User login
ACA exchange plans present reimbursement challenges
Physicians face a number of new hurdles in getting paid for the care they provide to patients covered by the Affordable Care Act’s health care marketplace plans.
Texas physicians are reporting difficulties in getting information on patients’ coverage from exchange plans, as well as a lack of understanding from patients about their coverage and financial responsibilities, according to Dr. Austin King, president of the Texas Medical Association and an otolaryngologist in Abilene.
Without this information, it is difficult to have a clear conversation about what patients will owe out of pocket, Dr. King said, adding that patients have a steep learning curve when it comes to the marketplace plans. "It’s a matter of educating patients as to what to expect from these policies."
Another looming problem: The 90-day "grace period" for plan members who have not paid their premiums. During the first 30 days of the grace period, plans must pay claims, but for the next 60 days, they can withhold payment, and if a policy is canceled because of nonpayment of premiums, plans are not required to pay physicians for claims.
Dr. King noted that in Texas, some plans are refusing to pay claims in that 60-day period. However, the single statewide carrier, a Blue Cross Blue Shield plan, is paying claims during the final 60 days of the grace period, but will seek to recoup payments made to physicians if coverage is canceled because of premium nonpayment.
The severity of this problem is not yet known, Dr. King said, but "it will be interesting to see how this impacts the bottom line," particularly for primary care doctors, who he expects to be more severely impacted than specialists.
Dr. King’s observations mirror the results of a recent survey by the Medical Group Management Association.
More than half (60%) of respondents to an April survey said that they believe that the ACA marketplaces will have a "very unfavorable" or "unfavorable" impact on their practices. Nearly 94% have seen patients with marketplace coverage.
Half of respondents said that payment rates offered by the marketplace plans are either "much lower" or "somewhat lower" than those offered by traditional commercial contracts. A little less than half (46%) said the rates are "much lower" or "somewhat lower" than other traditional products offered by the same payer.
The majority of respondents reported having a "somewhat more difficult" or "much more difficult" experience with marketplace plans in verifying patient eligibility (63%), obtaining cost-sharing information (62%), and obtaining provider network information to facilitate referrals (57%).
It is that difficulty in obtaining information that is driving the dissatisfaction in dealing with ACA marketplace plans, said Anders Gilberg, senior vice president of government affairs at MGMA. He added that practices are hiring staff just to deal with getting information from exchange plans.
The MGMA survey gleaned responses from 728 medical groups composed of more than 40,000 physicians nationwide.
Physicians face a number of new hurdles in getting paid for the care they provide to patients covered by the Affordable Care Act’s health care marketplace plans.
Texas physicians are reporting difficulties in getting information on patients’ coverage from exchange plans, as well as a lack of understanding from patients about their coverage and financial responsibilities, according to Dr. Austin King, president of the Texas Medical Association and an otolaryngologist in Abilene.
Without this information, it is difficult to have a clear conversation about what patients will owe out of pocket, Dr. King said, adding that patients have a steep learning curve when it comes to the marketplace plans. "It’s a matter of educating patients as to what to expect from these policies."
Another looming problem: The 90-day "grace period" for plan members who have not paid their premiums. During the first 30 days of the grace period, plans must pay claims, but for the next 60 days, they can withhold payment, and if a policy is canceled because of nonpayment of premiums, plans are not required to pay physicians for claims.
Dr. King noted that in Texas, some plans are refusing to pay claims in that 60-day period. However, the single statewide carrier, a Blue Cross Blue Shield plan, is paying claims during the final 60 days of the grace period, but will seek to recoup payments made to physicians if coverage is canceled because of premium nonpayment.
The severity of this problem is not yet known, Dr. King said, but "it will be interesting to see how this impacts the bottom line," particularly for primary care doctors, who he expects to be more severely impacted than specialists.
Dr. King’s observations mirror the results of a recent survey by the Medical Group Management Association.
More than half (60%) of respondents to an April survey said that they believe that the ACA marketplaces will have a "very unfavorable" or "unfavorable" impact on their practices. Nearly 94% have seen patients with marketplace coverage.
Half of respondents said that payment rates offered by the marketplace plans are either "much lower" or "somewhat lower" than those offered by traditional commercial contracts. A little less than half (46%) said the rates are "much lower" or "somewhat lower" than other traditional products offered by the same payer.
The majority of respondents reported having a "somewhat more difficult" or "much more difficult" experience with marketplace plans in verifying patient eligibility (63%), obtaining cost-sharing information (62%), and obtaining provider network information to facilitate referrals (57%).
It is that difficulty in obtaining information that is driving the dissatisfaction in dealing with ACA marketplace plans, said Anders Gilberg, senior vice president of government affairs at MGMA. He added that practices are hiring staff just to deal with getting information from exchange plans.
The MGMA survey gleaned responses from 728 medical groups composed of more than 40,000 physicians nationwide.
Physicians face a number of new hurdles in getting paid for the care they provide to patients covered by the Affordable Care Act’s health care marketplace plans.
Texas physicians are reporting difficulties in getting information on patients’ coverage from exchange plans, as well as a lack of understanding from patients about their coverage and financial responsibilities, according to Dr. Austin King, president of the Texas Medical Association and an otolaryngologist in Abilene.
Without this information, it is difficult to have a clear conversation about what patients will owe out of pocket, Dr. King said, adding that patients have a steep learning curve when it comes to the marketplace plans. "It’s a matter of educating patients as to what to expect from these policies."
Another looming problem: The 90-day "grace period" for plan members who have not paid their premiums. During the first 30 days of the grace period, plans must pay claims, but for the next 60 days, they can withhold payment, and if a policy is canceled because of nonpayment of premiums, plans are not required to pay physicians for claims.
Dr. King noted that in Texas, some plans are refusing to pay claims in that 60-day period. However, the single statewide carrier, a Blue Cross Blue Shield plan, is paying claims during the final 60 days of the grace period, but will seek to recoup payments made to physicians if coverage is canceled because of premium nonpayment.
The severity of this problem is not yet known, Dr. King said, but "it will be interesting to see how this impacts the bottom line," particularly for primary care doctors, who he expects to be more severely impacted than specialists.
Dr. King’s observations mirror the results of a recent survey by the Medical Group Management Association.
More than half (60%) of respondents to an April survey said that they believe that the ACA marketplaces will have a "very unfavorable" or "unfavorable" impact on their practices. Nearly 94% have seen patients with marketplace coverage.
Half of respondents said that payment rates offered by the marketplace plans are either "much lower" or "somewhat lower" than those offered by traditional commercial contracts. A little less than half (46%) said the rates are "much lower" or "somewhat lower" than other traditional products offered by the same payer.
The majority of respondents reported having a "somewhat more difficult" or "much more difficult" experience with marketplace plans in verifying patient eligibility (63%), obtaining cost-sharing information (62%), and obtaining provider network information to facilitate referrals (57%).
It is that difficulty in obtaining information that is driving the dissatisfaction in dealing with ACA marketplace plans, said Anders Gilberg, senior vice president of government affairs at MGMA. He added that practices are hiring staff just to deal with getting information from exchange plans.
The MGMA survey gleaned responses from 728 medical groups composed of more than 40,000 physicians nationwide.
Emergency docs worry about low pay under the ACA
Emergency departments are bracing for lower expected payments for the delivery of heath services as a result of the Affordable Care Act, according to a recent survey by the American College of Emergency Physicians.
Just over half (51%) of 1,845 current ACEP members who responded to the survey predicted that payments for emergency care will be reduced as a result of the health care reform bill, 19% expected it to remain the same, 13% forecasted an increase. And 17% were unsure.
The nature of the plans for sale in the ACA’s health care marketplaces is a key factor in the expected decline of payments to hospitals. Dr. Alexander M. Rosenau, ACEP president, noted that bronze-level plans, aimed at people with lower incomes typically come with high deductibles. Those deductibles could reach as high as $6,000, which could make it "difficult for people to actually pay these bills," he said.
The specter of lower payments comes as emergency physicians expect volume to increase. According to the survey, 45% of respondents look for volume to increase either slightly, while 41% expect it to increase greatly.
The expansion of Medicaid under the ACA also could contribute to the expected decline of payments to hospitals, Dr. Rosenau said.
Lower payments to hospitals could lead to additional issues, survey respondents noted. Almost half (42%) expressed concern that their ED would become financially unsustainable if balance billing were disallowed, while 37% forecast longer wait times for patients and 30% said they expected access to care to decline.
Marketing General Inc. conducted the survey on behalf of ACEP.
Emergency departments are bracing for lower expected payments for the delivery of heath services as a result of the Affordable Care Act, according to a recent survey by the American College of Emergency Physicians.
Just over half (51%) of 1,845 current ACEP members who responded to the survey predicted that payments for emergency care will be reduced as a result of the health care reform bill, 19% expected it to remain the same, 13% forecasted an increase. And 17% were unsure.
The nature of the plans for sale in the ACA’s health care marketplaces is a key factor in the expected decline of payments to hospitals. Dr. Alexander M. Rosenau, ACEP president, noted that bronze-level plans, aimed at people with lower incomes typically come with high deductibles. Those deductibles could reach as high as $6,000, which could make it "difficult for people to actually pay these bills," he said.
The specter of lower payments comes as emergency physicians expect volume to increase. According to the survey, 45% of respondents look for volume to increase either slightly, while 41% expect it to increase greatly.
The expansion of Medicaid under the ACA also could contribute to the expected decline of payments to hospitals, Dr. Rosenau said.
Lower payments to hospitals could lead to additional issues, survey respondents noted. Almost half (42%) expressed concern that their ED would become financially unsustainable if balance billing were disallowed, while 37% forecast longer wait times for patients and 30% said they expected access to care to decline.
Marketing General Inc. conducted the survey on behalf of ACEP.
Emergency departments are bracing for lower expected payments for the delivery of heath services as a result of the Affordable Care Act, according to a recent survey by the American College of Emergency Physicians.
Just over half (51%) of 1,845 current ACEP members who responded to the survey predicted that payments for emergency care will be reduced as a result of the health care reform bill, 19% expected it to remain the same, 13% forecasted an increase. And 17% were unsure.
The nature of the plans for sale in the ACA’s health care marketplaces is a key factor in the expected decline of payments to hospitals. Dr. Alexander M. Rosenau, ACEP president, noted that bronze-level plans, aimed at people with lower incomes typically come with high deductibles. Those deductibles could reach as high as $6,000, which could make it "difficult for people to actually pay these bills," he said.
The specter of lower payments comes as emergency physicians expect volume to increase. According to the survey, 45% of respondents look for volume to increase either slightly, while 41% expect it to increase greatly.
The expansion of Medicaid under the ACA also could contribute to the expected decline of payments to hospitals, Dr. Rosenau said.
Lower payments to hospitals could lead to additional issues, survey respondents noted. Almost half (42%) expressed concern that their ED would become financially unsustainable if balance billing were disallowed, while 37% forecast longer wait times for patients and 30% said they expected access to care to decline.
Marketing General Inc. conducted the survey on behalf of ACEP.
Medicare to cover hepatitis C screening
Medicare will cover screening for hepatitis C virus infection in high-risk beneficiaries, including a one-time screening for all beneficiaries born between 1946 and 1964, according to a national coverage decision announced June 2.
High risk is defined in the coverage memo as persons who have "a current or past history of illicit injection drug use; and persons who have a history of receiving a blood transfusion prior to 1992." To be covered, screening must be ordered by the beneficiary’s primary care physician or another practitioner within the primary care setting.
Annual rescreening is also covered for high-risk beneficiaries who continue to use illicit injection drugs, according to the decision memo.
The Centers for Medicare & Medicaid Services proposed the coverage, which follows U.S. Preventive Services Task Force recommendations for screening in March. That proposal followed an overwhelmingly positive response to the agency’s initial consideration of coverage for HCV screening in September 2013.
Treatment options for hepatitis C are expanding, with FDA approving three protease inhibitors in recent years – boceprevir (Victrelis), telaprevir (Incivek), and simeprevir (Olysio) – for treatment of patients with genotype 1 infection. Each of these treatments can be used in combination with pegylated interferon and ribavirin for the treatment of genotype 1 infection.
Last year, FDA approved sofosbuvir (Sovaldi), indicated for infections from genotypes 1, 2, 3, or 4, although access is hindered by its cost: $84,000 for a 12-week course of treatment ($1,000 a pill).
Medicare will cover screening for hepatitis C virus infection in high-risk beneficiaries, including a one-time screening for all beneficiaries born between 1946 and 1964, according to a national coverage decision announced June 2.
High risk is defined in the coverage memo as persons who have "a current or past history of illicit injection drug use; and persons who have a history of receiving a blood transfusion prior to 1992." To be covered, screening must be ordered by the beneficiary’s primary care physician or another practitioner within the primary care setting.
Annual rescreening is also covered for high-risk beneficiaries who continue to use illicit injection drugs, according to the decision memo.
The Centers for Medicare & Medicaid Services proposed the coverage, which follows U.S. Preventive Services Task Force recommendations for screening in March. That proposal followed an overwhelmingly positive response to the agency’s initial consideration of coverage for HCV screening in September 2013.
Treatment options for hepatitis C are expanding, with FDA approving three protease inhibitors in recent years – boceprevir (Victrelis), telaprevir (Incivek), and simeprevir (Olysio) – for treatment of patients with genotype 1 infection. Each of these treatments can be used in combination with pegylated interferon and ribavirin for the treatment of genotype 1 infection.
Last year, FDA approved sofosbuvir (Sovaldi), indicated for infections from genotypes 1, 2, 3, or 4, although access is hindered by its cost: $84,000 for a 12-week course of treatment ($1,000 a pill).
Medicare will cover screening for hepatitis C virus infection in high-risk beneficiaries, including a one-time screening for all beneficiaries born between 1946 and 1964, according to a national coverage decision announced June 2.
High risk is defined in the coverage memo as persons who have "a current or past history of illicit injection drug use; and persons who have a history of receiving a blood transfusion prior to 1992." To be covered, screening must be ordered by the beneficiary’s primary care physician or another practitioner within the primary care setting.
Annual rescreening is also covered for high-risk beneficiaries who continue to use illicit injection drugs, according to the decision memo.
The Centers for Medicare & Medicaid Services proposed the coverage, which follows U.S. Preventive Services Task Force recommendations for screening in March. That proposal followed an overwhelmingly positive response to the agency’s initial consideration of coverage for HCV screening in September 2013.
Treatment options for hepatitis C are expanding, with FDA approving three protease inhibitors in recent years – boceprevir (Victrelis), telaprevir (Incivek), and simeprevir (Olysio) – for treatment of patients with genotype 1 infection. Each of these treatments can be used in combination with pegylated interferon and ribavirin for the treatment of genotype 1 infection.
Last year, FDA approved sofosbuvir (Sovaldi), indicated for infections from genotypes 1, 2, 3, or 4, although access is hindered by its cost: $84,000 for a 12-week course of treatment ($1,000 a pill).
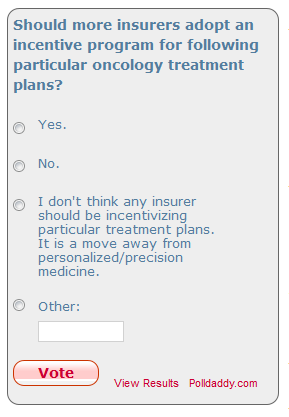
WellPoint incentivizes certain cancer treatment pathways with reimbursement bonuses
WellPoint Inc. is offering a reimbursement incentive to oncologists who follow treatment regimens that follow specific "pathways" identified by the insurer.
The program, announced May 28, will provide oncologists with $350 in additional reimbursement for the initial treatment in one of three cancer categories – breast cancer, colorectal cancer, and non–small-cell lung cancer – that follow the pathway established by WellPoint. Providers registered into the program will get an additional $350/month for following treatments identified in the pathway.
It is being rolled out first in Indiana, Kentucky, Missouri, Ohio, Wisconsin, and Georgia and will expand to other states throughout the balance of the year and into 2015 and covers fully insured and self-insured members, Medicare Advantage members and national account members who live in states in which the program has launched.
Dr. Jennifer Malin, medical director for oncology at WellPoint, notes that the program is not meant to be one that drives oncologists to specific treatments and that providers can deviate from the pathways if that is what is considered the best treatment option for their patients without any penalty to normal reimbursement terms of the member’s health plan.
However, WellPoint is expecting that the pathways will be followed. According to a document outlining the pathways – 24 for breast cancer, 16 for colorectal cancer, and 22 for lung cancer – pathways "are not available for every patient medical condition but are intended to be applicable for 80%-90% of patients. ... Given the complexity of cancer and all of the unique individual circumstances, it would not be possible to have a pathway for every specific situation. The treating oncologist will determine if, in his/her medical opinion, a pathway treatment is the best option or whether, given his or her unique circumstance, another treatment regimen will be a better treatment for him or her."
The document said the pathways are developed "using a rigorous process of evidence-based medicine," and are based on clinical benefit, safety/side effects, especially those that lead to hospitalizations and impact quality of life, strength of national guideline recommendations, and cost of the treatments. They differ from clinical practice guidelines "in that the objective of a pathway is to identify a subset of regimens supported by clinical evidence and practice guidelines with the goal of further reducing unwarranted variation in care and cost."
Dr. Malin, who also continues her clinical practice by volunteering at the Veterans Affairs Greater Los Angeles Healthcare System, says the program will not interfere with the trend toward personalized medicine.
"Pathways are tailored to the evolving science of genomically targeted therapies," she said. "In addition, multiple regimens are included to provide options for oncologists to personalize therapy to their individual patient."
For example, there are six pathway options for first and subsequent lines of therapy for treating metastatic breast cancer in HER2-negative patients. In fact, most pathways offer at least two options, with the exception of colorectal cancer patients with metastatic disease and KRAS mutations on third or subsequent lines of therapy (only treatment with regorafenib is eligible for the reimbursement bonus) and first-line treatment of metastatic non–small-cell lung cancer that is ALK positive (crizotinib).
WellPoint says it will review identified pathways at least quarterly, if not more often, to ensure the evidence continues to support inclusion, or if new guidelines or therapies emerge that warrant change or inclusion, and the document asks providers to submit feedback on an ongoing basis.
While the idea of getting additional reimbursement for doing something oncologists already are doing might be appealing, WellPoint’s plan to offer extra reimbursement if specific treatment pathways are followed is giving some a reason to pause.
"I don’t feel comfortable with this," Dr. Benedito A. Carneiro said, noting that the reimbursement bonus could raise a conflict of interest on behalf of the oncologist. He compared it with simply following National Comprehensive Cancer Network guidelines, which offer an evidence-based recommendation without any reimbursement incentive. If the WellPoint pathway that earns the extra reimbursement matches an NCCN guideline, "fine," but where there might be divergent recommendations, there is the potential for issues.
Overall, Dr. Carneiro is not sure how this will enhance the practice of oncology. "I am not completely convinced that will add more to what we already have," referring to the NCCN guidelines.
Dr. Benedito Carneiro is a fellow at the Northwestern Medicine Developmental Therapeutics Institute at Northwestern University, Chicago.
While the idea of getting additional reimbursement for doing something oncologists already are doing might be appealing, WellPoint’s plan to offer extra reimbursement if specific treatment pathways are followed is giving some a reason to pause.
"I don’t feel comfortable with this," Dr. Benedito A. Carneiro said, noting that the reimbursement bonus could raise a conflict of interest on behalf of the oncologist. He compared it with simply following National Comprehensive Cancer Network guidelines, which offer an evidence-based recommendation without any reimbursement incentive. If the WellPoint pathway that earns the extra reimbursement matches an NCCN guideline, "fine," but where there might be divergent recommendations, there is the potential for issues.
Overall, Dr. Carneiro is not sure how this will enhance the practice of oncology. "I am not completely convinced that will add more to what we already have," referring to the NCCN guidelines.
Dr. Benedito Carneiro is a fellow at the Northwestern Medicine Developmental Therapeutics Institute at Northwestern University, Chicago.
While the idea of getting additional reimbursement for doing something oncologists already are doing might be appealing, WellPoint’s plan to offer extra reimbursement if specific treatment pathways are followed is giving some a reason to pause.
"I don’t feel comfortable with this," Dr. Benedito A. Carneiro said, noting that the reimbursement bonus could raise a conflict of interest on behalf of the oncologist. He compared it with simply following National Comprehensive Cancer Network guidelines, which offer an evidence-based recommendation without any reimbursement incentive. If the WellPoint pathway that earns the extra reimbursement matches an NCCN guideline, "fine," but where there might be divergent recommendations, there is the potential for issues.
Overall, Dr. Carneiro is not sure how this will enhance the practice of oncology. "I am not completely convinced that will add more to what we already have," referring to the NCCN guidelines.
Dr. Benedito Carneiro is a fellow at the Northwestern Medicine Developmental Therapeutics Institute at Northwestern University, Chicago.
WellPoint Inc. is offering a reimbursement incentive to oncologists who follow treatment regimens that follow specific "pathways" identified by the insurer.
The program, announced May 28, will provide oncologists with $350 in additional reimbursement for the initial treatment in one of three cancer categories – breast cancer, colorectal cancer, and non–small-cell lung cancer – that follow the pathway established by WellPoint. Providers registered into the program will get an additional $350/month for following treatments identified in the pathway.
It is being rolled out first in Indiana, Kentucky, Missouri, Ohio, Wisconsin, and Georgia and will expand to other states throughout the balance of the year and into 2015 and covers fully insured and self-insured members, Medicare Advantage members and national account members who live in states in which the program has launched.
Dr. Jennifer Malin, medical director for oncology at WellPoint, notes that the program is not meant to be one that drives oncologists to specific treatments and that providers can deviate from the pathways if that is what is considered the best treatment option for their patients without any penalty to normal reimbursement terms of the member’s health plan.
However, WellPoint is expecting that the pathways will be followed. According to a document outlining the pathways – 24 for breast cancer, 16 for colorectal cancer, and 22 for lung cancer – pathways "are not available for every patient medical condition but are intended to be applicable for 80%-90% of patients. ... Given the complexity of cancer and all of the unique individual circumstances, it would not be possible to have a pathway for every specific situation. The treating oncologist will determine if, in his/her medical opinion, a pathway treatment is the best option or whether, given his or her unique circumstance, another treatment regimen will be a better treatment for him or her."
The document said the pathways are developed "using a rigorous process of evidence-based medicine," and are based on clinical benefit, safety/side effects, especially those that lead to hospitalizations and impact quality of life, strength of national guideline recommendations, and cost of the treatments. They differ from clinical practice guidelines "in that the objective of a pathway is to identify a subset of regimens supported by clinical evidence and practice guidelines with the goal of further reducing unwarranted variation in care and cost."
Dr. Malin, who also continues her clinical practice by volunteering at the Veterans Affairs Greater Los Angeles Healthcare System, says the program will not interfere with the trend toward personalized medicine.
"Pathways are tailored to the evolving science of genomically targeted therapies," she said. "In addition, multiple regimens are included to provide options for oncologists to personalize therapy to their individual patient."
For example, there are six pathway options for first and subsequent lines of therapy for treating metastatic breast cancer in HER2-negative patients. In fact, most pathways offer at least two options, with the exception of colorectal cancer patients with metastatic disease and KRAS mutations on third or subsequent lines of therapy (only treatment with regorafenib is eligible for the reimbursement bonus) and first-line treatment of metastatic non–small-cell lung cancer that is ALK positive (crizotinib).
WellPoint says it will review identified pathways at least quarterly, if not more often, to ensure the evidence continues to support inclusion, or if new guidelines or therapies emerge that warrant change or inclusion, and the document asks providers to submit feedback on an ongoing basis.
WellPoint Inc. is offering a reimbursement incentive to oncologists who follow treatment regimens that follow specific "pathways" identified by the insurer.
The program, announced May 28, will provide oncologists with $350 in additional reimbursement for the initial treatment in one of three cancer categories – breast cancer, colorectal cancer, and non–small-cell lung cancer – that follow the pathway established by WellPoint. Providers registered into the program will get an additional $350/month for following treatments identified in the pathway.
It is being rolled out first in Indiana, Kentucky, Missouri, Ohio, Wisconsin, and Georgia and will expand to other states throughout the balance of the year and into 2015 and covers fully insured and self-insured members, Medicare Advantage members and national account members who live in states in which the program has launched.
Dr. Jennifer Malin, medical director for oncology at WellPoint, notes that the program is not meant to be one that drives oncologists to specific treatments and that providers can deviate from the pathways if that is what is considered the best treatment option for their patients without any penalty to normal reimbursement terms of the member’s health plan.
However, WellPoint is expecting that the pathways will be followed. According to a document outlining the pathways – 24 for breast cancer, 16 for colorectal cancer, and 22 for lung cancer – pathways "are not available for every patient medical condition but are intended to be applicable for 80%-90% of patients. ... Given the complexity of cancer and all of the unique individual circumstances, it would not be possible to have a pathway for every specific situation. The treating oncologist will determine if, in his/her medical opinion, a pathway treatment is the best option or whether, given his or her unique circumstance, another treatment regimen will be a better treatment for him or her."
The document said the pathways are developed "using a rigorous process of evidence-based medicine," and are based on clinical benefit, safety/side effects, especially those that lead to hospitalizations and impact quality of life, strength of national guideline recommendations, and cost of the treatments. They differ from clinical practice guidelines "in that the objective of a pathway is to identify a subset of regimens supported by clinical evidence and practice guidelines with the goal of further reducing unwarranted variation in care and cost."
Dr. Malin, who also continues her clinical practice by volunteering at the Veterans Affairs Greater Los Angeles Healthcare System, says the program will not interfere with the trend toward personalized medicine.
"Pathways are tailored to the evolving science of genomically targeted therapies," she said. "In addition, multiple regimens are included to provide options for oncologists to personalize therapy to their individual patient."
For example, there are six pathway options for first and subsequent lines of therapy for treating metastatic breast cancer in HER2-negative patients. In fact, most pathways offer at least two options, with the exception of colorectal cancer patients with metastatic disease and KRAS mutations on third or subsequent lines of therapy (only treatment with regorafenib is eligible for the reimbursement bonus) and first-line treatment of metastatic non–small-cell lung cancer that is ALK positive (crizotinib).
WellPoint says it will review identified pathways at least quarterly, if not more often, to ensure the evidence continues to support inclusion, or if new guidelines or therapies emerge that warrant change or inclusion, and the document asks providers to submit feedback on an ongoing basis.
Childhood cancer survivors: Less frequent heart screening may be more cost effective
Less frequent cardiac screening may be just as effective for monitoring risk in survivors of childhood cancer, according to two analyses of the Childhood Cancer Survivor Study and other data.
F. Lennie Wong, Ph.D., of City of Hope National Medical Center in Duarte, Calif., and colleagues looked at the simulated life histories of 10 million childhood cancer survivors from 5 years after cancer diagnosis until death for each risk profile described in the Children’s Oncology Group (COG) long-term follow-up guidelines. Their findings were published May 19 in the Annals of Internal Medicine.
Survivors included children with cancer diagnosed and treated between ages 0 and 20 years, and the simulated population mirrored the Childhood Cancer Survivor Study cohort in terms of sex, age at cancer diagnosis, chest irradiation, and cumulative anthracycline dose (Ann. Intern. Med. 2014;160:672-83).
Lifetime costs and health outcomes (expected life-years, quality adjusted life years, and cumulative incidence of heart failure at 20, 30, and 50 years after cancer diagnosis) achieved by each COG screening schedule based on risk profile, compared with no screening and an incremental cost-effectiveness ratio was calculated for the schedule recommended for each profile.
The base-case analyses examined screening frequencies recommended by the COG guidelines, which researchers found might not be optimal.
"Our results indicate that the costliest – but most effective – strategy was annual screening (incremental cost-effectiveness ratio between $43,100 and $368, 400), and the least expensive was screening every 5 years (between $18,300 and $138,200)," the researchers noted. "Given these observations, we identified the most cost-effective screening frequencies costing less than $100,000 per QALY by reducing annual screening to every 2-4 years depending on risk profile, and biennial screening was reduced to every 5 years."
Reduced frequency screening maintained 80% of the health benefits of the COG guidelines at nearly half the cost, relative to no screening, they noted. Life expectancy was increased 4.9 months (vs. 6.1 months), QALY gain was 0.11 (vs. 0.13), and the reduction in heart failure risk at 30 years after diagnosis was 14.3% (vs. 17.5%).
"When compared with the overall less frequent screening strategy, the COG guidelines had an overall [incremental cost-effectiveness ratio] of $185,300," the investigators said.
In a separate study also published May 19 in the Annals of Internal Medicine, Dr. Jennifer Yeh of Harvard School of Public Health and her associates also examined a cohort of patients who at age 15 years had survived cancer for 5 years (age 10 at diagnosis). All were at risk for asymptomatic left ventricular dysfunction based on treatment with anthracyclines and chest radiation.
They found that cardiac assessment every 10 years had a incremental cost-effectiveness ratio of $111,600 per quality adjusted life year (QALY) gained, compared with no assessment. Assessment every 5 years had an incremental cost-effectiveness ration of $117,900 per QALY gained (Ann. Intern. Med. 2014;160:661-71).
"Incremental cost-effectiveness ratios for more frequent assessments exceeded $165,000 per QALY. [Ratios] for all assessment strategies exceeded $196,000 per QALY gained for the subgroup that received no anthracycline," the researchers noted. "Current recommendations for cardiac assessment may reduce systolic [heart failure] incidence, but less frequent screening than currently recommended may be preferred and possible revision of current recommendations is warranted."
The studies were funded by the National Cancer Institute and the Lance Armstrong Foundation. Dr. Wong and Dr. Yeh reported no relevant conflicts of interest.
While two separate analyses of the Children’s Oncology Group guidelines for screening for asymptomatic left ventricular dysfunction may have room to be adjusted for less frequency to make them more cost-effective, the guidelines as they currently stand need not be discounted, according to Dr. Richard M. Steingart, Dr. Jennifer E. Liu, and Dr. Kevin C. Oeffinger, all of Memorial Sloan Kettering Cancer Center in New York.
While the analyses showed more cost-effective screening algorithms, the guidelines are "relatively cost-effective from a societal perspective."
"Clinician and patient should be assured that screening for [asymptomatic left ventricular dysfunction] is a valuable undertaking and that state-of-the-art cost-effectiveness analyses allow for variations in their choices based on the details of the clinical presentation, patient preference, and local imaging expertise," the doctors noted.
Dr. Richard M. Steingart, Dr. Jennifer E. Liu, and Dr. Kevin C. Oeffinger are all at Memorial Sloan Kettering Cancer Center in New York. Their comments are taken from an editorial accompanying the studies by Dr. Wong and Dr. Yeh (Ann. Intern. Med. 2014;160:731-2).
While two separate analyses of the Children’s Oncology Group guidelines for screening for asymptomatic left ventricular dysfunction may have room to be adjusted for less frequency to make them more cost-effective, the guidelines as they currently stand need not be discounted, according to Dr. Richard M. Steingart, Dr. Jennifer E. Liu, and Dr. Kevin C. Oeffinger, all of Memorial Sloan Kettering Cancer Center in New York.
While the analyses showed more cost-effective screening algorithms, the guidelines are "relatively cost-effective from a societal perspective."
"Clinician and patient should be assured that screening for [asymptomatic left ventricular dysfunction] is a valuable undertaking and that state-of-the-art cost-effectiveness analyses allow for variations in their choices based on the details of the clinical presentation, patient preference, and local imaging expertise," the doctors noted.
Dr. Richard M. Steingart, Dr. Jennifer E. Liu, and Dr. Kevin C. Oeffinger are all at Memorial Sloan Kettering Cancer Center in New York. Their comments are taken from an editorial accompanying the studies by Dr. Wong and Dr. Yeh (Ann. Intern. Med. 2014;160:731-2).
While two separate analyses of the Children’s Oncology Group guidelines for screening for asymptomatic left ventricular dysfunction may have room to be adjusted for less frequency to make them more cost-effective, the guidelines as they currently stand need not be discounted, according to Dr. Richard M. Steingart, Dr. Jennifer E. Liu, and Dr. Kevin C. Oeffinger, all of Memorial Sloan Kettering Cancer Center in New York.
While the analyses showed more cost-effective screening algorithms, the guidelines are "relatively cost-effective from a societal perspective."
"Clinician and patient should be assured that screening for [asymptomatic left ventricular dysfunction] is a valuable undertaking and that state-of-the-art cost-effectiveness analyses allow for variations in their choices based on the details of the clinical presentation, patient preference, and local imaging expertise," the doctors noted.
Dr. Richard M. Steingart, Dr. Jennifer E. Liu, and Dr. Kevin C. Oeffinger are all at Memorial Sloan Kettering Cancer Center in New York. Their comments are taken from an editorial accompanying the studies by Dr. Wong and Dr. Yeh (Ann. Intern. Med. 2014;160:731-2).
Less frequent cardiac screening may be just as effective for monitoring risk in survivors of childhood cancer, according to two analyses of the Childhood Cancer Survivor Study and other data.
F. Lennie Wong, Ph.D., of City of Hope National Medical Center in Duarte, Calif., and colleagues looked at the simulated life histories of 10 million childhood cancer survivors from 5 years after cancer diagnosis until death for each risk profile described in the Children’s Oncology Group (COG) long-term follow-up guidelines. Their findings were published May 19 in the Annals of Internal Medicine.
Survivors included children with cancer diagnosed and treated between ages 0 and 20 years, and the simulated population mirrored the Childhood Cancer Survivor Study cohort in terms of sex, age at cancer diagnosis, chest irradiation, and cumulative anthracycline dose (Ann. Intern. Med. 2014;160:672-83).
Lifetime costs and health outcomes (expected life-years, quality adjusted life years, and cumulative incidence of heart failure at 20, 30, and 50 years after cancer diagnosis) achieved by each COG screening schedule based on risk profile, compared with no screening and an incremental cost-effectiveness ratio was calculated for the schedule recommended for each profile.
The base-case analyses examined screening frequencies recommended by the COG guidelines, which researchers found might not be optimal.
"Our results indicate that the costliest – but most effective – strategy was annual screening (incremental cost-effectiveness ratio between $43,100 and $368, 400), and the least expensive was screening every 5 years (between $18,300 and $138,200)," the researchers noted. "Given these observations, we identified the most cost-effective screening frequencies costing less than $100,000 per QALY by reducing annual screening to every 2-4 years depending on risk profile, and biennial screening was reduced to every 5 years."
Reduced frequency screening maintained 80% of the health benefits of the COG guidelines at nearly half the cost, relative to no screening, they noted. Life expectancy was increased 4.9 months (vs. 6.1 months), QALY gain was 0.11 (vs. 0.13), and the reduction in heart failure risk at 30 years after diagnosis was 14.3% (vs. 17.5%).
"When compared with the overall less frequent screening strategy, the COG guidelines had an overall [incremental cost-effectiveness ratio] of $185,300," the investigators said.
In a separate study also published May 19 in the Annals of Internal Medicine, Dr. Jennifer Yeh of Harvard School of Public Health and her associates also examined a cohort of patients who at age 15 years had survived cancer for 5 years (age 10 at diagnosis). All were at risk for asymptomatic left ventricular dysfunction based on treatment with anthracyclines and chest radiation.
They found that cardiac assessment every 10 years had a incremental cost-effectiveness ratio of $111,600 per quality adjusted life year (QALY) gained, compared with no assessment. Assessment every 5 years had an incremental cost-effectiveness ration of $117,900 per QALY gained (Ann. Intern. Med. 2014;160:661-71).
"Incremental cost-effectiveness ratios for more frequent assessments exceeded $165,000 per QALY. [Ratios] for all assessment strategies exceeded $196,000 per QALY gained for the subgroup that received no anthracycline," the researchers noted. "Current recommendations for cardiac assessment may reduce systolic [heart failure] incidence, but less frequent screening than currently recommended may be preferred and possible revision of current recommendations is warranted."
The studies were funded by the National Cancer Institute and the Lance Armstrong Foundation. Dr. Wong and Dr. Yeh reported no relevant conflicts of interest.
Less frequent cardiac screening may be just as effective for monitoring risk in survivors of childhood cancer, according to two analyses of the Childhood Cancer Survivor Study and other data.
F. Lennie Wong, Ph.D., of City of Hope National Medical Center in Duarte, Calif., and colleagues looked at the simulated life histories of 10 million childhood cancer survivors from 5 years after cancer diagnosis until death for each risk profile described in the Children’s Oncology Group (COG) long-term follow-up guidelines. Their findings were published May 19 in the Annals of Internal Medicine.
Survivors included children with cancer diagnosed and treated between ages 0 and 20 years, and the simulated population mirrored the Childhood Cancer Survivor Study cohort in terms of sex, age at cancer diagnosis, chest irradiation, and cumulative anthracycline dose (Ann. Intern. Med. 2014;160:672-83).
Lifetime costs and health outcomes (expected life-years, quality adjusted life years, and cumulative incidence of heart failure at 20, 30, and 50 years after cancer diagnosis) achieved by each COG screening schedule based on risk profile, compared with no screening and an incremental cost-effectiveness ratio was calculated for the schedule recommended for each profile.
The base-case analyses examined screening frequencies recommended by the COG guidelines, which researchers found might not be optimal.
"Our results indicate that the costliest – but most effective – strategy was annual screening (incremental cost-effectiveness ratio between $43,100 and $368, 400), and the least expensive was screening every 5 years (between $18,300 and $138,200)," the researchers noted. "Given these observations, we identified the most cost-effective screening frequencies costing less than $100,000 per QALY by reducing annual screening to every 2-4 years depending on risk profile, and biennial screening was reduced to every 5 years."
Reduced frequency screening maintained 80% of the health benefits of the COG guidelines at nearly half the cost, relative to no screening, they noted. Life expectancy was increased 4.9 months (vs. 6.1 months), QALY gain was 0.11 (vs. 0.13), and the reduction in heart failure risk at 30 years after diagnosis was 14.3% (vs. 17.5%).
"When compared with the overall less frequent screening strategy, the COG guidelines had an overall [incremental cost-effectiveness ratio] of $185,300," the investigators said.
In a separate study also published May 19 in the Annals of Internal Medicine, Dr. Jennifer Yeh of Harvard School of Public Health and her associates also examined a cohort of patients who at age 15 years had survived cancer for 5 years (age 10 at diagnosis). All were at risk for asymptomatic left ventricular dysfunction based on treatment with anthracyclines and chest radiation.
They found that cardiac assessment every 10 years had a incremental cost-effectiveness ratio of $111,600 per quality adjusted life year (QALY) gained, compared with no assessment. Assessment every 5 years had an incremental cost-effectiveness ration of $117,900 per QALY gained (Ann. Intern. Med. 2014;160:661-71).
"Incremental cost-effectiveness ratios for more frequent assessments exceeded $165,000 per QALY. [Ratios] for all assessment strategies exceeded $196,000 per QALY gained for the subgroup that received no anthracycline," the researchers noted. "Current recommendations for cardiac assessment may reduce systolic [heart failure] incidence, but less frequent screening than currently recommended may be preferred and possible revision of current recommendations is warranted."
The studies were funded by the National Cancer Institute and the Lance Armstrong Foundation. Dr. Wong and Dr. Yeh reported no relevant conflicts of interest.
FROM THE ANNALS OF INTERNAL MEDICINE
Key clinical point Consider lengthening cardiac screening intervals for childhood cancer survivors.
Major finding: The most cost-effective screening frequencies costing less than $100,000 per QALY were 2-4 years (vs. 1 year) and 5 years (vs. every other year), depending on risk profile.
Data source: Analysis of the Childhood Cancer Survivor Study and other data.
Disclosures: The studies were funded by the National Cancer Institute and the Lance Armstrong Foundation. Dr. Wong and Dr. Yeh reported no relevant conflicts of interest.
Evidence Called Insufficient For Comparing PsA Drugs
Gregory Twachtman is a writer for “The Pink Sheet.” This news organization and “The Pink Sheet” are owned by Elsevier.
A comparative effectiveness study on drug therapies used to treat psoriatic arthritis in adults determined that evidence is insufficient to draw any conclusions.
“Overall, the data are quite limited and the evidence is insufficient to draw firm conclusions on comparative efficacy, effectiveness, and harms of either oral or biologic DMARDs [disease-modifying antirheumatic drugs] in this condition,” the draft report stated. AHRQ uploaded the draft report to the Effective Care portion of its Web site. The draft did not identify the lead investigators of the study.
AHRQ's findings come soon after the U.K.'s National Institute for Clinical Excellence rejected Simponi for the treatment of active and progressive psoriatic arthritis (PsA) in adults, claiming that evidence revealed that the Schering Plough/Johnson & Johnson product was not as effective as Pfizer's Enbrel.
The draft report noted that about 520,000 U.S. adults have PsA, with treatments aimed primarily at controlling pain and inflammation and, ultimately, at slowing or arresting the progression of joint destruction.
The study compared a variety of oral and biologic DMARDs, including Simponi (golimumab) and Enbrel (etanercept), as well as Sanofi-Synthelabo's Plaquenil (hydroxychloroquine), Sanofi-Aventis' Arava (leflunomide), methotrexate, sulfasalazine, Abbott's Humira (adalimumab), UCB's Cimzia (certolizumab) and J&J's Remicade (infliximab). Humira, Enbrel, Simponi, and Remicade are approved by FDA to be used in patients with PsA.
The comparative effectiveness study for PsA aimed to answer four key questions:
▸ Do drug therapies differ in their ability to reduce disease activity, to slow or limit progression of radiographic joint damage, or to maintain remission?
▸ Do drug therapies differ in their ability to improve patient-reported symptoms, functional capacity, or quality of life?
▸ Do drug therapies differ in harms, tolerability, adherence, or adverse effects?
▸ What are the comparative benefits and harms of drug therapies for PsA in subgroups of patients based on stage of disease, history of prior therapy, demographics, concomitant therapies, or comorbidities?
The limited evidence that surfaced during research addressed the first three questions but nothing could be found on the fourth.
The draft report noted that experts “have not arrived at consensus about the comparative effectiveness of corticosteroids, oral DMARDs, and biologic DMARDs for treating PsA. More importantly, it is unclear how the effectiveness and safety of different types of combination therapy compare. In addition, there is debate about how early in the disease process combination therapy should be initiated and whether patients will respond to a biologic agent if they have previously failed a different biologic agent.”
The draft report added that questions remain about the risks of these agents. There is also limited understanding of the benefits and risks regarding subpopulations, including ethnic minorities, the elderly, pregnant women, and patients with other comorbidities.
Gregory Twachtman is a writer for “The Pink Sheet.” This news organization and “The Pink Sheet” are owned by Elsevier.
A comparative effectiveness study on drug therapies used to treat psoriatic arthritis in adults determined that evidence is insufficient to draw any conclusions.
“Overall, the data are quite limited and the evidence is insufficient to draw firm conclusions on comparative efficacy, effectiveness, and harms of either oral or biologic DMARDs [disease-modifying antirheumatic drugs] in this condition,” the draft report stated. AHRQ uploaded the draft report to the Effective Care portion of its Web site. The draft did not identify the lead investigators of the study.
AHRQ's findings come soon after the U.K.'s National Institute for Clinical Excellence rejected Simponi for the treatment of active and progressive psoriatic arthritis (PsA) in adults, claiming that evidence revealed that the Schering Plough/Johnson & Johnson product was not as effective as Pfizer's Enbrel.
The draft report noted that about 520,000 U.S. adults have PsA, with treatments aimed primarily at controlling pain and inflammation and, ultimately, at slowing or arresting the progression of joint destruction.
The study compared a variety of oral and biologic DMARDs, including Simponi (golimumab) and Enbrel (etanercept), as well as Sanofi-Synthelabo's Plaquenil (hydroxychloroquine), Sanofi-Aventis' Arava (leflunomide), methotrexate, sulfasalazine, Abbott's Humira (adalimumab), UCB's Cimzia (certolizumab) and J&J's Remicade (infliximab). Humira, Enbrel, Simponi, and Remicade are approved by FDA to be used in patients with PsA.
The comparative effectiveness study for PsA aimed to answer four key questions:
▸ Do drug therapies differ in their ability to reduce disease activity, to slow or limit progression of radiographic joint damage, or to maintain remission?
▸ Do drug therapies differ in their ability to improve patient-reported symptoms, functional capacity, or quality of life?
▸ Do drug therapies differ in harms, tolerability, adherence, or adverse effects?
▸ What are the comparative benefits and harms of drug therapies for PsA in subgroups of patients based on stage of disease, history of prior therapy, demographics, concomitant therapies, or comorbidities?
The limited evidence that surfaced during research addressed the first three questions but nothing could be found on the fourth.
The draft report noted that experts “have not arrived at consensus about the comparative effectiveness of corticosteroids, oral DMARDs, and biologic DMARDs for treating PsA. More importantly, it is unclear how the effectiveness and safety of different types of combination therapy compare. In addition, there is debate about how early in the disease process combination therapy should be initiated and whether patients will respond to a biologic agent if they have previously failed a different biologic agent.”
The draft report added that questions remain about the risks of these agents. There is also limited understanding of the benefits and risks regarding subpopulations, including ethnic minorities, the elderly, pregnant women, and patients with other comorbidities.
Gregory Twachtman is a writer for “The Pink Sheet.” This news organization and “The Pink Sheet” are owned by Elsevier.
A comparative effectiveness study on drug therapies used to treat psoriatic arthritis in adults determined that evidence is insufficient to draw any conclusions.
“Overall, the data are quite limited and the evidence is insufficient to draw firm conclusions on comparative efficacy, effectiveness, and harms of either oral or biologic DMARDs [disease-modifying antirheumatic drugs] in this condition,” the draft report stated. AHRQ uploaded the draft report to the Effective Care portion of its Web site. The draft did not identify the lead investigators of the study.
AHRQ's findings come soon after the U.K.'s National Institute for Clinical Excellence rejected Simponi for the treatment of active and progressive psoriatic arthritis (PsA) in adults, claiming that evidence revealed that the Schering Plough/Johnson & Johnson product was not as effective as Pfizer's Enbrel.
The draft report noted that about 520,000 U.S. adults have PsA, with treatments aimed primarily at controlling pain and inflammation and, ultimately, at slowing or arresting the progression of joint destruction.
The study compared a variety of oral and biologic DMARDs, including Simponi (golimumab) and Enbrel (etanercept), as well as Sanofi-Synthelabo's Plaquenil (hydroxychloroquine), Sanofi-Aventis' Arava (leflunomide), methotrexate, sulfasalazine, Abbott's Humira (adalimumab), UCB's Cimzia (certolizumab) and J&J's Remicade (infliximab). Humira, Enbrel, Simponi, and Remicade are approved by FDA to be used in patients with PsA.
The comparative effectiveness study for PsA aimed to answer four key questions:
▸ Do drug therapies differ in their ability to reduce disease activity, to slow or limit progression of radiographic joint damage, or to maintain remission?
▸ Do drug therapies differ in their ability to improve patient-reported symptoms, functional capacity, or quality of life?
▸ Do drug therapies differ in harms, tolerability, adherence, or adverse effects?
▸ What are the comparative benefits and harms of drug therapies for PsA in subgroups of patients based on stage of disease, history of prior therapy, demographics, concomitant therapies, or comorbidities?
The limited evidence that surfaced during research addressed the first three questions but nothing could be found on the fourth.
The draft report noted that experts “have not arrived at consensus about the comparative effectiveness of corticosteroids, oral DMARDs, and biologic DMARDs for treating PsA. More importantly, it is unclear how the effectiveness and safety of different types of combination therapy compare. In addition, there is debate about how early in the disease process combination therapy should be initiated and whether patients will respond to a biologic agent if they have previously failed a different biologic agent.”
The draft report added that questions remain about the risks of these agents. There is also limited understanding of the benefits and risks regarding subpopulations, including ethnic minorities, the elderly, pregnant women, and patients with other comorbidities.
AHRQ: Evidence Insufficient to Compare Psoriatic Arthritis Drugs
A comparative effectiveness study on drug therapies used to treat psoriatic arthritis in adults determined that evidence is insufficient to draw any conclusions.
"Overall, the data are quite limited and the evidence is insufficient to draw firm conclusions on comparative efficacy, effectiveness, and harms of either oral or biologic DMARDs [disease-modifying antirheumatic drugs] in this condition," the draft report stated. AHRQ uploaded the draft report Dec. 21 to the Effective Care portion of its Web site. Comments on the report are due by Jan. 19. http://www.effectivehealthcare.ahrq.gov/index.cfm/research-available-for-comment/comment-draft-reports/?pageaction=displaydraftcommentform&topicid=203&productid=598&documenttype=draftReport The draft did not identify the lead investigators of the study.
AHRQ's findings come soon after the U.K.'s National Institute for Clinical Excellence rejected Simponi for the treatment of active and progressive psoriatic arthritis in adults, claiming that evidence revealed that the Schering Plough/Johnson & Johnson product was not as effective as Pfizer’s Enbrel. http://www.skinandallergynews.com/index.php?id=372&cHash=071010&tx_ttnews[tt_news]=17519
The draft report noted that about 520,000 adults in the U.S. have psoriatic arthritis, with treatments aimed primarily at controlling pain and inflammation and, ultimately, at slowing or arresting the progression of joint destruction.
The study compared a variety of oral and biologic DMARDs, including Simponi (golimumab) and Enbrel (etanercept), as well as Sanofi-Synthelabo's Plaquenil (hydroxychloroquine), Sanofi-Aventis' Arava (leflunomide), methotrexate, sulfasalazine, Abbott's Humira (adalimumab), UCB's Cimzia (certolizumab) and J&J's Remicade (infliximab). Humira, Enbrel, Simponi and Remicade are approved by FDA to be used in patients with PsA.
Key Questions
The comparative effectiveness study aimed to answer four key questions:
For patients with PsA, do drug therapies differ in their ability to reduce disease activity, to slow or limit progression of radiographic joint damage, or to maintain remission?
For patients with PsA, do drug therapies differ in their ability to improve patient reported symptoms, functional capacity or quality of life?
For patients with PsA, do drug therapies differ in harms, tolerability, adherence or adverse effects?
What are the comparative benefits and harms of drug therapies for PsA in subgroups of patients based on stage of disease, history of prior therapy, demographics, concomitant therapies or comorbidities?
The limited evidence that surfaced during research addressed the first three questions but nothing could be found on the fourth.
No Clinical Consensus
The draft report noted that experts "have not arrived at consensus about the comparative effectiveness of corticosteroids, oral DMARDs, and biologic DMARDs for treating PsA. More importantly, it is unclear how the effectiveness and safety of different types of combination therapy compare – e.g. oral DMARDs with corticosteroids, oral DMARDs with biologic DMARDs, triple combination of corticosteroids, oral DMARDs and biologic DMARDs. In addition, there is debate about how early in the disease process combination therapy should be initiated and whether patients will respond to a biologic agent if they have previously failed a different biologic agent."
The draft report added that questions remain about the risks of these agents. There is also limited understanding of the benefits and risks regarding subpopulations, including ethnic minorities, the elderly, pregnant women, and patients with other comorbidities.
Contributing to the issue is the lack of trial evidence. "In patients with PsA, historically, few trials have been conducted with only minimal research before biologic agents were introduced; management options tended to be adopted from rheumatoid arthritis (RA) trial evidence," the draft report stated.
Starting from a base of 3,487 citations, researchers included 19 published articles reporting on 12 studies, including no head-to-head randomized controlled trials, no head-to-head nonrandomized controlled trials, 9 placebo-controlled trials, 2 meta-analyses or systematic reviews, and 1 observational study.
Report authors called for more comparative research to be done "to help clinicians and researchers arrive at stronger conclusions on the comparative efficacy, effectiveness, quality of life, and harms of medications for PsA," with a specific call for head-to-head randomized controlled trials to build the knowledge base.
Gregory Twachtman is a writer for "The Pink Sheet." This news organization and "The Pink Sheet" are owned by Elsevier.
A comparative effectiveness study on drug therapies used to treat psoriatic arthritis in adults determined that evidence is insufficient to draw any conclusions.
"Overall, the data are quite limited and the evidence is insufficient to draw firm conclusions on comparative efficacy, effectiveness, and harms of either oral or biologic DMARDs [disease-modifying antirheumatic drugs] in this condition," the draft report stated. AHRQ uploaded the draft report Dec. 21 to the Effective Care portion of its Web site. Comments on the report are due by Jan. 19. http://www.effectivehealthcare.ahrq.gov/index.cfm/research-available-for-comment/comment-draft-reports/?pageaction=displaydraftcommentform&topicid=203&productid=598&documenttype=draftReport The draft did not identify the lead investigators of the study.
AHRQ's findings come soon after the U.K.'s National Institute for Clinical Excellence rejected Simponi for the treatment of active and progressive psoriatic arthritis in adults, claiming that evidence revealed that the Schering Plough/Johnson & Johnson product was not as effective as Pfizer’s Enbrel. http://www.skinandallergynews.com/index.php?id=372&cHash=071010&tx_ttnews[tt_news]=17519
The draft report noted that about 520,000 adults in the U.S. have psoriatic arthritis, with treatments aimed primarily at controlling pain and inflammation and, ultimately, at slowing or arresting the progression of joint destruction.
The study compared a variety of oral and biologic DMARDs, including Simponi (golimumab) and Enbrel (etanercept), as well as Sanofi-Synthelabo's Plaquenil (hydroxychloroquine), Sanofi-Aventis' Arava (leflunomide), methotrexate, sulfasalazine, Abbott's Humira (adalimumab), UCB's Cimzia (certolizumab) and J&J's Remicade (infliximab). Humira, Enbrel, Simponi and Remicade are approved by FDA to be used in patients with PsA.
Key Questions
The comparative effectiveness study aimed to answer four key questions:
For patients with PsA, do drug therapies differ in their ability to reduce disease activity, to slow or limit progression of radiographic joint damage, or to maintain remission?
For patients with PsA, do drug therapies differ in their ability to improve patient reported symptoms, functional capacity or quality of life?
For patients with PsA, do drug therapies differ in harms, tolerability, adherence or adverse effects?
What are the comparative benefits and harms of drug therapies for PsA in subgroups of patients based on stage of disease, history of prior therapy, demographics, concomitant therapies or comorbidities?
The limited evidence that surfaced during research addressed the first three questions but nothing could be found on the fourth.
No Clinical Consensus
The draft report noted that experts "have not arrived at consensus about the comparative effectiveness of corticosteroids, oral DMARDs, and biologic DMARDs for treating PsA. More importantly, it is unclear how the effectiveness and safety of different types of combination therapy compare – e.g. oral DMARDs with corticosteroids, oral DMARDs with biologic DMARDs, triple combination of corticosteroids, oral DMARDs and biologic DMARDs. In addition, there is debate about how early in the disease process combination therapy should be initiated and whether patients will respond to a biologic agent if they have previously failed a different biologic agent."
The draft report added that questions remain about the risks of these agents. There is also limited understanding of the benefits and risks regarding subpopulations, including ethnic minorities, the elderly, pregnant women, and patients with other comorbidities.
Contributing to the issue is the lack of trial evidence. "In patients with PsA, historically, few trials have been conducted with only minimal research before biologic agents were introduced; management options tended to be adopted from rheumatoid arthritis (RA) trial evidence," the draft report stated.
Starting from a base of 3,487 citations, researchers included 19 published articles reporting on 12 studies, including no head-to-head randomized controlled trials, no head-to-head nonrandomized controlled trials, 9 placebo-controlled trials, 2 meta-analyses or systematic reviews, and 1 observational study.
Report authors called for more comparative research to be done "to help clinicians and researchers arrive at stronger conclusions on the comparative efficacy, effectiveness, quality of life, and harms of medications for PsA," with a specific call for head-to-head randomized controlled trials to build the knowledge base.
Gregory Twachtman is a writer for "The Pink Sheet." This news organization and "The Pink Sheet" are owned by Elsevier.
A comparative effectiveness study on drug therapies used to treat psoriatic arthritis in adults determined that evidence is insufficient to draw any conclusions.
"Overall, the data are quite limited and the evidence is insufficient to draw firm conclusions on comparative efficacy, effectiveness, and harms of either oral or biologic DMARDs [disease-modifying antirheumatic drugs] in this condition," the draft report stated. AHRQ uploaded the draft report Dec. 21 to the Effective Care portion of its Web site. Comments on the report are due by Jan. 19. http://www.effectivehealthcare.ahrq.gov/index.cfm/research-available-for-comment/comment-draft-reports/?pageaction=displaydraftcommentform&topicid=203&productid=598&documenttype=draftReport The draft did not identify the lead investigators of the study.
AHRQ's findings come soon after the U.K.'s National Institute for Clinical Excellence rejected Simponi for the treatment of active and progressive psoriatic arthritis in adults, claiming that evidence revealed that the Schering Plough/Johnson & Johnson product was not as effective as Pfizer’s Enbrel. http://www.skinandallergynews.com/index.php?id=372&cHash=071010&tx_ttnews[tt_news]=17519
The draft report noted that about 520,000 adults in the U.S. have psoriatic arthritis, with treatments aimed primarily at controlling pain and inflammation and, ultimately, at slowing or arresting the progression of joint destruction.
The study compared a variety of oral and biologic DMARDs, including Simponi (golimumab) and Enbrel (etanercept), as well as Sanofi-Synthelabo's Plaquenil (hydroxychloroquine), Sanofi-Aventis' Arava (leflunomide), methotrexate, sulfasalazine, Abbott's Humira (adalimumab), UCB's Cimzia (certolizumab) and J&J's Remicade (infliximab). Humira, Enbrel, Simponi and Remicade are approved by FDA to be used in patients with PsA.
Key Questions
The comparative effectiveness study aimed to answer four key questions:
For patients with PsA, do drug therapies differ in their ability to reduce disease activity, to slow or limit progression of radiographic joint damage, or to maintain remission?
For patients with PsA, do drug therapies differ in their ability to improve patient reported symptoms, functional capacity or quality of life?
For patients with PsA, do drug therapies differ in harms, tolerability, adherence or adverse effects?
What are the comparative benefits and harms of drug therapies for PsA in subgroups of patients based on stage of disease, history of prior therapy, demographics, concomitant therapies or comorbidities?
The limited evidence that surfaced during research addressed the first three questions but nothing could be found on the fourth.
No Clinical Consensus
The draft report noted that experts "have not arrived at consensus about the comparative effectiveness of corticosteroids, oral DMARDs, and biologic DMARDs for treating PsA. More importantly, it is unclear how the effectiveness and safety of different types of combination therapy compare – e.g. oral DMARDs with corticosteroids, oral DMARDs with biologic DMARDs, triple combination of corticosteroids, oral DMARDs and biologic DMARDs. In addition, there is debate about how early in the disease process combination therapy should be initiated and whether patients will respond to a biologic agent if they have previously failed a different biologic agent."
The draft report added that questions remain about the risks of these agents. There is also limited understanding of the benefits and risks regarding subpopulations, including ethnic minorities, the elderly, pregnant women, and patients with other comorbidities.
Contributing to the issue is the lack of trial evidence. "In patients with PsA, historically, few trials have been conducted with only minimal research before biologic agents were introduced; management options tended to be adopted from rheumatoid arthritis (RA) trial evidence," the draft report stated.
Starting from a base of 3,487 citations, researchers included 19 published articles reporting on 12 studies, including no head-to-head randomized controlled trials, no head-to-head nonrandomized controlled trials, 9 placebo-controlled trials, 2 meta-analyses or systematic reviews, and 1 observational study.
Report authors called for more comparative research to be done "to help clinicians and researchers arrive at stronger conclusions on the comparative efficacy, effectiveness, quality of life, and harms of medications for PsA," with a specific call for head-to-head randomized controlled trials to build the knowledge base.
Gregory Twachtman is a writer for "The Pink Sheet." This news organization and "The Pink Sheet" are owned by Elsevier.
FROM THE AGENCY FOR HEALTHCARE RESEARCH AND QUALITY
Study: Oral Drugs Beat Inhaled Ones for Controlling Asthma
The WellPoint health plan has lifted prior authorization requirements on oral asthma medications based on a comparative effectiveness analysis of claims data for oral and inhaled asthma medications.
Despite inhaled drugs' clinical superiority in controlled trials, the study, conducted by HealthCore (WellPoint's health outcomes research subsidiary), revealed that users of oral asthma controllers appeared to have better clinical outcomes than did the inhaled corticosteroid (ICS) group, as indicated by less use of short-acting beta-agonists and a smaller risk of inpatient and emergency department visits, according to the study authors.
The study came about, according to WellPoint's National Pharmacy and Therapeutics Committee, when it found that oral asthma medications were being used as front-line therapy, a use that either wasn't part of the drug's approved indication or didn't follow the National Heart, Lung, and Blood Institute's asthma treatment guidelines.
WellPoint said it was hearing anecdotal evidence that members did not like inhaled treatments or were struggling to take them, prompting the insurer to find out “which therapy was best for members in the real world and align our formulary appropriately.”
For the study, HealthCore examined the medical and pharmacy claims of more than 55,000 patients from eight health plans who had used at least one of six types of asthma controller medications between 2003 and 2005.
The data were integrated with quality of life surveys of more than 800 asthma patients from the same plans to evaluate potential differences in quality of life between the types of controller medication. The oral medications that patients in the study were using were the leukotriene modifiers zafirlukast (Accolate), montelukast (Singulair), and zileuton (Zyflo).
Lead author Hiangkiat Tan and colleagues suggested that the reason for the better outcomes among the oral medication users compared with the ICS users comes down to real-world usage patterns.
“This conflict could be due to the observation that the patients in this study were less adherent to an inhaled controller medication (inhaled cortico-steroid, long-acting beta-agonist) regimen than to an oral controller medication regimen,” the authors suggested. “This observation concurred with the findings of other studies, which indicated that adherence was poor for inhaled medications, both in general and in comparison with oral medications” (Mayo Clin. Proc. 2009;84:675-84).
“Only 3% of patients in the ICS monotherapy group were considered adherent, a finding that underlines the urgent need for a better understanding of the barriers to patient acceptance of the most proven and effective therapy,” the researchers added. “When ICS adherence cannot be achieved, our findings indicate that a [leukotriene modifier] may be a reasonable alternative, although at a higher cost.”
The investigators noted that among patients who adhered to their controller medication regimen, the risk of inpatient or emergency department visits was lower for patients receiving an ICS than for those taking an oral medication.
But the findings underscore a common theme that has surfaced in broader discussions regarding comparative effectiveness research: How an intervention is used in the real-world setting can differ from its use in the clinical trials that are used to determine a drug's safety and efficacy, with different results.
This newspaper and “The Pink Sheet” are published by Elsevier.
The WellPoint health plan has lifted prior authorization requirements on oral asthma medications based on a comparative effectiveness analysis of claims data for oral and inhaled asthma medications.
Despite inhaled drugs' clinical superiority in controlled trials, the study, conducted by HealthCore (WellPoint's health outcomes research subsidiary), revealed that users of oral asthma controllers appeared to have better clinical outcomes than did the inhaled corticosteroid (ICS) group, as indicated by less use of short-acting beta-agonists and a smaller risk of inpatient and emergency department visits, according to the study authors.
The study came about, according to WellPoint's National Pharmacy and Therapeutics Committee, when it found that oral asthma medications were being used as front-line therapy, a use that either wasn't part of the drug's approved indication or didn't follow the National Heart, Lung, and Blood Institute's asthma treatment guidelines.
WellPoint said it was hearing anecdotal evidence that members did not like inhaled treatments or were struggling to take them, prompting the insurer to find out “which therapy was best for members in the real world and align our formulary appropriately.”
For the study, HealthCore examined the medical and pharmacy claims of more than 55,000 patients from eight health plans who had used at least one of six types of asthma controller medications between 2003 and 2005.
The data were integrated with quality of life surveys of more than 800 asthma patients from the same plans to evaluate potential differences in quality of life between the types of controller medication. The oral medications that patients in the study were using were the leukotriene modifiers zafirlukast (Accolate), montelukast (Singulair), and zileuton (Zyflo).
Lead author Hiangkiat Tan and colleagues suggested that the reason for the better outcomes among the oral medication users compared with the ICS users comes down to real-world usage patterns.
“This conflict could be due to the observation that the patients in this study were less adherent to an inhaled controller medication (inhaled cortico-steroid, long-acting beta-agonist) regimen than to an oral controller medication regimen,” the authors suggested. “This observation concurred with the findings of other studies, which indicated that adherence was poor for inhaled medications, both in general and in comparison with oral medications” (Mayo Clin. Proc. 2009;84:675-84).
“Only 3% of patients in the ICS monotherapy group were considered adherent, a finding that underlines the urgent need for a better understanding of the barriers to patient acceptance of the most proven and effective therapy,” the researchers added. “When ICS adherence cannot be achieved, our findings indicate that a [leukotriene modifier] may be a reasonable alternative, although at a higher cost.”
The investigators noted that among patients who adhered to their controller medication regimen, the risk of inpatient or emergency department visits was lower for patients receiving an ICS than for those taking an oral medication.
But the findings underscore a common theme that has surfaced in broader discussions regarding comparative effectiveness research: How an intervention is used in the real-world setting can differ from its use in the clinical trials that are used to determine a drug's safety and efficacy, with different results.
This newspaper and “The Pink Sheet” are published by Elsevier.
The WellPoint health plan has lifted prior authorization requirements on oral asthma medications based on a comparative effectiveness analysis of claims data for oral and inhaled asthma medications.
Despite inhaled drugs' clinical superiority in controlled trials, the study, conducted by HealthCore (WellPoint's health outcomes research subsidiary), revealed that users of oral asthma controllers appeared to have better clinical outcomes than did the inhaled corticosteroid (ICS) group, as indicated by less use of short-acting beta-agonists and a smaller risk of inpatient and emergency department visits, according to the study authors.
The study came about, according to WellPoint's National Pharmacy and Therapeutics Committee, when it found that oral asthma medications were being used as front-line therapy, a use that either wasn't part of the drug's approved indication or didn't follow the National Heart, Lung, and Blood Institute's asthma treatment guidelines.
WellPoint said it was hearing anecdotal evidence that members did not like inhaled treatments or were struggling to take them, prompting the insurer to find out “which therapy was best for members in the real world and align our formulary appropriately.”
For the study, HealthCore examined the medical and pharmacy claims of more than 55,000 patients from eight health plans who had used at least one of six types of asthma controller medications between 2003 and 2005.
The data were integrated with quality of life surveys of more than 800 asthma patients from the same plans to evaluate potential differences in quality of life between the types of controller medication. The oral medications that patients in the study were using were the leukotriene modifiers zafirlukast (Accolate), montelukast (Singulair), and zileuton (Zyflo).
Lead author Hiangkiat Tan and colleagues suggested that the reason for the better outcomes among the oral medication users compared with the ICS users comes down to real-world usage patterns.
“This conflict could be due to the observation that the patients in this study were less adherent to an inhaled controller medication (inhaled cortico-steroid, long-acting beta-agonist) regimen than to an oral controller medication regimen,” the authors suggested. “This observation concurred with the findings of other studies, which indicated that adherence was poor for inhaled medications, both in general and in comparison with oral medications” (Mayo Clin. Proc. 2009;84:675-84).
“Only 3% of patients in the ICS monotherapy group were considered adherent, a finding that underlines the urgent need for a better understanding of the barriers to patient acceptance of the most proven and effective therapy,” the researchers added. “When ICS adherence cannot be achieved, our findings indicate that a [leukotriene modifier] may be a reasonable alternative, although at a higher cost.”
The investigators noted that among patients who adhered to their controller medication regimen, the risk of inpatient or emergency department visits was lower for patients receiving an ICS than for those taking an oral medication.
But the findings underscore a common theme that has surfaced in broader discussions regarding comparative effectiveness research: How an intervention is used in the real-world setting can differ from its use in the clinical trials that are used to determine a drug's safety and efficacy, with different results.
This newspaper and “The Pink Sheet” are published by Elsevier.