User login
ACOG seeks to increase LARC acceptance
About half of pregnancies in the United States are unintentional – an “unacceptably high” rate that underscores the need for ob.gyns. to help improve access to contraceptive implants and intrauterine devices, according to an updated committee opinion from the American College of Obstetricians and Gynecologists.
Physicians should “consider most women good candidates for [long-acting reversible contraception], including teens and nulliparous women,” said Dr. Eve Espey, who chaired ACOG’s working group on long-acting reversible contraception (LARC).
Clinicians also should promote same-day insertion protocols; offer LARC after abortion, miscarriage, and immediately postpartum; and routinely offer the copper IUD for emergency contraception, added Dr. Espey, who is chair of the department of obstetrics and gynecology at the University of New Mexico in Albuquerque.
The ACOG guidance emphasizes recent findings from the Contraceptive CHOICE Project, a large observational clinical trial in which LARC was 20 times more effective at preventing unintended pregnancies than oral contraceptive pills, patches, or rings. And other studies have tied the use of LARC to declines in rapid repeat pregnancy among adolescents and repeat abortion among women who have had an induced abortion, according to ACOG (Obstet Gynecol. 2015;126:e44–8.).
The updated ACOG opinion recommends that ob.gyns. adopt best practices for LARC insertion, including:
• Ensuring that women who request LARC receive it the same day whenever possible, as long as pregnancy can reasonably be ruled out.
• Offering LARC at the time of delivery, abortion, or dilation and curettage for miscarriage.
• Screening for sexually transmitted infections at the time of IUD insertion and treating without removing the IUD.
• Offering the copper IUD as the most effective form of emergency contraception.
The contraceptive mandate under the Affordable Care Act requires that most private insurers cover contraception methods approved by the Food and Drug Administration, including LARC, without copayments or deductibles, Dr. Espey said. But coverage of immediately postpartum IUD insertion is still in the works, with advocates focused on expanding coverage under Medicaid.
“For the time being, Medicaid in only 12 to 15 states reimburses or will soon reimburse for postpartum LARC,” Dr. Espey said. “Busy ob.gyns. can contact ACOG to find out if they live in such a state, and can be a champion to get their hospital on board for offering that service.”
The five LARC devices that are currently available in the United States include four IUDs and a single-rod etonogestrel implant that is approved for up to 3 years of use, according to ACOG. The copper T380A IUD is approved for up to 10 years of use, while two of the levonorgestrel-releasing intrauterine systems can be used for up to 3 years and one can be used for up to 5 years.
About half of pregnancies in the United States are unintentional – an “unacceptably high” rate that underscores the need for ob.gyns. to help improve access to contraceptive implants and intrauterine devices, according to an updated committee opinion from the American College of Obstetricians and Gynecologists.
Physicians should “consider most women good candidates for [long-acting reversible contraception], including teens and nulliparous women,” said Dr. Eve Espey, who chaired ACOG’s working group on long-acting reversible contraception (LARC).
Clinicians also should promote same-day insertion protocols; offer LARC after abortion, miscarriage, and immediately postpartum; and routinely offer the copper IUD for emergency contraception, added Dr. Espey, who is chair of the department of obstetrics and gynecology at the University of New Mexico in Albuquerque.
The ACOG guidance emphasizes recent findings from the Contraceptive CHOICE Project, a large observational clinical trial in which LARC was 20 times more effective at preventing unintended pregnancies than oral contraceptive pills, patches, or rings. And other studies have tied the use of LARC to declines in rapid repeat pregnancy among adolescents and repeat abortion among women who have had an induced abortion, according to ACOG (Obstet Gynecol. 2015;126:e44–8.).
The updated ACOG opinion recommends that ob.gyns. adopt best practices for LARC insertion, including:
• Ensuring that women who request LARC receive it the same day whenever possible, as long as pregnancy can reasonably be ruled out.
• Offering LARC at the time of delivery, abortion, or dilation and curettage for miscarriage.
• Screening for sexually transmitted infections at the time of IUD insertion and treating without removing the IUD.
• Offering the copper IUD as the most effective form of emergency contraception.
The contraceptive mandate under the Affordable Care Act requires that most private insurers cover contraception methods approved by the Food and Drug Administration, including LARC, without copayments or deductibles, Dr. Espey said. But coverage of immediately postpartum IUD insertion is still in the works, with advocates focused on expanding coverage under Medicaid.
“For the time being, Medicaid in only 12 to 15 states reimburses or will soon reimburse for postpartum LARC,” Dr. Espey said. “Busy ob.gyns. can contact ACOG to find out if they live in such a state, and can be a champion to get their hospital on board for offering that service.”
The five LARC devices that are currently available in the United States include four IUDs and a single-rod etonogestrel implant that is approved for up to 3 years of use, according to ACOG. The copper T380A IUD is approved for up to 10 years of use, while two of the levonorgestrel-releasing intrauterine systems can be used for up to 3 years and one can be used for up to 5 years.
About half of pregnancies in the United States are unintentional – an “unacceptably high” rate that underscores the need for ob.gyns. to help improve access to contraceptive implants and intrauterine devices, according to an updated committee opinion from the American College of Obstetricians and Gynecologists.
Physicians should “consider most women good candidates for [long-acting reversible contraception], including teens and nulliparous women,” said Dr. Eve Espey, who chaired ACOG’s working group on long-acting reversible contraception (LARC).
Clinicians also should promote same-day insertion protocols; offer LARC after abortion, miscarriage, and immediately postpartum; and routinely offer the copper IUD for emergency contraception, added Dr. Espey, who is chair of the department of obstetrics and gynecology at the University of New Mexico in Albuquerque.
The ACOG guidance emphasizes recent findings from the Contraceptive CHOICE Project, a large observational clinical trial in which LARC was 20 times more effective at preventing unintended pregnancies than oral contraceptive pills, patches, or rings. And other studies have tied the use of LARC to declines in rapid repeat pregnancy among adolescents and repeat abortion among women who have had an induced abortion, according to ACOG (Obstet Gynecol. 2015;126:e44–8.).
The updated ACOG opinion recommends that ob.gyns. adopt best practices for LARC insertion, including:
• Ensuring that women who request LARC receive it the same day whenever possible, as long as pregnancy can reasonably be ruled out.
• Offering LARC at the time of delivery, abortion, or dilation and curettage for miscarriage.
• Screening for sexually transmitted infections at the time of IUD insertion and treating without removing the IUD.
• Offering the copper IUD as the most effective form of emergency contraception.
The contraceptive mandate under the Affordable Care Act requires that most private insurers cover contraception methods approved by the Food and Drug Administration, including LARC, without copayments or deductibles, Dr. Espey said. But coverage of immediately postpartum IUD insertion is still in the works, with advocates focused on expanding coverage under Medicaid.
“For the time being, Medicaid in only 12 to 15 states reimburses or will soon reimburse for postpartum LARC,” Dr. Espey said. “Busy ob.gyns. can contact ACOG to find out if they live in such a state, and can be a champion to get their hospital on board for offering that service.”
The five LARC devices that are currently available in the United States include four IUDs and a single-rod etonogestrel implant that is approved for up to 3 years of use, according to ACOG. The copper T380A IUD is approved for up to 10 years of use, while two of the levonorgestrel-releasing intrauterine systems can be used for up to 3 years and one can be used for up to 5 years.
FROM OBSTETRICS AND GYNECOLOGY
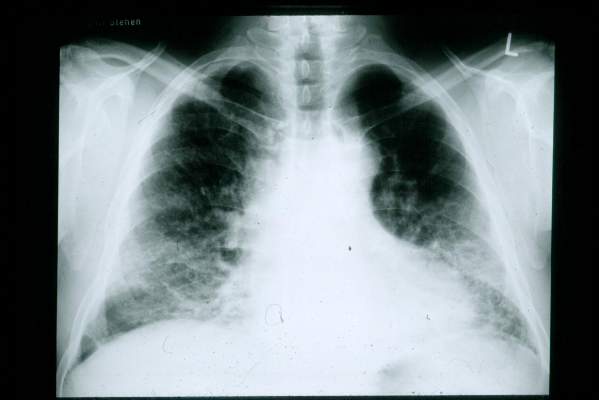
Hypothyroidism tied to idiopathic pulmonary fibrosis mortality
Hypothyroidism affected almost 17% of patients with idiopathic pulmonary fibrosis and was independently associated with their mortality, according to a report in the September issue of CHEST.
“We report, to our knowledge for the first time, an association between hypothyroidism and idiopathic pulmonary fibrosis,” wrote Dr. Justin Oldham of the pulmonary and critical care section of the University of Chicago and his associates. “Hypothyroidism, a largely autoimmune process, is common among patients with IPF and may represent an additional feature of autoimmunity in this patient population.” The retrospective study could not assess causality, but raises questions about whether autoimmune abnormalities contribte to or exacerbate IPF, and whether hypothyroidism and IPF share common underlying causes, they added.
Recent years have seen a “paradigm shift” away from immunologic or inflammatory causes of IPF in favor of alveolar injury and abnormal cellular repair mechanisms, but some studies point to autoimmunity in IPF, said the investigators. To further explore the question, they studied hypothyroidism – which in developed countries is most often autoimmune – among 196 patients with IPF with an equal number of age-and sex-matched controls with COPD (Chest 2015;148:692-700). Nearly 17% of IPF patients – including 13% of women and 28% of men – reported using thyroid replacement therapy with no history of thyroidectomy or radioactive iodine ablation. In contrast only 7% of COPD controls had a recorded diagnosis of hypothyroidism (odds ratio, 2.7; 95% confidence interval, 1.3 to 5.5; P = .01). Men and women with IPF and comorbid hypothyroidism had significantly shorter survival than did patients who had IPF only (P = .001). Hypothyroidism also independently predicted mortality in the multivariable analysis (hazard ratio, 2.1; 95% CI, 1.3 to 3.4), as did sequential increases in gender, age, and physiology (GAP) stage, the investigators said. “These conclusions held when transplant-free, transplant-excluded, and transplant-as-a-competing-event Cox regression models were constructed,” they reported. Furthermore, multivariable analyses of data from two IPF clinical trials (ACE-IPF and PANTHER) revealed similar associations among hypothyroidism, GAP stage, and mortality, they said.
Exactly how hypothyroidism contributes to IPF and IPF-related mortality is unclear, said Dr. Oldham and his associates. Because the study did not examine longitudinal changes in thyroid stage, they could not relate those trends to IPF progression, they noted. Although they excluded patients whose thyroid disease was known not to be autoimmune, they could not specifically confirm that all remaining patients with hypothyroidism had autoimmune thyroiditis, because most had been diagnosed years before. Future longitudinal studies should examine whether IPF and hypothyroidism share underlying causes, and should examine why hypothyroidism seems to increase IPF-related mortality, they concluded.
The National Institutes of Health funded the study. Dr. Oldham and five coauthors declared no competing interests. Senior author Dr. Imre Noth and one coauthor reported grant support and honoraria from NIH, Brystol-Myers Squibb, Gilead Sciences, Intermune, Medimmune, and several other pharmaceutical companies.
Hypothyroidism affected almost 17% of patients with idiopathic pulmonary fibrosis and was independently associated with their mortality, according to a report in the September issue of CHEST.
“We report, to our knowledge for the first time, an association between hypothyroidism and idiopathic pulmonary fibrosis,” wrote Dr. Justin Oldham of the pulmonary and critical care section of the University of Chicago and his associates. “Hypothyroidism, a largely autoimmune process, is common among patients with IPF and may represent an additional feature of autoimmunity in this patient population.” The retrospective study could not assess causality, but raises questions about whether autoimmune abnormalities contribte to or exacerbate IPF, and whether hypothyroidism and IPF share common underlying causes, they added.
Recent years have seen a “paradigm shift” away from immunologic or inflammatory causes of IPF in favor of alveolar injury and abnormal cellular repair mechanisms, but some studies point to autoimmunity in IPF, said the investigators. To further explore the question, they studied hypothyroidism – which in developed countries is most often autoimmune – among 196 patients with IPF with an equal number of age-and sex-matched controls with COPD (Chest 2015;148:692-700). Nearly 17% of IPF patients – including 13% of women and 28% of men – reported using thyroid replacement therapy with no history of thyroidectomy or radioactive iodine ablation. In contrast only 7% of COPD controls had a recorded diagnosis of hypothyroidism (odds ratio, 2.7; 95% confidence interval, 1.3 to 5.5; P = .01). Men and women with IPF and comorbid hypothyroidism had significantly shorter survival than did patients who had IPF only (P = .001). Hypothyroidism also independently predicted mortality in the multivariable analysis (hazard ratio, 2.1; 95% CI, 1.3 to 3.4), as did sequential increases in gender, age, and physiology (GAP) stage, the investigators said. “These conclusions held when transplant-free, transplant-excluded, and transplant-as-a-competing-event Cox regression models were constructed,” they reported. Furthermore, multivariable analyses of data from two IPF clinical trials (ACE-IPF and PANTHER) revealed similar associations among hypothyroidism, GAP stage, and mortality, they said.
Exactly how hypothyroidism contributes to IPF and IPF-related mortality is unclear, said Dr. Oldham and his associates. Because the study did not examine longitudinal changes in thyroid stage, they could not relate those trends to IPF progression, they noted. Although they excluded patients whose thyroid disease was known not to be autoimmune, they could not specifically confirm that all remaining patients with hypothyroidism had autoimmune thyroiditis, because most had been diagnosed years before. Future longitudinal studies should examine whether IPF and hypothyroidism share underlying causes, and should examine why hypothyroidism seems to increase IPF-related mortality, they concluded.
The National Institutes of Health funded the study. Dr. Oldham and five coauthors declared no competing interests. Senior author Dr. Imre Noth and one coauthor reported grant support and honoraria from NIH, Brystol-Myers Squibb, Gilead Sciences, Intermune, Medimmune, and several other pharmaceutical companies.
Hypothyroidism affected almost 17% of patients with idiopathic pulmonary fibrosis and was independently associated with their mortality, according to a report in the September issue of CHEST.
“We report, to our knowledge for the first time, an association between hypothyroidism and idiopathic pulmonary fibrosis,” wrote Dr. Justin Oldham of the pulmonary and critical care section of the University of Chicago and his associates. “Hypothyroidism, a largely autoimmune process, is common among patients with IPF and may represent an additional feature of autoimmunity in this patient population.” The retrospective study could not assess causality, but raises questions about whether autoimmune abnormalities contribte to or exacerbate IPF, and whether hypothyroidism and IPF share common underlying causes, they added.
Recent years have seen a “paradigm shift” away from immunologic or inflammatory causes of IPF in favor of alveolar injury and abnormal cellular repair mechanisms, but some studies point to autoimmunity in IPF, said the investigators. To further explore the question, they studied hypothyroidism – which in developed countries is most often autoimmune – among 196 patients with IPF with an equal number of age-and sex-matched controls with COPD (Chest 2015;148:692-700). Nearly 17% of IPF patients – including 13% of women and 28% of men – reported using thyroid replacement therapy with no history of thyroidectomy or radioactive iodine ablation. In contrast only 7% of COPD controls had a recorded diagnosis of hypothyroidism (odds ratio, 2.7; 95% confidence interval, 1.3 to 5.5; P = .01). Men and women with IPF and comorbid hypothyroidism had significantly shorter survival than did patients who had IPF only (P = .001). Hypothyroidism also independently predicted mortality in the multivariable analysis (hazard ratio, 2.1; 95% CI, 1.3 to 3.4), as did sequential increases in gender, age, and physiology (GAP) stage, the investigators said. “These conclusions held when transplant-free, transplant-excluded, and transplant-as-a-competing-event Cox regression models were constructed,” they reported. Furthermore, multivariable analyses of data from two IPF clinical trials (ACE-IPF and PANTHER) revealed similar associations among hypothyroidism, GAP stage, and mortality, they said.
Exactly how hypothyroidism contributes to IPF and IPF-related mortality is unclear, said Dr. Oldham and his associates. Because the study did not examine longitudinal changes in thyroid stage, they could not relate those trends to IPF progression, they noted. Although they excluded patients whose thyroid disease was known not to be autoimmune, they could not specifically confirm that all remaining patients with hypothyroidism had autoimmune thyroiditis, because most had been diagnosed years before. Future longitudinal studies should examine whether IPF and hypothyroidism share underlying causes, and should examine why hypothyroidism seems to increase IPF-related mortality, they concluded.
The National Institutes of Health funded the study. Dr. Oldham and five coauthors declared no competing interests. Senior author Dr. Imre Noth and one coauthor reported grant support and honoraria from NIH, Brystol-Myers Squibb, Gilead Sciences, Intermune, Medimmune, and several other pharmaceutical companies.
FROM CHEST
Key clinical point: Hypothyroidism was common among patients with idiopathic pulmonary fibrosis and was independently associated with mortality.
Major finding: Hypothyroidism predicted mortality in the multivariable analysis (hazard ratio, 2.1).
Data source: A retrospective hospital-based study of 392 patients with IPF (cases) or COPD (controls).
Disclosures: The National Institutes of Health funded the study. Dr. Oldham and five coauthors declared no competing interests. Senior author Dr. Imre Noth and one coauthor reported grant support and honoraria from NIH, Brystol-Myers Squibb, Gilead Sciences, Intermune, Medimmune, and several other pharmaceutical companies.
Oropharyngeal exercises significantly cuts snoring
Eight minutes of oropharyngeal exercises performed three times a day significantly reduced snoring, according to a report in the September issue of CHEST.
At 3 months, the snore index and the total snore index dropped significantly for the exercise group but not the control group, said Vanessa Ieto. Ph.D., of the Sleep Laboratory of the University of São Paulo in Brazil and her associates. The regimen improved snoring symptoms among primary snorers as well as patients with mild to moderate obstructive sleep apnea, although the apnea-hypopnea index only improved among patients with moderate OSA, the researchers added. “This set of oropharyngeal exercises is a promising treatment of large populations suffering from snoring who are currently largely ignored by the medical community,” they said.
Snoring is embarrassing and disruptive, and can exacerbate pharyngeal neurogenic lesions and carotid artery atherosclerosis, but few studies have objectively examined interventions for primary snorers or patients with mild OSA, the researchers said. In their randomized trial of 39 such patients, the intervention group performed six oropharyngeal exercises three times daily, while the control group patients practiced breathing exercises and wore nasal dilator strips at night. Both groups performed nasal lavage with saline solution three times a day. Average age was 46 years, and mean body-mass index was 28.2 kg/m2. A blinded researcher evaluated data from computerized polysomnography and a snoring recorder (Chest 2015;148:683-81). Nasopharyngeal exercises used in the study were as follows:
- Push tip of tongue against hard palate and slide tongue backward (20 times).
- Suck entire tongue up against palate (20 times).
- Force back of tongue against floor of mouth while touching tip of tongue to bottom incisors (20 times).
- Elevation soft palate and uvula while intermittently saying “A” (20 times).
- Place finger in mouth while pressing buccinator muscle outward (10 times per side).
- Chew and deglutinate on both sides of mouth whenever eating. Avoid perioral contraction.
After 3 months, the intervention group had significantly improved on both the snore index (snores per hour; P = .041 for change from baseline) and the total snore index (the total sound intensity of snores per hour; P = .033), the researchers said. The intervention group also improved significantly on several subjective measures, including perceived intensity and frequency of snoring and sleep quality. The control group only improved in terms of subjective snore frequency, the researchers said.
The apnea-hypopnea index did not drop significantly for the overall intervention group, but did improve significantly among patients with moderate OSA, they added. “The most likely explanation is that a ‘floor effect’ in the AHI prevented the observation of any effect on this metric among patients with mild or no OSA at study entry,” they said. “Our results point out that snoring, rather than AHI, is probably the best metric to follow patients with mild forms of OSA in whom the most significant complaint is snoring.”
The study was funded by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). The researchers declared they had no competing interests.
Eight minutes of oropharyngeal exercises performed three times a day significantly reduced snoring, according to a report in the September issue of CHEST.
At 3 months, the snore index and the total snore index dropped significantly for the exercise group but not the control group, said Vanessa Ieto. Ph.D., of the Sleep Laboratory of the University of São Paulo in Brazil and her associates. The regimen improved snoring symptoms among primary snorers as well as patients with mild to moderate obstructive sleep apnea, although the apnea-hypopnea index only improved among patients with moderate OSA, the researchers added. “This set of oropharyngeal exercises is a promising treatment of large populations suffering from snoring who are currently largely ignored by the medical community,” they said.
Snoring is embarrassing and disruptive, and can exacerbate pharyngeal neurogenic lesions and carotid artery atherosclerosis, but few studies have objectively examined interventions for primary snorers or patients with mild OSA, the researchers said. In their randomized trial of 39 such patients, the intervention group performed six oropharyngeal exercises three times daily, while the control group patients practiced breathing exercises and wore nasal dilator strips at night. Both groups performed nasal lavage with saline solution three times a day. Average age was 46 years, and mean body-mass index was 28.2 kg/m2. A blinded researcher evaluated data from computerized polysomnography and a snoring recorder (Chest 2015;148:683-81). Nasopharyngeal exercises used in the study were as follows:
- Push tip of tongue against hard palate and slide tongue backward (20 times).
- Suck entire tongue up against palate (20 times).
- Force back of tongue against floor of mouth while touching tip of tongue to bottom incisors (20 times).
- Elevation soft palate and uvula while intermittently saying “A” (20 times).
- Place finger in mouth while pressing buccinator muscle outward (10 times per side).
- Chew and deglutinate on both sides of mouth whenever eating. Avoid perioral contraction.
After 3 months, the intervention group had significantly improved on both the snore index (snores per hour; P = .041 for change from baseline) and the total snore index (the total sound intensity of snores per hour; P = .033), the researchers said. The intervention group also improved significantly on several subjective measures, including perceived intensity and frequency of snoring and sleep quality. The control group only improved in terms of subjective snore frequency, the researchers said.
The apnea-hypopnea index did not drop significantly for the overall intervention group, but did improve significantly among patients with moderate OSA, they added. “The most likely explanation is that a ‘floor effect’ in the AHI prevented the observation of any effect on this metric among patients with mild or no OSA at study entry,” they said. “Our results point out that snoring, rather than AHI, is probably the best metric to follow patients with mild forms of OSA in whom the most significant complaint is snoring.”
The study was funded by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). The researchers declared they had no competing interests.
Eight minutes of oropharyngeal exercises performed three times a day significantly reduced snoring, according to a report in the September issue of CHEST.
At 3 months, the snore index and the total snore index dropped significantly for the exercise group but not the control group, said Vanessa Ieto. Ph.D., of the Sleep Laboratory of the University of São Paulo in Brazil and her associates. The regimen improved snoring symptoms among primary snorers as well as patients with mild to moderate obstructive sleep apnea, although the apnea-hypopnea index only improved among patients with moderate OSA, the researchers added. “This set of oropharyngeal exercises is a promising treatment of large populations suffering from snoring who are currently largely ignored by the medical community,” they said.
Snoring is embarrassing and disruptive, and can exacerbate pharyngeal neurogenic lesions and carotid artery atherosclerosis, but few studies have objectively examined interventions for primary snorers or patients with mild OSA, the researchers said. In their randomized trial of 39 such patients, the intervention group performed six oropharyngeal exercises three times daily, while the control group patients practiced breathing exercises and wore nasal dilator strips at night. Both groups performed nasal lavage with saline solution three times a day. Average age was 46 years, and mean body-mass index was 28.2 kg/m2. A blinded researcher evaluated data from computerized polysomnography and a snoring recorder (Chest 2015;148:683-81). Nasopharyngeal exercises used in the study were as follows:
- Push tip of tongue against hard palate and slide tongue backward (20 times).
- Suck entire tongue up against palate (20 times).
- Force back of tongue against floor of mouth while touching tip of tongue to bottom incisors (20 times).
- Elevation soft palate and uvula while intermittently saying “A” (20 times).
- Place finger in mouth while pressing buccinator muscle outward (10 times per side).
- Chew and deglutinate on both sides of mouth whenever eating. Avoid perioral contraction.
After 3 months, the intervention group had significantly improved on both the snore index (snores per hour; P = .041 for change from baseline) and the total snore index (the total sound intensity of snores per hour; P = .033), the researchers said. The intervention group also improved significantly on several subjective measures, including perceived intensity and frequency of snoring and sleep quality. The control group only improved in terms of subjective snore frequency, the researchers said.
The apnea-hypopnea index did not drop significantly for the overall intervention group, but did improve significantly among patients with moderate OSA, they added. “The most likely explanation is that a ‘floor effect’ in the AHI prevented the observation of any effect on this metric among patients with mild or no OSA at study entry,” they said. “Our results point out that snoring, rather than AHI, is probably the best metric to follow patients with mild forms of OSA in whom the most significant complaint is snoring.”
The study was funded by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). The researchers declared they had no competing interests.
FROM CHEST
Key clinical point: Eight minutes of oropharyngeal exercises performed three times a day for 3 months significantly reduced snoring.
Major finding: The snore index and total snore index significantly dropped for the exercise group (P .017 and .03) but not for the control group.
Data source: A randomized single-blinded trial of 39 patients with primary snoring or mild to moderate obstructive sleep apnea.
Disclosures: The study was funded by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). The researchers declared they had no competing interests.
Tissue-based treatment could improve psoriatic arthritis outcomes
Efforts underway to tailor psoriatic arthritis treatments to the various tissues involved in the pathogenesis of the disease could optimize therapeutic approaches, Dr. Iain McInnes said at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education.
“Psoriatic arthritis [PsA] is a disease whose treatment is evolving quickly, ” added Dr. McInnes, professor of medicine and director of the Institute of Infection, Immunity, and Inflammation at the University of Glasgow (Scotland). “We have new ideas about pathogenesis, emerging studies that inform the best strategic approach to disease management, including potential value in a treat-to-target approach, and new therapeutics that offer a range of options to allow us to optimize treatment.”
He pointed to recent evidence for a diverse pathogenesis of PsA subtypes. Synovial membranes in PsA have high levels of tumor necrosis factor (TNF)-alpha, while resident populations of interleukin (IL)-23 receptor–positive T cells are found in entheses and IL-17 is abundant in psoriatic lesions. Genome-wide association studies have underscored the role of the IL-23 and IL-17 cytokine axis, while other work has implicated Th17 cytokines in mesenchymal tissue changes.
Although drug development efforts have typically viewed rheumatoid arthritis and PsA as homogeneous, “we can appreciate the extent of articular, entheseal, and cutaneous involvement, and look to tailor therapies accordingly,” Dr. McInnes said.
So what will the next decade look like for PsA? Therapy will center around TNF-alpha inhibitors, new cytokine pathways, and small-molecule inhibitors, according to Dr. McInnes. While anti-TNF agents are not universally tolerated or effective, their “well-established safety profile” and positive effects on American College of Rheumatology response criteria and radiographic endpoints generally outweigh risks of infection and problems with decreasing long-term drug survival, he said. These agents also can improve disease activity, skin symptoms, physical function, fatigue, overall quality of life, enthesitis, and dactylitis, he noted.
Other recent additions to the PsA arsenal include the IL-12/IL-23 inhibitor ustekinumab (Stelara), which in the PSUMMIT 1 and 2 trials was associated with decreased rates of radiographic progression and dose-dependent improvements in enthesitis, Dr. McInnes said. The phosphodiesterase-4 inhibitor apremilast (Otezla) was associated with significantly better ACR 20 response at week 16 and significantly greater improvements in Maastricht Ankylosing Spondylitis Enthesis Score and measures of dactylitis at week 24 of the PALACE trials. Most recently, in the FUTURE1 and FUTURE2 trials, the IL-17A inhibitor secukinumab (Cosentyx) beat placebo in terms of ACR 20, ACR 50, ACR 70, resolution of dactylitis and enthesitis, and radiographic measures of disease progression.
The availability of effective biologics raises the possibility of a treat-to-target approach geared toward clinical remission or low disease activity, Dr. McInnes concluded. “Targets for low disease activity in PsA are now available. Composite measures of disease activity, such as minimal disease activity (MDA), encompass all clinically important aspects of PsA,” he emphasized. While studies still need to pinpoint the best therapeutic pathways for disease subtypes, the first treat-to-target study of PsA found that tailoring therapy based on remission or minimal disease activity led to significantly better ACR 20, ACR 50, and ACR 70 responses at week 48, compared with standard care, he noted.
Dr. McInnes reported receiving research funding or honoraria from Novartis, Janssen, AbbVie, UCB, Pfizer, and MSD Pharmaceuticals, all of which make medications for rheumatic diseases. Global Academy for Medical Education and this news organization are owned by the same parent company.
Efforts underway to tailor psoriatic arthritis treatments to the various tissues involved in the pathogenesis of the disease could optimize therapeutic approaches, Dr. Iain McInnes said at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education.
“Psoriatic arthritis [PsA] is a disease whose treatment is evolving quickly, ” added Dr. McInnes, professor of medicine and director of the Institute of Infection, Immunity, and Inflammation at the University of Glasgow (Scotland). “We have new ideas about pathogenesis, emerging studies that inform the best strategic approach to disease management, including potential value in a treat-to-target approach, and new therapeutics that offer a range of options to allow us to optimize treatment.”
He pointed to recent evidence for a diverse pathogenesis of PsA subtypes. Synovial membranes in PsA have high levels of tumor necrosis factor (TNF)-alpha, while resident populations of interleukin (IL)-23 receptor–positive T cells are found in entheses and IL-17 is abundant in psoriatic lesions. Genome-wide association studies have underscored the role of the IL-23 and IL-17 cytokine axis, while other work has implicated Th17 cytokines in mesenchymal tissue changes.
Although drug development efforts have typically viewed rheumatoid arthritis and PsA as homogeneous, “we can appreciate the extent of articular, entheseal, and cutaneous involvement, and look to tailor therapies accordingly,” Dr. McInnes said.
So what will the next decade look like for PsA? Therapy will center around TNF-alpha inhibitors, new cytokine pathways, and small-molecule inhibitors, according to Dr. McInnes. While anti-TNF agents are not universally tolerated or effective, their “well-established safety profile” and positive effects on American College of Rheumatology response criteria and radiographic endpoints generally outweigh risks of infection and problems with decreasing long-term drug survival, he said. These agents also can improve disease activity, skin symptoms, physical function, fatigue, overall quality of life, enthesitis, and dactylitis, he noted.
Other recent additions to the PsA arsenal include the IL-12/IL-23 inhibitor ustekinumab (Stelara), which in the PSUMMIT 1 and 2 trials was associated with decreased rates of radiographic progression and dose-dependent improvements in enthesitis, Dr. McInnes said. The phosphodiesterase-4 inhibitor apremilast (Otezla) was associated with significantly better ACR 20 response at week 16 and significantly greater improvements in Maastricht Ankylosing Spondylitis Enthesis Score and measures of dactylitis at week 24 of the PALACE trials. Most recently, in the FUTURE1 and FUTURE2 trials, the IL-17A inhibitor secukinumab (Cosentyx) beat placebo in terms of ACR 20, ACR 50, ACR 70, resolution of dactylitis and enthesitis, and radiographic measures of disease progression.
The availability of effective biologics raises the possibility of a treat-to-target approach geared toward clinical remission or low disease activity, Dr. McInnes concluded. “Targets for low disease activity in PsA are now available. Composite measures of disease activity, such as minimal disease activity (MDA), encompass all clinically important aspects of PsA,” he emphasized. While studies still need to pinpoint the best therapeutic pathways for disease subtypes, the first treat-to-target study of PsA found that tailoring therapy based on remission or minimal disease activity led to significantly better ACR 20, ACR 50, and ACR 70 responses at week 48, compared with standard care, he noted.
Dr. McInnes reported receiving research funding or honoraria from Novartis, Janssen, AbbVie, UCB, Pfizer, and MSD Pharmaceuticals, all of which make medications for rheumatic diseases. Global Academy for Medical Education and this news organization are owned by the same parent company.
Efforts underway to tailor psoriatic arthritis treatments to the various tissues involved in the pathogenesis of the disease could optimize therapeutic approaches, Dr. Iain McInnes said at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education.
“Psoriatic arthritis [PsA] is a disease whose treatment is evolving quickly, ” added Dr. McInnes, professor of medicine and director of the Institute of Infection, Immunity, and Inflammation at the University of Glasgow (Scotland). “We have new ideas about pathogenesis, emerging studies that inform the best strategic approach to disease management, including potential value in a treat-to-target approach, and new therapeutics that offer a range of options to allow us to optimize treatment.”
He pointed to recent evidence for a diverse pathogenesis of PsA subtypes. Synovial membranes in PsA have high levels of tumor necrosis factor (TNF)-alpha, while resident populations of interleukin (IL)-23 receptor–positive T cells are found in entheses and IL-17 is abundant in psoriatic lesions. Genome-wide association studies have underscored the role of the IL-23 and IL-17 cytokine axis, while other work has implicated Th17 cytokines in mesenchymal tissue changes.
Although drug development efforts have typically viewed rheumatoid arthritis and PsA as homogeneous, “we can appreciate the extent of articular, entheseal, and cutaneous involvement, and look to tailor therapies accordingly,” Dr. McInnes said.
So what will the next decade look like for PsA? Therapy will center around TNF-alpha inhibitors, new cytokine pathways, and small-molecule inhibitors, according to Dr. McInnes. While anti-TNF agents are not universally tolerated or effective, their “well-established safety profile” and positive effects on American College of Rheumatology response criteria and radiographic endpoints generally outweigh risks of infection and problems with decreasing long-term drug survival, he said. These agents also can improve disease activity, skin symptoms, physical function, fatigue, overall quality of life, enthesitis, and dactylitis, he noted.
Other recent additions to the PsA arsenal include the IL-12/IL-23 inhibitor ustekinumab (Stelara), which in the PSUMMIT 1 and 2 trials was associated with decreased rates of radiographic progression and dose-dependent improvements in enthesitis, Dr. McInnes said. The phosphodiesterase-4 inhibitor apremilast (Otezla) was associated with significantly better ACR 20 response at week 16 and significantly greater improvements in Maastricht Ankylosing Spondylitis Enthesis Score and measures of dactylitis at week 24 of the PALACE trials. Most recently, in the FUTURE1 and FUTURE2 trials, the IL-17A inhibitor secukinumab (Cosentyx) beat placebo in terms of ACR 20, ACR 50, ACR 70, resolution of dactylitis and enthesitis, and radiographic measures of disease progression.
The availability of effective biologics raises the possibility of a treat-to-target approach geared toward clinical remission or low disease activity, Dr. McInnes concluded. “Targets for low disease activity in PsA are now available. Composite measures of disease activity, such as minimal disease activity (MDA), encompass all clinically important aspects of PsA,” he emphasized. While studies still need to pinpoint the best therapeutic pathways for disease subtypes, the first treat-to-target study of PsA found that tailoring therapy based on remission or minimal disease activity led to significantly better ACR 20, ACR 50, and ACR 70 responses at week 48, compared with standard care, he noted.
Dr. McInnes reported receiving research funding or honoraria from Novartis, Janssen, AbbVie, UCB, Pfizer, and MSD Pharmaceuticals, all of which make medications for rheumatic diseases. Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM THE ANNUAL PERSPECTIVES IN RHEUMATIC DISEASES
Methotrexate ups risk of liver abnormalities, but not serious hepatic events
Methotrexate use more than doubled the risk of liver enzyme abnormalities but was not tied to serious hepatic outcomes among patients with rheumatic diseases, according to a meta-analysis of 32 randomized, controlled trials.
“Serious liver events were rare, with a suggestion of a trend towards fewer poor liver outcomes,” wrote Dr. Richard Conway of Galway (Ireland) University Hospitals. “The short duration of the included studies and the lack of liver biopsies are limitations, but the available data provide robust evidence for short-term safety” of methotrexate, wrote Dr. Conway and his associates.
Methotrexate is a first-line RA therapy with efficacy in several other inflammatory diseases, but concerns about toxicity have limited its use, the researchers noted. Clinicians have particularly debated its hepatic effects, in part because it can be “exceedingly difficult” to determine if liver disease is preexisting, methotrexate related, or caused by other medications or comorbidities, they said. To better assess the issue, they searched PubMed and the Cochrane Central Register of Controlled Trials for relevant double-blind, randomized, controlled trials published between 1990 and 2014. They found 32 such trials that included 13,177 patients with rheumatoid arthritis, psoriasis, psoriatic arthritis or inflammatory bowel disease (Semin Arthritis Rheum. 2015;45:156-62). Methotrexate use approximately doubled the risk of any adverse hepatic event (relative risk, 2.19; 95% confidence interval, 1.73-2.77) and of major and minor liver enzyme abnormalities (RR, 2.16; 95% CI, 1.67-2.79), but did not increase the risk of liver failure, cirrhosis, or liver-related mortality (RR, 0.12; 95% CI, 0.01-1.09), the investigators reported. “Clinical trials have inherent limitations, including short duration, selection bias, failure to collect information or reports that are not part of a prespecified protocol, and limited power to evaluate rare or unusual reports,” they cautioned. “While meta-analyses help overcome the last of these, the others raise some concern.”
But several other reports align with their results, the researchers noted. In an analysis of methotrexate studies lasting at least 2 years, about 10% of patients developed at least one minor liver enzyme abnormality, but less than 4% stopped methotrexate because of liver toxicity. Other controlled studies did not link methotrexate to severe fibrosis or cirrhosis – even after 4 years of treatment, they added. “It appears likely that serious liver-related complications due to methotrexate may take many years of treatment to manifest,” the investigators concluded.
The researchers reported no funding sources or conflicts of interest.
Methotrexate use more than doubled the risk of liver enzyme abnormalities but was not tied to serious hepatic outcomes among patients with rheumatic diseases, according to a meta-analysis of 32 randomized, controlled trials.
“Serious liver events were rare, with a suggestion of a trend towards fewer poor liver outcomes,” wrote Dr. Richard Conway of Galway (Ireland) University Hospitals. “The short duration of the included studies and the lack of liver biopsies are limitations, but the available data provide robust evidence for short-term safety” of methotrexate, wrote Dr. Conway and his associates.
Methotrexate is a first-line RA therapy with efficacy in several other inflammatory diseases, but concerns about toxicity have limited its use, the researchers noted. Clinicians have particularly debated its hepatic effects, in part because it can be “exceedingly difficult” to determine if liver disease is preexisting, methotrexate related, or caused by other medications or comorbidities, they said. To better assess the issue, they searched PubMed and the Cochrane Central Register of Controlled Trials for relevant double-blind, randomized, controlled trials published between 1990 and 2014. They found 32 such trials that included 13,177 patients with rheumatoid arthritis, psoriasis, psoriatic arthritis or inflammatory bowel disease (Semin Arthritis Rheum. 2015;45:156-62). Methotrexate use approximately doubled the risk of any adverse hepatic event (relative risk, 2.19; 95% confidence interval, 1.73-2.77) and of major and minor liver enzyme abnormalities (RR, 2.16; 95% CI, 1.67-2.79), but did not increase the risk of liver failure, cirrhosis, or liver-related mortality (RR, 0.12; 95% CI, 0.01-1.09), the investigators reported. “Clinical trials have inherent limitations, including short duration, selection bias, failure to collect information or reports that are not part of a prespecified protocol, and limited power to evaluate rare or unusual reports,” they cautioned. “While meta-analyses help overcome the last of these, the others raise some concern.”
But several other reports align with their results, the researchers noted. In an analysis of methotrexate studies lasting at least 2 years, about 10% of patients developed at least one minor liver enzyme abnormality, but less than 4% stopped methotrexate because of liver toxicity. Other controlled studies did not link methotrexate to severe fibrosis or cirrhosis – even after 4 years of treatment, they added. “It appears likely that serious liver-related complications due to methotrexate may take many years of treatment to manifest,” the investigators concluded.
The researchers reported no funding sources or conflicts of interest.
Methotrexate use more than doubled the risk of liver enzyme abnormalities but was not tied to serious hepatic outcomes among patients with rheumatic diseases, according to a meta-analysis of 32 randomized, controlled trials.
“Serious liver events were rare, with a suggestion of a trend towards fewer poor liver outcomes,” wrote Dr. Richard Conway of Galway (Ireland) University Hospitals. “The short duration of the included studies and the lack of liver biopsies are limitations, but the available data provide robust evidence for short-term safety” of methotrexate, wrote Dr. Conway and his associates.
Methotrexate is a first-line RA therapy with efficacy in several other inflammatory diseases, but concerns about toxicity have limited its use, the researchers noted. Clinicians have particularly debated its hepatic effects, in part because it can be “exceedingly difficult” to determine if liver disease is preexisting, methotrexate related, or caused by other medications or comorbidities, they said. To better assess the issue, they searched PubMed and the Cochrane Central Register of Controlled Trials for relevant double-blind, randomized, controlled trials published between 1990 and 2014. They found 32 such trials that included 13,177 patients with rheumatoid arthritis, psoriasis, psoriatic arthritis or inflammatory bowel disease (Semin Arthritis Rheum. 2015;45:156-62). Methotrexate use approximately doubled the risk of any adverse hepatic event (relative risk, 2.19; 95% confidence interval, 1.73-2.77) and of major and minor liver enzyme abnormalities (RR, 2.16; 95% CI, 1.67-2.79), but did not increase the risk of liver failure, cirrhosis, or liver-related mortality (RR, 0.12; 95% CI, 0.01-1.09), the investigators reported. “Clinical trials have inherent limitations, including short duration, selection bias, failure to collect information or reports that are not part of a prespecified protocol, and limited power to evaluate rare or unusual reports,” they cautioned. “While meta-analyses help overcome the last of these, the others raise some concern.”
But several other reports align with their results, the researchers noted. In an analysis of methotrexate studies lasting at least 2 years, about 10% of patients developed at least one minor liver enzyme abnormality, but less than 4% stopped methotrexate because of liver toxicity. Other controlled studies did not link methotrexate to severe fibrosis or cirrhosis – even after 4 years of treatment, they added. “It appears likely that serious liver-related complications due to methotrexate may take many years of treatment to manifest,” the investigators concluded.
The researchers reported no funding sources or conflicts of interest.
FROM SEMINARS IN ARTHRITIS AND RHEUMATISM
Key clinical point: Use of methotrexate increased the risk of hepatic enzyme abnormalities but not serious liver-related events among patients with inflammatory diseases.
Major finding: Methotrexate use approximately doubled the risk of any adverse liver event (RR, 2.19) but did not increase the risk of cirrhosis, liver failure, or liver-related death.
Data source: A meta-analysis of 32 randomized, controlled trials of methotrexate in rheumatoid arthritis, psoriasis, psoriatic arthritis, and inflammatory bowel disease.
Disclosures: The investigators reported no funding sources or conflicts of interest.
Nighttime caffeine delayed circadian clock
A double espresso-sized dose of caffeine consumed 3 hours before bedtime delayed the normal onset of the melatonin rhythm by about 40 minutes, researchers reported in Science Translational Medicine.
“In addition to increasing daytime exposure to sunlight and reducing evening exposure to electrical light, avoiding evening caffeine may help treat problematic delayed sleep timing,” according to Tina Burke of the University of Colorado Boulder and her associates. The results also could support consuming caffeine in the morning to help recover from jet lag, but further studies would need to test that possibility, the researchers added.
Caffeine is known to affect circadian rhythms in rats and flies, but its circadian effects in humans were unknown, said the investigators. Their 49-day, double-blinded study included five healthy, normal-weight adults who averaged 24 years of age. For a week before each scheduled laboratory visit, participants slept 8 hours a night as verified with the help of sleep logs, wrist actigraphy, and time-stamped voice mail reminders. In the laboratory, they received caffeine or placebo 3 hours before their normal bedtime and were exposed to either bright or dim (control) light at bedtime (Sci Transl Med. 2015;7:1-9).
Caffeine plus dim light was associated with about a 40-minute longer phase delay than placebo and dim light (P = .011), the investigators reported. Bright light with placebo led to about a 85-minute phase delay (P = .0007), while bright light plus caffeine caused a 105-minute shift (P = .0003). Experiments with cultured human cells also showed that caffeine competitively bound to adenosine receptors, which disrupted signaling of cyclic adenosine monophosphate (cAMP), a key part of the circadian clock, the researchers said.
The study was funded by the National Institutes of Health, the National Center for Advancing Translational Sciences, and the Howard Hughes Medical Institute in collaboration with the University of Colorado. Ms. Burke declared no competing interests.
A double espresso-sized dose of caffeine consumed 3 hours before bedtime delayed the normal onset of the melatonin rhythm by about 40 minutes, researchers reported in Science Translational Medicine.
“In addition to increasing daytime exposure to sunlight and reducing evening exposure to electrical light, avoiding evening caffeine may help treat problematic delayed sleep timing,” according to Tina Burke of the University of Colorado Boulder and her associates. The results also could support consuming caffeine in the morning to help recover from jet lag, but further studies would need to test that possibility, the researchers added.
Caffeine is known to affect circadian rhythms in rats and flies, but its circadian effects in humans were unknown, said the investigators. Their 49-day, double-blinded study included five healthy, normal-weight adults who averaged 24 years of age. For a week before each scheduled laboratory visit, participants slept 8 hours a night as verified with the help of sleep logs, wrist actigraphy, and time-stamped voice mail reminders. In the laboratory, they received caffeine or placebo 3 hours before their normal bedtime and were exposed to either bright or dim (control) light at bedtime (Sci Transl Med. 2015;7:1-9).
Caffeine plus dim light was associated with about a 40-minute longer phase delay than placebo and dim light (P = .011), the investigators reported. Bright light with placebo led to about a 85-minute phase delay (P = .0007), while bright light plus caffeine caused a 105-minute shift (P = .0003). Experiments with cultured human cells also showed that caffeine competitively bound to adenosine receptors, which disrupted signaling of cyclic adenosine monophosphate (cAMP), a key part of the circadian clock, the researchers said.
The study was funded by the National Institutes of Health, the National Center for Advancing Translational Sciences, and the Howard Hughes Medical Institute in collaboration with the University of Colorado. Ms. Burke declared no competing interests.
A double espresso-sized dose of caffeine consumed 3 hours before bedtime delayed the normal onset of the melatonin rhythm by about 40 minutes, researchers reported in Science Translational Medicine.
“In addition to increasing daytime exposure to sunlight and reducing evening exposure to electrical light, avoiding evening caffeine may help treat problematic delayed sleep timing,” according to Tina Burke of the University of Colorado Boulder and her associates. The results also could support consuming caffeine in the morning to help recover from jet lag, but further studies would need to test that possibility, the researchers added.
Caffeine is known to affect circadian rhythms in rats and flies, but its circadian effects in humans were unknown, said the investigators. Their 49-day, double-blinded study included five healthy, normal-weight adults who averaged 24 years of age. For a week before each scheduled laboratory visit, participants slept 8 hours a night as verified with the help of sleep logs, wrist actigraphy, and time-stamped voice mail reminders. In the laboratory, they received caffeine or placebo 3 hours before their normal bedtime and were exposed to either bright or dim (control) light at bedtime (Sci Transl Med. 2015;7:1-9).
Caffeine plus dim light was associated with about a 40-minute longer phase delay than placebo and dim light (P = .011), the investigators reported. Bright light with placebo led to about a 85-minute phase delay (P = .0007), while bright light plus caffeine caused a 105-minute shift (P = .0003). Experiments with cultured human cells also showed that caffeine competitively bound to adenosine receptors, which disrupted signaling of cyclic adenosine monophosphate (cAMP), a key part of the circadian clock, the researchers said.
The study was funded by the National Institutes of Health, the National Center for Advancing Translational Sciences, and the Howard Hughes Medical Institute in collaboration with the University of Colorado. Ms. Burke declared no competing interests.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point:Consuming caffeine at night delayed the human circadian clock, primarily by disrupting cyclic adenosine monophosphate (cAMP) signaling.
Major finding: When consumed 3 hours before bedtime, a caffeine dose equivalent to a double espresso delayed the circadian melatonin rhythm by about 40 minutes.
Data source: A double-blind, placebo-controlled, within-subject study of 5 individuals over about 49 days.
Disclosures: The study was funded by the National Institutes of Health, the National Center for Advancing Translational Sciences, and the Howard Hughes Medical Institute in collaboration with the University of Colorado. Dr. Burke declared no competing interests.
Paroxetine Found Neither Safe nor Effective for Adolescent Depression
Paroxetine is not a safe or effective drug for adolescent major depression, according to a reanalysis of data from a prominent and controversial trial.
The findings highlight the problem of bias in published studies, including underreporting of harms, Joanna Le Noury, Ph.D., of Bangor (Wales) University and her associates wrote online Sept. 16 in The BMJ. “Regulatory authorities should mandate accessibility of data and protocols,” the investigators added (BMJ 2015;351:h4320. doi: 10.1136/bmj.h4320).
Published in 2001, Study 329 was a randomized, multicenter, double-blind, placebo-controlled trial of 275 adolescents aged 12-18 whose major depression had lasted at least 8 weeks. Patients received 20-40 mg paroxetine once daily, 200-300 mg imipramine once daily, or placebo. Dr. Martin B. Keller of Brown University, Providence, R.I., and his colleagues concluded that paroxetine “is generally well tolerated and effective for major depression in adolescents” (J Am Acad Child Adolesc Psychiatry. 2001;40:762-72).
However, that “largely ghostwritten” article drew conclusions about paroxetine that were “at odds with the data,” wrote Dr. Le Noury and her associates. They cited other researchers who previously concluded that Dr. Keller and his colleagues introduced new outcome measures, conflated primary and secondary outcomes, downplayed a nonsignificant difference for a primary outcome, and reversed their stance on whether emergent suicidal ideation and other psychiatric events were related to paroxetine use.
Dr. Le Noury and her associates therefore obtained and reanalyzed the original Study 329 trial data as part of the restoring invisible and abandoned trials (RIAT) initiative of The BMJ. They concluded that the efficacy of paroxetine and imipramine did not statistically or clinically differ from placebo for any prespecified primary or secondary outcome measure. For example, Hamilton Depression Rating Scale scores dropped by an average of 10.7 (95% confidence interval, 9.1-12.3) for the paroxetine group, compared with 9 (7.4-10.5) for the imipramine group, and 9.1 (7.5-10.7) for placebo (P = .20), they reported.
Furthermore, the reanalysis uncovered “clinically significant” increases in psychiatric harms in the paroxetine group and cardiovascular effects in the imipramine group, said Dr. Le Noury and her associates. “The extent of the clinically significant increases in adverse events in the paroxetine and imipramine arms, including serious, severe, and suicide-related adverse events, became apparent only when the data were made available for reanalysis,” they wrote. “As with most scientific papers, Keller and colleagues convey an impression that ‘the data have spoken.’ This authoritative stance is possible only in the absence of access to the data. When the data become accessible to others, it becomes clear that scientific authorship is provisional rather than authoritative.”
In a statement, the American Academy of Child and Adolescent Psychiatry (AACAP), publisher of the Study 329 findings, said statements and opinions found in its journal “are those of the authors and not necessarily those of AACAP, the editors, or the publisher.” In addition AACAP said it has the “utmost respect for the BMJ” and thanks the journal for its “continued efforts to bring science to the forefront.”
SmithKline Beecham was the manufacturer of Paxil, the trade name for paroxetine. The company merged with Glaxo Wellcome in 2000 and became GlaxoSmithKline. Dr. Le Noury and her associates reported receiving no specific funding for the reanalysis. One coauthor reported having served as an expert witness for plaintiffs in lawsuits involving paroxetine, and as a witness for plaintiffs in lawsuits involving antidepressants with the same mechanism of action. Another coauthor reported receiving fees to provide expert analysis and opinion for a class action over Study 329 and an action over pediatric use of the antidepressant citalopram.
“Few studies have sustained as much criticism as Study 329,” wrote Peter Doshi, Ph.D. In fact, an officer of the Food and Drug Administration who reviewed the trial formally in 2002 said “on balance, this trial should be considered as a failed trial, in that neither active treatment group showed superiority over placebo by a statistically significant margin.” But more than 2 million prescriptions were written for children and adolescents in the United States that same year.
“The first draft of the manuscript ultimately published in the Journal of the American Academy of Child and Adolescent Psychiatry (JAACAP) was not written by any of the 22 named authors but by an outside medical writer hired by [GlaxoSmithKline].” In addition, Dr. Martin Keller, the lead author, “had been the focus of a front-page investigation in the Boston Globe in 1999 that documented his under-reporting of financial ties to drug companies.
“For those who have been calling for a retraction of the Keller paper for many years, the system has failed. None of the paper’s 22 mostly academic university authors, nor the journal’s editors, nor the academic and professional institutions they belong to, have intervened to correct the record. The paper remains without so much as an erratum, and none of its authors ... have been disciplined.”
Dr. Doshi is an assistant professor of pharmaceutical health services research at the University of Maryland School of Pharmacy and an associate editor at BMJ. He declared being first author of the reanalysis under the restoring invisible and abandoned trials (RIAT) declaration, which was coauthored by Dr. David Healy, a member of the group that reanalyzed Study 329. He was a reviewer for the reanalysis manuscript and provided unpaid advice on the RIAT process before and during the submission process. He also successfully requested data from clinical study reports of Study 329 and eight other GSK studies. These comments are taken from his accompanying feature (BMJ. 2015;351:h4629. doi: 10.1136/bmj.h4629).
“Few studies have sustained as much criticism as Study 329,” wrote Peter Doshi, Ph.D. In fact, an officer of the Food and Drug Administration who reviewed the trial formally in 2002 said “on balance, this trial should be considered as a failed trial, in that neither active treatment group showed superiority over placebo by a statistically significant margin.” But more than 2 million prescriptions were written for children and adolescents in the United States that same year.
“The first draft of the manuscript ultimately published in the Journal of the American Academy of Child and Adolescent Psychiatry (JAACAP) was not written by any of the 22 named authors but by an outside medical writer hired by [GlaxoSmithKline].” In addition, Dr. Martin Keller, the lead author, “had been the focus of a front-page investigation in the Boston Globe in 1999 that documented his under-reporting of financial ties to drug companies.
“For those who have been calling for a retraction of the Keller paper for many years, the system has failed. None of the paper’s 22 mostly academic university authors, nor the journal’s editors, nor the academic and professional institutions they belong to, have intervened to correct the record. The paper remains without so much as an erratum, and none of its authors ... have been disciplined.”
Dr. Doshi is an assistant professor of pharmaceutical health services research at the University of Maryland School of Pharmacy and an associate editor at BMJ. He declared being first author of the reanalysis under the restoring invisible and abandoned trials (RIAT) declaration, which was coauthored by Dr. David Healy, a member of the group that reanalyzed Study 329. He was a reviewer for the reanalysis manuscript and provided unpaid advice on the RIAT process before and during the submission process. He also successfully requested data from clinical study reports of Study 329 and eight other GSK studies. These comments are taken from his accompanying feature (BMJ. 2015;351:h4629. doi: 10.1136/bmj.h4629).
“Few studies have sustained as much criticism as Study 329,” wrote Peter Doshi, Ph.D. In fact, an officer of the Food and Drug Administration who reviewed the trial formally in 2002 said “on balance, this trial should be considered as a failed trial, in that neither active treatment group showed superiority over placebo by a statistically significant margin.” But more than 2 million prescriptions were written for children and adolescents in the United States that same year.
“The first draft of the manuscript ultimately published in the Journal of the American Academy of Child and Adolescent Psychiatry (JAACAP) was not written by any of the 22 named authors but by an outside medical writer hired by [GlaxoSmithKline].” In addition, Dr. Martin Keller, the lead author, “had been the focus of a front-page investigation in the Boston Globe in 1999 that documented his under-reporting of financial ties to drug companies.
“For those who have been calling for a retraction of the Keller paper for many years, the system has failed. None of the paper’s 22 mostly academic university authors, nor the journal’s editors, nor the academic and professional institutions they belong to, have intervened to correct the record. The paper remains without so much as an erratum, and none of its authors ... have been disciplined.”
Dr. Doshi is an assistant professor of pharmaceutical health services research at the University of Maryland School of Pharmacy and an associate editor at BMJ. He declared being first author of the reanalysis under the restoring invisible and abandoned trials (RIAT) declaration, which was coauthored by Dr. David Healy, a member of the group that reanalyzed Study 329. He was a reviewer for the reanalysis manuscript and provided unpaid advice on the RIAT process before and during the submission process. He also successfully requested data from clinical study reports of Study 329 and eight other GSK studies. These comments are taken from his accompanying feature (BMJ. 2015;351:h4629. doi: 10.1136/bmj.h4629).
Paroxetine is not a safe or effective drug for adolescent major depression, according to a reanalysis of data from a prominent and controversial trial.
The findings highlight the problem of bias in published studies, including underreporting of harms, Joanna Le Noury, Ph.D., of Bangor (Wales) University and her associates wrote online Sept. 16 in The BMJ. “Regulatory authorities should mandate accessibility of data and protocols,” the investigators added (BMJ 2015;351:h4320. doi: 10.1136/bmj.h4320).
Published in 2001, Study 329 was a randomized, multicenter, double-blind, placebo-controlled trial of 275 adolescents aged 12-18 whose major depression had lasted at least 8 weeks. Patients received 20-40 mg paroxetine once daily, 200-300 mg imipramine once daily, or placebo. Dr. Martin B. Keller of Brown University, Providence, R.I., and his colleagues concluded that paroxetine “is generally well tolerated and effective for major depression in adolescents” (J Am Acad Child Adolesc Psychiatry. 2001;40:762-72).
However, that “largely ghostwritten” article drew conclusions about paroxetine that were “at odds with the data,” wrote Dr. Le Noury and her associates. They cited other researchers who previously concluded that Dr. Keller and his colleagues introduced new outcome measures, conflated primary and secondary outcomes, downplayed a nonsignificant difference for a primary outcome, and reversed their stance on whether emergent suicidal ideation and other psychiatric events were related to paroxetine use.
Dr. Le Noury and her associates therefore obtained and reanalyzed the original Study 329 trial data as part of the restoring invisible and abandoned trials (RIAT) initiative of The BMJ. They concluded that the efficacy of paroxetine and imipramine did not statistically or clinically differ from placebo for any prespecified primary or secondary outcome measure. For example, Hamilton Depression Rating Scale scores dropped by an average of 10.7 (95% confidence interval, 9.1-12.3) for the paroxetine group, compared with 9 (7.4-10.5) for the imipramine group, and 9.1 (7.5-10.7) for placebo (P = .20), they reported.
Furthermore, the reanalysis uncovered “clinically significant” increases in psychiatric harms in the paroxetine group and cardiovascular effects in the imipramine group, said Dr. Le Noury and her associates. “The extent of the clinically significant increases in adverse events in the paroxetine and imipramine arms, including serious, severe, and suicide-related adverse events, became apparent only when the data were made available for reanalysis,” they wrote. “As with most scientific papers, Keller and colleagues convey an impression that ‘the data have spoken.’ This authoritative stance is possible only in the absence of access to the data. When the data become accessible to others, it becomes clear that scientific authorship is provisional rather than authoritative.”
In a statement, the American Academy of Child and Adolescent Psychiatry (AACAP), publisher of the Study 329 findings, said statements and opinions found in its journal “are those of the authors and not necessarily those of AACAP, the editors, or the publisher.” In addition AACAP said it has the “utmost respect for the BMJ” and thanks the journal for its “continued efforts to bring science to the forefront.”
SmithKline Beecham was the manufacturer of Paxil, the trade name for paroxetine. The company merged with Glaxo Wellcome in 2000 and became GlaxoSmithKline. Dr. Le Noury and her associates reported receiving no specific funding for the reanalysis. One coauthor reported having served as an expert witness for plaintiffs in lawsuits involving paroxetine, and as a witness for plaintiffs in lawsuits involving antidepressants with the same mechanism of action. Another coauthor reported receiving fees to provide expert analysis and opinion for a class action over Study 329 and an action over pediatric use of the antidepressant citalopram.
Paroxetine is not a safe or effective drug for adolescent major depression, according to a reanalysis of data from a prominent and controversial trial.
The findings highlight the problem of bias in published studies, including underreporting of harms, Joanna Le Noury, Ph.D., of Bangor (Wales) University and her associates wrote online Sept. 16 in The BMJ. “Regulatory authorities should mandate accessibility of data and protocols,” the investigators added (BMJ 2015;351:h4320. doi: 10.1136/bmj.h4320).
Published in 2001, Study 329 was a randomized, multicenter, double-blind, placebo-controlled trial of 275 adolescents aged 12-18 whose major depression had lasted at least 8 weeks. Patients received 20-40 mg paroxetine once daily, 200-300 mg imipramine once daily, or placebo. Dr. Martin B. Keller of Brown University, Providence, R.I., and his colleagues concluded that paroxetine “is generally well tolerated and effective for major depression in adolescents” (J Am Acad Child Adolesc Psychiatry. 2001;40:762-72).
However, that “largely ghostwritten” article drew conclusions about paroxetine that were “at odds with the data,” wrote Dr. Le Noury and her associates. They cited other researchers who previously concluded that Dr. Keller and his colleagues introduced new outcome measures, conflated primary and secondary outcomes, downplayed a nonsignificant difference for a primary outcome, and reversed their stance on whether emergent suicidal ideation and other psychiatric events were related to paroxetine use.
Dr. Le Noury and her associates therefore obtained and reanalyzed the original Study 329 trial data as part of the restoring invisible and abandoned trials (RIAT) initiative of The BMJ. They concluded that the efficacy of paroxetine and imipramine did not statistically or clinically differ from placebo for any prespecified primary or secondary outcome measure. For example, Hamilton Depression Rating Scale scores dropped by an average of 10.7 (95% confidence interval, 9.1-12.3) for the paroxetine group, compared with 9 (7.4-10.5) for the imipramine group, and 9.1 (7.5-10.7) for placebo (P = .20), they reported.
Furthermore, the reanalysis uncovered “clinically significant” increases in psychiatric harms in the paroxetine group and cardiovascular effects in the imipramine group, said Dr. Le Noury and her associates. “The extent of the clinically significant increases in adverse events in the paroxetine and imipramine arms, including serious, severe, and suicide-related adverse events, became apparent only when the data were made available for reanalysis,” they wrote. “As with most scientific papers, Keller and colleagues convey an impression that ‘the data have spoken.’ This authoritative stance is possible only in the absence of access to the data. When the data become accessible to others, it becomes clear that scientific authorship is provisional rather than authoritative.”
In a statement, the American Academy of Child and Adolescent Psychiatry (AACAP), publisher of the Study 329 findings, said statements and opinions found in its journal “are those of the authors and not necessarily those of AACAP, the editors, or the publisher.” In addition AACAP said it has the “utmost respect for the BMJ” and thanks the journal for its “continued efforts to bring science to the forefront.”
SmithKline Beecham was the manufacturer of Paxil, the trade name for paroxetine. The company merged with Glaxo Wellcome in 2000 and became GlaxoSmithKline. Dr. Le Noury and her associates reported receiving no specific funding for the reanalysis. One coauthor reported having served as an expert witness for plaintiffs in lawsuits involving paroxetine, and as a witness for plaintiffs in lawsuits involving antidepressants with the same mechanism of action. Another coauthor reported receiving fees to provide expert analysis and opinion for a class action over Study 329 and an action over pediatric use of the antidepressant citalopram.
FROM THE BMJ
Paroxetine found neither safe nor effective for adolescent depression
Paroxetine is not a safe or effective drug for adolescent major depression, according to a reanalysis of data from a prominent and controversial trial.
The findings highlight the problem of bias in published studies, including underreporting of harms, Joanna Le Noury, Ph.D., of Bangor (Wales) University and her associates wrote online Sept. 16 in The BMJ. “Regulatory authorities should mandate accessibility of data and protocols,” the investigators added (BMJ 2015;351:h4320. doi: 10.1136/bmj.h4320).
Published in 2001, Study 329 was a randomized, multicenter, double-blind, placebo-controlled trial of 275 adolescents aged 12-18 whose major depression had lasted at least 8 weeks. Patients received 20-40 mg paroxetine once daily, 200-300 mg imipramine once daily, or placebo. Dr. Martin B. Keller of Brown University, Providence, R.I., and his colleagues concluded that paroxetine “is generally well tolerated and effective for major depression in adolescents” (J Am Acad Child Adolesc Psychiatry. 2001;40:762-72).
However, that “largely ghostwritten” article drew conclusions about paroxetine that were “at odds with the data,” wrote Dr. Le Noury and her associates. They cited other researchers who previously concluded that Dr. Keller and his colleagues introduced new outcome measures, conflated primary and secondary outcomes, downplayed a nonsignificant difference for a primary outcome, and reversed their stance on whether emergent suicidal ideation and other psychiatric events were related to paroxetine use.
Dr. Le Noury and her associates therefore obtained and reanalyzed the original Study 329 trial data as part of the restoring invisible and abandoned trials (RIAT) initiative of The BMJ. They concluded that the efficacy of paroxetine and imipramine did not statistically or clinically differ from placebo for any prespecified primary or secondary outcome measure. For example, Hamilton Depression Rating Scale scores dropped by an average of 10.7 (95% confidence interval, 9.1-12.3) for the paroxetine group, compared with 9 (7.4-10.5) for the imipramine group, and 9.1 (7.5-10.7) for placebo (P = .20), they reported.
Furthermore, the reanalysis uncovered “clinically significant” increases in psychiatric harms in the paroxetine group and cardiovascular effects in the imipramine group, said Dr. Le Noury and her associates. “The extent of the clinically significant increases in adverse events in the paroxetine and imipramine arms, including serious, severe, and suicide-related adverse events, became apparent only when the data were made available for reanalysis,” they wrote. “As with most scientific papers, Keller and colleagues convey an impression that ‘the data have spoken.’ This authoritative stance is possible only in the absence of access to the data. When the data become accessible to others, it becomes clear that scientific authorship is provisional rather than authoritative.”
In a statement, the American Academy of Child and Adolescent Psychiatry (AACAP), publisher of the Study 329 findings, said statements and opinions found in its journal “are those of the authors and not necessarily those of AACAP, the editors, or the publisher.” In addition AACAP said it has the “utmost respect for the BMJ” and thanks the journal for its “continued efforts to bring science to the forefront.”
SmithKline Beecham was the manufacturer of Paxil, the trade name for paroxetine. The company merged with Glaxo Wellcome in 2000 and became GlaxoSmithKline. Dr. Le Noury and her associates reported receiving no specific funding for the reanalysis. One coauthor reported having served as an expert witness for plaintiffs in lawsuits involving paroxetine, and as a witness for plaintiffs in lawsuits involving antidepressants with the same mechanism of action. Another coauthor reported receiving fees to provide expert analysis and opinion for a class action over Study 329 and an action over pediatric use of the antidepressant citalopram.
“Few studies have sustained as much criticism as Study 329,” wrote Peter Doshi, Ph.D. In fact, an officer of the Food and Drug Administration who reviewed the trial formally in 2002 said “on balance, this trial should be considered as a failed trial, in that neither active treatment group showed superiority over placebo by a statistically significant margin.” But more than 2 million prescriptions were written for children and adolescents in the United States that same year.
“The first draft of the manuscript ultimately published in the Journal of the American Academy of Child and Adolescent Psychiatry (JAACAP) was not written by any of the 22 named authors but by an outside medical writer hired by [GlaxoSmithKline].” In addition, Dr. Martin Keller, the lead author, “had been the focus of a front-page investigation in the Boston Globe in 1999 that documented his under-reporting of financial ties to drug companies.
“For those who have been calling for a retraction of the Keller paper for many years, the system has failed. None of the paper’s 22 mostly academic university authors, nor the journal’s editors, nor the academic and professional institutions they belong to, have intervened to correct the record. The paper remains without so much as an erratum, and none of its authors ... have been disciplined.”
Dr. Doshi is an assistant professor of pharmaceutical health services research at the University of Maryland School of Pharmacy and an associate editor at BMJ. He declared being first author of the reanalysis under the restoring invisible and abandoned trials (RIAT) declaration, which was coauthored by Dr. David Healy, a member of the group that reanalyzed Study 329. He was a reviewer for the reanalysis manuscript and provided unpaid advice on the RIAT process before and during the submission process. He also successfully requested data from clinical study reports of Study 329 and eight other GSK studies. These comments are taken from his accompanying feature (BMJ. 2015;351:h4629. doi: 10.1136/bmj.h4629).
“Few studies have sustained as much criticism as Study 329,” wrote Peter Doshi, Ph.D. In fact, an officer of the Food and Drug Administration who reviewed the trial formally in 2002 said “on balance, this trial should be considered as a failed trial, in that neither active treatment group showed superiority over placebo by a statistically significant margin.” But more than 2 million prescriptions were written for children and adolescents in the United States that same year.
“The first draft of the manuscript ultimately published in the Journal of the American Academy of Child and Adolescent Psychiatry (JAACAP) was not written by any of the 22 named authors but by an outside medical writer hired by [GlaxoSmithKline].” In addition, Dr. Martin Keller, the lead author, “had been the focus of a front-page investigation in the Boston Globe in 1999 that documented his under-reporting of financial ties to drug companies.
“For those who have been calling for a retraction of the Keller paper for many years, the system has failed. None of the paper’s 22 mostly academic university authors, nor the journal’s editors, nor the academic and professional institutions they belong to, have intervened to correct the record. The paper remains without so much as an erratum, and none of its authors ... have been disciplined.”
Dr. Doshi is an assistant professor of pharmaceutical health services research at the University of Maryland School of Pharmacy and an associate editor at BMJ. He declared being first author of the reanalysis under the restoring invisible and abandoned trials (RIAT) declaration, which was coauthored by Dr. David Healy, a member of the group that reanalyzed Study 329. He was a reviewer for the reanalysis manuscript and provided unpaid advice on the RIAT process before and during the submission process. He also successfully requested data from clinical study reports of Study 329 and eight other GSK studies. These comments are taken from his accompanying feature (BMJ. 2015;351:h4629. doi: 10.1136/bmj.h4629).
“Few studies have sustained as much criticism as Study 329,” wrote Peter Doshi, Ph.D. In fact, an officer of the Food and Drug Administration who reviewed the trial formally in 2002 said “on balance, this trial should be considered as a failed trial, in that neither active treatment group showed superiority over placebo by a statistically significant margin.” But more than 2 million prescriptions were written for children and adolescents in the United States that same year.
“The first draft of the manuscript ultimately published in the Journal of the American Academy of Child and Adolescent Psychiatry (JAACAP) was not written by any of the 22 named authors but by an outside medical writer hired by [GlaxoSmithKline].” In addition, Dr. Martin Keller, the lead author, “had been the focus of a front-page investigation in the Boston Globe in 1999 that documented his under-reporting of financial ties to drug companies.
“For those who have been calling for a retraction of the Keller paper for many years, the system has failed. None of the paper’s 22 mostly academic university authors, nor the journal’s editors, nor the academic and professional institutions they belong to, have intervened to correct the record. The paper remains without so much as an erratum, and none of its authors ... have been disciplined.”
Dr. Doshi is an assistant professor of pharmaceutical health services research at the University of Maryland School of Pharmacy and an associate editor at BMJ. He declared being first author of the reanalysis under the restoring invisible and abandoned trials (RIAT) declaration, which was coauthored by Dr. David Healy, a member of the group that reanalyzed Study 329. He was a reviewer for the reanalysis manuscript and provided unpaid advice on the RIAT process before and during the submission process. He also successfully requested data from clinical study reports of Study 329 and eight other GSK studies. These comments are taken from his accompanying feature (BMJ. 2015;351:h4629. doi: 10.1136/bmj.h4629).
Paroxetine is not a safe or effective drug for adolescent major depression, according to a reanalysis of data from a prominent and controversial trial.
The findings highlight the problem of bias in published studies, including underreporting of harms, Joanna Le Noury, Ph.D., of Bangor (Wales) University and her associates wrote online Sept. 16 in The BMJ. “Regulatory authorities should mandate accessibility of data and protocols,” the investigators added (BMJ 2015;351:h4320. doi: 10.1136/bmj.h4320).
Published in 2001, Study 329 was a randomized, multicenter, double-blind, placebo-controlled trial of 275 adolescents aged 12-18 whose major depression had lasted at least 8 weeks. Patients received 20-40 mg paroxetine once daily, 200-300 mg imipramine once daily, or placebo. Dr. Martin B. Keller of Brown University, Providence, R.I., and his colleagues concluded that paroxetine “is generally well tolerated and effective for major depression in adolescents” (J Am Acad Child Adolesc Psychiatry. 2001;40:762-72).
However, that “largely ghostwritten” article drew conclusions about paroxetine that were “at odds with the data,” wrote Dr. Le Noury and her associates. They cited other researchers who previously concluded that Dr. Keller and his colleagues introduced new outcome measures, conflated primary and secondary outcomes, downplayed a nonsignificant difference for a primary outcome, and reversed their stance on whether emergent suicidal ideation and other psychiatric events were related to paroxetine use.
Dr. Le Noury and her associates therefore obtained and reanalyzed the original Study 329 trial data as part of the restoring invisible and abandoned trials (RIAT) initiative of The BMJ. They concluded that the efficacy of paroxetine and imipramine did not statistically or clinically differ from placebo for any prespecified primary or secondary outcome measure. For example, Hamilton Depression Rating Scale scores dropped by an average of 10.7 (95% confidence interval, 9.1-12.3) for the paroxetine group, compared with 9 (7.4-10.5) for the imipramine group, and 9.1 (7.5-10.7) for placebo (P = .20), they reported.
Furthermore, the reanalysis uncovered “clinically significant” increases in psychiatric harms in the paroxetine group and cardiovascular effects in the imipramine group, said Dr. Le Noury and her associates. “The extent of the clinically significant increases in adverse events in the paroxetine and imipramine arms, including serious, severe, and suicide-related adverse events, became apparent only when the data were made available for reanalysis,” they wrote. “As with most scientific papers, Keller and colleagues convey an impression that ‘the data have spoken.’ This authoritative stance is possible only in the absence of access to the data. When the data become accessible to others, it becomes clear that scientific authorship is provisional rather than authoritative.”
In a statement, the American Academy of Child and Adolescent Psychiatry (AACAP), publisher of the Study 329 findings, said statements and opinions found in its journal “are those of the authors and not necessarily those of AACAP, the editors, or the publisher.” In addition AACAP said it has the “utmost respect for the BMJ” and thanks the journal for its “continued efforts to bring science to the forefront.”
SmithKline Beecham was the manufacturer of Paxil, the trade name for paroxetine. The company merged with Glaxo Wellcome in 2000 and became GlaxoSmithKline. Dr. Le Noury and her associates reported receiving no specific funding for the reanalysis. One coauthor reported having served as an expert witness for plaintiffs in lawsuits involving paroxetine, and as a witness for plaintiffs in lawsuits involving antidepressants with the same mechanism of action. Another coauthor reported receiving fees to provide expert analysis and opinion for a class action over Study 329 and an action over pediatric use of the antidepressant citalopram.
Paroxetine is not a safe or effective drug for adolescent major depression, according to a reanalysis of data from a prominent and controversial trial.
The findings highlight the problem of bias in published studies, including underreporting of harms, Joanna Le Noury, Ph.D., of Bangor (Wales) University and her associates wrote online Sept. 16 in The BMJ. “Regulatory authorities should mandate accessibility of data and protocols,” the investigators added (BMJ 2015;351:h4320. doi: 10.1136/bmj.h4320).
Published in 2001, Study 329 was a randomized, multicenter, double-blind, placebo-controlled trial of 275 adolescents aged 12-18 whose major depression had lasted at least 8 weeks. Patients received 20-40 mg paroxetine once daily, 200-300 mg imipramine once daily, or placebo. Dr. Martin B. Keller of Brown University, Providence, R.I., and his colleagues concluded that paroxetine “is generally well tolerated and effective for major depression in adolescents” (J Am Acad Child Adolesc Psychiatry. 2001;40:762-72).
However, that “largely ghostwritten” article drew conclusions about paroxetine that were “at odds with the data,” wrote Dr. Le Noury and her associates. They cited other researchers who previously concluded that Dr. Keller and his colleagues introduced new outcome measures, conflated primary and secondary outcomes, downplayed a nonsignificant difference for a primary outcome, and reversed their stance on whether emergent suicidal ideation and other psychiatric events were related to paroxetine use.
Dr. Le Noury and her associates therefore obtained and reanalyzed the original Study 329 trial data as part of the restoring invisible and abandoned trials (RIAT) initiative of The BMJ. They concluded that the efficacy of paroxetine and imipramine did not statistically or clinically differ from placebo for any prespecified primary or secondary outcome measure. For example, Hamilton Depression Rating Scale scores dropped by an average of 10.7 (95% confidence interval, 9.1-12.3) for the paroxetine group, compared with 9 (7.4-10.5) for the imipramine group, and 9.1 (7.5-10.7) for placebo (P = .20), they reported.
Furthermore, the reanalysis uncovered “clinically significant” increases in psychiatric harms in the paroxetine group and cardiovascular effects in the imipramine group, said Dr. Le Noury and her associates. “The extent of the clinically significant increases in adverse events in the paroxetine and imipramine arms, including serious, severe, and suicide-related adverse events, became apparent only when the data were made available for reanalysis,” they wrote. “As with most scientific papers, Keller and colleagues convey an impression that ‘the data have spoken.’ This authoritative stance is possible only in the absence of access to the data. When the data become accessible to others, it becomes clear that scientific authorship is provisional rather than authoritative.”
In a statement, the American Academy of Child and Adolescent Psychiatry (AACAP), publisher of the Study 329 findings, said statements and opinions found in its journal “are those of the authors and not necessarily those of AACAP, the editors, or the publisher.” In addition AACAP said it has the “utmost respect for the BMJ” and thanks the journal for its “continued efforts to bring science to the forefront.”
SmithKline Beecham was the manufacturer of Paxil, the trade name for paroxetine. The company merged with Glaxo Wellcome in 2000 and became GlaxoSmithKline. Dr. Le Noury and her associates reported receiving no specific funding for the reanalysis. One coauthor reported having served as an expert witness for plaintiffs in lawsuits involving paroxetine, and as a witness for plaintiffs in lawsuits involving antidepressants with the same mechanism of action. Another coauthor reported receiving fees to provide expert analysis and opinion for a class action over Study 329 and an action over pediatric use of the antidepressant citalopram.
FROM THE BMJ
Key clinical point:A reanalysis of original trial data found that paroxetine was neither safe nor effective in the treatment of adolescent major depression.
Major finding: Neither paroxetine nor high-dose imipramine outperformed placebo. Both drugs yielded major safety signals.
Data source: Reanalysis of SmithKline Beecham’s controversial Study 329, a double-blind, randomized, placebo-controlled trial of 275 adolescents with major depression.
Disclosures: SmithKline Beecham was the manufacturer of Paxil, the trade name for paroxetine. The company merged with Glaxo Wellcome in 2000 and became GlaxoSmithKline. The investigators received no specific funding to conduct the analysis. One coauthor reported having served as an expert witness for plaintiffs in lawsuits involving paroxetine, and as a witness for plaintiffs in lawsuits involving antidepressants that have the same mechanism of action. Another coauthor reported receiving fees to provide expert analysis and opinion for a class action over Study 329 and another lawsuit over pediatric use of citalopram.
Sunscreens with DNA repair enzymes might lessen AK progression
Patients with actinic keratosis who used UPF 50 sunscreen containing DNA repair enzymes improved significantly more on two measures of malignant progression than did those who used sunscreen alone, according to research published in the Journal of Drugs in Dermatology.
At 6 months, improvements in field cancerization and levels of cyclobutane pyrimidine dimers were significantly greater (P less than .001) for the sunscreen-plus-enzymes group compared with sunscreen-only patients, wrote Dr. Mauro Carducci of Centro Ortopedico di Quadrante in Omegna, Italy, and his associates.
The study is the first of its type to directly compare the clinical effects of two such topicals, the investigators wrote. The findings set the stage for longer, larger trials that are powered to assess the risk of progression to squamous cell carcinoma, they added.
For the study, 28 patients with AK were randomly assigned to use SPF 50 sunscreen alone or a formula that contained 1% photolyase from Anacystis nidulans and 1% endonuclease from Micrococcus luteus. Patients applied 2 mg/cm2 of sunscreen to treatment areas that contained 4-10 AKs. They were not allowed to use other topicals during the trial or for 2 weeks beforehand.
All of the patients were white and aged older than 65 years; three-quarters were men. The investigators used fluorescence diagnostics with methylaminolaevulinate to measure field cancerization, and analyzed skin biopsies to quantify CPD levels (J Drugs Dermatol. 2015;14[9]:986-90.).
Hyperkeratosis improved the same amount in both groups at month 6, according to the researchers. But field cancerizations dropped 29% from baseline in the sunscreen-plus-enzymes group, compared with a 10% decrease with sunscreen alone (P less than .0001). Likewise, CPD levels fell 61% from baseline in the sunscreen-plus-enzymes group compared with a 35% drop with sunscreen alone (P less than .0001).
Despite those significant differences, the study was not powered to detect differences in the risk of transformation to SCC, the researchers cautioned.
Biodue S.p.A. provided the methyl aminolevulinate used in the study. Dr. Enzo Emanuele, the study’s senior author, is a major shareholder of Living Research S.A.S., a privately held biomedical research organization that provided funding for the work. The other researchers reported no conflicts of interest.
Patients with actinic keratosis who used UPF 50 sunscreen containing DNA repair enzymes improved significantly more on two measures of malignant progression than did those who used sunscreen alone, according to research published in the Journal of Drugs in Dermatology.
At 6 months, improvements in field cancerization and levels of cyclobutane pyrimidine dimers were significantly greater (P less than .001) for the sunscreen-plus-enzymes group compared with sunscreen-only patients, wrote Dr. Mauro Carducci of Centro Ortopedico di Quadrante in Omegna, Italy, and his associates.
The study is the first of its type to directly compare the clinical effects of two such topicals, the investigators wrote. The findings set the stage for longer, larger trials that are powered to assess the risk of progression to squamous cell carcinoma, they added.
For the study, 28 patients with AK were randomly assigned to use SPF 50 sunscreen alone or a formula that contained 1% photolyase from Anacystis nidulans and 1% endonuclease from Micrococcus luteus. Patients applied 2 mg/cm2 of sunscreen to treatment areas that contained 4-10 AKs. They were not allowed to use other topicals during the trial or for 2 weeks beforehand.
All of the patients were white and aged older than 65 years; three-quarters were men. The investigators used fluorescence diagnostics with methylaminolaevulinate to measure field cancerization, and analyzed skin biopsies to quantify CPD levels (J Drugs Dermatol. 2015;14[9]:986-90.).
Hyperkeratosis improved the same amount in both groups at month 6, according to the researchers. But field cancerizations dropped 29% from baseline in the sunscreen-plus-enzymes group, compared with a 10% decrease with sunscreen alone (P less than .0001). Likewise, CPD levels fell 61% from baseline in the sunscreen-plus-enzymes group compared with a 35% drop with sunscreen alone (P less than .0001).
Despite those significant differences, the study was not powered to detect differences in the risk of transformation to SCC, the researchers cautioned.
Biodue S.p.A. provided the methyl aminolevulinate used in the study. Dr. Enzo Emanuele, the study’s senior author, is a major shareholder of Living Research S.A.S., a privately held biomedical research organization that provided funding for the work. The other researchers reported no conflicts of interest.
Patients with actinic keratosis who used UPF 50 sunscreen containing DNA repair enzymes improved significantly more on two measures of malignant progression than did those who used sunscreen alone, according to research published in the Journal of Drugs in Dermatology.
At 6 months, improvements in field cancerization and levels of cyclobutane pyrimidine dimers were significantly greater (P less than .001) for the sunscreen-plus-enzymes group compared with sunscreen-only patients, wrote Dr. Mauro Carducci of Centro Ortopedico di Quadrante in Omegna, Italy, and his associates.
The study is the first of its type to directly compare the clinical effects of two such topicals, the investigators wrote. The findings set the stage for longer, larger trials that are powered to assess the risk of progression to squamous cell carcinoma, they added.
For the study, 28 patients with AK were randomly assigned to use SPF 50 sunscreen alone or a formula that contained 1% photolyase from Anacystis nidulans and 1% endonuclease from Micrococcus luteus. Patients applied 2 mg/cm2 of sunscreen to treatment areas that contained 4-10 AKs. They were not allowed to use other topicals during the trial or for 2 weeks beforehand.
All of the patients were white and aged older than 65 years; three-quarters were men. The investigators used fluorescence diagnostics with methylaminolaevulinate to measure field cancerization, and analyzed skin biopsies to quantify CPD levels (J Drugs Dermatol. 2015;14[9]:986-90.).
Hyperkeratosis improved the same amount in both groups at month 6, according to the researchers. But field cancerizations dropped 29% from baseline in the sunscreen-plus-enzymes group, compared with a 10% decrease with sunscreen alone (P less than .0001). Likewise, CPD levels fell 61% from baseline in the sunscreen-plus-enzymes group compared with a 35% drop with sunscreen alone (P less than .0001).
Despite those significant differences, the study was not powered to detect differences in the risk of transformation to SCC, the researchers cautioned.
Biodue S.p.A. provided the methyl aminolevulinate used in the study. Dr. Enzo Emanuele, the study’s senior author, is a major shareholder of Living Research S.A.S., a privately held biomedical research organization that provided funding for the work. The other researchers reported no conflicts of interest.
FROM THE JOURNAL OF DRUGS IN DERMATOLOGY
Key clinical point:Sunscreen containing DNA repair enzymes might prevent malignant progression of actinic keratosis better than sunscreen alone.
Major finding: Field cancerization and cyclobutane pyrimidine dimer levels improved significantly more with sunscreen plus enzymes than with sunscreen only (P less than .0001 for each).
Data source: Six-month randomized trial of 28 patients with actinic keratosis.
Disclosures: Biodue S.p.A. provided the methyl aminolevulinate used in the study. Dr. Enzo Emanuele, the study’s senior author, is a major shareholder of Living Research S.A.S., a privately held biomedical research organization that provided funding for the work. The other researchers reported no conflicts of interest.
Corticosteroids Far Outpaced Minoxidil Use for Alopecia Areata
Alopecia areata sends “hundreds of thousands” of patients to the doctor every year in the United States, and six in ten of those visits end with a corticosteroid prescription, investigators reported in the Journal of Drugs in Dermatology.
In contrast, “minoxidil appears either underreported or underutilized in this population of patients, which suggests the need to educate both dermatologists and patients on the potential usefulness of this medication in alopecia areata,” wrote Michael Farhangian and his associates at Wake Forest University in Winston-Salem, N.C.
About 2% of individuals develop alopecia areata during their lives, but there are no consensus guidelines for disease in the United States. To better understand treatment patterns here, the investigators analyzed data on about 2.6 outpatient visits for alopecia areata between 2001 and 2010. The data came from two national ambulatory health care surveys (J Drugs Dermatol. 2015;14[9]:1012-14).
Patients with alopecia areata most often sought care from dermatologists (85%), the researchers reported. Providers prescribed topical and injected corticosteroids far more often (61%) than other drugs, such as minoxidil (5.9%), topical tacrolimus (5.7%), topical retinoid (3.3%), oral steroids (1.8%), or anthralin (1.8%).
The British Association of Dermatologists recommends corticosteroids for localized alopecia areata, but long-term use can lead to skin atrophy, hypopigmentation, and telangiectasia, the researchers warned. “This risk may be increased in patients who are prescribed both topical and injected corticosteroids, as was observed in 9.9% of patients,” they added.
Frequencies of minoxidil and tacrolimus use were nearly identical even though tacrolimus has been found ineffectivein alopecia areata, according to the researchers.
“Patients may be hesitant to use minoxidil since it is only FDA-approved for androgenetic alopecia and not for alopecia areata,” they wrote. Minoxidil also is available over-the-counter, which could explain its scarcity in the dataset, they added.
Galderma Laboratories helped fund the work through an unrestricted educational grant. Mr. Farhangian declared no competing interests. Senior author Dr. Steven Feldman reported relationships with Galderma, Janssen, Taro, Abbott Labs, and a number of other pharmaceutical companies. Dr. Feldman also reported holding stock in Causa Research and Medical Quality Enhancement Corporation. Another coauthor reported relationships with several pharmaceutical companies.
Alopecia areata sends “hundreds of thousands” of patients to the doctor every year in the United States, and six in ten of those visits end with a corticosteroid prescription, investigators reported in the Journal of Drugs in Dermatology.
In contrast, “minoxidil appears either underreported or underutilized in this population of patients, which suggests the need to educate both dermatologists and patients on the potential usefulness of this medication in alopecia areata,” wrote Michael Farhangian and his associates at Wake Forest University in Winston-Salem, N.C.
About 2% of individuals develop alopecia areata during their lives, but there are no consensus guidelines for disease in the United States. To better understand treatment patterns here, the investigators analyzed data on about 2.6 outpatient visits for alopecia areata between 2001 and 2010. The data came from two national ambulatory health care surveys (J Drugs Dermatol. 2015;14[9]:1012-14).
Patients with alopecia areata most often sought care from dermatologists (85%), the researchers reported. Providers prescribed topical and injected corticosteroids far more often (61%) than other drugs, such as minoxidil (5.9%), topical tacrolimus (5.7%), topical retinoid (3.3%), oral steroids (1.8%), or anthralin (1.8%).
The British Association of Dermatologists recommends corticosteroids for localized alopecia areata, but long-term use can lead to skin atrophy, hypopigmentation, and telangiectasia, the researchers warned. “This risk may be increased in patients who are prescribed both topical and injected corticosteroids, as was observed in 9.9% of patients,” they added.
Frequencies of minoxidil and tacrolimus use were nearly identical even though tacrolimus has been found ineffectivein alopecia areata, according to the researchers.
“Patients may be hesitant to use minoxidil since it is only FDA-approved for androgenetic alopecia and not for alopecia areata,” they wrote. Minoxidil also is available over-the-counter, which could explain its scarcity in the dataset, they added.
Galderma Laboratories helped fund the work through an unrestricted educational grant. Mr. Farhangian declared no competing interests. Senior author Dr. Steven Feldman reported relationships with Galderma, Janssen, Taro, Abbott Labs, and a number of other pharmaceutical companies. Dr. Feldman also reported holding stock in Causa Research and Medical Quality Enhancement Corporation. Another coauthor reported relationships with several pharmaceutical companies.
Alopecia areata sends “hundreds of thousands” of patients to the doctor every year in the United States, and six in ten of those visits end with a corticosteroid prescription, investigators reported in the Journal of Drugs in Dermatology.
In contrast, “minoxidil appears either underreported or underutilized in this population of patients, which suggests the need to educate both dermatologists and patients on the potential usefulness of this medication in alopecia areata,” wrote Michael Farhangian and his associates at Wake Forest University in Winston-Salem, N.C.
About 2% of individuals develop alopecia areata during their lives, but there are no consensus guidelines for disease in the United States. To better understand treatment patterns here, the investigators analyzed data on about 2.6 outpatient visits for alopecia areata between 2001 and 2010. The data came from two national ambulatory health care surveys (J Drugs Dermatol. 2015;14[9]:1012-14).
Patients with alopecia areata most often sought care from dermatologists (85%), the researchers reported. Providers prescribed topical and injected corticosteroids far more often (61%) than other drugs, such as minoxidil (5.9%), topical tacrolimus (5.7%), topical retinoid (3.3%), oral steroids (1.8%), or anthralin (1.8%).
The British Association of Dermatologists recommends corticosteroids for localized alopecia areata, but long-term use can lead to skin atrophy, hypopigmentation, and telangiectasia, the researchers warned. “This risk may be increased in patients who are prescribed both topical and injected corticosteroids, as was observed in 9.9% of patients,” they added.
Frequencies of minoxidil and tacrolimus use were nearly identical even though tacrolimus has been found ineffectivein alopecia areata, according to the researchers.
“Patients may be hesitant to use minoxidil since it is only FDA-approved for androgenetic alopecia and not for alopecia areata,” they wrote. Minoxidil also is available over-the-counter, which could explain its scarcity in the dataset, they added.
Galderma Laboratories helped fund the work through an unrestricted educational grant. Mr. Farhangian declared no competing interests. Senior author Dr. Steven Feldman reported relationships with Galderma, Janssen, Taro, Abbott Labs, and a number of other pharmaceutical companies. Dr. Feldman also reported holding stock in Causa Research and Medical Quality Enhancement Corporation. Another coauthor reported relationships with several pharmaceutical companies.
FROM JOURNAL OF DRUGS IN DERMATOLOGY