User login
2014 budget reduces spending for ACA, IPAB
A $1 trillion spending bill that funds the government through Sept. 30 restores money for some health programs but delivers a blow to the Affordable Care Act.
Even so, President Obama is expected to sign it.
The House approved the Consolidated Appropriations Act for FY 2014 (H.R. 3547) on Jan. 15 by a vote of 359-67, and the Senate approved it a day later 72-26.
Republican members of the House Appropriations Committee added language to the bill that puts a hold on any new funding for the ACA in fiscal 2014 and takes $1 billion out of the law’s Prevention and Public Health Fund. The fund is hotly contested and has been labeled a "slush fund," by opponents.
The House Appropriations panel also succeeded in cutting $10 million in funding for the Independent Payment Advisory Board (IPAB). The IPAB was due to make its first recommendations by mid-January; however, the Obama administration has yet to appoint any members.
The spending bill continues to ban the use federal funds for needle exchanges; for research that creates or uses embryos; and for abortion, except in the case of rape, incest, or endangerment of the life of the mother.
The bill includes a $3.7 billion budget for the Centers for Medicare and Medicaid Services – almost $200 million less than it received in fiscal year 2013 but equal to what it would receive under sequestration. Some $305 million is earmarked for the timely processing and payment of benefits.
The bill increases funding for other federal health-related agencies. The National Institutes of Health budget was increased $1 billion, which should allow it to begin 385 clinical trials, according to the Senate Appropriations Committee.
There is new funding for the Brain Research through Advancing of Innovative Neurotechnologies (BRAIN) Initiative, and funding for an initiative to study prevention and treatments for Alzheimer’s disease.
Mental health programs at various labor, health, and education agencies will receive $1.13 billion, an increase of $213 million, according to the Senate panel. Those programs include violence prevention and grants to schools to help train teachers and to help build a mental health workforce. The Senate Committee estimates that new training will help add 4,375 social workers, psychologists, therapists and other mental health professionals to the behavioral health workforce. The Substance Abuse and Mental Health Services Administration received a $144 million increase in its budget, bringing it to $3.6 billion.
Funding for the Centers for Disease Control and Prevention was increased $567 million to $6.9 billion. That budget includes $30 million to support the Advanced Molecular Detection initiative, which helps the agency detect and stop infectious disease outbreaks and $160 million for the Preventive Health & Health Services Block Grant.
The legislation also includes $3.6 billion to improve the quantity and quality of health care services in medically underserved areas and populations. As part of that, $350 million is appropriated to create more than 450 new community health centers and expand services at existing ones.
On Twitter @aliciaault
A $1 trillion spending bill that funds the government through Sept. 30 restores money for some health programs but delivers a blow to the Affordable Care Act.
Even so, President Obama is expected to sign it.
The House approved the Consolidated Appropriations Act for FY 2014 (H.R. 3547) on Jan. 15 by a vote of 359-67, and the Senate approved it a day later 72-26.
Republican members of the House Appropriations Committee added language to the bill that puts a hold on any new funding for the ACA in fiscal 2014 and takes $1 billion out of the law’s Prevention and Public Health Fund. The fund is hotly contested and has been labeled a "slush fund," by opponents.
The House Appropriations panel also succeeded in cutting $10 million in funding for the Independent Payment Advisory Board (IPAB). The IPAB was due to make its first recommendations by mid-January; however, the Obama administration has yet to appoint any members.
The spending bill continues to ban the use federal funds for needle exchanges; for research that creates or uses embryos; and for abortion, except in the case of rape, incest, or endangerment of the life of the mother.
The bill includes a $3.7 billion budget for the Centers for Medicare and Medicaid Services – almost $200 million less than it received in fiscal year 2013 but equal to what it would receive under sequestration. Some $305 million is earmarked for the timely processing and payment of benefits.
The bill increases funding for other federal health-related agencies. The National Institutes of Health budget was increased $1 billion, which should allow it to begin 385 clinical trials, according to the Senate Appropriations Committee.
There is new funding for the Brain Research through Advancing of Innovative Neurotechnologies (BRAIN) Initiative, and funding for an initiative to study prevention and treatments for Alzheimer’s disease.
Mental health programs at various labor, health, and education agencies will receive $1.13 billion, an increase of $213 million, according to the Senate panel. Those programs include violence prevention and grants to schools to help train teachers and to help build a mental health workforce. The Senate Committee estimates that new training will help add 4,375 social workers, psychologists, therapists and other mental health professionals to the behavioral health workforce. The Substance Abuse and Mental Health Services Administration received a $144 million increase in its budget, bringing it to $3.6 billion.
Funding for the Centers for Disease Control and Prevention was increased $567 million to $6.9 billion. That budget includes $30 million to support the Advanced Molecular Detection initiative, which helps the agency detect and stop infectious disease outbreaks and $160 million for the Preventive Health & Health Services Block Grant.
The legislation also includes $3.6 billion to improve the quantity and quality of health care services in medically underserved areas and populations. As part of that, $350 million is appropriated to create more than 450 new community health centers and expand services at existing ones.
On Twitter @aliciaault
A $1 trillion spending bill that funds the government through Sept. 30 restores money for some health programs but delivers a blow to the Affordable Care Act.
Even so, President Obama is expected to sign it.
The House approved the Consolidated Appropriations Act for FY 2014 (H.R. 3547) on Jan. 15 by a vote of 359-67, and the Senate approved it a day later 72-26.
Republican members of the House Appropriations Committee added language to the bill that puts a hold on any new funding for the ACA in fiscal 2014 and takes $1 billion out of the law’s Prevention and Public Health Fund. The fund is hotly contested and has been labeled a "slush fund," by opponents.
The House Appropriations panel also succeeded in cutting $10 million in funding for the Independent Payment Advisory Board (IPAB). The IPAB was due to make its first recommendations by mid-January; however, the Obama administration has yet to appoint any members.
The spending bill continues to ban the use federal funds for needle exchanges; for research that creates or uses embryos; and for abortion, except in the case of rape, incest, or endangerment of the life of the mother.
The bill includes a $3.7 billion budget for the Centers for Medicare and Medicaid Services – almost $200 million less than it received in fiscal year 2013 but equal to what it would receive under sequestration. Some $305 million is earmarked for the timely processing and payment of benefits.
The bill increases funding for other federal health-related agencies. The National Institutes of Health budget was increased $1 billion, which should allow it to begin 385 clinical trials, according to the Senate Appropriations Committee.
There is new funding for the Brain Research through Advancing of Innovative Neurotechnologies (BRAIN) Initiative, and funding for an initiative to study prevention and treatments for Alzheimer’s disease.
Mental health programs at various labor, health, and education agencies will receive $1.13 billion, an increase of $213 million, according to the Senate panel. Those programs include violence prevention and grants to schools to help train teachers and to help build a mental health workforce. The Senate Committee estimates that new training will help add 4,375 social workers, psychologists, therapists and other mental health professionals to the behavioral health workforce. The Substance Abuse and Mental Health Services Administration received a $144 million increase in its budget, bringing it to $3.6 billion.
Funding for the Centers for Disease Control and Prevention was increased $567 million to $6.9 billion. That budget includes $30 million to support the Advanced Molecular Detection initiative, which helps the agency detect and stop infectious disease outbreaks and $160 million for the Preventive Health & Health Services Block Grant.
The legislation also includes $3.6 billion to improve the quantity and quality of health care services in medically underserved areas and populations. As part of that, $350 million is appropriated to create more than 450 new community health centers and expand services at existing ones.
On Twitter @aliciaault
Surgeon General report links smoking to diseases beyond cancer
While smoking rates have dropped precipitously since the landmark 1964 Surgeon General’s report, "Smoking and Health," smoking is still the leading cause of preventable disease and death in the United States and is now causally linked to additional diseases and conditions across most organ systems.
A new Surgeon General's report, "The Health Consequences of Smoking – 50 Years of Progress," released at a White House event Jan. 17, synthesizes original and review evidence in an effort to further federal antismoking efforts.
The report causally links cigarette smoking to type 2 diabetes, rheumatoid arthritis, ectopic pregnancy, and erectile dysfunction. Secondhand smoke is now causally linked to cancers, respiratory diseases, and cardiovascular diseases, as well as adverse effects on the health of children, the authors wrote.
In addition, the 980-page report establishes that secondhand smoke is a cause of stroke, and that smoking increases the risk of dying in cancer patients and cancer survivors.
Another finding: Cigarette smokers today have a higher risk of lung cancer than did those who smoked in 1964, because of the higher number of chemical additives now used.
Women smokers now have the same risk of death from lung cancer as that of men and a higher relative risk of dying from coronary heart disease than that of men. Because of smoking, the number of women dying from chronic obstructive pulmonary disease (COPD) is now higher than in men.
With this report, the federal government is launching a new effort to prevent children from using tobacco.
"Today, we’re asking Americans to join a sustained effort to make the next generation a tobacco-free generation," Health and Human Services Secretary Kathleen Sebelius said in a statement. "This is not something the federal government can do alone. We need to partner with the business community, local elected officials, schools and universities, the medical community, the faith community, and committed citizens in communities across the country to make the next generation tobacco free."
The report finds that youth smoking rates declined by 50% between 1997 and 2011, but 3,200 children under age 18 still start smoking each day, and an additional 2,100 youth and young adults become daily smokers. The report places most of the blame for continued interest in smoking on the tobacco industry, saying it has used "aggressive strategies" to deliberately mislead the public about the harms of smoking.
Acting Surgeon General Boris Lushniak noted that smoking rates are disproportionately higher among people with less education and lower incomes, among the mentally ill, and among gay, lesbian, bisexual, and transgender individuals.
Dr. Lushniak and other officials at the White House event called for greater tobacco control efforts, including stricter regulation. The Food and Drug Administration was given the power to regulate tobacco through the 2009 Family Smoking Prevention and Tobacco Control Act.
FDA Commissioner Margaret Hamburg said that the agency is ready to take action.
"The FDA is funding and conducting regulatory science research on tobacco products, enforcing the laws that reduce the access and attractiveness of tobacco products to young people, and preparing to launch an unprecedented national public education campaign to prevent youth tobacco use," Dr. Hamburg said in a statement.
Dr. Thomas R. Frieden, director of the Centers for Disease Control and Prevention, noted that while states collect some $80 per person a year in tobacco taxes and payments from the 1998 tobacco industry master settlement agreement, they spend an average of $1.50 per person on control.
The CDC has urged states to spend $12 per person on control, Dr. Frieden said.
Dr. Lushniak noted that for current and about-to-start smokers, "the clock is ticking – they can’t wait for slow and steady progress to end the epidemic. Enough is enough."
On Twitter @aliciaault
While smoking rates have dropped precipitously since the landmark 1964 Surgeon General’s report, "Smoking and Health," smoking is still the leading cause of preventable disease and death in the United States and is now causally linked to additional diseases and conditions across most organ systems.
A new Surgeon General's report, "The Health Consequences of Smoking – 50 Years of Progress," released at a White House event Jan. 17, synthesizes original and review evidence in an effort to further federal antismoking efforts.
The report causally links cigarette smoking to type 2 diabetes, rheumatoid arthritis, ectopic pregnancy, and erectile dysfunction. Secondhand smoke is now causally linked to cancers, respiratory diseases, and cardiovascular diseases, as well as adverse effects on the health of children, the authors wrote.
In addition, the 980-page report establishes that secondhand smoke is a cause of stroke, and that smoking increases the risk of dying in cancer patients and cancer survivors.
Another finding: Cigarette smokers today have a higher risk of lung cancer than did those who smoked in 1964, because of the higher number of chemical additives now used.
Women smokers now have the same risk of death from lung cancer as that of men and a higher relative risk of dying from coronary heart disease than that of men. Because of smoking, the number of women dying from chronic obstructive pulmonary disease (COPD) is now higher than in men.
With this report, the federal government is launching a new effort to prevent children from using tobacco.
"Today, we’re asking Americans to join a sustained effort to make the next generation a tobacco-free generation," Health and Human Services Secretary Kathleen Sebelius said in a statement. "This is not something the federal government can do alone. We need to partner with the business community, local elected officials, schools and universities, the medical community, the faith community, and committed citizens in communities across the country to make the next generation tobacco free."
The report finds that youth smoking rates declined by 50% between 1997 and 2011, but 3,200 children under age 18 still start smoking each day, and an additional 2,100 youth and young adults become daily smokers. The report places most of the blame for continued interest in smoking on the tobacco industry, saying it has used "aggressive strategies" to deliberately mislead the public about the harms of smoking.
Acting Surgeon General Boris Lushniak noted that smoking rates are disproportionately higher among people with less education and lower incomes, among the mentally ill, and among gay, lesbian, bisexual, and transgender individuals.
Dr. Lushniak and other officials at the White House event called for greater tobacco control efforts, including stricter regulation. The Food and Drug Administration was given the power to regulate tobacco through the 2009 Family Smoking Prevention and Tobacco Control Act.
FDA Commissioner Margaret Hamburg said that the agency is ready to take action.
"The FDA is funding and conducting regulatory science research on tobacco products, enforcing the laws that reduce the access and attractiveness of tobacco products to young people, and preparing to launch an unprecedented national public education campaign to prevent youth tobacco use," Dr. Hamburg said in a statement.
Dr. Thomas R. Frieden, director of the Centers for Disease Control and Prevention, noted that while states collect some $80 per person a year in tobacco taxes and payments from the 1998 tobacco industry master settlement agreement, they spend an average of $1.50 per person on control.
The CDC has urged states to spend $12 per person on control, Dr. Frieden said.
Dr. Lushniak noted that for current and about-to-start smokers, "the clock is ticking – they can’t wait for slow and steady progress to end the epidemic. Enough is enough."
On Twitter @aliciaault
While smoking rates have dropped precipitously since the landmark 1964 Surgeon General’s report, "Smoking and Health," smoking is still the leading cause of preventable disease and death in the United States and is now causally linked to additional diseases and conditions across most organ systems.
A new Surgeon General's report, "The Health Consequences of Smoking – 50 Years of Progress," released at a White House event Jan. 17, synthesizes original and review evidence in an effort to further federal antismoking efforts.
The report causally links cigarette smoking to type 2 diabetes, rheumatoid arthritis, ectopic pregnancy, and erectile dysfunction. Secondhand smoke is now causally linked to cancers, respiratory diseases, and cardiovascular diseases, as well as adverse effects on the health of children, the authors wrote.
In addition, the 980-page report establishes that secondhand smoke is a cause of stroke, and that smoking increases the risk of dying in cancer patients and cancer survivors.
Another finding: Cigarette smokers today have a higher risk of lung cancer than did those who smoked in 1964, because of the higher number of chemical additives now used.
Women smokers now have the same risk of death from lung cancer as that of men and a higher relative risk of dying from coronary heart disease than that of men. Because of smoking, the number of women dying from chronic obstructive pulmonary disease (COPD) is now higher than in men.
With this report, the federal government is launching a new effort to prevent children from using tobacco.
"Today, we’re asking Americans to join a sustained effort to make the next generation a tobacco-free generation," Health and Human Services Secretary Kathleen Sebelius said in a statement. "This is not something the federal government can do alone. We need to partner with the business community, local elected officials, schools and universities, the medical community, the faith community, and committed citizens in communities across the country to make the next generation tobacco free."
The report finds that youth smoking rates declined by 50% between 1997 and 2011, but 3,200 children under age 18 still start smoking each day, and an additional 2,100 youth and young adults become daily smokers. The report places most of the blame for continued interest in smoking on the tobacco industry, saying it has used "aggressive strategies" to deliberately mislead the public about the harms of smoking.
Acting Surgeon General Boris Lushniak noted that smoking rates are disproportionately higher among people with less education and lower incomes, among the mentally ill, and among gay, lesbian, bisexual, and transgender individuals.
Dr. Lushniak and other officials at the White House event called for greater tobacco control efforts, including stricter regulation. The Food and Drug Administration was given the power to regulate tobacco through the 2009 Family Smoking Prevention and Tobacco Control Act.
FDA Commissioner Margaret Hamburg said that the agency is ready to take action.
"The FDA is funding and conducting regulatory science research on tobacco products, enforcing the laws that reduce the access and attractiveness of tobacco products to young people, and preparing to launch an unprecedented national public education campaign to prevent youth tobacco use," Dr. Hamburg said in a statement.
Dr. Thomas R. Frieden, director of the Centers for Disease Control and Prevention, noted that while states collect some $80 per person a year in tobacco taxes and payments from the 1998 tobacco industry master settlement agreement, they spend an average of $1.50 per person on control.
The CDC has urged states to spend $12 per person on control, Dr. Frieden said.
Dr. Lushniak noted that for current and about-to-start smokers, "the clock is ticking – they can’t wait for slow and steady progress to end the epidemic. Enough is enough."
On Twitter @aliciaault
FDA: Stop prescribing combo drugs with high-dose acetaminophen
The Food and Drug Administration is turning to doctors, dentists, and pharmacists to accomplish what some drug manufacturers won’t help it do.
In 2011, the agency recommended manufacturers cease marketing of acetaminophen/opioid combination products with more than 325 mg of acetaminophen per dose, in an effort to reduce the risk of severe liver injury. Not all manufacturers complied.
Now, the agency on Jan. 14 issued a MedWatch recommendation that health care providers refrain from prescribing combinations with larger acetaminophen doses. The recommendation goes further, urging pharmacists to contact prescribers when they receive a prescription for a combination product with more than 325 mg of acetaminophen per dose to discuss a substitute product with a lower acetaminophen dose.
"Inadvertent overdose from prescription combination drugs containing acetaminophen accounts for nearly half of all cases of acetaminophen-related liver failure in the United States, some of which result in liver transplant or death," the agency said, in a statement.
In the same 2011 notice, the FDA is requiring prescription acetaminophen combinations to carry a boxed warning on the potential for liver damage.
Acetaminophen-containing prescription combinations are among the most-prescribed pharmaceuticals in the United States, and include products such as Vicodin (acetaminophen/hydrocodone), Percocet (acetaminophen/oxycodone), and Tylenol with codeine.
The FDA has been examining acetaminophen since at least 2002. The recommendations of a joint meeting of several advisory committees in 2009 resulted in the 2011 policy changes and recommendations.
The agency now has sent letters to manufacturers that have not lowered the acetaminophen dose warning them that the FDA will withdraw approval of those products.
Physicians can report adverse events or side effects related to the use of acetaminophen products to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program either online or at 800-332-1088.
On Twitter @aliciaault
The Food and Drug Administration is turning to doctors, dentists, and pharmacists to accomplish what some drug manufacturers won’t help it do.
In 2011, the agency recommended manufacturers cease marketing of acetaminophen/opioid combination products with more than 325 mg of acetaminophen per dose, in an effort to reduce the risk of severe liver injury. Not all manufacturers complied.
Now, the agency on Jan. 14 issued a MedWatch recommendation that health care providers refrain from prescribing combinations with larger acetaminophen doses. The recommendation goes further, urging pharmacists to contact prescribers when they receive a prescription for a combination product with more than 325 mg of acetaminophen per dose to discuss a substitute product with a lower acetaminophen dose.
"Inadvertent overdose from prescription combination drugs containing acetaminophen accounts for nearly half of all cases of acetaminophen-related liver failure in the United States, some of which result in liver transplant or death," the agency said, in a statement.
In the same 2011 notice, the FDA is requiring prescription acetaminophen combinations to carry a boxed warning on the potential for liver damage.
Acetaminophen-containing prescription combinations are among the most-prescribed pharmaceuticals in the United States, and include products such as Vicodin (acetaminophen/hydrocodone), Percocet (acetaminophen/oxycodone), and Tylenol with codeine.
The FDA has been examining acetaminophen since at least 2002. The recommendations of a joint meeting of several advisory committees in 2009 resulted in the 2011 policy changes and recommendations.
The agency now has sent letters to manufacturers that have not lowered the acetaminophen dose warning them that the FDA will withdraw approval of those products.
Physicians can report adverse events or side effects related to the use of acetaminophen products to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program either online or at 800-332-1088.
On Twitter @aliciaault
The Food and Drug Administration is turning to doctors, dentists, and pharmacists to accomplish what some drug manufacturers won’t help it do.
In 2011, the agency recommended manufacturers cease marketing of acetaminophen/opioid combination products with more than 325 mg of acetaminophen per dose, in an effort to reduce the risk of severe liver injury. Not all manufacturers complied.
Now, the agency on Jan. 14 issued a MedWatch recommendation that health care providers refrain from prescribing combinations with larger acetaminophen doses. The recommendation goes further, urging pharmacists to contact prescribers when they receive a prescription for a combination product with more than 325 mg of acetaminophen per dose to discuss a substitute product with a lower acetaminophen dose.
"Inadvertent overdose from prescription combination drugs containing acetaminophen accounts for nearly half of all cases of acetaminophen-related liver failure in the United States, some of which result in liver transplant or death," the agency said, in a statement.
In the same 2011 notice, the FDA is requiring prescription acetaminophen combinations to carry a boxed warning on the potential for liver damage.
Acetaminophen-containing prescription combinations are among the most-prescribed pharmaceuticals in the United States, and include products such as Vicodin (acetaminophen/hydrocodone), Percocet (acetaminophen/oxycodone), and Tylenol with codeine.
The FDA has been examining acetaminophen since at least 2002. The recommendations of a joint meeting of several advisory committees in 2009 resulted in the 2011 policy changes and recommendations.
The agency now has sent letters to manufacturers that have not lowered the acetaminophen dose warning them that the FDA will withdraw approval of those products.
Physicians can report adverse events or side effects related to the use of acetaminophen products to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program either online or at 800-332-1088.
On Twitter @aliciaault
Rural Coverage a Key to Meeting Primary Care Demand
WASHINGTON – Rural family medicine residency programs are doing what they can to attract more primary care physicians to underserved areas and keep them there, but they are faced with an ever-larger task. Rural communities will be the most hard-pressed to meet growing demand for physicians as more Americans gain health insurance and seek a regular medical care provider, said several experts at a forum on Capitol Hill sponsored by the American Academy of Family Physicians.
The majority of the nation’s rural areas are underserved by physicians, and in particular by primary care.
The problem is exacerbated by the fact that the number of medical school students choosing primary care residencies still lags far behind those electing to pursue other specialties, said Dr. Ted Epperly, president and chief executive officer of the Family Medicine Residency of Idaho in Boise.
"It all starts with making sure we have a pipeline developed of training broad, well-trained, comprehensivists," said Dr. Epperly. Generalism is the most important attribute needed for primary care, but "what we’ve created is a system of subspecialization, so at a time when we need a complex skill set to be able to handle problems, we’ve micro-detailed our physicians into looking at the left kidney," Dr. Epperly said.
Some 62 million Americans, or 20% of the nation’s population, live in a rural area, said Amy Elizondo, vice president of program services at the National Rural Health Association. Only 9% of the nation’s physicians practice in rural areas, and 77% of the 2,050 rural counties in America are designated as Health Professional Shortage Areas by the Health Resources and Services Administration (HRSA). A shortage area is one in which there is one or fewer primary care physicians per 3,500 people, according to HRSA. The agency estimates that, as of Nov. 14, there were 5,800 total primary care shortage areas in the United States, which can be located in urban or rural areas. It would take an additional 7,500 primary care physicians to end the shortages in all of those areas, said HRSA.
Physician organizations and HRSA, among others, have been trying to figure out how to draw more primary care doctors to those areas. The Affordable Care Act established a grant program for states looking to study their workforce issues, but so far HRSA has not been given any money by Congress to fund any grants. When the State Health Workforce Development Grants were announced in 2010, the Department of Health and Human Services said that almost $6 million would be made available to 26 states.
The ACA also established a National Health Care Workforce Commission, but that, too, has never been funded, although members were appointed in 2010 by the head of the Government Accountability Office. The GAO was given the authority under the health law to appoint the commission’s members.
"Right now we don’t have a unified policy or approach to addressing our workforce," said Dr. Stan Kozakowski, director of medical education at the American Academy of Family Physicians.
Dr. Kozakowski said that another way to boost the numbers of rural physicians was to increase training slots devoted to family medicine and, more specifically, residents trained in delivering medicine in rural areas.
A number of family medicine residency programs have developed a rural training track, which requires residents to spend 1 year in the larger academic medical center, followed by 2 years in the rural area, which may or may not have a hospital. Currently, there are 26 active rural training track programs. All are strapped for funding because fewer than half are eligible to receive traditional graduate medical education funding from the Centers for Medicare and Medicaid Services (CMS), said Dr. Randall Longenecker, professor of family medicine and assistant dean for rural and underserved programsat the Ohio University Heritage College of Osteopathic Medicine in Athens.
But the programs have proven to be effective, said Dr. Longenecker, who is also the executive director of the new nonprofit RTT Collaborative. He cited data showing that, 3 years after graduation, almost half of recent rural training track participants had continued to practice in rural areas and about a third were serving in professional shortage areas.
"The biggest challenge for retention is getting people to live in a rural place," said Dr. Longenecker, adding that, by living and training in the area for 2 years, physicians learn how to live there.
"The longer they stay, the longer they stay," agreed Dr. Epperly. He said that 85% of the physicians trained through the rural sites of the Family Medicine Residency of Idaho end up practicing in those areas. Another key is to help spouses become acclimated, which his program does through group outreach, Dr. Epperly said.
He noted that 35 of the nation’s 165 medical schools have started to look at training for rural areas in "a more serious way."
In addition, 13 states are contemplating developing rural track training, said Dr. Longenecker.
On Twitter @aliciaault
WASHINGTON – Rural family medicine residency programs are doing what they can to attract more primary care physicians to underserved areas and keep them there, but they are faced with an ever-larger task. Rural communities will be the most hard-pressed to meet growing demand for physicians as more Americans gain health insurance and seek a regular medical care provider, said several experts at a forum on Capitol Hill sponsored by the American Academy of Family Physicians.
The majority of the nation’s rural areas are underserved by physicians, and in particular by primary care.
The problem is exacerbated by the fact that the number of medical school students choosing primary care residencies still lags far behind those electing to pursue other specialties, said Dr. Ted Epperly, president and chief executive officer of the Family Medicine Residency of Idaho in Boise.
"It all starts with making sure we have a pipeline developed of training broad, well-trained, comprehensivists," said Dr. Epperly. Generalism is the most important attribute needed for primary care, but "what we’ve created is a system of subspecialization, so at a time when we need a complex skill set to be able to handle problems, we’ve micro-detailed our physicians into looking at the left kidney," Dr. Epperly said.
Some 62 million Americans, or 20% of the nation’s population, live in a rural area, said Amy Elizondo, vice president of program services at the National Rural Health Association. Only 9% of the nation’s physicians practice in rural areas, and 77% of the 2,050 rural counties in America are designated as Health Professional Shortage Areas by the Health Resources and Services Administration (HRSA). A shortage area is one in which there is one or fewer primary care physicians per 3,500 people, according to HRSA. The agency estimates that, as of Nov. 14, there were 5,800 total primary care shortage areas in the United States, which can be located in urban or rural areas. It would take an additional 7,500 primary care physicians to end the shortages in all of those areas, said HRSA.
Physician organizations and HRSA, among others, have been trying to figure out how to draw more primary care doctors to those areas. The Affordable Care Act established a grant program for states looking to study their workforce issues, but so far HRSA has not been given any money by Congress to fund any grants. When the State Health Workforce Development Grants were announced in 2010, the Department of Health and Human Services said that almost $6 million would be made available to 26 states.
The ACA also established a National Health Care Workforce Commission, but that, too, has never been funded, although members were appointed in 2010 by the head of the Government Accountability Office. The GAO was given the authority under the health law to appoint the commission’s members.
"Right now we don’t have a unified policy or approach to addressing our workforce," said Dr. Stan Kozakowski, director of medical education at the American Academy of Family Physicians.
Dr. Kozakowski said that another way to boost the numbers of rural physicians was to increase training slots devoted to family medicine and, more specifically, residents trained in delivering medicine in rural areas.
A number of family medicine residency programs have developed a rural training track, which requires residents to spend 1 year in the larger academic medical center, followed by 2 years in the rural area, which may or may not have a hospital. Currently, there are 26 active rural training track programs. All are strapped for funding because fewer than half are eligible to receive traditional graduate medical education funding from the Centers for Medicare and Medicaid Services (CMS), said Dr. Randall Longenecker, professor of family medicine and assistant dean for rural and underserved programsat the Ohio University Heritage College of Osteopathic Medicine in Athens.
But the programs have proven to be effective, said Dr. Longenecker, who is also the executive director of the new nonprofit RTT Collaborative. He cited data showing that, 3 years after graduation, almost half of recent rural training track participants had continued to practice in rural areas and about a third were serving in professional shortage areas.
"The biggest challenge for retention is getting people to live in a rural place," said Dr. Longenecker, adding that, by living and training in the area for 2 years, physicians learn how to live there.
"The longer they stay, the longer they stay," agreed Dr. Epperly. He said that 85% of the physicians trained through the rural sites of the Family Medicine Residency of Idaho end up practicing in those areas. Another key is to help spouses become acclimated, which his program does through group outreach, Dr. Epperly said.
He noted that 35 of the nation’s 165 medical schools have started to look at training for rural areas in "a more serious way."
In addition, 13 states are contemplating developing rural track training, said Dr. Longenecker.
On Twitter @aliciaault
WASHINGTON – Rural family medicine residency programs are doing what they can to attract more primary care physicians to underserved areas and keep them there, but they are faced with an ever-larger task. Rural communities will be the most hard-pressed to meet growing demand for physicians as more Americans gain health insurance and seek a regular medical care provider, said several experts at a forum on Capitol Hill sponsored by the American Academy of Family Physicians.
The majority of the nation’s rural areas are underserved by physicians, and in particular by primary care.
The problem is exacerbated by the fact that the number of medical school students choosing primary care residencies still lags far behind those electing to pursue other specialties, said Dr. Ted Epperly, president and chief executive officer of the Family Medicine Residency of Idaho in Boise.
"It all starts with making sure we have a pipeline developed of training broad, well-trained, comprehensivists," said Dr. Epperly. Generalism is the most important attribute needed for primary care, but "what we’ve created is a system of subspecialization, so at a time when we need a complex skill set to be able to handle problems, we’ve micro-detailed our physicians into looking at the left kidney," Dr. Epperly said.
Some 62 million Americans, or 20% of the nation’s population, live in a rural area, said Amy Elizondo, vice president of program services at the National Rural Health Association. Only 9% of the nation’s physicians practice in rural areas, and 77% of the 2,050 rural counties in America are designated as Health Professional Shortage Areas by the Health Resources and Services Administration (HRSA). A shortage area is one in which there is one or fewer primary care physicians per 3,500 people, according to HRSA. The agency estimates that, as of Nov. 14, there were 5,800 total primary care shortage areas in the United States, which can be located in urban or rural areas. It would take an additional 7,500 primary care physicians to end the shortages in all of those areas, said HRSA.
Physician organizations and HRSA, among others, have been trying to figure out how to draw more primary care doctors to those areas. The Affordable Care Act established a grant program for states looking to study their workforce issues, but so far HRSA has not been given any money by Congress to fund any grants. When the State Health Workforce Development Grants were announced in 2010, the Department of Health and Human Services said that almost $6 million would be made available to 26 states.
The ACA also established a National Health Care Workforce Commission, but that, too, has never been funded, although members were appointed in 2010 by the head of the Government Accountability Office. The GAO was given the authority under the health law to appoint the commission’s members.
"Right now we don’t have a unified policy or approach to addressing our workforce," said Dr. Stan Kozakowski, director of medical education at the American Academy of Family Physicians.
Dr. Kozakowski said that another way to boost the numbers of rural physicians was to increase training slots devoted to family medicine and, more specifically, residents trained in delivering medicine in rural areas.
A number of family medicine residency programs have developed a rural training track, which requires residents to spend 1 year in the larger academic medical center, followed by 2 years in the rural area, which may or may not have a hospital. Currently, there are 26 active rural training track programs. All are strapped for funding because fewer than half are eligible to receive traditional graduate medical education funding from the Centers for Medicare and Medicaid Services (CMS), said Dr. Randall Longenecker, professor of family medicine and assistant dean for rural and underserved programsat the Ohio University Heritage College of Osteopathic Medicine in Athens.
But the programs have proven to be effective, said Dr. Longenecker, who is also the executive director of the new nonprofit RTT Collaborative. He cited data showing that, 3 years after graduation, almost half of recent rural training track participants had continued to practice in rural areas and about a third were serving in professional shortage areas.
"The biggest challenge for retention is getting people to live in a rural place," said Dr. Longenecker, adding that, by living and training in the area for 2 years, physicians learn how to live there.
"The longer they stay, the longer they stay," agreed Dr. Epperly. He said that 85% of the physicians trained through the rural sites of the Family Medicine Residency of Idaho end up practicing in those areas. Another key is to help spouses become acclimated, which his program does through group outreach, Dr. Epperly said.
He noted that 35 of the nation’s 165 medical schools have started to look at training for rural areas in "a more serious way."
In addition, 13 states are contemplating developing rural track training, said Dr. Longenecker.
On Twitter @aliciaault
FROM AN AAFP BRIEFING
Rural coverage a key to meeting primary care demand
WASHINGTON – Rural family medicine residency programs are doing what they can to attract more primary care physicians to underserved areas and keep them there, but they are faced with an ever-larger task. Rural communities will be the most hard-pressed to meet growing demand for physicians as more Americans gain health insurance and seek a regular medical care provider, said several experts at a forum on Capitol Hill sponsored by the American Academy of Family Physicians.
The majority of the nation’s rural areas are underserved by physicians, and in particular by primary care.
The problem is exacerbated by the fact that the number of medical school students choosing primary care residencies still lags far behind those electing to pursue other specialties, said Dr. Ted Epperly, president and chief executive officer of the Family Medicine Residency of Idaho in Boise.
"It all starts with making sure we have a pipeline developed of training broad, well-trained, comprehensivists," said Dr. Epperly. Generalism is the most important attribute needed for primary care, but "what we’ve created is a system of subspecialization, so at a time when we need a complex skill set to be able to handle problems, we’ve micro-detailed our physicians into looking at the left kidney," Dr. Epperly said.
Some 62 million Americans, or 20% of the nation’s population, live in a rural area, said Amy Elizondo, vice president of program services at the National Rural Health Association. Only 9% of the nation’s physicians practice in rural areas, and 77% of the 2,050 rural counties in America are designated as Health Professional Shortage Areas by the Health Resources and Services Administration (HRSA). A shortage area is one in which there is one or fewer primary care physicians per 3,500 people, according to HRSA. The agency estimates that, as of Nov. 14, there were 5,800 total primary care shortage areas in the United States, which can be located in urban or rural areas. It would take an additional 7,500 primary care physicians to end the shortages in all of those areas, said HRSA.
Physician organizations and HRSA, among others, have been trying to figure out how to draw more primary care doctors to those areas. The Affordable Care Act established a grant program for states looking to study their workforce issues, but so far HRSA has not been given any money by Congress to fund any grants. When the State Health Workforce Development Grants were announced in 2010, the Department of Health and Human Services said that almost $6 million would be made available to 26 states.
The ACA also established a National Health Care Workforce Commission, but that, too, has never been funded, although members were appointed in 2010 by the head of the Government Accountability Office. The GAO was given the authority under the health law to appoint the commission’s members.
"Right now we don’t have a unified policy or approach to addressing our workforce," said Dr. Stan Kozakowski, director of medical education at the American Academy of Family Physicians.
Dr. Kozakowski said that another way to boost the numbers of rural physicians was to increase training slots devoted to family medicine and, more specifically, residents trained in delivering medicine in rural areas.
A number of family medicine residency programs have developed a rural training track, which requires residents to spend 1 year in the larger academic medical center, followed by 2 years in the rural area, which may or may not have a hospital. Currently, there are 26 active rural training track programs. All are strapped for funding because fewer than half are eligible to receive traditional graduate medical education funding from the Centers for Medicare and Medicaid Services (CMS), said Dr. Randall Longenecker, professor of family medicine and assistant dean for rural and underserved programsat the Ohio University Heritage College of Osteopathic Medicine in Athens.
But the programs have proven to be effective, said Dr. Longenecker, who is also the executive director of the new nonprofit RTT Collaborative. He cited data showing that, 3 years after graduation, almost half of recent rural training track participants had continued to practice in rural areas and about a third were serving in professional shortage areas.
"The biggest challenge for retention is getting people to live in a rural place," said Dr. Longenecker, adding that, by living and training in the area for 2 years, physicians learn how to live there.
"The longer they stay, the longer they stay," agreed Dr. Epperly. He said that 85% of the physicians trained through the rural sites of the Family Medicine Residency of Idaho end up practicing in those areas. Another key is to help spouses become acclimated, which his program does through group outreach, Dr. Epperly said.
He noted that 35 of the nation’s 165 medical schools have started to look at training for rural areas in "a more serious way."
In addition, 13 states are contemplating developing rural track training, said Dr. Longenecker.
On Twitter @aliciaault
WASHINGTON – Rural family medicine residency programs are doing what they can to attract more primary care physicians to underserved areas and keep them there, but they are faced with an ever-larger task. Rural communities will be the most hard-pressed to meet growing demand for physicians as more Americans gain health insurance and seek a regular medical care provider, said several experts at a forum on Capitol Hill sponsored by the American Academy of Family Physicians.
The majority of the nation’s rural areas are underserved by physicians, and in particular by primary care.
The problem is exacerbated by the fact that the number of medical school students choosing primary care residencies still lags far behind those electing to pursue other specialties, said Dr. Ted Epperly, president and chief executive officer of the Family Medicine Residency of Idaho in Boise.
"It all starts with making sure we have a pipeline developed of training broad, well-trained, comprehensivists," said Dr. Epperly. Generalism is the most important attribute needed for primary care, but "what we’ve created is a system of subspecialization, so at a time when we need a complex skill set to be able to handle problems, we’ve micro-detailed our physicians into looking at the left kidney," Dr. Epperly said.
Some 62 million Americans, or 20% of the nation’s population, live in a rural area, said Amy Elizondo, vice president of program services at the National Rural Health Association. Only 9% of the nation’s physicians practice in rural areas, and 77% of the 2,050 rural counties in America are designated as Health Professional Shortage Areas by the Health Resources and Services Administration (HRSA). A shortage area is one in which there is one or fewer primary care physicians per 3,500 people, according to HRSA. The agency estimates that, as of Nov. 14, there were 5,800 total primary care shortage areas in the United States, which can be located in urban or rural areas. It would take an additional 7,500 primary care physicians to end the shortages in all of those areas, said HRSA.
Physician organizations and HRSA, among others, have been trying to figure out how to draw more primary care doctors to those areas. The Affordable Care Act established a grant program for states looking to study their workforce issues, but so far HRSA has not been given any money by Congress to fund any grants. When the State Health Workforce Development Grants were announced in 2010, the Department of Health and Human Services said that almost $6 million would be made available to 26 states.
The ACA also established a National Health Care Workforce Commission, but that, too, has never been funded, although members were appointed in 2010 by the head of the Government Accountability Office. The GAO was given the authority under the health law to appoint the commission’s members.
"Right now we don’t have a unified policy or approach to addressing our workforce," said Dr. Stan Kozakowski, director of medical education at the American Academy of Family Physicians.
Dr. Kozakowski said that another way to boost the numbers of rural physicians was to increase training slots devoted to family medicine and, more specifically, residents trained in delivering medicine in rural areas.
A number of family medicine residency programs have developed a rural training track, which requires residents to spend 1 year in the larger academic medical center, followed by 2 years in the rural area, which may or may not have a hospital. Currently, there are 26 active rural training track programs. All are strapped for funding because fewer than half are eligible to receive traditional graduate medical education funding from the Centers for Medicare and Medicaid Services (CMS), said Dr. Randall Longenecker, professor of family medicine and assistant dean for rural and underserved programsat the Ohio University Heritage College of Osteopathic Medicine in Athens.
But the programs have proven to be effective, said Dr. Longenecker, who is also the executive director of the new nonprofit RTT Collaborative. He cited data showing that, 3 years after graduation, almost half of recent rural training track participants had continued to practice in rural areas and about a third were serving in professional shortage areas.
"The biggest challenge for retention is getting people to live in a rural place," said Dr. Longenecker, adding that, by living and training in the area for 2 years, physicians learn how to live there.
"The longer they stay, the longer they stay," agreed Dr. Epperly. He said that 85% of the physicians trained through the rural sites of the Family Medicine Residency of Idaho end up practicing in those areas. Another key is to help spouses become acclimated, which his program does through group outreach, Dr. Epperly said.
He noted that 35 of the nation’s 165 medical schools have started to look at training for rural areas in "a more serious way."
In addition, 13 states are contemplating developing rural track training, said Dr. Longenecker.
On Twitter @aliciaault
WASHINGTON – Rural family medicine residency programs are doing what they can to attract more primary care physicians to underserved areas and keep them there, but they are faced with an ever-larger task. Rural communities will be the most hard-pressed to meet growing demand for physicians as more Americans gain health insurance and seek a regular medical care provider, said several experts at a forum on Capitol Hill sponsored by the American Academy of Family Physicians.
The majority of the nation’s rural areas are underserved by physicians, and in particular by primary care.
The problem is exacerbated by the fact that the number of medical school students choosing primary care residencies still lags far behind those electing to pursue other specialties, said Dr. Ted Epperly, president and chief executive officer of the Family Medicine Residency of Idaho in Boise.
"It all starts with making sure we have a pipeline developed of training broad, well-trained, comprehensivists," said Dr. Epperly. Generalism is the most important attribute needed for primary care, but "what we’ve created is a system of subspecialization, so at a time when we need a complex skill set to be able to handle problems, we’ve micro-detailed our physicians into looking at the left kidney," Dr. Epperly said.
Some 62 million Americans, or 20% of the nation’s population, live in a rural area, said Amy Elizondo, vice president of program services at the National Rural Health Association. Only 9% of the nation’s physicians practice in rural areas, and 77% of the 2,050 rural counties in America are designated as Health Professional Shortage Areas by the Health Resources and Services Administration (HRSA). A shortage area is one in which there is one or fewer primary care physicians per 3,500 people, according to HRSA. The agency estimates that, as of Nov. 14, there were 5,800 total primary care shortage areas in the United States, which can be located in urban or rural areas. It would take an additional 7,500 primary care physicians to end the shortages in all of those areas, said HRSA.
Physician organizations and HRSA, among others, have been trying to figure out how to draw more primary care doctors to those areas. The Affordable Care Act established a grant program for states looking to study their workforce issues, but so far HRSA has not been given any money by Congress to fund any grants. When the State Health Workforce Development Grants were announced in 2010, the Department of Health and Human Services said that almost $6 million would be made available to 26 states.
The ACA also established a National Health Care Workforce Commission, but that, too, has never been funded, although members were appointed in 2010 by the head of the Government Accountability Office. The GAO was given the authority under the health law to appoint the commission’s members.
"Right now we don’t have a unified policy or approach to addressing our workforce," said Dr. Stan Kozakowski, director of medical education at the American Academy of Family Physicians.
Dr. Kozakowski said that another way to boost the numbers of rural physicians was to increase training slots devoted to family medicine and, more specifically, residents trained in delivering medicine in rural areas.
A number of family medicine residency programs have developed a rural training track, which requires residents to spend 1 year in the larger academic medical center, followed by 2 years in the rural area, which may or may not have a hospital. Currently, there are 26 active rural training track programs. All are strapped for funding because fewer than half are eligible to receive traditional graduate medical education funding from the Centers for Medicare and Medicaid Services (CMS), said Dr. Randall Longenecker, professor of family medicine and assistant dean for rural and underserved programsat the Ohio University Heritage College of Osteopathic Medicine in Athens.
But the programs have proven to be effective, said Dr. Longenecker, who is also the executive director of the new nonprofit RTT Collaborative. He cited data showing that, 3 years after graduation, almost half of recent rural training track participants had continued to practice in rural areas and about a third were serving in professional shortage areas.
"The biggest challenge for retention is getting people to live in a rural place," said Dr. Longenecker, adding that, by living and training in the area for 2 years, physicians learn how to live there.
"The longer they stay, the longer they stay," agreed Dr. Epperly. He said that 85% of the physicians trained through the rural sites of the Family Medicine Residency of Idaho end up practicing in those areas. Another key is to help spouses become acclimated, which his program does through group outreach, Dr. Epperly said.
He noted that 35 of the nation’s 165 medical schools have started to look at training for rural areas in "a more serious way."
In addition, 13 states are contemplating developing rural track training, said Dr. Longenecker.
On Twitter @aliciaault
FROM AN AAFP BRIEFING
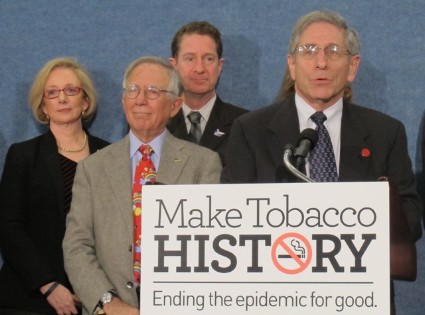
Pediatricians, cancer groups ask regulators to help cut tobacco use
WASHINGTON – A coalition of health groups including the American Academy of Pediatrics, the American Heart Association, and the American Cancer Society Cancer Action Network are urging regulators to help the nation achieve at least an 8% reduction in adult smoking rates by 2024.
Smoking kills 440,000 Americans a year and leads to $193 billion in health costs, according to the coalition, which also includes the American Lung Association, the Campaign for Tobacco-Free Kids, the Legacy Foundation, and Americans for Nonsmokers’ Rights. The groups noted that tobacco is the leading cause of preventable death in the United States.
Tobacco control is effective, Dr. Kenneth E. Warner, a distinguished university professor of public health at the University of Michigan, Ann Arbor, said at a briefing with reporters. He cited just-published data from a JAMA study he conducted with colleagues showing that control efforts had resulted in 8 million saved lives since 1964 and a 30% gain in life expectancy during the same time period (JAMA 2014;311:164-71).
The group said it wants regulators at all levels of government to help reduce smoking from about 18% of adults to less than 10% by 2024, protect all Americans from second-hand smoke within 5 years, and eventually eliminate death and disease caused by tobacco use.
The call to action was issued a week before the release of a new report from the U.S. Surgeon General’s Office on smoking and health that will tabulate the progress in the 50 years since the first Surgeon General’s report on smoking and also lay out the challenges still ahead.
"What has been accomplished in the last 50 years is nothing short of astounding," Matthew L. Myers, president of the Campaign for Tobacco-Free Kids, said in a briefing with reporters. He noted that the adult smoking rate has dropped by more than half, from 42% in 1964 to 18%. Among high school seniors, smoking rates have dropped from 36% in 1997 to 16%. Half of the U.S. population is protected from second-hand smoke by laws that bar smoking in public places.
But 44 million adults and almost 4 million children are still current smokers, and each day, 3,000 children start what usually becomes a lifetime habit. Mr. Myers called smoking a "pediatric epidemic."
Mr. Myers and other speakers decried what they said are continued efforts by tobacco makers to target children. Dr. James M. Perrin, president of the American Academy of Pediatrics, noted that although the Food and Drug Administration halted sales of candy-flavored cigarettes in 2010, other candy-like products have emerged, including dissolvables, cigars, and e-cigarettes that have flavors like cotton candy and grape.
"Strong tobacco regulation by the Food and Drug Administration is essential," said Dr. Perrin.
The coalition said that local, state, and federal governments could also help deter tobacco use by increasing excise taxes on tobacco products and raising the age of purchase. New York City and the big island of Hawaii both have banned sales to anyone under age 21 years. High school students may be friends with 18- and 19-year olds, but they aren’t as likely to have peers older than age 20, said Dr. Perrin. Raising the purchase age thus "limits the exposure of younger children ... to tobacco," he said.
E-cigarettes are also a growing concern, even though they are being pitched as a potential smoking cessation tool by their manufacturers, coalition members said. The products also are being marketed to children in a similar way that tobacco has been, said Mr. Myers. The coalition wants FDA regulation of those products "to ensure that the potential for their use to get people to quit is realized, but the danger of their becoming the next generation’s nicotine addiction is avoided," he said.
The Obama Administration may be poised to give the FDA more power to regulate e-cigarettes, said Paul Billings, senior vice president for advocacy at the Lung Association. "There are no e-cigarette products that have been demonstrated to be safe and effective to the Food and Drug Administration," said Mr. Billings.
The rules have been under review for more than 90 days, said Mr. Billings, adding "it’s time for action."
On Twitter @aliciaault
WASHINGTON – A coalition of health groups including the American Academy of Pediatrics, the American Heart Association, and the American Cancer Society Cancer Action Network are urging regulators to help the nation achieve at least an 8% reduction in adult smoking rates by 2024.
Smoking kills 440,000 Americans a year and leads to $193 billion in health costs, according to the coalition, which also includes the American Lung Association, the Campaign for Tobacco-Free Kids, the Legacy Foundation, and Americans for Nonsmokers’ Rights. The groups noted that tobacco is the leading cause of preventable death in the United States.
Tobacco control is effective, Dr. Kenneth E. Warner, a distinguished university professor of public health at the University of Michigan, Ann Arbor, said at a briefing with reporters. He cited just-published data from a JAMA study he conducted with colleagues showing that control efforts had resulted in 8 million saved lives since 1964 and a 30% gain in life expectancy during the same time period (JAMA 2014;311:164-71).
The group said it wants regulators at all levels of government to help reduce smoking from about 18% of adults to less than 10% by 2024, protect all Americans from second-hand smoke within 5 years, and eventually eliminate death and disease caused by tobacco use.
The call to action was issued a week before the release of a new report from the U.S. Surgeon General’s Office on smoking and health that will tabulate the progress in the 50 years since the first Surgeon General’s report on smoking and also lay out the challenges still ahead.
"What has been accomplished in the last 50 years is nothing short of astounding," Matthew L. Myers, president of the Campaign for Tobacco-Free Kids, said in a briefing with reporters. He noted that the adult smoking rate has dropped by more than half, from 42% in 1964 to 18%. Among high school seniors, smoking rates have dropped from 36% in 1997 to 16%. Half of the U.S. population is protected from second-hand smoke by laws that bar smoking in public places.
But 44 million adults and almost 4 million children are still current smokers, and each day, 3,000 children start what usually becomes a lifetime habit. Mr. Myers called smoking a "pediatric epidemic."
Mr. Myers and other speakers decried what they said are continued efforts by tobacco makers to target children. Dr. James M. Perrin, president of the American Academy of Pediatrics, noted that although the Food and Drug Administration halted sales of candy-flavored cigarettes in 2010, other candy-like products have emerged, including dissolvables, cigars, and e-cigarettes that have flavors like cotton candy and grape.
"Strong tobacco regulation by the Food and Drug Administration is essential," said Dr. Perrin.
The coalition said that local, state, and federal governments could also help deter tobacco use by increasing excise taxes on tobacco products and raising the age of purchase. New York City and the big island of Hawaii both have banned sales to anyone under age 21 years. High school students may be friends with 18- and 19-year olds, but they aren’t as likely to have peers older than age 20, said Dr. Perrin. Raising the purchase age thus "limits the exposure of younger children ... to tobacco," he said.
E-cigarettes are also a growing concern, even though they are being pitched as a potential smoking cessation tool by their manufacturers, coalition members said. The products also are being marketed to children in a similar way that tobacco has been, said Mr. Myers. The coalition wants FDA regulation of those products "to ensure that the potential for their use to get people to quit is realized, but the danger of their becoming the next generation’s nicotine addiction is avoided," he said.
The Obama Administration may be poised to give the FDA more power to regulate e-cigarettes, said Paul Billings, senior vice president for advocacy at the Lung Association. "There are no e-cigarette products that have been demonstrated to be safe and effective to the Food and Drug Administration," said Mr. Billings.
The rules have been under review for more than 90 days, said Mr. Billings, adding "it’s time for action."
On Twitter @aliciaault
WASHINGTON – A coalition of health groups including the American Academy of Pediatrics, the American Heart Association, and the American Cancer Society Cancer Action Network are urging regulators to help the nation achieve at least an 8% reduction in adult smoking rates by 2024.
Smoking kills 440,000 Americans a year and leads to $193 billion in health costs, according to the coalition, which also includes the American Lung Association, the Campaign for Tobacco-Free Kids, the Legacy Foundation, and Americans for Nonsmokers’ Rights. The groups noted that tobacco is the leading cause of preventable death in the United States.
Tobacco control is effective, Dr. Kenneth E. Warner, a distinguished university professor of public health at the University of Michigan, Ann Arbor, said at a briefing with reporters. He cited just-published data from a JAMA study he conducted with colleagues showing that control efforts had resulted in 8 million saved lives since 1964 and a 30% gain in life expectancy during the same time period (JAMA 2014;311:164-71).
The group said it wants regulators at all levels of government to help reduce smoking from about 18% of adults to less than 10% by 2024, protect all Americans from second-hand smoke within 5 years, and eventually eliminate death and disease caused by tobacco use.
The call to action was issued a week before the release of a new report from the U.S. Surgeon General’s Office on smoking and health that will tabulate the progress in the 50 years since the first Surgeon General’s report on smoking and also lay out the challenges still ahead.
"What has been accomplished in the last 50 years is nothing short of astounding," Matthew L. Myers, president of the Campaign for Tobacco-Free Kids, said in a briefing with reporters. He noted that the adult smoking rate has dropped by more than half, from 42% in 1964 to 18%. Among high school seniors, smoking rates have dropped from 36% in 1997 to 16%. Half of the U.S. population is protected from second-hand smoke by laws that bar smoking in public places.
But 44 million adults and almost 4 million children are still current smokers, and each day, 3,000 children start what usually becomes a lifetime habit. Mr. Myers called smoking a "pediatric epidemic."
Mr. Myers and other speakers decried what they said are continued efforts by tobacco makers to target children. Dr. James M. Perrin, president of the American Academy of Pediatrics, noted that although the Food and Drug Administration halted sales of candy-flavored cigarettes in 2010, other candy-like products have emerged, including dissolvables, cigars, and e-cigarettes that have flavors like cotton candy and grape.
"Strong tobacco regulation by the Food and Drug Administration is essential," said Dr. Perrin.
The coalition said that local, state, and federal governments could also help deter tobacco use by increasing excise taxes on tobacco products and raising the age of purchase. New York City and the big island of Hawaii both have banned sales to anyone under age 21 years. High school students may be friends with 18- and 19-year olds, but they aren’t as likely to have peers older than age 20, said Dr. Perrin. Raising the purchase age thus "limits the exposure of younger children ... to tobacco," he said.
E-cigarettes are also a growing concern, even though they are being pitched as a potential smoking cessation tool by their manufacturers, coalition members said. The products also are being marketed to children in a similar way that tobacco has been, said Mr. Myers. The coalition wants FDA regulation of those products "to ensure that the potential for their use to get people to quit is realized, but the danger of their becoming the next generation’s nicotine addiction is avoided," he said.
The Obama Administration may be poised to give the FDA more power to regulate e-cigarettes, said Paul Billings, senior vice president for advocacy at the Lung Association. "There are no e-cigarette products that have been demonstrated to be safe and effective to the Food and Drug Administration," said Mr. Billings.
The rules have been under review for more than 90 days, said Mr. Billings, adding "it’s time for action."
On Twitter @aliciaault
AT A BRIEFING SPONSORED BY THE CAMPAIGN FOR TOBACCO-FREE KIDS
CMS: Spending on physician services grew faster in 2012
WASHINGTON - Spending for physician services grew half a percentage point more in 2012 than 2011, according to an annual analysis of health care spending from the National Health Expenditure Accounts Team at the Centers for Medicare and Medicaid Services.
The uptick in spending growth was partially attributable to more physician visits as American pocketbooks began to rebound from the recent recession, Anne B. Martin and her colleagues at the CMS Office of the Actuary said at a briefing Jan. 6.
The impact of the Affordable Care Act on spending growth remained negligible in 2012, as it was in the two prior years, according to their analysis, published simultaneously in the journal Health Affairs (2014;33:67-77 [doi 10/1377/hlthaff.2013.1254]).
The CMS actuaries estimated that, overall, the law increased spending by 0.1% from 2010 to 2012. A few ACA provisions – such as coverage for dependents under age 26 and for patients with pre-existing conditions – increased spending, while others – such as payment cuts to hospitals and rebates for drugs under Medicaid – decreased spending.
Overall, the nation’s health spending – $2.8 *trillion in 2012, the most recent year for which there are accurate and complete data – grew 3.7% in 2012, a historically low rate similar to that seen in the previous 3 years. The flat spending reflects trends seen over the years, in particular with the last three boom-and-bust cycles of the economy, said the CMS actuaries. That is, when the economy does well, health spending rises. When there is a recession, health spending decreases; the rebound in spending often lags an economic recovery by several years, said Aaron Catlin, deputy director of the National Health Statistics Group in the Office of the Actuary.
Certain categories of spending did see growth increases or decreases in 2012 that were the result of one-time events, they said.
Spending on physician services by all payers grew by 4% to $452 billion in 2012. While still not approaching the 5.3% increase in 2008, it’s a rebound from just over 3% growth in 2009 and 2010. Physician services grew 3.5% in 2011 and the upward trend continued in 2012 "primarily because of an increase in visits to doctors’ offices as the economy continued to recover from the recent severe economic recession," Ms. Martin said.
Consumers are shouldering a growing share of their health costs, especially for physician services. Out-of-pocket spending on deductibles and copays grew by 3.8% in 2012. The amount Americans spent on health care, including premiums for private insurance and Medicare, and copays, deductibles, and other uncovered costs, grew 4.3% in 2012, compared to 3.1% in 2011.
Medicare, on the other hand, clamped down on physician pay rates and the volume of care it paid for, even as enrollment grew 4.1% in 2012 – the largest 1-year increase in enrollment in 39 years.
That enrollment growth helped drive an uptick in overall spending on hospital services, which is the largest category of national health expenditures, eating up 32% of the total pie. Hospital spending increased 4.9% in 2012 to $882 billion.
Medicaid spending in 2012 continued a pattern of historically low growth, in part because of slower enrollment as the economy rebounded and also as states continued efforts to rein in the program’s costs. Overall, the Medicaid tab was $421 billion in 2012.
Finally, growth in prescription drug spending slowed precipitously for all Americans – from 2.5% in 2011 to 0.4% in 2012 – even as the number of dispensed prescriptions grew by 1.4%, compared to only a 0.5% increase in 2011. The actuaries noted that this slowing was due in large part to the expanded use of generic drugs. Three top sellers went off patent in late 2011 and 2012: atorvastatin (Lipitor), clopidogrel (Plavix), and montelukast (Singulair). Generic drugs accounted for 77% of all dispensed prescriptions in 2012.
The authors disclosed no relevant conflicts of interest and noted that opinions expressed are their own and not necessarily those of the CMS.
On Twitter @aliciaault
*CORRECTION 1/13/14: A previous version of this article incorrectly reported the cost of the nation's overall health spending. This article has been updated.
WASHINGTON - Spending for physician services grew half a percentage point more in 2012 than 2011, according to an annual analysis of health care spending from the National Health Expenditure Accounts Team at the Centers for Medicare and Medicaid Services.
The uptick in spending growth was partially attributable to more physician visits as American pocketbooks began to rebound from the recent recession, Anne B. Martin and her colleagues at the CMS Office of the Actuary said at a briefing Jan. 6.
The impact of the Affordable Care Act on spending growth remained negligible in 2012, as it was in the two prior years, according to their analysis, published simultaneously in the journal Health Affairs (2014;33:67-77 [doi 10/1377/hlthaff.2013.1254]).
The CMS actuaries estimated that, overall, the law increased spending by 0.1% from 2010 to 2012. A few ACA provisions – such as coverage for dependents under age 26 and for patients with pre-existing conditions – increased spending, while others – such as payment cuts to hospitals and rebates for drugs under Medicaid – decreased spending.
Overall, the nation’s health spending – $2.8 *trillion in 2012, the most recent year for which there are accurate and complete data – grew 3.7% in 2012, a historically low rate similar to that seen in the previous 3 years. The flat spending reflects trends seen over the years, in particular with the last three boom-and-bust cycles of the economy, said the CMS actuaries. That is, when the economy does well, health spending rises. When there is a recession, health spending decreases; the rebound in spending often lags an economic recovery by several years, said Aaron Catlin, deputy director of the National Health Statistics Group in the Office of the Actuary.
Certain categories of spending did see growth increases or decreases in 2012 that were the result of one-time events, they said.
Spending on physician services by all payers grew by 4% to $452 billion in 2012. While still not approaching the 5.3% increase in 2008, it’s a rebound from just over 3% growth in 2009 and 2010. Physician services grew 3.5% in 2011 and the upward trend continued in 2012 "primarily because of an increase in visits to doctors’ offices as the economy continued to recover from the recent severe economic recession," Ms. Martin said.
Consumers are shouldering a growing share of their health costs, especially for physician services. Out-of-pocket spending on deductibles and copays grew by 3.8% in 2012. The amount Americans spent on health care, including premiums for private insurance and Medicare, and copays, deductibles, and other uncovered costs, grew 4.3% in 2012, compared to 3.1% in 2011.
Medicare, on the other hand, clamped down on physician pay rates and the volume of care it paid for, even as enrollment grew 4.1% in 2012 – the largest 1-year increase in enrollment in 39 years.
That enrollment growth helped drive an uptick in overall spending on hospital services, which is the largest category of national health expenditures, eating up 32% of the total pie. Hospital spending increased 4.9% in 2012 to $882 billion.
Medicaid spending in 2012 continued a pattern of historically low growth, in part because of slower enrollment as the economy rebounded and also as states continued efforts to rein in the program’s costs. Overall, the Medicaid tab was $421 billion in 2012.
Finally, growth in prescription drug spending slowed precipitously for all Americans – from 2.5% in 2011 to 0.4% in 2012 – even as the number of dispensed prescriptions grew by 1.4%, compared to only a 0.5% increase in 2011. The actuaries noted that this slowing was due in large part to the expanded use of generic drugs. Three top sellers went off patent in late 2011 and 2012: atorvastatin (Lipitor), clopidogrel (Plavix), and montelukast (Singulair). Generic drugs accounted for 77% of all dispensed prescriptions in 2012.
The authors disclosed no relevant conflicts of interest and noted that opinions expressed are their own and not necessarily those of the CMS.
On Twitter @aliciaault
*CORRECTION 1/13/14: A previous version of this article incorrectly reported the cost of the nation's overall health spending. This article has been updated.
WASHINGTON - Spending for physician services grew half a percentage point more in 2012 than 2011, according to an annual analysis of health care spending from the National Health Expenditure Accounts Team at the Centers for Medicare and Medicaid Services.
The uptick in spending growth was partially attributable to more physician visits as American pocketbooks began to rebound from the recent recession, Anne B. Martin and her colleagues at the CMS Office of the Actuary said at a briefing Jan. 6.
The impact of the Affordable Care Act on spending growth remained negligible in 2012, as it was in the two prior years, according to their analysis, published simultaneously in the journal Health Affairs (2014;33:67-77 [doi 10/1377/hlthaff.2013.1254]).
The CMS actuaries estimated that, overall, the law increased spending by 0.1% from 2010 to 2012. A few ACA provisions – such as coverage for dependents under age 26 and for patients with pre-existing conditions – increased spending, while others – such as payment cuts to hospitals and rebates for drugs under Medicaid – decreased spending.
Overall, the nation’s health spending – $2.8 *trillion in 2012, the most recent year for which there are accurate and complete data – grew 3.7% in 2012, a historically low rate similar to that seen in the previous 3 years. The flat spending reflects trends seen over the years, in particular with the last three boom-and-bust cycles of the economy, said the CMS actuaries. That is, when the economy does well, health spending rises. When there is a recession, health spending decreases; the rebound in spending often lags an economic recovery by several years, said Aaron Catlin, deputy director of the National Health Statistics Group in the Office of the Actuary.
Certain categories of spending did see growth increases or decreases in 2012 that were the result of one-time events, they said.
Spending on physician services by all payers grew by 4% to $452 billion in 2012. While still not approaching the 5.3% increase in 2008, it’s a rebound from just over 3% growth in 2009 and 2010. Physician services grew 3.5% in 2011 and the upward trend continued in 2012 "primarily because of an increase in visits to doctors’ offices as the economy continued to recover from the recent severe economic recession," Ms. Martin said.
Consumers are shouldering a growing share of their health costs, especially for physician services. Out-of-pocket spending on deductibles and copays grew by 3.8% in 2012. The amount Americans spent on health care, including premiums for private insurance and Medicare, and copays, deductibles, and other uncovered costs, grew 4.3% in 2012, compared to 3.1% in 2011.
Medicare, on the other hand, clamped down on physician pay rates and the volume of care it paid for, even as enrollment grew 4.1% in 2012 – the largest 1-year increase in enrollment in 39 years.
That enrollment growth helped drive an uptick in overall spending on hospital services, which is the largest category of national health expenditures, eating up 32% of the total pie. Hospital spending increased 4.9% in 2012 to $882 billion.
Medicaid spending in 2012 continued a pattern of historically low growth, in part because of slower enrollment as the economy rebounded and also as states continued efforts to rein in the program’s costs. Overall, the Medicaid tab was $421 billion in 2012.
Finally, growth in prescription drug spending slowed precipitously for all Americans – from 2.5% in 2011 to 0.4% in 2012 – even as the number of dispensed prescriptions grew by 1.4%, compared to only a 0.5% increase in 2011. The actuaries noted that this slowing was due in large part to the expanded use of generic drugs. Three top sellers went off patent in late 2011 and 2012: atorvastatin (Lipitor), clopidogrel (Plavix), and montelukast (Singulair). Generic drugs accounted for 77% of all dispensed prescriptions in 2012.
The authors disclosed no relevant conflicts of interest and noted that opinions expressed are their own and not necessarily those of the CMS.
On Twitter @aliciaault
*CORRECTION 1/13/14: A previous version of this article incorrectly reported the cost of the nation's overall health spending. This article has been updated.
FROM A HEALTH AFFAIRS BRIEFING
Major finding: Growth in national health care spending for 2012 was 3.7%, a low, but slightly larger rate of growth than in 2011.
Data source: Several federal databases including those managed by the Centers for Medicare and Medicaid Services, the Department of Commerce, the Bureau of Economic Analysis, and the Census Bureau.
Disclosures: The authors disclosed no relevant conflicts of interest and noted that opinions expressed are their own and not necessarily those of the CMS.
President signs budget deal, short-term SGR fix
Physicians will get a 0.5% raise in Medicare pay on Jan. 1, thanks to a last-minute legislative fix to the Sustainable Growth Rate formula signed into law by President Obama on Dec. 26.
The Pathway for SGR Reform Act of 2013 was attached as an amendment to the Bipartisan Budget Agreement of 2013. The budget deal, brokered by Sen. Patty Murray (D-Wash.) and Rep. Paul Ryan (R-Wisc.), passed the House on Dec. 12 and the Senate on Dec. 18. The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. It would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
The law also extends the 2% sequestration cut to Medicare payments by 2 years, to 2023.
It encourages the Centers for Medicare and Medicaid Services to simplify physicians’ administrative burden by trying to more closely coordinate quality measure requirements and give doctors more timely feedback on those measures.
The law extends funding for a variety of other health-related federal programs for an additional 3 months, including for Area Agencies on Aging.
Congress is expected to start consideration again of a permanent replacement for the SGR when it returns on Jan. 6.
On Twitter @aliciaault
*Correction 2/05/14: The following passage was deleted from a previous version of this story as the provision was not included in the law as signed.
Finally, the law delays enforcement of the "two-midnight rule" until Oct. 2014. The goal of the two-midnight policy, which was included in the fiscal 2014 Inpatient Prospective Payment System final rule, is to cut down on hospitals using observation status to keep from admitting patients. Hospitals now have until Oct. 1, 2014 to adjust to the new policy, which requires patients to be admitted if physicians think they will need a stay longer than 48 hours.
Physicians will get a 0.5% raise in Medicare pay on Jan. 1, thanks to a last-minute legislative fix to the Sustainable Growth Rate formula signed into law by President Obama on Dec. 26.
The Pathway for SGR Reform Act of 2013 was attached as an amendment to the Bipartisan Budget Agreement of 2013. The budget deal, brokered by Sen. Patty Murray (D-Wash.) and Rep. Paul Ryan (R-Wisc.), passed the House on Dec. 12 and the Senate on Dec. 18. The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. It would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
The law also extends the 2% sequestration cut to Medicare payments by 2 years, to 2023.
It encourages the Centers for Medicare and Medicaid Services to simplify physicians’ administrative burden by trying to more closely coordinate quality measure requirements and give doctors more timely feedback on those measures.
The law extends funding for a variety of other health-related federal programs for an additional 3 months, including for Area Agencies on Aging.
Congress is expected to start consideration again of a permanent replacement for the SGR when it returns on Jan. 6.
On Twitter @aliciaault
*Correction 2/05/14: The following passage was deleted from a previous version of this story as the provision was not included in the law as signed.
Finally, the law delays enforcement of the "two-midnight rule" until Oct. 2014. The goal of the two-midnight policy, which was included in the fiscal 2014 Inpatient Prospective Payment System final rule, is to cut down on hospitals using observation status to keep from admitting patients. Hospitals now have until Oct. 1, 2014 to adjust to the new policy, which requires patients to be admitted if physicians think they will need a stay longer than 48 hours.
Physicians will get a 0.5% raise in Medicare pay on Jan. 1, thanks to a last-minute legislative fix to the Sustainable Growth Rate formula signed into law by President Obama on Dec. 26.
The Pathway for SGR Reform Act of 2013 was attached as an amendment to the Bipartisan Budget Agreement of 2013. The budget deal, brokered by Sen. Patty Murray (D-Wash.) and Rep. Paul Ryan (R-Wisc.), passed the House on Dec. 12 and the Senate on Dec. 18. The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. It would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
The law also extends the 2% sequestration cut to Medicare payments by 2 years, to 2023.
It encourages the Centers for Medicare and Medicaid Services to simplify physicians’ administrative burden by trying to more closely coordinate quality measure requirements and give doctors more timely feedback on those measures.
The law extends funding for a variety of other health-related federal programs for an additional 3 months, including for Area Agencies on Aging.
Congress is expected to start consideration again of a permanent replacement for the SGR when it returns on Jan. 6.
On Twitter @aliciaault
*Correction 2/05/14: The following passage was deleted from a previous version of this story as the provision was not included in the law as signed.
Finally, the law delays enforcement of the "two-midnight rule" until Oct. 2014. The goal of the two-midnight policy, which was included in the fiscal 2014 Inpatient Prospective Payment System final rule, is to cut down on hospitals using observation status to keep from admitting patients. Hospitals now have until Oct. 1, 2014 to adjust to the new policy, which requires patients to be admitted if physicians think they will need a stay longer than 48 hours.
Senate passes SGR and budget bill; White House next
The Senate has passed a budget package that includes a 3-month delay in physician pay cuts mandated by the Medicare Sustainable Growth Rate formula but also extends other overall Medicare budget cuts for 2 years.
The Senate voted 64-36 on Dec. 18 to approve the Bipartisan Budget Act of 2013 crafted by Senate Budget Committee Chairman Patty Murray (D-Wash.) and House Budget Committee Chairman Paul Ryan (R-Wisc.). Nine Republican senators voted in favor of the deal, joining 55 Democrats.
The 3-month reprieve from the SGR cuts was added to the budget deal by the House before it voted to approve the package on Dec. 12.
Now, if President Obama signs the budget bill, which is expected, physicians will see 0.5% a month pay increase through Mar. 31.
The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. It would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
The bill also would extend the 2% sequestration cut to Medicare payments by 2 years, to 2023.
The House has recessed and is not due back until Jan. 7. The Senate has not set its adjournment date yet, but is expected to reconvene on Jan. 6.
Congress is expected to start consideration again of a permanent replacement for the SGR when it returns.
On Twitter @aliciaault
The Senate has passed a budget package that includes a 3-month delay in physician pay cuts mandated by the Medicare Sustainable Growth Rate formula but also extends other overall Medicare budget cuts for 2 years.
The Senate voted 64-36 on Dec. 18 to approve the Bipartisan Budget Act of 2013 crafted by Senate Budget Committee Chairman Patty Murray (D-Wash.) and House Budget Committee Chairman Paul Ryan (R-Wisc.). Nine Republican senators voted in favor of the deal, joining 55 Democrats.
The 3-month reprieve from the SGR cuts was added to the budget deal by the House before it voted to approve the package on Dec. 12.
Now, if President Obama signs the budget bill, which is expected, physicians will see 0.5% a month pay increase through Mar. 31.
The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. It would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
The bill also would extend the 2% sequestration cut to Medicare payments by 2 years, to 2023.
The House has recessed and is not due back until Jan. 7. The Senate has not set its adjournment date yet, but is expected to reconvene on Jan. 6.
Congress is expected to start consideration again of a permanent replacement for the SGR when it returns.
On Twitter @aliciaault
The Senate has passed a budget package that includes a 3-month delay in physician pay cuts mandated by the Medicare Sustainable Growth Rate formula but also extends other overall Medicare budget cuts for 2 years.
The Senate voted 64-36 on Dec. 18 to approve the Bipartisan Budget Act of 2013 crafted by Senate Budget Committee Chairman Patty Murray (D-Wash.) and House Budget Committee Chairman Paul Ryan (R-Wisc.). Nine Republican senators voted in favor of the deal, joining 55 Democrats.
The 3-month reprieve from the SGR cuts was added to the budget deal by the House before it voted to approve the package on Dec. 12.
Now, if President Obama signs the budget bill, which is expected, physicians will see 0.5% a month pay increase through Mar. 31.
The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. It would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
The bill also would extend the 2% sequestration cut to Medicare payments by 2 years, to 2023.
The House has recessed and is not due back until Jan. 7. The Senate has not set its adjournment date yet, but is expected to reconvene on Jan. 6.
Congress is expected to start consideration again of a permanent replacement for the SGR when it returns.
On Twitter @aliciaault
Senate passes SGR and budget bill; White House next
The Senate has passed a budget package that includes a 3-month delay in physician pay cuts mandated by the Medicare Sustainable Growth Rate formula but also extends other overall Medicare budget cuts for 2 years.
The Senate voted 64-36 on Dec. 18 to approve the Bipartisan Budget Act of 2013 crafted by Senate Budget Committee Chairman Patty Murray (D-Wash.) and House Budget Committee Chairman Paul Ryan (R-Wisc.). Nine Republican senators voted in favor of the deal, joining 55 Democrats.
The 3-month reprieve from the SGR cuts was added to the budget deal by the House before it voted to approve the package on Dec. 12.
Now, if President Obama signs the budget bill, which is expected, physicians will see 0.5% a month pay increase through Mar. 31.
The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. It would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
The bill also would extend the 2% sequestration cut to Medicare payments by 2 years, to 2023.
The House has recessed and is not due back until Jan. 7. The Senate has not set its adjournment date yet, but is expected to reconvene on Jan. 6.
Congress is expected to start consideration again of a permanent replacement for the SGR when it returns.
On Twitter @aliciaault
The Senate has passed a budget package that includes a 3-month delay in physician pay cuts mandated by the Medicare Sustainable Growth Rate formula but also extends other overall Medicare budget cuts for 2 years.
The Senate voted 64-36 on Dec. 18 to approve the Bipartisan Budget Act of 2013 crafted by Senate Budget Committee Chairman Patty Murray (D-Wash.) and House Budget Committee Chairman Paul Ryan (R-Wisc.). Nine Republican senators voted in favor of the deal, joining 55 Democrats.
The 3-month reprieve from the SGR cuts was added to the budget deal by the House before it voted to approve the package on Dec. 12.
Now, if President Obama signs the budget bill, which is expected, physicians will see 0.5% a month pay increase through Mar. 31.
The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. It would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
The bill also would extend the 2% sequestration cut to Medicare payments by 2 years, to 2023.
The House has recessed and is not due back until Jan. 7. The Senate has not set its adjournment date yet, but is expected to reconvene on Jan. 6.
Congress is expected to start consideration again of a permanent replacement for the SGR when it returns.
On Twitter @aliciaault
The Senate has passed a budget package that includes a 3-month delay in physician pay cuts mandated by the Medicare Sustainable Growth Rate formula but also extends other overall Medicare budget cuts for 2 years.
The Senate voted 64-36 on Dec. 18 to approve the Bipartisan Budget Act of 2013 crafted by Senate Budget Committee Chairman Patty Murray (D-Wash.) and House Budget Committee Chairman Paul Ryan (R-Wisc.). Nine Republican senators voted in favor of the deal, joining 55 Democrats.
The 3-month reprieve from the SGR cuts was added to the budget deal by the House before it voted to approve the package on Dec. 12.
Now, if President Obama signs the budget bill, which is expected, physicians will see 0.5% a month pay increase through Mar. 31.
The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. It would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
The bill also would extend the 2% sequestration cut to Medicare payments by 2 years, to 2023.
The House has recessed and is not due back until Jan. 7. The Senate has not set its adjournment date yet, but is expected to reconvene on Jan. 6.
Congress is expected to start consideration again of a permanent replacement for the SGR when it returns.
On Twitter @aliciaault