User login
SGR replacement promises small pay boost over 5 years
Doctors could see a 0.5% pay increase for 5 years and a transition to alternative delivery and payment models under consensus legislation to repeal the Medicare Sustainable Growth Rate formula.
The legislation, the SGR Repeal and Medicare Provider Payment Modernization Act of 2014 (H.R. 4015), is based on three separate proposals approved last year by the House Energy and Commerce Committee, the House Ways and Means Committee, and the Senate Finance Committee. It was introduced Feb. 6.
The bill does not address how to pay for the SGR replacement. One recent estimate by the Congressional Budget Office put that price tag at $120 billion to $150 billion.
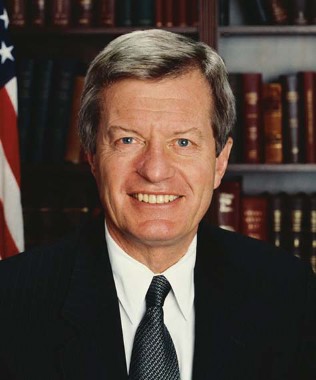
Sen. Max Baucus (D-Mont.), chairman of the Finance committee, hailed the agreement. "This proposal would bring that cycle to an end and fix the broken system," he said in a statement. "Our bill makes Medicare’s physician payments more modern and efficient, and it will protect seniors’ access to their doctors."
American Medical Association President Ardis Dee Hoven commented that this consensus bill means that "Congress is closer than it has ever been to enacting fiscally-prudent legislation that would repeal Medicare’s fatally flawed sustainable growth rate formula."
Dr. Charles Cutler, chair of the American College of Physicians’ Board of Regents, said in a statement that the ACP was encouraged that the bill contained many of the elements it had backed, including:
• Replacing the SGR with a system focused on quality, value, and accountability.
• Consolidating the three existing quality programs into a streamlined and improved program that rewards physicians who meet performance thresholds and improve care for seniors.
• Implementing a process to improve payment accuracy.
• Creating incentives for physicians to move into advanced payment models.
Dr. Reid Blackwelder, president of the American Academy of Family Physicians said, "For more than a decade, the SGR has threatened our most vulnerable patients’ access to care by requiring drastic cuts in payment for medical services. By ending the annual, biannual, monthly, sometimes even bimonthly cycle of last-minute ‘fixes’ to prevent mandated SGR cuts, Congress will stabilize Medicare and bring peace of mind to their elderly and disabled constituents."
"Much work remains to create a system that can finally provide certainty to seniors and their doctors," Rep. Fred Upton (R-Mich.), chairman of the Energy and Commerce committee, said in a statement. "I look forward to building upon this progress and continuing the momentum until this is across the finish line."
The most recent cuts called for by the SGR were deferred as part of federal budget legislation enacted at the end of 2013. A short-term 0.5% increase in Medicare physician fees is slated to expire March 31.
On Twitter @aliciaault
Doctors could see a 0.5% pay increase for 5 years and a transition to alternative delivery and payment models under consensus legislation to repeal the Medicare Sustainable Growth Rate formula.
The legislation, the SGR Repeal and Medicare Provider Payment Modernization Act of 2014 (H.R. 4015), is based on three separate proposals approved last year by the House Energy and Commerce Committee, the House Ways and Means Committee, and the Senate Finance Committee. It was introduced Feb. 6.
The bill does not address how to pay for the SGR replacement. One recent estimate by the Congressional Budget Office put that price tag at $120 billion to $150 billion.
Sen. Max Baucus (D-Mont.), chairman of the Finance committee, hailed the agreement. "This proposal would bring that cycle to an end and fix the broken system," he said in a statement. "Our bill makes Medicare’s physician payments more modern and efficient, and it will protect seniors’ access to their doctors."
American Medical Association President Ardis Dee Hoven commented that this consensus bill means that "Congress is closer than it has ever been to enacting fiscally-prudent legislation that would repeal Medicare’s fatally flawed sustainable growth rate formula."
Dr. Charles Cutler, chair of the American College of Physicians’ Board of Regents, said in a statement that the ACP was encouraged that the bill contained many of the elements it had backed, including:
• Replacing the SGR with a system focused on quality, value, and accountability.
• Consolidating the three existing quality programs into a streamlined and improved program that rewards physicians who meet performance thresholds and improve care for seniors.
• Implementing a process to improve payment accuracy.
• Creating incentives for physicians to move into advanced payment models.
Dr. Reid Blackwelder, president of the American Academy of Family Physicians said, "For more than a decade, the SGR has threatened our most vulnerable patients’ access to care by requiring drastic cuts in payment for medical services. By ending the annual, biannual, monthly, sometimes even bimonthly cycle of last-minute ‘fixes’ to prevent mandated SGR cuts, Congress will stabilize Medicare and bring peace of mind to their elderly and disabled constituents."
"Much work remains to create a system that can finally provide certainty to seniors and their doctors," Rep. Fred Upton (R-Mich.), chairman of the Energy and Commerce committee, said in a statement. "I look forward to building upon this progress and continuing the momentum until this is across the finish line."
The most recent cuts called for by the SGR were deferred as part of federal budget legislation enacted at the end of 2013. A short-term 0.5% increase in Medicare physician fees is slated to expire March 31.
On Twitter @aliciaault
Doctors could see a 0.5% pay increase for 5 years and a transition to alternative delivery and payment models under consensus legislation to repeal the Medicare Sustainable Growth Rate formula.
The legislation, the SGR Repeal and Medicare Provider Payment Modernization Act of 2014 (H.R. 4015), is based on three separate proposals approved last year by the House Energy and Commerce Committee, the House Ways and Means Committee, and the Senate Finance Committee. It was introduced Feb. 6.
The bill does not address how to pay for the SGR replacement. One recent estimate by the Congressional Budget Office put that price tag at $120 billion to $150 billion.
Sen. Max Baucus (D-Mont.), chairman of the Finance committee, hailed the agreement. "This proposal would bring that cycle to an end and fix the broken system," he said in a statement. "Our bill makes Medicare’s physician payments more modern and efficient, and it will protect seniors’ access to their doctors."
American Medical Association President Ardis Dee Hoven commented that this consensus bill means that "Congress is closer than it has ever been to enacting fiscally-prudent legislation that would repeal Medicare’s fatally flawed sustainable growth rate formula."
Dr. Charles Cutler, chair of the American College of Physicians’ Board of Regents, said in a statement that the ACP was encouraged that the bill contained many of the elements it had backed, including:
• Replacing the SGR with a system focused on quality, value, and accountability.
• Consolidating the three existing quality programs into a streamlined and improved program that rewards physicians who meet performance thresholds and improve care for seniors.
• Implementing a process to improve payment accuracy.
• Creating incentives for physicians to move into advanced payment models.
Dr. Reid Blackwelder, president of the American Academy of Family Physicians said, "For more than a decade, the SGR has threatened our most vulnerable patients’ access to care by requiring drastic cuts in payment for medical services. By ending the annual, biannual, monthly, sometimes even bimonthly cycle of last-minute ‘fixes’ to prevent mandated SGR cuts, Congress will stabilize Medicare and bring peace of mind to their elderly and disabled constituents."
"Much work remains to create a system that can finally provide certainty to seniors and their doctors," Rep. Fred Upton (R-Mich.), chairman of the Energy and Commerce committee, said in a statement. "I look forward to building upon this progress and continuing the momentum until this is across the finish line."
The most recent cuts called for by the SGR were deferred as part of federal budget legislation enacted at the end of 2013. A short-term 0.5% increase in Medicare physician fees is slated to expire March 31.
On Twitter @aliciaault
DeSalvo: Interoperability is the IT focus now
WASHINGTON – Dr. Karen B. DeSalvo feels your pain.
As the government’s National Coordinator for Health Technology, Dr. DeSalvo says that she wants to redouble efforts to help all physicians adopt electronic health records (EHRs).
"We really want to help," Dr. DeSalvo said at a Feb. 5 forum on telemedicine sponsored by the journal Health Affairs. "We want to bring folks along," and ensure there is not a digital divide.
But her primary focus is interoperability.
Achieving interoperability "is going to be a complex and exciting endeavor," that will be not only about the basics of making it work, but also pulling all the stakeholders together to brainstorm creative solutions, Dr. DeSalvo said Feb. 6. at a health IT conference, sponsored by West Health Institute and the Office of the National Coordinator.
Dr. DeSalvo has experience in creating interoperable systems. After Hurricane Katrina, Dr. DeSalvo, then chief of general internal medicine and geriatrics at Tulane University and special assistant to its president for health policy, helped resurrect New Orleans’s health care system.
Paper records were lost or destroyed. Many patients were displaced and had patchy recollections of their medical histories. Health care professionals too were displaced; those that remained decided to "take this tipping point and move forward," she said. That meant building a new infrastructure – one that would be portable and easily accessible to providers and patients.
Health IT played a huge role in helping the city regain its medical bearings. "We skipped right to ... electronic health records and how we could use telehealth," Dr. DeSalvo said. Use of EHRs allowed physicians to quickly transition their practices into patient-centered medical homes and also meant that patients would be treated holistically, she said. Interoperability was key.
Although America "is not facing the urgency of a catastrophe like Katrina," she said, "it is at a slow boil," with costs continuing to rise and ongoing challenges with access to care and quality improvement.
On Twitter @aliciaault
WASHINGTON – Dr. Karen B. DeSalvo feels your pain.
As the government’s National Coordinator for Health Technology, Dr. DeSalvo says that she wants to redouble efforts to help all physicians adopt electronic health records (EHRs).
"We really want to help," Dr. DeSalvo said at a Feb. 5 forum on telemedicine sponsored by the journal Health Affairs. "We want to bring folks along," and ensure there is not a digital divide.
But her primary focus is interoperability.
Achieving interoperability "is going to be a complex and exciting endeavor," that will be not only about the basics of making it work, but also pulling all the stakeholders together to brainstorm creative solutions, Dr. DeSalvo said Feb. 6. at a health IT conference, sponsored by West Health Institute and the Office of the National Coordinator.
Dr. DeSalvo has experience in creating interoperable systems. After Hurricane Katrina, Dr. DeSalvo, then chief of general internal medicine and geriatrics at Tulane University and special assistant to its president for health policy, helped resurrect New Orleans’s health care system.
Paper records were lost or destroyed. Many patients were displaced and had patchy recollections of their medical histories. Health care professionals too were displaced; those that remained decided to "take this tipping point and move forward," she said. That meant building a new infrastructure – one that would be portable and easily accessible to providers and patients.
Health IT played a huge role in helping the city regain its medical bearings. "We skipped right to ... electronic health records and how we could use telehealth," Dr. DeSalvo said. Use of EHRs allowed physicians to quickly transition their practices into patient-centered medical homes and also meant that patients would be treated holistically, she said. Interoperability was key.
Although America "is not facing the urgency of a catastrophe like Katrina," she said, "it is at a slow boil," with costs continuing to rise and ongoing challenges with access to care and quality improvement.
On Twitter @aliciaault
WASHINGTON – Dr. Karen B. DeSalvo feels your pain.
As the government’s National Coordinator for Health Technology, Dr. DeSalvo says that she wants to redouble efforts to help all physicians adopt electronic health records (EHRs).
"We really want to help," Dr. DeSalvo said at a Feb. 5 forum on telemedicine sponsored by the journal Health Affairs. "We want to bring folks along," and ensure there is not a digital divide.
But her primary focus is interoperability.
Achieving interoperability "is going to be a complex and exciting endeavor," that will be not only about the basics of making it work, but also pulling all the stakeholders together to brainstorm creative solutions, Dr. DeSalvo said Feb. 6. at a health IT conference, sponsored by West Health Institute and the Office of the National Coordinator.
Dr. DeSalvo has experience in creating interoperable systems. After Hurricane Katrina, Dr. DeSalvo, then chief of general internal medicine and geriatrics at Tulane University and special assistant to its president for health policy, helped resurrect New Orleans’s health care system.
Paper records were lost or destroyed. Many patients were displaced and had patchy recollections of their medical histories. Health care professionals too were displaced; those that remained decided to "take this tipping point and move forward," she said. That meant building a new infrastructure – one that would be portable and easily accessible to providers and patients.
Health IT played a huge role in helping the city regain its medical bearings. "We skipped right to ... electronic health records and how we could use telehealth," Dr. DeSalvo said. Use of EHRs allowed physicians to quickly transition their practices into patient-centered medical homes and also meant that patients would be treated holistically, she said. Interoperability was key.
Although America "is not facing the urgency of a catastrophe like Katrina," she said, "it is at a slow boil," with costs continuing to rise and ongoing challenges with access to care and quality improvement.
On Twitter @aliciaault
HHS rule lets patients get results directly from labs
Very soon, patients across the country will be allowed to call the lab and get their test results, without having to interact with a physician or health care professional.
A final rule issued Feb. 3 by the U.S. Department of Health & Human Services eliminates exceptions under the Health Insurance Portability and Accountability Act (HIPAA) and the Clinical Laboratory Improvement Amendments (CLIA) that allowed labs to withhold information from patients and their personal representatives.
"Information like lab results can empower patients to track their health progress, make decisions with their health care professionals, and adhere to important treatment plans," HHS Secretary Kathleen Sebelius said in a statement.
The rule supersedes state laws that prohibit patients from getting results directly from a lab. Currently, 13 states require labs to give results only to health care providers. Seven states, Puerto Rico, and the District of Columbia allow results to be given to patients, and seven allow this with the provider’s approval. The remainder have no laws governing the communication of test results.
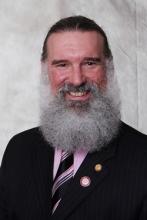
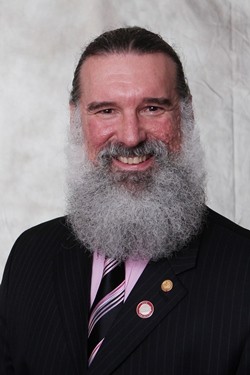
Patients can still get their test results from their physicians – and that’s a situation many physicians prefer, Dr. Reid Blackwelder, president of the American Academy of Family Physicians, said in an interview.
"Patients have a right to [access] their records and notes," Dr. Blackwelder said. But since physicians treat patients, not numbers, there’s a need to explain why tests are being done, and to put the results into context, he said. "If you just have numbers out there without that context, it can create anxiety."
The HHS originally proposed the change in 2011. At the time, the American Medical Association, the American College of Physicians, and the American Academy of Pediatrics submitted comments to the agency asking that lab results given out directly should also tell patients to consult the ordering physicians for interpretation.
The final rule notes that labs will not be required to interpret the results and that they are given 30 days to respond to an individual’s request. With that time frame, physicians might get the results before patients do, and could provide context, according to the rule.
The rule goes into effect April 4.
On Twitter @aliciaault
Very soon, patients across the country will be allowed to call the lab and get their test results, without having to interact with a physician or health care professional.
A final rule issued Feb. 3 by the U.S. Department of Health & Human Services eliminates exceptions under the Health Insurance Portability and Accountability Act (HIPAA) and the Clinical Laboratory Improvement Amendments (CLIA) that allowed labs to withhold information from patients and their personal representatives.
"Information like lab results can empower patients to track their health progress, make decisions with their health care professionals, and adhere to important treatment plans," HHS Secretary Kathleen Sebelius said in a statement.
The rule supersedes state laws that prohibit patients from getting results directly from a lab. Currently, 13 states require labs to give results only to health care providers. Seven states, Puerto Rico, and the District of Columbia allow results to be given to patients, and seven allow this with the provider’s approval. The remainder have no laws governing the communication of test results.
Patients can still get their test results from their physicians – and that’s a situation many physicians prefer, Dr. Reid Blackwelder, president of the American Academy of Family Physicians, said in an interview.
"Patients have a right to [access] their records and notes," Dr. Blackwelder said. But since physicians treat patients, not numbers, there’s a need to explain why tests are being done, and to put the results into context, he said. "If you just have numbers out there without that context, it can create anxiety."
The HHS originally proposed the change in 2011. At the time, the American Medical Association, the American College of Physicians, and the American Academy of Pediatrics submitted comments to the agency asking that lab results given out directly should also tell patients to consult the ordering physicians for interpretation.
The final rule notes that labs will not be required to interpret the results and that they are given 30 days to respond to an individual’s request. With that time frame, physicians might get the results before patients do, and could provide context, according to the rule.
The rule goes into effect April 4.
On Twitter @aliciaault
Very soon, patients across the country will be allowed to call the lab and get their test results, without having to interact with a physician or health care professional.
A final rule issued Feb. 3 by the U.S. Department of Health & Human Services eliminates exceptions under the Health Insurance Portability and Accountability Act (HIPAA) and the Clinical Laboratory Improvement Amendments (CLIA) that allowed labs to withhold information from patients and their personal representatives.
"Information like lab results can empower patients to track their health progress, make decisions with their health care professionals, and adhere to important treatment plans," HHS Secretary Kathleen Sebelius said in a statement.
The rule supersedes state laws that prohibit patients from getting results directly from a lab. Currently, 13 states require labs to give results only to health care providers. Seven states, Puerto Rico, and the District of Columbia allow results to be given to patients, and seven allow this with the provider’s approval. The remainder have no laws governing the communication of test results.
Patients can still get their test results from their physicians – and that’s a situation many physicians prefer, Dr. Reid Blackwelder, president of the American Academy of Family Physicians, said in an interview.
"Patients have a right to [access] their records and notes," Dr. Blackwelder said. But since physicians treat patients, not numbers, there’s a need to explain why tests are being done, and to put the results into context, he said. "If you just have numbers out there without that context, it can create anxiety."
The HHS originally proposed the change in 2011. At the time, the American Medical Association, the American College of Physicians, and the American Academy of Pediatrics submitted comments to the agency asking that lab results given out directly should also tell patients to consult the ordering physicians for interpretation.
The final rule notes that labs will not be required to interpret the results and that they are given 30 days to respond to an individual’s request. With that time frame, physicians might get the results before patients do, and could provide context, according to the rule.
The rule goes into effect April 4.
On Twitter @aliciaault
Initial results indicate ACOs a measured success for Medicare
Fewer hospital readmissions, high-cost imaging studies, and emergency department visits helped 29 of 114 accountable care organizations earn $126 million in shared Medicare savings in 2012, the Centers for Medicare & Medicaid Services announced.
CMS issued interim financial results for the first year that ACOs participated in the Medicare Shared Savings Program. Under the program, ACOs that reduce costs while providing high-quality care can share in the savings to Medicare. They must report on 33 quality measures relating to care coordination and patient safety, use of appropriate preventive health services, improved care for at-risk populations, and patient and caregiver experience of care.
According to the report, 54 of 114 ACOs that started in 2012 spent less than anticipated, and 29 of the 54 collectively received $126 million as their share of the savings. Medicare kept $128 million of savings.
"What I think is impressive is that so many of the organizations did save in the first year," CMS Principal Deputy Administrator Jon Blum said. The agency had anticipated that more rebuilding systems of care, training and hiring new staff, and purchasing data systems would be required in the first year, Mr. Blum said, adding that savings – especially large savings – were not anticipated.
"We are tremendously surprised with the growth of the program," Mr. Blum said. "If these results and these growth trends continue, it’s going to be a continued phenomenal story for the Medicare program," he said.
CMS would not reveal which ACOs met their benchmarks, which were compensated for saving, or how much any ACO received. Mr. Blum said that data eventually would be published.
The agency also recalculated the first-year savings for the Pioneer ACO program. Pioneers must meet more aggressive quality and savings targets. According to the recalculation, 13 of 32 Pioneers hit their targets, and would share in $76 million in savings. Medicare kept $33 million.
An independent analysis by Washington, DC–based L&M Policy Research found that the total savings to the Pioneers and Medicare was $147 million – some $38 million more than what CMS had calculated. The new analysis takes into account factors that had not been figured in by the CMS, said an agency spokesman.
CMS also announced the final savings results for the 5-year Physician Group Practice Demonstration, which ran from 2005 to 2010. Ten physician groups participated in the program, which offered incentives for coordinating care and generating Medicare savings. Seven of the 10 groups met their targets and earned $108 million. All 10 practices are participating in a 2-year extension of the program.
And the agency announced that 232 acute care hospitals, skilled nursing homes, physician group practices, long-term care hospitals and home health agencies were moving into the next phase of the Bundled Payments for Care Improvement initiative. The participants were announced last January, and spent 2013 preparing to be accountable for episodes of care involving some 48 clinical conditions. The goal of the program is to encourage hospitals, physician, and other providers to work together to coordinate care for patients in the hospital and post discharge.
Starting this year, those 232 providers will now start bearing risk for the care they provide.
The agency has also added thousands of conditions that can become eligible for shared risk, said Dr. Patrick Conway, deputy administrator for innovation and quality at the CMS.
Final results for the first year of the Shared Savings Program will be released later in this year.
On Twitter @aliciaault
Fewer hospital readmissions, high-cost imaging studies, and emergency department visits helped 29 of 114 accountable care organizations earn $126 million in shared Medicare savings in 2012, the Centers for Medicare & Medicaid Services announced.
CMS issued interim financial results for the first year that ACOs participated in the Medicare Shared Savings Program. Under the program, ACOs that reduce costs while providing high-quality care can share in the savings to Medicare. They must report on 33 quality measures relating to care coordination and patient safety, use of appropriate preventive health services, improved care for at-risk populations, and patient and caregiver experience of care.
According to the report, 54 of 114 ACOs that started in 2012 spent less than anticipated, and 29 of the 54 collectively received $126 million as their share of the savings. Medicare kept $128 million of savings.
"What I think is impressive is that so many of the organizations did save in the first year," CMS Principal Deputy Administrator Jon Blum said. The agency had anticipated that more rebuilding systems of care, training and hiring new staff, and purchasing data systems would be required in the first year, Mr. Blum said, adding that savings – especially large savings – were not anticipated.
"We are tremendously surprised with the growth of the program," Mr. Blum said. "If these results and these growth trends continue, it’s going to be a continued phenomenal story for the Medicare program," he said.
CMS would not reveal which ACOs met their benchmarks, which were compensated for saving, or how much any ACO received. Mr. Blum said that data eventually would be published.
The agency also recalculated the first-year savings for the Pioneer ACO program. Pioneers must meet more aggressive quality and savings targets. According to the recalculation, 13 of 32 Pioneers hit their targets, and would share in $76 million in savings. Medicare kept $33 million.
An independent analysis by Washington, DC–based L&M Policy Research found that the total savings to the Pioneers and Medicare was $147 million – some $38 million more than what CMS had calculated. The new analysis takes into account factors that had not been figured in by the CMS, said an agency spokesman.
CMS also announced the final savings results for the 5-year Physician Group Practice Demonstration, which ran from 2005 to 2010. Ten physician groups participated in the program, which offered incentives for coordinating care and generating Medicare savings. Seven of the 10 groups met their targets and earned $108 million. All 10 practices are participating in a 2-year extension of the program.
And the agency announced that 232 acute care hospitals, skilled nursing homes, physician group practices, long-term care hospitals and home health agencies were moving into the next phase of the Bundled Payments for Care Improvement initiative. The participants were announced last January, and spent 2013 preparing to be accountable for episodes of care involving some 48 clinical conditions. The goal of the program is to encourage hospitals, physician, and other providers to work together to coordinate care for patients in the hospital and post discharge.
Starting this year, those 232 providers will now start bearing risk for the care they provide.
The agency has also added thousands of conditions that can become eligible for shared risk, said Dr. Patrick Conway, deputy administrator for innovation and quality at the CMS.
Final results for the first year of the Shared Savings Program will be released later in this year.
On Twitter @aliciaault
Fewer hospital readmissions, high-cost imaging studies, and emergency department visits helped 29 of 114 accountable care organizations earn $126 million in shared Medicare savings in 2012, the Centers for Medicare & Medicaid Services announced.
CMS issued interim financial results for the first year that ACOs participated in the Medicare Shared Savings Program. Under the program, ACOs that reduce costs while providing high-quality care can share in the savings to Medicare. They must report on 33 quality measures relating to care coordination and patient safety, use of appropriate preventive health services, improved care for at-risk populations, and patient and caregiver experience of care.
According to the report, 54 of 114 ACOs that started in 2012 spent less than anticipated, and 29 of the 54 collectively received $126 million as their share of the savings. Medicare kept $128 million of savings.
"What I think is impressive is that so many of the organizations did save in the first year," CMS Principal Deputy Administrator Jon Blum said. The agency had anticipated that more rebuilding systems of care, training and hiring new staff, and purchasing data systems would be required in the first year, Mr. Blum said, adding that savings – especially large savings – were not anticipated.
"We are tremendously surprised with the growth of the program," Mr. Blum said. "If these results and these growth trends continue, it’s going to be a continued phenomenal story for the Medicare program," he said.
CMS would not reveal which ACOs met their benchmarks, which were compensated for saving, or how much any ACO received. Mr. Blum said that data eventually would be published.
The agency also recalculated the first-year savings for the Pioneer ACO program. Pioneers must meet more aggressive quality and savings targets. According to the recalculation, 13 of 32 Pioneers hit their targets, and would share in $76 million in savings. Medicare kept $33 million.
An independent analysis by Washington, DC–based L&M Policy Research found that the total savings to the Pioneers and Medicare was $147 million – some $38 million more than what CMS had calculated. The new analysis takes into account factors that had not been figured in by the CMS, said an agency spokesman.
CMS also announced the final savings results for the 5-year Physician Group Practice Demonstration, which ran from 2005 to 2010. Ten physician groups participated in the program, which offered incentives for coordinating care and generating Medicare savings. Seven of the 10 groups met their targets and earned $108 million. All 10 practices are participating in a 2-year extension of the program.
And the agency announced that 232 acute care hospitals, skilled nursing homes, physician group practices, long-term care hospitals and home health agencies were moving into the next phase of the Bundled Payments for Care Improvement initiative. The participants were announced last January, and spent 2013 preparing to be accountable for episodes of care involving some 48 clinical conditions. The goal of the program is to encourage hospitals, physician, and other providers to work together to coordinate care for patients in the hospital and post discharge.
Starting this year, those 232 providers will now start bearing risk for the care they provide.
The agency has also added thousands of conditions that can become eligible for shared risk, said Dr. Patrick Conway, deputy administrator for innovation and quality at the CMS.
Final results for the first year of the Shared Savings Program will be released later in this year.
On Twitter @aliciaault
FDA approves tasimelteon for sleep-wake disorder
The U.S. Food and Drug Administration approved tasimelteon (Hetlioz) for sleep disturbances in the blind.
The drug, a melatonin receptor agonist, is indicated only for totally blind individuals who have chronic non-24-hour sleep-wake disorder.
With non-24, as it is called, the circadian rhythm is disrupted, causing difficulty with the timing of sleep. People who have the condition sleep when they should not and can’t sleep when they should.
"Non-24-hour sleep-wake disorder can prevent blind individuals from following the normal daily schedule that we all take for granted," said Dr. Eric Bastings, deputy director of the division of neurology products in the FDA’s Center for Drug Evaluation and Research, Silver Spring, Md. "Hetlioz can improve the ability to sleep at night and to be active during the day."
The FDA and tasimelteon’s maker, Vanda Pharmaceuticals, estimate that 80,000-100,000 blind individuals have non-24 disorder. Tasimelteon was given priority review by the FDA because it was deemed to have the potential to significantly improve patients’ lives. Non-24 also is considered a rare condition, so tasimelteon received orphan-drug designation by the FDA, which gives it additional years of market exclusivity.
"Totally blind people have struggled with the problems brought on by non-24-hour sleep-wake disorder, sometimes for their entire life, without understanding what causes it and without being able to do anything about it," said Steven W. Lockley, Ph.D., of the sleep medicine division at Brigham and Women’s Hospital, Boston, and an investigator for Vanda. The approval "means that, for the first time, these patients have access to an approved, safe and effective treatment for their difficult debilitating disorder," Dr. Lockley said in a statement issued by Vanda.
The company evaluated tasimelteon’s effectiveness in 104 participants in two clinical trials of totally blind individuals with non-24 disorder. Patients receiving the therapy had significantly increased nighttime sleep and decreased daytime sleep duration, compared with placebo, according to the FDA.
The most common side effects were headache, elevated liver enzymes (alanine aminotransferase), nightmares or unusual dreams, disturbed night’s sleep, upper respiratory or urinary tract infection, and drowsiness. To reduce the risk of decreased mental alertness, tasimelteon should be taken at the same time every night before bedtime and activities should be limited after taking the drug, the agency said.
Vanda said that tasimelteon should be available within a few months as a 20-mg capsule. The company also has studied the drug for chronic insomnia and depression. It ended the depression studies in early 2013 and is not currently actively pursuing the insomnia indication.
On Twitter @aliciaault
The U.S. Food and Drug Administration approved tasimelteon (Hetlioz) for sleep disturbances in the blind.
The drug, a melatonin receptor agonist, is indicated only for totally blind individuals who have chronic non-24-hour sleep-wake disorder.
With non-24, as it is called, the circadian rhythm is disrupted, causing difficulty with the timing of sleep. People who have the condition sleep when they should not and can’t sleep when they should.
"Non-24-hour sleep-wake disorder can prevent blind individuals from following the normal daily schedule that we all take for granted," said Dr. Eric Bastings, deputy director of the division of neurology products in the FDA’s Center for Drug Evaluation and Research, Silver Spring, Md. "Hetlioz can improve the ability to sleep at night and to be active during the day."
The FDA and tasimelteon’s maker, Vanda Pharmaceuticals, estimate that 80,000-100,000 blind individuals have non-24 disorder. Tasimelteon was given priority review by the FDA because it was deemed to have the potential to significantly improve patients’ lives. Non-24 also is considered a rare condition, so tasimelteon received orphan-drug designation by the FDA, which gives it additional years of market exclusivity.
"Totally blind people have struggled with the problems brought on by non-24-hour sleep-wake disorder, sometimes for their entire life, without understanding what causes it and without being able to do anything about it," said Steven W. Lockley, Ph.D., of the sleep medicine division at Brigham and Women’s Hospital, Boston, and an investigator for Vanda. The approval "means that, for the first time, these patients have access to an approved, safe and effective treatment for their difficult debilitating disorder," Dr. Lockley said in a statement issued by Vanda.
The company evaluated tasimelteon’s effectiveness in 104 participants in two clinical trials of totally blind individuals with non-24 disorder. Patients receiving the therapy had significantly increased nighttime sleep and decreased daytime sleep duration, compared with placebo, according to the FDA.
The most common side effects were headache, elevated liver enzymes (alanine aminotransferase), nightmares or unusual dreams, disturbed night’s sleep, upper respiratory or urinary tract infection, and drowsiness. To reduce the risk of decreased mental alertness, tasimelteon should be taken at the same time every night before bedtime and activities should be limited after taking the drug, the agency said.
Vanda said that tasimelteon should be available within a few months as a 20-mg capsule. The company also has studied the drug for chronic insomnia and depression. It ended the depression studies in early 2013 and is not currently actively pursuing the insomnia indication.
On Twitter @aliciaault
The U.S. Food and Drug Administration approved tasimelteon (Hetlioz) for sleep disturbances in the blind.
The drug, a melatonin receptor agonist, is indicated only for totally blind individuals who have chronic non-24-hour sleep-wake disorder.
With non-24, as it is called, the circadian rhythm is disrupted, causing difficulty with the timing of sleep. People who have the condition sleep when they should not and can’t sleep when they should.
"Non-24-hour sleep-wake disorder can prevent blind individuals from following the normal daily schedule that we all take for granted," said Dr. Eric Bastings, deputy director of the division of neurology products in the FDA’s Center for Drug Evaluation and Research, Silver Spring, Md. "Hetlioz can improve the ability to sleep at night and to be active during the day."
The FDA and tasimelteon’s maker, Vanda Pharmaceuticals, estimate that 80,000-100,000 blind individuals have non-24 disorder. Tasimelteon was given priority review by the FDA because it was deemed to have the potential to significantly improve patients’ lives. Non-24 also is considered a rare condition, so tasimelteon received orphan-drug designation by the FDA, which gives it additional years of market exclusivity.
"Totally blind people have struggled with the problems brought on by non-24-hour sleep-wake disorder, sometimes for their entire life, without understanding what causes it and without being able to do anything about it," said Steven W. Lockley, Ph.D., of the sleep medicine division at Brigham and Women’s Hospital, Boston, and an investigator for Vanda. The approval "means that, for the first time, these patients have access to an approved, safe and effective treatment for their difficult debilitating disorder," Dr. Lockley said in a statement issued by Vanda.
The company evaluated tasimelteon’s effectiveness in 104 participants in two clinical trials of totally blind individuals with non-24 disorder. Patients receiving the therapy had significantly increased nighttime sleep and decreased daytime sleep duration, compared with placebo, according to the FDA.
The most common side effects were headache, elevated liver enzymes (alanine aminotransferase), nightmares or unusual dreams, disturbed night’s sleep, upper respiratory or urinary tract infection, and drowsiness. To reduce the risk of decreased mental alertness, tasimelteon should be taken at the same time every night before bedtime and activities should be limited after taking the drug, the agency said.
Vanda said that tasimelteon should be available within a few months as a 20-mg capsule. The company also has studied the drug for chronic insomnia and depression. It ended the depression studies in early 2013 and is not currently actively pursuing the insomnia indication.
On Twitter @aliciaault
Whither IPAB? Cost-cutting board is idle, but not gone
January came and went with nary a whisper from the once feared but now nearly forgotten Independent Payment Advisory Board.
Enacted as part of the Affordable Care Act and originally slated to have made its first cost-cutting recommendations by now, the IPAB has no members and has never met. For 2 years in a row, Congress and the President have stripped most of the board’s funding from the federal budget.
Under the ACA, the IPAB is charged with looking at 5-year Medicare spending trends and recommending cuts for the following year if per capita spending exceeds a set target.
The IPAB’s recommendations in any given year automatically take effect if Congress does not pass legislation to achieve the savings by Aug. 15. The board cannot recommend rationing care, increasing revenues, changing benefits, modifying eligibility, increasing cost-sharing, or changing the percentage of the premium that beneficiaries pay or the subsidies they receive under Medicare Part D.
Last year, the Medicare chief actuary determined spending would stay below the 2015 target, so the IPAB did not need to act. Further, the Congressional Budget Office has estimated that continuing slow growth in health care costs could mean that the board may not be called into play for another decade.
Physician organizations remain interested in either repealing the board or revising its scope and composition.
The American Medical Association objects to the IPAB on principle. In Feb. 2012, AMA Executive Vice President and CEO James L. Madara wrote to congressional leaders in support of a House bill to repeal the IPAB, noting that the IPAB "puts important health care payment and policy decisions in the hands of an independent body that has far too little accountability."
For the American Academy of Family Physicians, the IPAB "just isn’t a high priority right now," Dr. Reid Blackwelder, AAFP president, said in an interview.
The AAFP is more focused on replacing the Medicare Sustainable Growth Rate formula. Should the IPAB’s work get under way, the AAFP would go back to trying to get its recommendations reconsidered, Dr. Blackwelder said.
In fact, the AAFP isn’t completely opposed to the IPAB. "We like the concept, however, we really oppose the way the IPAB was set up," Dr. Blackwelder said.
The AAFP supports several changes to the IPAB, including:
• Addition of a primary care physician and a consumer representative to the board.
• A public comment period after IPAB recommendations are sent to Congress.
• Increased focus on quality improvement.
• Inclusion of all health care sectors – not just physician fees – in the board’s immediate mandate.
While the American College of Physicians supports the general concept of an independent panel to help evaluate Medicare fiscal soundness, it wants primary care representation and equal responsibility for meeting targets among all providers.
Bob Doherty, senior vice president of governmental affairs and public policy at the ACP, said that he does not expect any movement from the IPAB in the near future.
"The administration has made no effort to start the appointment process, which inevitably would run into Republican resistance to recommending appointees and Republican resistance in the Senate to their confirmation," he said. Mr. Doherty noted that many Democrats don’t support the IPAB, either.
That makes the IPAB "a fight that the administration and Democrats don’t need to take on now," Mr. Doherty said.
Paul N. Van de Water, a senior fellow at the Center on Budget and Policy Priorities in Washington, predicted that while action from the IPAB is unlikely in 2014, the board eventually will be called to action.
And, Mr. Van de Water said that he thought that physicians should take a more favorable view of the IPAB. "It allows for the application of expert human judgment about how a cost growth problem should be dealt with," he said.
"It’s not an SGR, an automatic formula that you are stuck with."
On Twitter @aliciaault
January came and went with nary a whisper from the once feared but now nearly forgotten Independent Payment Advisory Board.
Enacted as part of the Affordable Care Act and originally slated to have made its first cost-cutting recommendations by now, the IPAB has no members and has never met. For 2 years in a row, Congress and the President have stripped most of the board’s funding from the federal budget.
Under the ACA, the IPAB is charged with looking at 5-year Medicare spending trends and recommending cuts for the following year if per capita spending exceeds a set target.
The IPAB’s recommendations in any given year automatically take effect if Congress does not pass legislation to achieve the savings by Aug. 15. The board cannot recommend rationing care, increasing revenues, changing benefits, modifying eligibility, increasing cost-sharing, or changing the percentage of the premium that beneficiaries pay or the subsidies they receive under Medicare Part D.
Last year, the Medicare chief actuary determined spending would stay below the 2015 target, so the IPAB did not need to act. Further, the Congressional Budget Office has estimated that continuing slow growth in health care costs could mean that the board may not be called into play for another decade.
Physician organizations remain interested in either repealing the board or revising its scope and composition.
The American Medical Association objects to the IPAB on principle. In Feb. 2012, AMA Executive Vice President and CEO James L. Madara wrote to congressional leaders in support of a House bill to repeal the IPAB, noting that the IPAB "puts important health care payment and policy decisions in the hands of an independent body that has far too little accountability."
For the American Academy of Family Physicians, the IPAB "just isn’t a high priority right now," Dr. Reid Blackwelder, AAFP president, said in an interview.
The AAFP is more focused on replacing the Medicare Sustainable Growth Rate formula. Should the IPAB’s work get under way, the AAFP would go back to trying to get its recommendations reconsidered, Dr. Blackwelder said.
In fact, the AAFP isn’t completely opposed to the IPAB. "We like the concept, however, we really oppose the way the IPAB was set up," Dr. Blackwelder said.
The AAFP supports several changes to the IPAB, including:
• Addition of a primary care physician and a consumer representative to the board.
• A public comment period after IPAB recommendations are sent to Congress.
• Increased focus on quality improvement.
• Inclusion of all health care sectors – not just physician fees – in the board’s immediate mandate.
While the American College of Physicians supports the general concept of an independent panel to help evaluate Medicare fiscal soundness, it wants primary care representation and equal responsibility for meeting targets among all providers.
Bob Doherty, senior vice president of governmental affairs and public policy at the ACP, said that he does not expect any movement from the IPAB in the near future.
"The administration has made no effort to start the appointment process, which inevitably would run into Republican resistance to recommending appointees and Republican resistance in the Senate to their confirmation," he said. Mr. Doherty noted that many Democrats don’t support the IPAB, either.
That makes the IPAB "a fight that the administration and Democrats don’t need to take on now," Mr. Doherty said.
Paul N. Van de Water, a senior fellow at the Center on Budget and Policy Priorities in Washington, predicted that while action from the IPAB is unlikely in 2014, the board eventually will be called to action.
And, Mr. Van de Water said that he thought that physicians should take a more favorable view of the IPAB. "It allows for the application of expert human judgment about how a cost growth problem should be dealt with," he said.
"It’s not an SGR, an automatic formula that you are stuck with."
On Twitter @aliciaault
January came and went with nary a whisper from the once feared but now nearly forgotten Independent Payment Advisory Board.
Enacted as part of the Affordable Care Act and originally slated to have made its first cost-cutting recommendations by now, the IPAB has no members and has never met. For 2 years in a row, Congress and the President have stripped most of the board’s funding from the federal budget.
Under the ACA, the IPAB is charged with looking at 5-year Medicare spending trends and recommending cuts for the following year if per capita spending exceeds a set target.
The IPAB’s recommendations in any given year automatically take effect if Congress does not pass legislation to achieve the savings by Aug. 15. The board cannot recommend rationing care, increasing revenues, changing benefits, modifying eligibility, increasing cost-sharing, or changing the percentage of the premium that beneficiaries pay or the subsidies they receive under Medicare Part D.
Last year, the Medicare chief actuary determined spending would stay below the 2015 target, so the IPAB did not need to act. Further, the Congressional Budget Office has estimated that continuing slow growth in health care costs could mean that the board may not be called into play for another decade.
Physician organizations remain interested in either repealing the board or revising its scope and composition.
The American Medical Association objects to the IPAB on principle. In Feb. 2012, AMA Executive Vice President and CEO James L. Madara wrote to congressional leaders in support of a House bill to repeal the IPAB, noting that the IPAB "puts important health care payment and policy decisions in the hands of an independent body that has far too little accountability."
For the American Academy of Family Physicians, the IPAB "just isn’t a high priority right now," Dr. Reid Blackwelder, AAFP president, said in an interview.
The AAFP is more focused on replacing the Medicare Sustainable Growth Rate formula. Should the IPAB’s work get under way, the AAFP would go back to trying to get its recommendations reconsidered, Dr. Blackwelder said.
In fact, the AAFP isn’t completely opposed to the IPAB. "We like the concept, however, we really oppose the way the IPAB was set up," Dr. Blackwelder said.
The AAFP supports several changes to the IPAB, including:
• Addition of a primary care physician and a consumer representative to the board.
• A public comment period after IPAB recommendations are sent to Congress.
• Increased focus on quality improvement.
• Inclusion of all health care sectors – not just physician fees – in the board’s immediate mandate.
While the American College of Physicians supports the general concept of an independent panel to help evaluate Medicare fiscal soundness, it wants primary care representation and equal responsibility for meeting targets among all providers.
Bob Doherty, senior vice president of governmental affairs and public policy at the ACP, said that he does not expect any movement from the IPAB in the near future.
"The administration has made no effort to start the appointment process, which inevitably would run into Republican resistance to recommending appointees and Republican resistance in the Senate to their confirmation," he said. Mr. Doherty noted that many Democrats don’t support the IPAB, either.
That makes the IPAB "a fight that the administration and Democrats don’t need to take on now," Mr. Doherty said.
Paul N. Van de Water, a senior fellow at the Center on Budget and Policy Priorities in Washington, predicted that while action from the IPAB is unlikely in 2014, the board eventually will be called to action.
And, Mr. Van de Water said that he thought that physicians should take a more favorable view of the IPAB. "It allows for the application of expert human judgment about how a cost growth problem should be dealt with," he said.
"It’s not an SGR, an automatic formula that you are stuck with."
On Twitter @aliciaault
FDA: Naproxen may pose lower CV risk
The Food and Drug Administration says that the nonsteroidal anti-inflammatory drug naproxen may carry a lower risk of cardiovascular thromboembolic events than that of other selective or nonselective NSAIDs.
The agency presented evidence for that finding in briefing documents that were issued ahead of a Feb. 10-11 joint meeting of the Arthritis Advisory Committee and the Drug Safety and Risk Management Advisory Committee.
At that meeting, the FDA will ask the two advisory committees if the data show that naproxen may have a lower risk for CV thrombotic events. The agency also will ask whether warnings or restrictions should be considered for patients who might be at higher risk for CV events, and whether over-the-counter NSAIDs are acceptable at the currently available doses.
According to the documents, the primary evidence for a better cardiovascular safety profile for naproxen comes from a meta-analysis conducted by the Coxib and traditional NSAID Trialists’ (CNT) Collaboration at Oxford University. The principal investigators gave the FDA a prepublication copy of the study in February 2013. The meta-analysis, which assessed both the gastrointestinal and the cardiovascular risks of nonselective NSAIDs, concluded that naproxen had a lower risk of CV thromboembolic events than did celecoxib and ibuprofen (Lancet 2013;382:769-79).
The FDA has been assessing the safety profile of both cyclooxygenase-2 (COX-2) selective NSAIDs and nonselective NSAIDs for almost a decade. In 2005, the arthritis and drug safety committees pondered the safety of rofecoxib and celecoxib. Based on the panels’ conclusions, the FDA concluded that the risk for CV thromboembolic events was present for both COX-2 selective NSAIDs and nonselective NSAIDs.
The agency subsequently asked Pfizer to voluntarily withdraw valdecoxib (Bextra) from the U.S. market, and all prescription NSAIDs were given a boxed warning on the potential for serious adverse CV events. (Merck had previously withdrawn rofecoxib voluntarily from the U.S. market in 2004.) NSAIDs also carry a warning on the potential for gastrointestinal events. A Medication Guide was developed for patients to inform them of the risk of CV events and gastrointestinal bleeding with all NSAIDs. And companies that made nonselective NSAIDs were asked to conduct comprehensive reviews of their existing controlled clinical trial databases to evaluate CV safety.
The Oxford meta-analysis reinforces the agency’s conclusions from 2005, according to the briefing documents. It also brings into question whether Pfizer should continue its long-term study, Prospective Randomized Evaluation of Celecoxib Integrated Safety vs. Ibuprofen or Naproxen (PRECISION), which was begun in the wake of the 2005 panel meeting at the agency’s behest.
The necessity – and wisdom – of continuing that trial is one of the issues that will be discussed at the Feb. 10-11 joint advisory committee meeting.
On Twitter @aliciaault
The Food and Drug Administration says that the nonsteroidal anti-inflammatory drug naproxen may carry a lower risk of cardiovascular thromboembolic events than that of other selective or nonselective NSAIDs.
The agency presented evidence for that finding in briefing documents that were issued ahead of a Feb. 10-11 joint meeting of the Arthritis Advisory Committee and the Drug Safety and Risk Management Advisory Committee.
At that meeting, the FDA will ask the two advisory committees if the data show that naproxen may have a lower risk for CV thrombotic events. The agency also will ask whether warnings or restrictions should be considered for patients who might be at higher risk for CV events, and whether over-the-counter NSAIDs are acceptable at the currently available doses.
According to the documents, the primary evidence for a better cardiovascular safety profile for naproxen comes from a meta-analysis conducted by the Coxib and traditional NSAID Trialists’ (CNT) Collaboration at Oxford University. The principal investigators gave the FDA a prepublication copy of the study in February 2013. The meta-analysis, which assessed both the gastrointestinal and the cardiovascular risks of nonselective NSAIDs, concluded that naproxen had a lower risk of CV thromboembolic events than did celecoxib and ibuprofen (Lancet 2013;382:769-79).
The FDA has been assessing the safety profile of both cyclooxygenase-2 (COX-2) selective NSAIDs and nonselective NSAIDs for almost a decade. In 2005, the arthritis and drug safety committees pondered the safety of rofecoxib and celecoxib. Based on the panels’ conclusions, the FDA concluded that the risk for CV thromboembolic events was present for both COX-2 selective NSAIDs and nonselective NSAIDs.
The agency subsequently asked Pfizer to voluntarily withdraw valdecoxib (Bextra) from the U.S. market, and all prescription NSAIDs were given a boxed warning on the potential for serious adverse CV events. (Merck had previously withdrawn rofecoxib voluntarily from the U.S. market in 2004.) NSAIDs also carry a warning on the potential for gastrointestinal events. A Medication Guide was developed for patients to inform them of the risk of CV events and gastrointestinal bleeding with all NSAIDs. And companies that made nonselective NSAIDs were asked to conduct comprehensive reviews of their existing controlled clinical trial databases to evaluate CV safety.
The Oxford meta-analysis reinforces the agency’s conclusions from 2005, according to the briefing documents. It also brings into question whether Pfizer should continue its long-term study, Prospective Randomized Evaluation of Celecoxib Integrated Safety vs. Ibuprofen or Naproxen (PRECISION), which was begun in the wake of the 2005 panel meeting at the agency’s behest.
The necessity – and wisdom – of continuing that trial is one of the issues that will be discussed at the Feb. 10-11 joint advisory committee meeting.
On Twitter @aliciaault
The Food and Drug Administration says that the nonsteroidal anti-inflammatory drug naproxen may carry a lower risk of cardiovascular thromboembolic events than that of other selective or nonselective NSAIDs.
The agency presented evidence for that finding in briefing documents that were issued ahead of a Feb. 10-11 joint meeting of the Arthritis Advisory Committee and the Drug Safety and Risk Management Advisory Committee.
At that meeting, the FDA will ask the two advisory committees if the data show that naproxen may have a lower risk for CV thrombotic events. The agency also will ask whether warnings or restrictions should be considered for patients who might be at higher risk for CV events, and whether over-the-counter NSAIDs are acceptable at the currently available doses.
According to the documents, the primary evidence for a better cardiovascular safety profile for naproxen comes from a meta-analysis conducted by the Coxib and traditional NSAID Trialists’ (CNT) Collaboration at Oxford University. The principal investigators gave the FDA a prepublication copy of the study in February 2013. The meta-analysis, which assessed both the gastrointestinal and the cardiovascular risks of nonselective NSAIDs, concluded that naproxen had a lower risk of CV thromboembolic events than did celecoxib and ibuprofen (Lancet 2013;382:769-79).
The FDA has been assessing the safety profile of both cyclooxygenase-2 (COX-2) selective NSAIDs and nonselective NSAIDs for almost a decade. In 2005, the arthritis and drug safety committees pondered the safety of rofecoxib and celecoxib. Based on the panels’ conclusions, the FDA concluded that the risk for CV thromboembolic events was present for both COX-2 selective NSAIDs and nonselective NSAIDs.
The agency subsequently asked Pfizer to voluntarily withdraw valdecoxib (Bextra) from the U.S. market, and all prescription NSAIDs were given a boxed warning on the potential for serious adverse CV events. (Merck had previously withdrawn rofecoxib voluntarily from the U.S. market in 2004.) NSAIDs also carry a warning on the potential for gastrointestinal events. A Medication Guide was developed for patients to inform them of the risk of CV events and gastrointestinal bleeding with all NSAIDs. And companies that made nonselective NSAIDs were asked to conduct comprehensive reviews of their existing controlled clinical trial databases to evaluate CV safety.
The Oxford meta-analysis reinforces the agency’s conclusions from 2005, according to the briefing documents. It also brings into question whether Pfizer should continue its long-term study, Prospective Randomized Evaluation of Celecoxib Integrated Safety vs. Ibuprofen or Naproxen (PRECISION), which was begun in the wake of the 2005 panel meeting at the agency’s behest.
The necessity – and wisdom – of continuing that trial is one of the issues that will be discussed at the Feb. 10-11 joint advisory committee meeting.
On Twitter @aliciaault
Inpatient safety efforts yield mixed results
Adverse events decreased over the last decade for Medicare inpatients with acute myocardial infarction or heart failure but barely changed for those with pneumonia or conditions requiring surgery, according to an analysis of a Medicare database.
The improvements likely translated to 81,000 fewer adverse events for patients with acute MI (AMI) and heart failure (HF) from 2010 to 2011 alone, according to the study published Jan. 22 in the New England Journal of Medicine.
"Although this suggests that national efforts focused on patient safety have made some inroads, the lack of reductions across the board is disappointing," Yun Wang, Ph.D., of the Harvard School of Public Health, Boston, and his colleagues wrote.
The researchers examined whether hospitalized patients are any better off in light of the current focus on patient safety, including the launch of initiatives such as the American College of Surgeons’ National Surgical Quality Improvement Program and the federal government’s Surgical Infection Prevention Project.
They used three composite outcomes measures: the rate of occurrence for adverse events for which patients were at risk (for instance, only patients receiving warfarin were at risk for warfarin-related events); the proportion of patients with one or more adverse events; and the number of adverse events per 1,000 hospitalizations. They analyzed data on 61,523 patients who were discharged from 4,372 hospitals; the data were extracted from the Medicare Patient Safety Monitoring System database (N. Engl. J. Med. 2014:370;341-51).
The 61,523 patients included 11,399 with AMI, 15,374 with HF, 18,269 with pneumonia, and 16,481 with conditions requiring surgery. Postsurgical patients largely were being treated for joint replacement procedures and other osteoarthritis-related conditions, femur fracture, colon cancer, post-AMI procedures, or other forms of chronic ischemic heart disease.
From 2005-2006 to 2010-2011, AMI and HF patients saw a 1.3 percentage point decline in the rate of adverse events, from 5% to 3.7%. The proportion who had one or more such events decreased from 26% to 19%. The number of adverse events per 1,000 hospitalizations declined from 402 to 262 for AMI patients and from 235 to 167 for HF patients.
Infection-related and drug-related adverse events declined significantly in heart attack and HF patients. There was also a substantial improvement in postprocedure events in HF patients.
Postsurgical patients experienced slight increases in all three outcomes measures, in particular, increases in infection-related and postprocedural events such as venous thromboembolism, and cardiac and catheter-related events. The number of events per 1,000 hospitalizations for pneumonia patients increased insignificantly from 216 to 223. For postsurgical patients, the number of events increased insignificantly from 352/1,000 to 368/1,000.
Patients who had adverse events had significantly longer hospital stays and were at higher risk for death. As the number of adverse events increased, so did the risk of death.
The authors noted that declines in events for AMI and HF patients might be a reflection of the numerous efforts and initiatives to improve care in those two conditions.
But they also found that concerted efforts to improve safety did not necessarily work. There was an increase in pressure ulcers in postsurgical patients, and no decline in ventilator-associated pneumonia in most patients, even though there have been initiatives focused on those conditions.
"Our finding of an increased adverse-event rate among surgical patients indicates a continuing challenge and identifies an important target for patient-safety initiatives," the researchers said.
The study was supported by the Agency for Healthcare Research and Quality as well as academic and federal grants. Dr. Wang was a consultant to and other researchers were employees of the research firm Qualidigm and participated in the analysis. One of the researchers, Dr. Harlan M. Krumholz, disclosed being on a scientific advisory board for UnitedHealthcare and receiving grant money from Medtronic.
On Twitter @aliciaault
Adverse events decreased over the last decade for Medicare inpatients with acute myocardial infarction or heart failure but barely changed for those with pneumonia or conditions requiring surgery, according to an analysis of a Medicare database.
The improvements likely translated to 81,000 fewer adverse events for patients with acute MI (AMI) and heart failure (HF) from 2010 to 2011 alone, according to the study published Jan. 22 in the New England Journal of Medicine.
"Although this suggests that national efforts focused on patient safety have made some inroads, the lack of reductions across the board is disappointing," Yun Wang, Ph.D., of the Harvard School of Public Health, Boston, and his colleagues wrote.
The researchers examined whether hospitalized patients are any better off in light of the current focus on patient safety, including the launch of initiatives such as the American College of Surgeons’ National Surgical Quality Improvement Program and the federal government’s Surgical Infection Prevention Project.
They used three composite outcomes measures: the rate of occurrence for adverse events for which patients were at risk (for instance, only patients receiving warfarin were at risk for warfarin-related events); the proportion of patients with one or more adverse events; and the number of adverse events per 1,000 hospitalizations. They analyzed data on 61,523 patients who were discharged from 4,372 hospitals; the data were extracted from the Medicare Patient Safety Monitoring System database (N. Engl. J. Med. 2014:370;341-51).
The 61,523 patients included 11,399 with AMI, 15,374 with HF, 18,269 with pneumonia, and 16,481 with conditions requiring surgery. Postsurgical patients largely were being treated for joint replacement procedures and other osteoarthritis-related conditions, femur fracture, colon cancer, post-AMI procedures, or other forms of chronic ischemic heart disease.
From 2005-2006 to 2010-2011, AMI and HF patients saw a 1.3 percentage point decline in the rate of adverse events, from 5% to 3.7%. The proportion who had one or more such events decreased from 26% to 19%. The number of adverse events per 1,000 hospitalizations declined from 402 to 262 for AMI patients and from 235 to 167 for HF patients.
Infection-related and drug-related adverse events declined significantly in heart attack and HF patients. There was also a substantial improvement in postprocedure events in HF patients.
Postsurgical patients experienced slight increases in all three outcomes measures, in particular, increases in infection-related and postprocedural events such as venous thromboembolism, and cardiac and catheter-related events. The number of events per 1,000 hospitalizations for pneumonia patients increased insignificantly from 216 to 223. For postsurgical patients, the number of events increased insignificantly from 352/1,000 to 368/1,000.
Patients who had adverse events had significantly longer hospital stays and were at higher risk for death. As the number of adverse events increased, so did the risk of death.
The authors noted that declines in events for AMI and HF patients might be a reflection of the numerous efforts and initiatives to improve care in those two conditions.
But they also found that concerted efforts to improve safety did not necessarily work. There was an increase in pressure ulcers in postsurgical patients, and no decline in ventilator-associated pneumonia in most patients, even though there have been initiatives focused on those conditions.
"Our finding of an increased adverse-event rate among surgical patients indicates a continuing challenge and identifies an important target for patient-safety initiatives," the researchers said.
The study was supported by the Agency for Healthcare Research and Quality as well as academic and federal grants. Dr. Wang was a consultant to and other researchers were employees of the research firm Qualidigm and participated in the analysis. One of the researchers, Dr. Harlan M. Krumholz, disclosed being on a scientific advisory board for UnitedHealthcare and receiving grant money from Medtronic.
On Twitter @aliciaault
Adverse events decreased over the last decade for Medicare inpatients with acute myocardial infarction or heart failure but barely changed for those with pneumonia or conditions requiring surgery, according to an analysis of a Medicare database.
The improvements likely translated to 81,000 fewer adverse events for patients with acute MI (AMI) and heart failure (HF) from 2010 to 2011 alone, according to the study published Jan. 22 in the New England Journal of Medicine.
"Although this suggests that national efforts focused on patient safety have made some inroads, the lack of reductions across the board is disappointing," Yun Wang, Ph.D., of the Harvard School of Public Health, Boston, and his colleagues wrote.
The researchers examined whether hospitalized patients are any better off in light of the current focus on patient safety, including the launch of initiatives such as the American College of Surgeons’ National Surgical Quality Improvement Program and the federal government’s Surgical Infection Prevention Project.
They used three composite outcomes measures: the rate of occurrence for adverse events for which patients were at risk (for instance, only patients receiving warfarin were at risk for warfarin-related events); the proportion of patients with one or more adverse events; and the number of adverse events per 1,000 hospitalizations. They analyzed data on 61,523 patients who were discharged from 4,372 hospitals; the data were extracted from the Medicare Patient Safety Monitoring System database (N. Engl. J. Med. 2014:370;341-51).
The 61,523 patients included 11,399 with AMI, 15,374 with HF, 18,269 with pneumonia, and 16,481 with conditions requiring surgery. Postsurgical patients largely were being treated for joint replacement procedures and other osteoarthritis-related conditions, femur fracture, colon cancer, post-AMI procedures, or other forms of chronic ischemic heart disease.
From 2005-2006 to 2010-2011, AMI and HF patients saw a 1.3 percentage point decline in the rate of adverse events, from 5% to 3.7%. The proportion who had one or more such events decreased from 26% to 19%. The number of adverse events per 1,000 hospitalizations declined from 402 to 262 for AMI patients and from 235 to 167 for HF patients.
Infection-related and drug-related adverse events declined significantly in heart attack and HF patients. There was also a substantial improvement in postprocedure events in HF patients.
Postsurgical patients experienced slight increases in all three outcomes measures, in particular, increases in infection-related and postprocedural events such as venous thromboembolism, and cardiac and catheter-related events. The number of events per 1,000 hospitalizations for pneumonia patients increased insignificantly from 216 to 223. For postsurgical patients, the number of events increased insignificantly from 352/1,000 to 368/1,000.
Patients who had adverse events had significantly longer hospital stays and were at higher risk for death. As the number of adverse events increased, so did the risk of death.
The authors noted that declines in events for AMI and HF patients might be a reflection of the numerous efforts and initiatives to improve care in those two conditions.
But they also found that concerted efforts to improve safety did not necessarily work. There was an increase in pressure ulcers in postsurgical patients, and no decline in ventilator-associated pneumonia in most patients, even though there have been initiatives focused on those conditions.
"Our finding of an increased adverse-event rate among surgical patients indicates a continuing challenge and identifies an important target for patient-safety initiatives," the researchers said.
The study was supported by the Agency for Healthcare Research and Quality as well as academic and federal grants. Dr. Wang was a consultant to and other researchers were employees of the research firm Qualidigm and participated in the analysis. One of the researchers, Dr. Harlan M. Krumholz, disclosed being on a scientific advisory board for UnitedHealthcare and receiving grant money from Medtronic.
On Twitter @aliciaault
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major finding: At least 81,000 adverse events were avoided in a single year in patients hospitalized for acute MI and heart failure.
Data source: A retrospective analysis of data from 61,523 patients in the Medicare Patient Safety Monitoring System.
Disclosures: The study was supported by the Agency for Healthcare Research and Quality as well as academic and federal grants. Dr. Wang was a consultant to and other researchers were employees of the research firm Qualidigm and participated in the analysis. One of the researchers, Dr. Harlan M. Krumholz, disclosed being on a scientific advisory board for UnitedHealthcare and receiving grant money from Medtronic.
Will 100% coverage spur more use of breast cancer chemopreventives?
Breast cancer chemopreventive drugs such as tamoxifen should be covered as a preventive service with no out-of-pocket cost for high-risk women, according to the Health and Human Services department. But it’s not clear if the HHS clarification of covered preventive benefits under the Affordable Care Act will encourage more primary care physicians to prescribe the medications and more women to take the drugs.
Dr. Jeffery Ward, an oncologist at the Swedish Cancer Institute, Edmonds, Wash., said that he did not think cost was a big obstacle, as tamoxifen is available generically. Concern about side effects and a lack of knowledge among primary care physicians are larger issues, said Dr. Ward, who is the immediate past chairman of the American Society of Clinical Oncology’s clinical practice committee.
The policy – clarified by HHS on Jan. 9 – would apply to group and individual health insurance policies that went into effect after the March 2010 enactment of the Affordable Care Act, as well as those that have been substantially changed since then.
The ACA mandates that services or therapies given an "A" or "B" rating by the U.S. Preventive Services Task Force be covered as preventive care by individual and group health plans and Medicare. States have the option to cover these benefits for Medicaid recipients.
Preventive benefits must be covered with no copayments, deductibles, or other out-of-pocket costs.
The breast cancer prevention coverage must start on or after Sept. 24, 2014, 1 year after the USPSTF first issued a "B" rating also, for use of the selective estrogen receptor modulators, tamoxifen, or raloxifene for women at high-risk for breast cancer and low risk for side effects. ASCO urged use of tamoxifen and raloxifene for breast cancer prevention in guidelines issued in July (J. Clin. Onc. 2013;31:2942-62).
Currently, tamoxifen and raloxifene are the only Food and Drug Administration–approved drugs for breast cancer prevention in high-risk women. Tamoxifen is approved for women aged 35 years and older; and raloxifene for postmenopausal women. The USPSTF backed the use of the FDA-approved therapies only. Likewise, the HHS policy applies to only FDA-approved drugs.
As many of 5% of U.S. women may be eligible for breast cancer chemoprevention, according to Dr. Mark H. Ebell, a USPSTF member and epidemiologist with the University of Georgia, Athens, who spoke with Frontline Medical News after the guidelines were issued. Few seem to be currently taking any of these prevention drugs, however, according to data compiled by the USPSTF. The task force cited surveys showing that, after being told of the risks and benefits, 50%-75% of high-risk women declined to accept a prescription for tamoxifen or raloxifene. Concerns about side effects seemed to be the main concern.
There is also a lag in prescribing. Only 96 of 350 primary care physicians – including ob.gyns – who responded to a survey, said that they had prescribed tamoxifen as a preventive, according to a study.
Dr. Ward said that primary care physicians may not understand who is an appropriate candidate or may be reluctant to refer healthy women to an oncologist. They also might not be comfortable prescribing a medication they regard as a cancer drug, he said. Many of the high-risk women referred to him ultimately end up taking a chemopreventive, he said, adding that for every patient who refuses, there are probably 4 who agree to try the therapy, but "15 after that who never hear about it," because of gaps in knowledge in the primary care setting.
While the HHS clarification will likely help many of his patients, he also sees it leading to some confusion. For instance, patients who already have breast cancer might think that their medications will now be covered without any out-of-pocket costs. "The consequences have not been well thought out," said Dr. Ward, of the coverage policy.
The coverage requirement also gave insurers pause. "We are concerned about the precedent of expanding the definition of prevention to now include some treatments that must be covered with no cost-sharing," said Robert Zirkelbach, a spokesman for America’s Health Insurance Plans (AHIP). He said that while, "helping women with breast cancer get the care they need has long been a top priority for health plans," the cost of therapies that appear to be "free" are actually "reflected in the premiums consumers pay for coverage."
Dr. Ward noted, however, that it might be less expensive for insurers to cover the cost of chemopreventives than for the treatment of a woman with breast cancer.
On Twitter @aliciaault
Breast cancer chemopreventive drugs such as tamoxifen should be covered as a preventive service with no out-of-pocket cost for high-risk women, according to the Health and Human Services department. But it’s not clear if the HHS clarification of covered preventive benefits under the Affordable Care Act will encourage more primary care physicians to prescribe the medications and more women to take the drugs.
Dr. Jeffery Ward, an oncologist at the Swedish Cancer Institute, Edmonds, Wash., said that he did not think cost was a big obstacle, as tamoxifen is available generically. Concern about side effects and a lack of knowledge among primary care physicians are larger issues, said Dr. Ward, who is the immediate past chairman of the American Society of Clinical Oncology’s clinical practice committee.
The policy – clarified by HHS on Jan. 9 – would apply to group and individual health insurance policies that went into effect after the March 2010 enactment of the Affordable Care Act, as well as those that have been substantially changed since then.
The ACA mandates that services or therapies given an "A" or "B" rating by the U.S. Preventive Services Task Force be covered as preventive care by individual and group health plans and Medicare. States have the option to cover these benefits for Medicaid recipients.
Preventive benefits must be covered with no copayments, deductibles, or other out-of-pocket costs.
The breast cancer prevention coverage must start on or after Sept. 24, 2014, 1 year after the USPSTF first issued a "B" rating also, for use of the selective estrogen receptor modulators, tamoxifen, or raloxifene for women at high-risk for breast cancer and low risk for side effects. ASCO urged use of tamoxifen and raloxifene for breast cancer prevention in guidelines issued in July (J. Clin. Onc. 2013;31:2942-62).
Currently, tamoxifen and raloxifene are the only Food and Drug Administration–approved drugs for breast cancer prevention in high-risk women. Tamoxifen is approved for women aged 35 years and older; and raloxifene for postmenopausal women. The USPSTF backed the use of the FDA-approved therapies only. Likewise, the HHS policy applies to only FDA-approved drugs.
As many of 5% of U.S. women may be eligible for breast cancer chemoprevention, according to Dr. Mark H. Ebell, a USPSTF member and epidemiologist with the University of Georgia, Athens, who spoke with Frontline Medical News after the guidelines were issued. Few seem to be currently taking any of these prevention drugs, however, according to data compiled by the USPSTF. The task force cited surveys showing that, after being told of the risks and benefits, 50%-75% of high-risk women declined to accept a prescription for tamoxifen or raloxifene. Concerns about side effects seemed to be the main concern.
There is also a lag in prescribing. Only 96 of 350 primary care physicians – including ob.gyns – who responded to a survey, said that they had prescribed tamoxifen as a preventive, according to a study.
Dr. Ward said that primary care physicians may not understand who is an appropriate candidate or may be reluctant to refer healthy women to an oncologist. They also might not be comfortable prescribing a medication they regard as a cancer drug, he said. Many of the high-risk women referred to him ultimately end up taking a chemopreventive, he said, adding that for every patient who refuses, there are probably 4 who agree to try the therapy, but "15 after that who never hear about it," because of gaps in knowledge in the primary care setting.
While the HHS clarification will likely help many of his patients, he also sees it leading to some confusion. For instance, patients who already have breast cancer might think that their medications will now be covered without any out-of-pocket costs. "The consequences have not been well thought out," said Dr. Ward, of the coverage policy.
The coverage requirement also gave insurers pause. "We are concerned about the precedent of expanding the definition of prevention to now include some treatments that must be covered with no cost-sharing," said Robert Zirkelbach, a spokesman for America’s Health Insurance Plans (AHIP). He said that while, "helping women with breast cancer get the care they need has long been a top priority for health plans," the cost of therapies that appear to be "free" are actually "reflected in the premiums consumers pay for coverage."
Dr. Ward noted, however, that it might be less expensive for insurers to cover the cost of chemopreventives than for the treatment of a woman with breast cancer.
On Twitter @aliciaault
Breast cancer chemopreventive drugs such as tamoxifen should be covered as a preventive service with no out-of-pocket cost for high-risk women, according to the Health and Human Services department. But it’s not clear if the HHS clarification of covered preventive benefits under the Affordable Care Act will encourage more primary care physicians to prescribe the medications and more women to take the drugs.
Dr. Jeffery Ward, an oncologist at the Swedish Cancer Institute, Edmonds, Wash., said that he did not think cost was a big obstacle, as tamoxifen is available generically. Concern about side effects and a lack of knowledge among primary care physicians are larger issues, said Dr. Ward, who is the immediate past chairman of the American Society of Clinical Oncology’s clinical practice committee.
The policy – clarified by HHS on Jan. 9 – would apply to group and individual health insurance policies that went into effect after the March 2010 enactment of the Affordable Care Act, as well as those that have been substantially changed since then.
The ACA mandates that services or therapies given an "A" or "B" rating by the U.S. Preventive Services Task Force be covered as preventive care by individual and group health plans and Medicare. States have the option to cover these benefits for Medicaid recipients.
Preventive benefits must be covered with no copayments, deductibles, or other out-of-pocket costs.
The breast cancer prevention coverage must start on or after Sept. 24, 2014, 1 year after the USPSTF first issued a "B" rating also, for use of the selective estrogen receptor modulators, tamoxifen, or raloxifene for women at high-risk for breast cancer and low risk for side effects. ASCO urged use of tamoxifen and raloxifene for breast cancer prevention in guidelines issued in July (J. Clin. Onc. 2013;31:2942-62).
Currently, tamoxifen and raloxifene are the only Food and Drug Administration–approved drugs for breast cancer prevention in high-risk women. Tamoxifen is approved for women aged 35 years and older; and raloxifene for postmenopausal women. The USPSTF backed the use of the FDA-approved therapies only. Likewise, the HHS policy applies to only FDA-approved drugs.
As many of 5% of U.S. women may be eligible for breast cancer chemoprevention, according to Dr. Mark H. Ebell, a USPSTF member and epidemiologist with the University of Georgia, Athens, who spoke with Frontline Medical News after the guidelines were issued. Few seem to be currently taking any of these prevention drugs, however, according to data compiled by the USPSTF. The task force cited surveys showing that, after being told of the risks and benefits, 50%-75% of high-risk women declined to accept a prescription for tamoxifen or raloxifene. Concerns about side effects seemed to be the main concern.
There is also a lag in prescribing. Only 96 of 350 primary care physicians – including ob.gyns – who responded to a survey, said that they had prescribed tamoxifen as a preventive, according to a study.
Dr. Ward said that primary care physicians may not understand who is an appropriate candidate or may be reluctant to refer healthy women to an oncologist. They also might not be comfortable prescribing a medication they regard as a cancer drug, he said. Many of the high-risk women referred to him ultimately end up taking a chemopreventive, he said, adding that for every patient who refuses, there are probably 4 who agree to try the therapy, but "15 after that who never hear about it," because of gaps in knowledge in the primary care setting.
While the HHS clarification will likely help many of his patients, he also sees it leading to some confusion. For instance, patients who already have breast cancer might think that their medications will now be covered without any out-of-pocket costs. "The consequences have not been well thought out," said Dr. Ward, of the coverage policy.
The coverage requirement also gave insurers pause. "We are concerned about the precedent of expanding the definition of prevention to now include some treatments that must be covered with no cost-sharing," said Robert Zirkelbach, a spokesman for America’s Health Insurance Plans (AHIP). He said that while, "helping women with breast cancer get the care they need has long been a top priority for health plans," the cost of therapies that appear to be "free" are actually "reflected in the premiums consumers pay for coverage."
Dr. Ward noted, however, that it might be less expensive for insurers to cover the cost of chemopreventives than for the treatment of a woman with breast cancer.
On Twitter @aliciaault
Budget, short-term SGR fix signed
Physicians will get a 0.5% raise in Medicare pay on Jan. 1, thanks to a last-minute legislative fix to the Sustainable Growth Rate formula signed into law by President Obama on Dec. 26.
The Pathway for SGR Reform Act of 2013 was attached as an amendment to the Bipartisan Budget Agreement of 2013. The budget deal, brokered by Sen. Patty Murray (D-Wash.) and Rep. Paul Ryan (R-Wis.), passed the House on Dec. 12 and the Senate on Dec. 18. The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. It would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
The law also extends the 2% sequestration cut to Medicare payments by 2 years, to 2023.
It encourages the CMS to simplify physicians’ administrative burden by more closely coordinating quality measure requirements and giving doctors timely feedback.
The law extends funding for a variety of other health-related federal programs for an additional 3 months, including for Area Agencies on Aging. Finally, the law delays enforcement of the "two-midnight rule" until October 2014. The goal of the rule is to cut down on hospitals using observation status to keep from admitting patients. Hospitals have until Oct. 1, 2014, to adjust to the new policy, which requires admission if a physician thinks a patient will need a stay longer than 48 hours.
Congress was expected to consider a permanent replacement for the SGR when it returned on Jan. 6.
Physicians will get a 0.5% raise in Medicare pay on Jan. 1, thanks to a last-minute legislative fix to the Sustainable Growth Rate formula signed into law by President Obama on Dec. 26.
The Pathway for SGR Reform Act of 2013 was attached as an amendment to the Bipartisan Budget Agreement of 2013. The budget deal, brokered by Sen. Patty Murray (D-Wash.) and Rep. Paul Ryan (R-Wis.), passed the House on Dec. 12 and the Senate on Dec. 18. The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. It would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
The law also extends the 2% sequestration cut to Medicare payments by 2 years, to 2023.
It encourages the CMS to simplify physicians’ administrative burden by more closely coordinating quality measure requirements and giving doctors timely feedback.
The law extends funding for a variety of other health-related federal programs for an additional 3 months, including for Area Agencies on Aging. Finally, the law delays enforcement of the "two-midnight rule" until October 2014. The goal of the rule is to cut down on hospitals using observation status to keep from admitting patients. Hospitals have until Oct. 1, 2014, to adjust to the new policy, which requires admission if a physician thinks a patient will need a stay longer than 48 hours.
Congress was expected to consider a permanent replacement for the SGR when it returned on Jan. 6.
Physicians will get a 0.5% raise in Medicare pay on Jan. 1, thanks to a last-minute legislative fix to the Sustainable Growth Rate formula signed into law by President Obama on Dec. 26.
The Pathway for SGR Reform Act of 2013 was attached as an amendment to the Bipartisan Budget Agreement of 2013. The budget deal, brokered by Sen. Patty Murray (D-Wash.) and Rep. Paul Ryan (R-Wis.), passed the House on Dec. 12 and the Senate on Dec. 18. The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. It would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
The law also extends the 2% sequestration cut to Medicare payments by 2 years, to 2023.
It encourages the CMS to simplify physicians’ administrative burden by more closely coordinating quality measure requirements and giving doctors timely feedback.
The law extends funding for a variety of other health-related federal programs for an additional 3 months, including for Area Agencies on Aging. Finally, the law delays enforcement of the "two-midnight rule" until October 2014. The goal of the rule is to cut down on hospitals using observation status to keep from admitting patients. Hospitals have until Oct. 1, 2014, to adjust to the new policy, which requires admission if a physician thinks a patient will need a stay longer than 48 hours.
Congress was expected to consider a permanent replacement for the SGR when it returned on Jan. 6.