User login
Multimodal approach is state of the art for ulcerated infantile hemangiomas
CHICAGO –
About 16% of infantile hemangiomas become ulcerated at some point during their proliferative phase, said Kate Puttgen, MD, during a talk at the World Congress of Pediatric Dermatology.
One clinical clue to picking up an infantile hemangioma (IH) that’s destined to ulcerate is an early grayish to white discoloration of the lesion, said Dr. Puttgen, chief of the division of pediatric dermatology at Johns Hopkins Medicine, Baltimore.
“Multimodal therapy is an absolute necessity” in treating an ulcerated IH, said Dr. Puttgen. Using an “all hands on deck” approach – a combination of topical and systemic modalities – can help bring the lesion under control.
Beta-blockers are first-line therapy to manage complicated IHs, with propranolol yielding a 98% response rate for all complicated IHs in the literature, said Dr. Puttgen.
Propranolol can decrease the volume and color of IHs and speed involution, in part by its ability to continue working after the proliferative growth phase of an IH. It’s also been shown to reduce the need for surgery in nasal IH, and it’s well tolerated, she added.
Evidence-based therapies for ulcerated hemangiomas include systemic propranolol at 1-3 mg/kg per day. That protocol will result in a healed ulcer within 2-6 weeks in most of the published case series, Dr. Puttgen noted.
Topical timolol also has evidence supporting its use for an ulcerated IH, and it has been found generally safe. In one study of 30 patients with IH, she said, three had mild adverse events consisting of sleep disturbance, diarrhea, and acrocyanosis. Another study reported success when brimonidine 0.2% and timolol 0.5% were used together. It’s possible, said Dr. Puttgen, that there’s a synergistic effect when combining the selective alpha-2 adrenergic agonist effect of brimonidine with timolol, which provides nonselective beta adrenergic blockade. However, she said, there has been an isolated report of brimonidine toxicity.
The ulcerated IHs need wound care, Dr. Puttgen added, with barrier creams and dressings. Pain management should be considered, because an ulcerated IH may have a large, friable, bleeding area. Pulsed-dye laser can also be a useful treatment modality for an ulcerating IH.
Going beyond the treatments for which the evidence is strongest and moving into more “state-of-the-art” treatments, “there may be a niche role for oral corticosteroids” as combination systemic therapy with propranolol, Dr. Puttgen said.
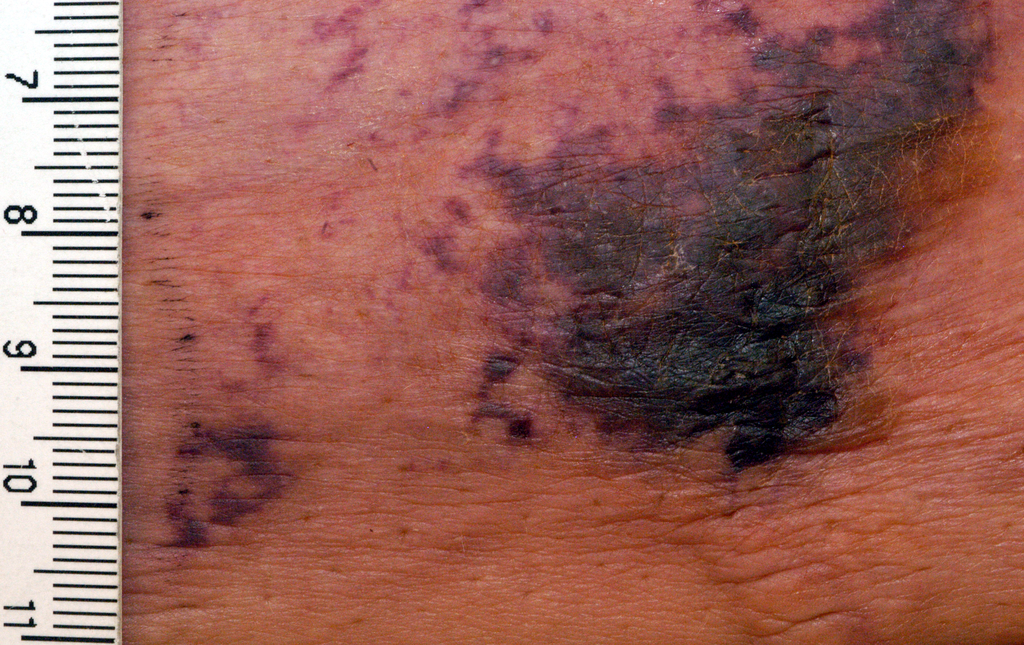
She shared images from a recently published report, in which she’s the senior author, showing the progression of an ulcerated IH. The hemangioma had received wound care and pulsed-dye laser treatment, and the infant was started on systemic propranolol. After 2 weeks, the IH had decreased significantly in volume, but the ulcerated area had actually increased. With the addition of oral corticosteroids, there was a reduction in ulceration after 2 weeks; and after 5 weeks of prednisolone, “the ulceration resolved without rebound,” said Dr. Puttgen. The corticosteroid was then tapered and propranolol was continued for an additional 2 months, then tapered. By 10 months, the IH had almost completely resolved (Br J Dermatol. 2017 Apr;176[4]:1064-7).
If a corticosteroid is added to propranolol, there may be benefit to a slower propranolol dose, Dr. Puttgen said. She suggests an altered dosing schedule, beginning with 1 mg/kg per day in two or three divided doses. Then, over a period of 2-7 days, the total daily dose can be increased to 1.5 mg/kg per day. Bumping the dose up to 2 mg/kg per day or higher should not happen until after 2 weeks at the reduced dosing schedule, she explained.
Dr. Puttgen disclosed that she is on the advisory board and has received honoraria from Pierre Fabre Dermatologie.
[email protected]
On Twitter @karioakes
CHICAGO –
About 16% of infantile hemangiomas become ulcerated at some point during their proliferative phase, said Kate Puttgen, MD, during a talk at the World Congress of Pediatric Dermatology.
One clinical clue to picking up an infantile hemangioma (IH) that’s destined to ulcerate is an early grayish to white discoloration of the lesion, said Dr. Puttgen, chief of the division of pediatric dermatology at Johns Hopkins Medicine, Baltimore.
“Multimodal therapy is an absolute necessity” in treating an ulcerated IH, said Dr. Puttgen. Using an “all hands on deck” approach – a combination of topical and systemic modalities – can help bring the lesion under control.
Beta-blockers are first-line therapy to manage complicated IHs, with propranolol yielding a 98% response rate for all complicated IHs in the literature, said Dr. Puttgen.
Propranolol can decrease the volume and color of IHs and speed involution, in part by its ability to continue working after the proliferative growth phase of an IH. It’s also been shown to reduce the need for surgery in nasal IH, and it’s well tolerated, she added.
Evidence-based therapies for ulcerated hemangiomas include systemic propranolol at 1-3 mg/kg per day. That protocol will result in a healed ulcer within 2-6 weeks in most of the published case series, Dr. Puttgen noted.
Topical timolol also has evidence supporting its use for an ulcerated IH, and it has been found generally safe. In one study of 30 patients with IH, she said, three had mild adverse events consisting of sleep disturbance, diarrhea, and acrocyanosis. Another study reported success when brimonidine 0.2% and timolol 0.5% were used together. It’s possible, said Dr. Puttgen, that there’s a synergistic effect when combining the selective alpha-2 adrenergic agonist effect of brimonidine with timolol, which provides nonselective beta adrenergic blockade. However, she said, there has been an isolated report of brimonidine toxicity.
The ulcerated IHs need wound care, Dr. Puttgen added, with barrier creams and dressings. Pain management should be considered, because an ulcerated IH may have a large, friable, bleeding area. Pulsed-dye laser can also be a useful treatment modality for an ulcerating IH.
Going beyond the treatments for which the evidence is strongest and moving into more “state-of-the-art” treatments, “there may be a niche role for oral corticosteroids” as combination systemic therapy with propranolol, Dr. Puttgen said.
She shared images from a recently published report, in which she’s the senior author, showing the progression of an ulcerated IH. The hemangioma had received wound care and pulsed-dye laser treatment, and the infant was started on systemic propranolol. After 2 weeks, the IH had decreased significantly in volume, but the ulcerated area had actually increased. With the addition of oral corticosteroids, there was a reduction in ulceration after 2 weeks; and after 5 weeks of prednisolone, “the ulceration resolved without rebound,” said Dr. Puttgen. The corticosteroid was then tapered and propranolol was continued for an additional 2 months, then tapered. By 10 months, the IH had almost completely resolved (Br J Dermatol. 2017 Apr;176[4]:1064-7).
If a corticosteroid is added to propranolol, there may be benefit to a slower propranolol dose, Dr. Puttgen said. She suggests an altered dosing schedule, beginning with 1 mg/kg per day in two or three divided doses. Then, over a period of 2-7 days, the total daily dose can be increased to 1.5 mg/kg per day. Bumping the dose up to 2 mg/kg per day or higher should not happen until after 2 weeks at the reduced dosing schedule, she explained.
Dr. Puttgen disclosed that she is on the advisory board and has received honoraria from Pierre Fabre Dermatologie.
[email protected]
On Twitter @karioakes
CHICAGO –
About 16% of infantile hemangiomas become ulcerated at some point during their proliferative phase, said Kate Puttgen, MD, during a talk at the World Congress of Pediatric Dermatology.
One clinical clue to picking up an infantile hemangioma (IH) that’s destined to ulcerate is an early grayish to white discoloration of the lesion, said Dr. Puttgen, chief of the division of pediatric dermatology at Johns Hopkins Medicine, Baltimore.
“Multimodal therapy is an absolute necessity” in treating an ulcerated IH, said Dr. Puttgen. Using an “all hands on deck” approach – a combination of topical and systemic modalities – can help bring the lesion under control.
Beta-blockers are first-line therapy to manage complicated IHs, with propranolol yielding a 98% response rate for all complicated IHs in the literature, said Dr. Puttgen.
Propranolol can decrease the volume and color of IHs and speed involution, in part by its ability to continue working after the proliferative growth phase of an IH. It’s also been shown to reduce the need for surgery in nasal IH, and it’s well tolerated, she added.
Evidence-based therapies for ulcerated hemangiomas include systemic propranolol at 1-3 mg/kg per day. That protocol will result in a healed ulcer within 2-6 weeks in most of the published case series, Dr. Puttgen noted.
Topical timolol also has evidence supporting its use for an ulcerated IH, and it has been found generally safe. In one study of 30 patients with IH, she said, three had mild adverse events consisting of sleep disturbance, diarrhea, and acrocyanosis. Another study reported success when brimonidine 0.2% and timolol 0.5% were used together. It’s possible, said Dr. Puttgen, that there’s a synergistic effect when combining the selective alpha-2 adrenergic agonist effect of brimonidine with timolol, which provides nonselective beta adrenergic blockade. However, she said, there has been an isolated report of brimonidine toxicity.
The ulcerated IHs need wound care, Dr. Puttgen added, with barrier creams and dressings. Pain management should be considered, because an ulcerated IH may have a large, friable, bleeding area. Pulsed-dye laser can also be a useful treatment modality for an ulcerating IH.
Going beyond the treatments for which the evidence is strongest and moving into more “state-of-the-art” treatments, “there may be a niche role for oral corticosteroids” as combination systemic therapy with propranolol, Dr. Puttgen said.
She shared images from a recently published report, in which she’s the senior author, showing the progression of an ulcerated IH. The hemangioma had received wound care and pulsed-dye laser treatment, and the infant was started on systemic propranolol. After 2 weeks, the IH had decreased significantly in volume, but the ulcerated area had actually increased. With the addition of oral corticosteroids, there was a reduction in ulceration after 2 weeks; and after 5 weeks of prednisolone, “the ulceration resolved without rebound,” said Dr. Puttgen. The corticosteroid was then tapered and propranolol was continued for an additional 2 months, then tapered. By 10 months, the IH had almost completely resolved (Br J Dermatol. 2017 Apr;176[4]:1064-7).
If a corticosteroid is added to propranolol, there may be benefit to a slower propranolol dose, Dr. Puttgen said. She suggests an altered dosing schedule, beginning with 1 mg/kg per day in two or three divided doses. Then, over a period of 2-7 days, the total daily dose can be increased to 1.5 mg/kg per day. Bumping the dose up to 2 mg/kg per day or higher should not happen until after 2 weeks at the reduced dosing schedule, she explained.
Dr. Puttgen disclosed that she is on the advisory board and has received honoraria from Pierre Fabre Dermatologie.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM WCPD 2017
Pregnancy not a barrier to providing cutaneous surgery
NEW YORK – For some dermatologists, surgical care of the pregnant patient represents an area of uncertainty. But with few exceptions, dermatologists can continue with business as usual for their pregnant patients, according to Keith Harrigill, MD.
Dr. Harrigill, a dermatologist who previously was a practicing obstetrician-gynecologist, delineated the safe zones of dermatologic surgery in these patients at the summer meeting of the American Academy of Dermatology.
About 2% of pregnant women will require nonobstetric surgery and about 75,000 pregnant women in the United States will have surgery annually, he said. Appendectomies and other emergent abdominal surgery account for a large proportion of these cases; dermatologic surgeries are not included in these figures, and cutaneous procedures in pregnant women are not usually tracked. The literature on dermatologic treatments during pregnancy is “scant,” said Dr. Harrigill, a dermatologist in private practice in Birmingham, Ala.
However, it’s known that one-third of women with melanoma are of childbearing age, and melanoma accounts for 8% of the malignancies diagnosed during pregnancy, with a rate estimated at 0.14 to 2.8 per 1,000 live births, he said.
Since some women will have to address potentially serious skin issues during pregnancy, what’s safe, and what isn’t? Dr. Harrigill said that the American College of Obstetrics and Gynecology has provided guidance with an April 2017 opinion, prepared in conjunction with the American Society for Anesthesia, on nonobstetric surgery during pregnancy (Obstet Gynecol. 2017;129:777-8).
The opinion primarily focuses on major surgery. “What we do – cutaneous surgeries – they consider to be minor surgery,” he said. But even with major procedures, the good news is that “there’s no increase in birth defects in fetal exposure to anesthesia at any age,” he noted.
Dr. Harrigill’s approach, which conforms to the general guidance provided by the opinion, is to think of dermatologic procedures in three categories: urgent, nonurgent, and elective. Urgent procedures might include biopsying and treating a lesion suspicious for melanoma or an aggressive nonmelanoma skin cancer, or controlling a friable, bleeding pyogenic granuloma. “Do these right away,” he said.
Nonurgent procedures, such as treatment of a nodular basal cell carcinoma, should be done during the second trimester, when possible. Elective procedures, such as a scar excision, should be deferred until after delivery.
Dermatologists can almost always achieve adequate pain control with local anesthesia alone, said Dr. Harrigill, pointing out that local anesthesia is “the safest known way to give anesthesia during pregnancy.”
However, when thinking about even a remote risk of teratogenesis, it’s important to understand that fetal organogenesis occurs from day 15 to day 56, and that before 15 days, adverse events are limited to spontaneous abortion. So it’s particularly important to avoid teratogenic medications during the first 2 months of gestation, Dr. Harrigill said.
Part of the concern, he noted, is that it’s ethically problematic to perform large randomized trials in pregnant women, so the guidelines regarding surgery and medication safety are drawn from retrospective studies, registries, meta-analyses, and expert consensus.
Still, according to the ACOG guidelines, “a pregnant woman should never be denied indicated surgery, regardless of trimester.”
There’s no reason to risk delaying a diagnosis of malignancy in a pregnant patient, Dr. Harrigill said. “My dermatologic surgery approach is to biopsy anything that is clinically suspicious for malignancy, at any gestational age.”
When performing biopsies in pregnant patients, he uses the same protocol as he uses with any other patient. Skin preparation can be done with either isopropyl alcohol or chlorhexidine. Some practitioners avoid using povidone iodine because of a theoretical risk of fetal hypothyroidism.
For anesthesia, Dr. Harrigill noted that lidocaine is generally considered safe in pregnancy. He is also comfortable using epinephrine, despite the theoretical concern of uterine artery spasm, for which “studies are lacking.” The relatively minute amount of epinephrine used in dermatologic anesthesia, he said, is not likely to have an impact on such a large vessel.
Prilocaine is generally safe, and combination creams with prilocaine are fine to use, he said. Diphenhydramine is also safe to use. However, he advised avoiding long-acting anesthetic agents, such as mepivacaine and bupivacaine.
His advice regarding sedation? “Don’t do it.” Dr. Harrigill said he doesn’t use sedation in the office for his nonpregnant patients, either.
Before about 20 weeks of pregnancy, Dr. Harrigill said not to worry about how the patient is positioned. But after that, the lateral decubitus position is best because it keeps the gravid uterus from compressing the great vessels.
“Pregnant women are prone to fainting due to progesterone-mediated vasodilation,” he said. Dermatologists can work with their office staff to keep these patients well hydrated, and make sure they get in and out of chairs and off exam tables slowly.
No changes are needed in excision or suturing techniques. Because cicatrization is delayed in pregnant women, Dr. Harrigill uses longer-lasting absorbable sutures with high tensile strength, especially when performing procedures on the trunk or abdomen. This means that his closures will use delayed-absorption epidermal sutures with running nylon pull-through subcuticular sutures as well. He will leave these in for 5-7 days longer than usual.
Pregnant women are not at a higher risk of infection than the general population, so he follows the standard procedures here as well. If an antibiotic is indicated, penicillin, a cephalosporin, azithromycin, and erythromycin base are all logical choices.
To be avoided are sulfamethoxazole/trimethoprim, which carries a risk of feta hyperbilirubinemia, especially when given in the second trimester; doxycycline and tetracycline, which can cause permanent brown discoloration of the teeth; and fluoroquinolones, which have been associated with cartilage defects.
For analgesia, acetaminophen is an option. Ibuprofen and salicylates should be avoided, especially at the end of pregnancy when their administration is associated with premature closure of the ductus arteriosus, and, possibly, placental abruption, Dr. Harrigill noted.
However, short-term use of opioids is generally considered safe for the fetus. If larger doses are given just before delivery, the neonate may experience respiratory depression. This scenario is unlikely to be faced by the dermatologist, noted Dr. Harrigill. “I use these without reservation” in terms of fetal risk, he said.
Collaboration is key when caring for pregnant patients, said Dr. Harrigill, who recommends consulting the obstetrician of record for any procedures other than a simple biopsy or shave removal.
Dr. Harrigill reported that he had no conflicts of interest.
[email protected]
On Twitter @karioakes
NEW YORK – For some dermatologists, surgical care of the pregnant patient represents an area of uncertainty. But with few exceptions, dermatologists can continue with business as usual for their pregnant patients, according to Keith Harrigill, MD.
Dr. Harrigill, a dermatologist who previously was a practicing obstetrician-gynecologist, delineated the safe zones of dermatologic surgery in these patients at the summer meeting of the American Academy of Dermatology.
About 2% of pregnant women will require nonobstetric surgery and about 75,000 pregnant women in the United States will have surgery annually, he said. Appendectomies and other emergent abdominal surgery account for a large proportion of these cases; dermatologic surgeries are not included in these figures, and cutaneous procedures in pregnant women are not usually tracked. The literature on dermatologic treatments during pregnancy is “scant,” said Dr. Harrigill, a dermatologist in private practice in Birmingham, Ala.
However, it’s known that one-third of women with melanoma are of childbearing age, and melanoma accounts for 8% of the malignancies diagnosed during pregnancy, with a rate estimated at 0.14 to 2.8 per 1,000 live births, he said.
Since some women will have to address potentially serious skin issues during pregnancy, what’s safe, and what isn’t? Dr. Harrigill said that the American College of Obstetrics and Gynecology has provided guidance with an April 2017 opinion, prepared in conjunction with the American Society for Anesthesia, on nonobstetric surgery during pregnancy (Obstet Gynecol. 2017;129:777-8).
The opinion primarily focuses on major surgery. “What we do – cutaneous surgeries – they consider to be minor surgery,” he said. But even with major procedures, the good news is that “there’s no increase in birth defects in fetal exposure to anesthesia at any age,” he noted.
Dr. Harrigill’s approach, which conforms to the general guidance provided by the opinion, is to think of dermatologic procedures in three categories: urgent, nonurgent, and elective. Urgent procedures might include biopsying and treating a lesion suspicious for melanoma or an aggressive nonmelanoma skin cancer, or controlling a friable, bleeding pyogenic granuloma. “Do these right away,” he said.
Nonurgent procedures, such as treatment of a nodular basal cell carcinoma, should be done during the second trimester, when possible. Elective procedures, such as a scar excision, should be deferred until after delivery.
Dermatologists can almost always achieve adequate pain control with local anesthesia alone, said Dr. Harrigill, pointing out that local anesthesia is “the safest known way to give anesthesia during pregnancy.”
However, when thinking about even a remote risk of teratogenesis, it’s important to understand that fetal organogenesis occurs from day 15 to day 56, and that before 15 days, adverse events are limited to spontaneous abortion. So it’s particularly important to avoid teratogenic medications during the first 2 months of gestation, Dr. Harrigill said.
Part of the concern, he noted, is that it’s ethically problematic to perform large randomized trials in pregnant women, so the guidelines regarding surgery and medication safety are drawn from retrospective studies, registries, meta-analyses, and expert consensus.
Still, according to the ACOG guidelines, “a pregnant woman should never be denied indicated surgery, regardless of trimester.”
There’s no reason to risk delaying a diagnosis of malignancy in a pregnant patient, Dr. Harrigill said. “My dermatologic surgery approach is to biopsy anything that is clinically suspicious for malignancy, at any gestational age.”
When performing biopsies in pregnant patients, he uses the same protocol as he uses with any other patient. Skin preparation can be done with either isopropyl alcohol or chlorhexidine. Some practitioners avoid using povidone iodine because of a theoretical risk of fetal hypothyroidism.
For anesthesia, Dr. Harrigill noted that lidocaine is generally considered safe in pregnancy. He is also comfortable using epinephrine, despite the theoretical concern of uterine artery spasm, for which “studies are lacking.” The relatively minute amount of epinephrine used in dermatologic anesthesia, he said, is not likely to have an impact on such a large vessel.
Prilocaine is generally safe, and combination creams with prilocaine are fine to use, he said. Diphenhydramine is also safe to use. However, he advised avoiding long-acting anesthetic agents, such as mepivacaine and bupivacaine.
His advice regarding sedation? “Don’t do it.” Dr. Harrigill said he doesn’t use sedation in the office for his nonpregnant patients, either.
Before about 20 weeks of pregnancy, Dr. Harrigill said not to worry about how the patient is positioned. But after that, the lateral decubitus position is best because it keeps the gravid uterus from compressing the great vessels.
“Pregnant women are prone to fainting due to progesterone-mediated vasodilation,” he said. Dermatologists can work with their office staff to keep these patients well hydrated, and make sure they get in and out of chairs and off exam tables slowly.
No changes are needed in excision or suturing techniques. Because cicatrization is delayed in pregnant women, Dr. Harrigill uses longer-lasting absorbable sutures with high tensile strength, especially when performing procedures on the trunk or abdomen. This means that his closures will use delayed-absorption epidermal sutures with running nylon pull-through subcuticular sutures as well. He will leave these in for 5-7 days longer than usual.
Pregnant women are not at a higher risk of infection than the general population, so he follows the standard procedures here as well. If an antibiotic is indicated, penicillin, a cephalosporin, azithromycin, and erythromycin base are all logical choices.
To be avoided are sulfamethoxazole/trimethoprim, which carries a risk of feta hyperbilirubinemia, especially when given in the second trimester; doxycycline and tetracycline, which can cause permanent brown discoloration of the teeth; and fluoroquinolones, which have been associated with cartilage defects.
For analgesia, acetaminophen is an option. Ibuprofen and salicylates should be avoided, especially at the end of pregnancy when their administration is associated with premature closure of the ductus arteriosus, and, possibly, placental abruption, Dr. Harrigill noted.
However, short-term use of opioids is generally considered safe for the fetus. If larger doses are given just before delivery, the neonate may experience respiratory depression. This scenario is unlikely to be faced by the dermatologist, noted Dr. Harrigill. “I use these without reservation” in terms of fetal risk, he said.
Collaboration is key when caring for pregnant patients, said Dr. Harrigill, who recommends consulting the obstetrician of record for any procedures other than a simple biopsy or shave removal.
Dr. Harrigill reported that he had no conflicts of interest.
[email protected]
On Twitter @karioakes
NEW YORK – For some dermatologists, surgical care of the pregnant patient represents an area of uncertainty. But with few exceptions, dermatologists can continue with business as usual for their pregnant patients, according to Keith Harrigill, MD.
Dr. Harrigill, a dermatologist who previously was a practicing obstetrician-gynecologist, delineated the safe zones of dermatologic surgery in these patients at the summer meeting of the American Academy of Dermatology.
About 2% of pregnant women will require nonobstetric surgery and about 75,000 pregnant women in the United States will have surgery annually, he said. Appendectomies and other emergent abdominal surgery account for a large proportion of these cases; dermatologic surgeries are not included in these figures, and cutaneous procedures in pregnant women are not usually tracked. The literature on dermatologic treatments during pregnancy is “scant,” said Dr. Harrigill, a dermatologist in private practice in Birmingham, Ala.
However, it’s known that one-third of women with melanoma are of childbearing age, and melanoma accounts for 8% of the malignancies diagnosed during pregnancy, with a rate estimated at 0.14 to 2.8 per 1,000 live births, he said.
Since some women will have to address potentially serious skin issues during pregnancy, what’s safe, and what isn’t? Dr. Harrigill said that the American College of Obstetrics and Gynecology has provided guidance with an April 2017 opinion, prepared in conjunction with the American Society for Anesthesia, on nonobstetric surgery during pregnancy (Obstet Gynecol. 2017;129:777-8).
The opinion primarily focuses on major surgery. “What we do – cutaneous surgeries – they consider to be minor surgery,” he said. But even with major procedures, the good news is that “there’s no increase in birth defects in fetal exposure to anesthesia at any age,” he noted.
Dr. Harrigill’s approach, which conforms to the general guidance provided by the opinion, is to think of dermatologic procedures in three categories: urgent, nonurgent, and elective. Urgent procedures might include biopsying and treating a lesion suspicious for melanoma or an aggressive nonmelanoma skin cancer, or controlling a friable, bleeding pyogenic granuloma. “Do these right away,” he said.
Nonurgent procedures, such as treatment of a nodular basal cell carcinoma, should be done during the second trimester, when possible. Elective procedures, such as a scar excision, should be deferred until after delivery.
Dermatologists can almost always achieve adequate pain control with local anesthesia alone, said Dr. Harrigill, pointing out that local anesthesia is “the safest known way to give anesthesia during pregnancy.”
However, when thinking about even a remote risk of teratogenesis, it’s important to understand that fetal organogenesis occurs from day 15 to day 56, and that before 15 days, adverse events are limited to spontaneous abortion. So it’s particularly important to avoid teratogenic medications during the first 2 months of gestation, Dr. Harrigill said.
Part of the concern, he noted, is that it’s ethically problematic to perform large randomized trials in pregnant women, so the guidelines regarding surgery and medication safety are drawn from retrospective studies, registries, meta-analyses, and expert consensus.
Still, according to the ACOG guidelines, “a pregnant woman should never be denied indicated surgery, regardless of trimester.”
There’s no reason to risk delaying a diagnosis of malignancy in a pregnant patient, Dr. Harrigill said. “My dermatologic surgery approach is to biopsy anything that is clinically suspicious for malignancy, at any gestational age.”
When performing biopsies in pregnant patients, he uses the same protocol as he uses with any other patient. Skin preparation can be done with either isopropyl alcohol or chlorhexidine. Some practitioners avoid using povidone iodine because of a theoretical risk of fetal hypothyroidism.
For anesthesia, Dr. Harrigill noted that lidocaine is generally considered safe in pregnancy. He is also comfortable using epinephrine, despite the theoretical concern of uterine artery spasm, for which “studies are lacking.” The relatively minute amount of epinephrine used in dermatologic anesthesia, he said, is not likely to have an impact on such a large vessel.
Prilocaine is generally safe, and combination creams with prilocaine are fine to use, he said. Diphenhydramine is also safe to use. However, he advised avoiding long-acting anesthetic agents, such as mepivacaine and bupivacaine.
His advice regarding sedation? “Don’t do it.” Dr. Harrigill said he doesn’t use sedation in the office for his nonpregnant patients, either.
Before about 20 weeks of pregnancy, Dr. Harrigill said not to worry about how the patient is positioned. But after that, the lateral decubitus position is best because it keeps the gravid uterus from compressing the great vessels.
“Pregnant women are prone to fainting due to progesterone-mediated vasodilation,” he said. Dermatologists can work with their office staff to keep these patients well hydrated, and make sure they get in and out of chairs and off exam tables slowly.
No changes are needed in excision or suturing techniques. Because cicatrization is delayed in pregnant women, Dr. Harrigill uses longer-lasting absorbable sutures with high tensile strength, especially when performing procedures on the trunk or abdomen. This means that his closures will use delayed-absorption epidermal sutures with running nylon pull-through subcuticular sutures as well. He will leave these in for 5-7 days longer than usual.
Pregnant women are not at a higher risk of infection than the general population, so he follows the standard procedures here as well. If an antibiotic is indicated, penicillin, a cephalosporin, azithromycin, and erythromycin base are all logical choices.
To be avoided are sulfamethoxazole/trimethoprim, which carries a risk of feta hyperbilirubinemia, especially when given in the second trimester; doxycycline and tetracycline, which can cause permanent brown discoloration of the teeth; and fluoroquinolones, which have been associated with cartilage defects.
For analgesia, acetaminophen is an option. Ibuprofen and salicylates should be avoided, especially at the end of pregnancy when their administration is associated with premature closure of the ductus arteriosus, and, possibly, placental abruption, Dr. Harrigill noted.
However, short-term use of opioids is generally considered safe for the fetus. If larger doses are given just before delivery, the neonate may experience respiratory depression. This scenario is unlikely to be faced by the dermatologist, noted Dr. Harrigill. “I use these without reservation” in terms of fetal risk, he said.
Collaboration is key when caring for pregnant patients, said Dr. Harrigill, who recommends consulting the obstetrician of record for any procedures other than a simple biopsy or shave removal.
Dr. Harrigill reported that he had no conflicts of interest.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM THE 2017 AAD SUMMER MEETING
Clues to rosacea in patients of skin of color
NEW YORK – A middle-aged patient with Fitzpatrick type V skin comes to the office with a 10-year history of “breakouts” on her face. When asked about topical treatments, she reports that “everything burns or stings,” and says she just has very sensitive skin. What could this be?
Rosacea may often be missed in skin of color, said Dr. Alexis, speaking at the summer meeting of the American Academy of Dermatology. “It’s reportedly rare in darker skin types, especially in blacks,” and as a result, dermatologists and patients alike have a low index of suspicion for the diagnosis, he noted.
Also, rosacea looks different on darker skin than it does on lighter skin, which is featured in much of the dermatology teaching material. “In richly pigmented [Fitzpatrick] type VI skin, the erythema of rosacea can be masked,” said Dr. Alexis, chairman of the department of dermatology at Mount Sinai St. Luke’s and at Mount Sinai West, both in New York.
Dermatologists, in this case, may have to do some detective work: looking at the distribution of the lesions, thinking about trigger factors from the patient history, and noting the lack of comedones – although the patient has “pimples.” Patient complaints that they are sensitive to almost all topical products and experience stinging with “everything” is another very good clue that the patient may have rosacea.
Keep rosacea on the differential for this picture, advised Dr. Alexis. In skin of color, “rosacea may not be as rare as previously thought – less common, maybe – but not rare.”
Dr. Alexis reported financial relationships with multiple pharmaceutical companies.
[email protected]
On Twitter @karioakes
NEW YORK – A middle-aged patient with Fitzpatrick type V skin comes to the office with a 10-year history of “breakouts” on her face. When asked about topical treatments, she reports that “everything burns or stings,” and says she just has very sensitive skin. What could this be?
Rosacea may often be missed in skin of color, said Dr. Alexis, speaking at the summer meeting of the American Academy of Dermatology. “It’s reportedly rare in darker skin types, especially in blacks,” and as a result, dermatologists and patients alike have a low index of suspicion for the diagnosis, he noted.
Also, rosacea looks different on darker skin than it does on lighter skin, which is featured in much of the dermatology teaching material. “In richly pigmented [Fitzpatrick] type VI skin, the erythema of rosacea can be masked,” said Dr. Alexis, chairman of the department of dermatology at Mount Sinai St. Luke’s and at Mount Sinai West, both in New York.
Dermatologists, in this case, may have to do some detective work: looking at the distribution of the lesions, thinking about trigger factors from the patient history, and noting the lack of comedones – although the patient has “pimples.” Patient complaints that they are sensitive to almost all topical products and experience stinging with “everything” is another very good clue that the patient may have rosacea.
Keep rosacea on the differential for this picture, advised Dr. Alexis. In skin of color, “rosacea may not be as rare as previously thought – less common, maybe – but not rare.”
Dr. Alexis reported financial relationships with multiple pharmaceutical companies.
[email protected]
On Twitter @karioakes
NEW YORK – A middle-aged patient with Fitzpatrick type V skin comes to the office with a 10-year history of “breakouts” on her face. When asked about topical treatments, she reports that “everything burns or stings,” and says she just has very sensitive skin. What could this be?
Rosacea may often be missed in skin of color, said Dr. Alexis, speaking at the summer meeting of the American Academy of Dermatology. “It’s reportedly rare in darker skin types, especially in blacks,” and as a result, dermatologists and patients alike have a low index of suspicion for the diagnosis, he noted.
Also, rosacea looks different on darker skin than it does on lighter skin, which is featured in much of the dermatology teaching material. “In richly pigmented [Fitzpatrick] type VI skin, the erythema of rosacea can be masked,” said Dr. Alexis, chairman of the department of dermatology at Mount Sinai St. Luke’s and at Mount Sinai West, both in New York.
Dermatologists, in this case, may have to do some detective work: looking at the distribution of the lesions, thinking about trigger factors from the patient history, and noting the lack of comedones – although the patient has “pimples.” Patient complaints that they are sensitive to almost all topical products and experience stinging with “everything” is another very good clue that the patient may have rosacea.
Keep rosacea on the differential for this picture, advised Dr. Alexis. In skin of color, “rosacea may not be as rare as previously thought – less common, maybe – but not rare.”
Dr. Alexis reported financial relationships with multiple pharmaceutical companies.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM THE 2017 AAD SUMMER MEETING
Acne-associated hyperpigmentation an important consideration in patients with skin of color
NEW YORK – When treating patients with skin of color for acne, treatment goals may vary from those of patients with lighter skin, according to Andrew F. Alexis, MD.
For example, in patients with Fitzpatrick skin types V and VI, the desired treatment outcome is not only resolution of acne, but also resolution of hyperpigmentation, said Dr. Alexis, chairman of the department of dermatology at Mount Sinai St. Luke’s and Mount Sinai West, New York, N.Y.
“Postinflammatory hyperpigmentation is often the driving force for the dermatology consult” in individuals with skin of color, Dr. Alexis said at the summer meeting of the American Academy of Dermatology. “They may be just as concerned about their dark spots as underlying acne,” he noted, citing a study that he coauthored (J Clin Aesthet Dermatol. 2014 Jul;7[7]:19-31).
In the study – a survey of patients with acne to determine which treatment outcomes were most important – 41.6% of the nonwhite female patients reported that clearance of postinflammatory hyperpigmentation was the most important goal, compared with 8.4% of white female respondents (P less than .0001).
It’s important to avoid undertreating patients, especially darker-skinned patients, where ongoing subclinical inflammation may contribute to hyperpigmentation. Even in lesions that appear grossly noninflamed, biopsies may find histological evidence of inflammation, with increased T-cell infiltration of the pilosebaceous units, Dr. Alexis said.
However, there’s always a balancing act in determining how aggressively to treat patients, he added. Dermatologists have to be aware of the risk of hypertrophic scar formation in darker-skinned individuals, especially in truncal areas.
When addressing the acne, step one is to aggressively reduce acne-associated inflammation to reduce potential sequelae. This can be done with any of a number of agents, such as retinoids, benzoyl peroxide, dapsone, azelaic acid, and even intralesional corticosteroid injections, he said.
“All agents have been considered in darker skin types,” he said, noting that “retinoids are particularly important because they can also treat postinflammatory hyperpigmentation.” Tretinoin 0.1% cream and tazarotene 0.1% cream are both good choices, he added.
Adapalene in a fixed combination with benzoyl peroxide has been studied in darker-skinned patients, with no difference in tolerability or higher incidence of pigmentary sequelae than in lighter-skinned patients, he pointed out.
Dapsone 5% and 7.5% have also been studied in patients with darker skin, and both concentrations showed comparable results for safety and efficacy.
The thinking about second-line agents can shift a bit when treating acne in darker skin. For example, azelaic acid as a 20% cream or 15% gel can be a good choice, and can be helpful in treating postinflammatory hyperpigmentation, but azelaic acid is “not as good an antiacne agent as retinoids,” Dr. Alexis said.
Patients should understand that any of these choices are primarily acne-directed treatments, to be deployed over the first 3-6 months of treatment. Then, beginning at about the 3-month mark and continuing for up to a year, hyperpigmentation can be addressed. “Really emphasize the duration of treatment,” when treating hyperpigmentation, Dr. Alexis advised.
Once the acne is under control and hyperpigmentation can be assessed on its own, dermatologists can consider whether bleaching agents are appropriate. “Should they be used? If so, how?” he asked.
Bleaching agents can be effective, said Dr. Alexis, who recommends lesion-directed rather than broad-field therapy, unless there are many larger hyperpigmented macules. “The more common scenario is smaller, more distributed lesions,” he said. “Superficial chemical peels, if used with caution, can be a good adjunct,” to bleaching agents, he added.
Coming down the road are topical nitric oxide preparations, which he said are looking good for darker skin in clinical trials.
“The key to great outcomes is to initiate a combination regimen that targets inflammation and reduces hyperpigmentation,” said Dr. Alexis. Then, he advised, minimize irritation but don’t undertreat, consider adjunctive chemical peels, and above all, “set realistic timeline expectations.”
Dr. Alexis reported financial relationships with multiple pharmaceutical companies.
[email protected]
On Twitter @karioakes
NEW YORK – When treating patients with skin of color for acne, treatment goals may vary from those of patients with lighter skin, according to Andrew F. Alexis, MD.
For example, in patients with Fitzpatrick skin types V and VI, the desired treatment outcome is not only resolution of acne, but also resolution of hyperpigmentation, said Dr. Alexis, chairman of the department of dermatology at Mount Sinai St. Luke’s and Mount Sinai West, New York, N.Y.
“Postinflammatory hyperpigmentation is often the driving force for the dermatology consult” in individuals with skin of color, Dr. Alexis said at the summer meeting of the American Academy of Dermatology. “They may be just as concerned about their dark spots as underlying acne,” he noted, citing a study that he coauthored (J Clin Aesthet Dermatol. 2014 Jul;7[7]:19-31).
In the study – a survey of patients with acne to determine which treatment outcomes were most important – 41.6% of the nonwhite female patients reported that clearance of postinflammatory hyperpigmentation was the most important goal, compared with 8.4% of white female respondents (P less than .0001).
It’s important to avoid undertreating patients, especially darker-skinned patients, where ongoing subclinical inflammation may contribute to hyperpigmentation. Even in lesions that appear grossly noninflamed, biopsies may find histological evidence of inflammation, with increased T-cell infiltration of the pilosebaceous units, Dr. Alexis said.
However, there’s always a balancing act in determining how aggressively to treat patients, he added. Dermatologists have to be aware of the risk of hypertrophic scar formation in darker-skinned individuals, especially in truncal areas.
When addressing the acne, step one is to aggressively reduce acne-associated inflammation to reduce potential sequelae. This can be done with any of a number of agents, such as retinoids, benzoyl peroxide, dapsone, azelaic acid, and even intralesional corticosteroid injections, he said.
“All agents have been considered in darker skin types,” he said, noting that “retinoids are particularly important because they can also treat postinflammatory hyperpigmentation.” Tretinoin 0.1% cream and tazarotene 0.1% cream are both good choices, he added.
Adapalene in a fixed combination with benzoyl peroxide has been studied in darker-skinned patients, with no difference in tolerability or higher incidence of pigmentary sequelae than in lighter-skinned patients, he pointed out.
Dapsone 5% and 7.5% have also been studied in patients with darker skin, and both concentrations showed comparable results for safety and efficacy.
The thinking about second-line agents can shift a bit when treating acne in darker skin. For example, azelaic acid as a 20% cream or 15% gel can be a good choice, and can be helpful in treating postinflammatory hyperpigmentation, but azelaic acid is “not as good an antiacne agent as retinoids,” Dr. Alexis said.
Patients should understand that any of these choices are primarily acne-directed treatments, to be deployed over the first 3-6 months of treatment. Then, beginning at about the 3-month mark and continuing for up to a year, hyperpigmentation can be addressed. “Really emphasize the duration of treatment,” when treating hyperpigmentation, Dr. Alexis advised.
Once the acne is under control and hyperpigmentation can be assessed on its own, dermatologists can consider whether bleaching agents are appropriate. “Should they be used? If so, how?” he asked.
Bleaching agents can be effective, said Dr. Alexis, who recommends lesion-directed rather than broad-field therapy, unless there are many larger hyperpigmented macules. “The more common scenario is smaller, more distributed lesions,” he said. “Superficial chemical peels, if used with caution, can be a good adjunct,” to bleaching agents, he added.
Coming down the road are topical nitric oxide preparations, which he said are looking good for darker skin in clinical trials.
“The key to great outcomes is to initiate a combination regimen that targets inflammation and reduces hyperpigmentation,” said Dr. Alexis. Then, he advised, minimize irritation but don’t undertreat, consider adjunctive chemical peels, and above all, “set realistic timeline expectations.”
Dr. Alexis reported financial relationships with multiple pharmaceutical companies.
[email protected]
On Twitter @karioakes
NEW YORK – When treating patients with skin of color for acne, treatment goals may vary from those of patients with lighter skin, according to Andrew F. Alexis, MD.
For example, in patients with Fitzpatrick skin types V and VI, the desired treatment outcome is not only resolution of acne, but also resolution of hyperpigmentation, said Dr. Alexis, chairman of the department of dermatology at Mount Sinai St. Luke’s and Mount Sinai West, New York, N.Y.
“Postinflammatory hyperpigmentation is often the driving force for the dermatology consult” in individuals with skin of color, Dr. Alexis said at the summer meeting of the American Academy of Dermatology. “They may be just as concerned about their dark spots as underlying acne,” he noted, citing a study that he coauthored (J Clin Aesthet Dermatol. 2014 Jul;7[7]:19-31).
In the study – a survey of patients with acne to determine which treatment outcomes were most important – 41.6% of the nonwhite female patients reported that clearance of postinflammatory hyperpigmentation was the most important goal, compared with 8.4% of white female respondents (P less than .0001).
It’s important to avoid undertreating patients, especially darker-skinned patients, where ongoing subclinical inflammation may contribute to hyperpigmentation. Even in lesions that appear grossly noninflamed, biopsies may find histological evidence of inflammation, with increased T-cell infiltration of the pilosebaceous units, Dr. Alexis said.
However, there’s always a balancing act in determining how aggressively to treat patients, he added. Dermatologists have to be aware of the risk of hypertrophic scar formation in darker-skinned individuals, especially in truncal areas.
When addressing the acne, step one is to aggressively reduce acne-associated inflammation to reduce potential sequelae. This can be done with any of a number of agents, such as retinoids, benzoyl peroxide, dapsone, azelaic acid, and even intralesional corticosteroid injections, he said.
“All agents have been considered in darker skin types,” he said, noting that “retinoids are particularly important because they can also treat postinflammatory hyperpigmentation.” Tretinoin 0.1% cream and tazarotene 0.1% cream are both good choices, he added.
Adapalene in a fixed combination with benzoyl peroxide has been studied in darker-skinned patients, with no difference in tolerability or higher incidence of pigmentary sequelae than in lighter-skinned patients, he pointed out.
Dapsone 5% and 7.5% have also been studied in patients with darker skin, and both concentrations showed comparable results for safety and efficacy.
The thinking about second-line agents can shift a bit when treating acne in darker skin. For example, azelaic acid as a 20% cream or 15% gel can be a good choice, and can be helpful in treating postinflammatory hyperpigmentation, but azelaic acid is “not as good an antiacne agent as retinoids,” Dr. Alexis said.
Patients should understand that any of these choices are primarily acne-directed treatments, to be deployed over the first 3-6 months of treatment. Then, beginning at about the 3-month mark and continuing for up to a year, hyperpigmentation can be addressed. “Really emphasize the duration of treatment,” when treating hyperpigmentation, Dr. Alexis advised.
Once the acne is under control and hyperpigmentation can be assessed on its own, dermatologists can consider whether bleaching agents are appropriate. “Should they be used? If so, how?” he asked.
Bleaching agents can be effective, said Dr. Alexis, who recommends lesion-directed rather than broad-field therapy, unless there are many larger hyperpigmented macules. “The more common scenario is smaller, more distributed lesions,” he said. “Superficial chemical peels, if used with caution, can be a good adjunct,” to bleaching agents, he added.
Coming down the road are topical nitric oxide preparations, which he said are looking good for darker skin in clinical trials.
“The key to great outcomes is to initiate a combination regimen that targets inflammation and reduces hyperpigmentation,” said Dr. Alexis. Then, he advised, minimize irritation but don’t undertreat, consider adjunctive chemical peels, and above all, “set realistic timeline expectations.”
Dr. Alexis reported financial relationships with multiple pharmaceutical companies.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM THE 2017 SUMMER AAD MEETING
Screening MRI misses Sturge-Weber in babies with port-wine stain
CHICAGO – Screening infants with a port-wine stain for Sturge-Weber syndrome (SWS) with a magnetic resonance imaging brain scan had a 23% false-negative rate and actually delayed seizure detection, according to a recent study.
When infants with port-wine stains receive a dermatology consult, they may also be screened for SWS by means of MRI and by electroencephalography, particularly if their lesion phenotype puts them at higher risk for SWS. But the accuracy and benefit of the screenings has not been well established, said Michaela Zallmann, MD, the study’s first author. Hemifacial lesions that involve both the forehead and cheek and median lesions that are centered around the facial midline are both considered high-risk lesions.
Dr. Zallmann, a dermatologist at Monash University and the Royal Children’s Hospital, Melbourne, and her coinvestigators examined data on 126 patients with facial port-wine stains who came to a laser clinic over a 12-month period. Of these, 32 (25.4%) had a high-risk port-wine stain, and 9 of those 32 (28.1%) had a capillary-venous malformation characteristic of SWS. Of the high-risk patients, 14 received a screening MRI or EEG before having had a first seizure. Of those 14 scans, 1 resulted in a diagnosis of SWS; of the 13 patients with a negative MRI screen, 3 (23.1%) were later found to have SWS when their parents or caregivers detected seizures. Thus, a total of four of the high-risk infants who were screened eventually were diagnosed with SWS.
Of the 18 high-risk patients who did not receive a screening MRI, 3 (16.7%) developed seizures, while 2 (11.1%) were seizure free but developed glaucoma severe enough to require treatment. One patient who was also seizure free developed an autism spectrum disorder.
Two patients who were in the high-risk group received screening EEGs that detected abnormalities that were not yet clinically evident. These included sub-clinical seizures and posterior-quadrant focal slowing. Both of these patients had initial negative screening MRIs.
Scanning early in life, using inappropriate imaging protocols, and having an inexperienced radiologist were all factors associated with a higher probability of false negative screening MRI, according to the researchers’ analysis, which was presented in a poster session at the World Congress of Pediatric Dermatology.
All of the false negative MRIs in the study cohort were conducted in infants younger than 9 weeks old. But whether it is useful to reserve imaging for later in infancy is debatable. “While later imaging may have improved sensitivity, 75% of infants with SWS will have already had their first seizure by 12 months of age,” wrote Dr. Zallmann and her colleagues.
Of the infants involved in the study, two of the three patients with false negative scans did not receive a referral to a neurologist, nor did their parents receive seizure education. “False reassurance may delay seizure detection,” Dr. Zallmann said.
For infants with positive MRIs who went on to develop seizures, the mean age of when they experienced their first documented seizure was 10 weeks. For those who did not receive an MRI, the mean age was 14 months, compared with 28 months for patients who had received a false negative MRI.
In discussing the findings, Dr. Zallmann and her colleagues made the point that early referral to a pediatric neurologist is important, especially for infants with the higher-risk port-wine stain patterns of hemifacial and median lesions. Seizure education can help parents detect the often subtle signs of seizures in infants with SWS, which can include staring spells, subtle limb twitching, and lip smacking.
The fact that seizures were detected an average of 14 months later in patients with negative screening MRIs may mean that such subtle signs were missed. “False reassurance may delay the recognition and treatment of seizures and impact neurodevelopmental outcomes,” Dr. Zallmann and her colleagues wrote in the abstract that accompanied the poster.
The study, while small, helps fill in some knowledge gaps, the researchers pointed out; they noted that there is no consensus on what level or type of facial involvement warrants screening, which protocols are best for MRI and EEG, or even whether the screening will improve seizure detection or outcomes.
“Currently there is no evidence that screening improves neurodevelopmental outcomes,” they said. “Conversely, there is a role for early neurological referral, symptom education, and potentially of EEGs in the prevention of complications related to SWS.”
Dr. Zallmann reported no conflicts of interest.
[email protected]
On Twitter @karioakes
CHICAGO – Screening infants with a port-wine stain for Sturge-Weber syndrome (SWS) with a magnetic resonance imaging brain scan had a 23% false-negative rate and actually delayed seizure detection, according to a recent study.
When infants with port-wine stains receive a dermatology consult, they may also be screened for SWS by means of MRI and by electroencephalography, particularly if their lesion phenotype puts them at higher risk for SWS. But the accuracy and benefit of the screenings has not been well established, said Michaela Zallmann, MD, the study’s first author. Hemifacial lesions that involve both the forehead and cheek and median lesions that are centered around the facial midline are both considered high-risk lesions.
Dr. Zallmann, a dermatologist at Monash University and the Royal Children’s Hospital, Melbourne, and her coinvestigators examined data on 126 patients with facial port-wine stains who came to a laser clinic over a 12-month period. Of these, 32 (25.4%) had a high-risk port-wine stain, and 9 of those 32 (28.1%) had a capillary-venous malformation characteristic of SWS. Of the high-risk patients, 14 received a screening MRI or EEG before having had a first seizure. Of those 14 scans, 1 resulted in a diagnosis of SWS; of the 13 patients with a negative MRI screen, 3 (23.1%) were later found to have SWS when their parents or caregivers detected seizures. Thus, a total of four of the high-risk infants who were screened eventually were diagnosed with SWS.
Of the 18 high-risk patients who did not receive a screening MRI, 3 (16.7%) developed seizures, while 2 (11.1%) were seizure free but developed glaucoma severe enough to require treatment. One patient who was also seizure free developed an autism spectrum disorder.
Two patients who were in the high-risk group received screening EEGs that detected abnormalities that were not yet clinically evident. These included sub-clinical seizures and posterior-quadrant focal slowing. Both of these patients had initial negative screening MRIs.
Scanning early in life, using inappropriate imaging protocols, and having an inexperienced radiologist were all factors associated with a higher probability of false negative screening MRI, according to the researchers’ analysis, which was presented in a poster session at the World Congress of Pediatric Dermatology.
All of the false negative MRIs in the study cohort were conducted in infants younger than 9 weeks old. But whether it is useful to reserve imaging for later in infancy is debatable. “While later imaging may have improved sensitivity, 75% of infants with SWS will have already had their first seizure by 12 months of age,” wrote Dr. Zallmann and her colleagues.
Of the infants involved in the study, two of the three patients with false negative scans did not receive a referral to a neurologist, nor did their parents receive seizure education. “False reassurance may delay seizure detection,” Dr. Zallmann said.
For infants with positive MRIs who went on to develop seizures, the mean age of when they experienced their first documented seizure was 10 weeks. For those who did not receive an MRI, the mean age was 14 months, compared with 28 months for patients who had received a false negative MRI.
In discussing the findings, Dr. Zallmann and her colleagues made the point that early referral to a pediatric neurologist is important, especially for infants with the higher-risk port-wine stain patterns of hemifacial and median lesions. Seizure education can help parents detect the often subtle signs of seizures in infants with SWS, which can include staring spells, subtle limb twitching, and lip smacking.
The fact that seizures were detected an average of 14 months later in patients with negative screening MRIs may mean that such subtle signs were missed. “False reassurance may delay the recognition and treatment of seizures and impact neurodevelopmental outcomes,” Dr. Zallmann and her colleagues wrote in the abstract that accompanied the poster.
The study, while small, helps fill in some knowledge gaps, the researchers pointed out; they noted that there is no consensus on what level or type of facial involvement warrants screening, which protocols are best for MRI and EEG, or even whether the screening will improve seizure detection or outcomes.
“Currently there is no evidence that screening improves neurodevelopmental outcomes,” they said. “Conversely, there is a role for early neurological referral, symptom education, and potentially of EEGs in the prevention of complications related to SWS.”
Dr. Zallmann reported no conflicts of interest.
[email protected]
On Twitter @karioakes
CHICAGO – Screening infants with a port-wine stain for Sturge-Weber syndrome (SWS) with a magnetic resonance imaging brain scan had a 23% false-negative rate and actually delayed seizure detection, according to a recent study.
When infants with port-wine stains receive a dermatology consult, they may also be screened for SWS by means of MRI and by electroencephalography, particularly if their lesion phenotype puts them at higher risk for SWS. But the accuracy and benefit of the screenings has not been well established, said Michaela Zallmann, MD, the study’s first author. Hemifacial lesions that involve both the forehead and cheek and median lesions that are centered around the facial midline are both considered high-risk lesions.
Dr. Zallmann, a dermatologist at Monash University and the Royal Children’s Hospital, Melbourne, and her coinvestigators examined data on 126 patients with facial port-wine stains who came to a laser clinic over a 12-month period. Of these, 32 (25.4%) had a high-risk port-wine stain, and 9 of those 32 (28.1%) had a capillary-venous malformation characteristic of SWS. Of the high-risk patients, 14 received a screening MRI or EEG before having had a first seizure. Of those 14 scans, 1 resulted in a diagnosis of SWS; of the 13 patients with a negative MRI screen, 3 (23.1%) were later found to have SWS when their parents or caregivers detected seizures. Thus, a total of four of the high-risk infants who were screened eventually were diagnosed with SWS.
Of the 18 high-risk patients who did not receive a screening MRI, 3 (16.7%) developed seizures, while 2 (11.1%) were seizure free but developed glaucoma severe enough to require treatment. One patient who was also seizure free developed an autism spectrum disorder.
Two patients who were in the high-risk group received screening EEGs that detected abnormalities that were not yet clinically evident. These included sub-clinical seizures and posterior-quadrant focal slowing. Both of these patients had initial negative screening MRIs.
Scanning early in life, using inappropriate imaging protocols, and having an inexperienced radiologist were all factors associated with a higher probability of false negative screening MRI, according to the researchers’ analysis, which was presented in a poster session at the World Congress of Pediatric Dermatology.
All of the false negative MRIs in the study cohort were conducted in infants younger than 9 weeks old. But whether it is useful to reserve imaging for later in infancy is debatable. “While later imaging may have improved sensitivity, 75% of infants with SWS will have already had their first seizure by 12 months of age,” wrote Dr. Zallmann and her colleagues.
Of the infants involved in the study, two of the three patients with false negative scans did not receive a referral to a neurologist, nor did their parents receive seizure education. “False reassurance may delay seizure detection,” Dr. Zallmann said.
For infants with positive MRIs who went on to develop seizures, the mean age of when they experienced their first documented seizure was 10 weeks. For those who did not receive an MRI, the mean age was 14 months, compared with 28 months for patients who had received a false negative MRI.
In discussing the findings, Dr. Zallmann and her colleagues made the point that early referral to a pediatric neurologist is important, especially for infants with the higher-risk port-wine stain patterns of hemifacial and median lesions. Seizure education can help parents detect the often subtle signs of seizures in infants with SWS, which can include staring spells, subtle limb twitching, and lip smacking.
The fact that seizures were detected an average of 14 months later in patients with negative screening MRIs may mean that such subtle signs were missed. “False reassurance may delay the recognition and treatment of seizures and impact neurodevelopmental outcomes,” Dr. Zallmann and her colleagues wrote in the abstract that accompanied the poster.
The study, while small, helps fill in some knowledge gaps, the researchers pointed out; they noted that there is no consensus on what level or type of facial involvement warrants screening, which protocols are best for MRI and EEG, or even whether the screening will improve seizure detection or outcomes.
“Currently there is no evidence that screening improves neurodevelopmental outcomes,” they said. “Conversely, there is a role for early neurological referral, symptom education, and potentially of EEGs in the prevention of complications related to SWS.”
Dr. Zallmann reported no conflicts of interest.
[email protected]
On Twitter @karioakes
AT WCPD 2017
Key clinical point:
Major finding: Magnetic resonance imaging screening for Sturge-Weber syndrome resulted in a 23.2% false negative rate in babies with port-wine stain.
Data source: A review of screening and outcomes for 126 infants with port-wine stain seen in a laser clinic over a 12-month period. Disclosures: The lead author reported no disclosures.
Alopecia may be permanent in one in four pediatric HSCT patients
CHICAGO – Late dermatologic manifestations in children who have received hematopoietic stem cell transplants may be more common than previously thought, according to results of a new study.
Johanna Song, MD, and her collaborators reported that, in their prospective pediatric study, 25% of patients had permanent alopecia and 16% had psoriasis, noting that late nonmalignant skin effects of hematopoietic stem cell transplantation (HSCT) have been studied primarily retrospectively, and in adults. Vitiligo and nail changes were also seen.
In a poster presentation at the World Congress of Dermatology, Dr. Song and her colleagues noted that these figures are higher than the previously reported pediatric rates of 1.7% for vitiligo and 15.6% for permanent alopecia. “Early recognition of these late effects can facilitate prompt and appropriate treatment, if desired,” they said.
The single-center, cross-sectional cohort study tracked pediatric patients over an 18-month period and included patients who were at least 1 year post allogeneic HSCT and had not relapsed. Patients who were not English speaking were excluded.
The median age of the 85 patients enrolled in the study was 13.8 years, and participants were a median of 3.6 years post transplant at the time of enrollment. The study’s analysis attempted to determine which patient, transplant, and disease factors might be associated with the late nonmalignant skin changes, according to Dr. Song, a resident dermatologist at Harvard University, Boston, and her colleagues.
Most – 52– of the patients (61.2%) had hematologic malignancies; 12 patients (14.1%) received their transplant for bone marrow failure, and 11 patients (12.5%) had immunodeficiency. Three patients (3.5%) received HSCT for other malignancies, and seven (8.2%) for nonmalignant diseases.
Diffuse hair thinning was seen in 13 (62%) of the 21 patients who had alopecia, while 11 (52%) of the patients with alopecia had an androgenetic hair loss pattern. Chronic graft versus host disease (GVHD), skin chronic GVHD, a HSCT regimen that included busulfan conditioning, and a family history of early male-pattern alopecia were all significantly associated with post-HSCT permanent alopecia (P less than .05 for all).
The patients with androgenetic alopecia may be experiencing an accelerated time course of a condition to which they are already genetically disposed, noted Dr. Song and her colleagues.
Psoriasis was commonly seen on the scalp, affecting 11 of the 14 patients with psoriasis (79%), and involved the face in five of the patients (36%). Just one patient had psoriasis elsewhere on the body. There was a nonsignificant trend towards human leukocyte antigen mismatch among patients who had psoriasis. Although “psoriasis may be a marker of persistent immune dysregulation,” the investigators said, they did not identify any associated risk factors that would point toward this mechanism in their analysis.
Twelve patients (14%) had vitiligo, with halo nevi seen in four of these patients. Children who were younger than age 10 years and those who received their transplant for primary immunodeficiency were significantly more likely to have vitiligo (P less than .05 for both). Specific possible mechanisms triggering vitiligo could include thymic dysfunction resulting in loss of self-tolerance, and donor alloreactivity against the patient’s host antigens, according to the authors.
Nail changes such as pterygium and nail pitting, ridging, or thickening were seen in just five patients, all of whom had chronic GVHD of the skin. “Nail changes are likely a result of persistent inflammation and immune dysregulation from chronic GVHD,” said Dr. Song.
These late effects “can significantly impact patients’ quality of life,” according to the authors, who called for larger studies that follow pediatric HSCT patients longitudinally, beginning before the transplant – and for more investigation into the pathogenesis of specific late effects.
Dr. Song reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
CHICAGO – Late dermatologic manifestations in children who have received hematopoietic stem cell transplants may be more common than previously thought, according to results of a new study.
Johanna Song, MD, and her collaborators reported that, in their prospective pediatric study, 25% of patients had permanent alopecia and 16% had psoriasis, noting that late nonmalignant skin effects of hematopoietic stem cell transplantation (HSCT) have been studied primarily retrospectively, and in adults. Vitiligo and nail changes were also seen.
In a poster presentation at the World Congress of Dermatology, Dr. Song and her colleagues noted that these figures are higher than the previously reported pediatric rates of 1.7% for vitiligo and 15.6% for permanent alopecia. “Early recognition of these late effects can facilitate prompt and appropriate treatment, if desired,” they said.
The single-center, cross-sectional cohort study tracked pediatric patients over an 18-month period and included patients who were at least 1 year post allogeneic HSCT and had not relapsed. Patients who were not English speaking were excluded.
The median age of the 85 patients enrolled in the study was 13.8 years, and participants were a median of 3.6 years post transplant at the time of enrollment. The study’s analysis attempted to determine which patient, transplant, and disease factors might be associated with the late nonmalignant skin changes, according to Dr. Song, a resident dermatologist at Harvard University, Boston, and her colleagues.
Most – 52– of the patients (61.2%) had hematologic malignancies; 12 patients (14.1%) received their transplant for bone marrow failure, and 11 patients (12.5%) had immunodeficiency. Three patients (3.5%) received HSCT for other malignancies, and seven (8.2%) for nonmalignant diseases.
Diffuse hair thinning was seen in 13 (62%) of the 21 patients who had alopecia, while 11 (52%) of the patients with alopecia had an androgenetic hair loss pattern. Chronic graft versus host disease (GVHD), skin chronic GVHD, a HSCT regimen that included busulfan conditioning, and a family history of early male-pattern alopecia were all significantly associated with post-HSCT permanent alopecia (P less than .05 for all).
The patients with androgenetic alopecia may be experiencing an accelerated time course of a condition to which they are already genetically disposed, noted Dr. Song and her colleagues.
Psoriasis was commonly seen on the scalp, affecting 11 of the 14 patients with psoriasis (79%), and involved the face in five of the patients (36%). Just one patient had psoriasis elsewhere on the body. There was a nonsignificant trend towards human leukocyte antigen mismatch among patients who had psoriasis. Although “psoriasis may be a marker of persistent immune dysregulation,” the investigators said, they did not identify any associated risk factors that would point toward this mechanism in their analysis.
Twelve patients (14%) had vitiligo, with halo nevi seen in four of these patients. Children who were younger than age 10 years and those who received their transplant for primary immunodeficiency were significantly more likely to have vitiligo (P less than .05 for both). Specific possible mechanisms triggering vitiligo could include thymic dysfunction resulting in loss of self-tolerance, and donor alloreactivity against the patient’s host antigens, according to the authors.
Nail changes such as pterygium and nail pitting, ridging, or thickening were seen in just five patients, all of whom had chronic GVHD of the skin. “Nail changes are likely a result of persistent inflammation and immune dysregulation from chronic GVHD,” said Dr. Song.
These late effects “can significantly impact patients’ quality of life,” according to the authors, who called for larger studies that follow pediatric HSCT patients longitudinally, beginning before the transplant – and for more investigation into the pathogenesis of specific late effects.
Dr. Song reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
CHICAGO – Late dermatologic manifestations in children who have received hematopoietic stem cell transplants may be more common than previously thought, according to results of a new study.
Johanna Song, MD, and her collaborators reported that, in their prospective pediatric study, 25% of patients had permanent alopecia and 16% had psoriasis, noting that late nonmalignant skin effects of hematopoietic stem cell transplantation (HSCT) have been studied primarily retrospectively, and in adults. Vitiligo and nail changes were also seen.
In a poster presentation at the World Congress of Dermatology, Dr. Song and her colleagues noted that these figures are higher than the previously reported pediatric rates of 1.7% for vitiligo and 15.6% for permanent alopecia. “Early recognition of these late effects can facilitate prompt and appropriate treatment, if desired,” they said.
The single-center, cross-sectional cohort study tracked pediatric patients over an 18-month period and included patients who were at least 1 year post allogeneic HSCT and had not relapsed. Patients who were not English speaking were excluded.
The median age of the 85 patients enrolled in the study was 13.8 years, and participants were a median of 3.6 years post transplant at the time of enrollment. The study’s analysis attempted to determine which patient, transplant, and disease factors might be associated with the late nonmalignant skin changes, according to Dr. Song, a resident dermatologist at Harvard University, Boston, and her colleagues.
Most – 52– of the patients (61.2%) had hematologic malignancies; 12 patients (14.1%) received their transplant for bone marrow failure, and 11 patients (12.5%) had immunodeficiency. Three patients (3.5%) received HSCT for other malignancies, and seven (8.2%) for nonmalignant diseases.
Diffuse hair thinning was seen in 13 (62%) of the 21 patients who had alopecia, while 11 (52%) of the patients with alopecia had an androgenetic hair loss pattern. Chronic graft versus host disease (GVHD), skin chronic GVHD, a HSCT regimen that included busulfan conditioning, and a family history of early male-pattern alopecia were all significantly associated with post-HSCT permanent alopecia (P less than .05 for all).
The patients with androgenetic alopecia may be experiencing an accelerated time course of a condition to which they are already genetically disposed, noted Dr. Song and her colleagues.
Psoriasis was commonly seen on the scalp, affecting 11 of the 14 patients with psoriasis (79%), and involved the face in five of the patients (36%). Just one patient had psoriasis elsewhere on the body. There was a nonsignificant trend towards human leukocyte antigen mismatch among patients who had psoriasis. Although “psoriasis may be a marker of persistent immune dysregulation,” the investigators said, they did not identify any associated risk factors that would point toward this mechanism in their analysis.
Twelve patients (14%) had vitiligo, with halo nevi seen in four of these patients. Children who were younger than age 10 years and those who received their transplant for primary immunodeficiency were significantly more likely to have vitiligo (P less than .05 for both). Specific possible mechanisms triggering vitiligo could include thymic dysfunction resulting in loss of self-tolerance, and donor alloreactivity against the patient’s host antigens, according to the authors.
Nail changes such as pterygium and nail pitting, ridging, or thickening were seen in just five patients, all of whom had chronic GVHD of the skin. “Nail changes are likely a result of persistent inflammation and immune dysregulation from chronic GVHD,” said Dr. Song.
These late effects “can significantly impact patients’ quality of life,” according to the authors, who called for larger studies that follow pediatric HSCT patients longitudinally, beginning before the transplant – and for more investigation into the pathogenesis of specific late effects.
Dr. Song reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
AT WCPD 2017
Key clinical point:
Major finding: Permanent alopecia was seen in 25% of patients, and 16% had psoriasis a median of 3.6 years after transplant.
Data source: A single-center prospective study of 85 children in routine post-HSCT follow-up.
Disclosures: Dr. Song reported no conflicts of interest.
What’s on the dermatopathologist’s wish list
NEW YORK – If dermatopathologists had a wish list they could give their dermatologist colleagues, what might it include? High up on the list for many, said Robert Phelps, MD, might be to have them share the clinical picture, treat the specimen gently, and give the best landmarks possible.
Speaking at the summer meeting of the American Academy of Dermatology, Dr. Phelps, director of the dermatopathology service at Mount Sinai Medical Center in New York, led off the dermatopathologist-run session – appropriately titled “Help Me Help You” – by asking, “How can the clinician provide the optimal biopsy?”
It’s always helpful to have as much clinical information as possible, said Dr. Phelps, whose discussion focused on tips for neoplastic lesions. This might include prior history of malignancy, autoimmune disease, pathergy, or other relevant medical history, but clinical pictures can also be a big help, although there can be technical and patient privacy issues to overcome, he noted. If, for example, a larger lesion or rash is being biopsied rather than excised, it can be very helpful to see the larger field and full area of distribution of the lesion in question. Submitting multiple specimens for rashes and larger lesions is always a good idea too, he added.
Although curettage can be a great way to biopsy – and perhaps even definitively treat some lesions – problems can arise on the dermatopathologist’s side when melanocytic lesions are curetted for biopsy, according to Dr. Phelps, a practicing dermatologist and a dermatopathologist. “By virtue of the force of the biopsy, the specimen is often fragmented, and histology can be distorted,” he said. One element of that distortion can be that melanocytes can appear to be free floating, which is a problem. “Dyshesion of melanocytes is usually an indication of atypia … It is an important histologic clue as to the possibility of a malignancy supervening.”
These factors can make it tough for a dermatopathologist to make an accurate call. “If there are free-floating melanocytes from a curetted specimen, I can’t rule out invasive melanoma,” explained Dr. Phelps, since he can’t tell if he is seeing true atypia or disruption that’s an artifact of the collection technique.
In this instance, he said, a dermatopathologist would be “obligated to overcall, because one couldn’t really determine the pathology.” The bottom line? “Don’t curette biopsies of melanocytic lesions.”
Another technique that can interfere with the ability to read a tissue specimen accurately is electrodesiccation. Although it’s often performed in conjunction with curettage, electrodesiccation can cause changes in tissue consistent with thermal injury. “Essentially, the tissue has been burned,” Dr. Phelps pointed out. This can result in a characteristic streaming pattern of nuclei, and the dermis can acquire a “peculiar homogenized appearance,” he said.
Although electrodesiccation can be a useful technique to make sure margins are controlled, “when you do this, just be aware that the interpretation is difficult,” he noted. “It’s difficult to tell where the margins are and if they are the appropriate and correct margins,” he said.
When possible, try to avoid squeezing the tumor, Dr. Phelps advised. Excessive pressure on the specimen can distort cell architecture and make pathological diagnosis really challenging, particularly in lymphoid tumors, he said.
“Often, the tumor is not recognizable,” he added. Crush artifact can result in an appearance of small bluish clumps and smearing of collagen fibers. The effect, he said, can be particularly pronounced with small cell carcinoma and lymphoma, and with rapidly proliferating tumors.
Dr. Phelps said that during his training, he was taught not to use forceps to extract a stubborn punch biopsy specimen; rather, he was trained to use a needle to tease out the specimen. Fear of a self-inflicted needle stick with this technique may be a deterrent, he acknowledged. If forceps are used, he suggested being as gentle as possible and using the finest forceps available.
When pathologists receive an intact excised lesion – one not obtained using a Mohs technique, “delineation of the margin is essential,” Dr. Phelps said. Further, accurate mapping is critical to helping the examiner understand the anatomic orientation of the specimen, a key prerequisite that enables accurate communication from the dermatopathologist back to the clinician if there’s a question regarding the need for retreatment, he added.
For an elliptical excision, ideally, both poles of the ellipse would be suture-tagged, and at least one tag is essential, he said. Then superior and inferior borders can be inked with contrasting colors, and the epidermal borders of the lesion should be marked as well. When the specimen is submitted, it should be accompanied by an accurate map that clearly indicates the coding for medial, lateral, inferior, and superior aspects of the specimen. “Always prepare a specimen diagram for oriented specimens,” Dr. Phelps noted.
Don’t forget to make sure that the left-right orientation on the diagram corresponds to the specimen’s orientation on the patient, he added. Some facilities use a clock face system to indicate orientation and positioning, which may be the clearest method of all.
Sometimes, it’s difficult for the dermatopathologist to visualize whether the specimen is aligned in true medial-lateral fashion, or along skin tension lines, which tend to run diagonally, so “the more clinical information, the better,” he said. “With good mapping, precise retreatment can be optimal,” he said.
Dr. Phelps reported that he had no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
NEW YORK – If dermatopathologists had a wish list they could give their dermatologist colleagues, what might it include? High up on the list for many, said Robert Phelps, MD, might be to have them share the clinical picture, treat the specimen gently, and give the best landmarks possible.
Speaking at the summer meeting of the American Academy of Dermatology, Dr. Phelps, director of the dermatopathology service at Mount Sinai Medical Center in New York, led off the dermatopathologist-run session – appropriately titled “Help Me Help You” – by asking, “How can the clinician provide the optimal biopsy?”
It’s always helpful to have as much clinical information as possible, said Dr. Phelps, whose discussion focused on tips for neoplastic lesions. This might include prior history of malignancy, autoimmune disease, pathergy, or other relevant medical history, but clinical pictures can also be a big help, although there can be technical and patient privacy issues to overcome, he noted. If, for example, a larger lesion or rash is being biopsied rather than excised, it can be very helpful to see the larger field and full area of distribution of the lesion in question. Submitting multiple specimens for rashes and larger lesions is always a good idea too, he added.
Although curettage can be a great way to biopsy – and perhaps even definitively treat some lesions – problems can arise on the dermatopathologist’s side when melanocytic lesions are curetted for biopsy, according to Dr. Phelps, a practicing dermatologist and a dermatopathologist. “By virtue of the force of the biopsy, the specimen is often fragmented, and histology can be distorted,” he said. One element of that distortion can be that melanocytes can appear to be free floating, which is a problem. “Dyshesion of melanocytes is usually an indication of atypia … It is an important histologic clue as to the possibility of a malignancy supervening.”
These factors can make it tough for a dermatopathologist to make an accurate call. “If there are free-floating melanocytes from a curetted specimen, I can’t rule out invasive melanoma,” explained Dr. Phelps, since he can’t tell if he is seeing true atypia or disruption that’s an artifact of the collection technique.
In this instance, he said, a dermatopathologist would be “obligated to overcall, because one couldn’t really determine the pathology.” The bottom line? “Don’t curette biopsies of melanocytic lesions.”
Another technique that can interfere with the ability to read a tissue specimen accurately is electrodesiccation. Although it’s often performed in conjunction with curettage, electrodesiccation can cause changes in tissue consistent with thermal injury. “Essentially, the tissue has been burned,” Dr. Phelps pointed out. This can result in a characteristic streaming pattern of nuclei, and the dermis can acquire a “peculiar homogenized appearance,” he said.
Although electrodesiccation can be a useful technique to make sure margins are controlled, “when you do this, just be aware that the interpretation is difficult,” he noted. “It’s difficult to tell where the margins are and if they are the appropriate and correct margins,” he said.
When possible, try to avoid squeezing the tumor, Dr. Phelps advised. Excessive pressure on the specimen can distort cell architecture and make pathological diagnosis really challenging, particularly in lymphoid tumors, he said.
“Often, the tumor is not recognizable,” he added. Crush artifact can result in an appearance of small bluish clumps and smearing of collagen fibers. The effect, he said, can be particularly pronounced with small cell carcinoma and lymphoma, and with rapidly proliferating tumors.
Dr. Phelps said that during his training, he was taught not to use forceps to extract a stubborn punch biopsy specimen; rather, he was trained to use a needle to tease out the specimen. Fear of a self-inflicted needle stick with this technique may be a deterrent, he acknowledged. If forceps are used, he suggested being as gentle as possible and using the finest forceps available.
When pathologists receive an intact excised lesion – one not obtained using a Mohs technique, “delineation of the margin is essential,” Dr. Phelps said. Further, accurate mapping is critical to helping the examiner understand the anatomic orientation of the specimen, a key prerequisite that enables accurate communication from the dermatopathologist back to the clinician if there’s a question regarding the need for retreatment, he added.
For an elliptical excision, ideally, both poles of the ellipse would be suture-tagged, and at least one tag is essential, he said. Then superior and inferior borders can be inked with contrasting colors, and the epidermal borders of the lesion should be marked as well. When the specimen is submitted, it should be accompanied by an accurate map that clearly indicates the coding for medial, lateral, inferior, and superior aspects of the specimen. “Always prepare a specimen diagram for oriented specimens,” Dr. Phelps noted.
Don’t forget to make sure that the left-right orientation on the diagram corresponds to the specimen’s orientation on the patient, he added. Some facilities use a clock face system to indicate orientation and positioning, which may be the clearest method of all.
Sometimes, it’s difficult for the dermatopathologist to visualize whether the specimen is aligned in true medial-lateral fashion, or along skin tension lines, which tend to run diagonally, so “the more clinical information, the better,” he said. “With good mapping, precise retreatment can be optimal,” he said.
Dr. Phelps reported that he had no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
NEW YORK – If dermatopathologists had a wish list they could give their dermatologist colleagues, what might it include? High up on the list for many, said Robert Phelps, MD, might be to have them share the clinical picture, treat the specimen gently, and give the best landmarks possible.
Speaking at the summer meeting of the American Academy of Dermatology, Dr. Phelps, director of the dermatopathology service at Mount Sinai Medical Center in New York, led off the dermatopathologist-run session – appropriately titled “Help Me Help You” – by asking, “How can the clinician provide the optimal biopsy?”
It’s always helpful to have as much clinical information as possible, said Dr. Phelps, whose discussion focused on tips for neoplastic lesions. This might include prior history of malignancy, autoimmune disease, pathergy, or other relevant medical history, but clinical pictures can also be a big help, although there can be technical and patient privacy issues to overcome, he noted. If, for example, a larger lesion or rash is being biopsied rather than excised, it can be very helpful to see the larger field and full area of distribution of the lesion in question. Submitting multiple specimens for rashes and larger lesions is always a good idea too, he added.
Although curettage can be a great way to biopsy – and perhaps even definitively treat some lesions – problems can arise on the dermatopathologist’s side when melanocytic lesions are curetted for biopsy, according to Dr. Phelps, a practicing dermatologist and a dermatopathologist. “By virtue of the force of the biopsy, the specimen is often fragmented, and histology can be distorted,” he said. One element of that distortion can be that melanocytes can appear to be free floating, which is a problem. “Dyshesion of melanocytes is usually an indication of atypia … It is an important histologic clue as to the possibility of a malignancy supervening.”
These factors can make it tough for a dermatopathologist to make an accurate call. “If there are free-floating melanocytes from a curetted specimen, I can’t rule out invasive melanoma,” explained Dr. Phelps, since he can’t tell if he is seeing true atypia or disruption that’s an artifact of the collection technique.
In this instance, he said, a dermatopathologist would be “obligated to overcall, because one couldn’t really determine the pathology.” The bottom line? “Don’t curette biopsies of melanocytic lesions.”
Another technique that can interfere with the ability to read a tissue specimen accurately is electrodesiccation. Although it’s often performed in conjunction with curettage, electrodesiccation can cause changes in tissue consistent with thermal injury. “Essentially, the tissue has been burned,” Dr. Phelps pointed out. This can result in a characteristic streaming pattern of nuclei, and the dermis can acquire a “peculiar homogenized appearance,” he said.
Although electrodesiccation can be a useful technique to make sure margins are controlled, “when you do this, just be aware that the interpretation is difficult,” he noted. “It’s difficult to tell where the margins are and if they are the appropriate and correct margins,” he said.
When possible, try to avoid squeezing the tumor, Dr. Phelps advised. Excessive pressure on the specimen can distort cell architecture and make pathological diagnosis really challenging, particularly in lymphoid tumors, he said.
“Often, the tumor is not recognizable,” he added. Crush artifact can result in an appearance of small bluish clumps and smearing of collagen fibers. The effect, he said, can be particularly pronounced with small cell carcinoma and lymphoma, and with rapidly proliferating tumors.
Dr. Phelps said that during his training, he was taught not to use forceps to extract a stubborn punch biopsy specimen; rather, he was trained to use a needle to tease out the specimen. Fear of a self-inflicted needle stick with this technique may be a deterrent, he acknowledged. If forceps are used, he suggested being as gentle as possible and using the finest forceps available.
When pathologists receive an intact excised lesion – one not obtained using a Mohs technique, “delineation of the margin is essential,” Dr. Phelps said. Further, accurate mapping is critical to helping the examiner understand the anatomic orientation of the specimen, a key prerequisite that enables accurate communication from the dermatopathologist back to the clinician if there’s a question regarding the need for retreatment, he added.
For an elliptical excision, ideally, both poles of the ellipse would be suture-tagged, and at least one tag is essential, he said. Then superior and inferior borders can be inked with contrasting colors, and the epidermal borders of the lesion should be marked as well. When the specimen is submitted, it should be accompanied by an accurate map that clearly indicates the coding for medial, lateral, inferior, and superior aspects of the specimen. “Always prepare a specimen diagram for oriented specimens,” Dr. Phelps noted.
Don’t forget to make sure that the left-right orientation on the diagram corresponds to the specimen’s orientation on the patient, he added. Some facilities use a clock face system to indicate orientation and positioning, which may be the clearest method of all.
Sometimes, it’s difficult for the dermatopathologist to visualize whether the specimen is aligned in true medial-lateral fashion, or along skin tension lines, which tend to run diagonally, so “the more clinical information, the better,” he said. “With good mapping, precise retreatment can be optimal,” he said.
Dr. Phelps reported that he had no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM THE 2017 AAD SUMMER MEETING
When – and how – to do a full-thickness graft repair
NEW YORK – Though flap reconstruction can provide elegant solutions with very good cosmesis after Mohs surgery and other excisional procedures, skin grafts provide another set of options.
Both split and full thickness grafts have a place in the dermatologist’s repertoire, but some tips and tricks can make a full thickness graft an attractive option in many instances, according to Marc Brown, MD, professor of dermatology and oncology at the University of Rochester (N.Y.).
Speaking at the summer meeting of the American Academy of Dermatology, Dr. Brown said that retrospective studies have shown that patients are highly satisfied with the cosmesis of full thickness skin grafting for reconstruction post Mohs surgery – if they’re asked after enough time has passed for the graft to mature and the dermatologist to perform some of the tweaks that are occasionally necessary. “It takes time to get to that point, but the overall satisfaction improves over time,” he said.
Full thickness skin grafts may be a good option when flap coverage is suboptimal or infeasible, he said. Some other pros of opting for a full thickness graft are that better cosmesis can be achieved in certain cases, and the donor site can be sutured, allowing for quicker healing with less downtime. However, a full thickness graft is a thicker graft, with resulting high metabolic demand. To ensure good “take,” dermatologists must be mindful that the graft site has a good vascular supply. Also, he added, full thickness grafts often need thinning, and physicians shouldn’t be afraid of being aggressive.
Both to reduce unwanted bulk and to help with better graft take, subcutaneous fat should be stripped completely from the graft, Dr. Brown noted. “You should see nothing that looks yellow,” he said. Fine serrated scissors are an excellent defatting tool, and while expensive, “they’re worth the cost,” he added.
Areas to be considered for full thickness grafts include the nasal ala, the medial canthus of the eye, the upper eyelid, fingers, and the ear. Larger defects on the scalp or forehead may also be good candidates, and full thickness grafts can work well on the lower leg.
For smaller grafts – those less than 1 or 2 cm diameter – Dr. Brown said that the preauricular area can work well as a donor site for facial grafts, since there’s often extra tissue with little tension there. Patients who are worried about donor site cosmesis may prefer the postauricular area, though the result is usually very good in either case, he said. Other potential donor sites are the glabella, nasolabial area, and the eyelid.
When grafts of more than 2 cm diameter are needed, Dr. Brown said the lateral neck, the supraclavicular area, or the lateral chest area can provide a good match in color and texture to facial skin.
Other tips for surgical technique are to use an appropriately-sized nonadherent gauze pad as a template for exact graft sizing. Precision counts, said Dr. Brown: “Measure twice, cut once.”
A central basting suture can be used to hold the graft in place while getting started, and Dr. Brown often uses a bolster for grafts of less than 1 cm. “Bolsters are helpful to prevent bleeding and improve contact in larger grafts,” he added.
Sutures should be placed graft to skin – “up and under,” Dr. Brown noted. He uses rapid-absorbing chromic suture material, with silk on the outside for the tie-over bolster. It’s also important to avoid tension on the wound edge, and he advised always using a pressure bandage for 48-72 hours.
If there’s concern about blood supply when grafting over cartilage, Dr. Brown advises making a few 2-mm punch defects in the cartilage to boost blood supply and help with engraftment.
For larger grafts where hematoma formation might result in graft failure, he will place a few parallel incisions through the graft as a means of escape should there be significant bleeding. At about 1 week post procedure, the graft should be purplish-pink in color, and patients should be counseled about the appearance of the graft as healing progresses, he said.
Physicians can manage patient expectations by letting them know not to expect the best cosmesis right away. However, said Dr. Brown, if the graft remains thickened, there are lots of options. Intralesional triamcinolone injections can help with thinning, and can be used beginning about 3 months after the graft. Dermabrasion is another good option, but he likes to wait 4-6 months before performing this procedure.
With appropriate site selection, meticulous technique, and good patient communication, dermatologists can keep full thickness skin grafting in the repertoire of viable options for excellent cosmesis, and a valuable tool in their own right. “Skin grafts are not a failure of reconstruction,” Dr. Brown said.
Dr. Brown had no conflicts to disclose.
[email protected]
On Twitter @karioakes
NEW YORK – Though flap reconstruction can provide elegant solutions with very good cosmesis after Mohs surgery and other excisional procedures, skin grafts provide another set of options.
Both split and full thickness grafts have a place in the dermatologist’s repertoire, but some tips and tricks can make a full thickness graft an attractive option in many instances, according to Marc Brown, MD, professor of dermatology and oncology at the University of Rochester (N.Y.).
Speaking at the summer meeting of the American Academy of Dermatology, Dr. Brown said that retrospective studies have shown that patients are highly satisfied with the cosmesis of full thickness skin grafting for reconstruction post Mohs surgery – if they’re asked after enough time has passed for the graft to mature and the dermatologist to perform some of the tweaks that are occasionally necessary. “It takes time to get to that point, but the overall satisfaction improves over time,” he said.
Full thickness skin grafts may be a good option when flap coverage is suboptimal or infeasible, he said. Some other pros of opting for a full thickness graft are that better cosmesis can be achieved in certain cases, and the donor site can be sutured, allowing for quicker healing with less downtime. However, a full thickness graft is a thicker graft, with resulting high metabolic demand. To ensure good “take,” dermatologists must be mindful that the graft site has a good vascular supply. Also, he added, full thickness grafts often need thinning, and physicians shouldn’t be afraid of being aggressive.
Both to reduce unwanted bulk and to help with better graft take, subcutaneous fat should be stripped completely from the graft, Dr. Brown noted. “You should see nothing that looks yellow,” he said. Fine serrated scissors are an excellent defatting tool, and while expensive, “they’re worth the cost,” he added.
Areas to be considered for full thickness grafts include the nasal ala, the medial canthus of the eye, the upper eyelid, fingers, and the ear. Larger defects on the scalp or forehead may also be good candidates, and full thickness grafts can work well on the lower leg.
For smaller grafts – those less than 1 or 2 cm diameter – Dr. Brown said that the preauricular area can work well as a donor site for facial grafts, since there’s often extra tissue with little tension there. Patients who are worried about donor site cosmesis may prefer the postauricular area, though the result is usually very good in either case, he said. Other potential donor sites are the glabella, nasolabial area, and the eyelid.
When grafts of more than 2 cm diameter are needed, Dr. Brown said the lateral neck, the supraclavicular area, or the lateral chest area can provide a good match in color and texture to facial skin.
Other tips for surgical technique are to use an appropriately-sized nonadherent gauze pad as a template for exact graft sizing. Precision counts, said Dr. Brown: “Measure twice, cut once.”
A central basting suture can be used to hold the graft in place while getting started, and Dr. Brown often uses a bolster for grafts of less than 1 cm. “Bolsters are helpful to prevent bleeding and improve contact in larger grafts,” he added.
Sutures should be placed graft to skin – “up and under,” Dr. Brown noted. He uses rapid-absorbing chromic suture material, with silk on the outside for the tie-over bolster. It’s also important to avoid tension on the wound edge, and he advised always using a pressure bandage for 48-72 hours.
If there’s concern about blood supply when grafting over cartilage, Dr. Brown advises making a few 2-mm punch defects in the cartilage to boost blood supply and help with engraftment.
For larger grafts where hematoma formation might result in graft failure, he will place a few parallel incisions through the graft as a means of escape should there be significant bleeding. At about 1 week post procedure, the graft should be purplish-pink in color, and patients should be counseled about the appearance of the graft as healing progresses, he said.
Physicians can manage patient expectations by letting them know not to expect the best cosmesis right away. However, said Dr. Brown, if the graft remains thickened, there are lots of options. Intralesional triamcinolone injections can help with thinning, and can be used beginning about 3 months after the graft. Dermabrasion is another good option, but he likes to wait 4-6 months before performing this procedure.
With appropriate site selection, meticulous technique, and good patient communication, dermatologists can keep full thickness skin grafting in the repertoire of viable options for excellent cosmesis, and a valuable tool in their own right. “Skin grafts are not a failure of reconstruction,” Dr. Brown said.
Dr. Brown had no conflicts to disclose.
[email protected]
On Twitter @karioakes
NEW YORK – Though flap reconstruction can provide elegant solutions with very good cosmesis after Mohs surgery and other excisional procedures, skin grafts provide another set of options.
Both split and full thickness grafts have a place in the dermatologist’s repertoire, but some tips and tricks can make a full thickness graft an attractive option in many instances, according to Marc Brown, MD, professor of dermatology and oncology at the University of Rochester (N.Y.).
Speaking at the summer meeting of the American Academy of Dermatology, Dr. Brown said that retrospective studies have shown that patients are highly satisfied with the cosmesis of full thickness skin grafting for reconstruction post Mohs surgery – if they’re asked after enough time has passed for the graft to mature and the dermatologist to perform some of the tweaks that are occasionally necessary. “It takes time to get to that point, but the overall satisfaction improves over time,” he said.
Full thickness skin grafts may be a good option when flap coverage is suboptimal or infeasible, he said. Some other pros of opting for a full thickness graft are that better cosmesis can be achieved in certain cases, and the donor site can be sutured, allowing for quicker healing with less downtime. However, a full thickness graft is a thicker graft, with resulting high metabolic demand. To ensure good “take,” dermatologists must be mindful that the graft site has a good vascular supply. Also, he added, full thickness grafts often need thinning, and physicians shouldn’t be afraid of being aggressive.
Both to reduce unwanted bulk and to help with better graft take, subcutaneous fat should be stripped completely from the graft, Dr. Brown noted. “You should see nothing that looks yellow,” he said. Fine serrated scissors are an excellent defatting tool, and while expensive, “they’re worth the cost,” he added.
Areas to be considered for full thickness grafts include the nasal ala, the medial canthus of the eye, the upper eyelid, fingers, and the ear. Larger defects on the scalp or forehead may also be good candidates, and full thickness grafts can work well on the lower leg.
For smaller grafts – those less than 1 or 2 cm diameter – Dr. Brown said that the preauricular area can work well as a donor site for facial grafts, since there’s often extra tissue with little tension there. Patients who are worried about donor site cosmesis may prefer the postauricular area, though the result is usually very good in either case, he said. Other potential donor sites are the glabella, nasolabial area, and the eyelid.
When grafts of more than 2 cm diameter are needed, Dr. Brown said the lateral neck, the supraclavicular area, or the lateral chest area can provide a good match in color and texture to facial skin.
Other tips for surgical technique are to use an appropriately-sized nonadherent gauze pad as a template for exact graft sizing. Precision counts, said Dr. Brown: “Measure twice, cut once.”
A central basting suture can be used to hold the graft in place while getting started, and Dr. Brown often uses a bolster for grafts of less than 1 cm. “Bolsters are helpful to prevent bleeding and improve contact in larger grafts,” he added.
Sutures should be placed graft to skin – “up and under,” Dr. Brown noted. He uses rapid-absorbing chromic suture material, with silk on the outside for the tie-over bolster. It’s also important to avoid tension on the wound edge, and he advised always using a pressure bandage for 48-72 hours.
If there’s concern about blood supply when grafting over cartilage, Dr. Brown advises making a few 2-mm punch defects in the cartilage to boost blood supply and help with engraftment.
For larger grafts where hematoma formation might result in graft failure, he will place a few parallel incisions through the graft as a means of escape should there be significant bleeding. At about 1 week post procedure, the graft should be purplish-pink in color, and patients should be counseled about the appearance of the graft as healing progresses, he said.
Physicians can manage patient expectations by letting them know not to expect the best cosmesis right away. However, said Dr. Brown, if the graft remains thickened, there are lots of options. Intralesional triamcinolone injections can help with thinning, and can be used beginning about 3 months after the graft. Dermabrasion is another good option, but he likes to wait 4-6 months before performing this procedure.
With appropriate site selection, meticulous technique, and good patient communication, dermatologists can keep full thickness skin grafting in the repertoire of viable options for excellent cosmesis, and a valuable tool in their own right. “Skin grafts are not a failure of reconstruction,” Dr. Brown said.
Dr. Brown had no conflicts to disclose.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM the 2017 AAD SUMMER MEETING
When the painful ‘bumps’ are calciphylaxis, what’s next?
EXPERT ANALYSIS FROM THE 2017 AAD SUMMER MEETING
NEW YORK – When patients come to the office with painful “bumps” on the legs or elsewhere, panniculitis should be in the differential. And for some patients, said Alina Bridges, DO, the panniculitis may come with the dire diagnosis of calciphylaxis.
Calciphylaxis is an underrecognized crystal deposition disease that’s associated with panniculitis, said Dr. Bridges, speaking at the American Academy of Dermatology summer meeting. When calcium accumulates in small subcutaneous vessels, an occlusive vasculopathy is created within the dermis.
A soft-tissue radiograph of the affected area may also be helpful. Calciphylaxis shows as a fine netlike pattern of calcification, a finding that Dr. Bridges said has 90% specificity for the condition.
However, Dr. Bridges said, patients with panniculitis need a biopsy. “Careful selection of biopsy site and a deep specimen containing abundant fat obtained by incisional or excisional biopsy” is the best approach, allowing the pathologist to see the complete picture. In some cases, she said, a double-punch biopsy could also produce adequate specimens.
In addition to the calcium deposition, other pathologic findings may be lobular fat necrosis, with a pannicular vascular thrombosis. Though extravascular calcification can be seen in the panniculus, it’s not uncommon also to see intravascular calcification, said Dr. Bridges, who is the dermatopathology fellowship program director at the Mayo Clinic, Rochester, Minn.
Dr. Bridges said that the patients with calciphylaxis can present with predominant panniculitis or vasculitis, or a mixed picture; patients can also have bullae, ulcers, or livedo reticularis.
The lesions are extremely painful and become increasingly violaceous, with firm subcutaneous nodules. They are variably necrotic, and become more ulcerated over time.
Calciphylaxis is multifactorial and progressive. The prognosis is very poor for individuals with the condition, Dr. Bridges said. The median survival is 10 months, with 1-year survival rates of 46%, and just 20% of individuals with calciphylaxis surviving 2 years after diagnosis.
Gangrene is a frequent complication, and multisystem organ failure often occurs as well, she said.
Calciphylaxis most commonly occurs in individuals with chronic kidney disease and is seen in 4% of hemodialysis patients. However, it may also occur in individuals without uremia. In associations that are incompletely understood, calciphylaxis has been associated with warfarin therapy, connective tissue disorders, Crohn’s disease, liver disease, diabetes, hematologic malignancies, factor V Leiden deficiency, and protein C and S deficiency.
There’s a need for clinical suspicion of calciphylaxis when individuals with any of these conditions present with painful erythematous nodules, or with a vasculitic picture, she said.
Other, more common crystal deposition diseases can also be associated with panniculitis and can be in the differential, Dr. Bridges said. In patients with gout, sodium urate crystal deposition can occur in subcutaneous tissues.
Cutaneous oxalosis can occur as a primary disorder, when patients have metabolic errors and lack alanine-glyoxylate aminotransferase or D-glycerate dehydrogenase. Oxalosis can also be an acquired syndrome in patients with chronic renal failure who have been on long-term hemodialysis.
Although there is not a clearly effective treatment for calciphylaxis, a multitargeted, multidisciplinary approach is needed to help improve tissue health and patient quality of life. Since the primary mechanism of tissue damage is thrombotic tissue ischemia, strategies are aimed at existing clots and at preventing further clot formation.
To correct the calcium-phosphate balance, several medications have been used, including sodium thiosulfate and cinacalcet. For individuals on hemodialysis, a low-calcium dialysate may be used.
Tissue perfusion and oxygenation can be improved using tissue plasminogen activator, hyperbaric oxygen therapy, and the avoidance of warfarin if the patient requires anticoagulation.
To address wounds directly, debridement can begin with whirlpool time for patients. Surgical debridement may be required, and maggots can also help clean up wound beds.
Palliative care for patients should always include optimizing pain control and improving quality of life for patients with this serious and often life-limiting condition, Dr. Bridges said.
She reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM THE 2017 AAD SUMMER MEETING
NEW YORK – When patients come to the office with painful “bumps” on the legs or elsewhere, panniculitis should be in the differential. And for some patients, said Alina Bridges, DO, the panniculitis may come with the dire diagnosis of calciphylaxis.
Calciphylaxis is an underrecognized crystal deposition disease that’s associated with panniculitis, said Dr. Bridges, speaking at the American Academy of Dermatology summer meeting. When calcium accumulates in small subcutaneous vessels, an occlusive vasculopathy is created within the dermis.
A soft-tissue radiograph of the affected area may also be helpful. Calciphylaxis shows as a fine netlike pattern of calcification, a finding that Dr. Bridges said has 90% specificity for the condition.
However, Dr. Bridges said, patients with panniculitis need a biopsy. “Careful selection of biopsy site and a deep specimen containing abundant fat obtained by incisional or excisional biopsy” is the best approach, allowing the pathologist to see the complete picture. In some cases, she said, a double-punch biopsy could also produce adequate specimens.
In addition to the calcium deposition, other pathologic findings may be lobular fat necrosis, with a pannicular vascular thrombosis. Though extravascular calcification can be seen in the panniculus, it’s not uncommon also to see intravascular calcification, said Dr. Bridges, who is the dermatopathology fellowship program director at the Mayo Clinic, Rochester, Minn.
Dr. Bridges said that the patients with calciphylaxis can present with predominant panniculitis or vasculitis, or a mixed picture; patients can also have bullae, ulcers, or livedo reticularis.
The lesions are extremely painful and become increasingly violaceous, with firm subcutaneous nodules. They are variably necrotic, and become more ulcerated over time.
Calciphylaxis is multifactorial and progressive. The prognosis is very poor for individuals with the condition, Dr. Bridges said. The median survival is 10 months, with 1-year survival rates of 46%, and just 20% of individuals with calciphylaxis surviving 2 years after diagnosis.
Gangrene is a frequent complication, and multisystem organ failure often occurs as well, she said.
Calciphylaxis most commonly occurs in individuals with chronic kidney disease and is seen in 4% of hemodialysis patients. However, it may also occur in individuals without uremia. In associations that are incompletely understood, calciphylaxis has been associated with warfarin therapy, connective tissue disorders, Crohn’s disease, liver disease, diabetes, hematologic malignancies, factor V Leiden deficiency, and protein C and S deficiency.
There’s a need for clinical suspicion of calciphylaxis when individuals with any of these conditions present with painful erythematous nodules, or with a vasculitic picture, she said.
Other, more common crystal deposition diseases can also be associated with panniculitis and can be in the differential, Dr. Bridges said. In patients with gout, sodium urate crystal deposition can occur in subcutaneous tissues.
Cutaneous oxalosis can occur as a primary disorder, when patients have metabolic errors and lack alanine-glyoxylate aminotransferase or D-glycerate dehydrogenase. Oxalosis can also be an acquired syndrome in patients with chronic renal failure who have been on long-term hemodialysis.
Although there is not a clearly effective treatment for calciphylaxis, a multitargeted, multidisciplinary approach is needed to help improve tissue health and patient quality of life. Since the primary mechanism of tissue damage is thrombotic tissue ischemia, strategies are aimed at existing clots and at preventing further clot formation.
To correct the calcium-phosphate balance, several medications have been used, including sodium thiosulfate and cinacalcet. For individuals on hemodialysis, a low-calcium dialysate may be used.
Tissue perfusion and oxygenation can be improved using tissue plasminogen activator, hyperbaric oxygen therapy, and the avoidance of warfarin if the patient requires anticoagulation.
To address wounds directly, debridement can begin with whirlpool time for patients. Surgical debridement may be required, and maggots can also help clean up wound beds.
Palliative care for patients should always include optimizing pain control and improving quality of life for patients with this serious and often life-limiting condition, Dr. Bridges said.
She reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM THE 2017 AAD SUMMER MEETING
NEW YORK – When patients come to the office with painful “bumps” on the legs or elsewhere, panniculitis should be in the differential. And for some patients, said Alina Bridges, DO, the panniculitis may come with the dire diagnosis of calciphylaxis.
Calciphylaxis is an underrecognized crystal deposition disease that’s associated with panniculitis, said Dr. Bridges, speaking at the American Academy of Dermatology summer meeting. When calcium accumulates in small subcutaneous vessels, an occlusive vasculopathy is created within the dermis.
A soft-tissue radiograph of the affected area may also be helpful. Calciphylaxis shows as a fine netlike pattern of calcification, a finding that Dr. Bridges said has 90% specificity for the condition.
However, Dr. Bridges said, patients with panniculitis need a biopsy. “Careful selection of biopsy site and a deep specimen containing abundant fat obtained by incisional or excisional biopsy” is the best approach, allowing the pathologist to see the complete picture. In some cases, she said, a double-punch biopsy could also produce adequate specimens.
In addition to the calcium deposition, other pathologic findings may be lobular fat necrosis, with a pannicular vascular thrombosis. Though extravascular calcification can be seen in the panniculus, it’s not uncommon also to see intravascular calcification, said Dr. Bridges, who is the dermatopathology fellowship program director at the Mayo Clinic, Rochester, Minn.
Dr. Bridges said that the patients with calciphylaxis can present with predominant panniculitis or vasculitis, or a mixed picture; patients can also have bullae, ulcers, or livedo reticularis.
The lesions are extremely painful and become increasingly violaceous, with firm subcutaneous nodules. They are variably necrotic, and become more ulcerated over time.
Calciphylaxis is multifactorial and progressive. The prognosis is very poor for individuals with the condition, Dr. Bridges said. The median survival is 10 months, with 1-year survival rates of 46%, and just 20% of individuals with calciphylaxis surviving 2 years after diagnosis.
Gangrene is a frequent complication, and multisystem organ failure often occurs as well, she said.
Calciphylaxis most commonly occurs in individuals with chronic kidney disease and is seen in 4% of hemodialysis patients. However, it may also occur in individuals without uremia. In associations that are incompletely understood, calciphylaxis has been associated with warfarin therapy, connective tissue disorders, Crohn’s disease, liver disease, diabetes, hematologic malignancies, factor V Leiden deficiency, and protein C and S deficiency.
There’s a need for clinical suspicion of calciphylaxis when individuals with any of these conditions present with painful erythematous nodules, or with a vasculitic picture, she said.
Other, more common crystal deposition diseases can also be associated with panniculitis and can be in the differential, Dr. Bridges said. In patients with gout, sodium urate crystal deposition can occur in subcutaneous tissues.
Cutaneous oxalosis can occur as a primary disorder, when patients have metabolic errors and lack alanine-glyoxylate aminotransferase or D-glycerate dehydrogenase. Oxalosis can also be an acquired syndrome in patients with chronic renal failure who have been on long-term hemodialysis.
Although there is not a clearly effective treatment for calciphylaxis, a multitargeted, multidisciplinary approach is needed to help improve tissue health and patient quality of life. Since the primary mechanism of tissue damage is thrombotic tissue ischemia, strategies are aimed at existing clots and at preventing further clot formation.
To correct the calcium-phosphate balance, several medications have been used, including sodium thiosulfate and cinacalcet. For individuals on hemodialysis, a low-calcium dialysate may be used.
Tissue perfusion and oxygenation can be improved using tissue plasminogen activator, hyperbaric oxygen therapy, and the avoidance of warfarin if the patient requires anticoagulation.
To address wounds directly, debridement can begin with whirlpool time for patients. Surgical debridement may be required, and maggots can also help clean up wound beds.
Palliative care for patients should always include optimizing pain control and improving quality of life for patients with this serious and often life-limiting condition, Dr. Bridges said.
She reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
Clues to drug adulteration may lie skin deep
CHICAGO – Sometimes, the skin can provide the first clues that a patient has been exposed to a drug product that has been adulterated or an over-the-counter product illegally sold in this country that contains a prescription medication, according to pediatric dermatologist Scott Norton, MD.
Speaking at the World Congress of Pediatric Dermatology, he reviewed some of the reactions associated with exposure to counterfeit drugs, contraband drugs, as well as products, misrepresented as drugs that do not include any active pharmaceutical ingredients. The worldwide market for these products is a “hugely profitable industry,” and the scope of the problem should not be underestimated, said Dr. Norton, chief of dermatology at Children’s National Health System, Washington.
It’s particularly important to have a high index of suspicion for such products given an increasingly mobile worldwide population. Today, patients and their family members who travel out of the country – and even local shopkeepers – may bring in these sorts of products from outside the United States, many of which would require a prescription in the United States.
In the United States, there have been several reports of a mysterious fixed drug eruption in patients reported to have taken Baczol, a cold and flu remedy available over the counter in El Salvador for upper respiratory infections. Two of the ingredients listed on the Baczol label are sulfamethoxazole and trimethoprim, two prescription antibiotics. After determining that two Salvadoran American children with a suspected fixed drug eruption had taken a Baczol product, Dr. Norton, with the aid of medical students, was able to find Baczol containing trimethoprim-sulfamethoxazole for sale over the counter in more than one-third of the shops visited in the greater Washington area (MMWR Morb Mortal Wkly Rep. 2013 Nov 22;62[46]:914-6). Eventually, the Food and Drug Administration issued a consumer alert regarding certain Baczol products containing these ingredients, but Dr. Norton said he is still concerned about the possibility for more grave hypersensitivity reactions to these sulfa antibiotics in the Salvadoran product.
Sometimes, said Dr. Norton, the problem lies in the lack of an expected ingredient. He and his team at Children’s National Health System helped solve a medical mystery involving a skin ailment in very premature infants with cholestasis. An interdisciplinary team was convened after the neonatal intensive care unit at the hospital saw its third infant with severe blistering and erosions in an acral, perianal, and perioral pattern that did not respond to empiric treatment for herpes simplex virus and staphylococcal infection – a pattern reminiscent of zinc deficiency dermatitis. Dietitians reported that there was a nationwide shortage of sterile injectable zinc, so total parenteral nutrition was being formulated without zinc. All three of the premature infants were receiving total parenteral nutrition and were so premature that they had insufficient zinc stores. The problem was identified and corrected (MMWR 2014 Jan. 17;63[02];35-7).
A more pervasive issue, which has global significance, pertains to counterfeit vaccines prepared with absolutely no vaccine components, often made in China or Nigeria with high-quality and sophisticated packaging, said Dr. Norton.
Keeping a lid on counterfeit drugs is challenging since there are so many potential entry points into the supply chain, Dr. Norton pointed out. Weak points include mislabeled raw ingredients, packaging, storage, transportation, repackaging, and distribution. The proliferation of online pharmacies also makes regulation more difficult.
There is some international cooperation to detect and combat drug counterfeiting and adulteration: For example, Interpol, the International Coalition of Medicines Regulatory Authorities, the Pharmaceutical Security Institute, and even the United Nations are developing cooperative strategies to combat the problem.
In the meantime, he emphasized that physicians must maintain a high index of suspicion and keep in mind that the first signs of adulterated drugs or prescription drugs available OTC may appear on the skin.
Dr. Norton reported no conflicts of interest.
[email protected]
On Twitter @karioakes
CHICAGO – Sometimes, the skin can provide the first clues that a patient has been exposed to a drug product that has been adulterated or an over-the-counter product illegally sold in this country that contains a prescription medication, according to pediatric dermatologist Scott Norton, MD.
Speaking at the World Congress of Pediatric Dermatology, he reviewed some of the reactions associated with exposure to counterfeit drugs, contraband drugs, as well as products, misrepresented as drugs that do not include any active pharmaceutical ingredients. The worldwide market for these products is a “hugely profitable industry,” and the scope of the problem should not be underestimated, said Dr. Norton, chief of dermatology at Children’s National Health System, Washington.
It’s particularly important to have a high index of suspicion for such products given an increasingly mobile worldwide population. Today, patients and their family members who travel out of the country – and even local shopkeepers – may bring in these sorts of products from outside the United States, many of which would require a prescription in the United States.
In the United States, there have been several reports of a mysterious fixed drug eruption in patients reported to have taken Baczol, a cold and flu remedy available over the counter in El Salvador for upper respiratory infections. Two of the ingredients listed on the Baczol label are sulfamethoxazole and trimethoprim, two prescription antibiotics. After determining that two Salvadoran American children with a suspected fixed drug eruption had taken a Baczol product, Dr. Norton, with the aid of medical students, was able to find Baczol containing trimethoprim-sulfamethoxazole for sale over the counter in more than one-third of the shops visited in the greater Washington area (MMWR Morb Mortal Wkly Rep. 2013 Nov 22;62[46]:914-6). Eventually, the Food and Drug Administration issued a consumer alert regarding certain Baczol products containing these ingredients, but Dr. Norton said he is still concerned about the possibility for more grave hypersensitivity reactions to these sulfa antibiotics in the Salvadoran product.
Sometimes, said Dr. Norton, the problem lies in the lack of an expected ingredient. He and his team at Children’s National Health System helped solve a medical mystery involving a skin ailment in very premature infants with cholestasis. An interdisciplinary team was convened after the neonatal intensive care unit at the hospital saw its third infant with severe blistering and erosions in an acral, perianal, and perioral pattern that did not respond to empiric treatment for herpes simplex virus and staphylococcal infection – a pattern reminiscent of zinc deficiency dermatitis. Dietitians reported that there was a nationwide shortage of sterile injectable zinc, so total parenteral nutrition was being formulated without zinc. All three of the premature infants were receiving total parenteral nutrition and were so premature that they had insufficient zinc stores. The problem was identified and corrected (MMWR 2014 Jan. 17;63[02];35-7).
A more pervasive issue, which has global significance, pertains to counterfeit vaccines prepared with absolutely no vaccine components, often made in China or Nigeria with high-quality and sophisticated packaging, said Dr. Norton.
Keeping a lid on counterfeit drugs is challenging since there are so many potential entry points into the supply chain, Dr. Norton pointed out. Weak points include mislabeled raw ingredients, packaging, storage, transportation, repackaging, and distribution. The proliferation of online pharmacies also makes regulation more difficult.
There is some international cooperation to detect and combat drug counterfeiting and adulteration: For example, Interpol, the International Coalition of Medicines Regulatory Authorities, the Pharmaceutical Security Institute, and even the United Nations are developing cooperative strategies to combat the problem.
In the meantime, he emphasized that physicians must maintain a high index of suspicion and keep in mind that the first signs of adulterated drugs or prescription drugs available OTC may appear on the skin.
Dr. Norton reported no conflicts of interest.
[email protected]
On Twitter @karioakes
CHICAGO – Sometimes, the skin can provide the first clues that a patient has been exposed to a drug product that has been adulterated or an over-the-counter product illegally sold in this country that contains a prescription medication, according to pediatric dermatologist Scott Norton, MD.
Speaking at the World Congress of Pediatric Dermatology, he reviewed some of the reactions associated with exposure to counterfeit drugs, contraband drugs, as well as products, misrepresented as drugs that do not include any active pharmaceutical ingredients. The worldwide market for these products is a “hugely profitable industry,” and the scope of the problem should not be underestimated, said Dr. Norton, chief of dermatology at Children’s National Health System, Washington.
It’s particularly important to have a high index of suspicion for such products given an increasingly mobile worldwide population. Today, patients and their family members who travel out of the country – and even local shopkeepers – may bring in these sorts of products from outside the United States, many of which would require a prescription in the United States.
In the United States, there have been several reports of a mysterious fixed drug eruption in patients reported to have taken Baczol, a cold and flu remedy available over the counter in El Salvador for upper respiratory infections. Two of the ingredients listed on the Baczol label are sulfamethoxazole and trimethoprim, two prescription antibiotics. After determining that two Salvadoran American children with a suspected fixed drug eruption had taken a Baczol product, Dr. Norton, with the aid of medical students, was able to find Baczol containing trimethoprim-sulfamethoxazole for sale over the counter in more than one-third of the shops visited in the greater Washington area (MMWR Morb Mortal Wkly Rep. 2013 Nov 22;62[46]:914-6). Eventually, the Food and Drug Administration issued a consumer alert regarding certain Baczol products containing these ingredients, but Dr. Norton said he is still concerned about the possibility for more grave hypersensitivity reactions to these sulfa antibiotics in the Salvadoran product.
Sometimes, said Dr. Norton, the problem lies in the lack of an expected ingredient. He and his team at Children’s National Health System helped solve a medical mystery involving a skin ailment in very premature infants with cholestasis. An interdisciplinary team was convened after the neonatal intensive care unit at the hospital saw its third infant with severe blistering and erosions in an acral, perianal, and perioral pattern that did not respond to empiric treatment for herpes simplex virus and staphylococcal infection – a pattern reminiscent of zinc deficiency dermatitis. Dietitians reported that there was a nationwide shortage of sterile injectable zinc, so total parenteral nutrition was being formulated without zinc. All three of the premature infants were receiving total parenteral nutrition and were so premature that they had insufficient zinc stores. The problem was identified and corrected (MMWR 2014 Jan. 17;63[02];35-7).
A more pervasive issue, which has global significance, pertains to counterfeit vaccines prepared with absolutely no vaccine components, often made in China or Nigeria with high-quality and sophisticated packaging, said Dr. Norton.
Keeping a lid on counterfeit drugs is challenging since there are so many potential entry points into the supply chain, Dr. Norton pointed out. Weak points include mislabeled raw ingredients, packaging, storage, transportation, repackaging, and distribution. The proliferation of online pharmacies also makes regulation more difficult.
There is some international cooperation to detect and combat drug counterfeiting and adulteration: For example, Interpol, the International Coalition of Medicines Regulatory Authorities, the Pharmaceutical Security Institute, and even the United Nations are developing cooperative strategies to combat the problem.
In the meantime, he emphasized that physicians must maintain a high index of suspicion and keep in mind that the first signs of adulterated drugs or prescription drugs available OTC may appear on the skin.
Dr. Norton reported no conflicts of interest.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM WCPD 2017