User login
2015 ACR RA guidelines criticized on steroid, HBV screening, cancer history advice
Rheumatologists have criticized what they described as omissions and problems with the 2015 American College of Rheumatology guidelines for treating rheumatoid arthritis.
Although the authors (Arthritis Care Res. 2016;68[1]:1-25) evaluated evidence with GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methods and solicited public feedback on core questions, the final document minimized the use of early low-dose glucocorticoids, failed to address screening for hepatitis B virus (HBV) infection before starting biologics, and underestimated their risks in patients with a history of cancer or lymphoproliferative disease, according to separate editorial letters published in Arthritis Care & Research.
Although the guidelines recommend initial methotrexate monotherapy regardless of disease activity level, “experienced clinicians know that before any effect of the methotrexate is realized, the patient will experience joint pain, swelling, functional impairment, and morning stiffness, making the patient quite miserable,” wrote Dr. Doyt L. Conn of Emory University, Atlanta. Patients will then self-treat with NSAIDs, he added (Arthritis Care Res. 2016 Feb 11. doi: 10.1002/acr.22864). “Do the authors of the 2015 ACR guidelines think that NSAIDs are as effective as and safer than low dose prednisone?” Furthermore, the guidelines seem to rank tumor necrosis factor (TNF) inhibitors and non-TNF biologics above short-term, low-dose prednisone, he wrote. “Do the authors really mean that?’’
In a reply letter (Arthritis Care Res. Feb 11. doi: 10.1002/acr.22862), Dr. Jasvinder A. Singh of the University of Alabama at Birmingham and guideline coauthors denied recommending a “rigid” treatment sequence. They recommend short-term, low-dose steroids any time after initial disease-modifying antirheumatic drug (DMARD) therapy if disease activity remains moderate or high, or during flares, they wrote. “The guideline does not mandate that patients must fail any particular therapy before glucocorticoid can be given. It merely suggests that a DMARD should be tried first.”
Regarding HBV screening, Dr. Leonard H. Calabrese was “disappointed” to see no changes since the 2008 ACR RA guidance (Arthritis Care Res. Feb 11. doi: 10.1002/acr.22865). One biologic, rituximab, now has a black box warning for potentially fatal HBV reactivation, mandating HBV screening before its use, said Dr. Calabrese, of the Cleveland Clinic. “We suggest that the standards of screening for and prevention of HBV reactivation have changed dramatically, and assert that the ACR guidelines are accordingly overdue for changes,” he wrote.
Dr. Singh and colleagues replied that viral hepatitis screening was “vital,” but that “it was not our charge – nor was it feasible – to cover every topic relevant to the care of RA patients in this guideline.” The field lacks data on the cost-effectiveness of universally screening RA patients for HBV before starting biologics, they added. They recommended working with hepatology/gastroenterology providers to manage RA patients with chronic viral hepatitis who need potentially immunosuppressive therapies.
Finally, the guidelines cite relatively small observational studies when addressing the use of biologics in patients with a history of cancer or lymphoproliferative disorders, wrote Dr. Hasan Yazici of Academic Hospital, Istanbul, Turkey, and his associates. Interpreting these studies as negating risk is especially concerning because of “depletion of the susceptibles bias,” when one takes into consideration that one-sixth of patients with cancer have a second or higher order primary cancer; that most national registries do not differentiate between a first primary cancer and second or higher order primary cancer in their cancer incidence rates in the general population; and that RA patients on biologics probably have no cancer history. This leads to skewed results when comparing standardized incidence ratios for cancer in TNF inhibitor users versus the general population, they added (Arthritis Care Res. 2016 Feb 11. doi: 10.1002/acr.22863).
Dr. Singh and colleagues responded that “the 2015 recommendations for RA treatment in persons with past lymphoproliferative disorders or solid cancers, are conditional, not strong.” Because of the lack of evidence establishing risk in these patients, the voting panel recommended treating them the same way as other patients, they added. “The panel recognized, and the readership of these guidelines should also understand, that lack of evidence of difference does not imply an evidence of lack of difference.” They called for better studies of DMARDs and biologics in RA patients with current or historical hepatitis, cancer, heart failure, and serious infections.
Going forward, the ACR is considering how to better publicize its 30-day public comment period when developing future guidelines to better capture perspectives at the beginning, instead of at the end when GRADE protocols preclude further adjustments, Dr. Singh and his associates wrote. In addition, the ACR will broaden its RA guidelines, post drafts on its website for comment, and use a “dynamic” process “to ensure timeliness, more frequent updating, online updates, and approaches to harmonize with recommendations of other professional organizations, as needed.”
None of these authors reported funding sources or conflicts of interest.
Rheumatologists have criticized what they described as omissions and problems with the 2015 American College of Rheumatology guidelines for treating rheumatoid arthritis.
Although the authors (Arthritis Care Res. 2016;68[1]:1-25) evaluated evidence with GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methods and solicited public feedback on core questions, the final document minimized the use of early low-dose glucocorticoids, failed to address screening for hepatitis B virus (HBV) infection before starting biologics, and underestimated their risks in patients with a history of cancer or lymphoproliferative disease, according to separate editorial letters published in Arthritis Care & Research.
Although the guidelines recommend initial methotrexate monotherapy regardless of disease activity level, “experienced clinicians know that before any effect of the methotrexate is realized, the patient will experience joint pain, swelling, functional impairment, and morning stiffness, making the patient quite miserable,” wrote Dr. Doyt L. Conn of Emory University, Atlanta. Patients will then self-treat with NSAIDs, he added (Arthritis Care Res. 2016 Feb 11. doi: 10.1002/acr.22864). “Do the authors of the 2015 ACR guidelines think that NSAIDs are as effective as and safer than low dose prednisone?” Furthermore, the guidelines seem to rank tumor necrosis factor (TNF) inhibitors and non-TNF biologics above short-term, low-dose prednisone, he wrote. “Do the authors really mean that?’’
In a reply letter (Arthritis Care Res. Feb 11. doi: 10.1002/acr.22862), Dr. Jasvinder A. Singh of the University of Alabama at Birmingham and guideline coauthors denied recommending a “rigid” treatment sequence. They recommend short-term, low-dose steroids any time after initial disease-modifying antirheumatic drug (DMARD) therapy if disease activity remains moderate or high, or during flares, they wrote. “The guideline does not mandate that patients must fail any particular therapy before glucocorticoid can be given. It merely suggests that a DMARD should be tried first.”
Regarding HBV screening, Dr. Leonard H. Calabrese was “disappointed” to see no changes since the 2008 ACR RA guidance (Arthritis Care Res. Feb 11. doi: 10.1002/acr.22865). One biologic, rituximab, now has a black box warning for potentially fatal HBV reactivation, mandating HBV screening before its use, said Dr. Calabrese, of the Cleveland Clinic. “We suggest that the standards of screening for and prevention of HBV reactivation have changed dramatically, and assert that the ACR guidelines are accordingly overdue for changes,” he wrote.
Dr. Singh and colleagues replied that viral hepatitis screening was “vital,” but that “it was not our charge – nor was it feasible – to cover every topic relevant to the care of RA patients in this guideline.” The field lacks data on the cost-effectiveness of universally screening RA patients for HBV before starting biologics, they added. They recommended working with hepatology/gastroenterology providers to manage RA patients with chronic viral hepatitis who need potentially immunosuppressive therapies.
Finally, the guidelines cite relatively small observational studies when addressing the use of biologics in patients with a history of cancer or lymphoproliferative disorders, wrote Dr. Hasan Yazici of Academic Hospital, Istanbul, Turkey, and his associates. Interpreting these studies as negating risk is especially concerning because of “depletion of the susceptibles bias,” when one takes into consideration that one-sixth of patients with cancer have a second or higher order primary cancer; that most national registries do not differentiate between a first primary cancer and second or higher order primary cancer in their cancer incidence rates in the general population; and that RA patients on biologics probably have no cancer history. This leads to skewed results when comparing standardized incidence ratios for cancer in TNF inhibitor users versus the general population, they added (Arthritis Care Res. 2016 Feb 11. doi: 10.1002/acr.22863).
Dr. Singh and colleagues responded that “the 2015 recommendations for RA treatment in persons with past lymphoproliferative disorders or solid cancers, are conditional, not strong.” Because of the lack of evidence establishing risk in these patients, the voting panel recommended treating them the same way as other patients, they added. “The panel recognized, and the readership of these guidelines should also understand, that lack of evidence of difference does not imply an evidence of lack of difference.” They called for better studies of DMARDs and biologics in RA patients with current or historical hepatitis, cancer, heart failure, and serious infections.
Going forward, the ACR is considering how to better publicize its 30-day public comment period when developing future guidelines to better capture perspectives at the beginning, instead of at the end when GRADE protocols preclude further adjustments, Dr. Singh and his associates wrote. In addition, the ACR will broaden its RA guidelines, post drafts on its website for comment, and use a “dynamic” process “to ensure timeliness, more frequent updating, online updates, and approaches to harmonize with recommendations of other professional organizations, as needed.”
None of these authors reported funding sources or conflicts of interest.
Rheumatologists have criticized what they described as omissions and problems with the 2015 American College of Rheumatology guidelines for treating rheumatoid arthritis.
Although the authors (Arthritis Care Res. 2016;68[1]:1-25) evaluated evidence with GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methods and solicited public feedback on core questions, the final document minimized the use of early low-dose glucocorticoids, failed to address screening for hepatitis B virus (HBV) infection before starting biologics, and underestimated their risks in patients with a history of cancer or lymphoproliferative disease, according to separate editorial letters published in Arthritis Care & Research.
Although the guidelines recommend initial methotrexate monotherapy regardless of disease activity level, “experienced clinicians know that before any effect of the methotrexate is realized, the patient will experience joint pain, swelling, functional impairment, and morning stiffness, making the patient quite miserable,” wrote Dr. Doyt L. Conn of Emory University, Atlanta. Patients will then self-treat with NSAIDs, he added (Arthritis Care Res. 2016 Feb 11. doi: 10.1002/acr.22864). “Do the authors of the 2015 ACR guidelines think that NSAIDs are as effective as and safer than low dose prednisone?” Furthermore, the guidelines seem to rank tumor necrosis factor (TNF) inhibitors and non-TNF biologics above short-term, low-dose prednisone, he wrote. “Do the authors really mean that?’’
In a reply letter (Arthritis Care Res. Feb 11. doi: 10.1002/acr.22862), Dr. Jasvinder A. Singh of the University of Alabama at Birmingham and guideline coauthors denied recommending a “rigid” treatment sequence. They recommend short-term, low-dose steroids any time after initial disease-modifying antirheumatic drug (DMARD) therapy if disease activity remains moderate or high, or during flares, they wrote. “The guideline does not mandate that patients must fail any particular therapy before glucocorticoid can be given. It merely suggests that a DMARD should be tried first.”
Regarding HBV screening, Dr. Leonard H. Calabrese was “disappointed” to see no changes since the 2008 ACR RA guidance (Arthritis Care Res. Feb 11. doi: 10.1002/acr.22865). One biologic, rituximab, now has a black box warning for potentially fatal HBV reactivation, mandating HBV screening before its use, said Dr. Calabrese, of the Cleveland Clinic. “We suggest that the standards of screening for and prevention of HBV reactivation have changed dramatically, and assert that the ACR guidelines are accordingly overdue for changes,” he wrote.
Dr. Singh and colleagues replied that viral hepatitis screening was “vital,” but that “it was not our charge – nor was it feasible – to cover every topic relevant to the care of RA patients in this guideline.” The field lacks data on the cost-effectiveness of universally screening RA patients for HBV before starting biologics, they added. They recommended working with hepatology/gastroenterology providers to manage RA patients with chronic viral hepatitis who need potentially immunosuppressive therapies.
Finally, the guidelines cite relatively small observational studies when addressing the use of biologics in patients with a history of cancer or lymphoproliferative disorders, wrote Dr. Hasan Yazici of Academic Hospital, Istanbul, Turkey, and his associates. Interpreting these studies as negating risk is especially concerning because of “depletion of the susceptibles bias,” when one takes into consideration that one-sixth of patients with cancer have a second or higher order primary cancer; that most national registries do not differentiate between a first primary cancer and second or higher order primary cancer in their cancer incidence rates in the general population; and that RA patients on biologics probably have no cancer history. This leads to skewed results when comparing standardized incidence ratios for cancer in TNF inhibitor users versus the general population, they added (Arthritis Care Res. 2016 Feb 11. doi: 10.1002/acr.22863).
Dr. Singh and colleagues responded that “the 2015 recommendations for RA treatment in persons with past lymphoproliferative disorders or solid cancers, are conditional, not strong.” Because of the lack of evidence establishing risk in these patients, the voting panel recommended treating them the same way as other patients, they added. “The panel recognized, and the readership of these guidelines should also understand, that lack of evidence of difference does not imply an evidence of lack of difference.” They called for better studies of DMARDs and biologics in RA patients with current or historical hepatitis, cancer, heart failure, and serious infections.
Going forward, the ACR is considering how to better publicize its 30-day public comment period when developing future guidelines to better capture perspectives at the beginning, instead of at the end when GRADE protocols preclude further adjustments, Dr. Singh and his associates wrote. In addition, the ACR will broaden its RA guidelines, post drafts on its website for comment, and use a “dynamic” process “to ensure timeliness, more frequent updating, online updates, and approaches to harmonize with recommendations of other professional organizations, as needed.”
None of these authors reported funding sources or conflicts of interest.
Influenza linked to atrial fibrillation in large observational study
A diagnosis of influenza increased the risk of subsequent atrial fibrillation by about 18%, investigators reported online in Heart Rhythm.
Clinicians therefore should consider atrial fibrillation (AF) in patients with influenza-like symptoms who report palpitations or experience an ischemic stroke, said Dr. Ting-Yung Chang of Taipei Veterans General Hospital in Taiwan and his associates. Influenza vaccination might help prevent AF, and high-risk patients should be encouraged to receive the vaccination annually, they said. However, a large prospective study is needed to clarify whether influenza vaccination reduces the risk of AF and subsequent ischemic stroke and systemic thromboembolic events, they added.
Atrial fibrillation increases the risk of stroke about fivefold, triples the risk of heart failure, and doubles the chances of dementia and death, the researchers noted. Mounting evidence implicates inflammation and sympathetic nervous system dysregulation in the pathogenesis of AF, raising questions about whether influenza might underlie or contribute to some cases of AF. To explore relationships among AF, influenza, and influenza vaccination, the investigators analyzed data for 11,374 patients with AF who were enrolled in the Taiwan National Health Insurance Research Database between 2000 and 2010. They matched each patient with AF to four controls based on age, sex, enrollment date, and the Charlson comorbidity index (
Heart Rhythm. 2016 Feb. doi: 10.1016/j.hrthm.2016.01.026
).
Unvaccinated patients with influenza were 18% more likely to develop AF than unvaccinated patients without influenza (odds ratio, 1.18; 95% confidence interval, 1.01-1.38; P = .032), even after adjusting for demographic factors, medical history, and use of relevant health care services, the researchers reported. In contrast, vaccinated patients who later developed influenza were about as likely to develop AF as unvaccinated patients who did not develop influenza, both in the overall analysis and in subgroups stratified by age, sex, and comorbidities. Moreover, vaccinated patients without influenza were even less likely to develop AF than unvaccinated patients without influenza (OR, 0.88; 95% CI, 0.84-0.93; P less than .001).
The registry database excluded relevant data on smoking history, body mass index, and physical activity level, the researchers said. “Influenza infection was diagnosed using ICD-9 codes with concomitant use of antiviral agents, and was not further confirmed based on the results of viral culture with throat swab,” they added. “The diagnostic accuracy of influenza infection cannot be fully ascertained.”
The National Science Council and the Taipei Veterans General Hospital funded the study. The researchers had no disclosures.
The authors readily acknowledge the limitations of [this] large, observational study using an insurance database. Despite these admitted limitations, the authors should be commended on adding to the literature regarding modifiable risk factor reduction for the prevention of AF. Recently, a growing body of literature has examined this topic with several straightforward yet promising interventions identified. Weight loss, moderate exercise, and treatment for underlying obstructive sleep apnea have all been shown to reduce the risk of atrial fibrillation incidence or recurrence. Influenza vaccination could represent another simple, cost‐effective intervention to prevent AF. Although the flu vaccine is already recommended for many patient groups, this study suggests that there are even more potential public health benefits of the vaccine.
Dr. Bradley P. Knight is with the division of cardiology, department of medicine, at Northwestern University, Chicago. He had no disclosures. These comments were adapted from his editorial (Heart Rhythm. 2016 Feb. doi: 10.1016/j.hrthm.2016.01.025).
The authors readily acknowledge the limitations of [this] large, observational study using an insurance database. Despite these admitted limitations, the authors should be commended on adding to the literature regarding modifiable risk factor reduction for the prevention of AF. Recently, a growing body of literature has examined this topic with several straightforward yet promising interventions identified. Weight loss, moderate exercise, and treatment for underlying obstructive sleep apnea have all been shown to reduce the risk of atrial fibrillation incidence or recurrence. Influenza vaccination could represent another simple, cost‐effective intervention to prevent AF. Although the flu vaccine is already recommended for many patient groups, this study suggests that there are even more potential public health benefits of the vaccine.
Dr. Bradley P. Knight is with the division of cardiology, department of medicine, at Northwestern University, Chicago. He had no disclosures. These comments were adapted from his editorial (Heart Rhythm. 2016 Feb. doi: 10.1016/j.hrthm.2016.01.025).
The authors readily acknowledge the limitations of [this] large, observational study using an insurance database. Despite these admitted limitations, the authors should be commended on adding to the literature regarding modifiable risk factor reduction for the prevention of AF. Recently, a growing body of literature has examined this topic with several straightforward yet promising interventions identified. Weight loss, moderate exercise, and treatment for underlying obstructive sleep apnea have all been shown to reduce the risk of atrial fibrillation incidence or recurrence. Influenza vaccination could represent another simple, cost‐effective intervention to prevent AF. Although the flu vaccine is already recommended for many patient groups, this study suggests that there are even more potential public health benefits of the vaccine.
Dr. Bradley P. Knight is with the division of cardiology, department of medicine, at Northwestern University, Chicago. He had no disclosures. These comments were adapted from his editorial (Heart Rhythm. 2016 Feb. doi: 10.1016/j.hrthm.2016.01.025).
A diagnosis of influenza increased the risk of subsequent atrial fibrillation by about 18%, investigators reported online in Heart Rhythm.
Clinicians therefore should consider atrial fibrillation (AF) in patients with influenza-like symptoms who report palpitations or experience an ischemic stroke, said Dr. Ting-Yung Chang of Taipei Veterans General Hospital in Taiwan and his associates. Influenza vaccination might help prevent AF, and high-risk patients should be encouraged to receive the vaccination annually, they said. However, a large prospective study is needed to clarify whether influenza vaccination reduces the risk of AF and subsequent ischemic stroke and systemic thromboembolic events, they added.
Atrial fibrillation increases the risk of stroke about fivefold, triples the risk of heart failure, and doubles the chances of dementia and death, the researchers noted. Mounting evidence implicates inflammation and sympathetic nervous system dysregulation in the pathogenesis of AF, raising questions about whether influenza might underlie or contribute to some cases of AF. To explore relationships among AF, influenza, and influenza vaccination, the investigators analyzed data for 11,374 patients with AF who were enrolled in the Taiwan National Health Insurance Research Database between 2000 and 2010. They matched each patient with AF to four controls based on age, sex, enrollment date, and the Charlson comorbidity index (
Heart Rhythm. 2016 Feb. doi: 10.1016/j.hrthm.2016.01.026
).
Unvaccinated patients with influenza were 18% more likely to develop AF than unvaccinated patients without influenza (odds ratio, 1.18; 95% confidence interval, 1.01-1.38; P = .032), even after adjusting for demographic factors, medical history, and use of relevant health care services, the researchers reported. In contrast, vaccinated patients who later developed influenza were about as likely to develop AF as unvaccinated patients who did not develop influenza, both in the overall analysis and in subgroups stratified by age, sex, and comorbidities. Moreover, vaccinated patients without influenza were even less likely to develop AF than unvaccinated patients without influenza (OR, 0.88; 95% CI, 0.84-0.93; P less than .001).
The registry database excluded relevant data on smoking history, body mass index, and physical activity level, the researchers said. “Influenza infection was diagnosed using ICD-9 codes with concomitant use of antiviral agents, and was not further confirmed based on the results of viral culture with throat swab,” they added. “The diagnostic accuracy of influenza infection cannot be fully ascertained.”
The National Science Council and the Taipei Veterans General Hospital funded the study. The researchers had no disclosures.
A diagnosis of influenza increased the risk of subsequent atrial fibrillation by about 18%, investigators reported online in Heart Rhythm.
Clinicians therefore should consider atrial fibrillation (AF) in patients with influenza-like symptoms who report palpitations or experience an ischemic stroke, said Dr. Ting-Yung Chang of Taipei Veterans General Hospital in Taiwan and his associates. Influenza vaccination might help prevent AF, and high-risk patients should be encouraged to receive the vaccination annually, they said. However, a large prospective study is needed to clarify whether influenza vaccination reduces the risk of AF and subsequent ischemic stroke and systemic thromboembolic events, they added.
Atrial fibrillation increases the risk of stroke about fivefold, triples the risk of heart failure, and doubles the chances of dementia and death, the researchers noted. Mounting evidence implicates inflammation and sympathetic nervous system dysregulation in the pathogenesis of AF, raising questions about whether influenza might underlie or contribute to some cases of AF. To explore relationships among AF, influenza, and influenza vaccination, the investigators analyzed data for 11,374 patients with AF who were enrolled in the Taiwan National Health Insurance Research Database between 2000 and 2010. They matched each patient with AF to four controls based on age, sex, enrollment date, and the Charlson comorbidity index (
Heart Rhythm. 2016 Feb. doi: 10.1016/j.hrthm.2016.01.026
).
Unvaccinated patients with influenza were 18% more likely to develop AF than unvaccinated patients without influenza (odds ratio, 1.18; 95% confidence interval, 1.01-1.38; P = .032), even after adjusting for demographic factors, medical history, and use of relevant health care services, the researchers reported. In contrast, vaccinated patients who later developed influenza were about as likely to develop AF as unvaccinated patients who did not develop influenza, both in the overall analysis and in subgroups stratified by age, sex, and comorbidities. Moreover, vaccinated patients without influenza were even less likely to develop AF than unvaccinated patients without influenza (OR, 0.88; 95% CI, 0.84-0.93; P less than .001).
The registry database excluded relevant data on smoking history, body mass index, and physical activity level, the researchers said. “Influenza infection was diagnosed using ICD-9 codes with concomitant use of antiviral agents, and was not further confirmed based on the results of viral culture with throat swab,” they added. “The diagnostic accuracy of influenza infection cannot be fully ascertained.”
The National Science Council and the Taipei Veterans General Hospital funded the study. The researchers had no disclosures.
Key clinical point: Influenza might underlie some cases of atrial fibrillation.
Major finding: Among unvaccinated patients, an influenza diagnosis increased the odds of atrial fibrillation by 18% (OR, 1.18; P = .03).
Data source: An observational registry study of 11,374 patients with atrial fibrillation and 45,496 healthy controls.
Disclosures: The National Science Council and the Taipei Veterans General Hospital funded the study. The researchers had no disclosures.
Epoetin alfa missed its safety endpoint in metastatic breast cancer
A randomized phase III trial failed to allay safety concerns about the use of erythropoietin-stimulating agents in cancer patients, researchers reported online Feb. 8 in the Journal of Clinical Oncology.
The analysis could not rule out a 15% increase in the risk of progressive disease or death when women with metastatic breast cancer received epoetin alfa (EPO) instead of best standard of care for anemia, said Dr. Brian Leyland-Jones of Avera Cancer Institute in Sioux Falls, S.D., and his associates. Red blood cell transfusions should remain the preferred treatment for anemia in these patients, and any use of epoetin alfa for advanced cases “should be done with caution and based on careful risk-benefit assessment,” the researchers said.
Erythropoietin-stimulating agents can effectively treat cancer-associated anemia but have been linked to worse survival and locoregional control. However, the agents were used off label in several of these trials, the researchers noted. Therefore, they studied 2,098 women undergoing first- or second-line chemotherapy for metastatic breast cancer who had less than 11 mg/dL hemoglobin, an ECOG performance status of 0 or 1, and a life expectancy of at least 6 months. They randomly assigned patients to receive either standard treatment or 40,000 IU EPO once weekly until disease progression or the end of chemotherapy (J Clin Onc. 2016 Feb 8. doi: 10.1200/JCO.2015.63.5649). Median progression-free survival (PFS) was 7.4 months in both groups, but the EPO group was 9% more likely to die or develop progressive disease during the study, and the upper bound of the hazard ratio exceeded the prespecified noninferiority margin of 1.15 (hazard ratio, 1.089; 95% confidence interval, 0.988-1.200). An independent review committee calculated a median PFS of 7.6 months for both groups, and a hazard ratio whose upper bound fell just within the prespecified noninferiority margin (1.146). The EPO group needed about half as many red blood cell transfusions as did the control group (P less than .001), but experienced twice as many thrombotic vascular events (2.8% vs. 1.4%; P = .04).
“The results of this study do not suggest any new safety signal associated with EPO treatment and are consistent with the known safety risk to patients,” the researchers concluded. An ongoing randomized phase III study comparing darbepoetin with best standard of care for anemia in patients undergoing platinum-based treatment of stage IV non–small cell lung cancer “will further inform the benefit-risk profile of erythropoietin-stimulating agents in the oncology setting,” they said.
A randomized phase III trial failed to allay safety concerns about the use of erythropoietin-stimulating agents in cancer patients, researchers reported online Feb. 8 in the Journal of Clinical Oncology.
The analysis could not rule out a 15% increase in the risk of progressive disease or death when women with metastatic breast cancer received epoetin alfa (EPO) instead of best standard of care for anemia, said Dr. Brian Leyland-Jones of Avera Cancer Institute in Sioux Falls, S.D., and his associates. Red blood cell transfusions should remain the preferred treatment for anemia in these patients, and any use of epoetin alfa for advanced cases “should be done with caution and based on careful risk-benefit assessment,” the researchers said.
Erythropoietin-stimulating agents can effectively treat cancer-associated anemia but have been linked to worse survival and locoregional control. However, the agents were used off label in several of these trials, the researchers noted. Therefore, they studied 2,098 women undergoing first- or second-line chemotherapy for metastatic breast cancer who had less than 11 mg/dL hemoglobin, an ECOG performance status of 0 or 1, and a life expectancy of at least 6 months. They randomly assigned patients to receive either standard treatment or 40,000 IU EPO once weekly until disease progression or the end of chemotherapy (J Clin Onc. 2016 Feb 8. doi: 10.1200/JCO.2015.63.5649). Median progression-free survival (PFS) was 7.4 months in both groups, but the EPO group was 9% more likely to die or develop progressive disease during the study, and the upper bound of the hazard ratio exceeded the prespecified noninferiority margin of 1.15 (hazard ratio, 1.089; 95% confidence interval, 0.988-1.200). An independent review committee calculated a median PFS of 7.6 months for both groups, and a hazard ratio whose upper bound fell just within the prespecified noninferiority margin (1.146). The EPO group needed about half as many red blood cell transfusions as did the control group (P less than .001), but experienced twice as many thrombotic vascular events (2.8% vs. 1.4%; P = .04).
“The results of this study do not suggest any new safety signal associated with EPO treatment and are consistent with the known safety risk to patients,” the researchers concluded. An ongoing randomized phase III study comparing darbepoetin with best standard of care for anemia in patients undergoing platinum-based treatment of stage IV non–small cell lung cancer “will further inform the benefit-risk profile of erythropoietin-stimulating agents in the oncology setting,” they said.
A randomized phase III trial failed to allay safety concerns about the use of erythropoietin-stimulating agents in cancer patients, researchers reported online Feb. 8 in the Journal of Clinical Oncology.
The analysis could not rule out a 15% increase in the risk of progressive disease or death when women with metastatic breast cancer received epoetin alfa (EPO) instead of best standard of care for anemia, said Dr. Brian Leyland-Jones of Avera Cancer Institute in Sioux Falls, S.D., and his associates. Red blood cell transfusions should remain the preferred treatment for anemia in these patients, and any use of epoetin alfa for advanced cases “should be done with caution and based on careful risk-benefit assessment,” the researchers said.
Erythropoietin-stimulating agents can effectively treat cancer-associated anemia but have been linked to worse survival and locoregional control. However, the agents were used off label in several of these trials, the researchers noted. Therefore, they studied 2,098 women undergoing first- or second-line chemotherapy for metastatic breast cancer who had less than 11 mg/dL hemoglobin, an ECOG performance status of 0 or 1, and a life expectancy of at least 6 months. They randomly assigned patients to receive either standard treatment or 40,000 IU EPO once weekly until disease progression or the end of chemotherapy (J Clin Onc. 2016 Feb 8. doi: 10.1200/JCO.2015.63.5649). Median progression-free survival (PFS) was 7.4 months in both groups, but the EPO group was 9% more likely to die or develop progressive disease during the study, and the upper bound of the hazard ratio exceeded the prespecified noninferiority margin of 1.15 (hazard ratio, 1.089; 95% confidence interval, 0.988-1.200). An independent review committee calculated a median PFS of 7.6 months for both groups, and a hazard ratio whose upper bound fell just within the prespecified noninferiority margin (1.146). The EPO group needed about half as many red blood cell transfusions as did the control group (P less than .001), but experienced twice as many thrombotic vascular events (2.8% vs. 1.4%; P = .04).
“The results of this study do not suggest any new safety signal associated with EPO treatment and are consistent with the known safety risk to patients,” the researchers concluded. An ongoing randomized phase III study comparing darbepoetin with best standard of care for anemia in patients undergoing platinum-based treatment of stage IV non–small cell lung cancer “will further inform the benefit-risk profile of erythropoietin-stimulating agents in the oncology setting,” they said.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: The erythropoietin-stimulating agent epoetin alfa was associated with lower rates of progression-free survival, compared with best standard of care for anemia in women with metastatic breast cancer.
Major finding: The 95% confidence interval for the hazard ratio had an upper limit of 1.20, exceeding the prespecified noninferiority margin of 1.15.
Data source: An open-label, randomized, controlled, noninferiority trial of 2,098 patients.
Disclosures: Janssen Research and Development makes epoetin alfa and supported the study. Dr. Leyland-Jones reported receiving honoraria from Janssen Research and Development, and other funding from Genentech, GlaxoSmithKline, Amgen, and Johnson & Johnson. Seven coinvestigators reported employment with Janssen Research and Development. The other 15 coinvestigators had no disclosures.
HIV care disparities remain stark for African Americans
Only 38% of African Americans newly diagnosed with HIV infection received consistent care during the next 3 years, compared with half of Hispanic/Latino and non-Hispanic white patients, investigators reported. The results were published online Feb. 4 in Morbidity and Mortality Weekly Report.
The care gap affected African Americans of all genders, regardless of how they were infected, said Dr. Sharoda Dasgupta and her associates at the Centers for Disease Control and Prevention. Moreover, although African Americans make up just 12% of the United States population, they comprised 45% of newly diagnosed HIV infections in 2013, the researchers said. “Racial and ethnic disparities in HIV care limit access to antiretroviral therapy, perpetuating disparities in survival and reduced HIV transmission,” they added.
Consistent HIV care is essential for long-term viral suppression, which not only improves individual outcomes but helps prevent HIV transmission. To parse out retention in care by race and ethnicity, the researchers analyzed National HIV Surveillance System data on patients who were diagnosed with HIV infection in 2010 and remained alive in 2013. They found that proportionately fewer blacks were retained in care for each year analyzed. Retention in care was even less common for black male patients (35%) than black females (44%), particularly if black males injected drugs (33%) or injected drugs and had sex with other men (26%) (Morb Mortal Wkly Rep. 2016;65[4]:77-82).
Efforts to promote early diagnosis and linkage to care for African Americans might help reduce these disparities, the researchers said. They offered no new ideas, but recommended “continued collaboration among health care providers, community-based organizations, and state and local health departments [to] strengthen programs that support both early linkage to care after HIV diagnosis across all racial and ethnic groups, and expansion of proven methods for improving retention in care.”
Historically, African American women have faced especially high burdens related to HIV infection, and that disparity persists, according to another study by CDC investigators. Dr. Renee Stein and her associates analyzed national data on HIV testing events and prevention services that were funded by the CDC and led by state and local health departments and community-based organizations between 2012 and 2014 (Morb Mortal Wkly Rep. 2016;65[4]:83-5).
Testing events for black women fell by 8% during this period, despite the fact that they made up 62% of all new diagnoses of HIV infection in 2014 and experienced no decline in infection rate, the researchers said. Although the percentage of black females who were linked to HIV care within 90 days of diagnosis rose from 34% to 50%, that proportion remained well below the White House goal of 85%.
The investigators recommended boosting HIV testing among black females to raise awareness of HIV status and “ensure that every black female with HIV infection is linked to HIV medical care soon after her diagnosis, is retained in care, and achieves viral suppression.”
The investigators in both studies made no disclosures.
Only 38% of African Americans newly diagnosed with HIV infection received consistent care during the next 3 years, compared with half of Hispanic/Latino and non-Hispanic white patients, investigators reported. The results were published online Feb. 4 in Morbidity and Mortality Weekly Report.
The care gap affected African Americans of all genders, regardless of how they were infected, said Dr. Sharoda Dasgupta and her associates at the Centers for Disease Control and Prevention. Moreover, although African Americans make up just 12% of the United States population, they comprised 45% of newly diagnosed HIV infections in 2013, the researchers said. “Racial and ethnic disparities in HIV care limit access to antiretroviral therapy, perpetuating disparities in survival and reduced HIV transmission,” they added.
Consistent HIV care is essential for long-term viral suppression, which not only improves individual outcomes but helps prevent HIV transmission. To parse out retention in care by race and ethnicity, the researchers analyzed National HIV Surveillance System data on patients who were diagnosed with HIV infection in 2010 and remained alive in 2013. They found that proportionately fewer blacks were retained in care for each year analyzed. Retention in care was even less common for black male patients (35%) than black females (44%), particularly if black males injected drugs (33%) or injected drugs and had sex with other men (26%) (Morb Mortal Wkly Rep. 2016;65[4]:77-82).
Efforts to promote early diagnosis and linkage to care for African Americans might help reduce these disparities, the researchers said. They offered no new ideas, but recommended “continued collaboration among health care providers, community-based organizations, and state and local health departments [to] strengthen programs that support both early linkage to care after HIV diagnosis across all racial and ethnic groups, and expansion of proven methods for improving retention in care.”
Historically, African American women have faced especially high burdens related to HIV infection, and that disparity persists, according to another study by CDC investigators. Dr. Renee Stein and her associates analyzed national data on HIV testing events and prevention services that were funded by the CDC and led by state and local health departments and community-based organizations between 2012 and 2014 (Morb Mortal Wkly Rep. 2016;65[4]:83-5).
Testing events for black women fell by 8% during this period, despite the fact that they made up 62% of all new diagnoses of HIV infection in 2014 and experienced no decline in infection rate, the researchers said. Although the percentage of black females who were linked to HIV care within 90 days of diagnosis rose from 34% to 50%, that proportion remained well below the White House goal of 85%.
The investigators recommended boosting HIV testing among black females to raise awareness of HIV status and “ensure that every black female with HIV infection is linked to HIV medical care soon after her diagnosis, is retained in care, and achieves viral suppression.”
The investigators in both studies made no disclosures.
Only 38% of African Americans newly diagnosed with HIV infection received consistent care during the next 3 years, compared with half of Hispanic/Latino and non-Hispanic white patients, investigators reported. The results were published online Feb. 4 in Morbidity and Mortality Weekly Report.
The care gap affected African Americans of all genders, regardless of how they were infected, said Dr. Sharoda Dasgupta and her associates at the Centers for Disease Control and Prevention. Moreover, although African Americans make up just 12% of the United States population, they comprised 45% of newly diagnosed HIV infections in 2013, the researchers said. “Racial and ethnic disparities in HIV care limit access to antiretroviral therapy, perpetuating disparities in survival and reduced HIV transmission,” they added.
Consistent HIV care is essential for long-term viral suppression, which not only improves individual outcomes but helps prevent HIV transmission. To parse out retention in care by race and ethnicity, the researchers analyzed National HIV Surveillance System data on patients who were diagnosed with HIV infection in 2010 and remained alive in 2013. They found that proportionately fewer blacks were retained in care for each year analyzed. Retention in care was even less common for black male patients (35%) than black females (44%), particularly if black males injected drugs (33%) or injected drugs and had sex with other men (26%) (Morb Mortal Wkly Rep. 2016;65[4]:77-82).
Efforts to promote early diagnosis and linkage to care for African Americans might help reduce these disparities, the researchers said. They offered no new ideas, but recommended “continued collaboration among health care providers, community-based organizations, and state and local health departments [to] strengthen programs that support both early linkage to care after HIV diagnosis across all racial and ethnic groups, and expansion of proven methods for improving retention in care.”
Historically, African American women have faced especially high burdens related to HIV infection, and that disparity persists, according to another study by CDC investigators. Dr. Renee Stein and her associates analyzed national data on HIV testing events and prevention services that were funded by the CDC and led by state and local health departments and community-based organizations between 2012 and 2014 (Morb Mortal Wkly Rep. 2016;65[4]:83-5).
Testing events for black women fell by 8% during this period, despite the fact that they made up 62% of all new diagnoses of HIV infection in 2014 and experienced no decline in infection rate, the researchers said. Although the percentage of black females who were linked to HIV care within 90 days of diagnosis rose from 34% to 50%, that proportion remained well below the White House goal of 85%.
The investigators recommended boosting HIV testing among black females to raise awareness of HIV status and “ensure that every black female with HIV infection is linked to HIV medical care soon after her diagnosis, is retained in care, and achieves viral suppression.”
The investigators in both studies made no disclosures.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Key clinical point: Multiple and stark disparities in HIV care continue to affect African Americans.
Major finding: Only 38% of African-Americans newly diagnosed with HIV infection in 2010 received consistent care during the next 3 years, compared with 50% of Hispanics/Latino patients and 49% of non-Hispanic white patients.
Data source: Analyses of National HIV Surveillance System and National HIV Prevention Program Monitoring and Evaluation data.
Disclosures: The investigators in both studies made no disclosures.
New test showed promise in ocular myasthenia gravis
A test for ocular vestibular evoked myogenic potentials (oVEMP) had a sensitivity of 89% and a specificity of 64% for detecting myasthenia gravis (MG), according to a case-control study of 55 adults published online in Neurology.
“The presence of an oVEMP decrement is a sensitive and specific marker for MG,” said Dr. Yulia Valko at University Hospital Zurich in Switzerland and her associates. “This test allows direct and noninvasive examination of extraocular muscle activity, with similarly good diagnostic accuracy in ocular and generalized MG.”
Myasthenia gravis usually manifests first in the eyes, and early diagnosis and treatment can limit generalization. But nearly half of patients remain undiagnosed a year after onset, partly because standard tests often fail to detect isolated ocular MG, the researchers noted. The recently developed oVEMP test directly measures the activity of the extraocular inferior oblique muscle in response to repeated bursts of vibratory stimulation to the forehead. A decreased response, or decrement, indicates failed neuromuscular transmission, as with standard repetitive nerve stimulation. The researchers evaluated the test in 13 patients with isolated ocular MG, 14 patients with generalized MG, and 28 healthy controls. They defined the oVEMP decrement as the decrease between the second stimulus and the average of the fifth through ninth stimuli (Neurology. 2016 Jan 20. doi: 10.1212/WNL.0000000000002383).
A repetition rate of 20 Hz best differentiated between cases (average decrement, –21.5% plus or minus 29.6%) and controls (–2.8% plus or minus 16.9%), the researchers reported. When at least one eye showed a decrement, the ideal cutoff was a drop of at least 15.2%, which detected MG with a sensitivity of 89% and a sensitivity of 64%. When both eyes were affected, the ideal cutoff for the smallest of the two decrements was at least 20.4%, which yielded a sensitivity of 100% and a specificity of 63%. For both cutoffs, the test was similarly sensitive for detecting ocular and generalized MG, the investigators noted. For the unilateral cutoff, the sensitivity was 92% for patients with isolated ocular MG and 86% for patients with generalized MG. For the bilateral cutoff, specificity was 62% in ocular MG and 64% in generalized MG.
The results provide class III evidence that oVEMP can distinguish between patients with MG and healthy controls, “but future studies will need to confirm its diagnostic utility in clinical practice, where the main challenge is differentiation from patients with other neuro-opthalmologic conditions,” the researchers said. “The possibility to apply fast repetition rates is one important advantage of oVEMP, which is not possible by measuring voluntary saccadic eye movements. As a consequence, oVEMP allowed us to unmask myasthenic decrements even in clinically asymptomatic eyes,” they added.
Because the study used a confirmed diagnosis of MG as a benchmark, all patients were already being treated with cholinesterase inhibitors, the investigators noted. Although they underwent oVEMP testing in the morning before their first dose of medication, the test needs further study in drug-naïve patients, as well as in patients with worse limitations in their upward gaze, they added.
The study was funded by the University of Zurich, the Betty and David Koetser Foundation for Brain Research, the Albert Bruppacher Foundation for Eye Research, and the OPOS Foundation. The investigators had no relevant disclosures.
Autoimmune myasthenia gravis (MG) commonly presents with fatigable ptosis and diplopia. In isolation, these symptoms often herald the restricted form of the disease known as ocular MG. In some cases, ocular MG progresses to involve bulbar musculature as well as limb muscles. Because some individuals with myasthenia have the signs intermittently or may never have ptosis, the diagnosis is sometimes difficult to ascertain on clinical grounds alone.
Clinical and laboratory tests available for confirming the diagnosis have been in use for many years, as well as some recent refinements. These include serologic testing for acetylcholine receptor and MuSK antibodies; the edrophonium (Tensilon) test in which an acetylcholinesterase inhibitor is delivered intravenously to temporarily improve ptosis and diplopia; slow repetitive (electrical) nerve stimulation (RNS), particularly of proximal limb and facial nerves and single fiber electromyography (SFEMG). Each of these approaches has limitations. Antibody testing has relatively low sensitivity (in the range of 0.50-0.71 for ocular MG and 0.87-0.98 for generalized MG). For RNS, the sensitivity numbers are even less positive (0.11-0.39 for ocular MG and 0.53-0.98 for generalized MG). Even though the edrophonium test is said to have a sensitivity of 0.60-0.90, this procedure has largely fallen into disuse among neuromuscular specialists partly because of the risks of bradycardia, syncope, and even asystole, as well as high rates of false positivity. Some neurologists use an icepack on the forehead as a diagnostic substitute or so-called “poor man’s edrophonium test,” although false positive rates are considerable. SFEMG is considered the most sensitive diagnostic test for MG (sensitivity of 0.62-1.0 in ocular MG and 0.75-0.98 in generalized MG) but is technically demanding, time consuming, available almost exclusively in academic centers, and until relatively recently meant using expensive SFEMG needle electrodes requiring sterilization and periodic sharpening.

|
Dr. Benn E. Smith |
Two recent publications have introduced advances in the diagnosis of MG. The first is a report by Dr. Erik Stålberg and colleagues from Sweden, the United States, United Kingdom, Slovenia, Norway, Brazil, and Spain of normative data for concentric SFEMG using both the stimulated and the volitional techniques in the extensor digitorum, frontalis, and orbicularis oculi muscles from 59 to 92 subjects for each muscle (Muscle Nerve. 2016 Mar;53[3]:351-62). The value of this set of reference data is that neurologists who perform SFEMG now have a rigorously collected reliable set of statistically validated normal values using commercially available concentric needle electrodes as conventional single fiber needle electrodes are becoming more and more challenging to use in practice.
A second publication by Yulia Valko and colleagues from Zurich and Sydney describes the novel application of ocular vestibular myogenic potentials (oVEMP) as a new form of RNS in MG. By delivering 4-ms bursts of 500-Hz bone conducted vibration in trains of 10 stimuli and recording just below the inferior orbital rim with surface electrodes, the investigators found that a frequency of 20 Hz resulted in the cleanest separation of tracings in subjects with documented MG from age- and gender-matched healthy controls. The oVEMP technique has been in use for evaluating vestibular disorders for more than 10 years and is an accepted diagnostic technique for this purpose. While this novel approach also shows promise as a candidate diagnostic technique in evaluating extraocular neuromuscular junction dysfunction, further prospective studies are needed. By comparing the sensitivity and specificity of oVEMP RNS with that of accepted diagnostic tests, including conventional facial RNS and SFEMG, in subjects suspected of having MG, the neurology and neuromuscular communities will be in a better position to judge whether oVEMP will one day be an accepted diagnostic test for MG.
Dr. Benn E. Smith is with the department of neurology at the Mayo Clinic, Scottsdale, Ariz. He has no relevant disclosures.
Autoimmune myasthenia gravis (MG) commonly presents with fatigable ptosis and diplopia. In isolation, these symptoms often herald the restricted form of the disease known as ocular MG. In some cases, ocular MG progresses to involve bulbar musculature as well as limb muscles. Because some individuals with myasthenia have the signs intermittently or may never have ptosis, the diagnosis is sometimes difficult to ascertain on clinical grounds alone.
Clinical and laboratory tests available for confirming the diagnosis have been in use for many years, as well as some recent refinements. These include serologic testing for acetylcholine receptor and MuSK antibodies; the edrophonium (Tensilon) test in which an acetylcholinesterase inhibitor is delivered intravenously to temporarily improve ptosis and diplopia; slow repetitive (electrical) nerve stimulation (RNS), particularly of proximal limb and facial nerves and single fiber electromyography (SFEMG). Each of these approaches has limitations. Antibody testing has relatively low sensitivity (in the range of 0.50-0.71 for ocular MG and 0.87-0.98 for generalized MG). For RNS, the sensitivity numbers are even less positive (0.11-0.39 for ocular MG and 0.53-0.98 for generalized MG). Even though the edrophonium test is said to have a sensitivity of 0.60-0.90, this procedure has largely fallen into disuse among neuromuscular specialists partly because of the risks of bradycardia, syncope, and even asystole, as well as high rates of false positivity. Some neurologists use an icepack on the forehead as a diagnostic substitute or so-called “poor man’s edrophonium test,” although false positive rates are considerable. SFEMG is considered the most sensitive diagnostic test for MG (sensitivity of 0.62-1.0 in ocular MG and 0.75-0.98 in generalized MG) but is technically demanding, time consuming, available almost exclusively in academic centers, and until relatively recently meant using expensive SFEMG needle electrodes requiring sterilization and periodic sharpening.

|
Dr. Benn E. Smith |
Two recent publications have introduced advances in the diagnosis of MG. The first is a report by Dr. Erik Stålberg and colleagues from Sweden, the United States, United Kingdom, Slovenia, Norway, Brazil, and Spain of normative data for concentric SFEMG using both the stimulated and the volitional techniques in the extensor digitorum, frontalis, and orbicularis oculi muscles from 59 to 92 subjects for each muscle (Muscle Nerve. 2016 Mar;53[3]:351-62). The value of this set of reference data is that neurologists who perform SFEMG now have a rigorously collected reliable set of statistically validated normal values using commercially available concentric needle electrodes as conventional single fiber needle electrodes are becoming more and more challenging to use in practice.
A second publication by Yulia Valko and colleagues from Zurich and Sydney describes the novel application of ocular vestibular myogenic potentials (oVEMP) as a new form of RNS in MG. By delivering 4-ms bursts of 500-Hz bone conducted vibration in trains of 10 stimuli and recording just below the inferior orbital rim with surface electrodes, the investigators found that a frequency of 20 Hz resulted in the cleanest separation of tracings in subjects with documented MG from age- and gender-matched healthy controls. The oVEMP technique has been in use for evaluating vestibular disorders for more than 10 years and is an accepted diagnostic technique for this purpose. While this novel approach also shows promise as a candidate diagnostic technique in evaluating extraocular neuromuscular junction dysfunction, further prospective studies are needed. By comparing the sensitivity and specificity of oVEMP RNS with that of accepted diagnostic tests, including conventional facial RNS and SFEMG, in subjects suspected of having MG, the neurology and neuromuscular communities will be in a better position to judge whether oVEMP will one day be an accepted diagnostic test for MG.
Dr. Benn E. Smith is with the department of neurology at the Mayo Clinic, Scottsdale, Ariz. He has no relevant disclosures.
Autoimmune myasthenia gravis (MG) commonly presents with fatigable ptosis and diplopia. In isolation, these symptoms often herald the restricted form of the disease known as ocular MG. In some cases, ocular MG progresses to involve bulbar musculature as well as limb muscles. Because some individuals with myasthenia have the signs intermittently or may never have ptosis, the diagnosis is sometimes difficult to ascertain on clinical grounds alone.
Clinical and laboratory tests available for confirming the diagnosis have been in use for many years, as well as some recent refinements. These include serologic testing for acetylcholine receptor and MuSK antibodies; the edrophonium (Tensilon) test in which an acetylcholinesterase inhibitor is delivered intravenously to temporarily improve ptosis and diplopia; slow repetitive (electrical) nerve stimulation (RNS), particularly of proximal limb and facial nerves and single fiber electromyography (SFEMG). Each of these approaches has limitations. Antibody testing has relatively low sensitivity (in the range of 0.50-0.71 for ocular MG and 0.87-0.98 for generalized MG). For RNS, the sensitivity numbers are even less positive (0.11-0.39 for ocular MG and 0.53-0.98 for generalized MG). Even though the edrophonium test is said to have a sensitivity of 0.60-0.90, this procedure has largely fallen into disuse among neuromuscular specialists partly because of the risks of bradycardia, syncope, and even asystole, as well as high rates of false positivity. Some neurologists use an icepack on the forehead as a diagnostic substitute or so-called “poor man’s edrophonium test,” although false positive rates are considerable. SFEMG is considered the most sensitive diagnostic test for MG (sensitivity of 0.62-1.0 in ocular MG and 0.75-0.98 in generalized MG) but is technically demanding, time consuming, available almost exclusively in academic centers, and until relatively recently meant using expensive SFEMG needle electrodes requiring sterilization and periodic sharpening.

|
Dr. Benn E. Smith |
Two recent publications have introduced advances in the diagnosis of MG. The first is a report by Dr. Erik Stålberg and colleagues from Sweden, the United States, United Kingdom, Slovenia, Norway, Brazil, and Spain of normative data for concentric SFEMG using both the stimulated and the volitional techniques in the extensor digitorum, frontalis, and orbicularis oculi muscles from 59 to 92 subjects for each muscle (Muscle Nerve. 2016 Mar;53[3]:351-62). The value of this set of reference data is that neurologists who perform SFEMG now have a rigorously collected reliable set of statistically validated normal values using commercially available concentric needle electrodes as conventional single fiber needle electrodes are becoming more and more challenging to use in practice.
A second publication by Yulia Valko and colleagues from Zurich and Sydney describes the novel application of ocular vestibular myogenic potentials (oVEMP) as a new form of RNS in MG. By delivering 4-ms bursts of 500-Hz bone conducted vibration in trains of 10 stimuli and recording just below the inferior orbital rim with surface electrodes, the investigators found that a frequency of 20 Hz resulted in the cleanest separation of tracings in subjects with documented MG from age- and gender-matched healthy controls. The oVEMP technique has been in use for evaluating vestibular disorders for more than 10 years and is an accepted diagnostic technique for this purpose. While this novel approach also shows promise as a candidate diagnostic technique in evaluating extraocular neuromuscular junction dysfunction, further prospective studies are needed. By comparing the sensitivity and specificity of oVEMP RNS with that of accepted diagnostic tests, including conventional facial RNS and SFEMG, in subjects suspected of having MG, the neurology and neuromuscular communities will be in a better position to judge whether oVEMP will one day be an accepted diagnostic test for MG.
Dr. Benn E. Smith is with the department of neurology at the Mayo Clinic, Scottsdale, Ariz. He has no relevant disclosures.
A test for ocular vestibular evoked myogenic potentials (oVEMP) had a sensitivity of 89% and a specificity of 64% for detecting myasthenia gravis (MG), according to a case-control study of 55 adults published online in Neurology.
“The presence of an oVEMP decrement is a sensitive and specific marker for MG,” said Dr. Yulia Valko at University Hospital Zurich in Switzerland and her associates. “This test allows direct and noninvasive examination of extraocular muscle activity, with similarly good diagnostic accuracy in ocular and generalized MG.”
Myasthenia gravis usually manifests first in the eyes, and early diagnosis and treatment can limit generalization. But nearly half of patients remain undiagnosed a year after onset, partly because standard tests often fail to detect isolated ocular MG, the researchers noted. The recently developed oVEMP test directly measures the activity of the extraocular inferior oblique muscle in response to repeated bursts of vibratory stimulation to the forehead. A decreased response, or decrement, indicates failed neuromuscular transmission, as with standard repetitive nerve stimulation. The researchers evaluated the test in 13 patients with isolated ocular MG, 14 patients with generalized MG, and 28 healthy controls. They defined the oVEMP decrement as the decrease between the second stimulus and the average of the fifth through ninth stimuli (Neurology. 2016 Jan 20. doi: 10.1212/WNL.0000000000002383).
A repetition rate of 20 Hz best differentiated between cases (average decrement, –21.5% plus or minus 29.6%) and controls (–2.8% plus or minus 16.9%), the researchers reported. When at least one eye showed a decrement, the ideal cutoff was a drop of at least 15.2%, which detected MG with a sensitivity of 89% and a sensitivity of 64%. When both eyes were affected, the ideal cutoff for the smallest of the two decrements was at least 20.4%, which yielded a sensitivity of 100% and a specificity of 63%. For both cutoffs, the test was similarly sensitive for detecting ocular and generalized MG, the investigators noted. For the unilateral cutoff, the sensitivity was 92% for patients with isolated ocular MG and 86% for patients with generalized MG. For the bilateral cutoff, specificity was 62% in ocular MG and 64% in generalized MG.
The results provide class III evidence that oVEMP can distinguish between patients with MG and healthy controls, “but future studies will need to confirm its diagnostic utility in clinical practice, where the main challenge is differentiation from patients with other neuro-opthalmologic conditions,” the researchers said. “The possibility to apply fast repetition rates is one important advantage of oVEMP, which is not possible by measuring voluntary saccadic eye movements. As a consequence, oVEMP allowed us to unmask myasthenic decrements even in clinically asymptomatic eyes,” they added.
Because the study used a confirmed diagnosis of MG as a benchmark, all patients were already being treated with cholinesterase inhibitors, the investigators noted. Although they underwent oVEMP testing in the morning before their first dose of medication, the test needs further study in drug-naïve patients, as well as in patients with worse limitations in their upward gaze, they added.
The study was funded by the University of Zurich, the Betty and David Koetser Foundation for Brain Research, the Albert Bruppacher Foundation for Eye Research, and the OPOS Foundation. The investigators had no relevant disclosures.
A test for ocular vestibular evoked myogenic potentials (oVEMP) had a sensitivity of 89% and a specificity of 64% for detecting myasthenia gravis (MG), according to a case-control study of 55 adults published online in Neurology.
“The presence of an oVEMP decrement is a sensitive and specific marker for MG,” said Dr. Yulia Valko at University Hospital Zurich in Switzerland and her associates. “This test allows direct and noninvasive examination of extraocular muscle activity, with similarly good diagnostic accuracy in ocular and generalized MG.”
Myasthenia gravis usually manifests first in the eyes, and early diagnosis and treatment can limit generalization. But nearly half of patients remain undiagnosed a year after onset, partly because standard tests often fail to detect isolated ocular MG, the researchers noted. The recently developed oVEMP test directly measures the activity of the extraocular inferior oblique muscle in response to repeated bursts of vibratory stimulation to the forehead. A decreased response, or decrement, indicates failed neuromuscular transmission, as with standard repetitive nerve stimulation. The researchers evaluated the test in 13 patients with isolated ocular MG, 14 patients with generalized MG, and 28 healthy controls. They defined the oVEMP decrement as the decrease between the second stimulus and the average of the fifth through ninth stimuli (Neurology. 2016 Jan 20. doi: 10.1212/WNL.0000000000002383).
A repetition rate of 20 Hz best differentiated between cases (average decrement, –21.5% plus or minus 29.6%) and controls (–2.8% plus or minus 16.9%), the researchers reported. When at least one eye showed a decrement, the ideal cutoff was a drop of at least 15.2%, which detected MG with a sensitivity of 89% and a sensitivity of 64%. When both eyes were affected, the ideal cutoff for the smallest of the two decrements was at least 20.4%, which yielded a sensitivity of 100% and a specificity of 63%. For both cutoffs, the test was similarly sensitive for detecting ocular and generalized MG, the investigators noted. For the unilateral cutoff, the sensitivity was 92% for patients with isolated ocular MG and 86% for patients with generalized MG. For the bilateral cutoff, specificity was 62% in ocular MG and 64% in generalized MG.
The results provide class III evidence that oVEMP can distinguish between patients with MG and healthy controls, “but future studies will need to confirm its diagnostic utility in clinical practice, where the main challenge is differentiation from patients with other neuro-opthalmologic conditions,” the researchers said. “The possibility to apply fast repetition rates is one important advantage of oVEMP, which is not possible by measuring voluntary saccadic eye movements. As a consequence, oVEMP allowed us to unmask myasthenic decrements even in clinically asymptomatic eyes,” they added.
Because the study used a confirmed diagnosis of MG as a benchmark, all patients were already being treated with cholinesterase inhibitors, the investigators noted. Although they underwent oVEMP testing in the morning before their first dose of medication, the test needs further study in drug-naïve patients, as well as in patients with worse limitations in their upward gaze, they added.
The study was funded by the University of Zurich, the Betty and David Koetser Foundation for Brain Research, the Albert Bruppacher Foundation for Eye Research, and the OPOS Foundation. The investigators had no relevant disclosures.
FROM NEUROLOGY
Key clinical point:Testing ocular vestibular evoked myogenic potentials (oVEMP) shows promise for diagnosing ocular myasthenia gravis.
Major finding: The sensitivity of the test when at least one eye was affected was 89%, and its specificity was 64%.
Data source: A case-control study of 27 patients with myasthenia gravis and 28 healthy controls.
Disclosures: The study was funded by the University of Zurich, the Betty and David Koetser Foundation for Brain Research, the Albert Bruppacher Foundation for Eye Research, and the OPOS Foundation. The investigators had no relevant disclosures.
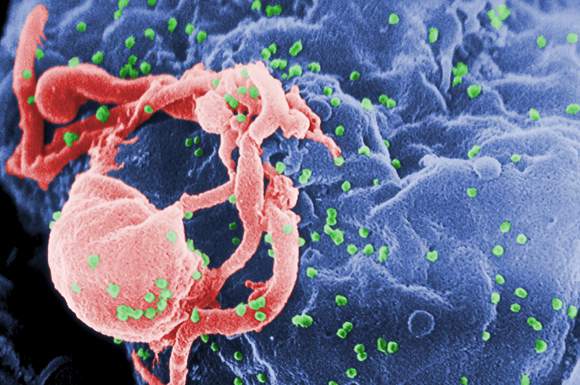
Novel HIV-1 vaccines found safe, immunogenic in healthy adults
Two novel HIV-1 vaccines produced significant humoral and cellular immune responses in healthy adults, according to a multicenter randomized trial published in Annals of Internal Medicine.
“Both heterologous and homologous adenovirus vaccine regimens are promising vaccination strategies,” said Dr. Lindsey Baden of Brigham and Women’s Hospital in Boston and her associates. Baseline immunity did not significantly alter immune responses, and second vaccinations of all regimens significantly boosted antibody titers, the researchers added.
Developing HIV vaccines remains a global priority, but only one of four prior strategies showed any promise, and efficacy was “modest and short-lived,” the researchers said. To assess the two novel HIV-1 vaccines, they randomized 217 healthy, uninfected adults to receive placebo or vaccines consisting of either adenovirus serotype 26 or serotype 35, each with an HIV-1 envelope A insert. Both vaccines were administered at a dose of 5 x 1010 viral particles and in homologous and heterologous combinations. The double-blinded trial was conducted in East Africa, South Africa, and the United States (Ann Intern Med. 2016 Feb 1. doi: 10.7326/M15-0880). The vaccines produced humoral and cellular immune responses in all populations, regardless of baseline vector immunity, said the investigators. The second vaccination boosted envelope A antibody titers about 20-fold in both the homologous and heterologous regimens. However, vaccine order seemed to matter in the heterologous regimen, as envelope A antibody titers were significantly higher when the adenovirus serotype 26 vaccine was given first instead of second.
T-cell responses were “modest” for all regimens, although they differed somewhat by regimen and were lower in East Africa than at other sites, the researchers reported. There were no serious vaccine-related adverse events. Because a 3-month vaccination schedule had similar immunogenicity as a 6-month schedule, the investigators recommended further studies of the durability of immune response with this shorter schedule.
The study was supported by the Ragon Institute, the National Institutes of Health, the International AIDS Vaccine Initiative, and the U.S. Agency for International Development. Dr. Baden reported receiving grants from the Ragon Institute, NIH, and the Bill & Melinda Gates Foundation, and involvement in HIV vaccine clinical trials conducted with NIH, HIV Vaccine Trials Network, International AIDS Vaccine Initiative, Crucell Holland BV/Janssen Pharmaceuticals, Military HIV Research Program, the Bill & Melinda Gates Foundation, and the Ragon Institute. Ten coinvestigators reported financial relationships with these and other nonprofit and pharmaceutical companies. Two coinvestigators also reported holding relevant patents.
Two novel HIV-1 vaccines produced significant humoral and cellular immune responses in healthy adults, according to a multicenter randomized trial published in Annals of Internal Medicine.
“Both heterologous and homologous adenovirus vaccine regimens are promising vaccination strategies,” said Dr. Lindsey Baden of Brigham and Women’s Hospital in Boston and her associates. Baseline immunity did not significantly alter immune responses, and second vaccinations of all regimens significantly boosted antibody titers, the researchers added.
Developing HIV vaccines remains a global priority, but only one of four prior strategies showed any promise, and efficacy was “modest and short-lived,” the researchers said. To assess the two novel HIV-1 vaccines, they randomized 217 healthy, uninfected adults to receive placebo or vaccines consisting of either adenovirus serotype 26 or serotype 35, each with an HIV-1 envelope A insert. Both vaccines were administered at a dose of 5 x 1010 viral particles and in homologous and heterologous combinations. The double-blinded trial was conducted in East Africa, South Africa, and the United States (Ann Intern Med. 2016 Feb 1. doi: 10.7326/M15-0880). The vaccines produced humoral and cellular immune responses in all populations, regardless of baseline vector immunity, said the investigators. The second vaccination boosted envelope A antibody titers about 20-fold in both the homologous and heterologous regimens. However, vaccine order seemed to matter in the heterologous regimen, as envelope A antibody titers were significantly higher when the adenovirus serotype 26 vaccine was given first instead of second.
T-cell responses were “modest” for all regimens, although they differed somewhat by regimen and were lower in East Africa than at other sites, the researchers reported. There were no serious vaccine-related adverse events. Because a 3-month vaccination schedule had similar immunogenicity as a 6-month schedule, the investigators recommended further studies of the durability of immune response with this shorter schedule.
The study was supported by the Ragon Institute, the National Institutes of Health, the International AIDS Vaccine Initiative, and the U.S. Agency for International Development. Dr. Baden reported receiving grants from the Ragon Institute, NIH, and the Bill & Melinda Gates Foundation, and involvement in HIV vaccine clinical trials conducted with NIH, HIV Vaccine Trials Network, International AIDS Vaccine Initiative, Crucell Holland BV/Janssen Pharmaceuticals, Military HIV Research Program, the Bill & Melinda Gates Foundation, and the Ragon Institute. Ten coinvestigators reported financial relationships with these and other nonprofit and pharmaceutical companies. Two coinvestigators also reported holding relevant patents.
Two novel HIV-1 vaccines produced significant humoral and cellular immune responses in healthy adults, according to a multicenter randomized trial published in Annals of Internal Medicine.
“Both heterologous and homologous adenovirus vaccine regimens are promising vaccination strategies,” said Dr. Lindsey Baden of Brigham and Women’s Hospital in Boston and her associates. Baseline immunity did not significantly alter immune responses, and second vaccinations of all regimens significantly boosted antibody titers, the researchers added.
Developing HIV vaccines remains a global priority, but only one of four prior strategies showed any promise, and efficacy was “modest and short-lived,” the researchers said. To assess the two novel HIV-1 vaccines, they randomized 217 healthy, uninfected adults to receive placebo or vaccines consisting of either adenovirus serotype 26 or serotype 35, each with an HIV-1 envelope A insert. Both vaccines were administered at a dose of 5 x 1010 viral particles and in homologous and heterologous combinations. The double-blinded trial was conducted in East Africa, South Africa, and the United States (Ann Intern Med. 2016 Feb 1. doi: 10.7326/M15-0880). The vaccines produced humoral and cellular immune responses in all populations, regardless of baseline vector immunity, said the investigators. The second vaccination boosted envelope A antibody titers about 20-fold in both the homologous and heterologous regimens. However, vaccine order seemed to matter in the heterologous regimen, as envelope A antibody titers were significantly higher when the adenovirus serotype 26 vaccine was given first instead of second.
T-cell responses were “modest” for all regimens, although they differed somewhat by regimen and were lower in East Africa than at other sites, the researchers reported. There were no serious vaccine-related adverse events. Because a 3-month vaccination schedule had similar immunogenicity as a 6-month schedule, the investigators recommended further studies of the durability of immune response with this shorter schedule.
The study was supported by the Ragon Institute, the National Institutes of Health, the International AIDS Vaccine Initiative, and the U.S. Agency for International Development. Dr. Baden reported receiving grants from the Ragon Institute, NIH, and the Bill & Melinda Gates Foundation, and involvement in HIV vaccine clinical trials conducted with NIH, HIV Vaccine Trials Network, International AIDS Vaccine Initiative, Crucell Holland BV/Janssen Pharmaceuticals, Military HIV Research Program, the Bill & Melinda Gates Foundation, and the Ragon Institute. Ten coinvestigators reported financial relationships with these and other nonprofit and pharmaceutical companies. Two coinvestigators also reported holding relevant patents.
Key clinical point: Two novel HIV-1 vaccines induced significant humoral and cellular immunity in healthy, uninfected adults.
Major finding: All regimens induced humoral and cellular immunity in almost all participants.
Data source: A multicenter, randomized, double-blind, placebo-controlled trial of 217 healthy adults without HIV infection.
Disclosures: The study was supported by the Ragon Institute of Massachusetts General Hospital, Massachusetts Institute of Technology, and Harvard University and by the National Institutes of Health, International AIDS Vaccine Initiative, and the U.S. Agency for International Development. Dr. Baden reported receiving grants from the Ragon Institute, NIH, and the Bill & Melinda Gates Foundation, and involvement in HIV vaccine clinical trials conducted with NIH, HIV Vaccine Trials Network, International AIDS Vaccine Initiative, Crucell Holland BV/Janssen Pharmaceuticals, Military HIV Research Program, the Bill & Melinda Gates Foundation, and the Ragon Institute. Ten coinvestigators reported relationships with these and other nonprofit and pharmaceutical companies. Two coinvestigators also reported holding relevant patents.
Minor Residual Staining Found Adequate for Colonoscopy
A Boston Bowel Preparation Scale (BBPS) score of 2 – indicating mild residual staining and small stool fragments – was as good as the optimal preparation score of 3 for visualizing polyps and adenomas larger than 5 mm and advanced adenomas during colonoscopy, researchers said.
A score of 2 might increase the chances of missing smaller polyps, but is adequate for detecting clinically significant masses, Dr. Brian Clark of Yale University, New Haven, Conn., and his associates reported in the February issue of Gastroenterology. But a score of 1 – meaning that there is enough staining or stool to obscure the mucosa – significantly increased the chances of missing adenomas larger than 5 mm, they said. Patients should undergo early repeat colonoscopy if their BBPS score is 1 or 0 in any colon segment, they emphasized.
Source: American Gastroenterological Association
Bowel preparation for colonoscopy is considered adequate if endoscopists can detect polyps larger than 5 mm, but no prior study had quantified the amount of preparation needed. This prospective observational study assessed adequate preparation in terms of the BBPS, which scores each of three colon segments on a scale of 0 (solid stool covering the mucosa) to 3 points (entire mucosa seen well, with no residual staining). Study participants included 438 men aged 50-75 years who underwent screening or surveillance colonoscopy at a single Veterans Affairs center, followed by repeat colonoscopies within 60 days performed by different blinded endoscopists. The investigators excluded patients who scored 0 in all colon segments or had familial polyposis syndrome, inflammatory bowel disease, polyps so large that they could not be completely removed, or a history of colonic or rectal resection. In all, they analyzed 1,161 colon segments (Gastroenterology. 2015 Dec 7. doi: 10.1053/j.gastro.2015.09.041).
Endoscopists missed about 5% of adenomas greater than 5 mm, regardless of whether BBPS scores were 2 or 3 in a model that accounted for age, reason for colonoscopy, colon segment, number of polyps removed in the first examination, and endoscopist performing the procedure, the researchers said. But when BBPS scores were 1, endoscopists missed 16% of adenomas larger than 5 mm, a difference of about 10%. Furthermore, 43% of screening and surveillance intervals would have been incorrect had they been based solely on an initial examination for which scores were 1 in at least one segment. In contrast, only about 15% of intervals would have been incorrect for patients who scored 2 or 3 in all segments.
In all, 80% of patients were sufficiently prepared, having scored at least 2 in all segments on the first examination. “Determining whether a patient’s preparation quality is adequate is one of the most common and important decisions made by gastroenterologists each day,” the researchers said. Between 25% and 30% of screening and surveillance colonoscopies occur at “inappropriately shortened intervals,” often because of uncertainty about what constitutes adequate visualization, they added. Defining adequate visualization based on bowel preparation could save billions of dollars in health care costs every year, minimize complications from unnecessary procedures, and pinpoint those patients who truly need an early repeat colonoscopy to help prevent interval colorectal cancer, they emphasized.
The National Institutes of Health funded the study. The investigators had no disclosures.
We have seen a dramatic increase in attention to improving the adenoma detection rate (ADR) during colonoscopy because patients of endoscopists with a higher ADR have a lower risk of colorectal cancer after colonoscopy. One major contributor to missed adenomas is inadequate bowel preparation, though little was known about how best to define adequacy.

|
| Dr. Jason Domonitz |
Clark and colleagues’ elegant tandem colonoscopy study helps address this knowledge gap using the Boston Bowel Preparation Scale (BBPS), a validated instrument that is easy to implement. They hypothesized that a BBPS colon-segment score of 2 was noninferior to a score of 3 for identifying adenomas greater than 5 mm, but that a BBPS colon-segment score of 1 would be inferior to scores of 2 or 3. Their findings support this hypothesis and give us long overdue data that we can now use to define an adequate bowel preparation. Given that the adenoma miss rate was 16% when the segment score was 1, but only about 5% with higher scores, it is reasonable to recommend repeat colonoscopy within 12 months if any segment score is less than 2. Otherwise, standard surveillance intervals should be recommended. Finally, unless and until other scoring systems are similarly validated, these findings should encourage the widespread adoption of the BBPS.
Dr. Jason A. Dominitz, AGAF, is the national program director for gastroenterology for the Veterans Health Administration and is professor of medicine in the division of gastroenterology at the University of Washington, Seattle. He has no conflicts of interest.
We have seen a dramatic increase in attention to improving the adenoma detection rate (ADR) during colonoscopy because patients of endoscopists with a higher ADR have a lower risk of colorectal cancer after colonoscopy. One major contributor to missed adenomas is inadequate bowel preparation, though little was known about how best to define adequacy.

|
| Dr. Jason Domonitz |
Clark and colleagues’ elegant tandem colonoscopy study helps address this knowledge gap using the Boston Bowel Preparation Scale (BBPS), a validated instrument that is easy to implement. They hypothesized that a BBPS colon-segment score of 2 was noninferior to a score of 3 for identifying adenomas greater than 5 mm, but that a BBPS colon-segment score of 1 would be inferior to scores of 2 or 3. Their findings support this hypothesis and give us long overdue data that we can now use to define an adequate bowel preparation. Given that the adenoma miss rate was 16% when the segment score was 1, but only about 5% with higher scores, it is reasonable to recommend repeat colonoscopy within 12 months if any segment score is less than 2. Otherwise, standard surveillance intervals should be recommended. Finally, unless and until other scoring systems are similarly validated, these findings should encourage the widespread adoption of the BBPS.
Dr. Jason A. Dominitz, AGAF, is the national program director for gastroenterology for the Veterans Health Administration and is professor of medicine in the division of gastroenterology at the University of Washington, Seattle. He has no conflicts of interest.
We have seen a dramatic increase in attention to improving the adenoma detection rate (ADR) during colonoscopy because patients of endoscopists with a higher ADR have a lower risk of colorectal cancer after colonoscopy. One major contributor to missed adenomas is inadequate bowel preparation, though little was known about how best to define adequacy.

|
| Dr. Jason Domonitz |
Clark and colleagues’ elegant tandem colonoscopy study helps address this knowledge gap using the Boston Bowel Preparation Scale (BBPS), a validated instrument that is easy to implement. They hypothesized that a BBPS colon-segment score of 2 was noninferior to a score of 3 for identifying adenomas greater than 5 mm, but that a BBPS colon-segment score of 1 would be inferior to scores of 2 or 3. Their findings support this hypothesis and give us long overdue data that we can now use to define an adequate bowel preparation. Given that the adenoma miss rate was 16% when the segment score was 1, but only about 5% with higher scores, it is reasonable to recommend repeat colonoscopy within 12 months if any segment score is less than 2. Otherwise, standard surveillance intervals should be recommended. Finally, unless and until other scoring systems are similarly validated, these findings should encourage the widespread adoption of the BBPS.
Dr. Jason A. Dominitz, AGAF, is the national program director for gastroenterology for the Veterans Health Administration and is professor of medicine in the division of gastroenterology at the University of Washington, Seattle. He has no conflicts of interest.
A Boston Bowel Preparation Scale (BBPS) score of 2 – indicating mild residual staining and small stool fragments – was as good as the optimal preparation score of 3 for visualizing polyps and adenomas larger than 5 mm and advanced adenomas during colonoscopy, researchers said.
A score of 2 might increase the chances of missing smaller polyps, but is adequate for detecting clinically significant masses, Dr. Brian Clark of Yale University, New Haven, Conn., and his associates reported in the February issue of Gastroenterology. But a score of 1 – meaning that there is enough staining or stool to obscure the mucosa – significantly increased the chances of missing adenomas larger than 5 mm, they said. Patients should undergo early repeat colonoscopy if their BBPS score is 1 or 0 in any colon segment, they emphasized.
Source: American Gastroenterological Association
Bowel preparation for colonoscopy is considered adequate if endoscopists can detect polyps larger than 5 mm, but no prior study had quantified the amount of preparation needed. This prospective observational study assessed adequate preparation in terms of the BBPS, which scores each of three colon segments on a scale of 0 (solid stool covering the mucosa) to 3 points (entire mucosa seen well, with no residual staining). Study participants included 438 men aged 50-75 years who underwent screening or surveillance colonoscopy at a single Veterans Affairs center, followed by repeat colonoscopies within 60 days performed by different blinded endoscopists. The investigators excluded patients who scored 0 in all colon segments or had familial polyposis syndrome, inflammatory bowel disease, polyps so large that they could not be completely removed, or a history of colonic or rectal resection. In all, they analyzed 1,161 colon segments (Gastroenterology. 2015 Dec 7. doi: 10.1053/j.gastro.2015.09.041).
Endoscopists missed about 5% of adenomas greater than 5 mm, regardless of whether BBPS scores were 2 or 3 in a model that accounted for age, reason for colonoscopy, colon segment, number of polyps removed in the first examination, and endoscopist performing the procedure, the researchers said. But when BBPS scores were 1, endoscopists missed 16% of adenomas larger than 5 mm, a difference of about 10%. Furthermore, 43% of screening and surveillance intervals would have been incorrect had they been based solely on an initial examination for which scores were 1 in at least one segment. In contrast, only about 15% of intervals would have been incorrect for patients who scored 2 or 3 in all segments.
In all, 80% of patients were sufficiently prepared, having scored at least 2 in all segments on the first examination. “Determining whether a patient’s preparation quality is adequate is one of the most common and important decisions made by gastroenterologists each day,” the researchers said. Between 25% and 30% of screening and surveillance colonoscopies occur at “inappropriately shortened intervals,” often because of uncertainty about what constitutes adequate visualization, they added. Defining adequate visualization based on bowel preparation could save billions of dollars in health care costs every year, minimize complications from unnecessary procedures, and pinpoint those patients who truly need an early repeat colonoscopy to help prevent interval colorectal cancer, they emphasized.
The National Institutes of Health funded the study. The investigators had no disclosures.
A Boston Bowel Preparation Scale (BBPS) score of 2 – indicating mild residual staining and small stool fragments – was as good as the optimal preparation score of 3 for visualizing polyps and adenomas larger than 5 mm and advanced adenomas during colonoscopy, researchers said.
A score of 2 might increase the chances of missing smaller polyps, but is adequate for detecting clinically significant masses, Dr. Brian Clark of Yale University, New Haven, Conn., and his associates reported in the February issue of Gastroenterology. But a score of 1 – meaning that there is enough staining or stool to obscure the mucosa – significantly increased the chances of missing adenomas larger than 5 mm, they said. Patients should undergo early repeat colonoscopy if their BBPS score is 1 or 0 in any colon segment, they emphasized.
Source: American Gastroenterological Association
Bowel preparation for colonoscopy is considered adequate if endoscopists can detect polyps larger than 5 mm, but no prior study had quantified the amount of preparation needed. This prospective observational study assessed adequate preparation in terms of the BBPS, which scores each of three colon segments on a scale of 0 (solid stool covering the mucosa) to 3 points (entire mucosa seen well, with no residual staining). Study participants included 438 men aged 50-75 years who underwent screening or surveillance colonoscopy at a single Veterans Affairs center, followed by repeat colonoscopies within 60 days performed by different blinded endoscopists. The investigators excluded patients who scored 0 in all colon segments or had familial polyposis syndrome, inflammatory bowel disease, polyps so large that they could not be completely removed, or a history of colonic or rectal resection. In all, they analyzed 1,161 colon segments (Gastroenterology. 2015 Dec 7. doi: 10.1053/j.gastro.2015.09.041).
Endoscopists missed about 5% of adenomas greater than 5 mm, regardless of whether BBPS scores were 2 or 3 in a model that accounted for age, reason for colonoscopy, colon segment, number of polyps removed in the first examination, and endoscopist performing the procedure, the researchers said. But when BBPS scores were 1, endoscopists missed 16% of adenomas larger than 5 mm, a difference of about 10%. Furthermore, 43% of screening and surveillance intervals would have been incorrect had they been based solely on an initial examination for which scores were 1 in at least one segment. In contrast, only about 15% of intervals would have been incorrect for patients who scored 2 or 3 in all segments.
In all, 80% of patients were sufficiently prepared, having scored at least 2 in all segments on the first examination. “Determining whether a patient’s preparation quality is adequate is one of the most common and important decisions made by gastroenterologists each day,” the researchers said. Between 25% and 30% of screening and surveillance colonoscopies occur at “inappropriately shortened intervals,” often because of uncertainty about what constitutes adequate visualization, they added. Defining adequate visualization based on bowel preparation could save billions of dollars in health care costs every year, minimize complications from unnecessary procedures, and pinpoint those patients who truly need an early repeat colonoscopy to help prevent interval colorectal cancer, they emphasized.
The National Institutes of Health funded the study. The investigators had no disclosures.
FROM GASTROENTEROLOGY
Minor residual staining found adequate for colonoscopy
A Boston Bowel Preparation Scale (BBPS) score of 2 – indicating mild residual staining and small stool fragments – was as good as the optimal preparation score of 3 for visualizing polyps and adenomas larger than 5 mm and advanced adenomas during colonoscopy, researchers said.
A score of 2 might increase the chances of missing smaller polyps, but is adequate for detecting clinically significant masses, Dr. Brian Clark of Yale University, New Haven, Conn., and his associates reported in the February issue of Gastroenterology. But a score of 1 – meaning that there is enough staining or stool to obscure the mucosa – significantly increased the chances of missing adenomas larger than 5 mm, they said. Patients should undergo early repeat colonoscopy if their BBPS score is 1 or 0 in any colon segment, they emphasized.
Source: American Gastroenterological Association
Bowel preparation for colonoscopy is considered adequate if endoscopists can detect polyps larger than 5 mm, but no prior study had quantified the amount of preparation needed. This prospective observational study assessed adequate preparation in terms of the BBPS, which scores each of three colon segments on a scale of 0 (solid stool covering the mucosa) to 3 points (entire mucosa seen well, with no residual staining). Study participants included 438 men aged 50-75 years who underwent screening or surveillance colonoscopy at a single Veterans Affairs center, followed by repeat colonoscopies within 60 days performed by different blinded endoscopists. The investigators excluded patients who scored 0 in all colon segments or had familial polyposis syndrome, inflammatory bowel disease, polyps so large that they could not be completely removed, or a history of colonic or rectal resection. In all, they analyzed 1,161 colon segments (Gastroenterology. 2015 Dec 7. doi: 10.1053/j.gastro.2015.09.041).
Endoscopists missed about 5% of adenomas greater than 5 mm, regardless of whether BBPS scores were 2 or 3 in a model that accounted for age, reason for colonoscopy, colon segment, number of polyps removed in the first examination, and endoscopist performing the procedure, the researchers said. But when BBPS scores were 1, endoscopists missed 16% of adenomas larger than 5 mm, a difference of about 10%. Furthermore, 43% of screening and surveillance intervals would have been incorrect had they been based solely on an initial examination for which scores were 1 in at least one segment. In contrast, only about 15% of intervals would have been incorrect for patients who scored 2 or 3 in all segments.
In all, 80% of patients were sufficiently prepared, having scored at least 2 in all segments on the first examination. “Determining whether a patient’s preparation quality is adequate is one of the most common and important decisions made by gastroenterologists each day,” the researchers said. Between 25% and 30% of screening and surveillance colonoscopies occur at “inappropriately shortened intervals,” often because of uncertainty about what constitutes adequate visualization, they added. Defining adequate visualization based on bowel preparation could save billions of dollars in health care costs every year, minimize complications from unnecessary procedures, and pinpoint those patients who truly need an early repeat colonoscopy to help prevent interval colorectal cancer, they emphasized.
The National Institutes of Health funded the study. The investigators had no disclosures.
We have seen a dramatic increase in attention to improving the adenoma detection rate (ADR) during colonoscopy because patients of endoscopists with a higher ADR have a lower risk of colorectal cancer after colonoscopy. One major contributor to missed adenomas is inadequate bowel preparation, though little was known about how best to define adequacy.

|
| Dr. Jason Domonitz |
Clark and colleagues’ elegant tandem colonoscopy study helps address this knowledge gap using the Boston Bowel Preparation Scale (BBPS), a validated instrument that is easy to implement. They hypothesized that a BBPS colon-segment score of 2 was noninferior to a score of 3 for identifying adenomas greater than 5 mm, but that a BBPS colon-segment score of 1 would be inferior to scores of 2 or 3. Their findings support this hypothesis and give us long overdue data that we can now use to define an adequate bowel preparation. Given that the adenoma miss rate was 16% when the segment score was 1, but only about 5% with higher scores, it is reasonable to recommend repeat colonoscopy within 12 months if any segment score is less than 2. Otherwise, standard surveillance intervals should be recommended. Finally, unless and until other scoring systems are similarly validated, these findings should encourage the widespread adoption of the BBPS.
Dr. Jason A. Dominitz, AGAF, is the national program director for gastroenterology for the Veterans Health Administration and is professor of medicine in the division of gastroenterology at the University of Washington, Seattle. He has no conflicts of interest.
We have seen a dramatic increase in attention to improving the adenoma detection rate (ADR) during colonoscopy because patients of endoscopists with a higher ADR have a lower risk of colorectal cancer after colonoscopy. One major contributor to missed adenomas is inadequate bowel preparation, though little was known about how best to define adequacy.

|
| Dr. Jason Domonitz |
Clark and colleagues’ elegant tandem colonoscopy study helps address this knowledge gap using the Boston Bowel Preparation Scale (BBPS), a validated instrument that is easy to implement. They hypothesized that a BBPS colon-segment score of 2 was noninferior to a score of 3 for identifying adenomas greater than 5 mm, but that a BBPS colon-segment score of 1 would be inferior to scores of 2 or 3. Their findings support this hypothesis and give us long overdue data that we can now use to define an adequate bowel preparation. Given that the adenoma miss rate was 16% when the segment score was 1, but only about 5% with higher scores, it is reasonable to recommend repeat colonoscopy within 12 months if any segment score is less than 2. Otherwise, standard surveillance intervals should be recommended. Finally, unless and until other scoring systems are similarly validated, these findings should encourage the widespread adoption of the BBPS.
Dr. Jason A. Dominitz, AGAF, is the national program director for gastroenterology for the Veterans Health Administration and is professor of medicine in the division of gastroenterology at the University of Washington, Seattle. He has no conflicts of interest.
We have seen a dramatic increase in attention to improving the adenoma detection rate (ADR) during colonoscopy because patients of endoscopists with a higher ADR have a lower risk of colorectal cancer after colonoscopy. One major contributor to missed adenomas is inadequate bowel preparation, though little was known about how best to define adequacy.

|
| Dr. Jason Domonitz |
Clark and colleagues’ elegant tandem colonoscopy study helps address this knowledge gap using the Boston Bowel Preparation Scale (BBPS), a validated instrument that is easy to implement. They hypothesized that a BBPS colon-segment score of 2 was noninferior to a score of 3 for identifying adenomas greater than 5 mm, but that a BBPS colon-segment score of 1 would be inferior to scores of 2 or 3. Their findings support this hypothesis and give us long overdue data that we can now use to define an adequate bowel preparation. Given that the adenoma miss rate was 16% when the segment score was 1, but only about 5% with higher scores, it is reasonable to recommend repeat colonoscopy within 12 months if any segment score is less than 2. Otherwise, standard surveillance intervals should be recommended. Finally, unless and until other scoring systems are similarly validated, these findings should encourage the widespread adoption of the BBPS.
Dr. Jason A. Dominitz, AGAF, is the national program director for gastroenterology for the Veterans Health Administration and is professor of medicine in the division of gastroenterology at the University of Washington, Seattle. He has no conflicts of interest.
A Boston Bowel Preparation Scale (BBPS) score of 2 – indicating mild residual staining and small stool fragments – was as good as the optimal preparation score of 3 for visualizing polyps and adenomas larger than 5 mm and advanced adenomas during colonoscopy, researchers said.
A score of 2 might increase the chances of missing smaller polyps, but is adequate for detecting clinically significant masses, Dr. Brian Clark of Yale University, New Haven, Conn., and his associates reported in the February issue of Gastroenterology. But a score of 1 – meaning that there is enough staining or stool to obscure the mucosa – significantly increased the chances of missing adenomas larger than 5 mm, they said. Patients should undergo early repeat colonoscopy if their BBPS score is 1 or 0 in any colon segment, they emphasized.
Source: American Gastroenterological Association
Bowel preparation for colonoscopy is considered adequate if endoscopists can detect polyps larger than 5 mm, but no prior study had quantified the amount of preparation needed. This prospective observational study assessed adequate preparation in terms of the BBPS, which scores each of three colon segments on a scale of 0 (solid stool covering the mucosa) to 3 points (entire mucosa seen well, with no residual staining). Study participants included 438 men aged 50-75 years who underwent screening or surveillance colonoscopy at a single Veterans Affairs center, followed by repeat colonoscopies within 60 days performed by different blinded endoscopists. The investigators excluded patients who scored 0 in all colon segments or had familial polyposis syndrome, inflammatory bowel disease, polyps so large that they could not be completely removed, or a history of colonic or rectal resection. In all, they analyzed 1,161 colon segments (Gastroenterology. 2015 Dec 7. doi: 10.1053/j.gastro.2015.09.041).
Endoscopists missed about 5% of adenomas greater than 5 mm, regardless of whether BBPS scores were 2 or 3 in a model that accounted for age, reason for colonoscopy, colon segment, number of polyps removed in the first examination, and endoscopist performing the procedure, the researchers said. But when BBPS scores were 1, endoscopists missed 16% of adenomas larger than 5 mm, a difference of about 10%. Furthermore, 43% of screening and surveillance intervals would have been incorrect had they been based solely on an initial examination for which scores were 1 in at least one segment. In contrast, only about 15% of intervals would have been incorrect for patients who scored 2 or 3 in all segments.
In all, 80% of patients were sufficiently prepared, having scored at least 2 in all segments on the first examination. “Determining whether a patient’s preparation quality is adequate is one of the most common and important decisions made by gastroenterologists each day,” the researchers said. Between 25% and 30% of screening and surveillance colonoscopies occur at “inappropriately shortened intervals,” often because of uncertainty about what constitutes adequate visualization, they added. Defining adequate visualization based on bowel preparation could save billions of dollars in health care costs every year, minimize complications from unnecessary procedures, and pinpoint those patients who truly need an early repeat colonoscopy to help prevent interval colorectal cancer, they emphasized.
The National Institutes of Health funded the study. The investigators had no disclosures.
A Boston Bowel Preparation Scale (BBPS) score of 2 – indicating mild residual staining and small stool fragments – was as good as the optimal preparation score of 3 for visualizing polyps and adenomas larger than 5 mm and advanced adenomas during colonoscopy, researchers said.
A score of 2 might increase the chances of missing smaller polyps, but is adequate for detecting clinically significant masses, Dr. Brian Clark of Yale University, New Haven, Conn., and his associates reported in the February issue of Gastroenterology. But a score of 1 – meaning that there is enough staining or stool to obscure the mucosa – significantly increased the chances of missing adenomas larger than 5 mm, they said. Patients should undergo early repeat colonoscopy if their BBPS score is 1 or 0 in any colon segment, they emphasized.
Source: American Gastroenterological Association
Bowel preparation for colonoscopy is considered adequate if endoscopists can detect polyps larger than 5 mm, but no prior study had quantified the amount of preparation needed. This prospective observational study assessed adequate preparation in terms of the BBPS, which scores each of three colon segments on a scale of 0 (solid stool covering the mucosa) to 3 points (entire mucosa seen well, with no residual staining). Study participants included 438 men aged 50-75 years who underwent screening or surveillance colonoscopy at a single Veterans Affairs center, followed by repeat colonoscopies within 60 days performed by different blinded endoscopists. The investigators excluded patients who scored 0 in all colon segments or had familial polyposis syndrome, inflammatory bowel disease, polyps so large that they could not be completely removed, or a history of colonic or rectal resection. In all, they analyzed 1,161 colon segments (Gastroenterology. 2015 Dec 7. doi: 10.1053/j.gastro.2015.09.041).
Endoscopists missed about 5% of adenomas greater than 5 mm, regardless of whether BBPS scores were 2 or 3 in a model that accounted for age, reason for colonoscopy, colon segment, number of polyps removed in the first examination, and endoscopist performing the procedure, the researchers said. But when BBPS scores were 1, endoscopists missed 16% of adenomas larger than 5 mm, a difference of about 10%. Furthermore, 43% of screening and surveillance intervals would have been incorrect had they been based solely on an initial examination for which scores were 1 in at least one segment. In contrast, only about 15% of intervals would have been incorrect for patients who scored 2 or 3 in all segments.
In all, 80% of patients were sufficiently prepared, having scored at least 2 in all segments on the first examination. “Determining whether a patient’s preparation quality is adequate is one of the most common and important decisions made by gastroenterologists each day,” the researchers said. Between 25% and 30% of screening and surveillance colonoscopies occur at “inappropriately shortened intervals,” often because of uncertainty about what constitutes adequate visualization, they added. Defining adequate visualization based on bowel preparation could save billions of dollars in health care costs every year, minimize complications from unnecessary procedures, and pinpoint those patients who truly need an early repeat colonoscopy to help prevent interval colorectal cancer, they emphasized.
The National Institutes of Health funded the study. The investigators had no disclosures.
FROM GASTROENTEROLOGY
Key clinical point: Minor residual staining that does not obscure the bowel mucosa is adequate for detection of adenomas greater than 5 mm during surveillance or screening colonoscopy.
Major finding: Endoscopists missed about 5% of clinically significant adenomas, regardless of whether the Boston Bowel Preparation Score was 2 (minor residual staining) or 3 (entire mucosa seen well).
Data source: A blinded prospective observational study of 438 men at a single Veterans Affairs center.
Disclosures: The National Institutes of Health funded the study. The investigators had no disclosures.
Drug combo held up in real-world HCV study
A 12-week, ribavirin-free regimen achieved sustained virologic response for 85% of patients with genotype 1 hepatitis C virus (HCV) infection, researchers reported in the February issue of Gastroenterology.
“This represents one of the first applications of a highly effective HCV regimen outside clinical trials,” said Dr. Mark S. Sulkowski of John Hopkins University in Baltimore and his associates. Adding ribavirin to the simeprevir and sofosbuvir combination regimen did not improve sustained virologic response (SVR), but patients were less likely to achieve it if they had cirrhosis, current or prior hepatic decompensation, or a history of failing other protease inhibitors, the investigators said.
Novel hepatitis C therapies have yielded “substantially lower” rates of SVR and more side effects in everyday practice than in clinical trials, the investigators noted. To better understand how some of newest HCV drugs perform in the real world, they conducted an observational cohort study of the safety, tolerability, and efficacy of simeprevir plus sofosbuvir for treating genotype 1 HCV infections in academic and nonacademic settings (HCV-TARGET) (Gastroenterology 2015 doi: 10.1053/j.gastro.2015.10.013).
A total of 836 patients received once-daily simeprevir (150 mg) and sofosbuvir (400 mg), and 169 of them also received ribavirin. Most (61%) patients had genotype 1a infection and were white (76%), male (61%), and cirrhotic (59%); 13% were black. Patients usually were treatment experienced, having failed peginterferon and ribavirin either with (12%) or without (46%) telaprevir or boceprevir, the researchers said.
In all, 675 (84%) patients achieved SVR after 12 weeks of treatment (SVR12; 95% confidence interval, 81%-87%). Adding ribavirin to the combination PI regimen did not improve SVR, regardless of cirrhosis status, genetic subtype, or treatment history. However, crude SVR12 rates were only 75% for patients with hepatic decompensation and 81% for those with cirrhosis, and these patients had significantly lower adjusted odds of achieving SVR, compared with other patients. In hindsight, decompensated and cirrhotic patients might have needed 24 weeks of treatment, as the Food and Drug Administration now recommends based on the COSMOS trial results (Lancet. 2014;384[9956]:1756-65), the investigators said.
The adjusted model did not uncover a link between genotype 1 subtype and SVR, but only about 10% of patients were tested for the Q80K polymorphism, which is more common in genotype 1a infections and is associated with treatment resistance, the investigators noted. Crude SVR12 rates were 92% for patients with genotype 1b infection and 86% for those with 1a infection, they said.
Only 3% of patients stopped treatment; 2% did so because of side effects, and ribavirin did not significantly affect rates of treatment discontinuation, said the investigators. The most common side effects were fatigue, headache, nausea, rash, and insomnia. Serious adverse events affected 5% of patients and included gastrointestinal bleeding (0.5%), hepatic failure or encephalopathy (1.2%), and infections (1.1%).
Taken together, these results show that simeprevir and sofosbuvir effectively translate from the clinical trial setting into clinical practice, said the researchers. “Additional research is needed to understand which patients may benefit from different treatment regimens or longer treatment durations,” they emphasized.
The study was supported by the University of Florida at Gainesville, the University of North Carolina at Chapel Hill, AbbVie, Bristol-Myers Squibb, Gilead, Janssen, Kadmon, Merck, Vertex, and the National Institutes of Health. Dr. Sulkowski reported grants and personal fees from Gilead, Janssen, Achillion, Abbvie, Merck, and Bristol-Myers Squibb. Of 14 coinvestigators, 13 reported financial relationships with a number of pharmaceutical companies.
A 12-week, ribavirin-free regimen achieved sustained virologic response for 85% of patients with genotype 1 hepatitis C virus (HCV) infection, researchers reported in the February issue of Gastroenterology.
“This represents one of the first applications of a highly effective HCV regimen outside clinical trials,” said Dr. Mark S. Sulkowski of John Hopkins University in Baltimore and his associates. Adding ribavirin to the simeprevir and sofosbuvir combination regimen did not improve sustained virologic response (SVR), but patients were less likely to achieve it if they had cirrhosis, current or prior hepatic decompensation, or a history of failing other protease inhibitors, the investigators said.
Novel hepatitis C therapies have yielded “substantially lower” rates of SVR and more side effects in everyday practice than in clinical trials, the investigators noted. To better understand how some of newest HCV drugs perform in the real world, they conducted an observational cohort study of the safety, tolerability, and efficacy of simeprevir plus sofosbuvir for treating genotype 1 HCV infections in academic and nonacademic settings (HCV-TARGET) (Gastroenterology 2015 doi: 10.1053/j.gastro.2015.10.013).
A total of 836 patients received once-daily simeprevir (150 mg) and sofosbuvir (400 mg), and 169 of them also received ribavirin. Most (61%) patients had genotype 1a infection and were white (76%), male (61%), and cirrhotic (59%); 13% were black. Patients usually were treatment experienced, having failed peginterferon and ribavirin either with (12%) or without (46%) telaprevir or boceprevir, the researchers said.
In all, 675 (84%) patients achieved SVR after 12 weeks of treatment (SVR12; 95% confidence interval, 81%-87%). Adding ribavirin to the combination PI regimen did not improve SVR, regardless of cirrhosis status, genetic subtype, or treatment history. However, crude SVR12 rates were only 75% for patients with hepatic decompensation and 81% for those with cirrhosis, and these patients had significantly lower adjusted odds of achieving SVR, compared with other patients. In hindsight, decompensated and cirrhotic patients might have needed 24 weeks of treatment, as the Food and Drug Administration now recommends based on the COSMOS trial results (Lancet. 2014;384[9956]:1756-65), the investigators said.
The adjusted model did not uncover a link between genotype 1 subtype and SVR, but only about 10% of patients were tested for the Q80K polymorphism, which is more common in genotype 1a infections and is associated with treatment resistance, the investigators noted. Crude SVR12 rates were 92% for patients with genotype 1b infection and 86% for those with 1a infection, they said.
Only 3% of patients stopped treatment; 2% did so because of side effects, and ribavirin did not significantly affect rates of treatment discontinuation, said the investigators. The most common side effects were fatigue, headache, nausea, rash, and insomnia. Serious adverse events affected 5% of patients and included gastrointestinal bleeding (0.5%), hepatic failure or encephalopathy (1.2%), and infections (1.1%).
Taken together, these results show that simeprevir and sofosbuvir effectively translate from the clinical trial setting into clinical practice, said the researchers. “Additional research is needed to understand which patients may benefit from different treatment regimens or longer treatment durations,” they emphasized.
The study was supported by the University of Florida at Gainesville, the University of North Carolina at Chapel Hill, AbbVie, Bristol-Myers Squibb, Gilead, Janssen, Kadmon, Merck, Vertex, and the National Institutes of Health. Dr. Sulkowski reported grants and personal fees from Gilead, Janssen, Achillion, Abbvie, Merck, and Bristol-Myers Squibb. Of 14 coinvestigators, 13 reported financial relationships with a number of pharmaceutical companies.
A 12-week, ribavirin-free regimen achieved sustained virologic response for 85% of patients with genotype 1 hepatitis C virus (HCV) infection, researchers reported in the February issue of Gastroenterology.
“This represents one of the first applications of a highly effective HCV regimen outside clinical trials,” said Dr. Mark S. Sulkowski of John Hopkins University in Baltimore and his associates. Adding ribavirin to the simeprevir and sofosbuvir combination regimen did not improve sustained virologic response (SVR), but patients were less likely to achieve it if they had cirrhosis, current or prior hepatic decompensation, or a history of failing other protease inhibitors, the investigators said.
Novel hepatitis C therapies have yielded “substantially lower” rates of SVR and more side effects in everyday practice than in clinical trials, the investigators noted. To better understand how some of newest HCV drugs perform in the real world, they conducted an observational cohort study of the safety, tolerability, and efficacy of simeprevir plus sofosbuvir for treating genotype 1 HCV infections in academic and nonacademic settings (HCV-TARGET) (Gastroenterology 2015 doi: 10.1053/j.gastro.2015.10.013).
A total of 836 patients received once-daily simeprevir (150 mg) and sofosbuvir (400 mg), and 169 of them also received ribavirin. Most (61%) patients had genotype 1a infection and were white (76%), male (61%), and cirrhotic (59%); 13% were black. Patients usually were treatment experienced, having failed peginterferon and ribavirin either with (12%) or without (46%) telaprevir or boceprevir, the researchers said.
In all, 675 (84%) patients achieved SVR after 12 weeks of treatment (SVR12; 95% confidence interval, 81%-87%). Adding ribavirin to the combination PI regimen did not improve SVR, regardless of cirrhosis status, genetic subtype, or treatment history. However, crude SVR12 rates were only 75% for patients with hepatic decompensation and 81% for those with cirrhosis, and these patients had significantly lower adjusted odds of achieving SVR, compared with other patients. In hindsight, decompensated and cirrhotic patients might have needed 24 weeks of treatment, as the Food and Drug Administration now recommends based on the COSMOS trial results (Lancet. 2014;384[9956]:1756-65), the investigators said.
The adjusted model did not uncover a link between genotype 1 subtype and SVR, but only about 10% of patients were tested for the Q80K polymorphism, which is more common in genotype 1a infections and is associated with treatment resistance, the investigators noted. Crude SVR12 rates were 92% for patients with genotype 1b infection and 86% for those with 1a infection, they said.
Only 3% of patients stopped treatment; 2% did so because of side effects, and ribavirin did not significantly affect rates of treatment discontinuation, said the investigators. The most common side effects were fatigue, headache, nausea, rash, and insomnia. Serious adverse events affected 5% of patients and included gastrointestinal bleeding (0.5%), hepatic failure or encephalopathy (1.2%), and infections (1.1%).
Taken together, these results show that simeprevir and sofosbuvir effectively translate from the clinical trial setting into clinical practice, said the researchers. “Additional research is needed to understand which patients may benefit from different treatment regimens or longer treatment durations,” they emphasized.
The study was supported by the University of Florida at Gainesville, the University of North Carolina at Chapel Hill, AbbVie, Bristol-Myers Squibb, Gilead, Janssen, Kadmon, Merck, Vertex, and the National Institutes of Health. Dr. Sulkowski reported grants and personal fees from Gilead, Janssen, Achillion, Abbvie, Merck, and Bristol-Myers Squibb. Of 14 coinvestigators, 13 reported financial relationships with a number of pharmaceutical companies.
FROM GASTROENTEROLOGY
Key clinical point: Twelve weeks of simeprevir and sofosbuvir cured about 85% of real-world patients with genotype 1 hepatitis C virus infection.
Major finding: The unadjusted rate of SVR12 was 85% (95% CI, 82%-88%).
Data source: An analysis of an observational cohort study of protease inhibitor combination regimen with or without ribavirin for 836 patients (HCV-TARGET).
Disclosures: The study was supported by the University of Florida at Gainesville, the University of North Carolina at Chapel Hill, AbbVie, Bristol-Myers Squibb, Gilead, Janssen, Kadmon, Merck, Vertex, and the National Institutes of Health. Dr. Sulkowski reported grants and personal fees from Gilead, Janssen, Achillion, Abbvie, Merck, and Bristol-Myers Squibb. Of 14 coinvestigators, 13 reported financial relationships with a number of pharmaceutical companies.
Factors within VA control could help prevent missed, canceled appointments
Opt-out scheduling protocols and long appointment lead times contributed significantly to missed and canceled colonoscopy appointments at Veterans Health Administration facilities, researchers reported in the February issue of Clinical Gastroenterology and Hepatology.
These factors are within the control of the Veterans Affairs and could be altered to improve productivity and efficiency, said Melissa Partin, Ph.D., of the Center for Chronic Disease Outcomes Research at the Minneapolis Veterans Affairs Health Care System in Minneapolis, and her associates.
Source: American Gastroenterological Association
Missed and canceled medical appointments are always a concern, but particularly so for colonoscopy clinics, where they incur an average daily net loss of $725, the investigators noted. Most clinics have limited colonoscopy capacity, and even a 30-day wait for diagnostic colonoscopy has been linked to “modest but significantly elevated” chances of detecting cancer on exam, they added. To better understand these problems, they separately examined predictors of missed and canceled appointments among 27,994 patients who had positive fecal occult blood tests with diagnostic colonoscopies scheduled at 69 VA facilities between 2009 and 2011 (Clin Gastroenterol Hepatol. 2015 Aug 21. doi: 10.1016/j.cgh.2015.07.051).
Having a life expectancy of 6 months or less and no personal history of polyps best predicted missing an appointment, with odds ratios of 2.74 for each factor, the researchers said. However, only 0.47% of patients had such a short life expectancy. Other significant predictors of missed appointments included being seen at the largest and most complex facilities (odds ratio, 2.69; P = .007), having both psychiatric and substance abuse disorders (OR, 1.82; P less than .0001), and the use of opt-out scheduling, in which patients were automatically scheduled rather than having to schedule appointments themselves (OR, 1.57; P = .02). Canceled appointments also were linked to opt-out scheduling, as well as to older age and having no history of polyps.
Most appointment lead times were 28 days, and each 12-day increase in lead time increased the odds of missing or canceling appointments by about 15% (P less than .0001). The problem could be curtailed by the Veterans Access, Choice and Accountability Act of 2014, which allows those who cannot schedule VA appointments within 30 days to receive care from eligible non–VA providers, the investigators said. “Future research should focus on assessing the effect of the Choice Act on colonoscopy appointment lead time and on developing and evaluating efficient and effective approaches to implementing the other clinic-level changes supported by our findings,” they added.
The study might have oversimplified or missed changes in protocols because it used single-item survey measures at one point in time, the investigators said. For some patients, the first appointment after the fecal occult blood test may have been for another procedure besides colonoscopy, they added. Furthermore, they did not distinguish between appointments canceled by patients versus clinics. “The VHA is a unique context, characterized by a predominantly male, low-income population with high rates of mental health and substance abuse diagnoses. Therefore, our findings may not generalize to other settings,” they added. “However, our findings do have important implications for a substantial population of health providers and consumers in this country, because the VHA is the largest integrated health care system in the United States.”
The study was funded by the Department of Veterans Affairs Clinical Science Service and Health Services Research & Development Service. The investigators had no disclosures.
Opt-out scheduling protocols and long appointment lead times contributed significantly to missed and canceled colonoscopy appointments at Veterans Health Administration facilities, researchers reported in the February issue of Clinical Gastroenterology and Hepatology.
These factors are within the control of the Veterans Affairs and could be altered to improve productivity and efficiency, said Melissa Partin, Ph.D., of the Center for Chronic Disease Outcomes Research at the Minneapolis Veterans Affairs Health Care System in Minneapolis, and her associates.
Source: American Gastroenterological Association
Missed and canceled medical appointments are always a concern, but particularly so for colonoscopy clinics, where they incur an average daily net loss of $725, the investigators noted. Most clinics have limited colonoscopy capacity, and even a 30-day wait for diagnostic colonoscopy has been linked to “modest but significantly elevated” chances of detecting cancer on exam, they added. To better understand these problems, they separately examined predictors of missed and canceled appointments among 27,994 patients who had positive fecal occult blood tests with diagnostic colonoscopies scheduled at 69 VA facilities between 2009 and 2011 (Clin Gastroenterol Hepatol. 2015 Aug 21. doi: 10.1016/j.cgh.2015.07.051).
Having a life expectancy of 6 months or less and no personal history of polyps best predicted missing an appointment, with odds ratios of 2.74 for each factor, the researchers said. However, only 0.47% of patients had such a short life expectancy. Other significant predictors of missed appointments included being seen at the largest and most complex facilities (odds ratio, 2.69; P = .007), having both psychiatric and substance abuse disorders (OR, 1.82; P less than .0001), and the use of opt-out scheduling, in which patients were automatically scheduled rather than having to schedule appointments themselves (OR, 1.57; P = .02). Canceled appointments also were linked to opt-out scheduling, as well as to older age and having no history of polyps.
Most appointment lead times were 28 days, and each 12-day increase in lead time increased the odds of missing or canceling appointments by about 15% (P less than .0001). The problem could be curtailed by the Veterans Access, Choice and Accountability Act of 2014, which allows those who cannot schedule VA appointments within 30 days to receive care from eligible non–VA providers, the investigators said. “Future research should focus on assessing the effect of the Choice Act on colonoscopy appointment lead time and on developing and evaluating efficient and effective approaches to implementing the other clinic-level changes supported by our findings,” they added.
The study might have oversimplified or missed changes in protocols because it used single-item survey measures at one point in time, the investigators said. For some patients, the first appointment after the fecal occult blood test may have been for another procedure besides colonoscopy, they added. Furthermore, they did not distinguish between appointments canceled by patients versus clinics. “The VHA is a unique context, characterized by a predominantly male, low-income population with high rates of mental health and substance abuse diagnoses. Therefore, our findings may not generalize to other settings,” they added. “However, our findings do have important implications for a substantial population of health providers and consumers in this country, because the VHA is the largest integrated health care system in the United States.”
The study was funded by the Department of Veterans Affairs Clinical Science Service and Health Services Research & Development Service. The investigators had no disclosures.
Opt-out scheduling protocols and long appointment lead times contributed significantly to missed and canceled colonoscopy appointments at Veterans Health Administration facilities, researchers reported in the February issue of Clinical Gastroenterology and Hepatology.
These factors are within the control of the Veterans Affairs and could be altered to improve productivity and efficiency, said Melissa Partin, Ph.D., of the Center for Chronic Disease Outcomes Research at the Minneapolis Veterans Affairs Health Care System in Minneapolis, and her associates.
Source: American Gastroenterological Association
Missed and canceled medical appointments are always a concern, but particularly so for colonoscopy clinics, where they incur an average daily net loss of $725, the investigators noted. Most clinics have limited colonoscopy capacity, and even a 30-day wait for diagnostic colonoscopy has been linked to “modest but significantly elevated” chances of detecting cancer on exam, they added. To better understand these problems, they separately examined predictors of missed and canceled appointments among 27,994 patients who had positive fecal occult blood tests with diagnostic colonoscopies scheduled at 69 VA facilities between 2009 and 2011 (Clin Gastroenterol Hepatol. 2015 Aug 21. doi: 10.1016/j.cgh.2015.07.051).
Having a life expectancy of 6 months or less and no personal history of polyps best predicted missing an appointment, with odds ratios of 2.74 for each factor, the researchers said. However, only 0.47% of patients had such a short life expectancy. Other significant predictors of missed appointments included being seen at the largest and most complex facilities (odds ratio, 2.69; P = .007), having both psychiatric and substance abuse disorders (OR, 1.82; P less than .0001), and the use of opt-out scheduling, in which patients were automatically scheduled rather than having to schedule appointments themselves (OR, 1.57; P = .02). Canceled appointments also were linked to opt-out scheduling, as well as to older age and having no history of polyps.
Most appointment lead times were 28 days, and each 12-day increase in lead time increased the odds of missing or canceling appointments by about 15% (P less than .0001). The problem could be curtailed by the Veterans Access, Choice and Accountability Act of 2014, which allows those who cannot schedule VA appointments within 30 days to receive care from eligible non–VA providers, the investigators said. “Future research should focus on assessing the effect of the Choice Act on colonoscopy appointment lead time and on developing and evaluating efficient and effective approaches to implementing the other clinic-level changes supported by our findings,” they added.
The study might have oversimplified or missed changes in protocols because it used single-item survey measures at one point in time, the investigators said. For some patients, the first appointment after the fecal occult blood test may have been for another procedure besides colonoscopy, they added. Furthermore, they did not distinguish between appointments canceled by patients versus clinics. “The VHA is a unique context, characterized by a predominantly male, low-income population with high rates of mental health and substance abuse diagnoses. Therefore, our findings may not generalize to other settings,” they added. “However, our findings do have important implications for a substantial population of health providers and consumers in this country, because the VHA is the largest integrated health care system in the United States.”
The study was funded by the Department of Veterans Affairs Clinical Science Service and Health Services Research & Development Service. The investigators had no disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Opt-out scheduling practices and long appointment lead times predicted missed and canceled colonoscopies at the VA.
Major finding: Estimated ratios for these predictors ranged between 1.12 and 1.57, and all were statistically significant.
Data source: An analysis of data from 27,994 patients who had positive fecal occult blood tests with diagnostic colonoscopies scheduled at 69 VA facilities between 2009 and 2011.
Disclosures: The study was funded by the Department of Veterans Affairs Clinical Science Service and Health Services Research and Development Service. The investigators had no disclosures.