User login
VIDEO: Post-stroke pioglitazone modestly protective against secondary vascular events
LOS ANGELES – Nondiabetic, insulin-resistant patients who started pioglitazone within 6 months of an ischemic stroke or transient ischemic attack had almost a 3% absolute risk reduction in secondary strokes and myocardial infarctions after 5 years, in a randomized, clinical trial published online Feb. 17 in the New England Journal of Medicine.
Stroke or MI – the study’s primary combined outcome – occurred in 175 of 1,939 (9.0%) pioglitazone (Actos) patients, but 228 of 1,937 (11.8%) placebo patients (hazard ratio, 0.76; P = 0.007). There was no significant difference in all-cause mortality (HR, 0.93; P = 0.52).
Seventy-three pioglitazone patients (3.8%) developed diabetes, compared with 149 (7.7%) in the placebo group (HR, 0.48; P less than 0.001). That wasn’t a surprise; pioglitazone has been shown to protect insulin resistant patients against diabetes, the study investigators noted (N Engl J Med. 2016 Feb 17; doi: 10.1056/NEJMoa1506930).
Known side effects showed up as well. Pioglitazone was associated with a greater frequency of weight gain exceeding 4.5 kg (52.2% versus 33.7%, P less than 0.001), edema (35.6% versus 24.9%, P less than 0.001), and bone fracture requiring surgery or hospitalization (5.1% versus 3.2%, P = 0.003).
Heart failure – another known risk with the drug – did not show up in the trial; people with heart failure histories or other risk factors were excluded.
The median baseline modified Rankin Scale in both groups was 1, and the median NIH Stroke Scale score was 0. The pioglitazone target dose was 45 mg daily.
Insulin resistance is a risk factor for heart attack and stroke, which may help explain the thiazolidinedione’s apparent protective effects. It was defined in the trial as a score greater than 3.0 on the homeostasis model assessment of insulin resistance (HOMA-IR) index.
So, should pioglitazone be a part of routine post-stroke care?
In a video interview at the International Stroke Conference, lead investigator Dr. Walter N. Kernan, a professor of general medicine at Yale University, New Haven, Conn., shared his thoughts.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LOS ANGELES – Nondiabetic, insulin-resistant patients who started pioglitazone within 6 months of an ischemic stroke or transient ischemic attack had almost a 3% absolute risk reduction in secondary strokes and myocardial infarctions after 5 years, in a randomized, clinical trial published online Feb. 17 in the New England Journal of Medicine.
Stroke or MI – the study’s primary combined outcome – occurred in 175 of 1,939 (9.0%) pioglitazone (Actos) patients, but 228 of 1,937 (11.8%) placebo patients (hazard ratio, 0.76; P = 0.007). There was no significant difference in all-cause mortality (HR, 0.93; P = 0.52).
Seventy-three pioglitazone patients (3.8%) developed diabetes, compared with 149 (7.7%) in the placebo group (HR, 0.48; P less than 0.001). That wasn’t a surprise; pioglitazone has been shown to protect insulin resistant patients against diabetes, the study investigators noted (N Engl J Med. 2016 Feb 17; doi: 10.1056/NEJMoa1506930).
Known side effects showed up as well. Pioglitazone was associated with a greater frequency of weight gain exceeding 4.5 kg (52.2% versus 33.7%, P less than 0.001), edema (35.6% versus 24.9%, P less than 0.001), and bone fracture requiring surgery or hospitalization (5.1% versus 3.2%, P = 0.003).
Heart failure – another known risk with the drug – did not show up in the trial; people with heart failure histories or other risk factors were excluded.
The median baseline modified Rankin Scale in both groups was 1, and the median NIH Stroke Scale score was 0. The pioglitazone target dose was 45 mg daily.
Insulin resistance is a risk factor for heart attack and stroke, which may help explain the thiazolidinedione’s apparent protective effects. It was defined in the trial as a score greater than 3.0 on the homeostasis model assessment of insulin resistance (HOMA-IR) index.
So, should pioglitazone be a part of routine post-stroke care?
In a video interview at the International Stroke Conference, lead investigator Dr. Walter N. Kernan, a professor of general medicine at Yale University, New Haven, Conn., shared his thoughts.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LOS ANGELES – Nondiabetic, insulin-resistant patients who started pioglitazone within 6 months of an ischemic stroke or transient ischemic attack had almost a 3% absolute risk reduction in secondary strokes and myocardial infarctions after 5 years, in a randomized, clinical trial published online Feb. 17 in the New England Journal of Medicine.
Stroke or MI – the study’s primary combined outcome – occurred in 175 of 1,939 (9.0%) pioglitazone (Actos) patients, but 228 of 1,937 (11.8%) placebo patients (hazard ratio, 0.76; P = 0.007). There was no significant difference in all-cause mortality (HR, 0.93; P = 0.52).
Seventy-three pioglitazone patients (3.8%) developed diabetes, compared with 149 (7.7%) in the placebo group (HR, 0.48; P less than 0.001). That wasn’t a surprise; pioglitazone has been shown to protect insulin resistant patients against diabetes, the study investigators noted (N Engl J Med. 2016 Feb 17; doi: 10.1056/NEJMoa1506930).
Known side effects showed up as well. Pioglitazone was associated with a greater frequency of weight gain exceeding 4.5 kg (52.2% versus 33.7%, P less than 0.001), edema (35.6% versus 24.9%, P less than 0.001), and bone fracture requiring surgery or hospitalization (5.1% versus 3.2%, P = 0.003).
Heart failure – another known risk with the drug – did not show up in the trial; people with heart failure histories or other risk factors were excluded.
The median baseline modified Rankin Scale in both groups was 1, and the median NIH Stroke Scale score was 0. The pioglitazone target dose was 45 mg daily.
Insulin resistance is a risk factor for heart attack and stroke, which may help explain the thiazolidinedione’s apparent protective effects. It was defined in the trial as a score greater than 3.0 on the homeostasis model assessment of insulin resistance (HOMA-IR) index.
So, should pioglitazone be a part of routine post-stroke care?
In a video interview at the International Stroke Conference, lead investigator Dr. Walter N. Kernan, a professor of general medicine at Yale University, New Haven, Conn., shared his thoughts.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE INTERNATIONAL STROKE CONFERENCE
VIDEO: Migraine plus aura doubles ischemic stroke rate
LOS ANGELES – Adults who have migraine with aura had twice the rate of ischemic strokes, compared with people with migraine without aura in a review of 11,663 older Americans followed for an average of 18 years.
Migraine with aura appeared to increase the rate of cardioembolic strokes particularly, and the findings highlighted that middle-aged and older adults diagnosed with migraine with aura require special attention to interventions that could reduce their cardiovascular disease risks, Dr. Souvik Sen said in a video interview during the International Stroke Conference.
While results from prior studies have implicated migraine with aura as a risk factor for ischemic stroke, the new analysis was notable for involving an especially large number of community-dwelling older Americans, suggesting that the finding is broadly applicable to the general population of people with an average age of 58-60 years, said Dr. Sen, professor of clinical neurology and chairman of the department of neurology at the University of South Carolina in Columbia.
“It’s been known that migraine can increase the risk of stroke and that certain subgroups of migraine patients are especially important, such as patients with aura,” commented Dr. Ralph Sacco, professor and chairman of neurology at the University of Miami. “When I see patients with migraine I think about treating their migraine effectively and getting it under control, and putting even greater focus on controlling stroke risk factors. I also warn women with migraine about their increased stroke risk from using estrogen-containing oral contraceptives or hormone replacement,” Dr. Sacco noted.
Dr. Sen noted that the new analysis included people enrolled in the Atherosclerosis Risk in Communities (ARIC) study, which enrolled a random sample of more than 15,000 participants from four U.S. communities in 1987. The analysis focused on 11,663 people with migraine information collected during the third ARIC examination during 1993-1995, which identified 458 people (4%) who had migraine with aura, 1,158 (10%) who had migraine without aura, and 10,047 (86%) who were migraine free. During 18 years of follow-up the incidence of ischemic stroke among those with migraine with aura was twofold higher than among those with migraine without aura after adjustment for baseline rate of stroke risk factors, a statistically significant difference, he reported at the meeting sponsored by the American Heart Association. This difference seemed largely driven by a significant increase in the rate of cardioembolic strokes among the people with migraine with aura.
One hypothesis explaining the increased stroke rate in patients with aura is that, in patients with this presentation of migraine, the neurologic activity of migraine appears to spread to cerebral blood vessels and may affect blood flow within those vessels, Dr. Sen explained. It is also possible that migraine with aura may be a risk marker for or may predispose people to more extensive cardiovascular disease including atrial fibrillation.
The primary clinical implication of the finding is that people with migraine with aura should especially undergo a thorough assessment for cardiovascular disease risk factors, and should receive especially aggressive risk factor management, including controlling hypertension and smoking cessation, assessing ECG and atrial fibrillation, and avoiding estrogen treatment, Dr. Sen said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
LOS ANGELES – Adults who have migraine with aura had twice the rate of ischemic strokes, compared with people with migraine without aura in a review of 11,663 older Americans followed for an average of 18 years.
Migraine with aura appeared to increase the rate of cardioembolic strokes particularly, and the findings highlighted that middle-aged and older adults diagnosed with migraine with aura require special attention to interventions that could reduce their cardiovascular disease risks, Dr. Souvik Sen said in a video interview during the International Stroke Conference.
While results from prior studies have implicated migraine with aura as a risk factor for ischemic stroke, the new analysis was notable for involving an especially large number of community-dwelling older Americans, suggesting that the finding is broadly applicable to the general population of people with an average age of 58-60 years, said Dr. Sen, professor of clinical neurology and chairman of the department of neurology at the University of South Carolina in Columbia.
“It’s been known that migraine can increase the risk of stroke and that certain subgroups of migraine patients are especially important, such as patients with aura,” commented Dr. Ralph Sacco, professor and chairman of neurology at the University of Miami. “When I see patients with migraine I think about treating their migraine effectively and getting it under control, and putting even greater focus on controlling stroke risk factors. I also warn women with migraine about their increased stroke risk from using estrogen-containing oral contraceptives or hormone replacement,” Dr. Sacco noted.
Dr. Sen noted that the new analysis included people enrolled in the Atherosclerosis Risk in Communities (ARIC) study, which enrolled a random sample of more than 15,000 participants from four U.S. communities in 1987. The analysis focused on 11,663 people with migraine information collected during the third ARIC examination during 1993-1995, which identified 458 people (4%) who had migraine with aura, 1,158 (10%) who had migraine without aura, and 10,047 (86%) who were migraine free. During 18 years of follow-up the incidence of ischemic stroke among those with migraine with aura was twofold higher than among those with migraine without aura after adjustment for baseline rate of stroke risk factors, a statistically significant difference, he reported at the meeting sponsored by the American Heart Association. This difference seemed largely driven by a significant increase in the rate of cardioembolic strokes among the people with migraine with aura.
One hypothesis explaining the increased stroke rate in patients with aura is that, in patients with this presentation of migraine, the neurologic activity of migraine appears to spread to cerebral blood vessels and may affect blood flow within those vessels, Dr. Sen explained. It is also possible that migraine with aura may be a risk marker for or may predispose people to more extensive cardiovascular disease including atrial fibrillation.
The primary clinical implication of the finding is that people with migraine with aura should especially undergo a thorough assessment for cardiovascular disease risk factors, and should receive especially aggressive risk factor management, including controlling hypertension and smoking cessation, assessing ECG and atrial fibrillation, and avoiding estrogen treatment, Dr. Sen said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
LOS ANGELES – Adults who have migraine with aura had twice the rate of ischemic strokes, compared with people with migraine without aura in a review of 11,663 older Americans followed for an average of 18 years.
Migraine with aura appeared to increase the rate of cardioembolic strokes particularly, and the findings highlighted that middle-aged and older adults diagnosed with migraine with aura require special attention to interventions that could reduce their cardiovascular disease risks, Dr. Souvik Sen said in a video interview during the International Stroke Conference.
While results from prior studies have implicated migraine with aura as a risk factor for ischemic stroke, the new analysis was notable for involving an especially large number of community-dwelling older Americans, suggesting that the finding is broadly applicable to the general population of people with an average age of 58-60 years, said Dr. Sen, professor of clinical neurology and chairman of the department of neurology at the University of South Carolina in Columbia.
“It’s been known that migraine can increase the risk of stroke and that certain subgroups of migraine patients are especially important, such as patients with aura,” commented Dr. Ralph Sacco, professor and chairman of neurology at the University of Miami. “When I see patients with migraine I think about treating their migraine effectively and getting it under control, and putting even greater focus on controlling stroke risk factors. I also warn women with migraine about their increased stroke risk from using estrogen-containing oral contraceptives or hormone replacement,” Dr. Sacco noted.
Dr. Sen noted that the new analysis included people enrolled in the Atherosclerosis Risk in Communities (ARIC) study, which enrolled a random sample of more than 15,000 participants from four U.S. communities in 1987. The analysis focused on 11,663 people with migraine information collected during the third ARIC examination during 1993-1995, which identified 458 people (4%) who had migraine with aura, 1,158 (10%) who had migraine without aura, and 10,047 (86%) who were migraine free. During 18 years of follow-up the incidence of ischemic stroke among those with migraine with aura was twofold higher than among those with migraine without aura after adjustment for baseline rate of stroke risk factors, a statistically significant difference, he reported at the meeting sponsored by the American Heart Association. This difference seemed largely driven by a significant increase in the rate of cardioembolic strokes among the people with migraine with aura.
One hypothesis explaining the increased stroke rate in patients with aura is that, in patients with this presentation of migraine, the neurologic activity of migraine appears to spread to cerebral blood vessels and may affect blood flow within those vessels, Dr. Sen explained. It is also possible that migraine with aura may be a risk marker for or may predispose people to more extensive cardiovascular disease including atrial fibrillation.
The primary clinical implication of the finding is that people with migraine with aura should especially undergo a thorough assessment for cardiovascular disease risk factors, and should receive especially aggressive risk factor management, including controlling hypertension and smoking cessation, assessing ECG and atrial fibrillation, and avoiding estrogen treatment, Dr. Sen said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point: Older adults with migraine and aura had twice the ischemic strokes, compared with patients with aura-free migraines.
Major finding: Strokes occurred twofold more often in patients with migraine with aura, compared with patients with migraine alone after adjustments.
Data source: Review of 11,663 older adult Americans enrolled in the Atherosclerosis Risk in Communities study.
Disclosures: Dr. Sen had no disclosures.
VIDEO: Could noninvasive prenatal testing mean gene profiling for every pregnancy?
ATLANTA – The decision of whether to screen a pregnancy for genetic anomalies should not be taken lightly, especially in light of the invasive procedures required. But what if a simple maternal blood test could provide everything we needed to know about a fetus’ genetic health?
At the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine, Dr. Ronald J. Wapner of Columbia University, New York, said that time is quickly approaching, and that cell-free fetal DNA testing should – and will – become a routine part of prenatal care.
Watch an interview with Dr. Wapner here.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – The decision of whether to screen a pregnancy for genetic anomalies should not be taken lightly, especially in light of the invasive procedures required. But what if a simple maternal blood test could provide everything we needed to know about a fetus’ genetic health?
At the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine, Dr. Ronald J. Wapner of Columbia University, New York, said that time is quickly approaching, and that cell-free fetal DNA testing should – and will – become a routine part of prenatal care.
Watch an interview with Dr. Wapner here.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – The decision of whether to screen a pregnancy for genetic anomalies should not be taken lightly, especially in light of the invasive procedures required. But what if a simple maternal blood test could provide everything we needed to know about a fetus’ genetic health?
At the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine, Dr. Ronald J. Wapner of Columbia University, New York, said that time is quickly approaching, and that cell-free fetal DNA testing should – and will – become a routine part of prenatal care.
Watch an interview with Dr. Wapner here.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE PREGNANCY MEETING
VIDEO: To optimize children’s oral health, take care of moms first
ATLANTA – Oral health – whether poor or good – seems to run in families. Is it behavior, biology, or both?
At the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine, Dr. Renee Samelson, a maternal-fetal medicine specialist with a certification in preventive medicine, said that taking care of moms’ teeth and gums, even before pregnancy, gives children the best shot at maintaining a healthy mouth from infancy to old age.
Watch an interview with Dr. Samelson here.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – Oral health – whether poor or good – seems to run in families. Is it behavior, biology, or both?
At the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine, Dr. Renee Samelson, a maternal-fetal medicine specialist with a certification in preventive medicine, said that taking care of moms’ teeth and gums, even before pregnancy, gives children the best shot at maintaining a healthy mouth from infancy to old age.
Watch an interview with Dr. Samelson here.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – Oral health – whether poor or good – seems to run in families. Is it behavior, biology, or both?
At the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine, Dr. Renee Samelson, a maternal-fetal medicine specialist with a certification in preventive medicine, said that taking care of moms’ teeth and gums, even before pregnancy, gives children the best shot at maintaining a healthy mouth from infancy to old age.
Watch an interview with Dr. Samelson here.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE PREGNANCY MEETING
VIDEO: Which patients are best for new onychomycosis topicals?
WAIKOLOA, HAWAII – Two new topical treatments for nail fungal infections are more effective than previous topical therapies, but the key to successful results is picking the right onychomycosis patient, according to Dr. Theodore Rosen.
The two new agents, tavaborole and efinaconazole, “are both better than what we had previously, especially considering topical agents don’t do quite as well as oral agents do,” explained Dr. Rosen, professor of dermatology at Baylor College of Medicine, Houston.
The new topicals are “very convenient, in that it’s an easy-to-do regimen, once a day,” Dr. Rosen noted. But “they are inconvenient, in that they both have to be used about 48 weeks. So, that’s about a year’s worth of therapy.”
In an interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation, Dr. Rosen discussed approaches to achieving the best outcomes with the new agents, and he outlined other practical steps patients can take to prevent the return of nail fungal infections.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAIKOLOA, HAWAII – Two new topical treatments for nail fungal infections are more effective than previous topical therapies, but the key to successful results is picking the right onychomycosis patient, according to Dr. Theodore Rosen.
The two new agents, tavaborole and efinaconazole, “are both better than what we had previously, especially considering topical agents don’t do quite as well as oral agents do,” explained Dr. Rosen, professor of dermatology at Baylor College of Medicine, Houston.
The new topicals are “very convenient, in that it’s an easy-to-do regimen, once a day,” Dr. Rosen noted. But “they are inconvenient, in that they both have to be used about 48 weeks. So, that’s about a year’s worth of therapy.”
In an interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation, Dr. Rosen discussed approaches to achieving the best outcomes with the new agents, and he outlined other practical steps patients can take to prevent the return of nail fungal infections.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAIKOLOA, HAWAII – Two new topical treatments for nail fungal infections are more effective than previous topical therapies, but the key to successful results is picking the right onychomycosis patient, according to Dr. Theodore Rosen.
The two new agents, tavaborole and efinaconazole, “are both better than what we had previously, especially considering topical agents don’t do quite as well as oral agents do,” explained Dr. Rosen, professor of dermatology at Baylor College of Medicine, Houston.
The new topicals are “very convenient, in that it’s an easy-to-do regimen, once a day,” Dr. Rosen noted. But “they are inconvenient, in that they both have to be used about 48 weeks. So, that’s about a year’s worth of therapy.”
In an interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation, Dr. Rosen discussed approaches to achieving the best outcomes with the new agents, and he outlined other practical steps patients can take to prevent the return of nail fungal infections.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF HAWAII DERMATOLOGY SEMINAR
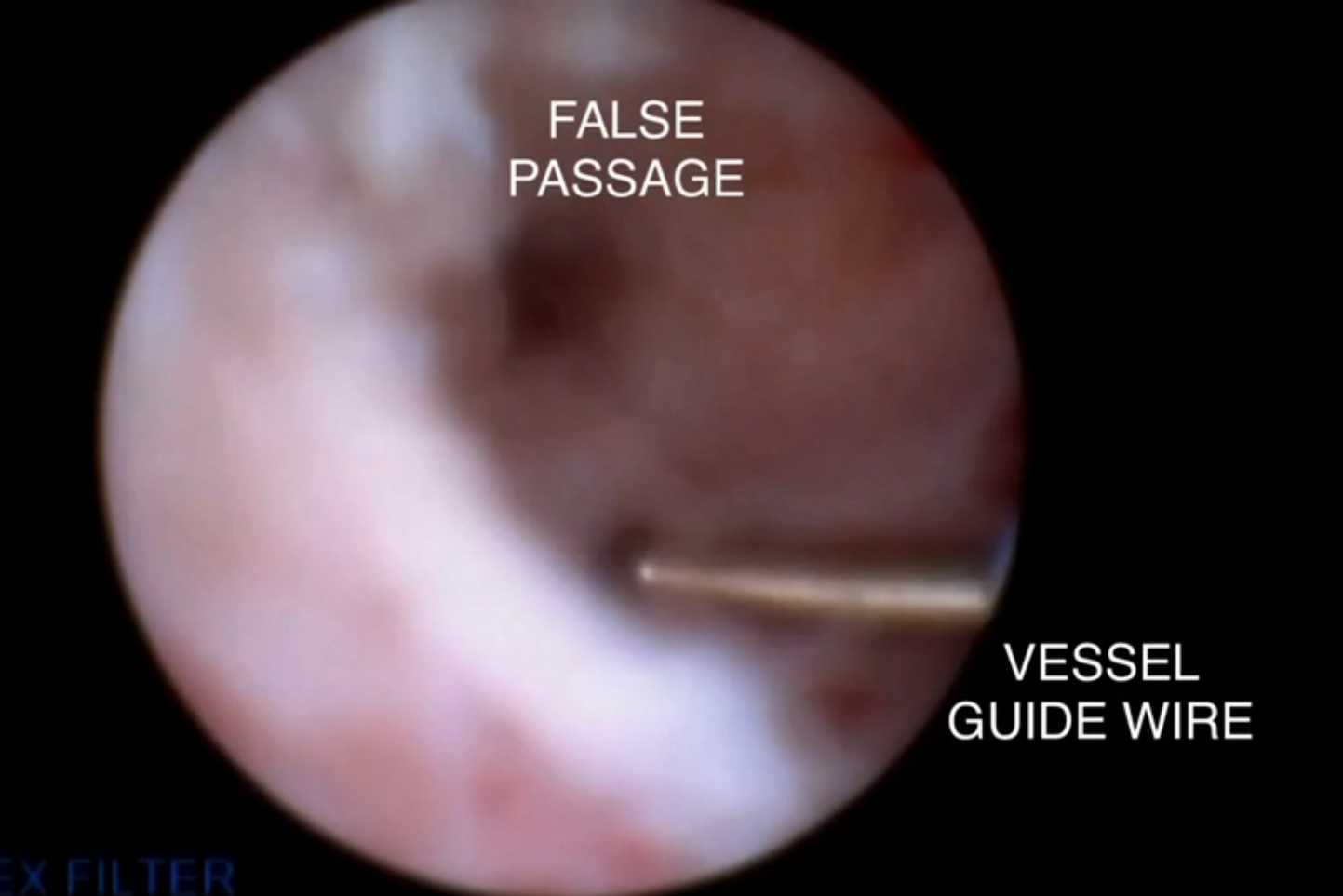
A novel approach to overcoming cervical stenosis and false passages

For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org

For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org

For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org
This video is brought to you by ![]()
VIDEO: New topical acne therapies will target sebum
WAIKOLOA, HAWAII – Three new approaches to topical treatment of acne are on the horizon, and they all share a common foe: sebum.
“One exciting new avenue for topical therapy are drugs that actually target the production of sebum,” explained Dr. Linda F. Stein Gold, director of dermatology research at Henry Ford Health System, Detroit. “For the first time, we have a drug that potentially targets sebum with a topical mechanism. In the past, we’ve only been able to do that with oral therapy.”
In an interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation, Dr. Stein Gold discussed three topical, sebum-focused drugs in clinical trials and outlined their differing mechanisms of action.
SDEF and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – Three new approaches to topical treatment of acne are on the horizon, and they all share a common foe: sebum.
“One exciting new avenue for topical therapy are drugs that actually target the production of sebum,” explained Dr. Linda F. Stein Gold, director of dermatology research at Henry Ford Health System, Detroit. “For the first time, we have a drug that potentially targets sebum with a topical mechanism. In the past, we’ve only been able to do that with oral therapy.”
In an interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation, Dr. Stein Gold discussed three topical, sebum-focused drugs in clinical trials and outlined their differing mechanisms of action.
SDEF and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – Three new approaches to topical treatment of acne are on the horizon, and they all share a common foe: sebum.
“One exciting new avenue for topical therapy are drugs that actually target the production of sebum,” explained Dr. Linda F. Stein Gold, director of dermatology research at Henry Ford Health System, Detroit. “For the first time, we have a drug that potentially targets sebum with a topical mechanism. In the past, we’ve only been able to do that with oral therapy.”
In an interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation, Dr. Stein Gold discussed three topical, sebum-focused drugs in clinical trials and outlined their differing mechanisms of action.
SDEF and this news organization are owned by the same parent company.
AT SDEF HAWAII DERMATOLOGY SEMINAR
VIDEO: What’s new on atopic dermatitis drugs and cancer concerns?
WAIKOLOA, HAWAII – Topical calcineurin inhibitors’ boxed warnings give many patients and physicians pause over cancer concerns – but a new database analysis may put some minds at ease about the drugs’ use for atopic dermatitis.
“Pimecrolimus and tacrolimus are given topically, not internally – very little absorption occurs. So, it was hoped that ... we wouldn’t see cancer increases in these patients,” explained Dr. Joseph F. Fowler Jr., clinical professor of dermatology at the University of Louisville (Ky.). “And in fact, that’s exactly what was shown in this large study.”
In an interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation, Dr. Fowler discussed the data from new research examining cancer incidence and calcineurin inhibitor use.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAIKOLOA, HAWAII – Topical calcineurin inhibitors’ boxed warnings give many patients and physicians pause over cancer concerns – but a new database analysis may put some minds at ease about the drugs’ use for atopic dermatitis.
“Pimecrolimus and tacrolimus are given topically, not internally – very little absorption occurs. So, it was hoped that ... we wouldn’t see cancer increases in these patients,” explained Dr. Joseph F. Fowler Jr., clinical professor of dermatology at the University of Louisville (Ky.). “And in fact, that’s exactly what was shown in this large study.”
In an interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation, Dr. Fowler discussed the data from new research examining cancer incidence and calcineurin inhibitor use.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAIKOLOA, HAWAII – Topical calcineurin inhibitors’ boxed warnings give many patients and physicians pause over cancer concerns – but a new database analysis may put some minds at ease about the drugs’ use for atopic dermatitis.
“Pimecrolimus and tacrolimus are given topically, not internally – very little absorption occurs. So, it was hoped that ... we wouldn’t see cancer increases in these patients,” explained Dr. Joseph F. Fowler Jr., clinical professor of dermatology at the University of Louisville (Ky.). “And in fact, that’s exactly what was shown in this large study.”
In an interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation, Dr. Fowler discussed the data from new research examining cancer incidence and calcineurin inhibitor use.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF HAWAII DERMATOLOGY SEMINAR
VIDEO: IL-17 antagonists continue reshaping psoriasis therapy in 2016
WAIKOLOA, HAWAII – What’s going to be the biggest development in the field of psoriasis in 2016?
Hint: Look for a repeat of 2015.
The first of the interleukin-17 antagonists, secukinumab, was the biggest development of 2015, explained Dr. Craig L. Leonardi, associate clinical professor of dermatology at Saint Louis University, St. Louis. “It’s always good when we get another mechanism of action.”
2016 should see the debut of another IL-17 antagonist, ixekizumab, which “seems to be more efficacious than secukinumab,” Dr. Leonardi said in an interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAIKOLOA, HAWAII – What’s going to be the biggest development in the field of psoriasis in 2016?
Hint: Look for a repeat of 2015.
The first of the interleukin-17 antagonists, secukinumab, was the biggest development of 2015, explained Dr. Craig L. Leonardi, associate clinical professor of dermatology at Saint Louis University, St. Louis. “It’s always good when we get another mechanism of action.”
2016 should see the debut of another IL-17 antagonist, ixekizumab, which “seems to be more efficacious than secukinumab,” Dr. Leonardi said in an interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAIKOLOA, HAWAII – What’s going to be the biggest development in the field of psoriasis in 2016?
Hint: Look for a repeat of 2015.
The first of the interleukin-17 antagonists, secukinumab, was the biggest development of 2015, explained Dr. Craig L. Leonardi, associate clinical professor of dermatology at Saint Louis University, St. Louis. “It’s always good when we get another mechanism of action.”
2016 should see the debut of another IL-17 antagonist, ixekizumab, which “seems to be more efficacious than secukinumab,” Dr. Leonardi said in an interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF HAWAII DERMATOLOGY SEMINAR