User login
Same-day antiretroviral treatment increased viral suppression in HIV patients
Patients who received antiretroviral treatment (ART) on the day they underwent HIV testing were more likely to continue treatment and have a lower mortality rate, a study conducted in Port-au-Prince, Haiti, showed.
According to the World Health Organization, ART treatment is essential in stopping the spread of HIV; however, one-quarter to one-third of patients do not continue the treatment process after starting ART, the investigators reported.
Starting ART treatment the same day as HIV testing showed the potential to reduce this problem. “Our findings suggest that ART initiation as soon as possible after HIV testing may be beneficial for clinically stable patients,” wrote Serena Koenig, MD, of the department of infectious diseases at Brigham and Women’s Hospital, Boston, and her coinvestigators. “In resource-poor settings with fragile delivery systems, such as Haiti, the provision of immediate support by care providers at the time of HIV diagnosis can have both structural and individual impact.”
In a randomized, controlled study of 703 patients, 277 of 347 same-day ART patients (80%) retained care, and 10 (3%) died, compared with 256 of 356 patients (72%) in the standard care group, 20 (6%) of whom died (PLoS Med. 2017 Jul 25. doi: 10.1371/journal.pmed.1002357).
Retention of care was defined as attending one clinic visit between 12 months and 15 months after testing, the investigators reported.
The median age of participating patients was 37 years; the median CD4 count was 247 cells/mm3 in the standard care group and 249 cells/mm3 in the same-day group.
At the end of the study, the adjusted mortality risk among patients in the same-day ART group was less than half that of the standard care group (risk ratio, 0.43; P = .033).
Care retention might be related to a more positive mindset among those who start ART immediately after diagnosis, the investigators said.
“Making treatment initiation logistically easier for patients, we believe that same-day counseling and ART initiation increase the sense of hope, optimism, and overall connectedness to the health care system for patients, which have been shown to be important for retention,” Dr. Koenig and her colleagues wrote.
The findings update the 2016 World Health Organization standard guidelines for ART treatment, which report that there is not enough information to recommend same-day treatment. The study was limited by the single-center patient population. Patients also had lower than usual CD4 counts, which may have exaggerated successful results.
The National Institute of Allergy and Infectious Diseases funded the study. The investigators reported they had no relevant financial disclosures.
[email protected]On Twitter @eaztweets
Patients who received antiretroviral treatment (ART) on the day they underwent HIV testing were more likely to continue treatment and have a lower mortality rate, a study conducted in Port-au-Prince, Haiti, showed.
According to the World Health Organization, ART treatment is essential in stopping the spread of HIV; however, one-quarter to one-third of patients do not continue the treatment process after starting ART, the investigators reported.
Starting ART treatment the same day as HIV testing showed the potential to reduce this problem. “Our findings suggest that ART initiation as soon as possible after HIV testing may be beneficial for clinically stable patients,” wrote Serena Koenig, MD, of the department of infectious diseases at Brigham and Women’s Hospital, Boston, and her coinvestigators. “In resource-poor settings with fragile delivery systems, such as Haiti, the provision of immediate support by care providers at the time of HIV diagnosis can have both structural and individual impact.”
In a randomized, controlled study of 703 patients, 277 of 347 same-day ART patients (80%) retained care, and 10 (3%) died, compared with 256 of 356 patients (72%) in the standard care group, 20 (6%) of whom died (PLoS Med. 2017 Jul 25. doi: 10.1371/journal.pmed.1002357).
Retention of care was defined as attending one clinic visit between 12 months and 15 months after testing, the investigators reported.
The median age of participating patients was 37 years; the median CD4 count was 247 cells/mm3 in the standard care group and 249 cells/mm3 in the same-day group.
At the end of the study, the adjusted mortality risk among patients in the same-day ART group was less than half that of the standard care group (risk ratio, 0.43; P = .033).
Care retention might be related to a more positive mindset among those who start ART immediately after diagnosis, the investigators said.
“Making treatment initiation logistically easier for patients, we believe that same-day counseling and ART initiation increase the sense of hope, optimism, and overall connectedness to the health care system for patients, which have been shown to be important for retention,” Dr. Koenig and her colleagues wrote.
The findings update the 2016 World Health Organization standard guidelines for ART treatment, which report that there is not enough information to recommend same-day treatment. The study was limited by the single-center patient population. Patients also had lower than usual CD4 counts, which may have exaggerated successful results.
The National Institute of Allergy and Infectious Diseases funded the study. The investigators reported they had no relevant financial disclosures.
[email protected]On Twitter @eaztweets
Patients who received antiretroviral treatment (ART) on the day they underwent HIV testing were more likely to continue treatment and have a lower mortality rate, a study conducted in Port-au-Prince, Haiti, showed.
According to the World Health Organization, ART treatment is essential in stopping the spread of HIV; however, one-quarter to one-third of patients do not continue the treatment process after starting ART, the investigators reported.
Starting ART treatment the same day as HIV testing showed the potential to reduce this problem. “Our findings suggest that ART initiation as soon as possible after HIV testing may be beneficial for clinically stable patients,” wrote Serena Koenig, MD, of the department of infectious diseases at Brigham and Women’s Hospital, Boston, and her coinvestigators. “In resource-poor settings with fragile delivery systems, such as Haiti, the provision of immediate support by care providers at the time of HIV diagnosis can have both structural and individual impact.”
In a randomized, controlled study of 703 patients, 277 of 347 same-day ART patients (80%) retained care, and 10 (3%) died, compared with 256 of 356 patients (72%) in the standard care group, 20 (6%) of whom died (PLoS Med. 2017 Jul 25. doi: 10.1371/journal.pmed.1002357).
Retention of care was defined as attending one clinic visit between 12 months and 15 months after testing, the investigators reported.
The median age of participating patients was 37 years; the median CD4 count was 247 cells/mm3 in the standard care group and 249 cells/mm3 in the same-day group.
At the end of the study, the adjusted mortality risk among patients in the same-day ART group was less than half that of the standard care group (risk ratio, 0.43; P = .033).
Care retention might be related to a more positive mindset among those who start ART immediately after diagnosis, the investigators said.
“Making treatment initiation logistically easier for patients, we believe that same-day counseling and ART initiation increase the sense of hope, optimism, and overall connectedness to the health care system for patients, which have been shown to be important for retention,” Dr. Koenig and her colleagues wrote.
The findings update the 2016 World Health Organization standard guidelines for ART treatment, which report that there is not enough information to recommend same-day treatment. The study was limited by the single-center patient population. Patients also had lower than usual CD4 counts, which may have exaggerated successful results.
The National Institute of Allergy and Infectious Diseases funded the study. The investigators reported they had no relevant financial disclosures.
[email protected]On Twitter @eaztweets
FROM PLOS MEDICINE
Key clinical point:
Major finding: Of 347 same-day ART patients, 277 (80%) retained care, and 10 (3%) died, compared with 256 (72%) and 20 (6%) in the standard treatment group.
Data source: An unblinded, randomized controlled study of 703 HIV patients from the Haitian Study Group for the Study of Kaposi’s Sarcoma and Opportunistic Infections between August 2013 and October 2015.
Disclosures: The National Institute of Allergy and Infectious Diseases sponsored the study. The investigators reported they had no relevant financial disclosures.
VIDEO: Further CTE correlation found in deceased American football players
Evidence of a correlation between chronic traumatic encephalopathy (CTE) and playing American football was strengthened in the largest retrospective study cohort to date.
The progressive neurodegenerative disease associated with recurrent head trauma has been linked to football over the past decade. However, this new study took steps to solidify the connection by studying 202 deceased brains, more than double the size of a previous 2013 report.
First author Jesse Mez, MD, of Boston University, and his colleagues examined the brains donated to a brain bank jointly run by the VA Boston Healthcare System, Boston University, and the Concussion Legacy Foundation. They correlated their findings with interviews and questionnaires filled out in 2014 by those close to the donors (JAMA. 2017 Jul 25. doi: 10.1001/jama.2017.8334).
The donors were male, and a majority (79%) were white. The average age at death was 67 years. In the mild cases, there was an average of 13 years of play; in severe cases, the average was 15.8 years.
The researchers found evidence of CTE in 177 (88%) of the 202 brains of football players, with cases found in 3 (21%) who played only in high school, 48 (91%) who played in college, 9 (64%) semiprofessional players, 7 (88%) Canadian Football League players, and 110 (99%) NFL players, according to investigators.
“Nearly all of the former NFL players in this study had CTE pathology, and this pathology was frequently severe,” noted Dr. Mez and his coinvestigators. ”These findings suggest that CTE may be related to prior participation in football and that a high level of play may be related to substantial disease burden.”
Severity of CTE positively correlated with longer playing history and more competitive levels of play. According to the investigators, severe cases of CTE were found in none of the high school players, 27 college players (56%), 5 semiprofessional players (56%), 6 Canadian professional players (86%), and 95 NFL players (86%).
All participants with CTE commonly displayed certain symptoms regardless of severity level.
Impulsiveness occurred in 23 mild cases (89%) and 65 severe cases (80%). Depression was seen in 18 mild cases (67%) and 46 severe cases (56%). A total of 13 players (50%) with mild symptoms showed apathy, compared with 43 with severe symptoms (52%). Anxiety was reported for 14 mild cases (52%) and 41 severe cases (50%). Cognitive symptoms such as problems with memory and attention were also common at both levels of severity, with 19 cases (73%) and 18 cases (69%), respectively, among donors with mild CTE, and 76 (92%) and 67 (81%) among donors with severe CTE.
Those interviewed who were close to the donors also reported other behavior or mood symptoms that the investigators inferred to be related to CTE.
“Many of these participants had a substance use disorder, demonstrated suicidality, or had a family history of psychiatric illness,” the investigators wrote. “Behavior or mood symptoms may be the initial presentation for a subset of individuals with CTE, or alternatively, CTE [phosphorylated tau] pathology may lower the threshold for psychiatric manifestations in susceptible individuals.”
The investigators asserted that the correlation of CTE diagnosis and severity may be more nuanced than just how many times a player is hit.
“Several other football-related factors may influence CTE risk and disease severity, including but not limited to age at first exposure to football, duration of play, player position, cumulative hits, and linear and rotational acceleration of hits,” Dr. Mez and his associates wrote. “Recent work in living former football players has shown that age at first exposure may be related to impaired cognitive performance and altered corpus callosum white matter and that cumulative hits may be related to impairment on self-report and objective measures of cognition, mood, and behavior, although it is unclear if any of these outcomes are related to CTE pathology.”
This study was limited by the potential bias of donors who participated in the program. Researchers acknowledge that public awareness of the issue of CTE and head trauma may have influenced players with symptoms to donate their brains, thereby increasing the CTE frequency in the sample.
In addition, the brain bank where the sample was taken is not representative of the entire population of American football players, as most donors played at the college, semi-professional, and professional level, as opposed to only high school or youth leagues.
The senior author of the study, Ann C. McKee, MD, discussed the study further in a related video interview.
The National Institute of Neurological Disorders and Stroke, the National Institute of Aging, the U.S. Department of Defense, the U.S. Department of Veterans Affairs, the National Operating Committee on Standards for Athletic Equipment, the Alzheimer’s Association, the Concussion Legacy Foundation, the Andlinger Family Foundation, the WWE, and the NFL supported the study. Five authors reported receiving support from relevant sources, including the NFL.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @eaztweets
Traumatic brain injuries (TBIs) are a serious health concern that currently affect 10 million people per year worldwide.
While a majority of TBIs are caused by car crashes, contact sports are estimated to cause between 1.6-3.8 million concussions in the United States every year, making the root of this study – to learn more about CTE among those in contact sports – imperative.
This study used the largest CTE cohort to date, but it is important to read the results, which are concerning, within the context of the study.
Results from the informants who filled out the questionnaires – most commonly friends or family of the deceased – showed cognitive symptoms in 88% of donors and behavioral symptoms in 95%, compared with 5% and 20% prevalence, respectively, among a questionnaire-based study filled out by retired National Football League players. This may mean that rates of symptomatic CTE may be lower outside of a selected cohort of former players.
While early-stage CTE was found in some high school players, most individuals do not play football beyond a high school level, and the link between high school football and future neurological decline was not well established in this study.
This study is a good example of the progress that has been made in TBI research, but there are still many fundamental questions that need to be answered. The next step will be improving disease models and expanding the studies of at-risk populations.
It is of the utmost importance that these improvements are made immediately; increasing our knowledge and public awareness of TBIs is paramount.
Gil Rabinovici, MD, is associate professor of neurology at the University of California–San Francisco, and an associate editor for JAMA Neurology. He receives research support from Avid Radiopharmaceuticals, Eli Lilly, GE Healthcare, and Piramal. He has received consulting or speaking honoraria from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche. These comments were taken from an editorial (JAMA 2017 Jul 25. doi: 10.1001/jama.2017.9353 ).
Traumatic brain injuries (TBIs) are a serious health concern that currently affect 10 million people per year worldwide.
While a majority of TBIs are caused by car crashes, contact sports are estimated to cause between 1.6-3.8 million concussions in the United States every year, making the root of this study – to learn more about CTE among those in contact sports – imperative.
This study used the largest CTE cohort to date, but it is important to read the results, which are concerning, within the context of the study.
Results from the informants who filled out the questionnaires – most commonly friends or family of the deceased – showed cognitive symptoms in 88% of donors and behavioral symptoms in 95%, compared with 5% and 20% prevalence, respectively, among a questionnaire-based study filled out by retired National Football League players. This may mean that rates of symptomatic CTE may be lower outside of a selected cohort of former players.
While early-stage CTE was found in some high school players, most individuals do not play football beyond a high school level, and the link between high school football and future neurological decline was not well established in this study.
This study is a good example of the progress that has been made in TBI research, but there are still many fundamental questions that need to be answered. The next step will be improving disease models and expanding the studies of at-risk populations.
It is of the utmost importance that these improvements are made immediately; increasing our knowledge and public awareness of TBIs is paramount.
Gil Rabinovici, MD, is associate professor of neurology at the University of California–San Francisco, and an associate editor for JAMA Neurology. He receives research support from Avid Radiopharmaceuticals, Eli Lilly, GE Healthcare, and Piramal. He has received consulting or speaking honoraria from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche. These comments were taken from an editorial (JAMA 2017 Jul 25. doi: 10.1001/jama.2017.9353 ).
Traumatic brain injuries (TBIs) are a serious health concern that currently affect 10 million people per year worldwide.
While a majority of TBIs are caused by car crashes, contact sports are estimated to cause between 1.6-3.8 million concussions in the United States every year, making the root of this study – to learn more about CTE among those in contact sports – imperative.
This study used the largest CTE cohort to date, but it is important to read the results, which are concerning, within the context of the study.
Results from the informants who filled out the questionnaires – most commonly friends or family of the deceased – showed cognitive symptoms in 88% of donors and behavioral symptoms in 95%, compared with 5% and 20% prevalence, respectively, among a questionnaire-based study filled out by retired National Football League players. This may mean that rates of symptomatic CTE may be lower outside of a selected cohort of former players.
While early-stage CTE was found in some high school players, most individuals do not play football beyond a high school level, and the link between high school football and future neurological decline was not well established in this study.
This study is a good example of the progress that has been made in TBI research, but there are still many fundamental questions that need to be answered. The next step will be improving disease models and expanding the studies of at-risk populations.
It is of the utmost importance that these improvements are made immediately; increasing our knowledge and public awareness of TBIs is paramount.
Gil Rabinovici, MD, is associate professor of neurology at the University of California–San Francisco, and an associate editor for JAMA Neurology. He receives research support from Avid Radiopharmaceuticals, Eli Lilly, GE Healthcare, and Piramal. He has received consulting or speaking honoraria from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche. These comments were taken from an editorial (JAMA 2017 Jul 25. doi: 10.1001/jama.2017.9353 ).
Evidence of a correlation between chronic traumatic encephalopathy (CTE) and playing American football was strengthened in the largest retrospective study cohort to date.
The progressive neurodegenerative disease associated with recurrent head trauma has been linked to football over the past decade. However, this new study took steps to solidify the connection by studying 202 deceased brains, more than double the size of a previous 2013 report.
First author Jesse Mez, MD, of Boston University, and his colleagues examined the brains donated to a brain bank jointly run by the VA Boston Healthcare System, Boston University, and the Concussion Legacy Foundation. They correlated their findings with interviews and questionnaires filled out in 2014 by those close to the donors (JAMA. 2017 Jul 25. doi: 10.1001/jama.2017.8334).
The donors were male, and a majority (79%) were white. The average age at death was 67 years. In the mild cases, there was an average of 13 years of play; in severe cases, the average was 15.8 years.
The researchers found evidence of CTE in 177 (88%) of the 202 brains of football players, with cases found in 3 (21%) who played only in high school, 48 (91%) who played in college, 9 (64%) semiprofessional players, 7 (88%) Canadian Football League players, and 110 (99%) NFL players, according to investigators.
“Nearly all of the former NFL players in this study had CTE pathology, and this pathology was frequently severe,” noted Dr. Mez and his coinvestigators. ”These findings suggest that CTE may be related to prior participation in football and that a high level of play may be related to substantial disease burden.”
Severity of CTE positively correlated with longer playing history and more competitive levels of play. According to the investigators, severe cases of CTE were found in none of the high school players, 27 college players (56%), 5 semiprofessional players (56%), 6 Canadian professional players (86%), and 95 NFL players (86%).
All participants with CTE commonly displayed certain symptoms regardless of severity level.
Impulsiveness occurred in 23 mild cases (89%) and 65 severe cases (80%). Depression was seen in 18 mild cases (67%) and 46 severe cases (56%). A total of 13 players (50%) with mild symptoms showed apathy, compared with 43 with severe symptoms (52%). Anxiety was reported for 14 mild cases (52%) and 41 severe cases (50%). Cognitive symptoms such as problems with memory and attention were also common at both levels of severity, with 19 cases (73%) and 18 cases (69%), respectively, among donors with mild CTE, and 76 (92%) and 67 (81%) among donors with severe CTE.
Those interviewed who were close to the donors also reported other behavior or mood symptoms that the investigators inferred to be related to CTE.
“Many of these participants had a substance use disorder, demonstrated suicidality, or had a family history of psychiatric illness,” the investigators wrote. “Behavior or mood symptoms may be the initial presentation for a subset of individuals with CTE, or alternatively, CTE [phosphorylated tau] pathology may lower the threshold for psychiatric manifestations in susceptible individuals.”
The investigators asserted that the correlation of CTE diagnosis and severity may be more nuanced than just how many times a player is hit.
“Several other football-related factors may influence CTE risk and disease severity, including but not limited to age at first exposure to football, duration of play, player position, cumulative hits, and linear and rotational acceleration of hits,” Dr. Mez and his associates wrote. “Recent work in living former football players has shown that age at first exposure may be related to impaired cognitive performance and altered corpus callosum white matter and that cumulative hits may be related to impairment on self-report and objective measures of cognition, mood, and behavior, although it is unclear if any of these outcomes are related to CTE pathology.”
This study was limited by the potential bias of donors who participated in the program. Researchers acknowledge that public awareness of the issue of CTE and head trauma may have influenced players with symptoms to donate their brains, thereby increasing the CTE frequency in the sample.
In addition, the brain bank where the sample was taken is not representative of the entire population of American football players, as most donors played at the college, semi-professional, and professional level, as opposed to only high school or youth leagues.
The senior author of the study, Ann C. McKee, MD, discussed the study further in a related video interview.
The National Institute of Neurological Disorders and Stroke, the National Institute of Aging, the U.S. Department of Defense, the U.S. Department of Veterans Affairs, the National Operating Committee on Standards for Athletic Equipment, the Alzheimer’s Association, the Concussion Legacy Foundation, the Andlinger Family Foundation, the WWE, and the NFL supported the study. Five authors reported receiving support from relevant sources, including the NFL.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @eaztweets
Evidence of a correlation between chronic traumatic encephalopathy (CTE) and playing American football was strengthened in the largest retrospective study cohort to date.
The progressive neurodegenerative disease associated with recurrent head trauma has been linked to football over the past decade. However, this new study took steps to solidify the connection by studying 202 deceased brains, more than double the size of a previous 2013 report.
First author Jesse Mez, MD, of Boston University, and his colleagues examined the brains donated to a brain bank jointly run by the VA Boston Healthcare System, Boston University, and the Concussion Legacy Foundation. They correlated their findings with interviews and questionnaires filled out in 2014 by those close to the donors (JAMA. 2017 Jul 25. doi: 10.1001/jama.2017.8334).
The donors were male, and a majority (79%) were white. The average age at death was 67 years. In the mild cases, there was an average of 13 years of play; in severe cases, the average was 15.8 years.
The researchers found evidence of CTE in 177 (88%) of the 202 brains of football players, with cases found in 3 (21%) who played only in high school, 48 (91%) who played in college, 9 (64%) semiprofessional players, 7 (88%) Canadian Football League players, and 110 (99%) NFL players, according to investigators.
“Nearly all of the former NFL players in this study had CTE pathology, and this pathology was frequently severe,” noted Dr. Mez and his coinvestigators. ”These findings suggest that CTE may be related to prior participation in football and that a high level of play may be related to substantial disease burden.”
Severity of CTE positively correlated with longer playing history and more competitive levels of play. According to the investigators, severe cases of CTE were found in none of the high school players, 27 college players (56%), 5 semiprofessional players (56%), 6 Canadian professional players (86%), and 95 NFL players (86%).
All participants with CTE commonly displayed certain symptoms regardless of severity level.
Impulsiveness occurred in 23 mild cases (89%) and 65 severe cases (80%). Depression was seen in 18 mild cases (67%) and 46 severe cases (56%). A total of 13 players (50%) with mild symptoms showed apathy, compared with 43 with severe symptoms (52%). Anxiety was reported for 14 mild cases (52%) and 41 severe cases (50%). Cognitive symptoms such as problems with memory and attention were also common at both levels of severity, with 19 cases (73%) and 18 cases (69%), respectively, among donors with mild CTE, and 76 (92%) and 67 (81%) among donors with severe CTE.
Those interviewed who were close to the donors also reported other behavior or mood symptoms that the investigators inferred to be related to CTE.
“Many of these participants had a substance use disorder, demonstrated suicidality, or had a family history of psychiatric illness,” the investigators wrote. “Behavior or mood symptoms may be the initial presentation for a subset of individuals with CTE, or alternatively, CTE [phosphorylated tau] pathology may lower the threshold for psychiatric manifestations in susceptible individuals.”
The investigators asserted that the correlation of CTE diagnosis and severity may be more nuanced than just how many times a player is hit.
“Several other football-related factors may influence CTE risk and disease severity, including but not limited to age at first exposure to football, duration of play, player position, cumulative hits, and linear and rotational acceleration of hits,” Dr. Mez and his associates wrote. “Recent work in living former football players has shown that age at first exposure may be related to impaired cognitive performance and altered corpus callosum white matter and that cumulative hits may be related to impairment on self-report and objective measures of cognition, mood, and behavior, although it is unclear if any of these outcomes are related to CTE pathology.”
This study was limited by the potential bias of donors who participated in the program. Researchers acknowledge that public awareness of the issue of CTE and head trauma may have influenced players with symptoms to donate their brains, thereby increasing the CTE frequency in the sample.
In addition, the brain bank where the sample was taken is not representative of the entire population of American football players, as most donors played at the college, semi-professional, and professional level, as opposed to only high school or youth leagues.
The senior author of the study, Ann C. McKee, MD, discussed the study further in a related video interview.
The National Institute of Neurological Disorders and Stroke, the National Institute of Aging, the U.S. Department of Defense, the U.S. Department of Veterans Affairs, the National Operating Committee on Standards for Athletic Equipment, the Alzheimer’s Association, the Concussion Legacy Foundation, the Andlinger Family Foundation, the WWE, and the NFL supported the study. Five authors reported receiving support from relevant sources, including the NFL.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @eaztweets
FROM JAMA
Key clinical point:
Major finding: Of 202 deceased football players who played at levels ranging from high school to the NFL and who donated their brains, 177 (88%) were diagnosed with CTE.
Data source: A blinded, retrospective study of 202 donated brains, as well as questionnaires and interviews with informants close to the deceased.
Disclosures: The National Institute of Neurological Disorders and Stroke, the National Institute of Aging, U.S. Department of Defense, U.S. Department of Veterans Affairs, the National Operating Committee on Standards for Athletic Equipment, the Alzheimer’s Association, the Concussion Legacy Foundation, the Andlinger Family Foundation, the WWE, and the NFL supported the study. Five authors reported receiving support from relevant sources, including the NFL.
Meta-analysis shows correlation between diabetes and erectile dysfunction
WASHINGTON – More than half of men with type 1 or type 2 diabetes develop erectile dysfunction, making them more than three times as likely to develop ED, compared with healthy men, according to a systematic review of diabetes studies.
Data on the exact prevalence of erectile dysfunction in this population has been lacking until now. More precise figures are available from a meta-analysis of 145 studies taken from international diabetes databases.
In terms of risk, men with diabetes were 3.62 (95% CI, 2.53-5.16; P less than .0001) times more likely to develop ED, compared with healthy controls, according to investigators (Diabet Med. 2017 Jul 18. doi: 10.1111/dme.13403).
“Regarding sexual activity and the psychological impact of erectile dysfunction in men with diabetes mellitus, significant and positive associations have been found between depressive symptoms and erectile dysfunction,” said Youssef Kouidrat, MD, PhD, of the department of psychosis studies, Institute of Psychiatry, King’s College London, and his fellow researchers. “Therefore, early detection of erectile dysfunction is essential to improve the psychological health and men’s quality of life.”
Given ED’s serious effects on patients’ physical and emotional well being, it is essential for physicians to have a better understanding of the root causes of the condition in order to help patients as soon as possible, wrote the investigators.
The studies included in the meta-analysis represented a population of 88.755 men with an average age of 56 years, with dates of the studies ranging from the inception of the databases they were taken from up until November 2016.
A majority of the studies included were conducted in Asia (61), followed by Europe (48), North America (17), Africa (15), and Oceania, South America, and multiple continents (4 in total).
South America reported the highest prevalence of ED (74.6%), while the lowest prevalence reported was among studies in North America (34.5%).
Patients who were assessed using the Sexual Health Inventory for Men (SHIM) score reported a higher ED prevalence (82.2%), as did men above the age of 60 years old (62.2%).
With ED correlated to cardiovascular health and mortality, investigators advise physicians to keep testing in mind when assessing patients’ cardiovascular risk.
This study was limited by incomplete data from studies included, which made it difficult to determine prevalence by certain categories.
Other limitations included the lack of separation between type 1 and type 2 diabetes among many of the studies analyzed, as well as a lack of information from the studies analyzed on other risk factors concerning diabetes-related erectile dysfunction.
Investigators reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
WASHINGTON – More than half of men with type 1 or type 2 diabetes develop erectile dysfunction, making them more than three times as likely to develop ED, compared with healthy men, according to a systematic review of diabetes studies.
Data on the exact prevalence of erectile dysfunction in this population has been lacking until now. More precise figures are available from a meta-analysis of 145 studies taken from international diabetes databases.
In terms of risk, men with diabetes were 3.62 (95% CI, 2.53-5.16; P less than .0001) times more likely to develop ED, compared with healthy controls, according to investigators (Diabet Med. 2017 Jul 18. doi: 10.1111/dme.13403).
“Regarding sexual activity and the psychological impact of erectile dysfunction in men with diabetes mellitus, significant and positive associations have been found between depressive symptoms and erectile dysfunction,” said Youssef Kouidrat, MD, PhD, of the department of psychosis studies, Institute of Psychiatry, King’s College London, and his fellow researchers. “Therefore, early detection of erectile dysfunction is essential to improve the psychological health and men’s quality of life.”
Given ED’s serious effects on patients’ physical and emotional well being, it is essential for physicians to have a better understanding of the root causes of the condition in order to help patients as soon as possible, wrote the investigators.
The studies included in the meta-analysis represented a population of 88.755 men with an average age of 56 years, with dates of the studies ranging from the inception of the databases they were taken from up until November 2016.
A majority of the studies included were conducted in Asia (61), followed by Europe (48), North America (17), Africa (15), and Oceania, South America, and multiple continents (4 in total).
South America reported the highest prevalence of ED (74.6%), while the lowest prevalence reported was among studies in North America (34.5%).
Patients who were assessed using the Sexual Health Inventory for Men (SHIM) score reported a higher ED prevalence (82.2%), as did men above the age of 60 years old (62.2%).
With ED correlated to cardiovascular health and mortality, investigators advise physicians to keep testing in mind when assessing patients’ cardiovascular risk.
This study was limited by incomplete data from studies included, which made it difficult to determine prevalence by certain categories.
Other limitations included the lack of separation between type 1 and type 2 diabetes among many of the studies analyzed, as well as a lack of information from the studies analyzed on other risk factors concerning diabetes-related erectile dysfunction.
Investigators reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
WASHINGTON – More than half of men with type 1 or type 2 diabetes develop erectile dysfunction, making them more than three times as likely to develop ED, compared with healthy men, according to a systematic review of diabetes studies.
Data on the exact prevalence of erectile dysfunction in this population has been lacking until now. More precise figures are available from a meta-analysis of 145 studies taken from international diabetes databases.
In terms of risk, men with diabetes were 3.62 (95% CI, 2.53-5.16; P less than .0001) times more likely to develop ED, compared with healthy controls, according to investigators (Diabet Med. 2017 Jul 18. doi: 10.1111/dme.13403).
“Regarding sexual activity and the psychological impact of erectile dysfunction in men with diabetes mellitus, significant and positive associations have been found between depressive symptoms and erectile dysfunction,” said Youssef Kouidrat, MD, PhD, of the department of psychosis studies, Institute of Psychiatry, King’s College London, and his fellow researchers. “Therefore, early detection of erectile dysfunction is essential to improve the psychological health and men’s quality of life.”
Given ED’s serious effects on patients’ physical and emotional well being, it is essential for physicians to have a better understanding of the root causes of the condition in order to help patients as soon as possible, wrote the investigators.
The studies included in the meta-analysis represented a population of 88.755 men with an average age of 56 years, with dates of the studies ranging from the inception of the databases they were taken from up until November 2016.
A majority of the studies included were conducted in Asia (61), followed by Europe (48), North America (17), Africa (15), and Oceania, South America, and multiple continents (4 in total).
South America reported the highest prevalence of ED (74.6%), while the lowest prevalence reported was among studies in North America (34.5%).
Patients who were assessed using the Sexual Health Inventory for Men (SHIM) score reported a higher ED prevalence (82.2%), as did men above the age of 60 years old (62.2%).
With ED correlated to cardiovascular health and mortality, investigators advise physicians to keep testing in mind when assessing patients’ cardiovascular risk.
This study was limited by incomplete data from studies included, which made it difficult to determine prevalence by certain categories.
Other limitations included the lack of separation between type 1 and type 2 diabetes among many of the studies analyzed, as well as a lack of information from the studies analyzed on other risk factors concerning diabetes-related erectile dysfunction.
Investigators reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
FROM DIABETIC MEDICINE
Key clinical point:
Major finding: Men with diabetes showed an odds ratio of 3.62 (95% CI, 2.53-5.16; P less than .0001) of developing erectile dysfunction, compared with healthy controls.
Data source: An analysis of 145 studies representing 88,577 men from international databases spanning from creation of the database to November 2016.
Disclosures: Investigators report no relevant financial disclosures.
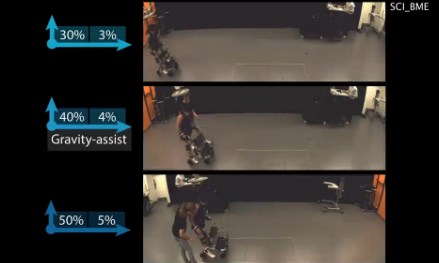
Algorithm-based trunk support system shows potential for recovery of walking ability
A multidirectional gravity-assist device that delivers precise trunk support to stroke and spinal cord injury (SCI) patients via an artificial intelligence algorithm has demonstrated significantly improved locomotor performance beyond treadmill-based systems in a new study.
The harness device used in the study adjusts patients’ balance while they stand still or walk by employing a unique, adaptive multidirectional gravity-assist (MGA) algorithm tailored to the specific needs of the patient, according to Jean-Baptiste Mignardot, PhD, of the Center for Neuroprosthetics and Brain Mind Institute, Swiss Federal Institute of Technology, Lausanne, Switzerland, and fellow investigators.
“The MGA establishes a safe and natural rehabilitation environment wherein individuals with neurological deficits can perform basic and skilled locomotor activities that would not be possible without robotic assistance,” according to the investigators. “The immediate and short-term ameliorations of gait performance during locomotion with MGA illustrate the potential of this environment to augment motor recovery.”
Current gait rehabilitation methods in stroke or SCI patients most commonly involves counterweight mechanisms or force-controlled equipment that apply upward support while walking on a treadmill. However Dr. Mignardot and his colleagues believe these methods are flawed.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Treadmill-restricted environments markedly differ from the rich repertoire of natural locomotor activities underlying daily living,” the investigators wrote. “Vertically restricted trunk support creates undesired forces that impede gait execution.”
To counteract these negative effects, the MGA adjusts both upward and forward forces on the patient’s body, re-creating a more naturally occurring gait posture, which investigators have likened to an inverted pendulum with a natural forward tilt. In order to create the algorithm, investigators ran through a series of procedures, starting with calibrations based on the gait of healthy subjects and adjusting for necessary upward and forward assistance for stroke and SCI patients.
The artificial neural network within the algorithm analyzes patients’ support needs, a job that therapists currently have to do based on visual observations. This opens a window to faster and more accurate estimations, according to the investigators (Sci Transl Med. 2017 Jul 19. doi: 10.1126/scitranslmed.aah3621).
Investigators tested the algorithm on 15 SCI patients and 12 stroke patients. The stroke patients had an average age of 51 years, with length of time after stroke varying from 8 to 235 months. The SCI patients had an average age of 47 years, with a length of time since injury ranging from 12 to 264 months. Most patients in both groups were male.
When tested, the algorithm showed varying success depending on the severity of the injury, according to the researchers.
“For example, the MGA enabled subjects who could not stand independently to walk overground with or without assistive device.” Subjects who were able to move around only with crutches or a walker progressed without the use of assistive devices and exhibited improved spatiotemporal gait features, according to Dr. Mignardot and fellow investigators. “Individuals with stroke exhibited similar or even superior amelioration of locomotor performance and showed that individuals who could only walk with crutches exhibited improved intralimb coordination.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
After initial efficacy tests, the researchers tested the MGA’s effectiveness in five SCI patients immediately after 1 hour of training with the device and found that their gait speed increased during the training. However, the improvements were not evident in a similar test 1 week later. Similar tests using treadmill-restricted step training without the MGA device did not show any improvement during either week of testing.
Although the study’s small sample size limited the conclusions that could be reached, the investigators were encouraged by the overall effects of the algorithm. They noted that further tests are required to test the potential sensitivity and accuracy of the software.
The study was supported by the European Commission’s Seventh Framework Programme, various foundations, and the Swiss National Science Foundation.
Investigators reported holding patents on the step-by-step procedure and use of the MGA algorithm in this study.
[email protected]
On Twitter @eaztweets
A multidirectional gravity-assist device that delivers precise trunk support to stroke and spinal cord injury (SCI) patients via an artificial intelligence algorithm has demonstrated significantly improved locomotor performance beyond treadmill-based systems in a new study.
The harness device used in the study adjusts patients’ balance while they stand still or walk by employing a unique, adaptive multidirectional gravity-assist (MGA) algorithm tailored to the specific needs of the patient, according to Jean-Baptiste Mignardot, PhD, of the Center for Neuroprosthetics and Brain Mind Institute, Swiss Federal Institute of Technology, Lausanne, Switzerland, and fellow investigators.
“The MGA establishes a safe and natural rehabilitation environment wherein individuals with neurological deficits can perform basic and skilled locomotor activities that would not be possible without robotic assistance,” according to the investigators. “The immediate and short-term ameliorations of gait performance during locomotion with MGA illustrate the potential of this environment to augment motor recovery.”
Current gait rehabilitation methods in stroke or SCI patients most commonly involves counterweight mechanisms or force-controlled equipment that apply upward support while walking on a treadmill. However Dr. Mignardot and his colleagues believe these methods are flawed.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Treadmill-restricted environments markedly differ from the rich repertoire of natural locomotor activities underlying daily living,” the investigators wrote. “Vertically restricted trunk support creates undesired forces that impede gait execution.”
To counteract these negative effects, the MGA adjusts both upward and forward forces on the patient’s body, re-creating a more naturally occurring gait posture, which investigators have likened to an inverted pendulum with a natural forward tilt. In order to create the algorithm, investigators ran through a series of procedures, starting with calibrations based on the gait of healthy subjects and adjusting for necessary upward and forward assistance for stroke and SCI patients.
The artificial neural network within the algorithm analyzes patients’ support needs, a job that therapists currently have to do based on visual observations. This opens a window to faster and more accurate estimations, according to the investigators (Sci Transl Med. 2017 Jul 19. doi: 10.1126/scitranslmed.aah3621).
Investigators tested the algorithm on 15 SCI patients and 12 stroke patients. The stroke patients had an average age of 51 years, with length of time after stroke varying from 8 to 235 months. The SCI patients had an average age of 47 years, with a length of time since injury ranging from 12 to 264 months. Most patients in both groups were male.
When tested, the algorithm showed varying success depending on the severity of the injury, according to the researchers.
“For example, the MGA enabled subjects who could not stand independently to walk overground with or without assistive device.” Subjects who were able to move around only with crutches or a walker progressed without the use of assistive devices and exhibited improved spatiotemporal gait features, according to Dr. Mignardot and fellow investigators. “Individuals with stroke exhibited similar or even superior amelioration of locomotor performance and showed that individuals who could only walk with crutches exhibited improved intralimb coordination.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
After initial efficacy tests, the researchers tested the MGA’s effectiveness in five SCI patients immediately after 1 hour of training with the device and found that their gait speed increased during the training. However, the improvements were not evident in a similar test 1 week later. Similar tests using treadmill-restricted step training without the MGA device did not show any improvement during either week of testing.
Although the study’s small sample size limited the conclusions that could be reached, the investigators were encouraged by the overall effects of the algorithm. They noted that further tests are required to test the potential sensitivity and accuracy of the software.
The study was supported by the European Commission’s Seventh Framework Programme, various foundations, and the Swiss National Science Foundation.
Investigators reported holding patents on the step-by-step procedure and use of the MGA algorithm in this study.
[email protected]
On Twitter @eaztweets
A multidirectional gravity-assist device that delivers precise trunk support to stroke and spinal cord injury (SCI) patients via an artificial intelligence algorithm has demonstrated significantly improved locomotor performance beyond treadmill-based systems in a new study.
The harness device used in the study adjusts patients’ balance while they stand still or walk by employing a unique, adaptive multidirectional gravity-assist (MGA) algorithm tailored to the specific needs of the patient, according to Jean-Baptiste Mignardot, PhD, of the Center for Neuroprosthetics and Brain Mind Institute, Swiss Federal Institute of Technology, Lausanne, Switzerland, and fellow investigators.
“The MGA establishes a safe and natural rehabilitation environment wherein individuals with neurological deficits can perform basic and skilled locomotor activities that would not be possible without robotic assistance,” according to the investigators. “The immediate and short-term ameliorations of gait performance during locomotion with MGA illustrate the potential of this environment to augment motor recovery.”
Current gait rehabilitation methods in stroke or SCI patients most commonly involves counterweight mechanisms or force-controlled equipment that apply upward support while walking on a treadmill. However Dr. Mignardot and his colleagues believe these methods are flawed.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Treadmill-restricted environments markedly differ from the rich repertoire of natural locomotor activities underlying daily living,” the investigators wrote. “Vertically restricted trunk support creates undesired forces that impede gait execution.”
To counteract these negative effects, the MGA adjusts both upward and forward forces on the patient’s body, re-creating a more naturally occurring gait posture, which investigators have likened to an inverted pendulum with a natural forward tilt. In order to create the algorithm, investigators ran through a series of procedures, starting with calibrations based on the gait of healthy subjects and adjusting for necessary upward and forward assistance for stroke and SCI patients.
The artificial neural network within the algorithm analyzes patients’ support needs, a job that therapists currently have to do based on visual observations. This opens a window to faster and more accurate estimations, according to the investigators (Sci Transl Med. 2017 Jul 19. doi: 10.1126/scitranslmed.aah3621).
Investigators tested the algorithm on 15 SCI patients and 12 stroke patients. The stroke patients had an average age of 51 years, with length of time after stroke varying from 8 to 235 months. The SCI patients had an average age of 47 years, with a length of time since injury ranging from 12 to 264 months. Most patients in both groups were male.
When tested, the algorithm showed varying success depending on the severity of the injury, according to the researchers.
“For example, the MGA enabled subjects who could not stand independently to walk overground with or without assistive device.” Subjects who were able to move around only with crutches or a walker progressed without the use of assistive devices and exhibited improved spatiotemporal gait features, according to Dr. Mignardot and fellow investigators. “Individuals with stroke exhibited similar or even superior amelioration of locomotor performance and showed that individuals who could only walk with crutches exhibited improved intralimb coordination.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
After initial efficacy tests, the researchers tested the MGA’s effectiveness in five SCI patients immediately after 1 hour of training with the device and found that their gait speed increased during the training. However, the improvements were not evident in a similar test 1 week later. Similar tests using treadmill-restricted step training without the MGA device did not show any improvement during either week of testing.
Although the study’s small sample size limited the conclusions that could be reached, the investigators were encouraged by the overall effects of the algorithm. They noted that further tests are required to test the potential sensitivity and accuracy of the software.
The study was supported by the European Commission’s Seventh Framework Programme, various foundations, and the Swiss National Science Foundation.
Investigators reported holding patents on the step-by-step procedure and use of the MGA algorithm in this study.
[email protected]
On Twitter @eaztweets
FROM SCIENCE TRANSLATIONAL MEDICINE
New C. difficile drug shows promise
Ridinilazole, a new antibiotic for treatment of Clostridium difficile infection (CDI) proved noninferior to vancomycin, showing promise especially in lower recurrence risk, according to a study funded in part by ridinilazole manufacturer Summit Therapeutics.
In a phase 2, 1:1 randomized, double-blind trial of 69 CDI patients, 24 of 36 (66.7%) ridinilazole patients reported a sustained clinical response, compared with 14 of 33 vancomycin patients (42.4%), indicating statistical noninferiority – and even superiority at the upper confidence level – of ridinilazole (Lancet Infect Dis. 2017 Apr 28. doi: 10.1016/S1473-3099[17]30235-9).
Over the course of 10 days, investigators gave the ridinilazole group 200 mg orally twice per day, as well as two placebo doses. Those in the vancomycin group took 125 mg orally four times per day.
Investigators assessed both groups on days 4-6, 10-11, 12-14, and routine weekly follow-ups until 30 days after treatment.
Most of the patients were white females, with an average age of 58 years for the ridinilazole group, and 56 years for the vancomycin group.
Ridinilazole correlated with more sustained clinical responses across almost all subgroups as well, including with treatment differences (respectively) of 42.7%, 15.9%, 19.9%, and 8.9% for those over 75 years, with a more severe diagnosis, more than one previous CDI episode, and those taking other antibiotics before study participation, according to the investigators. Both groups saw similar rates of adverse events related to treatment.
The outcome of this trial could be significant in reducing recurrence risk in CDI patients, which occurs in up to 30% of patients after first treatment, and can increase up to 65% after multiple reinfections, according to Richard Vickers, PhD, chief scientific officer on antimicrobials at Summit Therapeutics PLC, and his fellow investigators.
CDI patients also are subject to significantly higher inpatient mortality, spend longer periods in intensive care, and have higher rates of all-cause readmission over 3 months than do matched controls, the investigators noted.
Unlike the three common CDI drugs on the market, metronidazole, vancomycin, and fidaxomicin, ridinilazole is restricted to the gastrointestinal tract and, according to the investigators, has shown encouraging results in previous studies.
“In vitro studies have shown its high inhibitory activity against C. difficile and minimal activity against both Gram-positive and Gram-negative aerobic and anaerobic intestinal microorganisms,” they wrote. “In a phase 1 study, ridinilazole was safe and well tolerated in healthy human volunteers, with little systemic absorption and little effect on normal gut microbiota.”
They asserted it was this lack of effect that caused the drug to show success in phase 2, noting ridinilazole’s superiority was “likely to be due to the highly selective activity of ridinilazole against CDI and the absence of collateral damage to the microbiota during therapy.”
The study was limited by its sample, which was younger and had a milder form of CDI than is usually represented. The study also formed its power calculations based on the original sample size of 100, and not the adjusted, intended-to-treat population of 69 which became its primary analysis.
Finally, the investigators advised further trials be conducted with a follow-up schedule longer than 30 days.
Dr. Vickers, Dr. Bina Tejura, and Dr. David Roblin reported working for Summit Therapeutics, the drug manufacturer, and hold share options with the company. Other authors reported holding close relationships with other, similar drug manufacturing companies.
[email protected]
On Twitter @eaztweets
With a 30-day mortality margin of 9%-38% and recurrence risk baseline of 15%-25%, Clostridium difficile infection continues to be a significant global problem. Yet, for decades there had only been a minimal number of drugs available to treat this disease, namely metronidazole and vancomycin.
As new resistant strains of this disease phased out metronidazole, even in mild cases, fidaxomicin emerged as an adequate replacement, although it was soon clear that because of its high price, fidaxomicin would remain as an initial treatment, disadvantaging those with multiple episodes.
This lack of reliable, effective antimicrobials puts into sharp relief the need for new drug development, and ridinilazole may be a step in the right direction.
While the study conducted by Richard Vickers and colleagues was limited by a slightly younger sample with a milder form of the disease than a true representative sample, the superior recurrence reduction related to ridinilazole is an advantage.
It is important that we build upon this study, and push further to expand the array of tools we have to fight C. difficile to optimize treatment for patients at all stages of this disease.
Simon D. Goldenberg, MBBS, MSc, FRCPath, MD, DipHIC, is a consultant microbiologist at the Centre for Clinical Infection and Diagnostics Research, King’s College London. He has received grants and personal fees from Astellas, BD, Luminex, Abbott, Orion Diagnostics, Qiagen, MSD, and DNA electronics.
With a 30-day mortality margin of 9%-38% and recurrence risk baseline of 15%-25%, Clostridium difficile infection continues to be a significant global problem. Yet, for decades there had only been a minimal number of drugs available to treat this disease, namely metronidazole and vancomycin.
As new resistant strains of this disease phased out metronidazole, even in mild cases, fidaxomicin emerged as an adequate replacement, although it was soon clear that because of its high price, fidaxomicin would remain as an initial treatment, disadvantaging those with multiple episodes.
This lack of reliable, effective antimicrobials puts into sharp relief the need for new drug development, and ridinilazole may be a step in the right direction.
While the study conducted by Richard Vickers and colleagues was limited by a slightly younger sample with a milder form of the disease than a true representative sample, the superior recurrence reduction related to ridinilazole is an advantage.
It is important that we build upon this study, and push further to expand the array of tools we have to fight C. difficile to optimize treatment for patients at all stages of this disease.
Simon D. Goldenberg, MBBS, MSc, FRCPath, MD, DipHIC, is a consultant microbiologist at the Centre for Clinical Infection and Diagnostics Research, King’s College London. He has received grants and personal fees from Astellas, BD, Luminex, Abbott, Orion Diagnostics, Qiagen, MSD, and DNA electronics.
With a 30-day mortality margin of 9%-38% and recurrence risk baseline of 15%-25%, Clostridium difficile infection continues to be a significant global problem. Yet, for decades there had only been a minimal number of drugs available to treat this disease, namely metronidazole and vancomycin.
As new resistant strains of this disease phased out metronidazole, even in mild cases, fidaxomicin emerged as an adequate replacement, although it was soon clear that because of its high price, fidaxomicin would remain as an initial treatment, disadvantaging those with multiple episodes.
This lack of reliable, effective antimicrobials puts into sharp relief the need for new drug development, and ridinilazole may be a step in the right direction.
While the study conducted by Richard Vickers and colleagues was limited by a slightly younger sample with a milder form of the disease than a true representative sample, the superior recurrence reduction related to ridinilazole is an advantage.
It is important that we build upon this study, and push further to expand the array of tools we have to fight C. difficile to optimize treatment for patients at all stages of this disease.
Simon D. Goldenberg, MBBS, MSc, FRCPath, MD, DipHIC, is a consultant microbiologist at the Centre for Clinical Infection and Diagnostics Research, King’s College London. He has received grants and personal fees from Astellas, BD, Luminex, Abbott, Orion Diagnostics, Qiagen, MSD, and DNA electronics.
Ridinilazole, a new antibiotic for treatment of Clostridium difficile infection (CDI) proved noninferior to vancomycin, showing promise especially in lower recurrence risk, according to a study funded in part by ridinilazole manufacturer Summit Therapeutics.
In a phase 2, 1:1 randomized, double-blind trial of 69 CDI patients, 24 of 36 (66.7%) ridinilazole patients reported a sustained clinical response, compared with 14 of 33 vancomycin patients (42.4%), indicating statistical noninferiority – and even superiority at the upper confidence level – of ridinilazole (Lancet Infect Dis. 2017 Apr 28. doi: 10.1016/S1473-3099[17]30235-9).
Over the course of 10 days, investigators gave the ridinilazole group 200 mg orally twice per day, as well as two placebo doses. Those in the vancomycin group took 125 mg orally four times per day.
Investigators assessed both groups on days 4-6, 10-11, 12-14, and routine weekly follow-ups until 30 days after treatment.
Most of the patients were white females, with an average age of 58 years for the ridinilazole group, and 56 years for the vancomycin group.
Ridinilazole correlated with more sustained clinical responses across almost all subgroups as well, including with treatment differences (respectively) of 42.7%, 15.9%, 19.9%, and 8.9% for those over 75 years, with a more severe diagnosis, more than one previous CDI episode, and those taking other antibiotics before study participation, according to the investigators. Both groups saw similar rates of adverse events related to treatment.
The outcome of this trial could be significant in reducing recurrence risk in CDI patients, which occurs in up to 30% of patients after first treatment, and can increase up to 65% after multiple reinfections, according to Richard Vickers, PhD, chief scientific officer on antimicrobials at Summit Therapeutics PLC, and his fellow investigators.
CDI patients also are subject to significantly higher inpatient mortality, spend longer periods in intensive care, and have higher rates of all-cause readmission over 3 months than do matched controls, the investigators noted.
Unlike the three common CDI drugs on the market, metronidazole, vancomycin, and fidaxomicin, ridinilazole is restricted to the gastrointestinal tract and, according to the investigators, has shown encouraging results in previous studies.
“In vitro studies have shown its high inhibitory activity against C. difficile and minimal activity against both Gram-positive and Gram-negative aerobic and anaerobic intestinal microorganisms,” they wrote. “In a phase 1 study, ridinilazole was safe and well tolerated in healthy human volunteers, with little systemic absorption and little effect on normal gut microbiota.”
They asserted it was this lack of effect that caused the drug to show success in phase 2, noting ridinilazole’s superiority was “likely to be due to the highly selective activity of ridinilazole against CDI and the absence of collateral damage to the microbiota during therapy.”
The study was limited by its sample, which was younger and had a milder form of CDI than is usually represented. The study also formed its power calculations based on the original sample size of 100, and not the adjusted, intended-to-treat population of 69 which became its primary analysis.
Finally, the investigators advised further trials be conducted with a follow-up schedule longer than 30 days.
Dr. Vickers, Dr. Bina Tejura, and Dr. David Roblin reported working for Summit Therapeutics, the drug manufacturer, and hold share options with the company. Other authors reported holding close relationships with other, similar drug manufacturing companies.
[email protected]
On Twitter @eaztweets
Ridinilazole, a new antibiotic for treatment of Clostridium difficile infection (CDI) proved noninferior to vancomycin, showing promise especially in lower recurrence risk, according to a study funded in part by ridinilazole manufacturer Summit Therapeutics.
In a phase 2, 1:1 randomized, double-blind trial of 69 CDI patients, 24 of 36 (66.7%) ridinilazole patients reported a sustained clinical response, compared with 14 of 33 vancomycin patients (42.4%), indicating statistical noninferiority – and even superiority at the upper confidence level – of ridinilazole (Lancet Infect Dis. 2017 Apr 28. doi: 10.1016/S1473-3099[17]30235-9).
Over the course of 10 days, investigators gave the ridinilazole group 200 mg orally twice per day, as well as two placebo doses. Those in the vancomycin group took 125 mg orally four times per day.
Investigators assessed both groups on days 4-6, 10-11, 12-14, and routine weekly follow-ups until 30 days after treatment.
Most of the patients were white females, with an average age of 58 years for the ridinilazole group, and 56 years for the vancomycin group.
Ridinilazole correlated with more sustained clinical responses across almost all subgroups as well, including with treatment differences (respectively) of 42.7%, 15.9%, 19.9%, and 8.9% for those over 75 years, with a more severe diagnosis, more than one previous CDI episode, and those taking other antibiotics before study participation, according to the investigators. Both groups saw similar rates of adverse events related to treatment.
The outcome of this trial could be significant in reducing recurrence risk in CDI patients, which occurs in up to 30% of patients after first treatment, and can increase up to 65% after multiple reinfections, according to Richard Vickers, PhD, chief scientific officer on antimicrobials at Summit Therapeutics PLC, and his fellow investigators.
CDI patients also are subject to significantly higher inpatient mortality, spend longer periods in intensive care, and have higher rates of all-cause readmission over 3 months than do matched controls, the investigators noted.
Unlike the three common CDI drugs on the market, metronidazole, vancomycin, and fidaxomicin, ridinilazole is restricted to the gastrointestinal tract and, according to the investigators, has shown encouraging results in previous studies.
“In vitro studies have shown its high inhibitory activity against C. difficile and minimal activity against both Gram-positive and Gram-negative aerobic and anaerobic intestinal microorganisms,” they wrote. “In a phase 1 study, ridinilazole was safe and well tolerated in healthy human volunteers, with little systemic absorption and little effect on normal gut microbiota.”
They asserted it was this lack of effect that caused the drug to show success in phase 2, noting ridinilazole’s superiority was “likely to be due to the highly selective activity of ridinilazole against CDI and the absence of collateral damage to the microbiota during therapy.”
The study was limited by its sample, which was younger and had a milder form of CDI than is usually represented. The study also formed its power calculations based on the original sample size of 100, and not the adjusted, intended-to-treat population of 69 which became its primary analysis.
Finally, the investigators advised further trials be conducted with a follow-up schedule longer than 30 days.
Dr. Vickers, Dr. Bina Tejura, and Dr. David Roblin reported working for Summit Therapeutics, the drug manufacturer, and hold share options with the company. Other authors reported holding close relationships with other, similar drug manufacturing companies.
[email protected]
On Twitter @eaztweets
FROM LANCET INFECTIOUS DISEASES
Key clinical point:
Major finding: A total of 24 of 36 (66.7%) of the ridinilazole patients showed sustained clinical response, compared with 14 of 33 (42.4%) of vancomycin patients, proving ridinilazole noninferior (treatment difference: 21.1%, CI, 90% [3.1-39.1] P = .0004).
Data source: A phase 2, double-blind, randomized noninferiority study of 69 patients gathered from 21 North American sites between June 16, 2014, and Aug. 31, 2015.
Disclosures: Dr. Richard Vickers, Dr. Bina Tejura, and Dr. David Roblin reported working for Summit Therapeutics, the drug manufacturer, and hold share options with the company. Other authors reported holding close relationships with other, similar drug manufacturing companies.
Vaccination does not eliminate risk for meningococcal disease in eculizumab recipients
Patients taking eculizumab are at a significant risk for meningococcal disease even if they have received the quadrivalent meningococcal conjugate (MenACWY) and serogroup B (MenB) meningococcal vaccines, according to the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report, released July 7.
Between 2008 and 2016, 16 cases of meningococcal disease were reported in eculizumab users in 10 jurisdictions within the United States. Of those infected, 14 had received MenACWY and MenB vaccines as recommended by the Advisory Committee on Immunization Practices, according to the CDC report.
Required vaccination plus antimicrobial prophylaxis for the duration of eculizumab treatment might reduce the risk for meningococcal disease in these patients, but the addition of antibiotic prophylaxis is no guarantee that all cases of meningococcal disease would be prevented, wrote Lucy A. McNamara, PhD, of the division of bacterial diseases, National Center for Immunization and Respiratory Diseases, CDC, and her colleagues.
They advised physician and patient vigilance regarding meningococcal disease symptoms and urged that patients be advised to seek immediate care and be rapidly treated, regardless of meningococcal vaccination or antimicrobial prophylaxis status.
Health organizations in Europe, including France and the United Kingdom, are recommending eculizumab users receive penicillin during eculizumab treatment. A recent study of invasive meningococcal isolates in the United States found most were susceptible to penicillin, according to the report.
In the 16 U.S. cases reported, nongroupable Neisseria meningitidis caused meningococcal disease in 11 of the patients, serogroup Y was the cause in 4 patients, and the cause was not identified in 1 patient.
Ten patients had meningococcemia without meningitis, the researchers noted. “Initial symptoms of meningococcemia are often relatively mild and nonspecific and might include fever, chills, fatigue, vomiting, diarrhea, and aches or pains in the muscles, joints, chest, or abdomen; however, these symptoms can progress to severe illness and death within hours.”
Eculizumab (Soliris, Alexion Pharmaceuticals) is licensed in the United States for treatment of paroxysmal nocturnal hemoglobinuria and atypical hemolytic uremic syndrome, two diseases that are rare and can be fatal.
Eculizumab is associated with a 1,000-fold to 2,000-fold increased incidence of meningococcal disease among persons receiving the drug. The Food and Drug Administration–approved prescribing information includes a boxed warning regarding increased risk for meningococcal disease.
The CDC is collecting reports from state health departments for further analysis of the risk among eculizumab recipients.
The researchers reported having no conflicts of interest.
[email protected]
On Twitter @eaztweets
Patients taking eculizumab are at a significant risk for meningococcal disease even if they have received the quadrivalent meningococcal conjugate (MenACWY) and serogroup B (MenB) meningococcal vaccines, according to the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report, released July 7.
Between 2008 and 2016, 16 cases of meningococcal disease were reported in eculizumab users in 10 jurisdictions within the United States. Of those infected, 14 had received MenACWY and MenB vaccines as recommended by the Advisory Committee on Immunization Practices, according to the CDC report.
Required vaccination plus antimicrobial prophylaxis for the duration of eculizumab treatment might reduce the risk for meningococcal disease in these patients, but the addition of antibiotic prophylaxis is no guarantee that all cases of meningococcal disease would be prevented, wrote Lucy A. McNamara, PhD, of the division of bacterial diseases, National Center for Immunization and Respiratory Diseases, CDC, and her colleagues.
They advised physician and patient vigilance regarding meningococcal disease symptoms and urged that patients be advised to seek immediate care and be rapidly treated, regardless of meningococcal vaccination or antimicrobial prophylaxis status.
Health organizations in Europe, including France and the United Kingdom, are recommending eculizumab users receive penicillin during eculizumab treatment. A recent study of invasive meningococcal isolates in the United States found most were susceptible to penicillin, according to the report.
In the 16 U.S. cases reported, nongroupable Neisseria meningitidis caused meningococcal disease in 11 of the patients, serogroup Y was the cause in 4 patients, and the cause was not identified in 1 patient.
Ten patients had meningococcemia without meningitis, the researchers noted. “Initial symptoms of meningococcemia are often relatively mild and nonspecific and might include fever, chills, fatigue, vomiting, diarrhea, and aches or pains in the muscles, joints, chest, or abdomen; however, these symptoms can progress to severe illness and death within hours.”
Eculizumab (Soliris, Alexion Pharmaceuticals) is licensed in the United States for treatment of paroxysmal nocturnal hemoglobinuria and atypical hemolytic uremic syndrome, two diseases that are rare and can be fatal.
Eculizumab is associated with a 1,000-fold to 2,000-fold increased incidence of meningococcal disease among persons receiving the drug. The Food and Drug Administration–approved prescribing information includes a boxed warning regarding increased risk for meningococcal disease.
The CDC is collecting reports from state health departments for further analysis of the risk among eculizumab recipients.
The researchers reported having no conflicts of interest.
[email protected]
On Twitter @eaztweets
Patients taking eculizumab are at a significant risk for meningococcal disease even if they have received the quadrivalent meningococcal conjugate (MenACWY) and serogroup B (MenB) meningococcal vaccines, according to the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report, released July 7.
Between 2008 and 2016, 16 cases of meningococcal disease were reported in eculizumab users in 10 jurisdictions within the United States. Of those infected, 14 had received MenACWY and MenB vaccines as recommended by the Advisory Committee on Immunization Practices, according to the CDC report.
Required vaccination plus antimicrobial prophylaxis for the duration of eculizumab treatment might reduce the risk for meningococcal disease in these patients, but the addition of antibiotic prophylaxis is no guarantee that all cases of meningococcal disease would be prevented, wrote Lucy A. McNamara, PhD, of the division of bacterial diseases, National Center for Immunization and Respiratory Diseases, CDC, and her colleagues.
They advised physician and patient vigilance regarding meningococcal disease symptoms and urged that patients be advised to seek immediate care and be rapidly treated, regardless of meningococcal vaccination or antimicrobial prophylaxis status.
Health organizations in Europe, including France and the United Kingdom, are recommending eculizumab users receive penicillin during eculizumab treatment. A recent study of invasive meningococcal isolates in the United States found most were susceptible to penicillin, according to the report.
In the 16 U.S. cases reported, nongroupable Neisseria meningitidis caused meningococcal disease in 11 of the patients, serogroup Y was the cause in 4 patients, and the cause was not identified in 1 patient.
Ten patients had meningococcemia without meningitis, the researchers noted. “Initial symptoms of meningococcemia are often relatively mild and nonspecific and might include fever, chills, fatigue, vomiting, diarrhea, and aches or pains in the muscles, joints, chest, or abdomen; however, these symptoms can progress to severe illness and death within hours.”
Eculizumab (Soliris, Alexion Pharmaceuticals) is licensed in the United States for treatment of paroxysmal nocturnal hemoglobinuria and atypical hemolytic uremic syndrome, two diseases that are rare and can be fatal.
Eculizumab is associated with a 1,000-fold to 2,000-fold increased incidence of meningococcal disease among persons receiving the drug. The Food and Drug Administration–approved prescribing information includes a boxed warning regarding increased risk for meningococcal disease.
The CDC is collecting reports from state health departments for further analysis of the risk among eculizumab recipients.
The researchers reported having no conflicts of interest.
[email protected]
On Twitter @eaztweets
FROM MMWR
July 2017: Click for Credit
Here are 6 articles in the July issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. High-dose Oral Vitamin D3 Significantly Reduced Effects of Sunburn
To take the posttest, go to: http://bit.ly/2tmDiKc
Expires May 23, 2018
2. Women Less Likely to Be Diagnosed With Sleep Disorders
To take the posttest, go to: http://bit.ly/2rgLdne
Expires May 30, 2018
3. RA Treatment Delays Raise Risk for Long-term Disability
To take the posttest, go to: http://bit.ly/2tC0IGF
Expires May 30, 2018
4. Target Self-medication of Mood and Anxiety Symptoms
To take the posttest, go to: http://bit.ly/2vy5jel
Expires May 2, 2018
5. Two New Biomarkers for Breast Cancer Show Validity
To take the posttest, go to: http://bit.ly/2ve9H2L
Expires May 2, 2018
6. Time to Therapy for Gram-positive Bacteremia Reduced From 60 Hours to 4 Hours
To take the posttest, go to: http://bit.ly/2ssacIf
Expires May 25, 2018
Here are 6 articles in the July issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. High-dose Oral Vitamin D3 Significantly Reduced Effects of Sunburn
To take the posttest, go to: http://bit.ly/2tmDiKc
Expires May 23, 2018
2. Women Less Likely to Be Diagnosed With Sleep Disorders
To take the posttest, go to: http://bit.ly/2rgLdne
Expires May 30, 2018
3. RA Treatment Delays Raise Risk for Long-term Disability
To take the posttest, go to: http://bit.ly/2tC0IGF
Expires May 30, 2018
4. Target Self-medication of Mood and Anxiety Symptoms
To take the posttest, go to: http://bit.ly/2vy5jel
Expires May 2, 2018
5. Two New Biomarkers for Breast Cancer Show Validity
To take the posttest, go to: http://bit.ly/2ve9H2L
Expires May 2, 2018
6. Time to Therapy for Gram-positive Bacteremia Reduced From 60 Hours to 4 Hours
To take the posttest, go to: http://bit.ly/2ssacIf
Expires May 25, 2018
Here are 6 articles in the July issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. High-dose Oral Vitamin D3 Significantly Reduced Effects of Sunburn
To take the posttest, go to: http://bit.ly/2tmDiKc
Expires May 23, 2018
2. Women Less Likely to Be Diagnosed With Sleep Disorders
To take the posttest, go to: http://bit.ly/2rgLdne
Expires May 30, 2018
3. RA Treatment Delays Raise Risk for Long-term Disability
To take the posttest, go to: http://bit.ly/2tC0IGF
Expires May 30, 2018
4. Target Self-medication of Mood and Anxiety Symptoms
To take the posttest, go to: http://bit.ly/2vy5jel
Expires May 2, 2018
5. Two New Biomarkers for Breast Cancer Show Validity
To take the posttest, go to: http://bit.ly/2ve9H2L
Expires May 2, 2018
6. Time to Therapy for Gram-positive Bacteremia Reduced From 60 Hours to 4 Hours
To take the posttest, go to: http://bit.ly/2ssacIf
Expires May 25, 2018
Health IT: Cybercrime risks are real
Aging equipment, valuable data, and an improperly trained workforce make health care IT extraordinarily vulnerable to external malfeasance, as demonstrated by the WannaCry virus episode that occurred this spring in the United Kingdom.
Computer hackers used a weakness in the operating system employed by the U.K. National Health Service, allowing the WannaCry virus to spread quickly across connected systems. The ransomware attack locked clinicians out of patient records and diagnostic machines that were connected, bringing patient care to a near standstill.
The attack lasted 3 days until Marcus Hutchins, a 22-year-old security researcher, stumbled onto a way to slow the spread of the virus enough to manage it, but not before nearly 60 million attacks had been conducted, Salim Neino, CEO of Kryptos Logic, testified June 15 at a joint hearing of two subcommittees of the House Science, Space & Technology Committee. Mr. Hutchins is employed by Kryptos Logic.
U.S. officials are keenly aware that a similar attack could happen here. In June, the federally sponsored Health Care Industry Cybersecurity Task Force issued a report on their year-long look at the state of the health care IT in this country. The task force was mandated by the Cybersecurity Act of 2015and formed in March 2016.
Specifically, the task force recommended:
• Defining and streamlining leadership, governance, and expectations for health care industry cybersecurity.
• Increasing the security and resilience of medical devices and health IT.
• Developing the health care workforce capacity necessary to prioritize and ensure cybersecurity awareness and technical capabilities.
• Increasing health care industry readiness through improved cybersecurity awareness and education.
• Identifying mechanisms to protect research and development efforts and intellectual property from attacks or exposure.
• Improving information sharing of industry threats, weaknesses, and mitigations.
Health care cybercrime is a significant problem in the United States. In 2016, 328 U.S. health care firms reported data breaches, up from 268 in 2015, with a total of 16.6 million Americans affected, according to a report conducted by Bitglass (registration required), a security software company. In February 2016, a hospital in California was forced to pay about $17,000 in Bitcoin, an electronic currency that is known to be favored by cybercriminals, to access electronic health records (EHRs) that were held in a similar manner to last month’s attack on the NHS.
For physicians, this may seem like someone else’s problem; however, unsafe day-to-day interactions with connected devices and patient EHRs were among the task force’s primary concerns.
For many, creating a safe password or not giving out critical information may seem like common sense, but many physicians are not able or willing to take the time to make sure they are interacting with systems safely, or they are overconfident in their security system, according to task force member Mark Jarrett, MD, senior vice president and chief quality officer at Northwell Health in New York.
“Most physicians now will try to access medical records of their patients who have been in the hospital because that’s good care,” Dr. Jarrett said in an interview. But they have to recognize that “they cannot give these passwords to other people and they need to make these passwords complex.”
“Phishing” is another concern. In a phishing scam, cybercriminals will pose as a fraudulent institution or individual in order to trick a target into downloading a virus, sending additional valuable information, or even paying money directly to the criminals.
“Physicians checking their emails need to be aware of possible phishing episodes, because they could be infected, and then there is the possibility that infection could be introduced into the system, Dr. Jarrett said. “I think the disconnect is [that physicians] are not used to [cybersecurity]. It’s not part of their daily life and they also, up until recently, thought ‘it’s never going to happen to me.’ ”
While hospitals are not completely incapable of protecting themselves, experts are concerned about an overinflated sense of confidence among health care professionals.
“Health care workers often assume that the IT network and the devices they support function efficiently and that their level of cybersecurity vulnerability is low,” according to the task force report.
This can be a costly assumption, financially, as well for safety; the price per stolen EHR averaged at $380 in 2016-2017, according to the Ponemon Institute’s 2017 Cost of Data Breach Study, released in June. That is nearly triple the average cost of all breaches – $141– and higher than the price of $241 for information stolen from financial industries because, unlike a credit card number, patients’ data are unique and cannot be replaced.
Aging equipment is another concern. Legacy software and machine systems used in medical practices and hospitals are not equipped with the necessary security services needed to handle the growing risks of connectivity, despite being included in the network.
“Every CT machine, every x-ray machine today is connected online, on one consolidated Internet” cybersecurity expert Idan Udi Edry of Trustifi said in an interview. “The more comfortable we are with the digital edge coming into our lives, the more vulnerable we become and the more security we need to implement to protect ourselves.”
Some solutions already have been suggested to help health care professionals replace their outdated equipment, especially private practice physicians or smaller hospitals without much financial wiggle room,
The cybersecurity task force report recommended creating health IT version of Cash for Clunkers, an Obama administration program that offered rebates to consumers who traded in older, less fuel efficient cars when purchasing a new car.
While experts agree that the growing focus on connected health care will continue to create cybersecurity risks, with all members of the health care industry working together, it is possible to keep hospitals and patients safe from would-be criminals.
The next key step is creating regulations that would encourage a cohesive structure of cybersecurity guidelines. According to the task force report, “a priority for regulatory agencies should be to ensure consistency among various federal and state cybersecurity regulations so that health care providers can focus on deploying their resources appropriately between securing patient information and the quality, safety, and accessibility of patient care” rather than having to focus on statutory and regulatory inconsistencies.
[email protected]
On Twitter @eaztweets
When computer hackers took control of the United Kingdom’s National Health Service using a virus known as “WannaCry,” doctors and nurses were left helpless, blocked from the files they would need to treat their patients until they paid to get them those files back.
Doctors were forced to revert to older methods, slowing everything to a snail’s pace.
The media coverage of the event was dramatic, but there is no doubt the effects made it justifiably so.
NHS hospitals had not achieved their goal of being paperless; had they been, the service would have been completely unable to stop the attack.
It was not just software that was affected but medical devices as well. Physicians were unable to perform x-rays, and some hospitals found that the refrigerators used to store blood products were shut down.
While the NHS was particularly vulnerable to the WannaCry because of budget cuts, this cybercrime could have happened to any hospital, and its lessons are applicable far all.
Doctors do understand the value of patients records, but they seem to be unaware of the physical harm that could befall patients from a cyberattack.
This attack needs to serve as a wake-up call for health care professionals who are not invested in their facilities’ cybersecurity practices.
Underfunding left NHS hospitals terribly exposed and, if physicians continue to be complacent with how to handle this issue, the results are sure to be more severe.
Rachel Clarke, MD, is at Oxford (England) University Hospitals NHS Foundation Trust, and Taryn Youngstein, MD, is at Imperial College Healthcare NHS Trust, London. They reported having no relevant financial conflicts of interest. Their remarks were make in a perspective published in the New England Journal of Medicine (doi: 10.1056/NEJMp1706754).
When computer hackers took control of the United Kingdom’s National Health Service using a virus known as “WannaCry,” doctors and nurses were left helpless, blocked from the files they would need to treat their patients until they paid to get them those files back.
Doctors were forced to revert to older methods, slowing everything to a snail’s pace.
The media coverage of the event was dramatic, but there is no doubt the effects made it justifiably so.
NHS hospitals had not achieved their goal of being paperless; had they been, the service would have been completely unable to stop the attack.
It was not just software that was affected but medical devices as well. Physicians were unable to perform x-rays, and some hospitals found that the refrigerators used to store blood products were shut down.
While the NHS was particularly vulnerable to the WannaCry because of budget cuts, this cybercrime could have happened to any hospital, and its lessons are applicable far all.
Doctors do understand the value of patients records, but they seem to be unaware of the physical harm that could befall patients from a cyberattack.
This attack needs to serve as a wake-up call for health care professionals who are not invested in their facilities’ cybersecurity practices.
Underfunding left NHS hospitals terribly exposed and, if physicians continue to be complacent with how to handle this issue, the results are sure to be more severe.
Rachel Clarke, MD, is at Oxford (England) University Hospitals NHS Foundation Trust, and Taryn Youngstein, MD, is at Imperial College Healthcare NHS Trust, London. They reported having no relevant financial conflicts of interest. Their remarks were make in a perspective published in the New England Journal of Medicine (doi: 10.1056/NEJMp1706754).
When computer hackers took control of the United Kingdom’s National Health Service using a virus known as “WannaCry,” doctors and nurses were left helpless, blocked from the files they would need to treat their patients until they paid to get them those files back.
Doctors were forced to revert to older methods, slowing everything to a snail’s pace.
The media coverage of the event was dramatic, but there is no doubt the effects made it justifiably so.
NHS hospitals had not achieved their goal of being paperless; had they been, the service would have been completely unable to stop the attack.
It was not just software that was affected but medical devices as well. Physicians were unable to perform x-rays, and some hospitals found that the refrigerators used to store blood products were shut down.
While the NHS was particularly vulnerable to the WannaCry because of budget cuts, this cybercrime could have happened to any hospital, and its lessons are applicable far all.
Doctors do understand the value of patients records, but they seem to be unaware of the physical harm that could befall patients from a cyberattack.
This attack needs to serve as a wake-up call for health care professionals who are not invested in their facilities’ cybersecurity practices.
Underfunding left NHS hospitals terribly exposed and, if physicians continue to be complacent with how to handle this issue, the results are sure to be more severe.
Rachel Clarke, MD, is at Oxford (England) University Hospitals NHS Foundation Trust, and Taryn Youngstein, MD, is at Imperial College Healthcare NHS Trust, London. They reported having no relevant financial conflicts of interest. Their remarks were make in a perspective published in the New England Journal of Medicine (doi: 10.1056/NEJMp1706754).
Aging equipment, valuable data, and an improperly trained workforce make health care IT extraordinarily vulnerable to external malfeasance, as demonstrated by the WannaCry virus episode that occurred this spring in the United Kingdom.
Computer hackers used a weakness in the operating system employed by the U.K. National Health Service, allowing the WannaCry virus to spread quickly across connected systems. The ransomware attack locked clinicians out of patient records and diagnostic machines that were connected, bringing patient care to a near standstill.
The attack lasted 3 days until Marcus Hutchins, a 22-year-old security researcher, stumbled onto a way to slow the spread of the virus enough to manage it, but not before nearly 60 million attacks had been conducted, Salim Neino, CEO of Kryptos Logic, testified June 15 at a joint hearing of two subcommittees of the House Science, Space & Technology Committee. Mr. Hutchins is employed by Kryptos Logic.
U.S. officials are keenly aware that a similar attack could happen here. In June, the federally sponsored Health Care Industry Cybersecurity Task Force issued a report on their year-long look at the state of the health care IT in this country. The task force was mandated by the Cybersecurity Act of 2015and formed in March 2016.
Specifically, the task force recommended:
• Defining and streamlining leadership, governance, and expectations for health care industry cybersecurity.
• Increasing the security and resilience of medical devices and health IT.
• Developing the health care workforce capacity necessary to prioritize and ensure cybersecurity awareness and technical capabilities.
• Increasing health care industry readiness through improved cybersecurity awareness and education.
• Identifying mechanisms to protect research and development efforts and intellectual property from attacks or exposure.
• Improving information sharing of industry threats, weaknesses, and mitigations.
Health care cybercrime is a significant problem in the United States. In 2016, 328 U.S. health care firms reported data breaches, up from 268 in 2015, with a total of 16.6 million Americans affected, according to a report conducted by Bitglass (registration required), a security software company. In February 2016, a hospital in California was forced to pay about $17,000 in Bitcoin, an electronic currency that is known to be favored by cybercriminals, to access electronic health records (EHRs) that were held in a similar manner to last month’s attack on the NHS.
For physicians, this may seem like someone else’s problem; however, unsafe day-to-day interactions with connected devices and patient EHRs were among the task force’s primary concerns.
For many, creating a safe password or not giving out critical information may seem like common sense, but many physicians are not able or willing to take the time to make sure they are interacting with systems safely, or they are overconfident in their security system, according to task force member Mark Jarrett, MD, senior vice president and chief quality officer at Northwell Health in New York.
“Most physicians now will try to access medical records of their patients who have been in the hospital because that’s good care,” Dr. Jarrett said in an interview. But they have to recognize that “they cannot give these passwords to other people and they need to make these passwords complex.”
“Phishing” is another concern. In a phishing scam, cybercriminals will pose as a fraudulent institution or individual in order to trick a target into downloading a virus, sending additional valuable information, or even paying money directly to the criminals.
“Physicians checking their emails need to be aware of possible phishing episodes, because they could be infected, and then there is the possibility that infection could be introduced into the system, Dr. Jarrett said. “I think the disconnect is [that physicians] are not used to [cybersecurity]. It’s not part of their daily life and they also, up until recently, thought ‘it’s never going to happen to me.’ ”
While hospitals are not completely incapable of protecting themselves, experts are concerned about an overinflated sense of confidence among health care professionals.
“Health care workers often assume that the IT network and the devices they support function efficiently and that their level of cybersecurity vulnerability is low,” according to the task force report.
This can be a costly assumption, financially, as well for safety; the price per stolen EHR averaged at $380 in 2016-2017, according to the Ponemon Institute’s 2017 Cost of Data Breach Study, released in June. That is nearly triple the average cost of all breaches – $141– and higher than the price of $241 for information stolen from financial industries because, unlike a credit card number, patients’ data are unique and cannot be replaced.
Aging equipment is another concern. Legacy software and machine systems used in medical practices and hospitals are not equipped with the necessary security services needed to handle the growing risks of connectivity, despite being included in the network.
“Every CT machine, every x-ray machine today is connected online, on one consolidated Internet” cybersecurity expert Idan Udi Edry of Trustifi said in an interview. “The more comfortable we are with the digital edge coming into our lives, the more vulnerable we become and the more security we need to implement to protect ourselves.”
Some solutions already have been suggested to help health care professionals replace their outdated equipment, especially private practice physicians or smaller hospitals without much financial wiggle room,
The cybersecurity task force report recommended creating health IT version of Cash for Clunkers, an Obama administration program that offered rebates to consumers who traded in older, less fuel efficient cars when purchasing a new car.
While experts agree that the growing focus on connected health care will continue to create cybersecurity risks, with all members of the health care industry working together, it is possible to keep hospitals and patients safe from would-be criminals.
The next key step is creating regulations that would encourage a cohesive structure of cybersecurity guidelines. According to the task force report, “a priority for regulatory agencies should be to ensure consistency among various federal and state cybersecurity regulations so that health care providers can focus on deploying their resources appropriately between securing patient information and the quality, safety, and accessibility of patient care” rather than having to focus on statutory and regulatory inconsistencies.
[email protected]
On Twitter @eaztweets
Aging equipment, valuable data, and an improperly trained workforce make health care IT extraordinarily vulnerable to external malfeasance, as demonstrated by the WannaCry virus episode that occurred this spring in the United Kingdom.
Computer hackers used a weakness in the operating system employed by the U.K. National Health Service, allowing the WannaCry virus to spread quickly across connected systems. The ransomware attack locked clinicians out of patient records and diagnostic machines that were connected, bringing patient care to a near standstill.
The attack lasted 3 days until Marcus Hutchins, a 22-year-old security researcher, stumbled onto a way to slow the spread of the virus enough to manage it, but not before nearly 60 million attacks had been conducted, Salim Neino, CEO of Kryptos Logic, testified June 15 at a joint hearing of two subcommittees of the House Science, Space & Technology Committee. Mr. Hutchins is employed by Kryptos Logic.
U.S. officials are keenly aware that a similar attack could happen here. In June, the federally sponsored Health Care Industry Cybersecurity Task Force issued a report on their year-long look at the state of the health care IT in this country. The task force was mandated by the Cybersecurity Act of 2015and formed in March 2016.
Specifically, the task force recommended:
• Defining and streamlining leadership, governance, and expectations for health care industry cybersecurity.
• Increasing the security and resilience of medical devices and health IT.
• Developing the health care workforce capacity necessary to prioritize and ensure cybersecurity awareness and technical capabilities.
• Increasing health care industry readiness through improved cybersecurity awareness and education.
• Identifying mechanisms to protect research and development efforts and intellectual property from attacks or exposure.
• Improving information sharing of industry threats, weaknesses, and mitigations.
Health care cybercrime is a significant problem in the United States. In 2016, 328 U.S. health care firms reported data breaches, up from 268 in 2015, with a total of 16.6 million Americans affected, according to a report conducted by Bitglass (registration required), a security software company. In February 2016, a hospital in California was forced to pay about $17,000 in Bitcoin, an electronic currency that is known to be favored by cybercriminals, to access electronic health records (EHRs) that were held in a similar manner to last month’s attack on the NHS.
For physicians, this may seem like someone else’s problem; however, unsafe day-to-day interactions with connected devices and patient EHRs were among the task force’s primary concerns.
For many, creating a safe password or not giving out critical information may seem like common sense, but many physicians are not able or willing to take the time to make sure they are interacting with systems safely, or they are overconfident in their security system, according to task force member Mark Jarrett, MD, senior vice president and chief quality officer at Northwell Health in New York.
“Most physicians now will try to access medical records of their patients who have been in the hospital because that’s good care,” Dr. Jarrett said in an interview. But they have to recognize that “they cannot give these passwords to other people and they need to make these passwords complex.”
“Phishing” is another concern. In a phishing scam, cybercriminals will pose as a fraudulent institution or individual in order to trick a target into downloading a virus, sending additional valuable information, or even paying money directly to the criminals.
“Physicians checking their emails need to be aware of possible phishing episodes, because they could be infected, and then there is the possibility that infection could be introduced into the system, Dr. Jarrett said. “I think the disconnect is [that physicians] are not used to [cybersecurity]. It’s not part of their daily life and they also, up until recently, thought ‘it’s never going to happen to me.’ ”
While hospitals are not completely incapable of protecting themselves, experts are concerned about an overinflated sense of confidence among health care professionals.
“Health care workers often assume that the IT network and the devices they support function efficiently and that their level of cybersecurity vulnerability is low,” according to the task force report.
This can be a costly assumption, financially, as well for safety; the price per stolen EHR averaged at $380 in 2016-2017, according to the Ponemon Institute’s 2017 Cost of Data Breach Study, released in June. That is nearly triple the average cost of all breaches – $141– and higher than the price of $241 for information stolen from financial industries because, unlike a credit card number, patients’ data are unique and cannot be replaced.
Aging equipment is another concern. Legacy software and machine systems used in medical practices and hospitals are not equipped with the necessary security services needed to handle the growing risks of connectivity, despite being included in the network.
“Every CT machine, every x-ray machine today is connected online, on one consolidated Internet” cybersecurity expert Idan Udi Edry of Trustifi said in an interview. “The more comfortable we are with the digital edge coming into our lives, the more vulnerable we become and the more security we need to implement to protect ourselves.”
Some solutions already have been suggested to help health care professionals replace their outdated equipment, especially private practice physicians or smaller hospitals without much financial wiggle room,
The cybersecurity task force report recommended creating health IT version of Cash for Clunkers, an Obama administration program that offered rebates to consumers who traded in older, less fuel efficient cars when purchasing a new car.
While experts agree that the growing focus on connected health care will continue to create cybersecurity risks, with all members of the health care industry working together, it is possible to keep hospitals and patients safe from would-be criminals.
The next key step is creating regulations that would encourage a cohesive structure of cybersecurity guidelines. According to the task force report, “a priority for regulatory agencies should be to ensure consistency among various federal and state cybersecurity regulations so that health care providers can focus on deploying their resources appropriately between securing patient information and the quality, safety, and accessibility of patient care” rather than having to focus on statutory and regulatory inconsistencies.
[email protected]
On Twitter @eaztweets
Small study: Patients prefer microneedle flu vaccine
Influenza vaccinations given through a microneedle patch (MNP) received higher patient approval compared with traditional inoculation methods, according to a small study funded by the National Institutes of Health.
In a phase I, randomized, placebo-controlled study, 100 patients between the ages of 18 and 49 years were split into four groups: one given the patch by a health care worker, one instructed to apply the patch at home, one given a vaccine through a traditional intramuscular injection, and one given a placebo.
Of those who took the patch, 70% (33 of 47) preferred the patch to intramuscular injection (The Lancet. 2017 Jun 27. doi: 10.1016/S0140-6736[17]30575-5).
All nonplacebo groups were given Fluvirin, the 2014-2015 licensed trivalent inactivated influenza vaccine, according to the researchers.
Protection against the virus 6 months after vaccination was similar across all groups other than the placebo group: 20-24 (83%-100%) of 24 participants given the patch by a health care worker, 18-24 (75%-100%) of 24 in the group of patients who gave themselves the patch, and 20-25 (80%-100%) of 25 in the injection group having achieved seroprotection against the three influenza strains 6 months after vaccination.
When measuring reactogenicity, the investigators did find more patients (41 of 50) reported cases of pruritis in the microneedle group than in the injection group (4 of 25).
However, these cases were mostly mild, while the injection group reported more grade 2 and grade 3 reactions, with grade 4 being the most severe.
Given the storage temperature of 40° C and ease of use without a health care provider, the investigators discussed the financial and clinical prospects of the patch.
“Increased acceptability could enable increased rates of influenza vaccination, which are currently less than 50% in adult populations,” they noted. “Moreover, because participants were able to self-vaccinate and 70% or more preferred it, significant cost savings could be enabled by microneedle patches due to a reduction in health-care worker time devoted to vaccination.”
Along with storage life and simple application process, the fact that the microneedles dissolve safely into the skin creates the potential for use in patients’ homes and offices, the researchers noted.
There may also be potential for use among pediatric patients, who may be resistant to vaccinations because of the injection method, they added.
“Microneedle patches have the potential to become ideal candidates for vaccination programmes, not only in poorly resourced settings, but also for individuals who currently prefer not to get vaccinated, potentially even being an attractive vaccine for the paediatric population,” Katja Höschler, PhD, and Maria C. Zambon, PhD, of Public Health England, London, said in a comment published with the study (The Lancet. 2017 Jun 27. doi: 10.1016/S0140-6736[17]31364-8). “The delivery advantages could also be exploited for non-influenza vaccines.”
Further studies must be conducted to test the efficacy of this vaccination system, because this study was limited by its size, the researchers noted.
The population was less inclined to receive an influenza injection because of the method itself, which may have affected the levels of preference for the patch, they added.
Some of the researchers are employees of Micron Biomedical, a company that manufactures microneedle products, and are listed as inventors on the licensed patents of these products. The investigators reported no other relevant financial disclosures.
[email protected]
On Twitter@eaztweets
Influenza vaccinations given through a microneedle patch (MNP) received higher patient approval compared with traditional inoculation methods, according to a small study funded by the National Institutes of Health.
In a phase I, randomized, placebo-controlled study, 100 patients between the ages of 18 and 49 years were split into four groups: one given the patch by a health care worker, one instructed to apply the patch at home, one given a vaccine through a traditional intramuscular injection, and one given a placebo.
Of those who took the patch, 70% (33 of 47) preferred the patch to intramuscular injection (The Lancet. 2017 Jun 27. doi: 10.1016/S0140-6736[17]30575-5).
All nonplacebo groups were given Fluvirin, the 2014-2015 licensed trivalent inactivated influenza vaccine, according to the researchers.
Protection against the virus 6 months after vaccination was similar across all groups other than the placebo group: 20-24 (83%-100%) of 24 participants given the patch by a health care worker, 18-24 (75%-100%) of 24 in the group of patients who gave themselves the patch, and 20-25 (80%-100%) of 25 in the injection group having achieved seroprotection against the three influenza strains 6 months after vaccination.
When measuring reactogenicity, the investigators did find more patients (41 of 50) reported cases of pruritis in the microneedle group than in the injection group (4 of 25).
However, these cases were mostly mild, while the injection group reported more grade 2 and grade 3 reactions, with grade 4 being the most severe.
Given the storage temperature of 40° C and ease of use without a health care provider, the investigators discussed the financial and clinical prospects of the patch.
“Increased acceptability could enable increased rates of influenza vaccination, which are currently less than 50% in adult populations,” they noted. “Moreover, because participants were able to self-vaccinate and 70% or more preferred it, significant cost savings could be enabled by microneedle patches due to a reduction in health-care worker time devoted to vaccination.”
Along with storage life and simple application process, the fact that the microneedles dissolve safely into the skin creates the potential for use in patients’ homes and offices, the researchers noted.
There may also be potential for use among pediatric patients, who may be resistant to vaccinations because of the injection method, they added.
“Microneedle patches have the potential to become ideal candidates for vaccination programmes, not only in poorly resourced settings, but also for individuals who currently prefer not to get vaccinated, potentially even being an attractive vaccine for the paediatric population,” Katja Höschler, PhD, and Maria C. Zambon, PhD, of Public Health England, London, said in a comment published with the study (The Lancet. 2017 Jun 27. doi: 10.1016/S0140-6736[17]31364-8). “The delivery advantages could also be exploited for non-influenza vaccines.”
Further studies must be conducted to test the efficacy of this vaccination system, because this study was limited by its size, the researchers noted.
The population was less inclined to receive an influenza injection because of the method itself, which may have affected the levels of preference for the patch, they added.
Some of the researchers are employees of Micron Biomedical, a company that manufactures microneedle products, and are listed as inventors on the licensed patents of these products. The investigators reported no other relevant financial disclosures.
[email protected]
On Twitter@eaztweets
Influenza vaccinations given through a microneedle patch (MNP) received higher patient approval compared with traditional inoculation methods, according to a small study funded by the National Institutes of Health.
In a phase I, randomized, placebo-controlled study, 100 patients between the ages of 18 and 49 years were split into four groups: one given the patch by a health care worker, one instructed to apply the patch at home, one given a vaccine through a traditional intramuscular injection, and one given a placebo.
Of those who took the patch, 70% (33 of 47) preferred the patch to intramuscular injection (The Lancet. 2017 Jun 27. doi: 10.1016/S0140-6736[17]30575-5).
All nonplacebo groups were given Fluvirin, the 2014-2015 licensed trivalent inactivated influenza vaccine, according to the researchers.
Protection against the virus 6 months after vaccination was similar across all groups other than the placebo group: 20-24 (83%-100%) of 24 participants given the patch by a health care worker, 18-24 (75%-100%) of 24 in the group of patients who gave themselves the patch, and 20-25 (80%-100%) of 25 in the injection group having achieved seroprotection against the three influenza strains 6 months after vaccination.
When measuring reactogenicity, the investigators did find more patients (41 of 50) reported cases of pruritis in the microneedle group than in the injection group (4 of 25).
However, these cases were mostly mild, while the injection group reported more grade 2 and grade 3 reactions, with grade 4 being the most severe.
Given the storage temperature of 40° C and ease of use without a health care provider, the investigators discussed the financial and clinical prospects of the patch.
“Increased acceptability could enable increased rates of influenza vaccination, which are currently less than 50% in adult populations,” they noted. “Moreover, because participants were able to self-vaccinate and 70% or more preferred it, significant cost savings could be enabled by microneedle patches due to a reduction in health-care worker time devoted to vaccination.”
Along with storage life and simple application process, the fact that the microneedles dissolve safely into the skin creates the potential for use in patients’ homes and offices, the researchers noted.
There may also be potential for use among pediatric patients, who may be resistant to vaccinations because of the injection method, they added.
“Microneedle patches have the potential to become ideal candidates for vaccination programmes, not only in poorly resourced settings, but also for individuals who currently prefer not to get vaccinated, potentially even being an attractive vaccine for the paediatric population,” Katja Höschler, PhD, and Maria C. Zambon, PhD, of Public Health England, London, said in a comment published with the study (The Lancet. 2017 Jun 27. doi: 10.1016/S0140-6736[17]31364-8). “The delivery advantages could also be exploited for non-influenza vaccines.”
Further studies must be conducted to test the efficacy of this vaccination system, because this study was limited by its size, the researchers noted.
The population was less inclined to receive an influenza injection because of the method itself, which may have affected the levels of preference for the patch, they added.
Some of the researchers are employees of Micron Biomedical, a company that manufactures microneedle products, and are listed as inventors on the licensed patents of these products. The investigators reported no other relevant financial disclosures.
[email protected]
On Twitter@eaztweets
FROM THE LANCET
Key clinical point:
Major finding: Twenty-eight days after vaccination, 33 of 47 of patients (70%) who received the microneedle patch vaccine preferred that method to traditional inoculation.
Data source: A phase I, randomized, placebo-controlled study of 100 patients between the ages of 18 and 49 years.
Disclosures: Three of the researchers are employees of Micron Biomedical, a company that manufactures microneedle products, and are listed as inventors on the licensed patents of these products. The investigators reported no other relevant financial disclosures.
High TAVR rates linked to fewer readmissions
WASHINGTON – Hospitals with a higher volume of transcatheter aortic valve replacements (TAVRs) have significantly lower 30-day readmission rates, according to an observational study.
In a study of 129 hospitals, those that performed more than 100 TAVR procedures had a 24% and 25% lower readmission rate compared with hospitals that performed 50 to100 TAVRs (P less than .001) and hospitals that performed fewer that 50 TAVRs (P = .007) respectively (JAMA Cardiol. 2017 May 11. doi: 10.1001/jamacardio.2017.1630).
This finding could have serious financial and medical implications for hospitals that are deciding whether or not to focus on this minimally invasive procedure, according to Sahil Khera, MD, MPH, chief resident and cardiology fellow at New York Medical College, Valhalla, and his colleagues.
“Lower readmission rates at high-volume hospitals substantially reduce health care expenditure,” said Dr. Khera and colleagues. “As new TAVR programs open across the country, these data will guide policymakers to identify targets for optimizing and standardizing TAVR outcomes across hospitals.”
To study the correlation between TAVR procedures and readmission rates, the investigators gathered records on hospitals that performed at least five TAVRs in 2014, which were then categorized into high-, medium-, or low-volume categories, and cross-referenced with the 2014 Nationwide Readmissions Database.
Of the 16,252 TAVR procedures conducted in 2014, 663 (4%), 3,067 (19%), and 12,522 (77%) were performed at low-, medium-, and high-volume hospitals, respectively, according to the investigators.
Patients undergoing these procedures were on average 81 years of age, with an average of four Elixhauser comorbidities, most commonly dyslipidemia (64%), hypertension (80%), heart failure (75%), and known coronary artery disease (69%), with a majority having undergone an endovascular procedure (83%).
However, the researchers found the population of TAVR patients of high volume hospitals were slightly younger, had fewer women, were more likely to be in a higher income household, and were less likely to undergo a transapical procedure than in low volume hospitals, which Dr. Khera and fellow researchers believe may have some impact on their findings.
“Low-volume hospitals were more likely to operate on patients with a higher number of comorbidities compared with high-volume hospitals and were more likely to use the TA approach,” according to investigators, “Transapical TAVR is associated with poorer short- and intermediate-term mortality, increased use of skilled nursing care facilities, longer hospital stays, and readmissions when compared with transfemoral TAVR.”
Overall, there were 2,667 readmissions reported, among which high volume hospitals reported a 30-day readmission rate of 15.6%, while low- and medium-volume hospitals reported similarly higher rates of 19.5% and 19%.
When looking into the causes for these readmissions, the investigators found that 1,619 (61%) were due to noncardiac causes, which appeared in all three hospitals, despite a larger proportion present in low-volume hospitals as opposed to medium and high-volume hospitals (65.6% vs. 60.1% and 60.6%, respectively).
“Infection, respiratory, endocrine/metabolic, renal, and trauma problems were more common in low-volume hospitals,” according to the researchers. “Whereas gastrointestinal and TIA/stroke issues were more common in medium and high volume hospitals.”
While price and length of stay did not differ among the volume categories, the investigators estimate the lower rate of readmissions saved high-volume hospitals approximately $6.5 million.
They found that while the difference of readmissions between hospital classifications narrowed when controlling for experience, the margin was still significant. They admitted, however, that the possibility of greater access to more technologically advanced TAVR in high-volume hospitals may affect the findings.
This study was limited by administrative nature of the database used, which does not make available information such as valve type, patient risk scores, or medications.
One investigator has received personal fees from Edwards Lifesciences and Medtronic; another has received grants and personal fees from various pharmaceutical companies, educational institutions, and publications; and a third has consulted for Medtronic.
[email protected]
On Twitter @eaztweets
Considering the idea of using readmissions in comparison to rate of TAVR procedures is interesting, the number of confounds are too great to give any kind of accurate representation of medical practice. While the authors of this study do address its limitations, including a learning curve as it relates to the risk of inpatient mortality, the number of adjustments that must be made to account for the additional confounding factors are simply too insurmountable to give an accurate estimate of statistical and clinical importance.
For example, researchers found TAVR readmissions were associated with certain baseline comorbidities, access sites, and complications. However, association does not mean causation and so the categorization of cardiac-related vs. noncardiac-related readmissions must be approached with some caution.
If one were to try to use readmission rates after TAVR to argue for reimbursement of the procedure, one would need to determine a well established, validated reimbursement rate for TAVR readmissions, which has not been done.
Also, the advancing nature of this procedure, combined with a constant focus from hospitals to reduce readmission rates means any baseline for readmissions used would most likely be out of date.
It would be unlikely for investigators to factor in the cause of reduced readmission rates, which could be a factor of increased technology, more experienced physicians, lower-risk patients, or any combination thereof.
Holding TAVR sites accountable for quality of care is of course important, but using readmission rates to determine something like funding is not appropriate when the measurement being used is so complex.
Perhaps a better approach would be to widen access for low volume hospitals to resources that would improve the TAVR processes and encourage using financial incentives.
Evaluations by physical therapists or a similar procedure should be put into place before discharge to assess a patient’s risk of readmission.
Overall, this is a multifaceted issue that would be better helped by promoting TAVR best practices and encouraging hospitals to compare themselves against each other to reduce unnecessary readmissions.
John D. Carroll, MD, is professor of medicine and director of the Cardiac and Vascular Center at the University of Colorado, Denver. He made his remarks in an editorial in JAMA Cardiology ( doi: 10.1001/jamacardio.2017.1650 ).
Considering the idea of using readmissions in comparison to rate of TAVR procedures is interesting, the number of confounds are too great to give any kind of accurate representation of medical practice. While the authors of this study do address its limitations, including a learning curve as it relates to the risk of inpatient mortality, the number of adjustments that must be made to account for the additional confounding factors are simply too insurmountable to give an accurate estimate of statistical and clinical importance.
For example, researchers found TAVR readmissions were associated with certain baseline comorbidities, access sites, and complications. However, association does not mean causation and so the categorization of cardiac-related vs. noncardiac-related readmissions must be approached with some caution.
If one were to try to use readmission rates after TAVR to argue for reimbursement of the procedure, one would need to determine a well established, validated reimbursement rate for TAVR readmissions, which has not been done.
Also, the advancing nature of this procedure, combined with a constant focus from hospitals to reduce readmission rates means any baseline for readmissions used would most likely be out of date.
It would be unlikely for investigators to factor in the cause of reduced readmission rates, which could be a factor of increased technology, more experienced physicians, lower-risk patients, or any combination thereof.
Holding TAVR sites accountable for quality of care is of course important, but using readmission rates to determine something like funding is not appropriate when the measurement being used is so complex.
Perhaps a better approach would be to widen access for low volume hospitals to resources that would improve the TAVR processes and encourage using financial incentives.
Evaluations by physical therapists or a similar procedure should be put into place before discharge to assess a patient’s risk of readmission.
Overall, this is a multifaceted issue that would be better helped by promoting TAVR best practices and encouraging hospitals to compare themselves against each other to reduce unnecessary readmissions.
John D. Carroll, MD, is professor of medicine and director of the Cardiac and Vascular Center at the University of Colorado, Denver. He made his remarks in an editorial in JAMA Cardiology ( doi: 10.1001/jamacardio.2017.1650 ).
Considering the idea of using readmissions in comparison to rate of TAVR procedures is interesting, the number of confounds are too great to give any kind of accurate representation of medical practice. While the authors of this study do address its limitations, including a learning curve as it relates to the risk of inpatient mortality, the number of adjustments that must be made to account for the additional confounding factors are simply too insurmountable to give an accurate estimate of statistical and clinical importance.
For example, researchers found TAVR readmissions were associated with certain baseline comorbidities, access sites, and complications. However, association does not mean causation and so the categorization of cardiac-related vs. noncardiac-related readmissions must be approached with some caution.
If one were to try to use readmission rates after TAVR to argue for reimbursement of the procedure, one would need to determine a well established, validated reimbursement rate for TAVR readmissions, which has not been done.
Also, the advancing nature of this procedure, combined with a constant focus from hospitals to reduce readmission rates means any baseline for readmissions used would most likely be out of date.
It would be unlikely for investigators to factor in the cause of reduced readmission rates, which could be a factor of increased technology, more experienced physicians, lower-risk patients, or any combination thereof.
Holding TAVR sites accountable for quality of care is of course important, but using readmission rates to determine something like funding is not appropriate when the measurement being used is so complex.
Perhaps a better approach would be to widen access for low volume hospitals to resources that would improve the TAVR processes and encourage using financial incentives.
Evaluations by physical therapists or a similar procedure should be put into place before discharge to assess a patient’s risk of readmission.
Overall, this is a multifaceted issue that would be better helped by promoting TAVR best practices and encouraging hospitals to compare themselves against each other to reduce unnecessary readmissions.
John D. Carroll, MD, is professor of medicine and director of the Cardiac and Vascular Center at the University of Colorado, Denver. He made his remarks in an editorial in JAMA Cardiology ( doi: 10.1001/jamacardio.2017.1650 ).
WASHINGTON – Hospitals with a higher volume of transcatheter aortic valve replacements (TAVRs) have significantly lower 30-day readmission rates, according to an observational study.
In a study of 129 hospitals, those that performed more than 100 TAVR procedures had a 24% and 25% lower readmission rate compared with hospitals that performed 50 to100 TAVRs (P less than .001) and hospitals that performed fewer that 50 TAVRs (P = .007) respectively (JAMA Cardiol. 2017 May 11. doi: 10.1001/jamacardio.2017.1630).
This finding could have serious financial and medical implications for hospitals that are deciding whether or not to focus on this minimally invasive procedure, according to Sahil Khera, MD, MPH, chief resident and cardiology fellow at New York Medical College, Valhalla, and his colleagues.
“Lower readmission rates at high-volume hospitals substantially reduce health care expenditure,” said Dr. Khera and colleagues. “As new TAVR programs open across the country, these data will guide policymakers to identify targets for optimizing and standardizing TAVR outcomes across hospitals.”
To study the correlation between TAVR procedures and readmission rates, the investigators gathered records on hospitals that performed at least five TAVRs in 2014, which were then categorized into high-, medium-, or low-volume categories, and cross-referenced with the 2014 Nationwide Readmissions Database.
Of the 16,252 TAVR procedures conducted in 2014, 663 (4%), 3,067 (19%), and 12,522 (77%) were performed at low-, medium-, and high-volume hospitals, respectively, according to the investigators.
Patients undergoing these procedures were on average 81 years of age, with an average of four Elixhauser comorbidities, most commonly dyslipidemia (64%), hypertension (80%), heart failure (75%), and known coronary artery disease (69%), with a majority having undergone an endovascular procedure (83%).
However, the researchers found the population of TAVR patients of high volume hospitals were slightly younger, had fewer women, were more likely to be in a higher income household, and were less likely to undergo a transapical procedure than in low volume hospitals, which Dr. Khera and fellow researchers believe may have some impact on their findings.
“Low-volume hospitals were more likely to operate on patients with a higher number of comorbidities compared with high-volume hospitals and were more likely to use the TA approach,” according to investigators, “Transapical TAVR is associated with poorer short- and intermediate-term mortality, increased use of skilled nursing care facilities, longer hospital stays, and readmissions when compared with transfemoral TAVR.”
Overall, there were 2,667 readmissions reported, among which high volume hospitals reported a 30-day readmission rate of 15.6%, while low- and medium-volume hospitals reported similarly higher rates of 19.5% and 19%.
When looking into the causes for these readmissions, the investigators found that 1,619 (61%) were due to noncardiac causes, which appeared in all three hospitals, despite a larger proportion present in low-volume hospitals as opposed to medium and high-volume hospitals (65.6% vs. 60.1% and 60.6%, respectively).
“Infection, respiratory, endocrine/metabolic, renal, and trauma problems were more common in low-volume hospitals,” according to the researchers. “Whereas gastrointestinal and TIA/stroke issues were more common in medium and high volume hospitals.”
While price and length of stay did not differ among the volume categories, the investigators estimate the lower rate of readmissions saved high-volume hospitals approximately $6.5 million.
They found that while the difference of readmissions between hospital classifications narrowed when controlling for experience, the margin was still significant. They admitted, however, that the possibility of greater access to more technologically advanced TAVR in high-volume hospitals may affect the findings.
This study was limited by administrative nature of the database used, which does not make available information such as valve type, patient risk scores, or medications.
One investigator has received personal fees from Edwards Lifesciences and Medtronic; another has received grants and personal fees from various pharmaceutical companies, educational institutions, and publications; and a third has consulted for Medtronic.
[email protected]
On Twitter @eaztweets
WASHINGTON – Hospitals with a higher volume of transcatheter aortic valve replacements (TAVRs) have significantly lower 30-day readmission rates, according to an observational study.
In a study of 129 hospitals, those that performed more than 100 TAVR procedures had a 24% and 25% lower readmission rate compared with hospitals that performed 50 to100 TAVRs (P less than .001) and hospitals that performed fewer that 50 TAVRs (P = .007) respectively (JAMA Cardiol. 2017 May 11. doi: 10.1001/jamacardio.2017.1630).
This finding could have serious financial and medical implications for hospitals that are deciding whether or not to focus on this minimally invasive procedure, according to Sahil Khera, MD, MPH, chief resident and cardiology fellow at New York Medical College, Valhalla, and his colleagues.
“Lower readmission rates at high-volume hospitals substantially reduce health care expenditure,” said Dr. Khera and colleagues. “As new TAVR programs open across the country, these data will guide policymakers to identify targets for optimizing and standardizing TAVR outcomes across hospitals.”
To study the correlation between TAVR procedures and readmission rates, the investigators gathered records on hospitals that performed at least five TAVRs in 2014, which were then categorized into high-, medium-, or low-volume categories, and cross-referenced with the 2014 Nationwide Readmissions Database.
Of the 16,252 TAVR procedures conducted in 2014, 663 (4%), 3,067 (19%), and 12,522 (77%) were performed at low-, medium-, and high-volume hospitals, respectively, according to the investigators.
Patients undergoing these procedures were on average 81 years of age, with an average of four Elixhauser comorbidities, most commonly dyslipidemia (64%), hypertension (80%), heart failure (75%), and known coronary artery disease (69%), with a majority having undergone an endovascular procedure (83%).
However, the researchers found the population of TAVR patients of high volume hospitals were slightly younger, had fewer women, were more likely to be in a higher income household, and were less likely to undergo a transapical procedure than in low volume hospitals, which Dr. Khera and fellow researchers believe may have some impact on their findings.
“Low-volume hospitals were more likely to operate on patients with a higher number of comorbidities compared with high-volume hospitals and were more likely to use the TA approach,” according to investigators, “Transapical TAVR is associated with poorer short- and intermediate-term mortality, increased use of skilled nursing care facilities, longer hospital stays, and readmissions when compared with transfemoral TAVR.”
Overall, there were 2,667 readmissions reported, among which high volume hospitals reported a 30-day readmission rate of 15.6%, while low- and medium-volume hospitals reported similarly higher rates of 19.5% and 19%.
When looking into the causes for these readmissions, the investigators found that 1,619 (61%) were due to noncardiac causes, which appeared in all three hospitals, despite a larger proportion present in low-volume hospitals as opposed to medium and high-volume hospitals (65.6% vs. 60.1% and 60.6%, respectively).
“Infection, respiratory, endocrine/metabolic, renal, and trauma problems were more common in low-volume hospitals,” according to the researchers. “Whereas gastrointestinal and TIA/stroke issues were more common in medium and high volume hospitals.”
While price and length of stay did not differ among the volume categories, the investigators estimate the lower rate of readmissions saved high-volume hospitals approximately $6.5 million.
They found that while the difference of readmissions between hospital classifications narrowed when controlling for experience, the margin was still significant. They admitted, however, that the possibility of greater access to more technologically advanced TAVR in high-volume hospitals may affect the findings.
This study was limited by administrative nature of the database used, which does not make available information such as valve type, patient risk scores, or medications.
One investigator has received personal fees from Edwards Lifesciences and Medtronic; another has received grants and personal fees from various pharmaceutical companies, educational institutions, and publications; and a third has consulted for Medtronic.
[email protected]
On Twitter @eaztweets
FROM JAMA CARDIOLOGY
Key clinical point:
Major finding: Hospitals that performed more than 100 TAVR procedures reported significantly lower 30-day readmission rates, compared with those that performed 50-100 procedures and hospitals that performed less than 50.
Data source: Observational study of 129 hospitals that performed at least five TAVRs in 2015, and documents gathered from the 2014 Nationwide Readmissions Database.
Disclosures: One investigator has received personal fees from Edwards Lifesciences and Medtronic; another has received grants and personal fees from various pharmaceutical companies, educational institutions, and publications; and a third has consulted for Medtronic.