User login
Making a case for patient-reported outcomes in clinical inflammatory bowel disease practice
Patients seek medical care when they perceive a deterioration in their health. Gastroenterologists and health care providers are trained to seek out clinical, laboratory, radiologic, and endoscopic evidence of pathology. Conventional endpoints in inflammatory bowel disease (IBD) clinical trials and clinical care may fail to capture the full health status and disease experience from the patient perspective. The Food and Drug Administration has called for the development of coprimary endpoints in research trials to include an objective measure of inflammation in conjunction with patient-reported outcomes (PROs). The objective is to support labeling claims and improve safety and effectiveness in the drug approval process.1,2 There is also growing recognition that high-value care includes management of biologic and psychosocial factors to enable patients with chronic diseases to regain their health. Clinicians might follow suit by incorporating valid, reliable PRO measures to usual IBD care in order better to achieve patient-centered care, inform decision making, and improve the care provided.
What are patient-reported outcomes?
The FDA defines a PRO as “any report of the status of a patient’s health condition that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else.” Two PROs are used to measure various aspects of health including physical, emotional, or social domains. PROs have emerged as tools that may foster a better understanding of the patient’s condition, which may go beyond disease activity or symptoms. In effect, incorporating PROs into clinical practice enables a model of “coproduction” of health care, and may contribute to a more reciprocal patient-provider interaction where the needs of the patient may be more fully understood and incorporated into decision-making that may lead to improved patient satisfaction and outcomes.3,4
There are hundreds of available PROs in gastroenterology,5 ranging from simple (characterizing pain with a basic numeric rating scale) to complex multidomain, multi-item instruments. PROs may cover symptom assessment, health-related quality of life, and adherence to and satisfaction with treatment, and may be generic or disease specific. Numerous PROs have been developed for patients with IBD. Commonly used PROs in IBD include severity scales for pain, defecatory urgency, and bloody stool, and several disease-specific and generic instruments assessing different health-related quality-of-life domains have been used in research studies for patients with IBD.
The current approach to patient-centered care for IBD is limited
IBD is a difficult disease to manage – in part because there is no known biomarker that accurately reflects the full spectrum of disease activity. Numerous indices have been developed to better quantify disease activity and measure response to treatment. Among the most frequently used indices in clinical trials are the Crohn’s Disease Activity Index (CDAI) and (for ulcerative colitis [UC]) the Mayo Clinic Score. These endpoints incorporate signs and symptoms, laboratory findings (in the CDAI), and endoscopic assessments. The CDAI is a suboptimal instrument because of a lack of correlation with endoscopic inflammation and potential confounding with concomitant gastrointestinal illnesses, such as irritable bowel syndrome.6 The Mayo Clinic Score is difficult to interpret because of some subjective elements (what is considered a normal number of stools per day?); vagueness (mostly bloody stools more than half the time?); and need for a physician assessment, which often does not correspond with the patient’s perception of their disease.7 From a research perspective, this disconnect can compromise the quality of trial data. Clinically, it can negatively impact patients’ satisfaction and impair the patient-provider relationship.8
To that end, regulatory agencies, scientific bodies, and health care payors are shifting toward a more “patient-centered” approach with an emphasis on PROs. However, although the FDA is incorporating the patient perspective in its trials, measuring meaningful outcomes in day-to-day clinical care is challenging. In the absence of active inflammation, more than 30% of patients with IBD still suffer from gastrointestinal symptoms.9 Furthermore, physicians frequently underestimate the effect of depression, anxiety, fatigue, and sleep on patient health. Likewise, some patients with active small-bowel Crohn’s disease (CD) may experience few gastrointestinal symptoms but have profound fatigue, weight loss, and impaired quality of life. A focused assessment for disease activity may fail to identify aspects of health most relevant or important to individual patient well-being. There is a need for effective, efficient, and standardized strategies to better understand the concerns of the individual seeking help.
Although there are several PROs that measure disease activity primarily for clinical research trials,10 their prevalence in gastroenterology practices has not been assessed. Most likely, few clinical practices currently integrate standardized PROs in routine patient care. This may be because of several reasons, including lack of awareness of newly developed PROs, administrative burden including time and resources to collect PROs, potentially complex interpretation of results, and perhaps a reluctance among physicians to alter traditional patient interview methods of obtaining information about the health status of their patients. For effective use in clinical care, PROs require simple and relevant interpretation to add value to the clinician’s practice, and must minimally impact clinical flow and resources. The use of Internet-enabled tablets has been shown to be a feasible, efficient, and effective means of PRO assessment in gastroenterology practices, with good levels of patient satisfaction.11
Reaping potential benefits of patient-reported outcomes
The National Institutes of Health Patient-Reported Outcomes Measurement Information System (PROMIS) is an initiative developed to investigate and promote implementation of PRO measures among patients with chronic diseases. The collection of PROMIS measures has been shown to be feasible at a tertiary care IBD center, enabling a biopsychosocial model of care.12 Likewise, implementation of PROs in other clinical areas including oncology, orthopedics, and rheumatology has been robust.
In an innovative orthopedic study, PROMIS measures collected and linked to the electronic medical record predicted the likelihood of a clinically meaningful benefit from foot and ankle surgery.13 This facilitated tailored patient-specific preoperative discussions about the expected benefit of surgery. In a study at a rheumatology clinic patients with rheumatoid arthritis were asked to identify their highest priority treatment targets using PROMIS domains (fatigue, pain, depression, social function). The highest priority domain was tracked over time as a patient-centered marker of health, essentially personalizing measures of success for the individual patient.14
PROs have the unique potential to affect multiple levels of health care. At the patient level, PRO data can identify specific concerns, manage expectations of recovery, and tailor treatment decisions to personal preference. At the population level, PRO data can be used to standardize aspects of care to understand comparative health and disease among all patients in a practice or relative to outside practices, identify outliers, and drive improvement.
Optimizing PROs for use in clinical trials: CD–PROs and UC–PROs
Developing standardized, validated instruments according to FDA guidance is a complex process. The lack of an FDA-approved PRO has resulted in substantial variability in the definitions of clinical response or remission in clinical trials to date.15 As a result, IBD-specific PROs (CD-PRO and UC-PRO) are being developed under FDA guidance for use in clinical trials.16 With achievement of prequalification for open use, UC-PRO and CD-PRO will cover five IBD-specific outcomes domains or modules: 1) bowel signs and symptoms, 2) systemic symptoms, 3) emotional impact, 4) coping behaviors, and 5) IBD impact on daily life. The bowel signs and symptoms module may also incorporate a functional impact assessment. Each module includes numerous pertinent items (e.g., “I feel worried,” “I feel scared,” “I feel alone” in the emotional impact module) and are currently being tailored and scored for practicality and relevance. It is hoped that UC-PRO and CD-PRO in final form will be relevant and applicable for clinical trials and gastroenterology practices alike.
Because the development of the UC-PRO and the CD-PRO is still underway, interim PROs are being used in ongoing clinical trials. These interim measures were extracted from existing components of the CDAI, Mayo Clinic Score, and UC Disease Activity Index. The CD PRO-2 consists of two items: abdominal pain and stool frequency. The UC PRO-2 is composed of rectal bleeding and stool frequency. The PRO-3 adds an item regarding general well-being. The sensitivity of these PROs was tested in studies for CD and UC. Both PROs performed similarly to their respective parent instrument. Important limitations include the lack of validation, and the fact that these interim measures were derived from parent measures with acknowledged limitations as previously discussed. Current clinical trials are coupling these interim measures with endoscopic data as coprimary endpoints.
PROs in routine clinical practice: Are we ready for prime time?
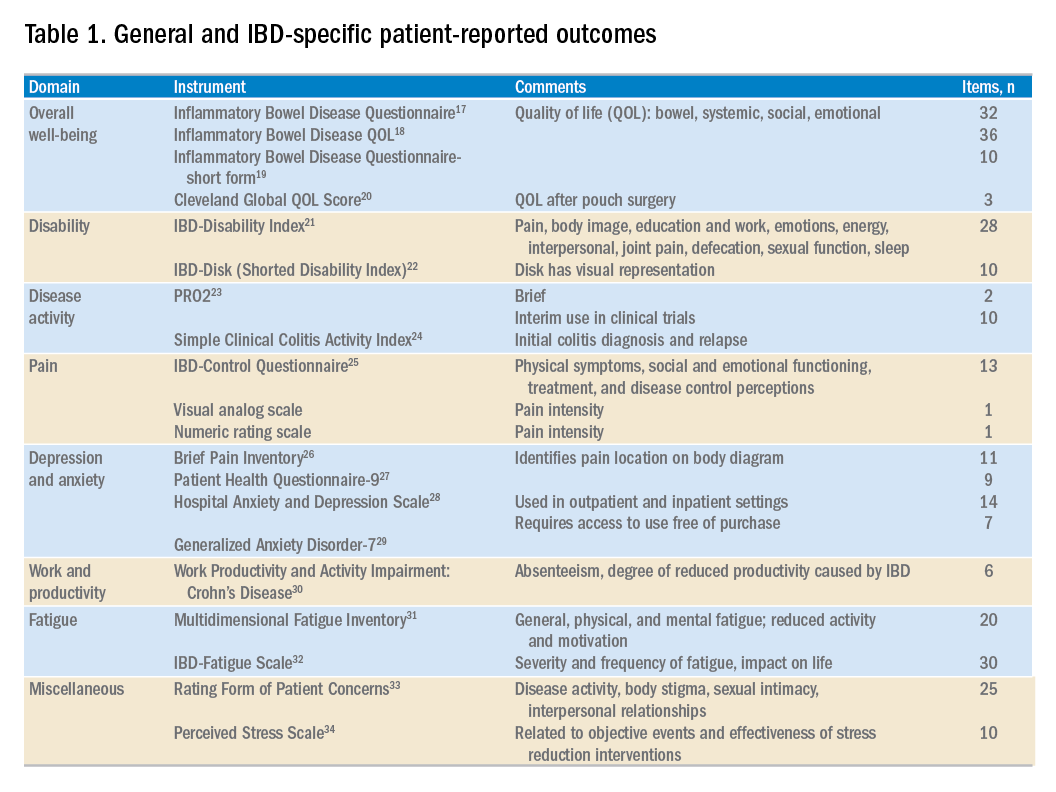
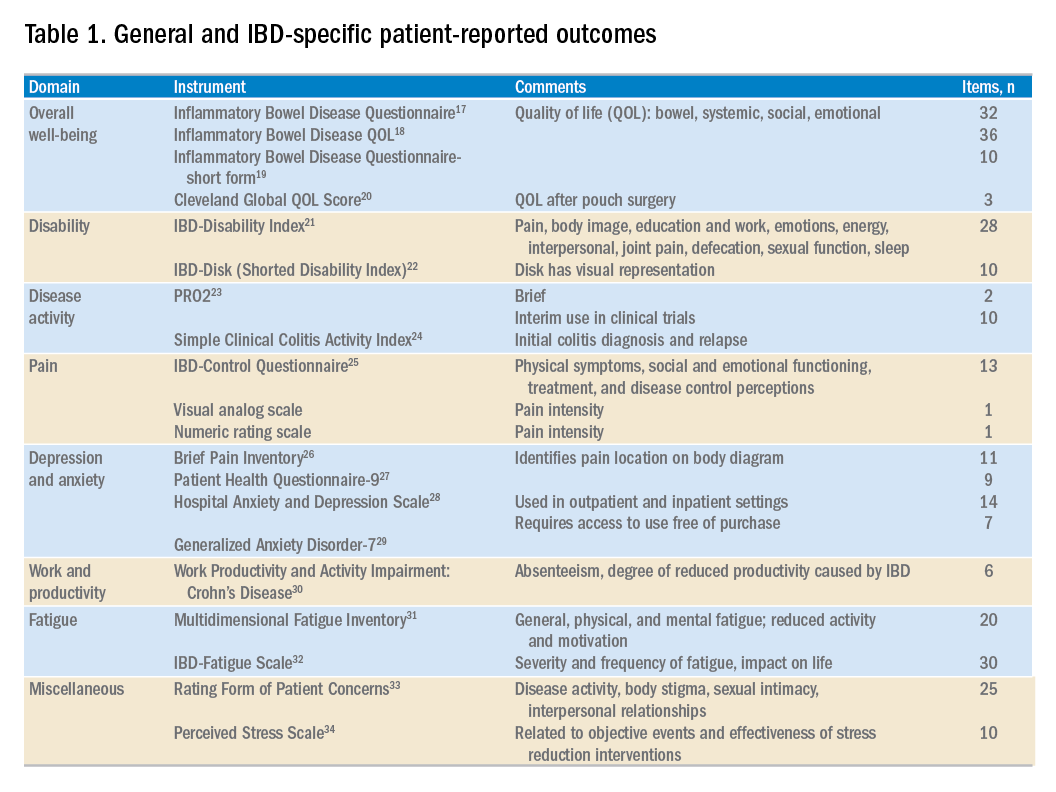
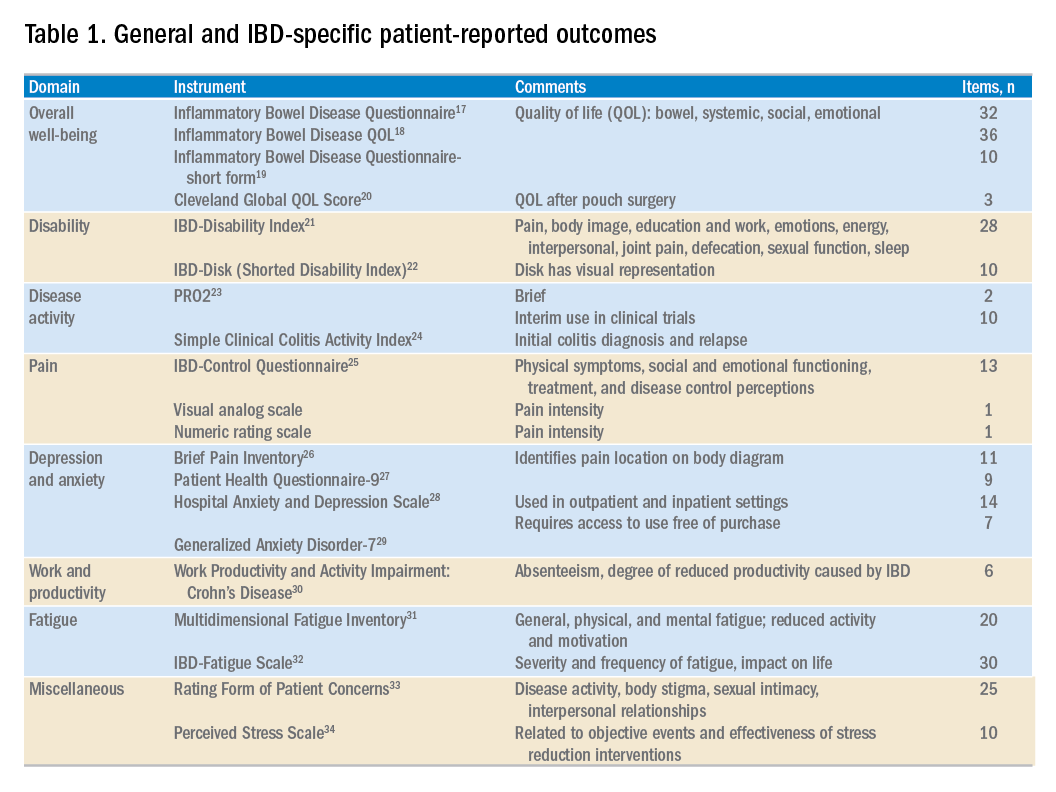
Few instruments developed to date have been widely implemented into routine IBD clinical practice. Table 1 highlights commonly available or recently developed PROs for IBD care. As clinicians strive to more effectively integrate PROs into clinical practice, we propose a three-step process to getting started: 1) select and administer a PRO instrument, 2) identify areas of impairment and create a targeted treatment strategy to focus on those areas, and 3) repeat the same PRO at follow-up to assess for improvement. The instrument can be administered before the visit or in the clinic waiting room. Focus a portion of the patient’s visit on discussing the results and identifying one or more domains to target for improvement. For example, the patient may indicate diarrhea as his/her most important area to target, triggering a symptom-specific investigation and therapeutic approach. The PRO may also highlight social or emotional impairment that may require an ancillary referral. The benefits of this PRO-driven approach to IBD care are twofold. First, the patient’s primary concerns are positioned at the forefront of the clinical visit. Second, aligning the clinician’s focus with the patient input may actually help to streamline each visit and improve overall visit efficiency and patient satisfaction.
Conclusions
As therapies for IBD improve, so should standards of patient-centered care. Clinicians must actively seek and then listen to the concerns of patients and be able to address the multiple facets of living with a chronic disease. PROs empower patients, helping them identify important topics for discussion at the clinical visit. This affords clinicians a better understanding of primary patient concerns before the visit, and potentially improves the quality and value of care. At first, the process of incorporating PROs into a busy clinical practice may be challenging, but targeted treatment plans have the potential to foster a better patient – and physician – experience.
Content from this column was originally published in the “Practice Management: The Road Ahead” section of Clinical Gastroenterology and Hepatology (2018;16[5]:603-7).
References
1. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes. 2006;4:79.
2. Burke, L.B., Kennedy, D.L., Miskala, P.H., et al. The use of patient-reported outcome measures in the evaluation of medical products for regulatory approval. Clin Pharmacol Ther. 2008;84:281-3.
3. Batalden, M., Baltalden, P., Margolis, P., et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;25:509-17.
4. Johnson, L.C. Melmed, G.Y., Nelson, E.C., et al. Fostering collaboration through creation of an IBD learning health system. Am J Gastroenterol. 2017;112:406-8.
5. Khanna, P., Agarwal, N., Khanna, D., et al. Development of an online library of patient reported outcome measures in gastroenterology: the GI-PRO database. Am J Gastroenterol. 2014;109:234-48.
6. Bruining, D.H. Sandborn, W.J. Do not assume symptoms indicate failure of anti-tumor necrosis factor therapy in January 2015 Emerging Treatment Goals in IBD Trials and Practice 45 REVIEWS AND PERSPECTIVES Crohn’s disease. Clin Gastroenterol Hepatol. 2011;9:395-9.
7. Surti, B., Spiegel, B., Ippoliti, A., et al. Assessing health status in inflammatory bowel disease using a novel single-item numeric rating scale. Dig Dis Sci. 2013;58:1313-21.
8. Marshall, S., Haywood, K. Fitzpatrick R. Impact of patient-reported outcome measures on routine practice: a structured review. J Eval Clin Pract. 2006;12:559-68.
9. Simren, M., Axelsson, J., Gillberg, R., et al. Quality of life in inflammatory bowel disease in remission: the impact of IBD-like symptoms and associated psychological factors. Am J Gastroenterol. 2002;97:389-96.
10. De Jong, M.J., Huibregtse, R., Masclee, A.A.M., et al. Patient-reported outcome measures for use in clinical trials and clinical practice in inflammatory bowel diseases: a systematic review. Clin Gastroenterol Hepatol. 2018;16:648-63.
11. Atreja, A., Rizk, M. Capturing patient reported outcomes and quality of life in routine clinical practice: ready to prime time? Minerva Gastroenterol Dietol. 2012;58:19-24.
12. Ishak, W.W., Pan, D., Steiner, A.J., et al. Patient reported outcomes of quality of life, functioning, and GI/psychiatric symptom severity in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2017;23:798-803.
13. Ho, B., Houck, J.R., Flemister, A.S., et al. Preoperative PROMIS scores predict postoperative success in foot and ankle patients. Foot Ankle Int. 2016;37:911-8. 14. Bacalao, E., Greene, G.J., Beaumont, J.L., et al. Standardizing and personalizing the treat to target (T2T) approach for rheumatoid arthritis using the Patient-Reported Outcomes Measurement Information System (PROMIS): baseline findings on patient-centered treatment priorities. Clin Rheumatol. 2017;36:1729-36.
15. Ma, C., Panaccione, R., Fedorak, R.N., et al. Heterogeneity in definitions of endpoints for clinical trials of ulcerative colitis: a systematic review for development of a core outcome set. Clin Gastroenterol Hepatol. 2018;16:637-47.
16. Higgins P. Patient reported outcomes in IBD 2017. Available at: ibdctworkshop.files.wordpress.com/2017/01/patient-reported-outcomes-in-ibd___peter-higgins.pdf. Accessed Aug. 27, 2017.
17. Guyatt, G., Mitchell, A. Irvine, E.J., et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989;96:804-10.
18. Love, J.R., Irvine, E.J., Fedorak, R.N. Quality of life in inflammatory bowel disease. J Clin Gastroenterol. 1992;14:15-9.
19. Irvine, E.J., Zhou, Q., Thompson, A.K. The short inflammatory bowel disease questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT investigators. Canadian Crohn’s Relapse Prevention Trial. Am J Gastroenterol. 1996;91:1571-8.
20. Fazio, V.W., O’Riordain, M.G., Lavery, I.C., et al. Long-term functional outcome and quality of life after stapled restorative proctocolectomy. Ann Surg. 1999;230:575-84.
21. Gower-Rousseau, C., Sarter, H., Savoye, G., et al. Validation of the inflammatory bowel disease disability index in a population-based cohort. Gut. 2017;66:588-96.
22. Gosh, S., Louis, E., Beaugerie, L., et al. Development of the IBD-Disk: a visual self-administered tool assessing disability in inflammatory bowel diseases. Inflamm Bowel Dis. 2017;23:333-40.
23. Khanna, R., Zou, G., D’Haens, G., et al. A retrospective analysis: the development of patient reported outcome measures for the assessment of Crohn’s disease activity. Aliment Pharmacol Ther. 2015;41:77-86.
24. Walmsley, R.S., Ayres, R.C.S., Pounder, P.R., et al. A simple clinical colitis activity index. Gut. 1998;43:29-32.
25. Bodger, K., Ormerod, C., Shackcloth, D., et al. Development and validation of a rapid, general measure of disease control from the patient perspective: the IBD-Control questionnaire. Gut. 2014;63:1092-102.
26. Cleeland, C.S., Ryan, K.M. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129-38.
27. Kroenke, K., Spitzer, R.L., Williams, J.B.W. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-13.
28. Zigmond, A.S., Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361-70.
29. Spitzer, R.L., Korneke, K., Williams, J.B., et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092-7.
30. Reilly, M.C., Zbrozek, A.S. Dukes, E.M. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmachoeconomics. 1993;4:353-65.
31. Smets, E.M., Garssen, B. Bonke, B., et al. The Multidimensional Fatigue Inventory psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995;39:315-25.
32. Czuber-Dochan, W., Norton, C., Bassettt, P., et al. Development and psychometric testing of inflammatory bowel disease fatigue (IBD-F) patient self-assessment scale. J Crohns Colitis. 2014;8:1398-406.
33. Drossman, D.A., Leserman, J., Li, Z.M., et al. The rating form of IBD patient concerns: a new measure of health status. Psychosom Med. 1991;53:701-12. 34. Cohen, S., Kamarck, T., Mermelstein, R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385-96.
Dr. Cohen is in the division of digestive and liver diseases; Dr. Melmed is director, clinical inflammatory bowel disease, director, clinical research in the division of gastroenterology, and director, advanced inflammatory bowel disease fellowship program, Cedars-Sinai Medical Center, Los Angeles. Dr. Melmed is a consultant for AbbVie, Boehringer Ingelheim, Celgene, Genentech, Janssen, Pfizer, Samsung Bioepis, Takeda, and UCB; and received support for research from Prometheus Labs. The remaining author discloses no conflicts.
Patients seek medical care when they perceive a deterioration in their health. Gastroenterologists and health care providers are trained to seek out clinical, laboratory, radiologic, and endoscopic evidence of pathology. Conventional endpoints in inflammatory bowel disease (IBD) clinical trials and clinical care may fail to capture the full health status and disease experience from the patient perspective. The Food and Drug Administration has called for the development of coprimary endpoints in research trials to include an objective measure of inflammation in conjunction with patient-reported outcomes (PROs). The objective is to support labeling claims and improve safety and effectiveness in the drug approval process.1,2 There is also growing recognition that high-value care includes management of biologic and psychosocial factors to enable patients with chronic diseases to regain their health. Clinicians might follow suit by incorporating valid, reliable PRO measures to usual IBD care in order better to achieve patient-centered care, inform decision making, and improve the care provided.
What are patient-reported outcomes?
The FDA defines a PRO as “any report of the status of a patient’s health condition that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else.” Two PROs are used to measure various aspects of health including physical, emotional, or social domains. PROs have emerged as tools that may foster a better understanding of the patient’s condition, which may go beyond disease activity or symptoms. In effect, incorporating PROs into clinical practice enables a model of “coproduction” of health care, and may contribute to a more reciprocal patient-provider interaction where the needs of the patient may be more fully understood and incorporated into decision-making that may lead to improved patient satisfaction and outcomes.3,4
There are hundreds of available PROs in gastroenterology,5 ranging from simple (characterizing pain with a basic numeric rating scale) to complex multidomain, multi-item instruments. PROs may cover symptom assessment, health-related quality of life, and adherence to and satisfaction with treatment, and may be generic or disease specific. Numerous PROs have been developed for patients with IBD. Commonly used PROs in IBD include severity scales for pain, defecatory urgency, and bloody stool, and several disease-specific and generic instruments assessing different health-related quality-of-life domains have been used in research studies for patients with IBD.
The current approach to patient-centered care for IBD is limited
IBD is a difficult disease to manage – in part because there is no known biomarker that accurately reflects the full spectrum of disease activity. Numerous indices have been developed to better quantify disease activity and measure response to treatment. Among the most frequently used indices in clinical trials are the Crohn’s Disease Activity Index (CDAI) and (for ulcerative colitis [UC]) the Mayo Clinic Score. These endpoints incorporate signs and symptoms, laboratory findings (in the CDAI), and endoscopic assessments. The CDAI is a suboptimal instrument because of a lack of correlation with endoscopic inflammation and potential confounding with concomitant gastrointestinal illnesses, such as irritable bowel syndrome.6 The Mayo Clinic Score is difficult to interpret because of some subjective elements (what is considered a normal number of stools per day?); vagueness (mostly bloody stools more than half the time?); and need for a physician assessment, which often does not correspond with the patient’s perception of their disease.7 From a research perspective, this disconnect can compromise the quality of trial data. Clinically, it can negatively impact patients’ satisfaction and impair the patient-provider relationship.8
To that end, regulatory agencies, scientific bodies, and health care payors are shifting toward a more “patient-centered” approach with an emphasis on PROs. However, although the FDA is incorporating the patient perspective in its trials, measuring meaningful outcomes in day-to-day clinical care is challenging. In the absence of active inflammation, more than 30% of patients with IBD still suffer from gastrointestinal symptoms.9 Furthermore, physicians frequently underestimate the effect of depression, anxiety, fatigue, and sleep on patient health. Likewise, some patients with active small-bowel Crohn’s disease (CD) may experience few gastrointestinal symptoms but have profound fatigue, weight loss, and impaired quality of life. A focused assessment for disease activity may fail to identify aspects of health most relevant or important to individual patient well-being. There is a need for effective, efficient, and standardized strategies to better understand the concerns of the individual seeking help.
Although there are several PROs that measure disease activity primarily for clinical research trials,10 their prevalence in gastroenterology practices has not been assessed. Most likely, few clinical practices currently integrate standardized PROs in routine patient care. This may be because of several reasons, including lack of awareness of newly developed PROs, administrative burden including time and resources to collect PROs, potentially complex interpretation of results, and perhaps a reluctance among physicians to alter traditional patient interview methods of obtaining information about the health status of their patients. For effective use in clinical care, PROs require simple and relevant interpretation to add value to the clinician’s practice, and must minimally impact clinical flow and resources. The use of Internet-enabled tablets has been shown to be a feasible, efficient, and effective means of PRO assessment in gastroenterology practices, with good levels of patient satisfaction.11
Reaping potential benefits of patient-reported outcomes
The National Institutes of Health Patient-Reported Outcomes Measurement Information System (PROMIS) is an initiative developed to investigate and promote implementation of PRO measures among patients with chronic diseases. The collection of PROMIS measures has been shown to be feasible at a tertiary care IBD center, enabling a biopsychosocial model of care.12 Likewise, implementation of PROs in other clinical areas including oncology, orthopedics, and rheumatology has been robust.
In an innovative orthopedic study, PROMIS measures collected and linked to the electronic medical record predicted the likelihood of a clinically meaningful benefit from foot and ankle surgery.13 This facilitated tailored patient-specific preoperative discussions about the expected benefit of surgery. In a study at a rheumatology clinic patients with rheumatoid arthritis were asked to identify their highest priority treatment targets using PROMIS domains (fatigue, pain, depression, social function). The highest priority domain was tracked over time as a patient-centered marker of health, essentially personalizing measures of success for the individual patient.14
PROs have the unique potential to affect multiple levels of health care. At the patient level, PRO data can identify specific concerns, manage expectations of recovery, and tailor treatment decisions to personal preference. At the population level, PRO data can be used to standardize aspects of care to understand comparative health and disease among all patients in a practice or relative to outside practices, identify outliers, and drive improvement.
Optimizing PROs for use in clinical trials: CD–PROs and UC–PROs
Developing standardized, validated instruments according to FDA guidance is a complex process. The lack of an FDA-approved PRO has resulted in substantial variability in the definitions of clinical response or remission in clinical trials to date.15 As a result, IBD-specific PROs (CD-PRO and UC-PRO) are being developed under FDA guidance for use in clinical trials.16 With achievement of prequalification for open use, UC-PRO and CD-PRO will cover five IBD-specific outcomes domains or modules: 1) bowel signs and symptoms, 2) systemic symptoms, 3) emotional impact, 4) coping behaviors, and 5) IBD impact on daily life. The bowel signs and symptoms module may also incorporate a functional impact assessment. Each module includes numerous pertinent items (e.g., “I feel worried,” “I feel scared,” “I feel alone” in the emotional impact module) and are currently being tailored and scored for practicality and relevance. It is hoped that UC-PRO and CD-PRO in final form will be relevant and applicable for clinical trials and gastroenterology practices alike.
Because the development of the UC-PRO and the CD-PRO is still underway, interim PROs are being used in ongoing clinical trials. These interim measures were extracted from existing components of the CDAI, Mayo Clinic Score, and UC Disease Activity Index. The CD PRO-2 consists of two items: abdominal pain and stool frequency. The UC PRO-2 is composed of rectal bleeding and stool frequency. The PRO-3 adds an item regarding general well-being. The sensitivity of these PROs was tested in studies for CD and UC. Both PROs performed similarly to their respective parent instrument. Important limitations include the lack of validation, and the fact that these interim measures were derived from parent measures with acknowledged limitations as previously discussed. Current clinical trials are coupling these interim measures with endoscopic data as coprimary endpoints.
PROs in routine clinical practice: Are we ready for prime time?
Few instruments developed to date have been widely implemented into routine IBD clinical practice. Table 1 highlights commonly available or recently developed PROs for IBD care. As clinicians strive to more effectively integrate PROs into clinical practice, we propose a three-step process to getting started: 1) select and administer a PRO instrument, 2) identify areas of impairment and create a targeted treatment strategy to focus on those areas, and 3) repeat the same PRO at follow-up to assess for improvement. The instrument can be administered before the visit or in the clinic waiting room. Focus a portion of the patient’s visit on discussing the results and identifying one or more domains to target for improvement. For example, the patient may indicate diarrhea as his/her most important area to target, triggering a symptom-specific investigation and therapeutic approach. The PRO may also highlight social or emotional impairment that may require an ancillary referral. The benefits of this PRO-driven approach to IBD care are twofold. First, the patient’s primary concerns are positioned at the forefront of the clinical visit. Second, aligning the clinician’s focus with the patient input may actually help to streamline each visit and improve overall visit efficiency and patient satisfaction.
Conclusions
As therapies for IBD improve, so should standards of patient-centered care. Clinicians must actively seek and then listen to the concerns of patients and be able to address the multiple facets of living with a chronic disease. PROs empower patients, helping them identify important topics for discussion at the clinical visit. This affords clinicians a better understanding of primary patient concerns before the visit, and potentially improves the quality and value of care. At first, the process of incorporating PROs into a busy clinical practice may be challenging, but targeted treatment plans have the potential to foster a better patient – and physician – experience.
Content from this column was originally published in the “Practice Management: The Road Ahead” section of Clinical Gastroenterology and Hepatology (2018;16[5]:603-7).
References
1. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes. 2006;4:79.
2. Burke, L.B., Kennedy, D.L., Miskala, P.H., et al. The use of patient-reported outcome measures in the evaluation of medical products for regulatory approval. Clin Pharmacol Ther. 2008;84:281-3.
3. Batalden, M., Baltalden, P., Margolis, P., et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;25:509-17.
4. Johnson, L.C. Melmed, G.Y., Nelson, E.C., et al. Fostering collaboration through creation of an IBD learning health system. Am J Gastroenterol. 2017;112:406-8.
5. Khanna, P., Agarwal, N., Khanna, D., et al. Development of an online library of patient reported outcome measures in gastroenterology: the GI-PRO database. Am J Gastroenterol. 2014;109:234-48.
6. Bruining, D.H. Sandborn, W.J. Do not assume symptoms indicate failure of anti-tumor necrosis factor therapy in January 2015 Emerging Treatment Goals in IBD Trials and Practice 45 REVIEWS AND PERSPECTIVES Crohn’s disease. Clin Gastroenterol Hepatol. 2011;9:395-9.
7. Surti, B., Spiegel, B., Ippoliti, A., et al. Assessing health status in inflammatory bowel disease using a novel single-item numeric rating scale. Dig Dis Sci. 2013;58:1313-21.
8. Marshall, S., Haywood, K. Fitzpatrick R. Impact of patient-reported outcome measures on routine practice: a structured review. J Eval Clin Pract. 2006;12:559-68.
9. Simren, M., Axelsson, J., Gillberg, R., et al. Quality of life in inflammatory bowel disease in remission: the impact of IBD-like symptoms and associated psychological factors. Am J Gastroenterol. 2002;97:389-96.
10. De Jong, M.J., Huibregtse, R., Masclee, A.A.M., et al. Patient-reported outcome measures for use in clinical trials and clinical practice in inflammatory bowel diseases: a systematic review. Clin Gastroenterol Hepatol. 2018;16:648-63.
11. Atreja, A., Rizk, M. Capturing patient reported outcomes and quality of life in routine clinical practice: ready to prime time? Minerva Gastroenterol Dietol. 2012;58:19-24.
12. Ishak, W.W., Pan, D., Steiner, A.J., et al. Patient reported outcomes of quality of life, functioning, and GI/psychiatric symptom severity in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2017;23:798-803.
13. Ho, B., Houck, J.R., Flemister, A.S., et al. Preoperative PROMIS scores predict postoperative success in foot and ankle patients. Foot Ankle Int. 2016;37:911-8. 14. Bacalao, E., Greene, G.J., Beaumont, J.L., et al. Standardizing and personalizing the treat to target (T2T) approach for rheumatoid arthritis using the Patient-Reported Outcomes Measurement Information System (PROMIS): baseline findings on patient-centered treatment priorities. Clin Rheumatol. 2017;36:1729-36.
15. Ma, C., Panaccione, R., Fedorak, R.N., et al. Heterogeneity in definitions of endpoints for clinical trials of ulcerative colitis: a systematic review for development of a core outcome set. Clin Gastroenterol Hepatol. 2018;16:637-47.
16. Higgins P. Patient reported outcomes in IBD 2017. Available at: ibdctworkshop.files.wordpress.com/2017/01/patient-reported-outcomes-in-ibd___peter-higgins.pdf. Accessed Aug. 27, 2017.
17. Guyatt, G., Mitchell, A. Irvine, E.J., et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989;96:804-10.
18. Love, J.R., Irvine, E.J., Fedorak, R.N. Quality of life in inflammatory bowel disease. J Clin Gastroenterol. 1992;14:15-9.
19. Irvine, E.J., Zhou, Q., Thompson, A.K. The short inflammatory bowel disease questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT investigators. Canadian Crohn’s Relapse Prevention Trial. Am J Gastroenterol. 1996;91:1571-8.
20. Fazio, V.W., O’Riordain, M.G., Lavery, I.C., et al. Long-term functional outcome and quality of life after stapled restorative proctocolectomy. Ann Surg. 1999;230:575-84.
21. Gower-Rousseau, C., Sarter, H., Savoye, G., et al. Validation of the inflammatory bowel disease disability index in a population-based cohort. Gut. 2017;66:588-96.
22. Gosh, S., Louis, E., Beaugerie, L., et al. Development of the IBD-Disk: a visual self-administered tool assessing disability in inflammatory bowel diseases. Inflamm Bowel Dis. 2017;23:333-40.
23. Khanna, R., Zou, G., D’Haens, G., et al. A retrospective analysis: the development of patient reported outcome measures for the assessment of Crohn’s disease activity. Aliment Pharmacol Ther. 2015;41:77-86.
24. Walmsley, R.S., Ayres, R.C.S., Pounder, P.R., et al. A simple clinical colitis activity index. Gut. 1998;43:29-32.
25. Bodger, K., Ormerod, C., Shackcloth, D., et al. Development and validation of a rapid, general measure of disease control from the patient perspective: the IBD-Control questionnaire. Gut. 2014;63:1092-102.
26. Cleeland, C.S., Ryan, K.M. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129-38.
27. Kroenke, K., Spitzer, R.L., Williams, J.B.W. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-13.
28. Zigmond, A.S., Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361-70.
29. Spitzer, R.L., Korneke, K., Williams, J.B., et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092-7.
30. Reilly, M.C., Zbrozek, A.S. Dukes, E.M. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmachoeconomics. 1993;4:353-65.
31. Smets, E.M., Garssen, B. Bonke, B., et al. The Multidimensional Fatigue Inventory psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995;39:315-25.
32. Czuber-Dochan, W., Norton, C., Bassettt, P., et al. Development and psychometric testing of inflammatory bowel disease fatigue (IBD-F) patient self-assessment scale. J Crohns Colitis. 2014;8:1398-406.
33. Drossman, D.A., Leserman, J., Li, Z.M., et al. The rating form of IBD patient concerns: a new measure of health status. Psychosom Med. 1991;53:701-12. 34. Cohen, S., Kamarck, T., Mermelstein, R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385-96.
Dr. Cohen is in the division of digestive and liver diseases; Dr. Melmed is director, clinical inflammatory bowel disease, director, clinical research in the division of gastroenterology, and director, advanced inflammatory bowel disease fellowship program, Cedars-Sinai Medical Center, Los Angeles. Dr. Melmed is a consultant for AbbVie, Boehringer Ingelheim, Celgene, Genentech, Janssen, Pfizer, Samsung Bioepis, Takeda, and UCB; and received support for research from Prometheus Labs. The remaining author discloses no conflicts.
Patients seek medical care when they perceive a deterioration in their health. Gastroenterologists and health care providers are trained to seek out clinical, laboratory, radiologic, and endoscopic evidence of pathology. Conventional endpoints in inflammatory bowel disease (IBD) clinical trials and clinical care may fail to capture the full health status and disease experience from the patient perspective. The Food and Drug Administration has called for the development of coprimary endpoints in research trials to include an objective measure of inflammation in conjunction with patient-reported outcomes (PROs). The objective is to support labeling claims and improve safety and effectiveness in the drug approval process.1,2 There is also growing recognition that high-value care includes management of biologic and psychosocial factors to enable patients with chronic diseases to regain their health. Clinicians might follow suit by incorporating valid, reliable PRO measures to usual IBD care in order better to achieve patient-centered care, inform decision making, and improve the care provided.
What are patient-reported outcomes?
The FDA defines a PRO as “any report of the status of a patient’s health condition that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else.” Two PROs are used to measure various aspects of health including physical, emotional, or social domains. PROs have emerged as tools that may foster a better understanding of the patient’s condition, which may go beyond disease activity or symptoms. In effect, incorporating PROs into clinical practice enables a model of “coproduction” of health care, and may contribute to a more reciprocal patient-provider interaction where the needs of the patient may be more fully understood and incorporated into decision-making that may lead to improved patient satisfaction and outcomes.3,4
There are hundreds of available PROs in gastroenterology,5 ranging from simple (characterizing pain with a basic numeric rating scale) to complex multidomain, multi-item instruments. PROs may cover symptom assessment, health-related quality of life, and adherence to and satisfaction with treatment, and may be generic or disease specific. Numerous PROs have been developed for patients with IBD. Commonly used PROs in IBD include severity scales for pain, defecatory urgency, and bloody stool, and several disease-specific and generic instruments assessing different health-related quality-of-life domains have been used in research studies for patients with IBD.
The current approach to patient-centered care for IBD is limited
IBD is a difficult disease to manage – in part because there is no known biomarker that accurately reflects the full spectrum of disease activity. Numerous indices have been developed to better quantify disease activity and measure response to treatment. Among the most frequently used indices in clinical trials are the Crohn’s Disease Activity Index (CDAI) and (for ulcerative colitis [UC]) the Mayo Clinic Score. These endpoints incorporate signs and symptoms, laboratory findings (in the CDAI), and endoscopic assessments. The CDAI is a suboptimal instrument because of a lack of correlation with endoscopic inflammation and potential confounding with concomitant gastrointestinal illnesses, such as irritable bowel syndrome.6 The Mayo Clinic Score is difficult to interpret because of some subjective elements (what is considered a normal number of stools per day?); vagueness (mostly bloody stools more than half the time?); and need for a physician assessment, which often does not correspond with the patient’s perception of their disease.7 From a research perspective, this disconnect can compromise the quality of trial data. Clinically, it can negatively impact patients’ satisfaction and impair the patient-provider relationship.8
To that end, regulatory agencies, scientific bodies, and health care payors are shifting toward a more “patient-centered” approach with an emphasis on PROs. However, although the FDA is incorporating the patient perspective in its trials, measuring meaningful outcomes in day-to-day clinical care is challenging. In the absence of active inflammation, more than 30% of patients with IBD still suffer from gastrointestinal symptoms.9 Furthermore, physicians frequently underestimate the effect of depression, anxiety, fatigue, and sleep on patient health. Likewise, some patients with active small-bowel Crohn’s disease (CD) may experience few gastrointestinal symptoms but have profound fatigue, weight loss, and impaired quality of life. A focused assessment for disease activity may fail to identify aspects of health most relevant or important to individual patient well-being. There is a need for effective, efficient, and standardized strategies to better understand the concerns of the individual seeking help.
Although there are several PROs that measure disease activity primarily for clinical research trials,10 their prevalence in gastroenterology practices has not been assessed. Most likely, few clinical practices currently integrate standardized PROs in routine patient care. This may be because of several reasons, including lack of awareness of newly developed PROs, administrative burden including time and resources to collect PROs, potentially complex interpretation of results, and perhaps a reluctance among physicians to alter traditional patient interview methods of obtaining information about the health status of their patients. For effective use in clinical care, PROs require simple and relevant interpretation to add value to the clinician’s practice, and must minimally impact clinical flow and resources. The use of Internet-enabled tablets has been shown to be a feasible, efficient, and effective means of PRO assessment in gastroenterology practices, with good levels of patient satisfaction.11
Reaping potential benefits of patient-reported outcomes
The National Institutes of Health Patient-Reported Outcomes Measurement Information System (PROMIS) is an initiative developed to investigate and promote implementation of PRO measures among patients with chronic diseases. The collection of PROMIS measures has been shown to be feasible at a tertiary care IBD center, enabling a biopsychosocial model of care.12 Likewise, implementation of PROs in other clinical areas including oncology, orthopedics, and rheumatology has been robust.
In an innovative orthopedic study, PROMIS measures collected and linked to the electronic medical record predicted the likelihood of a clinically meaningful benefit from foot and ankle surgery.13 This facilitated tailored patient-specific preoperative discussions about the expected benefit of surgery. In a study at a rheumatology clinic patients with rheumatoid arthritis were asked to identify their highest priority treatment targets using PROMIS domains (fatigue, pain, depression, social function). The highest priority domain was tracked over time as a patient-centered marker of health, essentially personalizing measures of success for the individual patient.14
PROs have the unique potential to affect multiple levels of health care. At the patient level, PRO data can identify specific concerns, manage expectations of recovery, and tailor treatment decisions to personal preference. At the population level, PRO data can be used to standardize aspects of care to understand comparative health and disease among all patients in a practice or relative to outside practices, identify outliers, and drive improvement.
Optimizing PROs for use in clinical trials: CD–PROs and UC–PROs
Developing standardized, validated instruments according to FDA guidance is a complex process. The lack of an FDA-approved PRO has resulted in substantial variability in the definitions of clinical response or remission in clinical trials to date.15 As a result, IBD-specific PROs (CD-PRO and UC-PRO) are being developed under FDA guidance for use in clinical trials.16 With achievement of prequalification for open use, UC-PRO and CD-PRO will cover five IBD-specific outcomes domains or modules: 1) bowel signs and symptoms, 2) systemic symptoms, 3) emotional impact, 4) coping behaviors, and 5) IBD impact on daily life. The bowel signs and symptoms module may also incorporate a functional impact assessment. Each module includes numerous pertinent items (e.g., “I feel worried,” “I feel scared,” “I feel alone” in the emotional impact module) and are currently being tailored and scored for practicality and relevance. It is hoped that UC-PRO and CD-PRO in final form will be relevant and applicable for clinical trials and gastroenterology practices alike.
Because the development of the UC-PRO and the CD-PRO is still underway, interim PROs are being used in ongoing clinical trials. These interim measures were extracted from existing components of the CDAI, Mayo Clinic Score, and UC Disease Activity Index. The CD PRO-2 consists of two items: abdominal pain and stool frequency. The UC PRO-2 is composed of rectal bleeding and stool frequency. The PRO-3 adds an item regarding general well-being. The sensitivity of these PROs was tested in studies for CD and UC. Both PROs performed similarly to their respective parent instrument. Important limitations include the lack of validation, and the fact that these interim measures were derived from parent measures with acknowledged limitations as previously discussed. Current clinical trials are coupling these interim measures with endoscopic data as coprimary endpoints.
PROs in routine clinical practice: Are we ready for prime time?
Few instruments developed to date have been widely implemented into routine IBD clinical practice. Table 1 highlights commonly available or recently developed PROs for IBD care. As clinicians strive to more effectively integrate PROs into clinical practice, we propose a three-step process to getting started: 1) select and administer a PRO instrument, 2) identify areas of impairment and create a targeted treatment strategy to focus on those areas, and 3) repeat the same PRO at follow-up to assess for improvement. The instrument can be administered before the visit or in the clinic waiting room. Focus a portion of the patient’s visit on discussing the results and identifying one or more domains to target for improvement. For example, the patient may indicate diarrhea as his/her most important area to target, triggering a symptom-specific investigation and therapeutic approach. The PRO may also highlight social or emotional impairment that may require an ancillary referral. The benefits of this PRO-driven approach to IBD care are twofold. First, the patient’s primary concerns are positioned at the forefront of the clinical visit. Second, aligning the clinician’s focus with the patient input may actually help to streamline each visit and improve overall visit efficiency and patient satisfaction.
Conclusions
As therapies for IBD improve, so should standards of patient-centered care. Clinicians must actively seek and then listen to the concerns of patients and be able to address the multiple facets of living with a chronic disease. PROs empower patients, helping them identify important topics for discussion at the clinical visit. This affords clinicians a better understanding of primary patient concerns before the visit, and potentially improves the quality and value of care. At first, the process of incorporating PROs into a busy clinical practice may be challenging, but targeted treatment plans have the potential to foster a better patient – and physician – experience.
Content from this column was originally published in the “Practice Management: The Road Ahead” section of Clinical Gastroenterology and Hepatology (2018;16[5]:603-7).
References
1. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes. 2006;4:79.
2. Burke, L.B., Kennedy, D.L., Miskala, P.H., et al. The use of patient-reported outcome measures in the evaluation of medical products for regulatory approval. Clin Pharmacol Ther. 2008;84:281-3.
3. Batalden, M., Baltalden, P., Margolis, P., et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;25:509-17.
4. Johnson, L.C. Melmed, G.Y., Nelson, E.C., et al. Fostering collaboration through creation of an IBD learning health system. Am J Gastroenterol. 2017;112:406-8.
5. Khanna, P., Agarwal, N., Khanna, D., et al. Development of an online library of patient reported outcome measures in gastroenterology: the GI-PRO database. Am J Gastroenterol. 2014;109:234-48.
6. Bruining, D.H. Sandborn, W.J. Do not assume symptoms indicate failure of anti-tumor necrosis factor therapy in January 2015 Emerging Treatment Goals in IBD Trials and Practice 45 REVIEWS AND PERSPECTIVES Crohn’s disease. Clin Gastroenterol Hepatol. 2011;9:395-9.
7. Surti, B., Spiegel, B., Ippoliti, A., et al. Assessing health status in inflammatory bowel disease using a novel single-item numeric rating scale. Dig Dis Sci. 2013;58:1313-21.
8. Marshall, S., Haywood, K. Fitzpatrick R. Impact of patient-reported outcome measures on routine practice: a structured review. J Eval Clin Pract. 2006;12:559-68.
9. Simren, M., Axelsson, J., Gillberg, R., et al. Quality of life in inflammatory bowel disease in remission: the impact of IBD-like symptoms and associated psychological factors. Am J Gastroenterol. 2002;97:389-96.
10. De Jong, M.J., Huibregtse, R., Masclee, A.A.M., et al. Patient-reported outcome measures for use in clinical trials and clinical practice in inflammatory bowel diseases: a systematic review. Clin Gastroenterol Hepatol. 2018;16:648-63.
11. Atreja, A., Rizk, M. Capturing patient reported outcomes and quality of life in routine clinical practice: ready to prime time? Minerva Gastroenterol Dietol. 2012;58:19-24.
12. Ishak, W.W., Pan, D., Steiner, A.J., et al. Patient reported outcomes of quality of life, functioning, and GI/psychiatric symptom severity in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2017;23:798-803.
13. Ho, B., Houck, J.R., Flemister, A.S., et al. Preoperative PROMIS scores predict postoperative success in foot and ankle patients. Foot Ankle Int. 2016;37:911-8. 14. Bacalao, E., Greene, G.J., Beaumont, J.L., et al. Standardizing and personalizing the treat to target (T2T) approach for rheumatoid arthritis using the Patient-Reported Outcomes Measurement Information System (PROMIS): baseline findings on patient-centered treatment priorities. Clin Rheumatol. 2017;36:1729-36.
15. Ma, C., Panaccione, R., Fedorak, R.N., et al. Heterogeneity in definitions of endpoints for clinical trials of ulcerative colitis: a systematic review for development of a core outcome set. Clin Gastroenterol Hepatol. 2018;16:637-47.
16. Higgins P. Patient reported outcomes in IBD 2017. Available at: ibdctworkshop.files.wordpress.com/2017/01/patient-reported-outcomes-in-ibd___peter-higgins.pdf. Accessed Aug. 27, 2017.
17. Guyatt, G., Mitchell, A. Irvine, E.J., et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989;96:804-10.
18. Love, J.R., Irvine, E.J., Fedorak, R.N. Quality of life in inflammatory bowel disease. J Clin Gastroenterol. 1992;14:15-9.
19. Irvine, E.J., Zhou, Q., Thompson, A.K. The short inflammatory bowel disease questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT investigators. Canadian Crohn’s Relapse Prevention Trial. Am J Gastroenterol. 1996;91:1571-8.
20. Fazio, V.W., O’Riordain, M.G., Lavery, I.C., et al. Long-term functional outcome and quality of life after stapled restorative proctocolectomy. Ann Surg. 1999;230:575-84.
21. Gower-Rousseau, C., Sarter, H., Savoye, G., et al. Validation of the inflammatory bowel disease disability index in a population-based cohort. Gut. 2017;66:588-96.
22. Gosh, S., Louis, E., Beaugerie, L., et al. Development of the IBD-Disk: a visual self-administered tool assessing disability in inflammatory bowel diseases. Inflamm Bowel Dis. 2017;23:333-40.
23. Khanna, R., Zou, G., D’Haens, G., et al. A retrospective analysis: the development of patient reported outcome measures for the assessment of Crohn’s disease activity. Aliment Pharmacol Ther. 2015;41:77-86.
24. Walmsley, R.S., Ayres, R.C.S., Pounder, P.R., et al. A simple clinical colitis activity index. Gut. 1998;43:29-32.
25. Bodger, K., Ormerod, C., Shackcloth, D., et al. Development and validation of a rapid, general measure of disease control from the patient perspective: the IBD-Control questionnaire. Gut. 2014;63:1092-102.
26. Cleeland, C.S., Ryan, K.M. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129-38.
27. Kroenke, K., Spitzer, R.L., Williams, J.B.W. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-13.
28. Zigmond, A.S., Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361-70.
29. Spitzer, R.L., Korneke, K., Williams, J.B., et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092-7.
30. Reilly, M.C., Zbrozek, A.S. Dukes, E.M. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmachoeconomics. 1993;4:353-65.
31. Smets, E.M., Garssen, B. Bonke, B., et al. The Multidimensional Fatigue Inventory psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995;39:315-25.
32. Czuber-Dochan, W., Norton, C., Bassettt, P., et al. Development and psychometric testing of inflammatory bowel disease fatigue (IBD-F) patient self-assessment scale. J Crohns Colitis. 2014;8:1398-406.
33. Drossman, D.A., Leserman, J., Li, Z.M., et al. The rating form of IBD patient concerns: a new measure of health status. Psychosom Med. 1991;53:701-12. 34. Cohen, S., Kamarck, T., Mermelstein, R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385-96.
Dr. Cohen is in the division of digestive and liver diseases; Dr. Melmed is director, clinical inflammatory bowel disease, director, clinical research in the division of gastroenterology, and director, advanced inflammatory bowel disease fellowship program, Cedars-Sinai Medical Center, Los Angeles. Dr. Melmed is a consultant for AbbVie, Boehringer Ingelheim, Celgene, Genentech, Janssen, Pfizer, Samsung Bioepis, Takeda, and UCB; and received support for research from Prometheus Labs. The remaining author discloses no conflicts.
Night sweats
A 46-year-old man comes to clinic for evaluation of night sweats. He has been having drenching night sweats for the past 3 months. He has to change his night shirt at least once per night. He has had a 10-pound weight gain over the past 6 months. No chest pain, nausea, or fatigue. He has had a cough for the past 6 months.
Which is the most likely diagnosis?
A. Gastroesophageal reflux disease.
B. Tuberculosis.
C. Lymphoma.
D. Multiple myeloma.
Night sweats are a common symptom in the general population, estimated to occur in about 10% of people. They can range in frequency and severity. We become most concerned when the patient is concerned, usually when they report drenching night sweats.
What do we need to know about this symptom to help us think of more likely causes and guide us in a more appropriate workup?
Night sweats do not seem to be a bad prognostic symptom. James W. Mold, MD, and his colleagues looked at the prognostic significance of night sweats in two cohorts of elderly patients.1 The prevalence of night sweats in this study was 10%. These two cohorts were followed for a little more than 7 years. More than 1,500 patients were included in the two cohorts. Patients who reported night sweats were not more likely to die, or die sooner, than were those who didn’t have night sweats. The severity of the night sweats did not make a difference.
Lea et al. described the prevalence of night sweats among different inpatient populations, with a range from 33% in surgical and medicine patients, to 60% on obstetrics service.2
Night sweats are common, and don’t appear to be correlated with worse prognosis. So, what are the likely common causes?
There just aren’t good studies on causes of night sweats, but there are studies that suggest that they are seen in some very common diseases. It is always good to look at medication lists as a start when evaluating unexplained symptoms.
Dr. Mold, along with Barbara J. Holtzclaw, PhD, reported higher odds ratios for night sweats for patients on SSRIs (OR, 3.01), angiotensin receptor blockers (OR, 3.44) and thyroid hormone supplements (OR, 2.53).3 W.A. Reynolds, MD, looked at the prevalence of night sweats in a GI practice.4 A total of 41% of the patients reported night sweats, and 12 of 12 patients with GERD who had night sweats had resolution of the night sweats with effective treatment of the GERD.
Dr. Mold and his colleagues found that night sweats were associated with several sleep-related symptoms, including waking up with a bitter taste in the mouth (OR, 1.94), daytime tiredness (OR, 1.99), and legs jerking during sleep (OR, 1.87).5
Erna Arnardottir, PhD, and her colleagues found that obstructive sleep apnea was associated with frequent nocturnal sweating.6 They found that 31% of men and 33% of women with OSA had nocturnal sweating, compared with about 10% of the general population. When the OSA patients were treated with positive airway pressure, the prevalence of nocturnal sweating decreased to 11.5%, similar to general population numbers.
Pearl: Night sweats are associated with common conditions: medications, GERD, and sleep disorders. These are more likely than lymphoma and tuberculosis.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. J Am Board Fam Med. 2010 Jan-Feb;23(1):97-103.
2. South Med J. 1985 Sep;78(9):1065-7.
3. Drugs Real World Outcomes. 2015 Mar;2(1):29-33.
4. J Clin Gastroenterol. 1989 Oct;11(5):590-1.
5. Ann Fam Med. 2006 Sep-Oct;4(5):423-6.
6. BMJ Open. 2013 May 14;3(5).
A 46-year-old man comes to clinic for evaluation of night sweats. He has been having drenching night sweats for the past 3 months. He has to change his night shirt at least once per night. He has had a 10-pound weight gain over the past 6 months. No chest pain, nausea, or fatigue. He has had a cough for the past 6 months.
Which is the most likely diagnosis?
A. Gastroesophageal reflux disease.
B. Tuberculosis.
C. Lymphoma.
D. Multiple myeloma.
Night sweats are a common symptom in the general population, estimated to occur in about 10% of people. They can range in frequency and severity. We become most concerned when the patient is concerned, usually when they report drenching night sweats.
What do we need to know about this symptom to help us think of more likely causes and guide us in a more appropriate workup?
Night sweats do not seem to be a bad prognostic symptom. James W. Mold, MD, and his colleagues looked at the prognostic significance of night sweats in two cohorts of elderly patients.1 The prevalence of night sweats in this study was 10%. These two cohorts were followed for a little more than 7 years. More than 1,500 patients were included in the two cohorts. Patients who reported night sweats were not more likely to die, or die sooner, than were those who didn’t have night sweats. The severity of the night sweats did not make a difference.
Lea et al. described the prevalence of night sweats among different inpatient populations, with a range from 33% in surgical and medicine patients, to 60% on obstetrics service.2
Night sweats are common, and don’t appear to be correlated with worse prognosis. So, what are the likely common causes?
There just aren’t good studies on causes of night sweats, but there are studies that suggest that they are seen in some very common diseases. It is always good to look at medication lists as a start when evaluating unexplained symptoms.
Dr. Mold, along with Barbara J. Holtzclaw, PhD, reported higher odds ratios for night sweats for patients on SSRIs (OR, 3.01), angiotensin receptor blockers (OR, 3.44) and thyroid hormone supplements (OR, 2.53).3 W.A. Reynolds, MD, looked at the prevalence of night sweats in a GI practice.4 A total of 41% of the patients reported night sweats, and 12 of 12 patients with GERD who had night sweats had resolution of the night sweats with effective treatment of the GERD.
Dr. Mold and his colleagues found that night sweats were associated with several sleep-related symptoms, including waking up with a bitter taste in the mouth (OR, 1.94), daytime tiredness (OR, 1.99), and legs jerking during sleep (OR, 1.87).5
Erna Arnardottir, PhD, and her colleagues found that obstructive sleep apnea was associated with frequent nocturnal sweating.6 They found that 31% of men and 33% of women with OSA had nocturnal sweating, compared with about 10% of the general population. When the OSA patients were treated with positive airway pressure, the prevalence of nocturnal sweating decreased to 11.5%, similar to general population numbers.
Pearl: Night sweats are associated with common conditions: medications, GERD, and sleep disorders. These are more likely than lymphoma and tuberculosis.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. J Am Board Fam Med. 2010 Jan-Feb;23(1):97-103.
2. South Med J. 1985 Sep;78(9):1065-7.
3. Drugs Real World Outcomes. 2015 Mar;2(1):29-33.
4. J Clin Gastroenterol. 1989 Oct;11(5):590-1.
5. Ann Fam Med. 2006 Sep-Oct;4(5):423-6.
6. BMJ Open. 2013 May 14;3(5).
A 46-year-old man comes to clinic for evaluation of night sweats. He has been having drenching night sweats for the past 3 months. He has to change his night shirt at least once per night. He has had a 10-pound weight gain over the past 6 months. No chest pain, nausea, or fatigue. He has had a cough for the past 6 months.
Which is the most likely diagnosis?
A. Gastroesophageal reflux disease.
B. Tuberculosis.
C. Lymphoma.
D. Multiple myeloma.
Night sweats are a common symptom in the general population, estimated to occur in about 10% of people. They can range in frequency and severity. We become most concerned when the patient is concerned, usually when they report drenching night sweats.
What do we need to know about this symptom to help us think of more likely causes and guide us in a more appropriate workup?
Night sweats do not seem to be a bad prognostic symptom. James W. Mold, MD, and his colleagues looked at the prognostic significance of night sweats in two cohorts of elderly patients.1 The prevalence of night sweats in this study was 10%. These two cohorts were followed for a little more than 7 years. More than 1,500 patients were included in the two cohorts. Patients who reported night sweats were not more likely to die, or die sooner, than were those who didn’t have night sweats. The severity of the night sweats did not make a difference.
Lea et al. described the prevalence of night sweats among different inpatient populations, with a range from 33% in surgical and medicine patients, to 60% on obstetrics service.2
Night sweats are common, and don’t appear to be correlated with worse prognosis. So, what are the likely common causes?
There just aren’t good studies on causes of night sweats, but there are studies that suggest that they are seen in some very common diseases. It is always good to look at medication lists as a start when evaluating unexplained symptoms.
Dr. Mold, along with Barbara J. Holtzclaw, PhD, reported higher odds ratios for night sweats for patients on SSRIs (OR, 3.01), angiotensin receptor blockers (OR, 3.44) and thyroid hormone supplements (OR, 2.53).3 W.A. Reynolds, MD, looked at the prevalence of night sweats in a GI practice.4 A total of 41% of the patients reported night sweats, and 12 of 12 patients with GERD who had night sweats had resolution of the night sweats with effective treatment of the GERD.
Dr. Mold and his colleagues found that night sweats were associated with several sleep-related symptoms, including waking up with a bitter taste in the mouth (OR, 1.94), daytime tiredness (OR, 1.99), and legs jerking during sleep (OR, 1.87).5
Erna Arnardottir, PhD, and her colleagues found that obstructive sleep apnea was associated with frequent nocturnal sweating.6 They found that 31% of men and 33% of women with OSA had nocturnal sweating, compared with about 10% of the general population. When the OSA patients were treated with positive airway pressure, the prevalence of nocturnal sweating decreased to 11.5%, similar to general population numbers.
Pearl: Night sweats are associated with common conditions: medications, GERD, and sleep disorders. These are more likely than lymphoma and tuberculosis.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. J Am Board Fam Med. 2010 Jan-Feb;23(1):97-103.
2. South Med J. 1985 Sep;78(9):1065-7.
3. Drugs Real World Outcomes. 2015 Mar;2(1):29-33.
4. J Clin Gastroenterol. 1989 Oct;11(5):590-1.
5. Ann Fam Med. 2006 Sep-Oct;4(5):423-6.
6. BMJ Open. 2013 May 14;3(5).
Hospitalists can meet the demand for physician executives
HM provides “foundational leadership skills”
Hospitals and health systems are increasingly looking to physicians to provide leadership at the most senior executive level. While the chief medical officer (CMO) or similar role has given physicians a seat at the executive table at many organizations, physicians are also being sought for the CEO role at the head of that table.
A commonly referenced study from 2011 by Amanda Goodall, MD, in Social Science & Medicine concluded that, among a cohort of highly ranked hospitals, overall quality metrics were approximately 25% higher in hospitals where a physician was CEO, in comparison to hospitals with non-physician CEOs (2011 Aug;73[4]:535-9). In addition, new positions at both the hospital and health system level are coming into existence: Examples include chief (or VP) of population health, chief innovation officer, chief quality officer, chief patient experience officer, and others.
There is every reason to think that these senior executive physician roles can – and in many cases perhaps should – be filled by hospitalists. Hospital medicine is an ideal “proving ground” for future physician executives and leaders. I believe that the best practitioners of hospital medicine are also the best candidates for hospital, health care, and health system physician executive leadership, because many of the characteristics essential for success as an executive are the same characteristics that are essential for success as a hospitalist. Strong candidates should have the following characteristics:
- A patient-centered perspective. Perhaps the most important characteristic of a leader is empathy. To appreciate the complex, and often (if not usual) challenging emotional states of our patients keeps us connected at the most fundamental, human level to the work we do and to our patients and families. Empathy can – and should – extend to fellow caregivers as well, and allows us to practice and lead teams in the most human of professions. No leader – in health care, anyway – can last long without being able to demonstrate empathy, through words and behavior.
- A systems-based practice: A hospitalist must be able to have a foot in each of two canoes – to be able to see each patient and their family individually and develop preference-based plans of care, and also to be able to focus on process, structure, and outcomes for the hospital system as a whole. The former trait is imbued in us during training and is the critical foundation for the patient-physician relationship. The latter, however, is something different entirely and reflects an ability to have perspective on the entire ecosystem of care – and apply principles of process and quality improvement to achieve forward looking results. That’s leadership.
- Team leadership: Another fundamental attribute of leaders is to assemble a talented and diverse team around an objective, and then to delegate both tasks and their ownership, deferring to expertise. Hospitalists – the best ones, anyway – similarly recognize that for the vast majority of a patient’s hospital stay, the most important caregiver in a patient’s care is someone other than themselves. At any given time, it might be the nurse, aide, pharmacist, care manager, transporter, radiology tech, urologist, housekeeper, surgical resident, or anyone involved in that patient’s care. The hospitalist’s greatest value is in developing the plan of care with the patient and their family, and then communicating – and therefore delegating – that plan to individuals with the expertise to execute that plan. I believe the biggest difficulty hospitalists have in assuming leadership roles is getting out of the comfortable weeds of daily clinical operations and instead focusing on goals, strategies, and teams to accomplish them. The best hospitalists are doing this already as part of their daily care.
- The ability to manage relationships: Hospitalists manage and work among a team of diverse talents. They also often have accountability relationships to a myriad of clinical and administrative leaders in the hospital, each of whom may be in a position of authority to place demands on the hospitalists: A partial list might include the CEO, the chief medical officer, chief nurse, chief of staff, other medical staff departments, academic leaders, and of course, patients and their families. Functioning in a “matrixed” organization – in which lines of authority can go in many directions, depending on the situation – is standard fare, even at the executive level, and the key competency is open and frequent communication.
- Experience: Already, hospitalists assume leadership roles in their hospitals – leaders in quality, medical informatics, patient experience, and continuous improvement. In these roles, physicians work with senior executives and other hospital leaders to both set goals and implement strategies, providing visibility and working relationships that can be helpful to aspiring leaders.
Perhaps more so than most other specialties, then, hospitalists demonstrate foundational leadership skills in their day-to-day practice – an ideal start to a leadership path. This is not to say or suggest that a career devoted purely to clinical practice is somehow inferior – far from it. However, as health care organizations turn to the medical community to provider leadership, hospitalists are well positioned to develop and be developed as executive leaders.
How can the Society of Hospital Medicine help? While management degrees become a common pathway for many, some health systems and professional organizations support their membership with a leadership development curriculum which may be a better place to start. In my opinion, SHM provides one of the most thorough and relevant experiences available. The SHM Leadership Academy focuses on developing a broad set of additional leadership competencies across a spectrum of experience. The format varies depending on the course, but all rely heavily upon experienced hospitalist leaders – in fact, many current and former Board members and officers volunteer their time to facilitate and teach at the Academy, including at the entry level. It’s a powerful way to learn from others who have started walking the leadership path.
Dr. Harte is a past president of SHM and president of Cleveland Clinic Akron General and Southern Region.
HM provides “foundational leadership skills”
HM provides “foundational leadership skills”
Hospitals and health systems are increasingly looking to physicians to provide leadership at the most senior executive level. While the chief medical officer (CMO) or similar role has given physicians a seat at the executive table at many organizations, physicians are also being sought for the CEO role at the head of that table.
A commonly referenced study from 2011 by Amanda Goodall, MD, in Social Science & Medicine concluded that, among a cohort of highly ranked hospitals, overall quality metrics were approximately 25% higher in hospitals where a physician was CEO, in comparison to hospitals with non-physician CEOs (2011 Aug;73[4]:535-9). In addition, new positions at both the hospital and health system level are coming into existence: Examples include chief (or VP) of population health, chief innovation officer, chief quality officer, chief patient experience officer, and others.
There is every reason to think that these senior executive physician roles can – and in many cases perhaps should – be filled by hospitalists. Hospital medicine is an ideal “proving ground” for future physician executives and leaders. I believe that the best practitioners of hospital medicine are also the best candidates for hospital, health care, and health system physician executive leadership, because many of the characteristics essential for success as an executive are the same characteristics that are essential for success as a hospitalist. Strong candidates should have the following characteristics:
- A patient-centered perspective. Perhaps the most important characteristic of a leader is empathy. To appreciate the complex, and often (if not usual) challenging emotional states of our patients keeps us connected at the most fundamental, human level to the work we do and to our patients and families. Empathy can – and should – extend to fellow caregivers as well, and allows us to practice and lead teams in the most human of professions. No leader – in health care, anyway – can last long without being able to demonstrate empathy, through words and behavior.
- A systems-based practice: A hospitalist must be able to have a foot in each of two canoes – to be able to see each patient and their family individually and develop preference-based plans of care, and also to be able to focus on process, structure, and outcomes for the hospital system as a whole. The former trait is imbued in us during training and is the critical foundation for the patient-physician relationship. The latter, however, is something different entirely and reflects an ability to have perspective on the entire ecosystem of care – and apply principles of process and quality improvement to achieve forward looking results. That’s leadership.
- Team leadership: Another fundamental attribute of leaders is to assemble a talented and diverse team around an objective, and then to delegate both tasks and their ownership, deferring to expertise. Hospitalists – the best ones, anyway – similarly recognize that for the vast majority of a patient’s hospital stay, the most important caregiver in a patient’s care is someone other than themselves. At any given time, it might be the nurse, aide, pharmacist, care manager, transporter, radiology tech, urologist, housekeeper, surgical resident, or anyone involved in that patient’s care. The hospitalist’s greatest value is in developing the plan of care with the patient and their family, and then communicating – and therefore delegating – that plan to individuals with the expertise to execute that plan. I believe the biggest difficulty hospitalists have in assuming leadership roles is getting out of the comfortable weeds of daily clinical operations and instead focusing on goals, strategies, and teams to accomplish them. The best hospitalists are doing this already as part of their daily care.
- The ability to manage relationships: Hospitalists manage and work among a team of diverse talents. They also often have accountability relationships to a myriad of clinical and administrative leaders in the hospital, each of whom may be in a position of authority to place demands on the hospitalists: A partial list might include the CEO, the chief medical officer, chief nurse, chief of staff, other medical staff departments, academic leaders, and of course, patients and their families. Functioning in a “matrixed” organization – in which lines of authority can go in many directions, depending on the situation – is standard fare, even at the executive level, and the key competency is open and frequent communication.
- Experience: Already, hospitalists assume leadership roles in their hospitals – leaders in quality, medical informatics, patient experience, and continuous improvement. In these roles, physicians work with senior executives and other hospital leaders to both set goals and implement strategies, providing visibility and working relationships that can be helpful to aspiring leaders.
Perhaps more so than most other specialties, then, hospitalists demonstrate foundational leadership skills in their day-to-day practice – an ideal start to a leadership path. This is not to say or suggest that a career devoted purely to clinical practice is somehow inferior – far from it. However, as health care organizations turn to the medical community to provider leadership, hospitalists are well positioned to develop and be developed as executive leaders.
How can the Society of Hospital Medicine help? While management degrees become a common pathway for many, some health systems and professional organizations support their membership with a leadership development curriculum which may be a better place to start. In my opinion, SHM provides one of the most thorough and relevant experiences available. The SHM Leadership Academy focuses on developing a broad set of additional leadership competencies across a spectrum of experience. The format varies depending on the course, but all rely heavily upon experienced hospitalist leaders – in fact, many current and former Board members and officers volunteer their time to facilitate and teach at the Academy, including at the entry level. It’s a powerful way to learn from others who have started walking the leadership path.
Dr. Harte is a past president of SHM and president of Cleveland Clinic Akron General and Southern Region.
Hospitals and health systems are increasingly looking to physicians to provide leadership at the most senior executive level. While the chief medical officer (CMO) or similar role has given physicians a seat at the executive table at many organizations, physicians are also being sought for the CEO role at the head of that table.
A commonly referenced study from 2011 by Amanda Goodall, MD, in Social Science & Medicine concluded that, among a cohort of highly ranked hospitals, overall quality metrics were approximately 25% higher in hospitals where a physician was CEO, in comparison to hospitals with non-physician CEOs (2011 Aug;73[4]:535-9). In addition, new positions at both the hospital and health system level are coming into existence: Examples include chief (or VP) of population health, chief innovation officer, chief quality officer, chief patient experience officer, and others.
There is every reason to think that these senior executive physician roles can – and in many cases perhaps should – be filled by hospitalists. Hospital medicine is an ideal “proving ground” for future physician executives and leaders. I believe that the best practitioners of hospital medicine are also the best candidates for hospital, health care, and health system physician executive leadership, because many of the characteristics essential for success as an executive are the same characteristics that are essential for success as a hospitalist. Strong candidates should have the following characteristics:
- A patient-centered perspective. Perhaps the most important characteristic of a leader is empathy. To appreciate the complex, and often (if not usual) challenging emotional states of our patients keeps us connected at the most fundamental, human level to the work we do and to our patients and families. Empathy can – and should – extend to fellow caregivers as well, and allows us to practice and lead teams in the most human of professions. No leader – in health care, anyway – can last long without being able to demonstrate empathy, through words and behavior.
- A systems-based practice: A hospitalist must be able to have a foot in each of two canoes – to be able to see each patient and their family individually and develop preference-based plans of care, and also to be able to focus on process, structure, and outcomes for the hospital system as a whole. The former trait is imbued in us during training and is the critical foundation for the patient-physician relationship. The latter, however, is something different entirely and reflects an ability to have perspective on the entire ecosystem of care – and apply principles of process and quality improvement to achieve forward looking results. That’s leadership.
- Team leadership: Another fundamental attribute of leaders is to assemble a talented and diverse team around an objective, and then to delegate both tasks and their ownership, deferring to expertise. Hospitalists – the best ones, anyway – similarly recognize that for the vast majority of a patient’s hospital stay, the most important caregiver in a patient’s care is someone other than themselves. At any given time, it might be the nurse, aide, pharmacist, care manager, transporter, radiology tech, urologist, housekeeper, surgical resident, or anyone involved in that patient’s care. The hospitalist’s greatest value is in developing the plan of care with the patient and their family, and then communicating – and therefore delegating – that plan to individuals with the expertise to execute that plan. I believe the biggest difficulty hospitalists have in assuming leadership roles is getting out of the comfortable weeds of daily clinical operations and instead focusing on goals, strategies, and teams to accomplish them. The best hospitalists are doing this already as part of their daily care.
- The ability to manage relationships: Hospitalists manage and work among a team of diverse talents. They also often have accountability relationships to a myriad of clinical and administrative leaders in the hospital, each of whom may be in a position of authority to place demands on the hospitalists: A partial list might include the CEO, the chief medical officer, chief nurse, chief of staff, other medical staff departments, academic leaders, and of course, patients and their families. Functioning in a “matrixed” organization – in which lines of authority can go in many directions, depending on the situation – is standard fare, even at the executive level, and the key competency is open and frequent communication.
- Experience: Already, hospitalists assume leadership roles in their hospitals – leaders in quality, medical informatics, patient experience, and continuous improvement. In these roles, physicians work with senior executives and other hospital leaders to both set goals and implement strategies, providing visibility and working relationships that can be helpful to aspiring leaders.
Perhaps more so than most other specialties, then, hospitalists demonstrate foundational leadership skills in their day-to-day practice – an ideal start to a leadership path. This is not to say or suggest that a career devoted purely to clinical practice is somehow inferior – far from it. However, as health care organizations turn to the medical community to provider leadership, hospitalists are well positioned to develop and be developed as executive leaders.
How can the Society of Hospital Medicine help? While management degrees become a common pathway for many, some health systems and professional organizations support their membership with a leadership development curriculum which may be a better place to start. In my opinion, SHM provides one of the most thorough and relevant experiences available. The SHM Leadership Academy focuses on developing a broad set of additional leadership competencies across a spectrum of experience. The format varies depending on the course, but all rely heavily upon experienced hospitalist leaders – in fact, many current and former Board members and officers volunteer their time to facilitate and teach at the Academy, including at the entry level. It’s a powerful way to learn from others who have started walking the leadership path.
Dr. Harte is a past president of SHM and president of Cleveland Clinic Akron General and Southern Region.
What is your diagnosis? - December 2018
A KOH (potassium hydroxide) test done at the visit was negative as well as a fungal culture of each toenail.
The patient was diagnosed with congenital malalignment of the great toenails (CMGTN) based on history and morphologic appearance.
Congenital malalignment of the great toenails is an underrecognized and underreported nail disorder characterized by lateral deviation of the nail plate, which is not parallel to the longitudinal axis of the distal phalanx.1 The cause is unknown. Some reports suggest a genetic cause being transmitted in an autosomal dominant fashion with variable expression.2 There have been reports of CMGTN in monozygotic and dizygotic twins making this theory likely.3 Other authors consider an external cause such as amniotic bands, neonatal asphyxia, vascular malformations, and uterine pressure. This condition also has been reported in patients with Rubinstein-Taybi syndrome.4
The nail changes can occur at birth but in some cases, such as our patient, the nails become dystrophic months to years after birth. Characteristic nail changes include shorter, discolored, hyperkeratotic nails with transverse groove or ridges. In some cases, the dystrophic nails may cause inflammation and tenderness and is the most common cause of ingrown toenails in children.
The differential diagnosis includes onychomycosis, traumatic nails, nail psoriasis, pachyonychia congenital (PC), and onychomadesis. Onychomycosis can present with white or yellow discoloration of the nail that in some cases can be associated with nail breakage, hyperkeratosis, onycholysis, and subungual debris. Either fungal culture or periodic acid shift stain of nail clippings can help confirm or exclude this diagnosis. Psoriatic nails present with nail pits, oils spots, and onycholysis. Traumatic nail changes may occur from using small shoes and trauma from running or playing soccer, and presents with subungual hemorrhage and nail dystrophy of the first or second toenail. PC is a genetic disorder caused by a mutation in certain keratin proteins of the skin (k6a, k6b, K16 and K17). These patients usually have other skin findings including palmoplantar keratoderma, white plaques on the mouth, and skin cysts (steatocystoma multiplex and vellus hair cysts). Nail changes characteristic of PC includes subungual hyperkeratosis that causes a wedge shape thickening of the nail bed (pincer nails).5 Onychomadesis can be seen after viral infections such as hand-foot-mouth disease or in patients taking chemotherapy drugs that affect nail growth.
CMGTN usually resolves with time, but some patients with severe deviation and paronychia may need surgical correction.6
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. Email her at [email protected].
References
1. Dermatol Online J. 2014 Jan 15;20(1):21251.
2. J Dtsch Dermatol Ges. 2012 May;10(5):326-30.
3. J Am Acad Dermatol. 2007 Oct;57(4):711-5.
4. Pediatr Dermatol. 2004 Jan-Feb;21(1):44-7.
5. Curr Opin Pediatr. 2014 Aug;26(4):440-5.
6. Skin Appendage Disord. 2018 Oct;4(4):230-5.
A KOH (potassium hydroxide) test done at the visit was negative as well as a fungal culture of each toenail.
The patient was diagnosed with congenital malalignment of the great toenails (CMGTN) based on history and morphologic appearance.
Congenital malalignment of the great toenails is an underrecognized and underreported nail disorder characterized by lateral deviation of the nail plate, which is not parallel to the longitudinal axis of the distal phalanx.1 The cause is unknown. Some reports suggest a genetic cause being transmitted in an autosomal dominant fashion with variable expression.2 There have been reports of CMGTN in monozygotic and dizygotic twins making this theory likely.3 Other authors consider an external cause such as amniotic bands, neonatal asphyxia, vascular malformations, and uterine pressure. This condition also has been reported in patients with Rubinstein-Taybi syndrome.4
The nail changes can occur at birth but in some cases, such as our patient, the nails become dystrophic months to years after birth. Characteristic nail changes include shorter, discolored, hyperkeratotic nails with transverse groove or ridges. In some cases, the dystrophic nails may cause inflammation and tenderness and is the most common cause of ingrown toenails in children.
The differential diagnosis includes onychomycosis, traumatic nails, nail psoriasis, pachyonychia congenital (PC), and onychomadesis. Onychomycosis can present with white or yellow discoloration of the nail that in some cases can be associated with nail breakage, hyperkeratosis, onycholysis, and subungual debris. Either fungal culture or periodic acid shift stain of nail clippings can help confirm or exclude this diagnosis. Psoriatic nails present with nail pits, oils spots, and onycholysis. Traumatic nail changes may occur from using small shoes and trauma from running or playing soccer, and presents with subungual hemorrhage and nail dystrophy of the first or second toenail. PC is a genetic disorder caused by a mutation in certain keratin proteins of the skin (k6a, k6b, K16 and K17). These patients usually have other skin findings including palmoplantar keratoderma, white plaques on the mouth, and skin cysts (steatocystoma multiplex and vellus hair cysts). Nail changes characteristic of PC includes subungual hyperkeratosis that causes a wedge shape thickening of the nail bed (pincer nails).5 Onychomadesis can be seen after viral infections such as hand-foot-mouth disease or in patients taking chemotherapy drugs that affect nail growth.
CMGTN usually resolves with time, but some patients with severe deviation and paronychia may need surgical correction.6
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. Email her at [email protected].
References
1. Dermatol Online J. 2014 Jan 15;20(1):21251.
2. J Dtsch Dermatol Ges. 2012 May;10(5):326-30.
3. J Am Acad Dermatol. 2007 Oct;57(4):711-5.
4. Pediatr Dermatol. 2004 Jan-Feb;21(1):44-7.
5. Curr Opin Pediatr. 2014 Aug;26(4):440-5.
6. Skin Appendage Disord. 2018 Oct;4(4):230-5.
A KOH (potassium hydroxide) test done at the visit was negative as well as a fungal culture of each toenail.
The patient was diagnosed with congenital malalignment of the great toenails (CMGTN) based on history and morphologic appearance.
Congenital malalignment of the great toenails is an underrecognized and underreported nail disorder characterized by lateral deviation of the nail plate, which is not parallel to the longitudinal axis of the distal phalanx.1 The cause is unknown. Some reports suggest a genetic cause being transmitted in an autosomal dominant fashion with variable expression.2 There have been reports of CMGTN in monozygotic and dizygotic twins making this theory likely.3 Other authors consider an external cause such as amniotic bands, neonatal asphyxia, vascular malformations, and uterine pressure. This condition also has been reported in patients with Rubinstein-Taybi syndrome.4
The nail changes can occur at birth but in some cases, such as our patient, the nails become dystrophic months to years after birth. Characteristic nail changes include shorter, discolored, hyperkeratotic nails with transverse groove or ridges. In some cases, the dystrophic nails may cause inflammation and tenderness and is the most common cause of ingrown toenails in children.
The differential diagnosis includes onychomycosis, traumatic nails, nail psoriasis, pachyonychia congenital (PC), and onychomadesis. Onychomycosis can present with white or yellow discoloration of the nail that in some cases can be associated with nail breakage, hyperkeratosis, onycholysis, and subungual debris. Either fungal culture or periodic acid shift stain of nail clippings can help confirm or exclude this diagnosis. Psoriatic nails present with nail pits, oils spots, and onycholysis. Traumatic nail changes may occur from using small shoes and trauma from running or playing soccer, and presents with subungual hemorrhage and nail dystrophy of the first or second toenail. PC is a genetic disorder caused by a mutation in certain keratin proteins of the skin (k6a, k6b, K16 and K17). These patients usually have other skin findings including palmoplantar keratoderma, white plaques on the mouth, and skin cysts (steatocystoma multiplex and vellus hair cysts). Nail changes characteristic of PC includes subungual hyperkeratosis that causes a wedge shape thickening of the nail bed (pincer nails).5 Onychomadesis can be seen after viral infections such as hand-foot-mouth disease or in patients taking chemotherapy drugs that affect nail growth.
CMGTN usually resolves with time, but some patients with severe deviation and paronychia may need surgical correction.6
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. Email her at [email protected].
References
1. Dermatol Online J. 2014 Jan 15;20(1):21251.
2. J Dtsch Dermatol Ges. 2012 May;10(5):326-30.
3. J Am Acad Dermatol. 2007 Oct;57(4):711-5.
4. Pediatr Dermatol. 2004 Jan-Feb;21(1):44-7.
5. Curr Opin Pediatr. 2014 Aug;26(4):440-5.
6. Skin Appendage Disord. 2018 Oct;4(4):230-5.
A 4-year-old boy is brought to our pediatric dermatology clinic by his mother with the concern of difficult to treat toenail fungus.
The mother reported that she started noticing the toenail changes at around 8 months of age, and it has been progressively getting worse.
He has been treated with several courses of topical antifungals and 3 months of oral terbinafine without success.
A fungal culture done 1 year prior showed slight growth of Cladosporium Sp., but the nails failed to improve after systemic therapy. He denied any associated pain or inflammation. He likes playing softball and plays soccer sometimes. The mother is very worried because the father also has a history of onychomycosis that he has not been able to clear for years.
On physical exam, he is a very pleasant young boy. His cutaneous exam is normal including hair and teeth except for thickening of the bilateral first toenails associated with transverse ridging and yellow discoloration.
Data on perinatal choline, neurodevelopment sparking practice changes
Pregnant women at University of Illinois at Chicago will be offered choline supplements
Finally, the evidence is in: Three evidence-based studies show that perinatal choline supports proper neurodevelopment in fetuses.1,2,3
As anyone who has been following my prevention efforts knows, 4 out of 10 patients at Jackson Park Hospital on Chicago’s Southside who presented to their family medicine clinic for psychiatric care have clinical profiles that are consistent with neurobehavioral disorder associated with prenatal alcohol exposure (ND-PAE).4 Furthermore, since only a little can be done to ameliorate these patients’ psychopathology, I have sought out prevention interventions to stem the tide of what I have thought was a silent epidemic (“occult prenatal alcohol exposure”) for decades.
So I have been heartened that there is some sound science to suggest that perinatal choline supplementation could help. That reality, along with the American Medical Association’s resolution to support evidence-based amounts of choline in all prenatal vitamins, spurred the University of Illinois at Chicago to do something.
Thanks to the support of Enrico Benedetti, MD, professor and head of the department of surgery at the University of Illinois at Chicago, pregnant women will be offered choline supplements to support their fetuses’ neurodevelopment. In addition,
Other efforts are afoot aimed at getting this prevention intervention up and running. For example, Yavar Moghimi, MD, who is the behavioral health director for a Medicaid managed care organization in Washington, recently informed me that its clinical policy committee approved a policy highlighting the evidence behind choline supplements during pregnancy.
I am hoping the University of Illinois at Chicago initiative, entitled the “Healthy Prenatal Brain Program” will help all women by preventing the unrecognized problem I have seen among African American women who engage in social drinking before they realize that they are pregnant.5 After all, the problem of choline deficiency is not tied simply to prenatal alcohol exposure but also to dietary habits. For example, a study by Helen H. Jensen, PhD, and her associates found that 90% of pregnant women do not get enough choline.6 It is just that low-income people are the “canaries in the coal mine” when it comes to being alerted to major public health problems in America.
Another positive development is a website set up by Robert R. Freedman, MD, former chairman of the psychiatry department at the University of Colorado Denver. The site, called prenataldoctoradvice.com, provides guidance to patients about steps they can take, such as taking choline supplements during pregnancy, to improve their children's brain development and mental health.
The public health fix we are suggesting in not difficult; after all, choline is an over-the-counter nutrient, and it does not have to be prescribed by a physician. Ideally, the public health initiatives being advocated are so affordable and easy to implement that this practice will become ubiquitous, and our children will be healthier as a result. It is just a matter of taking action. Now that the evidence is finally in that perinatal choline supplements support proper neurodevelopment in fetuses, we all should move forward – and do something.
Dr. Bell is staff psychiatrist at Jackson Park Hospital’s surgical-medical/psychiatric inpatient unit in Chicago and chairman of the department of psychiatry at Windsor University, St. Kitts, USVI. He also is clinical professor emeritus in the department of psychiatry at the University of Illinois at Chicago; former president/CEO of Community Mental Health Council; and former director of the Institute for Juvenile Research (the birthplace of child psychiatry), all in Chicago.
References
1. Alcohol Clin Exp Res. 2018 Jul;42(7):1327-41.
2. Am J Psychiatry. 2016 May 1;173(5):509-16.
3. Alcohol. 2015 Nov;49(7):647-56.
4. Psychiatr Serv. 2015 May 1;66(5):539-42.
5. MDedge Psychcast. 2018 Oct 17. Fetal alcohol spectrum disorder, part II.
6. The FASEB Journal. 2007;21(6):1b21.
*This column was updated 11/30/2018.
Pregnant women at University of Illinois at Chicago will be offered choline supplements
Pregnant women at University of Illinois at Chicago will be offered choline supplements
Finally, the evidence is in: Three evidence-based studies show that perinatal choline supports proper neurodevelopment in fetuses.1,2,3
As anyone who has been following my prevention efforts knows, 4 out of 10 patients at Jackson Park Hospital on Chicago’s Southside who presented to their family medicine clinic for psychiatric care have clinical profiles that are consistent with neurobehavioral disorder associated with prenatal alcohol exposure (ND-PAE).4 Furthermore, since only a little can be done to ameliorate these patients’ psychopathology, I have sought out prevention interventions to stem the tide of what I have thought was a silent epidemic (“occult prenatal alcohol exposure”) for decades.
So I have been heartened that there is some sound science to suggest that perinatal choline supplementation could help. That reality, along with the American Medical Association’s resolution to support evidence-based amounts of choline in all prenatal vitamins, spurred the University of Illinois at Chicago to do something.
Thanks to the support of Enrico Benedetti, MD, professor and head of the department of surgery at the University of Illinois at Chicago, pregnant women will be offered choline supplements to support their fetuses’ neurodevelopment. In addition,
Other efforts are afoot aimed at getting this prevention intervention up and running. For example, Yavar Moghimi, MD, who is the behavioral health director for a Medicaid managed care organization in Washington, recently informed me that its clinical policy committee approved a policy highlighting the evidence behind choline supplements during pregnancy.
I am hoping the University of Illinois at Chicago initiative, entitled the “Healthy Prenatal Brain Program” will help all women by preventing the unrecognized problem I have seen among African American women who engage in social drinking before they realize that they are pregnant.5 After all, the problem of choline deficiency is not tied simply to prenatal alcohol exposure but also to dietary habits. For example, a study by Helen H. Jensen, PhD, and her associates found that 90% of pregnant women do not get enough choline.6 It is just that low-income people are the “canaries in the coal mine” when it comes to being alerted to major public health problems in America.
Another positive development is a website set up by Robert R. Freedman, MD, former chairman of the psychiatry department at the University of Colorado Denver. The site, called prenataldoctoradvice.com, provides guidance to patients about steps they can take, such as taking choline supplements during pregnancy, to improve their children's brain development and mental health.
The public health fix we are suggesting in not difficult; after all, choline is an over-the-counter nutrient, and it does not have to be prescribed by a physician. Ideally, the public health initiatives being advocated are so affordable and easy to implement that this practice will become ubiquitous, and our children will be healthier as a result. It is just a matter of taking action. Now that the evidence is finally in that perinatal choline supplements support proper neurodevelopment in fetuses, we all should move forward – and do something.
Dr. Bell is staff psychiatrist at Jackson Park Hospital’s surgical-medical/psychiatric inpatient unit in Chicago and chairman of the department of psychiatry at Windsor University, St. Kitts, USVI. He also is clinical professor emeritus in the department of psychiatry at the University of Illinois at Chicago; former president/CEO of Community Mental Health Council; and former director of the Institute for Juvenile Research (the birthplace of child psychiatry), all in Chicago.
References
1. Alcohol Clin Exp Res. 2018 Jul;42(7):1327-41.
2. Am J Psychiatry. 2016 May 1;173(5):509-16.
3. Alcohol. 2015 Nov;49(7):647-56.
4. Psychiatr Serv. 2015 May 1;66(5):539-42.
5. MDedge Psychcast. 2018 Oct 17. Fetal alcohol spectrum disorder, part II.
6. The FASEB Journal. 2007;21(6):1b21.
*This column was updated 11/30/2018.
Finally, the evidence is in: Three evidence-based studies show that perinatal choline supports proper neurodevelopment in fetuses.1,2,3
As anyone who has been following my prevention efforts knows, 4 out of 10 patients at Jackson Park Hospital on Chicago’s Southside who presented to their family medicine clinic for psychiatric care have clinical profiles that are consistent with neurobehavioral disorder associated with prenatal alcohol exposure (ND-PAE).4 Furthermore, since only a little can be done to ameliorate these patients’ psychopathology, I have sought out prevention interventions to stem the tide of what I have thought was a silent epidemic (“occult prenatal alcohol exposure”) for decades.
So I have been heartened that there is some sound science to suggest that perinatal choline supplementation could help. That reality, along with the American Medical Association’s resolution to support evidence-based amounts of choline in all prenatal vitamins, spurred the University of Illinois at Chicago to do something.
Thanks to the support of Enrico Benedetti, MD, professor and head of the department of surgery at the University of Illinois at Chicago, pregnant women will be offered choline supplements to support their fetuses’ neurodevelopment. In addition,
Other efforts are afoot aimed at getting this prevention intervention up and running. For example, Yavar Moghimi, MD, who is the behavioral health director for a Medicaid managed care organization in Washington, recently informed me that its clinical policy committee approved a policy highlighting the evidence behind choline supplements during pregnancy.
I am hoping the University of Illinois at Chicago initiative, entitled the “Healthy Prenatal Brain Program” will help all women by preventing the unrecognized problem I have seen among African American women who engage in social drinking before they realize that they are pregnant.5 After all, the problem of choline deficiency is not tied simply to prenatal alcohol exposure but also to dietary habits. For example, a study by Helen H. Jensen, PhD, and her associates found that 90% of pregnant women do not get enough choline.6 It is just that low-income people are the “canaries in the coal mine” when it comes to being alerted to major public health problems in America.
Another positive development is a website set up by Robert R. Freedman, MD, former chairman of the psychiatry department at the University of Colorado Denver. The site, called prenataldoctoradvice.com, provides guidance to patients about steps they can take, such as taking choline supplements during pregnancy, to improve their children's brain development and mental health.
The public health fix we are suggesting in not difficult; after all, choline is an over-the-counter nutrient, and it does not have to be prescribed by a physician. Ideally, the public health initiatives being advocated are so affordable and easy to implement that this practice will become ubiquitous, and our children will be healthier as a result. It is just a matter of taking action. Now that the evidence is finally in that perinatal choline supplements support proper neurodevelopment in fetuses, we all should move forward – and do something.
Dr. Bell is staff psychiatrist at Jackson Park Hospital’s surgical-medical/psychiatric inpatient unit in Chicago and chairman of the department of psychiatry at Windsor University, St. Kitts, USVI. He also is clinical professor emeritus in the department of psychiatry at the University of Illinois at Chicago; former president/CEO of Community Mental Health Council; and former director of the Institute for Juvenile Research (the birthplace of child psychiatry), all in Chicago.
References
1. Alcohol Clin Exp Res. 2018 Jul;42(7):1327-41.
2. Am J Psychiatry. 2016 May 1;173(5):509-16.
3. Alcohol. 2015 Nov;49(7):647-56.
4. Psychiatr Serv. 2015 May 1;66(5):539-42.
5. MDedge Psychcast. 2018 Oct 17. Fetal alcohol spectrum disorder, part II.
6. The FASEB Journal. 2007;21(6):1b21.
*This column was updated 11/30/2018.
NIH director expresses concern over CRISPR-cas9 baby claim
The National Institutes of Health is deeply concerned about the work just presented at the Second International Summit on Human Genome Editing in Hong Kong by Dr. He Jiankui, who described his effort using CRISPR-Cas9 on human embryos to disable the CCR5 gene. He claims that the two embryos were subsequently implanted, and infant twins have been born.
This work represents a deeply disturbing willingness by Dr. He and his team to flout international ethical norms. The project was largely carried out in secret, the medical necessity for inactivation of CCR5 in these infants is utterly unconvincing, the informed consent process appears highly questionable, and the possibility of damaging off-target effects has not been satisfactorily explored. It is profoundly unfortunate that the first apparent application of this powerful technique to the human germline has been carried out so irresponsibly.
The need for development of binding international consensus on setting limits for this kind of research, now being debated in Hong Kong, has never been more apparent. Without such limits, the world will face the serious risk of a deluge of similarly ill-considered and unethical projects.
Should such epic scientific misadventures proceed, a technology with enormous promise for prevention and treatment of disease will be overshadowed by justifiable public outrage, fear, and disgust.
Lest there be any doubt, and as we have stated previously, NIH does not support the use of gene-editing technologies in human embryos.
Francis S. Collins, M.D., Ph.D. is director of the National Institutes of Health. His comments were made in a statement Nov. 28.
The National Institutes of Health is deeply concerned about the work just presented at the Second International Summit on Human Genome Editing in Hong Kong by Dr. He Jiankui, who described his effort using CRISPR-Cas9 on human embryos to disable the CCR5 gene. He claims that the two embryos were subsequently implanted, and infant twins have been born.
This work represents a deeply disturbing willingness by Dr. He and his team to flout international ethical norms. The project was largely carried out in secret, the medical necessity for inactivation of CCR5 in these infants is utterly unconvincing, the informed consent process appears highly questionable, and the possibility of damaging off-target effects has not been satisfactorily explored. It is profoundly unfortunate that the first apparent application of this powerful technique to the human germline has been carried out so irresponsibly.
The need for development of binding international consensus on setting limits for this kind of research, now being debated in Hong Kong, has never been more apparent. Without such limits, the world will face the serious risk of a deluge of similarly ill-considered and unethical projects.
Should such epic scientific misadventures proceed, a technology with enormous promise for prevention and treatment of disease will be overshadowed by justifiable public outrage, fear, and disgust.
Lest there be any doubt, and as we have stated previously, NIH does not support the use of gene-editing technologies in human embryos.
Francis S. Collins, M.D., Ph.D. is director of the National Institutes of Health. His comments were made in a statement Nov. 28.
The National Institutes of Health is deeply concerned about the work just presented at the Second International Summit on Human Genome Editing in Hong Kong by Dr. He Jiankui, who described his effort using CRISPR-Cas9 on human embryos to disable the CCR5 gene. He claims that the two embryos were subsequently implanted, and infant twins have been born.
This work represents a deeply disturbing willingness by Dr. He and his team to flout international ethical norms. The project was largely carried out in secret, the medical necessity for inactivation of CCR5 in these infants is utterly unconvincing, the informed consent process appears highly questionable, and the possibility of damaging off-target effects has not been satisfactorily explored. It is profoundly unfortunate that the first apparent application of this powerful technique to the human germline has been carried out so irresponsibly.
The need for development of binding international consensus on setting limits for this kind of research, now being debated in Hong Kong, has never been more apparent. Without such limits, the world will face the serious risk of a deluge of similarly ill-considered and unethical projects.
Should such epic scientific misadventures proceed, a technology with enormous promise for prevention and treatment of disease will be overshadowed by justifiable public outrage, fear, and disgust.
Lest there be any doubt, and as we have stated previously, NIH does not support the use of gene-editing technologies in human embryos.
Francis S. Collins, M.D., Ph.D. is director of the National Institutes of Health. His comments were made in a statement Nov. 28.
Recognize gender expression in youth
It has been known for decades that sex and gender cannot be determined solely by birth anatomy and chromosomes.1 Over the past decade, the medical community has been able to better understand the biologic underpinnings of gender identity, and we are gaining a better appreciation for the diversity of gender identities and gender expressions that exist.
Gender expression can be defined as the manner in which an individual chooses to present their gender to others through physical appearance and behaviors, such as style of hair or dress, voice or movement.2 Gender nonconformity (GNC) is when an individual’s gender expression does not fully conform with societal expectations often based on an individual’s sex assigned at birth. It is important to note that gender expression is independent of gender identity and may or may not align with gender identity. For example, a person whose sex assigned at birth is female may adopt hairstyles and clothing that are considered more masculine and enjoy activities that are typically associated with masculinity (for example, sports) yet identify as female. The majority of research to date focuses most on transgender individuals, broadly defined as those whose gender identity does not fully align with the sex assigned at birth.3,4 As our understanding of gender expression and GNC expands, more research is emerging on the prevalence of gender nonconformity in youth and potential associations with various health outcomes.
Stigma, discrimination, and harassment are known to have documented effects on health. GNC youth have been shown to experience discrimination and harassment at rates higher than their gender conforming peers.5,6 A recent study by Lowry et al. sought to examine the association between GNC and indicators of mental distress and substance use in adolescents.7 The authors analyzed a subset of cross-sectional data from more than 6,000 youth who had participated in the Youth Risk Behavior Surveillance–United States, 2015 (YRBS) in three large urban school districts (two in California and one in Florida). In addition to the standard YRBS questions, students at these three school districts were asked about their gender expression using the following question: “A person’s appearance style, dress, or the way they walk or talk may affect how people describe them. How do you think people at your school would describe you?” Based on responses, youth were categorized on a 7-point GNC scale with 1 being most gender conforming (a very feminine female student or very masculine male student) to 7 being most GNC (a very masculine female student or a very feminine male student). The study sample was ethnically diverse with 16% of students identifying as white non-Hispanic, 19% identifying as black non-Hispanic, and 55% identifying as Hispanic of any race.
In the study population, approximately one in five students reported either moderate (students who described themselves as equally feminine and masculine) or high (female students who described themselves as very/mostly/somewhat masculine or male students who described themselves as very/mostly/somewhat feminine) levels of GNC. Among female students, moderate GNC was significantly associated with feeling sad and hopeless, seriously considering attempting suicide, and making a suicide plan. However, in female students substance use was not associated with GNC. Among male students, suicidal thoughts, plans, and attempts all demonstrated a linear increase with GNC, with the greatest prevalence occurring in male students expressing high levels of GNC. Prevalence of substance use, specifically nonmedical use of prescription drugs, cocaine use, methamphetamine use, heroin use, and intravenous drug also was associated with high GNC in male students. Study authors hypothesize that these differences occur because GNC male youth experience more overt harassment, compared with GNC female youth, but further study is needed.
Our understanding of the diversity of gender expressions present in youth populations continues to evolve. Findings from this study add to a growing body of evidence demonstrating a relatively high prevalence of GNC in youth populations, and potential health disparities these youth may face. This study underscores the need for continued study in this area. Family support and acceptance have been demonstrated to be strong protective factors for transgender-, lesbian-, and gay-identified youth. Studies identifying protective factors for GNC youth are needed.4
As health care providers, we need to continue to ask patients and families about gender identity and be aware of gender expression. When youth present as GNC, we should recognize that they may be at increased risk and, in addition to assessing overall mental health and risk for substance use, also assess for degree of social/familial support and potential stressors.4 We also should continue to advocate for support systems within schools sensitive to the needs of GNC students, as these may be a potential avenue to improve overall mental health for students. It is important to continue to expand our understanding of the diverse gender identities and expressions of the youth we serve. This hopefully will allow us to identify not only potential risk factors and health disparities, but also protective factors that can help better inform the development of effective interventions so all youth can reach their full potential.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus. Email her at [email protected].
References
1. “WPATH (World Professional Association of Transgender Health) Board Responds to Federal Effort to Redefine Gender,” press release, Oct. 23, 2018.
2. “LGBTQ+ Definitions” at Trans Student Educational Resources.3. J Sex Res. 2013;50(3-4):299-317.
4. JAMA Pediatr. 2018 Nov 1;172(11):1010-1.
5. Psychol Sex Orientat Gend Divers. 2016 Dec;3(4):489-98.
6. J Adolesc Health. 2016; 58(2)(supple):S1-2.
7. JAMA Pediatr. 2018 Nov;172(11):1020-8.
It has been known for decades that sex and gender cannot be determined solely by birth anatomy and chromosomes.1 Over the past decade, the medical community has been able to better understand the biologic underpinnings of gender identity, and we are gaining a better appreciation for the diversity of gender identities and gender expressions that exist.
Gender expression can be defined as the manner in which an individual chooses to present their gender to others through physical appearance and behaviors, such as style of hair or dress, voice or movement.2 Gender nonconformity (GNC) is when an individual’s gender expression does not fully conform with societal expectations often based on an individual’s sex assigned at birth. It is important to note that gender expression is independent of gender identity and may or may not align with gender identity. For example, a person whose sex assigned at birth is female may adopt hairstyles and clothing that are considered more masculine and enjoy activities that are typically associated with masculinity (for example, sports) yet identify as female. The majority of research to date focuses most on transgender individuals, broadly defined as those whose gender identity does not fully align with the sex assigned at birth.3,4 As our understanding of gender expression and GNC expands, more research is emerging on the prevalence of gender nonconformity in youth and potential associations with various health outcomes.
Stigma, discrimination, and harassment are known to have documented effects on health. GNC youth have been shown to experience discrimination and harassment at rates higher than their gender conforming peers.5,6 A recent study by Lowry et al. sought to examine the association between GNC and indicators of mental distress and substance use in adolescents.7 The authors analyzed a subset of cross-sectional data from more than 6,000 youth who had participated in the Youth Risk Behavior Surveillance–United States, 2015 (YRBS) in three large urban school districts (two in California and one in Florida). In addition to the standard YRBS questions, students at these three school districts were asked about their gender expression using the following question: “A person’s appearance style, dress, or the way they walk or talk may affect how people describe them. How do you think people at your school would describe you?” Based on responses, youth were categorized on a 7-point GNC scale with 1 being most gender conforming (a very feminine female student or very masculine male student) to 7 being most GNC (a very masculine female student or a very feminine male student). The study sample was ethnically diverse with 16% of students identifying as white non-Hispanic, 19% identifying as black non-Hispanic, and 55% identifying as Hispanic of any race.
In the study population, approximately one in five students reported either moderate (students who described themselves as equally feminine and masculine) or high (female students who described themselves as very/mostly/somewhat masculine or male students who described themselves as very/mostly/somewhat feminine) levels of GNC. Among female students, moderate GNC was significantly associated with feeling sad and hopeless, seriously considering attempting suicide, and making a suicide plan. However, in female students substance use was not associated with GNC. Among male students, suicidal thoughts, plans, and attempts all demonstrated a linear increase with GNC, with the greatest prevalence occurring in male students expressing high levels of GNC. Prevalence of substance use, specifically nonmedical use of prescription drugs, cocaine use, methamphetamine use, heroin use, and intravenous drug also was associated with high GNC in male students. Study authors hypothesize that these differences occur because GNC male youth experience more overt harassment, compared with GNC female youth, but further study is needed.
Our understanding of the diversity of gender expressions present in youth populations continues to evolve. Findings from this study add to a growing body of evidence demonstrating a relatively high prevalence of GNC in youth populations, and potential health disparities these youth may face. This study underscores the need for continued study in this area. Family support and acceptance have been demonstrated to be strong protective factors for transgender-, lesbian-, and gay-identified youth. Studies identifying protective factors for GNC youth are needed.4
As health care providers, we need to continue to ask patients and families about gender identity and be aware of gender expression. When youth present as GNC, we should recognize that they may be at increased risk and, in addition to assessing overall mental health and risk for substance use, also assess for degree of social/familial support and potential stressors.4 We also should continue to advocate for support systems within schools sensitive to the needs of GNC students, as these may be a potential avenue to improve overall mental health for students. It is important to continue to expand our understanding of the diverse gender identities and expressions of the youth we serve. This hopefully will allow us to identify not only potential risk factors and health disparities, but also protective factors that can help better inform the development of effective interventions so all youth can reach their full potential.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus. Email her at [email protected].
References
1. “WPATH (World Professional Association of Transgender Health) Board Responds to Federal Effort to Redefine Gender,” press release, Oct. 23, 2018.
2. “LGBTQ+ Definitions” at Trans Student Educational Resources.3. J Sex Res. 2013;50(3-4):299-317.
4. JAMA Pediatr. 2018 Nov 1;172(11):1010-1.
5. Psychol Sex Orientat Gend Divers. 2016 Dec;3(4):489-98.
6. J Adolesc Health. 2016; 58(2)(supple):S1-2.
7. JAMA Pediatr. 2018 Nov;172(11):1020-8.
It has been known for decades that sex and gender cannot be determined solely by birth anatomy and chromosomes.1 Over the past decade, the medical community has been able to better understand the biologic underpinnings of gender identity, and we are gaining a better appreciation for the diversity of gender identities and gender expressions that exist.
Gender expression can be defined as the manner in which an individual chooses to present their gender to others through physical appearance and behaviors, such as style of hair or dress, voice or movement.2 Gender nonconformity (GNC) is when an individual’s gender expression does not fully conform with societal expectations often based on an individual’s sex assigned at birth. It is important to note that gender expression is independent of gender identity and may or may not align with gender identity. For example, a person whose sex assigned at birth is female may adopt hairstyles and clothing that are considered more masculine and enjoy activities that are typically associated with masculinity (for example, sports) yet identify as female. The majority of research to date focuses most on transgender individuals, broadly defined as those whose gender identity does not fully align with the sex assigned at birth.3,4 As our understanding of gender expression and GNC expands, more research is emerging on the prevalence of gender nonconformity in youth and potential associations with various health outcomes.
Stigma, discrimination, and harassment are known to have documented effects on health. GNC youth have been shown to experience discrimination and harassment at rates higher than their gender conforming peers.5,6 A recent study by Lowry et al. sought to examine the association between GNC and indicators of mental distress and substance use in adolescents.7 The authors analyzed a subset of cross-sectional data from more than 6,000 youth who had participated in the Youth Risk Behavior Surveillance–United States, 2015 (YRBS) in three large urban school districts (two in California and one in Florida). In addition to the standard YRBS questions, students at these three school districts were asked about their gender expression using the following question: “A person’s appearance style, dress, or the way they walk or talk may affect how people describe them. How do you think people at your school would describe you?” Based on responses, youth were categorized on a 7-point GNC scale with 1 being most gender conforming (a very feminine female student or very masculine male student) to 7 being most GNC (a very masculine female student or a very feminine male student). The study sample was ethnically diverse with 16% of students identifying as white non-Hispanic, 19% identifying as black non-Hispanic, and 55% identifying as Hispanic of any race.
In the study population, approximately one in five students reported either moderate (students who described themselves as equally feminine and masculine) or high (female students who described themselves as very/mostly/somewhat masculine or male students who described themselves as very/mostly/somewhat feminine) levels of GNC. Among female students, moderate GNC was significantly associated with feeling sad and hopeless, seriously considering attempting suicide, and making a suicide plan. However, in female students substance use was not associated with GNC. Among male students, suicidal thoughts, plans, and attempts all demonstrated a linear increase with GNC, with the greatest prevalence occurring in male students expressing high levels of GNC. Prevalence of substance use, specifically nonmedical use of prescription drugs, cocaine use, methamphetamine use, heroin use, and intravenous drug also was associated with high GNC in male students. Study authors hypothesize that these differences occur because GNC male youth experience more overt harassment, compared with GNC female youth, but further study is needed.
Our understanding of the diversity of gender expressions present in youth populations continues to evolve. Findings from this study add to a growing body of evidence demonstrating a relatively high prevalence of GNC in youth populations, and potential health disparities these youth may face. This study underscores the need for continued study in this area. Family support and acceptance have been demonstrated to be strong protective factors for transgender-, lesbian-, and gay-identified youth. Studies identifying protective factors for GNC youth are needed.4
As health care providers, we need to continue to ask patients and families about gender identity and be aware of gender expression. When youth present as GNC, we should recognize that they may be at increased risk and, in addition to assessing overall mental health and risk for substance use, also assess for degree of social/familial support and potential stressors.4 We also should continue to advocate for support systems within schools sensitive to the needs of GNC students, as these may be a potential avenue to improve overall mental health for students. It is important to continue to expand our understanding of the diverse gender identities and expressions of the youth we serve. This hopefully will allow us to identify not only potential risk factors and health disparities, but also protective factors that can help better inform the development of effective interventions so all youth can reach their full potential.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus. Email her at [email protected].
References
1. “WPATH (World Professional Association of Transgender Health) Board Responds to Federal Effort to Redefine Gender,” press release, Oct. 23, 2018.
2. “LGBTQ+ Definitions” at Trans Student Educational Resources.3. J Sex Res. 2013;50(3-4):299-317.
4. JAMA Pediatr. 2018 Nov 1;172(11):1010-1.
5. Psychol Sex Orientat Gend Divers. 2016 Dec;3(4):489-98.
6. J Adolesc Health. 2016; 58(2)(supple):S1-2.
7. JAMA Pediatr. 2018 Nov;172(11):1020-8.
The powerful virus inflammatory response
Inflammation is a double-edged sword. Controlled and modest proinflammatory responses can enhance host immunity against viruses and decrease bacterial colonization and infection, whereas excessive uncontrolled proinflammatory responses may increase the susceptibility to bacterial colonization and secondary infection to facilitate disease pathogenesis. The immune system produces both proinflammatory and anti-inflammatory cytokines and chemokines. It is a balanced response that is key to maintaining good health.
Viral upper respiratory tract infections (URIs) are caused by rhinoviruses, coronaviruses, enteroviruses, respiratory syncytial viruses, influenza A and B viruses, parainfluenza viruses, adenoviruses, and human metapneumoviruses. Viruses are powerful. In the nose, they induce hypersecretion of mucus, slow cilia beating, up-regulate nasal epithelial cell receptors to facilitate bacterial attachment, suppress neutrophil function, and cause increased release of proinflammatory cytokines and chemokines. All these actions by respiratory viruses promote bacterial overgrowth in the nasopharynx and thereby facilitate bacterial superinfections. In fact, progression in pathogenesis of the common bacterial respiratory infections – acute otitis media, acute sinusitis, acute conjunctivitis, and pneumonia – almost always is preceded by a viral URI. Viruses activate multiple target cells in the upper respiratory tract to produce an array of proinflammatory cytokines and chemokines. The symptoms of a viral URI resolve coinciding with an anti-inflammatory response and adaptive immunity.
In recent work, we found a higher frequency of viral URIs in children who experienced more frequent acute otitis media (AOM). We sought to understand why this might occur by comparing levels of inflammatory cytokines/chemokines in the nose during viral URI that did not precipitate AOM versus when a viral URI precipitated an AOM episode. When a child had a viral URI but did not go on to experience an AOM, the child had higher proinflammatory responses than when the viral URI precipitated an AOM. When differences of levels of proinflammatory cytokines/chemokines were compared in otitis-prone and non–otitis-prone children, lower nasal responses were associated with higher otitis-prone classification frequency (Clin Infect Dis. 2018. doi: 10.1093/cid/ciy750).
The powerful virus and the inflammatory response it can induce also play a major role in allergy and asthma. Viral URIs enhance allergic sensitization to respiratory viruses, such as influenza and respiratory syncytial virus, cause cytopathic damage to airway epithelium, promote excessive proinflammatory cytokine/chemokine production, and increase the exposure of allergens and irritants to antigen-presenting cells. Viral infections also may induce the release of epithelial mediators and cytokines that may propagate eosinophilia. Viral URIs, particularly with respiratory syncytial virus and rhinovirus, are the most common causes of wheezing in children, and they have important influences on the development of asthma. Studies have shown that viral infections trigger up to 85% of asthma exacerbations in school-aged children.
Because this column is being published during the winter, a brief discussion of influenza as a powerful virus is appropriate. Influenza occurs in winter outbreaks of varying extent every year. The severity of the influenza season reflects the changing nature of the antigenic properties of influenza viruses, and their spread depends on susceptibility of the population. Influenza outbreaks typically peak over a 2-3 week period and last for 2-3 months. Most outbreaks have attack rates of 10%-20% in children. There may be variations in disease severity caused by different influenza virus types. The symptoms are caused by excessive proinflammatory cytokine/chemokine production in the nose and lung.
Influenza and other viruses can precipitate the systemic inflammatory response syndrome (SIRS), a manifestation of extreme immune dysregulation resulting in organ dysfunction that clinically resembles bacterial sepsis. In this syndrome, tissues remote from the original insult display the cardinal signs of inflammation, including vasodilation, increased microvascular permeability, and leukocyte accumulation. SIRS is another example of the double-edged sword of inflammation.
The onset and progression of SIRS occurs because of dysregulation of the normal inflammatory response, usually with an increase in both proinflammatory and anti-inflammatory cytokines and chemokines, initiating a chain of events that leads to organ failure.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. He reported having no conflicts of interest. Email him at [email protected].
Inflammation is a double-edged sword. Controlled and modest proinflammatory responses can enhance host immunity against viruses and decrease bacterial colonization and infection, whereas excessive uncontrolled proinflammatory responses may increase the susceptibility to bacterial colonization and secondary infection to facilitate disease pathogenesis. The immune system produces both proinflammatory and anti-inflammatory cytokines and chemokines. It is a balanced response that is key to maintaining good health.
Viral upper respiratory tract infections (URIs) are caused by rhinoviruses, coronaviruses, enteroviruses, respiratory syncytial viruses, influenza A and B viruses, parainfluenza viruses, adenoviruses, and human metapneumoviruses. Viruses are powerful. In the nose, they induce hypersecretion of mucus, slow cilia beating, up-regulate nasal epithelial cell receptors to facilitate bacterial attachment, suppress neutrophil function, and cause increased release of proinflammatory cytokines and chemokines. All these actions by respiratory viruses promote bacterial overgrowth in the nasopharynx and thereby facilitate bacterial superinfections. In fact, progression in pathogenesis of the common bacterial respiratory infections – acute otitis media, acute sinusitis, acute conjunctivitis, and pneumonia – almost always is preceded by a viral URI. Viruses activate multiple target cells in the upper respiratory tract to produce an array of proinflammatory cytokines and chemokines. The symptoms of a viral URI resolve coinciding with an anti-inflammatory response and adaptive immunity.
In recent work, we found a higher frequency of viral URIs in children who experienced more frequent acute otitis media (AOM). We sought to understand why this might occur by comparing levels of inflammatory cytokines/chemokines in the nose during viral URI that did not precipitate AOM versus when a viral URI precipitated an AOM episode. When a child had a viral URI but did not go on to experience an AOM, the child had higher proinflammatory responses than when the viral URI precipitated an AOM. When differences of levels of proinflammatory cytokines/chemokines were compared in otitis-prone and non–otitis-prone children, lower nasal responses were associated with higher otitis-prone classification frequency (Clin Infect Dis. 2018. doi: 10.1093/cid/ciy750).
The powerful virus and the inflammatory response it can induce also play a major role in allergy and asthma. Viral URIs enhance allergic sensitization to respiratory viruses, such as influenza and respiratory syncytial virus, cause cytopathic damage to airway epithelium, promote excessive proinflammatory cytokine/chemokine production, and increase the exposure of allergens and irritants to antigen-presenting cells. Viral infections also may induce the release of epithelial mediators and cytokines that may propagate eosinophilia. Viral URIs, particularly with respiratory syncytial virus and rhinovirus, are the most common causes of wheezing in children, and they have important influences on the development of asthma. Studies have shown that viral infections trigger up to 85% of asthma exacerbations in school-aged children.
Because this column is being published during the winter, a brief discussion of influenza as a powerful virus is appropriate. Influenza occurs in winter outbreaks of varying extent every year. The severity of the influenza season reflects the changing nature of the antigenic properties of influenza viruses, and their spread depends on susceptibility of the population. Influenza outbreaks typically peak over a 2-3 week period and last for 2-3 months. Most outbreaks have attack rates of 10%-20% in children. There may be variations in disease severity caused by different influenza virus types. The symptoms are caused by excessive proinflammatory cytokine/chemokine production in the nose and lung.
Influenza and other viruses can precipitate the systemic inflammatory response syndrome (SIRS), a manifestation of extreme immune dysregulation resulting in organ dysfunction that clinically resembles bacterial sepsis. In this syndrome, tissues remote from the original insult display the cardinal signs of inflammation, including vasodilation, increased microvascular permeability, and leukocyte accumulation. SIRS is another example of the double-edged sword of inflammation.
The onset and progression of SIRS occurs because of dysregulation of the normal inflammatory response, usually with an increase in both proinflammatory and anti-inflammatory cytokines and chemokines, initiating a chain of events that leads to organ failure.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. He reported having no conflicts of interest. Email him at [email protected].
Inflammation is a double-edged sword. Controlled and modest proinflammatory responses can enhance host immunity against viruses and decrease bacterial colonization and infection, whereas excessive uncontrolled proinflammatory responses may increase the susceptibility to bacterial colonization and secondary infection to facilitate disease pathogenesis. The immune system produces both proinflammatory and anti-inflammatory cytokines and chemokines. It is a balanced response that is key to maintaining good health.
Viral upper respiratory tract infections (URIs) are caused by rhinoviruses, coronaviruses, enteroviruses, respiratory syncytial viruses, influenza A and B viruses, parainfluenza viruses, adenoviruses, and human metapneumoviruses. Viruses are powerful. In the nose, they induce hypersecretion of mucus, slow cilia beating, up-regulate nasal epithelial cell receptors to facilitate bacterial attachment, suppress neutrophil function, and cause increased release of proinflammatory cytokines and chemokines. All these actions by respiratory viruses promote bacterial overgrowth in the nasopharynx and thereby facilitate bacterial superinfections. In fact, progression in pathogenesis of the common bacterial respiratory infections – acute otitis media, acute sinusitis, acute conjunctivitis, and pneumonia – almost always is preceded by a viral URI. Viruses activate multiple target cells in the upper respiratory tract to produce an array of proinflammatory cytokines and chemokines. The symptoms of a viral URI resolve coinciding with an anti-inflammatory response and adaptive immunity.
In recent work, we found a higher frequency of viral URIs in children who experienced more frequent acute otitis media (AOM). We sought to understand why this might occur by comparing levels of inflammatory cytokines/chemokines in the nose during viral URI that did not precipitate AOM versus when a viral URI precipitated an AOM episode. When a child had a viral URI but did not go on to experience an AOM, the child had higher proinflammatory responses than when the viral URI precipitated an AOM. When differences of levels of proinflammatory cytokines/chemokines were compared in otitis-prone and non–otitis-prone children, lower nasal responses were associated with higher otitis-prone classification frequency (Clin Infect Dis. 2018. doi: 10.1093/cid/ciy750).
The powerful virus and the inflammatory response it can induce also play a major role in allergy and asthma. Viral URIs enhance allergic sensitization to respiratory viruses, such as influenza and respiratory syncytial virus, cause cytopathic damage to airway epithelium, promote excessive proinflammatory cytokine/chemokine production, and increase the exposure of allergens and irritants to antigen-presenting cells. Viral infections also may induce the release of epithelial mediators and cytokines that may propagate eosinophilia. Viral URIs, particularly with respiratory syncytial virus and rhinovirus, are the most common causes of wheezing in children, and they have important influences on the development of asthma. Studies have shown that viral infections trigger up to 85% of asthma exacerbations in school-aged children.
Because this column is being published during the winter, a brief discussion of influenza as a powerful virus is appropriate. Influenza occurs in winter outbreaks of varying extent every year. The severity of the influenza season reflects the changing nature of the antigenic properties of influenza viruses, and their spread depends on susceptibility of the population. Influenza outbreaks typically peak over a 2-3 week period and last for 2-3 months. Most outbreaks have attack rates of 10%-20% in children. There may be variations in disease severity caused by different influenza virus types. The symptoms are caused by excessive proinflammatory cytokine/chemokine production in the nose and lung.
Influenza and other viruses can precipitate the systemic inflammatory response syndrome (SIRS), a manifestation of extreme immune dysregulation resulting in organ dysfunction that clinically resembles bacterial sepsis. In this syndrome, tissues remote from the original insult display the cardinal signs of inflammation, including vasodilation, increased microvascular permeability, and leukocyte accumulation. SIRS is another example of the double-edged sword of inflammation.
The onset and progression of SIRS occurs because of dysregulation of the normal inflammatory response, usually with an increase in both proinflammatory and anti-inflammatory cytokines and chemokines, initiating a chain of events that leads to organ failure.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. He reported having no conflicts of interest. Email him at [email protected].
Probative pee, Pilgrim obesity, and med school baked bribes
He tweets, he (doesn’t) score!
We all know that less sleep equals poor job performance. Up way too late on a Sunday night means you might fall face first into your keyboard the next morning and accidentally send an email that ends with “hhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhh.” So, yeah, sleep is important.
It’s especially important when you are a professional athlete and your entire livelihood depends on you being in tip-top shape. Researchers from the State University of New York at Stony Brook studied the performance of NBA players in relation to their late-night Twitter binges. Unsurprisingly, tweeting in the wee hours correlated with fewer points and fewer rebounds in the next day’s game. We’re sure coaches are just thrilled to hear about their players spending precious night hours @-ing random trolls on Twitter. Does this mean less tweeting and more sleep means anyone can be the next LeBron? Or, um, the next @KingJames? Probably not … but give it a try.
Poppy seeds and probative pee
As you tuck into your Thanksgiving leftovers, give a thought to a valiant physician who ate and drank – and peed – for science. Not just once, but twice.
At the recent Pain Care for Primary Care symposium in San Diego, Mount Sinai Beth Israel addiction specialist Edwin Salsitz, MD, gave a presentation about drug screening and mentioned his own homegrown investigation into two reputed sources of false positives.
A few years ago, a patient tested positive for opiates and, like many before him, blamed his fondness for poppy-seed bagels. Dr. Salsitz asked the patient to buy him a poppy bagel from his usual source, then the doctor went home and ate it on a Sunday prior to collecting his own pee. The doctor’s subsequent urine test was positive for opiates, and the patient was off the hook. (For more about the poppy-seed menace to accurate opiate testing, check this clinical update from the Aegis testing company.)
Later, it was time to check another possible urban legend. Dr. Salsitz got some mate de coca tea from a friend who’d returned from South America. Again, he took time out of a Sunday, this time to enjoy a hot beverage, mate de coca style, and collect his own pee. The urine test was positive this time, too – for cocaine.
The moral of the story? If you have a drug test looming, be safe and just stick to a croissant and coffee.
Psst … want a cookie?
In medical school, the best and brightest sacrifice their bodies and social lives to absorb knowledge like human sponges. Or maybe it’s where they absorb cookies in exchange for positive end-of-course evaluations.
Investigators from the University of Münster (Germany) decided to give 118 of the school’s third-year medical students a little test. During a course on emergency medicine, some groups were given access to free chocolate cookies (Discus deliciosum spp.) in their sessions, and some groups were not. When it came time to fill out their “student evaluations of teaching” at the end of the semester, the “cookie group” was more generous in its ratings of the course material and gave significantly higher scores to the teachers and to the course overall, compared with the control group (Med Educ. 2018 Oct;52[10]:1064-72).
This all seemed a little suspicious, so we did a little digging. Turns out that the cookie group – the one that provided all that warm, chocolatey positive reinforcement – was chock full of the usual suspects: Ernie the elf, Mrs. Fields, Famous Amos, and Mr. Big himself, Cookie Monster.
Why Myles Standish wasn’t fat
In the autumn of 1621, obesity didn’t dine with the 53 Pilgrims who gave culinary thanks for surviving their first disappointing Boston Bruins season. Er, for their first harvest after a brutal New England winter. Why was that first Thanksgiving such a svelte affair, free of the high-BMI epidemic that afflicts so many Bruins faithful nearly 4 centuries later? Was it the free-range turkey? The lean venison? The Wampanoag guests’ demands for a DASH-diet dinner?
A modern study may help reveal the historical truth: 17th century Plymouth Plantation wasn’t yet bisected by the 21st century Cape Cod traffic snarling the Pilgrims Highway, a.k.a. Massachusetts Route 3.
It was Spanish researchers, not English Puritans, who unbuckled the portly puzzle’s Pilgrim hat. Investigators with the Barcelona Institute for Global Health examined the link between traffic noise exposure and obesity markers among a group of Swiss adults. The verdict? Those exposed to the highest levels of traffic noise ran the greatest risk of becoming obese. Specifically, every 10-decibel rise in road noise packed on another 17% increase in obesity. Seems tractor-trailer downshifts and honking horns may disturb sleep, gridlocking glucose metabolism and diverting everyone to the nearest drive-thru.
Next on the Spaniards’ research to-do list: Can your New England uncle’s annual Turkey Day tales of Red Sox triumphs trigger psychosis among familial Yankees fans?
He tweets, he (doesn’t) score!
We all know that less sleep equals poor job performance. Up way too late on a Sunday night means you might fall face first into your keyboard the next morning and accidentally send an email that ends with “hhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhh.” So, yeah, sleep is important.
It’s especially important when you are a professional athlete and your entire livelihood depends on you being in tip-top shape. Researchers from the State University of New York at Stony Brook studied the performance of NBA players in relation to their late-night Twitter binges. Unsurprisingly, tweeting in the wee hours correlated with fewer points and fewer rebounds in the next day’s game. We’re sure coaches are just thrilled to hear about their players spending precious night hours @-ing random trolls on Twitter. Does this mean less tweeting and more sleep means anyone can be the next LeBron? Or, um, the next @KingJames? Probably not … but give it a try.
Poppy seeds and probative pee
As you tuck into your Thanksgiving leftovers, give a thought to a valiant physician who ate and drank – and peed – for science. Not just once, but twice.
At the recent Pain Care for Primary Care symposium in San Diego, Mount Sinai Beth Israel addiction specialist Edwin Salsitz, MD, gave a presentation about drug screening and mentioned his own homegrown investigation into two reputed sources of false positives.
A few years ago, a patient tested positive for opiates and, like many before him, blamed his fondness for poppy-seed bagels. Dr. Salsitz asked the patient to buy him a poppy bagel from his usual source, then the doctor went home and ate it on a Sunday prior to collecting his own pee. The doctor’s subsequent urine test was positive for opiates, and the patient was off the hook. (For more about the poppy-seed menace to accurate opiate testing, check this clinical update from the Aegis testing company.)
Later, it was time to check another possible urban legend. Dr. Salsitz got some mate de coca tea from a friend who’d returned from South America. Again, he took time out of a Sunday, this time to enjoy a hot beverage, mate de coca style, and collect his own pee. The urine test was positive this time, too – for cocaine.
The moral of the story? If you have a drug test looming, be safe and just stick to a croissant and coffee.
Psst … want a cookie?
In medical school, the best and brightest sacrifice their bodies and social lives to absorb knowledge like human sponges. Or maybe it’s where they absorb cookies in exchange for positive end-of-course evaluations.
Investigators from the University of Münster (Germany) decided to give 118 of the school’s third-year medical students a little test. During a course on emergency medicine, some groups were given access to free chocolate cookies (Discus deliciosum spp.) in their sessions, and some groups were not. When it came time to fill out their “student evaluations of teaching” at the end of the semester, the “cookie group” was more generous in its ratings of the course material and gave significantly higher scores to the teachers and to the course overall, compared with the control group (Med Educ. 2018 Oct;52[10]:1064-72).
This all seemed a little suspicious, so we did a little digging. Turns out that the cookie group – the one that provided all that warm, chocolatey positive reinforcement – was chock full of the usual suspects: Ernie the elf, Mrs. Fields, Famous Amos, and Mr. Big himself, Cookie Monster.
Why Myles Standish wasn’t fat
In the autumn of 1621, obesity didn’t dine with the 53 Pilgrims who gave culinary thanks for surviving their first disappointing Boston Bruins season. Er, for their first harvest after a brutal New England winter. Why was that first Thanksgiving such a svelte affair, free of the high-BMI epidemic that afflicts so many Bruins faithful nearly 4 centuries later? Was it the free-range turkey? The lean venison? The Wampanoag guests’ demands for a DASH-diet dinner?
A modern study may help reveal the historical truth: 17th century Plymouth Plantation wasn’t yet bisected by the 21st century Cape Cod traffic snarling the Pilgrims Highway, a.k.a. Massachusetts Route 3.
It was Spanish researchers, not English Puritans, who unbuckled the portly puzzle’s Pilgrim hat. Investigators with the Barcelona Institute for Global Health examined the link between traffic noise exposure and obesity markers among a group of Swiss adults. The verdict? Those exposed to the highest levels of traffic noise ran the greatest risk of becoming obese. Specifically, every 10-decibel rise in road noise packed on another 17% increase in obesity. Seems tractor-trailer downshifts and honking horns may disturb sleep, gridlocking glucose metabolism and diverting everyone to the nearest drive-thru.
Next on the Spaniards’ research to-do list: Can your New England uncle’s annual Turkey Day tales of Red Sox triumphs trigger psychosis among familial Yankees fans?
He tweets, he (doesn’t) score!
We all know that less sleep equals poor job performance. Up way too late on a Sunday night means you might fall face first into your keyboard the next morning and accidentally send an email that ends with “hhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhh.” So, yeah, sleep is important.
It’s especially important when you are a professional athlete and your entire livelihood depends on you being in tip-top shape. Researchers from the State University of New York at Stony Brook studied the performance of NBA players in relation to their late-night Twitter binges. Unsurprisingly, tweeting in the wee hours correlated with fewer points and fewer rebounds in the next day’s game. We’re sure coaches are just thrilled to hear about their players spending precious night hours @-ing random trolls on Twitter. Does this mean less tweeting and more sleep means anyone can be the next LeBron? Or, um, the next @KingJames? Probably not … but give it a try.
Poppy seeds and probative pee
As you tuck into your Thanksgiving leftovers, give a thought to a valiant physician who ate and drank – and peed – for science. Not just once, but twice.
At the recent Pain Care for Primary Care symposium in San Diego, Mount Sinai Beth Israel addiction specialist Edwin Salsitz, MD, gave a presentation about drug screening and mentioned his own homegrown investigation into two reputed sources of false positives.
A few years ago, a patient tested positive for opiates and, like many before him, blamed his fondness for poppy-seed bagels. Dr. Salsitz asked the patient to buy him a poppy bagel from his usual source, then the doctor went home and ate it on a Sunday prior to collecting his own pee. The doctor’s subsequent urine test was positive for opiates, and the patient was off the hook. (For more about the poppy-seed menace to accurate opiate testing, check this clinical update from the Aegis testing company.)
Later, it was time to check another possible urban legend. Dr. Salsitz got some mate de coca tea from a friend who’d returned from South America. Again, he took time out of a Sunday, this time to enjoy a hot beverage, mate de coca style, and collect his own pee. The urine test was positive this time, too – for cocaine.
The moral of the story? If you have a drug test looming, be safe and just stick to a croissant and coffee.
Psst … want a cookie?
In medical school, the best and brightest sacrifice their bodies and social lives to absorb knowledge like human sponges. Or maybe it’s where they absorb cookies in exchange for positive end-of-course evaluations.
Investigators from the University of Münster (Germany) decided to give 118 of the school’s third-year medical students a little test. During a course on emergency medicine, some groups were given access to free chocolate cookies (Discus deliciosum spp.) in their sessions, and some groups were not. When it came time to fill out their “student evaluations of teaching” at the end of the semester, the “cookie group” was more generous in its ratings of the course material and gave significantly higher scores to the teachers and to the course overall, compared with the control group (Med Educ. 2018 Oct;52[10]:1064-72).
This all seemed a little suspicious, so we did a little digging. Turns out that the cookie group – the one that provided all that warm, chocolatey positive reinforcement – was chock full of the usual suspects: Ernie the elf, Mrs. Fields, Famous Amos, and Mr. Big himself, Cookie Monster.
Why Myles Standish wasn’t fat
In the autumn of 1621, obesity didn’t dine with the 53 Pilgrims who gave culinary thanks for surviving their first disappointing Boston Bruins season. Er, for their first harvest after a brutal New England winter. Why was that first Thanksgiving such a svelte affair, free of the high-BMI epidemic that afflicts so many Bruins faithful nearly 4 centuries later? Was it the free-range turkey? The lean venison? The Wampanoag guests’ demands for a DASH-diet dinner?
A modern study may help reveal the historical truth: 17th century Plymouth Plantation wasn’t yet bisected by the 21st century Cape Cod traffic snarling the Pilgrims Highway, a.k.a. Massachusetts Route 3.
It was Spanish researchers, not English Puritans, who unbuckled the portly puzzle’s Pilgrim hat. Investigators with the Barcelona Institute for Global Health examined the link between traffic noise exposure and obesity markers among a group of Swiss adults. The verdict? Those exposed to the highest levels of traffic noise ran the greatest risk of becoming obese. Specifically, every 10-decibel rise in road noise packed on another 17% increase in obesity. Seems tractor-trailer downshifts and honking horns may disturb sleep, gridlocking glucose metabolism and diverting everyone to the nearest drive-thru.
Next on the Spaniards’ research to-do list: Can your New England uncle’s annual Turkey Day tales of Red Sox triumphs trigger psychosis among familial Yankees fans?
Transforming glycemic control at Norwalk Hospital
SHM eQUIPS program yields new protocols, guidelines
The Hospitalist recently sat down with Nancy J. Rennert, MD, FACE, FACP, CPHQ, chief of endocrinology and diabetes at Norwalk (Conn.) Hospital, Western Connecticut Health Network, to discuss her institution’s glycemic control initiatives.
Tell us a bit about your program:
Norwalk Hospital is a 366-bed community teaching hospital founded 125 years ago, now part of the growing Western Connecticut Health Network. Our residency and fellowship training programs are affiliated with Yale University, New Haven, Conn., and we are a branch campus of the University of Vermont, Burlington.
With leadership support, we created our Glycemic Care Team (GCT) 4 years ago to focus on improving the quality of care for persons with diabetes who were admitted to our hospital (often for another primary medical reason). Our hospitalists – 8 on the teaching service and 11 on the nonteaching service – are key players in our efforts as they care for the majority of medical inpatients. GCT is interdisciplinary and includes stakeholders at all levels, including quality, pharmacy, nutrition, hospital medicine, diabetes education, administrative leadership, endocrinology, information technology, point-of-care testing/pathology, surgery and more. We meet monthly with an agenda that includes safety events, glucometrics, and discussion of policies and protocols. Subgroups complete tasks in between the monthly meetings, and we bring in other clinical specialties as indicated based on the issues at hand.
What prior challenges did you encounter that led you to enroll in the Glycemic Control (GC) eQUIPS Program?
In order to know if our GCT was making a positive difference, we needed to first measure our baseline metrics and then identify our goals and develop our processes. We wanted actionable data analysis and the ability to differentiate areas of our hospital such as individual clinical units. After researching the options, we chose SHM’s GC eQUIPS Program, which we found to be user friendly. The national benchmarking was an important aspect for us as well. As a kick-off event, I invited Greg Maynard, MD, MHM, a hospitalist and the chief quality officer, UC Davis Medical Center, to speak on inpatient diabetes and was thrilled when he accepted my invitation. This provided an exciting start to our journey with SHM’s eQUIPS data management program.
As we began to obtain baseline measurements of glucose control, we needed a standardized, validated tool. The point-of-care glucose meters generated an enormous amount of data, but we were unable to sort this and analyze it in a meaningful and potentially actionable way. We were especially concerned about hypoglycemia. Our first task was to develop a prescriber ordered and nurse driven hypoglycemia protocol. How would we measure the overall effectiveness and success of the stepwise components of the protocol? The eQUIPS hypoglycemia management report was ideal in that it detailed metrics in stepwise fashion as it related to our protocol. For example, we were able to see the time from detection of hypoglycemia to the next point-of-care glucose check and to resolution of the event.
In addition, we wanted some comparative benchmarking data. The GC eQUIPS Program has a robust database of U.S. hospitals, which helped us define our ultimate goal – to be in the upper quartile of all measures. And we did it! Because of the amazing teamwork and leadership support, we were able to achieve national distinction from SHM as a “Top Performer” hospital for glycemic care.
How did the program help you and the team design your initiatives?
Data are powerful and convincing. We post and report our eQUIPS Glucometrics to our clinical staff monthly by unit, and through this process, we obtain the necessary “buy-ins” as well as participation to design clinical protocols and order sets. For example, we noted that many patients would be placed on “sliding scale”/coverage insulin alone at the time of hospital admission. This often would not be adjusted during the hospital stay. Our data showed that this practice was associated with more glucose fluctuations and hypoglycemia. When we reviewed this with our hospitalists, we achieved consensus and developed basal/bolus correction insulin protocols, which are embedded in the admission care sets. Following use of these order sets, we noted less hypoglycemia (decreased from 5.9% and remains less than 3.6%) and lower glucose variability. With the help of the eQUIPS metrics and benchmarking, we now have more than 20 protocols and safety rules built into our EHR system.
What were the key benefits that the GC eQUIPS Program provided that you were unable to find elsewhere?
The unique features we found most useful are the national benchmarking and “real-world” data presentation. National benchmarking allows us to compare ourselves with other hospitals (we can sort for like hospitals or all hospitals) and to periodically evaluate our processes and reexamine our goals. As part of this program, we can communicate with leaders of other high-performing hospitals and share strategies and challenges as well as discuss successes and failures. The quarterly benchmark webinar is another opportunity to be part of this professional community and we often pick up helpful information.
We particularly like the hyperglycemia/hypoglycemia scatter plots, which demonstrate the practical and important impact of glycemic control. Often there is a see-saw effect in which, if one parameter goes up, the other goes down; finding the sweet spot between hyperglycemia and hypoglycemia is key and clinically important.
Do you have any other comments to share related to your institution’s participation in the program?
We are fortunate to have many successes driven by our participation with the GC eQUIPS Program:
- Coordination of capillary blood glucose (CBG) testing, insulin administration and meal delivery: Use of rapid-acting insulin premeal is standard of care and requires that CBG testing, insulin, and meal delivery be precisely coordinated for optimal insulin action. We developed a process in which the catering associate calls the nurse using a voice-activated pager when the meal tray leaves the kitchen. Then, the nurse checks the CBG and gives insulin when the tray arrives. The tray contains a card to empower the patient to wait for the nurse to administer insulin prior to eating. This also provides an opportunity for nutritional education and carbohydrate awareness. Implementation of this process increased the percentage of patients who had a CBG and insulin administration within 15 minutes before a meal from less than 10% to more than 60%.
- Patient education regarding insulin use: In many cases, hospital patients may be started on insulin and their oral agents may be discontinued. This can be confusing and frightening to patients who often do not know if they will need to be on insulin long term. Our GCT created a script for the staff nurse to inform and reassure patients that this is standard practice and does not mean that they will need to remain on insulin after hospital discharge. The clinical team will communicate with the patient and together they will review treatment options. We have received many positive reviews from patients and staff for improving communication around this aspect of insulin therapy.
- Clinician and leader education: When our data revealed an uptick in hypoglycemia in our critical care units, we engaged the physicians, nurses, and staff and reviewed patient charts to identify potential process changes. To keep hypoglycemia in the spotlight, our director of critical care added hypoglycemia to the ICU checklist, which is discussed on all team clinical rounds. We are also developing an electronic metric (24-hour glucose maximum and minimum values) that can be quickly reviewed by the clinical team daily.
- Hypoglycemia and hyperkalemia: Analysis of our hypoglycemia data revealed a higher-than-expected rate in the ED in patients who did not have a diabetes diagnosis. Further review showed that this was associated with insulin treatment of hyperkalemia. Subsequently, we engaged our resident trainees and other team members in a study to characterize this hypoglycemia-hyperkalemia, and we have recently submitted a manuscript for publication detailing our findings and recommendations for glucose monitoring in these patients.
- Guideline for medical consultation on nonmedical services: Based on review of glucometrics on the nonmedical units and discussions with our hospitalist teams, we designed a guideline that includes recommendations for Medical Consultation in Nonmedical Admissions. Comanagement by a medical consultant will be requested earlier, and we will monitor if this influences glucometrics, patient and hospitalist satisfaction, etc.
- Medical student and house staff education: Two of our GCT hospitalists organize a monthly patient safety conference. After the students and trainees are asked to propose actionable solutions, the hospitalists discuss proposals generated at our GCT meetings. The students and trainees have the opportunity to participate in quality improvement, and we get great ideas from them as well.
Perhaps our biggest success is our Glycemic Care Team itself. We now receive questions and items to review from all departments and are seen as the hospital’s expert team on diabetes and hyperglycemia. It is truly a pleasure to lead this group of extremely high functioning and dedicated professionals. It is said that “team work makes the dream work.” Moving forward, I hope to expand our Glycemic Care Team to all the hospitals in our network.
SHM eQUIPS program yields new protocols, guidelines
SHM eQUIPS program yields new protocols, guidelines
The Hospitalist recently sat down with Nancy J. Rennert, MD, FACE, FACP, CPHQ, chief of endocrinology and diabetes at Norwalk (Conn.) Hospital, Western Connecticut Health Network, to discuss her institution’s glycemic control initiatives.
Tell us a bit about your program:
Norwalk Hospital is a 366-bed community teaching hospital founded 125 years ago, now part of the growing Western Connecticut Health Network. Our residency and fellowship training programs are affiliated with Yale University, New Haven, Conn., and we are a branch campus of the University of Vermont, Burlington.
With leadership support, we created our Glycemic Care Team (GCT) 4 years ago to focus on improving the quality of care for persons with diabetes who were admitted to our hospital (often for another primary medical reason). Our hospitalists – 8 on the teaching service and 11 on the nonteaching service – are key players in our efforts as they care for the majority of medical inpatients. GCT is interdisciplinary and includes stakeholders at all levels, including quality, pharmacy, nutrition, hospital medicine, diabetes education, administrative leadership, endocrinology, information technology, point-of-care testing/pathology, surgery and more. We meet monthly with an agenda that includes safety events, glucometrics, and discussion of policies and protocols. Subgroups complete tasks in between the monthly meetings, and we bring in other clinical specialties as indicated based on the issues at hand.
What prior challenges did you encounter that led you to enroll in the Glycemic Control (GC) eQUIPS Program?
In order to know if our GCT was making a positive difference, we needed to first measure our baseline metrics and then identify our goals and develop our processes. We wanted actionable data analysis and the ability to differentiate areas of our hospital such as individual clinical units. After researching the options, we chose SHM’s GC eQUIPS Program, which we found to be user friendly. The national benchmarking was an important aspect for us as well. As a kick-off event, I invited Greg Maynard, MD, MHM, a hospitalist and the chief quality officer, UC Davis Medical Center, to speak on inpatient diabetes and was thrilled when he accepted my invitation. This provided an exciting start to our journey with SHM’s eQUIPS data management program.
As we began to obtain baseline measurements of glucose control, we needed a standardized, validated tool. The point-of-care glucose meters generated an enormous amount of data, but we were unable to sort this and analyze it in a meaningful and potentially actionable way. We were especially concerned about hypoglycemia. Our first task was to develop a prescriber ordered and nurse driven hypoglycemia protocol. How would we measure the overall effectiveness and success of the stepwise components of the protocol? The eQUIPS hypoglycemia management report was ideal in that it detailed metrics in stepwise fashion as it related to our protocol. For example, we were able to see the time from detection of hypoglycemia to the next point-of-care glucose check and to resolution of the event.
In addition, we wanted some comparative benchmarking data. The GC eQUIPS Program has a robust database of U.S. hospitals, which helped us define our ultimate goal – to be in the upper quartile of all measures. And we did it! Because of the amazing teamwork and leadership support, we were able to achieve national distinction from SHM as a “Top Performer” hospital for glycemic care.
How did the program help you and the team design your initiatives?
Data are powerful and convincing. We post and report our eQUIPS Glucometrics to our clinical staff monthly by unit, and through this process, we obtain the necessary “buy-ins” as well as participation to design clinical protocols and order sets. For example, we noted that many patients would be placed on “sliding scale”/coverage insulin alone at the time of hospital admission. This often would not be adjusted during the hospital stay. Our data showed that this practice was associated with more glucose fluctuations and hypoglycemia. When we reviewed this with our hospitalists, we achieved consensus and developed basal/bolus correction insulin protocols, which are embedded in the admission care sets. Following use of these order sets, we noted less hypoglycemia (decreased from 5.9% and remains less than 3.6%) and lower glucose variability. With the help of the eQUIPS metrics and benchmarking, we now have more than 20 protocols and safety rules built into our EHR system.
What were the key benefits that the GC eQUIPS Program provided that you were unable to find elsewhere?
The unique features we found most useful are the national benchmarking and “real-world” data presentation. National benchmarking allows us to compare ourselves with other hospitals (we can sort for like hospitals or all hospitals) and to periodically evaluate our processes and reexamine our goals. As part of this program, we can communicate with leaders of other high-performing hospitals and share strategies and challenges as well as discuss successes and failures. The quarterly benchmark webinar is another opportunity to be part of this professional community and we often pick up helpful information.
We particularly like the hyperglycemia/hypoglycemia scatter plots, which demonstrate the practical and important impact of glycemic control. Often there is a see-saw effect in which, if one parameter goes up, the other goes down; finding the sweet spot between hyperglycemia and hypoglycemia is key and clinically important.
Do you have any other comments to share related to your institution’s participation in the program?
We are fortunate to have many successes driven by our participation with the GC eQUIPS Program:
- Coordination of capillary blood glucose (CBG) testing, insulin administration and meal delivery: Use of rapid-acting insulin premeal is standard of care and requires that CBG testing, insulin, and meal delivery be precisely coordinated for optimal insulin action. We developed a process in which the catering associate calls the nurse using a voice-activated pager when the meal tray leaves the kitchen. Then, the nurse checks the CBG and gives insulin when the tray arrives. The tray contains a card to empower the patient to wait for the nurse to administer insulin prior to eating. This also provides an opportunity for nutritional education and carbohydrate awareness. Implementation of this process increased the percentage of patients who had a CBG and insulin administration within 15 minutes before a meal from less than 10% to more than 60%.
- Patient education regarding insulin use: In many cases, hospital patients may be started on insulin and their oral agents may be discontinued. This can be confusing and frightening to patients who often do not know if they will need to be on insulin long term. Our GCT created a script for the staff nurse to inform and reassure patients that this is standard practice and does not mean that they will need to remain on insulin after hospital discharge. The clinical team will communicate with the patient and together they will review treatment options. We have received many positive reviews from patients and staff for improving communication around this aspect of insulin therapy.
- Clinician and leader education: When our data revealed an uptick in hypoglycemia in our critical care units, we engaged the physicians, nurses, and staff and reviewed patient charts to identify potential process changes. To keep hypoglycemia in the spotlight, our director of critical care added hypoglycemia to the ICU checklist, which is discussed on all team clinical rounds. We are also developing an electronic metric (24-hour glucose maximum and minimum values) that can be quickly reviewed by the clinical team daily.
- Hypoglycemia and hyperkalemia: Analysis of our hypoglycemia data revealed a higher-than-expected rate in the ED in patients who did not have a diabetes diagnosis. Further review showed that this was associated with insulin treatment of hyperkalemia. Subsequently, we engaged our resident trainees and other team members in a study to characterize this hypoglycemia-hyperkalemia, and we have recently submitted a manuscript for publication detailing our findings and recommendations for glucose monitoring in these patients.
- Guideline for medical consultation on nonmedical services: Based on review of glucometrics on the nonmedical units and discussions with our hospitalist teams, we designed a guideline that includes recommendations for Medical Consultation in Nonmedical Admissions. Comanagement by a medical consultant will be requested earlier, and we will monitor if this influences glucometrics, patient and hospitalist satisfaction, etc.
- Medical student and house staff education: Two of our GCT hospitalists organize a monthly patient safety conference. After the students and trainees are asked to propose actionable solutions, the hospitalists discuss proposals generated at our GCT meetings. The students and trainees have the opportunity to participate in quality improvement, and we get great ideas from them as well.
Perhaps our biggest success is our Glycemic Care Team itself. We now receive questions and items to review from all departments and are seen as the hospital’s expert team on diabetes and hyperglycemia. It is truly a pleasure to lead this group of extremely high functioning and dedicated professionals. It is said that “team work makes the dream work.” Moving forward, I hope to expand our Glycemic Care Team to all the hospitals in our network.
The Hospitalist recently sat down with Nancy J. Rennert, MD, FACE, FACP, CPHQ, chief of endocrinology and diabetes at Norwalk (Conn.) Hospital, Western Connecticut Health Network, to discuss her institution’s glycemic control initiatives.
Tell us a bit about your program:
Norwalk Hospital is a 366-bed community teaching hospital founded 125 years ago, now part of the growing Western Connecticut Health Network. Our residency and fellowship training programs are affiliated with Yale University, New Haven, Conn., and we are a branch campus of the University of Vermont, Burlington.
With leadership support, we created our Glycemic Care Team (GCT) 4 years ago to focus on improving the quality of care for persons with diabetes who were admitted to our hospital (often for another primary medical reason). Our hospitalists – 8 on the teaching service and 11 on the nonteaching service – are key players in our efforts as they care for the majority of medical inpatients. GCT is interdisciplinary and includes stakeholders at all levels, including quality, pharmacy, nutrition, hospital medicine, diabetes education, administrative leadership, endocrinology, information technology, point-of-care testing/pathology, surgery and more. We meet monthly with an agenda that includes safety events, glucometrics, and discussion of policies and protocols. Subgroups complete tasks in between the monthly meetings, and we bring in other clinical specialties as indicated based on the issues at hand.
What prior challenges did you encounter that led you to enroll in the Glycemic Control (GC) eQUIPS Program?
In order to know if our GCT was making a positive difference, we needed to first measure our baseline metrics and then identify our goals and develop our processes. We wanted actionable data analysis and the ability to differentiate areas of our hospital such as individual clinical units. After researching the options, we chose SHM’s GC eQUIPS Program, which we found to be user friendly. The national benchmarking was an important aspect for us as well. As a kick-off event, I invited Greg Maynard, MD, MHM, a hospitalist and the chief quality officer, UC Davis Medical Center, to speak on inpatient diabetes and was thrilled when he accepted my invitation. This provided an exciting start to our journey with SHM’s eQUIPS data management program.
As we began to obtain baseline measurements of glucose control, we needed a standardized, validated tool. The point-of-care glucose meters generated an enormous amount of data, but we were unable to sort this and analyze it in a meaningful and potentially actionable way. We were especially concerned about hypoglycemia. Our first task was to develop a prescriber ordered and nurse driven hypoglycemia protocol. How would we measure the overall effectiveness and success of the stepwise components of the protocol? The eQUIPS hypoglycemia management report was ideal in that it detailed metrics in stepwise fashion as it related to our protocol. For example, we were able to see the time from detection of hypoglycemia to the next point-of-care glucose check and to resolution of the event.
In addition, we wanted some comparative benchmarking data. The GC eQUIPS Program has a robust database of U.S. hospitals, which helped us define our ultimate goal – to be in the upper quartile of all measures. And we did it! Because of the amazing teamwork and leadership support, we were able to achieve national distinction from SHM as a “Top Performer” hospital for glycemic care.
How did the program help you and the team design your initiatives?
Data are powerful and convincing. We post and report our eQUIPS Glucometrics to our clinical staff monthly by unit, and through this process, we obtain the necessary “buy-ins” as well as participation to design clinical protocols and order sets. For example, we noted that many patients would be placed on “sliding scale”/coverage insulin alone at the time of hospital admission. This often would not be adjusted during the hospital stay. Our data showed that this practice was associated with more glucose fluctuations and hypoglycemia. When we reviewed this with our hospitalists, we achieved consensus and developed basal/bolus correction insulin protocols, which are embedded in the admission care sets. Following use of these order sets, we noted less hypoglycemia (decreased from 5.9% and remains less than 3.6%) and lower glucose variability. With the help of the eQUIPS metrics and benchmarking, we now have more than 20 protocols and safety rules built into our EHR system.
What were the key benefits that the GC eQUIPS Program provided that you were unable to find elsewhere?
The unique features we found most useful are the national benchmarking and “real-world” data presentation. National benchmarking allows us to compare ourselves with other hospitals (we can sort for like hospitals or all hospitals) and to periodically evaluate our processes and reexamine our goals. As part of this program, we can communicate with leaders of other high-performing hospitals and share strategies and challenges as well as discuss successes and failures. The quarterly benchmark webinar is another opportunity to be part of this professional community and we often pick up helpful information.
We particularly like the hyperglycemia/hypoglycemia scatter plots, which demonstrate the practical and important impact of glycemic control. Often there is a see-saw effect in which, if one parameter goes up, the other goes down; finding the sweet spot between hyperglycemia and hypoglycemia is key and clinically important.
Do you have any other comments to share related to your institution’s participation in the program?
We are fortunate to have many successes driven by our participation with the GC eQUIPS Program:
- Coordination of capillary blood glucose (CBG) testing, insulin administration and meal delivery: Use of rapid-acting insulin premeal is standard of care and requires that CBG testing, insulin, and meal delivery be precisely coordinated for optimal insulin action. We developed a process in which the catering associate calls the nurse using a voice-activated pager when the meal tray leaves the kitchen. Then, the nurse checks the CBG and gives insulin when the tray arrives. The tray contains a card to empower the patient to wait for the nurse to administer insulin prior to eating. This also provides an opportunity for nutritional education and carbohydrate awareness. Implementation of this process increased the percentage of patients who had a CBG and insulin administration within 15 minutes before a meal from less than 10% to more than 60%.
- Patient education regarding insulin use: In many cases, hospital patients may be started on insulin and their oral agents may be discontinued. This can be confusing and frightening to patients who often do not know if they will need to be on insulin long term. Our GCT created a script for the staff nurse to inform and reassure patients that this is standard practice and does not mean that they will need to remain on insulin after hospital discharge. The clinical team will communicate with the patient and together they will review treatment options. We have received many positive reviews from patients and staff for improving communication around this aspect of insulin therapy.
- Clinician and leader education: When our data revealed an uptick in hypoglycemia in our critical care units, we engaged the physicians, nurses, and staff and reviewed patient charts to identify potential process changes. To keep hypoglycemia in the spotlight, our director of critical care added hypoglycemia to the ICU checklist, which is discussed on all team clinical rounds. We are also developing an electronic metric (24-hour glucose maximum and minimum values) that can be quickly reviewed by the clinical team daily.
- Hypoglycemia and hyperkalemia: Analysis of our hypoglycemia data revealed a higher-than-expected rate in the ED in patients who did not have a diabetes diagnosis. Further review showed that this was associated with insulin treatment of hyperkalemia. Subsequently, we engaged our resident trainees and other team members in a study to characterize this hypoglycemia-hyperkalemia, and we have recently submitted a manuscript for publication detailing our findings and recommendations for glucose monitoring in these patients.
- Guideline for medical consultation on nonmedical services: Based on review of glucometrics on the nonmedical units and discussions with our hospitalist teams, we designed a guideline that includes recommendations for Medical Consultation in Nonmedical Admissions. Comanagement by a medical consultant will be requested earlier, and we will monitor if this influences glucometrics, patient and hospitalist satisfaction, etc.
- Medical student and house staff education: Two of our GCT hospitalists organize a monthly patient safety conference. After the students and trainees are asked to propose actionable solutions, the hospitalists discuss proposals generated at our GCT meetings. The students and trainees have the opportunity to participate in quality improvement, and we get great ideas from them as well.
Perhaps our biggest success is our Glycemic Care Team itself. We now receive questions and items to review from all departments and are seen as the hospital’s expert team on diabetes and hyperglycemia. It is truly a pleasure to lead this group of extremely high functioning and dedicated professionals. It is said that “team work makes the dream work.” Moving forward, I hope to expand our Glycemic Care Team to all the hospitals in our network.