User login
Do New Antiobesity Meds Still Require Lifestyle Management?
Is lifestyle counseling needed with the more effective second-generation nutrient-stimulated, hormone-based medications like semaglutide and tirzepatide?
If so, how intensive does the counseling need to be, and what components should be emphasized?
These are the clinical practice questions at the top of mind for healthcare professionals and researchers who provide care to patients who have overweight and/or obesity.
This is what we know. Lifestyle management is considered foundational in the care of patients with obesity.
Because obesity is fundamentally a disease of energy dysregulation, counseling has traditionally focused on dietary caloric reduction, increased physical activity, and strategies to adapt new cognitive and lifestyle behaviors.
On the basis of trial results from the Diabetes Prevention Program and the Look AHEAD studies, provision of intensive behavioral therapy (IBT) is recommended for treatment of obesity by the Centers for Medicare & Medicaid Services and by the US Preventive Services Task Force (Moyer VA; US Preventive Services Task Force).
IBT is commonly defined as consisting of 12-26 comprehensive and multicomponent sessions over the course of a year.
Reaffirming the primacy of lifestyle management, all antiobesity medications are approved by the US Food and Drug Administration as an adjunct to a reduced-calorie diet and increased physical activity.
The beneficial effect of combining IBT with earlier-generation medications like naltrexone/bupropion or liraglutide demonstrated that more participants in the trials achieved ≥ 10% weight loss with IBT compared with those taking the medication without IBT: 38.4% vs 20% for naltrexone/bupropion and 46% vs 33% for liraglutide.
Although there aren’t trial data for other first-generation medications like phentermine, orlistat, or phentermine/topiramate, it is assumed that patients taking these medications would also achieve greater weight loss when combined with IBT.
The obesity pharmacotherapy landscape was upended, however, with the approval of semaglutide (Wegovy), a glucagon-like peptide-1 (GLP-1) receptor agonist, in 2021; and tirzepatide (Zepbound), a GLP-1 and glucose-dependent insulinotropic polypeptide dual receptor agonist, in 2023.
These highly effective medications harness the effect of naturally occurring incretin hormones that reduce appetite through direct and indirect effects on the brain. Although the study designs differed between the STEP 1 and STEP 3 trials, the addition of IBT to semaglutide increased mean percent weight loss from 15% to 16% after 68 weeks of treatment (Wilding JPH et al; Wadden TA).
Comparable benefits from the STEP 3 and SURMOUNT-1 trials of adding IBT to tirzepatide at the maximal tolerated dose increased mean percent weight loss from 21% to 24% after 72 weeks (Wadden TA; Jastreboff AM). Though multicomponent IBT appears to provide greater weight loss when used with nutrient-stimulated hormone-based therapeutics, the additional benefit may be less when compared with first-generation medications.
So, how should we view the role and importance of lifestyle management when a patient is taking a second-generation medication? We need to shift the focus from prescribing a calorie-reduced diet to counseling for healthy eating patterns.
Because the second-generation drugs are more biologically effective in suppressing appetite (ie, reducing hunger, food noise, and cravings, and increasing satiation and satiety), it is easier for patients to reduce their food intake without a sense of deprivation. Furthermore, many patients express less desire to consume savory, sweet, and other enticing foods.
Patients should be encouraged to optimize the quality of their diet, prioritizing lean protein sources with meals and snacks; increasing fruits, vegetables, fiber, and complex carbohydrates; and keeping well hydrated. Because of the risk of developing micronutrient deficiencies while consuming a low-calorie diet — most notably calcium, iron, and vitamin D — patients may be advised to take a daily multivitamin supplement. Dietary counseling should be introduced when patients start pharmacotherapy, and if needed, referral to a registered dietitian nutritionist may be helpful in making these changes.
Additional counseling tips to mitigate the gastrointestinal side effects of these drugs that most commonly occur during the early dose-escalation phase include eating slowly; choosing smaller portion sizes; stopping eating when full; not skipping meals; and avoiding fatty, fried, and greasy foods. These dietary changes are particularly important over the first days after patients take the injection.
The increased weight loss achieved also raises concerns about the need to maintain lean body mass and the importance of physical activity and exercise counseling. All weight loss interventions, including dietary restriction, pharmacotherapy, or bariatric surgery, result in loss of fat mass and lean body mass.
The goal of lifestyle counseling is to minimize and preserve muscle mass (a component of lean body mass) which is needed for optimal health, mobility, daily function, and quality of life. Counseling should incorporate both aerobic and resistance training. Aerobic exercise (eg, brisk walking, jogging, dancing, elliptical machine, and cycling) improves cardiovascular fitness, metabolic health, and energy expenditure. Resistance (strength) training (eg, weightlifting, resistance bands, and circuit training) lessens the loss of muscle mass, enhances functional strength and mobility, and improves bone density (Gorgojo-Martinez JJ et al; Oppert JM et al).
Robust physical activity has also been shown to be a predictor of weight loss maintenance. A recently published randomized placebo-controlled trial demonstrated the benefit of supervised exercise in maintaining body weight and lean body mass after discontinuing 52 weeks of liraglutide treatment compared with no exercise.
Rather than minimizing the provision of lifestyle management, using highly effective second-generation therapeutics redirects the focus on how patients with obesity can strive to achieve a healthy and productive life.
A version of this article first appeared on Medscape.com.
Is lifestyle counseling needed with the more effective second-generation nutrient-stimulated, hormone-based medications like semaglutide and tirzepatide?
If so, how intensive does the counseling need to be, and what components should be emphasized?
These are the clinical practice questions at the top of mind for healthcare professionals and researchers who provide care to patients who have overweight and/or obesity.
This is what we know. Lifestyle management is considered foundational in the care of patients with obesity.
Because obesity is fundamentally a disease of energy dysregulation, counseling has traditionally focused on dietary caloric reduction, increased physical activity, and strategies to adapt new cognitive and lifestyle behaviors.
On the basis of trial results from the Diabetes Prevention Program and the Look AHEAD studies, provision of intensive behavioral therapy (IBT) is recommended for treatment of obesity by the Centers for Medicare & Medicaid Services and by the US Preventive Services Task Force (Moyer VA; US Preventive Services Task Force).
IBT is commonly defined as consisting of 12-26 comprehensive and multicomponent sessions over the course of a year.
Reaffirming the primacy of lifestyle management, all antiobesity medications are approved by the US Food and Drug Administration as an adjunct to a reduced-calorie diet and increased physical activity.
The beneficial effect of combining IBT with earlier-generation medications like naltrexone/bupropion or liraglutide demonstrated that more participants in the trials achieved ≥ 10% weight loss with IBT compared with those taking the medication without IBT: 38.4% vs 20% for naltrexone/bupropion and 46% vs 33% for liraglutide.
Although there aren’t trial data for other first-generation medications like phentermine, orlistat, or phentermine/topiramate, it is assumed that patients taking these medications would also achieve greater weight loss when combined with IBT.
The obesity pharmacotherapy landscape was upended, however, with the approval of semaglutide (Wegovy), a glucagon-like peptide-1 (GLP-1) receptor agonist, in 2021; and tirzepatide (Zepbound), a GLP-1 and glucose-dependent insulinotropic polypeptide dual receptor agonist, in 2023.
These highly effective medications harness the effect of naturally occurring incretin hormones that reduce appetite through direct and indirect effects on the brain. Although the study designs differed between the STEP 1 and STEP 3 trials, the addition of IBT to semaglutide increased mean percent weight loss from 15% to 16% after 68 weeks of treatment (Wilding JPH et al; Wadden TA).
Comparable benefits from the STEP 3 and SURMOUNT-1 trials of adding IBT to tirzepatide at the maximal tolerated dose increased mean percent weight loss from 21% to 24% after 72 weeks (Wadden TA; Jastreboff AM). Though multicomponent IBT appears to provide greater weight loss when used with nutrient-stimulated hormone-based therapeutics, the additional benefit may be less when compared with first-generation medications.
So, how should we view the role and importance of lifestyle management when a patient is taking a second-generation medication? We need to shift the focus from prescribing a calorie-reduced diet to counseling for healthy eating patterns.
Because the second-generation drugs are more biologically effective in suppressing appetite (ie, reducing hunger, food noise, and cravings, and increasing satiation and satiety), it is easier for patients to reduce their food intake without a sense of deprivation. Furthermore, many patients express less desire to consume savory, sweet, and other enticing foods.
Patients should be encouraged to optimize the quality of their diet, prioritizing lean protein sources with meals and snacks; increasing fruits, vegetables, fiber, and complex carbohydrates; and keeping well hydrated. Because of the risk of developing micronutrient deficiencies while consuming a low-calorie diet — most notably calcium, iron, and vitamin D — patients may be advised to take a daily multivitamin supplement. Dietary counseling should be introduced when patients start pharmacotherapy, and if needed, referral to a registered dietitian nutritionist may be helpful in making these changes.
Additional counseling tips to mitigate the gastrointestinal side effects of these drugs that most commonly occur during the early dose-escalation phase include eating slowly; choosing smaller portion sizes; stopping eating when full; not skipping meals; and avoiding fatty, fried, and greasy foods. These dietary changes are particularly important over the first days after patients take the injection.
The increased weight loss achieved also raises concerns about the need to maintain lean body mass and the importance of physical activity and exercise counseling. All weight loss interventions, including dietary restriction, pharmacotherapy, or bariatric surgery, result in loss of fat mass and lean body mass.
The goal of lifestyle counseling is to minimize and preserve muscle mass (a component of lean body mass) which is needed for optimal health, mobility, daily function, and quality of life. Counseling should incorporate both aerobic and resistance training. Aerobic exercise (eg, brisk walking, jogging, dancing, elliptical machine, and cycling) improves cardiovascular fitness, metabolic health, and energy expenditure. Resistance (strength) training (eg, weightlifting, resistance bands, and circuit training) lessens the loss of muscle mass, enhances functional strength and mobility, and improves bone density (Gorgojo-Martinez JJ et al; Oppert JM et al).
Robust physical activity has also been shown to be a predictor of weight loss maintenance. A recently published randomized placebo-controlled trial demonstrated the benefit of supervised exercise in maintaining body weight and lean body mass after discontinuing 52 weeks of liraglutide treatment compared with no exercise.
Rather than minimizing the provision of lifestyle management, using highly effective second-generation therapeutics redirects the focus on how patients with obesity can strive to achieve a healthy and productive life.
A version of this article first appeared on Medscape.com.
Is lifestyle counseling needed with the more effective second-generation nutrient-stimulated, hormone-based medications like semaglutide and tirzepatide?
If so, how intensive does the counseling need to be, and what components should be emphasized?
These are the clinical practice questions at the top of mind for healthcare professionals and researchers who provide care to patients who have overweight and/or obesity.
This is what we know. Lifestyle management is considered foundational in the care of patients with obesity.
Because obesity is fundamentally a disease of energy dysregulation, counseling has traditionally focused on dietary caloric reduction, increased physical activity, and strategies to adapt new cognitive and lifestyle behaviors.
On the basis of trial results from the Diabetes Prevention Program and the Look AHEAD studies, provision of intensive behavioral therapy (IBT) is recommended for treatment of obesity by the Centers for Medicare & Medicaid Services and by the US Preventive Services Task Force (Moyer VA; US Preventive Services Task Force).
IBT is commonly defined as consisting of 12-26 comprehensive and multicomponent sessions over the course of a year.
Reaffirming the primacy of lifestyle management, all antiobesity medications are approved by the US Food and Drug Administration as an adjunct to a reduced-calorie diet and increased physical activity.
The beneficial effect of combining IBT with earlier-generation medications like naltrexone/bupropion or liraglutide demonstrated that more participants in the trials achieved ≥ 10% weight loss with IBT compared with those taking the medication without IBT: 38.4% vs 20% for naltrexone/bupropion and 46% vs 33% for liraglutide.
Although there aren’t trial data for other first-generation medications like phentermine, orlistat, or phentermine/topiramate, it is assumed that patients taking these medications would also achieve greater weight loss when combined with IBT.
The obesity pharmacotherapy landscape was upended, however, with the approval of semaglutide (Wegovy), a glucagon-like peptide-1 (GLP-1) receptor agonist, in 2021; and tirzepatide (Zepbound), a GLP-1 and glucose-dependent insulinotropic polypeptide dual receptor agonist, in 2023.
These highly effective medications harness the effect of naturally occurring incretin hormones that reduce appetite through direct and indirect effects on the brain. Although the study designs differed between the STEP 1 and STEP 3 trials, the addition of IBT to semaglutide increased mean percent weight loss from 15% to 16% after 68 weeks of treatment (Wilding JPH et al; Wadden TA).
Comparable benefits from the STEP 3 and SURMOUNT-1 trials of adding IBT to tirzepatide at the maximal tolerated dose increased mean percent weight loss from 21% to 24% after 72 weeks (Wadden TA; Jastreboff AM). Though multicomponent IBT appears to provide greater weight loss when used with nutrient-stimulated hormone-based therapeutics, the additional benefit may be less when compared with first-generation medications.
So, how should we view the role and importance of lifestyle management when a patient is taking a second-generation medication? We need to shift the focus from prescribing a calorie-reduced diet to counseling for healthy eating patterns.
Because the second-generation drugs are more biologically effective in suppressing appetite (ie, reducing hunger, food noise, and cravings, and increasing satiation and satiety), it is easier for patients to reduce their food intake without a sense of deprivation. Furthermore, many patients express less desire to consume savory, sweet, and other enticing foods.
Patients should be encouraged to optimize the quality of their diet, prioritizing lean protein sources with meals and snacks; increasing fruits, vegetables, fiber, and complex carbohydrates; and keeping well hydrated. Because of the risk of developing micronutrient deficiencies while consuming a low-calorie diet — most notably calcium, iron, and vitamin D — patients may be advised to take a daily multivitamin supplement. Dietary counseling should be introduced when patients start pharmacotherapy, and if needed, referral to a registered dietitian nutritionist may be helpful in making these changes.
Additional counseling tips to mitigate the gastrointestinal side effects of these drugs that most commonly occur during the early dose-escalation phase include eating slowly; choosing smaller portion sizes; stopping eating when full; not skipping meals; and avoiding fatty, fried, and greasy foods. These dietary changes are particularly important over the first days after patients take the injection.
The increased weight loss achieved also raises concerns about the need to maintain lean body mass and the importance of physical activity and exercise counseling. All weight loss interventions, including dietary restriction, pharmacotherapy, or bariatric surgery, result in loss of fat mass and lean body mass.
The goal of lifestyle counseling is to minimize and preserve muscle mass (a component of lean body mass) which is needed for optimal health, mobility, daily function, and quality of life. Counseling should incorporate both aerobic and resistance training. Aerobic exercise (eg, brisk walking, jogging, dancing, elliptical machine, and cycling) improves cardiovascular fitness, metabolic health, and energy expenditure. Resistance (strength) training (eg, weightlifting, resistance bands, and circuit training) lessens the loss of muscle mass, enhances functional strength and mobility, and improves bone density (Gorgojo-Martinez JJ et al; Oppert JM et al).
Robust physical activity has also been shown to be a predictor of weight loss maintenance. A recently published randomized placebo-controlled trial demonstrated the benefit of supervised exercise in maintaining body weight and lean body mass after discontinuing 52 weeks of liraglutide treatment compared with no exercise.
Rather than minimizing the provision of lifestyle management, using highly effective second-generation therapeutics redirects the focus on how patients with obesity can strive to achieve a healthy and productive life.
A version of this article first appeared on Medscape.com.
A Banned Chemical That Is Still Causing Cancer
This transcript has been edited for clarity.
These types of stories usually end with a call for regulation — to ban said chemical or substance, or to regulate it — but in this case, that has already happened. This new carcinogen I’m telling you about is actually an old chemical. And it has not been manufactured or legally imported in the US since 2013.
So, why bother? Because in this case, the chemical — or, really, a group of chemicals called polybrominated diphenyl ethers (PBDEs) — are still around: in our soil, in our food, and in our blood.
PBDEs are a group of compounds that confer flame-retardant properties to plastics, and they were used extensively in the latter part of the 20th century in electronic enclosures, business equipment, and foam cushioning in upholstery.
But there was a problem. They don’t chemically bond to plastics; they are just sort of mixed in, which means they can leach out. They are hydrophobic, meaning they don’t get washed out of soil, and, when ingested or inhaled by humans, they dissolve in our fat stores, making it difficult for our normal excretory systems to excrete them.
PBDEs biomagnify. Small animals can take them up from contaminated soil or water, and those animals are eaten by larger animals, which accumulate higher concentrations of the chemicals. This bioaccumulation increases as you move up the food web until you get to an apex predator — like you and me.
This is true of lots of chemicals, of course. The concern arises when these chemicals are toxic. To date, the toxicity data for PBDEs were pretty limited. There were some animal studies where rats were exposed to extremely high doses and they developed liver lesions — but I am always very wary of extrapolating high-dose rat toxicity studies to humans. There was also some suggestion that the chemicals could be endocrine disruptors, affecting breast and thyroid tissue.
What about cancer? In 2016, the International Agency for Research on Cancer concluded there was “inadequate evidence in humans for the carcinogencity of” PBDEs.
In the same report, though, they suggested PBDEs are “probably carcinogenic to humans” based on mechanistic studies.
In other words, we can’t prove they’re cancerous — but come on, they probably are.
Finally, we have some evidence that really pushes us toward the carcinogenic conclusion, in the form of this study, appearing in JAMA Network Open. It’s a nice bit of epidemiology leveraging the population-based National Health and Nutrition Examination Survey (NHANES).
Researchers measured PBDE levels in blood samples from 1100 people enrolled in NHANES in 2003 and 2004 and linked them to death records collected over the next 20 years or so.
The first thing to note is that the researchers were able to measure PBDEs in the blood samples. They were in there. They were detectable. And they were variable. Dividing the 1100 participants into low, medium, and high PBDE tertiles, you can see a nearly 10-fold difference across the population.
Importantly, not many baseline variables correlated with PBDE levels. People in the highest group were a bit younger but had a fairly similar sex distribution, race, ethnicity, education, income, physical activity, smoking status, and body mass index.
This is not a randomized trial, of course — but at least based on these data, exposure levels do seem fairly random, which is what you would expect from an environmental toxin that percolates up through the food chain. They are often somewhat indiscriminate.
This similarity in baseline characteristics between people with low or high blood levels of PBDE also allows us to make some stronger inferences about the observed outcomes. Let’s take a look at them.
After adjustment for baseline factors, individuals in the highest PBDE group had a 43% higher rate of death from any cause over the follow-up period. This was not enough to achieve statistical significance, but it was close.
But the key finding is deaths due to cancer. After adjustment, cancer deaths occurred four times as frequently among those in the high PBDE group, and that is a statistically significant difference.
To be fair, cancer deaths were rare in this cohort. The vast majority of people did not die of anything during the follow-up period regardless of PBDE level. But the data are strongly suggestive of the carcinogenicity of these chemicals.
I should also point out that the researchers are linking the PBDE level at a single time point to all these future events. If PBDE levels remain relatively stable within an individual over time, that’s fine, but if they tend to vary with intake of different foods for example, this would not be captured and would actually lead to an underestimation of the cancer risk.
The researchers also didn’t have granular enough data to determine the type of cancer, but they do show that rates are similar between men and women, which might point away from the more sex-specific cancer etiologies. Clearly, some more work is needed.
Of course, I started this piece by telling you that these chemicals are already pretty much banned in the United States. What are we supposed to do about these findings? Studies have examined the primary ongoing sources of PBDE in our environment and it seems like most of our exposure will be coming from the food we eat due to that biomagnification thing: high-fat fish, meat and dairy products, and fish oil supplements. It may be worth some investigation into the relative adulteration of these products with this new old carcinogen.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
These types of stories usually end with a call for regulation — to ban said chemical or substance, or to regulate it — but in this case, that has already happened. This new carcinogen I’m telling you about is actually an old chemical. And it has not been manufactured or legally imported in the US since 2013.
So, why bother? Because in this case, the chemical — or, really, a group of chemicals called polybrominated diphenyl ethers (PBDEs) — are still around: in our soil, in our food, and in our blood.
PBDEs are a group of compounds that confer flame-retardant properties to plastics, and they were used extensively in the latter part of the 20th century in electronic enclosures, business equipment, and foam cushioning in upholstery.
But there was a problem. They don’t chemically bond to plastics; they are just sort of mixed in, which means they can leach out. They are hydrophobic, meaning they don’t get washed out of soil, and, when ingested or inhaled by humans, they dissolve in our fat stores, making it difficult for our normal excretory systems to excrete them.
PBDEs biomagnify. Small animals can take them up from contaminated soil or water, and those animals are eaten by larger animals, which accumulate higher concentrations of the chemicals. This bioaccumulation increases as you move up the food web until you get to an apex predator — like you and me.
This is true of lots of chemicals, of course. The concern arises when these chemicals are toxic. To date, the toxicity data for PBDEs were pretty limited. There were some animal studies where rats were exposed to extremely high doses and they developed liver lesions — but I am always very wary of extrapolating high-dose rat toxicity studies to humans. There was also some suggestion that the chemicals could be endocrine disruptors, affecting breast and thyroid tissue.
What about cancer? In 2016, the International Agency for Research on Cancer concluded there was “inadequate evidence in humans for the carcinogencity of” PBDEs.
In the same report, though, they suggested PBDEs are “probably carcinogenic to humans” based on mechanistic studies.
In other words, we can’t prove they’re cancerous — but come on, they probably are.
Finally, we have some evidence that really pushes us toward the carcinogenic conclusion, in the form of this study, appearing in JAMA Network Open. It’s a nice bit of epidemiology leveraging the population-based National Health and Nutrition Examination Survey (NHANES).
Researchers measured PBDE levels in blood samples from 1100 people enrolled in NHANES in 2003 and 2004 and linked them to death records collected over the next 20 years or so.
The first thing to note is that the researchers were able to measure PBDEs in the blood samples. They were in there. They were detectable. And they were variable. Dividing the 1100 participants into low, medium, and high PBDE tertiles, you can see a nearly 10-fold difference across the population.
Importantly, not many baseline variables correlated with PBDE levels. People in the highest group were a bit younger but had a fairly similar sex distribution, race, ethnicity, education, income, physical activity, smoking status, and body mass index.
This is not a randomized trial, of course — but at least based on these data, exposure levels do seem fairly random, which is what you would expect from an environmental toxin that percolates up through the food chain. They are often somewhat indiscriminate.
This similarity in baseline characteristics between people with low or high blood levels of PBDE also allows us to make some stronger inferences about the observed outcomes. Let’s take a look at them.
After adjustment for baseline factors, individuals in the highest PBDE group had a 43% higher rate of death from any cause over the follow-up period. This was not enough to achieve statistical significance, but it was close.
But the key finding is deaths due to cancer. After adjustment, cancer deaths occurred four times as frequently among those in the high PBDE group, and that is a statistically significant difference.
To be fair, cancer deaths were rare in this cohort. The vast majority of people did not die of anything during the follow-up period regardless of PBDE level. But the data are strongly suggestive of the carcinogenicity of these chemicals.
I should also point out that the researchers are linking the PBDE level at a single time point to all these future events. If PBDE levels remain relatively stable within an individual over time, that’s fine, but if they tend to vary with intake of different foods for example, this would not be captured and would actually lead to an underestimation of the cancer risk.
The researchers also didn’t have granular enough data to determine the type of cancer, but they do show that rates are similar between men and women, which might point away from the more sex-specific cancer etiologies. Clearly, some more work is needed.
Of course, I started this piece by telling you that these chemicals are already pretty much banned in the United States. What are we supposed to do about these findings? Studies have examined the primary ongoing sources of PBDE in our environment and it seems like most of our exposure will be coming from the food we eat due to that biomagnification thing: high-fat fish, meat and dairy products, and fish oil supplements. It may be worth some investigation into the relative adulteration of these products with this new old carcinogen.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
These types of stories usually end with a call for regulation — to ban said chemical or substance, or to regulate it — but in this case, that has already happened. This new carcinogen I’m telling you about is actually an old chemical. And it has not been manufactured or legally imported in the US since 2013.
So, why bother? Because in this case, the chemical — or, really, a group of chemicals called polybrominated diphenyl ethers (PBDEs) — are still around: in our soil, in our food, and in our blood.
PBDEs are a group of compounds that confer flame-retardant properties to plastics, and they were used extensively in the latter part of the 20th century in electronic enclosures, business equipment, and foam cushioning in upholstery.
But there was a problem. They don’t chemically bond to plastics; they are just sort of mixed in, which means they can leach out. They are hydrophobic, meaning they don’t get washed out of soil, and, when ingested or inhaled by humans, they dissolve in our fat stores, making it difficult for our normal excretory systems to excrete them.
PBDEs biomagnify. Small animals can take them up from contaminated soil or water, and those animals are eaten by larger animals, which accumulate higher concentrations of the chemicals. This bioaccumulation increases as you move up the food web until you get to an apex predator — like you and me.
This is true of lots of chemicals, of course. The concern arises when these chemicals are toxic. To date, the toxicity data for PBDEs were pretty limited. There were some animal studies where rats were exposed to extremely high doses and they developed liver lesions — but I am always very wary of extrapolating high-dose rat toxicity studies to humans. There was also some suggestion that the chemicals could be endocrine disruptors, affecting breast and thyroid tissue.
What about cancer? In 2016, the International Agency for Research on Cancer concluded there was “inadequate evidence in humans for the carcinogencity of” PBDEs.
In the same report, though, they suggested PBDEs are “probably carcinogenic to humans” based on mechanistic studies.
In other words, we can’t prove they’re cancerous — but come on, they probably are.
Finally, we have some evidence that really pushes us toward the carcinogenic conclusion, in the form of this study, appearing in JAMA Network Open. It’s a nice bit of epidemiology leveraging the population-based National Health and Nutrition Examination Survey (NHANES).
Researchers measured PBDE levels in blood samples from 1100 people enrolled in NHANES in 2003 and 2004 and linked them to death records collected over the next 20 years or so.
The first thing to note is that the researchers were able to measure PBDEs in the blood samples. They were in there. They were detectable. And they were variable. Dividing the 1100 participants into low, medium, and high PBDE tertiles, you can see a nearly 10-fold difference across the population.
Importantly, not many baseline variables correlated with PBDE levels. People in the highest group were a bit younger but had a fairly similar sex distribution, race, ethnicity, education, income, physical activity, smoking status, and body mass index.
This is not a randomized trial, of course — but at least based on these data, exposure levels do seem fairly random, which is what you would expect from an environmental toxin that percolates up through the food chain. They are often somewhat indiscriminate.
This similarity in baseline characteristics between people with low or high blood levels of PBDE also allows us to make some stronger inferences about the observed outcomes. Let’s take a look at them.
After adjustment for baseline factors, individuals in the highest PBDE group had a 43% higher rate of death from any cause over the follow-up period. This was not enough to achieve statistical significance, but it was close.
But the key finding is deaths due to cancer. After adjustment, cancer deaths occurred four times as frequently among those in the high PBDE group, and that is a statistically significant difference.
To be fair, cancer deaths were rare in this cohort. The vast majority of people did not die of anything during the follow-up period regardless of PBDE level. But the data are strongly suggestive of the carcinogenicity of these chemicals.
I should also point out that the researchers are linking the PBDE level at a single time point to all these future events. If PBDE levels remain relatively stable within an individual over time, that’s fine, but if they tend to vary with intake of different foods for example, this would not be captured and would actually lead to an underestimation of the cancer risk.
The researchers also didn’t have granular enough data to determine the type of cancer, but they do show that rates are similar between men and women, which might point away from the more sex-specific cancer etiologies. Clearly, some more work is needed.
Of course, I started this piece by telling you that these chemicals are already pretty much banned in the United States. What are we supposed to do about these findings? Studies have examined the primary ongoing sources of PBDE in our environment and it seems like most of our exposure will be coming from the food we eat due to that biomagnification thing: high-fat fish, meat and dairy products, and fish oil supplements. It may be worth some investigation into the relative adulteration of these products with this new old carcinogen.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
When Does a Disease Become Its Own Specialty?
Once upon a time, treating multiple sclerosis (MS) was easy — steroids.
Then, in the 1990s, came Betaseron, then Avonex, then Copaxone. Suddenly we had three options to choose from, though overall roughly similar in efficacy (yeah, I’m leaving Novantrone out; it’s a niche drug). Treatment required some decision making, though not a huge amount. I usually laid out the different schedules and side effect to patients and let them decide.
MS treatment was uncomplicated enough that I knew family doctors who treated MS patients on their own, and I can’t say I could have done any better. If you’ve got a clear MRI, then prescribe Betaseron and hope.
Then came Rebif, then Tysabri, and then pretty much an explosion of new drugs which hasn’t slowed down. Next up are the BTK agents. An embarrassment of riches, though for patients, their families, and neurologists, a very welcome one.
But as more drugs come out, with different mechanisms of action and monitoring requirements, the treatment of MS becomes more complicated, slowly moving from the realm of a general neurologist to an MS subspecialist.
At some point it raises the question of when does a disease become its own specialty? Perhaps this is a bit of hyperbole — I’m pretty sure I’ll be seeing MS patients for a long time to come — but it’s a valid point. Especially as further research may subdivide MS treatment by genetics and other breakdowns.
Alzheimer’s disease may follow a similar (albeit very welcome) trajectory. While nothing really game-changing has come out in the 20 years, the number of new drugs and different mechanisms of action in development is large. Granted, not all of them will work, but hopefully some will. At some point it may come down to treating patients with a cocktail of drugs with separate ways of managing the disease, with guidance based on genetic or clinical profiles.
And that’s a good thing, but it may, again, move the disease from the province of general neurologists to subspecialists. Maybe that would be a good, maybe not. Probably will depend on the patient, their families, and other factors.
Of course, I may be overthinking this. The number of drugs we have for MS is nothing compared with the available treatments we have for hypertension, yet it’s certainly well within the capabilities of most internists to treat without referring to a cardiologist or nephrologist.
Perhaps the new drugs won’t make a difference except in a handful of cases. As new drugs come out we also move on from the old ones, dropping them from our mental armamentarium except in rare cases. When was the last time you prescribed Betaseron?
These drugs are very welcome, and very needed. I will be happy if we can beat back some of the diseases neurologist see, regardless of whom the patients and up seeing.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Once upon a time, treating multiple sclerosis (MS) was easy — steroids.
Then, in the 1990s, came Betaseron, then Avonex, then Copaxone. Suddenly we had three options to choose from, though overall roughly similar in efficacy (yeah, I’m leaving Novantrone out; it’s a niche drug). Treatment required some decision making, though not a huge amount. I usually laid out the different schedules and side effect to patients and let them decide.
MS treatment was uncomplicated enough that I knew family doctors who treated MS patients on their own, and I can’t say I could have done any better. If you’ve got a clear MRI, then prescribe Betaseron and hope.
Then came Rebif, then Tysabri, and then pretty much an explosion of new drugs which hasn’t slowed down. Next up are the BTK agents. An embarrassment of riches, though for patients, their families, and neurologists, a very welcome one.
But as more drugs come out, with different mechanisms of action and monitoring requirements, the treatment of MS becomes more complicated, slowly moving from the realm of a general neurologist to an MS subspecialist.
At some point it raises the question of when does a disease become its own specialty? Perhaps this is a bit of hyperbole — I’m pretty sure I’ll be seeing MS patients for a long time to come — but it’s a valid point. Especially as further research may subdivide MS treatment by genetics and other breakdowns.
Alzheimer’s disease may follow a similar (albeit very welcome) trajectory. While nothing really game-changing has come out in the 20 years, the number of new drugs and different mechanisms of action in development is large. Granted, not all of them will work, but hopefully some will. At some point it may come down to treating patients with a cocktail of drugs with separate ways of managing the disease, with guidance based on genetic or clinical profiles.
And that’s a good thing, but it may, again, move the disease from the province of general neurologists to subspecialists. Maybe that would be a good, maybe not. Probably will depend on the patient, their families, and other factors.
Of course, I may be overthinking this. The number of drugs we have for MS is nothing compared with the available treatments we have for hypertension, yet it’s certainly well within the capabilities of most internists to treat without referring to a cardiologist or nephrologist.
Perhaps the new drugs won’t make a difference except in a handful of cases. As new drugs come out we also move on from the old ones, dropping them from our mental armamentarium except in rare cases. When was the last time you prescribed Betaseron?
These drugs are very welcome, and very needed. I will be happy if we can beat back some of the diseases neurologist see, regardless of whom the patients and up seeing.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Once upon a time, treating multiple sclerosis (MS) was easy — steroids.
Then, in the 1990s, came Betaseron, then Avonex, then Copaxone. Suddenly we had three options to choose from, though overall roughly similar in efficacy (yeah, I’m leaving Novantrone out; it’s a niche drug). Treatment required some decision making, though not a huge amount. I usually laid out the different schedules and side effect to patients and let them decide.
MS treatment was uncomplicated enough that I knew family doctors who treated MS patients on their own, and I can’t say I could have done any better. If you’ve got a clear MRI, then prescribe Betaseron and hope.
Then came Rebif, then Tysabri, and then pretty much an explosion of new drugs which hasn’t slowed down. Next up are the BTK agents. An embarrassment of riches, though for patients, their families, and neurologists, a very welcome one.
But as more drugs come out, with different mechanisms of action and monitoring requirements, the treatment of MS becomes more complicated, slowly moving from the realm of a general neurologist to an MS subspecialist.
At some point it raises the question of when does a disease become its own specialty? Perhaps this is a bit of hyperbole — I’m pretty sure I’ll be seeing MS patients for a long time to come — but it’s a valid point. Especially as further research may subdivide MS treatment by genetics and other breakdowns.
Alzheimer’s disease may follow a similar (albeit very welcome) trajectory. While nothing really game-changing has come out in the 20 years, the number of new drugs and different mechanisms of action in development is large. Granted, not all of them will work, but hopefully some will. At some point it may come down to treating patients with a cocktail of drugs with separate ways of managing the disease, with guidance based on genetic or clinical profiles.
And that’s a good thing, but it may, again, move the disease from the province of general neurologists to subspecialists. Maybe that would be a good, maybe not. Probably will depend on the patient, their families, and other factors.
Of course, I may be overthinking this. The number of drugs we have for MS is nothing compared with the available treatments we have for hypertension, yet it’s certainly well within the capabilities of most internists to treat without referring to a cardiologist or nephrologist.
Perhaps the new drugs won’t make a difference except in a handful of cases. As new drugs come out we also move on from the old ones, dropping them from our mental armamentarium except in rare cases. When was the last time you prescribed Betaseron?
These drugs are very welcome, and very needed. I will be happy if we can beat back some of the diseases neurologist see, regardless of whom the patients and up seeing.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Congratulations to AGA’s New Leaders
Each January, the AGA Nominating Committee meets to complete a very important task — namely, selection of new members of AGA’s Governing Board, pending approval by the membership.
Having served on this committee in the past, I can attest to how challenging a task it is to select these leaders from such a talented and committed pool of candidates, each of whom have served the organization in numerous impactful roles over the course of many years.
This year’s recently announced additions to the Governing Board, who will assume their roles this summer, include Dr. Byron Cryer (incoming Vice President), Dr. Shahnaz Sultan (Clinical Research Councillor), and Dr. Jonathan Rosenberg (Practice Councillor). I have had the pleasure of working with each of them over the years from my very early days at AGA and am confident that AGA will continue to thrive under their leadership. Please join me in congratulating Byron, Shahnaz, and Jonathan on their new roles!
In this month’s issue of GIHN, we highlight a phase 3 RCT from NEJM demonstrating the efficacy of seladelpar, an alternative to ursodeoxycholic acid in patients with PBC with refractory pruritus. From the CGH Practice Management section, Dr. Michelle Kim (Cleveland Clinic) and colleagues provide helpful tips on how to optimize EHR use in GI practice, including by incorporating novel tools based on AI, natural language processing, and speech recognition. In our April Member Spotlight, we are excited to feature gastroenterologist and stand-up comedienne Dr. Shida Haghighat of UCLA, who shares her passion for addressing health disparities and highlights how humor helped her cope with the demands of medical training. We hope you enjoy these, and all the stories included in our April issue.
Megan A. Adams, MD, JD, MSc
Editor-in-Chief
Each January, the AGA Nominating Committee meets to complete a very important task — namely, selection of new members of AGA’s Governing Board, pending approval by the membership.
Having served on this committee in the past, I can attest to how challenging a task it is to select these leaders from such a talented and committed pool of candidates, each of whom have served the organization in numerous impactful roles over the course of many years.
This year’s recently announced additions to the Governing Board, who will assume their roles this summer, include Dr. Byron Cryer (incoming Vice President), Dr. Shahnaz Sultan (Clinical Research Councillor), and Dr. Jonathan Rosenberg (Practice Councillor). I have had the pleasure of working with each of them over the years from my very early days at AGA and am confident that AGA will continue to thrive under their leadership. Please join me in congratulating Byron, Shahnaz, and Jonathan on their new roles!
In this month’s issue of GIHN, we highlight a phase 3 RCT from NEJM demonstrating the efficacy of seladelpar, an alternative to ursodeoxycholic acid in patients with PBC with refractory pruritus. From the CGH Practice Management section, Dr. Michelle Kim (Cleveland Clinic) and colleagues provide helpful tips on how to optimize EHR use in GI practice, including by incorporating novel tools based on AI, natural language processing, and speech recognition. In our April Member Spotlight, we are excited to feature gastroenterologist and stand-up comedienne Dr. Shida Haghighat of UCLA, who shares her passion for addressing health disparities and highlights how humor helped her cope with the demands of medical training. We hope you enjoy these, and all the stories included in our April issue.
Megan A. Adams, MD, JD, MSc
Editor-in-Chief
Each January, the AGA Nominating Committee meets to complete a very important task — namely, selection of new members of AGA’s Governing Board, pending approval by the membership.
Having served on this committee in the past, I can attest to how challenging a task it is to select these leaders from such a talented and committed pool of candidates, each of whom have served the organization in numerous impactful roles over the course of many years.
This year’s recently announced additions to the Governing Board, who will assume their roles this summer, include Dr. Byron Cryer (incoming Vice President), Dr. Shahnaz Sultan (Clinical Research Councillor), and Dr. Jonathan Rosenberg (Practice Councillor). I have had the pleasure of working with each of them over the years from my very early days at AGA and am confident that AGA will continue to thrive under their leadership. Please join me in congratulating Byron, Shahnaz, and Jonathan on their new roles!
In this month’s issue of GIHN, we highlight a phase 3 RCT from NEJM demonstrating the efficacy of seladelpar, an alternative to ursodeoxycholic acid in patients with PBC with refractory pruritus. From the CGH Practice Management section, Dr. Michelle Kim (Cleveland Clinic) and colleagues provide helpful tips on how to optimize EHR use in GI practice, including by incorporating novel tools based on AI, natural language processing, and speech recognition. In our April Member Spotlight, we are excited to feature gastroenterologist and stand-up comedienne Dr. Shida Haghighat of UCLA, who shares her passion for addressing health disparities and highlights how humor helped her cope with the demands of medical training. We hope you enjoy these, and all the stories included in our April issue.
Megan A. Adams, MD, JD, MSc
Editor-in-Chief
Ultrasound and Its Role In Diagnosing and Managing Endometriosis
Introduction: Imaging for Endometriosis — A Necessary Prerequisite
While the gold standard in the diagnosis of endometriosis remains laparoscopy, it is now recognized that thorough evaluation via ultrasound offers an acceptable, less expensive, and less invasive alternative. It is especially useful for the diagnosis of deep infiltrative disease, which penetrates more than 5 mm into the peritoneum, ovarian endometrioma, and when anatomic distortion occurs, such as to the path of the ureter.
Besides establishing the diagnosis, ultrasound imaging has become, along with MRI, the most important aid for proper preoperative planning. Not only does imaging provide the surgeon and patient with knowledge regarding the extent of the upcoming procedure, but it also allows the minimally invasive gynecologic (MIG) surgeon to involve colleagues, such as colorectal surgeons or urologists. For example, deep infiltrative endometriosis penetrating into the bowel mucosa will require a discoid or segmental bowel resection.
While many endometriosis experts rely on MRI, many MIG surgeons are dependent on ultrasound. I would not consider taking a patient with signs and symptoms suggestive of endometriosis to surgery without 2D/3D transvaginal ultrasound. If the patient possesses a uterus, a saline-infused sonogram is performed to potentially diagnose adenomyosis.
It is a pleasure and honor to welcome Professor Caterina Exacoustos MD, PhD, associate professor of ob.gyn. at the University of Rome “Tor Vergata,” to this edition of the Master Class in Gynecologic Surgery to discuss “Ultrasound and Its Role in the Diagnosis of and Management of Endometriosis, Including DIE.”
Prof. Exacoustos’ main areas of interest are endometriosis and benign diseases including uterine pathology and infertility. Her extensive body of work comprises over 120 scientific publications and numerous book chapters both in English and in Italian.
Prof. Exacoustos continues to be one of the most well respected lecturers speaking about ultrasound throughout the world.
Dr. Miller is professor of obstetrics and gynecology, department of clinical sciences, Rosalind Franklin University of Medicine and Science, North Chicago. Dr. Miller has no conflicts of interest to report.
Ultrasound and Its Role In Diagnosing and Managing Endometriosis
Endometriosis affects approximately 10%-20% of premenopausal women worldwide. It is the leading cause of chronic pelvic pain, is often associated with infertility, and has a significant impact on quality of life. Although the natural history of endometriosis remains unknown, emerging evidence suggests that the pathophysiological steps of initiation and development of endometriosis must occur earlier in the lifespan. Most notably, the onset of endometriosis-associated pain symptoms is often reported during adolescence and young adulthood.1
While many patients with endometriosis are referred with dysmenorrhea at a young age, at age ≤ 25 years,2 symptoms are often highly underestimated and considered to be normal and transient.3,4 Clinical and pelvic exams are often negative in young women, and delays in endometriosis diagnosis are well known.
The presentation of primary dysmenorrhea with no anatomical cause embodies the paradigm that dysmenorrhea in adolescents is most often an insignificant disorder. This perspective is probably a root cause of delayed endometriosis diagnosis in young patients. However, another issue behind delayed diagnosis is the reluctance of the physician to perform a diagnostic laparoscopy — historically the gold standard for diagnosing endometriosis — for seemingly common symptoms such as dysmenorrhea in young patients.
Today we know that there are typical aspects of ultrasound imaging that identify endometriosis in the pelvis, and notably, the 2022 European Society for Human Reproduction and Embryology (ESHRE) endometriosis guideline5 recognizes imaging (ultrasound or MRI) as the standard for endometriosis diagnosis without requiring laparoscopic or histological confirmation.
An early and noninvasive method of diagnosis aids in timely diagnosis and provides for the timely initiation of medical management to improve quality of life and prevent progression of disease (Figure 1).
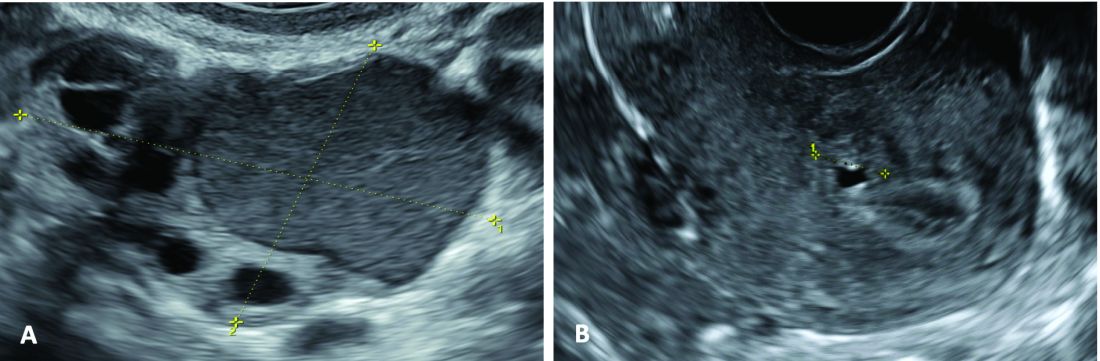
(A. Transvaginal ultrasound appearance of a small ovarian endometrioma in a 16-year-old girl. Note the unilocular cyst with ground glass echogenicity surrounded by multifollicular ovarian tissue. B. Ultrasound image of a retroverted uterus of an 18-year-old girl with focal adenomyosis of the posterior wall. Note the round cystic anechoic areas in the inner myometrium or junctional zone. The small intra-myometrial cyst is surrounded by a hyperechoic ring).
Indeed, the typical appearance of endometriotic pelvic lesions on transvaginal sonography, such as endometriomas and rectal deep infiltrating endometriosis (DIE) — as well as adenomyosis – can be medically treated without histologic confirmation .
When surgery is advisable, ultrasound findings also play a valuable role in presurgical staging, planning, and counseling for patients of all ages. Determining the extent and location of DIE preoperatively, for instance, facilitates the engagement of the appropriate surgical specialists so that multiple surgeries can be avoided. It also enables patients to be optimally informed before surgery of possible outcomes and complications.
Moreover, in the context of infertility, ultrasound can be a valuable tool for understanding uterine pathology and assessing for adenomyosis so that affected patients may be treated surgically or medically before turning to assisted reproductive technology.
Uniformity, Standardization in the Sonographic Assessment
In Europe, as in the United States, transvaginal sonography (TVS) is the first-line imaging tool for the diagnosis and management of endometriosis. In Europe, many ob.gyns. perform ultrasound themselves, as do treating surgeons. When diagnostic findings are negative but clinical suspicion is high, MRI is often utilized. Laparoscopy may then be considered in patients with negative imaging results.
Efforts to standardize terms, definitions, measurements, and sonographic features of different types of endometriosis have been made to make it easier for physicians to share data and communicate with each other. A lack of uniformity has contributed to variability in the reported diagnostic accuracy of TVS.
About 10 years ago, in one such effort, we assessed the accuracy of TVS for DIE by comparing TVS results with laparoscopic/histologic findings, and developed an ultrasound mapping system to accurately record the location, size and depth of lesions visualized by TVS. The accuracy of TVS ranged from 76% for the diagnosis of vaginal endometriosis to 97% for the diagnosis of bladder lesions and posterior cul-de-sac obliteration. Accuracy was 93% and 91% for detecting ureteral involvement (right and left); 87% for uterosacral ligament endometriotic lesions; and 87% for parametrial involvement.6
Shortly after, with a focus on DIE, expert sonographers and physician-sonographers from across Europe — as well as some experts from Australia, Japan, Brazil, Chile, and the United States (Y. Osuga from Brigham and Women’s Hospital and Harvard Medical School) — came together to agree on a uniform approach to the sonographic evaluation for suspected endometriosis and a standardization of terminology.
The consensus opinion from the International Deep Endometriosis Analysis (IDEA) group details four steps for examining women with suspected DIE: 1) Evaluation of the uterus and adnexa, 2) evaluation of transvaginal sonographic “soft markers” (ie. site-specific tenderness and ovarian mobility), 3) assessment of the status of the posterior cul-de-sac using real-time ultrasound-based “sliding sign,” and 4) assessment for DIE nodules in the anterior and posterior compartments.7
Our paper describing a mapping system and the IDEA paper describe how to detect deep endometriosis in the pelvis by utilizing an ultrasound view of normal anatomy and pelvic organ structure to provide landmarks for accurately defining the site of DIE lesions (Figure 2).
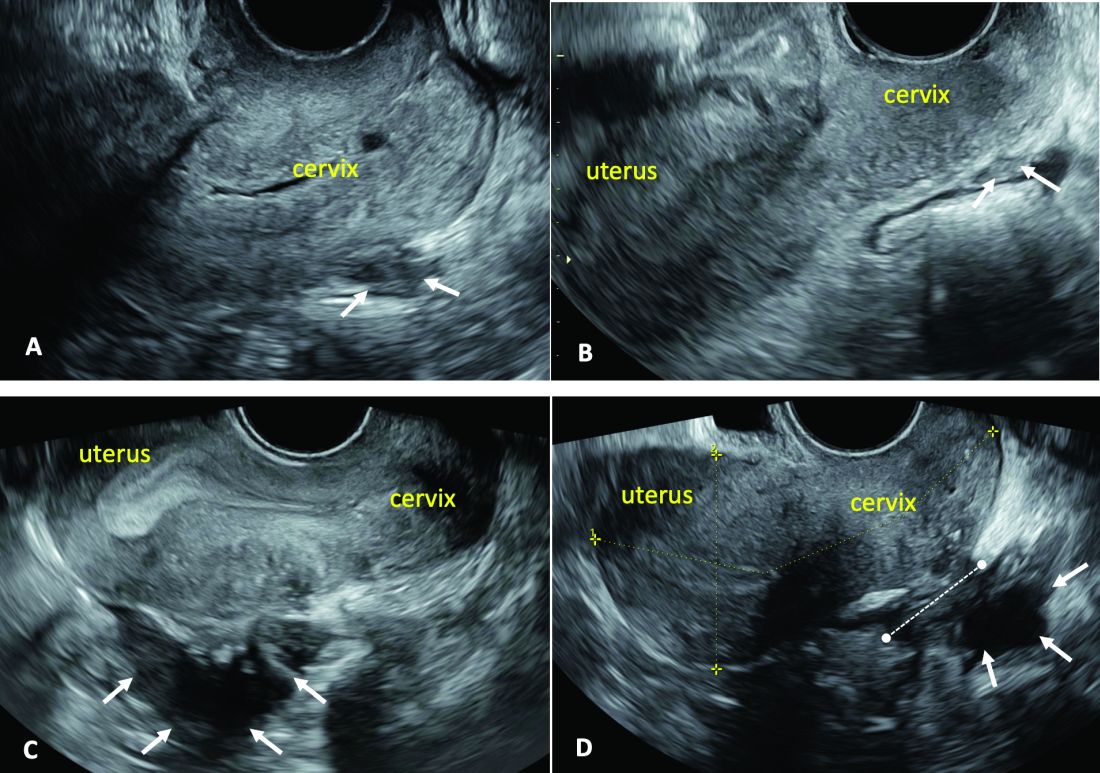
(A. Ultrasound appearance of a small DIE lesion of the retrocervical area [white arrows], which involved the torus uterinum and the right uterosacral ligament [USL]. The lesion appears as hypoechoic tissue with irregular margins caused by the fibrosis induced by the DIE. B. TVS appearance of small nodules of DIE of the left USL. Note the small retrocervical DIE lesion [white arrows], which appears hypoechoic due to the infiltration of the hyperechoic USL. C) Ultrasound appearance of a DIE nodule of the recto-sigmoid wall. Note the hypoechoic thickening of the muscular layers of the bowel wall attached to the corpus of the uterus and the adenomyosis of the posterior wall. The retrocervical area is free. D. TVS appearance of nodules of DIE of the lower rectal wall. Note the hypoechoic lesion [white arrows] of the rectum is attached to a retrocervical DIE fibrosis of the torus and USL [white dotted line]).
So-called rectovaginal endometriosis can be well assessed, for instance, since the involvement of the rectum, sigmoid colon, vaginal wall, rectovaginal septum, and posterior cul-de-sac uterosacral ligament can be seen by ultrasound as a single structure, making the location, size, and depth of any lesions discernible.
Again, this evaluation of the extent of disease is important for presurgical assessment so the surgeon can organize the right team and time of surgery and so the patient can be counseled on the advantages and possible complications of the treatment.
Notably, an accurate ultrasound description of pelvic endometriosis is helpful for accurate classification of disease. Endometriosis classification systems such as that of the American Association of Gynecologic Laparoscopists (AAGL)8 and the American Society of Reproductive Medicine (ASRM),9 as well as the #Enzian surgical description system,10 have been adapted to cover findings from ultrasound as well as MRI imaging.
A Systematic Evaluation
In keeping with the IDEA consensus opinion and based on our years of experience at the University of Rome, I advise that patients with typical pain symptoms of endometriosis or infertility undergo an accurate sonographic assessment of the pelvis with particular evaluation not only of the uterus and ovaries but of all pelvic retroperitoneal spaces.
The TVS examination should start with a slightly filled bladder, which permits a better evaluation of the bladder walls and the presence of endometriotic nodules. These nodules appear as hyperechoic linear or spherical lesions bulging toward the lumen and involving the serosa, muscularis, or (sub)mucosa of the bladder.
Then, an accurate evaluation of the uterus in 2D and 3D permits the diagnosis of adenomyosis. 3D sonographic evaluation of the myometrium and of the junctional zone are important; alteration and infiltration of the junctional zone and the presence of small adenomyotic cysts in the inner or outer myometrium are direct, specific signs of adenomyosis and should be ruled out in patients with dysmenorrhea, heavy menstrual bleeding, infertility, and pregnancy complications.
Endometriomas of the ovaries can be easily detected as having the typical appearance of a cyst with ground glass content. Adhesions of the ovaries and the uterus also should be evaluated with a dynamic ultrasound approach that utilizes the sliding sign and mobilization by palpation of the organs during the TVS scan.
Finally, the posterior and lateral retroperitoneal compartments should be carefully evaluated, with symptoms guiding the TVS examination whenever possible. Deep endometriotic nodules of the rectum appear as hypoechoic lesions or linear or nodular retroperitoneal thickening with irregular borders, penetrating into the intestinal wall and distorting its normal structure. In young patients, it seems very important to assess for small lesions below the peritoneum between the vagina and rectum, and in the parametria and around the ureter and nerves — lesions that, notably, would not be seen by diagnostic laparoscopy.
The Evaluation of Young Patients
In adolescent and young patients, endometriosis and adenomyosis are often present with small lesions and shallow tissue invasion, making a very careful and experienced approach to ultrasound essential for detection. Endometriomas are often of small diameter, and DIE is not always easily diagnosed because retroperitoneal lesions are similarly very small.
In a series of 270 adolescents (ages 12-20) who were referred to our outpatient gynecologic ultrasound unit over a 5-year period for various indications, at least one ultrasound feature of endometriosis was observed in 13.3%. In those with dysmenorrhea, the detection of endometriosis increased to 21%. Endometrioma was the most common type of endometriosis we found in the study, but DIE and adenomyosis were found in 4%-11%.
Although endometriotic lesions typically are small in young patients, they are often associated with severe pain symptoms, including chronic pelvic pain, dysmenorrhea, dyspareunia, dysuria, and dyschezia, all of which can have a serious effect on the quality of life of these young women. These symptoms keep them away from school during menstruation, away from sports, and cause painful intercourse and infertility. In young patients, an accurate TVS can provide a lot of information, and the ability to detect retroperitoneal endometriotic lesions and adenomyosis is probably better than with purely diagnostic laparoscopy, which would evaluate only superficial lesions.
TVS or, when needed, transrectal ultrasound, can enable adequate treatment and follow-up of the disease and its symptoms. There are no guidelines recommending adequate follow-up times to evaluate the effectiveness of medical therapy in patients with ultrasound signs of endometriosis. (Likewise, there are no indications for follow-up in patients with severe dysmenorrhea without ultrasound signs of endometriosis.) Certainly, our studies suggest careful evaluation over time of young patients with severe dysmenorrhea by serial ultrasound scans. With such follow-up, disease progress can be monitored and the medical or surgical treatment approach modified if needed.
The diagnosis of endometriosis at a young age has significant benefits not only in avoiding or reducing progression of the disease, but also in improving quality of life and aiding women in their desire for pregnancy.
Dr. Exacoustos is associate professor of ob.gyn. at the University of Rome “Tor Vergata.” She has no conflicts of interest to report.
References
1. Zondervan KT et al. N Engl J Med. 2020;382:1244-56.
2. Greene R et al. Fertil Steril. 2009;91:32-9.
3. Chapron C et al. J Pediatr Adolesc Gynecol. 2011;24:S7-12.
4. Randhawa AE et al. J Pediatr Adolesc Gynecol. 2021;34:643-8.
5. Becker CM et al. Hum Reprod Open. 2022(2):hoac009.
6. Exacoustos C et al. Fertil Steril. 2014;102:143-9. 7. Guerriero S et al. Ultrasound Obstet Gynecol. 2016;48(3):318-32.
8. Abrao MS et al. J Minim Invasive Gynecol. 2021;28:1941-50.9. Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril. 1997;67:817-21. 10. Keckstein J et al. Acta Obstet Gynecol Scand. 2021;100:1165-75.
11. Martire FG et al. Fertil Steril. 2020;114(5):1049-57.
Introduction: Imaging for Endometriosis — A Necessary Prerequisite
While the gold standard in the diagnosis of endometriosis remains laparoscopy, it is now recognized that thorough evaluation via ultrasound offers an acceptable, less expensive, and less invasive alternative. It is especially useful for the diagnosis of deep infiltrative disease, which penetrates more than 5 mm into the peritoneum, ovarian endometrioma, and when anatomic distortion occurs, such as to the path of the ureter.
Besides establishing the diagnosis, ultrasound imaging has become, along with MRI, the most important aid for proper preoperative planning. Not only does imaging provide the surgeon and patient with knowledge regarding the extent of the upcoming procedure, but it also allows the minimally invasive gynecologic (MIG) surgeon to involve colleagues, such as colorectal surgeons or urologists. For example, deep infiltrative endometriosis penetrating into the bowel mucosa will require a discoid or segmental bowel resection.
While many endometriosis experts rely on MRI, many MIG surgeons are dependent on ultrasound. I would not consider taking a patient with signs and symptoms suggestive of endometriosis to surgery without 2D/3D transvaginal ultrasound. If the patient possesses a uterus, a saline-infused sonogram is performed to potentially diagnose adenomyosis.
It is a pleasure and honor to welcome Professor Caterina Exacoustos MD, PhD, associate professor of ob.gyn. at the University of Rome “Tor Vergata,” to this edition of the Master Class in Gynecologic Surgery to discuss “Ultrasound and Its Role in the Diagnosis of and Management of Endometriosis, Including DIE.”
Prof. Exacoustos’ main areas of interest are endometriosis and benign diseases including uterine pathology and infertility. Her extensive body of work comprises over 120 scientific publications and numerous book chapters both in English and in Italian.
Prof. Exacoustos continues to be one of the most well respected lecturers speaking about ultrasound throughout the world.
Dr. Miller is professor of obstetrics and gynecology, department of clinical sciences, Rosalind Franklin University of Medicine and Science, North Chicago. Dr. Miller has no conflicts of interest to report.
Ultrasound and Its Role In Diagnosing and Managing Endometriosis
Endometriosis affects approximately 10%-20% of premenopausal women worldwide. It is the leading cause of chronic pelvic pain, is often associated with infertility, and has a significant impact on quality of life. Although the natural history of endometriosis remains unknown, emerging evidence suggests that the pathophysiological steps of initiation and development of endometriosis must occur earlier in the lifespan. Most notably, the onset of endometriosis-associated pain symptoms is often reported during adolescence and young adulthood.1
While many patients with endometriosis are referred with dysmenorrhea at a young age, at age ≤ 25 years,2 symptoms are often highly underestimated and considered to be normal and transient.3,4 Clinical and pelvic exams are often negative in young women, and delays in endometriosis diagnosis are well known.
The presentation of primary dysmenorrhea with no anatomical cause embodies the paradigm that dysmenorrhea in adolescents is most often an insignificant disorder. This perspective is probably a root cause of delayed endometriosis diagnosis in young patients. However, another issue behind delayed diagnosis is the reluctance of the physician to perform a diagnostic laparoscopy — historically the gold standard for diagnosing endometriosis — for seemingly common symptoms such as dysmenorrhea in young patients.
Today we know that there are typical aspects of ultrasound imaging that identify endometriosis in the pelvis, and notably, the 2022 European Society for Human Reproduction and Embryology (ESHRE) endometriosis guideline5 recognizes imaging (ultrasound or MRI) as the standard for endometriosis diagnosis without requiring laparoscopic or histological confirmation.
An early and noninvasive method of diagnosis aids in timely diagnosis and provides for the timely initiation of medical management to improve quality of life and prevent progression of disease (Figure 1).
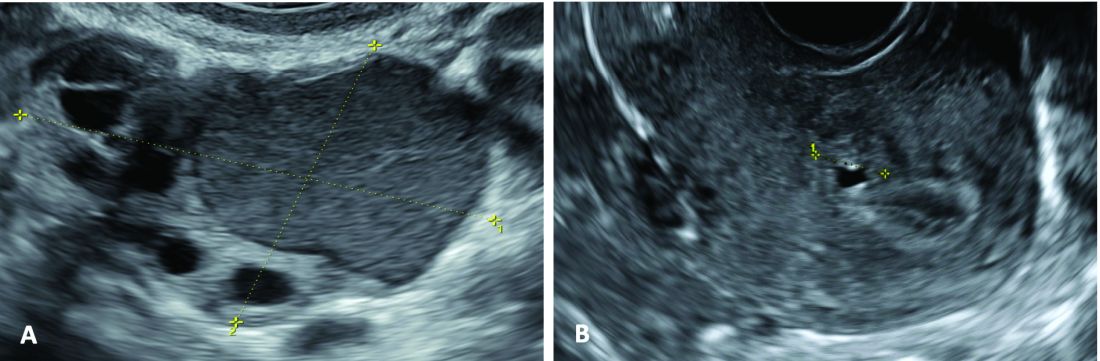
(A. Transvaginal ultrasound appearance of a small ovarian endometrioma in a 16-year-old girl. Note the unilocular cyst with ground glass echogenicity surrounded by multifollicular ovarian tissue. B. Ultrasound image of a retroverted uterus of an 18-year-old girl with focal adenomyosis of the posterior wall. Note the round cystic anechoic areas in the inner myometrium or junctional zone. The small intra-myometrial cyst is surrounded by a hyperechoic ring).
Indeed, the typical appearance of endometriotic pelvic lesions on transvaginal sonography, such as endometriomas and rectal deep infiltrating endometriosis (DIE) — as well as adenomyosis – can be medically treated without histologic confirmation .
When surgery is advisable, ultrasound findings also play a valuable role in presurgical staging, planning, and counseling for patients of all ages. Determining the extent and location of DIE preoperatively, for instance, facilitates the engagement of the appropriate surgical specialists so that multiple surgeries can be avoided. It also enables patients to be optimally informed before surgery of possible outcomes and complications.
Moreover, in the context of infertility, ultrasound can be a valuable tool for understanding uterine pathology and assessing for adenomyosis so that affected patients may be treated surgically or medically before turning to assisted reproductive technology.
Uniformity, Standardization in the Sonographic Assessment
In Europe, as in the United States, transvaginal sonography (TVS) is the first-line imaging tool for the diagnosis and management of endometriosis. In Europe, many ob.gyns. perform ultrasound themselves, as do treating surgeons. When diagnostic findings are negative but clinical suspicion is high, MRI is often utilized. Laparoscopy may then be considered in patients with negative imaging results.
Efforts to standardize terms, definitions, measurements, and sonographic features of different types of endometriosis have been made to make it easier for physicians to share data and communicate with each other. A lack of uniformity has contributed to variability in the reported diagnostic accuracy of TVS.
About 10 years ago, in one such effort, we assessed the accuracy of TVS for DIE by comparing TVS results with laparoscopic/histologic findings, and developed an ultrasound mapping system to accurately record the location, size and depth of lesions visualized by TVS. The accuracy of TVS ranged from 76% for the diagnosis of vaginal endometriosis to 97% for the diagnosis of bladder lesions and posterior cul-de-sac obliteration. Accuracy was 93% and 91% for detecting ureteral involvement (right and left); 87% for uterosacral ligament endometriotic lesions; and 87% for parametrial involvement.6
Shortly after, with a focus on DIE, expert sonographers and physician-sonographers from across Europe — as well as some experts from Australia, Japan, Brazil, Chile, and the United States (Y. Osuga from Brigham and Women’s Hospital and Harvard Medical School) — came together to agree on a uniform approach to the sonographic evaluation for suspected endometriosis and a standardization of terminology.
The consensus opinion from the International Deep Endometriosis Analysis (IDEA) group details four steps for examining women with suspected DIE: 1) Evaluation of the uterus and adnexa, 2) evaluation of transvaginal sonographic “soft markers” (ie. site-specific tenderness and ovarian mobility), 3) assessment of the status of the posterior cul-de-sac using real-time ultrasound-based “sliding sign,” and 4) assessment for DIE nodules in the anterior and posterior compartments.7
Our paper describing a mapping system and the IDEA paper describe how to detect deep endometriosis in the pelvis by utilizing an ultrasound view of normal anatomy and pelvic organ structure to provide landmarks for accurately defining the site of DIE lesions (Figure 2).
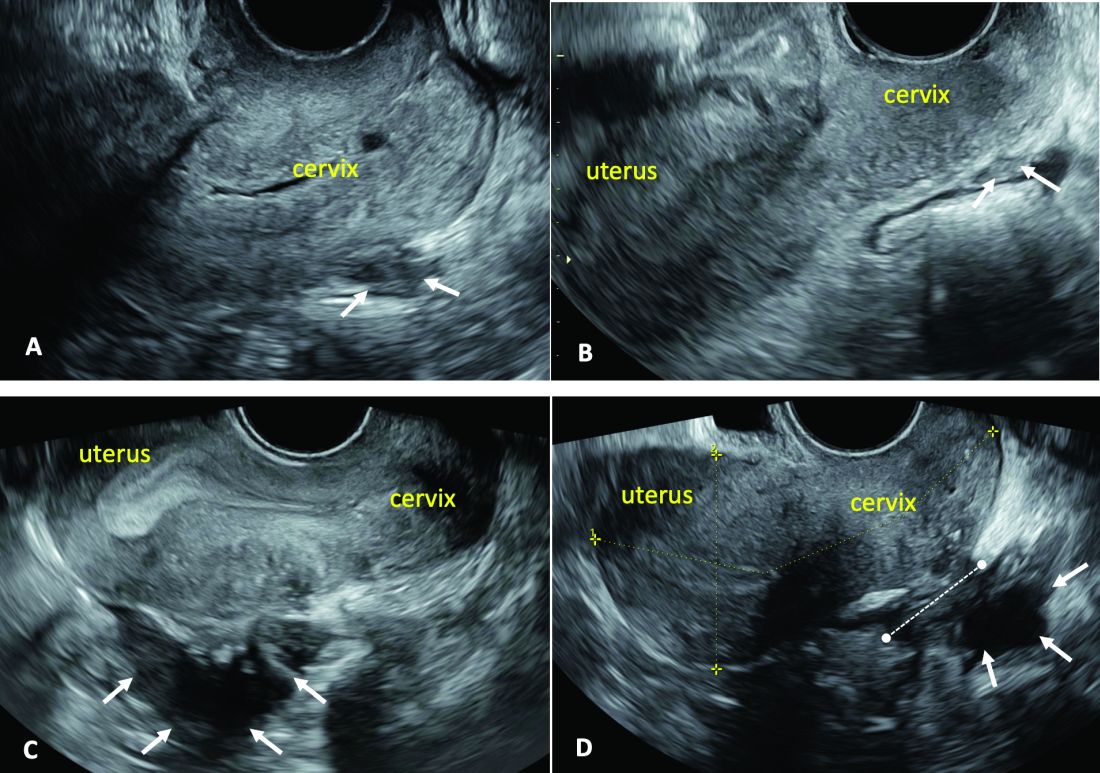
(A. Ultrasound appearance of a small DIE lesion of the retrocervical area [white arrows], which involved the torus uterinum and the right uterosacral ligament [USL]. The lesion appears as hypoechoic tissue with irregular margins caused by the fibrosis induced by the DIE. B. TVS appearance of small nodules of DIE of the left USL. Note the small retrocervical DIE lesion [white arrows], which appears hypoechoic due to the infiltration of the hyperechoic USL. C) Ultrasound appearance of a DIE nodule of the recto-sigmoid wall. Note the hypoechoic thickening of the muscular layers of the bowel wall attached to the corpus of the uterus and the adenomyosis of the posterior wall. The retrocervical area is free. D. TVS appearance of nodules of DIE of the lower rectal wall. Note the hypoechoic lesion [white arrows] of the rectum is attached to a retrocervical DIE fibrosis of the torus and USL [white dotted line]).
So-called rectovaginal endometriosis can be well assessed, for instance, since the involvement of the rectum, sigmoid colon, vaginal wall, rectovaginal septum, and posterior cul-de-sac uterosacral ligament can be seen by ultrasound as a single structure, making the location, size, and depth of any lesions discernible.
Again, this evaluation of the extent of disease is important for presurgical assessment so the surgeon can organize the right team and time of surgery and so the patient can be counseled on the advantages and possible complications of the treatment.
Notably, an accurate ultrasound description of pelvic endometriosis is helpful for accurate classification of disease. Endometriosis classification systems such as that of the American Association of Gynecologic Laparoscopists (AAGL)8 and the American Society of Reproductive Medicine (ASRM),9 as well as the #Enzian surgical description system,10 have been adapted to cover findings from ultrasound as well as MRI imaging.
A Systematic Evaluation
In keeping with the IDEA consensus opinion and based on our years of experience at the University of Rome, I advise that patients with typical pain symptoms of endometriosis or infertility undergo an accurate sonographic assessment of the pelvis with particular evaluation not only of the uterus and ovaries but of all pelvic retroperitoneal spaces.
The TVS examination should start with a slightly filled bladder, which permits a better evaluation of the bladder walls and the presence of endometriotic nodules. These nodules appear as hyperechoic linear or spherical lesions bulging toward the lumen and involving the serosa, muscularis, or (sub)mucosa of the bladder.
Then, an accurate evaluation of the uterus in 2D and 3D permits the diagnosis of adenomyosis. 3D sonographic evaluation of the myometrium and of the junctional zone are important; alteration and infiltration of the junctional zone and the presence of small adenomyotic cysts in the inner or outer myometrium are direct, specific signs of adenomyosis and should be ruled out in patients with dysmenorrhea, heavy menstrual bleeding, infertility, and pregnancy complications.
Endometriomas of the ovaries can be easily detected as having the typical appearance of a cyst with ground glass content. Adhesions of the ovaries and the uterus also should be evaluated with a dynamic ultrasound approach that utilizes the sliding sign and mobilization by palpation of the organs during the TVS scan.
Finally, the posterior and lateral retroperitoneal compartments should be carefully evaluated, with symptoms guiding the TVS examination whenever possible. Deep endometriotic nodules of the rectum appear as hypoechoic lesions or linear or nodular retroperitoneal thickening with irregular borders, penetrating into the intestinal wall and distorting its normal structure. In young patients, it seems very important to assess for small lesions below the peritoneum between the vagina and rectum, and in the parametria and around the ureter and nerves — lesions that, notably, would not be seen by diagnostic laparoscopy.
The Evaluation of Young Patients
In adolescent and young patients, endometriosis and adenomyosis are often present with small lesions and shallow tissue invasion, making a very careful and experienced approach to ultrasound essential for detection. Endometriomas are often of small diameter, and DIE is not always easily diagnosed because retroperitoneal lesions are similarly very small.
In a series of 270 adolescents (ages 12-20) who were referred to our outpatient gynecologic ultrasound unit over a 5-year period for various indications, at least one ultrasound feature of endometriosis was observed in 13.3%. In those with dysmenorrhea, the detection of endometriosis increased to 21%. Endometrioma was the most common type of endometriosis we found in the study, but DIE and adenomyosis were found in 4%-11%.
Although endometriotic lesions typically are small in young patients, they are often associated with severe pain symptoms, including chronic pelvic pain, dysmenorrhea, dyspareunia, dysuria, and dyschezia, all of which can have a serious effect on the quality of life of these young women. These symptoms keep them away from school during menstruation, away from sports, and cause painful intercourse and infertility. In young patients, an accurate TVS can provide a lot of information, and the ability to detect retroperitoneal endometriotic lesions and adenomyosis is probably better than with purely diagnostic laparoscopy, which would evaluate only superficial lesions.
TVS or, when needed, transrectal ultrasound, can enable adequate treatment and follow-up of the disease and its symptoms. There are no guidelines recommending adequate follow-up times to evaluate the effectiveness of medical therapy in patients with ultrasound signs of endometriosis. (Likewise, there are no indications for follow-up in patients with severe dysmenorrhea without ultrasound signs of endometriosis.) Certainly, our studies suggest careful evaluation over time of young patients with severe dysmenorrhea by serial ultrasound scans. With such follow-up, disease progress can be monitored and the medical or surgical treatment approach modified if needed.
The diagnosis of endometriosis at a young age has significant benefits not only in avoiding or reducing progression of the disease, but also in improving quality of life and aiding women in their desire for pregnancy.
Dr. Exacoustos is associate professor of ob.gyn. at the University of Rome “Tor Vergata.” She has no conflicts of interest to report.
References
1. Zondervan KT et al. N Engl J Med. 2020;382:1244-56.
2. Greene R et al. Fertil Steril. 2009;91:32-9.
3. Chapron C et al. J Pediatr Adolesc Gynecol. 2011;24:S7-12.
4. Randhawa AE et al. J Pediatr Adolesc Gynecol. 2021;34:643-8.
5. Becker CM et al. Hum Reprod Open. 2022(2):hoac009.
6. Exacoustos C et al. Fertil Steril. 2014;102:143-9. 7. Guerriero S et al. Ultrasound Obstet Gynecol. 2016;48(3):318-32.
8. Abrao MS et al. J Minim Invasive Gynecol. 2021;28:1941-50.9. Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril. 1997;67:817-21. 10. Keckstein J et al. Acta Obstet Gynecol Scand. 2021;100:1165-75.
11. Martire FG et al. Fertil Steril. 2020;114(5):1049-57.
Introduction: Imaging for Endometriosis — A Necessary Prerequisite
While the gold standard in the diagnosis of endometriosis remains laparoscopy, it is now recognized that thorough evaluation via ultrasound offers an acceptable, less expensive, and less invasive alternative. It is especially useful for the diagnosis of deep infiltrative disease, which penetrates more than 5 mm into the peritoneum, ovarian endometrioma, and when anatomic distortion occurs, such as to the path of the ureter.
Besides establishing the diagnosis, ultrasound imaging has become, along with MRI, the most important aid for proper preoperative planning. Not only does imaging provide the surgeon and patient with knowledge regarding the extent of the upcoming procedure, but it also allows the minimally invasive gynecologic (MIG) surgeon to involve colleagues, such as colorectal surgeons or urologists. For example, deep infiltrative endometriosis penetrating into the bowel mucosa will require a discoid or segmental bowel resection.
While many endometriosis experts rely on MRI, many MIG surgeons are dependent on ultrasound. I would not consider taking a patient with signs and symptoms suggestive of endometriosis to surgery without 2D/3D transvaginal ultrasound. If the patient possesses a uterus, a saline-infused sonogram is performed to potentially diagnose adenomyosis.
It is a pleasure and honor to welcome Professor Caterina Exacoustos MD, PhD, associate professor of ob.gyn. at the University of Rome “Tor Vergata,” to this edition of the Master Class in Gynecologic Surgery to discuss “Ultrasound and Its Role in the Diagnosis of and Management of Endometriosis, Including DIE.”
Prof. Exacoustos’ main areas of interest are endometriosis and benign diseases including uterine pathology and infertility. Her extensive body of work comprises over 120 scientific publications and numerous book chapters both in English and in Italian.
Prof. Exacoustos continues to be one of the most well respected lecturers speaking about ultrasound throughout the world.
Dr. Miller is professor of obstetrics and gynecology, department of clinical sciences, Rosalind Franklin University of Medicine and Science, North Chicago. Dr. Miller has no conflicts of interest to report.
Ultrasound and Its Role In Diagnosing and Managing Endometriosis
Endometriosis affects approximately 10%-20% of premenopausal women worldwide. It is the leading cause of chronic pelvic pain, is often associated with infertility, and has a significant impact on quality of life. Although the natural history of endometriosis remains unknown, emerging evidence suggests that the pathophysiological steps of initiation and development of endometriosis must occur earlier in the lifespan. Most notably, the onset of endometriosis-associated pain symptoms is often reported during adolescence and young adulthood.1
While many patients with endometriosis are referred with dysmenorrhea at a young age, at age ≤ 25 years,2 symptoms are often highly underestimated and considered to be normal and transient.3,4 Clinical and pelvic exams are often negative in young women, and delays in endometriosis diagnosis are well known.
The presentation of primary dysmenorrhea with no anatomical cause embodies the paradigm that dysmenorrhea in adolescents is most often an insignificant disorder. This perspective is probably a root cause of delayed endometriosis diagnosis in young patients. However, another issue behind delayed diagnosis is the reluctance of the physician to perform a diagnostic laparoscopy — historically the gold standard for diagnosing endometriosis — for seemingly common symptoms such as dysmenorrhea in young patients.
Today we know that there are typical aspects of ultrasound imaging that identify endometriosis in the pelvis, and notably, the 2022 European Society for Human Reproduction and Embryology (ESHRE) endometriosis guideline5 recognizes imaging (ultrasound or MRI) as the standard for endometriosis diagnosis without requiring laparoscopic or histological confirmation.
An early and noninvasive method of diagnosis aids in timely diagnosis and provides for the timely initiation of medical management to improve quality of life and prevent progression of disease (Figure 1).
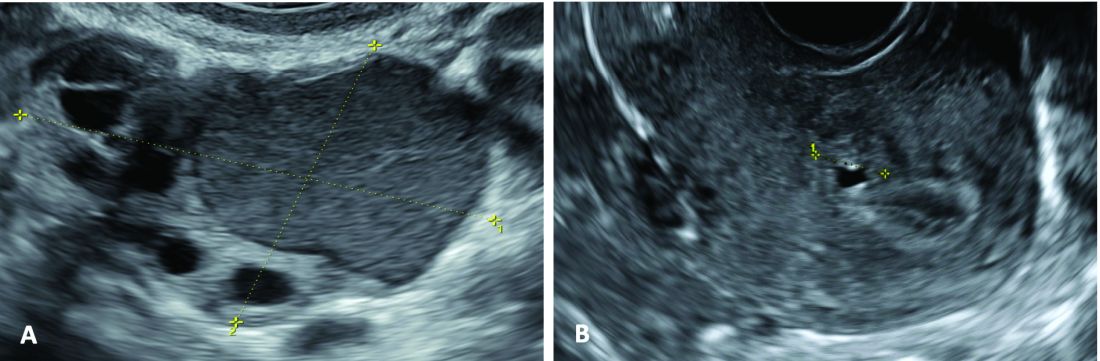
(A. Transvaginal ultrasound appearance of a small ovarian endometrioma in a 16-year-old girl. Note the unilocular cyst with ground glass echogenicity surrounded by multifollicular ovarian tissue. B. Ultrasound image of a retroverted uterus of an 18-year-old girl with focal adenomyosis of the posterior wall. Note the round cystic anechoic areas in the inner myometrium or junctional zone. The small intra-myometrial cyst is surrounded by a hyperechoic ring).
Indeed, the typical appearance of endometriotic pelvic lesions on transvaginal sonography, such as endometriomas and rectal deep infiltrating endometriosis (DIE) — as well as adenomyosis – can be medically treated without histologic confirmation .
When surgery is advisable, ultrasound findings also play a valuable role in presurgical staging, planning, and counseling for patients of all ages. Determining the extent and location of DIE preoperatively, for instance, facilitates the engagement of the appropriate surgical specialists so that multiple surgeries can be avoided. It also enables patients to be optimally informed before surgery of possible outcomes and complications.
Moreover, in the context of infertility, ultrasound can be a valuable tool for understanding uterine pathology and assessing for adenomyosis so that affected patients may be treated surgically or medically before turning to assisted reproductive technology.
Uniformity, Standardization in the Sonographic Assessment
In Europe, as in the United States, transvaginal sonography (TVS) is the first-line imaging tool for the diagnosis and management of endometriosis. In Europe, many ob.gyns. perform ultrasound themselves, as do treating surgeons. When diagnostic findings are negative but clinical suspicion is high, MRI is often utilized. Laparoscopy may then be considered in patients with negative imaging results.
Efforts to standardize terms, definitions, measurements, and sonographic features of different types of endometriosis have been made to make it easier for physicians to share data and communicate with each other. A lack of uniformity has contributed to variability in the reported diagnostic accuracy of TVS.
About 10 years ago, in one such effort, we assessed the accuracy of TVS for DIE by comparing TVS results with laparoscopic/histologic findings, and developed an ultrasound mapping system to accurately record the location, size and depth of lesions visualized by TVS. The accuracy of TVS ranged from 76% for the diagnosis of vaginal endometriosis to 97% for the diagnosis of bladder lesions and posterior cul-de-sac obliteration. Accuracy was 93% and 91% for detecting ureteral involvement (right and left); 87% for uterosacral ligament endometriotic lesions; and 87% for parametrial involvement.6
Shortly after, with a focus on DIE, expert sonographers and physician-sonographers from across Europe — as well as some experts from Australia, Japan, Brazil, Chile, and the United States (Y. Osuga from Brigham and Women’s Hospital and Harvard Medical School) — came together to agree on a uniform approach to the sonographic evaluation for suspected endometriosis and a standardization of terminology.
The consensus opinion from the International Deep Endometriosis Analysis (IDEA) group details four steps for examining women with suspected DIE: 1) Evaluation of the uterus and adnexa, 2) evaluation of transvaginal sonographic “soft markers” (ie. site-specific tenderness and ovarian mobility), 3) assessment of the status of the posterior cul-de-sac using real-time ultrasound-based “sliding sign,” and 4) assessment for DIE nodules in the anterior and posterior compartments.7
Our paper describing a mapping system and the IDEA paper describe how to detect deep endometriosis in the pelvis by utilizing an ultrasound view of normal anatomy and pelvic organ structure to provide landmarks for accurately defining the site of DIE lesions (Figure 2).
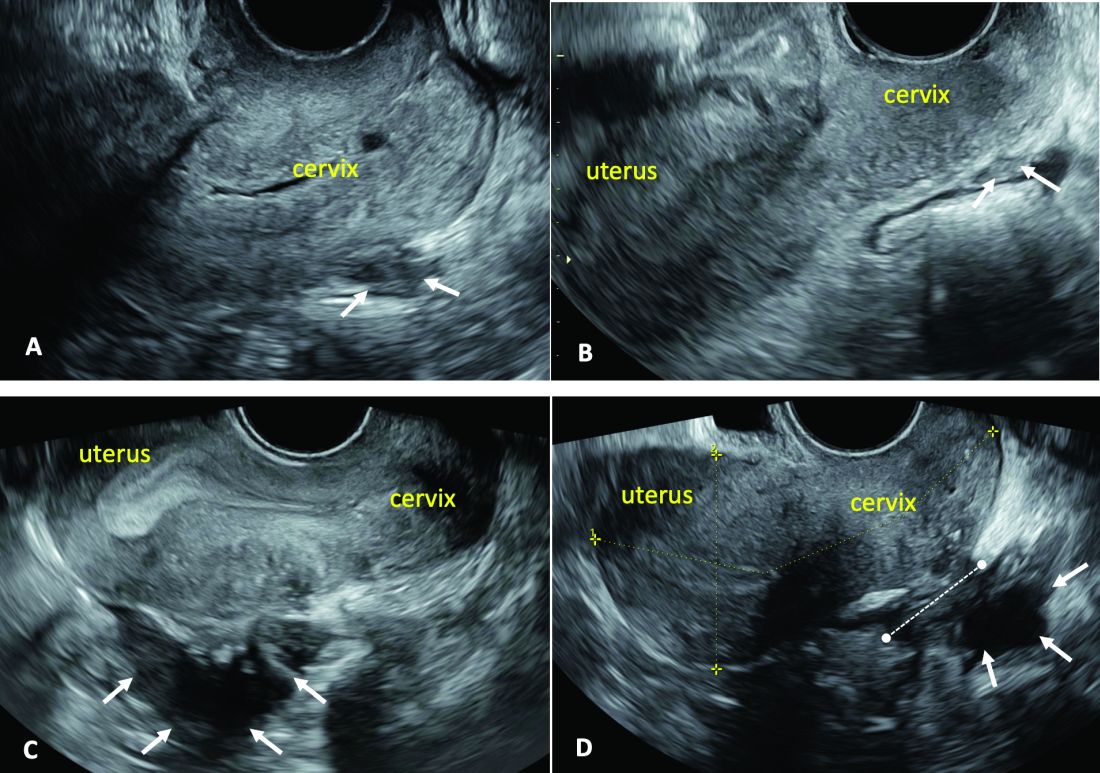
(A. Ultrasound appearance of a small DIE lesion of the retrocervical area [white arrows], which involved the torus uterinum and the right uterosacral ligament [USL]. The lesion appears as hypoechoic tissue with irregular margins caused by the fibrosis induced by the DIE. B. TVS appearance of small nodules of DIE of the left USL. Note the small retrocervical DIE lesion [white arrows], which appears hypoechoic due to the infiltration of the hyperechoic USL. C) Ultrasound appearance of a DIE nodule of the recto-sigmoid wall. Note the hypoechoic thickening of the muscular layers of the bowel wall attached to the corpus of the uterus and the adenomyosis of the posterior wall. The retrocervical area is free. D. TVS appearance of nodules of DIE of the lower rectal wall. Note the hypoechoic lesion [white arrows] of the rectum is attached to a retrocervical DIE fibrosis of the torus and USL [white dotted line]).
So-called rectovaginal endometriosis can be well assessed, for instance, since the involvement of the rectum, sigmoid colon, vaginal wall, rectovaginal septum, and posterior cul-de-sac uterosacral ligament can be seen by ultrasound as a single structure, making the location, size, and depth of any lesions discernible.
Again, this evaluation of the extent of disease is important for presurgical assessment so the surgeon can organize the right team and time of surgery and so the patient can be counseled on the advantages and possible complications of the treatment.
Notably, an accurate ultrasound description of pelvic endometriosis is helpful for accurate classification of disease. Endometriosis classification systems such as that of the American Association of Gynecologic Laparoscopists (AAGL)8 and the American Society of Reproductive Medicine (ASRM),9 as well as the #Enzian surgical description system,10 have been adapted to cover findings from ultrasound as well as MRI imaging.
A Systematic Evaluation
In keeping with the IDEA consensus opinion and based on our years of experience at the University of Rome, I advise that patients with typical pain symptoms of endometriosis or infertility undergo an accurate sonographic assessment of the pelvis with particular evaluation not only of the uterus and ovaries but of all pelvic retroperitoneal spaces.
The TVS examination should start with a slightly filled bladder, which permits a better evaluation of the bladder walls and the presence of endometriotic nodules. These nodules appear as hyperechoic linear or spherical lesions bulging toward the lumen and involving the serosa, muscularis, or (sub)mucosa of the bladder.
Then, an accurate evaluation of the uterus in 2D and 3D permits the diagnosis of adenomyosis. 3D sonographic evaluation of the myometrium and of the junctional zone are important; alteration and infiltration of the junctional zone and the presence of small adenomyotic cysts in the inner or outer myometrium are direct, specific signs of adenomyosis and should be ruled out in patients with dysmenorrhea, heavy menstrual bleeding, infertility, and pregnancy complications.
Endometriomas of the ovaries can be easily detected as having the typical appearance of a cyst with ground glass content. Adhesions of the ovaries and the uterus also should be evaluated with a dynamic ultrasound approach that utilizes the sliding sign and mobilization by palpation of the organs during the TVS scan.
Finally, the posterior and lateral retroperitoneal compartments should be carefully evaluated, with symptoms guiding the TVS examination whenever possible. Deep endometriotic nodules of the rectum appear as hypoechoic lesions or linear or nodular retroperitoneal thickening with irregular borders, penetrating into the intestinal wall and distorting its normal structure. In young patients, it seems very important to assess for small lesions below the peritoneum between the vagina and rectum, and in the parametria and around the ureter and nerves — lesions that, notably, would not be seen by diagnostic laparoscopy.
The Evaluation of Young Patients
In adolescent and young patients, endometriosis and adenomyosis are often present with small lesions and shallow tissue invasion, making a very careful and experienced approach to ultrasound essential for detection. Endometriomas are often of small diameter, and DIE is not always easily diagnosed because retroperitoneal lesions are similarly very small.
In a series of 270 adolescents (ages 12-20) who were referred to our outpatient gynecologic ultrasound unit over a 5-year period for various indications, at least one ultrasound feature of endometriosis was observed in 13.3%. In those with dysmenorrhea, the detection of endometriosis increased to 21%. Endometrioma was the most common type of endometriosis we found in the study, but DIE and adenomyosis were found in 4%-11%.
Although endometriotic lesions typically are small in young patients, they are often associated with severe pain symptoms, including chronic pelvic pain, dysmenorrhea, dyspareunia, dysuria, and dyschezia, all of which can have a serious effect on the quality of life of these young women. These symptoms keep them away from school during menstruation, away from sports, and cause painful intercourse and infertility. In young patients, an accurate TVS can provide a lot of information, and the ability to detect retroperitoneal endometriotic lesions and adenomyosis is probably better than with purely diagnostic laparoscopy, which would evaluate only superficial lesions.
TVS or, when needed, transrectal ultrasound, can enable adequate treatment and follow-up of the disease and its symptoms. There are no guidelines recommending adequate follow-up times to evaluate the effectiveness of medical therapy in patients with ultrasound signs of endometriosis. (Likewise, there are no indications for follow-up in patients with severe dysmenorrhea without ultrasound signs of endometriosis.) Certainly, our studies suggest careful evaluation over time of young patients with severe dysmenorrhea by serial ultrasound scans. With such follow-up, disease progress can be monitored and the medical or surgical treatment approach modified if needed.
The diagnosis of endometriosis at a young age has significant benefits not only in avoiding or reducing progression of the disease, but also in improving quality of life and aiding women in their desire for pregnancy.
Dr. Exacoustos is associate professor of ob.gyn. at the University of Rome “Tor Vergata.” She has no conflicts of interest to report.
References
1. Zondervan KT et al. N Engl J Med. 2020;382:1244-56.
2. Greene R et al. Fertil Steril. 2009;91:32-9.
3. Chapron C et al. J Pediatr Adolesc Gynecol. 2011;24:S7-12.
4. Randhawa AE et al. J Pediatr Adolesc Gynecol. 2021;34:643-8.
5. Becker CM et al. Hum Reprod Open. 2022(2):hoac009.
6. Exacoustos C et al. Fertil Steril. 2014;102:143-9. 7. Guerriero S et al. Ultrasound Obstet Gynecol. 2016;48(3):318-32.
8. Abrao MS et al. J Minim Invasive Gynecol. 2021;28:1941-50.9. Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril. 1997;67:817-21. 10. Keckstein J et al. Acta Obstet Gynecol Scand. 2021;100:1165-75.
11. Martire FG et al. Fertil Steril. 2020;114(5):1049-57.
AI and Suicide Prevention in Primary Care: A Q&A
Primary care physicians play a critical role in identifying patients at risk for serious mental health issues, including suicidality. But the ever-increasing demands on their clinical time can hinder the ability to identify emotional distress in time to intervene. Can artificial intelligence (AI) help?
This news organization spoke with Tom Zaubler, MD, a psychiatrist and chief medical officer of NeuroFlow, about how AI can improve the ability of primary care physicians and other clinicians to screen their patients for suicidal ideation and boost rates of treatment for mental health issues in their patients. This interview has been edited for clarity and length.
Question: How can AI help in suicide prevention and mental health screening in primary care?
Answer: Recent studies have demonstrated the potential of AI in mental health screening and suicide prevention. One method is natural language processing (NLP), which can analyze patients› journal entries for signs of suicidal thoughts or behaviors. This technology has shown promise in detecting suicidal ideation in patients who may not report such thoughts on traditional screening tools like the Patient Health Questionnaire-9 (PHQ-9). AI can be part of an integrated approach to identify and provide support to individuals at risk for suicide or those without a psychiatric history but who may still be at risk.
Q: A recent study by [Maria] Oquendo and colleagues found that one fifth of patients who attempt suicide do not meet the criteria for a mental health disorder.
Improved screening is obviously important, but in some ways it’s not the most important part of the problem. The lack of accessibility to specialized mental health care is a critical obstacle to treating patients with acute psychiatric needs.
How can primary care doctors effectively connect patients with mental health support, given the scarcity of mental health professionals?
A: Primary care doctors can leverage technology to extend mental health support. This includes using platforms for safety screening and providing patients with immediate access to local and national resources and digital interventions. Alerts can be sent to professionals within the practice or employed by technology companies to offer immediate support, including suicide safety planning and counseling. Users can hit a button to “Find a Therapist.” Also, if they acknowledge feelings of self-harm, these keywords are detected within the app by NLP. “Urgent alerts” are then sent to clinicians who are overseeing patient care. If someone is flagged, a social worker or member of a response services team intervenes and calls the person at risk to tailor care. These interventions do not always require a psychiatrist or masters-prepared clinician but can be effectively managed by trained paraprofessionals. These staff members can provide suicide safety planning and lethal-means-restriction counseling, and can assess the need for escalation of care.
Q: How is technology likely to manifest in physician practices in the near future to support mental health care?
A: Automated screening platforms for depression and anxiety, alerts for physicians when patients screen positively, and integration with collaborative care models are a few of the ways technology will become part of clinical practice. Additionally, advanced data analytics and predictive modeling using electronic health records and claims data will help identify high-risk patients. Technologies like voice recognition and machine learning can analyze patient journals and possibly, in the future, social media feeds to detect mental health issues. These technologies aim to extend and augment the capabilities of healthcare practices, improving the identification and management of patients at risk for mental health issues.
Q: Are these technologies as effective in pediatric populations, and are there any specific challenges?
A: Technologies for mental health screening and support are effective in pediatric populations, with certain age-specific considerations and legal restrictions on technology use. For adolescents and older children comfortable with technology, digital tools can significantly impact mental health care. For younger children, technology must facilitate information-gathering from various sources, including parents and teachers. Despite challenges, technology is crucial for early identification and intervention in pediatric mental health, potentially shortening the time to diagnosis and improving outcomes.
The statistics are horrifying. One third of adolescent girls have seriously thought about suicide over the past year; 13% attempt suicide. So there’s a need in the adolescent population and in the preadolescent population, too, because there’s an 8- to 10-year lag between onset of symptoms and diagnosis of mental illness. If we can shorten that lag, you see improved performance in schools; you see decreased truancy; you see greater economic achievement and so on. It makes such a profound difference. Not to mention it saves lives. So, yes, technology is critical in a pediatric population. It exists and it’s happening right now. There are challenges, but the goal can be met.
Q: A 2014 study found that 45% of people who completed suicide visited a primary care physician in the preceding month. And only 23% of people who attempt suicide have not seen a primary care physician within the past year. What does that say about the importance of screening at the primary care level?
A: The fact that a significant percentage of individuals who die by suicide have visited a primary care physician within a month or year prior to their death underscores the critical role of primary care in suicide prevention. This highlights the potential for primary care settings to identify and intervene with individuals at risk for suicide, making the case for the importance of integrating effective mental health screenings and support technologies in primary care practices.
Q: In other words, we’re not talking about a marginal benefit.
A: No, the potential benefit is huge. The United States Preventive Services Task Force did not endorse universal screening for suicide in its 2023 recommendations; they felt — and I accept that conclusion — there wasn›t enough evidence [at the time] to really support that recommendation. I think when you talk to a lot of suicide researchers, what you will hear is that providing suicide assessments as far upstream as possible is critical, especially when you start seeing more and more research showing that 20% of the population who die by suicide are not likely to have any psychiatric pathology at all. I believe the evidence base will soon support a recommendation for universal screening for adults. I believe it is especially important to screen for suicidal ideation in kids, given the high rates of suicide in this population.
Dr. Zaubler has disclosed the following relevant financial relationships: chief medical officer, NeuroFlow.
A version of this article appeared on Medscape.com.
Primary care physicians play a critical role in identifying patients at risk for serious mental health issues, including suicidality. But the ever-increasing demands on their clinical time can hinder the ability to identify emotional distress in time to intervene. Can artificial intelligence (AI) help?
This news organization spoke with Tom Zaubler, MD, a psychiatrist and chief medical officer of NeuroFlow, about how AI can improve the ability of primary care physicians and other clinicians to screen their patients for suicidal ideation and boost rates of treatment for mental health issues in their patients. This interview has been edited for clarity and length.
Question: How can AI help in suicide prevention and mental health screening in primary care?
Answer: Recent studies have demonstrated the potential of AI in mental health screening and suicide prevention. One method is natural language processing (NLP), which can analyze patients› journal entries for signs of suicidal thoughts or behaviors. This technology has shown promise in detecting suicidal ideation in patients who may not report such thoughts on traditional screening tools like the Patient Health Questionnaire-9 (PHQ-9). AI can be part of an integrated approach to identify and provide support to individuals at risk for suicide or those without a psychiatric history but who may still be at risk.
Q: A recent study by [Maria] Oquendo and colleagues found that one fifth of patients who attempt suicide do not meet the criteria for a mental health disorder.
Improved screening is obviously important, but in some ways it’s not the most important part of the problem. The lack of accessibility to specialized mental health care is a critical obstacle to treating patients with acute psychiatric needs.
How can primary care doctors effectively connect patients with mental health support, given the scarcity of mental health professionals?
A: Primary care doctors can leverage technology to extend mental health support. This includes using platforms for safety screening and providing patients with immediate access to local and national resources and digital interventions. Alerts can be sent to professionals within the practice or employed by technology companies to offer immediate support, including suicide safety planning and counseling. Users can hit a button to “Find a Therapist.” Also, if they acknowledge feelings of self-harm, these keywords are detected within the app by NLP. “Urgent alerts” are then sent to clinicians who are overseeing patient care. If someone is flagged, a social worker or member of a response services team intervenes and calls the person at risk to tailor care. These interventions do not always require a psychiatrist or masters-prepared clinician but can be effectively managed by trained paraprofessionals. These staff members can provide suicide safety planning and lethal-means-restriction counseling, and can assess the need for escalation of care.
Q: How is technology likely to manifest in physician practices in the near future to support mental health care?
A: Automated screening platforms for depression and anxiety, alerts for physicians when patients screen positively, and integration with collaborative care models are a few of the ways technology will become part of clinical practice. Additionally, advanced data analytics and predictive modeling using electronic health records and claims data will help identify high-risk patients. Technologies like voice recognition and machine learning can analyze patient journals and possibly, in the future, social media feeds to detect mental health issues. These technologies aim to extend and augment the capabilities of healthcare practices, improving the identification and management of patients at risk for mental health issues.
Q: Are these technologies as effective in pediatric populations, and are there any specific challenges?
A: Technologies for mental health screening and support are effective in pediatric populations, with certain age-specific considerations and legal restrictions on technology use. For adolescents and older children comfortable with technology, digital tools can significantly impact mental health care. For younger children, technology must facilitate information-gathering from various sources, including parents and teachers. Despite challenges, technology is crucial for early identification and intervention in pediatric mental health, potentially shortening the time to diagnosis and improving outcomes.
The statistics are horrifying. One third of adolescent girls have seriously thought about suicide over the past year; 13% attempt suicide. So there’s a need in the adolescent population and in the preadolescent population, too, because there’s an 8- to 10-year lag between onset of symptoms and diagnosis of mental illness. If we can shorten that lag, you see improved performance in schools; you see decreased truancy; you see greater economic achievement and so on. It makes such a profound difference. Not to mention it saves lives. So, yes, technology is critical in a pediatric population. It exists and it’s happening right now. There are challenges, but the goal can be met.
Q: A 2014 study found that 45% of people who completed suicide visited a primary care physician in the preceding month. And only 23% of people who attempt suicide have not seen a primary care physician within the past year. What does that say about the importance of screening at the primary care level?
A: The fact that a significant percentage of individuals who die by suicide have visited a primary care physician within a month or year prior to their death underscores the critical role of primary care in suicide prevention. This highlights the potential for primary care settings to identify and intervene with individuals at risk for suicide, making the case for the importance of integrating effective mental health screenings and support technologies in primary care practices.
Q: In other words, we’re not talking about a marginal benefit.
A: No, the potential benefit is huge. The United States Preventive Services Task Force did not endorse universal screening for suicide in its 2023 recommendations; they felt — and I accept that conclusion — there wasn›t enough evidence [at the time] to really support that recommendation. I think when you talk to a lot of suicide researchers, what you will hear is that providing suicide assessments as far upstream as possible is critical, especially when you start seeing more and more research showing that 20% of the population who die by suicide are not likely to have any psychiatric pathology at all. I believe the evidence base will soon support a recommendation for universal screening for adults. I believe it is especially important to screen for suicidal ideation in kids, given the high rates of suicide in this population.
Dr. Zaubler has disclosed the following relevant financial relationships: chief medical officer, NeuroFlow.
A version of this article appeared on Medscape.com.
Primary care physicians play a critical role in identifying patients at risk for serious mental health issues, including suicidality. But the ever-increasing demands on their clinical time can hinder the ability to identify emotional distress in time to intervene. Can artificial intelligence (AI) help?
This news organization spoke with Tom Zaubler, MD, a psychiatrist and chief medical officer of NeuroFlow, about how AI can improve the ability of primary care physicians and other clinicians to screen their patients for suicidal ideation and boost rates of treatment for mental health issues in their patients. This interview has been edited for clarity and length.
Question: How can AI help in suicide prevention and mental health screening in primary care?
Answer: Recent studies have demonstrated the potential of AI in mental health screening and suicide prevention. One method is natural language processing (NLP), which can analyze patients› journal entries for signs of suicidal thoughts or behaviors. This technology has shown promise in detecting suicidal ideation in patients who may not report such thoughts on traditional screening tools like the Patient Health Questionnaire-9 (PHQ-9). AI can be part of an integrated approach to identify and provide support to individuals at risk for suicide or those without a psychiatric history but who may still be at risk.
Q: A recent study by [Maria] Oquendo and colleagues found that one fifth of patients who attempt suicide do not meet the criteria for a mental health disorder.
Improved screening is obviously important, but in some ways it’s not the most important part of the problem. The lack of accessibility to specialized mental health care is a critical obstacle to treating patients with acute psychiatric needs.
How can primary care doctors effectively connect patients with mental health support, given the scarcity of mental health professionals?
A: Primary care doctors can leverage technology to extend mental health support. This includes using platforms for safety screening and providing patients with immediate access to local and national resources and digital interventions. Alerts can be sent to professionals within the practice or employed by technology companies to offer immediate support, including suicide safety planning and counseling. Users can hit a button to “Find a Therapist.” Also, if they acknowledge feelings of self-harm, these keywords are detected within the app by NLP. “Urgent alerts” are then sent to clinicians who are overseeing patient care. If someone is flagged, a social worker or member of a response services team intervenes and calls the person at risk to tailor care. These interventions do not always require a psychiatrist or masters-prepared clinician but can be effectively managed by trained paraprofessionals. These staff members can provide suicide safety planning and lethal-means-restriction counseling, and can assess the need for escalation of care.
Q: How is technology likely to manifest in physician practices in the near future to support mental health care?
A: Automated screening platforms for depression and anxiety, alerts for physicians when patients screen positively, and integration with collaborative care models are a few of the ways technology will become part of clinical practice. Additionally, advanced data analytics and predictive modeling using electronic health records and claims data will help identify high-risk patients. Technologies like voice recognition and machine learning can analyze patient journals and possibly, in the future, social media feeds to detect mental health issues. These technologies aim to extend and augment the capabilities of healthcare practices, improving the identification and management of patients at risk for mental health issues.
Q: Are these technologies as effective in pediatric populations, and are there any specific challenges?
A: Technologies for mental health screening and support are effective in pediatric populations, with certain age-specific considerations and legal restrictions on technology use. For adolescents and older children comfortable with technology, digital tools can significantly impact mental health care. For younger children, technology must facilitate information-gathering from various sources, including parents and teachers. Despite challenges, technology is crucial for early identification and intervention in pediatric mental health, potentially shortening the time to diagnosis and improving outcomes.
The statistics are horrifying. One third of adolescent girls have seriously thought about suicide over the past year; 13% attempt suicide. So there’s a need in the adolescent population and in the preadolescent population, too, because there’s an 8- to 10-year lag between onset of symptoms and diagnosis of mental illness. If we can shorten that lag, you see improved performance in schools; you see decreased truancy; you see greater economic achievement and so on. It makes such a profound difference. Not to mention it saves lives. So, yes, technology is critical in a pediatric population. It exists and it’s happening right now. There are challenges, but the goal can be met.
Q: A 2014 study found that 45% of people who completed suicide visited a primary care physician in the preceding month. And only 23% of people who attempt suicide have not seen a primary care physician within the past year. What does that say about the importance of screening at the primary care level?
A: The fact that a significant percentage of individuals who die by suicide have visited a primary care physician within a month or year prior to their death underscores the critical role of primary care in suicide prevention. This highlights the potential for primary care settings to identify and intervene with individuals at risk for suicide, making the case for the importance of integrating effective mental health screenings and support technologies in primary care practices.
Q: In other words, we’re not talking about a marginal benefit.
A: No, the potential benefit is huge. The United States Preventive Services Task Force did not endorse universal screening for suicide in its 2023 recommendations; they felt — and I accept that conclusion — there wasn›t enough evidence [at the time] to really support that recommendation. I think when you talk to a lot of suicide researchers, what you will hear is that providing suicide assessments as far upstream as possible is critical, especially when you start seeing more and more research showing that 20% of the population who die by suicide are not likely to have any psychiatric pathology at all. I believe the evidence base will soon support a recommendation for universal screening for adults. I believe it is especially important to screen for suicidal ideation in kids, given the high rates of suicide in this population.
Dr. Zaubler has disclosed the following relevant financial relationships: chief medical officer, NeuroFlow.
A version of this article appeared on Medscape.com.
You Can’t Spell ‘Medicine’ Without D, E, and I
Please note that this is a commentary, an opinion piece: my opinion. The statements here do not necessarily represent those of this news organization or any of the myriad people or institutions that comprise this corner of the human universe.
Some days, speaking as a long-time physician and editor, I wish that there were no such things as race or ethnicity or even geographic origin for that matter. We can’t get away from sex, gender, disability, age, or culture. I’m not sure about religion. I wish people were just people.
But race is deeply embedded in the American experience — an almost invisible but inevitable presence in all of our thoughts and expressions about human activities.
In medical education (for eons it seems) the student has been taught to mention race in the first sentence of a given patient presentation, along with age and sex. In human epidemiologic research, race is almost always a studied variable. In clinical and basic medical research, looking at the impact of race on this, that, or the other is commonplace. “Mixed race not otherwise specified” is ubiquitous in the United States yet blithely ignored by most who tally these statistics. Race is rarely gene-specific. It is more of a social and cultural construct but with plainly visible overt phenotypic markers — an almost infinite mix of daily reality.
Our country, and much of Western civilization in 2024, is based on the principle that all men are created equal, although the originators of that notion were unaware of their own “equity-challenged” situation.
Many organizations, in and out of government, are now understanding, developing, and implementing programs (and thought/language patterns) to socialize diversity, equity, and inclusion (known as DEI) into their culture. It should not be surprising that many who prefer the status quo are not happy with the pressure from this movement and are using whatever methods are available to them to prevent full DEI. Such it always is.
The trusty Copilot from Bing provides these definitions:
- Diversity refers to the presence of variety within the organizational workforce. This includes aspects such as gender, culture, ethnicity, religion, disability, age, and opinion.
- Equity encompasses concepts of fairness and justice. It involves fair compensation, substantive equality, and addressing societal disparities. Equity also considers unique circumstances and adjusts treatment to achieve equal outcomes.
- Inclusion focuses on creating an organizational culture where all employees feel heard, fostering a sense of belonging and integration.
I am more than proud that my old domain of peer-reviewed, primary source, medical (and science) journals is taking a leading role in this noble, necessary, and long overdue movement for medicine.
As the central repository and transmitter of new medical information, including scientific studies, clinical medicine reports, ethics measures, and education, medical journals (including those deemed prestigious) have historically been among the worst offenders in perpetuating non-DEI objectives in their leadership, staffing, focus, instructions for authors, style manuals, and published materials.
This issue came to a head in March 2021 when a JAMA podcast about racism in American medicine was followed by this promotional tweet: “No physician is racist, so how can there be structural racism in health care?”
Reactions and actions were rapid, strong, and decisive. After an interregnum at JAMA, a new editor in chief, Kirsten Bibbins-Domingo, PhD, MD, MAS, was named. She and her large staff of editors and editorial board members from the multijournal JAMA Network joined a worldwide movement of (currently) 56 publishing organizations representing 15,000 journals called the Joint Commitment for Action on Inclusion and Diversity in Publishing.
A recent JAMA editorial with 29 authors describes the entire commitment initiative of publishers-editors. It reports JAMA Network data from 2023 and 2024 from surveys of 455 editors (a 91% response rate) about their own gender (five choices), ethnic origins or geographic ancestry (13 choices), and race (eight choices), demonstrating considerable progress toward DEI goals. The survey’s complex multinational classifications may not jibe with the categorizations used in some countries (too bad that “mixed” is not “mixed in” — a missed opportunity).
This encouraging movement will not fix it all. But when people of certain groups are represented at the table, that point of view is far more likely to make it into the lexicon, language, and omnipresent work products, potentially changing cultural norms. Even the measurement of movement related to disparity in healthcare is marred by frequent variations of data accuracy. More consistency in what to measure can help a lot, and the medical literature can be very influential.
A personal anecdote: When I was a professor at UC Davis in 1978, Allan Bakke, MD, was my student. Some of you will remember the saga of affirmative action on admissions, which was just revisited in the light of a recent decision by the US Supreme Court.
Back in 1978, the dean at UC Davis told me that he kept two file folders on the admission processes in different desk drawers. One categorized all applicants and enrollees by race, and the other did not. Depending on who came to visit and ask questions, he would choose one or the other file to share once he figured out what they were looking for (this is not a joke).
The strength of the current active political pushback against the entire DEI movement has deep roots and should not be underestimated. There will be a lot of to-ing and fro-ing.
French writer Victor Hugo is credited with stating, “There is nothing as powerful as an idea whose time has come.” A majority of Americans, physicians, and other healthcare professionals believe in basic fairness. The time for DEI in all aspects of medicine is now.
Dr. Lundberg, editor in chief of Cancer Commons, disclosed having no relevant financial relationships.
A version of this article appeared on Medscape.com.
Please note that this is a commentary, an opinion piece: my opinion. The statements here do not necessarily represent those of this news organization or any of the myriad people or institutions that comprise this corner of the human universe.
Some days, speaking as a long-time physician and editor, I wish that there were no such things as race or ethnicity or even geographic origin for that matter. We can’t get away from sex, gender, disability, age, or culture. I’m not sure about religion. I wish people were just people.
But race is deeply embedded in the American experience — an almost invisible but inevitable presence in all of our thoughts and expressions about human activities.
In medical education (for eons it seems) the student has been taught to mention race in the first sentence of a given patient presentation, along with age and sex. In human epidemiologic research, race is almost always a studied variable. In clinical and basic medical research, looking at the impact of race on this, that, or the other is commonplace. “Mixed race not otherwise specified” is ubiquitous in the United States yet blithely ignored by most who tally these statistics. Race is rarely gene-specific. It is more of a social and cultural construct but with plainly visible overt phenotypic markers — an almost infinite mix of daily reality.
Our country, and much of Western civilization in 2024, is based on the principle that all men are created equal, although the originators of that notion were unaware of their own “equity-challenged” situation.
Many organizations, in and out of government, are now understanding, developing, and implementing programs (and thought/language patterns) to socialize diversity, equity, and inclusion (known as DEI) into their culture. It should not be surprising that many who prefer the status quo are not happy with the pressure from this movement and are using whatever methods are available to them to prevent full DEI. Such it always is.
The trusty Copilot from Bing provides these definitions:
- Diversity refers to the presence of variety within the organizational workforce. This includes aspects such as gender, culture, ethnicity, religion, disability, age, and opinion.
- Equity encompasses concepts of fairness and justice. It involves fair compensation, substantive equality, and addressing societal disparities. Equity also considers unique circumstances and adjusts treatment to achieve equal outcomes.
- Inclusion focuses on creating an organizational culture where all employees feel heard, fostering a sense of belonging and integration.
I am more than proud that my old domain of peer-reviewed, primary source, medical (and science) journals is taking a leading role in this noble, necessary, and long overdue movement for medicine.
As the central repository and transmitter of new medical information, including scientific studies, clinical medicine reports, ethics measures, and education, medical journals (including those deemed prestigious) have historically been among the worst offenders in perpetuating non-DEI objectives in their leadership, staffing, focus, instructions for authors, style manuals, and published materials.
This issue came to a head in March 2021 when a JAMA podcast about racism in American medicine was followed by this promotional tweet: “No physician is racist, so how can there be structural racism in health care?”
Reactions and actions were rapid, strong, and decisive. After an interregnum at JAMA, a new editor in chief, Kirsten Bibbins-Domingo, PhD, MD, MAS, was named. She and her large staff of editors and editorial board members from the multijournal JAMA Network joined a worldwide movement of (currently) 56 publishing organizations representing 15,000 journals called the Joint Commitment for Action on Inclusion and Diversity in Publishing.
A recent JAMA editorial with 29 authors describes the entire commitment initiative of publishers-editors. It reports JAMA Network data from 2023 and 2024 from surveys of 455 editors (a 91% response rate) about their own gender (five choices), ethnic origins or geographic ancestry (13 choices), and race (eight choices), demonstrating considerable progress toward DEI goals. The survey’s complex multinational classifications may not jibe with the categorizations used in some countries (too bad that “mixed” is not “mixed in” — a missed opportunity).
This encouraging movement will not fix it all. But when people of certain groups are represented at the table, that point of view is far more likely to make it into the lexicon, language, and omnipresent work products, potentially changing cultural norms. Even the measurement of movement related to disparity in healthcare is marred by frequent variations of data accuracy. More consistency in what to measure can help a lot, and the medical literature can be very influential.
A personal anecdote: When I was a professor at UC Davis in 1978, Allan Bakke, MD, was my student. Some of you will remember the saga of affirmative action on admissions, which was just revisited in the light of a recent decision by the US Supreme Court.
Back in 1978, the dean at UC Davis told me that he kept two file folders on the admission processes in different desk drawers. One categorized all applicants and enrollees by race, and the other did not. Depending on who came to visit and ask questions, he would choose one or the other file to share once he figured out what they were looking for (this is not a joke).
The strength of the current active political pushback against the entire DEI movement has deep roots and should not be underestimated. There will be a lot of to-ing and fro-ing.
French writer Victor Hugo is credited with stating, “There is nothing as powerful as an idea whose time has come.” A majority of Americans, physicians, and other healthcare professionals believe in basic fairness. The time for DEI in all aspects of medicine is now.
Dr. Lundberg, editor in chief of Cancer Commons, disclosed having no relevant financial relationships.
A version of this article appeared on Medscape.com.
Please note that this is a commentary, an opinion piece: my opinion. The statements here do not necessarily represent those of this news organization or any of the myriad people or institutions that comprise this corner of the human universe.
Some days, speaking as a long-time physician and editor, I wish that there were no such things as race or ethnicity or even geographic origin for that matter. We can’t get away from sex, gender, disability, age, or culture. I’m not sure about religion. I wish people were just people.
But race is deeply embedded in the American experience — an almost invisible but inevitable presence in all of our thoughts and expressions about human activities.
In medical education (for eons it seems) the student has been taught to mention race in the first sentence of a given patient presentation, along with age and sex. In human epidemiologic research, race is almost always a studied variable. In clinical and basic medical research, looking at the impact of race on this, that, or the other is commonplace. “Mixed race not otherwise specified” is ubiquitous in the United States yet blithely ignored by most who tally these statistics. Race is rarely gene-specific. It is more of a social and cultural construct but with plainly visible overt phenotypic markers — an almost infinite mix of daily reality.
Our country, and much of Western civilization in 2024, is based on the principle that all men are created equal, although the originators of that notion were unaware of their own “equity-challenged” situation.
Many organizations, in and out of government, are now understanding, developing, and implementing programs (and thought/language patterns) to socialize diversity, equity, and inclusion (known as DEI) into their culture. It should not be surprising that many who prefer the status quo are not happy with the pressure from this movement and are using whatever methods are available to them to prevent full DEI. Such it always is.
The trusty Copilot from Bing provides these definitions:
- Diversity refers to the presence of variety within the organizational workforce. This includes aspects such as gender, culture, ethnicity, religion, disability, age, and opinion.
- Equity encompasses concepts of fairness and justice. It involves fair compensation, substantive equality, and addressing societal disparities. Equity also considers unique circumstances and adjusts treatment to achieve equal outcomes.
- Inclusion focuses on creating an organizational culture where all employees feel heard, fostering a sense of belonging and integration.
I am more than proud that my old domain of peer-reviewed, primary source, medical (and science) journals is taking a leading role in this noble, necessary, and long overdue movement for medicine.
As the central repository and transmitter of new medical information, including scientific studies, clinical medicine reports, ethics measures, and education, medical journals (including those deemed prestigious) have historically been among the worst offenders in perpetuating non-DEI objectives in their leadership, staffing, focus, instructions for authors, style manuals, and published materials.
This issue came to a head in March 2021 when a JAMA podcast about racism in American medicine was followed by this promotional tweet: “No physician is racist, so how can there be structural racism in health care?”
Reactions and actions were rapid, strong, and decisive. After an interregnum at JAMA, a new editor in chief, Kirsten Bibbins-Domingo, PhD, MD, MAS, was named. She and her large staff of editors and editorial board members from the multijournal JAMA Network joined a worldwide movement of (currently) 56 publishing organizations representing 15,000 journals called the Joint Commitment for Action on Inclusion and Diversity in Publishing.
A recent JAMA editorial with 29 authors describes the entire commitment initiative of publishers-editors. It reports JAMA Network data from 2023 and 2024 from surveys of 455 editors (a 91% response rate) about their own gender (five choices), ethnic origins or geographic ancestry (13 choices), and race (eight choices), demonstrating considerable progress toward DEI goals. The survey’s complex multinational classifications may not jibe with the categorizations used in some countries (too bad that “mixed” is not “mixed in” — a missed opportunity).
This encouraging movement will not fix it all. But when people of certain groups are represented at the table, that point of view is far more likely to make it into the lexicon, language, and omnipresent work products, potentially changing cultural norms. Even the measurement of movement related to disparity in healthcare is marred by frequent variations of data accuracy. More consistency in what to measure can help a lot, and the medical literature can be very influential.
A personal anecdote: When I was a professor at UC Davis in 1978, Allan Bakke, MD, was my student. Some of you will remember the saga of affirmative action on admissions, which was just revisited in the light of a recent decision by the US Supreme Court.
Back in 1978, the dean at UC Davis told me that he kept two file folders on the admission processes in different desk drawers. One categorized all applicants and enrollees by race, and the other did not. Depending on who came to visit and ask questions, he would choose one or the other file to share once he figured out what they were looking for (this is not a joke).
The strength of the current active political pushback against the entire DEI movement has deep roots and should not be underestimated. There will be a lot of to-ing and fro-ing.
French writer Victor Hugo is credited with stating, “There is nothing as powerful as an idea whose time has come.” A majority of Americans, physicians, and other healthcare professionals believe in basic fairness. The time for DEI in all aspects of medicine is now.
Dr. Lundberg, editor in chief of Cancer Commons, disclosed having no relevant financial relationships.
A version of this article appeared on Medscape.com.
Losing More Than Fat
Whether you have totally bought into the “obesity is a disease” paradigm or are still in denial, you must admit that the development of a suite of effective weight loss medications has created a tsunami of interest and economic activity in this country on a scale not seen since the Beanie Baby craze of the mid-1990s. But, obesity management is serious business. While most of those soft cuddly toys are gathering dust in shoeboxes across this country, weight loss medications are likely to be the vanguard of rapidly evolving revolution in healthcare management that will be with us for the foreseeable future.
Most thoughtful folks who purchased Beanie Babies in 1994 had no illusions and knew that in a few short years this bubble of soft cuddly toys was going to burst. However, do those of us on the front line of medical care know what the future holds for the patients who are being prescribed or are scavenging those too-good-to-be-true medications?
My guess is that in the long run we will need a combination of some serious tinkering by the pharmaceutical industry and a trek up some steep learning curves before we eventually arrive at a safe and effective chemical management for obese patients. I recently read an article by an obesity management specialist at Harvard Medical School who voiced her concerns that we are missing an opportunity to make this explosion of popularity in GLP-1 drugs into an important learning experience.
In an opinion piece in JAMA Internal Medicine, Dr. Fatima Cody Stanford and her coauthors argue that we, actually the US Food and Drug Administration (FDA), is over-focused on weight loss in determining the efficacy of anti-obesity medications. Dr. Stanford and colleagues point out that when a patient loses weight it isn’t just fat — it is complex process that may include muscle and bone mineralization as well. She has consulted for at least one obesity-drug manufacturer and says that these companies have the resources to produce data on body composition that could help clinicians create management plans that would address the patients’ overall health. However, the FDA has not demanded this broader and deeper assessment of general health when reviewing the drug trials.
I don’t think we can blame the patients for not asking whether they will healthier while taking these medications. They have already spent a lifetime, even if it is just a decade, of suffering as the “fat one.” A new outfit and a look in the mirror can’t help but make them feel better ... in the short term anyway. We as physicians must shoulder some of the blame for focusing on weight. Our spoken or unspoken message has been “Lose weight and you will be healthier.” We may make our message sound more professional by tossing around terms like “BMI,” but as Dr. Stanford points out, “we have known BMI is a flawed metric for a long time.”
There is the notion that obese people have had to build more muscle to help them carry around the extra weight, so that we should expect them to lose that extra muscle along with the fat. However, in older adults there is an entity called sarcopenic obesity, in which the patient doesn’t have that extra muscle to lose.
In a brief Internet research venture, I could find little on the subject of muscle loss and GLP-1s, other than “it can happen.” And, nothing on the effect in adolescents. And that is one of Dr. Stanford’s points. We just don’t know. She said that looking at body composition can be costly and not something that the clinician can do. However, as far as muscle mass is concerned, we need to be alert to the potential for loss. Simple assessments of strength can help us tailor our management to the specific patient’s need.
The bottom line is this ... now that we have effective medications for “weight loss,” we need to redefine the relationship between weight and health. “We” means us as clinicians. It means the folks at FDA. And, if we can improve our messaging, it will osmose to the rest of the population. Just because you’ve dropped two dress sizes doesn’t mean you’re healthy.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Whether you have totally bought into the “obesity is a disease” paradigm or are still in denial, you must admit that the development of a suite of effective weight loss medications has created a tsunami of interest and economic activity in this country on a scale not seen since the Beanie Baby craze of the mid-1990s. But, obesity management is serious business. While most of those soft cuddly toys are gathering dust in shoeboxes across this country, weight loss medications are likely to be the vanguard of rapidly evolving revolution in healthcare management that will be with us for the foreseeable future.
Most thoughtful folks who purchased Beanie Babies in 1994 had no illusions and knew that in a few short years this bubble of soft cuddly toys was going to burst. However, do those of us on the front line of medical care know what the future holds for the patients who are being prescribed or are scavenging those too-good-to-be-true medications?
My guess is that in the long run we will need a combination of some serious tinkering by the pharmaceutical industry and a trek up some steep learning curves before we eventually arrive at a safe and effective chemical management for obese patients. I recently read an article by an obesity management specialist at Harvard Medical School who voiced her concerns that we are missing an opportunity to make this explosion of popularity in GLP-1 drugs into an important learning experience.
In an opinion piece in JAMA Internal Medicine, Dr. Fatima Cody Stanford and her coauthors argue that we, actually the US Food and Drug Administration (FDA), is over-focused on weight loss in determining the efficacy of anti-obesity medications. Dr. Stanford and colleagues point out that when a patient loses weight it isn’t just fat — it is complex process that may include muscle and bone mineralization as well. She has consulted for at least one obesity-drug manufacturer and says that these companies have the resources to produce data on body composition that could help clinicians create management plans that would address the patients’ overall health. However, the FDA has not demanded this broader and deeper assessment of general health when reviewing the drug trials.
I don’t think we can blame the patients for not asking whether they will healthier while taking these medications. They have already spent a lifetime, even if it is just a decade, of suffering as the “fat one.” A new outfit and a look in the mirror can’t help but make them feel better ... in the short term anyway. We as physicians must shoulder some of the blame for focusing on weight. Our spoken or unspoken message has been “Lose weight and you will be healthier.” We may make our message sound more professional by tossing around terms like “BMI,” but as Dr. Stanford points out, “we have known BMI is a flawed metric for a long time.”
There is the notion that obese people have had to build more muscle to help them carry around the extra weight, so that we should expect them to lose that extra muscle along with the fat. However, in older adults there is an entity called sarcopenic obesity, in which the patient doesn’t have that extra muscle to lose.
In a brief Internet research venture, I could find little on the subject of muscle loss and GLP-1s, other than “it can happen.” And, nothing on the effect in adolescents. And that is one of Dr. Stanford’s points. We just don’t know. She said that looking at body composition can be costly and not something that the clinician can do. However, as far as muscle mass is concerned, we need to be alert to the potential for loss. Simple assessments of strength can help us tailor our management to the specific patient’s need.
The bottom line is this ... now that we have effective medications for “weight loss,” we need to redefine the relationship between weight and health. “We” means us as clinicians. It means the folks at FDA. And, if we can improve our messaging, it will osmose to the rest of the population. Just because you’ve dropped two dress sizes doesn’t mean you’re healthy.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Whether you have totally bought into the “obesity is a disease” paradigm or are still in denial, you must admit that the development of a suite of effective weight loss medications has created a tsunami of interest and economic activity in this country on a scale not seen since the Beanie Baby craze of the mid-1990s. But, obesity management is serious business. While most of those soft cuddly toys are gathering dust in shoeboxes across this country, weight loss medications are likely to be the vanguard of rapidly evolving revolution in healthcare management that will be with us for the foreseeable future.
Most thoughtful folks who purchased Beanie Babies in 1994 had no illusions and knew that in a few short years this bubble of soft cuddly toys was going to burst. However, do those of us on the front line of medical care know what the future holds for the patients who are being prescribed or are scavenging those too-good-to-be-true medications?
My guess is that in the long run we will need a combination of some serious tinkering by the pharmaceutical industry and a trek up some steep learning curves before we eventually arrive at a safe and effective chemical management for obese patients. I recently read an article by an obesity management specialist at Harvard Medical School who voiced her concerns that we are missing an opportunity to make this explosion of popularity in GLP-1 drugs into an important learning experience.
In an opinion piece in JAMA Internal Medicine, Dr. Fatima Cody Stanford and her coauthors argue that we, actually the US Food and Drug Administration (FDA), is over-focused on weight loss in determining the efficacy of anti-obesity medications. Dr. Stanford and colleagues point out that when a patient loses weight it isn’t just fat — it is complex process that may include muscle and bone mineralization as well. She has consulted for at least one obesity-drug manufacturer and says that these companies have the resources to produce data on body composition that could help clinicians create management plans that would address the patients’ overall health. However, the FDA has not demanded this broader and deeper assessment of general health when reviewing the drug trials.
I don’t think we can blame the patients for not asking whether they will healthier while taking these medications. They have already spent a lifetime, even if it is just a decade, of suffering as the “fat one.” A new outfit and a look in the mirror can’t help but make them feel better ... in the short term anyway. We as physicians must shoulder some of the blame for focusing on weight. Our spoken or unspoken message has been “Lose weight and you will be healthier.” We may make our message sound more professional by tossing around terms like “BMI,” but as Dr. Stanford points out, “we have known BMI is a flawed metric for a long time.”
There is the notion that obese people have had to build more muscle to help them carry around the extra weight, so that we should expect them to lose that extra muscle along with the fat. However, in older adults there is an entity called sarcopenic obesity, in which the patient doesn’t have that extra muscle to lose.
In a brief Internet research venture, I could find little on the subject of muscle loss and GLP-1s, other than “it can happen.” And, nothing on the effect in adolescents. And that is one of Dr. Stanford’s points. We just don’t know. She said that looking at body composition can be costly and not something that the clinician can do. However, as far as muscle mass is concerned, we need to be alert to the potential for loss. Simple assessments of strength can help us tailor our management to the specific patient’s need.
The bottom line is this ... now that we have effective medications for “weight loss,” we need to redefine the relationship between weight and health. “We” means us as clinicians. It means the folks at FDA. And, if we can improve our messaging, it will osmose to the rest of the population. Just because you’ve dropped two dress sizes doesn’t mean you’re healthy.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
What is the Best Approach to “Sinus Headaches”?
A 27-year-old woman presents requesting antibiotics for a sinus headache. She reports she has had 3-4 episodes a year with pain in her maxillary area and congestion. She has not had fevers with these episodes. She had the onset of this headache 6 hours ago. She has had resolution of the pain within 24 hours in the past with the use of antibiotics and decongestants. What would be the best treatment for her?
A. Amoxicillin
B. Amoxicillin/clavulanate
C. Amoxicillin + fluticasone nasal spray
D. Sumatriptan
The best treatment would be sumatriptan. This is very likely a variant of migraine headache and migraine-directed therapy is the best option. In regard to sinus headache, the International Headache Society (IHS) classification states that chronic sinusitis is not a cause of headache and facial pain unless it relapses into an acute sinusitis.1
The recurrent nature of the headaches in this patient suggests a primary headache disorder with migraine being the most likely. In a study of 2991 patients with self-diagnosed or physician-diagnosed “sinus headaches,” 88% of the patients met IHS criteria for migraine.2 In this study, most of the patients had symptoms suggesting sinus problems, with the most common symptoms being sinus pressure (84%), sinus pain (82%), and nasal congestion (63%). The likely cause for these symptoms in migraine patients is vasodilation of the nasal mucosa that can be part of the migraine event.
Foroughipour and colleagues found similar results.3 In their study, 58 patients with “sinus headache” were evaluated, with the final diagnosis of migraine in 40 patients (69%), tension-type headache in 16 patients (27%), and chronic sinusitis with recurrent acute episodes in 2 patients (3%). Recurrent antibiotic therapy had been given to 73% of the tension-type headache patients and 66% of the migraine patients.
Obermann et al. looked at how common trigeminal autonomic symptoms were in patients with migraine in a population-based study.4 They found of 841 patients who had migraine, 226 reported accompanying unilateral trigeminal autonomic symptoms (26.9%).
Al-Hashel et al. reported on how patients with frequent migraine are misdiagnosed and how long it takes when they present with sinus symptoms. A total of 130 migraine patients were recruited for the study; of these, 81.5% were misdiagnosed with sinusitis. The mean time delay of migraine diagnosis was almost 8 years.5
In a study by Dr. Elina Kari and Dr. John M. DelGaudio, patients who had a history of “sinus headaches” were treated as though all these headaches were migraines. Fifty-four patients were enrolled, and 38 patients completed the study. All patients had nasal endoscopy and sinus CT scans that were negative. They were then given migraine-directed treatment to use for their headaches. Of the 38 patient who completed the study, 31 patients (82%) had a significant reduction in headache pain with triptan use, and 35 patients (92%) had a significant response to migraine-directed therapy.6 An expert panel consisting of otolaryngologists, neurologists, allergists, and primary care physicians concluded that the majority of sinus headaches can actually be classified as migraines.7
These references aren’t new. This information has been known in the medical literature for more than 2 decades, but I believe that the majority of medical professionals are not aware of it. In my own practice I have found great success treating patients with sinus headache histories with migraine-directed therapy (mostly triptans) when they have return of their headaches.
Pearl: When your patients say they have another sinus headache, think migraine.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Jones NS. Expert Rev Neurother. 2009;9:439-44.
2. Schreiber CP et al. Arch Intern Med. 2004;164:1769-72.
3. Foroughipour M et al. Eur Arch Otorhinolaryngol. 2011;268:1593-6.
4. Obermann M et al. Cephalalgia. 2007 Jun;27(6):504-9.
5. Al-Hashel JY et al. J Headache Pain. 2013 Dec 12;14(1):97.
6. Kari E and DelGaudi JM. Laryngoscope. 2008;118:2235-9.
7. Levine HL et al. Otolaryngol Head Neck Surg. 2006 Mar;134(3):516-23.
A 27-year-old woman presents requesting antibiotics for a sinus headache. She reports she has had 3-4 episodes a year with pain in her maxillary area and congestion. She has not had fevers with these episodes. She had the onset of this headache 6 hours ago. She has had resolution of the pain within 24 hours in the past with the use of antibiotics and decongestants. What would be the best treatment for her?
A. Amoxicillin
B. Amoxicillin/clavulanate
C. Amoxicillin + fluticasone nasal spray
D. Sumatriptan
The best treatment would be sumatriptan. This is very likely a variant of migraine headache and migraine-directed therapy is the best option. In regard to sinus headache, the International Headache Society (IHS) classification states that chronic sinusitis is not a cause of headache and facial pain unless it relapses into an acute sinusitis.1
The recurrent nature of the headaches in this patient suggests a primary headache disorder with migraine being the most likely. In a study of 2991 patients with self-diagnosed or physician-diagnosed “sinus headaches,” 88% of the patients met IHS criteria for migraine.2 In this study, most of the patients had symptoms suggesting sinus problems, with the most common symptoms being sinus pressure (84%), sinus pain (82%), and nasal congestion (63%). The likely cause for these symptoms in migraine patients is vasodilation of the nasal mucosa that can be part of the migraine event.
Foroughipour and colleagues found similar results.3 In their study, 58 patients with “sinus headache” were evaluated, with the final diagnosis of migraine in 40 patients (69%), tension-type headache in 16 patients (27%), and chronic sinusitis with recurrent acute episodes in 2 patients (3%). Recurrent antibiotic therapy had been given to 73% of the tension-type headache patients and 66% of the migraine patients.
Obermann et al. looked at how common trigeminal autonomic symptoms were in patients with migraine in a population-based study.4 They found of 841 patients who had migraine, 226 reported accompanying unilateral trigeminal autonomic symptoms (26.9%).
Al-Hashel et al. reported on how patients with frequent migraine are misdiagnosed and how long it takes when they present with sinus symptoms. A total of 130 migraine patients were recruited for the study; of these, 81.5% were misdiagnosed with sinusitis. The mean time delay of migraine diagnosis was almost 8 years.5
In a study by Dr. Elina Kari and Dr. John M. DelGaudio, patients who had a history of “sinus headaches” were treated as though all these headaches were migraines. Fifty-four patients were enrolled, and 38 patients completed the study. All patients had nasal endoscopy and sinus CT scans that were negative. They were then given migraine-directed treatment to use for their headaches. Of the 38 patient who completed the study, 31 patients (82%) had a significant reduction in headache pain with triptan use, and 35 patients (92%) had a significant response to migraine-directed therapy.6 An expert panel consisting of otolaryngologists, neurologists, allergists, and primary care physicians concluded that the majority of sinus headaches can actually be classified as migraines.7
These references aren’t new. This information has been known in the medical literature for more than 2 decades, but I believe that the majority of medical professionals are not aware of it. In my own practice I have found great success treating patients with sinus headache histories with migraine-directed therapy (mostly triptans) when they have return of their headaches.
Pearl: When your patients say they have another sinus headache, think migraine.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Jones NS. Expert Rev Neurother. 2009;9:439-44.
2. Schreiber CP et al. Arch Intern Med. 2004;164:1769-72.
3. Foroughipour M et al. Eur Arch Otorhinolaryngol. 2011;268:1593-6.
4. Obermann M et al. Cephalalgia. 2007 Jun;27(6):504-9.
5. Al-Hashel JY et al. J Headache Pain. 2013 Dec 12;14(1):97.
6. Kari E and DelGaudi JM. Laryngoscope. 2008;118:2235-9.
7. Levine HL et al. Otolaryngol Head Neck Surg. 2006 Mar;134(3):516-23.
A 27-year-old woman presents requesting antibiotics for a sinus headache. She reports she has had 3-4 episodes a year with pain in her maxillary area and congestion. She has not had fevers with these episodes. She had the onset of this headache 6 hours ago. She has had resolution of the pain within 24 hours in the past with the use of antibiotics and decongestants. What would be the best treatment for her?
A. Amoxicillin
B. Amoxicillin/clavulanate
C. Amoxicillin + fluticasone nasal spray
D. Sumatriptan
The best treatment would be sumatriptan. This is very likely a variant of migraine headache and migraine-directed therapy is the best option. In regard to sinus headache, the International Headache Society (IHS) classification states that chronic sinusitis is not a cause of headache and facial pain unless it relapses into an acute sinusitis.1
The recurrent nature of the headaches in this patient suggests a primary headache disorder with migraine being the most likely. In a study of 2991 patients with self-diagnosed or physician-diagnosed “sinus headaches,” 88% of the patients met IHS criteria for migraine.2 In this study, most of the patients had symptoms suggesting sinus problems, with the most common symptoms being sinus pressure (84%), sinus pain (82%), and nasal congestion (63%). The likely cause for these symptoms in migraine patients is vasodilation of the nasal mucosa that can be part of the migraine event.
Foroughipour and colleagues found similar results.3 In their study, 58 patients with “sinus headache” were evaluated, with the final diagnosis of migraine in 40 patients (69%), tension-type headache in 16 patients (27%), and chronic sinusitis with recurrent acute episodes in 2 patients (3%). Recurrent antibiotic therapy had been given to 73% of the tension-type headache patients and 66% of the migraine patients.
Obermann et al. looked at how common trigeminal autonomic symptoms were in patients with migraine in a population-based study.4 They found of 841 patients who had migraine, 226 reported accompanying unilateral trigeminal autonomic symptoms (26.9%).
Al-Hashel et al. reported on how patients with frequent migraine are misdiagnosed and how long it takes when they present with sinus symptoms. A total of 130 migraine patients were recruited for the study; of these, 81.5% were misdiagnosed with sinusitis. The mean time delay of migraine diagnosis was almost 8 years.5
In a study by Dr. Elina Kari and Dr. John M. DelGaudio, patients who had a history of “sinus headaches” were treated as though all these headaches were migraines. Fifty-four patients were enrolled, and 38 patients completed the study. All patients had nasal endoscopy and sinus CT scans that were negative. They were then given migraine-directed treatment to use for their headaches. Of the 38 patient who completed the study, 31 patients (82%) had a significant reduction in headache pain with triptan use, and 35 patients (92%) had a significant response to migraine-directed therapy.6 An expert panel consisting of otolaryngologists, neurologists, allergists, and primary care physicians concluded that the majority of sinus headaches can actually be classified as migraines.7
These references aren’t new. This information has been known in the medical literature for more than 2 decades, but I believe that the majority of medical professionals are not aware of it. In my own practice I have found great success treating patients with sinus headache histories with migraine-directed therapy (mostly triptans) when they have return of their headaches.
Pearl: When your patients say they have another sinus headache, think migraine.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Jones NS. Expert Rev Neurother. 2009;9:439-44.
2. Schreiber CP et al. Arch Intern Med. 2004;164:1769-72.
3. Foroughipour M et al. Eur Arch Otorhinolaryngol. 2011;268:1593-6.
4. Obermann M et al. Cephalalgia. 2007 Jun;27(6):504-9.
5. Al-Hashel JY et al. J Headache Pain. 2013 Dec 12;14(1):97.
6. Kari E and DelGaudi JM. Laryngoscope. 2008;118:2235-9.
7. Levine HL et al. Otolaryngol Head Neck Surg. 2006 Mar;134(3):516-23.
AI for Email Replies? Not Yet
An article in the March 20 JAMA Network Open looked into the use of AI for responding to patient emails. Basically, they found that this led to a reduction in physician burden, but didn’t save any time.
1. Not sure that’s worth the trouble.
2. Unless the AI is simply responding with something like “message received, thank you” I don’t think this is a good idea.
Yeah, we’re all stretched for time, I understand that. From the starting gun each morning we’re racing between patients, phone calls, incoming test results, staff questions, drug reps, sample closets, dictations, and a million other things.
But
Someday, yeah, maybe it can do this, like 2-1B, the surgical droid that replaced Luke’s hand in “The Empire Strikes Back.” But we’re not even close to that. Just because a log-in screen says “Jumping to Hyperspace” doesn’t mean you’re on the Millennium Falcon.
I generally know my patients, but even if I don’t remember them, I can quickly look up their charts and decide how to answer. AI can look up charts, too, but data is only a part of medicine.
There are a lot of things that don’t make it into a chart: our impressions of people and a knowledge of their personalities and anxieties. We take these into account when responding to their questions. People are different in how things need to be said to them, even if the answer is, overall, the same.
“It’s the AI’s fault” isn’t going to stand up in court, either.
I also have to question the benefit of the findings. If it lessens the “click burden” but still takes the same amount of time, are we really gaining anything?
I’m all for the digital age. In many ways it’s made my practice a lot easier. But I think it has a way to go before I let it start dealing directly with patients.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
An article in the March 20 JAMA Network Open looked into the use of AI for responding to patient emails. Basically, they found that this led to a reduction in physician burden, but didn’t save any time.
1. Not sure that’s worth the trouble.
2. Unless the AI is simply responding with something like “message received, thank you” I don’t think this is a good idea.
Yeah, we’re all stretched for time, I understand that. From the starting gun each morning we’re racing between patients, phone calls, incoming test results, staff questions, drug reps, sample closets, dictations, and a million other things.
But
Someday, yeah, maybe it can do this, like 2-1B, the surgical droid that replaced Luke’s hand in “The Empire Strikes Back.” But we’re not even close to that. Just because a log-in screen says “Jumping to Hyperspace” doesn’t mean you’re on the Millennium Falcon.
I generally know my patients, but even if I don’t remember them, I can quickly look up their charts and decide how to answer. AI can look up charts, too, but data is only a part of medicine.
There are a lot of things that don’t make it into a chart: our impressions of people and a knowledge of their personalities and anxieties. We take these into account when responding to their questions. People are different in how things need to be said to them, even if the answer is, overall, the same.
“It’s the AI’s fault” isn’t going to stand up in court, either.
I also have to question the benefit of the findings. If it lessens the “click burden” but still takes the same amount of time, are we really gaining anything?
I’m all for the digital age. In many ways it’s made my practice a lot easier. But I think it has a way to go before I let it start dealing directly with patients.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
An article in the March 20 JAMA Network Open looked into the use of AI for responding to patient emails. Basically, they found that this led to a reduction in physician burden, but didn’t save any time.
1. Not sure that’s worth the trouble.
2. Unless the AI is simply responding with something like “message received, thank you” I don’t think this is a good idea.
Yeah, we’re all stretched for time, I understand that. From the starting gun each morning we’re racing between patients, phone calls, incoming test results, staff questions, drug reps, sample closets, dictations, and a million other things.
But
Someday, yeah, maybe it can do this, like 2-1B, the surgical droid that replaced Luke’s hand in “The Empire Strikes Back.” But we’re not even close to that. Just because a log-in screen says “Jumping to Hyperspace” doesn’t mean you’re on the Millennium Falcon.
I generally know my patients, but even if I don’t remember them, I can quickly look up their charts and decide how to answer. AI can look up charts, too, but data is only a part of medicine.
There are a lot of things that don’t make it into a chart: our impressions of people and a knowledge of their personalities and anxieties. We take these into account when responding to their questions. People are different in how things need to be said to them, even if the answer is, overall, the same.
“It’s the AI’s fault” isn’t going to stand up in court, either.
I also have to question the benefit of the findings. If it lessens the “click burden” but still takes the same amount of time, are we really gaining anything?
I’m all for the digital age. In many ways it’s made my practice a lot easier. But I think it has a way to go before I let it start dealing directly with patients.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.









