User login
Seventy percent of docs using EHRs to e-prescribe
About 70% of U.S. physicians were using an electronic health record system to electronically transmit prescriptions to pharmacies as of April 2014, according to an analysis by the Office of the National Coordinator for Health Information Technology.
This represents a rapid scale-up in the use of EHRs with the passage of MIPPA [Medicare Improvements for Patients and Providers Act] in December 2008 (7%) and when the Medicare and Medicaid EHR Incentive Programs began (24%) in 2009, according to the ONCHIT report.
The figures are based on an analysis of data from Surescripts, which provides IT network infrastructure that transmits electronic prescriptions and other health-related data.
Nearly all community pharmacies across the United States are enabled to accept e-prescriptions, according to the report.
"The growth of physicians and pharmacies e-prescribing has corresponded with a 14-fold increase in the growth of new and renewal prescriptions sent electronically," the report states, growing from 4% in 2008 to 57% in 2013. For 2013, this translates to 1 billion of the total 1.8 billion new and renewal prescriptions being sent electronically.
About 70% of U.S. physicians were using an electronic health record system to electronically transmit prescriptions to pharmacies as of April 2014, according to an analysis by the Office of the National Coordinator for Health Information Technology.
This represents a rapid scale-up in the use of EHRs with the passage of MIPPA [Medicare Improvements for Patients and Providers Act] in December 2008 (7%) and when the Medicare and Medicaid EHR Incentive Programs began (24%) in 2009, according to the ONCHIT report.
The figures are based on an analysis of data from Surescripts, which provides IT network infrastructure that transmits electronic prescriptions and other health-related data.
Nearly all community pharmacies across the United States are enabled to accept e-prescriptions, according to the report.
"The growth of physicians and pharmacies e-prescribing has corresponded with a 14-fold increase in the growth of new and renewal prescriptions sent electronically," the report states, growing from 4% in 2008 to 57% in 2013. For 2013, this translates to 1 billion of the total 1.8 billion new and renewal prescriptions being sent electronically.
About 70% of U.S. physicians were using an electronic health record system to electronically transmit prescriptions to pharmacies as of April 2014, according to an analysis by the Office of the National Coordinator for Health Information Technology.
This represents a rapid scale-up in the use of EHRs with the passage of MIPPA [Medicare Improvements for Patients and Providers Act] in December 2008 (7%) and when the Medicare and Medicaid EHR Incentive Programs began (24%) in 2009, according to the ONCHIT report.
The figures are based on an analysis of data from Surescripts, which provides IT network infrastructure that transmits electronic prescriptions and other health-related data.
Nearly all community pharmacies across the United States are enabled to accept e-prescriptions, according to the report.
"The growth of physicians and pharmacies e-prescribing has corresponded with a 14-fold increase in the growth of new and renewal prescriptions sent electronically," the report states, growing from 4% in 2008 to 57% in 2013. For 2013, this translates to 1 billion of the total 1.8 billion new and renewal prescriptions being sent electronically.
EHR use hasn’t sent Medicare payments soaring
Concerns that electronic health records will result in an uptick in Medicare payments to hospitals – for legitimate or fraudulent reasons – appear to be unfounded.
Anecdotal reports have surfaced in the wake of a federal incentive program to push for the adoption of EHRs that hospitals might be using the systems to boost payments by more accurately capturing, and more accurately charging, for services rendered than previously recorded, by "upcoding" or selecting billing codes that reflect more intensive procedures or reflect a sicker patient population, or by simply "cloning" entries into an EHR to provide higher billing to multiple patients that might not reflect the care provided. These reports have led the Department of Health & Human Services Office of Inspector General to call for Medicare administrative and program integrity contractors to do more to detect potential fraud from the use of EHRs.
However, research by Julia Adler-Milstein, Ph.D., of the University of Michigan, Ann Arbor, and Dr. Ashish Jha of the Harvard School of Public Health, Boston, suggests that this kind of fraud has not been an issue.
"We found that hospitals that adopted EHRs increased billing to Medicare, but at a rate comparable to that of matched controls of non-EHR adopters," the researchers wrote in the article appearing in the July issue of Health Affairs (July 2014 [doi:10.1377/hlthaff.2014.0023]).
Researchers looked at 393 hospitals that had newly adopted a basic EHR (181 that adopted between 2008 and 2009 and 212 that adopted between 2009 and 2010) and compared them to 782 control hospitals that did not adopt during the same periods. New adopters were predominantly nonteaching (61%), for-profit (70%), and medium-size (47%) hospitals.
In the research models, "we found no significant relationship between EHR adoption and patient acuity," the report states. Also, "adopters and controls had indistinguishable changes in Medicare payments. Between the pre- and postadoption periods, payment per discharge to adopters grew by $849 and to controls by $945. This $96 difference in difference was not in the predicted direction, but it was not significant, either (P = .673)," the researchers wrote.
They suggested that the results were due to hospitals heavily investing in optimizing coding before adopting EHRs.
"Hospitals operate on thin financial margins and therefore likely work hard to maximize reimbursement," the researchers wrote. "Thus, simply having more electronic data or better documentation may not provide as much of an opportunity to increase coding as has been postulated."
They concluded that while there will always be outliers that engage in fraudulent behavior, "our findings suggest that a large-scale policy effort targeting EHR-driven fraudulent coding, such as the one recently recommended by the HHS Office of Inspector General, is not likely to be useful. Substantial savings are unlikely to result even from a policy targeting certain subgroups of hospitals that might be expected to experience the greatest pressure to increase billing after investing in an EHR system."
Concerns that electronic health records will result in an uptick in Medicare payments to hospitals – for legitimate or fraudulent reasons – appear to be unfounded.
Anecdotal reports have surfaced in the wake of a federal incentive program to push for the adoption of EHRs that hospitals might be using the systems to boost payments by more accurately capturing, and more accurately charging, for services rendered than previously recorded, by "upcoding" or selecting billing codes that reflect more intensive procedures or reflect a sicker patient population, or by simply "cloning" entries into an EHR to provide higher billing to multiple patients that might not reflect the care provided. These reports have led the Department of Health & Human Services Office of Inspector General to call for Medicare administrative and program integrity contractors to do more to detect potential fraud from the use of EHRs.
However, research by Julia Adler-Milstein, Ph.D., of the University of Michigan, Ann Arbor, and Dr. Ashish Jha of the Harvard School of Public Health, Boston, suggests that this kind of fraud has not been an issue.
"We found that hospitals that adopted EHRs increased billing to Medicare, but at a rate comparable to that of matched controls of non-EHR adopters," the researchers wrote in the article appearing in the July issue of Health Affairs (July 2014 [doi:10.1377/hlthaff.2014.0023]).
Researchers looked at 393 hospitals that had newly adopted a basic EHR (181 that adopted between 2008 and 2009 and 212 that adopted between 2009 and 2010) and compared them to 782 control hospitals that did not adopt during the same periods. New adopters were predominantly nonteaching (61%), for-profit (70%), and medium-size (47%) hospitals.
In the research models, "we found no significant relationship between EHR adoption and patient acuity," the report states. Also, "adopters and controls had indistinguishable changes in Medicare payments. Between the pre- and postadoption periods, payment per discharge to adopters grew by $849 and to controls by $945. This $96 difference in difference was not in the predicted direction, but it was not significant, either (P = .673)," the researchers wrote.
They suggested that the results were due to hospitals heavily investing in optimizing coding before adopting EHRs.
"Hospitals operate on thin financial margins and therefore likely work hard to maximize reimbursement," the researchers wrote. "Thus, simply having more electronic data or better documentation may not provide as much of an opportunity to increase coding as has been postulated."
They concluded that while there will always be outliers that engage in fraudulent behavior, "our findings suggest that a large-scale policy effort targeting EHR-driven fraudulent coding, such as the one recently recommended by the HHS Office of Inspector General, is not likely to be useful. Substantial savings are unlikely to result even from a policy targeting certain subgroups of hospitals that might be expected to experience the greatest pressure to increase billing after investing in an EHR system."
Concerns that electronic health records will result in an uptick in Medicare payments to hospitals – for legitimate or fraudulent reasons – appear to be unfounded.
Anecdotal reports have surfaced in the wake of a federal incentive program to push for the adoption of EHRs that hospitals might be using the systems to boost payments by more accurately capturing, and more accurately charging, for services rendered than previously recorded, by "upcoding" or selecting billing codes that reflect more intensive procedures or reflect a sicker patient population, or by simply "cloning" entries into an EHR to provide higher billing to multiple patients that might not reflect the care provided. These reports have led the Department of Health & Human Services Office of Inspector General to call for Medicare administrative and program integrity contractors to do more to detect potential fraud from the use of EHRs.
However, research by Julia Adler-Milstein, Ph.D., of the University of Michigan, Ann Arbor, and Dr. Ashish Jha of the Harvard School of Public Health, Boston, suggests that this kind of fraud has not been an issue.
"We found that hospitals that adopted EHRs increased billing to Medicare, but at a rate comparable to that of matched controls of non-EHR adopters," the researchers wrote in the article appearing in the July issue of Health Affairs (July 2014 [doi:10.1377/hlthaff.2014.0023]).
Researchers looked at 393 hospitals that had newly adopted a basic EHR (181 that adopted between 2008 and 2009 and 212 that adopted between 2009 and 2010) and compared them to 782 control hospitals that did not adopt during the same periods. New adopters were predominantly nonteaching (61%), for-profit (70%), and medium-size (47%) hospitals.
In the research models, "we found no significant relationship between EHR adoption and patient acuity," the report states. Also, "adopters and controls had indistinguishable changes in Medicare payments. Between the pre- and postadoption periods, payment per discharge to adopters grew by $849 and to controls by $945. This $96 difference in difference was not in the predicted direction, but it was not significant, either (P = .673)," the researchers wrote.
They suggested that the results were due to hospitals heavily investing in optimizing coding before adopting EHRs.
"Hospitals operate on thin financial margins and therefore likely work hard to maximize reimbursement," the researchers wrote. "Thus, simply having more electronic data or better documentation may not provide as much of an opportunity to increase coding as has been postulated."
They concluded that while there will always be outliers that engage in fraudulent behavior, "our findings suggest that a large-scale policy effort targeting EHR-driven fraudulent coding, such as the one recently recommended by the HHS Office of Inspector General, is not likely to be useful. Substantial savings are unlikely to result even from a policy targeting certain subgroups of hospitals that might be expected to experience the greatest pressure to increase billing after investing in an EHR system."
FROM HEALTH AFFAIRS
Major finding: Hospitals adopting EHRs are not showing greater increases in Medicare payments or patient acuity.
Data source: Analysis of data provided by the Centers for Medicare & Medicaid Services and the American Hospital Association.
Disclosures: Article was submitted to Health Affairs, no outside sources of financing were used to fund the research. Authors reported no financial disclosures.
CDC: Cross-contamination, lab closure shouldn’t impact flu season efforts
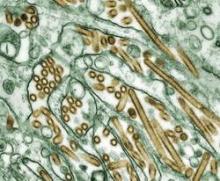
Cross-contamination of nonpathogenic avian influenza with a highly pathogenic H5N1 strain should not derail preparations for the upcoming influenza season, the Centers for Disease Control and Prevention announced July 11.
"We are confident that we will be able to get the flu lab reopened in time to do the essential work it does, like helping to prepare the influenza vaccinations for Americans and tracking the spread of flu around the world and around the country," CDC Director Dr. Tom Frieden said in a press conference. "We don’t see any risk to keeping the lab closed until we have a full assessment of what happened and we are sure that we can prevent future occurrences."
The CDC closed the influenza lab after Dr. Frieden learned that the cross-contamination of the sample had occurred, a revelation he called "distressing" since the cross-contamination was identified by USDA researchers on or about May 23. The CDC confirmed that the contamination occurred within its labs.
"We are still just beginning the investigation to determine how this happened," he said. "The work was done in one room. That leads to some early hypotheses of what might have happened, but it is going to take a detailed investigation and we may not know for certain exactly what happened, but we will do everything we can to find out." The agency said there were no exposures as a result of the incident.
The revelation came as the CDC released a report on its investigation into a June 5 incident of unintentional release of potentially viable anthrax within its Roybal Campus in Atlanta.
The agency attributed that incident to the use of unapproved sterilization techniques, the transfer of materials not confirmed to be inactive, the use of pathogenic Bacillus anthracis when nonpathogenic strains would have been more appropriate, inadequate knowledge of peer-reviewed literature, and a lack of standard operating procedure or process on inactivation and transfer to cover all procedures done with select agents in the Bioterrorism Rapid Response and Advanced Technology Laboratory.
None of the staff potentially exposed has become ill with anthrax, the agency said.
As a result of these incidents, the CDC issued a moratorium on the movement of dangerous biological agents, including infectious agents and active or inactivated specimens, from its labs. The moratorium will remain in place pending review by an advisory council. Dr. Frieden also called on a review of the agency’s safety culture to ensure that events like these don’t happen again.
CDC also announced that six undocumented vials of smallpox were discovered on the Bethesda, Md., campus of the National Institutes of Health. Dr. Frieden said that the vials were dated Feb. 10, 1954 – before the eradication of smallpox. He said they were not created with any malicious intent.
"The problem was not in the creation of the materials, but in inventory control which allowed them to remain unsecured for decades," Dr. Frieden said. "They should have been destroyed decades ago, and once we complete [testing on them] we will destroy them."
Cross-contamination of nonpathogenic avian influenza with a highly pathogenic H5N1 strain should not derail preparations for the upcoming influenza season, the Centers for Disease Control and Prevention announced July 11.
"We are confident that we will be able to get the flu lab reopened in time to do the essential work it does, like helping to prepare the influenza vaccinations for Americans and tracking the spread of flu around the world and around the country," CDC Director Dr. Tom Frieden said in a press conference. "We don’t see any risk to keeping the lab closed until we have a full assessment of what happened and we are sure that we can prevent future occurrences."
The CDC closed the influenza lab after Dr. Frieden learned that the cross-contamination of the sample had occurred, a revelation he called "distressing" since the cross-contamination was identified by USDA researchers on or about May 23. The CDC confirmed that the contamination occurred within its labs.
"We are still just beginning the investigation to determine how this happened," he said. "The work was done in one room. That leads to some early hypotheses of what might have happened, but it is going to take a detailed investigation and we may not know for certain exactly what happened, but we will do everything we can to find out." The agency said there were no exposures as a result of the incident.
The revelation came as the CDC released a report on its investigation into a June 5 incident of unintentional release of potentially viable anthrax within its Roybal Campus in Atlanta.
The agency attributed that incident to the use of unapproved sterilization techniques, the transfer of materials not confirmed to be inactive, the use of pathogenic Bacillus anthracis when nonpathogenic strains would have been more appropriate, inadequate knowledge of peer-reviewed literature, and a lack of standard operating procedure or process on inactivation and transfer to cover all procedures done with select agents in the Bioterrorism Rapid Response and Advanced Technology Laboratory.
None of the staff potentially exposed has become ill with anthrax, the agency said.
As a result of these incidents, the CDC issued a moratorium on the movement of dangerous biological agents, including infectious agents and active or inactivated specimens, from its labs. The moratorium will remain in place pending review by an advisory council. Dr. Frieden also called on a review of the agency’s safety culture to ensure that events like these don’t happen again.
CDC also announced that six undocumented vials of smallpox were discovered on the Bethesda, Md., campus of the National Institutes of Health. Dr. Frieden said that the vials were dated Feb. 10, 1954 – before the eradication of smallpox. He said they were not created with any malicious intent.
"The problem was not in the creation of the materials, but in inventory control which allowed them to remain unsecured for decades," Dr. Frieden said. "They should have been destroyed decades ago, and once we complete [testing on them] we will destroy them."
Cross-contamination of nonpathogenic avian influenza with a highly pathogenic H5N1 strain should not derail preparations for the upcoming influenza season, the Centers for Disease Control and Prevention announced July 11.
"We are confident that we will be able to get the flu lab reopened in time to do the essential work it does, like helping to prepare the influenza vaccinations for Americans and tracking the spread of flu around the world and around the country," CDC Director Dr. Tom Frieden said in a press conference. "We don’t see any risk to keeping the lab closed until we have a full assessment of what happened and we are sure that we can prevent future occurrences."
The CDC closed the influenza lab after Dr. Frieden learned that the cross-contamination of the sample had occurred, a revelation he called "distressing" since the cross-contamination was identified by USDA researchers on or about May 23. The CDC confirmed that the contamination occurred within its labs.
"We are still just beginning the investigation to determine how this happened," he said. "The work was done in one room. That leads to some early hypotheses of what might have happened, but it is going to take a detailed investigation and we may not know for certain exactly what happened, but we will do everything we can to find out." The agency said there were no exposures as a result of the incident.
The revelation came as the CDC released a report on its investigation into a June 5 incident of unintentional release of potentially viable anthrax within its Roybal Campus in Atlanta.
The agency attributed that incident to the use of unapproved sterilization techniques, the transfer of materials not confirmed to be inactive, the use of pathogenic Bacillus anthracis when nonpathogenic strains would have been more appropriate, inadequate knowledge of peer-reviewed literature, and a lack of standard operating procedure or process on inactivation and transfer to cover all procedures done with select agents in the Bioterrorism Rapid Response and Advanced Technology Laboratory.
None of the staff potentially exposed has become ill with anthrax, the agency said.
As a result of these incidents, the CDC issued a moratorium on the movement of dangerous biological agents, including infectious agents and active or inactivated specimens, from its labs. The moratorium will remain in place pending review by an advisory council. Dr. Frieden also called on a review of the agency’s safety culture to ensure that events like these don’t happen again.
CDC also announced that six undocumented vials of smallpox were discovered on the Bethesda, Md., campus of the National Institutes of Health. Dr. Frieden said that the vials were dated Feb. 10, 1954 – before the eradication of smallpox. He said they were not created with any malicious intent.
"The problem was not in the creation of the materials, but in inventory control which allowed them to remain unsecured for decades," Dr. Frieden said. "They should have been destroyed decades ago, and once we complete [testing on them] we will destroy them."
CMS proposes TMVR coverage with evidence development
The Centers for Medicare & Medicaid Services is proposing to cover transcatheter mitral valve repair procedures with the condition that the procedure is accompanied with the collection of data for research purposes to determine whether the evidence shows that TMVR is reasonable and necessary.
Heart teams and hospitals will be eligible for coverage. They must be participate in a prospective audited registry that will follow patients receiving the procedure under its Food and Drug Administration–approved indication for at least 1 year and track a number of outcomes, including quality of life, functional capacity, stroke, all-cause mortality, transient ischemic events, major vascular events, renal complications, repeat mitral valve surgery, or other mitral procedures and worsening mitral regurgitation. The registry "must be designed to permit identification and analysis of patient, practitioner and facility level variables that predict each of these outcomes," the agency said in the proposed coverage decision memo.
FDA approved the first transcatheter mitral valve repair (TMVR) device, Abbott Vascular’s MitraClip, in October 2013, following the agency’s Circulatory System Devices panel’s 5-3 vote in March 2013 that the device’s benefits outweighed its risks.
CMS is looking for information about outcomes and adverse events related to the procedure when conducted in a real-world setting, compared with those in pivotal clinical studies in general and within subpopulations; the long-term (at least 5 years) durability, outcomes, and adverse events, as well as demographic differences between registry patients and those enrolled in the clinical trials.
The agency also is proposing to cover TMVR for indications not expressly listed in the FDA approval when performed within an FDA-approved randomized clinical trial that evaluates a patient’s post TMVR quality of life and post-TMVR functional capacity at 1 year, compared with both outcomes prior to the procedure, as well as tracking outcomes similar to those for the registries covering the approved indication.
CMS opened the proposed TMVR coverage with evidence development proposal following a formal request from the Society of Thoracic Surgeons, the American College of Cardiology Foundation, the Society for Cardiovascular Angiography and Interventions and the American Association for Thoracic Surgery.
The agency is soliciting comments on the proposed coverage decision and will respond to those comments in its final decision memorandum. A deadline for comment submission was not listed in the proposal.
The Centers for Medicare & Medicaid Services is proposing to cover transcatheter mitral valve repair procedures with the condition that the procedure is accompanied with the collection of data for research purposes to determine whether the evidence shows that TMVR is reasonable and necessary.
Heart teams and hospitals will be eligible for coverage. They must be participate in a prospective audited registry that will follow patients receiving the procedure under its Food and Drug Administration–approved indication for at least 1 year and track a number of outcomes, including quality of life, functional capacity, stroke, all-cause mortality, transient ischemic events, major vascular events, renal complications, repeat mitral valve surgery, or other mitral procedures and worsening mitral regurgitation. The registry "must be designed to permit identification and analysis of patient, practitioner and facility level variables that predict each of these outcomes," the agency said in the proposed coverage decision memo.
FDA approved the first transcatheter mitral valve repair (TMVR) device, Abbott Vascular’s MitraClip, in October 2013, following the agency’s Circulatory System Devices panel’s 5-3 vote in March 2013 that the device’s benefits outweighed its risks.
CMS is looking for information about outcomes and adverse events related to the procedure when conducted in a real-world setting, compared with those in pivotal clinical studies in general and within subpopulations; the long-term (at least 5 years) durability, outcomes, and adverse events, as well as demographic differences between registry patients and those enrolled in the clinical trials.
The agency also is proposing to cover TMVR for indications not expressly listed in the FDA approval when performed within an FDA-approved randomized clinical trial that evaluates a patient’s post TMVR quality of life and post-TMVR functional capacity at 1 year, compared with both outcomes prior to the procedure, as well as tracking outcomes similar to those for the registries covering the approved indication.
CMS opened the proposed TMVR coverage with evidence development proposal following a formal request from the Society of Thoracic Surgeons, the American College of Cardiology Foundation, the Society for Cardiovascular Angiography and Interventions and the American Association for Thoracic Surgery.
The agency is soliciting comments on the proposed coverage decision and will respond to those comments in its final decision memorandum. A deadline for comment submission was not listed in the proposal.
The Centers for Medicare & Medicaid Services is proposing to cover transcatheter mitral valve repair procedures with the condition that the procedure is accompanied with the collection of data for research purposes to determine whether the evidence shows that TMVR is reasonable and necessary.
Heart teams and hospitals will be eligible for coverage. They must be participate in a prospective audited registry that will follow patients receiving the procedure under its Food and Drug Administration–approved indication for at least 1 year and track a number of outcomes, including quality of life, functional capacity, stroke, all-cause mortality, transient ischemic events, major vascular events, renal complications, repeat mitral valve surgery, or other mitral procedures and worsening mitral regurgitation. The registry "must be designed to permit identification and analysis of patient, practitioner and facility level variables that predict each of these outcomes," the agency said in the proposed coverage decision memo.
FDA approved the first transcatheter mitral valve repair (TMVR) device, Abbott Vascular’s MitraClip, in October 2013, following the agency’s Circulatory System Devices panel’s 5-3 vote in March 2013 that the device’s benefits outweighed its risks.
CMS is looking for information about outcomes and adverse events related to the procedure when conducted in a real-world setting, compared with those in pivotal clinical studies in general and within subpopulations; the long-term (at least 5 years) durability, outcomes, and adverse events, as well as demographic differences between registry patients and those enrolled in the clinical trials.
The agency also is proposing to cover TMVR for indications not expressly listed in the FDA approval when performed within an FDA-approved randomized clinical trial that evaluates a patient’s post TMVR quality of life and post-TMVR functional capacity at 1 year, compared with both outcomes prior to the procedure, as well as tracking outcomes similar to those for the registries covering the approved indication.
CMS opened the proposed TMVR coverage with evidence development proposal following a formal request from the Society of Thoracic Surgeons, the American College of Cardiology Foundation, the Society for Cardiovascular Angiography and Interventions and the American Association for Thoracic Surgery.
The agency is soliciting comments on the proposed coverage decision and will respond to those comments in its final decision memorandum. A deadline for comment submission was not listed in the proposal.
HHS commits $83 million in ACA money to train primary care docs
The Department of Health & Human Services will use $83.4 million in Affordable Care Act funding to train more than 550 residents during the 2014-2015 academic year.
Residents will be trained in family medicine, internal medicine, pediatrics, obstetrics and gynecology, psychiatry, geriatrics, and general dentistry at 60 teaching health centers across the country. The funding increases the number of residents trained from the previous academic year by more than 200.
The money comes from the Teaching Health Center Graduate Medical Education program, a $230 million, 5-year initiative designed to support increased numbers of primary care residents and dentists trained in community-based ambulatory patient care settings. The program began in 2011.
The new funding also increases the number of states with teaching health centers from 21 to 24, spanning a variety of settings, including urban, rural, and tribal communities nationwide.
The Department of Health & Human Services will use $83.4 million in Affordable Care Act funding to train more than 550 residents during the 2014-2015 academic year.
Residents will be trained in family medicine, internal medicine, pediatrics, obstetrics and gynecology, psychiatry, geriatrics, and general dentistry at 60 teaching health centers across the country. The funding increases the number of residents trained from the previous academic year by more than 200.
The money comes from the Teaching Health Center Graduate Medical Education program, a $230 million, 5-year initiative designed to support increased numbers of primary care residents and dentists trained in community-based ambulatory patient care settings. The program began in 2011.
The new funding also increases the number of states with teaching health centers from 21 to 24, spanning a variety of settings, including urban, rural, and tribal communities nationwide.
The Department of Health & Human Services will use $83.4 million in Affordable Care Act funding to train more than 550 residents during the 2014-2015 academic year.
Residents will be trained in family medicine, internal medicine, pediatrics, obstetrics and gynecology, psychiatry, geriatrics, and general dentistry at 60 teaching health centers across the country. The funding increases the number of residents trained from the previous academic year by more than 200.
The money comes from the Teaching Health Center Graduate Medical Education program, a $230 million, 5-year initiative designed to support increased numbers of primary care residents and dentists trained in community-based ambulatory patient care settings. The program began in 2011.
The new funding also increases the number of states with teaching health centers from 21 to 24, spanning a variety of settings, including urban, rural, and tribal communities nationwide.
NIH expands its Undiagnosed Diseases Network
Seven new sites join the National Institutes of Health’s Clinical Center in the Undiagnosed Diseases Network.
The network expands the NIH focus on "the rarest of disorders, those that affect fewer than 50 people in the entire world," Dr. Eric Green, director of the National Human Genome Research Institute, said during a July 1 press conference. "They are so rare that they may never have been discovered or doctors may never have encountered them."
In addition to the current Bethesda, Md., site at the NIH Clinical Center, the following institutions are now involved:
• Baylor College of Medicine, Houston.
• Boston Children’s Hospital, Brigham and Women’s Hospital, and Massachusetts General Hospital.
• Duke University, Durham, N.C.
• Stanford (Calif.) University.
University of California, Los Angeles.
• Vanderbilt University Medical Center, Nashville, Tenn.
The NIH Common Fund, which finances projects that cross through multiple individual institutes, has committed more than $120 million over 5 years fund the sites, as well as a coordinating center, gene function studies, and core laboratories.
The expanded Undiagnosed Diseases Network (UDN) will be "accelerating discovery and innovation in the way we diagnose and treat patients with previously undiagnosed diseases," said Dr. James Anderson, director of the NIH Division of Program Coordination, Planning, and Strategic Initiatives. "We anticipate the UDN will create a new paradigm in medical diagnostics that will improve our understanding of rare disorders and also generate insight into human biochemistry and physiology of common diseases."
Patients who have undiagnosed conditions can apply to be seen by the program. If selected, patients will be brought into one of the centers in the network for a week-long testing program. Currently, about 3,100 patients have applied and 750 have been accepted; 60% are adults. Once fully operational, the new sites are each expected to see about 50 patients a year. Applications take about 8-12 weeks to be evaluated, and there currently is a waiting list of 2-6 months to be seen by the multidisciplinary diagnostic team.
Data collected from the patients in the program ultimately will be made available to researchers outside of the network, though protocols on how it will be shared are still being developed.
Seven new sites join the National Institutes of Health’s Clinical Center in the Undiagnosed Diseases Network.
The network expands the NIH focus on "the rarest of disorders, those that affect fewer than 50 people in the entire world," Dr. Eric Green, director of the National Human Genome Research Institute, said during a July 1 press conference. "They are so rare that they may never have been discovered or doctors may never have encountered them."
In addition to the current Bethesda, Md., site at the NIH Clinical Center, the following institutions are now involved:
• Baylor College of Medicine, Houston.
• Boston Children’s Hospital, Brigham and Women’s Hospital, and Massachusetts General Hospital.
• Duke University, Durham, N.C.
• Stanford (Calif.) University.
University of California, Los Angeles.
• Vanderbilt University Medical Center, Nashville, Tenn.
The NIH Common Fund, which finances projects that cross through multiple individual institutes, has committed more than $120 million over 5 years fund the sites, as well as a coordinating center, gene function studies, and core laboratories.
The expanded Undiagnosed Diseases Network (UDN) will be "accelerating discovery and innovation in the way we diagnose and treat patients with previously undiagnosed diseases," said Dr. James Anderson, director of the NIH Division of Program Coordination, Planning, and Strategic Initiatives. "We anticipate the UDN will create a new paradigm in medical diagnostics that will improve our understanding of rare disorders and also generate insight into human biochemistry and physiology of common diseases."
Patients who have undiagnosed conditions can apply to be seen by the program. If selected, patients will be brought into one of the centers in the network for a week-long testing program. Currently, about 3,100 patients have applied and 750 have been accepted; 60% are adults. Once fully operational, the new sites are each expected to see about 50 patients a year. Applications take about 8-12 weeks to be evaluated, and there currently is a waiting list of 2-6 months to be seen by the multidisciplinary diagnostic team.
Data collected from the patients in the program ultimately will be made available to researchers outside of the network, though protocols on how it will be shared are still being developed.
Seven new sites join the National Institutes of Health’s Clinical Center in the Undiagnosed Diseases Network.
The network expands the NIH focus on "the rarest of disorders, those that affect fewer than 50 people in the entire world," Dr. Eric Green, director of the National Human Genome Research Institute, said during a July 1 press conference. "They are so rare that they may never have been discovered or doctors may never have encountered them."
In addition to the current Bethesda, Md., site at the NIH Clinical Center, the following institutions are now involved:
• Baylor College of Medicine, Houston.
• Boston Children’s Hospital, Brigham and Women’s Hospital, and Massachusetts General Hospital.
• Duke University, Durham, N.C.
• Stanford (Calif.) University.
University of California, Los Angeles.
• Vanderbilt University Medical Center, Nashville, Tenn.
The NIH Common Fund, which finances projects that cross through multiple individual institutes, has committed more than $120 million over 5 years fund the sites, as well as a coordinating center, gene function studies, and core laboratories.
The expanded Undiagnosed Diseases Network (UDN) will be "accelerating discovery and innovation in the way we diagnose and treat patients with previously undiagnosed diseases," said Dr. James Anderson, director of the NIH Division of Program Coordination, Planning, and Strategic Initiatives. "We anticipate the UDN will create a new paradigm in medical diagnostics that will improve our understanding of rare disorders and also generate insight into human biochemistry and physiology of common diseases."
Patients who have undiagnosed conditions can apply to be seen by the program. If selected, patients will be brought into one of the centers in the network for a week-long testing program. Currently, about 3,100 patients have applied and 750 have been accepted; 60% are adults. Once fully operational, the new sites are each expected to see about 50 patients a year. Applications take about 8-12 weeks to be evaluated, and there currently is a waiting list of 2-6 months to be seen by the multidisciplinary diagnostic team.
Data collected from the patients in the program ultimately will be made available to researchers outside of the network, though protocols on how it will be shared are still being developed.
More screening needed to detect injury, violence risk
Physicians need to do more to screen patients to find those at risk for preventable injuries and violence, according to the Centers for Disease Control and Prevention.
"Physicians and other health care workers have not yet included screening for injury risk into routine standard of care," representatives of the agency wrote in an article published July 2 in the online version of the Lancet (2014, July 2 [http://dx.doi.org/10.1016/S0140-6736(14)60074-x]).
The agency cited statistics that one in five adults visiting health care providers received counseling about injury prevention. The failure to provide such counseling is a function of time, according to the authors.
"This absence may be partly due to the increase in demands on practitioners – if primary care physicians were to satisfy fully the clinical recommendations of the U.S. Preventive Services Task Force, then they would need to devote longer than 7 hours per day to preventive services alone," according to Tamara M. Haegerich, Ph.D., associate director for science in the injury center in CDC’s Division of Unintentional Injury Prevention. "Managed care organizations and other health care institutions have not fully codified injury prevention counseling into clinical workflow and electronic medical records to improve the delivery of injury prevention services."
For 2010, the most frequent causes of deaths from unintentional injury included motor vehicle crashes (33,687 people), poisoning (33,041), falls (26,009), suffocation (6,165), drowning (3,782), and fire (2,845). Unintentional injury was the largest cause of potential life-years lost before age 65 years. Additionally, for nonfatal injuries, falling was the most common injury, leading to more than 9 million emergency department visits. The top three causes of death for people aged 1-30 years were unintentional injury, suicide, and homicide, which together accounted for close to 80% of deaths in this group. About 20% of deaths among the young were related to chronic diseases and only 1% was from infectious diseases.
One area in which physician counseling may be able to save lives is in prescription drug overdoses, according to the report. Overdose can occur through intentional or unintentional means, although most deaths from overdose are unintentional. In 2010, 38,329 people in the United States died from a drug overdose. Prescription drugs were involved in 22,134 of these deaths (nearly 60%). An overdose of opioid analgesics such as oxycodone, hydrocodone, and methadone accounted for 75% of prescription drug deaths. It is noteworthy that deaths from opioid analgesics have nearly quadrupled since 1990 and that four times more prescription painkillers were sold to pharmacies, hospitals, and doctors’ offices in 2010 than in 1999. Drug overdose is commonly viewed as an issue of substance misuse, mental health, or law enforcement rather than an injury and public health concern; however, this rise in overdose deaths coincides with an increase in the supply of prescription painkillers, indicating a need for intervention from health professionals.
Also in 2010, the 31.2 million unintentional and violence-related nonfatal injuries cost more than $513 billion in medical care and lost productivity, and this figure does not include costs associated with nonmedically treated injuries, legal costs, or indirect costs from other health problems associated with or exacerbated by violence and injuries.
The article notes that evidence-based interventions do exist to help prevent injuries and violence, "but too often they are not available, not affordable, or simply not used by patients, providers, and consumers. The gap between research and practice, or discovery and delivery, is large and continues to impede progress in the U.S.A."
However, opportunity now exists "to advance injury prevention through screening and referral for injury risk factors such as depression, domestic violence (for women of child-bearing age), alcohol misuse, and behavioral problems (for children)," according to Dr. Haegerich and her associates, who added that innovations in health information technology, such as clinical decision support tools embedded within electronic health records, "could enhance health providers’ ability to provide injury preventive services [such as triggering] alerts for screening on the basis of risk factors for patients, provide real-time information about evidence-based treatment guidelines, generate reports that share information about injury prevention with patients or automate referrals to community services."
Overall, the article calls for those in public health to work in partnership with clinical medicine "to ensure that health delivery systems are well integrated and are performing effectively, efficiently and equitably to prevent injury and improve outcomes throughout the continuum of care."
Physicians need to do more to screen patients to find those at risk for preventable injuries and violence, according to the Centers for Disease Control and Prevention.
"Physicians and other health care workers have not yet included screening for injury risk into routine standard of care," representatives of the agency wrote in an article published July 2 in the online version of the Lancet (2014, July 2 [http://dx.doi.org/10.1016/S0140-6736(14)60074-x]).
The agency cited statistics that one in five adults visiting health care providers received counseling about injury prevention. The failure to provide such counseling is a function of time, according to the authors.
"This absence may be partly due to the increase in demands on practitioners – if primary care physicians were to satisfy fully the clinical recommendations of the U.S. Preventive Services Task Force, then they would need to devote longer than 7 hours per day to preventive services alone," according to Tamara M. Haegerich, Ph.D., associate director for science in the injury center in CDC’s Division of Unintentional Injury Prevention. "Managed care organizations and other health care institutions have not fully codified injury prevention counseling into clinical workflow and electronic medical records to improve the delivery of injury prevention services."
For 2010, the most frequent causes of deaths from unintentional injury included motor vehicle crashes (33,687 people), poisoning (33,041), falls (26,009), suffocation (6,165), drowning (3,782), and fire (2,845). Unintentional injury was the largest cause of potential life-years lost before age 65 years. Additionally, for nonfatal injuries, falling was the most common injury, leading to more than 9 million emergency department visits. The top three causes of death for people aged 1-30 years were unintentional injury, suicide, and homicide, which together accounted for close to 80% of deaths in this group. About 20% of deaths among the young were related to chronic diseases and only 1% was from infectious diseases.
One area in which physician counseling may be able to save lives is in prescription drug overdoses, according to the report. Overdose can occur through intentional or unintentional means, although most deaths from overdose are unintentional. In 2010, 38,329 people in the United States died from a drug overdose. Prescription drugs were involved in 22,134 of these deaths (nearly 60%). An overdose of opioid analgesics such as oxycodone, hydrocodone, and methadone accounted for 75% of prescription drug deaths. It is noteworthy that deaths from opioid analgesics have nearly quadrupled since 1990 and that four times more prescription painkillers were sold to pharmacies, hospitals, and doctors’ offices in 2010 than in 1999. Drug overdose is commonly viewed as an issue of substance misuse, mental health, or law enforcement rather than an injury and public health concern; however, this rise in overdose deaths coincides with an increase in the supply of prescription painkillers, indicating a need for intervention from health professionals.
Also in 2010, the 31.2 million unintentional and violence-related nonfatal injuries cost more than $513 billion in medical care and lost productivity, and this figure does not include costs associated with nonmedically treated injuries, legal costs, or indirect costs from other health problems associated with or exacerbated by violence and injuries.
The article notes that evidence-based interventions do exist to help prevent injuries and violence, "but too often they are not available, not affordable, or simply not used by patients, providers, and consumers. The gap between research and practice, or discovery and delivery, is large and continues to impede progress in the U.S.A."
However, opportunity now exists "to advance injury prevention through screening and referral for injury risk factors such as depression, domestic violence (for women of child-bearing age), alcohol misuse, and behavioral problems (for children)," according to Dr. Haegerich and her associates, who added that innovations in health information technology, such as clinical decision support tools embedded within electronic health records, "could enhance health providers’ ability to provide injury preventive services [such as triggering] alerts for screening on the basis of risk factors for patients, provide real-time information about evidence-based treatment guidelines, generate reports that share information about injury prevention with patients or automate referrals to community services."
Overall, the article calls for those in public health to work in partnership with clinical medicine "to ensure that health delivery systems are well integrated and are performing effectively, efficiently and equitably to prevent injury and improve outcomes throughout the continuum of care."
Physicians need to do more to screen patients to find those at risk for preventable injuries and violence, according to the Centers for Disease Control and Prevention.
"Physicians and other health care workers have not yet included screening for injury risk into routine standard of care," representatives of the agency wrote in an article published July 2 in the online version of the Lancet (2014, July 2 [http://dx.doi.org/10.1016/S0140-6736(14)60074-x]).
The agency cited statistics that one in five adults visiting health care providers received counseling about injury prevention. The failure to provide such counseling is a function of time, according to the authors.
"This absence may be partly due to the increase in demands on practitioners – if primary care physicians were to satisfy fully the clinical recommendations of the U.S. Preventive Services Task Force, then they would need to devote longer than 7 hours per day to preventive services alone," according to Tamara M. Haegerich, Ph.D., associate director for science in the injury center in CDC’s Division of Unintentional Injury Prevention. "Managed care organizations and other health care institutions have not fully codified injury prevention counseling into clinical workflow and electronic medical records to improve the delivery of injury prevention services."
For 2010, the most frequent causes of deaths from unintentional injury included motor vehicle crashes (33,687 people), poisoning (33,041), falls (26,009), suffocation (6,165), drowning (3,782), and fire (2,845). Unintentional injury was the largest cause of potential life-years lost before age 65 years. Additionally, for nonfatal injuries, falling was the most common injury, leading to more than 9 million emergency department visits. The top three causes of death for people aged 1-30 years were unintentional injury, suicide, and homicide, which together accounted for close to 80% of deaths in this group. About 20% of deaths among the young were related to chronic diseases and only 1% was from infectious diseases.
One area in which physician counseling may be able to save lives is in prescription drug overdoses, according to the report. Overdose can occur through intentional or unintentional means, although most deaths from overdose are unintentional. In 2010, 38,329 people in the United States died from a drug overdose. Prescription drugs were involved in 22,134 of these deaths (nearly 60%). An overdose of opioid analgesics such as oxycodone, hydrocodone, and methadone accounted for 75% of prescription drug deaths. It is noteworthy that deaths from opioid analgesics have nearly quadrupled since 1990 and that four times more prescription painkillers were sold to pharmacies, hospitals, and doctors’ offices in 2010 than in 1999. Drug overdose is commonly viewed as an issue of substance misuse, mental health, or law enforcement rather than an injury and public health concern; however, this rise in overdose deaths coincides with an increase in the supply of prescription painkillers, indicating a need for intervention from health professionals.
Also in 2010, the 31.2 million unintentional and violence-related nonfatal injuries cost more than $513 billion in medical care and lost productivity, and this figure does not include costs associated with nonmedically treated injuries, legal costs, or indirect costs from other health problems associated with or exacerbated by violence and injuries.
The article notes that evidence-based interventions do exist to help prevent injuries and violence, "but too often they are not available, not affordable, or simply not used by patients, providers, and consumers. The gap between research and practice, or discovery and delivery, is large and continues to impede progress in the U.S.A."
However, opportunity now exists "to advance injury prevention through screening and referral for injury risk factors such as depression, domestic violence (for women of child-bearing age), alcohol misuse, and behavioral problems (for children)," according to Dr. Haegerich and her associates, who added that innovations in health information technology, such as clinical decision support tools embedded within electronic health records, "could enhance health providers’ ability to provide injury preventive services [such as triggering] alerts for screening on the basis of risk factors for patients, provide real-time information about evidence-based treatment guidelines, generate reports that share information about injury prevention with patients or automate referrals to community services."
Overall, the article calls for those in public health to work in partnership with clinical medicine "to ensure that health delivery systems are well integrated and are performing effectively, efficiently and equitably to prevent injury and improve outcomes throughout the continuum of care."
FROM THE LANCET
Key clinical point: It is now time to screen for preventable injury and violence.
Major finding: Nearly 80% of deaths between ages 1 and 30 years are from unintentional injury, suicide, and homicide, and more research is needed to determine what can be done to prevent this.
Data source: CDC research
Disclosures: CDC conducted the research for the article. No conflicts of interest were disclosed.
AHRQ report examines interventions for lowering readmissions in heart failure patients
Home-visiting programs, multidisciplinary heart failure clinics, and structured telephone support interventions "should receive the greatest consideration by systems or providers seeking to implement transitional care interventions" for people hospitalized for heart failure, according to a report issued May 27 by the Agency for Healthcare Research and Quality Effective Health Care Program.
But for these interventions to be effective, "you need a very mature infrastructure – communication infrastructure, information technology infrastructure, and systems-level infrastructure," Dr. Hiren Shah, medical director of the cardiac telemetry unit at Northwestern Memorial Hospital, Chicago, said in an interview about the implications of the report. "A lot of people point to cost and the fact that these interventions are expensive. But even if you have the ability to invest in these interventions, do you have the infrastructure that’s necessary to implement them?"
Further, the report lacks details on the cost-effectiveness of these interventions, a vital bit of information for hospitals looking to potentially implement them, Dr. Shah said. "It’s very important that not only do we know what may potentially work as an intervention, but we need to know whether that intervention or those interventions are cost effective. Within the scientific literature, we have very little information on the cost effectiveness of interventions."
The report’s conclusions are based on a systematic review and meta-analysis of the efficacy, comparative effectiveness, and harms of transitional care interventions aimed at reducing hospital readmissions and mortality for adults hospitalized with heart failure. The researchers, led by Dr. Cynthia Feltner of Duke University Medical Center in Durham, N.C., drew from 53 published articles on 47 randomized, controlled trials. Most studies compared a transitional care intervention with usual care, though the report notes that usual care was not consistently or well described.
In general, the trials included patients around age 70 years with moderate to severe heart failure. Most patients were prescribed an angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker; the percentage of patients prescribed a beta-blocker varied widely across the study populations. Trial settings included academic medical centers, Veteran Affairs hospitals, and community hospitals.
Few trials reported 30-day readmission rates, as most measured outcomes over 3-6 months. Home-visiting programs and multidisciplinary heart failure clinic interventions reduced all-cause readmissions and mortality; structured telephone support reduced heart failure–specific readmissions and mortality.
Successful programs and interventions included heart failure education that emphasized self-care and recognition of symptoms and weight monitoring; patient education about medications and adherence to regimens as well as evidence-based therapies before and after discharge; face-to-face contact with visiting or clinic personnel within a week following discharge; streamlined mechanisms for contacting care delivery personnel outside of scheduled visits; and mechanisms for postdischarge medication adjustment.
"Separating out individual components from the overall categories [or "bundles"] of interventions that showed efficacy was not possible," the report notes.
None of the investigators have affiliations or financial involvements that constitute a conflict of interest with the material presented in the report.
Home-visiting programs, multidisciplinary heart failure clinics, and structured telephone support interventions "should receive the greatest consideration by systems or providers seeking to implement transitional care interventions" for people hospitalized for heart failure, according to a report issued May 27 by the Agency for Healthcare Research and Quality Effective Health Care Program.
But for these interventions to be effective, "you need a very mature infrastructure – communication infrastructure, information technology infrastructure, and systems-level infrastructure," Dr. Hiren Shah, medical director of the cardiac telemetry unit at Northwestern Memorial Hospital, Chicago, said in an interview about the implications of the report. "A lot of people point to cost and the fact that these interventions are expensive. But even if you have the ability to invest in these interventions, do you have the infrastructure that’s necessary to implement them?"
Further, the report lacks details on the cost-effectiveness of these interventions, a vital bit of information for hospitals looking to potentially implement them, Dr. Shah said. "It’s very important that not only do we know what may potentially work as an intervention, but we need to know whether that intervention or those interventions are cost effective. Within the scientific literature, we have very little information on the cost effectiveness of interventions."
The report’s conclusions are based on a systematic review and meta-analysis of the efficacy, comparative effectiveness, and harms of transitional care interventions aimed at reducing hospital readmissions and mortality for adults hospitalized with heart failure. The researchers, led by Dr. Cynthia Feltner of Duke University Medical Center in Durham, N.C., drew from 53 published articles on 47 randomized, controlled trials. Most studies compared a transitional care intervention with usual care, though the report notes that usual care was not consistently or well described.
In general, the trials included patients around age 70 years with moderate to severe heart failure. Most patients were prescribed an angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker; the percentage of patients prescribed a beta-blocker varied widely across the study populations. Trial settings included academic medical centers, Veteran Affairs hospitals, and community hospitals.
Few trials reported 30-day readmission rates, as most measured outcomes over 3-6 months. Home-visiting programs and multidisciplinary heart failure clinic interventions reduced all-cause readmissions and mortality; structured telephone support reduced heart failure–specific readmissions and mortality.
Successful programs and interventions included heart failure education that emphasized self-care and recognition of symptoms and weight monitoring; patient education about medications and adherence to regimens as well as evidence-based therapies before and after discharge; face-to-face contact with visiting or clinic personnel within a week following discharge; streamlined mechanisms for contacting care delivery personnel outside of scheduled visits; and mechanisms for postdischarge medication adjustment.
"Separating out individual components from the overall categories [or "bundles"] of interventions that showed efficacy was not possible," the report notes.
None of the investigators have affiliations or financial involvements that constitute a conflict of interest with the material presented in the report.
Home-visiting programs, multidisciplinary heart failure clinics, and structured telephone support interventions "should receive the greatest consideration by systems or providers seeking to implement transitional care interventions" for people hospitalized for heart failure, according to a report issued May 27 by the Agency for Healthcare Research and Quality Effective Health Care Program.
But for these interventions to be effective, "you need a very mature infrastructure – communication infrastructure, information technology infrastructure, and systems-level infrastructure," Dr. Hiren Shah, medical director of the cardiac telemetry unit at Northwestern Memorial Hospital, Chicago, said in an interview about the implications of the report. "A lot of people point to cost and the fact that these interventions are expensive. But even if you have the ability to invest in these interventions, do you have the infrastructure that’s necessary to implement them?"
Further, the report lacks details on the cost-effectiveness of these interventions, a vital bit of information for hospitals looking to potentially implement them, Dr. Shah said. "It’s very important that not only do we know what may potentially work as an intervention, but we need to know whether that intervention or those interventions are cost effective. Within the scientific literature, we have very little information on the cost effectiveness of interventions."
The report’s conclusions are based on a systematic review and meta-analysis of the efficacy, comparative effectiveness, and harms of transitional care interventions aimed at reducing hospital readmissions and mortality for adults hospitalized with heart failure. The researchers, led by Dr. Cynthia Feltner of Duke University Medical Center in Durham, N.C., drew from 53 published articles on 47 randomized, controlled trials. Most studies compared a transitional care intervention with usual care, though the report notes that usual care was not consistently or well described.
In general, the trials included patients around age 70 years with moderate to severe heart failure. Most patients were prescribed an angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker; the percentage of patients prescribed a beta-blocker varied widely across the study populations. Trial settings included academic medical centers, Veteran Affairs hospitals, and community hospitals.
Few trials reported 30-day readmission rates, as most measured outcomes over 3-6 months. Home-visiting programs and multidisciplinary heart failure clinic interventions reduced all-cause readmissions and mortality; structured telephone support reduced heart failure–specific readmissions and mortality.
Successful programs and interventions included heart failure education that emphasized self-care and recognition of symptoms and weight monitoring; patient education about medications and adherence to regimens as well as evidence-based therapies before and after discharge; face-to-face contact with visiting or clinic personnel within a week following discharge; streamlined mechanisms for contacting care delivery personnel outside of scheduled visits; and mechanisms for postdischarge medication adjustment.
"Separating out individual components from the overall categories [or "bundles"] of interventions that showed efficacy was not possible," the report notes.
None of the investigators have affiliations or financial involvements that constitute a conflict of interest with the material presented in the report.
CDC: Teen smoking hits lowest level since 1991
Cigarette smoking among high school students has dropped to 15.7% – the lowest level recorded by the Youth Risk Behavior Surveillance System, the Centers for Disease Control and Prevention announced June 12.
The report shows a decrease from the 18.1% rate found in 2011 and continues a downward trend since the peak rate of 36.4% was recorded in 1997.
"That meets the Healthy People 2020 objective of under 16%, and that’s good news," Dr. Tom Frieden, CDC director, said during a news conference today. "But we still face big challenges in reducing overall tobacco use."
While cigarette smoking is down, other nationwide surveys show increased use of hookah and e-cigarettes. Further, overall tobacco use (cigarettes, cigars, and smokeless tobacco) rates are at 22.4%, according to the report, also continuing a downward trend from 43.4% reported in 1997.
"While this particular report doesn’t have data on e-cigarette use among high school students, we know that use of e-cigarettes is skyrocketing, and we’re concerned about that," Dr. Frieden said. "We’re particularly concerned with e-cigarettes reglamorizing smoking traditional cigarettes and maybe making it more complicated to enforce smoke-free laws that protect all nonsmokers."
He noted that young people are highly vulnerable to social, environmental, and physical influences that encourage them to start smoking and "no kids should be exposed to advertising that glorifies the use of nicotine or be able to easily buy e-cigarettes because their sales have not been restricted."
The survey found that of teens who drive, 41% reported texting or e-mailing while driving.
Sex amongst teens is down, with 34% of respondents reporting they were sexually active (had sexual intercourse during the past 3 months prior to being surveyed) in 2013 vs. 38% in 1991. Among the sexually active, condom use declined to 59% in 2013 from 63% in 2003, after having increased in the 1990s and early 2000s.
The percentage of teens who are sexually active is "too high," Dr. Frieden said, but it is going in the right direction. However the trend in condom use "shows the need for continued efforts from parents, schools, and communities to educate and ensure that [teens] have the knowledge and skills they need to protect themselves from HIV, STDs, and teen pregnancy."
Soda consumption – defined as drinking 1 or more servings per day – declined from 34% in 2007 to 27% in 2013. But teens are spending more time in front of a computer, with high school students spending 3 or more hours per day on a PCs, laptops, tablets, or smartphones for non–school related activities, nearly doubling from 2003 (22%) to 2013 (41%).
"We are concerned by the amount of screen time. It cuts into time for physical activity," Dr. Frieden said. "It cuts into time for sleep. It cuts into time for interacting in a healthy way with friends and learning. It’s a trend that we’re noting and some of this is ... a shift from watching TV on the television to watching it on the computer screen, but it’s still a whole lot of time being inactive, and that is a concern."
Survey results are based on 13,583 usable questionnaires collected from 148 public and private schools nationwide, with surveys conducted during the spring of 2013.
Cigarette smoking among high school students has dropped to 15.7% – the lowest level recorded by the Youth Risk Behavior Surveillance System, the Centers for Disease Control and Prevention announced June 12.
The report shows a decrease from the 18.1% rate found in 2011 and continues a downward trend since the peak rate of 36.4% was recorded in 1997.
"That meets the Healthy People 2020 objective of under 16%, and that’s good news," Dr. Tom Frieden, CDC director, said during a news conference today. "But we still face big challenges in reducing overall tobacco use."
While cigarette smoking is down, other nationwide surveys show increased use of hookah and e-cigarettes. Further, overall tobacco use (cigarettes, cigars, and smokeless tobacco) rates are at 22.4%, according to the report, also continuing a downward trend from 43.4% reported in 1997.
"While this particular report doesn’t have data on e-cigarette use among high school students, we know that use of e-cigarettes is skyrocketing, and we’re concerned about that," Dr. Frieden said. "We’re particularly concerned with e-cigarettes reglamorizing smoking traditional cigarettes and maybe making it more complicated to enforce smoke-free laws that protect all nonsmokers."
He noted that young people are highly vulnerable to social, environmental, and physical influences that encourage them to start smoking and "no kids should be exposed to advertising that glorifies the use of nicotine or be able to easily buy e-cigarettes because their sales have not been restricted."
The survey found that of teens who drive, 41% reported texting or e-mailing while driving.
Sex amongst teens is down, with 34% of respondents reporting they were sexually active (had sexual intercourse during the past 3 months prior to being surveyed) in 2013 vs. 38% in 1991. Among the sexually active, condom use declined to 59% in 2013 from 63% in 2003, after having increased in the 1990s and early 2000s.
The percentage of teens who are sexually active is "too high," Dr. Frieden said, but it is going in the right direction. However the trend in condom use "shows the need for continued efforts from parents, schools, and communities to educate and ensure that [teens] have the knowledge and skills they need to protect themselves from HIV, STDs, and teen pregnancy."
Soda consumption – defined as drinking 1 or more servings per day – declined from 34% in 2007 to 27% in 2013. But teens are spending more time in front of a computer, with high school students spending 3 or more hours per day on a PCs, laptops, tablets, or smartphones for non–school related activities, nearly doubling from 2003 (22%) to 2013 (41%).
"We are concerned by the amount of screen time. It cuts into time for physical activity," Dr. Frieden said. "It cuts into time for sleep. It cuts into time for interacting in a healthy way with friends and learning. It’s a trend that we’re noting and some of this is ... a shift from watching TV on the television to watching it on the computer screen, but it’s still a whole lot of time being inactive, and that is a concern."
Survey results are based on 13,583 usable questionnaires collected from 148 public and private schools nationwide, with surveys conducted during the spring of 2013.
Cigarette smoking among high school students has dropped to 15.7% – the lowest level recorded by the Youth Risk Behavior Surveillance System, the Centers for Disease Control and Prevention announced June 12.
The report shows a decrease from the 18.1% rate found in 2011 and continues a downward trend since the peak rate of 36.4% was recorded in 1997.
"That meets the Healthy People 2020 objective of under 16%, and that’s good news," Dr. Tom Frieden, CDC director, said during a news conference today. "But we still face big challenges in reducing overall tobacco use."
While cigarette smoking is down, other nationwide surveys show increased use of hookah and e-cigarettes. Further, overall tobacco use (cigarettes, cigars, and smokeless tobacco) rates are at 22.4%, according to the report, also continuing a downward trend from 43.4% reported in 1997.
"While this particular report doesn’t have data on e-cigarette use among high school students, we know that use of e-cigarettes is skyrocketing, and we’re concerned about that," Dr. Frieden said. "We’re particularly concerned with e-cigarettes reglamorizing smoking traditional cigarettes and maybe making it more complicated to enforce smoke-free laws that protect all nonsmokers."
He noted that young people are highly vulnerable to social, environmental, and physical influences that encourage them to start smoking and "no kids should be exposed to advertising that glorifies the use of nicotine or be able to easily buy e-cigarettes because their sales have not been restricted."
The survey found that of teens who drive, 41% reported texting or e-mailing while driving.
Sex amongst teens is down, with 34% of respondents reporting they were sexually active (had sexual intercourse during the past 3 months prior to being surveyed) in 2013 vs. 38% in 1991. Among the sexually active, condom use declined to 59% in 2013 from 63% in 2003, after having increased in the 1990s and early 2000s.
The percentage of teens who are sexually active is "too high," Dr. Frieden said, but it is going in the right direction. However the trend in condom use "shows the need for continued efforts from parents, schools, and communities to educate and ensure that [teens] have the knowledge and skills they need to protect themselves from HIV, STDs, and teen pregnancy."
Soda consumption – defined as drinking 1 or more servings per day – declined from 34% in 2007 to 27% in 2013. But teens are spending more time in front of a computer, with high school students spending 3 or more hours per day on a PCs, laptops, tablets, or smartphones for non–school related activities, nearly doubling from 2003 (22%) to 2013 (41%).
"We are concerned by the amount of screen time. It cuts into time for physical activity," Dr. Frieden said. "It cuts into time for sleep. It cuts into time for interacting in a healthy way with friends and learning. It’s a trend that we’re noting and some of this is ... a shift from watching TV on the television to watching it on the computer screen, but it’s still a whole lot of time being inactive, and that is a concern."
Survey results are based on 13,583 usable questionnaires collected from 148 public and private schools nationwide, with surveys conducted during the spring of 2013.
FROM MMWR
Feds urge pregnant women, young children to eat more fish
The Food and Drug Administration and the Environmental Protection Agency are encouraging pregnant women, as well as women who may become pregnant or are breastfeeding, and young children to eat more fish, setting for the first time a recommended lower limit of fish consumption to promote health.
In draft guidance released June 10, the agencies are calling for women to consume 8-12 ounces of a variety of fish that are lower in mercury; that amount works out to an average of two to three servings per week. Among the types of fish highlighted that are lower in mercury are salmon, shrimp, pollock, tuna (light canned), tilapia, catfish, and cod.
The U.S. Department of Agriculture suggests an amount of 3-5 ounces per week for children under the age of 6 and 4-6 ounces per week for children aged 6-8, the agencies said in an accompanying question-and-answer set. Appropriate amounts of fish for older children would increase up to the adult recommendation. Children should not be given fish until they are at least 6 months of age.
The agencies recommend four types of fish to avoid because of mercury content: tilefish from the Gulf of Mexico, shark, swordfish, and king mackerel. They also recommend limiting white (albacore) tuna to 6 ounces per week for adults and even less for children.
In addition, the agency is advising that those eating fish caught in local waters should listen for local advisories regarding those fish and, if no advice is available, fish consumption from those sources should be limited to 6 ounces per week in pregnant women and 1-3 ounces for young children. The recommendation reiterates that pregnant women and young children should avoid eating raw fish.
The agencies noted that they are issuing this draft guidance because recent reports "show many pregnant women in the United States are not consuming fish recommended" by 2010 United States Department of Agriculture guidelines. The agencies added that there is "longstanding evidence of the nutritional value of fish in the diet. Fish contain high-quality protein, many vitamins and minerals, omega-3 fatty acid, and are mostly low in saturated fat, and some fish even contain vitamin D. The nutritional value of fish is especially important during growth and development before birth, in early infancy for breastfed infants, and in childhood."
Citing its own analysis of seafood consumption data from more than 1,000 pregnant women in the United States, the FDA noted that 21% ate no fish in the previous month and those who ate fish consumed far less than recommended in USDA guidelines, with 50% eating fewer than 2 ounces per week and 75% eating fewer than 4 ounces per week.
This draft guidance would replace similar recommendations issued by the FDA/EPA in March 2004, with a recommendation of simply up to 12 ounces of a variety of fish per week (two average meals), avoiding the same four identified types of fish because of their high mercury content. Previous guidance did not set a recommended lower limit of consumption.
The agencies will begin accepting comments on new guidance June 11.
The Food and Drug Administration and the Environmental Protection Agency are encouraging pregnant women, as well as women who may become pregnant or are breastfeeding, and young children to eat more fish, setting for the first time a recommended lower limit of fish consumption to promote health.
In draft guidance released June 10, the agencies are calling for women to consume 8-12 ounces of a variety of fish that are lower in mercury; that amount works out to an average of two to three servings per week. Among the types of fish highlighted that are lower in mercury are salmon, shrimp, pollock, tuna (light canned), tilapia, catfish, and cod.
The U.S. Department of Agriculture suggests an amount of 3-5 ounces per week for children under the age of 6 and 4-6 ounces per week for children aged 6-8, the agencies said in an accompanying question-and-answer set. Appropriate amounts of fish for older children would increase up to the adult recommendation. Children should not be given fish until they are at least 6 months of age.
The agencies recommend four types of fish to avoid because of mercury content: tilefish from the Gulf of Mexico, shark, swordfish, and king mackerel. They also recommend limiting white (albacore) tuna to 6 ounces per week for adults and even less for children.
In addition, the agency is advising that those eating fish caught in local waters should listen for local advisories regarding those fish and, if no advice is available, fish consumption from those sources should be limited to 6 ounces per week in pregnant women and 1-3 ounces for young children. The recommendation reiterates that pregnant women and young children should avoid eating raw fish.
The agencies noted that they are issuing this draft guidance because recent reports "show many pregnant women in the United States are not consuming fish recommended" by 2010 United States Department of Agriculture guidelines. The agencies added that there is "longstanding evidence of the nutritional value of fish in the diet. Fish contain high-quality protein, many vitamins and minerals, omega-3 fatty acid, and are mostly low in saturated fat, and some fish even contain vitamin D. The nutritional value of fish is especially important during growth and development before birth, in early infancy for breastfed infants, and in childhood."
Citing its own analysis of seafood consumption data from more than 1,000 pregnant women in the United States, the FDA noted that 21% ate no fish in the previous month and those who ate fish consumed far less than recommended in USDA guidelines, with 50% eating fewer than 2 ounces per week and 75% eating fewer than 4 ounces per week.
This draft guidance would replace similar recommendations issued by the FDA/EPA in March 2004, with a recommendation of simply up to 12 ounces of a variety of fish per week (two average meals), avoiding the same four identified types of fish because of their high mercury content. Previous guidance did not set a recommended lower limit of consumption.
The agencies will begin accepting comments on new guidance June 11.
The Food and Drug Administration and the Environmental Protection Agency are encouraging pregnant women, as well as women who may become pregnant or are breastfeeding, and young children to eat more fish, setting for the first time a recommended lower limit of fish consumption to promote health.
In draft guidance released June 10, the agencies are calling for women to consume 8-12 ounces of a variety of fish that are lower in mercury; that amount works out to an average of two to three servings per week. Among the types of fish highlighted that are lower in mercury are salmon, shrimp, pollock, tuna (light canned), tilapia, catfish, and cod.
The U.S. Department of Agriculture suggests an amount of 3-5 ounces per week for children under the age of 6 and 4-6 ounces per week for children aged 6-8, the agencies said in an accompanying question-and-answer set. Appropriate amounts of fish for older children would increase up to the adult recommendation. Children should not be given fish until they are at least 6 months of age.
The agencies recommend four types of fish to avoid because of mercury content: tilefish from the Gulf of Mexico, shark, swordfish, and king mackerel. They also recommend limiting white (albacore) tuna to 6 ounces per week for adults and even less for children.
In addition, the agency is advising that those eating fish caught in local waters should listen for local advisories regarding those fish and, if no advice is available, fish consumption from those sources should be limited to 6 ounces per week in pregnant women and 1-3 ounces for young children. The recommendation reiterates that pregnant women and young children should avoid eating raw fish.
The agencies noted that they are issuing this draft guidance because recent reports "show many pregnant women in the United States are not consuming fish recommended" by 2010 United States Department of Agriculture guidelines. The agencies added that there is "longstanding evidence of the nutritional value of fish in the diet. Fish contain high-quality protein, many vitamins and minerals, omega-3 fatty acid, and are mostly low in saturated fat, and some fish even contain vitamin D. The nutritional value of fish is especially important during growth and development before birth, in early infancy for breastfed infants, and in childhood."
Citing its own analysis of seafood consumption data from more than 1,000 pregnant women in the United States, the FDA noted that 21% ate no fish in the previous month and those who ate fish consumed far less than recommended in USDA guidelines, with 50% eating fewer than 2 ounces per week and 75% eating fewer than 4 ounces per week.
This draft guidance would replace similar recommendations issued by the FDA/EPA in March 2004, with a recommendation of simply up to 12 ounces of a variety of fish per week (two average meals), avoiding the same four identified types of fish because of their high mercury content. Previous guidance did not set a recommended lower limit of consumption.
The agencies will begin accepting comments on new guidance June 11.