User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
HBV birth dose predicts vaccine adherence
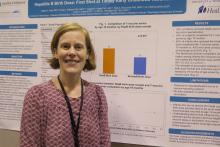
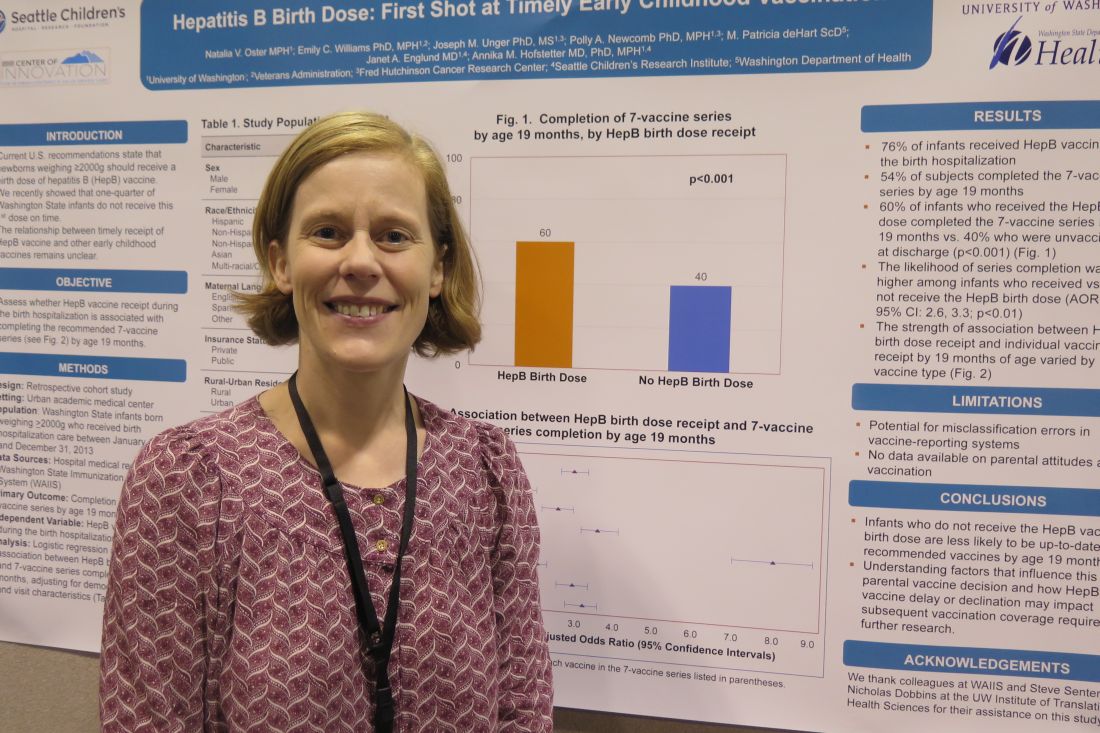
TORONTO – Infants who do not receive the hepatitis B vaccine birth dose are less likely to be up-to-date recipients of recommended vaccines by 19 months, based on results from a retrospective study of more than 9,000 infants.
“As pediatricians, we should be mindful of that when we are meeting families after the birth hospitalization and start a conversation at that point around vaccines,” one of the study authors, Annika M. Hofstetter, MD, PhD, said in an interview at the Pediatric Academic Societies meeting.
Of the 9,080 infants, 51% were male, 49% were non-Hispanic white, 56% were covered by public health insurance, and 47% stayed in the hospital for 48 hours or longer. The researchers reported that 76% infants received the HBV during the birth hospitalization, and 54% of subjects completed the seven-vaccine series by age 19 months. They also found that (P less than .001). Infants who received the HBV birth dose were 2.9 times more likely to complete the seven-vaccine series by age 19 months, compared with those who did not receive the HBV birth dose.
“Parents are making their first vaccine decision during that birth hospitalization,” said Dr. Hofstetter, who also conducts immunization research studies at Seattle Children’s Research Institute. “It’s unclear what underlies this decision, such as specific parent concerns or the way in which we as providers in the hospital are communicating vaccine information to the families. It’s telling, and it will be interesting to further explore the factors that are determining whether a family gets the vaccine during the birth hospitalization or not, and how we as a pediatric community can start having effective vaccine conversations earlier.”
She acknowledged certain limitations of the study, including the potential for misclassification errors in vaccine reporting systems and the fact that no data were available on parental attitudes about vaccination. The researchers reported having no financial disclosures.
TORONTO – Infants who do not receive the hepatitis B vaccine birth dose are less likely to be up-to-date recipients of recommended vaccines by 19 months, based on results from a retrospective study of more than 9,000 infants.
“As pediatricians, we should be mindful of that when we are meeting families after the birth hospitalization and start a conversation at that point around vaccines,” one of the study authors, Annika M. Hofstetter, MD, PhD, said in an interview at the Pediatric Academic Societies meeting.
Of the 9,080 infants, 51% were male, 49% were non-Hispanic white, 56% were covered by public health insurance, and 47% stayed in the hospital for 48 hours or longer. The researchers reported that 76% infants received the HBV during the birth hospitalization, and 54% of subjects completed the seven-vaccine series by age 19 months. They also found that (P less than .001). Infants who received the HBV birth dose were 2.9 times more likely to complete the seven-vaccine series by age 19 months, compared with those who did not receive the HBV birth dose.
“Parents are making their first vaccine decision during that birth hospitalization,” said Dr. Hofstetter, who also conducts immunization research studies at Seattle Children’s Research Institute. “It’s unclear what underlies this decision, such as specific parent concerns or the way in which we as providers in the hospital are communicating vaccine information to the families. It’s telling, and it will be interesting to further explore the factors that are determining whether a family gets the vaccine during the birth hospitalization or not, and how we as a pediatric community can start having effective vaccine conversations earlier.”
She acknowledged certain limitations of the study, including the potential for misclassification errors in vaccine reporting systems and the fact that no data were available on parental attitudes about vaccination. The researchers reported having no financial disclosures.
TORONTO – Infants who do not receive the hepatitis B vaccine birth dose are less likely to be up-to-date recipients of recommended vaccines by 19 months, based on results from a retrospective study of more than 9,000 infants.
“As pediatricians, we should be mindful of that when we are meeting families after the birth hospitalization and start a conversation at that point around vaccines,” one of the study authors, Annika M. Hofstetter, MD, PhD, said in an interview at the Pediatric Academic Societies meeting.
Of the 9,080 infants, 51% were male, 49% were non-Hispanic white, 56% were covered by public health insurance, and 47% stayed in the hospital for 48 hours or longer. The researchers reported that 76% infants received the HBV during the birth hospitalization, and 54% of subjects completed the seven-vaccine series by age 19 months. They also found that (P less than .001). Infants who received the HBV birth dose were 2.9 times more likely to complete the seven-vaccine series by age 19 months, compared with those who did not receive the HBV birth dose.
“Parents are making their first vaccine decision during that birth hospitalization,” said Dr. Hofstetter, who also conducts immunization research studies at Seattle Children’s Research Institute. “It’s unclear what underlies this decision, such as specific parent concerns or the way in which we as providers in the hospital are communicating vaccine information to the families. It’s telling, and it will be interesting to further explore the factors that are determining whether a family gets the vaccine during the birth hospitalization or not, and how we as a pediatric community can start having effective vaccine conversations earlier.”
She acknowledged certain limitations of the study, including the potential for misclassification errors in vaccine reporting systems and the fact that no data were available on parental attitudes about vaccination. The researchers reported having no financial disclosures.
AT PAS 2018
Key clinical point: Likelihood of completing the 7-vaccine series at 19 months was higher among infants who received the HBV birth dose.
Major finding: Infants who received the HBV birth dose were 2.9 times more likely to complete the 7-vaccine series by age 19 months, compared with those who did not receive the HBV birth dose.
Study details: A retrospective review of 9,080 infants born weighing at least 2,000 grams who received hospitalization care between January 1, 2008 and December 31, 2013.
Disclosures: The researchers reported having no financial disclosures.
Drug-related deaths continue to rise in United States
TORONTO – Drug-related deaths in America are rising faster than ever.
Rear Adm. Wanda D. Barfield, MD shared recent data from the U.S. National Center for Health Statistics on people aged 15 years and older at the Pediatric Academic Societies annual meeting. Between 1999 and 2016, for example, the number of drug overdose deaths rose more than threefold, from 6.1/100,000 standard population in 1999 to 19.8/100,000 in 2016. For males, the rate increased from 8.2/100,000 in 1999 to 26.2/100,000 in 2016. For females, the rate increased from 3.9/100,000 in 1999 to 13.4/100,000 in 2016.
Dr. Barfield, director of the division of reproductive health at the Centers for Disease Control and Prevention, said that in 2016, the NCHS also found that 22 states and the District of Columbia had drug overdoses that were significantly higher than the national average. The states with the highest number of drug overdose deaths were the District of Columbia, New Hampshire, Pennsylvania, and West Virginia while the states with the lowest observed rates were Nebraska, North Dakota, South Dakota, and Texas.
“Many of these drug overdose deaths are linked to opioids, but not exclusively,” Dr. Barfield said. “In the past, the overall opioid-related overdose deaths were mainly attributed to commonly prescribed opioid medications. However, in recent years, we’re seeing more deaths due to illicit drugs such as heroin and fentanyl.”
The NCHS found that the age-adjusted rate for drug overdose deaths involving synthetic opioids other than methadone doubled from 2015 to 2016, and that drug overdose deaths involving synthetic opioids other than methadone increased from 0.3/100,000 in 1999 to 6.2/100,000 in 2016. The rate increased an average of 18% per year from 1999 to 2006, remained steady from 2006 to 2013, but increased by 88% per year from 2013 to 2016. At the same time, drug overdose deaths involving heroin increased from 0.7/100,000 in 1999 to 1/100,000 in 2010, to 4.9/100,000 in 2016.
According to Dr. Barfield, the spike in opioid use since 1999 stems directly from increased prescribing rates. “In 2015, the number of opioids prescribed was enough so that every American could be medicated around the clock for 3 weeks,” she said. “In addition to the number of prescriptions, the average day’s supply of prescription opioids increased from 2006 to 2015, from 13.3 days in 2006 to 17.7 days in 2015.” What’s more, a recent CDC Vital Signs found that the amount of opioids prescribed per person varied widely among U.S. counties in 2015. “The wide variation among counties suggests a lack of consistency among providers when prescribing opioids,” Dr. Barfield said. “It’s concerning, as higher opioid prescribing puts patients at risk for addiction.”
At the same time, opioid overdose ED visits continue to rise. Data from the CDC’s National Syndromic Surveillance Program found that from July 2016 to September 2017, opioid overdose ED visits increased by 30% for men, by 24% for women, and for all adult age groups (31% among those aged 25-34 years, 36% among those aged 35-54 years, and 32% among those aged 55 years and older).
There’s a problem of prescription opioid use among pregnant women. Published estimates indicate that 14%-22% of women filled an opioid prescription during pregnancy, Dr. Barfield said. Among pregnant women, the prevalence of maternal opioid use or dependence during hospitalization for delivery has increased 127%, from 1.7 /1,000 delivery admissions in 1998 to 3.9/1,000 delivery admissions in 2011 (Anesthesiology 2014;121[6]:1158-65). There also has been a significant increase in neonatal abstinence syndrome (NAS), which is most commonly attributed to opioid exposure during pregnancy, from 1.2/1,000 U.S. hospital births in 2000 to 8/1,000 U.S. hospital births in 2014. “NAS is still on the rise,” Dr. Barfield said. “In 2012, we saw one baby with NAS born every 25 minutes. In 2014, that number jumped to one baby born with NAS every 15 minutes. That means about 96 infants with NAS are born daily,” she said. “Where do you think we’re going to be when we look at 2018 data?”
Role for pediatricians
Dr. Barfield closed her presentation by underscoring the role pediatricians play in counseling patients about opioid abuse or dependence during pregnancy. “We know that providers have a tremendous impact on patients and their families,” she said. “We also know that issues leading to a newborn having NAS are complex, so adopting a public health approach focused on prevention, expansion of treatment, and improvements in child welfare systems is vital.” Specifically, she said, health care providers can “bridge the gap” between clinical care and public health; lead in their communities, not just within their hospital or practice; work as a team member with colleagues in other fields of medicine such as obstetrics, family medicine, and addiction care when caring for infants with NAS, and by considering the social determinants of health.
“One way to adopt a public health perspective is to remember that the health of the fetus and baby rely on more than just prenatal care,” Dr. Barfield said. “We’re all part of a larger whole, surrounded by our families, communities, regions, state, and even our countries of origin. What’s going on with the mom, her family, and the larger community impacts the baby’s health. In other words, the social determinants of health matter, and are an important part of the conversation on NAS.”
She reported having no financial disclosures.
TORONTO – Drug-related deaths in America are rising faster than ever.
Rear Adm. Wanda D. Barfield, MD shared recent data from the U.S. National Center for Health Statistics on people aged 15 years and older at the Pediatric Academic Societies annual meeting. Between 1999 and 2016, for example, the number of drug overdose deaths rose more than threefold, from 6.1/100,000 standard population in 1999 to 19.8/100,000 in 2016. For males, the rate increased from 8.2/100,000 in 1999 to 26.2/100,000 in 2016. For females, the rate increased from 3.9/100,000 in 1999 to 13.4/100,000 in 2016.
Dr. Barfield, director of the division of reproductive health at the Centers for Disease Control and Prevention, said that in 2016, the NCHS also found that 22 states and the District of Columbia had drug overdoses that were significantly higher than the national average. The states with the highest number of drug overdose deaths were the District of Columbia, New Hampshire, Pennsylvania, and West Virginia while the states with the lowest observed rates were Nebraska, North Dakota, South Dakota, and Texas.
“Many of these drug overdose deaths are linked to opioids, but not exclusively,” Dr. Barfield said. “In the past, the overall opioid-related overdose deaths were mainly attributed to commonly prescribed opioid medications. However, in recent years, we’re seeing more deaths due to illicit drugs such as heroin and fentanyl.”
The NCHS found that the age-adjusted rate for drug overdose deaths involving synthetic opioids other than methadone doubled from 2015 to 2016, and that drug overdose deaths involving synthetic opioids other than methadone increased from 0.3/100,000 in 1999 to 6.2/100,000 in 2016. The rate increased an average of 18% per year from 1999 to 2006, remained steady from 2006 to 2013, but increased by 88% per year from 2013 to 2016. At the same time, drug overdose deaths involving heroin increased from 0.7/100,000 in 1999 to 1/100,000 in 2010, to 4.9/100,000 in 2016.
According to Dr. Barfield, the spike in opioid use since 1999 stems directly from increased prescribing rates. “In 2015, the number of opioids prescribed was enough so that every American could be medicated around the clock for 3 weeks,” she said. “In addition to the number of prescriptions, the average day’s supply of prescription opioids increased from 2006 to 2015, from 13.3 days in 2006 to 17.7 days in 2015.” What’s more, a recent CDC Vital Signs found that the amount of opioids prescribed per person varied widely among U.S. counties in 2015. “The wide variation among counties suggests a lack of consistency among providers when prescribing opioids,” Dr. Barfield said. “It’s concerning, as higher opioid prescribing puts patients at risk for addiction.”
At the same time, opioid overdose ED visits continue to rise. Data from the CDC’s National Syndromic Surveillance Program found that from July 2016 to September 2017, opioid overdose ED visits increased by 30% for men, by 24% for women, and for all adult age groups (31% among those aged 25-34 years, 36% among those aged 35-54 years, and 32% among those aged 55 years and older).
There’s a problem of prescription opioid use among pregnant women. Published estimates indicate that 14%-22% of women filled an opioid prescription during pregnancy, Dr. Barfield said. Among pregnant women, the prevalence of maternal opioid use or dependence during hospitalization for delivery has increased 127%, from 1.7 /1,000 delivery admissions in 1998 to 3.9/1,000 delivery admissions in 2011 (Anesthesiology 2014;121[6]:1158-65). There also has been a significant increase in neonatal abstinence syndrome (NAS), which is most commonly attributed to opioid exposure during pregnancy, from 1.2/1,000 U.S. hospital births in 2000 to 8/1,000 U.S. hospital births in 2014. “NAS is still on the rise,” Dr. Barfield said. “In 2012, we saw one baby with NAS born every 25 minutes. In 2014, that number jumped to one baby born with NAS every 15 minutes. That means about 96 infants with NAS are born daily,” she said. “Where do you think we’re going to be when we look at 2018 data?”
Role for pediatricians
Dr. Barfield closed her presentation by underscoring the role pediatricians play in counseling patients about opioid abuse or dependence during pregnancy. “We know that providers have a tremendous impact on patients and their families,” she said. “We also know that issues leading to a newborn having NAS are complex, so adopting a public health approach focused on prevention, expansion of treatment, and improvements in child welfare systems is vital.” Specifically, she said, health care providers can “bridge the gap” between clinical care and public health; lead in their communities, not just within their hospital or practice; work as a team member with colleagues in other fields of medicine such as obstetrics, family medicine, and addiction care when caring for infants with NAS, and by considering the social determinants of health.
“One way to adopt a public health perspective is to remember that the health of the fetus and baby rely on more than just prenatal care,” Dr. Barfield said. “We’re all part of a larger whole, surrounded by our families, communities, regions, state, and even our countries of origin. What’s going on with the mom, her family, and the larger community impacts the baby’s health. In other words, the social determinants of health matter, and are an important part of the conversation on NAS.”
She reported having no financial disclosures.
TORONTO – Drug-related deaths in America are rising faster than ever.
Rear Adm. Wanda D. Barfield, MD shared recent data from the U.S. National Center for Health Statistics on people aged 15 years and older at the Pediatric Academic Societies annual meeting. Between 1999 and 2016, for example, the number of drug overdose deaths rose more than threefold, from 6.1/100,000 standard population in 1999 to 19.8/100,000 in 2016. For males, the rate increased from 8.2/100,000 in 1999 to 26.2/100,000 in 2016. For females, the rate increased from 3.9/100,000 in 1999 to 13.4/100,000 in 2016.
Dr. Barfield, director of the division of reproductive health at the Centers for Disease Control and Prevention, said that in 2016, the NCHS also found that 22 states and the District of Columbia had drug overdoses that were significantly higher than the national average. The states with the highest number of drug overdose deaths were the District of Columbia, New Hampshire, Pennsylvania, and West Virginia while the states with the lowest observed rates were Nebraska, North Dakota, South Dakota, and Texas.
“Many of these drug overdose deaths are linked to opioids, but not exclusively,” Dr. Barfield said. “In the past, the overall opioid-related overdose deaths were mainly attributed to commonly prescribed opioid medications. However, in recent years, we’re seeing more deaths due to illicit drugs such as heroin and fentanyl.”
The NCHS found that the age-adjusted rate for drug overdose deaths involving synthetic opioids other than methadone doubled from 2015 to 2016, and that drug overdose deaths involving synthetic opioids other than methadone increased from 0.3/100,000 in 1999 to 6.2/100,000 in 2016. The rate increased an average of 18% per year from 1999 to 2006, remained steady from 2006 to 2013, but increased by 88% per year from 2013 to 2016. At the same time, drug overdose deaths involving heroin increased from 0.7/100,000 in 1999 to 1/100,000 in 2010, to 4.9/100,000 in 2016.
According to Dr. Barfield, the spike in opioid use since 1999 stems directly from increased prescribing rates. “In 2015, the number of opioids prescribed was enough so that every American could be medicated around the clock for 3 weeks,” she said. “In addition to the number of prescriptions, the average day’s supply of prescription opioids increased from 2006 to 2015, from 13.3 days in 2006 to 17.7 days in 2015.” What’s more, a recent CDC Vital Signs found that the amount of opioids prescribed per person varied widely among U.S. counties in 2015. “The wide variation among counties suggests a lack of consistency among providers when prescribing opioids,” Dr. Barfield said. “It’s concerning, as higher opioid prescribing puts patients at risk for addiction.”
At the same time, opioid overdose ED visits continue to rise. Data from the CDC’s National Syndromic Surveillance Program found that from July 2016 to September 2017, opioid overdose ED visits increased by 30% for men, by 24% for women, and for all adult age groups (31% among those aged 25-34 years, 36% among those aged 35-54 years, and 32% among those aged 55 years and older).
There’s a problem of prescription opioid use among pregnant women. Published estimates indicate that 14%-22% of women filled an opioid prescription during pregnancy, Dr. Barfield said. Among pregnant women, the prevalence of maternal opioid use or dependence during hospitalization for delivery has increased 127%, from 1.7 /1,000 delivery admissions in 1998 to 3.9/1,000 delivery admissions in 2011 (Anesthesiology 2014;121[6]:1158-65). There also has been a significant increase in neonatal abstinence syndrome (NAS), which is most commonly attributed to opioid exposure during pregnancy, from 1.2/1,000 U.S. hospital births in 2000 to 8/1,000 U.S. hospital births in 2014. “NAS is still on the rise,” Dr. Barfield said. “In 2012, we saw one baby with NAS born every 25 minutes. In 2014, that number jumped to one baby born with NAS every 15 minutes. That means about 96 infants with NAS are born daily,” she said. “Where do you think we’re going to be when we look at 2018 data?”
Role for pediatricians
Dr. Barfield closed her presentation by underscoring the role pediatricians play in counseling patients about opioid abuse or dependence during pregnancy. “We know that providers have a tremendous impact on patients and their families,” she said. “We also know that issues leading to a newborn having NAS are complex, so adopting a public health approach focused on prevention, expansion of treatment, and improvements in child welfare systems is vital.” Specifically, she said, health care providers can “bridge the gap” between clinical care and public health; lead in their communities, not just within their hospital or practice; work as a team member with colleagues in other fields of medicine such as obstetrics, family medicine, and addiction care when caring for infants with NAS, and by considering the social determinants of health.
“One way to adopt a public health perspective is to remember that the health of the fetus and baby rely on more than just prenatal care,” Dr. Barfield said. “We’re all part of a larger whole, surrounded by our families, communities, regions, state, and even our countries of origin. What’s going on with the mom, her family, and the larger community impacts the baby’s health. In other words, the social determinants of health matter, and are an important part of the conversation on NAS.”
She reported having no financial disclosures.
EXPERT ANALYSIS FROM PAS 2018
Simple QI intervention helped improve HPV vaccination rates
TORONTO – Teaching simple quality improvement principles to individual pediatric practices can improve adolescent human papillomavirus (HPV) vaccination rates, results from a multicenter study showed.
“We know that HPV vaccination rates are low, and there have been many efforts to improve the vaccination rates nationwide,” one of the study authors, Manika Suryadevara, MD, said in an interview at the Pediatric Academic Societies meeting. “One reason that vaccine rates are low in adolescents is missed opportunities. Adolescents don’t always show up for routine well-child visits where immunization records are reviewed, but they may show up with a cold, a sprained ankle, or a hospital follow-up. Providers do not routinely check immunizations at these visits, then don’t recommend vaccine to those who need it. These are the missed opportunities we need to act upon.”
Data were entered into the AAP Quality Improvement Data Aggregator and run charts were printed. Next, each practice held monthly team meetings for 5 months to discuss chart review data, run chart results, and to determine intervention change for the next cycle. “Most of the interventions included standing orders, optimizing nurse’s visits, using electronic medical reminders to review immunization records, and having immunization records pulled for all adolescents who show up in their practice,” Dr. Suryadevara said. “The goal of these systematic changes is to make the work flow seamless.”
Analysis of run chart data revealed that over the five monthly cycles, the HPV vaccine completion rate improved from 45% to 65%, while the overall HPV vaccine missed opportunities was reduced from 45% to 19%. Specifically, reductions in missed opportunities fell from 9% to 0% during well-child visits, from 80% to 61% during acute visits, from 25% to 0% during follow-up visits, and from 11% to 0% during nurse-only visits. “We did see missed opportunities for acute visits – those who come in sick, but even these missed opportunities decreased over the 6-month study period,” Dr. Suryadevara said.
During follow-up teleconference calls, practice representatives reported positive experiences about the QI process and outcome improvements. “Once the practices were able to pull everyone on board and develop practice changes, I wasn’t surprised that the interventions worked,” she said. “They were able to develop systematic interventions, change the work flow in their practice, and get the results we anticipated.”
The study was funded by the AAP Hub and Spoke Initiative. Dr. Suryadevara reported having no financial disclosures.
[email protected]
TORONTO – Teaching simple quality improvement principles to individual pediatric practices can improve adolescent human papillomavirus (HPV) vaccination rates, results from a multicenter study showed.
“We know that HPV vaccination rates are low, and there have been many efforts to improve the vaccination rates nationwide,” one of the study authors, Manika Suryadevara, MD, said in an interview at the Pediatric Academic Societies meeting. “One reason that vaccine rates are low in adolescents is missed opportunities. Adolescents don’t always show up for routine well-child visits where immunization records are reviewed, but they may show up with a cold, a sprained ankle, or a hospital follow-up. Providers do not routinely check immunizations at these visits, then don’t recommend vaccine to those who need it. These are the missed opportunities we need to act upon.”
Data were entered into the AAP Quality Improvement Data Aggregator and run charts were printed. Next, each practice held monthly team meetings for 5 months to discuss chart review data, run chart results, and to determine intervention change for the next cycle. “Most of the interventions included standing orders, optimizing nurse’s visits, using electronic medical reminders to review immunization records, and having immunization records pulled for all adolescents who show up in their practice,” Dr. Suryadevara said. “The goal of these systematic changes is to make the work flow seamless.”
Analysis of run chart data revealed that over the five monthly cycles, the HPV vaccine completion rate improved from 45% to 65%, while the overall HPV vaccine missed opportunities was reduced from 45% to 19%. Specifically, reductions in missed opportunities fell from 9% to 0% during well-child visits, from 80% to 61% during acute visits, from 25% to 0% during follow-up visits, and from 11% to 0% during nurse-only visits. “We did see missed opportunities for acute visits – those who come in sick, but even these missed opportunities decreased over the 6-month study period,” Dr. Suryadevara said.
During follow-up teleconference calls, practice representatives reported positive experiences about the QI process and outcome improvements. “Once the practices were able to pull everyone on board and develop practice changes, I wasn’t surprised that the interventions worked,” she said. “They were able to develop systematic interventions, change the work flow in their practice, and get the results we anticipated.”
The study was funded by the AAP Hub and Spoke Initiative. Dr. Suryadevara reported having no financial disclosures.
[email protected]
TORONTO – Teaching simple quality improvement principles to individual pediatric practices can improve adolescent human papillomavirus (HPV) vaccination rates, results from a multicenter study showed.
“We know that HPV vaccination rates are low, and there have been many efforts to improve the vaccination rates nationwide,” one of the study authors, Manika Suryadevara, MD, said in an interview at the Pediatric Academic Societies meeting. “One reason that vaccine rates are low in adolescents is missed opportunities. Adolescents don’t always show up for routine well-child visits where immunization records are reviewed, but they may show up with a cold, a sprained ankle, or a hospital follow-up. Providers do not routinely check immunizations at these visits, then don’t recommend vaccine to those who need it. These are the missed opportunities we need to act upon.”
Data were entered into the AAP Quality Improvement Data Aggregator and run charts were printed. Next, each practice held monthly team meetings for 5 months to discuss chart review data, run chart results, and to determine intervention change for the next cycle. “Most of the interventions included standing orders, optimizing nurse’s visits, using electronic medical reminders to review immunization records, and having immunization records pulled for all adolescents who show up in their practice,” Dr. Suryadevara said. “The goal of these systematic changes is to make the work flow seamless.”
Analysis of run chart data revealed that over the five monthly cycles, the HPV vaccine completion rate improved from 45% to 65%, while the overall HPV vaccine missed opportunities was reduced from 45% to 19%. Specifically, reductions in missed opportunities fell from 9% to 0% during well-child visits, from 80% to 61% during acute visits, from 25% to 0% during follow-up visits, and from 11% to 0% during nurse-only visits. “We did see missed opportunities for acute visits – those who come in sick, but even these missed opportunities decreased over the 6-month study period,” Dr. Suryadevara said.
During follow-up teleconference calls, practice representatives reported positive experiences about the QI process and outcome improvements. “Once the practices were able to pull everyone on board and develop practice changes, I wasn’t surprised that the interventions worked,” she said. “They were able to develop systematic interventions, change the work flow in their practice, and get the results we anticipated.”
The study was funded by the AAP Hub and Spoke Initiative. Dr. Suryadevara reported having no financial disclosures.
[email protected]
REPORTING FROM PAS 2018
Key clinical point: Teaching quality improvement to pediatric practices can improve adolescent human papillomavirus (HPV) vaccine completion rates.
Major finding:
Study details: A quality improvement project conducted at five large pediatric practices in New York state aimed at reducing missed vaccination opportunities in an effort to improve HPV vaccination completion rates.
Disclosures: The study was funded by the American Academy of Pediatrics Hub and Spoke Initiative. Dr. Suryadevara reported having no financial disclosures.
Which infants with invasive bacterial infections are at risk for adverse outcomes?
TORONTO – Among infants up to 60 days old with an invasive bacterial infection, adverse outcomes are associated with prematurity, ill appearance, and bacterial meningitis, a multicenter retrospective analysis found.
“Young infants are susceptible to serious bacterial infections, particularly when they’re less than 60 days of age,” Christopher Pruitt, MD, said at the annual Pediatric Academic Societies meeting. “Among these infants, bacteremia and bacterial meningitis, also referred to as invasive bacterial infections, are associated with higher rates of morbidity and mortality.”
The primary outcome measure was occurrence of an adverse clinical outcome within 30 days following the index ED visit. Adverse outcomes were defined as use of mechanical ventilation, vasoactive medications, any neurologic sequelae, and death. The researchers used a mixed-effects logistic regression model and retained covariates with a P value of less than .10. Covariates analyzed included age less than 28 days, prematurity, presence or absence of a complex chronic condition, presence of fever, ill appearance, bacterial meningitis, and concordant empiric antimicrobial therapy.
Of the 442 infants included in the final analysis, the majority (80%) had bacteremia, 14% had bacterial meningitis plus bacteremia, and 6% had bacterial meningitis only. “For purposes of this study, patients with bacterial meningitis with or without bacteremia were categorized as having bacterial meningitis,” Dr. Pruitt said. He and his associates found that 14.5% of infants had one or more adverse outcomes. Adverse outcomes occurred in 39% of infants with bacterial meningitis, compared with 8.2% of infants with isolated bacteremia. Need for mechanical ventilation, vasoactive medications, and neurologic disability also was more common among infants with bacterial meningitis than it was among children with isolated bacteremia. There were 10 deaths overall, which amounted to about 2% in both groups.
On multivariate analysis, the rate of adverse outcomes was significantly higher for patients with bacterial meningitis than it was for those with isolated bacteremia (adjusted odds ratio, 8.8), for premature versus term infants (AOR, 5.9), for infants who were ill appearing versus non-ill appearing (AOR, 3.9), and for infants with no fever versus those with fever (AOR, 2.4). No significant associations with 30-day adverse outcomes were seen in patients with a complex chronic condition, compared with those without a complex chronic condition (AOR, 2.0), nor in the those aged 29-60 days versus those younger than 29 days (15% vs. 14%, respectively; AOR 0.7).
“When looking at the most common scenario – a full-term infant without an ill appearance, and bacteremia as opposed to bacterial meningitis – 3 of these 219 infants, or 1.4%, had an adverse outcome,” said Dr. Pruitt, who cares for patients in the ED at Children’s of Alabama in Birmingham. “And there were no deaths.” He also reported that 12 infants with invasive bacterial infections were discharged from the index ED visit without antimicrobial treatment. All had bacteremia and none had an adverse outcome.
Dr. Pruitt acknowledged certain limitations of the study, including its retrospective design, that the outcomes were limited to 30 days, and the fact that the findings may not be generalizable to nontertiary settings. “Our findings have important implications for the care of infants with invasive bacterial infections,” he concluded. “In particular, the high rate of adverse outcomes for infants with bacterial meningitis can provide some context for clinicians in assessing the need for diagnostic evaluation for invasive bacterial infection and discussing testing and treatment with parents. Our findings may also help to inform inpatient management for hospitalized infants with invasive bacterial infections, as well as anticipatory guidance for parents, particularly around follow-up. Further prospective studies evaluating the long-term outcomes of infants with invasive bacterial infections are needed.”
The study was supported in part by a grant from the National Institutes of Health. Dr. Pruitt reported having no financial disclosures.
TORONTO – Among infants up to 60 days old with an invasive bacterial infection, adverse outcomes are associated with prematurity, ill appearance, and bacterial meningitis, a multicenter retrospective analysis found.
“Young infants are susceptible to serious bacterial infections, particularly when they’re less than 60 days of age,” Christopher Pruitt, MD, said at the annual Pediatric Academic Societies meeting. “Among these infants, bacteremia and bacterial meningitis, also referred to as invasive bacterial infections, are associated with higher rates of morbidity and mortality.”
The primary outcome measure was occurrence of an adverse clinical outcome within 30 days following the index ED visit. Adverse outcomes were defined as use of mechanical ventilation, vasoactive medications, any neurologic sequelae, and death. The researchers used a mixed-effects logistic regression model and retained covariates with a P value of less than .10. Covariates analyzed included age less than 28 days, prematurity, presence or absence of a complex chronic condition, presence of fever, ill appearance, bacterial meningitis, and concordant empiric antimicrobial therapy.
Of the 442 infants included in the final analysis, the majority (80%) had bacteremia, 14% had bacterial meningitis plus bacteremia, and 6% had bacterial meningitis only. “For purposes of this study, patients with bacterial meningitis with or without bacteremia were categorized as having bacterial meningitis,” Dr. Pruitt said. He and his associates found that 14.5% of infants had one or more adverse outcomes. Adverse outcomes occurred in 39% of infants with bacterial meningitis, compared with 8.2% of infants with isolated bacteremia. Need for mechanical ventilation, vasoactive medications, and neurologic disability also was more common among infants with bacterial meningitis than it was among children with isolated bacteremia. There were 10 deaths overall, which amounted to about 2% in both groups.
On multivariate analysis, the rate of adverse outcomes was significantly higher for patients with bacterial meningitis than it was for those with isolated bacteremia (adjusted odds ratio, 8.8), for premature versus term infants (AOR, 5.9), for infants who were ill appearing versus non-ill appearing (AOR, 3.9), and for infants with no fever versus those with fever (AOR, 2.4). No significant associations with 30-day adverse outcomes were seen in patients with a complex chronic condition, compared with those without a complex chronic condition (AOR, 2.0), nor in the those aged 29-60 days versus those younger than 29 days (15% vs. 14%, respectively; AOR 0.7).
“When looking at the most common scenario – a full-term infant without an ill appearance, and bacteremia as opposed to bacterial meningitis – 3 of these 219 infants, or 1.4%, had an adverse outcome,” said Dr. Pruitt, who cares for patients in the ED at Children’s of Alabama in Birmingham. “And there were no deaths.” He also reported that 12 infants with invasive bacterial infections were discharged from the index ED visit without antimicrobial treatment. All had bacteremia and none had an adverse outcome.
Dr. Pruitt acknowledged certain limitations of the study, including its retrospective design, that the outcomes were limited to 30 days, and the fact that the findings may not be generalizable to nontertiary settings. “Our findings have important implications for the care of infants with invasive bacterial infections,” he concluded. “In particular, the high rate of adverse outcomes for infants with bacterial meningitis can provide some context for clinicians in assessing the need for diagnostic evaluation for invasive bacterial infection and discussing testing and treatment with parents. Our findings may also help to inform inpatient management for hospitalized infants with invasive bacterial infections, as well as anticipatory guidance for parents, particularly around follow-up. Further prospective studies evaluating the long-term outcomes of infants with invasive bacterial infections are needed.”
The study was supported in part by a grant from the National Institutes of Health. Dr. Pruitt reported having no financial disclosures.
TORONTO – Among infants up to 60 days old with an invasive bacterial infection, adverse outcomes are associated with prematurity, ill appearance, and bacterial meningitis, a multicenter retrospective analysis found.
“Young infants are susceptible to serious bacterial infections, particularly when they’re less than 60 days of age,” Christopher Pruitt, MD, said at the annual Pediatric Academic Societies meeting. “Among these infants, bacteremia and bacterial meningitis, also referred to as invasive bacterial infections, are associated with higher rates of morbidity and mortality.”
The primary outcome measure was occurrence of an adverse clinical outcome within 30 days following the index ED visit. Adverse outcomes were defined as use of mechanical ventilation, vasoactive medications, any neurologic sequelae, and death. The researchers used a mixed-effects logistic regression model and retained covariates with a P value of less than .10. Covariates analyzed included age less than 28 days, prematurity, presence or absence of a complex chronic condition, presence of fever, ill appearance, bacterial meningitis, and concordant empiric antimicrobial therapy.
Of the 442 infants included in the final analysis, the majority (80%) had bacteremia, 14% had bacterial meningitis plus bacteremia, and 6% had bacterial meningitis only. “For purposes of this study, patients with bacterial meningitis with or without bacteremia were categorized as having bacterial meningitis,” Dr. Pruitt said. He and his associates found that 14.5% of infants had one or more adverse outcomes. Adverse outcomes occurred in 39% of infants with bacterial meningitis, compared with 8.2% of infants with isolated bacteremia. Need for mechanical ventilation, vasoactive medications, and neurologic disability also was more common among infants with bacterial meningitis than it was among children with isolated bacteremia. There were 10 deaths overall, which amounted to about 2% in both groups.
On multivariate analysis, the rate of adverse outcomes was significantly higher for patients with bacterial meningitis than it was for those with isolated bacteremia (adjusted odds ratio, 8.8), for premature versus term infants (AOR, 5.9), for infants who were ill appearing versus non-ill appearing (AOR, 3.9), and for infants with no fever versus those with fever (AOR, 2.4). No significant associations with 30-day adverse outcomes were seen in patients with a complex chronic condition, compared with those without a complex chronic condition (AOR, 2.0), nor in the those aged 29-60 days versus those younger than 29 days (15% vs. 14%, respectively; AOR 0.7).
“When looking at the most common scenario – a full-term infant without an ill appearance, and bacteremia as opposed to bacterial meningitis – 3 of these 219 infants, or 1.4%, had an adverse outcome,” said Dr. Pruitt, who cares for patients in the ED at Children’s of Alabama in Birmingham. “And there were no deaths.” He also reported that 12 infants with invasive bacterial infections were discharged from the index ED visit without antimicrobial treatment. All had bacteremia and none had an adverse outcome.
Dr. Pruitt acknowledged certain limitations of the study, including its retrospective design, that the outcomes were limited to 30 days, and the fact that the findings may not be generalizable to nontertiary settings. “Our findings have important implications for the care of infants with invasive bacterial infections,” he concluded. “In particular, the high rate of adverse outcomes for infants with bacterial meningitis can provide some context for clinicians in assessing the need for diagnostic evaluation for invasive bacterial infection and discussing testing and treatment with parents. Our findings may also help to inform inpatient management for hospitalized infants with invasive bacterial infections, as well as anticipatory guidance for parents, particularly around follow-up. Further prospective studies evaluating the long-term outcomes of infants with invasive bacterial infections are needed.”
The study was supported in part by a grant from the National Institutes of Health. Dr. Pruitt reported having no financial disclosures.
REPORTING FROM PAS 2018
Key clinical point:
Major finding: The rate of adverse outcomes was significantly higher for patients with bacterial meningitis versus those with isolated bacteremia (adjusted odds ratio, 8.8) and for premature versus term infants (AOR, 5.9).
Study details: A multicenter, retrospective review of 442 infants with invasive bacterial infections who were initially evaluated in the ED.
Disclosures: The study was supported in part by a grant from the National Institutes of Health. Dr. Pruitt reported having no financial disclosures.
Novel initiative aims to combat resident burnout
TORONTO – Studies have demonstrated that up to 50% of medical residents meet criteria for burnout, but a new initiative aims to change that worrisome trend.
At the Pediatric Academic Societies meeting, Michael Dolinger, MD, shared initial results from ResiLIEnCE (Resident-led Initiative to Empower a Change in Culture and Promote Resilience), a curriculum that is being carried out at Cohen Children’s Medical Center, New York. “We know that medical residents are a prime target for work burnout,” said Dr. Dolinger, one of the center’s pediatric chief residents, in an interview. “We wanted to study what we can do to combat that burnout on a daily basis, a monthly basis, and a longitudinal basis. How specific can we get so it’s portable, and that other programs can adapt what we are doing to help reduce this burnout?”
Interventions were enacted during traditional pediatric resident work hours to improve attendance. These included a resident-led wellness committee with faculty leadership and wellness champions, a longitudinal noon conference lecture series on nutrition (with topics such as how to eat on a budget and quick meal options), financial health (with topics such as student loan repayment, budgeting on a resident’s salary, and retirement planning), mindfulness, and resiliency. Optional activities after work included personal fitness boot camps, a book club, a minority support group, and other peer interest groups. Maslach Burnout Inventories were distributed to residents before implementation of the curriculum and at 3-month intervals. Surveys at the completion of activities assessed the effectiveness of sessions.
A total of 100 pediatric residents were surveyed. Dr. Dolinger reported that before implementation of the curriculum, 41.0% of third-year residents admitted to “feeling burned out from my work” and to “feeling more callous since I took this job,” while 8.8% of rising first-year residents admitted to feeling burned out prior to starting residency. In addition, 3 months after the curriculum began, 48.0% of first-year, 23.5% of second-year, and 83.3% of third-year residents reported believing that residency interfered with their personal wellness.
Analysis of the curriculum’s impact is ongoing, but Dr. Dolinger reported that among those who attended a nutrition series, 80% of residents planned to eat healthier, while only 15% reported eating healthy prior to the session. Among those who attended a financial series, 50% of those who did not previously contribute to their retirement planned to do so. In addition, 80% of residents who attended a resident fitness workshop joined a local fitness center, compared with only 20% of residents prior. Among those who attended a lecture series on resiliency, 90% of residents indicated that they were able to reflect on a negative patient experience and learn something valuable.
“Hopefully this curriculum helps reduce the overall burnout in our residents over time, by increasing their aspects of well-being and promoting resilience for them individually,” Dr. Dolinger said.
The initiative was funded by the Association of Pediatric Program Directors via the Harvey Aiges Memorial Trainee Investigator Award. Dr. Dolinger reported having no financial disclosures.
TORONTO – Studies have demonstrated that up to 50% of medical residents meet criteria for burnout, but a new initiative aims to change that worrisome trend.
At the Pediatric Academic Societies meeting, Michael Dolinger, MD, shared initial results from ResiLIEnCE (Resident-led Initiative to Empower a Change in Culture and Promote Resilience), a curriculum that is being carried out at Cohen Children’s Medical Center, New York. “We know that medical residents are a prime target for work burnout,” said Dr. Dolinger, one of the center’s pediatric chief residents, in an interview. “We wanted to study what we can do to combat that burnout on a daily basis, a monthly basis, and a longitudinal basis. How specific can we get so it’s portable, and that other programs can adapt what we are doing to help reduce this burnout?”
Interventions were enacted during traditional pediatric resident work hours to improve attendance. These included a resident-led wellness committee with faculty leadership and wellness champions, a longitudinal noon conference lecture series on nutrition (with topics such as how to eat on a budget and quick meal options), financial health (with topics such as student loan repayment, budgeting on a resident’s salary, and retirement planning), mindfulness, and resiliency. Optional activities after work included personal fitness boot camps, a book club, a minority support group, and other peer interest groups. Maslach Burnout Inventories were distributed to residents before implementation of the curriculum and at 3-month intervals. Surveys at the completion of activities assessed the effectiveness of sessions.
A total of 100 pediatric residents were surveyed. Dr. Dolinger reported that before implementation of the curriculum, 41.0% of third-year residents admitted to “feeling burned out from my work” and to “feeling more callous since I took this job,” while 8.8% of rising first-year residents admitted to feeling burned out prior to starting residency. In addition, 3 months after the curriculum began, 48.0% of first-year, 23.5% of second-year, and 83.3% of third-year residents reported believing that residency interfered with their personal wellness.
Analysis of the curriculum’s impact is ongoing, but Dr. Dolinger reported that among those who attended a nutrition series, 80% of residents planned to eat healthier, while only 15% reported eating healthy prior to the session. Among those who attended a financial series, 50% of those who did not previously contribute to their retirement planned to do so. In addition, 80% of residents who attended a resident fitness workshop joined a local fitness center, compared with only 20% of residents prior. Among those who attended a lecture series on resiliency, 90% of residents indicated that they were able to reflect on a negative patient experience and learn something valuable.
“Hopefully this curriculum helps reduce the overall burnout in our residents over time, by increasing their aspects of well-being and promoting resilience for them individually,” Dr. Dolinger said.
The initiative was funded by the Association of Pediatric Program Directors via the Harvey Aiges Memorial Trainee Investigator Award. Dr. Dolinger reported having no financial disclosures.
TORONTO – Studies have demonstrated that up to 50% of medical residents meet criteria for burnout, but a new initiative aims to change that worrisome trend.
At the Pediatric Academic Societies meeting, Michael Dolinger, MD, shared initial results from ResiLIEnCE (Resident-led Initiative to Empower a Change in Culture and Promote Resilience), a curriculum that is being carried out at Cohen Children’s Medical Center, New York. “We know that medical residents are a prime target for work burnout,” said Dr. Dolinger, one of the center’s pediatric chief residents, in an interview. “We wanted to study what we can do to combat that burnout on a daily basis, a monthly basis, and a longitudinal basis. How specific can we get so it’s portable, and that other programs can adapt what we are doing to help reduce this burnout?”
Interventions were enacted during traditional pediatric resident work hours to improve attendance. These included a resident-led wellness committee with faculty leadership and wellness champions, a longitudinal noon conference lecture series on nutrition (with topics such as how to eat on a budget and quick meal options), financial health (with topics such as student loan repayment, budgeting on a resident’s salary, and retirement planning), mindfulness, and resiliency. Optional activities after work included personal fitness boot camps, a book club, a minority support group, and other peer interest groups. Maslach Burnout Inventories were distributed to residents before implementation of the curriculum and at 3-month intervals. Surveys at the completion of activities assessed the effectiveness of sessions.
A total of 100 pediatric residents were surveyed. Dr. Dolinger reported that before implementation of the curriculum, 41.0% of third-year residents admitted to “feeling burned out from my work” and to “feeling more callous since I took this job,” while 8.8% of rising first-year residents admitted to feeling burned out prior to starting residency. In addition, 3 months after the curriculum began, 48.0% of first-year, 23.5% of second-year, and 83.3% of third-year residents reported believing that residency interfered with their personal wellness.
Analysis of the curriculum’s impact is ongoing, but Dr. Dolinger reported that among those who attended a nutrition series, 80% of residents planned to eat healthier, while only 15% reported eating healthy prior to the session. Among those who attended a financial series, 50% of those who did not previously contribute to their retirement planned to do so. In addition, 80% of residents who attended a resident fitness workshop joined a local fitness center, compared with only 20% of residents prior. Among those who attended a lecture series on resiliency, 90% of residents indicated that they were able to reflect on a negative patient experience and learn something valuable.
“Hopefully this curriculum helps reduce the overall burnout in our residents over time, by increasing their aspects of well-being and promoting resilience for them individually,” Dr. Dolinger said.
The initiative was funded by the Association of Pediatric Program Directors via the Harvey Aiges Memorial Trainee Investigator Award. Dr. Dolinger reported having no financial disclosures.
REPORTING FROM PAS 2018
Key clinical point: Interventions targeted at specific aspects of resident well-being yielded tangible improvement in resident wellness behaviors.
Major finding: Among those who attended a nutrition series as part of the curriculum, 80% of residents planned to eat healthier, while only 15% reported eating healthy prior to the session.
Study details: A survey of 100 pediatric residents who took part in a Resident-led Initiative to Empower a Change in Culture and Promote Resilience.
Disclosures: The initiative was funded by the Association of Pediatric Program Directors via the Harvey Aiges Memorial Trainee Investigator Award. Dr. Dolinger reported having no financial disclosures.
Multiple analgesia options for kids with acute pain
TORONTO – according to Naveen Poonai, MD, FRCPC.
“Too many times, nonpharmacologic therapies are relegated to the very last paragraph of recommendations or to the very bottom of a URL,” he said at the Pediatric Academic Societies meeting. “Nonpharmacologic therapies are things that our grandparents told us to do: common sense things that can be done at triage. They don’t require memorization of dosing, and most importantly, they don’t have side effects.”
When analgesia is indicated, clinicians can choose from a variety of agents in the postcodeine era. Dr. Poonai said that musculoskeletal injuries constitute 10-20% of pediatric emergency department visits, yet fewer than 60% of children receive adequate analgesia. “That’s what’s really important for patient and caregiver satisfaction,” he said.
Mounting evidence supports the use of ibuprofen as a go-to agent for mild to moderate pain in patients with musculoskeletal injuries, including results from a randomized, controlled multicenter trial of 500 youth (Canadian J Emerg Med. 2016:18:S29). “We know that ibuprofen is superior to acetaminophen or codeine and that it’s as good or better than oral opioids and with fewer side effects,” Dr. Poonai said, adding that it provides a 25 mm visual analog score (VAS) reduction in pain at 60 minutes. Another study that compared ibuprofen with codeine for acute pediatric arm fracture pain found that ibuprofen was associated with improved functioning and was at least as effective as acetaminophen plus codeine (Ann Emerg Med. 2009 Oct;54[4]:553-60).
A number of oral opioids have gained favor for use in children who present with acute pain. However, in a randomized trial, Dr. Poonai and his associates found no significant difference in analgesic efficacy between orally administered morphine and ibuprofen for the management of postfracture pain in 134 children (CMAJ. 2014 Dec 9;186[18]:1358-63). Oral morphine was also associated with more side effects. At the same time, tramadol and hydromorphone have not been well studied in children with musculoskeletal pain. “Currently, the use of hydromorphone is limited to children with sickle cell disease, but the use is branching out,” he said. “Oxycodone and oral morphine pose the greatest risk of side effects. The bottom line here is that opioids should be added to ibuprofen and acetaminophen rather than replacing them for mild to moderate pain.”
In 2014, a study from the Cochrane Database of Systematic Reviews concluded that intranasal fentanyl can be effective for the management of moderate to severe pain in children. A dose of 1.0-1.5 mcg/kg is associated with a 40-mm pain reduction in VAS at 10 minutes. “The benefits are that it is not an invasive approach, it’s been rigorously studied, and it is equivalent to IV morphine for moderate to severe pain,” said Dr. Poonai, who was not part of the Cochrane review. “It lasts about 60 minutes, with minimal side effects.”
A separate analysis found that intranasal fentanyl and ketamine were associated with similar pain reduction in children with moderate to severe pain from limb injury (Ann Emerg Med. 2015 Mar;65[3]:248-54.e1). Ketamine was associated with more minor adverse events. An intranasal dose of 1 mg/kg can cause a 40- to 45-mm reduction in VAS at 30 minutes.
Dr. Poonai went on to discuss treatment options for abdominal pain, noting that fewer than two-thirds of children with suspected appendicitis receive analgesia. “If they are receiving it, it’s often not until after the ultrasound is performed,” he said. “There is a still a reluctance toward providing opioid analgesia for a child with suspected appendicitis for fear of masking a diagnosis or leading to complications.” A systematic review led by Dr. Poonai found that the use of opioids in undifferentiated acute abdominal pain in children is associated with no difference in pain scores and an increased risk of mild side effects (Acad Emerg Med. 2014 21[11]:1183-92). However, there was no increased risk of perforation or abscess. “We found that single-dose IV opioids were actually beneficial,” he said.
Dr. Poonai characterized most of the current evidence on IV morphine for suspected appendicitis as being of low to moderate quality, “but they are generally favorable for the indication,” he said. “It is titratable to effect, and triage-initiated protocols improve timing and consistency of analgesia.” He reported having no financial disclosures.
TORONTO – according to Naveen Poonai, MD, FRCPC.
“Too many times, nonpharmacologic therapies are relegated to the very last paragraph of recommendations or to the very bottom of a URL,” he said at the Pediatric Academic Societies meeting. “Nonpharmacologic therapies are things that our grandparents told us to do: common sense things that can be done at triage. They don’t require memorization of dosing, and most importantly, they don’t have side effects.”
When analgesia is indicated, clinicians can choose from a variety of agents in the postcodeine era. Dr. Poonai said that musculoskeletal injuries constitute 10-20% of pediatric emergency department visits, yet fewer than 60% of children receive adequate analgesia. “That’s what’s really important for patient and caregiver satisfaction,” he said.
Mounting evidence supports the use of ibuprofen as a go-to agent for mild to moderate pain in patients with musculoskeletal injuries, including results from a randomized, controlled multicenter trial of 500 youth (Canadian J Emerg Med. 2016:18:S29). “We know that ibuprofen is superior to acetaminophen or codeine and that it’s as good or better than oral opioids and with fewer side effects,” Dr. Poonai said, adding that it provides a 25 mm visual analog score (VAS) reduction in pain at 60 minutes. Another study that compared ibuprofen with codeine for acute pediatric arm fracture pain found that ibuprofen was associated with improved functioning and was at least as effective as acetaminophen plus codeine (Ann Emerg Med. 2009 Oct;54[4]:553-60).
A number of oral opioids have gained favor for use in children who present with acute pain. However, in a randomized trial, Dr. Poonai and his associates found no significant difference in analgesic efficacy between orally administered morphine and ibuprofen for the management of postfracture pain in 134 children (CMAJ. 2014 Dec 9;186[18]:1358-63). Oral morphine was also associated with more side effects. At the same time, tramadol and hydromorphone have not been well studied in children with musculoskeletal pain. “Currently, the use of hydromorphone is limited to children with sickle cell disease, but the use is branching out,” he said. “Oxycodone and oral morphine pose the greatest risk of side effects. The bottom line here is that opioids should be added to ibuprofen and acetaminophen rather than replacing them for mild to moderate pain.”
In 2014, a study from the Cochrane Database of Systematic Reviews concluded that intranasal fentanyl can be effective for the management of moderate to severe pain in children. A dose of 1.0-1.5 mcg/kg is associated with a 40-mm pain reduction in VAS at 10 minutes. “The benefits are that it is not an invasive approach, it’s been rigorously studied, and it is equivalent to IV morphine for moderate to severe pain,” said Dr. Poonai, who was not part of the Cochrane review. “It lasts about 60 minutes, with minimal side effects.”
A separate analysis found that intranasal fentanyl and ketamine were associated with similar pain reduction in children with moderate to severe pain from limb injury (Ann Emerg Med. 2015 Mar;65[3]:248-54.e1). Ketamine was associated with more minor adverse events. An intranasal dose of 1 mg/kg can cause a 40- to 45-mm reduction in VAS at 30 minutes.
Dr. Poonai went on to discuss treatment options for abdominal pain, noting that fewer than two-thirds of children with suspected appendicitis receive analgesia. “If they are receiving it, it’s often not until after the ultrasound is performed,” he said. “There is a still a reluctance toward providing opioid analgesia for a child with suspected appendicitis for fear of masking a diagnosis or leading to complications.” A systematic review led by Dr. Poonai found that the use of opioids in undifferentiated acute abdominal pain in children is associated with no difference in pain scores and an increased risk of mild side effects (Acad Emerg Med. 2014 21[11]:1183-92). However, there was no increased risk of perforation or abscess. “We found that single-dose IV opioids were actually beneficial,” he said.
Dr. Poonai characterized most of the current evidence on IV morphine for suspected appendicitis as being of low to moderate quality, “but they are generally favorable for the indication,” he said. “It is titratable to effect, and triage-initiated protocols improve timing and consistency of analgesia.” He reported having no financial disclosures.
TORONTO – according to Naveen Poonai, MD, FRCPC.
“Too many times, nonpharmacologic therapies are relegated to the very last paragraph of recommendations or to the very bottom of a URL,” he said at the Pediatric Academic Societies meeting. “Nonpharmacologic therapies are things that our grandparents told us to do: common sense things that can be done at triage. They don’t require memorization of dosing, and most importantly, they don’t have side effects.”
When analgesia is indicated, clinicians can choose from a variety of agents in the postcodeine era. Dr. Poonai said that musculoskeletal injuries constitute 10-20% of pediatric emergency department visits, yet fewer than 60% of children receive adequate analgesia. “That’s what’s really important for patient and caregiver satisfaction,” he said.
Mounting evidence supports the use of ibuprofen as a go-to agent for mild to moderate pain in patients with musculoskeletal injuries, including results from a randomized, controlled multicenter trial of 500 youth (Canadian J Emerg Med. 2016:18:S29). “We know that ibuprofen is superior to acetaminophen or codeine and that it’s as good or better than oral opioids and with fewer side effects,” Dr. Poonai said, adding that it provides a 25 mm visual analog score (VAS) reduction in pain at 60 minutes. Another study that compared ibuprofen with codeine for acute pediatric arm fracture pain found that ibuprofen was associated with improved functioning and was at least as effective as acetaminophen plus codeine (Ann Emerg Med. 2009 Oct;54[4]:553-60).
A number of oral opioids have gained favor for use in children who present with acute pain. However, in a randomized trial, Dr. Poonai and his associates found no significant difference in analgesic efficacy between orally administered morphine and ibuprofen for the management of postfracture pain in 134 children (CMAJ. 2014 Dec 9;186[18]:1358-63). Oral morphine was also associated with more side effects. At the same time, tramadol and hydromorphone have not been well studied in children with musculoskeletal pain. “Currently, the use of hydromorphone is limited to children with sickle cell disease, but the use is branching out,” he said. “Oxycodone and oral morphine pose the greatest risk of side effects. The bottom line here is that opioids should be added to ibuprofen and acetaminophen rather than replacing them for mild to moderate pain.”
In 2014, a study from the Cochrane Database of Systematic Reviews concluded that intranasal fentanyl can be effective for the management of moderate to severe pain in children. A dose of 1.0-1.5 mcg/kg is associated with a 40-mm pain reduction in VAS at 10 minutes. “The benefits are that it is not an invasive approach, it’s been rigorously studied, and it is equivalent to IV morphine for moderate to severe pain,” said Dr. Poonai, who was not part of the Cochrane review. “It lasts about 60 minutes, with minimal side effects.”
A separate analysis found that intranasal fentanyl and ketamine were associated with similar pain reduction in children with moderate to severe pain from limb injury (Ann Emerg Med. 2015 Mar;65[3]:248-54.e1). Ketamine was associated with more minor adverse events. An intranasal dose of 1 mg/kg can cause a 40- to 45-mm reduction in VAS at 30 minutes.
Dr. Poonai went on to discuss treatment options for abdominal pain, noting that fewer than two-thirds of children with suspected appendicitis receive analgesia. “If they are receiving it, it’s often not until after the ultrasound is performed,” he said. “There is a still a reluctance toward providing opioid analgesia for a child with suspected appendicitis for fear of masking a diagnosis or leading to complications.” A systematic review led by Dr. Poonai found that the use of opioids in undifferentiated acute abdominal pain in children is associated with no difference in pain scores and an increased risk of mild side effects (Acad Emerg Med. 2014 21[11]:1183-92). However, there was no increased risk of perforation or abscess. “We found that single-dose IV opioids were actually beneficial,” he said.
Dr. Poonai characterized most of the current evidence on IV morphine for suspected appendicitis as being of low to moderate quality, “but they are generally favorable for the indication,” he said. “It is titratable to effect, and triage-initiated protocols improve timing and consistency of analgesia.” He reported having no financial disclosures.
EXPERT ANALYSIS FROM PAS 2018
Analysis finds inconsistent uptake of meningococcal B vaccines
TORONTO – results from a large analysis showed.
“In 2015, two meningococcal B (MenB) vaccines were given a Category B recommendation by the Advisory Committee on Immunization Practices with a preferred vaccination window of 16-18 years,” researchers led by Kristen A. Feemster, MD, MPH, wrote in an abstract presented at the Pediatric Academic Societies meeting. “Factors that may influence provider recommendation and subsequent uptake of a Category B vaccine are unknown.”
In an effort to identify sociodemographic and provider factors associated with MenB vaccine receipt, Dr. Feemster and her associates conducted a cross-sectional study of 85,789 Philadelphia youth aged 16-18 years who had a record in the KIDS Plus II Philadelphia database between Oct. 31, 2015 and July 31, 2017. They acquired neighborhood-level data from the 2016 U.S. Census American Community Survey. Next, the researchers used multivariate logistic regression to assess the association between MenB series initiation and individual- and neighborhood-level sociodemographic, clinical, and provider characteristics.
Of the 85,789 youth, only 16% received at least one MenB dose, while just 5% completed the series, reported Dr. Feemster, who is medical director of the Immunization Program and Acute Communicable Diseases at the Philadelphia department of public health in the division of disease control. Nearly half of youth (49%) were black or African-American, 25% were white, 5.5% were Asian, while the remainder were from “other” or “unknown” races. A private pediatrician was listed as the provider for 70% of the youth, followed by a community health center (11%), the Philadelphia District Center (7%), and hospitals (2%), while the remaining providers were “other” or “unknown.” The proportion of MenB recipients varied significantly by provider type, from 0.67% to 20%.
On multivariate logistic regression, MenB recipients were more likely to be female (adjusted odds ratio, 1.07; P = .0006); they were also more likely to be up-to-date on human papillomavirus vaccines (AOR, 1.65; P less than .0001) and measles-containing vaccines (AOR, 9.90; P less than .0001).
MenB recipients were more likely to be of “unknown” or “other” reported race, compared with those who were Black/African-American (AOR, 1.36 and 1.24, respectively; P less than .0001) or non-Hispanic/Latino (AOR, 1.21; P less than .0001); they were also more likely to reside in a neighborhood with median household income of greater than $100,000, compared with those who lived in a neighborhood where the median household income is less than $20,000 (AOR, 1.63; P less than .0001). Asian teens (AOR, 0.87; P = .0062) and teens who received care in community (AOR, 0.52; P less than .0001) or district health centers (AOR, 0.03; P less than .0001) also were less likely to receive the MenB vaccine, reported Dr. Feemster, who is also director of research for Children’s Hospital of Philadelphia’s Vaccine Education Center, and her colleagues.
“Variation in uptake by race, ethnicity, and neighborhood socioeconomic status suggest potential sociodemographic disparities in MenB receipt, [while] variation by neighborhood socioeconomic status may also suggest financial barriers related to access to care,” the researchers wrote in their abstract. They also speculated that variation in MenB receipt across different providers “may reflect different recommendation practices, perceived need for MenB vaccines in a provider’s patient population, or clinic-level purchasing decisions.”
The next steps in their research, they wrote, are to “investigate factors associated with provider recommendation of MenB vaccine to identify targets for initiatives to ensure equitable vaccine access.”
The researchers reported having no financial disclosures.
TORONTO – results from a large analysis showed.
“In 2015, two meningococcal B (MenB) vaccines were given a Category B recommendation by the Advisory Committee on Immunization Practices with a preferred vaccination window of 16-18 years,” researchers led by Kristen A. Feemster, MD, MPH, wrote in an abstract presented at the Pediatric Academic Societies meeting. “Factors that may influence provider recommendation and subsequent uptake of a Category B vaccine are unknown.”
In an effort to identify sociodemographic and provider factors associated with MenB vaccine receipt, Dr. Feemster and her associates conducted a cross-sectional study of 85,789 Philadelphia youth aged 16-18 years who had a record in the KIDS Plus II Philadelphia database between Oct. 31, 2015 and July 31, 2017. They acquired neighborhood-level data from the 2016 U.S. Census American Community Survey. Next, the researchers used multivariate logistic regression to assess the association between MenB series initiation and individual- and neighborhood-level sociodemographic, clinical, and provider characteristics.
Of the 85,789 youth, only 16% received at least one MenB dose, while just 5% completed the series, reported Dr. Feemster, who is medical director of the Immunization Program and Acute Communicable Diseases at the Philadelphia department of public health in the division of disease control. Nearly half of youth (49%) were black or African-American, 25% were white, 5.5% were Asian, while the remainder were from “other” or “unknown” races. A private pediatrician was listed as the provider for 70% of the youth, followed by a community health center (11%), the Philadelphia District Center (7%), and hospitals (2%), while the remaining providers were “other” or “unknown.” The proportion of MenB recipients varied significantly by provider type, from 0.67% to 20%.
On multivariate logistic regression, MenB recipients were more likely to be female (adjusted odds ratio, 1.07; P = .0006); they were also more likely to be up-to-date on human papillomavirus vaccines (AOR, 1.65; P less than .0001) and measles-containing vaccines (AOR, 9.90; P less than .0001).
MenB recipients were more likely to be of “unknown” or “other” reported race, compared with those who were Black/African-American (AOR, 1.36 and 1.24, respectively; P less than .0001) or non-Hispanic/Latino (AOR, 1.21; P less than .0001); they were also more likely to reside in a neighborhood with median household income of greater than $100,000, compared with those who lived in a neighborhood where the median household income is less than $20,000 (AOR, 1.63; P less than .0001). Asian teens (AOR, 0.87; P = .0062) and teens who received care in community (AOR, 0.52; P less than .0001) or district health centers (AOR, 0.03; P less than .0001) also were less likely to receive the MenB vaccine, reported Dr. Feemster, who is also director of research for Children’s Hospital of Philadelphia’s Vaccine Education Center, and her colleagues.
“Variation in uptake by race, ethnicity, and neighborhood socioeconomic status suggest potential sociodemographic disparities in MenB receipt, [while] variation by neighborhood socioeconomic status may also suggest financial barriers related to access to care,” the researchers wrote in their abstract. They also speculated that variation in MenB receipt across different providers “may reflect different recommendation practices, perceived need for MenB vaccines in a provider’s patient population, or clinic-level purchasing decisions.”
The next steps in their research, they wrote, are to “investigate factors associated with provider recommendation of MenB vaccine to identify targets for initiatives to ensure equitable vaccine access.”
The researchers reported having no financial disclosures.
TORONTO – results from a large analysis showed.
“In 2015, two meningococcal B (MenB) vaccines were given a Category B recommendation by the Advisory Committee on Immunization Practices with a preferred vaccination window of 16-18 years,” researchers led by Kristen A. Feemster, MD, MPH, wrote in an abstract presented at the Pediatric Academic Societies meeting. “Factors that may influence provider recommendation and subsequent uptake of a Category B vaccine are unknown.”
In an effort to identify sociodemographic and provider factors associated with MenB vaccine receipt, Dr. Feemster and her associates conducted a cross-sectional study of 85,789 Philadelphia youth aged 16-18 years who had a record in the KIDS Plus II Philadelphia database between Oct. 31, 2015 and July 31, 2017. They acquired neighborhood-level data from the 2016 U.S. Census American Community Survey. Next, the researchers used multivariate logistic regression to assess the association between MenB series initiation and individual- and neighborhood-level sociodemographic, clinical, and provider characteristics.
Of the 85,789 youth, only 16% received at least one MenB dose, while just 5% completed the series, reported Dr. Feemster, who is medical director of the Immunization Program and Acute Communicable Diseases at the Philadelphia department of public health in the division of disease control. Nearly half of youth (49%) were black or African-American, 25% were white, 5.5% were Asian, while the remainder were from “other” or “unknown” races. A private pediatrician was listed as the provider for 70% of the youth, followed by a community health center (11%), the Philadelphia District Center (7%), and hospitals (2%), while the remaining providers were “other” or “unknown.” The proportion of MenB recipients varied significantly by provider type, from 0.67% to 20%.
On multivariate logistic regression, MenB recipients were more likely to be female (adjusted odds ratio, 1.07; P = .0006); they were also more likely to be up-to-date on human papillomavirus vaccines (AOR, 1.65; P less than .0001) and measles-containing vaccines (AOR, 9.90; P less than .0001).
MenB recipients were more likely to be of “unknown” or “other” reported race, compared with those who were Black/African-American (AOR, 1.36 and 1.24, respectively; P less than .0001) or non-Hispanic/Latino (AOR, 1.21; P less than .0001); they were also more likely to reside in a neighborhood with median household income of greater than $100,000, compared with those who lived in a neighborhood where the median household income is less than $20,000 (AOR, 1.63; P less than .0001). Asian teens (AOR, 0.87; P = .0062) and teens who received care in community (AOR, 0.52; P less than .0001) or district health centers (AOR, 0.03; P less than .0001) also were less likely to receive the MenB vaccine, reported Dr. Feemster, who is also director of research for Children’s Hospital of Philadelphia’s Vaccine Education Center, and her colleagues.
“Variation in uptake by race, ethnicity, and neighborhood socioeconomic status suggest potential sociodemographic disparities in MenB receipt, [while] variation by neighborhood socioeconomic status may also suggest financial barriers related to access to care,” the researchers wrote in their abstract. They also speculated that variation in MenB receipt across different providers “may reflect different recommendation practices, perceived need for MenB vaccines in a provider’s patient population, or clinic-level purchasing decisions.”
The next steps in their research, they wrote, are to “investigate factors associated with provider recommendation of MenB vaccine to identify targets for initiatives to ensure equitable vaccine access.”
The researchers reported having no financial disclosures.
AT PAS 2018
Key clinical point: Significant variation in the likelihood of MenB vaccine receipt correlated with sociodemographic, clinical, and provider factors.
Major finding: Only 16% received at least one MenB dose while just 5% completed the series.
Study details: A cross-sectional study of 85,789 Philadelphia youth aged 16-18 years.
Disclosures: The researchers reported having no financial disclosures.
Pulsed-dye laser found effective for erythematotelangiectatic rosacea
DALLAS – in a single-center study of 20 patients.
“Recent advances in pulsed-dye laser technology enable 50% higher output energies and much longer dye life,” lead study author Eric F. Bernstein, MD, said at the annual conference of the American Society for Laser Medicine and Surgery. “A 15-mm treatment diameter is now possible, which makes treatment faster and possibly more effective due to increased penetration of laser energy. Compared with a 10-mm spot size, which most of us use, a 15 mm is a 125% larger beam diameter, so it’s a big difference in treatment area.”
Blinded assessment of digital and cross-polarized images taken 8 weeks following the last treatment was performed using an 11-point clearance scale. The Investigator Global Assessment Scale was used to evaluate inflammatory lesions, erythema, and telangiectasia, and safety was assessed by incidence and severity of side effects. The investigators and subjects assessed satisfaction with the treatment outcome on a 5-point Likert scale (–2, very dissatisfied; –1, dissatisfied; 0, no opinion; 1, satisfied; and 2, very satisfied). Dr. Bernstein also evaluated the patients for purpura, petechiae, edema, erythema, blistering, and crusting on a 0-3 point scale (0, absent; 1, mild; 2, moderate; and 3, severe).
Of the 20 subjects, 16 females and 3 males completed the study. All had Fitzpatrick skin types II-IV and 17 of 19 subjects received four treatments, while 2 received three treatments because of scheduling challenges. Between baseline and 8 weeks following the last treatment, mean Investigator Global Assessment scores improved significantly for overall score (from 4.3 to 1.8; P less than .0001), as well as for inflammatory lesions (from 1.7 to 1.0; P less than .005), erythema (from 4.5 to 1.6; P less than .0001), and for telangiectasia (from 4.2 to 1.1; P less than .0001).
Dr. Bernstein also reported that blinded evaluators correctly identified baseline images in 55 of 57 image pairs (96.5%), while the average score improvement in their rosacea was 52.5%, and ranged from 30.0% to 86.7%. In addition, 17 of 19 subjects (89%) showed a score improvement of more than 40%, while 57% of subjects had a score improvement of greater than 50%.
Patients and investigators both recorded a mean satisfaction score of 1.9, and 18 of 19 subjects reported being “very satisfied” with the treatment.
The average pain score was 5.6 on a 0-10 scale, while common side effects that resolved within 1-3 days without intervention included mild edema, mild to moderate erythema, and mild to moderate bruising. No cases of hyperpigmentation, hypopigmentation, blistering, or scarring occurred.
“The newly designed pulsed-dye laser is a major change in a device that has performed for over 10 years with wide acceptance,” Dr. Bernstein said. In addition to a longer-lasting dye kit, he said that new features include 50% more total energy enabling clinically relevant fluences to be delivered using a 15-mm diameter treatment beam, once-daily calibration instead of after every energy or spot size change, “both contact and dynamic spray cooling, and an Nd:YAG wavelength for treating larger vessels.”
Dr. Bernstein reported having received grant funding from Syneron Candela and Zeltiq. He also has received consulting fees from and holds ownership interest in Syneron Candela, and has served on the advisory board for Novoxel, Solta, Syneron Candela, and Zeltiq.
DALLAS – in a single-center study of 20 patients.
“Recent advances in pulsed-dye laser technology enable 50% higher output energies and much longer dye life,” lead study author Eric F. Bernstein, MD, said at the annual conference of the American Society for Laser Medicine and Surgery. “A 15-mm treatment diameter is now possible, which makes treatment faster and possibly more effective due to increased penetration of laser energy. Compared with a 10-mm spot size, which most of us use, a 15 mm is a 125% larger beam diameter, so it’s a big difference in treatment area.”
Blinded assessment of digital and cross-polarized images taken 8 weeks following the last treatment was performed using an 11-point clearance scale. The Investigator Global Assessment Scale was used to evaluate inflammatory lesions, erythema, and telangiectasia, and safety was assessed by incidence and severity of side effects. The investigators and subjects assessed satisfaction with the treatment outcome on a 5-point Likert scale (–2, very dissatisfied; –1, dissatisfied; 0, no opinion; 1, satisfied; and 2, very satisfied). Dr. Bernstein also evaluated the patients for purpura, petechiae, edema, erythema, blistering, and crusting on a 0-3 point scale (0, absent; 1, mild; 2, moderate; and 3, severe).
Of the 20 subjects, 16 females and 3 males completed the study. All had Fitzpatrick skin types II-IV and 17 of 19 subjects received four treatments, while 2 received three treatments because of scheduling challenges. Between baseline and 8 weeks following the last treatment, mean Investigator Global Assessment scores improved significantly for overall score (from 4.3 to 1.8; P less than .0001), as well as for inflammatory lesions (from 1.7 to 1.0; P less than .005), erythema (from 4.5 to 1.6; P less than .0001), and for telangiectasia (from 4.2 to 1.1; P less than .0001).
Dr. Bernstein also reported that blinded evaluators correctly identified baseline images in 55 of 57 image pairs (96.5%), while the average score improvement in their rosacea was 52.5%, and ranged from 30.0% to 86.7%. In addition, 17 of 19 subjects (89%) showed a score improvement of more than 40%, while 57% of subjects had a score improvement of greater than 50%.
Patients and investigators both recorded a mean satisfaction score of 1.9, and 18 of 19 subjects reported being “very satisfied” with the treatment.
The average pain score was 5.6 on a 0-10 scale, while common side effects that resolved within 1-3 days without intervention included mild edema, mild to moderate erythema, and mild to moderate bruising. No cases of hyperpigmentation, hypopigmentation, blistering, or scarring occurred.
“The newly designed pulsed-dye laser is a major change in a device that has performed for over 10 years with wide acceptance,” Dr. Bernstein said. In addition to a longer-lasting dye kit, he said that new features include 50% more total energy enabling clinically relevant fluences to be delivered using a 15-mm diameter treatment beam, once-daily calibration instead of after every energy or spot size change, “both contact and dynamic spray cooling, and an Nd:YAG wavelength for treating larger vessels.”
Dr. Bernstein reported having received grant funding from Syneron Candela and Zeltiq. He also has received consulting fees from and holds ownership interest in Syneron Candela, and has served on the advisory board for Novoxel, Solta, Syneron Candela, and Zeltiq.
DALLAS – in a single-center study of 20 patients.
“Recent advances in pulsed-dye laser technology enable 50% higher output energies and much longer dye life,” lead study author Eric F. Bernstein, MD, said at the annual conference of the American Society for Laser Medicine and Surgery. “A 15-mm treatment diameter is now possible, which makes treatment faster and possibly more effective due to increased penetration of laser energy. Compared with a 10-mm spot size, which most of us use, a 15 mm is a 125% larger beam diameter, so it’s a big difference in treatment area.”
Blinded assessment of digital and cross-polarized images taken 8 weeks following the last treatment was performed using an 11-point clearance scale. The Investigator Global Assessment Scale was used to evaluate inflammatory lesions, erythema, and telangiectasia, and safety was assessed by incidence and severity of side effects. The investigators and subjects assessed satisfaction with the treatment outcome on a 5-point Likert scale (–2, very dissatisfied; –1, dissatisfied; 0, no opinion; 1, satisfied; and 2, very satisfied). Dr. Bernstein also evaluated the patients for purpura, petechiae, edema, erythema, blistering, and crusting on a 0-3 point scale (0, absent; 1, mild; 2, moderate; and 3, severe).
Of the 20 subjects, 16 females and 3 males completed the study. All had Fitzpatrick skin types II-IV and 17 of 19 subjects received four treatments, while 2 received three treatments because of scheduling challenges. Between baseline and 8 weeks following the last treatment, mean Investigator Global Assessment scores improved significantly for overall score (from 4.3 to 1.8; P less than .0001), as well as for inflammatory lesions (from 1.7 to 1.0; P less than .005), erythema (from 4.5 to 1.6; P less than .0001), and for telangiectasia (from 4.2 to 1.1; P less than .0001).
Dr. Bernstein also reported that blinded evaluators correctly identified baseline images in 55 of 57 image pairs (96.5%), while the average score improvement in their rosacea was 52.5%, and ranged from 30.0% to 86.7%. In addition, 17 of 19 subjects (89%) showed a score improvement of more than 40%, while 57% of subjects had a score improvement of greater than 50%.
Patients and investigators both recorded a mean satisfaction score of 1.9, and 18 of 19 subjects reported being “very satisfied” with the treatment.
The average pain score was 5.6 on a 0-10 scale, while common side effects that resolved within 1-3 days without intervention included mild edema, mild to moderate erythema, and mild to moderate bruising. No cases of hyperpigmentation, hypopigmentation, blistering, or scarring occurred.
“The newly designed pulsed-dye laser is a major change in a device that has performed for over 10 years with wide acceptance,” Dr. Bernstein said. In addition to a longer-lasting dye kit, he said that new features include 50% more total energy enabling clinically relevant fluences to be delivered using a 15-mm diameter treatment beam, once-daily calibration instead of after every energy or spot size change, “both contact and dynamic spray cooling, and an Nd:YAG wavelength for treating larger vessels.”
Dr. Bernstein reported having received grant funding from Syneron Candela and Zeltiq. He also has received consulting fees from and holds ownership interest in Syneron Candela, and has served on the advisory board for Novoxel, Solta, Syneron Candela, and Zeltiq.
REPORTING FROM ASLMS 2018
Key clinical point: A newly designed pulsed-dye laser allows for fluences to be delivered with a 15-mm diameter treatment beam.
Major finding: Blinded evaluators rated the average score improvement in subjects’ rosacea as 52.5%, and ranged from 30.0% to 86.7%.
Study details: A study of 20 patients with erythematotelangiectatic rosacea who received pulsed-dye laser treatments every 4 weeks.
Disclosures: Dr. Bernstein reported having received grant funding from Syneron Candela and Zeltiq. He also has received consulting fees from and holds ownership interest in Syneron Candela, and has served on the advisory board for Novoxel, Solta, Syneron Candela, and Zeltiq.
Off-label prescribing of SGAs in children varies by diagnosis
TORONTO – On-label prescribing of second-generation antipsychotics in hospitalized pediatric patients with bipolar disorder and schizophrenia was greater than off-label prescribing, but not for patients with autism spectrum disorder, results from a single-center study showed.
“There is an increasing trend for using second-generation antipsychotics (SGAs) in children,” lead study author Debra V. McQuade, MD, PhD, said in an interview in advance of the Pediatric Academic Societies meeting. “This trend has already been widely acknowledged as concerning, due to the relatively high adverse event burden associated with them. Also, and perhaps more concerning, the great majority of these prescriptions are prescribed as ‘off-label’ (without Food and Drug Administration approval or indication). This is true in all settings, whether outpatient or inpatient. And, this off-label use is really high – usually reported as 60%-95% of all SGA prescriptions to children. We wanted to understand more about this practice of off-label prescribing of SGAs to children – to understand what drives it, to see if there were any organizing principles that might help to better explain it.”
Dr. McQuade and her associates found that for the three diagnostic groups overall, on-label prescribing of SGAs was greater than off-label prescribing (65% vs. 35%, respectively; P less than .001). Prescriptions for patients with bipolar disorder and schizophrenia followed this pattern, with on-label and off-label prescribing rates of 73% vs. 27%, for bipolar disorder, and 85% vs. 14% for schizophrenia. However, this prescription pattern was reversed for patients with autism spectrum disorder (35% vs. 64%; P less than .001), a finding that the researchers did not expect.
She said that while off-label prescribing of SGAs to pediatric patients remains widespread and is a concerning trend, the study findings suggested that prescribers “do select and prescribe SGAs in ways that are directly or indirectly influenced by FDA guidelines, mitigating risk to their pediatric patients.” Dr. McQuade acknowledged certain weaknesses of the study, including the fact that it was limited to one hospital setting and by the small number of prescribers who contributed to the overall pool of data.
She reported having no relevant financial disclosures.
TORONTO – On-label prescribing of second-generation antipsychotics in hospitalized pediatric patients with bipolar disorder and schizophrenia was greater than off-label prescribing, but not for patients with autism spectrum disorder, results from a single-center study showed.
“There is an increasing trend for using second-generation antipsychotics (SGAs) in children,” lead study author Debra V. McQuade, MD, PhD, said in an interview in advance of the Pediatric Academic Societies meeting. “This trend has already been widely acknowledged as concerning, due to the relatively high adverse event burden associated with them. Also, and perhaps more concerning, the great majority of these prescriptions are prescribed as ‘off-label’ (without Food and Drug Administration approval or indication). This is true in all settings, whether outpatient or inpatient. And, this off-label use is really high – usually reported as 60%-95% of all SGA prescriptions to children. We wanted to understand more about this practice of off-label prescribing of SGAs to children – to understand what drives it, to see if there were any organizing principles that might help to better explain it.”
Dr. McQuade and her associates found that for the three diagnostic groups overall, on-label prescribing of SGAs was greater than off-label prescribing (65% vs. 35%, respectively; P less than .001). Prescriptions for patients with bipolar disorder and schizophrenia followed this pattern, with on-label and off-label prescribing rates of 73% vs. 27%, for bipolar disorder, and 85% vs. 14% for schizophrenia. However, this prescription pattern was reversed for patients with autism spectrum disorder (35% vs. 64%; P less than .001), a finding that the researchers did not expect.
She said that while off-label prescribing of SGAs to pediatric patients remains widespread and is a concerning trend, the study findings suggested that prescribers “do select and prescribe SGAs in ways that are directly or indirectly influenced by FDA guidelines, mitigating risk to their pediatric patients.” Dr. McQuade acknowledged certain weaknesses of the study, including the fact that it was limited to one hospital setting and by the small number of prescribers who contributed to the overall pool of data.
She reported having no relevant financial disclosures.
TORONTO – On-label prescribing of second-generation antipsychotics in hospitalized pediatric patients with bipolar disorder and schizophrenia was greater than off-label prescribing, but not for patients with autism spectrum disorder, results from a single-center study showed.
“There is an increasing trend for using second-generation antipsychotics (SGAs) in children,” lead study author Debra V. McQuade, MD, PhD, said in an interview in advance of the Pediatric Academic Societies meeting. “This trend has already been widely acknowledged as concerning, due to the relatively high adverse event burden associated with them. Also, and perhaps more concerning, the great majority of these prescriptions are prescribed as ‘off-label’ (without Food and Drug Administration approval or indication). This is true in all settings, whether outpatient or inpatient. And, this off-label use is really high – usually reported as 60%-95% of all SGA prescriptions to children. We wanted to understand more about this practice of off-label prescribing of SGAs to children – to understand what drives it, to see if there were any organizing principles that might help to better explain it.”
Dr. McQuade and her associates found that for the three diagnostic groups overall, on-label prescribing of SGAs was greater than off-label prescribing (65% vs. 35%, respectively; P less than .001). Prescriptions for patients with bipolar disorder and schizophrenia followed this pattern, with on-label and off-label prescribing rates of 73% vs. 27%, for bipolar disorder, and 85% vs. 14% for schizophrenia. However, this prescription pattern was reversed for patients with autism spectrum disorder (35% vs. 64%; P less than .001), a finding that the researchers did not expect.
She said that while off-label prescribing of SGAs to pediatric patients remains widespread and is a concerning trend, the study findings suggested that prescribers “do select and prescribe SGAs in ways that are directly or indirectly influenced by FDA guidelines, mitigating risk to their pediatric patients.” Dr. McQuade acknowledged certain weaknesses of the study, including the fact that it was limited to one hospital setting and by the small number of prescribers who contributed to the overall pool of data.
She reported having no relevant financial disclosures.
Key clinical point:
Major finding: Overall, on-label prescribing of SGAs was greater than off-label prescribing (65% vs. 35%, respectively; P less than .001), but this prescription pattern did not hold true for patients with autism spectrum disorder.
Study details: A retrospective review of 86 hospitalized pediatric inpatients with a diagnosis of autism spectrum disorder, bipolar disorder, or schizophrenia.
Disclosures: Dr. McQuade reported having no financial disclosures.
Safety and support experiences of transgender and gender nonconforming youth explored
TORONTO – Youth with nonbinary identities – those that are beyond or outside of the categories of male/man and female/woman – feel significantly safer and more supported at school, compared with their transgender and gender nonconforming peers with binary identities, results from a survey of more than 300 youth showed.
“There has been little research specifically about the experiences of transgender and gender nonconforming youth that have nonbinary identities,” lead study author Brittany Allen, MD, said in an interview in advance of the Pediatric Academic Societies meeting.
Dr. Allen, a pediatrician at the University of Wisconsin–Madison, and her associates conducted an online survey of 311 transgender, nonbinary, and gender nonconforming youth in the state who ranged aged 12-22 years. Study participants were asked about their school safety and support experiences, and the researchers used Wilcoxon rank-sum tests to compare Likert scale responses among youth who reported nonbinary identities with those who reported binary identities. On the 1-5 scale, 1 meant “strongly agree” while 5 meant “strongly disagree.”
Dr. Allen, who is also comedical director of the Pediatric and Adolescent Transgender Health Clinic at American Family Children’s Hospital, Madison, reported that 311 young people completed more than 70% of the survey. Of those, 287 identified as having either binary (164; 57%) or nonbinary (123; 43%) gender identities. That percentage of those reporting nonbinary identities “is striking,” she said, and is “a much higher percentage than seen in adult studies of transgender and gender nonconforming people.”
Compared with respondents with binary identities, those with nonbinary identities were more often Caucasian/White (81% vs. 65% for those with binary identities; P = .003) and less likely to qualify for free lunch (28% vs. 55%; P = .001). Both binary and nonbinary groups reported similar school attendance and belonging. However, compared with the binary group, the nonbinary group reported significantly higher ratings of school safety (Likert score of 2.62 vs. 2.96, respectively; P = .0078) and peer support (Likert score of 2.54 vs. 2.87; P = .0139) and also were more likely to report being able to access adult support at school if needed (Likert score of 2.31 vs. 2.66; P = .0085).
“The primary message is that many transgender or gender nonconforming youth have identities outside of a gender binary and that transgender and gender nonconforming youth with different gender identities may have different strengths and challenges in different settings,” Dr. Allen said.
“Our work shows that nonbinary youth have relative safety and support at school compared to their transgender and gender nonconforming peers with binary identities – though it’s important to note that transgender and gender nonconforming youth overall are still at high risk of school harassment and violence. Interventions to promote school safety for youth of all gender identities should consider that transgender and gender nonconforming youth with different gender identities have different risks related to school safety and support.”
She acknowledged certain limitations of the study, including the fact that the researchers used a convenience sample to recruit participants, “which means that we may not have reached transgender and gender nonconforming youth that were less connected to support services or transgender and gender nonconforming peers,” Dr. Allen said. “This study also specifically assessed transgender and gender nonconforming youth; we did not have a comparison group of cisgender participants for comparison due to our study design.”
The study was funded by the National Institutes of Health, the Baldwin Wisconsin Ideas Endowment, the University of Wisconsin Advancing Health Equity and Diversity initiative, and the Wisconsin Partnership Program. Dr. Allen reported having no financial disclosures.
TORONTO – Youth with nonbinary identities – those that are beyond or outside of the categories of male/man and female/woman – feel significantly safer and more supported at school, compared with their transgender and gender nonconforming peers with binary identities, results from a survey of more than 300 youth showed.
“There has been little research specifically about the experiences of transgender and gender nonconforming youth that have nonbinary identities,” lead study author Brittany Allen, MD, said in an interview in advance of the Pediatric Academic Societies meeting.
Dr. Allen, a pediatrician at the University of Wisconsin–Madison, and her associates conducted an online survey of 311 transgender, nonbinary, and gender nonconforming youth in the state who ranged aged 12-22 years. Study participants were asked about their school safety and support experiences, and the researchers used Wilcoxon rank-sum tests to compare Likert scale responses among youth who reported nonbinary identities with those who reported binary identities. On the 1-5 scale, 1 meant “strongly agree” while 5 meant “strongly disagree.”
Dr. Allen, who is also comedical director of the Pediatric and Adolescent Transgender Health Clinic at American Family Children’s Hospital, Madison, reported that 311 young people completed more than 70% of the survey. Of those, 287 identified as having either binary (164; 57%) or nonbinary (123; 43%) gender identities. That percentage of those reporting nonbinary identities “is striking,” she said, and is “a much higher percentage than seen in adult studies of transgender and gender nonconforming people.”
Compared with respondents with binary identities, those with nonbinary identities were more often Caucasian/White (81% vs. 65% for those with binary identities; P = .003) and less likely to qualify for free lunch (28% vs. 55%; P = .001). Both binary and nonbinary groups reported similar school attendance and belonging. However, compared with the binary group, the nonbinary group reported significantly higher ratings of school safety (Likert score of 2.62 vs. 2.96, respectively; P = .0078) and peer support (Likert score of 2.54 vs. 2.87; P = .0139) and also were more likely to report being able to access adult support at school if needed (Likert score of 2.31 vs. 2.66; P = .0085).
“The primary message is that many transgender or gender nonconforming youth have identities outside of a gender binary and that transgender and gender nonconforming youth with different gender identities may have different strengths and challenges in different settings,” Dr. Allen said.
“Our work shows that nonbinary youth have relative safety and support at school compared to their transgender and gender nonconforming peers with binary identities – though it’s important to note that transgender and gender nonconforming youth overall are still at high risk of school harassment and violence. Interventions to promote school safety for youth of all gender identities should consider that transgender and gender nonconforming youth with different gender identities have different risks related to school safety and support.”
She acknowledged certain limitations of the study, including the fact that the researchers used a convenience sample to recruit participants, “which means that we may not have reached transgender and gender nonconforming youth that were less connected to support services or transgender and gender nonconforming peers,” Dr. Allen said. “This study also specifically assessed transgender and gender nonconforming youth; we did not have a comparison group of cisgender participants for comparison due to our study design.”
The study was funded by the National Institutes of Health, the Baldwin Wisconsin Ideas Endowment, the University of Wisconsin Advancing Health Equity and Diversity initiative, and the Wisconsin Partnership Program. Dr. Allen reported having no financial disclosures.
TORONTO – Youth with nonbinary identities – those that are beyond or outside of the categories of male/man and female/woman – feel significantly safer and more supported at school, compared with their transgender and gender nonconforming peers with binary identities, results from a survey of more than 300 youth showed.
“There has been little research specifically about the experiences of transgender and gender nonconforming youth that have nonbinary identities,” lead study author Brittany Allen, MD, said in an interview in advance of the Pediatric Academic Societies meeting.
Dr. Allen, a pediatrician at the University of Wisconsin–Madison, and her associates conducted an online survey of 311 transgender, nonbinary, and gender nonconforming youth in the state who ranged aged 12-22 years. Study participants were asked about their school safety and support experiences, and the researchers used Wilcoxon rank-sum tests to compare Likert scale responses among youth who reported nonbinary identities with those who reported binary identities. On the 1-5 scale, 1 meant “strongly agree” while 5 meant “strongly disagree.”
Dr. Allen, who is also comedical director of the Pediatric and Adolescent Transgender Health Clinic at American Family Children’s Hospital, Madison, reported that 311 young people completed more than 70% of the survey. Of those, 287 identified as having either binary (164; 57%) or nonbinary (123; 43%) gender identities. That percentage of those reporting nonbinary identities “is striking,” she said, and is “a much higher percentage than seen in adult studies of transgender and gender nonconforming people.”
Compared with respondents with binary identities, those with nonbinary identities were more often Caucasian/White (81% vs. 65% for those with binary identities; P = .003) and less likely to qualify for free lunch (28% vs. 55%; P = .001). Both binary and nonbinary groups reported similar school attendance and belonging. However, compared with the binary group, the nonbinary group reported significantly higher ratings of school safety (Likert score of 2.62 vs. 2.96, respectively; P = .0078) and peer support (Likert score of 2.54 vs. 2.87; P = .0139) and also were more likely to report being able to access adult support at school if needed (Likert score of 2.31 vs. 2.66; P = .0085).
“The primary message is that many transgender or gender nonconforming youth have identities outside of a gender binary and that transgender and gender nonconforming youth with different gender identities may have different strengths and challenges in different settings,” Dr. Allen said.
“Our work shows that nonbinary youth have relative safety and support at school compared to their transgender and gender nonconforming peers with binary identities – though it’s important to note that transgender and gender nonconforming youth overall are still at high risk of school harassment and violence. Interventions to promote school safety for youth of all gender identities should consider that transgender and gender nonconforming youth with different gender identities have different risks related to school safety and support.”
She acknowledged certain limitations of the study, including the fact that the researchers used a convenience sample to recruit participants, “which means that we may not have reached transgender and gender nonconforming youth that were less connected to support services or transgender and gender nonconforming peers,” Dr. Allen said. “This study also specifically assessed transgender and gender nonconforming youth; we did not have a comparison group of cisgender participants for comparison due to our study design.”
The study was funded by the National Institutes of Health, the Baldwin Wisconsin Ideas Endowment, the University of Wisconsin Advancing Health Equity and Diversity initiative, and the Wisconsin Partnership Program. Dr. Allen reported having no financial disclosures.
Key clinical point: Nonbinary youth felt significantly safer and more supported at school, compared with transgender peers with binary identities.
Major finding: Compared with the binary group, the nonbinary group reported significantly higher ratings of school safety (Likert score of 2.62 vs. 2.96, respectively) and peer support (Likert score of 2.54 vs. 2.87).
Study details: An online survey of 311 transgender, nonbinary, and gender nonconforming youth in Wisconsin who aged 12-22 years.
Disclosures: The study was funded by the National Institutes of Health, the Baldwin Wisconsin Ideas Endowment, the University of Wisconsin Advancing Health Equity and Diversity initiative, and the Wisconsin Partnership Program. Dr. Allen reported having no financial disclosures.