kroon did not have any disclosures.
SOURCE: Kroon F et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 1760.
ATLANTA – Dutch investigators at the annual meeting of the American College of Rheumatology made a good case for 6 weeks of low-dose prednisolone to help people with hand osteoarthritis get over a particularly bad spell.
A total of 42 patients randomized to prednisolone 10 mg/day fell a mean of 21.5 mm at 6 weeks from a baseline visual analog hand pain score of 54 mm (out of a possible 100 mm), versus a drop of 5.2 mm from a baseline score of 53 mm among 46 randomized to placebo; the mean group difference was 16.5 mm. Patients taking prednisolone did better on function, quality of life, and physician global assessments, too.
“This trial provides evidence that local inflammation is a suitable target for drug treatment in hand OA. We think this study provides clinicians with a short-term treatment option for patients who have a flare of their disease,” said lead investigator Féline Kroon, MD, a rheumatologist at Leiden (the Netherlands) University Medical Center.
“The large beneficial effect size exceeded that of all available therapeutic options for hand osteoarthritis,” including NSAIDs, she and her team noted in the study write-up, which was published to coincide with the meeting (Lancet. 2019 Nov 30;394[10213]:1993-2001).
Many physicians already use short-course prednisolone for hand OA, but there was no clinical evidence that it helped until now. The study also adds weight to the idea that OA has an inflammatory component – an idea that has been building for a while, Dr. Kroon said.
Leiden investigators and others have previously shown that synovial inflammation is often present in hand OA and a main determinant of pain and radiographic progression.
The 92 patients in the Low-Dose Prednisolone in Patients with Painful Hand Osteoarthritis (HOPE) trial had to have at least four interphalangeal joints (IPJs) with osteoarthritic nodes, at least one IPJ with soft swelling or erythema, and at least one with a positive power Doppler signal or grade 2 or higher synovitis on ultrasound. They also had to have flared at least 20 mm on the pain scale with NSAID washout.
There were more responders in the prednisolone group at 6 weeks (72% versus 33%), and significantly greater improvement in synovial thickening. There was no difference in power Doppler score or synovitis score per joint on MRI, but bone marrow lesions appeared less severe with prednisolone.
All the between-group differences disappeared when prednisolone was tapered after 6 weeks.
Four patients discontinued the study because of an adverse event: a myocardial infarction in the prednisolone group, and, in the control arm, a bowel surgery, an infected leg hematoma, and a case of Lyme arthritis of the knee. Adverse events were otherwise mild and similar in both arms.
The mean age in the study was 64 years, and 79% of the subjects were women. Exclusion criteria included chronic inflammatory rheumatic diseases, psoriasis, use of immune-modulating drugs within 90 days of baseline, and predominantly thumb base pain instead of finger pain.
The approach “is for short course. Long-term steroids can have important side effects, like osteoporosis. We do not think this study should be used to encourage prolonged prescribing of glucocorticoids in patients with hand OA,” Dr. Kroon said.
Two previous trials of glucocorticoids for hand OA were inconclusive. A dose of prednisone 5 mg/day for 4 weeks did not separate from placebo in one, and the second showed pain improvements with a combination of prednisolone and dipyridamole versus placebo, but with more adverse events, particularly dipyridamole headaches.
The work was funded by the Dutch Arthritis Society. Dr. Kroon did not have any disclosures.
SOURCE: Kroon F et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 1760.
ATLANTA – Dutch investigators at the annual meeting of the American College of Rheumatology made a good case for 6 weeks of low-dose prednisolone to help people with hand osteoarthritis get over a particularly bad spell.
A total of 42 patients randomized to prednisolone 10 mg/day fell a mean of 21.5 mm at 6 weeks from a baseline visual analog hand pain score of 54 mm (out of a possible 100 mm), versus a drop of 5.2 mm from a baseline score of 53 mm among 46 randomized to placebo; the mean group difference was 16.5 mm. Patients taking prednisolone did better on function, quality of life, and physician global assessments, too.
“This trial provides evidence that local inflammation is a suitable target for drug treatment in hand OA. We think this study provides clinicians with a short-term treatment option for patients who have a flare of their disease,” said lead investigator Féline Kroon, MD, a rheumatologist at Leiden (the Netherlands) University Medical Center.
“The large beneficial effect size exceeded that of all available therapeutic options for hand osteoarthritis,” including NSAIDs, she and her team noted in the study write-up, which was published to coincide with the meeting (Lancet. 2019 Nov 30;394[10213]:1993-2001).
Many physicians already use short-course prednisolone for hand OA, but there was no clinical evidence that it helped until now. The study also adds weight to the idea that OA has an inflammatory component – an idea that has been building for a while, Dr. Kroon said.
Leiden investigators and others have previously shown that synovial inflammation is often present in hand OA and a main determinant of pain and radiographic progression.
The 92 patients in the Low-Dose Prednisolone in Patients with Painful Hand Osteoarthritis (HOPE) trial had to have at least four interphalangeal joints (IPJs) with osteoarthritic nodes, at least one IPJ with soft swelling or erythema, and at least one with a positive power Doppler signal or grade 2 or higher synovitis on ultrasound. They also had to have flared at least 20 mm on the pain scale with NSAID washout.
There were more responders in the prednisolone group at 6 weeks (72% versus 33%), and significantly greater improvement in synovial thickening. There was no difference in power Doppler score or synovitis score per joint on MRI, but bone marrow lesions appeared less severe with prednisolone.
All the between-group differences disappeared when prednisolone was tapered after 6 weeks.
Four patients discontinued the study because of an adverse event: a myocardial infarction in the prednisolone group, and, in the control arm, a bowel surgery, an infected leg hematoma, and a case of Lyme arthritis of the knee. Adverse events were otherwise mild and similar in both arms.
The mean age in the study was 64 years, and 79% of the subjects were women. Exclusion criteria included chronic inflammatory rheumatic diseases, psoriasis, use of immune-modulating drugs within 90 days of baseline, and predominantly thumb base pain instead of finger pain.
The approach “is for short course. Long-term steroids can have important side effects, like osteoporosis. We do not think this study should be used to encourage prolonged prescribing of glucocorticoids in patients with hand OA,” Dr. Kroon said.
Two previous trials of glucocorticoids for hand OA were inconclusive. A dose of prednisone 5 mg/day for 4 weeks did not separate from placebo in one, and the second showed pain improvements with a combination of prednisolone and dipyridamole versus placebo, but with more adverse events, particularly dipyridamole headaches.
The work was funded by the Dutch Arthritis Society. Dr. Kroon did not have any disclosures.
SOURCE: Kroon F et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 1760.
REPORTING FROM ACR 2019
Methotrexate gives durable remission from idiopathic granulomatous mastitis
ATLANTA – Methotrexate, in combination with prednisone, might be emerging as the go-to option for idiopathic granulomatous mastitis, according to investigators from Oregon Health & Science University, Portland.
Idiopathic granulomatous mastitis (IGM) is an inflammatory disease in which granulomas form in breast tissue. It strikes mostly young to middle-aged women with painful, firm breast masses, sometimes with redness and drainage. Diagnosis is by biopsy with rule-out of known causes.
IGM does not respond to antibiotics. Prednisone and surgery have been the traditional approaches, but masses can recur after surgery, and a year or more of prednisone, with the weight gain and side effects, is problematic. As a result, cases are increasingly being referred to rheumatologists for other options, said lead investigator Sarah Ringsted, MD, a rheumatology fellow at the university.
A study she presented at the annual meeting of the American College of Rheumatology and previous work from others builds a case for methotrexate, which often seems to put the disease in remission and allows for shorter glucocorticoid courses. These days, “I offer this to patients as a great option. It’s really nice to have, instead of having women go on months and months of high-dose steroids, and I think we can save patients from unnecessary” surgery, Dr. Ringsted said.
Her usual regimen these days is methotrexate 15-20 mg/week for 12-18 months, with high-dose prednisone (greater than 20 mg/day) for the first 3 months, followed by a taper.
Dr. Ringsted and associates compared 23 women treated at the university during 2007-2018. Just 5 of the 12 women (42%) treated with high-dose prednisone alone went into remission and did not relapse over a mean follow-up of 27 months. Two out of three women who had both high-dose glucocorticoids and surgery achieved remission without relapse, as did all three women who received methotrexate and high-dose glucocorticoids (one also had surgery). Five other patients were treated with other options; just two had a durable remission.
The numbers are small, but they add to two previous reports. Among 19 women who had failed other treatments, 94% improved and 75% went into remission with 15 months of methotrexate in a review from Stanford (Calif.) University. An Iranian study of 17 patients treated with methotrexate, and also glucocorticoids in some, had a relapse rate of only 17.8%.
There were several cases of both inflammatory arthritis and erythema nodosum in the Oregon series, a higher incidence than what has been reported before for IGM. “It’s interesting because it makes me think of sarcoidosis. There have been cases of sarcoidosis causing mastitis, but mostly in patients with other features” of the disease. “It makes me wonder if any of these women will develop sarcoidosis later on; I think that’s an interesting question,” Dr. Ringsted said.
Women in the study were an average age of 32 years, and over half were Hispanic, which is associated with a higher risk for IGM. Almost all the women had been pregnant before and had breast fed in the previous 5 years. Cancer, tuberculosis, and fungal infections were among the things ruled out before mastitis was deemed idiopathic.
Women with IGM tend to be of childbearing age, and must be cautioned against the teratogenic effects of methotrexate, Dr. Ringsted noted.
There was no external funding, and the investigators didn’t report any disclosures.
SOURCE: Ringsted S et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 386.
ATLANTA – Methotrexate, in combination with prednisone, might be emerging as the go-to option for idiopathic granulomatous mastitis, according to investigators from Oregon Health & Science University, Portland.
Idiopathic granulomatous mastitis (IGM) is an inflammatory disease in which granulomas form in breast tissue. It strikes mostly young to middle-aged women with painful, firm breast masses, sometimes with redness and drainage. Diagnosis is by biopsy with rule-out of known causes.
IGM does not respond to antibiotics. Prednisone and surgery have been the traditional approaches, but masses can recur after surgery, and a year or more of prednisone, with the weight gain and side effects, is problematic. As a result, cases are increasingly being referred to rheumatologists for other options, said lead investigator Sarah Ringsted, MD, a rheumatology fellow at the university.
A study she presented at the annual meeting of the American College of Rheumatology and previous work from others builds a case for methotrexate, which often seems to put the disease in remission and allows for shorter glucocorticoid courses. These days, “I offer this to patients as a great option. It’s really nice to have, instead of having women go on months and months of high-dose steroids, and I think we can save patients from unnecessary” surgery, Dr. Ringsted said.
Her usual regimen these days is methotrexate 15-20 mg/week for 12-18 months, with high-dose prednisone (greater than 20 mg/day) for the first 3 months, followed by a taper.
Dr. Ringsted and associates compared 23 women treated at the university during 2007-2018. Just 5 of the 12 women (42%) treated with high-dose prednisone alone went into remission and did not relapse over a mean follow-up of 27 months. Two out of three women who had both high-dose glucocorticoids and surgery achieved remission without relapse, as did all three women who received methotrexate and high-dose glucocorticoids (one also had surgery). Five other patients were treated with other options; just two had a durable remission.
The numbers are small, but they add to two previous reports. Among 19 women who had failed other treatments, 94% improved and 75% went into remission with 15 months of methotrexate in a review from Stanford (Calif.) University. An Iranian study of 17 patients treated with methotrexate, and also glucocorticoids in some, had a relapse rate of only 17.8%.
There were several cases of both inflammatory arthritis and erythema nodosum in the Oregon series, a higher incidence than what has been reported before for IGM. “It’s interesting because it makes me think of sarcoidosis. There have been cases of sarcoidosis causing mastitis, but mostly in patients with other features” of the disease. “It makes me wonder if any of these women will develop sarcoidosis later on; I think that’s an interesting question,” Dr. Ringsted said.
Women in the study were an average age of 32 years, and over half were Hispanic, which is associated with a higher risk for IGM. Almost all the women had been pregnant before and had breast fed in the previous 5 years. Cancer, tuberculosis, and fungal infections were among the things ruled out before mastitis was deemed idiopathic.
Women with IGM tend to be of childbearing age, and must be cautioned against the teratogenic effects of methotrexate, Dr. Ringsted noted.
There was no external funding, and the investigators didn’t report any disclosures.
SOURCE: Ringsted S et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 386.
ATLANTA – Methotrexate, in combination with prednisone, might be emerging as the go-to option for idiopathic granulomatous mastitis, according to investigators from Oregon Health & Science University, Portland.
Idiopathic granulomatous mastitis (IGM) is an inflammatory disease in which granulomas form in breast tissue. It strikes mostly young to middle-aged women with painful, firm breast masses, sometimes with redness and drainage. Diagnosis is by biopsy with rule-out of known causes.
IGM does not respond to antibiotics. Prednisone and surgery have been the traditional approaches, but masses can recur after surgery, and a year or more of prednisone, with the weight gain and side effects, is problematic. As a result, cases are increasingly being referred to rheumatologists for other options, said lead investigator Sarah Ringsted, MD, a rheumatology fellow at the university.
A study she presented at the annual meeting of the American College of Rheumatology and previous work from others builds a case for methotrexate, which often seems to put the disease in remission and allows for shorter glucocorticoid courses. These days, “I offer this to patients as a great option. It’s really nice to have, instead of having women go on months and months of high-dose steroids, and I think we can save patients from unnecessary” surgery, Dr. Ringsted said.
Her usual regimen these days is methotrexate 15-20 mg/week for 12-18 months, with high-dose prednisone (greater than 20 mg/day) for the first 3 months, followed by a taper.
Dr. Ringsted and associates compared 23 women treated at the university during 2007-2018. Just 5 of the 12 women (42%) treated with high-dose prednisone alone went into remission and did not relapse over a mean follow-up of 27 months. Two out of three women who had both high-dose glucocorticoids and surgery achieved remission without relapse, as did all three women who received methotrexate and high-dose glucocorticoids (one also had surgery). Five other patients were treated with other options; just two had a durable remission.
The numbers are small, but they add to two previous reports. Among 19 women who had failed other treatments, 94% improved and 75% went into remission with 15 months of methotrexate in a review from Stanford (Calif.) University. An Iranian study of 17 patients treated with methotrexate, and also glucocorticoids in some, had a relapse rate of only 17.8%.
There were several cases of both inflammatory arthritis and erythema nodosum in the Oregon series, a higher incidence than what has been reported before for IGM. “It’s interesting because it makes me think of sarcoidosis. There have been cases of sarcoidosis causing mastitis, but mostly in patients with other features” of the disease. “It makes me wonder if any of these women will develop sarcoidosis later on; I think that’s an interesting question,” Dr. Ringsted said.
Women in the study were an average age of 32 years, and over half were Hispanic, which is associated with a higher risk for IGM. Almost all the women had been pregnant before and had breast fed in the previous 5 years. Cancer, tuberculosis, and fungal infections were among the things ruled out before mastitis was deemed idiopathic.
Women with IGM tend to be of childbearing age, and must be cautioned against the teratogenic effects of methotrexate, Dr. Ringsted noted.
There was no external funding, and the investigators didn’t report any disclosures.
SOURCE: Ringsted S et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 386.
REPORTING FROM ACR 2019
EEG surveillance, preseizure treatment prevents TSC epilepsy, cognitive loss
BALTIMORE – Monitoring children who have tuberous sclerosis with EEG and treating them with vigabatrin (Sabril) at the first sign of preseizure abnormalities, rather than the usual practice of no surveillance and waiting until they have seizures, prevents epilepsy and cognitive decline, according to European investigators.
Early surveillance is recommended and standard practice in Europe. That’s not the case in the United States, but might be someday pending the results of the PREVENT trial (Preventing Epilepsy Using Vigabatrin In Infants With Tuberous Sclerosis Complex), an ongoing, National Institute of Neurological Disorders and Stroke–funded study to confirm the European findings.
“We are trying to convince doctors” in the United States and other “countries to do this. If you are not convinced to do early treatment,” at least “do surveillance with EEG. You will diagnose epilepsy earlier, and treat earlier, and children will do much better,” said Sergiusz Jozwiak, MD, PhD, head of pediatric neurology at Warsaw Medical University and recipient of an award from the U.S. Tuberous Sclerosis Alliance for his pioneering work.
Some U.S. physicians are already doing preventive treatment, but it’s hit and miss. “We are talking about monitoring children below the age of 2 years,” when seizures are associated with cognitive decline, he noted at the annual meeting of the American Epilepsy Society.
Dr. Jozwiak presented a follow-up at the meeting to his 2011 investigation, the first prevention study in tuberous sclerosis. Fourteen infants diagnosed within 2 months of birth underwent video-EEG monitoring every 4-6 weeks until age 2 years and were treated with vigabatrin 100-150 mg/kg per day when multifocal epileptiform discharges – a sign of impending seizures – were detected. Outcomes were compared with infants treated traditionally, with no EEG monitoring and vigabatrin only after they seized.
The children are about 9 years old now; the median IQ in the prevention arm is 94 versus 46 in the control group (P less than .03). Seven of the 14 prevention children (50%) never had a clinical seizure, while all but 1 of 25 (96%) in the control arm did (P = .001). Six of 11 prevention children (55%) versus 4 of 24 in the control group (17%), were able to come off antiepileptic drugs altogether, with no seizures (P less than .03). The work was published shortly before the epilepsy meeting.
The original 2011 report, which had similarly favorable outcomes when the children were 2 years old, led directly to the EpiStop trial, conducted at 16 mostly European centers and also reported at the meeting. Dr. Jozwiak was the senior investigator.
The design was different; all of the infants had EEG monitoring every 4 weeks until month 6, then every 6 weeks until age 12 months, then every 2 months until age 2 years. At the first detection of multifocal epileptiform discharges, infants were randomized 1:1 to vigabatrin or to the control group, with further monitoring followed by vigabatrin at the first seizure on EEG or first clinical seizure. An additional group of children – the open-label arm – also had EEG monitoring, but when to start vigabatrin was left up to the study site.
Only 50 of the original 94 children completed the trial to the full 2 years; tuberous sclerosis comorbidities drove many of them out, said lead investigator Katarzyna Kotulska-Jozwiak, MD, PhD, head of neurology at Children’s Memorial Health Institute, Warsaw.
Even so, the 25 children treated preventively in the randomized and open-label cohorts were more than three times as likely to be seizure free at 2 years (P = .01), and 74% less likely to develop drug-resistant epilepsy (P = .013). None of the prevention children developed infantile spasms versus 10 controls (40%) treated at first clinical or EEG seizure.
The incidence of neurodevelopmental delay was 34%, and autism 33%, at 24 months, and did not differ between prevention and control subjects. It’s probably because even children in the control group benefited from EEG surveillance and early treatment, the investigators said.
Historically, the rate of intellectual disability with usual treatment is around 60%, Dr. Kotulska-Jozwiak noted.
Overall, Dr. Jozwiak said that European physicians are more comfortable using vigabatrin than U.S. doctors, where the drug hasn’t been on the market as long and carries a Food and Drug Administration boxed warning of visual impairment. Its indications in the United States include infantile spasms in children 1-24 months old.
Levetiracetam (Keppra) is another option, but it’s not as effective in tuberous sclerosis. The PREVENT trial is using vigabatrin, and some U.S. doctors “are changing their minds, but it takes time,” Dr. Jozwiak said.
He noted that TSC is increasingly being diagnosed in utero, which gives a leg up on early diagnosis and prevention. The giveaways are heart tumors on ECG and cortical tubers on fetal MRI.
Dr. Jozwiak thinks the prevention approach might also help in other early seizure disorders, such as Sturge-Weber syndrome.
The work was funded by the European Commission and Polish government. Dr. Jozwiak and Dr. Kotulska-Jozwiak didn’t have any disclosures.
SOURCES: Jozwiak S et al. AES 2019, Abstract 1.218; Kotulska-Jozwiak K et al. AES 2019, Abstract 2.121.
BALTIMORE – Monitoring children who have tuberous sclerosis with EEG and treating them with vigabatrin (Sabril) at the first sign of preseizure abnormalities, rather than the usual practice of no surveillance and waiting until they have seizures, prevents epilepsy and cognitive decline, according to European investigators.
Early surveillance is recommended and standard practice in Europe. That’s not the case in the United States, but might be someday pending the results of the PREVENT trial (Preventing Epilepsy Using Vigabatrin In Infants With Tuberous Sclerosis Complex), an ongoing, National Institute of Neurological Disorders and Stroke–funded study to confirm the European findings.
“We are trying to convince doctors” in the United States and other “countries to do this. If you are not convinced to do early treatment,” at least “do surveillance with EEG. You will diagnose epilepsy earlier, and treat earlier, and children will do much better,” said Sergiusz Jozwiak, MD, PhD, head of pediatric neurology at Warsaw Medical University and recipient of an award from the U.S. Tuberous Sclerosis Alliance for his pioneering work.
Some U.S. physicians are already doing preventive treatment, but it’s hit and miss. “We are talking about monitoring children below the age of 2 years,” when seizures are associated with cognitive decline, he noted at the annual meeting of the American Epilepsy Society.
Dr. Jozwiak presented a follow-up at the meeting to his 2011 investigation, the first prevention study in tuberous sclerosis. Fourteen infants diagnosed within 2 months of birth underwent video-EEG monitoring every 4-6 weeks until age 2 years and were treated with vigabatrin 100-150 mg/kg per day when multifocal epileptiform discharges – a sign of impending seizures – were detected. Outcomes were compared with infants treated traditionally, with no EEG monitoring and vigabatrin only after they seized.
The children are about 9 years old now; the median IQ in the prevention arm is 94 versus 46 in the control group (P less than .03). Seven of the 14 prevention children (50%) never had a clinical seizure, while all but 1 of 25 (96%) in the control arm did (P = .001). Six of 11 prevention children (55%) versus 4 of 24 in the control group (17%), were able to come off antiepileptic drugs altogether, with no seizures (P less than .03). The work was published shortly before the epilepsy meeting.
The original 2011 report, which had similarly favorable outcomes when the children were 2 years old, led directly to the EpiStop trial, conducted at 16 mostly European centers and also reported at the meeting. Dr. Jozwiak was the senior investigator.
The design was different; all of the infants had EEG monitoring every 4 weeks until month 6, then every 6 weeks until age 12 months, then every 2 months until age 2 years. At the first detection of multifocal epileptiform discharges, infants were randomized 1:1 to vigabatrin or to the control group, with further monitoring followed by vigabatrin at the first seizure on EEG or first clinical seizure. An additional group of children – the open-label arm – also had EEG monitoring, but when to start vigabatrin was left up to the study site.
Only 50 of the original 94 children completed the trial to the full 2 years; tuberous sclerosis comorbidities drove many of them out, said lead investigator Katarzyna Kotulska-Jozwiak, MD, PhD, head of neurology at Children’s Memorial Health Institute, Warsaw.
Even so, the 25 children treated preventively in the randomized and open-label cohorts were more than three times as likely to be seizure free at 2 years (P = .01), and 74% less likely to develop drug-resistant epilepsy (P = .013). None of the prevention children developed infantile spasms versus 10 controls (40%) treated at first clinical or EEG seizure.
The incidence of neurodevelopmental delay was 34%, and autism 33%, at 24 months, and did not differ between prevention and control subjects. It’s probably because even children in the control group benefited from EEG surveillance and early treatment, the investigators said.
Historically, the rate of intellectual disability with usual treatment is around 60%, Dr. Kotulska-Jozwiak noted.
Overall, Dr. Jozwiak said that European physicians are more comfortable using vigabatrin than U.S. doctors, where the drug hasn’t been on the market as long and carries a Food and Drug Administration boxed warning of visual impairment. Its indications in the United States include infantile spasms in children 1-24 months old.
Levetiracetam (Keppra) is another option, but it’s not as effective in tuberous sclerosis. The PREVENT trial is using vigabatrin, and some U.S. doctors “are changing their minds, but it takes time,” Dr. Jozwiak said.
He noted that TSC is increasingly being diagnosed in utero, which gives a leg up on early diagnosis and prevention. The giveaways are heart tumors on ECG and cortical tubers on fetal MRI.
Dr. Jozwiak thinks the prevention approach might also help in other early seizure disorders, such as Sturge-Weber syndrome.
The work was funded by the European Commission and Polish government. Dr. Jozwiak and Dr. Kotulska-Jozwiak didn’t have any disclosures.
SOURCES: Jozwiak S et al. AES 2019, Abstract 1.218; Kotulska-Jozwiak K et al. AES 2019, Abstract 2.121.
BALTIMORE – Monitoring children who have tuberous sclerosis with EEG and treating them with vigabatrin (Sabril) at the first sign of preseizure abnormalities, rather than the usual practice of no surveillance and waiting until they have seizures, prevents epilepsy and cognitive decline, according to European investigators.
Early surveillance is recommended and standard practice in Europe. That’s not the case in the United States, but might be someday pending the results of the PREVENT trial (Preventing Epilepsy Using Vigabatrin In Infants With Tuberous Sclerosis Complex), an ongoing, National Institute of Neurological Disorders and Stroke–funded study to confirm the European findings.
“We are trying to convince doctors” in the United States and other “countries to do this. If you are not convinced to do early treatment,” at least “do surveillance with EEG. You will diagnose epilepsy earlier, and treat earlier, and children will do much better,” said Sergiusz Jozwiak, MD, PhD, head of pediatric neurology at Warsaw Medical University and recipient of an award from the U.S. Tuberous Sclerosis Alliance for his pioneering work.
Some U.S. physicians are already doing preventive treatment, but it’s hit and miss. “We are talking about monitoring children below the age of 2 years,” when seizures are associated with cognitive decline, he noted at the annual meeting of the American Epilepsy Society.
Dr. Jozwiak presented a follow-up at the meeting to his 2011 investigation, the first prevention study in tuberous sclerosis. Fourteen infants diagnosed within 2 months of birth underwent video-EEG monitoring every 4-6 weeks until age 2 years and were treated with vigabatrin 100-150 mg/kg per day when multifocal epileptiform discharges – a sign of impending seizures – were detected. Outcomes were compared with infants treated traditionally, with no EEG monitoring and vigabatrin only after they seized.
The children are about 9 years old now; the median IQ in the prevention arm is 94 versus 46 in the control group (P less than .03). Seven of the 14 prevention children (50%) never had a clinical seizure, while all but 1 of 25 (96%) in the control arm did (P = .001). Six of 11 prevention children (55%) versus 4 of 24 in the control group (17%), were able to come off antiepileptic drugs altogether, with no seizures (P less than .03). The work was published shortly before the epilepsy meeting.
The original 2011 report, which had similarly favorable outcomes when the children were 2 years old, led directly to the EpiStop trial, conducted at 16 mostly European centers and also reported at the meeting. Dr. Jozwiak was the senior investigator.
The design was different; all of the infants had EEG monitoring every 4 weeks until month 6, then every 6 weeks until age 12 months, then every 2 months until age 2 years. At the first detection of multifocal epileptiform discharges, infants were randomized 1:1 to vigabatrin or to the control group, with further monitoring followed by vigabatrin at the first seizure on EEG or first clinical seizure. An additional group of children – the open-label arm – also had EEG monitoring, but when to start vigabatrin was left up to the study site.
Only 50 of the original 94 children completed the trial to the full 2 years; tuberous sclerosis comorbidities drove many of them out, said lead investigator Katarzyna Kotulska-Jozwiak, MD, PhD, head of neurology at Children’s Memorial Health Institute, Warsaw.
Even so, the 25 children treated preventively in the randomized and open-label cohorts were more than three times as likely to be seizure free at 2 years (P = .01), and 74% less likely to develop drug-resistant epilepsy (P = .013). None of the prevention children developed infantile spasms versus 10 controls (40%) treated at first clinical or EEG seizure.
The incidence of neurodevelopmental delay was 34%, and autism 33%, at 24 months, and did not differ between prevention and control subjects. It’s probably because even children in the control group benefited from EEG surveillance and early treatment, the investigators said.
Historically, the rate of intellectual disability with usual treatment is around 60%, Dr. Kotulska-Jozwiak noted.
Overall, Dr. Jozwiak said that European physicians are more comfortable using vigabatrin than U.S. doctors, where the drug hasn’t been on the market as long and carries a Food and Drug Administration boxed warning of visual impairment. Its indications in the United States include infantile spasms in children 1-24 months old.
Levetiracetam (Keppra) is another option, but it’s not as effective in tuberous sclerosis. The PREVENT trial is using vigabatrin, and some U.S. doctors “are changing their minds, but it takes time,” Dr. Jozwiak said.
He noted that TSC is increasingly being diagnosed in utero, which gives a leg up on early diagnosis and prevention. The giveaways are heart tumors on ECG and cortical tubers on fetal MRI.
Dr. Jozwiak thinks the prevention approach might also help in other early seizure disorders, such as Sturge-Weber syndrome.
The work was funded by the European Commission and Polish government. Dr. Jozwiak and Dr. Kotulska-Jozwiak didn’t have any disclosures.
SOURCES: Jozwiak S et al. AES 2019, Abstract 1.218; Kotulska-Jozwiak K et al. AES 2019, Abstract 2.121.
REPORTING FROM AES 2019