User login
Should beta-blockers be used in portal hypertension?
Dear colleagues and friends,
Thank you for your continued support of the Perspectives debates. In this edition, Dr. Guadalupe Garcia-Tsao and Dr. Marwan Ghabril discuss the rationale for and against beta-blocker therapy in portal hypertension, and ultimately highlight the nuances required for appropriate decision-making. This topic invariably generates controversy and debate, and is broadly relevant to general GI and hepatology practices. I hope you will find it as informative as I did, and I welcome your comments and suggestions for future topics at [email protected].
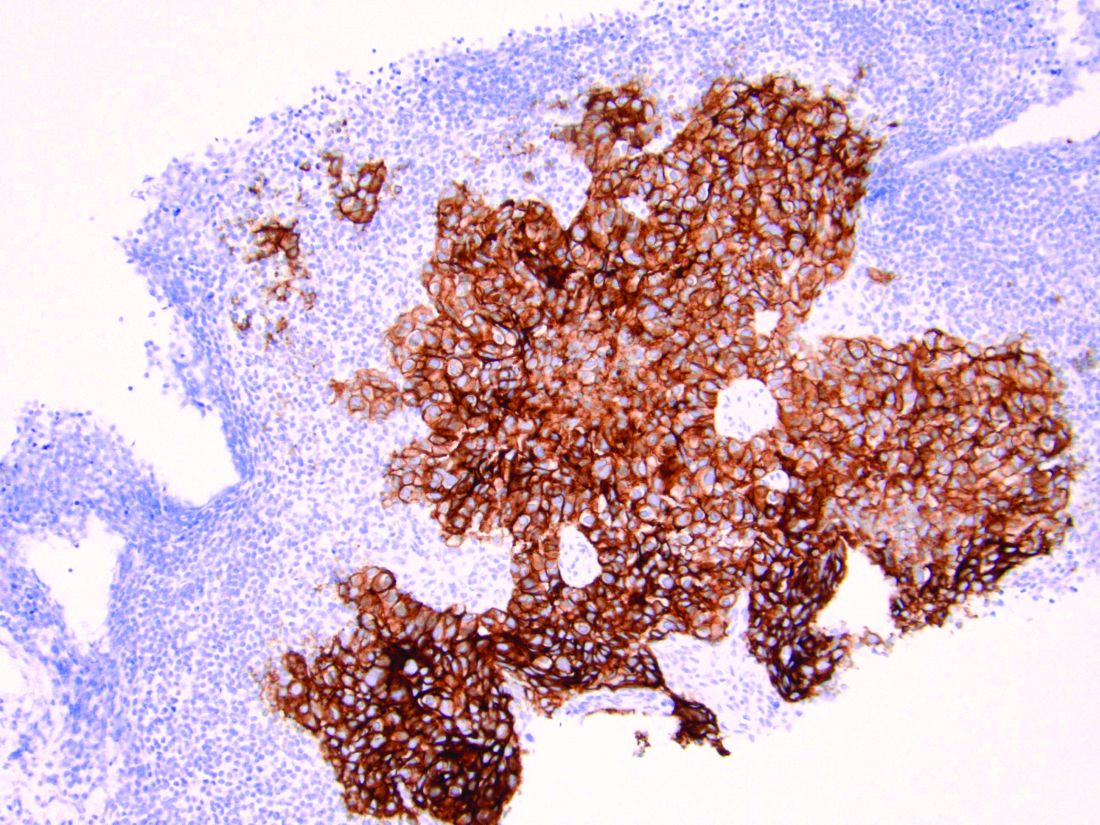
Charles J. Kahi, MD, MS, AGAF, professor of medicine, Indiana University, Indianapolis. He is also an associate editor for GI & Hepatology News.
Beta-blockers in portal hypertension – Yes!
BY GUADALUPE GARCIA-TSAO, MD
Portal hypertension is the main consequence of cirrhosis and is responsible for most of its complications. In compensated cirrhosis, a threshold portal pressure gradient, as determined by the hepatic venous pressure gradient (HVPG), of at least 10 mm Hg is the strongest predictor of clinical decompensation (ascites, variceal hemorrhage, or encephalopathy) which is, in turn, the main determinant of death in cirrhosis.
Portal hypertension is initially caused by an increase in intrahepatic resistance that leads to mild portal hypertension (HVPG, 5-10 mm Hg) but is then enhanced and maintained by an increase in portal venous inflow that leads to clinically significant portal hypertension (HVPG, at least 10 mm Hg).
Portal pressure can be reduced by either ameliorating intrahepatic resistance (which is mostly caused by structural changes that are difficult to reverse) and/or by decreasing portal vein blood inflow (the most modifiable pathogenic mechanism). For over 30 years, treatment of portal hypertension has been based on the use of nonselective beta-blockers (NSBB), drugs that decrease portal pressure through a reduction in splanchnic blood flow. Reduction in portal pressure is greater with NSBB (propranolol, nadolol) than with selective beta-blockers because, as demonstrated experimentally, the main portal pressure–reducing effect stems from splanchnic vasoconstriction because of beta2-adrenergic blockade. This has been confirmed in patients with cirrhosis, in whom the reduction in HVPG is greater with NSBB than with selective BB. On the other hand, carvedilol, an NSBB that also has a vasodilatory alpha1 adrenergic blocking effect, has a greater effect in reducing HVPG, compared with traditional NSBB.
A significant decrease in portal pressure has been associated with better outcomes in cirrhosis. A favorable portal pressure reduction (“response”) has been traditionally defined as a decrease in HVPG below 12 mm Hg or greater than 20% from baseline, although even decreases of 10% are associated with better outcomes. Initial studies had been focused on variceal hemorrhage, a complication that is clearly related to portal hypertension. In this setting, reducing portal pressure clearly leads to a decreased in the incidence of variceal hemorrhage and a decrease in mortality.1 More recently, the focus has been on preventing decompensation (in compensated cirrhosis) and preventing further decompensation/death (in decompensated cirrhosis).
In compensated cirrhosis, a recent meta-analysis of clinical trials of prevention of variceal hemorrhage showed that patients with varices (therefore with clinically significant portal hypertension) without ascites who were NSBB hemodynamic responders, had a reduced risk of developing not only variceal hemorrhage but also ascites and/or encephalopathy, and had lower mortality.2 More importantly, a recent seminal randomized, double-blind, placebo-controlled trial performed in patients with compensated cirrhosis and clinically significant portal hypertension with no or small varices, showed that NSBB (propranolol or carvedilol) led to a significantly lower incidence of decompensation, with ascites being the single event that was significantly lower in the NSBB group.3 This study thereby demonstrates that NSBBs not only reduce the risk of variceal hemorrhage, as previously demonstrated, but also significantly reduces the probability of developing ascites, the most common complication of cirrhosis.
In decompensated cirrhosis, a recent meta-analysis of clinical trials of prevention of variceal hemorrhage showed that patients with varices and ascites (decompensated) who were NSBB responders, had a reduced risk of developing not only variceal hemorrhage but also refractory ascites, spontaneous bacterial peritonitis and/or hepatorenal syndrome, and also had a lower mortality.2 In patients with variceal hemorrhage, the recommended therapy to prevent recurrent variceal hemorrhage is the combination of NSBB plus variceal ligation but this is based on trials that combined compensated and decompensated patients. An individual patient data meta-analysis of these trials showed that, in the group of patients with decompensated Child-Pugh class B/C cirrhosis, rebleeding and mortality were higher with ligation alone, compared with combined therapy with NSBBs and ligation, underlining that NSBB is the key element of combination therapy in these patients.4
There is a fading controversy regarding the potential for increased mortality with the use of NSBBs in patients with refractory ascites and SBP, reported in two retrospective studies.5 These studies lacked information regarding the number of patients in whom NSBBs were withdrawn before the last observation and number of patients in whom NSBBs were started in the course of follow-up. Notably, a recent meta-analysis that included these and subsequent retrospective studies, encompassing a collective of over 1,300 patients, demonstrated that NSBB use in patients with ascites is not related to increased mortality.1,4
Nevertheless, NSBBs should be used cautiously in patients with cirrhosis and ascites. Hemodynamic alterations typical of decompensated cirrhosis are maximal in patients with refractory ascites and spontaneous bacterial peritonitis and the use of NSBB in this setting could lead to worsening hemodynamics, with decreased mean arterial pressure and renal perfusion that could in turn lead to acute kidney injury and death. In studies showing a deleterious effect of NSBB, the mean arterial pressure was significantly lower in patients in the NSBB group.5 In a recent retrospective study, the beneficial effect of NSBBs in patients with refractory ascites, spontaneous bacterial peritonitis, and acute-on-chronic liver failure appeared to apply only to those with a mean arterial pressure of at least 65 mm Hg.6 This evidence has led to guideline recommendations that limit the dose of NSBB to a maximum of 160 mg/day for propranolol or 80 mg/day for nadolol in patients with ascites with close follow-up of arterial blood pressure. Carvedilol should preferably not be used. In the presence of a systolic blood pressure <90 mm Hg or acute kidney injury, NSBBs should be dose-reduced or discontinued. If a precipitant for hypotension is identified (e.g., spontaneous bacterial peritonitis), NSBB can be reinitiated once the precipitating event is resolved and hypotension/acute kidney injury has resolved.
In conclusion, NSBBs are a definite “yes” in the management of cirrhosis and portal hypertension as they prevent poor outcomes (including death) in patients with both compensated and decompensated cirrhosis. In patients with ascites and spontaneous bacterial peritonitis, NSBBs could have deleterious effects but these can be prevented by careful monitoring of blood pressure.
References
1. D’Amico G et al. Gastroenterology. 2006;131:1611-24.
2. Turco L et al. Clin Gastroenterol Hepatol. 2020;18:313-27.
3. Villanueva C et al. Lancet. 2019;393:1597-608.
4. Albillos A et al. Hepatology. 2017;66:1219-31.
5. Garcia-Tsao G. J Hepatol. 2016 Mar;64(3):532-4.
6. Tergast TL et al. Aliment Pharmacol. Ther 2019;50:696-706.
Dr. Garcia-Tsao is professor of medicine, digestive diseases; chief, digestive diseases, Veterans Affairs Connecticut Healthcare System; director, clinical and translational core, Yale Liver Center; program director, VA Connecticut Hepatitis C Resource Center, New Haven. She has no conflicts.
Can be a double-edged blade too dangerous to wield
BY MARWAN S. GHABRIL, MD, AGAF
Nonselective beta-blockers (NSBB) are a cornerstone in the primary and secondary prophylaxis of variceal bleeding in patients with cirrhosis and clinically significant portal hypertension (CSPH), defined as a hepatic venous pressure gradient (HVPG) of at least 10 mm Hg. In the absence of routine HVPG measurement in most clinical practices, NSBB therapy is targeted to a 25% heart rate reduction or target heart rate of 55-60 beats per minute. There is ample evidence supporting this indication for NSBB as summarized in the Baveno VI consensus recommendations in a wide range of liver disease severity, encompassing patients with low-risk small esophageal varices to those with large varices, stigmata, and advanced Child-Pugh class. Tasked with the contrarian perspective on NSBB use, the argument for caution hinges on observations that disease progression can shift the balance of risk and reward to NSBB minimization or avoidance. Understanding the hyperdynamic circulation in worsening portal hypertension of cirrhosis is paramount to these considerations.
The pathophysiology of portal hypertension
Portal hypertension arises as a result of both increased portal venous inflow and increased hepatic sinusoidal resistance and is characterized by splanchnic and systemic vasodilation and reduced effective systemic arterial volume. Compensatory mechanisms include systemic neurohormonal activation, increased heart rate and cardiac output, sodium and water retention (increased plasma volume), and vasoconstrictor system activation. These mechanisms suffice in restoring effective arterial volume initially but also contribute to increased splanchnic/portal inflow and portal hypertension. In advanced decompensation the cardiovascular reserve is overwhelmed with progressive systemic vasodilation, worsening sodium and water retention, vasoconstriction of vital organ vascular beds and an ineffective hyperdynamic state (tachycardia, inadequate cardiac output, and systemic hypotension). This pathophysiological state is heralded clinically by the development of worsening or refractory ascites, and belies the development of other complications of advanced cirrhosis including hyponatremia and hepatorenal syndrome.
The beneficial effects of NSBB in decreasing portal hypertension are mediated by inhibition of splanchnic vasodilation and cardiac effects (reduced heart rate and cardiac output) leading to reduced portal inflow. However, these cardiac effects can be deleterious to systemic hemodynamics in more advanced disease, particularly with acute insults that exacerbate arterial hypovolemia such as bleeding or infection. As such, blunting of sympathetic drive by NSBB carries different degrees of tolerance and risk depending on the hemodynamic reserve in the hyperdynamic state.
Reported clinical experiences
The controversy over NSBB use in advanced cirrhosis arises out of heterogeneous, commonly retrospective datasets and nonrandomized cohorts, with conflicting reports of positive, negative, or neutral effects on mortality and acute kidney injury. Not surprisingly, studies describing detrimental effects of NSBB are based on patients with strictly defined refractory ascites or those with spontaneous bacterial peritonitis.1,2 Importantly, these studies also describe significantly lower blood pressure in at-risk NSBB treated patients, This baseline hemodynamic difference is either not observed,or not explicitly compared in studies/subcohorts with decreased or unaffected mortality with NSBB use in advanced cirrhosis.2
In the largest prospective study of NSBB in cirrhosis with ascites (which used data from three randomized satavaptan trials), NSBB users and nonusers were more closely matched for baseline mean arterial pressure.3 There was no effect of NSBB on mortality but there was a 29% rate of NSBB discontinuation (i.e., intolerance) during the year of follow-up. Predictors of NSBB discontinuation were hospitalization, variceal bleeding, infection, hepatorenal syndrome, Child-Pugh class C, and refractory ascites. Furthermore, NSBB discontinuation was associated with a notable increase in mortality. Similarly, clinically driven discontinuation of NSBB was observed in half of hospitalized patients with acute-on-chronic liver failure in the prospective CANONIC study, and was also associated with significantly higher short-term mortality.
It is possible that NSBB tolerance may select patients with adequate hemodynamic reserve despite the severity of other liver decompensations. Conversely, intolerance of therapeutic NSBB may signify evolving inadequacy of hemodynamic reserve, giving rise to two distinctly different risk/benefit profiles. This double-edged blade perspective is supported by findings of impaired cardiac output in patients with refractory ascites with impaired renal perfusion, and increased wait-list mortality with NSBB use in patients with compromised global cardiac function.4,5
When is caution due?
Rather than a “therapeutic window” that is either wide open or suddenly shut, in nonhospitalized patients risk is on a continuum and there are no agreed upon liver-specific parameters that define strict barriers to NSBB treatment. Refractory ascites may not absolutely define the closure of this window but should put clinicians on notice for a patient’s vulnerability. The Baveno VI recommendations echo the need for caution, with NSBB in refractory ascites with close monitoring of blood pressure, serum sodium, and creatinine. Treatment cessation, reduction or temporary withholding, and careful reintroduction (with reversible insults) are advised in patients with systolic blood pressure <90 mm Hg, serum Na <130 mEq/L, or those with acute kidney injury.
In the absence of randomized trials that account for cirrhotic cardiomyopathy and cardiac reserve, the risks and putative nonvariceal benefits of NSBB (e.g., reducing gut bacterial translocation) are not truly defined in this patient population. We lack HVPG-based or surrogate assessments in routine practice to determine which patients are hemodynamically benefiting from NSBB therapy, or reliable indicators of imminent NSBB intolerance or risk. While the indications for NSBB may expand to prevention of decompensation, serious questions about their safety are being asked in advanced decompensation. Poor tolerance of therapeutic NSBB dosing and unquantified, but likely negative, impact on quality of life raise additional questions. In a shared decision-making partnership, the patient’s perspective on the utility, tolerance, and monitoring of NSBB therapy in preventing variceal bleeding is vital, particularly when there are endoscopic or earlier shunting alternatives. “Primum non nocere” is not a gladiatorial cry, and in the wrong patients NSBB can be a double-edged blade too dangerous to wield.
References
1. Serste T et al. Hepatology. 2010;52:1017-22.
2. Mandorfer M et al. Gastroenterology. 2014;146:1680-90 e1.
3. Bossen L et al. Hepatology. 2016;63:1968-76.
4. Giannelli V et al. J Hepatol. 2020;72:463-71.
5. Tellez L et al. J Hepatol. 2020 May 20. doi: 10.1016/j.jhep.2020.05.011.
Dr. Ghabril is a gastroenterologist with the Indiana University, Indianapolis. He has no conflicts.
Dear colleagues and friends,
Thank you for your continued support of the Perspectives debates. In this edition, Dr. Guadalupe Garcia-Tsao and Dr. Marwan Ghabril discuss the rationale for and against beta-blocker therapy in portal hypertension, and ultimately highlight the nuances required for appropriate decision-making. This topic invariably generates controversy and debate, and is broadly relevant to general GI and hepatology practices. I hope you will find it as informative as I did, and I welcome your comments and suggestions for future topics at [email protected].
Charles J. Kahi, MD, MS, AGAF, professor of medicine, Indiana University, Indianapolis. He is also an associate editor for GI & Hepatology News.
Beta-blockers in portal hypertension – Yes!
BY GUADALUPE GARCIA-TSAO, MD
Portal hypertension is the main consequence of cirrhosis and is responsible for most of its complications. In compensated cirrhosis, a threshold portal pressure gradient, as determined by the hepatic venous pressure gradient (HVPG), of at least 10 mm Hg is the strongest predictor of clinical decompensation (ascites, variceal hemorrhage, or encephalopathy) which is, in turn, the main determinant of death in cirrhosis.
Portal hypertension is initially caused by an increase in intrahepatic resistance that leads to mild portal hypertension (HVPG, 5-10 mm Hg) but is then enhanced and maintained by an increase in portal venous inflow that leads to clinically significant portal hypertension (HVPG, at least 10 mm Hg).
Portal pressure can be reduced by either ameliorating intrahepatic resistance (which is mostly caused by structural changes that are difficult to reverse) and/or by decreasing portal vein blood inflow (the most modifiable pathogenic mechanism). For over 30 years, treatment of portal hypertension has been based on the use of nonselective beta-blockers (NSBB), drugs that decrease portal pressure through a reduction in splanchnic blood flow. Reduction in portal pressure is greater with NSBB (propranolol, nadolol) than with selective beta-blockers because, as demonstrated experimentally, the main portal pressure–reducing effect stems from splanchnic vasoconstriction because of beta2-adrenergic blockade. This has been confirmed in patients with cirrhosis, in whom the reduction in HVPG is greater with NSBB than with selective BB. On the other hand, carvedilol, an NSBB that also has a vasodilatory alpha1 adrenergic blocking effect, has a greater effect in reducing HVPG, compared with traditional NSBB.
A significant decrease in portal pressure has been associated with better outcomes in cirrhosis. A favorable portal pressure reduction (“response”) has been traditionally defined as a decrease in HVPG below 12 mm Hg or greater than 20% from baseline, although even decreases of 10% are associated with better outcomes. Initial studies had been focused on variceal hemorrhage, a complication that is clearly related to portal hypertension. In this setting, reducing portal pressure clearly leads to a decreased in the incidence of variceal hemorrhage and a decrease in mortality.1 More recently, the focus has been on preventing decompensation (in compensated cirrhosis) and preventing further decompensation/death (in decompensated cirrhosis).
In compensated cirrhosis, a recent meta-analysis of clinical trials of prevention of variceal hemorrhage showed that patients with varices (therefore with clinically significant portal hypertension) without ascites who were NSBB hemodynamic responders, had a reduced risk of developing not only variceal hemorrhage but also ascites and/or encephalopathy, and had lower mortality.2 More importantly, a recent seminal randomized, double-blind, placebo-controlled trial performed in patients with compensated cirrhosis and clinically significant portal hypertension with no or small varices, showed that NSBB (propranolol or carvedilol) led to a significantly lower incidence of decompensation, with ascites being the single event that was significantly lower in the NSBB group.3 This study thereby demonstrates that NSBBs not only reduce the risk of variceal hemorrhage, as previously demonstrated, but also significantly reduces the probability of developing ascites, the most common complication of cirrhosis.
In decompensated cirrhosis, a recent meta-analysis of clinical trials of prevention of variceal hemorrhage showed that patients with varices and ascites (decompensated) who were NSBB responders, had a reduced risk of developing not only variceal hemorrhage but also refractory ascites, spontaneous bacterial peritonitis and/or hepatorenal syndrome, and also had a lower mortality.2 In patients with variceal hemorrhage, the recommended therapy to prevent recurrent variceal hemorrhage is the combination of NSBB plus variceal ligation but this is based on trials that combined compensated and decompensated patients. An individual patient data meta-analysis of these trials showed that, in the group of patients with decompensated Child-Pugh class B/C cirrhosis, rebleeding and mortality were higher with ligation alone, compared with combined therapy with NSBBs and ligation, underlining that NSBB is the key element of combination therapy in these patients.4
There is a fading controversy regarding the potential for increased mortality with the use of NSBBs in patients with refractory ascites and SBP, reported in two retrospective studies.5 These studies lacked information regarding the number of patients in whom NSBBs were withdrawn before the last observation and number of patients in whom NSBBs were started in the course of follow-up. Notably, a recent meta-analysis that included these and subsequent retrospective studies, encompassing a collective of over 1,300 patients, demonstrated that NSBB use in patients with ascites is not related to increased mortality.1,4
Nevertheless, NSBBs should be used cautiously in patients with cirrhosis and ascites. Hemodynamic alterations typical of decompensated cirrhosis are maximal in patients with refractory ascites and spontaneous bacterial peritonitis and the use of NSBB in this setting could lead to worsening hemodynamics, with decreased mean arterial pressure and renal perfusion that could in turn lead to acute kidney injury and death. In studies showing a deleterious effect of NSBB, the mean arterial pressure was significantly lower in patients in the NSBB group.5 In a recent retrospective study, the beneficial effect of NSBBs in patients with refractory ascites, spontaneous bacterial peritonitis, and acute-on-chronic liver failure appeared to apply only to those with a mean arterial pressure of at least 65 mm Hg.6 This evidence has led to guideline recommendations that limit the dose of NSBB to a maximum of 160 mg/day for propranolol or 80 mg/day for nadolol in patients with ascites with close follow-up of arterial blood pressure. Carvedilol should preferably not be used. In the presence of a systolic blood pressure <90 mm Hg or acute kidney injury, NSBBs should be dose-reduced or discontinued. If a precipitant for hypotension is identified (e.g., spontaneous bacterial peritonitis), NSBB can be reinitiated once the precipitating event is resolved and hypotension/acute kidney injury has resolved.
In conclusion, NSBBs are a definite “yes” in the management of cirrhosis and portal hypertension as they prevent poor outcomes (including death) in patients with both compensated and decompensated cirrhosis. In patients with ascites and spontaneous bacterial peritonitis, NSBBs could have deleterious effects but these can be prevented by careful monitoring of blood pressure.
References
1. D’Amico G et al. Gastroenterology. 2006;131:1611-24.
2. Turco L et al. Clin Gastroenterol Hepatol. 2020;18:313-27.
3. Villanueva C et al. Lancet. 2019;393:1597-608.
4. Albillos A et al. Hepatology. 2017;66:1219-31.
5. Garcia-Tsao G. J Hepatol. 2016 Mar;64(3):532-4.
6. Tergast TL et al. Aliment Pharmacol. Ther 2019;50:696-706.
Dr. Garcia-Tsao is professor of medicine, digestive diseases; chief, digestive diseases, Veterans Affairs Connecticut Healthcare System; director, clinical and translational core, Yale Liver Center; program director, VA Connecticut Hepatitis C Resource Center, New Haven. She has no conflicts.
Can be a double-edged blade too dangerous to wield
BY MARWAN S. GHABRIL, MD, AGAF
Nonselective beta-blockers (NSBB) are a cornerstone in the primary and secondary prophylaxis of variceal bleeding in patients with cirrhosis and clinically significant portal hypertension (CSPH), defined as a hepatic venous pressure gradient (HVPG) of at least 10 mm Hg. In the absence of routine HVPG measurement in most clinical practices, NSBB therapy is targeted to a 25% heart rate reduction or target heart rate of 55-60 beats per minute. There is ample evidence supporting this indication for NSBB as summarized in the Baveno VI consensus recommendations in a wide range of liver disease severity, encompassing patients with low-risk small esophageal varices to those with large varices, stigmata, and advanced Child-Pugh class. Tasked with the contrarian perspective on NSBB use, the argument for caution hinges on observations that disease progression can shift the balance of risk and reward to NSBB minimization or avoidance. Understanding the hyperdynamic circulation in worsening portal hypertension of cirrhosis is paramount to these considerations.
The pathophysiology of portal hypertension
Portal hypertension arises as a result of both increased portal venous inflow and increased hepatic sinusoidal resistance and is characterized by splanchnic and systemic vasodilation and reduced effective systemic arterial volume. Compensatory mechanisms include systemic neurohormonal activation, increased heart rate and cardiac output, sodium and water retention (increased plasma volume), and vasoconstrictor system activation. These mechanisms suffice in restoring effective arterial volume initially but also contribute to increased splanchnic/portal inflow and portal hypertension. In advanced decompensation the cardiovascular reserve is overwhelmed with progressive systemic vasodilation, worsening sodium and water retention, vasoconstriction of vital organ vascular beds and an ineffective hyperdynamic state (tachycardia, inadequate cardiac output, and systemic hypotension). This pathophysiological state is heralded clinically by the development of worsening or refractory ascites, and belies the development of other complications of advanced cirrhosis including hyponatremia and hepatorenal syndrome.
The beneficial effects of NSBB in decreasing portal hypertension are mediated by inhibition of splanchnic vasodilation and cardiac effects (reduced heart rate and cardiac output) leading to reduced portal inflow. However, these cardiac effects can be deleterious to systemic hemodynamics in more advanced disease, particularly with acute insults that exacerbate arterial hypovolemia such as bleeding or infection. As such, blunting of sympathetic drive by NSBB carries different degrees of tolerance and risk depending on the hemodynamic reserve in the hyperdynamic state.
Reported clinical experiences
The controversy over NSBB use in advanced cirrhosis arises out of heterogeneous, commonly retrospective datasets and nonrandomized cohorts, with conflicting reports of positive, negative, or neutral effects on mortality and acute kidney injury. Not surprisingly, studies describing detrimental effects of NSBB are based on patients with strictly defined refractory ascites or those with spontaneous bacterial peritonitis.1,2 Importantly, these studies also describe significantly lower blood pressure in at-risk NSBB treated patients, This baseline hemodynamic difference is either not observed,or not explicitly compared in studies/subcohorts with decreased or unaffected mortality with NSBB use in advanced cirrhosis.2
In the largest prospective study of NSBB in cirrhosis with ascites (which used data from three randomized satavaptan trials), NSBB users and nonusers were more closely matched for baseline mean arterial pressure.3 There was no effect of NSBB on mortality but there was a 29% rate of NSBB discontinuation (i.e., intolerance) during the year of follow-up. Predictors of NSBB discontinuation were hospitalization, variceal bleeding, infection, hepatorenal syndrome, Child-Pugh class C, and refractory ascites. Furthermore, NSBB discontinuation was associated with a notable increase in mortality. Similarly, clinically driven discontinuation of NSBB was observed in half of hospitalized patients with acute-on-chronic liver failure in the prospective CANONIC study, and was also associated with significantly higher short-term mortality.
It is possible that NSBB tolerance may select patients with adequate hemodynamic reserve despite the severity of other liver decompensations. Conversely, intolerance of therapeutic NSBB may signify evolving inadequacy of hemodynamic reserve, giving rise to two distinctly different risk/benefit profiles. This double-edged blade perspective is supported by findings of impaired cardiac output in patients with refractory ascites with impaired renal perfusion, and increased wait-list mortality with NSBB use in patients with compromised global cardiac function.4,5
When is caution due?
Rather than a “therapeutic window” that is either wide open or suddenly shut, in nonhospitalized patients risk is on a continuum and there are no agreed upon liver-specific parameters that define strict barriers to NSBB treatment. Refractory ascites may not absolutely define the closure of this window but should put clinicians on notice for a patient’s vulnerability. The Baveno VI recommendations echo the need for caution, with NSBB in refractory ascites with close monitoring of blood pressure, serum sodium, and creatinine. Treatment cessation, reduction or temporary withholding, and careful reintroduction (with reversible insults) are advised in patients with systolic blood pressure <90 mm Hg, serum Na <130 mEq/L, or those with acute kidney injury.
In the absence of randomized trials that account for cirrhotic cardiomyopathy and cardiac reserve, the risks and putative nonvariceal benefits of NSBB (e.g., reducing gut bacterial translocation) are not truly defined in this patient population. We lack HVPG-based or surrogate assessments in routine practice to determine which patients are hemodynamically benefiting from NSBB therapy, or reliable indicators of imminent NSBB intolerance or risk. While the indications for NSBB may expand to prevention of decompensation, serious questions about their safety are being asked in advanced decompensation. Poor tolerance of therapeutic NSBB dosing and unquantified, but likely negative, impact on quality of life raise additional questions. In a shared decision-making partnership, the patient’s perspective on the utility, tolerance, and monitoring of NSBB therapy in preventing variceal bleeding is vital, particularly when there are endoscopic or earlier shunting alternatives. “Primum non nocere” is not a gladiatorial cry, and in the wrong patients NSBB can be a double-edged blade too dangerous to wield.
References
1. Serste T et al. Hepatology. 2010;52:1017-22.
2. Mandorfer M et al. Gastroenterology. 2014;146:1680-90 e1.
3. Bossen L et al. Hepatology. 2016;63:1968-76.
4. Giannelli V et al. J Hepatol. 2020;72:463-71.
5. Tellez L et al. J Hepatol. 2020 May 20. doi: 10.1016/j.jhep.2020.05.011.
Dr. Ghabril is a gastroenterologist with the Indiana University, Indianapolis. He has no conflicts.
Dear colleagues and friends,
Thank you for your continued support of the Perspectives debates. In this edition, Dr. Guadalupe Garcia-Tsao and Dr. Marwan Ghabril discuss the rationale for and against beta-blocker therapy in portal hypertension, and ultimately highlight the nuances required for appropriate decision-making. This topic invariably generates controversy and debate, and is broadly relevant to general GI and hepatology practices. I hope you will find it as informative as I did, and I welcome your comments and suggestions for future topics at [email protected].
Charles J. Kahi, MD, MS, AGAF, professor of medicine, Indiana University, Indianapolis. He is also an associate editor for GI & Hepatology News.
Beta-blockers in portal hypertension – Yes!
BY GUADALUPE GARCIA-TSAO, MD
Portal hypertension is the main consequence of cirrhosis and is responsible for most of its complications. In compensated cirrhosis, a threshold portal pressure gradient, as determined by the hepatic venous pressure gradient (HVPG), of at least 10 mm Hg is the strongest predictor of clinical decompensation (ascites, variceal hemorrhage, or encephalopathy) which is, in turn, the main determinant of death in cirrhosis.
Portal hypertension is initially caused by an increase in intrahepatic resistance that leads to mild portal hypertension (HVPG, 5-10 mm Hg) but is then enhanced and maintained by an increase in portal venous inflow that leads to clinically significant portal hypertension (HVPG, at least 10 mm Hg).
Portal pressure can be reduced by either ameliorating intrahepatic resistance (which is mostly caused by structural changes that are difficult to reverse) and/or by decreasing portal vein blood inflow (the most modifiable pathogenic mechanism). For over 30 years, treatment of portal hypertension has been based on the use of nonselective beta-blockers (NSBB), drugs that decrease portal pressure through a reduction in splanchnic blood flow. Reduction in portal pressure is greater with NSBB (propranolol, nadolol) than with selective beta-blockers because, as demonstrated experimentally, the main portal pressure–reducing effect stems from splanchnic vasoconstriction because of beta2-adrenergic blockade. This has been confirmed in patients with cirrhosis, in whom the reduction in HVPG is greater with NSBB than with selective BB. On the other hand, carvedilol, an NSBB that also has a vasodilatory alpha1 adrenergic blocking effect, has a greater effect in reducing HVPG, compared with traditional NSBB.
A significant decrease in portal pressure has been associated with better outcomes in cirrhosis. A favorable portal pressure reduction (“response”) has been traditionally defined as a decrease in HVPG below 12 mm Hg or greater than 20% from baseline, although even decreases of 10% are associated with better outcomes. Initial studies had been focused on variceal hemorrhage, a complication that is clearly related to portal hypertension. In this setting, reducing portal pressure clearly leads to a decreased in the incidence of variceal hemorrhage and a decrease in mortality.1 More recently, the focus has been on preventing decompensation (in compensated cirrhosis) and preventing further decompensation/death (in decompensated cirrhosis).
In compensated cirrhosis, a recent meta-analysis of clinical trials of prevention of variceal hemorrhage showed that patients with varices (therefore with clinically significant portal hypertension) without ascites who were NSBB hemodynamic responders, had a reduced risk of developing not only variceal hemorrhage but also ascites and/or encephalopathy, and had lower mortality.2 More importantly, a recent seminal randomized, double-blind, placebo-controlled trial performed in patients with compensated cirrhosis and clinically significant portal hypertension with no or small varices, showed that NSBB (propranolol or carvedilol) led to a significantly lower incidence of decompensation, with ascites being the single event that was significantly lower in the NSBB group.3 This study thereby demonstrates that NSBBs not only reduce the risk of variceal hemorrhage, as previously demonstrated, but also significantly reduces the probability of developing ascites, the most common complication of cirrhosis.
In decompensated cirrhosis, a recent meta-analysis of clinical trials of prevention of variceal hemorrhage showed that patients with varices and ascites (decompensated) who were NSBB responders, had a reduced risk of developing not only variceal hemorrhage but also refractory ascites, spontaneous bacterial peritonitis and/or hepatorenal syndrome, and also had a lower mortality.2 In patients with variceal hemorrhage, the recommended therapy to prevent recurrent variceal hemorrhage is the combination of NSBB plus variceal ligation but this is based on trials that combined compensated and decompensated patients. An individual patient data meta-analysis of these trials showed that, in the group of patients with decompensated Child-Pugh class B/C cirrhosis, rebleeding and mortality were higher with ligation alone, compared with combined therapy with NSBBs and ligation, underlining that NSBB is the key element of combination therapy in these patients.4
There is a fading controversy regarding the potential for increased mortality with the use of NSBBs in patients with refractory ascites and SBP, reported in two retrospective studies.5 These studies lacked information regarding the number of patients in whom NSBBs were withdrawn before the last observation and number of patients in whom NSBBs were started in the course of follow-up. Notably, a recent meta-analysis that included these and subsequent retrospective studies, encompassing a collective of over 1,300 patients, demonstrated that NSBB use in patients with ascites is not related to increased mortality.1,4
Nevertheless, NSBBs should be used cautiously in patients with cirrhosis and ascites. Hemodynamic alterations typical of decompensated cirrhosis are maximal in patients with refractory ascites and spontaneous bacterial peritonitis and the use of NSBB in this setting could lead to worsening hemodynamics, with decreased mean arterial pressure and renal perfusion that could in turn lead to acute kidney injury and death. In studies showing a deleterious effect of NSBB, the mean arterial pressure was significantly lower in patients in the NSBB group.5 In a recent retrospective study, the beneficial effect of NSBBs in patients with refractory ascites, spontaneous bacterial peritonitis, and acute-on-chronic liver failure appeared to apply only to those with a mean arterial pressure of at least 65 mm Hg.6 This evidence has led to guideline recommendations that limit the dose of NSBB to a maximum of 160 mg/day for propranolol or 80 mg/day for nadolol in patients with ascites with close follow-up of arterial blood pressure. Carvedilol should preferably not be used. In the presence of a systolic blood pressure <90 mm Hg or acute kidney injury, NSBBs should be dose-reduced or discontinued. If a precipitant for hypotension is identified (e.g., spontaneous bacterial peritonitis), NSBB can be reinitiated once the precipitating event is resolved and hypotension/acute kidney injury has resolved.
In conclusion, NSBBs are a definite “yes” in the management of cirrhosis and portal hypertension as they prevent poor outcomes (including death) in patients with both compensated and decompensated cirrhosis. In patients with ascites and spontaneous bacterial peritonitis, NSBBs could have deleterious effects but these can be prevented by careful monitoring of blood pressure.
References
1. D’Amico G et al. Gastroenterology. 2006;131:1611-24.
2. Turco L et al. Clin Gastroenterol Hepatol. 2020;18:313-27.
3. Villanueva C et al. Lancet. 2019;393:1597-608.
4. Albillos A et al. Hepatology. 2017;66:1219-31.
5. Garcia-Tsao G. J Hepatol. 2016 Mar;64(3):532-4.
6. Tergast TL et al. Aliment Pharmacol. Ther 2019;50:696-706.
Dr. Garcia-Tsao is professor of medicine, digestive diseases; chief, digestive diseases, Veterans Affairs Connecticut Healthcare System; director, clinical and translational core, Yale Liver Center; program director, VA Connecticut Hepatitis C Resource Center, New Haven. She has no conflicts.
Can be a double-edged blade too dangerous to wield
BY MARWAN S. GHABRIL, MD, AGAF
Nonselective beta-blockers (NSBB) are a cornerstone in the primary and secondary prophylaxis of variceal bleeding in patients with cirrhosis and clinically significant portal hypertension (CSPH), defined as a hepatic venous pressure gradient (HVPG) of at least 10 mm Hg. In the absence of routine HVPG measurement in most clinical practices, NSBB therapy is targeted to a 25% heart rate reduction or target heart rate of 55-60 beats per minute. There is ample evidence supporting this indication for NSBB as summarized in the Baveno VI consensus recommendations in a wide range of liver disease severity, encompassing patients with low-risk small esophageal varices to those with large varices, stigmata, and advanced Child-Pugh class. Tasked with the contrarian perspective on NSBB use, the argument for caution hinges on observations that disease progression can shift the balance of risk and reward to NSBB minimization or avoidance. Understanding the hyperdynamic circulation in worsening portal hypertension of cirrhosis is paramount to these considerations.
The pathophysiology of portal hypertension
Portal hypertension arises as a result of both increased portal venous inflow and increased hepatic sinusoidal resistance and is characterized by splanchnic and systemic vasodilation and reduced effective systemic arterial volume. Compensatory mechanisms include systemic neurohormonal activation, increased heart rate and cardiac output, sodium and water retention (increased plasma volume), and vasoconstrictor system activation. These mechanisms suffice in restoring effective arterial volume initially but also contribute to increased splanchnic/portal inflow and portal hypertension. In advanced decompensation the cardiovascular reserve is overwhelmed with progressive systemic vasodilation, worsening sodium and water retention, vasoconstriction of vital organ vascular beds and an ineffective hyperdynamic state (tachycardia, inadequate cardiac output, and systemic hypotension). This pathophysiological state is heralded clinically by the development of worsening or refractory ascites, and belies the development of other complications of advanced cirrhosis including hyponatremia and hepatorenal syndrome.
The beneficial effects of NSBB in decreasing portal hypertension are mediated by inhibition of splanchnic vasodilation and cardiac effects (reduced heart rate and cardiac output) leading to reduced portal inflow. However, these cardiac effects can be deleterious to systemic hemodynamics in more advanced disease, particularly with acute insults that exacerbate arterial hypovolemia such as bleeding or infection. As such, blunting of sympathetic drive by NSBB carries different degrees of tolerance and risk depending on the hemodynamic reserve in the hyperdynamic state.
Reported clinical experiences
The controversy over NSBB use in advanced cirrhosis arises out of heterogeneous, commonly retrospective datasets and nonrandomized cohorts, with conflicting reports of positive, negative, or neutral effects on mortality and acute kidney injury. Not surprisingly, studies describing detrimental effects of NSBB are based on patients with strictly defined refractory ascites or those with spontaneous bacterial peritonitis.1,2 Importantly, these studies also describe significantly lower blood pressure in at-risk NSBB treated patients, This baseline hemodynamic difference is either not observed,or not explicitly compared in studies/subcohorts with decreased or unaffected mortality with NSBB use in advanced cirrhosis.2
In the largest prospective study of NSBB in cirrhosis with ascites (which used data from three randomized satavaptan trials), NSBB users and nonusers were more closely matched for baseline mean arterial pressure.3 There was no effect of NSBB on mortality but there was a 29% rate of NSBB discontinuation (i.e., intolerance) during the year of follow-up. Predictors of NSBB discontinuation were hospitalization, variceal bleeding, infection, hepatorenal syndrome, Child-Pugh class C, and refractory ascites. Furthermore, NSBB discontinuation was associated with a notable increase in mortality. Similarly, clinically driven discontinuation of NSBB was observed in half of hospitalized patients with acute-on-chronic liver failure in the prospective CANONIC study, and was also associated with significantly higher short-term mortality.
It is possible that NSBB tolerance may select patients with adequate hemodynamic reserve despite the severity of other liver decompensations. Conversely, intolerance of therapeutic NSBB may signify evolving inadequacy of hemodynamic reserve, giving rise to two distinctly different risk/benefit profiles. This double-edged blade perspective is supported by findings of impaired cardiac output in patients with refractory ascites with impaired renal perfusion, and increased wait-list mortality with NSBB use in patients with compromised global cardiac function.4,5
When is caution due?
Rather than a “therapeutic window” that is either wide open or suddenly shut, in nonhospitalized patients risk is on a continuum and there are no agreed upon liver-specific parameters that define strict barriers to NSBB treatment. Refractory ascites may not absolutely define the closure of this window but should put clinicians on notice for a patient’s vulnerability. The Baveno VI recommendations echo the need for caution, with NSBB in refractory ascites with close monitoring of blood pressure, serum sodium, and creatinine. Treatment cessation, reduction or temporary withholding, and careful reintroduction (with reversible insults) are advised in patients with systolic blood pressure <90 mm Hg, serum Na <130 mEq/L, or those with acute kidney injury.
In the absence of randomized trials that account for cirrhotic cardiomyopathy and cardiac reserve, the risks and putative nonvariceal benefits of NSBB (e.g., reducing gut bacterial translocation) are not truly defined in this patient population. We lack HVPG-based or surrogate assessments in routine practice to determine which patients are hemodynamically benefiting from NSBB therapy, or reliable indicators of imminent NSBB intolerance or risk. While the indications for NSBB may expand to prevention of decompensation, serious questions about their safety are being asked in advanced decompensation. Poor tolerance of therapeutic NSBB dosing and unquantified, but likely negative, impact on quality of life raise additional questions. In a shared decision-making partnership, the patient’s perspective on the utility, tolerance, and monitoring of NSBB therapy in preventing variceal bleeding is vital, particularly when there are endoscopic or earlier shunting alternatives. “Primum non nocere” is not a gladiatorial cry, and in the wrong patients NSBB can be a double-edged blade too dangerous to wield.
References
1. Serste T et al. Hepatology. 2010;52:1017-22.
2. Mandorfer M et al. Gastroenterology. 2014;146:1680-90 e1.
3. Bossen L et al. Hepatology. 2016;63:1968-76.
4. Giannelli V et al. J Hepatol. 2020;72:463-71.
5. Tellez L et al. J Hepatol. 2020 May 20. doi: 10.1016/j.jhep.2020.05.011.
Dr. Ghabril is a gastroenterologist with the Indiana University, Indianapolis. He has no conflicts.
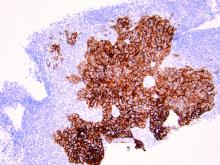
A woman with an asymptomatic eruption on her palms after exposure to water
This eruption can be accompanied by a mild burning or tingling sensation, which will subside with the rest of the symptoms in minutes to hours after drying.1
AWP is most frequently associated with cystic fibrosis (CF).2 It can be observed in up to 80% of CF patients and is considered a clinical sign of the disease. AWP can be present in CF carriers to a lesser extent,2,4 and has also been associated with focal hyperhidrosis, atopic dermatitis, Raynaud phenomenon, and COX-2 inhibitor use.5
While a definitive cause is unknown, it is thought that AWP is caused by dysregulation of sweat glands in the palms through increased expression of aquaporin, a protein crucial in the transport of water between cells.3
AWP is quite rare and benign in nature. However, because of its strong association with CF, genetic screening should be considered in asymptomatic patients. Our patient had been screened in the past and is not a CF carrier. Often, the itching or burning associated with CF is mild and easily controlled. The patient was placed on low dose isotretinoin for treatment of her acne. Interestingly, the patient claimed her eruption no longer appeared after starting isotretinoin therapy. To our knowledge, this is the first reported case of AWP resolving with isotretinoin use.
This case and photo were submitted by Mr. Birk, University of Texas, Austin, Texas; and Dr. Mamelak, Sanova Dermatology, in Austin. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at MDedge.com/Dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Katz M, Ramot Y. CMAJ. 2015 Dec 8;187(18):E515.
2. Tolland JP et al. Dermatology. 2010;221(4):326-30.
3. Kabashima K et al. J Am Acad Dermatol. 2008 Aug;59(2 Suppl 1):S28-32.
4. Gild R et al. Br J Dermatol. 2010 Nov;163(5):1082-4.
5. Glatz M and Muellegger RR. BMJ Case Rep. 2014. doi: 10.1136/bcr-2014-203929.
This eruption can be accompanied by a mild burning or tingling sensation, which will subside with the rest of the symptoms in minutes to hours after drying.1
AWP is most frequently associated with cystic fibrosis (CF).2 It can be observed in up to 80% of CF patients and is considered a clinical sign of the disease. AWP can be present in CF carriers to a lesser extent,2,4 and has also been associated with focal hyperhidrosis, atopic dermatitis, Raynaud phenomenon, and COX-2 inhibitor use.5
While a definitive cause is unknown, it is thought that AWP is caused by dysregulation of sweat glands in the palms through increased expression of aquaporin, a protein crucial in the transport of water between cells.3
AWP is quite rare and benign in nature. However, because of its strong association with CF, genetic screening should be considered in asymptomatic patients. Our patient had been screened in the past and is not a CF carrier. Often, the itching or burning associated with CF is mild and easily controlled. The patient was placed on low dose isotretinoin for treatment of her acne. Interestingly, the patient claimed her eruption no longer appeared after starting isotretinoin therapy. To our knowledge, this is the first reported case of AWP resolving with isotretinoin use.
This case and photo were submitted by Mr. Birk, University of Texas, Austin, Texas; and Dr. Mamelak, Sanova Dermatology, in Austin. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at MDedge.com/Dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Katz M, Ramot Y. CMAJ. 2015 Dec 8;187(18):E515.
2. Tolland JP et al. Dermatology. 2010;221(4):326-30.
3. Kabashima K et al. J Am Acad Dermatol. 2008 Aug;59(2 Suppl 1):S28-32.
4. Gild R et al. Br J Dermatol. 2010 Nov;163(5):1082-4.
5. Glatz M and Muellegger RR. BMJ Case Rep. 2014. doi: 10.1136/bcr-2014-203929.
This eruption can be accompanied by a mild burning or tingling sensation, which will subside with the rest of the symptoms in minutes to hours after drying.1
AWP is most frequently associated with cystic fibrosis (CF).2 It can be observed in up to 80% of CF patients and is considered a clinical sign of the disease. AWP can be present in CF carriers to a lesser extent,2,4 and has also been associated with focal hyperhidrosis, atopic dermatitis, Raynaud phenomenon, and COX-2 inhibitor use.5
While a definitive cause is unknown, it is thought that AWP is caused by dysregulation of sweat glands in the palms through increased expression of aquaporin, a protein crucial in the transport of water between cells.3
AWP is quite rare and benign in nature. However, because of its strong association with CF, genetic screening should be considered in asymptomatic patients. Our patient had been screened in the past and is not a CF carrier. Often, the itching or burning associated with CF is mild and easily controlled. The patient was placed on low dose isotretinoin for treatment of her acne. Interestingly, the patient claimed her eruption no longer appeared after starting isotretinoin therapy. To our knowledge, this is the first reported case of AWP resolving with isotretinoin use.
This case and photo were submitted by Mr. Birk, University of Texas, Austin, Texas; and Dr. Mamelak, Sanova Dermatology, in Austin. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at MDedge.com/Dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Katz M, Ramot Y. CMAJ. 2015 Dec 8;187(18):E515.
2. Tolland JP et al. Dermatology. 2010;221(4):326-30.
3. Kabashima K et al. J Am Acad Dermatol. 2008 Aug;59(2 Suppl 1):S28-32.
4. Gild R et al. Br J Dermatol. 2010 Nov;163(5):1082-4.
5. Glatz M and Muellegger RR. BMJ Case Rep. 2014. doi: 10.1136/bcr-2014-203929.
Five reasons why medical meetings will never be the same
In the wake of the COVID-19 pandemic, the virtual medical meeting is now the norm. And while it’s admirable that key data are being disseminated (often for free), there is no escaping the fact that it is a fundamentally different and lesser experience.
Watching from home, most of us split our attention between live streams of the meeting and work and family obligations. There is far less urgency when early live presentations are recorded and can be viewed later.
In terms of discussing the data, Twitter may offer broader participation than a live meeting, yet only a small number of attendees actively engage online.
And the exhibit halls for these online meetings? With neither free coffee nor company-branded tchotchkes, I expect that they have virtual tumbleweeds blowing through and crickets chirping.
Even still, the virtual meeting experience, while inferior to the live one, is a tremendous advance. It should never be banished as a historical footnote but rather should remain an option. It’s analogous to watching the Super Bowl at home: Obviously, it’s not the same as being there, but it’s a terrific alternative. Like telemedicine, this pandemic has provided a critical proof of concept that there is a better model.
Reshaping the medical meeting
Let’s consider five reasons why medical meetings should be permanently reshaped by this pandemic.
This pandemic isn’t going away in 2020. While nearly every country has done a far better job than the United States of containing COVID-19 thus far, outbreaks remain a problem wherever crowds assemble. You’d be hard-pressed to devise a setting more conducive to mass spread than a conference of 20,000 attendees from all over the world sitting alongside each other cheek to jowl for 5 days. Worse yet is the thought of them returning home and infecting their patients, families, and friends. What medical society wants to be remembered for creating a COVID-19 superspreader event? Professional medical societies will need to offer this option as the safest alternative moving forward.
Virtual learning still conveys the most important content. Despite the many social benefits of a live meeting, its core purpose is to disseminate new research and current and emerging treatment options. Virtual meetings have proven that this format can effectively deliver the content, and not as a secondary offering but as the sole platform in real time.
Virtual learning levels the playing field. Traveling to attend conferences typically costs thousands of dollars, accounting for the registration fees, inflated hotel rates, ground transportation, and meals out for days on end. Most meetings also demand several days away from our work and families, forcing many of us to work extra in the days before we leave and upon our return. Parents and those with commitments at home also face special challenges. For international participants, the financial and time costs are even greater. A virtual meeting helps overcome these hurdles and erases barriers that have long precluded many from attending a conference.
Virtual learning is efficient and comfortable. Virtual meetings over the past 6 months have given us a glimpse of an astonishingly more efficient form. If the content seems of a lower magnitude without the fanfare of a live conference, it is in part because so much of a live meeting is spent walking a mile between session rooms, waiting in concession or taxi lines, sitting in traffic between venues, or simply waiting for a session to begin. All of that has been replaced with time that you can use productively in between video sessions viewed either live or on demand. And with a virtual meeting, you can comfortably watch the sessions. There’s no need to stand along the back wall of an overcrowded room or step over 10 people to squeeze into an open middle seat. You can be focused, rather than having an end-of-day presentation wash over you as your eyes cross because you’ve been running around for the past 12 hours.
Virtual learning and social media will only improve. While virtual meetings unquestionably have limitations, it’s important to acknowledge that the successes thus far still represent only the earliest forays into this endeavor. In-person meetings evolved to their present form over centuries. In contrast, virtual meetings are being cobbled together within a few weeks or months. They can only be expected to improve as presenters adapt their skills to the online audience and new tools improve virtual discussions.
I am not implying that live meetings will or should be replaced by virtual ones. We still need that experience of trainees and experts presenting to a live audience and discussing the results together, all while sharing the energy of the moment. But there should be room for both a live conference and a virtual version.
Practically speaking, it is unclear whether professional societies could forgo the revenue they receive from registration fees, meeting sponsorships, and corporate exhibits. Yet, there are certainly ways to obtain sponsorship revenue for a virtual program. Even if the virtual version of a conference costs far less than attending in person, there is plenty of room between that number and free. It costs remarkably little for a professional society to share its content, and virtual offerings further the mission of distributing this content broadly.
We should not rush to return to the previous status quo. Despite their limitations, virtual meetings have brought a new, higher standard of access and efficiency for sharing important new data and treatment options in medicine.
H. Jack West, MD, associate clinical professor and executive director of employer services at City of Hope Comprehensive Cancer Center in Duarte, Calif., regularly comments on lung cancer for Medscape. West serves as web editor for JAMA Oncology, edits and writes several sections on lung cancer for UpToDate, and leads a wide range of continuing education programs and other educational programs, including hosting the audio podcast West Wind.
This article first appeared on Medscape.com.
In the wake of the COVID-19 pandemic, the virtual medical meeting is now the norm. And while it’s admirable that key data are being disseminated (often for free), there is no escaping the fact that it is a fundamentally different and lesser experience.
Watching from home, most of us split our attention between live streams of the meeting and work and family obligations. There is far less urgency when early live presentations are recorded and can be viewed later.
In terms of discussing the data, Twitter may offer broader participation than a live meeting, yet only a small number of attendees actively engage online.
And the exhibit halls for these online meetings? With neither free coffee nor company-branded tchotchkes, I expect that they have virtual tumbleweeds blowing through and crickets chirping.
Even still, the virtual meeting experience, while inferior to the live one, is a tremendous advance. It should never be banished as a historical footnote but rather should remain an option. It’s analogous to watching the Super Bowl at home: Obviously, it’s not the same as being there, but it’s a terrific alternative. Like telemedicine, this pandemic has provided a critical proof of concept that there is a better model.
Reshaping the medical meeting
Let’s consider five reasons why medical meetings should be permanently reshaped by this pandemic.
This pandemic isn’t going away in 2020. While nearly every country has done a far better job than the United States of containing COVID-19 thus far, outbreaks remain a problem wherever crowds assemble. You’d be hard-pressed to devise a setting more conducive to mass spread than a conference of 20,000 attendees from all over the world sitting alongside each other cheek to jowl for 5 days. Worse yet is the thought of them returning home and infecting their patients, families, and friends. What medical society wants to be remembered for creating a COVID-19 superspreader event? Professional medical societies will need to offer this option as the safest alternative moving forward.
Virtual learning still conveys the most important content. Despite the many social benefits of a live meeting, its core purpose is to disseminate new research and current and emerging treatment options. Virtual meetings have proven that this format can effectively deliver the content, and not as a secondary offering but as the sole platform in real time.
Virtual learning levels the playing field. Traveling to attend conferences typically costs thousands of dollars, accounting for the registration fees, inflated hotel rates, ground transportation, and meals out for days on end. Most meetings also demand several days away from our work and families, forcing many of us to work extra in the days before we leave and upon our return. Parents and those with commitments at home also face special challenges. For international participants, the financial and time costs are even greater. A virtual meeting helps overcome these hurdles and erases barriers that have long precluded many from attending a conference.
Virtual learning is efficient and comfortable. Virtual meetings over the past 6 months have given us a glimpse of an astonishingly more efficient form. If the content seems of a lower magnitude without the fanfare of a live conference, it is in part because so much of a live meeting is spent walking a mile between session rooms, waiting in concession or taxi lines, sitting in traffic between venues, or simply waiting for a session to begin. All of that has been replaced with time that you can use productively in between video sessions viewed either live or on demand. And with a virtual meeting, you can comfortably watch the sessions. There’s no need to stand along the back wall of an overcrowded room or step over 10 people to squeeze into an open middle seat. You can be focused, rather than having an end-of-day presentation wash over you as your eyes cross because you’ve been running around for the past 12 hours.
Virtual learning and social media will only improve. While virtual meetings unquestionably have limitations, it’s important to acknowledge that the successes thus far still represent only the earliest forays into this endeavor. In-person meetings evolved to their present form over centuries. In contrast, virtual meetings are being cobbled together within a few weeks or months. They can only be expected to improve as presenters adapt their skills to the online audience and new tools improve virtual discussions.
I am not implying that live meetings will or should be replaced by virtual ones. We still need that experience of trainees and experts presenting to a live audience and discussing the results together, all while sharing the energy of the moment. But there should be room for both a live conference and a virtual version.
Practically speaking, it is unclear whether professional societies could forgo the revenue they receive from registration fees, meeting sponsorships, and corporate exhibits. Yet, there are certainly ways to obtain sponsorship revenue for a virtual program. Even if the virtual version of a conference costs far less than attending in person, there is plenty of room between that number and free. It costs remarkably little for a professional society to share its content, and virtual offerings further the mission of distributing this content broadly.
We should not rush to return to the previous status quo. Despite their limitations, virtual meetings have brought a new, higher standard of access and efficiency for sharing important new data and treatment options in medicine.
H. Jack West, MD, associate clinical professor and executive director of employer services at City of Hope Comprehensive Cancer Center in Duarte, Calif., regularly comments on lung cancer for Medscape. West serves as web editor for JAMA Oncology, edits and writes several sections on lung cancer for UpToDate, and leads a wide range of continuing education programs and other educational programs, including hosting the audio podcast West Wind.
This article first appeared on Medscape.com.
In the wake of the COVID-19 pandemic, the virtual medical meeting is now the norm. And while it’s admirable that key data are being disseminated (often for free), there is no escaping the fact that it is a fundamentally different and lesser experience.
Watching from home, most of us split our attention between live streams of the meeting and work and family obligations. There is far less urgency when early live presentations are recorded and can be viewed later.
In terms of discussing the data, Twitter may offer broader participation than a live meeting, yet only a small number of attendees actively engage online.
And the exhibit halls for these online meetings? With neither free coffee nor company-branded tchotchkes, I expect that they have virtual tumbleweeds blowing through and crickets chirping.
Even still, the virtual meeting experience, while inferior to the live one, is a tremendous advance. It should never be banished as a historical footnote but rather should remain an option. It’s analogous to watching the Super Bowl at home: Obviously, it’s not the same as being there, but it’s a terrific alternative. Like telemedicine, this pandemic has provided a critical proof of concept that there is a better model.
Reshaping the medical meeting
Let’s consider five reasons why medical meetings should be permanently reshaped by this pandemic.
This pandemic isn’t going away in 2020. While nearly every country has done a far better job than the United States of containing COVID-19 thus far, outbreaks remain a problem wherever crowds assemble. You’d be hard-pressed to devise a setting more conducive to mass spread than a conference of 20,000 attendees from all over the world sitting alongside each other cheek to jowl for 5 days. Worse yet is the thought of them returning home and infecting their patients, families, and friends. What medical society wants to be remembered for creating a COVID-19 superspreader event? Professional medical societies will need to offer this option as the safest alternative moving forward.
Virtual learning still conveys the most important content. Despite the many social benefits of a live meeting, its core purpose is to disseminate new research and current and emerging treatment options. Virtual meetings have proven that this format can effectively deliver the content, and not as a secondary offering but as the sole platform in real time.
Virtual learning levels the playing field. Traveling to attend conferences typically costs thousands of dollars, accounting for the registration fees, inflated hotel rates, ground transportation, and meals out for days on end. Most meetings also demand several days away from our work and families, forcing many of us to work extra in the days before we leave and upon our return. Parents and those with commitments at home also face special challenges. For international participants, the financial and time costs are even greater. A virtual meeting helps overcome these hurdles and erases barriers that have long precluded many from attending a conference.
Virtual learning is efficient and comfortable. Virtual meetings over the past 6 months have given us a glimpse of an astonishingly more efficient form. If the content seems of a lower magnitude without the fanfare of a live conference, it is in part because so much of a live meeting is spent walking a mile between session rooms, waiting in concession or taxi lines, sitting in traffic between venues, or simply waiting for a session to begin. All of that has been replaced with time that you can use productively in between video sessions viewed either live or on demand. And with a virtual meeting, you can comfortably watch the sessions. There’s no need to stand along the back wall of an overcrowded room or step over 10 people to squeeze into an open middle seat. You can be focused, rather than having an end-of-day presentation wash over you as your eyes cross because you’ve been running around for the past 12 hours.
Virtual learning and social media will only improve. While virtual meetings unquestionably have limitations, it’s important to acknowledge that the successes thus far still represent only the earliest forays into this endeavor. In-person meetings evolved to their present form over centuries. In contrast, virtual meetings are being cobbled together within a few weeks or months. They can only be expected to improve as presenters adapt their skills to the online audience and new tools improve virtual discussions.
I am not implying that live meetings will or should be replaced by virtual ones. We still need that experience of trainees and experts presenting to a live audience and discussing the results together, all while sharing the energy of the moment. But there should be room for both a live conference and a virtual version.
Practically speaking, it is unclear whether professional societies could forgo the revenue they receive from registration fees, meeting sponsorships, and corporate exhibits. Yet, there are certainly ways to obtain sponsorship revenue for a virtual program. Even if the virtual version of a conference costs far less than attending in person, there is plenty of room between that number and free. It costs remarkably little for a professional society to share its content, and virtual offerings further the mission of distributing this content broadly.
We should not rush to return to the previous status quo. Despite their limitations, virtual meetings have brought a new, higher standard of access and efficiency for sharing important new data and treatment options in medicine.
H. Jack West, MD, associate clinical professor and executive director of employer services at City of Hope Comprehensive Cancer Center in Duarte, Calif., regularly comments on lung cancer for Medscape. West serves as web editor for JAMA Oncology, edits and writes several sections on lung cancer for UpToDate, and leads a wide range of continuing education programs and other educational programs, including hosting the audio podcast West Wind.
This article first appeared on Medscape.com.
Chronicles of Cancer: A history of mammography, part 2
The push and pull of social forces
Science and technology emerge from and are shaped by social forces outside the laboratory and clinic. This is an essential fact of most new medical technology. In the Chronicles of Cancer series, part 1 of the story of mammography focused on the technological determinants of its development and use. Part 2 will focus on some of the social forces that shaped the development of mammography.
“Few medical issues have been as controversial – or as political, at least in the United States – as the role of mammographic screening for breast cancer,” according to Donald A. Berry, PhD, a biostatistician at the University of Texas MD Anderson Cancer Center, Houston.1
In fact, technology aside, the history of mammography has been and remains rife with controversy on the one side and vigorous promotion on the other, all enmeshed within the War on Cancer, corporate and professional interests, and the women’s rights movement’s growing issues with what was seen as a patriarchal medical establishment.
Today the issue of conflicts of interest are paramount in any discussion of new medical developments, from the early preclinical stages to ultimate deployment. Then, as now, professional and advocacy societies had a profound influence on government and social decision-making, but in that earlier, more trusting era, buoyed by the amazing changes that technology was bringing to everyday life and an unshakable commitment to and belief in “progress,” science and the medical community held a far more effective sway over the beliefs and behavior of the general population.
Women’s health observed
Although the main focus of the women’s movement with regard to breast cancer was a struggle against the common practice of routine radical mastectomies and a push toward breast-conserving surgeries, the issue of preventive care and screening with regard to women’s health was also a major concern.
Regarding mammography, early enthusiasm in the medical community and among the general public was profound. In 1969, Robert Egan described how mammography had a “certain magic appeal.” The patient, he continued, “feels something special is being done for her.” Women whose cancers had been discovered on a mammogram praised radiologists as heroes who had saved their lives.2
In that era, however, beyond the confines of the doctor’s office, mammography and breast cancer remained topics not discussed among the public at large, despite efforts by the American Cancer Society to change this.
ACS weighs in
Various groups had been promoting the benefits of breast self-examination since the 1930s, and in 1947, the American Cancer Society launched an awareness campaign, “Look for a Lump or Thickening in the Breast,” instructing women to perform a monthly breast self-exam. Between self-examination and clinical breast examinations in physicians’ offices, the ACS believed that smaller and more treatable breast cancers could be discovered.
In 1972, the ACS, working with the National Cancer Institute (NCI), inaugurated the Breast Cancer Detection Demonstration Project (BCDDP), which planned to screen over a quarter of a million American women for breast cancer. The initiative was a direct outgrowth of the National Cancer Act of 1971,3 the key legislation of the War on Cancer, promoted by President Richard Nixon in his State of the Union address in 1971 and responsible for the creation of the National Cancer Institute.
Arthur I. Holleb, MD, ACS senior vice president for medical affairs and research, announced that, “[T]he time has come for the American Cancer Society to mount a massive program on mammography just as we did with the Pap test,”2 according to Barron Lerner, MD, whose book “The Breast Cancer Wars” provides a history of the long-term controversies involved.4
The Pap test, widely promulgated in the 1950s and 1960s, had produced a decline in mortality from cervical cancer.
Regardless of the lack of data on effectiveness at earlier ages, the ACS chose to include women as young as 35 in the BCDDP in order “to inculcate them with ‘good health habits’ ” and “to make our screenee want to return periodically and to want to act as a missionary to bring other women into the screening process.”2
Celebrity status matters
All of the elements of a social revolution in the use of mammography were in place in the late 1960s, but the final triggers to raise social consciousness were the cases of several high-profile female celebrities. In 1973, beloved former child star Shirley Temple Black revealed her breast cancer diagnosis and mastectomy in an era when public discussion of cancer – especially breast cancer – was rare.4
But it wasn’t until 1974 that public awareness and media coverage exploded, sparked by the impact of First Lady Betty Ford’s outspokenness on her own experience of breast cancer. “In obituaries prior to the 1950s and 1960s, women who died from breast cancer were often listed as dying from ‘a prolonged disease’ or ‘a woman’s disease,’ ” according to Tasha Dubriwny, PhD, now an associate professor of communication and women’s and gender studies at Texas A&M University, College Station, when interviewed by the American Association for Cancer Research.5Betty Ford openly addressed her breast cancer diagnosis and treatment and became a prominent advocate for early screening, transforming the landscape of breast cancer awareness. And although Betty Ford’s diagnosis was based on clinical examination rather than mammography, its boost to overall screening was indisputable.
“Within weeks [after Betty Ford’s announcement] thousands of women who had been reluctant to examine their breasts inundated cancer screening centers,” according to a 1987 article in the New York Times.6 Among these women was Happy Rockefeller, the wife of Vice President Nelson A. Rockefeller. Happy Rockefeller also found that she had breast cancer upon screening, and with Betty Ford would become another icon thereafter for breast cancer screening.
“Ford’s lesson for other women was straightforward: Get a mammogram, which she had not done. The American Cancer Society and National Cancer Institute had recently mounted a demonstration project to promote the detection of breast cancer as early as possible, when it was presumed to be more curable. The degree to which women embraced Ford’s message became clear through the famous ‘Betty Ford blip.’ So many women got breast examinations and mammograms for the first time after Ford’s announcement that the actual incidence of breast cancer in the United States went up by 15 percent.”4
In a 1975 address to the American Cancer Society, Betty Ford said: “One day I appeared to be fine and the next day I was in the hospital for a mastectomy. It made me realize how many women in the country could be in the same situation. That realization made me decide to discuss my breast cancer operation openly, because I thought of all the lives in jeopardy. My experience and frank discussion of breast cancer did prompt many women to learn about self-examination, regular checkups, and such detection techniques as mammography. These are so important. I just cannot stress enough how necessary it is for women to take an active interest in their own health and body.”7
ACS guidelines evolve
It wasn’t until 1976 that the ACS issued its first major guidelines for mammography screening. The ACS suggested mammograms may be called for in women aged 35-39 if there was a personal history of breast cancer, and between ages 40 and 49 if their mother or sisters had a history of breast cancer. Women aged 50 years and older could have yearly screening. Thereafter, the use of mammography was encouraged more and more with each new set of recommendations.8
Between 1980 and 1982, these guidelines expanded to advising a baseline mammogram for women aged 35-39 years; that women consult with their physician between ages 40 and 49; and that women over 50 have a yearly mammogram.
Between 1983 and 1991, the recommendations were for a baseline mammogram for women aged 35-39 years; a mammogram every 1-2 years for women aged 40-49; and yearly mammograms for women aged 50 and up. The baseline mammogram recommendation was dropped in 1992.
Between 1997 and 2015, the stakes were upped, and women aged 40-49 years were now recommended to have yearly mammograms, as were still all women aged 50 years and older.
In October 2015, the ACS changed their recommendation to say that women aged 40-44 years should have the choice of initiating mammogram screening, and that the risks and benefits of doing so should be discussed with their physicians. Women aged 45 years and older were still recommended for yearly mammogram screening. That recommendation stands today.
Controversies arise over risk/benefit
The technology was not, however, universally embraced. “By the late 1970s, mammography had diffused much more widely but had become a source of tremendous controversy. On the one hand, advocates of the technology enthusiastically touted its ability to detect smaller, more curable cancers. On the other hand, critics asked whether breast x-rays, particularly for women aged 50 and younger, actually caused more harm than benefit.”2
In addition, meta-analyses of the nine major screening trials conducted between 1965 and 1991 indicated that the reduced breast cancer mortality with screening was dependent on age. In particular, the results for women aged 40-49 years and 50-59 years showed only borderline statistical significance, and they varied depending on how cases were accrued in individual trials.
“Assuming that differences actually exist, the absolute breast cancer mortality reduction per 10,000 women screened for 10 years ranged from 3 for age 39-49 years; 5-8 for age 50-59 years; and 12-21 for age 60=69 years,” according to a review by the U.S. Preventive Services Task Force.9
The estimates for the group aged 70-74 years were limited by low numbers of events in trials that had smaller numbers of women in this age group.
Age has continued to be a major factor in determining the cost/benefit of routine mammography screening, with the American College of Physicians stating in its 2019 guidelines, “The potential harms outweigh the benefits in most women aged 40 to 49 years,” and adding, “In average-risk women aged 75 years or older or in women with a life expectancy of 10 years or less, clinicians should discontinue screening for breast cancer.”10
A Cochrane Report from 2013 was equally critical: “If we assume that screening reduces breast cancer mortality by 15% after 13 years of follow-up and that overdiagnosis and overtreatment is at 30%, it means that for every 2,000 women invited for screening throughout 10 years, one will avoid dying of breast cancer and 10 healthy women, who would not have been diagnosed if there had not been screening, will be treated unnecessarily. Furthermore, more than 200 women will experience important psychological distress including anxiety and uncertainty for years because of false positive findings.”11
Conflicting voices exist
These reports advising a more nuanced evaluation of the benefits of mammography, however, were received with skepticism from doctors committed to the vision of breast cancer screening and convinced by anecdotal evidence in their own practices.
These reports were also in direct contradiction to recommendations made in 1997 by the National Cancer Institute, which recommended screening mammograms every 3 years for women aged 40-49 years at average risk of breast cancer.
Such scientific vacillation has contributed to a love/hate relationship with mammography in the mainstream media, fueling new controversies with regard to breast cancer screening, sometimes as much driven by public suspicion and political advocacy as by scientific evolution.
Vocal opponents of universal mammography screening arose throughout the years, and even the cases of Betty Ford and Happy Rockefeller have been called into question as iconic demonstrations of the effectiveness of screening. And although not directly linked to the issue of screening, the rebellion against the routine use of radical mastectomies, a technique pioneered by Halsted in 1894 and in continuing use into the modern era, sparked outrage in women’s rights activists who saw it as evidence of a patriarchal medical establishment making arbitrary decisions concerning women’s bodies. For example, feminist and breast cancer activist Rose Kushner argued against the unnecessary disfigurement of women’s bodies and urged the use and development of less drastic techniques, including partial mastectomies and lumpectomies as viable choices. And these choices were increasingly supported by the medical community as safe and effective alternatives for many patients.12
A 2015 paper in the Journal of the Royal Society of Medicine was bluntly titled “Mammography screening is harmful and should be abandoned.”13 According to the author, who was the editor of the 2013 Cochrane Report, “I believe that if screening had been a drug, it would have been withdrawn from the market long ago.” And the popular press has not been shy at weighing in on the controversy, driven, in part, by the lack of consensus and continually changing guidelines, with major publications such as U.S. News and World Report, the Washington Post, and others addressing the issue over the years. And even public advocacy groups such as the Susan G. Komen organization14 are supporting the more modern professional guidelines in taking a more nuanced approach to the discussion of risks and benefits for individual women.
In 2014, the Swiss Medical Board, a nationally appointed body, recommended that new mammography screening programs should not be instituted in that country and that limits be placed on current programs because of the imbalance between risks and benefits of mammography screening.15 And a study done in Australia in 2020 agreed, stating, “Using data of 30% overdiagnosis of women aged 50 to 69 years in the NSW [New South Wales] BreastScreen program in 2012, we calculated an Australian ratio of harm of overdiagnosis to benefit (breast cancer deaths avoided) of 15:1 and recommended stopping the invitation to screening.”16
Conclusion
If nothing else, the history of mammography shows that the interconnection of social factors with the rise of a medical technology can have profound impacts on patient care. Technology developed by men for women became a touchstone of resentment in a world ever more aware of sex and gender biases in everything from the conduct of clinical trials to the care (or lack thereof) of women with heart disease. Tied for so many years to a radically disfiguring and drastic form of surgery that affected what many felt to be a hallmark and representation of womanhood1,17 mammography also carried the weight of both the real and imaginary fears of radiation exposure.
Well into its development, the technology still found itself under intense public scrutiny, and was enmeshed in a continual media circus, with ping-ponging discussions of risk/benefit in the scientific literature fueling complaints by many of the dominance of a patriarchal medical community over women’s bodies.
With guidelines for mammography still evolving, questions still remaining, and new technologies such as digital imaging falling short in their hoped-for promise, the story remains unfinished, and the future still uncertain. One thing remains clear, however: In the right circumstances, with the right patient population, and properly executed, mammography has saved lives when tied to effective, early treatment, whatever its flaws and failings. This truth goes hand in hand with another reality: It may have also contributed to considerable unanticipated harm through overdiagnosis and overtreatment.
Overall, the history of mammography is a cautionary tale for the entire medical community and for the development of new medical technologies. The push-pull of the demand for progress to save lives and the slowness and often inconclusiveness of scientific studies that validate new technologies create gray areas, where social determinants and professional interests vie in an information vacuum for control of the narrative of risks vs. benefits.
The story of mammography is not yet concluded, and may never be, especially given the unlikelihood of conducting the massive randomized clinical trials that would be needed to settle the issue. It is more likely to remain controversial, at least until the technology of mammography becomes obsolete, replaced by something new and different, which will likely start the push-pull cycle all over again.
And regardless of the risks and benefits of mammography screening, the issue of treatment once breast cancer is identified is perhaps one of more overwhelming import.
References
1. Berry, DA. The Breast. 2013;22[Supplement 2]:S73-S76.
2. Lerner, BH. “To See Today With the Eyes of Tomorrow: A History of Screening Mammography.” Background paper for the Institute of Medicine report Mammography and Beyond: Developing Technologies for the Early Detection of Breast Cancer. 2001.
3. NCI website. The National Cancer Act of 1971. www.cancer.gov/about-nci/overview/history/national-cancer-act-1971.
4. Lerner BH. The Huffington Post, Sep. 26, 2014.
5. Wu C. Cancer Today. 2012;2(3): Sep. 27.
6. “”The New York Times. Oct. 17, 1987.
7. Ford B. Remarks to the American Cancer Society. 1975.
8. The American Cancer Society website. History of ACS Recommendations for the Early Detection of Cancer in People Without Symptoms.
9. Nelson HD et al. Screening for Breast Cancer: A Systematic Review to Update the 2009 U.S. Preventive Services Task Force Recommendation. 2016; Evidence Syntheses, No. 124; pp.29-49.
10. Qasseem A et al. Annals of Internal Medicine. 2019;170(8):547-60.
11. Gotzsche PC et al. Cochrane Report 2013.
12. Lerner, BH. West J Med. May 2001;174(5):362-5.
13. Gotzsche PC. J R Soc Med. 2015;108(9): 341-5.
14. Susan G. Komen website. Weighing the Benefits and Risks of Mammography.
15. Biller-Andorno N et al. N Engl J Med 2014;370:1965-7.
16. Burton R et al. JAMA Netw Open. 2020;3(6):e208249.
17. Webb C et al. Plast Surg. 2019;27(1):49-53.
Mark Lesney is the editor of Hematology News and the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has worked as a writer/editor for the American Chemical Society, and has served as an adjunct assistant professor in the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
The push and pull of social forces
The push and pull of social forces
Science and technology emerge from and are shaped by social forces outside the laboratory and clinic. This is an essential fact of most new medical technology. In the Chronicles of Cancer series, part 1 of the story of mammography focused on the technological determinants of its development and use. Part 2 will focus on some of the social forces that shaped the development of mammography.
“Few medical issues have been as controversial – or as political, at least in the United States – as the role of mammographic screening for breast cancer,” according to Donald A. Berry, PhD, a biostatistician at the University of Texas MD Anderson Cancer Center, Houston.1
In fact, technology aside, the history of mammography has been and remains rife with controversy on the one side and vigorous promotion on the other, all enmeshed within the War on Cancer, corporate and professional interests, and the women’s rights movement’s growing issues with what was seen as a patriarchal medical establishment.
Today the issue of conflicts of interest are paramount in any discussion of new medical developments, from the early preclinical stages to ultimate deployment. Then, as now, professional and advocacy societies had a profound influence on government and social decision-making, but in that earlier, more trusting era, buoyed by the amazing changes that technology was bringing to everyday life and an unshakable commitment to and belief in “progress,” science and the medical community held a far more effective sway over the beliefs and behavior of the general population.
Women’s health observed
Although the main focus of the women’s movement with regard to breast cancer was a struggle against the common practice of routine radical mastectomies and a push toward breast-conserving surgeries, the issue of preventive care and screening with regard to women’s health was also a major concern.
Regarding mammography, early enthusiasm in the medical community and among the general public was profound. In 1969, Robert Egan described how mammography had a “certain magic appeal.” The patient, he continued, “feels something special is being done for her.” Women whose cancers had been discovered on a mammogram praised radiologists as heroes who had saved their lives.2
In that era, however, beyond the confines of the doctor’s office, mammography and breast cancer remained topics not discussed among the public at large, despite efforts by the American Cancer Society to change this.
ACS weighs in
Various groups had been promoting the benefits of breast self-examination since the 1930s, and in 1947, the American Cancer Society launched an awareness campaign, “Look for a Lump or Thickening in the Breast,” instructing women to perform a monthly breast self-exam. Between self-examination and clinical breast examinations in physicians’ offices, the ACS believed that smaller and more treatable breast cancers could be discovered.
In 1972, the ACS, working with the National Cancer Institute (NCI), inaugurated the Breast Cancer Detection Demonstration Project (BCDDP), which planned to screen over a quarter of a million American women for breast cancer. The initiative was a direct outgrowth of the National Cancer Act of 1971,3 the key legislation of the War on Cancer, promoted by President Richard Nixon in his State of the Union address in 1971 and responsible for the creation of the National Cancer Institute.
Arthur I. Holleb, MD, ACS senior vice president for medical affairs and research, announced that, “[T]he time has come for the American Cancer Society to mount a massive program on mammography just as we did with the Pap test,”2 according to Barron Lerner, MD, whose book “The Breast Cancer Wars” provides a history of the long-term controversies involved.4
The Pap test, widely promulgated in the 1950s and 1960s, had produced a decline in mortality from cervical cancer.
Regardless of the lack of data on effectiveness at earlier ages, the ACS chose to include women as young as 35 in the BCDDP in order “to inculcate them with ‘good health habits’ ” and “to make our screenee want to return periodically and to want to act as a missionary to bring other women into the screening process.”2
Celebrity status matters
All of the elements of a social revolution in the use of mammography were in place in the late 1960s, but the final triggers to raise social consciousness were the cases of several high-profile female celebrities. In 1973, beloved former child star Shirley Temple Black revealed her breast cancer diagnosis and mastectomy in an era when public discussion of cancer – especially breast cancer – was rare.4
But it wasn’t until 1974 that public awareness and media coverage exploded, sparked by the impact of First Lady Betty Ford’s outspokenness on her own experience of breast cancer. “In obituaries prior to the 1950s and 1960s, women who died from breast cancer were often listed as dying from ‘a prolonged disease’ or ‘a woman’s disease,’ ” according to Tasha Dubriwny, PhD, now an associate professor of communication and women’s and gender studies at Texas A&M University, College Station, when interviewed by the American Association for Cancer Research.5Betty Ford openly addressed her breast cancer diagnosis and treatment and became a prominent advocate for early screening, transforming the landscape of breast cancer awareness. And although Betty Ford’s diagnosis was based on clinical examination rather than mammography, its boost to overall screening was indisputable.
“Within weeks [after Betty Ford’s announcement] thousands of women who had been reluctant to examine their breasts inundated cancer screening centers,” according to a 1987 article in the New York Times.6 Among these women was Happy Rockefeller, the wife of Vice President Nelson A. Rockefeller. Happy Rockefeller also found that she had breast cancer upon screening, and with Betty Ford would become another icon thereafter for breast cancer screening.
“Ford’s lesson for other women was straightforward: Get a mammogram, which she had not done. The American Cancer Society and National Cancer Institute had recently mounted a demonstration project to promote the detection of breast cancer as early as possible, when it was presumed to be more curable. The degree to which women embraced Ford’s message became clear through the famous ‘Betty Ford blip.’ So many women got breast examinations and mammograms for the first time after Ford’s announcement that the actual incidence of breast cancer in the United States went up by 15 percent.”4
In a 1975 address to the American Cancer Society, Betty Ford said: “One day I appeared to be fine and the next day I was in the hospital for a mastectomy. It made me realize how many women in the country could be in the same situation. That realization made me decide to discuss my breast cancer operation openly, because I thought of all the lives in jeopardy. My experience and frank discussion of breast cancer did prompt many women to learn about self-examination, regular checkups, and such detection techniques as mammography. These are so important. I just cannot stress enough how necessary it is for women to take an active interest in their own health and body.”7
ACS guidelines evolve
It wasn’t until 1976 that the ACS issued its first major guidelines for mammography screening. The ACS suggested mammograms may be called for in women aged 35-39 if there was a personal history of breast cancer, and between ages 40 and 49 if their mother or sisters had a history of breast cancer. Women aged 50 years and older could have yearly screening. Thereafter, the use of mammography was encouraged more and more with each new set of recommendations.8
Between 1980 and 1982, these guidelines expanded to advising a baseline mammogram for women aged 35-39 years; that women consult with their physician between ages 40 and 49; and that women over 50 have a yearly mammogram.
Between 1983 and 1991, the recommendations were for a baseline mammogram for women aged 35-39 years; a mammogram every 1-2 years for women aged 40-49; and yearly mammograms for women aged 50 and up. The baseline mammogram recommendation was dropped in 1992.
Between 1997 and 2015, the stakes were upped, and women aged 40-49 years were now recommended to have yearly mammograms, as were still all women aged 50 years and older.
In October 2015, the ACS changed their recommendation to say that women aged 40-44 years should have the choice of initiating mammogram screening, and that the risks and benefits of doing so should be discussed with their physicians. Women aged 45 years and older were still recommended for yearly mammogram screening. That recommendation stands today.
Controversies arise over risk/benefit
The technology was not, however, universally embraced. “By the late 1970s, mammography had diffused much more widely but had become a source of tremendous controversy. On the one hand, advocates of the technology enthusiastically touted its ability to detect smaller, more curable cancers. On the other hand, critics asked whether breast x-rays, particularly for women aged 50 and younger, actually caused more harm than benefit.”2
In addition, meta-analyses of the nine major screening trials conducted between 1965 and 1991 indicated that the reduced breast cancer mortality with screening was dependent on age. In particular, the results for women aged 40-49 years and 50-59 years showed only borderline statistical significance, and they varied depending on how cases were accrued in individual trials.
“Assuming that differences actually exist, the absolute breast cancer mortality reduction per 10,000 women screened for 10 years ranged from 3 for age 39-49 years; 5-8 for age 50-59 years; and 12-21 for age 60=69 years,” according to a review by the U.S. Preventive Services Task Force.9
The estimates for the group aged 70-74 years were limited by low numbers of events in trials that had smaller numbers of women in this age group.
Age has continued to be a major factor in determining the cost/benefit of routine mammography screening, with the American College of Physicians stating in its 2019 guidelines, “The potential harms outweigh the benefits in most women aged 40 to 49 years,” and adding, “In average-risk women aged 75 years or older or in women with a life expectancy of 10 years or less, clinicians should discontinue screening for breast cancer.”10
A Cochrane Report from 2013 was equally critical: “If we assume that screening reduces breast cancer mortality by 15% after 13 years of follow-up and that overdiagnosis and overtreatment is at 30%, it means that for every 2,000 women invited for screening throughout 10 years, one will avoid dying of breast cancer and 10 healthy women, who would not have been diagnosed if there had not been screening, will be treated unnecessarily. Furthermore, more than 200 women will experience important psychological distress including anxiety and uncertainty for years because of false positive findings.”11
Conflicting voices exist
These reports advising a more nuanced evaluation of the benefits of mammography, however, were received with skepticism from doctors committed to the vision of breast cancer screening and convinced by anecdotal evidence in their own practices.
These reports were also in direct contradiction to recommendations made in 1997 by the National Cancer Institute, which recommended screening mammograms every 3 years for women aged 40-49 years at average risk of breast cancer.
Such scientific vacillation has contributed to a love/hate relationship with mammography in the mainstream media, fueling new controversies with regard to breast cancer screening, sometimes as much driven by public suspicion and political advocacy as by scientific evolution.
Vocal opponents of universal mammography screening arose throughout the years, and even the cases of Betty Ford and Happy Rockefeller have been called into question as iconic demonstrations of the effectiveness of screening. And although not directly linked to the issue of screening, the rebellion against the routine use of radical mastectomies, a technique pioneered by Halsted in 1894 and in continuing use into the modern era, sparked outrage in women’s rights activists who saw it as evidence of a patriarchal medical establishment making arbitrary decisions concerning women’s bodies. For example, feminist and breast cancer activist Rose Kushner argued against the unnecessary disfigurement of women’s bodies and urged the use and development of less drastic techniques, including partial mastectomies and lumpectomies as viable choices. And these choices were increasingly supported by the medical community as safe and effective alternatives for many patients.12
A 2015 paper in the Journal of the Royal Society of Medicine was bluntly titled “Mammography screening is harmful and should be abandoned.”13 According to the author, who was the editor of the 2013 Cochrane Report, “I believe that if screening had been a drug, it would have been withdrawn from the market long ago.” And the popular press has not been shy at weighing in on the controversy, driven, in part, by the lack of consensus and continually changing guidelines, with major publications such as U.S. News and World Report, the Washington Post, and others addressing the issue over the years. And even public advocacy groups such as the Susan G. Komen organization14 are supporting the more modern professional guidelines in taking a more nuanced approach to the discussion of risks and benefits for individual women.
In 2014, the Swiss Medical Board, a nationally appointed body, recommended that new mammography screening programs should not be instituted in that country and that limits be placed on current programs because of the imbalance between risks and benefits of mammography screening.15 And a study done in Australia in 2020 agreed, stating, “Using data of 30% overdiagnosis of women aged 50 to 69 years in the NSW [New South Wales] BreastScreen program in 2012, we calculated an Australian ratio of harm of overdiagnosis to benefit (breast cancer deaths avoided) of 15:1 and recommended stopping the invitation to screening.”16
Conclusion
If nothing else, the history of mammography shows that the interconnection of social factors with the rise of a medical technology can have profound impacts on patient care. Technology developed by men for women became a touchstone of resentment in a world ever more aware of sex and gender biases in everything from the conduct of clinical trials to the care (or lack thereof) of women with heart disease. Tied for so many years to a radically disfiguring and drastic form of surgery that affected what many felt to be a hallmark and representation of womanhood1,17 mammography also carried the weight of both the real and imaginary fears of radiation exposure.
Well into its development, the technology still found itself under intense public scrutiny, and was enmeshed in a continual media circus, with ping-ponging discussions of risk/benefit in the scientific literature fueling complaints by many of the dominance of a patriarchal medical community over women’s bodies.
With guidelines for mammography still evolving, questions still remaining, and new technologies such as digital imaging falling short in their hoped-for promise, the story remains unfinished, and the future still uncertain. One thing remains clear, however: In the right circumstances, with the right patient population, and properly executed, mammography has saved lives when tied to effective, early treatment, whatever its flaws and failings. This truth goes hand in hand with another reality: It may have also contributed to considerable unanticipated harm through overdiagnosis and overtreatment.
Overall, the history of mammography is a cautionary tale for the entire medical community and for the development of new medical technologies. The push-pull of the demand for progress to save lives and the slowness and often inconclusiveness of scientific studies that validate new technologies create gray areas, where social determinants and professional interests vie in an information vacuum for control of the narrative of risks vs. benefits.
The story of mammography is not yet concluded, and may never be, especially given the unlikelihood of conducting the massive randomized clinical trials that would be needed to settle the issue. It is more likely to remain controversial, at least until the technology of mammography becomes obsolete, replaced by something new and different, which will likely start the push-pull cycle all over again.
And regardless of the risks and benefits of mammography screening, the issue of treatment once breast cancer is identified is perhaps one of more overwhelming import.
References
1. Berry, DA. The Breast. 2013;22[Supplement 2]:S73-S76.
2. Lerner, BH. “To See Today With the Eyes of Tomorrow: A History of Screening Mammography.” Background paper for the Institute of Medicine report Mammography and Beyond: Developing Technologies for the Early Detection of Breast Cancer. 2001.
3. NCI website. The National Cancer Act of 1971. www.cancer.gov/about-nci/overview/history/national-cancer-act-1971.
4. Lerner BH. The Huffington Post, Sep. 26, 2014.
5. Wu C. Cancer Today. 2012;2(3): Sep. 27.
6. “”The New York Times. Oct. 17, 1987.
7. Ford B. Remarks to the American Cancer Society. 1975.
8. The American Cancer Society website. History of ACS Recommendations for the Early Detection of Cancer in People Without Symptoms.
9. Nelson HD et al. Screening for Breast Cancer: A Systematic Review to Update the 2009 U.S. Preventive Services Task Force Recommendation. 2016; Evidence Syntheses, No. 124; pp.29-49.
10. Qasseem A et al. Annals of Internal Medicine. 2019;170(8):547-60.
11. Gotzsche PC et al. Cochrane Report 2013.
12. Lerner, BH. West J Med. May 2001;174(5):362-5.
13. Gotzsche PC. J R Soc Med. 2015;108(9): 341-5.
14. Susan G. Komen website. Weighing the Benefits and Risks of Mammography.
15. Biller-Andorno N et al. N Engl J Med 2014;370:1965-7.
16. Burton R et al. JAMA Netw Open. 2020;3(6):e208249.
17. Webb C et al. Plast Surg. 2019;27(1):49-53.
Mark Lesney is the editor of Hematology News and the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has worked as a writer/editor for the American Chemical Society, and has served as an adjunct assistant professor in the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
Science and technology emerge from and are shaped by social forces outside the laboratory and clinic. This is an essential fact of most new medical technology. In the Chronicles of Cancer series, part 1 of the story of mammography focused on the technological determinants of its development and use. Part 2 will focus on some of the social forces that shaped the development of mammography.
“Few medical issues have been as controversial – or as political, at least in the United States – as the role of mammographic screening for breast cancer,” according to Donald A. Berry, PhD, a biostatistician at the University of Texas MD Anderson Cancer Center, Houston.1
In fact, technology aside, the history of mammography has been and remains rife with controversy on the one side and vigorous promotion on the other, all enmeshed within the War on Cancer, corporate and professional interests, and the women’s rights movement’s growing issues with what was seen as a patriarchal medical establishment.
Today the issue of conflicts of interest are paramount in any discussion of new medical developments, from the early preclinical stages to ultimate deployment. Then, as now, professional and advocacy societies had a profound influence on government and social decision-making, but in that earlier, more trusting era, buoyed by the amazing changes that technology was bringing to everyday life and an unshakable commitment to and belief in “progress,” science and the medical community held a far more effective sway over the beliefs and behavior of the general population.
Women’s health observed
Although the main focus of the women’s movement with regard to breast cancer was a struggle against the common practice of routine radical mastectomies and a push toward breast-conserving surgeries, the issue of preventive care and screening with regard to women’s health was also a major concern.
Regarding mammography, early enthusiasm in the medical community and among the general public was profound. In 1969, Robert Egan described how mammography had a “certain magic appeal.” The patient, he continued, “feels something special is being done for her.” Women whose cancers had been discovered on a mammogram praised radiologists as heroes who had saved their lives.2
In that era, however, beyond the confines of the doctor’s office, mammography and breast cancer remained topics not discussed among the public at large, despite efforts by the American Cancer Society to change this.
ACS weighs in
Various groups had been promoting the benefits of breast self-examination since the 1930s, and in 1947, the American Cancer Society launched an awareness campaign, “Look for a Lump or Thickening in the Breast,” instructing women to perform a monthly breast self-exam. Between self-examination and clinical breast examinations in physicians’ offices, the ACS believed that smaller and more treatable breast cancers could be discovered.
In 1972, the ACS, working with the National Cancer Institute (NCI), inaugurated the Breast Cancer Detection Demonstration Project (BCDDP), which planned to screen over a quarter of a million American women for breast cancer. The initiative was a direct outgrowth of the National Cancer Act of 1971,3 the key legislation of the War on Cancer, promoted by President Richard Nixon in his State of the Union address in 1971 and responsible for the creation of the National Cancer Institute.
Arthur I. Holleb, MD, ACS senior vice president for medical affairs and research, announced that, “[T]he time has come for the American Cancer Society to mount a massive program on mammography just as we did with the Pap test,”2 according to Barron Lerner, MD, whose book “The Breast Cancer Wars” provides a history of the long-term controversies involved.4
The Pap test, widely promulgated in the 1950s and 1960s, had produced a decline in mortality from cervical cancer.
Regardless of the lack of data on effectiveness at earlier ages, the ACS chose to include women as young as 35 in the BCDDP in order “to inculcate them with ‘good health habits’ ” and “to make our screenee want to return periodically and to want to act as a missionary to bring other women into the screening process.”2
Celebrity status matters
All of the elements of a social revolution in the use of mammography were in place in the late 1960s, but the final triggers to raise social consciousness were the cases of several high-profile female celebrities. In 1973, beloved former child star Shirley Temple Black revealed her breast cancer diagnosis and mastectomy in an era when public discussion of cancer – especially breast cancer – was rare.4
But it wasn’t until 1974 that public awareness and media coverage exploded, sparked by the impact of First Lady Betty Ford’s outspokenness on her own experience of breast cancer. “In obituaries prior to the 1950s and 1960s, women who died from breast cancer were often listed as dying from ‘a prolonged disease’ or ‘a woman’s disease,’ ” according to Tasha Dubriwny, PhD, now an associate professor of communication and women’s and gender studies at Texas A&M University, College Station, when interviewed by the American Association for Cancer Research.5Betty Ford openly addressed her breast cancer diagnosis and treatment and became a prominent advocate for early screening, transforming the landscape of breast cancer awareness. And although Betty Ford’s diagnosis was based on clinical examination rather than mammography, its boost to overall screening was indisputable.
“Within weeks [after Betty Ford’s announcement] thousands of women who had been reluctant to examine their breasts inundated cancer screening centers,” according to a 1987 article in the New York Times.6 Among these women was Happy Rockefeller, the wife of Vice President Nelson A. Rockefeller. Happy Rockefeller also found that she had breast cancer upon screening, and with Betty Ford would become another icon thereafter for breast cancer screening.
“Ford’s lesson for other women was straightforward: Get a mammogram, which she had not done. The American Cancer Society and National Cancer Institute had recently mounted a demonstration project to promote the detection of breast cancer as early as possible, when it was presumed to be more curable. The degree to which women embraced Ford’s message became clear through the famous ‘Betty Ford blip.’ So many women got breast examinations and mammograms for the first time after Ford’s announcement that the actual incidence of breast cancer in the United States went up by 15 percent.”4
In a 1975 address to the American Cancer Society, Betty Ford said: “One day I appeared to be fine and the next day I was in the hospital for a mastectomy. It made me realize how many women in the country could be in the same situation. That realization made me decide to discuss my breast cancer operation openly, because I thought of all the lives in jeopardy. My experience and frank discussion of breast cancer did prompt many women to learn about self-examination, regular checkups, and such detection techniques as mammography. These are so important. I just cannot stress enough how necessary it is for women to take an active interest in their own health and body.”7
ACS guidelines evolve
It wasn’t until 1976 that the ACS issued its first major guidelines for mammography screening. The ACS suggested mammograms may be called for in women aged 35-39 if there was a personal history of breast cancer, and between ages 40 and 49 if their mother or sisters had a history of breast cancer. Women aged 50 years and older could have yearly screening. Thereafter, the use of mammography was encouraged more and more with each new set of recommendations.8
Between 1980 and 1982, these guidelines expanded to advising a baseline mammogram for women aged 35-39 years; that women consult with their physician between ages 40 and 49; and that women over 50 have a yearly mammogram.
Between 1983 and 1991, the recommendations were for a baseline mammogram for women aged 35-39 years; a mammogram every 1-2 years for women aged 40-49; and yearly mammograms for women aged 50 and up. The baseline mammogram recommendation was dropped in 1992.
Between 1997 and 2015, the stakes were upped, and women aged 40-49 years were now recommended to have yearly mammograms, as were still all women aged 50 years and older.
In October 2015, the ACS changed their recommendation to say that women aged 40-44 years should have the choice of initiating mammogram screening, and that the risks and benefits of doing so should be discussed with their physicians. Women aged 45 years and older were still recommended for yearly mammogram screening. That recommendation stands today.
Controversies arise over risk/benefit
The technology was not, however, universally embraced. “By the late 1970s, mammography had diffused much more widely but had become a source of tremendous controversy. On the one hand, advocates of the technology enthusiastically touted its ability to detect smaller, more curable cancers. On the other hand, critics asked whether breast x-rays, particularly for women aged 50 and younger, actually caused more harm than benefit.”2
In addition, meta-analyses of the nine major screening trials conducted between 1965 and 1991 indicated that the reduced breast cancer mortality with screening was dependent on age. In particular, the results for women aged 40-49 years and 50-59 years showed only borderline statistical significance, and they varied depending on how cases were accrued in individual trials.
“Assuming that differences actually exist, the absolute breast cancer mortality reduction per 10,000 women screened for 10 years ranged from 3 for age 39-49 years; 5-8 for age 50-59 years; and 12-21 for age 60=69 years,” according to a review by the U.S. Preventive Services Task Force.9
The estimates for the group aged 70-74 years were limited by low numbers of events in trials that had smaller numbers of women in this age group.
Age has continued to be a major factor in determining the cost/benefit of routine mammography screening, with the American College of Physicians stating in its 2019 guidelines, “The potential harms outweigh the benefits in most women aged 40 to 49 years,” and adding, “In average-risk women aged 75 years or older or in women with a life expectancy of 10 years or less, clinicians should discontinue screening for breast cancer.”10
A Cochrane Report from 2013 was equally critical: “If we assume that screening reduces breast cancer mortality by 15% after 13 years of follow-up and that overdiagnosis and overtreatment is at 30%, it means that for every 2,000 women invited for screening throughout 10 years, one will avoid dying of breast cancer and 10 healthy women, who would not have been diagnosed if there had not been screening, will be treated unnecessarily. Furthermore, more than 200 women will experience important psychological distress including anxiety and uncertainty for years because of false positive findings.”11
Conflicting voices exist
These reports advising a more nuanced evaluation of the benefits of mammography, however, were received with skepticism from doctors committed to the vision of breast cancer screening and convinced by anecdotal evidence in their own practices.
These reports were also in direct contradiction to recommendations made in 1997 by the National Cancer Institute, which recommended screening mammograms every 3 years for women aged 40-49 years at average risk of breast cancer.
Such scientific vacillation has contributed to a love/hate relationship with mammography in the mainstream media, fueling new controversies with regard to breast cancer screening, sometimes as much driven by public suspicion and political advocacy as by scientific evolution.
Vocal opponents of universal mammography screening arose throughout the years, and even the cases of Betty Ford and Happy Rockefeller have been called into question as iconic demonstrations of the effectiveness of screening. And although not directly linked to the issue of screening, the rebellion against the routine use of radical mastectomies, a technique pioneered by Halsted in 1894 and in continuing use into the modern era, sparked outrage in women’s rights activists who saw it as evidence of a patriarchal medical establishment making arbitrary decisions concerning women’s bodies. For example, feminist and breast cancer activist Rose Kushner argued against the unnecessary disfigurement of women’s bodies and urged the use and development of less drastic techniques, including partial mastectomies and lumpectomies as viable choices. And these choices were increasingly supported by the medical community as safe and effective alternatives for many patients.12
A 2015 paper in the Journal of the Royal Society of Medicine was bluntly titled “Mammography screening is harmful and should be abandoned.”13 According to the author, who was the editor of the 2013 Cochrane Report, “I believe that if screening had been a drug, it would have been withdrawn from the market long ago.” And the popular press has not been shy at weighing in on the controversy, driven, in part, by the lack of consensus and continually changing guidelines, with major publications such as U.S. News and World Report, the Washington Post, and others addressing the issue over the years. And even public advocacy groups such as the Susan G. Komen organization14 are supporting the more modern professional guidelines in taking a more nuanced approach to the discussion of risks and benefits for individual women.
In 2014, the Swiss Medical Board, a nationally appointed body, recommended that new mammography screening programs should not be instituted in that country and that limits be placed on current programs because of the imbalance between risks and benefits of mammography screening.15 And a study done in Australia in 2020 agreed, stating, “Using data of 30% overdiagnosis of women aged 50 to 69 years in the NSW [New South Wales] BreastScreen program in 2012, we calculated an Australian ratio of harm of overdiagnosis to benefit (breast cancer deaths avoided) of 15:1 and recommended stopping the invitation to screening.”16
Conclusion
If nothing else, the history of mammography shows that the interconnection of social factors with the rise of a medical technology can have profound impacts on patient care. Technology developed by men for women became a touchstone of resentment in a world ever more aware of sex and gender biases in everything from the conduct of clinical trials to the care (or lack thereof) of women with heart disease. Tied for so many years to a radically disfiguring and drastic form of surgery that affected what many felt to be a hallmark and representation of womanhood1,17 mammography also carried the weight of both the real and imaginary fears of radiation exposure.
Well into its development, the technology still found itself under intense public scrutiny, and was enmeshed in a continual media circus, with ping-ponging discussions of risk/benefit in the scientific literature fueling complaints by many of the dominance of a patriarchal medical community over women’s bodies.
With guidelines for mammography still evolving, questions still remaining, and new technologies such as digital imaging falling short in their hoped-for promise, the story remains unfinished, and the future still uncertain. One thing remains clear, however: In the right circumstances, with the right patient population, and properly executed, mammography has saved lives when tied to effective, early treatment, whatever its flaws and failings. This truth goes hand in hand with another reality: It may have also contributed to considerable unanticipated harm through overdiagnosis and overtreatment.
Overall, the history of mammography is a cautionary tale for the entire medical community and for the development of new medical technologies. The push-pull of the demand for progress to save lives and the slowness and often inconclusiveness of scientific studies that validate new technologies create gray areas, where social determinants and professional interests vie in an information vacuum for control of the narrative of risks vs. benefits.
The story of mammography is not yet concluded, and may never be, especially given the unlikelihood of conducting the massive randomized clinical trials that would be needed to settle the issue. It is more likely to remain controversial, at least until the technology of mammography becomes obsolete, replaced by something new and different, which will likely start the push-pull cycle all over again.
And regardless of the risks and benefits of mammography screening, the issue of treatment once breast cancer is identified is perhaps one of more overwhelming import.
References
1. Berry, DA. The Breast. 2013;22[Supplement 2]:S73-S76.
2. Lerner, BH. “To See Today With the Eyes of Tomorrow: A History of Screening Mammography.” Background paper for the Institute of Medicine report Mammography and Beyond: Developing Technologies for the Early Detection of Breast Cancer. 2001.
3. NCI website. The National Cancer Act of 1971. www.cancer.gov/about-nci/overview/history/national-cancer-act-1971.
4. Lerner BH. The Huffington Post, Sep. 26, 2014.
5. Wu C. Cancer Today. 2012;2(3): Sep. 27.
6. “”The New York Times. Oct. 17, 1987.
7. Ford B. Remarks to the American Cancer Society. 1975.
8. The American Cancer Society website. History of ACS Recommendations for the Early Detection of Cancer in People Without Symptoms.
9. Nelson HD et al. Screening for Breast Cancer: A Systematic Review to Update the 2009 U.S. Preventive Services Task Force Recommendation. 2016; Evidence Syntheses, No. 124; pp.29-49.
10. Qasseem A et al. Annals of Internal Medicine. 2019;170(8):547-60.
11. Gotzsche PC et al. Cochrane Report 2013.
12. Lerner, BH. West J Med. May 2001;174(5):362-5.
13. Gotzsche PC. J R Soc Med. 2015;108(9): 341-5.
14. Susan G. Komen website. Weighing the Benefits and Risks of Mammography.
15. Biller-Andorno N et al. N Engl J Med 2014;370:1965-7.
16. Burton R et al. JAMA Netw Open. 2020;3(6):e208249.
17. Webb C et al. Plast Surg. 2019;27(1):49-53.
Mark Lesney is the editor of Hematology News and the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has worked as a writer/editor for the American Chemical Society, and has served as an adjunct assistant professor in the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
Identifying ovarian malignancy is not so easy
When an ovarian mass is anticipated or known, following evaluation of a patient’s history and physician examination, imaging via transvaginal and often abdominal ultrasound is the very next step. This evaluation likely will include both gray-scale and color Doppler examination. The initial concern always must be to identify ovarian malignancy.
Despite morphological scoring systems as well as the use of Doppler ultrasonography, there remains a lack of agreement and acceptance. In a 2008 multicenter study, Timmerman and colleagues evaluated 1,066 patients with 1,233 persistent adnexal tumors via transvaginal grayscale and Doppler ultrasound; 73% were benign tumors, and 27% were malignant tumors. Information on 42 gray-scale ultrasound variables and 6 Doppler variables was collected and evaluated to determine which variables had the highest positive predictive value for a malignant tumor and for a benign mass (Ultrasound Obstet Gynecol. 2008 Jun. doi: 10.1002/uog.5365).
Five simple rules were selected that best predict malignancy (M-rules), as follows:
- Irregular solid tumor.
- Ascites.
- At least four papillary projections.
- Irregular multilocular-solid tumor with a greatest diameter greater than or equal to 10 cm.
- Very high color content on Doppler exam.
The following five simple rules suggested that a mass is benign (B-rules):
- Unilocular cyst.
- Largest solid component less than 7 mm.
- Acoustic shadows.
- Smooth multilocular tumor less than 10 cm.
- No detectable blood flow with Doppler exam.
Unfortunately, despite a sensitivity of 93% and specificity of 90%, and a positive and negative predictive value of 80% and 97%, these 10 simple rules were applicable to only 76% of tumors.
To assist those of us who are not gynecologic oncologists and who are often faced with having to determine whether surgery is recommended, I have elicited the expertise of Jubilee Brown, MD, professor and associate director of gynecologic oncology at the Levine Cancer Institute, Carolinas HealthCare System, in Charlotte, N.C., and the current president of the AAGL, to lead us in a review of evaluating an ovarian mass.
Dr. Miller is professor of obstetrics & gynecology in the department of clinical sciences, Rosalind Franklin University, North Chicago, Ill., and director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, both in Illinois. Email him at [email protected].
When an ovarian mass is anticipated or known, following evaluation of a patient’s history and physician examination, imaging via transvaginal and often abdominal ultrasound is the very next step. This evaluation likely will include both gray-scale and color Doppler examination. The initial concern always must be to identify ovarian malignancy.
Despite morphological scoring systems as well as the use of Doppler ultrasonography, there remains a lack of agreement and acceptance. In a 2008 multicenter study, Timmerman and colleagues evaluated 1,066 patients with 1,233 persistent adnexal tumors via transvaginal grayscale and Doppler ultrasound; 73% were benign tumors, and 27% were malignant tumors. Information on 42 gray-scale ultrasound variables and 6 Doppler variables was collected and evaluated to determine which variables had the highest positive predictive value for a malignant tumor and for a benign mass (Ultrasound Obstet Gynecol. 2008 Jun. doi: 10.1002/uog.5365).
Five simple rules were selected that best predict malignancy (M-rules), as follows:
- Irregular solid tumor.
- Ascites.
- At least four papillary projections.
- Irregular multilocular-solid tumor with a greatest diameter greater than or equal to 10 cm.
- Very high color content on Doppler exam.
The following five simple rules suggested that a mass is benign (B-rules):
- Unilocular cyst.
- Largest solid component less than 7 mm.
- Acoustic shadows.
- Smooth multilocular tumor less than 10 cm.
- No detectable blood flow with Doppler exam.
Unfortunately, despite a sensitivity of 93% and specificity of 90%, and a positive and negative predictive value of 80% and 97%, these 10 simple rules were applicable to only 76% of tumors.
To assist those of us who are not gynecologic oncologists and who are often faced with having to determine whether surgery is recommended, I have elicited the expertise of Jubilee Brown, MD, professor and associate director of gynecologic oncology at the Levine Cancer Institute, Carolinas HealthCare System, in Charlotte, N.C., and the current president of the AAGL, to lead us in a review of evaluating an ovarian mass.
Dr. Miller is professor of obstetrics & gynecology in the department of clinical sciences, Rosalind Franklin University, North Chicago, Ill., and director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, both in Illinois. Email him at [email protected].
When an ovarian mass is anticipated or known, following evaluation of a patient’s history and physician examination, imaging via transvaginal and often abdominal ultrasound is the very next step. This evaluation likely will include both gray-scale and color Doppler examination. The initial concern always must be to identify ovarian malignancy.
Despite morphological scoring systems as well as the use of Doppler ultrasonography, there remains a lack of agreement and acceptance. In a 2008 multicenter study, Timmerman and colleagues evaluated 1,066 patients with 1,233 persistent adnexal tumors via transvaginal grayscale and Doppler ultrasound; 73% were benign tumors, and 27% were malignant tumors. Information on 42 gray-scale ultrasound variables and 6 Doppler variables was collected and evaluated to determine which variables had the highest positive predictive value for a malignant tumor and for a benign mass (Ultrasound Obstet Gynecol. 2008 Jun. doi: 10.1002/uog.5365).
Five simple rules were selected that best predict malignancy (M-rules), as follows:
- Irregular solid tumor.
- Ascites.
- At least four papillary projections.
- Irregular multilocular-solid tumor with a greatest diameter greater than or equal to 10 cm.
- Very high color content on Doppler exam.
The following five simple rules suggested that a mass is benign (B-rules):
- Unilocular cyst.
- Largest solid component less than 7 mm.
- Acoustic shadows.
- Smooth multilocular tumor less than 10 cm.
- No detectable blood flow with Doppler exam.
Unfortunately, despite a sensitivity of 93% and specificity of 90%, and a positive and negative predictive value of 80% and 97%, these 10 simple rules were applicable to only 76% of tumors.
To assist those of us who are not gynecologic oncologists and who are often faced with having to determine whether surgery is recommended, I have elicited the expertise of Jubilee Brown, MD, professor and associate director of gynecologic oncology at the Levine Cancer Institute, Carolinas HealthCare System, in Charlotte, N.C., and the current president of the AAGL, to lead us in a review of evaluating an ovarian mass.
Dr. Miller is professor of obstetrics & gynecology in the department of clinical sciences, Rosalind Franklin University, North Chicago, Ill., and director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, both in Illinois. Email him at [email protected].
How to evaluate a suspicious ovarian mass
Ovarian masses are common in women of all ages. It is important not to miss even one ovarian cancer, but we must also identify masses that will resolve on their own over time to avoid overtreatment. These concurrent goals of excluding malignancy while not overtreating patients are the basis for management of the pelvic mass. Additionally, fertility preservation is important when surgery is performed in a reproductive-aged woman.
An ovarian mass may be anything from a simple functional or physiologic cyst to an endometrioma to an epithelial carcinoma, a germ-cell tumor, or a stromal tumor (the latter three of which may metastasize). Across the general population, women have a 5%-10% lifetime risk of needing surgery for a suspected ovarian mass and a 1.4% (1 in 70) risk that this mass is cancerous. The majority of ovarian cysts or masses therefore are benign.
A thorough history – including family history – and physical examination with appropriate laboratory testing and directed imaging are important first steps for the ob.gyn. Fortunately, we have guidelines and criteria governing not only when observation or surgery is warranted but also when patients should be referred to a gynecologic oncologist. By following these guidelines,1 we are able to achieve the best outcomes.
Transvaginal ultrasound
A 2007 groundbreaking study led by Barbara Goff, MD, demonstrated that there are warning signs for ovarian cancer – symptoms that are significantly associated with malignancy. Dr. Goff and her coinvestigators evaluated the charts of hundreds of patients, including about 150 with ovarian cancer, and found that pelvic/abdominal pressure or pain, bloating, increase in abdominal size, and difficulty eating or feeling full were significantly and independently associated with cancer if these symptoms were present for less than a year and occurred at least 12 times per month.2
A pelvic examination is an integral part of evaluating every patient who has such concerns. That said, pelvic exams have limited ability to identify adnexal masses, especially in women who are obese – and that’s where imaging becomes especially important.
Masses generally can be considered simple or complex based on their appearance. A simple cyst is fluid-filled with thin, smooth walls and the absence of solid components or septations; it is significantly more likely to resolve on its own and is less likely to imply malignancy than a complex cyst, especially in a premenopausal woman. A complex cyst is multiseptated and/or solid – possibly with papillary projections – and is more concerning, especially if there is increased, new vascularity. Making this distinction helps us determine the risk of malignancy.
Transvaginal ultrasound (TVUS) is the preferred method for imaging, and our threshold for obtaining a TVUS should be very low. Women who have symptoms or concerns that can’t be attributed to a particular condition, and women in whom a mass can be palpated (even if asymptomatic) should have a TVUS. The imaging modality is cost effective and well tolerated by patients, does not expose the patient to ionizing radiation, and should generally be considered first-line imaging.3,4
Size is not predictive of malignancy, but it is important for determining whether surgery is warranted. In our experience, a mass of 8-10 cm or larger on TVUS is at risk of torsion and is unlikely to resolve on its own, even in a premenopausal woman. While large masses generally require surgery, patients of any age who have simple cysts smaller than 8-10 cm generally can be followed with serial exams and ultrasound; spontaneous regression is common.
Doppler ultrasonography is useful for evaluating blood flow in and around an ovarian mass and can be helpful for confirming suspected characteristics of a mass.
Recent studies from the radiology community have looked at the utility of the resistive index – a measure of the impedance and velocity of blood flow – as a predictor of ovarian malignancy. However, we caution against using Doppler to determine whether a mass is benign or malignant, or to determine the necessity of surgery. An abnormal ovary may have what is considered to be a normal resistive index, and the resistive index of a normal ovary may fall within the abnormal range. Doppler flow can be helpful, but it must be combined with other predictive features, like solid components with flow or papillary projections within a cyst, to define a decision about surgery.4,5
Magnetic resonance imaging can be useful in differentiating a fibroid from an ovarian mass, and a CT scan can be helpful in looking for disseminated disease when ovarian cancer is suspected based on ultrasound imaging, physical and history, and serum markers. A CT is useful, for instance, in a patient whose ovary is distended with ascites or who has upper abdominal complaints and a complex cyst. CT, PET, and MRI are not recommended in the initial evaluation of an ovarian mass.
The utility of serum biomarkers
Cancer antigen 125 (CA-125) testing may be helpful – in combination with other findings – for decision-making regarding the likelihood of malignancy and the need to refer patients. CA-125 is like Doppler in that a normal CA-125 cannot eliminate the possibility of cancer, and an abnormal CA-125 does not in and of itself imply malignancy. It’s far from a perfect cancer screening test.
CA-125 is a protein associated with epithelial ovarian malignancies, the type of ovarian cancer most commonly seen in postmenopausal women with genetic predispositions. Its specificity and positive predictive value are much higher in postmenopausal women than in average-risk premenopausal women (those without a family history or a known mutation that predisposes them to ovarian cancer). Levels of the marker are elevated in association with many nonmalignant conditions in premenopausal women – endometriosis, fibroids, and various inflammatory conditions, for instance – so the marker’s utility in this population is limited.
For women who have a family history of ovarian cancer or a known breast cancer gene 1 (BRCA1) or BRCA2 mutation, there are some data that suggest that monitoring with CA-125 measurements and TVUS may be a good approach to following patients prior to the age at which risk-reducing surgery can best be performed.
In an adolescent girl or a woman of reproductive age, we think less about epithelial cancer and more about germ-cell and stromal tumors. When a solid mass is palpated or visualized on imaging, we therefore will utilize a different set of markers; alpha-fetoprotein, L-lactate dehydrogenase, and beta-HCG, for instance, have much higher specificity than CA-125 does for germ-cell tumors in this age group and may be helpful in the evaluation. Similarly, in cases of a very large mass resembling a mucinous tumor, a carcinoembryonic antigen may be helpful.
A number of proprietary profiling technologies have been developed to determine the risk of a diagnosed mass being malignant. For instance, the OVA1 assay looks at five serum markers and scores the results, and the Risk of Ovarian Malignancy Algorithm (ROMA) combines the results of three serum markers with menopausal status into a numerical score. Both have Food and Drug Administration approval for use in women in whom surgery has been deemed necessary. These panels can be fairly predictive of risk and may be helpful – especially in rural areas – in determining which women should be referred to a gynecologic oncologist for surgery.
It is important to appreciate that an ovarian cyst or mass should never be biopsied or aspirated lest a malignant tumor confined to one ovary be potentially spread to the peritoneum.
Referral to a gynecologic oncologist
Postmenopausal women with a CA-125 greater than 35 U/mL should be referred, as should postmenopausal women with ascites, those with a nodular or fixed pelvic mass, and those with suspected abdominal or distant metastases (per a CT scan, for instance).
In premenopausal women, ascites, a nodular or fixed mass, and evidence of metastases also are reasons for referral to a gynecologic oncologist. CA-125, again, is much more likely to be elevated for reasons other than malignancy and therefore is not as strong a driver for referral as in postmenopausal women. Patients with markedly elevated levels, however, should probably be referred – particularly when other clinical factors also suggest the need for consultation. While there is no evidence-based threshold for CA-125 in premenopausal women, a CA-125 greater than 200 U/mL is a good cutoff for referral.
For any patient, family history of breast and/or ovarian cancer – especially in a first-degree relative – raises the risk of malignancy and should figure prominently into decision-making regarding referral. Criteria for referral are among the points discussed in the ACOG 2016 Practice Bulletin on Evaluation and Management of Adnexal Masses.1
A note on BRCA mutations
As the American College of Obstetricians and Gynecologists says in its practice bulletin, the most important personal risk factor for ovarian cancer is a strong family history of breast or ovarian cancer. Women with such a family history can undergo genetic testing for BRCA mutations and have the opportunity to prevent ovarian cancers when mutations are detected. This simple blood test can save lives.
A modeling study we recently completed – not yet published – shows that it actually would be cost effective to do population screening with BRCA testing performed on every woman at age 30 years.
According to the National Cancer Institute website (last review: 2018), it is estimated that about 44% of women who inherit a BRCA1 mutation, and about 17% of those who inherit a BRAC2 mutation, will develop ovarian cancer by the age of 80 years. By identifying those mutations, women may undergo risk-reducing surgery at designated ages after childbearing is complete and bring their risk down to under 5%.
An international take on managing adnexal masses
- Pelvic ultrasound should include the transvaginal approach. Use Doppler imaging as indicated.
- Although simple ovarian cysts are not precursor lesions to a malignant ovarian cancer, perform a high-quality examination to make sure there are no solid/papillary structures before classifying a cyst as a simple cyst. The risk of progression to malignancy is extremely low, but some follow-up is prudent.
- The most accurate method of characterizing an ovarian mass currently is real-time pattern recognition sonography in the hands of an experienced imager.
- Pattern recognition sonography or a risk model such as the International Ovarian Tumor Analysis (IOTA) Simple Rules can be used to initially characterize an ovarian mass.
- When an ovarian lesion is classified as benign, the patient may be followed conservatively, or if indicated, surgery can be performed by a general gynecologist.
- Serial sonography can be beneficial, but there are limited prospective data to support an exact interval and duration.
- Fewer surgical interventions may result in an increase in sonographic surveillance.
- When an ovarian lesion is considered indeterminate on initial sonography, and after appropriate clinical evaluation, a “second-step” evaluation may include referral to an expert sonologist, serial sonography, application of established risk-prediction models, correlation with serum biomarkers, correlation with MRI, or referral to a gynecologic oncologist for further evaluation.
From the First International Consensus Report on Adnexal Masses: Management Recommendations
Source: Glanc P et al. J Ultrasound Med. 2017 May;36(5):849-63.
Dr. Brown reported that she had received an earlier grant from Aspira Labs, the company that developed the OVA1 assay. Dr. Miller reported that he has no relevant financial disclosures.
References
1. Obstet Gynecol. 2016 Nov. doi: 10.1097/AOG.0000000000001768.
2. Cancer. 2007 Jan 15. doi: 10.1002/cncr.22371.
3. Clin Obstet Gynecol. 2015 Mar. doi: 10.1097/GRF.0000000000000083.
4. Ultrasound Q. 2013 Mar. doi: 10.1097/RUQ.0b013e3182814d9b.
5. Ultrasound Obstet Gynecol. 2008 Jun. doi: 10.1002/uog.5365.
Ovarian masses are common in women of all ages. It is important not to miss even one ovarian cancer, but we must also identify masses that will resolve on their own over time to avoid overtreatment. These concurrent goals of excluding malignancy while not overtreating patients are the basis for management of the pelvic mass. Additionally, fertility preservation is important when surgery is performed in a reproductive-aged woman.
An ovarian mass may be anything from a simple functional or physiologic cyst to an endometrioma to an epithelial carcinoma, a germ-cell tumor, or a stromal tumor (the latter three of which may metastasize). Across the general population, women have a 5%-10% lifetime risk of needing surgery for a suspected ovarian mass and a 1.4% (1 in 70) risk that this mass is cancerous. The majority of ovarian cysts or masses therefore are benign.
A thorough history – including family history – and physical examination with appropriate laboratory testing and directed imaging are important first steps for the ob.gyn. Fortunately, we have guidelines and criteria governing not only when observation or surgery is warranted but also when patients should be referred to a gynecologic oncologist. By following these guidelines,1 we are able to achieve the best outcomes.
Transvaginal ultrasound
A 2007 groundbreaking study led by Barbara Goff, MD, demonstrated that there are warning signs for ovarian cancer – symptoms that are significantly associated with malignancy. Dr. Goff and her coinvestigators evaluated the charts of hundreds of patients, including about 150 with ovarian cancer, and found that pelvic/abdominal pressure or pain, bloating, increase in abdominal size, and difficulty eating or feeling full were significantly and independently associated with cancer if these symptoms were present for less than a year and occurred at least 12 times per month.2
A pelvic examination is an integral part of evaluating every patient who has such concerns. That said, pelvic exams have limited ability to identify adnexal masses, especially in women who are obese – and that’s where imaging becomes especially important.
Masses generally can be considered simple or complex based on their appearance. A simple cyst is fluid-filled with thin, smooth walls and the absence of solid components or septations; it is significantly more likely to resolve on its own and is less likely to imply malignancy than a complex cyst, especially in a premenopausal woman. A complex cyst is multiseptated and/or solid – possibly with papillary projections – and is more concerning, especially if there is increased, new vascularity. Making this distinction helps us determine the risk of malignancy.
Transvaginal ultrasound (TVUS) is the preferred method for imaging, and our threshold for obtaining a TVUS should be very low. Women who have symptoms or concerns that can’t be attributed to a particular condition, and women in whom a mass can be palpated (even if asymptomatic) should have a TVUS. The imaging modality is cost effective and well tolerated by patients, does not expose the patient to ionizing radiation, and should generally be considered first-line imaging.3,4
Size is not predictive of malignancy, but it is important for determining whether surgery is warranted. In our experience, a mass of 8-10 cm or larger on TVUS is at risk of torsion and is unlikely to resolve on its own, even in a premenopausal woman. While large masses generally require surgery, patients of any age who have simple cysts smaller than 8-10 cm generally can be followed with serial exams and ultrasound; spontaneous regression is common.
Doppler ultrasonography is useful for evaluating blood flow in and around an ovarian mass and can be helpful for confirming suspected characteristics of a mass.
Recent studies from the radiology community have looked at the utility of the resistive index – a measure of the impedance and velocity of blood flow – as a predictor of ovarian malignancy. However, we caution against using Doppler to determine whether a mass is benign or malignant, or to determine the necessity of surgery. An abnormal ovary may have what is considered to be a normal resistive index, and the resistive index of a normal ovary may fall within the abnormal range. Doppler flow can be helpful, but it must be combined with other predictive features, like solid components with flow or papillary projections within a cyst, to define a decision about surgery.4,5
Magnetic resonance imaging can be useful in differentiating a fibroid from an ovarian mass, and a CT scan can be helpful in looking for disseminated disease when ovarian cancer is suspected based on ultrasound imaging, physical and history, and serum markers. A CT is useful, for instance, in a patient whose ovary is distended with ascites or who has upper abdominal complaints and a complex cyst. CT, PET, and MRI are not recommended in the initial evaluation of an ovarian mass.
The utility of serum biomarkers
Cancer antigen 125 (CA-125) testing may be helpful – in combination with other findings – for decision-making regarding the likelihood of malignancy and the need to refer patients. CA-125 is like Doppler in that a normal CA-125 cannot eliminate the possibility of cancer, and an abnormal CA-125 does not in and of itself imply malignancy. It’s far from a perfect cancer screening test.
CA-125 is a protein associated with epithelial ovarian malignancies, the type of ovarian cancer most commonly seen in postmenopausal women with genetic predispositions. Its specificity and positive predictive value are much higher in postmenopausal women than in average-risk premenopausal women (those without a family history or a known mutation that predisposes them to ovarian cancer). Levels of the marker are elevated in association with many nonmalignant conditions in premenopausal women – endometriosis, fibroids, and various inflammatory conditions, for instance – so the marker’s utility in this population is limited.
For women who have a family history of ovarian cancer or a known breast cancer gene 1 (BRCA1) or BRCA2 mutation, there are some data that suggest that monitoring with CA-125 measurements and TVUS may be a good approach to following patients prior to the age at which risk-reducing surgery can best be performed.
In an adolescent girl or a woman of reproductive age, we think less about epithelial cancer and more about germ-cell and stromal tumors. When a solid mass is palpated or visualized on imaging, we therefore will utilize a different set of markers; alpha-fetoprotein, L-lactate dehydrogenase, and beta-HCG, for instance, have much higher specificity than CA-125 does for germ-cell tumors in this age group and may be helpful in the evaluation. Similarly, in cases of a very large mass resembling a mucinous tumor, a carcinoembryonic antigen may be helpful.
A number of proprietary profiling technologies have been developed to determine the risk of a diagnosed mass being malignant. For instance, the OVA1 assay looks at five serum markers and scores the results, and the Risk of Ovarian Malignancy Algorithm (ROMA) combines the results of three serum markers with menopausal status into a numerical score. Both have Food and Drug Administration approval for use in women in whom surgery has been deemed necessary. These panels can be fairly predictive of risk and may be helpful – especially in rural areas – in determining which women should be referred to a gynecologic oncologist for surgery.
It is important to appreciate that an ovarian cyst or mass should never be biopsied or aspirated lest a malignant tumor confined to one ovary be potentially spread to the peritoneum.
Referral to a gynecologic oncologist
Postmenopausal women with a CA-125 greater than 35 U/mL should be referred, as should postmenopausal women with ascites, those with a nodular or fixed pelvic mass, and those with suspected abdominal or distant metastases (per a CT scan, for instance).
In premenopausal women, ascites, a nodular or fixed mass, and evidence of metastases also are reasons for referral to a gynecologic oncologist. CA-125, again, is much more likely to be elevated for reasons other than malignancy and therefore is not as strong a driver for referral as in postmenopausal women. Patients with markedly elevated levels, however, should probably be referred – particularly when other clinical factors also suggest the need for consultation. While there is no evidence-based threshold for CA-125 in premenopausal women, a CA-125 greater than 200 U/mL is a good cutoff for referral.
For any patient, family history of breast and/or ovarian cancer – especially in a first-degree relative – raises the risk of malignancy and should figure prominently into decision-making regarding referral. Criteria for referral are among the points discussed in the ACOG 2016 Practice Bulletin on Evaluation and Management of Adnexal Masses.1
A note on BRCA mutations
As the American College of Obstetricians and Gynecologists says in its practice bulletin, the most important personal risk factor for ovarian cancer is a strong family history of breast or ovarian cancer. Women with such a family history can undergo genetic testing for BRCA mutations and have the opportunity to prevent ovarian cancers when mutations are detected. This simple blood test can save lives.
A modeling study we recently completed – not yet published – shows that it actually would be cost effective to do population screening with BRCA testing performed on every woman at age 30 years.
According to the National Cancer Institute website (last review: 2018), it is estimated that about 44% of women who inherit a BRCA1 mutation, and about 17% of those who inherit a BRAC2 mutation, will develop ovarian cancer by the age of 80 years. By identifying those mutations, women may undergo risk-reducing surgery at designated ages after childbearing is complete and bring their risk down to under 5%.
An international take on managing adnexal masses
- Pelvic ultrasound should include the transvaginal approach. Use Doppler imaging as indicated.
- Although simple ovarian cysts are not precursor lesions to a malignant ovarian cancer, perform a high-quality examination to make sure there are no solid/papillary structures before classifying a cyst as a simple cyst. The risk of progression to malignancy is extremely low, but some follow-up is prudent.
- The most accurate method of characterizing an ovarian mass currently is real-time pattern recognition sonography in the hands of an experienced imager.
- Pattern recognition sonography or a risk model such as the International Ovarian Tumor Analysis (IOTA) Simple Rules can be used to initially characterize an ovarian mass.
- When an ovarian lesion is classified as benign, the patient may be followed conservatively, or if indicated, surgery can be performed by a general gynecologist.
- Serial sonography can be beneficial, but there are limited prospective data to support an exact interval and duration.
- Fewer surgical interventions may result in an increase in sonographic surveillance.
- When an ovarian lesion is considered indeterminate on initial sonography, and after appropriate clinical evaluation, a “second-step” evaluation may include referral to an expert sonologist, serial sonography, application of established risk-prediction models, correlation with serum biomarkers, correlation with MRI, or referral to a gynecologic oncologist for further evaluation.
From the First International Consensus Report on Adnexal Masses: Management Recommendations
Source: Glanc P et al. J Ultrasound Med. 2017 May;36(5):849-63.
Dr. Brown reported that she had received an earlier grant from Aspira Labs, the company that developed the OVA1 assay. Dr. Miller reported that he has no relevant financial disclosures.
References
1. Obstet Gynecol. 2016 Nov. doi: 10.1097/AOG.0000000000001768.
2. Cancer. 2007 Jan 15. doi: 10.1002/cncr.22371.
3. Clin Obstet Gynecol. 2015 Mar. doi: 10.1097/GRF.0000000000000083.
4. Ultrasound Q. 2013 Mar. doi: 10.1097/RUQ.0b013e3182814d9b.
5. Ultrasound Obstet Gynecol. 2008 Jun. doi: 10.1002/uog.5365.
Ovarian masses are common in women of all ages. It is important not to miss even one ovarian cancer, but we must also identify masses that will resolve on their own over time to avoid overtreatment. These concurrent goals of excluding malignancy while not overtreating patients are the basis for management of the pelvic mass. Additionally, fertility preservation is important when surgery is performed in a reproductive-aged woman.
An ovarian mass may be anything from a simple functional or physiologic cyst to an endometrioma to an epithelial carcinoma, a germ-cell tumor, or a stromal tumor (the latter three of which may metastasize). Across the general population, women have a 5%-10% lifetime risk of needing surgery for a suspected ovarian mass and a 1.4% (1 in 70) risk that this mass is cancerous. The majority of ovarian cysts or masses therefore are benign.
A thorough history – including family history – and physical examination with appropriate laboratory testing and directed imaging are important first steps for the ob.gyn. Fortunately, we have guidelines and criteria governing not only when observation or surgery is warranted but also when patients should be referred to a gynecologic oncologist. By following these guidelines,1 we are able to achieve the best outcomes.
Transvaginal ultrasound
A 2007 groundbreaking study led by Barbara Goff, MD, demonstrated that there are warning signs for ovarian cancer – symptoms that are significantly associated with malignancy. Dr. Goff and her coinvestigators evaluated the charts of hundreds of patients, including about 150 with ovarian cancer, and found that pelvic/abdominal pressure or pain, bloating, increase in abdominal size, and difficulty eating or feeling full were significantly and independently associated with cancer if these symptoms were present for less than a year and occurred at least 12 times per month.2
A pelvic examination is an integral part of evaluating every patient who has such concerns. That said, pelvic exams have limited ability to identify adnexal masses, especially in women who are obese – and that’s where imaging becomes especially important.
Masses generally can be considered simple or complex based on their appearance. A simple cyst is fluid-filled with thin, smooth walls and the absence of solid components or septations; it is significantly more likely to resolve on its own and is less likely to imply malignancy than a complex cyst, especially in a premenopausal woman. A complex cyst is multiseptated and/or solid – possibly with papillary projections – and is more concerning, especially if there is increased, new vascularity. Making this distinction helps us determine the risk of malignancy.
Transvaginal ultrasound (TVUS) is the preferred method for imaging, and our threshold for obtaining a TVUS should be very low. Women who have symptoms or concerns that can’t be attributed to a particular condition, and women in whom a mass can be palpated (even if asymptomatic) should have a TVUS. The imaging modality is cost effective and well tolerated by patients, does not expose the patient to ionizing radiation, and should generally be considered first-line imaging.3,4
Size is not predictive of malignancy, but it is important for determining whether surgery is warranted. In our experience, a mass of 8-10 cm or larger on TVUS is at risk of torsion and is unlikely to resolve on its own, even in a premenopausal woman. While large masses generally require surgery, patients of any age who have simple cysts smaller than 8-10 cm generally can be followed with serial exams and ultrasound; spontaneous regression is common.
Doppler ultrasonography is useful for evaluating blood flow in and around an ovarian mass and can be helpful for confirming suspected characteristics of a mass.
Recent studies from the radiology community have looked at the utility of the resistive index – a measure of the impedance and velocity of blood flow – as a predictor of ovarian malignancy. However, we caution against using Doppler to determine whether a mass is benign or malignant, or to determine the necessity of surgery. An abnormal ovary may have what is considered to be a normal resistive index, and the resistive index of a normal ovary may fall within the abnormal range. Doppler flow can be helpful, but it must be combined with other predictive features, like solid components with flow or papillary projections within a cyst, to define a decision about surgery.4,5
Magnetic resonance imaging can be useful in differentiating a fibroid from an ovarian mass, and a CT scan can be helpful in looking for disseminated disease when ovarian cancer is suspected based on ultrasound imaging, physical and history, and serum markers. A CT is useful, for instance, in a patient whose ovary is distended with ascites or who has upper abdominal complaints and a complex cyst. CT, PET, and MRI are not recommended in the initial evaluation of an ovarian mass.
The utility of serum biomarkers
Cancer antigen 125 (CA-125) testing may be helpful – in combination with other findings – for decision-making regarding the likelihood of malignancy and the need to refer patients. CA-125 is like Doppler in that a normal CA-125 cannot eliminate the possibility of cancer, and an abnormal CA-125 does not in and of itself imply malignancy. It’s far from a perfect cancer screening test.
CA-125 is a protein associated with epithelial ovarian malignancies, the type of ovarian cancer most commonly seen in postmenopausal women with genetic predispositions. Its specificity and positive predictive value are much higher in postmenopausal women than in average-risk premenopausal women (those without a family history or a known mutation that predisposes them to ovarian cancer). Levels of the marker are elevated in association with many nonmalignant conditions in premenopausal women – endometriosis, fibroids, and various inflammatory conditions, for instance – so the marker’s utility in this population is limited.
For women who have a family history of ovarian cancer or a known breast cancer gene 1 (BRCA1) or BRCA2 mutation, there are some data that suggest that monitoring with CA-125 measurements and TVUS may be a good approach to following patients prior to the age at which risk-reducing surgery can best be performed.
In an adolescent girl or a woman of reproductive age, we think less about epithelial cancer and more about germ-cell and stromal tumors. When a solid mass is palpated or visualized on imaging, we therefore will utilize a different set of markers; alpha-fetoprotein, L-lactate dehydrogenase, and beta-HCG, for instance, have much higher specificity than CA-125 does for germ-cell tumors in this age group and may be helpful in the evaluation. Similarly, in cases of a very large mass resembling a mucinous tumor, a carcinoembryonic antigen may be helpful.
A number of proprietary profiling technologies have been developed to determine the risk of a diagnosed mass being malignant. For instance, the OVA1 assay looks at five serum markers and scores the results, and the Risk of Ovarian Malignancy Algorithm (ROMA) combines the results of three serum markers with menopausal status into a numerical score. Both have Food and Drug Administration approval for use in women in whom surgery has been deemed necessary. These panels can be fairly predictive of risk and may be helpful – especially in rural areas – in determining which women should be referred to a gynecologic oncologist for surgery.
It is important to appreciate that an ovarian cyst or mass should never be biopsied or aspirated lest a malignant tumor confined to one ovary be potentially spread to the peritoneum.
Referral to a gynecologic oncologist
Postmenopausal women with a CA-125 greater than 35 U/mL should be referred, as should postmenopausal women with ascites, those with a nodular or fixed pelvic mass, and those with suspected abdominal or distant metastases (per a CT scan, for instance).
In premenopausal women, ascites, a nodular or fixed mass, and evidence of metastases also are reasons for referral to a gynecologic oncologist. CA-125, again, is much more likely to be elevated for reasons other than malignancy and therefore is not as strong a driver for referral as in postmenopausal women. Patients with markedly elevated levels, however, should probably be referred – particularly when other clinical factors also suggest the need for consultation. While there is no evidence-based threshold for CA-125 in premenopausal women, a CA-125 greater than 200 U/mL is a good cutoff for referral.
For any patient, family history of breast and/or ovarian cancer – especially in a first-degree relative – raises the risk of malignancy and should figure prominently into decision-making regarding referral. Criteria for referral are among the points discussed in the ACOG 2016 Practice Bulletin on Evaluation and Management of Adnexal Masses.1
A note on BRCA mutations
As the American College of Obstetricians and Gynecologists says in its practice bulletin, the most important personal risk factor for ovarian cancer is a strong family history of breast or ovarian cancer. Women with such a family history can undergo genetic testing for BRCA mutations and have the opportunity to prevent ovarian cancers when mutations are detected. This simple blood test can save lives.
A modeling study we recently completed – not yet published – shows that it actually would be cost effective to do population screening with BRCA testing performed on every woman at age 30 years.
According to the National Cancer Institute website (last review: 2018), it is estimated that about 44% of women who inherit a BRCA1 mutation, and about 17% of those who inherit a BRAC2 mutation, will develop ovarian cancer by the age of 80 years. By identifying those mutations, women may undergo risk-reducing surgery at designated ages after childbearing is complete and bring their risk down to under 5%.
An international take on managing adnexal masses
- Pelvic ultrasound should include the transvaginal approach. Use Doppler imaging as indicated.
- Although simple ovarian cysts are not precursor lesions to a malignant ovarian cancer, perform a high-quality examination to make sure there are no solid/papillary structures before classifying a cyst as a simple cyst. The risk of progression to malignancy is extremely low, but some follow-up is prudent.
- The most accurate method of characterizing an ovarian mass currently is real-time pattern recognition sonography in the hands of an experienced imager.
- Pattern recognition sonography or a risk model such as the International Ovarian Tumor Analysis (IOTA) Simple Rules can be used to initially characterize an ovarian mass.
- When an ovarian lesion is classified as benign, the patient may be followed conservatively, or if indicated, surgery can be performed by a general gynecologist.
- Serial sonography can be beneficial, but there are limited prospective data to support an exact interval and duration.
- Fewer surgical interventions may result in an increase in sonographic surveillance.
- When an ovarian lesion is considered indeterminate on initial sonography, and after appropriate clinical evaluation, a “second-step” evaluation may include referral to an expert sonologist, serial sonography, application of established risk-prediction models, correlation with serum biomarkers, correlation with MRI, or referral to a gynecologic oncologist for further evaluation.
From the First International Consensus Report on Adnexal Masses: Management Recommendations
Source: Glanc P et al. J Ultrasound Med. 2017 May;36(5):849-63.
Dr. Brown reported that she had received an earlier grant from Aspira Labs, the company that developed the OVA1 assay. Dr. Miller reported that he has no relevant financial disclosures.
References
1. Obstet Gynecol. 2016 Nov. doi: 10.1097/AOG.0000000000001768.
2. Cancer. 2007 Jan 15. doi: 10.1002/cncr.22371.
3. Clin Obstet Gynecol. 2015 Mar. doi: 10.1097/GRF.0000000000000083.
4. Ultrasound Q. 2013 Mar. doi: 10.1097/RUQ.0b013e3182814d9b.
5. Ultrasound Obstet Gynecol. 2008 Jun. doi: 10.1002/uog.5365.
Colorism can lead to intrafamily conflict
The color hue of a person’s skin is the most obvious criteria for society to judge a person and has always been deeply rooted in racism. Discrimination based on skin color is called colorism and is usually meted out by members of the same race and in the same family. The general belief is that someone with a lighter complexion is more beautiful, intelligent, or valuable than someone with a darker complexion. The term colorism can be widely applied in our assessment of conflict within families and society. The following case example gives guidance for psychiatrists faced with a family where colorism fuels family conflict.
Meeting the family
The Jaspers, a Black family, arrive at the psychiatrist’s office. They come in and look around before they choose their seats. Dr. Sally watches who sits next to whom and how they organize themselves in the office. After brief introductions, Mr. Jaspers begins, explaining why they are there.
“We are always fighting. We need this to stop. She, my wife, contradicts me all the time. Our kids are getting frustrated, and Bruce is acting out in school. He got in a fight again last week.”
Everyone looks at Bruce. He is darker skinned than the other siblings and carries all the African features in a family that favors the lighter end of the color spectrum. He sits next to his mother who leans into him. Mrs. Jaspers speaks next.
“Bruce gets picked on in school.”
Mr. Jaspers responds, “Well, if you didn’t run in there all the time and take him out, maybe he would learn how to deal with it better!”
“But they are mistreating him,” Mrs. Jaspers says.
The other children look away and play with their phones. Dr. Sally wonders whether this is a pattern: The parents fighting about how to deal with Bruce and his difficulties in the world – and the other siblings getting ignored and not included.
Dr. Sally asks Mrs. Jaspers for more details. She tells a narrative that is a strong thread in this family’s story.
“As you can see, Bruce is darker than the rest of our children. When we see the rest of our family, they all comment on what good skin and light coloring and good hair the other children have. Bruce just sits there. He is always being left out. He doesn’t speak up for himself. Maybe they think he can’t hear them, but I know he does and it affects him. They say the others are more intelligent, but I don’t think that is true. Bruce just gets picked on in school and he doesn’t feel like he matters. He doesn’t say anything, so maybe people think he doesn’t care, but I know he does.”
Dr. Sally turns to Bruce, who is still sitting silently next to his mother, his head down.
“Bruce, what do you have to say?”
Bruce shrugs his shoulders. His siblings still do not want to be drawn in and are otherwise occupied.
At this point, Dr. Sally might be thinking that she could see Bruce alone to assess his depression/self-esteem and maybe find ways to try to build him up. She does not want this to be an opportunity wasted. The goal is to work with the family to get Bruce where he needs to be faster and help the whole family.
Dr. Sally presses on. “Mr. Jaspers, what is your opinion?”
“She babies him. She treats him differently from the other kids. She is driving a wedge between him and his siblings. We fight about it all the time. She is driving a wedge between us, too.”
Mrs. Jaspers jumps in: “But you don’t know what it is like! When I was the only Black person in math class, I got picked on all the time! It made me self-conscious, and I couldn’t do my work. “
The other siblings look up briefly then back down at their devices. Dr. Sally asks them as a group:
“Can I ask you a question as a family? Can I ask the children a question?” They look up again. “Is this what goes on at home?” They all nod but offer no details.
Dr. Sally asks the oldest: “How does this affect your relationship with Bruce?”
They all look back and forth at each other. There is another long silence.
“See!” says Mr. Jaspers! “You can't protect him forever, and you are just ostracizing him from the rest of us! “
“But, but, he, he needs to learn different things. He is different. He faces different struggles. The police will stop him more. I am afraid for him.” Mrs. Jaspers starts to cry.
“You can’t protect him forever,” says her husband, gently reaching over to her.
Bruce has psychologically disappeared from the room, hiding behind his mother, who is now the largest and neediest presence in the room. Mr. Jaspers looks at Dr. Sally helplessly.
Dr. Sally asks the important question to the whole family.
“How do you all think this should work? If you don’t think Mrs. Jaspers is right, what do you think should be the way forward?”
This question is the turning point and indicates that Dr. Sally sees that the solution lies in how the family wants to manage things.
“I believe that your whole family has the answers, that you all have thought through this situation much more deeply and for much longer than I have. I am just hearing about it, and I am White and don’t have this experience. I have faith in your family, that with an opportunity to openly discuss this issue, that this knot can be unraveled. It does not mean that there are not more knots to unravel. For today, how to help you all help Bruce, is the work."
Dr. Sally talks to everyone but finishes up by looking at Mr. Jaspers, who has indicated that Bruce is part of the family and should not be treated differently from the other children.
Sean, the oldest sibling, now pipes up: “Bruce gets everything he wants. Mum spoils him; she always takes his side if there are arguments. Bruce knows this, and he steals our stuff because he knows he will get away with it.”
Bruce is quiet and leans in more to his mother. Dr. Sally motions to the mother not to speak.
“Is this true, Bruce?” Silence speaks that the answer is yes. The disparities in the family are aired for a while longer.
“Mrs. Jaspers, it is now your turn to respond.”
“Bruce is darker and faces more challenges than the others; he needs more protection and to know that he is loved.”
“Your family seems to think otherwise. They seem to think that your protection, while admirable, needs to be tempered to allow him to grow into a man who can stand on his own feet.”
Dr. Sally guides the family as a whole to a place where they can agree on the problem. The problem is now framed as a mother who cares too much and is too protective of Bruce but now her love and care need to be tempered. As a mother, she feels that it is her duty to protect her most vulnerable son. The family knows that Bruce will face more social scrutiny than the others, that he will have more internal struggles with self-worth than the others. How can the family help?
This conceptualization causes the family to look searchingly at one another. It is nothing they haven’t thought about privately, but this is the first time they are together thinking about it.
Dr. Sally says that she can help by providing time and space for them to wok through this together. They all agree to come back the following week with some thoughts about moving forward.
Offering perspective on colorism
In her book “Facing the Black Shadow,” couples and family therapist Marlene F. Watson, PhD, discusses colorism.
“African Americans still have a tough time talking about slavery – the origin of colorism. Seriously, what can we really expect to change without acknowledging and challenging the psychological residuals of slavery in our families and communities? What doesn’t get resolved in one generation is passed on to the next so our issues from slavery go from one generation to the next.”
Dr. Watson continues: “Confronting the secret about skin color in our families and communities is necessary for all Black girls to feel lovable, worthy, and deserving of care and for all Black boys to feel their value lies within them, not a dark, light, bright, near-white or White woman. African Americans need to get that preferring light over dark or dark over light is problematic for all of us. Skin color preferences in the African American community follow society’s racial hierarchy. African Americans as a group are at the bottom in the larger society and dark-skinned African Americans are at the bottom in the Black community.”
and patterns about skin color. Her advice is to ask each family member, from oldest to youngest, to identify the spoken and unspoken skin color beliefs he or she experiences in the family. Ask about skin color beliefs from outside that affect family members, and what each person thinks the family could do to stop promoting the “less than/better than” mentality that is often present with skin color assignment.
Thank you to Lynette Ramsingh Barros, who collaborated on creating the case.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest.
The color hue of a person’s skin is the most obvious criteria for society to judge a person and has always been deeply rooted in racism. Discrimination based on skin color is called colorism and is usually meted out by members of the same race and in the same family. The general belief is that someone with a lighter complexion is more beautiful, intelligent, or valuable than someone with a darker complexion. The term colorism can be widely applied in our assessment of conflict within families and society. The following case example gives guidance for psychiatrists faced with a family where colorism fuels family conflict.
Meeting the family
The Jaspers, a Black family, arrive at the psychiatrist’s office. They come in and look around before they choose their seats. Dr. Sally watches who sits next to whom and how they organize themselves in the office. After brief introductions, Mr. Jaspers begins, explaining why they are there.
“We are always fighting. We need this to stop. She, my wife, contradicts me all the time. Our kids are getting frustrated, and Bruce is acting out in school. He got in a fight again last week.”
Everyone looks at Bruce. He is darker skinned than the other siblings and carries all the African features in a family that favors the lighter end of the color spectrum. He sits next to his mother who leans into him. Mrs. Jaspers speaks next.
“Bruce gets picked on in school.”
Mr. Jaspers responds, “Well, if you didn’t run in there all the time and take him out, maybe he would learn how to deal with it better!”
“But they are mistreating him,” Mrs. Jaspers says.
The other children look away and play with their phones. Dr. Sally wonders whether this is a pattern: The parents fighting about how to deal with Bruce and his difficulties in the world – and the other siblings getting ignored and not included.
Dr. Sally asks Mrs. Jaspers for more details. She tells a narrative that is a strong thread in this family’s story.
“As you can see, Bruce is darker than the rest of our children. When we see the rest of our family, they all comment on what good skin and light coloring and good hair the other children have. Bruce just sits there. He is always being left out. He doesn’t speak up for himself. Maybe they think he can’t hear them, but I know he does and it affects him. They say the others are more intelligent, but I don’t think that is true. Bruce just gets picked on in school and he doesn’t feel like he matters. He doesn’t say anything, so maybe people think he doesn’t care, but I know he does.”
Dr. Sally turns to Bruce, who is still sitting silently next to his mother, his head down.
“Bruce, what do you have to say?”
Bruce shrugs his shoulders. His siblings still do not want to be drawn in and are otherwise occupied.
At this point, Dr. Sally might be thinking that she could see Bruce alone to assess his depression/self-esteem and maybe find ways to try to build him up. She does not want this to be an opportunity wasted. The goal is to work with the family to get Bruce where he needs to be faster and help the whole family.
Dr. Sally presses on. “Mr. Jaspers, what is your opinion?”
“She babies him. She treats him differently from the other kids. She is driving a wedge between him and his siblings. We fight about it all the time. She is driving a wedge between us, too.”
Mrs. Jaspers jumps in: “But you don’t know what it is like! When I was the only Black person in math class, I got picked on all the time! It made me self-conscious, and I couldn’t do my work. “
The other siblings look up briefly then back down at their devices. Dr. Sally asks them as a group:
“Can I ask you a question as a family? Can I ask the children a question?” They look up again. “Is this what goes on at home?” They all nod but offer no details.
Dr. Sally asks the oldest: “How does this affect your relationship with Bruce?”
They all look back and forth at each other. There is another long silence.
“See!” says Mr. Jaspers! “You can't protect him forever, and you are just ostracizing him from the rest of us! “
“But, but, he, he needs to learn different things. He is different. He faces different struggles. The police will stop him more. I am afraid for him.” Mrs. Jaspers starts to cry.
“You can’t protect him forever,” says her husband, gently reaching over to her.
Bruce has psychologically disappeared from the room, hiding behind his mother, who is now the largest and neediest presence in the room. Mr. Jaspers looks at Dr. Sally helplessly.
Dr. Sally asks the important question to the whole family.
“How do you all think this should work? If you don’t think Mrs. Jaspers is right, what do you think should be the way forward?”
This question is the turning point and indicates that Dr. Sally sees that the solution lies in how the family wants to manage things.
“I believe that your whole family has the answers, that you all have thought through this situation much more deeply and for much longer than I have. I am just hearing about it, and I am White and don’t have this experience. I have faith in your family, that with an opportunity to openly discuss this issue, that this knot can be unraveled. It does not mean that there are not more knots to unravel. For today, how to help you all help Bruce, is the work."
Dr. Sally talks to everyone but finishes up by looking at Mr. Jaspers, who has indicated that Bruce is part of the family and should not be treated differently from the other children.
Sean, the oldest sibling, now pipes up: “Bruce gets everything he wants. Mum spoils him; she always takes his side if there are arguments. Bruce knows this, and he steals our stuff because he knows he will get away with it.”
Bruce is quiet and leans in more to his mother. Dr. Sally motions to the mother not to speak.
“Is this true, Bruce?” Silence speaks that the answer is yes. The disparities in the family are aired for a while longer.
“Mrs. Jaspers, it is now your turn to respond.”
“Bruce is darker and faces more challenges than the others; he needs more protection and to know that he is loved.”
“Your family seems to think otherwise. They seem to think that your protection, while admirable, needs to be tempered to allow him to grow into a man who can stand on his own feet.”
Dr. Sally guides the family as a whole to a place where they can agree on the problem. The problem is now framed as a mother who cares too much and is too protective of Bruce but now her love and care need to be tempered. As a mother, she feels that it is her duty to protect her most vulnerable son. The family knows that Bruce will face more social scrutiny than the others, that he will have more internal struggles with self-worth than the others. How can the family help?
This conceptualization causes the family to look searchingly at one another. It is nothing they haven’t thought about privately, but this is the first time they are together thinking about it.
Dr. Sally says that she can help by providing time and space for them to wok through this together. They all agree to come back the following week with some thoughts about moving forward.
Offering perspective on colorism
In her book “Facing the Black Shadow,” couples and family therapist Marlene F. Watson, PhD, discusses colorism.
“African Americans still have a tough time talking about slavery – the origin of colorism. Seriously, what can we really expect to change without acknowledging and challenging the psychological residuals of slavery in our families and communities? What doesn’t get resolved in one generation is passed on to the next so our issues from slavery go from one generation to the next.”
Dr. Watson continues: “Confronting the secret about skin color in our families and communities is necessary for all Black girls to feel lovable, worthy, and deserving of care and for all Black boys to feel their value lies within them, not a dark, light, bright, near-white or White woman. African Americans need to get that preferring light over dark or dark over light is problematic for all of us. Skin color preferences in the African American community follow society’s racial hierarchy. African Americans as a group are at the bottom in the larger society and dark-skinned African Americans are at the bottom in the Black community.”
and patterns about skin color. Her advice is to ask each family member, from oldest to youngest, to identify the spoken and unspoken skin color beliefs he or she experiences in the family. Ask about skin color beliefs from outside that affect family members, and what each person thinks the family could do to stop promoting the “less than/better than” mentality that is often present with skin color assignment.
Thank you to Lynette Ramsingh Barros, who collaborated on creating the case.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest.
The color hue of a person’s skin is the most obvious criteria for society to judge a person and has always been deeply rooted in racism. Discrimination based on skin color is called colorism and is usually meted out by members of the same race and in the same family. The general belief is that someone with a lighter complexion is more beautiful, intelligent, or valuable than someone with a darker complexion. The term colorism can be widely applied in our assessment of conflict within families and society. The following case example gives guidance for psychiatrists faced with a family where colorism fuels family conflict.
Meeting the family
The Jaspers, a Black family, arrive at the psychiatrist’s office. They come in and look around before they choose their seats. Dr. Sally watches who sits next to whom and how they organize themselves in the office. After brief introductions, Mr. Jaspers begins, explaining why they are there.
“We are always fighting. We need this to stop. She, my wife, contradicts me all the time. Our kids are getting frustrated, and Bruce is acting out in school. He got in a fight again last week.”
Everyone looks at Bruce. He is darker skinned than the other siblings and carries all the African features in a family that favors the lighter end of the color spectrum. He sits next to his mother who leans into him. Mrs. Jaspers speaks next.
“Bruce gets picked on in school.”
Mr. Jaspers responds, “Well, if you didn’t run in there all the time and take him out, maybe he would learn how to deal with it better!”
“But they are mistreating him,” Mrs. Jaspers says.
The other children look away and play with their phones. Dr. Sally wonders whether this is a pattern: The parents fighting about how to deal with Bruce and his difficulties in the world – and the other siblings getting ignored and not included.
Dr. Sally asks Mrs. Jaspers for more details. She tells a narrative that is a strong thread in this family’s story.
“As you can see, Bruce is darker than the rest of our children. When we see the rest of our family, they all comment on what good skin and light coloring and good hair the other children have. Bruce just sits there. He is always being left out. He doesn’t speak up for himself. Maybe they think he can’t hear them, but I know he does and it affects him. They say the others are more intelligent, but I don’t think that is true. Bruce just gets picked on in school and he doesn’t feel like he matters. He doesn’t say anything, so maybe people think he doesn’t care, but I know he does.”
Dr. Sally turns to Bruce, who is still sitting silently next to his mother, his head down.
“Bruce, what do you have to say?”
Bruce shrugs his shoulders. His siblings still do not want to be drawn in and are otherwise occupied.
At this point, Dr. Sally might be thinking that she could see Bruce alone to assess his depression/self-esteem and maybe find ways to try to build him up. She does not want this to be an opportunity wasted. The goal is to work with the family to get Bruce where he needs to be faster and help the whole family.
Dr. Sally presses on. “Mr. Jaspers, what is your opinion?”
“She babies him. She treats him differently from the other kids. She is driving a wedge between him and his siblings. We fight about it all the time. She is driving a wedge between us, too.”
Mrs. Jaspers jumps in: “But you don’t know what it is like! When I was the only Black person in math class, I got picked on all the time! It made me self-conscious, and I couldn’t do my work. “
The other siblings look up briefly then back down at their devices. Dr. Sally asks them as a group:
“Can I ask you a question as a family? Can I ask the children a question?” They look up again. “Is this what goes on at home?” They all nod but offer no details.
Dr. Sally asks the oldest: “How does this affect your relationship with Bruce?”
They all look back and forth at each other. There is another long silence.
“See!” says Mr. Jaspers! “You can't protect him forever, and you are just ostracizing him from the rest of us! “
“But, but, he, he needs to learn different things. He is different. He faces different struggles. The police will stop him more. I am afraid for him.” Mrs. Jaspers starts to cry.
“You can’t protect him forever,” says her husband, gently reaching over to her.
Bruce has psychologically disappeared from the room, hiding behind his mother, who is now the largest and neediest presence in the room. Mr. Jaspers looks at Dr. Sally helplessly.
Dr. Sally asks the important question to the whole family.
“How do you all think this should work? If you don’t think Mrs. Jaspers is right, what do you think should be the way forward?”
This question is the turning point and indicates that Dr. Sally sees that the solution lies in how the family wants to manage things.
“I believe that your whole family has the answers, that you all have thought through this situation much more deeply and for much longer than I have. I am just hearing about it, and I am White and don’t have this experience. I have faith in your family, that with an opportunity to openly discuss this issue, that this knot can be unraveled. It does not mean that there are not more knots to unravel. For today, how to help you all help Bruce, is the work."
Dr. Sally talks to everyone but finishes up by looking at Mr. Jaspers, who has indicated that Bruce is part of the family and should not be treated differently from the other children.
Sean, the oldest sibling, now pipes up: “Bruce gets everything he wants. Mum spoils him; she always takes his side if there are arguments. Bruce knows this, and he steals our stuff because he knows he will get away with it.”
Bruce is quiet and leans in more to his mother. Dr. Sally motions to the mother not to speak.
“Is this true, Bruce?” Silence speaks that the answer is yes. The disparities in the family are aired for a while longer.
“Mrs. Jaspers, it is now your turn to respond.”
“Bruce is darker and faces more challenges than the others; he needs more protection and to know that he is loved.”
“Your family seems to think otherwise. They seem to think that your protection, while admirable, needs to be tempered to allow him to grow into a man who can stand on his own feet.”
Dr. Sally guides the family as a whole to a place where they can agree on the problem. The problem is now framed as a mother who cares too much and is too protective of Bruce but now her love and care need to be tempered. As a mother, she feels that it is her duty to protect her most vulnerable son. The family knows that Bruce will face more social scrutiny than the others, that he will have more internal struggles with self-worth than the others. How can the family help?
This conceptualization causes the family to look searchingly at one another. It is nothing they haven’t thought about privately, but this is the first time they are together thinking about it.
Dr. Sally says that she can help by providing time and space for them to wok through this together. They all agree to come back the following week with some thoughts about moving forward.
Offering perspective on colorism
In her book “Facing the Black Shadow,” couples and family therapist Marlene F. Watson, PhD, discusses colorism.
“African Americans still have a tough time talking about slavery – the origin of colorism. Seriously, what can we really expect to change without acknowledging and challenging the psychological residuals of slavery in our families and communities? What doesn’t get resolved in one generation is passed on to the next so our issues from slavery go from one generation to the next.”
Dr. Watson continues: “Confronting the secret about skin color in our families and communities is necessary for all Black girls to feel lovable, worthy, and deserving of care and for all Black boys to feel their value lies within them, not a dark, light, bright, near-white or White woman. African Americans need to get that preferring light over dark or dark over light is problematic for all of us. Skin color preferences in the African American community follow society’s racial hierarchy. African Americans as a group are at the bottom in the larger society and dark-skinned African Americans are at the bottom in the Black community.”
and patterns about skin color. Her advice is to ask each family member, from oldest to youngest, to identify the spoken and unspoken skin color beliefs he or she experiences in the family. Ask about skin color beliefs from outside that affect family members, and what each person thinks the family could do to stop promoting the “less than/better than” mentality that is often present with skin color assignment.
Thank you to Lynette Ramsingh Barros, who collaborated on creating the case.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest.
Molecular developments in treatment of UPSC
Uterine papillary serous carcinoma (UPSC) is an infrequent but deadly form of endometrial cancer comprising 10% of cases but contributing 40% of deaths from the disease. Recurrence rates are high for this disease. Five-year survival is 55% for all patients and only 70% for stage I disease.1 Patterns of recurrence tend to be distant (extrapelvic and extraabdominal) as frequently as they are localized to the pelvis, and metastases and recurrences are unrelated to the extent of uterine disease (such as myometrial invasion). It is for these reasons that the recommended course of adjuvant therapy for this disease is systemic therapy (typically six doses of carboplatin and paclitaxel chemotherapy) with consideration for radiation to the vagina or pelvis to consolidate pelvic and vaginal control.2 This differs from early-stage high/intermediate–risk endometrioid adenocarcinomas, for which adjuvant chemotherapy has not been found to be helpful.
Because of the lower incidence of UPSC, it frequently has been studied alongside endometrioid cell types in clinical trials which explore novel adjuvant therapies. However, UPSC is biologically distinct from endometrioid endometrial cancers, which likely results in inferior clinical responses to conventional interventions. Fortunately we are beginning to better understand UPSC at a molecular level, and advancements are being made in the targeted therapies for these patients that are unique, compared with those applied to other cancer subtypes.
As discussed above, UPSC is a particularly aggressive form of uterine cancer. Histologically it is characterized by a precursor lesion of endometrial glandular dysplasia progressing to endometrial intraepithelial neoplasia (EIC). Histologically it presents with a highly atypical slit-like glandular configuration, which appears similar to serous carcinomas of the fallopian tube and ovary. Molecularly these tumors commonly manifest mutations in tumor protein p53 (TP53) and phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA), which are both genes associated with oncogenic potential.1 While most UPSC tumors have loss of expression in hormone receptors such as estrogen and progesterone, 25%-30% of cases overexpress the tyrosine kinase receptor human epidermal growth factor receptor 2 (HER2).3-5 This has proven to provide an exciting target for therapeutic interventions.
A target for therapeutic intervention
HER2 is a transmembrane receptor which, when activated, signals complex downstream pathways responsible for cellular proliferation, dedifferentiation, and metastasis. In a recent multi-institutional analysis of early-stage UPSC, HER2 overexpression was identified among 25% of cases.4 Approximately 30% of cases of advanced disease manifest overexpression of this biomarker.5 HER2 overexpression (HER2-positive status) is significantly associated with higher rates of recurrence and mortality, even among patients treated with conventional therapies.3 Thus HER2-positive status is obviously an indicator of particularly aggressive disease.
Fortunately this particular biomarker is one for which we have established and developing therapeutics. The humanized monoclonal antibody, trastuzumab, has been highly effective in improving survival for HER2-positive breast cancer.6 More recently, it was studied in a phase 2 trial with carboplatin and paclitaxel chemotherapy for advanced or recurrent HER2-positive UPSC.5 This trial showed that the addition of this targeted therapy to conventional chemotherapy improved recurrence-free survival from 8 months to 12 months, and improved overall survival from 24.4 months to 29.6 months.5
One discovery leads to another treatment
This discovery led to the approval of trastuzumab to be used in addition to chemotherapy for advanced or recurrent disease.2 The most significant effects appear to be among those who have not received prior therapies, with a doubling of progression-free survival among these patients, and a more modest response among patients treated for recurrent, mostly pretreated disease.
Work currently is underway to explore an array of antibody or small-molecule blockades of HER2 in addition to vaccines against the protein or treatment with conjugate compounds in which an antibody to HER2 is paired with a cytotoxic drug able to be internalized into HER2-expressing cells.7 This represents a form of personalized medicine referred to as biomarker-driven targeted therapy, in which therapies are prescribed based on the expression of specific molecular markers (such as HER2 expression) typically in combination with other clinical markers such as surgical staging results, race, age, etc. These approaches can be very effective strategies in rare tumor subtypes with distinct molecular and clinical behaviors.
As previously mentioned, the targeting of HER2 overexpression with trastuzumab has been shown to be highly effective in the treatment of HER2-positive breast cancers where even patients with early-stage disease receive a multimodal therapy approach including antibody, chemotherapy, surgical, and often radiation treatments.6 We are moving towards a similar multimodal comprehensive treatment strategy for UPSC. If it is as successful as it is in breast cancer, it will be long overdue, and desperately necessary given the poor prognosis of this disease for all stages because of the inadequacies of current treatments strategies.
Routine testing of UPSC for HER2 expression is now a part of routine molecular substaging of uterine cancers in the same way we have embraced testing for microsatellite instability and hormone-receptor status. While a diagnosis of HER2 overexpression in UPSC portends a poor prognosis, patients can be reassured that treatment strategies exist that can target this malignant mechanism in advanced disease and more are under further development for early-stage disease.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Curr Opin Obstet Gynecol. 2010 Feb. doi: 10.1097/GCO.0b013e328334d8a3.
2. National Comprehensive Cancer Network. Uterine Neoplasms (version 2.2020).
3. Cancer 2005 Oct 1. doi: 10.1002/cncr.21308.
4. Gynecol Oncol 2020 doi: 10.1016/j.ygyno.2020.07.016.
5. J Clin Oncol 2018. doi: 10.1200/JCO.2017.76.5966.
6. N Engl J Med 2011. doi: 10.1056/NEJMoa0910383.
7. Discov Med. 2016 Apr;21(116):293-303.
Uterine papillary serous carcinoma (UPSC) is an infrequent but deadly form of endometrial cancer comprising 10% of cases but contributing 40% of deaths from the disease. Recurrence rates are high for this disease. Five-year survival is 55% for all patients and only 70% for stage I disease.1 Patterns of recurrence tend to be distant (extrapelvic and extraabdominal) as frequently as they are localized to the pelvis, and metastases and recurrences are unrelated to the extent of uterine disease (such as myometrial invasion). It is for these reasons that the recommended course of adjuvant therapy for this disease is systemic therapy (typically six doses of carboplatin and paclitaxel chemotherapy) with consideration for radiation to the vagina or pelvis to consolidate pelvic and vaginal control.2 This differs from early-stage high/intermediate–risk endometrioid adenocarcinomas, for which adjuvant chemotherapy has not been found to be helpful.
Because of the lower incidence of UPSC, it frequently has been studied alongside endometrioid cell types in clinical trials which explore novel adjuvant therapies. However, UPSC is biologically distinct from endometrioid endometrial cancers, which likely results in inferior clinical responses to conventional interventions. Fortunately we are beginning to better understand UPSC at a molecular level, and advancements are being made in the targeted therapies for these patients that are unique, compared with those applied to other cancer subtypes.
As discussed above, UPSC is a particularly aggressive form of uterine cancer. Histologically it is characterized by a precursor lesion of endometrial glandular dysplasia progressing to endometrial intraepithelial neoplasia (EIC). Histologically it presents with a highly atypical slit-like glandular configuration, which appears similar to serous carcinomas of the fallopian tube and ovary. Molecularly these tumors commonly manifest mutations in tumor protein p53 (TP53) and phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA), which are both genes associated with oncogenic potential.1 While most UPSC tumors have loss of expression in hormone receptors such as estrogen and progesterone, 25%-30% of cases overexpress the tyrosine kinase receptor human epidermal growth factor receptor 2 (HER2).3-5 This has proven to provide an exciting target for therapeutic interventions.
A target for therapeutic intervention
HER2 is a transmembrane receptor which, when activated, signals complex downstream pathways responsible for cellular proliferation, dedifferentiation, and metastasis. In a recent multi-institutional analysis of early-stage UPSC, HER2 overexpression was identified among 25% of cases.4 Approximately 30% of cases of advanced disease manifest overexpression of this biomarker.5 HER2 overexpression (HER2-positive status) is significantly associated with higher rates of recurrence and mortality, even among patients treated with conventional therapies.3 Thus HER2-positive status is obviously an indicator of particularly aggressive disease.
Fortunately this particular biomarker is one for which we have established and developing therapeutics. The humanized monoclonal antibody, trastuzumab, has been highly effective in improving survival for HER2-positive breast cancer.6 More recently, it was studied in a phase 2 trial with carboplatin and paclitaxel chemotherapy for advanced or recurrent HER2-positive UPSC.5 This trial showed that the addition of this targeted therapy to conventional chemotherapy improved recurrence-free survival from 8 months to 12 months, and improved overall survival from 24.4 months to 29.6 months.5
One discovery leads to another treatment
This discovery led to the approval of trastuzumab to be used in addition to chemotherapy for advanced or recurrent disease.2 The most significant effects appear to be among those who have not received prior therapies, with a doubling of progression-free survival among these patients, and a more modest response among patients treated for recurrent, mostly pretreated disease.
Work currently is underway to explore an array of antibody or small-molecule blockades of HER2 in addition to vaccines against the protein or treatment with conjugate compounds in which an antibody to HER2 is paired with a cytotoxic drug able to be internalized into HER2-expressing cells.7 This represents a form of personalized medicine referred to as biomarker-driven targeted therapy, in which therapies are prescribed based on the expression of specific molecular markers (such as HER2 expression) typically in combination with other clinical markers such as surgical staging results, race, age, etc. These approaches can be very effective strategies in rare tumor subtypes with distinct molecular and clinical behaviors.
As previously mentioned, the targeting of HER2 overexpression with trastuzumab has been shown to be highly effective in the treatment of HER2-positive breast cancers where even patients with early-stage disease receive a multimodal therapy approach including antibody, chemotherapy, surgical, and often radiation treatments.6 We are moving towards a similar multimodal comprehensive treatment strategy for UPSC. If it is as successful as it is in breast cancer, it will be long overdue, and desperately necessary given the poor prognosis of this disease for all stages because of the inadequacies of current treatments strategies.
Routine testing of UPSC for HER2 expression is now a part of routine molecular substaging of uterine cancers in the same way we have embraced testing for microsatellite instability and hormone-receptor status. While a diagnosis of HER2 overexpression in UPSC portends a poor prognosis, patients can be reassured that treatment strategies exist that can target this malignant mechanism in advanced disease and more are under further development for early-stage disease.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Curr Opin Obstet Gynecol. 2010 Feb. doi: 10.1097/GCO.0b013e328334d8a3.
2. National Comprehensive Cancer Network. Uterine Neoplasms (version 2.2020).
3. Cancer 2005 Oct 1. doi: 10.1002/cncr.21308.
4. Gynecol Oncol 2020 doi: 10.1016/j.ygyno.2020.07.016.
5. J Clin Oncol 2018. doi: 10.1200/JCO.2017.76.5966.
6. N Engl J Med 2011. doi: 10.1056/NEJMoa0910383.
7. Discov Med. 2016 Apr;21(116):293-303.
Uterine papillary serous carcinoma (UPSC) is an infrequent but deadly form of endometrial cancer comprising 10% of cases but contributing 40% of deaths from the disease. Recurrence rates are high for this disease. Five-year survival is 55% for all patients and only 70% for stage I disease.1 Patterns of recurrence tend to be distant (extrapelvic and extraabdominal) as frequently as they are localized to the pelvis, and metastases and recurrences are unrelated to the extent of uterine disease (such as myometrial invasion). It is for these reasons that the recommended course of adjuvant therapy for this disease is systemic therapy (typically six doses of carboplatin and paclitaxel chemotherapy) with consideration for radiation to the vagina or pelvis to consolidate pelvic and vaginal control.2 This differs from early-stage high/intermediate–risk endometrioid adenocarcinomas, for which adjuvant chemotherapy has not been found to be helpful.
Because of the lower incidence of UPSC, it frequently has been studied alongside endometrioid cell types in clinical trials which explore novel adjuvant therapies. However, UPSC is biologically distinct from endometrioid endometrial cancers, which likely results in inferior clinical responses to conventional interventions. Fortunately we are beginning to better understand UPSC at a molecular level, and advancements are being made in the targeted therapies for these patients that are unique, compared with those applied to other cancer subtypes.
As discussed above, UPSC is a particularly aggressive form of uterine cancer. Histologically it is characterized by a precursor lesion of endometrial glandular dysplasia progressing to endometrial intraepithelial neoplasia (EIC). Histologically it presents with a highly atypical slit-like glandular configuration, which appears similar to serous carcinomas of the fallopian tube and ovary. Molecularly these tumors commonly manifest mutations in tumor protein p53 (TP53) and phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA), which are both genes associated with oncogenic potential.1 While most UPSC tumors have loss of expression in hormone receptors such as estrogen and progesterone, 25%-30% of cases overexpress the tyrosine kinase receptor human epidermal growth factor receptor 2 (HER2).3-5 This has proven to provide an exciting target for therapeutic interventions.
A target for therapeutic intervention
HER2 is a transmembrane receptor which, when activated, signals complex downstream pathways responsible for cellular proliferation, dedifferentiation, and metastasis. In a recent multi-institutional analysis of early-stage UPSC, HER2 overexpression was identified among 25% of cases.4 Approximately 30% of cases of advanced disease manifest overexpression of this biomarker.5 HER2 overexpression (HER2-positive status) is significantly associated with higher rates of recurrence and mortality, even among patients treated with conventional therapies.3 Thus HER2-positive status is obviously an indicator of particularly aggressive disease.
Fortunately this particular biomarker is one for which we have established and developing therapeutics. The humanized monoclonal antibody, trastuzumab, has been highly effective in improving survival for HER2-positive breast cancer.6 More recently, it was studied in a phase 2 trial with carboplatin and paclitaxel chemotherapy for advanced or recurrent HER2-positive UPSC.5 This trial showed that the addition of this targeted therapy to conventional chemotherapy improved recurrence-free survival from 8 months to 12 months, and improved overall survival from 24.4 months to 29.6 months.5
One discovery leads to another treatment
This discovery led to the approval of trastuzumab to be used in addition to chemotherapy for advanced or recurrent disease.2 The most significant effects appear to be among those who have not received prior therapies, with a doubling of progression-free survival among these patients, and a more modest response among patients treated for recurrent, mostly pretreated disease.
Work currently is underway to explore an array of antibody or small-molecule blockades of HER2 in addition to vaccines against the protein or treatment with conjugate compounds in which an antibody to HER2 is paired with a cytotoxic drug able to be internalized into HER2-expressing cells.7 This represents a form of personalized medicine referred to as biomarker-driven targeted therapy, in which therapies are prescribed based on the expression of specific molecular markers (such as HER2 expression) typically in combination with other clinical markers such as surgical staging results, race, age, etc. These approaches can be very effective strategies in rare tumor subtypes with distinct molecular and clinical behaviors.
As previously mentioned, the targeting of HER2 overexpression with trastuzumab has been shown to be highly effective in the treatment of HER2-positive breast cancers where even patients with early-stage disease receive a multimodal therapy approach including antibody, chemotherapy, surgical, and often radiation treatments.6 We are moving towards a similar multimodal comprehensive treatment strategy for UPSC. If it is as successful as it is in breast cancer, it will be long overdue, and desperately necessary given the poor prognosis of this disease for all stages because of the inadequacies of current treatments strategies.
Routine testing of UPSC for HER2 expression is now a part of routine molecular substaging of uterine cancers in the same way we have embraced testing for microsatellite instability and hormone-receptor status. While a diagnosis of HER2 overexpression in UPSC portends a poor prognosis, patients can be reassured that treatment strategies exist that can target this malignant mechanism in advanced disease and more are under further development for early-stage disease.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Curr Opin Obstet Gynecol. 2010 Feb. doi: 10.1097/GCO.0b013e328334d8a3.
2. National Comprehensive Cancer Network. Uterine Neoplasms (version 2.2020).
3. Cancer 2005 Oct 1. doi: 10.1002/cncr.21308.
4. Gynecol Oncol 2020 doi: 10.1016/j.ygyno.2020.07.016.
5. J Clin Oncol 2018. doi: 10.1200/JCO.2017.76.5966.
6. N Engl J Med 2011. doi: 10.1056/NEJMoa0910383.
7. Discov Med. 2016 Apr;21(116):293-303.
The joys of telemedicine
Another great morning,
Here goes. I’ll invite Gretchen by text: 617-555-5555. “TOO LONG.” How can 10 digits be too long? Trying again: 617-555-5555. “TOO LONG!” What the heck, let me leave off the last digit: 617-555-555. “TOO SHORT.”
Never mind, I’ll invite her by email.
Five minutes have gone by. Better call to see if she got the invite.
“Hello, is this Gretchen? Don’t hang up, I’m not a telemarketer! This is Dr. Rockoff. I sent you an invitation for our computer visit.
“You got it, great. Yes, you have to click on it to sign in. I know, your appointment’s at 8:30. It’s now 8:28. Let’s start early, why not?
“Hi, there! I can see you. Can you hear me? You’re nodding and your lips are moving. I can’t hear you. Did you enable your microphone?
“Nope, still can’t hear. I’ll call your cell, and we’ll talk that way.
“Yes, it’s me, Dr. Rockoff. What’s that? You enabled the microphone along with your video when you logged on? Well, there we go. How can I help today?
“You want a refill on your tretinoin gel for age management? Not a problem. Let’s see, you’ve been using it since 1996. No, you look great! Not a day over 76, really! I’ll have the staff escribe it right over.
“Okay, take care. Three years should be about right. Happy 80th!”
Wonder what happened there. Maybe things will go better for the next patient. Okay, I’m emailing an invite to Rob.
There he is! “Hi. Can you see me? Hear me? Nope, can’t hear you. Let me just call your cell.”
Okay, 972-555-5555. Ringing ... oh no, right to voicemail. “You have reached 972-555-5555. The mailbox is full and cannot accept messages. Please try some other time.”
“Okay, I’m back with you on the screen, Rob. Nope, still can’t hear you. I tried your cell but it went to voicemail. Yes, I see you’re holding the phone in your hand. Let me try you again.
“972-555-5555. Right to voicemail. Doesn’t your phone ring? You never make voice calls, only send texts? Look, please call me: 781-555-5555, write it down.
“Excellent, we’re in business. You’re worried about a mole that’s changing. You sent a photo to the office. Great, I’ll look right now on your record ... nope, not uploaded. Can you email me the photo? Please write down my email address: alanrockoffmdskincarespecialistist@myfabuloustelemedicineportal.now. Got that? Okay, please send the picture ...
“Returned as undeliverable? Show me what you typed ... Oh, wait. It’s ‘telemedicine,’ not ‘TellaMedicine.’ ” Yeah, that should do it.
“Okay, got the picture. You do fabulous super-closeups! Is that your navel next to it? Your left nostril? Okay. You tried to razor off the hair growing out it? Yes, that could account for the bleeding. Tell you what, go easy on it for the next 2 weeks, and send me another picture. Same email address.
“You have another question? Sure. You want a refill of your clindamycin gel because the tube from 2013 ran out? Guess you haven’t grown out of your acne yet. Sure, happy to send it in for you. Same pharmacy we have on file? You’re bunking with your parents in Wichita? No problem. Just need the pharmacy name and street. Boston, Wichita, whatever.
“Sure, happy to help. Enjoy your stay with your parents. You’ve been there 4 months? Are you cleaning your room? Mostly? Good. Take care. I’ll respond to your email in 2 weeks. Meantime, you might empty out your full voicemail box ... Oh, right, your generation only texts ...”
Okay, one more. Here’s Henrietta. I emailed her an invitation ... Holy Cow, she’s checked in! Let’s see, click “Join.” I can see her!
“Henrietta, is that you? Can you hear me? You can? You can hear me! Henrietta can hear me! And I can hear her!
“Yes, Henrietta, I’m all right. Just doing cartwheels around my study. Between COVID and the 95-degree heat and 100% humidity, it’s all the exercise I get.
“How can I help you today?
“Henrietta? HENRIETTA! Where have you gone, Henrietta?”
THERE IS A PROBLEM WITH YOUR CALL. DISCONNECT YOUR ROUTER, WAIT 65 SECONDS, RECONNECT, THEN RESTART YOUR WIFI, AND LOG IN AGAIN.
Maybe it’s time to go back to the office. A face shield and HAZMAT suit are sounding better all the time.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Another great morning,
Here goes. I’ll invite Gretchen by text: 617-555-5555. “TOO LONG.” How can 10 digits be too long? Trying again: 617-555-5555. “TOO LONG!” What the heck, let me leave off the last digit: 617-555-555. “TOO SHORT.”
Never mind, I’ll invite her by email.
Five minutes have gone by. Better call to see if she got the invite.
“Hello, is this Gretchen? Don’t hang up, I’m not a telemarketer! This is Dr. Rockoff. I sent you an invitation for our computer visit.
“You got it, great. Yes, you have to click on it to sign in. I know, your appointment’s at 8:30. It’s now 8:28. Let’s start early, why not?
“Hi, there! I can see you. Can you hear me? You’re nodding and your lips are moving. I can’t hear you. Did you enable your microphone?
“Nope, still can’t hear. I’ll call your cell, and we’ll talk that way.
“Yes, it’s me, Dr. Rockoff. What’s that? You enabled the microphone along with your video when you logged on? Well, there we go. How can I help today?
“You want a refill on your tretinoin gel for age management? Not a problem. Let’s see, you’ve been using it since 1996. No, you look great! Not a day over 76, really! I’ll have the staff escribe it right over.
“Okay, take care. Three years should be about right. Happy 80th!”
Wonder what happened there. Maybe things will go better for the next patient. Okay, I’m emailing an invite to Rob.
There he is! “Hi. Can you see me? Hear me? Nope, can’t hear you. Let me just call your cell.”
Okay, 972-555-5555. Ringing ... oh no, right to voicemail. “You have reached 972-555-5555. The mailbox is full and cannot accept messages. Please try some other time.”
“Okay, I’m back with you on the screen, Rob. Nope, still can’t hear you. I tried your cell but it went to voicemail. Yes, I see you’re holding the phone in your hand. Let me try you again.
“972-555-5555. Right to voicemail. Doesn’t your phone ring? You never make voice calls, only send texts? Look, please call me: 781-555-5555, write it down.
“Excellent, we’re in business. You’re worried about a mole that’s changing. You sent a photo to the office. Great, I’ll look right now on your record ... nope, not uploaded. Can you email me the photo? Please write down my email address: alanrockoffmdskincarespecialistist@myfabuloustelemedicineportal.now. Got that? Okay, please send the picture ...
“Returned as undeliverable? Show me what you typed ... Oh, wait. It’s ‘telemedicine,’ not ‘TellaMedicine.’ ” Yeah, that should do it.
“Okay, got the picture. You do fabulous super-closeups! Is that your navel next to it? Your left nostril? Okay. You tried to razor off the hair growing out it? Yes, that could account for the bleeding. Tell you what, go easy on it for the next 2 weeks, and send me another picture. Same email address.
“You have another question? Sure. You want a refill of your clindamycin gel because the tube from 2013 ran out? Guess you haven’t grown out of your acne yet. Sure, happy to send it in for you. Same pharmacy we have on file? You’re bunking with your parents in Wichita? No problem. Just need the pharmacy name and street. Boston, Wichita, whatever.
“Sure, happy to help. Enjoy your stay with your parents. You’ve been there 4 months? Are you cleaning your room? Mostly? Good. Take care. I’ll respond to your email in 2 weeks. Meantime, you might empty out your full voicemail box ... Oh, right, your generation only texts ...”
Okay, one more. Here’s Henrietta. I emailed her an invitation ... Holy Cow, she’s checked in! Let’s see, click “Join.” I can see her!
“Henrietta, is that you? Can you hear me? You can? You can hear me! Henrietta can hear me! And I can hear her!
“Yes, Henrietta, I’m all right. Just doing cartwheels around my study. Between COVID and the 95-degree heat and 100% humidity, it’s all the exercise I get.
“How can I help you today?
“Henrietta? HENRIETTA! Where have you gone, Henrietta?”
THERE IS A PROBLEM WITH YOUR CALL. DISCONNECT YOUR ROUTER, WAIT 65 SECONDS, RECONNECT, THEN RESTART YOUR WIFI, AND LOG IN AGAIN.
Maybe it’s time to go back to the office. A face shield and HAZMAT suit are sounding better all the time.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Another great morning,
Here goes. I’ll invite Gretchen by text: 617-555-5555. “TOO LONG.” How can 10 digits be too long? Trying again: 617-555-5555. “TOO LONG!” What the heck, let me leave off the last digit: 617-555-555. “TOO SHORT.”
Never mind, I’ll invite her by email.
Five minutes have gone by. Better call to see if she got the invite.
“Hello, is this Gretchen? Don’t hang up, I’m not a telemarketer! This is Dr. Rockoff. I sent you an invitation for our computer visit.
“You got it, great. Yes, you have to click on it to sign in. I know, your appointment’s at 8:30. It’s now 8:28. Let’s start early, why not?
“Hi, there! I can see you. Can you hear me? You’re nodding and your lips are moving. I can’t hear you. Did you enable your microphone?
“Nope, still can’t hear. I’ll call your cell, and we’ll talk that way.
“Yes, it’s me, Dr. Rockoff. What’s that? You enabled the microphone along with your video when you logged on? Well, there we go. How can I help today?
“You want a refill on your tretinoin gel for age management? Not a problem. Let’s see, you’ve been using it since 1996. No, you look great! Not a day over 76, really! I’ll have the staff escribe it right over.
“Okay, take care. Three years should be about right. Happy 80th!”
Wonder what happened there. Maybe things will go better for the next patient. Okay, I’m emailing an invite to Rob.
There he is! “Hi. Can you see me? Hear me? Nope, can’t hear you. Let me just call your cell.”
Okay, 972-555-5555. Ringing ... oh no, right to voicemail. “You have reached 972-555-5555. The mailbox is full and cannot accept messages. Please try some other time.”
“Okay, I’m back with you on the screen, Rob. Nope, still can’t hear you. I tried your cell but it went to voicemail. Yes, I see you’re holding the phone in your hand. Let me try you again.
“972-555-5555. Right to voicemail. Doesn’t your phone ring? You never make voice calls, only send texts? Look, please call me: 781-555-5555, write it down.
“Excellent, we’re in business. You’re worried about a mole that’s changing. You sent a photo to the office. Great, I’ll look right now on your record ... nope, not uploaded. Can you email me the photo? Please write down my email address: alanrockoffmdskincarespecialistist@myfabuloustelemedicineportal.now. Got that? Okay, please send the picture ...
“Returned as undeliverable? Show me what you typed ... Oh, wait. It’s ‘telemedicine,’ not ‘TellaMedicine.’ ” Yeah, that should do it.
“Okay, got the picture. You do fabulous super-closeups! Is that your navel next to it? Your left nostril? Okay. You tried to razor off the hair growing out it? Yes, that could account for the bleeding. Tell you what, go easy on it for the next 2 weeks, and send me another picture. Same email address.
“You have another question? Sure. You want a refill of your clindamycin gel because the tube from 2013 ran out? Guess you haven’t grown out of your acne yet. Sure, happy to send it in for you. Same pharmacy we have on file? You’re bunking with your parents in Wichita? No problem. Just need the pharmacy name and street. Boston, Wichita, whatever.
“Sure, happy to help. Enjoy your stay with your parents. You’ve been there 4 months? Are you cleaning your room? Mostly? Good. Take care. I’ll respond to your email in 2 weeks. Meantime, you might empty out your full voicemail box ... Oh, right, your generation only texts ...”
Okay, one more. Here’s Henrietta. I emailed her an invitation ... Holy Cow, she’s checked in! Let’s see, click “Join.” I can see her!
“Henrietta, is that you? Can you hear me? You can? You can hear me! Henrietta can hear me! And I can hear her!
“Yes, Henrietta, I’m all right. Just doing cartwheels around my study. Between COVID and the 95-degree heat and 100% humidity, it’s all the exercise I get.
“How can I help you today?
“Henrietta? HENRIETTA! Where have you gone, Henrietta?”
THERE IS A PROBLEM WITH YOUR CALL. DISCONNECT YOUR ROUTER, WAIT 65 SECONDS, RECONNECT, THEN RESTART YOUR WIFI, AND LOG IN AGAIN.
Maybe it’s time to go back to the office. A face shield and HAZMAT suit are sounding better all the time.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
September marks 9 months
It has been a busy month. September will mark the ninth month of U.S. COVID-19 with the country now surpassing 5 million cases and more than 175,000 deaths. Daily life and our medical practices will never be the same. Many have lost friends, family, businesses, and hope. Instead of acting as a nation to pull through this together, we seem to be entering a continual state of Thoreau solitude combined with Garrett Hardin’s tragedy of the commons.
In the last 2 months GI & Hepatology News published a two-part opinion piece about the acquisition of physicians’ GI practices by private equity (PE) companies. I received a strongly worded (but justified) email criticizing the newspaper for being one sided and not declaring a conflict of interest on the part of the author. For both issues, I take sole responsibility. While it is important for us to understand how PE is affecting GI practices, the author did have a personal stake in the success of this financial model. It is important to note that details of a PE acquisition can vary greatly depending on the PE company involved and PE companies looking to acquire practices now can be counted in the hundreds. The pros and cons of PE acquisitions were argued prior to COVID-19, but since the first quarter of 2020, the model is even more confusing. We will find out over the next several years whether this ever-proliferating model of practice financing will be successful or disastrous.
In November, GI & Hepatology News will publish a special supplement called Gastroenterology Data Trends. This publication will include brief, but robust snapshots of major trends in topics ranging from NAFLD, IBD, and GI cancers to the impact of COVID-19 on GI practices. We have collected a stellar group of authors to help us.
This month, the school year begins in ways that are still being sorted out. The “Big House” will not host its usual 110,000 fans packed like sardines watching Michigan football. I hope all of our readers skipped Sturgis this year. Stay safe, stay apart, and mask up.
John I. Allen, MD, MBA, AGAF
Editor in Chief
It has been a busy month. September will mark the ninth month of U.S. COVID-19 with the country now surpassing 5 million cases and more than 175,000 deaths. Daily life and our medical practices will never be the same. Many have lost friends, family, businesses, and hope. Instead of acting as a nation to pull through this together, we seem to be entering a continual state of Thoreau solitude combined with Garrett Hardin’s tragedy of the commons.
In the last 2 months GI & Hepatology News published a two-part opinion piece about the acquisition of physicians’ GI practices by private equity (PE) companies. I received a strongly worded (but justified) email criticizing the newspaper for being one sided and not declaring a conflict of interest on the part of the author. For both issues, I take sole responsibility. While it is important for us to understand how PE is affecting GI practices, the author did have a personal stake in the success of this financial model. It is important to note that details of a PE acquisition can vary greatly depending on the PE company involved and PE companies looking to acquire practices now can be counted in the hundreds. The pros and cons of PE acquisitions were argued prior to COVID-19, but since the first quarter of 2020, the model is even more confusing. We will find out over the next several years whether this ever-proliferating model of practice financing will be successful or disastrous.
In November, GI & Hepatology News will publish a special supplement called Gastroenterology Data Trends. This publication will include brief, but robust snapshots of major trends in topics ranging from NAFLD, IBD, and GI cancers to the impact of COVID-19 on GI practices. We have collected a stellar group of authors to help us.
This month, the school year begins in ways that are still being sorted out. The “Big House” will not host its usual 110,000 fans packed like sardines watching Michigan football. I hope all of our readers skipped Sturgis this year. Stay safe, stay apart, and mask up.
John I. Allen, MD, MBA, AGAF
Editor in Chief
It has been a busy month. September will mark the ninth month of U.S. COVID-19 with the country now surpassing 5 million cases and more than 175,000 deaths. Daily life and our medical practices will never be the same. Many have lost friends, family, businesses, and hope. Instead of acting as a nation to pull through this together, we seem to be entering a continual state of Thoreau solitude combined with Garrett Hardin’s tragedy of the commons.
In the last 2 months GI & Hepatology News published a two-part opinion piece about the acquisition of physicians’ GI practices by private equity (PE) companies. I received a strongly worded (but justified) email criticizing the newspaper for being one sided and not declaring a conflict of interest on the part of the author. For both issues, I take sole responsibility. While it is important for us to understand how PE is affecting GI practices, the author did have a personal stake in the success of this financial model. It is important to note that details of a PE acquisition can vary greatly depending on the PE company involved and PE companies looking to acquire practices now can be counted in the hundreds. The pros and cons of PE acquisitions were argued prior to COVID-19, but since the first quarter of 2020, the model is even more confusing. We will find out over the next several years whether this ever-proliferating model of practice financing will be successful or disastrous.
In November, GI & Hepatology News will publish a special supplement called Gastroenterology Data Trends. This publication will include brief, but robust snapshots of major trends in topics ranging from NAFLD, IBD, and GI cancers to the impact of COVID-19 on GI practices. We have collected a stellar group of authors to help us.
This month, the school year begins in ways that are still being sorted out. The “Big House” will not host its usual 110,000 fans packed like sardines watching Michigan football. I hope all of our readers skipped Sturgis this year. Stay safe, stay apart, and mask up.
John I. Allen, MD, MBA, AGAF
Editor in Chief