User login
RA, JIA may raise risk of preterm delivery
according to a study examining autoimmune disease in pregnancy. Corticosteroid use in any trimester increased that risk from 100%-400%, regardless of how active the arthritis was.
The study found that women with RA had more than double the risk for preterm delivery, compared with a cohort without autoimmune disease (relative risk, 2.09; 95% confidence interval, 1.50-2.91). For women with juvenile idiopathic arthritis (JIA), the relative risk was 1.81 for preterm delivery (95% CI, 1.14-2.89).
The prospective cohort study, part of the Organization of Teratology Information Specialists Autoimmune Disease in Pregnancy Project, enrolled 657 women with RA and 170 women with JIA. The study also included a comparison group of 564 women without autoimmune disease. All of those included in the study were enrolled before 19 weeks’ gestation and delivered live-born infants during 2004-2017.
The study adds to a clinically important area of research that has yielded sometimes conflicting results; clarity has also been impeded by a variety of methodologies. Though several analyses have shown higher risk of preterm delivery in women with RA, not all studies have adjusted for medication use and disease activity, Chelsey F. Smith, MD, and her coauthors wrote in Arthritis Care & Research. Further, how women with JIA fare in pregnancy has not been well studied, they said.
Dr. Smith, a rheumatologist at the University of California, San Diego, and her colleagues included many baseline covariates in their analysis of pregnancy outcomes; these included maternal age and race, socioeconomic status, body mass index, previous adverse pregnancy outcomes, and comorbidities, including autoimmune disease. Adverse pregnancy outcomes during the studied pregnancy were also included as covariates, and deliveries were considered preterm if labor began before 37 weeks’ gestation.
For women with RA, a higher active disease score at any point during pregnancy was associated with a significantly higher risk of preterm delivery, even after adjustment for other potential risk factors, including first-trimester corticosteroid use (adjusted risk ratio, 1.52; 95% CI, 1.06-2.18). The persistence of this association, wrote Dr. Smith and her colleagues, implies “that active disease in RA may contribute to [preterm delivery] independent of medications,” perhaps through the action of proinflammatory cytokines that may stimulate prostaglandins and provoke uterine contractions.
The researchers found, though, that this association between disease activity and risk for preterm birth did not hold true for women with JIA, leaving part of the mystery unsolved.
However, women with both RA and JIA who used corticosteroids in any trimester were more likely to have a preterm delivery, as were women with JIA who used NSAIDs in the first trimester of pregnancy. The use of disease-modifying antirheumatic drugs (DMARDs) and biologics in any trimester did not confer increased risk for preterm delivery in women with either disease state.
There were other differences between the groups: Women with JIA were overall younger, but had more prepregnancy hypertension, which “may have contributed to the elevated incidence of preeclampsia seen in this group,” the investigators wrote. Fever was more common in women with JIA, and had an independent association with preterm delivery, as did first trimester NSAID use in this group alone.
Dr. Smith and her colleagues hypothesized that the relative heterogeneity of the JIA group may mean that disease activity still influenced outcomes.
Among other comorbidities, gestational diabetes (GDM) was more common in the RA group than in the JIA group or the comparison cohort, and was associated with a significantly higher risk for preterm delivery in women with RA, even after accounting for preeclampsia and hypertension in a multivariate analysis.
Dr. Smith and her colleagues pointed out that it was difficult to account for physician behavior in managing pregnancy in these high-risk women. “Additionally, given that women with both RA and GDM are at a particularly high risk for perinatal complications, we can speculate that the obstetricians in this group were perhaps more aggressive about inducing at an earlier gestational age than in other groups, but this information was not available in the dataset.”
Through phone interviews, investigators obtained information about prescription and nonprescription medication use during pregnancy; women were also asked about use of other substances and occupational exposures, infections, and prenatal testing and other medical procedures. Another telephone interview conducted soon after delivery asked about birth outcomes. Abstracted medical record data were used to verify and supplement the interview information.
When looking at treatments used, Dr. Smith and her colleagues grouped autoimmune disease medications into DMARDs, non-DMARD biologic medications, corticosteroids, and NSAIDs.
Disease activity assessment, conducted at intake and at 32 weeks’ gestation, used the Health Assessment Questionnaire, pain scores, and patient global disease activity to calculate a Patient Activity Scale score ranging from 0 to 10. Patients with a score over 3.7 were classified as having high disease activity.
Dr. Smith and her colleagues said that the study’s strengths included its prospective design and robust statistical schema. Also, using data about corticosteroid use and disease activity earlier in pregnancy avoided the inclusion of a reverse causation effect, where systemic inflammatory changes associated with preterm delivery might provoke more disease activity and a consequent boost in corticosteroid use.
However, the researchers said, the overall numbers of participants with preterm delivery was relatively small, and the JIA cohort was small as well.
“Further analyses are necessary to look at other categories of arthritis affecting women of childbearing age, racial disparities in these populations, as well as the influence of disease activity in the later stages of pregnancy on other perinatal factors” that can contribute to preterm delivery, said Dr. Smith and her colleagues.
The collaborative research group that collected data for the study receives research funding from several pharmaceutical companies. None of the authors reported any personal conflicts of interest.
SOURCE: Smith CF et al. Arthritis Care Res. 2018 Aug 21. doi: 10.1002/acr.23730.
according to a study examining autoimmune disease in pregnancy. Corticosteroid use in any trimester increased that risk from 100%-400%, regardless of how active the arthritis was.
The study found that women with RA had more than double the risk for preterm delivery, compared with a cohort without autoimmune disease (relative risk, 2.09; 95% confidence interval, 1.50-2.91). For women with juvenile idiopathic arthritis (JIA), the relative risk was 1.81 for preterm delivery (95% CI, 1.14-2.89).
The prospective cohort study, part of the Organization of Teratology Information Specialists Autoimmune Disease in Pregnancy Project, enrolled 657 women with RA and 170 women with JIA. The study also included a comparison group of 564 women without autoimmune disease. All of those included in the study were enrolled before 19 weeks’ gestation and delivered live-born infants during 2004-2017.
The study adds to a clinically important area of research that has yielded sometimes conflicting results; clarity has also been impeded by a variety of methodologies. Though several analyses have shown higher risk of preterm delivery in women with RA, not all studies have adjusted for medication use and disease activity, Chelsey F. Smith, MD, and her coauthors wrote in Arthritis Care & Research. Further, how women with JIA fare in pregnancy has not been well studied, they said.
Dr. Smith, a rheumatologist at the University of California, San Diego, and her colleagues included many baseline covariates in their analysis of pregnancy outcomes; these included maternal age and race, socioeconomic status, body mass index, previous adverse pregnancy outcomes, and comorbidities, including autoimmune disease. Adverse pregnancy outcomes during the studied pregnancy were also included as covariates, and deliveries were considered preterm if labor began before 37 weeks’ gestation.
For women with RA, a higher active disease score at any point during pregnancy was associated with a significantly higher risk of preterm delivery, even after adjustment for other potential risk factors, including first-trimester corticosteroid use (adjusted risk ratio, 1.52; 95% CI, 1.06-2.18). The persistence of this association, wrote Dr. Smith and her colleagues, implies “that active disease in RA may contribute to [preterm delivery] independent of medications,” perhaps through the action of proinflammatory cytokines that may stimulate prostaglandins and provoke uterine contractions.
The researchers found, though, that this association between disease activity and risk for preterm birth did not hold true for women with JIA, leaving part of the mystery unsolved.
However, women with both RA and JIA who used corticosteroids in any trimester were more likely to have a preterm delivery, as were women with JIA who used NSAIDs in the first trimester of pregnancy. The use of disease-modifying antirheumatic drugs (DMARDs) and biologics in any trimester did not confer increased risk for preterm delivery in women with either disease state.
There were other differences between the groups: Women with JIA were overall younger, but had more prepregnancy hypertension, which “may have contributed to the elevated incidence of preeclampsia seen in this group,” the investigators wrote. Fever was more common in women with JIA, and had an independent association with preterm delivery, as did first trimester NSAID use in this group alone.
Dr. Smith and her colleagues hypothesized that the relative heterogeneity of the JIA group may mean that disease activity still influenced outcomes.
Among other comorbidities, gestational diabetes (GDM) was more common in the RA group than in the JIA group or the comparison cohort, and was associated with a significantly higher risk for preterm delivery in women with RA, even after accounting for preeclampsia and hypertension in a multivariate analysis.
Dr. Smith and her colleagues pointed out that it was difficult to account for physician behavior in managing pregnancy in these high-risk women. “Additionally, given that women with both RA and GDM are at a particularly high risk for perinatal complications, we can speculate that the obstetricians in this group were perhaps more aggressive about inducing at an earlier gestational age than in other groups, but this information was not available in the dataset.”
Through phone interviews, investigators obtained information about prescription and nonprescription medication use during pregnancy; women were also asked about use of other substances and occupational exposures, infections, and prenatal testing and other medical procedures. Another telephone interview conducted soon after delivery asked about birth outcomes. Abstracted medical record data were used to verify and supplement the interview information.
When looking at treatments used, Dr. Smith and her colleagues grouped autoimmune disease medications into DMARDs, non-DMARD biologic medications, corticosteroids, and NSAIDs.
Disease activity assessment, conducted at intake and at 32 weeks’ gestation, used the Health Assessment Questionnaire, pain scores, and patient global disease activity to calculate a Patient Activity Scale score ranging from 0 to 10. Patients with a score over 3.7 were classified as having high disease activity.
Dr. Smith and her colleagues said that the study’s strengths included its prospective design and robust statistical schema. Also, using data about corticosteroid use and disease activity earlier in pregnancy avoided the inclusion of a reverse causation effect, where systemic inflammatory changes associated with preterm delivery might provoke more disease activity and a consequent boost in corticosteroid use.
However, the researchers said, the overall numbers of participants with preterm delivery was relatively small, and the JIA cohort was small as well.
“Further analyses are necessary to look at other categories of arthritis affecting women of childbearing age, racial disparities in these populations, as well as the influence of disease activity in the later stages of pregnancy on other perinatal factors” that can contribute to preterm delivery, said Dr. Smith and her colleagues.
The collaborative research group that collected data for the study receives research funding from several pharmaceutical companies. None of the authors reported any personal conflicts of interest.
SOURCE: Smith CF et al. Arthritis Care Res. 2018 Aug 21. doi: 10.1002/acr.23730.
according to a study examining autoimmune disease in pregnancy. Corticosteroid use in any trimester increased that risk from 100%-400%, regardless of how active the arthritis was.
The study found that women with RA had more than double the risk for preterm delivery, compared with a cohort without autoimmune disease (relative risk, 2.09; 95% confidence interval, 1.50-2.91). For women with juvenile idiopathic arthritis (JIA), the relative risk was 1.81 for preterm delivery (95% CI, 1.14-2.89).
The prospective cohort study, part of the Organization of Teratology Information Specialists Autoimmune Disease in Pregnancy Project, enrolled 657 women with RA and 170 women with JIA. The study also included a comparison group of 564 women without autoimmune disease. All of those included in the study were enrolled before 19 weeks’ gestation and delivered live-born infants during 2004-2017.
The study adds to a clinically important area of research that has yielded sometimes conflicting results; clarity has also been impeded by a variety of methodologies. Though several analyses have shown higher risk of preterm delivery in women with RA, not all studies have adjusted for medication use and disease activity, Chelsey F. Smith, MD, and her coauthors wrote in Arthritis Care & Research. Further, how women with JIA fare in pregnancy has not been well studied, they said.
Dr. Smith, a rheumatologist at the University of California, San Diego, and her colleagues included many baseline covariates in their analysis of pregnancy outcomes; these included maternal age and race, socioeconomic status, body mass index, previous adverse pregnancy outcomes, and comorbidities, including autoimmune disease. Adverse pregnancy outcomes during the studied pregnancy were also included as covariates, and deliveries were considered preterm if labor began before 37 weeks’ gestation.
For women with RA, a higher active disease score at any point during pregnancy was associated with a significantly higher risk of preterm delivery, even after adjustment for other potential risk factors, including first-trimester corticosteroid use (adjusted risk ratio, 1.52; 95% CI, 1.06-2.18). The persistence of this association, wrote Dr. Smith and her colleagues, implies “that active disease in RA may contribute to [preterm delivery] independent of medications,” perhaps through the action of proinflammatory cytokines that may stimulate prostaglandins and provoke uterine contractions.
The researchers found, though, that this association between disease activity and risk for preterm birth did not hold true for women with JIA, leaving part of the mystery unsolved.
However, women with both RA and JIA who used corticosteroids in any trimester were more likely to have a preterm delivery, as were women with JIA who used NSAIDs in the first trimester of pregnancy. The use of disease-modifying antirheumatic drugs (DMARDs) and biologics in any trimester did not confer increased risk for preterm delivery in women with either disease state.
There were other differences between the groups: Women with JIA were overall younger, but had more prepregnancy hypertension, which “may have contributed to the elevated incidence of preeclampsia seen in this group,” the investigators wrote. Fever was more common in women with JIA, and had an independent association with preterm delivery, as did first trimester NSAID use in this group alone.
Dr. Smith and her colleagues hypothesized that the relative heterogeneity of the JIA group may mean that disease activity still influenced outcomes.
Among other comorbidities, gestational diabetes (GDM) was more common in the RA group than in the JIA group or the comparison cohort, and was associated with a significantly higher risk for preterm delivery in women with RA, even after accounting for preeclampsia and hypertension in a multivariate analysis.
Dr. Smith and her colleagues pointed out that it was difficult to account for physician behavior in managing pregnancy in these high-risk women. “Additionally, given that women with both RA and GDM are at a particularly high risk for perinatal complications, we can speculate that the obstetricians in this group were perhaps more aggressive about inducing at an earlier gestational age than in other groups, but this information was not available in the dataset.”
Through phone interviews, investigators obtained information about prescription and nonprescription medication use during pregnancy; women were also asked about use of other substances and occupational exposures, infections, and prenatal testing and other medical procedures. Another telephone interview conducted soon after delivery asked about birth outcomes. Abstracted medical record data were used to verify and supplement the interview information.
When looking at treatments used, Dr. Smith and her colleagues grouped autoimmune disease medications into DMARDs, non-DMARD biologic medications, corticosteroids, and NSAIDs.
Disease activity assessment, conducted at intake and at 32 weeks’ gestation, used the Health Assessment Questionnaire, pain scores, and patient global disease activity to calculate a Patient Activity Scale score ranging from 0 to 10. Patients with a score over 3.7 were classified as having high disease activity.
Dr. Smith and her colleagues said that the study’s strengths included its prospective design and robust statistical schema. Also, using data about corticosteroid use and disease activity earlier in pregnancy avoided the inclusion of a reverse causation effect, where systemic inflammatory changes associated with preterm delivery might provoke more disease activity and a consequent boost in corticosteroid use.
However, the researchers said, the overall numbers of participants with preterm delivery was relatively small, and the JIA cohort was small as well.
“Further analyses are necessary to look at other categories of arthritis affecting women of childbearing age, racial disparities in these populations, as well as the influence of disease activity in the later stages of pregnancy on other perinatal factors” that can contribute to preterm delivery, said Dr. Smith and her colleagues.
The collaborative research group that collected data for the study receives research funding from several pharmaceutical companies. None of the authors reported any personal conflicts of interest.
SOURCE: Smith CF et al. Arthritis Care Res. 2018 Aug 21. doi: 10.1002/acr.23730.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point: The risk of preterm delivery was increased in women with RA and juvenile idiopathic arthritis.
Major finding: The risk ratio for preterm delivery in women with RA was 2.09.
Study details: A prospective cohort study of 657 women with RA, 170 women with juvenile idiopathic arthritis, and 564 women without autoimmune disease.
Disclosures: The study was part of the Organization of Teratology Information Specialists Autoimmune Disease in Pregnancy Project, which receives research funding from several pharmaceutical companies. None of the authors reported any personal conflicts of interest.
Source: Smith CF et al. Arthritis Care Res. 2018 Aug 21. doi: 10.1002/acr.23730.
Integrated pain program reduced LOS for sickle cell patients
WASHINGTON – Pediatric patients who received interdisciplinary outpatient care for sickle cell disease–related chronic pain experienced a reduction in average length of stay for pain-related hospitalizations, according to an exploratory analysis of patient outcomes at a single center.
Experiences at Children’s Mercy Hospital in Kansas City, Mo., have added to the body of evidence supporting integrative care for sickle cell disease (SCD) pain, Derrick L. Goubeaux, DO, said during an interview at the annual symposium of the Foundation for Sickle Cell Disease Research.
With time, chronic pain can become an overlay on pain from vasoocclusive crises as patients with SCD age, shifting the way that patients and providers think about pain, said Dr. Goubeaux, a pediatric hematology/oncology fellow at Children’s Mercy Hospital in Kansas City.
Using a collaborative approach that pulls in psychologists, social workers, and pain management specialists, the hospital’s multidisciplinary Sickle Cell Integrated Pain Program (SCIPP) seeks to optimize pain control by adding nonpharmacologic measures to medications, he said.
Dr. Goubeaux and his colleagues conducted a retrospective chart review that looked at individuals who received care from, or were referred to, the institution’s SCD program. Included in the study were patients who received care for SCD for at least 2 years before their referral to the SCIPP clinic, so that investigators could compare care for those patients before and after SCIPP clinic integration. The study also included patients who had not yet been integrated into SCIPP clinic care, for comparison.
Though the seven patients who were integrated into the SCIPP clinic did not have fewer hospitalizations than the five who were not referred, average length of stay (LOS) for the SCIPP patients dropped from 11 days to 8 days. Mean LOS also decreased for the non-SCIPP patients, from 7.4 to 5.8 days. The number of admissions per month for both groups increased over the study period, from a mean of 0.41 to 0.84 admissions per month for SCIPP patients, and from 0.27 to 0.43 for non-SCIPP patients.
The patients, who ranged in age from 138 to 253 months, mostly had HbSS SCD, but HbSbeta0, HbSD, and HbSC patients were also included. Four patients in the SCIPP group and two of the non-SCIPP patients were taking hydroxyurea.
Noting that data collection is still in the early stages, Dr. Goubeaux and his collaborators observed that “the LOS has shortened by 3 days in the integrated group, compared to 1.6 days in the [non-SCIPP] group.” They are currently also investigating whether costs per admission and admission-associated opioid use differs for patients integrated into the SCIPP clinic.
Aside from the small number of patients studied, Dr. Goubeaux and his colleagues acknowledged that even non-SCIPP patients are likely to have had pain management and psychology consultations during their inpatient stays – and these consults are conducted by SCIPP-associated providers.
Dr. Goubeaux reported no relevant disclosures or outside sources of funding.
WASHINGTON – Pediatric patients who received interdisciplinary outpatient care for sickle cell disease–related chronic pain experienced a reduction in average length of stay for pain-related hospitalizations, according to an exploratory analysis of patient outcomes at a single center.
Experiences at Children’s Mercy Hospital in Kansas City, Mo., have added to the body of evidence supporting integrative care for sickle cell disease (SCD) pain, Derrick L. Goubeaux, DO, said during an interview at the annual symposium of the Foundation for Sickle Cell Disease Research.
With time, chronic pain can become an overlay on pain from vasoocclusive crises as patients with SCD age, shifting the way that patients and providers think about pain, said Dr. Goubeaux, a pediatric hematology/oncology fellow at Children’s Mercy Hospital in Kansas City.
Using a collaborative approach that pulls in psychologists, social workers, and pain management specialists, the hospital’s multidisciplinary Sickle Cell Integrated Pain Program (SCIPP) seeks to optimize pain control by adding nonpharmacologic measures to medications, he said.
Dr. Goubeaux and his colleagues conducted a retrospective chart review that looked at individuals who received care from, or were referred to, the institution’s SCD program. Included in the study were patients who received care for SCD for at least 2 years before their referral to the SCIPP clinic, so that investigators could compare care for those patients before and after SCIPP clinic integration. The study also included patients who had not yet been integrated into SCIPP clinic care, for comparison.
Though the seven patients who were integrated into the SCIPP clinic did not have fewer hospitalizations than the five who were not referred, average length of stay (LOS) for the SCIPP patients dropped from 11 days to 8 days. Mean LOS also decreased for the non-SCIPP patients, from 7.4 to 5.8 days. The number of admissions per month for both groups increased over the study period, from a mean of 0.41 to 0.84 admissions per month for SCIPP patients, and from 0.27 to 0.43 for non-SCIPP patients.
The patients, who ranged in age from 138 to 253 months, mostly had HbSS SCD, but HbSbeta0, HbSD, and HbSC patients were also included. Four patients in the SCIPP group and two of the non-SCIPP patients were taking hydroxyurea.
Noting that data collection is still in the early stages, Dr. Goubeaux and his collaborators observed that “the LOS has shortened by 3 days in the integrated group, compared to 1.6 days in the [non-SCIPP] group.” They are currently also investigating whether costs per admission and admission-associated opioid use differs for patients integrated into the SCIPP clinic.
Aside from the small number of patients studied, Dr. Goubeaux and his colleagues acknowledged that even non-SCIPP patients are likely to have had pain management and psychology consultations during their inpatient stays – and these consults are conducted by SCIPP-associated providers.
Dr. Goubeaux reported no relevant disclosures or outside sources of funding.
WASHINGTON – Pediatric patients who received interdisciplinary outpatient care for sickle cell disease–related chronic pain experienced a reduction in average length of stay for pain-related hospitalizations, according to an exploratory analysis of patient outcomes at a single center.
Experiences at Children’s Mercy Hospital in Kansas City, Mo., have added to the body of evidence supporting integrative care for sickle cell disease (SCD) pain, Derrick L. Goubeaux, DO, said during an interview at the annual symposium of the Foundation for Sickle Cell Disease Research.
With time, chronic pain can become an overlay on pain from vasoocclusive crises as patients with SCD age, shifting the way that patients and providers think about pain, said Dr. Goubeaux, a pediatric hematology/oncology fellow at Children’s Mercy Hospital in Kansas City.
Using a collaborative approach that pulls in psychologists, social workers, and pain management specialists, the hospital’s multidisciplinary Sickle Cell Integrated Pain Program (SCIPP) seeks to optimize pain control by adding nonpharmacologic measures to medications, he said.
Dr. Goubeaux and his colleagues conducted a retrospective chart review that looked at individuals who received care from, or were referred to, the institution’s SCD program. Included in the study were patients who received care for SCD for at least 2 years before their referral to the SCIPP clinic, so that investigators could compare care for those patients before and after SCIPP clinic integration. The study also included patients who had not yet been integrated into SCIPP clinic care, for comparison.
Though the seven patients who were integrated into the SCIPP clinic did not have fewer hospitalizations than the five who were not referred, average length of stay (LOS) for the SCIPP patients dropped from 11 days to 8 days. Mean LOS also decreased for the non-SCIPP patients, from 7.4 to 5.8 days. The number of admissions per month for both groups increased over the study period, from a mean of 0.41 to 0.84 admissions per month for SCIPP patients, and from 0.27 to 0.43 for non-SCIPP patients.
The patients, who ranged in age from 138 to 253 months, mostly had HbSS SCD, but HbSbeta0, HbSD, and HbSC patients were also included. Four patients in the SCIPP group and two of the non-SCIPP patients were taking hydroxyurea.
Noting that data collection is still in the early stages, Dr. Goubeaux and his collaborators observed that “the LOS has shortened by 3 days in the integrated group, compared to 1.6 days in the [non-SCIPP] group.” They are currently also investigating whether costs per admission and admission-associated opioid use differs for patients integrated into the SCIPP clinic.
Aside from the small number of patients studied, Dr. Goubeaux and his colleagues acknowledged that even non-SCIPP patients are likely to have had pain management and psychology consultations during their inpatient stays – and these consults are conducted by SCIPP-associated providers.
Dr. Goubeaux reported no relevant disclosures or outside sources of funding.
REPORTING FROM FSCDR 2018
Key clinical point:
Major finding: Mean length of stay dropped from 11 days to 8 days after patients were referred to a multidisciplinary care clinic.
Study details: A retrospective chart review of 12 pediatric patients with chronic sickle cell disease-related pain.
Disclosures: The authors reported no conflicts of interest or outside sources of funding.
Longitudinal melanonychia: the good, the bad, and the confusing
CHICAGO – A discolored nail can give even seasoned dermatologists pause: Is the cause exogenous? Fungal or bacterial, perhaps? Could it be a subungual melanoma? Should it be followed, clipped, or biopsied? of the American Academy of Dermatology summer meeting.
The session came after a recent nationwide survey performed by Dr. Lipner and her collaborators who asked dermatologists at different practice stages how confident they were in the diagnosis and management of melanonychia. “On the whole, they were not very confident at all,” said Dr. Lipner, director of the nail division at Cornell University, New York.
Of 142 dermatology residents, as well as 58 junior and 199 senior attending dermatologists, just 18.2% performed nail exams at each visit, and most (58%) only looked at nails during the total body skin exam. Over half (62%) of resident physicians reported feeling not confident about melanonychia diagnosis and management, while that figure dropped to 8.6% for senior attending physicians. Still, most senior physicians (64.3%) were just “fairly confident” in their melanonychia skills (J Am Acad Dermatol. 2017 May;76[5]:994-6).
Tools of the trade
Dermoscopy can be an invaluable tool for determining the cause of longitudinal melanonychia (LM). “Contact dermoscopy is helpful, so I always have ultrasound gel available,” Dr. Lipner said. “The gel makes the nail more of a flat surface,” which makes accurate viewing easier. Other useful tools include a double-action nail clipper, which, she said, is a worthwhile investment.
Because patients who are concerned about one of their nails will often come to their appointment with nail polish still on the other nails, Dr. Lipner always has polish remover pads available in the office. It’s important to be able to see all nails, she said, but she and her collaborators, including first author Pierre Halteh, MD, who was then a medical student at Cornell, discovered from their survey that “few physicians (32/402; 8%) asked their patients to remove nail polish at every visit.”
Nonmelanocytic causes of LM
Longitudinal melanonychias can have a nonmelanocytic etiology, which can range from subungual hematomas to pseudomonas and fungal infections to exogenous pigment.
Overall, subungual hematomas are the most common cause of melanonychia, although longitudinal hematomas are not commonly seen. The more remote the causative trauma, the darker the subungual discoloration, Dr. Lipner said. “Dermoscopy is very helpful” for subungual hematomas, which will usually show a homogeneous pattern, although “you can also see peripheral fadings, streaks, and periungual hemorrhages,” she added.
It is important to monitor these patients “because melanomas can bleed,” she said. In-office photography, or even pictures taken by patients, can be used to track the hematoma to resolution.
When thinking about exogenous sources of pigment, in addition to clues from the history, a tip-off can be that the proximal nail fold is also discolored, Dr. Lipner pointed out. A wide variety of common and less-common culprits may crop up, including from tar, tobacco, henna and other hair dyes, potassium permanganate, and even newspaper print, she said. With an exogenous source, careful clinical and dermoscopic examination may show that the pigment does not extend all the way proximally to the lunula, although it may follow the outline of the proximal nail fold.
When fungus is the cause of LM, the band is often wider proximally and tapers distally, Dr. Lipner noted. While Trichophyton rubrum var. nigricans is a known culprit, nondermatophytes, such as Neoscytalidium dimidiatum, can also cause an LM that often runs along the proximal and lateral nail folds. “To make the diagnosis, sending a clipping to the dermatopathologist is helpful,” she said. Hyphae can often be seen on staining and culture, she said. Polymerase chain reaction “is also possible and very helpful for these nondermatophytes.”
Bacterial colonization of the nail bed can be a cause of LM. Pathogens can include Pseudomonas aeruginosa, which will often show the characteristic greenish tint. Klebsiella and Proteus species may result in more of a grayish-black discoloration. A history of wet work, such as farming and other agricultural and dairy occupations, as well as housekeeping work, increases the risk for bacterial colonization.
Commonly, a bacterial etiology will result in discoloration beginning at the lateral nail fold or at the juncture of the proximal and lateral nail folds. Dermoscopy will show irregular fading of the discoloration toward the medial aspect of the nail, and gram staining of affected clippings will show gram-negative rods.
Melanocytic causes of longitudinal melanonychia
The melanotic macule, sometimes called melanocytic activation, is the most common subtype of melanin-derived LM in adults, Dr. Lipner said. This benign condition results from increased melanin synthesis without an increase in the number of melanocytes, which will be evident on histopathologic examination of the nail bed. Any of a variety of triggers can provoke the increased pigment, which can range from endocrine disruptions to inflammatory conditions, such as psoriasis, to trauma (including nail biting or habit tics).
Pregnancy, normal ethnic variation, and chemotherapy administration are all also associated with melanotic macules. In any case, dermoscopy will show an LM characterized by a grayish background that contains darker grayish lines.
Melanocyte hyperplasia can also cause melanonychia, in which case the trick is sorting out which cases are benign and which are malignant, Dr. Lipner noted. And getting the diagnosis right in a timely fashion matters: “Ideally, we want to catch these melanomas in in situ stages where we can preserve the digit,” she said. “It’s been shown that there is no survival benefit for amputation versus en bloc excision for nail melanomas in situ.”
Nail matrix nevi are the most common cause of LM in children, Dr. Lipner said. Here, dermoscopy shows a brown background with brown lines, with regular color, thickness, and spacing.
On examination of a nail with a melanoma, “typically, we see features suggestive of melanoma but really no pathognomonic features,” she commented. Some signs that should prompt concern and a more thorough investigation, she said, include a dark brown or black band of LM; lack of homogeneity, such as the presence of lines of different colors; blurring of the borders of the pigmentation; and a triangular or wavering outline. Changes in the nail, such as fissuring or splitting, also are worrying, as is any associated discoloration of the periungual skin.
Dermoscopy may confirm the irregularity of the pigmentation pattern and show irregularly colored and spaced lines of varying thicknesses within the pigmented band. An LM caused by melanoma may also be marked by loss of parallelism within the pigmented band.
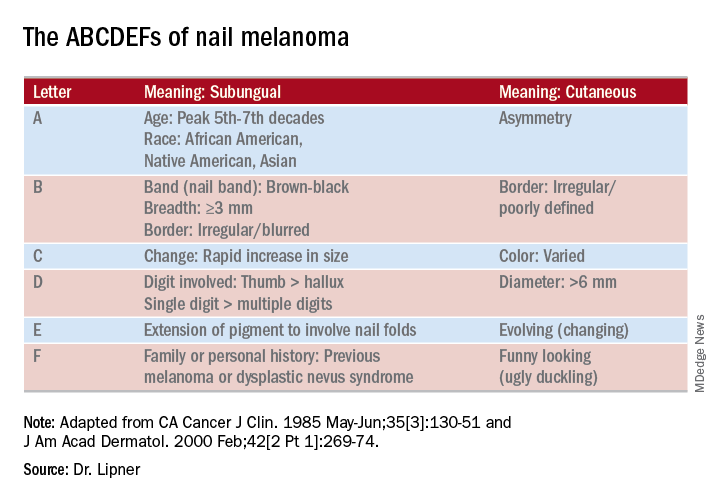
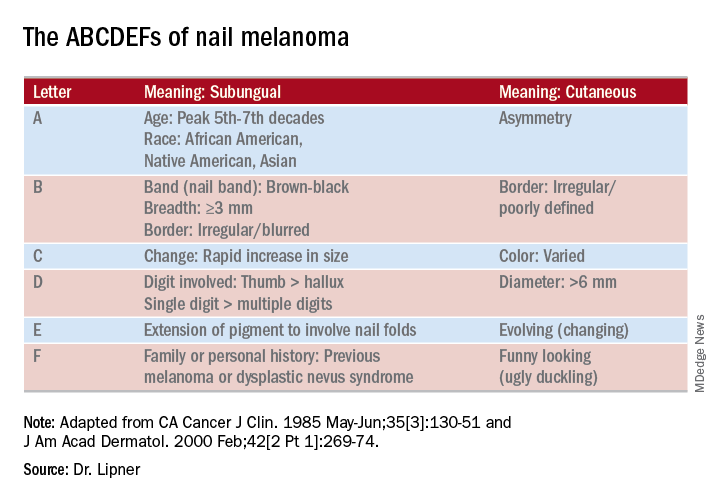
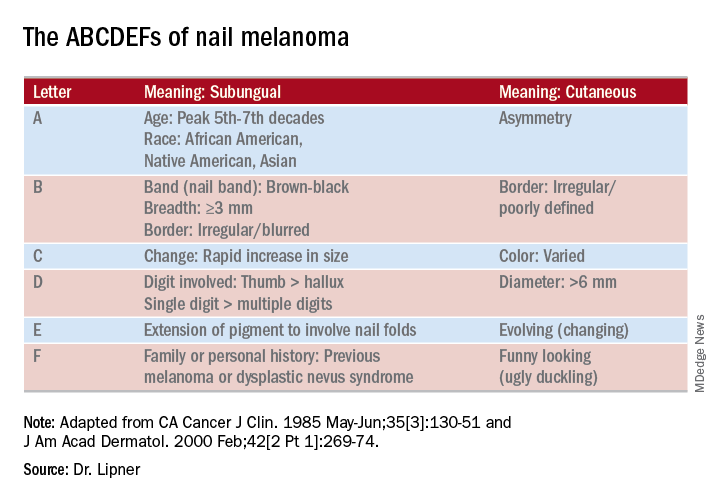
She pointed out that these concerning characteristics have been encapsulated in a mnemonic, first created in 2000, that’s meant to mirror the ABCDs of nonnail melanoma detection (J Am Acad Dermatol. Feb 2000;42[2 Pt 1]:269-74). Her survey found that overall, just one in four (24.8%) of respondents knew of the mnemonic for subungual melanomas.
Dr. Lipner reported that she has received research support from MOE Medical Devices and has served as a consultant to BAKO Therapeutics.
SOURCE: Lipner S. Summer AAD 2018, Presentation F004.
CHICAGO – A discolored nail can give even seasoned dermatologists pause: Is the cause exogenous? Fungal or bacterial, perhaps? Could it be a subungual melanoma? Should it be followed, clipped, or biopsied? of the American Academy of Dermatology summer meeting.
The session came after a recent nationwide survey performed by Dr. Lipner and her collaborators who asked dermatologists at different practice stages how confident they were in the diagnosis and management of melanonychia. “On the whole, they were not very confident at all,” said Dr. Lipner, director of the nail division at Cornell University, New York.
Of 142 dermatology residents, as well as 58 junior and 199 senior attending dermatologists, just 18.2% performed nail exams at each visit, and most (58%) only looked at nails during the total body skin exam. Over half (62%) of resident physicians reported feeling not confident about melanonychia diagnosis and management, while that figure dropped to 8.6% for senior attending physicians. Still, most senior physicians (64.3%) were just “fairly confident” in their melanonychia skills (J Am Acad Dermatol. 2017 May;76[5]:994-6).
Tools of the trade
Dermoscopy can be an invaluable tool for determining the cause of longitudinal melanonychia (LM). “Contact dermoscopy is helpful, so I always have ultrasound gel available,” Dr. Lipner said. “The gel makes the nail more of a flat surface,” which makes accurate viewing easier. Other useful tools include a double-action nail clipper, which, she said, is a worthwhile investment.
Because patients who are concerned about one of their nails will often come to their appointment with nail polish still on the other nails, Dr. Lipner always has polish remover pads available in the office. It’s important to be able to see all nails, she said, but she and her collaborators, including first author Pierre Halteh, MD, who was then a medical student at Cornell, discovered from their survey that “few physicians (32/402; 8%) asked their patients to remove nail polish at every visit.”
Nonmelanocytic causes of LM
Longitudinal melanonychias can have a nonmelanocytic etiology, which can range from subungual hematomas to pseudomonas and fungal infections to exogenous pigment.
Overall, subungual hematomas are the most common cause of melanonychia, although longitudinal hematomas are not commonly seen. The more remote the causative trauma, the darker the subungual discoloration, Dr. Lipner said. “Dermoscopy is very helpful” for subungual hematomas, which will usually show a homogeneous pattern, although “you can also see peripheral fadings, streaks, and periungual hemorrhages,” she added.
It is important to monitor these patients “because melanomas can bleed,” she said. In-office photography, or even pictures taken by patients, can be used to track the hematoma to resolution.
When thinking about exogenous sources of pigment, in addition to clues from the history, a tip-off can be that the proximal nail fold is also discolored, Dr. Lipner pointed out. A wide variety of common and less-common culprits may crop up, including from tar, tobacco, henna and other hair dyes, potassium permanganate, and even newspaper print, she said. With an exogenous source, careful clinical and dermoscopic examination may show that the pigment does not extend all the way proximally to the lunula, although it may follow the outline of the proximal nail fold.
When fungus is the cause of LM, the band is often wider proximally and tapers distally, Dr. Lipner noted. While Trichophyton rubrum var. nigricans is a known culprit, nondermatophytes, such as Neoscytalidium dimidiatum, can also cause an LM that often runs along the proximal and lateral nail folds. “To make the diagnosis, sending a clipping to the dermatopathologist is helpful,” she said. Hyphae can often be seen on staining and culture, she said. Polymerase chain reaction “is also possible and very helpful for these nondermatophytes.”
Bacterial colonization of the nail bed can be a cause of LM. Pathogens can include Pseudomonas aeruginosa, which will often show the characteristic greenish tint. Klebsiella and Proteus species may result in more of a grayish-black discoloration. A history of wet work, such as farming and other agricultural and dairy occupations, as well as housekeeping work, increases the risk for bacterial colonization.
Commonly, a bacterial etiology will result in discoloration beginning at the lateral nail fold or at the juncture of the proximal and lateral nail folds. Dermoscopy will show irregular fading of the discoloration toward the medial aspect of the nail, and gram staining of affected clippings will show gram-negative rods.
Melanocytic causes of longitudinal melanonychia
The melanotic macule, sometimes called melanocytic activation, is the most common subtype of melanin-derived LM in adults, Dr. Lipner said. This benign condition results from increased melanin synthesis without an increase in the number of melanocytes, which will be evident on histopathologic examination of the nail bed. Any of a variety of triggers can provoke the increased pigment, which can range from endocrine disruptions to inflammatory conditions, such as psoriasis, to trauma (including nail biting or habit tics).
Pregnancy, normal ethnic variation, and chemotherapy administration are all also associated with melanotic macules. In any case, dermoscopy will show an LM characterized by a grayish background that contains darker grayish lines.
Melanocyte hyperplasia can also cause melanonychia, in which case the trick is sorting out which cases are benign and which are malignant, Dr. Lipner noted. And getting the diagnosis right in a timely fashion matters: “Ideally, we want to catch these melanomas in in situ stages where we can preserve the digit,” she said. “It’s been shown that there is no survival benefit for amputation versus en bloc excision for nail melanomas in situ.”
Nail matrix nevi are the most common cause of LM in children, Dr. Lipner said. Here, dermoscopy shows a brown background with brown lines, with regular color, thickness, and spacing.
On examination of a nail with a melanoma, “typically, we see features suggestive of melanoma but really no pathognomonic features,” she commented. Some signs that should prompt concern and a more thorough investigation, she said, include a dark brown or black band of LM; lack of homogeneity, such as the presence of lines of different colors; blurring of the borders of the pigmentation; and a triangular or wavering outline. Changes in the nail, such as fissuring or splitting, also are worrying, as is any associated discoloration of the periungual skin.
Dermoscopy may confirm the irregularity of the pigmentation pattern and show irregularly colored and spaced lines of varying thicknesses within the pigmented band. An LM caused by melanoma may also be marked by loss of parallelism within the pigmented band.
She pointed out that these concerning characteristics have been encapsulated in a mnemonic, first created in 2000, that’s meant to mirror the ABCDs of nonnail melanoma detection (J Am Acad Dermatol. Feb 2000;42[2 Pt 1]:269-74). Her survey found that overall, just one in four (24.8%) of respondents knew of the mnemonic for subungual melanomas.
Dr. Lipner reported that she has received research support from MOE Medical Devices and has served as a consultant to BAKO Therapeutics.
SOURCE: Lipner S. Summer AAD 2018, Presentation F004.
CHICAGO – A discolored nail can give even seasoned dermatologists pause: Is the cause exogenous? Fungal or bacterial, perhaps? Could it be a subungual melanoma? Should it be followed, clipped, or biopsied? of the American Academy of Dermatology summer meeting.
The session came after a recent nationwide survey performed by Dr. Lipner and her collaborators who asked dermatologists at different practice stages how confident they were in the diagnosis and management of melanonychia. “On the whole, they were not very confident at all,” said Dr. Lipner, director of the nail division at Cornell University, New York.
Of 142 dermatology residents, as well as 58 junior and 199 senior attending dermatologists, just 18.2% performed nail exams at each visit, and most (58%) only looked at nails during the total body skin exam. Over half (62%) of resident physicians reported feeling not confident about melanonychia diagnosis and management, while that figure dropped to 8.6% for senior attending physicians. Still, most senior physicians (64.3%) were just “fairly confident” in their melanonychia skills (J Am Acad Dermatol. 2017 May;76[5]:994-6).
Tools of the trade
Dermoscopy can be an invaluable tool for determining the cause of longitudinal melanonychia (LM). “Contact dermoscopy is helpful, so I always have ultrasound gel available,” Dr. Lipner said. “The gel makes the nail more of a flat surface,” which makes accurate viewing easier. Other useful tools include a double-action nail clipper, which, she said, is a worthwhile investment.
Because patients who are concerned about one of their nails will often come to their appointment with nail polish still on the other nails, Dr. Lipner always has polish remover pads available in the office. It’s important to be able to see all nails, she said, but she and her collaborators, including first author Pierre Halteh, MD, who was then a medical student at Cornell, discovered from their survey that “few physicians (32/402; 8%) asked their patients to remove nail polish at every visit.”
Nonmelanocytic causes of LM
Longitudinal melanonychias can have a nonmelanocytic etiology, which can range from subungual hematomas to pseudomonas and fungal infections to exogenous pigment.
Overall, subungual hematomas are the most common cause of melanonychia, although longitudinal hematomas are not commonly seen. The more remote the causative trauma, the darker the subungual discoloration, Dr. Lipner said. “Dermoscopy is very helpful” for subungual hematomas, which will usually show a homogeneous pattern, although “you can also see peripheral fadings, streaks, and periungual hemorrhages,” she added.
It is important to monitor these patients “because melanomas can bleed,” she said. In-office photography, or even pictures taken by patients, can be used to track the hematoma to resolution.
When thinking about exogenous sources of pigment, in addition to clues from the history, a tip-off can be that the proximal nail fold is also discolored, Dr. Lipner pointed out. A wide variety of common and less-common culprits may crop up, including from tar, tobacco, henna and other hair dyes, potassium permanganate, and even newspaper print, she said. With an exogenous source, careful clinical and dermoscopic examination may show that the pigment does not extend all the way proximally to the lunula, although it may follow the outline of the proximal nail fold.
When fungus is the cause of LM, the band is often wider proximally and tapers distally, Dr. Lipner noted. While Trichophyton rubrum var. nigricans is a known culprit, nondermatophytes, such as Neoscytalidium dimidiatum, can also cause an LM that often runs along the proximal and lateral nail folds. “To make the diagnosis, sending a clipping to the dermatopathologist is helpful,” she said. Hyphae can often be seen on staining and culture, she said. Polymerase chain reaction “is also possible and very helpful for these nondermatophytes.”
Bacterial colonization of the nail bed can be a cause of LM. Pathogens can include Pseudomonas aeruginosa, which will often show the characteristic greenish tint. Klebsiella and Proteus species may result in more of a grayish-black discoloration. A history of wet work, such as farming and other agricultural and dairy occupations, as well as housekeeping work, increases the risk for bacterial colonization.
Commonly, a bacterial etiology will result in discoloration beginning at the lateral nail fold or at the juncture of the proximal and lateral nail folds. Dermoscopy will show irregular fading of the discoloration toward the medial aspect of the nail, and gram staining of affected clippings will show gram-negative rods.
Melanocytic causes of longitudinal melanonychia
The melanotic macule, sometimes called melanocytic activation, is the most common subtype of melanin-derived LM in adults, Dr. Lipner said. This benign condition results from increased melanin synthesis without an increase in the number of melanocytes, which will be evident on histopathologic examination of the nail bed. Any of a variety of triggers can provoke the increased pigment, which can range from endocrine disruptions to inflammatory conditions, such as psoriasis, to trauma (including nail biting or habit tics).
Pregnancy, normal ethnic variation, and chemotherapy administration are all also associated with melanotic macules. In any case, dermoscopy will show an LM characterized by a grayish background that contains darker grayish lines.
Melanocyte hyperplasia can also cause melanonychia, in which case the trick is sorting out which cases are benign and which are malignant, Dr. Lipner noted. And getting the diagnosis right in a timely fashion matters: “Ideally, we want to catch these melanomas in in situ stages where we can preserve the digit,” she said. “It’s been shown that there is no survival benefit for amputation versus en bloc excision for nail melanomas in situ.”
Nail matrix nevi are the most common cause of LM in children, Dr. Lipner said. Here, dermoscopy shows a brown background with brown lines, with regular color, thickness, and spacing.
On examination of a nail with a melanoma, “typically, we see features suggestive of melanoma but really no pathognomonic features,” she commented. Some signs that should prompt concern and a more thorough investigation, she said, include a dark brown or black band of LM; lack of homogeneity, such as the presence of lines of different colors; blurring of the borders of the pigmentation; and a triangular or wavering outline. Changes in the nail, such as fissuring or splitting, also are worrying, as is any associated discoloration of the periungual skin.
Dermoscopy may confirm the irregularity of the pigmentation pattern and show irregularly colored and spaced lines of varying thicknesses within the pigmented band. An LM caused by melanoma may also be marked by loss of parallelism within the pigmented band.
She pointed out that these concerning characteristics have been encapsulated in a mnemonic, first created in 2000, that’s meant to mirror the ABCDs of nonnail melanoma detection (J Am Acad Dermatol. Feb 2000;42[2 Pt 1]:269-74). Her survey found that overall, just one in four (24.8%) of respondents knew of the mnemonic for subungual melanomas.
Dr. Lipner reported that she has received research support from MOE Medical Devices and has served as a consultant to BAKO Therapeutics.
SOURCE: Lipner S. Summer AAD 2018, Presentation F004.
EXPERT ANALYSIS FROM SUMMER AAD 2018
Taking the sting out of nail surgery: Postoperative pain pearls
CHICAGO – In a busy clinic it can be hard to find the time to stop, talk, and listen. But doing so will “pay dividends in time spent later – and in reduced complications” of nail surgery, according to Molly A. Hinshaw, MD.
Dr. Hinshaw, director of the nail clinic at the University of Wisconsin–Madison, shared her
“One pearl is the importance of patient education before we start,” Dr. Hinshaw said. Preoperatively, she takes time to talk through the entire surgery and expected postoperative course. Critically, she reassures patients that pain will be controlled; she also reviews in detail what the pharmacologic and nonpharmacologic pain control strategies will be.
In addition, it’s important to address patients’ natural anxiety about what the surgical site will look and feel like and how healing will progress, particularly in those first few days after surgery. “I offer a first dressing change in my practice, either at 24 or 48 hours. This can be very anxiolytic for the patient,” she said.
At the preoperative stage, Dr. Hinshaw also tells patients that, from a healing and pain management standpoint, to make sure they plan “to have a restful 48 hours after surgery.” Her patient instructions for the immediate postoperative period include keeping the limb elevated and avoiding unnecessary activity with the affected limb while the digit, whether a finger or toe, is still anesthetized. To stay on top of the pain, the appropriate oral pain medication should be started once sensation starts to return to the digit. She recommends patients also take a dose of their pain medication at bedtime, as this will help them get a restful night of sleep.
“One thing that I’ve learned over the years is that throbbing and a little bit of swelling after surgery is not uncommon,” said Dr. Hinshaw, who uses elastic self-adherent wrap for the top layer of wound dressings after nail surgery. She tells her patients, “if you’re feeling throbbing, you’re welcome to unwrap it and rewrap it more loosely.” Just giving the patient the ability to find a comfortable level of pressure on the affected digit is often enough to alleviate the throbbing, as opposed to treating that throbbing with pain medication.
Dr. Hinshaw said she’s learned to tailor her postoperative analgesia to the surgery and to the patient. With all patients, she is sure to make medication and dosing choices that take comorbidities and potential drug-drug interactions into account. She does not ask patients to stop anticoagulation before nail procedures.
For phenolization procedures and punch biopsies, she’ll advise patients to use acetaminophen or NSAIDs. Some procedures are going to have a more painful recovery course, said Dr. Hinshaw, so she’ll use an opioid such as hydrocodone with acetaminophen for shave excisions and fusiform longitudinal excisions.
The physician and patient can also plan ahead for a brief course of more potent opioids for some procedures. “Certainly for lateral longitudinal excisions, they will need narcotic pain management for at least 48 hours after surgery,” she noted. “It’s a painful surgery.”
Other procedures that will need more postoperative analgesia include flaps and nail unit grafts, she said. In general, NSAIDs are useful to add after the first 24 hours. In addition, “I always call my patients the day after surgery to see how they’re doing. This helps identify any issues and questions early and is comforting to the patient,” she added.
Dr. Hinshaw disclosed that she has an ownership stake in and sits on the board of directors of Accure Medical.
CHICAGO – In a busy clinic it can be hard to find the time to stop, talk, and listen. But doing so will “pay dividends in time spent later – and in reduced complications” of nail surgery, according to Molly A. Hinshaw, MD.
Dr. Hinshaw, director of the nail clinic at the University of Wisconsin–Madison, shared her
“One pearl is the importance of patient education before we start,” Dr. Hinshaw said. Preoperatively, she takes time to talk through the entire surgery and expected postoperative course. Critically, she reassures patients that pain will be controlled; she also reviews in detail what the pharmacologic and nonpharmacologic pain control strategies will be.
In addition, it’s important to address patients’ natural anxiety about what the surgical site will look and feel like and how healing will progress, particularly in those first few days after surgery. “I offer a first dressing change in my practice, either at 24 or 48 hours. This can be very anxiolytic for the patient,” she said.
At the preoperative stage, Dr. Hinshaw also tells patients that, from a healing and pain management standpoint, to make sure they plan “to have a restful 48 hours after surgery.” Her patient instructions for the immediate postoperative period include keeping the limb elevated and avoiding unnecessary activity with the affected limb while the digit, whether a finger or toe, is still anesthetized. To stay on top of the pain, the appropriate oral pain medication should be started once sensation starts to return to the digit. She recommends patients also take a dose of their pain medication at bedtime, as this will help them get a restful night of sleep.
“One thing that I’ve learned over the years is that throbbing and a little bit of swelling after surgery is not uncommon,” said Dr. Hinshaw, who uses elastic self-adherent wrap for the top layer of wound dressings after nail surgery. She tells her patients, “if you’re feeling throbbing, you’re welcome to unwrap it and rewrap it more loosely.” Just giving the patient the ability to find a comfortable level of pressure on the affected digit is often enough to alleviate the throbbing, as opposed to treating that throbbing with pain medication.
Dr. Hinshaw said she’s learned to tailor her postoperative analgesia to the surgery and to the patient. With all patients, she is sure to make medication and dosing choices that take comorbidities and potential drug-drug interactions into account. She does not ask patients to stop anticoagulation before nail procedures.
For phenolization procedures and punch biopsies, she’ll advise patients to use acetaminophen or NSAIDs. Some procedures are going to have a more painful recovery course, said Dr. Hinshaw, so she’ll use an opioid such as hydrocodone with acetaminophen for shave excisions and fusiform longitudinal excisions.
The physician and patient can also plan ahead for a brief course of more potent opioids for some procedures. “Certainly for lateral longitudinal excisions, they will need narcotic pain management for at least 48 hours after surgery,” she noted. “It’s a painful surgery.”
Other procedures that will need more postoperative analgesia include flaps and nail unit grafts, she said. In general, NSAIDs are useful to add after the first 24 hours. In addition, “I always call my patients the day after surgery to see how they’re doing. This helps identify any issues and questions early and is comforting to the patient,” she added.
Dr. Hinshaw disclosed that she has an ownership stake in and sits on the board of directors of Accure Medical.
CHICAGO – In a busy clinic it can be hard to find the time to stop, talk, and listen. But doing so will “pay dividends in time spent later – and in reduced complications” of nail surgery, according to Molly A. Hinshaw, MD.
Dr. Hinshaw, director of the nail clinic at the University of Wisconsin–Madison, shared her
“One pearl is the importance of patient education before we start,” Dr. Hinshaw said. Preoperatively, she takes time to talk through the entire surgery and expected postoperative course. Critically, she reassures patients that pain will be controlled; she also reviews in detail what the pharmacologic and nonpharmacologic pain control strategies will be.
In addition, it’s important to address patients’ natural anxiety about what the surgical site will look and feel like and how healing will progress, particularly in those first few days after surgery. “I offer a first dressing change in my practice, either at 24 or 48 hours. This can be very anxiolytic for the patient,” she said.
At the preoperative stage, Dr. Hinshaw also tells patients that, from a healing and pain management standpoint, to make sure they plan “to have a restful 48 hours after surgery.” Her patient instructions for the immediate postoperative period include keeping the limb elevated and avoiding unnecessary activity with the affected limb while the digit, whether a finger or toe, is still anesthetized. To stay on top of the pain, the appropriate oral pain medication should be started once sensation starts to return to the digit. She recommends patients also take a dose of their pain medication at bedtime, as this will help them get a restful night of sleep.
“One thing that I’ve learned over the years is that throbbing and a little bit of swelling after surgery is not uncommon,” said Dr. Hinshaw, who uses elastic self-adherent wrap for the top layer of wound dressings after nail surgery. She tells her patients, “if you’re feeling throbbing, you’re welcome to unwrap it and rewrap it more loosely.” Just giving the patient the ability to find a comfortable level of pressure on the affected digit is often enough to alleviate the throbbing, as opposed to treating that throbbing with pain medication.
Dr. Hinshaw said she’s learned to tailor her postoperative analgesia to the surgery and to the patient. With all patients, she is sure to make medication and dosing choices that take comorbidities and potential drug-drug interactions into account. She does not ask patients to stop anticoagulation before nail procedures.
For phenolization procedures and punch biopsies, she’ll advise patients to use acetaminophen or NSAIDs. Some procedures are going to have a more painful recovery course, said Dr. Hinshaw, so she’ll use an opioid such as hydrocodone with acetaminophen for shave excisions and fusiform longitudinal excisions.
The physician and patient can also plan ahead for a brief course of more potent opioids for some procedures. “Certainly for lateral longitudinal excisions, they will need narcotic pain management for at least 48 hours after surgery,” she noted. “It’s a painful surgery.”
Other procedures that will need more postoperative analgesia include flaps and nail unit grafts, she said. In general, NSAIDs are useful to add after the first 24 hours. In addition, “I always call my patients the day after surgery to see how they’re doing. This helps identify any issues and questions early and is comforting to the patient,” she added.
Dr. Hinshaw disclosed that she has an ownership stake in and sits on the board of directors of Accure Medical.
EXPERT ANALYSIS FROM SUMMER AAD 2018
How to watch – and when to biopsy – atypical nevi
CHICAGO – Among the many difficult decisions dermatologists have to make, some of the more challenging involve caring for patients with atypical melanocytic lesions. A session at the summer meeting of the American Academy of Dermatology provided some guidance for surveillance of these patients.
Caroline C. Kim, MD, directs the pigmented lesion clinic at Beth Israel Deaconess Medical Center, Boston, and shared the evidence base for her management schema, along with some clinical pearls. No dermatologist ever wants to miss a melanoma, she acknowledged. “We want to avoid those scenarios but not make people feel like Swiss cheese” from multiple biopsies, she said during her presentation.
One key concept that can help physicians find the balance, she said, is that although the presence of atypical or dysplastic nevi increases the risk for melanoma in a given patient, the actual transformation rate of dysplastic nevi to melanomas is not known. In fact, she said, between 50% and 75% of melanomas may arise de novo.
From a dermatopathologic perspective, nevi exist along a continuum of mild to moderate to severe dysplasia, and some lesions are melanomas. But mildly dysplastic nevi are not fated to continue a transformation to increasingly severely dysplastic ones, or to melanomas.
Bringing these ideas to the patient discussion means that one should avoid ever calling a dysplastic nevus “precancerous,” said Dr. Kim; not only is this inaccurate, but it is unnecessarily anxiety provoking, she said.
Within this framework, . Each patient will have a pattern, or several patterns, that typify their nevi. Though the markings may be “atypical,” they’ll have some consistency; if the nevus has several neighbors that look just like it, it’s much less likely to be melanoma. “If they are matching partners, it’s more likely that it’s your typical nevus pattern,” said Dr. Kim, also an assistant professor of dermatology at Harvard Medical School, Boston.
By contrast, some lesions stand out from the patient’s other atypical nevi. They may be larger, darker, more elevated, but sometimes, “Even from the doorway, they just stand out,” Dr. Kim said. And these dual concepts of signature patterns and ugly ducklings are useful to talk over with patients, she said. “It’s so easy for patients to grab on to – they totally get it.”
“Use dermoscopy” when you get to the detailed skin exam, she said. “Data have shown that as clinicians, we are pretty good at picking up melanomas ... But with dermoscopy, our detection rate goes up to 70%-95%,” Dr. Kim said. The caveat is that dermoscopy without proper training is a dangerous tool: Several studies have shown that melanoma detection rates drop compared to the naked eye when dermoscopy is performed by untrained users, she said. “Training matters.”
A further tool to help train the eye and mind to recognize benign and malignant patterns when performing dermoscopy of atypical nevi is a now-classic paper that maps these patterns out, she said (Dermatol Surg. 2007;33[11]:1388-91).
“Beware of de novo and changing lesions,” Dr. Kim said. “A picture truly is worth a thousand words” for tracking these, she said.
Total body digital photography, if it’s available, is the best way to track subtle changes, and to spot new lesions as they crop up, said Dr. Kim. In head-to-head studies with dermoscopy and visual exam alone, digital photography can reduce the number of lesions excised, detect early melanoma, and reduce patient anxiety. One study found a 3.8-fold reduction in the mean rate of nevus biopsies when total body digital photography was used, she said (J Am Acad Dermatol. 2016 Mar. doi: 10.1016/j.jaad.2016.02.1152).
A patient care pearl Dr. Kim shared is that she’ll ask patients for their smartphones and take a photograph of the patients’ backs with those phones. This lets them have a handy reference image for monitoring their own skin in the intervals between visits. But make sure, she said, that patients know that “all change is not bad change – you can get new nevi through your 50s.
“Consider sharing care with a local pigmented lesion clinic” if digital photography is not available at your site, said Dr. Kim. She does this for several of her patients, alternating visits with the primary dermatologist.
When should you perform a biopsy?
“You don’t need to biopsy an atypical nevus to call it atypical. You biopsy lesions if you’re suspicious for calling it melanoma,” Dr. Kim said. Removal also can be considered if, for example, a patient lives alone and the nevi of concern are on her back so home monitoring is a challenge, she said.
Once you’ve decided to biopsy, a narrow excisional biopsy with saucerization and 1- to 3-mm margins is preferred when there’s a high suspicion for melanoma, said Dr. Kim, citing a study that found that 2-mm margins using this method yielded an 87% rate of clear pathologic specimen margins in dysplastic nevi (J Am Acad Dermatol. 2017 Dec;77[6]:1096-9). There is some leeway in the guidelines, but “the preferred technique is a narrow excisional biopsy when you are worried,” she said.
There may be times when a partial or incisional biopsy is a rational choice, as when lesions are very large, located on the face or acral areas, or when suspicion for melanoma is low. “If you do partial biopsies, you really have to be aware of the limitations” of the technique since it may miss the nidus of melanoma within an otherwise bland lesion, Dr. Kim pointed out.
And don’t forget to plan your closure with future follow-up in mind: Dr. Kim related that she’d seen a patient for melanoma who’d had the large excisional biopsy performed elsewhere; the patient’s site was closed with an advancement flap, which made sentinel node biopsy impossible.
When the results come back, then what?
Studies have found that atypical nevi are characterized differently at different sites and that management strategies vary geographically, Dr. Kim said. “There’s a need for large-scale data to further investigate the role of observation versus re-excision of dysplastic nevi,” and a multicenter study is underway to do just that, she said, under the auspices of the Pigmented Lesion Subcommittee of the Melanoma Prevention Working Group (ECOG/SWOG).
That same subcommittee has issued a consensus statement for dealing with histologically positive excisional biopsy margins. For mildly dysplastic lesions without clinically observable residual pigment, observation is preferred. Severely dysplastic lesions with unpigmented margins should be re-excised, says the statement (JAMA Dermatol. 2015;151[2]:212-18).
For the intermediate lesions, the group recommended that a reasonable option is to observe a moderately dysplastic nevus site that’s been excisionally biopsied with a finding of positive margins, while acknowledging that more data are needed.
All biopsy sites should be followed for regrowth, though recurrence of pigment alone doesn’t necessarily mean another excision is in the patient’s future, Dr. Kim said.
She reported no conflicts of interest.
SOURCE: Kim C. Summer AAD 2018, Presentation F014.
CHICAGO – Among the many difficult decisions dermatologists have to make, some of the more challenging involve caring for patients with atypical melanocytic lesions. A session at the summer meeting of the American Academy of Dermatology provided some guidance for surveillance of these patients.
Caroline C. Kim, MD, directs the pigmented lesion clinic at Beth Israel Deaconess Medical Center, Boston, and shared the evidence base for her management schema, along with some clinical pearls. No dermatologist ever wants to miss a melanoma, she acknowledged. “We want to avoid those scenarios but not make people feel like Swiss cheese” from multiple biopsies, she said during her presentation.
One key concept that can help physicians find the balance, she said, is that although the presence of atypical or dysplastic nevi increases the risk for melanoma in a given patient, the actual transformation rate of dysplastic nevi to melanomas is not known. In fact, she said, between 50% and 75% of melanomas may arise de novo.
From a dermatopathologic perspective, nevi exist along a continuum of mild to moderate to severe dysplasia, and some lesions are melanomas. But mildly dysplastic nevi are not fated to continue a transformation to increasingly severely dysplastic ones, or to melanomas.
Bringing these ideas to the patient discussion means that one should avoid ever calling a dysplastic nevus “precancerous,” said Dr. Kim; not only is this inaccurate, but it is unnecessarily anxiety provoking, she said.
Within this framework, . Each patient will have a pattern, or several patterns, that typify their nevi. Though the markings may be “atypical,” they’ll have some consistency; if the nevus has several neighbors that look just like it, it’s much less likely to be melanoma. “If they are matching partners, it’s more likely that it’s your typical nevus pattern,” said Dr. Kim, also an assistant professor of dermatology at Harvard Medical School, Boston.
By contrast, some lesions stand out from the patient’s other atypical nevi. They may be larger, darker, more elevated, but sometimes, “Even from the doorway, they just stand out,” Dr. Kim said. And these dual concepts of signature patterns and ugly ducklings are useful to talk over with patients, she said. “It’s so easy for patients to grab on to – they totally get it.”
“Use dermoscopy” when you get to the detailed skin exam, she said. “Data have shown that as clinicians, we are pretty good at picking up melanomas ... But with dermoscopy, our detection rate goes up to 70%-95%,” Dr. Kim said. The caveat is that dermoscopy without proper training is a dangerous tool: Several studies have shown that melanoma detection rates drop compared to the naked eye when dermoscopy is performed by untrained users, she said. “Training matters.”
A further tool to help train the eye and mind to recognize benign and malignant patterns when performing dermoscopy of atypical nevi is a now-classic paper that maps these patterns out, she said (Dermatol Surg. 2007;33[11]:1388-91).
“Beware of de novo and changing lesions,” Dr. Kim said. “A picture truly is worth a thousand words” for tracking these, she said.
Total body digital photography, if it’s available, is the best way to track subtle changes, and to spot new lesions as they crop up, said Dr. Kim. In head-to-head studies with dermoscopy and visual exam alone, digital photography can reduce the number of lesions excised, detect early melanoma, and reduce patient anxiety. One study found a 3.8-fold reduction in the mean rate of nevus biopsies when total body digital photography was used, she said (J Am Acad Dermatol. 2016 Mar. doi: 10.1016/j.jaad.2016.02.1152).
A patient care pearl Dr. Kim shared is that she’ll ask patients for their smartphones and take a photograph of the patients’ backs with those phones. This lets them have a handy reference image for monitoring their own skin in the intervals between visits. But make sure, she said, that patients know that “all change is not bad change – you can get new nevi through your 50s.
“Consider sharing care with a local pigmented lesion clinic” if digital photography is not available at your site, said Dr. Kim. She does this for several of her patients, alternating visits with the primary dermatologist.
When should you perform a biopsy?
“You don’t need to biopsy an atypical nevus to call it atypical. You biopsy lesions if you’re suspicious for calling it melanoma,” Dr. Kim said. Removal also can be considered if, for example, a patient lives alone and the nevi of concern are on her back so home monitoring is a challenge, she said.
Once you’ve decided to biopsy, a narrow excisional biopsy with saucerization and 1- to 3-mm margins is preferred when there’s a high suspicion for melanoma, said Dr. Kim, citing a study that found that 2-mm margins using this method yielded an 87% rate of clear pathologic specimen margins in dysplastic nevi (J Am Acad Dermatol. 2017 Dec;77[6]:1096-9). There is some leeway in the guidelines, but “the preferred technique is a narrow excisional biopsy when you are worried,” she said.
There may be times when a partial or incisional biopsy is a rational choice, as when lesions are very large, located on the face or acral areas, or when suspicion for melanoma is low. “If you do partial biopsies, you really have to be aware of the limitations” of the technique since it may miss the nidus of melanoma within an otherwise bland lesion, Dr. Kim pointed out.
And don’t forget to plan your closure with future follow-up in mind: Dr. Kim related that she’d seen a patient for melanoma who’d had the large excisional biopsy performed elsewhere; the patient’s site was closed with an advancement flap, which made sentinel node biopsy impossible.
When the results come back, then what?
Studies have found that atypical nevi are characterized differently at different sites and that management strategies vary geographically, Dr. Kim said. “There’s a need for large-scale data to further investigate the role of observation versus re-excision of dysplastic nevi,” and a multicenter study is underway to do just that, she said, under the auspices of the Pigmented Lesion Subcommittee of the Melanoma Prevention Working Group (ECOG/SWOG).
That same subcommittee has issued a consensus statement for dealing with histologically positive excisional biopsy margins. For mildly dysplastic lesions without clinically observable residual pigment, observation is preferred. Severely dysplastic lesions with unpigmented margins should be re-excised, says the statement (JAMA Dermatol. 2015;151[2]:212-18).
For the intermediate lesions, the group recommended that a reasonable option is to observe a moderately dysplastic nevus site that’s been excisionally biopsied with a finding of positive margins, while acknowledging that more data are needed.
All biopsy sites should be followed for regrowth, though recurrence of pigment alone doesn’t necessarily mean another excision is in the patient’s future, Dr. Kim said.
She reported no conflicts of interest.
SOURCE: Kim C. Summer AAD 2018, Presentation F014.
CHICAGO – Among the many difficult decisions dermatologists have to make, some of the more challenging involve caring for patients with atypical melanocytic lesions. A session at the summer meeting of the American Academy of Dermatology provided some guidance for surveillance of these patients.
Caroline C. Kim, MD, directs the pigmented lesion clinic at Beth Israel Deaconess Medical Center, Boston, and shared the evidence base for her management schema, along with some clinical pearls. No dermatologist ever wants to miss a melanoma, she acknowledged. “We want to avoid those scenarios but not make people feel like Swiss cheese” from multiple biopsies, she said during her presentation.
One key concept that can help physicians find the balance, she said, is that although the presence of atypical or dysplastic nevi increases the risk for melanoma in a given patient, the actual transformation rate of dysplastic nevi to melanomas is not known. In fact, she said, between 50% and 75% of melanomas may arise de novo.
From a dermatopathologic perspective, nevi exist along a continuum of mild to moderate to severe dysplasia, and some lesions are melanomas. But mildly dysplastic nevi are not fated to continue a transformation to increasingly severely dysplastic ones, or to melanomas.
Bringing these ideas to the patient discussion means that one should avoid ever calling a dysplastic nevus “precancerous,” said Dr. Kim; not only is this inaccurate, but it is unnecessarily anxiety provoking, she said.
Within this framework, . Each patient will have a pattern, or several patterns, that typify their nevi. Though the markings may be “atypical,” they’ll have some consistency; if the nevus has several neighbors that look just like it, it’s much less likely to be melanoma. “If they are matching partners, it’s more likely that it’s your typical nevus pattern,” said Dr. Kim, also an assistant professor of dermatology at Harvard Medical School, Boston.
By contrast, some lesions stand out from the patient’s other atypical nevi. They may be larger, darker, more elevated, but sometimes, “Even from the doorway, they just stand out,” Dr. Kim said. And these dual concepts of signature patterns and ugly ducklings are useful to talk over with patients, she said. “It’s so easy for patients to grab on to – they totally get it.”
“Use dermoscopy” when you get to the detailed skin exam, she said. “Data have shown that as clinicians, we are pretty good at picking up melanomas ... But with dermoscopy, our detection rate goes up to 70%-95%,” Dr. Kim said. The caveat is that dermoscopy without proper training is a dangerous tool: Several studies have shown that melanoma detection rates drop compared to the naked eye when dermoscopy is performed by untrained users, she said. “Training matters.”
A further tool to help train the eye and mind to recognize benign and malignant patterns when performing dermoscopy of atypical nevi is a now-classic paper that maps these patterns out, she said (Dermatol Surg. 2007;33[11]:1388-91).
“Beware of de novo and changing lesions,” Dr. Kim said. “A picture truly is worth a thousand words” for tracking these, she said.
Total body digital photography, if it’s available, is the best way to track subtle changes, and to spot new lesions as they crop up, said Dr. Kim. In head-to-head studies with dermoscopy and visual exam alone, digital photography can reduce the number of lesions excised, detect early melanoma, and reduce patient anxiety. One study found a 3.8-fold reduction in the mean rate of nevus biopsies when total body digital photography was used, she said (J Am Acad Dermatol. 2016 Mar. doi: 10.1016/j.jaad.2016.02.1152).
A patient care pearl Dr. Kim shared is that she’ll ask patients for their smartphones and take a photograph of the patients’ backs with those phones. This lets them have a handy reference image for monitoring their own skin in the intervals between visits. But make sure, she said, that patients know that “all change is not bad change – you can get new nevi through your 50s.
“Consider sharing care with a local pigmented lesion clinic” if digital photography is not available at your site, said Dr. Kim. She does this for several of her patients, alternating visits with the primary dermatologist.
When should you perform a biopsy?
“You don’t need to biopsy an atypical nevus to call it atypical. You biopsy lesions if you’re suspicious for calling it melanoma,” Dr. Kim said. Removal also can be considered if, for example, a patient lives alone and the nevi of concern are on her back so home monitoring is a challenge, she said.
Once you’ve decided to biopsy, a narrow excisional biopsy with saucerization and 1- to 3-mm margins is preferred when there’s a high suspicion for melanoma, said Dr. Kim, citing a study that found that 2-mm margins using this method yielded an 87% rate of clear pathologic specimen margins in dysplastic nevi (J Am Acad Dermatol. 2017 Dec;77[6]:1096-9). There is some leeway in the guidelines, but “the preferred technique is a narrow excisional biopsy when you are worried,” she said.
There may be times when a partial or incisional biopsy is a rational choice, as when lesions are very large, located on the face or acral areas, or when suspicion for melanoma is low. “If you do partial biopsies, you really have to be aware of the limitations” of the technique since it may miss the nidus of melanoma within an otherwise bland lesion, Dr. Kim pointed out.
And don’t forget to plan your closure with future follow-up in mind: Dr. Kim related that she’d seen a patient for melanoma who’d had the large excisional biopsy performed elsewhere; the patient’s site was closed with an advancement flap, which made sentinel node biopsy impossible.
When the results come back, then what?
Studies have found that atypical nevi are characterized differently at different sites and that management strategies vary geographically, Dr. Kim said. “There’s a need for large-scale data to further investigate the role of observation versus re-excision of dysplastic nevi,” and a multicenter study is underway to do just that, she said, under the auspices of the Pigmented Lesion Subcommittee of the Melanoma Prevention Working Group (ECOG/SWOG).
That same subcommittee has issued a consensus statement for dealing with histologically positive excisional biopsy margins. For mildly dysplastic lesions without clinically observable residual pigment, observation is preferred. Severely dysplastic lesions with unpigmented margins should be re-excised, says the statement (JAMA Dermatol. 2015;151[2]:212-18).
For the intermediate lesions, the group recommended that a reasonable option is to observe a moderately dysplastic nevus site that’s been excisionally biopsied with a finding of positive margins, while acknowledging that more data are needed.
All biopsy sites should be followed for regrowth, though recurrence of pigment alone doesn’t necessarily mean another excision is in the patient’s future, Dr. Kim said.
She reported no conflicts of interest.
SOURCE: Kim C. Summer AAD 2018, Presentation F014.
EXPERT ANALYSIS FROM SUMMER AAD 2018
When fingernails are the clue to a bigger problem
CHICAGO – When a child or adolescent comes to the dermatologist’s office with a concern about fingernails or toenails, physician antennae may go up. “The world is different in the world of pediatrics – and even in the world of adolescents,” said Sheila Fallon Friedlander, MD.
In adults, the most common cause of nail dystrophy is tinea, but for younger pediatric patients, less than 1% of nail problems are attributable to fungus, so dermatologists may need to look further.
“It’s so important in kids to do a good history and physical exam,” said Dr. Friedlander, professor of dermatology and pediatrics at the University of California, San Diego. History-taking should include determining whether the condition has been present since birth and how nail appearance has changed over time.
For Dr. Friedlander, the approach to nail abnormalities includes a full head and skin exam. “I always look at the teeth, the hair, the skin,” she said; underlying bony anomalies also may surface. A complete exam often will turn up important clues if a syndrome underpins the nail abnormalities, she said, speaking at the American Academy of Dermatology summer meeting.
Her exemplar patient, she said, is a 19-year-old male who comes in with a parent because he’s bothered by his fingernails, which are dystrophic and small. A head-to-toe exam shows micronychia of both toes and fingers, with lunulae that are triangularly shaped. The hair, skin, and teeth of the patient all were normal in appearance. However, “The knees and elbows were odd,” Dr. Friedlander said.
This patient has nail-patella syndrome. “Even though it’s rare, I want you to think about it,” Dr. Friedlander said. The autosomal dominant condition is seen in about 1 in 50,000 patients. It’s thought to be caused by heterozygous loss-of-function mutations in gene LMX1B, she said, that codes for a LIM homeobox transcription factor 1 beta.
Though the small nails and triangular lunulae may be what brings the patient to the dermatologist’s office, a careful exam and one radiograph can pick up a tetrad of anomalies, Dr. Friedlander said. Abnormalities can be seen in both the knees and elbows; the patellae are often small, and may even be absent. In addition, a hip radiograph will show characteristic “horns” on the posterior iliac crests.
Coming back to the dermatologic exam, Dr. Friedlander said nails may be absent, hypoplastic, and dystrophic – but those are features that can be shared with other nail disorders, inherited and acquired. The pathognomonic finding for nail-patella syndrome is the presence of the triangular lunula, she said.
Now that the diagnosis has been made, Dr. Friedlander asked about this young man: “Where will you refer him?” Knowing the diagnosis means that there are a lot of calls for your staff to make, she said.
The patient with knee patella syndrome should be referred to an orthopedist to assess knees and elbows; radial head subluxation also is common in these patients, she said.
An ophthalmologic referral is important as well; hyperpigmentation of the pupillary margin – a “Lester iris” – can be seen, and increased rates of cataracts and glaucoma also are associated with nail-patella syndrome.
“,” Dr. Friedlander said. Up to half of nail-patella syndrome patients will have kidney involvement that initially presents with hematuria and proteinuria. Because the LMX1B mutation impairs how podocytes and glomerular filtration slits develop and function, up to 10% can develop end-stage renal failure, she said.
Parents also should be on the lookout for associated behavioral issues: “The other thing that’s interesting is that these kids have an increased risk of [attention-deficit/hyperactivity disorder] and major depression,” Dr. Friedlander said.
Dr. Friedlander reported that she had no relevant conflicts of interest.
SOURCE: Friedlander, S. Summer AAD 2018. Session F004.
CHICAGO – When a child or adolescent comes to the dermatologist’s office with a concern about fingernails or toenails, physician antennae may go up. “The world is different in the world of pediatrics – and even in the world of adolescents,” said Sheila Fallon Friedlander, MD.
In adults, the most common cause of nail dystrophy is tinea, but for younger pediatric patients, less than 1% of nail problems are attributable to fungus, so dermatologists may need to look further.
“It’s so important in kids to do a good history and physical exam,” said Dr. Friedlander, professor of dermatology and pediatrics at the University of California, San Diego. History-taking should include determining whether the condition has been present since birth and how nail appearance has changed over time.
For Dr. Friedlander, the approach to nail abnormalities includes a full head and skin exam. “I always look at the teeth, the hair, the skin,” she said; underlying bony anomalies also may surface. A complete exam often will turn up important clues if a syndrome underpins the nail abnormalities, she said, speaking at the American Academy of Dermatology summer meeting.
Her exemplar patient, she said, is a 19-year-old male who comes in with a parent because he’s bothered by his fingernails, which are dystrophic and small. A head-to-toe exam shows micronychia of both toes and fingers, with lunulae that are triangularly shaped. The hair, skin, and teeth of the patient all were normal in appearance. However, “The knees and elbows were odd,” Dr. Friedlander said.
This patient has nail-patella syndrome. “Even though it’s rare, I want you to think about it,” Dr. Friedlander said. The autosomal dominant condition is seen in about 1 in 50,000 patients. It’s thought to be caused by heterozygous loss-of-function mutations in gene LMX1B, she said, that codes for a LIM homeobox transcription factor 1 beta.
Though the small nails and triangular lunulae may be what brings the patient to the dermatologist’s office, a careful exam and one radiograph can pick up a tetrad of anomalies, Dr. Friedlander said. Abnormalities can be seen in both the knees and elbows; the patellae are often small, and may even be absent. In addition, a hip radiograph will show characteristic “horns” on the posterior iliac crests.
Coming back to the dermatologic exam, Dr. Friedlander said nails may be absent, hypoplastic, and dystrophic – but those are features that can be shared with other nail disorders, inherited and acquired. The pathognomonic finding for nail-patella syndrome is the presence of the triangular lunula, she said.
Now that the diagnosis has been made, Dr. Friedlander asked about this young man: “Where will you refer him?” Knowing the diagnosis means that there are a lot of calls for your staff to make, she said.
The patient with knee patella syndrome should be referred to an orthopedist to assess knees and elbows; radial head subluxation also is common in these patients, she said.
An ophthalmologic referral is important as well; hyperpigmentation of the pupillary margin – a “Lester iris” – can be seen, and increased rates of cataracts and glaucoma also are associated with nail-patella syndrome.
“,” Dr. Friedlander said. Up to half of nail-patella syndrome patients will have kidney involvement that initially presents with hematuria and proteinuria. Because the LMX1B mutation impairs how podocytes and glomerular filtration slits develop and function, up to 10% can develop end-stage renal failure, she said.
Parents also should be on the lookout for associated behavioral issues: “The other thing that’s interesting is that these kids have an increased risk of [attention-deficit/hyperactivity disorder] and major depression,” Dr. Friedlander said.
Dr. Friedlander reported that she had no relevant conflicts of interest.
SOURCE: Friedlander, S. Summer AAD 2018. Session F004.
CHICAGO – When a child or adolescent comes to the dermatologist’s office with a concern about fingernails or toenails, physician antennae may go up. “The world is different in the world of pediatrics – and even in the world of adolescents,” said Sheila Fallon Friedlander, MD.
In adults, the most common cause of nail dystrophy is tinea, but for younger pediatric patients, less than 1% of nail problems are attributable to fungus, so dermatologists may need to look further.
“It’s so important in kids to do a good history and physical exam,” said Dr. Friedlander, professor of dermatology and pediatrics at the University of California, San Diego. History-taking should include determining whether the condition has been present since birth and how nail appearance has changed over time.
For Dr. Friedlander, the approach to nail abnormalities includes a full head and skin exam. “I always look at the teeth, the hair, the skin,” she said; underlying bony anomalies also may surface. A complete exam often will turn up important clues if a syndrome underpins the nail abnormalities, she said, speaking at the American Academy of Dermatology summer meeting.
Her exemplar patient, she said, is a 19-year-old male who comes in with a parent because he’s bothered by his fingernails, which are dystrophic and small. A head-to-toe exam shows micronychia of both toes and fingers, with lunulae that are triangularly shaped. The hair, skin, and teeth of the patient all were normal in appearance. However, “The knees and elbows were odd,” Dr. Friedlander said.
This patient has nail-patella syndrome. “Even though it’s rare, I want you to think about it,” Dr. Friedlander said. The autosomal dominant condition is seen in about 1 in 50,000 patients. It’s thought to be caused by heterozygous loss-of-function mutations in gene LMX1B, she said, that codes for a LIM homeobox transcription factor 1 beta.
Though the small nails and triangular lunulae may be what brings the patient to the dermatologist’s office, a careful exam and one radiograph can pick up a tetrad of anomalies, Dr. Friedlander said. Abnormalities can be seen in both the knees and elbows; the patellae are often small, and may even be absent. In addition, a hip radiograph will show characteristic “horns” on the posterior iliac crests.
Coming back to the dermatologic exam, Dr. Friedlander said nails may be absent, hypoplastic, and dystrophic – but those are features that can be shared with other nail disorders, inherited and acquired. The pathognomonic finding for nail-patella syndrome is the presence of the triangular lunula, she said.
Now that the diagnosis has been made, Dr. Friedlander asked about this young man: “Where will you refer him?” Knowing the diagnosis means that there are a lot of calls for your staff to make, she said.
The patient with knee patella syndrome should be referred to an orthopedist to assess knees and elbows; radial head subluxation also is common in these patients, she said.
An ophthalmologic referral is important as well; hyperpigmentation of the pupillary margin – a “Lester iris” – can be seen, and increased rates of cataracts and glaucoma also are associated with nail-patella syndrome.
“,” Dr. Friedlander said. Up to half of nail-patella syndrome patients will have kidney involvement that initially presents with hematuria and proteinuria. Because the LMX1B mutation impairs how podocytes and glomerular filtration slits develop and function, up to 10% can develop end-stage renal failure, she said.
Parents also should be on the lookout for associated behavioral issues: “The other thing that’s interesting is that these kids have an increased risk of [attention-deficit/hyperactivity disorder] and major depression,” Dr. Friedlander said.
Dr. Friedlander reported that she had no relevant conflicts of interest.
SOURCE: Friedlander, S. Summer AAD 2018. Session F004.
REPORTING FROM SUMMER AAD 2018
In Ghana, SCD research is meeting patients on home turf
WASHINGTON – Sometimes, the hardest part of solving a problem is figuring out how to work around misaligned resources, and so it has been with sickle cell disease research.
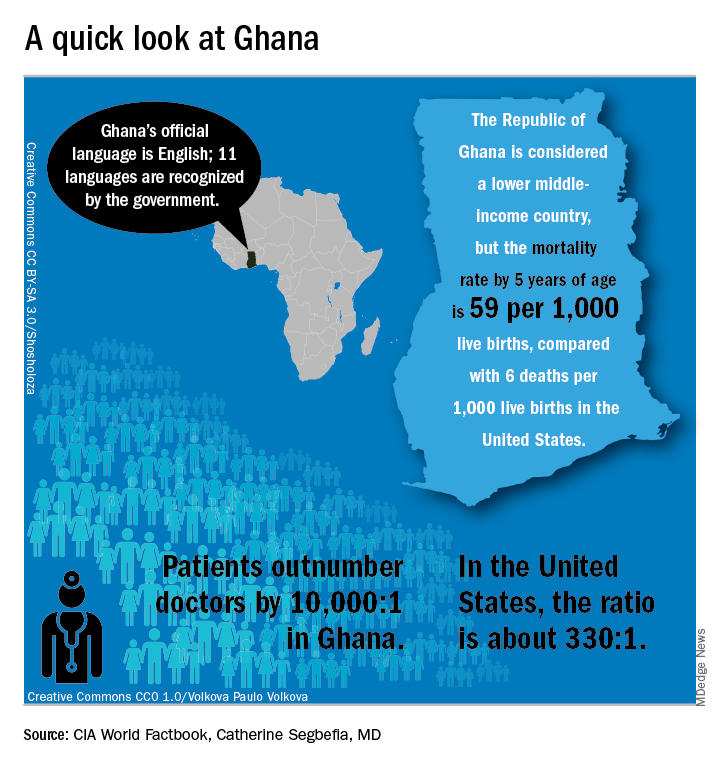
“From my point of view, what I call the geographical disparity in sickle cell disease research can be explained by the fact that the majority of affected individuals are living in the East, and the overwhelming majority of the research takes place in the West,” said Solomon Ofori-Acquah, PhD. He and three physician collaborators from Ghana shared their roadmap to conducting clinical trials in West Africa during an “East Meets West” session of the annual symposium of the Foundation for Sickle Cell Disease Research.
In Ghana, not far from where scientists now believe the hemoglobin sickling mutation originated, fully 2% of newborns have SCD; this translates into 16,000 new cases per year in a population of just 28 million, compared with the 2,000 new SCD cases seen annually in the entire United States. And access even to proven therapies can be limited; historically, little to no clinical drug development work has been conducted in this part of the world.
In the United States, half of the SCD trials that were withdrawn or terminated listed recruitment and retention of study participants as a factor in the study’s discontinuation, said Amma Owusu-Ansah, MD. “I see what we are doing as a very feasible solution to the problem of inadequate accrual to studies in the U.S.,” said Dr. Owusu-Ansah, a hematologist at the University of Pittsburgh’s Center for Translational and International Hematology (CTIH), where she serves as clinical director.
From the African perspective, hosting clinical trials – and building a robust infrastructure to do so – may help alleviate the delay in translation of disease-modifying therapies for SCD to Africa, where most people with the disease live, she said.
An existing example of resource sharing is the Human Heredity & Health in Africa (H3Africa) initiative, said Dr. Ofori-Acquah, who directs the CTIH and also holds an appointment at the University of Ghana. The project, funded by the National Institutes of Health and the Wellcome Trust, “aims to facilitate a contemporary research approach to the study of genomics and environmental determinants of common diseases with the goal of improving the health of African populations,” according to the H3Africa website. Within this framework of 40 research centers conducting genomics research and biobanking, several discrete projects aim to expand knowledge of sickle cell disease.
“All of these networks are going to study thousands of patients,” said Dr. Ofori-Acquah. “I see the H3 as a mechanism to accelerate genomics research in sickle cell disease.”
“We created a research team and built capacity for future work…. Ghana, and Africa, are capable of conducting clinical trials to global standards and producing quality data,” she said.
The story of one clinical trial is illustrative of the challenges and strengths of the multinational approach.
The phase 1b trial of a novel treatment for sickle cell disease, NVX-508, began with an initial hurdle of lack of access to emergency care at the study site, said Dr. Owusu-Ansah, a study investigator. Her first reaction, she said, was, “Well, we can’t do this, because we don’t have access to a big staff and emergency facilities.”
But after consulting with colleagues, she realized a shift in mindset was needed: “Rather than focus on what we don’t have, what do we actually have available? We have relationships we have built with institutions,” including the oldest SCD clinic in Ghana, the Ghana Institute of Clinical Genetics (GICG). This facility sits next door to a hospital with 24-hour care, Korle Bu Teaching Hospital (KBTH), a major tertiary care and referral center.
Open since 1974, the KBTH-allied GICG provides comprehensive outpatient health care to teens and adult with SCD. Currently, more than 25,000 SCD patients are registered at GICG; about half have the HbSS genotype, and another 40% have the HbSC genotype, said Yvonne Dei-Adomakoh, MD. Dr. Dei-Adomakoh of the University of Ghana is an investigator for an upcoming phase 3 trial to test voxelotor against placebo in SCD.
The GICG is working hard to become a site where clinical trials, as well as research and development, are embedded into clinic functions. In this way, not only will research be advanced for all those with SCD, but advances will be more easily incorporated into clinical care, said Dr. Dei-Adomakoh.
Dr. Owusu-Ansah noted that the facility offers a pharmacy, a laboratory, exam rooms, and information technology and medical record resources. Importantly, GICG is already staffed with physicians and allied health personnel with SCD expertise.
The University of Ghana campus is home to one of Africa’s leading biomedical research facilities, a sophisticated 11,000-square-foot laboratory that can perform testing ranging from polymerase chain reactions to DNA sequencing to genotyping and flow cytometry; it also houses a laboratory animal facility. This laboratory, the Noguchi Memorial Institute for Medical Research, also offers administrative, scientific, and research support, and houses an institutional review board.
The problem of the Noguchi laboratory site’s distance from the 24-hour support of KBTH has been solved by arranging to have an ambulance with paramedics available on site during the clinical trials.
Some other challenges the investigators discovered highlighted less-obvious infrastructure deficits; keeping a refrigerated chain of custody for biological samples, for example, can be difficult. In preparation for the trials, much basic laboratory and clinical equipment has been updated.
Conducting a U.S.-registered clinical trial in Ghana doesn’t obviate the need to meet that country’s considerable regulatory hurdles, said Dr. Owusu-Ansah. Requirements include a full regulatory submission to, and physical inspection by, Ghana’s FDA. Ghana also requires that the principal investigator must live in Ghana for the duration of the trial and that key study personnel complete Ghanaian good clinical practices training, she said.
The University of Pittsburgh is a U.S. partner in the NVX-508 study, and it was non-negotiable for that institution that a clinical trial monitor visit the African study sites. The institution’s institutional review board was sensitive to the importance of protecting vulnerable populations, and needed to hear complete plans for risk assessment, data protection, and compensation for Ghanaian study participants, Dr. Owusu-Ansah said.
But, in a turn of events typical of the ups and downs of drug development, the phase 1 trial had passed most of the administrative hurdles when in July the drug’s sponsor, NuvOx Pharma, suspended the NVX-508 trial to focus on other areas. For now, the trial registration has been withdrawn on clinicaltrials.gov and the new drug application is inactive. But Dr. Owusu-Ansah said study preparations could resume in the future, if the drug is made available to investigators.
Dr. Owusu-Ansah reported that she has received salary support from NuvOx Pharma. Dr. Segbefia reported that she has received support from Daiichi-Sankyo and Eli Lilly and Company.
WASHINGTON – Sometimes, the hardest part of solving a problem is figuring out how to work around misaligned resources, and so it has been with sickle cell disease research.
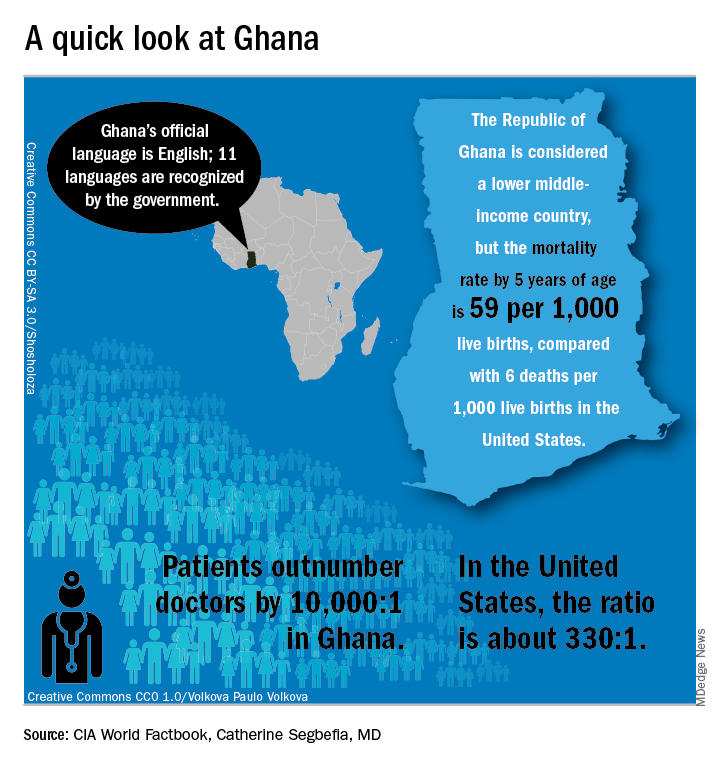
“From my point of view, what I call the geographical disparity in sickle cell disease research can be explained by the fact that the majority of affected individuals are living in the East, and the overwhelming majority of the research takes place in the West,” said Solomon Ofori-Acquah, PhD. He and three physician collaborators from Ghana shared their roadmap to conducting clinical trials in West Africa during an “East Meets West” session of the annual symposium of the Foundation for Sickle Cell Disease Research.
In Ghana, not far from where scientists now believe the hemoglobin sickling mutation originated, fully 2% of newborns have SCD; this translates into 16,000 new cases per year in a population of just 28 million, compared with the 2,000 new SCD cases seen annually in the entire United States. And access even to proven therapies can be limited; historically, little to no clinical drug development work has been conducted in this part of the world.
In the United States, half of the SCD trials that were withdrawn or terminated listed recruitment and retention of study participants as a factor in the study’s discontinuation, said Amma Owusu-Ansah, MD. “I see what we are doing as a very feasible solution to the problem of inadequate accrual to studies in the U.S.,” said Dr. Owusu-Ansah, a hematologist at the University of Pittsburgh’s Center for Translational and International Hematology (CTIH), where she serves as clinical director.
From the African perspective, hosting clinical trials – and building a robust infrastructure to do so – may help alleviate the delay in translation of disease-modifying therapies for SCD to Africa, where most people with the disease live, she said.
An existing example of resource sharing is the Human Heredity & Health in Africa (H3Africa) initiative, said Dr. Ofori-Acquah, who directs the CTIH and also holds an appointment at the University of Ghana. The project, funded by the National Institutes of Health and the Wellcome Trust, “aims to facilitate a contemporary research approach to the study of genomics and environmental determinants of common diseases with the goal of improving the health of African populations,” according to the H3Africa website. Within this framework of 40 research centers conducting genomics research and biobanking, several discrete projects aim to expand knowledge of sickle cell disease.
“All of these networks are going to study thousands of patients,” said Dr. Ofori-Acquah. “I see the H3 as a mechanism to accelerate genomics research in sickle cell disease.”
“We created a research team and built capacity for future work…. Ghana, and Africa, are capable of conducting clinical trials to global standards and producing quality data,” she said.
The story of one clinical trial is illustrative of the challenges and strengths of the multinational approach.
The phase 1b trial of a novel treatment for sickle cell disease, NVX-508, began with an initial hurdle of lack of access to emergency care at the study site, said Dr. Owusu-Ansah, a study investigator. Her first reaction, she said, was, “Well, we can’t do this, because we don’t have access to a big staff and emergency facilities.”
But after consulting with colleagues, she realized a shift in mindset was needed: “Rather than focus on what we don’t have, what do we actually have available? We have relationships we have built with institutions,” including the oldest SCD clinic in Ghana, the Ghana Institute of Clinical Genetics (GICG). This facility sits next door to a hospital with 24-hour care, Korle Bu Teaching Hospital (KBTH), a major tertiary care and referral center.
Open since 1974, the KBTH-allied GICG provides comprehensive outpatient health care to teens and adult with SCD. Currently, more than 25,000 SCD patients are registered at GICG; about half have the HbSS genotype, and another 40% have the HbSC genotype, said Yvonne Dei-Adomakoh, MD. Dr. Dei-Adomakoh of the University of Ghana is an investigator for an upcoming phase 3 trial to test voxelotor against placebo in SCD.
The GICG is working hard to become a site where clinical trials, as well as research and development, are embedded into clinic functions. In this way, not only will research be advanced for all those with SCD, but advances will be more easily incorporated into clinical care, said Dr. Dei-Adomakoh.
Dr. Owusu-Ansah noted that the facility offers a pharmacy, a laboratory, exam rooms, and information technology and medical record resources. Importantly, GICG is already staffed with physicians and allied health personnel with SCD expertise.
The University of Ghana campus is home to one of Africa’s leading biomedical research facilities, a sophisticated 11,000-square-foot laboratory that can perform testing ranging from polymerase chain reactions to DNA sequencing to genotyping and flow cytometry; it also houses a laboratory animal facility. This laboratory, the Noguchi Memorial Institute for Medical Research, also offers administrative, scientific, and research support, and houses an institutional review board.
The problem of the Noguchi laboratory site’s distance from the 24-hour support of KBTH has been solved by arranging to have an ambulance with paramedics available on site during the clinical trials.
Some other challenges the investigators discovered highlighted less-obvious infrastructure deficits; keeping a refrigerated chain of custody for biological samples, for example, can be difficult. In preparation for the trials, much basic laboratory and clinical equipment has been updated.
Conducting a U.S.-registered clinical trial in Ghana doesn’t obviate the need to meet that country’s considerable regulatory hurdles, said Dr. Owusu-Ansah. Requirements include a full regulatory submission to, and physical inspection by, Ghana’s FDA. Ghana also requires that the principal investigator must live in Ghana for the duration of the trial and that key study personnel complete Ghanaian good clinical practices training, she said.
The University of Pittsburgh is a U.S. partner in the NVX-508 study, and it was non-negotiable for that institution that a clinical trial monitor visit the African study sites. The institution’s institutional review board was sensitive to the importance of protecting vulnerable populations, and needed to hear complete plans for risk assessment, data protection, and compensation for Ghanaian study participants, Dr. Owusu-Ansah said.
But, in a turn of events typical of the ups and downs of drug development, the phase 1 trial had passed most of the administrative hurdles when in July the drug’s sponsor, NuvOx Pharma, suspended the NVX-508 trial to focus on other areas. For now, the trial registration has been withdrawn on clinicaltrials.gov and the new drug application is inactive. But Dr. Owusu-Ansah said study preparations could resume in the future, if the drug is made available to investigators.
Dr. Owusu-Ansah reported that she has received salary support from NuvOx Pharma. Dr. Segbefia reported that she has received support from Daiichi-Sankyo and Eli Lilly and Company.
WASHINGTON – Sometimes, the hardest part of solving a problem is figuring out how to work around misaligned resources, and so it has been with sickle cell disease research.
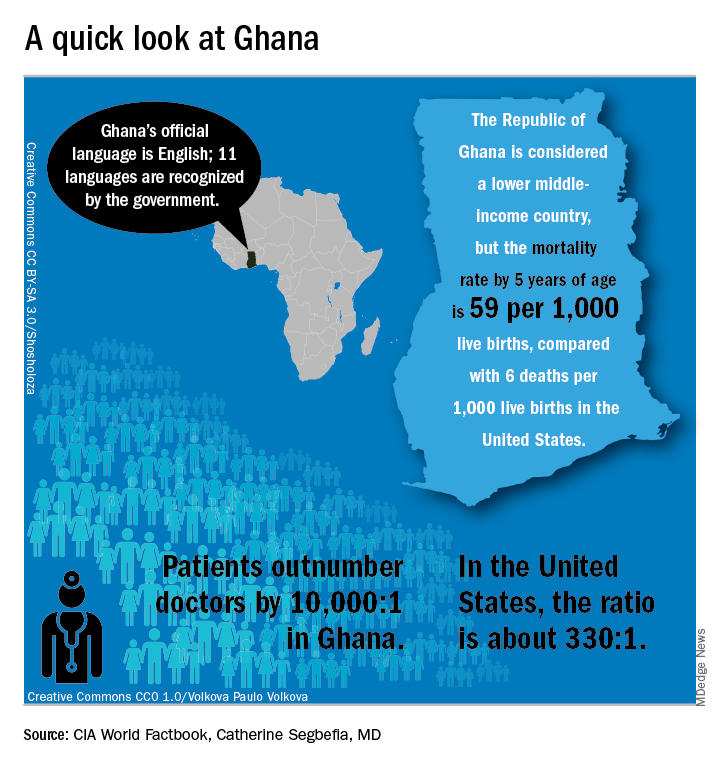
“From my point of view, what I call the geographical disparity in sickle cell disease research can be explained by the fact that the majority of affected individuals are living in the East, and the overwhelming majority of the research takes place in the West,” said Solomon Ofori-Acquah, PhD. He and three physician collaborators from Ghana shared their roadmap to conducting clinical trials in West Africa during an “East Meets West” session of the annual symposium of the Foundation for Sickle Cell Disease Research.
In Ghana, not far from where scientists now believe the hemoglobin sickling mutation originated, fully 2% of newborns have SCD; this translates into 16,000 new cases per year in a population of just 28 million, compared with the 2,000 new SCD cases seen annually in the entire United States. And access even to proven therapies can be limited; historically, little to no clinical drug development work has been conducted in this part of the world.
In the United States, half of the SCD trials that were withdrawn or terminated listed recruitment and retention of study participants as a factor in the study’s discontinuation, said Amma Owusu-Ansah, MD. “I see what we are doing as a very feasible solution to the problem of inadequate accrual to studies in the U.S.,” said Dr. Owusu-Ansah, a hematologist at the University of Pittsburgh’s Center for Translational and International Hematology (CTIH), where she serves as clinical director.
From the African perspective, hosting clinical trials – and building a robust infrastructure to do so – may help alleviate the delay in translation of disease-modifying therapies for SCD to Africa, where most people with the disease live, she said.
An existing example of resource sharing is the Human Heredity & Health in Africa (H3Africa) initiative, said Dr. Ofori-Acquah, who directs the CTIH and also holds an appointment at the University of Ghana. The project, funded by the National Institutes of Health and the Wellcome Trust, “aims to facilitate a contemporary research approach to the study of genomics and environmental determinants of common diseases with the goal of improving the health of African populations,” according to the H3Africa website. Within this framework of 40 research centers conducting genomics research and biobanking, several discrete projects aim to expand knowledge of sickle cell disease.
“All of these networks are going to study thousands of patients,” said Dr. Ofori-Acquah. “I see the H3 as a mechanism to accelerate genomics research in sickle cell disease.”
“We created a research team and built capacity for future work…. Ghana, and Africa, are capable of conducting clinical trials to global standards and producing quality data,” she said.
The story of one clinical trial is illustrative of the challenges and strengths of the multinational approach.
The phase 1b trial of a novel treatment for sickle cell disease, NVX-508, began with an initial hurdle of lack of access to emergency care at the study site, said Dr. Owusu-Ansah, a study investigator. Her first reaction, she said, was, “Well, we can’t do this, because we don’t have access to a big staff and emergency facilities.”
But after consulting with colleagues, she realized a shift in mindset was needed: “Rather than focus on what we don’t have, what do we actually have available? We have relationships we have built with institutions,” including the oldest SCD clinic in Ghana, the Ghana Institute of Clinical Genetics (GICG). This facility sits next door to a hospital with 24-hour care, Korle Bu Teaching Hospital (KBTH), a major tertiary care and referral center.
Open since 1974, the KBTH-allied GICG provides comprehensive outpatient health care to teens and adult with SCD. Currently, more than 25,000 SCD patients are registered at GICG; about half have the HbSS genotype, and another 40% have the HbSC genotype, said Yvonne Dei-Adomakoh, MD. Dr. Dei-Adomakoh of the University of Ghana is an investigator for an upcoming phase 3 trial to test voxelotor against placebo in SCD.
The GICG is working hard to become a site where clinical trials, as well as research and development, are embedded into clinic functions. In this way, not only will research be advanced for all those with SCD, but advances will be more easily incorporated into clinical care, said Dr. Dei-Adomakoh.
Dr. Owusu-Ansah noted that the facility offers a pharmacy, a laboratory, exam rooms, and information technology and medical record resources. Importantly, GICG is already staffed with physicians and allied health personnel with SCD expertise.
The University of Ghana campus is home to one of Africa’s leading biomedical research facilities, a sophisticated 11,000-square-foot laboratory that can perform testing ranging from polymerase chain reactions to DNA sequencing to genotyping and flow cytometry; it also houses a laboratory animal facility. This laboratory, the Noguchi Memorial Institute for Medical Research, also offers administrative, scientific, and research support, and houses an institutional review board.
The problem of the Noguchi laboratory site’s distance from the 24-hour support of KBTH has been solved by arranging to have an ambulance with paramedics available on site during the clinical trials.
Some other challenges the investigators discovered highlighted less-obvious infrastructure deficits; keeping a refrigerated chain of custody for biological samples, for example, can be difficult. In preparation for the trials, much basic laboratory and clinical equipment has been updated.
Conducting a U.S.-registered clinical trial in Ghana doesn’t obviate the need to meet that country’s considerable regulatory hurdles, said Dr. Owusu-Ansah. Requirements include a full regulatory submission to, and physical inspection by, Ghana’s FDA. Ghana also requires that the principal investigator must live in Ghana for the duration of the trial and that key study personnel complete Ghanaian good clinical practices training, she said.
The University of Pittsburgh is a U.S. partner in the NVX-508 study, and it was non-negotiable for that institution that a clinical trial monitor visit the African study sites. The institution’s institutional review board was sensitive to the importance of protecting vulnerable populations, and needed to hear complete plans for risk assessment, data protection, and compensation for Ghanaian study participants, Dr. Owusu-Ansah said.
But, in a turn of events typical of the ups and downs of drug development, the phase 1 trial had passed most of the administrative hurdles when in July the drug’s sponsor, NuvOx Pharma, suspended the NVX-508 trial to focus on other areas. For now, the trial registration has been withdrawn on clinicaltrials.gov and the new drug application is inactive. But Dr. Owusu-Ansah said study preparations could resume in the future, if the drug is made available to investigators.
Dr. Owusu-Ansah reported that she has received salary support from NuvOx Pharma. Dr. Segbefia reported that she has received support from Daiichi-Sankyo and Eli Lilly and Company.
EXPERT ANALYSIS FROM FSCDR 2018
Early escitalopram for post-ACS depression improves MACE, 8 years on
Even years after their cardiac events, acute coronary syndrome patients whose depression was treated with 6 months of an antidepressant had fewer cardiovascular events, according to a randomized, controlled trial.
Compared with patients who were given placebo for depression after experiencing acute coronary syndrome (ACS), patients who received escitalopram experienced a lower incidence of a composite outcome of major adverse cardiovascular events (MACE), in this extension study of a 6-month trial reported previously (J Clin Psychiatry. 2015 Jan;76[1]:62-8).
After a median of 8.1 years, MACE, the study’s primary outcome, was experienced by 40.9% of patients taking escitalopram, compared with 53.6% of those taking placebo (hazard ratio 0.69, 95% confidence interval 0.49-0.96, P = .03). The investigators also tracked the individual MACE components (all-cause mortality, myocardial infarction, and percutaneous coronary intervention), finding that MI was also significantly less common in the escitalopram group compared with those who took placebo (8.7% vs. 15.2%, HR 0.54, 95% CI, 0.27-0.96, P = .04).
The other MACE components were seen less frequently in the escitalopram group, but the differences from those taking placebo were not statistically significant. The study did not show a mortality benefit for those who took escitalopram, noted first author Jae-Min Kim, MD, of the department of psychiatry at Chonnam University Medical School, Gwangju, South Korea, and his coauthors.
The randomized, double-blind, placebo-controlled trial comprised 300 patients who recently had ACS and also met DSM-IV criteria for major or minor depression.
Over a 5-year period at a single site, patients were randomized to receive escitalopram at an initial dose of 10 mg daily (149 patients), or placebo (151), for 24 weeks after their ACS event. Escitalopram doses could be adjusted according to clinician judgment from 5 to 20 mg daily.
Patients who consented to participate were enrolled and screened for depression within 2 weeks of their ACS event, and any who scored higher than 10 on the Beck Depression Inventory at the initial screen or at follow-up appointments up to 12 weeks post enrollment went on for further screening.
Demographic data were collected with an eye toward identifying factors that could affect cardiac outcomes, said Dr. Kim and his colleagues. So in addition to age, sex, and educational level, the investigators tracked participants’ living situations and marital and employment status.
Patients were a mean of 60 years old, and about 60% were male. The median Beck Depression Inventory score was 16-17.
The study differed from others, said the investigators, because it followed patients for a longer period of time. In previous studies, “[E]ffects on cardiac outcomes have not generally been found within the treatment period,” they wrote.
Though the study’s generalizability might be limited by the fact that it was conducted at a single site and all participants were Asian, the single-site design and South Korea’s comprehensive patient data registries also allowed for complete data collection over a very long follow-up period, noted Dr. Kim and his colleagues.
Adherence was high, at 93% for those taking escitalopram and 95% for those taking placebo. Other work published from the study has shown that those taking 24 weeks of escitalopram had less depression than did those taking placebo, they added.
One coauthor reported receiving financial support from Janssen and Roche. The study was supported by the National Research Foundation of Korea.
SOURCE: Kim J-M et al. JAMA. 2018;320(4):350-8.
Even years after their cardiac events, acute coronary syndrome patients whose depression was treated with 6 months of an antidepressant had fewer cardiovascular events, according to a randomized, controlled trial.
Compared with patients who were given placebo for depression after experiencing acute coronary syndrome (ACS), patients who received escitalopram experienced a lower incidence of a composite outcome of major adverse cardiovascular events (MACE), in this extension study of a 6-month trial reported previously (J Clin Psychiatry. 2015 Jan;76[1]:62-8).
After a median of 8.1 years, MACE, the study’s primary outcome, was experienced by 40.9% of patients taking escitalopram, compared with 53.6% of those taking placebo (hazard ratio 0.69, 95% confidence interval 0.49-0.96, P = .03). The investigators also tracked the individual MACE components (all-cause mortality, myocardial infarction, and percutaneous coronary intervention), finding that MI was also significantly less common in the escitalopram group compared with those who took placebo (8.7% vs. 15.2%, HR 0.54, 95% CI, 0.27-0.96, P = .04).
The other MACE components were seen less frequently in the escitalopram group, but the differences from those taking placebo were not statistically significant. The study did not show a mortality benefit for those who took escitalopram, noted first author Jae-Min Kim, MD, of the department of psychiatry at Chonnam University Medical School, Gwangju, South Korea, and his coauthors.
The randomized, double-blind, placebo-controlled trial comprised 300 patients who recently had ACS and also met DSM-IV criteria for major or minor depression.
Over a 5-year period at a single site, patients were randomized to receive escitalopram at an initial dose of 10 mg daily (149 patients), or placebo (151), for 24 weeks after their ACS event. Escitalopram doses could be adjusted according to clinician judgment from 5 to 20 mg daily.
Patients who consented to participate were enrolled and screened for depression within 2 weeks of their ACS event, and any who scored higher than 10 on the Beck Depression Inventory at the initial screen or at follow-up appointments up to 12 weeks post enrollment went on for further screening.
Demographic data were collected with an eye toward identifying factors that could affect cardiac outcomes, said Dr. Kim and his colleagues. So in addition to age, sex, and educational level, the investigators tracked participants’ living situations and marital and employment status.
Patients were a mean of 60 years old, and about 60% were male. The median Beck Depression Inventory score was 16-17.
The study differed from others, said the investigators, because it followed patients for a longer period of time. In previous studies, “[E]ffects on cardiac outcomes have not generally been found within the treatment period,” they wrote.
Though the study’s generalizability might be limited by the fact that it was conducted at a single site and all participants were Asian, the single-site design and South Korea’s comprehensive patient data registries also allowed for complete data collection over a very long follow-up period, noted Dr. Kim and his colleagues.
Adherence was high, at 93% for those taking escitalopram and 95% for those taking placebo. Other work published from the study has shown that those taking 24 weeks of escitalopram had less depression than did those taking placebo, they added.
One coauthor reported receiving financial support from Janssen and Roche. The study was supported by the National Research Foundation of Korea.
SOURCE: Kim J-M et al. JAMA. 2018;320(4):350-8.
Even years after their cardiac events, acute coronary syndrome patients whose depression was treated with 6 months of an antidepressant had fewer cardiovascular events, according to a randomized, controlled trial.
Compared with patients who were given placebo for depression after experiencing acute coronary syndrome (ACS), patients who received escitalopram experienced a lower incidence of a composite outcome of major adverse cardiovascular events (MACE), in this extension study of a 6-month trial reported previously (J Clin Psychiatry. 2015 Jan;76[1]:62-8).
After a median of 8.1 years, MACE, the study’s primary outcome, was experienced by 40.9% of patients taking escitalopram, compared with 53.6% of those taking placebo (hazard ratio 0.69, 95% confidence interval 0.49-0.96, P = .03). The investigators also tracked the individual MACE components (all-cause mortality, myocardial infarction, and percutaneous coronary intervention), finding that MI was also significantly less common in the escitalopram group compared with those who took placebo (8.7% vs. 15.2%, HR 0.54, 95% CI, 0.27-0.96, P = .04).
The other MACE components were seen less frequently in the escitalopram group, but the differences from those taking placebo were not statistically significant. The study did not show a mortality benefit for those who took escitalopram, noted first author Jae-Min Kim, MD, of the department of psychiatry at Chonnam University Medical School, Gwangju, South Korea, and his coauthors.
The randomized, double-blind, placebo-controlled trial comprised 300 patients who recently had ACS and also met DSM-IV criteria for major or minor depression.
Over a 5-year period at a single site, patients were randomized to receive escitalopram at an initial dose of 10 mg daily (149 patients), or placebo (151), for 24 weeks after their ACS event. Escitalopram doses could be adjusted according to clinician judgment from 5 to 20 mg daily.
Patients who consented to participate were enrolled and screened for depression within 2 weeks of their ACS event, and any who scored higher than 10 on the Beck Depression Inventory at the initial screen or at follow-up appointments up to 12 weeks post enrollment went on for further screening.
Demographic data were collected with an eye toward identifying factors that could affect cardiac outcomes, said Dr. Kim and his colleagues. So in addition to age, sex, and educational level, the investigators tracked participants’ living situations and marital and employment status.
Patients were a mean of 60 years old, and about 60% were male. The median Beck Depression Inventory score was 16-17.
The study differed from others, said the investigators, because it followed patients for a longer period of time. In previous studies, “[E]ffects on cardiac outcomes have not generally been found within the treatment period,” they wrote.
Though the study’s generalizability might be limited by the fact that it was conducted at a single site and all participants were Asian, the single-site design and South Korea’s comprehensive patient data registries also allowed for complete data collection over a very long follow-up period, noted Dr. Kim and his colleagues.
Adherence was high, at 93% for those taking escitalopram and 95% for those taking placebo. Other work published from the study has shown that those taking 24 weeks of escitalopram had less depression than did those taking placebo, they added.
One coauthor reported receiving financial support from Janssen and Roche. The study was supported by the National Research Foundation of Korea.
SOURCE: Kim J-M et al. JAMA. 2018;320(4):350-8.
FROM JAMA
Key clinical point: .
Major finding: The hazard ratio was 0.69 for MACE in the escitalopram group compared with placebo (P = .03).
Study details: Randomized, double-blind, placebo-controlled trial of 300 patients with ACS given escitalopram or placebo.
Disclosures: The National Research Council of Korea sponsored the study. One author reported funding from Janssen and Roche.
Source: Kim J-M et al. JAMA. 2018;320(4):350-8.
For men with SCD and priapism, hypoxia may prompt RBC adhesion
WASHINGTON – For male patients with sickle cell disease, priapism can be more than just painful and embarrassing. The prolonged erections prompted by vasoocclusive events in the penis may lead to irreversible impotence, but little is known about risk factors for priapism, which remains a difficult-to-treat complication of the disease.
In males with HbSS sickle cell disease (SCD) and priapism, RBC adhesion is increased in hypoxic conditions, according to preliminary findings from work using a newly developed biochip that mimics microvascular conditions in SCD. This significant level of adhesion prompted by hypoxia was not seen in men who did not have priapism, according to study coauthor Erina Quinn, a research assistant in hematology and oncology at Case Western Reserve University, Cleveland, who presented the results at the annual meeting of the Foundation for Sickle Cell Disease Research.
When hemoglobin desaturation occurs, polymerization can be increased, leading to increased end-organ damage, Ms. Quinn said. The biochip is “an effort to measure cellular adhesion in a clinically meaningful way.” The tool can detect hemoglobin phenotype, differentiating among HbSS, HbSbeta+, and HbSC. It can also measure the degree of hemolysis and RBC deformability.
The biochip “mimics postcapillary flow conditions in microchannels,” Ms. Quinn said. The device forces blood samples through microchannels that are at the diameter of smaller venules, approximately 50 mcm, and at a physiological flow rate ranging from 1-13 mm/sec. The microfluidic channels are coated with laminin, a subendothelial matrix protein implicated in RBC adhesion. A second microfluidic biochip mimics hypoxic conditions.
The study enrolled 26 men with the HbSS genotype, 14 of whom reported priapism, and assessed RBC adhesion in blood samples run though both the SCD-modeled biochip and the hypoxia biochip. Investigators also assessed contemporaneous in vivo hemoglobin desaturation, and looked for associations with the in vitro biochip findings.
Of the 26 participants, 16 also had either nocturnal or exertional hemoglobin desaturation. In addition, 10 participants had both priapism and desaturations. These data were collected by retrospective chart review and patient survey.
Patients with priapism were a mean age of 34 years, compared with a mean age of 29 years for the other participants, a nonsignificant difference. There were no significant differences in mean hemoglobin or bilirubin levels, or in reticulocyte counts, between the two groups.
However, white blood count, absolute neutrophil count, and lactate dehydrogenase levels were significantly higher for men with priapism (P = .022, .037, and .008, respectively). Ferritin levels were higher as well, at a mean 2,433 (plus or minus 2,234) mcg/L for those with priapism, compared with a mean 269 (plus or minus 3,015) mcg/L for those without priapism (P = .031).
When absolute reticulocyte count was mapped against lactate dehydrogenase levels to create a measure of degree of hemolysis, “individuals with priapism had a more hemolytic lab profile,” said Ms. Quinn (P = .0186).
Though 10 of 14 men with priapism had hemoglobin desaturation, compared with 5 of 12 who did not have priapism, the difference was not statistically significant.
When the researchers compared microchip analysis of RBC adhesion, though, they found marked differences in RBC adhesion in hypoxic versus nonhypoxic conditions. Significantly more RBCs were adherent under hypoxic conditions – in the hypoxic biochip – for the patients with priapism than for patients without priapism (mean, 529 vs. 3,268 adherent cells; P = .016).
Though numbers were small, RBCs from patients with reported priapism and hemoglobin desaturation in vivo showed increased hypoxia enhanced adhesion in vitro (P = .013), Ms. Quinn said. These was no significant difference between adhesion in normoxic and hypoxic conditions for the patients without priapism.
Future directions of work with the biochip include prospective identification of desaturation events and better characterization of nocturnal symptoms, Ms. Quinn said. The investigators also plan to see whether treatment with supplemental oxygen affects RBC adhesion.
The research was supported by the National Institutes of Health, the Doris Duke Charitable Foundation, and the National Science Foundation. Two coauthors have filed an international patent for the biochip technology.
WASHINGTON – For male patients with sickle cell disease, priapism can be more than just painful and embarrassing. The prolonged erections prompted by vasoocclusive events in the penis may lead to irreversible impotence, but little is known about risk factors for priapism, which remains a difficult-to-treat complication of the disease.
In males with HbSS sickle cell disease (SCD) and priapism, RBC adhesion is increased in hypoxic conditions, according to preliminary findings from work using a newly developed biochip that mimics microvascular conditions in SCD. This significant level of adhesion prompted by hypoxia was not seen in men who did not have priapism, according to study coauthor Erina Quinn, a research assistant in hematology and oncology at Case Western Reserve University, Cleveland, who presented the results at the annual meeting of the Foundation for Sickle Cell Disease Research.
When hemoglobin desaturation occurs, polymerization can be increased, leading to increased end-organ damage, Ms. Quinn said. The biochip is “an effort to measure cellular adhesion in a clinically meaningful way.” The tool can detect hemoglobin phenotype, differentiating among HbSS, HbSbeta+, and HbSC. It can also measure the degree of hemolysis and RBC deformability.
The biochip “mimics postcapillary flow conditions in microchannels,” Ms. Quinn said. The device forces blood samples through microchannels that are at the diameter of smaller venules, approximately 50 mcm, and at a physiological flow rate ranging from 1-13 mm/sec. The microfluidic channels are coated with laminin, a subendothelial matrix protein implicated in RBC adhesion. A second microfluidic biochip mimics hypoxic conditions.
The study enrolled 26 men with the HbSS genotype, 14 of whom reported priapism, and assessed RBC adhesion in blood samples run though both the SCD-modeled biochip and the hypoxia biochip. Investigators also assessed contemporaneous in vivo hemoglobin desaturation, and looked for associations with the in vitro biochip findings.
Of the 26 participants, 16 also had either nocturnal or exertional hemoglobin desaturation. In addition, 10 participants had both priapism and desaturations. These data were collected by retrospective chart review and patient survey.
Patients with priapism were a mean age of 34 years, compared with a mean age of 29 years for the other participants, a nonsignificant difference. There were no significant differences in mean hemoglobin or bilirubin levels, or in reticulocyte counts, between the two groups.
However, white blood count, absolute neutrophil count, and lactate dehydrogenase levels were significantly higher for men with priapism (P = .022, .037, and .008, respectively). Ferritin levels were higher as well, at a mean 2,433 (plus or minus 2,234) mcg/L for those with priapism, compared with a mean 269 (plus or minus 3,015) mcg/L for those without priapism (P = .031).
When absolute reticulocyte count was mapped against lactate dehydrogenase levels to create a measure of degree of hemolysis, “individuals with priapism had a more hemolytic lab profile,” said Ms. Quinn (P = .0186).
Though 10 of 14 men with priapism had hemoglobin desaturation, compared with 5 of 12 who did not have priapism, the difference was not statistically significant.
When the researchers compared microchip analysis of RBC adhesion, though, they found marked differences in RBC adhesion in hypoxic versus nonhypoxic conditions. Significantly more RBCs were adherent under hypoxic conditions – in the hypoxic biochip – for the patients with priapism than for patients without priapism (mean, 529 vs. 3,268 adherent cells; P = .016).
Though numbers were small, RBCs from patients with reported priapism and hemoglobin desaturation in vivo showed increased hypoxia enhanced adhesion in vitro (P = .013), Ms. Quinn said. These was no significant difference between adhesion in normoxic and hypoxic conditions for the patients without priapism.
Future directions of work with the biochip include prospective identification of desaturation events and better characterization of nocturnal symptoms, Ms. Quinn said. The investigators also plan to see whether treatment with supplemental oxygen affects RBC adhesion.
The research was supported by the National Institutes of Health, the Doris Duke Charitable Foundation, and the National Science Foundation. Two coauthors have filed an international patent for the biochip technology.
WASHINGTON – For male patients with sickle cell disease, priapism can be more than just painful and embarrassing. The prolonged erections prompted by vasoocclusive events in the penis may lead to irreversible impotence, but little is known about risk factors for priapism, which remains a difficult-to-treat complication of the disease.
In males with HbSS sickle cell disease (SCD) and priapism, RBC adhesion is increased in hypoxic conditions, according to preliminary findings from work using a newly developed biochip that mimics microvascular conditions in SCD. This significant level of adhesion prompted by hypoxia was not seen in men who did not have priapism, according to study coauthor Erina Quinn, a research assistant in hematology and oncology at Case Western Reserve University, Cleveland, who presented the results at the annual meeting of the Foundation for Sickle Cell Disease Research.
When hemoglobin desaturation occurs, polymerization can be increased, leading to increased end-organ damage, Ms. Quinn said. The biochip is “an effort to measure cellular adhesion in a clinically meaningful way.” The tool can detect hemoglobin phenotype, differentiating among HbSS, HbSbeta+, and HbSC. It can also measure the degree of hemolysis and RBC deformability.
The biochip “mimics postcapillary flow conditions in microchannels,” Ms. Quinn said. The device forces blood samples through microchannels that are at the diameter of smaller venules, approximately 50 mcm, and at a physiological flow rate ranging from 1-13 mm/sec. The microfluidic channels are coated with laminin, a subendothelial matrix protein implicated in RBC adhesion. A second microfluidic biochip mimics hypoxic conditions.
The study enrolled 26 men with the HbSS genotype, 14 of whom reported priapism, and assessed RBC adhesion in blood samples run though both the SCD-modeled biochip and the hypoxia biochip. Investigators also assessed contemporaneous in vivo hemoglobin desaturation, and looked for associations with the in vitro biochip findings.
Of the 26 participants, 16 also had either nocturnal or exertional hemoglobin desaturation. In addition, 10 participants had both priapism and desaturations. These data were collected by retrospective chart review and patient survey.
Patients with priapism were a mean age of 34 years, compared with a mean age of 29 years for the other participants, a nonsignificant difference. There were no significant differences in mean hemoglobin or bilirubin levels, or in reticulocyte counts, between the two groups.
However, white blood count, absolute neutrophil count, and lactate dehydrogenase levels were significantly higher for men with priapism (P = .022, .037, and .008, respectively). Ferritin levels were higher as well, at a mean 2,433 (plus or minus 2,234) mcg/L for those with priapism, compared with a mean 269 (plus or minus 3,015) mcg/L for those without priapism (P = .031).
When absolute reticulocyte count was mapped against lactate dehydrogenase levels to create a measure of degree of hemolysis, “individuals with priapism had a more hemolytic lab profile,” said Ms. Quinn (P = .0186).
Though 10 of 14 men with priapism had hemoglobin desaturation, compared with 5 of 12 who did not have priapism, the difference was not statistically significant.
When the researchers compared microchip analysis of RBC adhesion, though, they found marked differences in RBC adhesion in hypoxic versus nonhypoxic conditions. Significantly more RBCs were adherent under hypoxic conditions – in the hypoxic biochip – for the patients with priapism than for patients without priapism (mean, 529 vs. 3,268 adherent cells; P = .016).
Though numbers were small, RBCs from patients with reported priapism and hemoglobin desaturation in vivo showed increased hypoxia enhanced adhesion in vitro (P = .013), Ms. Quinn said. These was no significant difference between adhesion in normoxic and hypoxic conditions for the patients without priapism.
Future directions of work with the biochip include prospective identification of desaturation events and better characterization of nocturnal symptoms, Ms. Quinn said. The investigators also plan to see whether treatment with supplemental oxygen affects RBC adhesion.
The research was supported by the National Institutes of Health, the Doris Duke Charitable Foundation, and the National Science Foundation. Two coauthors have filed an international patent for the biochip technology.
REPORTING FROM FSCDR 2018
Key clinical point: RBC adhesion was increased, but only in hypoxia, for men with sickle cell disease and priapism.
Major finding: Men who had desaturations and priapism had significantly higher RBC adhesion than those without priapism (P = .013).
Study details: An in vitro and in vivo study of 26 men with HbSS sickle cell disease, with and without priapism.
Disclosures: The study was funded by the National Institutes of Health, the Doris Duke Charitable Foundation, and the National Science Foundation. Two coauthors have filed an international patent for the biochip technology.
Few women know that IUDs are effective emergency contraception
Although IUDs are effective as emergency contraception, few young women knew about this use of the device, according to a recent, multisite survey published in Contraception.
Only 7.5% of young female participants in a recent study had heard that the IUD could be used for emergency contraception (EC), according to a cluster-randomized trial of 1,500 women aged 18-25 years receiving contraception counseling at 40 U.S. Planned Parenthood centers. Race, ethnicity, and insurance status had no effect on the likelihood that a woman would know about IUDs as EC.
However, the study found, 68% of women surveyed would want to know about IUD use for EC, and those for whom a pregnancy would cause the most unhappiness were especially likely to want to know about this option (adjusted odds ratio, 1.26; 95% confidence interval, 1.01-1.58; P = .04). Again, demographic factors did not affect the likelihood that women would want to know about the IUD as an alternative to EC pills.
“In this 40-site U.S. study of sexually active young women, very few had heard of the IUD as a form of EC or knew of its significantly higher efficacy compared to EC pills, but most would desire to learn about it if they needed EC,” wrote Suzan Goodman, MD, MPH, and her coauthors.
Office visits where women request EC “provide a unique and time-sensitive opportunity to prevent an unwanted pregnancy, as well as to offer ongoing contraception,” wrote Dr. Goodman of the University of California, San Francisco, and her coauthors. But previous work showed that teens and young women are not generally well-informed about EC, including the window of effectiveness and methods that can be used for EC.
Dr. Goodman and her collaborators conducted a secondary analysis of a cluster-randomized trial that delivered a 4-hour training module to half of the Planned Parenthood centers; the evidence-based training focused on contraceptive counseling, long-acting reversible contraception, and IUD placement. Patients seen at the 40 centers were surveyed before receiving contraception counseling, and at 3 and 6 months post counseling.
Participant assignment to a center where the intervention had been administered to clinic staff had no bearing on how likely they were to have heard that IUDs could be used as EC.
Of the original survey respondents, who were young women not intending to become pregnant for at least 12 months, a total of 1,138 participants completed the relevant portions of the survey. The mean age of the respondents was 21.5 years, and were mostly (94%) never married. About one-quarter (26%) had private insurance, 31% had public insurance, and 38% were uninsured. About half were white, one-quarter were black, and 17% identified as Hispanic.
Study participants were very likely to view a doctor or nurse as their most trusted sources of information about EC, with 91% identifying this source over the Internet (6%) or friends (2%). Previous work, Dr. Goodman and her colleagues wrote, has found that women are more likely to consider an IUD if they had heard about it from a health care provider.
Although incorporating the ability to place an IUD at an EC visit may present some challenges in terms of clinic work flow and staff training, it’s an option that should be considered for many reasons, the authors noted.
IUDs are overall more effective than EC pills, with marked advantages in some instances: IUDs have higher efficacy in women with obesity, for women who have had multiple episodes of intercourse within the 5-day efficacy window, and for women at the fertile point of their menstrual cycles. Once inserted, they afford the additional advantage of ongoing protection against pregnancy.
“Contraceptive education should explicitly address IUD as EC,” wrote Dr. Goodman and her coauthors. “A coordinated effort to improve counseling, provider training, and same-day access to IUD as EC will be critical to offering women their full range of contraceptive options.”
This study was funded by the William and Flora Hewlett Foundation and the National Institutes of Health. Dr. Goodman reported no conflicts of interest. Two study coauthors are employees of Planned Parenthood, which participates in unrelated studies funded by HRA Pharma.
SOURCE: Goodman S et al. Contraception. 2018 Apr 18. doi: 10.1016/j.contraception.2018.04.009.
Although IUDs are effective as emergency contraception, few young women knew about this use of the device, according to a recent, multisite survey published in Contraception.
Only 7.5% of young female participants in a recent study had heard that the IUD could be used for emergency contraception (EC), according to a cluster-randomized trial of 1,500 women aged 18-25 years receiving contraception counseling at 40 U.S. Planned Parenthood centers. Race, ethnicity, and insurance status had no effect on the likelihood that a woman would know about IUDs as EC.
However, the study found, 68% of women surveyed would want to know about IUD use for EC, and those for whom a pregnancy would cause the most unhappiness were especially likely to want to know about this option (adjusted odds ratio, 1.26; 95% confidence interval, 1.01-1.58; P = .04). Again, demographic factors did not affect the likelihood that women would want to know about the IUD as an alternative to EC pills.
“In this 40-site U.S. study of sexually active young women, very few had heard of the IUD as a form of EC or knew of its significantly higher efficacy compared to EC pills, but most would desire to learn about it if they needed EC,” wrote Suzan Goodman, MD, MPH, and her coauthors.
Office visits where women request EC “provide a unique and time-sensitive opportunity to prevent an unwanted pregnancy, as well as to offer ongoing contraception,” wrote Dr. Goodman of the University of California, San Francisco, and her coauthors. But previous work showed that teens and young women are not generally well-informed about EC, including the window of effectiveness and methods that can be used for EC.
Dr. Goodman and her collaborators conducted a secondary analysis of a cluster-randomized trial that delivered a 4-hour training module to half of the Planned Parenthood centers; the evidence-based training focused on contraceptive counseling, long-acting reversible contraception, and IUD placement. Patients seen at the 40 centers were surveyed before receiving contraception counseling, and at 3 and 6 months post counseling.
Participant assignment to a center where the intervention had been administered to clinic staff had no bearing on how likely they were to have heard that IUDs could be used as EC.
Of the original survey respondents, who were young women not intending to become pregnant for at least 12 months, a total of 1,138 participants completed the relevant portions of the survey. The mean age of the respondents was 21.5 years, and were mostly (94%) never married. About one-quarter (26%) had private insurance, 31% had public insurance, and 38% were uninsured. About half were white, one-quarter were black, and 17% identified as Hispanic.
Study participants were very likely to view a doctor or nurse as their most trusted sources of information about EC, with 91% identifying this source over the Internet (6%) or friends (2%). Previous work, Dr. Goodman and her colleagues wrote, has found that women are more likely to consider an IUD if they had heard about it from a health care provider.
Although incorporating the ability to place an IUD at an EC visit may present some challenges in terms of clinic work flow and staff training, it’s an option that should be considered for many reasons, the authors noted.
IUDs are overall more effective than EC pills, with marked advantages in some instances: IUDs have higher efficacy in women with obesity, for women who have had multiple episodes of intercourse within the 5-day efficacy window, and for women at the fertile point of their menstrual cycles. Once inserted, they afford the additional advantage of ongoing protection against pregnancy.
“Contraceptive education should explicitly address IUD as EC,” wrote Dr. Goodman and her coauthors. “A coordinated effort to improve counseling, provider training, and same-day access to IUD as EC will be critical to offering women their full range of contraceptive options.”
This study was funded by the William and Flora Hewlett Foundation and the National Institutes of Health. Dr. Goodman reported no conflicts of interest. Two study coauthors are employees of Planned Parenthood, which participates in unrelated studies funded by HRA Pharma.
SOURCE: Goodman S et al. Contraception. 2018 Apr 18. doi: 10.1016/j.contraception.2018.04.009.
Although IUDs are effective as emergency contraception, few young women knew about this use of the device, according to a recent, multisite survey published in Contraception.
Only 7.5% of young female participants in a recent study had heard that the IUD could be used for emergency contraception (EC), according to a cluster-randomized trial of 1,500 women aged 18-25 years receiving contraception counseling at 40 U.S. Planned Parenthood centers. Race, ethnicity, and insurance status had no effect on the likelihood that a woman would know about IUDs as EC.
However, the study found, 68% of women surveyed would want to know about IUD use for EC, and those for whom a pregnancy would cause the most unhappiness were especially likely to want to know about this option (adjusted odds ratio, 1.26; 95% confidence interval, 1.01-1.58; P = .04). Again, demographic factors did not affect the likelihood that women would want to know about the IUD as an alternative to EC pills.
“In this 40-site U.S. study of sexually active young women, very few had heard of the IUD as a form of EC or knew of its significantly higher efficacy compared to EC pills, but most would desire to learn about it if they needed EC,” wrote Suzan Goodman, MD, MPH, and her coauthors.
Office visits where women request EC “provide a unique and time-sensitive opportunity to prevent an unwanted pregnancy, as well as to offer ongoing contraception,” wrote Dr. Goodman of the University of California, San Francisco, and her coauthors. But previous work showed that teens and young women are not generally well-informed about EC, including the window of effectiveness and methods that can be used for EC.
Dr. Goodman and her collaborators conducted a secondary analysis of a cluster-randomized trial that delivered a 4-hour training module to half of the Planned Parenthood centers; the evidence-based training focused on contraceptive counseling, long-acting reversible contraception, and IUD placement. Patients seen at the 40 centers were surveyed before receiving contraception counseling, and at 3 and 6 months post counseling.
Participant assignment to a center where the intervention had been administered to clinic staff had no bearing on how likely they were to have heard that IUDs could be used as EC.
Of the original survey respondents, who were young women not intending to become pregnant for at least 12 months, a total of 1,138 participants completed the relevant portions of the survey. The mean age of the respondents was 21.5 years, and were mostly (94%) never married. About one-quarter (26%) had private insurance, 31% had public insurance, and 38% were uninsured. About half were white, one-quarter were black, and 17% identified as Hispanic.
Study participants were very likely to view a doctor or nurse as their most trusted sources of information about EC, with 91% identifying this source over the Internet (6%) or friends (2%). Previous work, Dr. Goodman and her colleagues wrote, has found that women are more likely to consider an IUD if they had heard about it from a health care provider.
Although incorporating the ability to place an IUD at an EC visit may present some challenges in terms of clinic work flow and staff training, it’s an option that should be considered for many reasons, the authors noted.
IUDs are overall more effective than EC pills, with marked advantages in some instances: IUDs have higher efficacy in women with obesity, for women who have had multiple episodes of intercourse within the 5-day efficacy window, and for women at the fertile point of their menstrual cycles. Once inserted, they afford the additional advantage of ongoing protection against pregnancy.
“Contraceptive education should explicitly address IUD as EC,” wrote Dr. Goodman and her coauthors. “A coordinated effort to improve counseling, provider training, and same-day access to IUD as EC will be critical to offering women their full range of contraceptive options.”
This study was funded by the William and Flora Hewlett Foundation and the National Institutes of Health. Dr. Goodman reported no conflicts of interest. Two study coauthors are employees of Planned Parenthood, which participates in unrelated studies funded by HRA Pharma.
SOURCE: Goodman S et al. Contraception. 2018 Apr 18. doi: 10.1016/j.contraception.2018.04.009.
FROM CONTRACEPTION
Key clinical point: Few young women knew that an IUD is an effective emergency contraceptive.
Major finding: IUDs were identified as emergency contraception by 7.5% of respondents.
Study details: Secondary analysis of 1,138 responses from a 40-site, cluster-controlled trial of a contraceptive training intervention.
Disclosures: The study was sponsored by the William and Flora Hewlett Foundation and the National Institutes of Health. Two coauthors are employed by Planned Parenthood, which participates in unrelated research by HRA Pharma.
Source: Goodman S et al. Contraception. 2018 Apr 18. doi: 10.1016/j.contraception.2018.04.009.












