User login
An assessment of asthma drugs in pregnancy
Asthma effects about 10% of pregnant women worldwide. About 10% of these will have severe disease requiring oral corticosteroids. Brief reviews of asthma drugs are shown below.
The trade names (if available) and molecular weights (rounded to the nearest whole number) are shown in parentheses. Nearly all of these drugs will cross the placenta.
Beclomethasone (Beconase AQ) (539)
Either beclomethasone or budesonide was considered the inhaled steroids of choice for use during pregnancy, according to a position statement from a joint committee of the American College of Obstetricians and Gynecologists and the American College of Allergy, Asthma, and Immunology published in 2000. Although the drug is teratogenic in animals, no human reports associating the use of inhaled beclomethasone with human congenital anomalies have been found.
Benralizumab (Fasenra) (150,000)
There is no published human pregnancy data. Based on studies in monkeys, the drug crosses the placenta in the third trimester. It caused no fetal harm in monkeys when given throughout pregnancy. There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to the drug during pregnancy. Health care providers can enroll patients or encourage patients to enroll themselves by calling 1-877-311-8972 or visiting mothertobaby.org/Fasenra.
Budesonide (Rhinocort) (431)
Either budesonide or beclomethasone was considered the inhaled steroids of choice for use during pregnancy in a position statement from a joint committee of ACOG and ACAAI published in 2000. Although the drug is teratogenic in animals, no human reports associating the use of inhaled beclomethasone with human congenital anomalies have been found.
Caffeine (194)
Although the amount of caffeine in commonly used beverages varies widely, caffeine consumption in pregnancy in moderate amounts does not pose a risk to the fetus. When used in moderation, no association with congenital malformations, spontaneous abortions, preterm birth, and low birth weight have been proven.
Ciclesonide (Alvesco) (541)
Ciclesonide is an inhaled corticosteroid. There is no published human pregnancy data but the molecular weight suggests that it will cross the placenta throughout pregnancy. The drug produced no defects in rats but caused fetal toxicity in rabbits. Although the risk may be low because it is inhaled, avoiding it in the first trimester should be considered (see dexamethasone).
Cromolyn sodium (490)
Cromolyn was available as a nasal spray and oral solution, but it is no longer available in the United States. It is poorly absorbed into the systemic circulation. Neither the human nor the animal data suggest a risk of embryo-fetal harm.
Dexamethasone (392)
This is a corticosteroid with potency similar to betamethasone. Because large epidemiologic studies have found positive associations between systemic corticosteroids and nonsyndromic orofacial clefts, it is best to avoid this agent in the first trimester. However, when used for the treatment of asthma, other studies have not found a significantly increased risk of maternal or fetal complications. The difference in these outcomes may be related to the systemic concentrations of the drug.
Dyphylline (254) + guaifenesin (198) (Difil-G Forte) (Dilex-G 400) (Dy-G)
This is an OTC liquid drug taken orally. It has not been studied in pregnant animals, and there is no published human pregnancy data. However, these bronchodilator agents probably can be classified as low risk for the embryo and fetus. Dyphylline alone has been removed from the market.
Fluticasone (539) + vilanterol (Breo Ellipta) (775)
Fluticasone is a corticosteroid and vilanterol is a long acting beta2-adrenergic agonist that are given by inhalation. The molecular weights suggest that the two agents will cross the placenta throughout pregnancy. The drug did not cause fetal harm in animals. There is no published human pregnancy data for this fixed combination.
Fluticasone (539) + umeclidinium (509) + vilanterol (Trelegy Ellipta) (776)
The combination of fluticasone (glucocorticoid), umeclidinium, and vilanterol (long-acting beta2-adrenergic agonists) is given by inhalation. The molecular weights suggest that the three agents will cross the placenta throughout pregnancy. Although the three-drug combination has not been studied in pregnant rats and rabbits, the individual agents did not cause embryo-fetal harm in these species. There is no evidence that these agents, when given by inhalation, will harm the human embryo and/or fetus. No published human pregnancy reports for this fixed combination have been located.
Formoterol + mometasone (Dulera Aerosol) (841 / 521)
This combination is an aerosol product. Formoterol is a long-acting beta2-adrenergic agonist and mometasone is a topical corticosteroid. There is no published human pregnancy data for this fixed combination. The molecular weights suggest that both drugs will cross the placenta throughout pregnancy. In animals given high oral doses, both were teratogenic.
Ipratropium (Atrovent) (430)
Inhaled ipratropium, an anticholinergic bronchodilator, is recommended for asthma in patients not responding adequately to other therapy. It was not teratogenic mice, rats, and rabbits. Although the human pregnancy data is limited, there is no evidence that the drug is hazardous to the fetus. It produces fewer systemic effects then atropine and may have an additive bronchodilatory effect to beta2 agonists.
Isoproterenol (211)
Isoproterenol is a sympathomimetic (bronchodilator) with beta-adrenergic effects that is given intravenously. No reports linking this agent with congenital defects have been located. The drug was not teratogenic in rats and rabbits but was in hamsters.
Levalbuterol (Xopenex HFA) (240)
Levalbuterol is the (R)-enantiomer of racemic albuterol. It is given by inhalation. No reports of its use in human pregnancy have been located. However, racemic albuterol is considered compatible in pregnancy, and there is no apparent reason not to classify levalbuterol the same way. The drug, when given orally, is teratogenic in animals. If levalbuterol is used in pregnancy for the treatment of asthma, health care professionals are encouraged to call the toll-free number (1-877-311-8972) for information about patient enrollment in an Organization of Teratology Specialists study.
Mepolizumab (Nucala) (149,000)
Mepolizumab is given by subcutaneous injection. It is not indicated for status asthmaticus. There is no published human pregnancy data but the molecular weight suggests that it will not cross the placenta in the first half of pregnancy. The drug did not cause defects in monkeys and mice. There is a pregnancy exposure registry that monitors pregnancy outcomes in women with asthma exposed to Nucala during pregnancy. Health care providers can enroll patients or encourage patients to enroll themselves by calling 1-877-311-8972 or visiting www.mothertobaby.org/asthma.
Metaproterenol (521)
Metaproterenol, a selective beta2-adrenergic agonist, is a respiratory (bronchodilator) that is given orally. Use of this agent in pregnancy has not been linked with congenital defects. However, the drug is teratogenic in animals.
Methylprednisolone (Medrol) (374)
This is an oral glucocorticoid. The molecular weight suggests that it will cross the placenta throughout pregnancy. No reports relating to its use in human pregnancy or in pregnant animals have been located. However, teratogenicity is a potential problem (see below). If high doses of the drug are used in pregnancy, the newborn infants should be carefully observed for signs of hypoadrenalism. In addition, all corticosteroids increase calcium excretion.
Methylprednisolone acetate (Depo-Medrol) (417)
This is an injectable glucocorticoid. See below.
Methylprednisolone sodium succinate (Solu-Medrol) (497)
Methylprednisolone is a glucocorticoid given parenterally. The molecular weight suggests that it will cross the placenta throughout pregnancy. As with other corticosteroids, the drug was teratogenic, at doses equivalent to the human dose, in mice, rats, and rabbits. If the drug is used in pregnancy, the newborn infant should be carefully observed for signs of hypoadrenalism. In addition, all corticosteroids increase calcium excretion.
Mometasone + formoterol (Dulera) (321 + 841)
Dulera is a combination product of mometasone (corticosteroid) and formoterol (beta2-adrenergic agonist). There is no published human data for Dulera but the molecular weights suggest that the drugs will cross the placenta. Oral doses of formoterol were not teratogenic in animals but were with mometasone. The limited human pregnancy data with formoterol did not suggest a risk of embryo/fetal harm, but there is no human pregnancy data for mometasone.
Montelukast (Singulair) (608)
Montelukast is a leukotriene receptor antagonist that is given orally. Although the human data are limited, the drug does not appear to cause harm to the embryo and/or fetus. The drug was not teratogenic in rats and rabbits. The manufacturer maintains a pregnancy registry for women exposed to montelukast. Health care professionals are encouraged to report pregnancy exposures to the registry by calling the toll-free number 1-800-986-8999.
Omalizumab (Xolair) (149,000)
Omalizumab is a recombinant DNA–derived humanized immunoglobulin (IgG1k) monoclonal antibody that is administered subcutaneously for patients with moderate to severe persistent asthma. In monkeys, the drug did not cause embryotoxicity or teratogenicity. The human pregnancy data is very limited but does not suggest an increased embryo-fetal risk.
Prednisone (Rayos) (358)
The use of oral prednisone appears to represent a small risk to the developing fetus. One of these risks appears to be orofacial clefts. The drug causes birth defects in rats, mice, rabbits, and hamsters. However, the available evidence supports its use to control various maternal diseases, one of which is asthma.
Reslizumab (Cinqair) (147,000)
Reslizumab is given intravenously. Even though the molecular weight is high, the drug crosses the placenta during pregnancy. In placebo-controlled studies, anaphylaxis occurred in 0.3% of patients receiving the drug. No adverse effects were observed when the drug was given to pregnant mice and rabbits.
Salmeterol (Serevent Diskus) (416)
Salmeterol is a long-acting beta2-adrenergic agonist that is given as an aerosol or dry powder for oral inhalation. Because the drug acts locally in the lung, plasma levels are very low or undetectable and are a result of swallowed salmeterol. The limited human pregnancy data does not suggest risk of embryo-fetal harm. High oral doses in animals were not teratogenic.
Theophylline (180)
Oral theophylline is a methylxanthine that is indicated for the treatment of symptoms of chronic asthma and other chronic lung diseases. According to ACOG, theophylline is not a preferred asthma therapy but considered an alternative agent. No published reports linking the use of theophylline with congenital defects have been located. However, the drug is teratogenic in mice, rats, and rabbits at doses close to the human dose.
Tiotropium (Spiriva Respimat) (490)
Tiotropium, an anticholinergic bronchodilator, is given by oral inhalation only. No reports describing the use of tiotropium during human pregnancy have been located. The animal data suggest low risk. However, because of its long elimination half-life (about 25 hours), use of tiotropium immediately before the diagnosis of an inadvertent pregnancy would most likely result in the exposure of a portion of organogenesis.
Triamcinolone (Kenalog-40) (435)
Triamcinolone is an inhaled corticosteroid with potency slightly greater than prednisone. Although the systemic use of the drug has a small absolute risk of oral clefts and fetal growth restriction, inhaled triamcinolone does not appear to cause embryo-fetal harm. The drug is teratogenic when given orally to animals.
Breastfeeding
It is not known if the above drugs are excreted into breast milk. Agents with relatively low molecular weights will probably be in milk. However, if the maternal levels are low, the amount in milk will probably be very small, if at all. Nevertheless, it is doubtful if any of these agents, even if they are excreted into milk, will have a harmful effect on a nursing infant.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
Asthma effects about 10% of pregnant women worldwide. About 10% of these will have severe disease requiring oral corticosteroids. Brief reviews of asthma drugs are shown below.
The trade names (if available) and molecular weights (rounded to the nearest whole number) are shown in parentheses. Nearly all of these drugs will cross the placenta.
Beclomethasone (Beconase AQ) (539)
Either beclomethasone or budesonide was considered the inhaled steroids of choice for use during pregnancy, according to a position statement from a joint committee of the American College of Obstetricians and Gynecologists and the American College of Allergy, Asthma, and Immunology published in 2000. Although the drug is teratogenic in animals, no human reports associating the use of inhaled beclomethasone with human congenital anomalies have been found.
Benralizumab (Fasenra) (150,000)
There is no published human pregnancy data. Based on studies in monkeys, the drug crosses the placenta in the third trimester. It caused no fetal harm in monkeys when given throughout pregnancy. There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to the drug during pregnancy. Health care providers can enroll patients or encourage patients to enroll themselves by calling 1-877-311-8972 or visiting mothertobaby.org/Fasenra.
Budesonide (Rhinocort) (431)
Either budesonide or beclomethasone was considered the inhaled steroids of choice for use during pregnancy in a position statement from a joint committee of ACOG and ACAAI published in 2000. Although the drug is teratogenic in animals, no human reports associating the use of inhaled beclomethasone with human congenital anomalies have been found.
Caffeine (194)
Although the amount of caffeine in commonly used beverages varies widely, caffeine consumption in pregnancy in moderate amounts does not pose a risk to the fetus. When used in moderation, no association with congenital malformations, spontaneous abortions, preterm birth, and low birth weight have been proven.
Ciclesonide (Alvesco) (541)
Ciclesonide is an inhaled corticosteroid. There is no published human pregnancy data but the molecular weight suggests that it will cross the placenta throughout pregnancy. The drug produced no defects in rats but caused fetal toxicity in rabbits. Although the risk may be low because it is inhaled, avoiding it in the first trimester should be considered (see dexamethasone).
Cromolyn sodium (490)
Cromolyn was available as a nasal spray and oral solution, but it is no longer available in the United States. It is poorly absorbed into the systemic circulation. Neither the human nor the animal data suggest a risk of embryo-fetal harm.
Dexamethasone (392)
This is a corticosteroid with potency similar to betamethasone. Because large epidemiologic studies have found positive associations between systemic corticosteroids and nonsyndromic orofacial clefts, it is best to avoid this agent in the first trimester. However, when used for the treatment of asthma, other studies have not found a significantly increased risk of maternal or fetal complications. The difference in these outcomes may be related to the systemic concentrations of the drug.
Dyphylline (254) + guaifenesin (198) (Difil-G Forte) (Dilex-G 400) (Dy-G)
This is an OTC liquid drug taken orally. It has not been studied in pregnant animals, and there is no published human pregnancy data. However, these bronchodilator agents probably can be classified as low risk for the embryo and fetus. Dyphylline alone has been removed from the market.
Fluticasone (539) + vilanterol (Breo Ellipta) (775)
Fluticasone is a corticosteroid and vilanterol is a long acting beta2-adrenergic agonist that are given by inhalation. The molecular weights suggest that the two agents will cross the placenta throughout pregnancy. The drug did not cause fetal harm in animals. There is no published human pregnancy data for this fixed combination.
Fluticasone (539) + umeclidinium (509) + vilanterol (Trelegy Ellipta) (776)
The combination of fluticasone (glucocorticoid), umeclidinium, and vilanterol (long-acting beta2-adrenergic agonists) is given by inhalation. The molecular weights suggest that the three agents will cross the placenta throughout pregnancy. Although the three-drug combination has not been studied in pregnant rats and rabbits, the individual agents did not cause embryo-fetal harm in these species. There is no evidence that these agents, when given by inhalation, will harm the human embryo and/or fetus. No published human pregnancy reports for this fixed combination have been located.
Formoterol + mometasone (Dulera Aerosol) (841 / 521)
This combination is an aerosol product. Formoterol is a long-acting beta2-adrenergic agonist and mometasone is a topical corticosteroid. There is no published human pregnancy data for this fixed combination. The molecular weights suggest that both drugs will cross the placenta throughout pregnancy. In animals given high oral doses, both were teratogenic.
Ipratropium (Atrovent) (430)
Inhaled ipratropium, an anticholinergic bronchodilator, is recommended for asthma in patients not responding adequately to other therapy. It was not teratogenic mice, rats, and rabbits. Although the human pregnancy data is limited, there is no evidence that the drug is hazardous to the fetus. It produces fewer systemic effects then atropine and may have an additive bronchodilatory effect to beta2 agonists.
Isoproterenol (211)
Isoproterenol is a sympathomimetic (bronchodilator) with beta-adrenergic effects that is given intravenously. No reports linking this agent with congenital defects have been located. The drug was not teratogenic in rats and rabbits but was in hamsters.
Levalbuterol (Xopenex HFA) (240)
Levalbuterol is the (R)-enantiomer of racemic albuterol. It is given by inhalation. No reports of its use in human pregnancy have been located. However, racemic albuterol is considered compatible in pregnancy, and there is no apparent reason not to classify levalbuterol the same way. The drug, when given orally, is teratogenic in animals. If levalbuterol is used in pregnancy for the treatment of asthma, health care professionals are encouraged to call the toll-free number (1-877-311-8972) for information about patient enrollment in an Organization of Teratology Specialists study.
Mepolizumab (Nucala) (149,000)
Mepolizumab is given by subcutaneous injection. It is not indicated for status asthmaticus. There is no published human pregnancy data but the molecular weight suggests that it will not cross the placenta in the first half of pregnancy. The drug did not cause defects in monkeys and mice. There is a pregnancy exposure registry that monitors pregnancy outcomes in women with asthma exposed to Nucala during pregnancy. Health care providers can enroll patients or encourage patients to enroll themselves by calling 1-877-311-8972 or visiting www.mothertobaby.org/asthma.
Metaproterenol (521)
Metaproterenol, a selective beta2-adrenergic agonist, is a respiratory (bronchodilator) that is given orally. Use of this agent in pregnancy has not been linked with congenital defects. However, the drug is teratogenic in animals.
Methylprednisolone (Medrol) (374)
This is an oral glucocorticoid. The molecular weight suggests that it will cross the placenta throughout pregnancy. No reports relating to its use in human pregnancy or in pregnant animals have been located. However, teratogenicity is a potential problem (see below). If high doses of the drug are used in pregnancy, the newborn infants should be carefully observed for signs of hypoadrenalism. In addition, all corticosteroids increase calcium excretion.
Methylprednisolone acetate (Depo-Medrol) (417)
This is an injectable glucocorticoid. See below.
Methylprednisolone sodium succinate (Solu-Medrol) (497)
Methylprednisolone is a glucocorticoid given parenterally. The molecular weight suggests that it will cross the placenta throughout pregnancy. As with other corticosteroids, the drug was teratogenic, at doses equivalent to the human dose, in mice, rats, and rabbits. If the drug is used in pregnancy, the newborn infant should be carefully observed for signs of hypoadrenalism. In addition, all corticosteroids increase calcium excretion.
Mometasone + formoterol (Dulera) (321 + 841)
Dulera is a combination product of mometasone (corticosteroid) and formoterol (beta2-adrenergic agonist). There is no published human data for Dulera but the molecular weights suggest that the drugs will cross the placenta. Oral doses of formoterol were not teratogenic in animals but were with mometasone. The limited human pregnancy data with formoterol did not suggest a risk of embryo/fetal harm, but there is no human pregnancy data for mometasone.
Montelukast (Singulair) (608)
Montelukast is a leukotriene receptor antagonist that is given orally. Although the human data are limited, the drug does not appear to cause harm to the embryo and/or fetus. The drug was not teratogenic in rats and rabbits. The manufacturer maintains a pregnancy registry for women exposed to montelukast. Health care professionals are encouraged to report pregnancy exposures to the registry by calling the toll-free number 1-800-986-8999.
Omalizumab (Xolair) (149,000)
Omalizumab is a recombinant DNA–derived humanized immunoglobulin (IgG1k) monoclonal antibody that is administered subcutaneously for patients with moderate to severe persistent asthma. In monkeys, the drug did not cause embryotoxicity or teratogenicity. The human pregnancy data is very limited but does not suggest an increased embryo-fetal risk.
Prednisone (Rayos) (358)
The use of oral prednisone appears to represent a small risk to the developing fetus. One of these risks appears to be orofacial clefts. The drug causes birth defects in rats, mice, rabbits, and hamsters. However, the available evidence supports its use to control various maternal diseases, one of which is asthma.
Reslizumab (Cinqair) (147,000)
Reslizumab is given intravenously. Even though the molecular weight is high, the drug crosses the placenta during pregnancy. In placebo-controlled studies, anaphylaxis occurred in 0.3% of patients receiving the drug. No adverse effects were observed when the drug was given to pregnant mice and rabbits.
Salmeterol (Serevent Diskus) (416)
Salmeterol is a long-acting beta2-adrenergic agonist that is given as an aerosol or dry powder for oral inhalation. Because the drug acts locally in the lung, plasma levels are very low or undetectable and are a result of swallowed salmeterol. The limited human pregnancy data does not suggest risk of embryo-fetal harm. High oral doses in animals were not teratogenic.
Theophylline (180)
Oral theophylline is a methylxanthine that is indicated for the treatment of symptoms of chronic asthma and other chronic lung diseases. According to ACOG, theophylline is not a preferred asthma therapy but considered an alternative agent. No published reports linking the use of theophylline with congenital defects have been located. However, the drug is teratogenic in mice, rats, and rabbits at doses close to the human dose.
Tiotropium (Spiriva Respimat) (490)
Tiotropium, an anticholinergic bronchodilator, is given by oral inhalation only. No reports describing the use of tiotropium during human pregnancy have been located. The animal data suggest low risk. However, because of its long elimination half-life (about 25 hours), use of tiotropium immediately before the diagnosis of an inadvertent pregnancy would most likely result in the exposure of a portion of organogenesis.
Triamcinolone (Kenalog-40) (435)
Triamcinolone is an inhaled corticosteroid with potency slightly greater than prednisone. Although the systemic use of the drug has a small absolute risk of oral clefts and fetal growth restriction, inhaled triamcinolone does not appear to cause embryo-fetal harm. The drug is teratogenic when given orally to animals.
Breastfeeding
It is not known if the above drugs are excreted into breast milk. Agents with relatively low molecular weights will probably be in milk. However, if the maternal levels are low, the amount in milk will probably be very small, if at all. Nevertheless, it is doubtful if any of these agents, even if they are excreted into milk, will have a harmful effect on a nursing infant.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
Asthma effects about 10% of pregnant women worldwide. About 10% of these will have severe disease requiring oral corticosteroids. Brief reviews of asthma drugs are shown below.
The trade names (if available) and molecular weights (rounded to the nearest whole number) are shown in parentheses. Nearly all of these drugs will cross the placenta.
Beclomethasone (Beconase AQ) (539)
Either beclomethasone or budesonide was considered the inhaled steroids of choice for use during pregnancy, according to a position statement from a joint committee of the American College of Obstetricians and Gynecologists and the American College of Allergy, Asthma, and Immunology published in 2000. Although the drug is teratogenic in animals, no human reports associating the use of inhaled beclomethasone with human congenital anomalies have been found.
Benralizumab (Fasenra) (150,000)
There is no published human pregnancy data. Based on studies in monkeys, the drug crosses the placenta in the third trimester. It caused no fetal harm in monkeys when given throughout pregnancy. There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to the drug during pregnancy. Health care providers can enroll patients or encourage patients to enroll themselves by calling 1-877-311-8972 or visiting mothertobaby.org/Fasenra.
Budesonide (Rhinocort) (431)
Either budesonide or beclomethasone was considered the inhaled steroids of choice for use during pregnancy in a position statement from a joint committee of ACOG and ACAAI published in 2000. Although the drug is teratogenic in animals, no human reports associating the use of inhaled beclomethasone with human congenital anomalies have been found.
Caffeine (194)
Although the amount of caffeine in commonly used beverages varies widely, caffeine consumption in pregnancy in moderate amounts does not pose a risk to the fetus. When used in moderation, no association with congenital malformations, spontaneous abortions, preterm birth, and low birth weight have been proven.
Ciclesonide (Alvesco) (541)
Ciclesonide is an inhaled corticosteroid. There is no published human pregnancy data but the molecular weight suggests that it will cross the placenta throughout pregnancy. The drug produced no defects in rats but caused fetal toxicity in rabbits. Although the risk may be low because it is inhaled, avoiding it in the first trimester should be considered (see dexamethasone).
Cromolyn sodium (490)
Cromolyn was available as a nasal spray and oral solution, but it is no longer available in the United States. It is poorly absorbed into the systemic circulation. Neither the human nor the animal data suggest a risk of embryo-fetal harm.
Dexamethasone (392)
This is a corticosteroid with potency similar to betamethasone. Because large epidemiologic studies have found positive associations between systemic corticosteroids and nonsyndromic orofacial clefts, it is best to avoid this agent in the first trimester. However, when used for the treatment of asthma, other studies have not found a significantly increased risk of maternal or fetal complications. The difference in these outcomes may be related to the systemic concentrations of the drug.
Dyphylline (254) + guaifenesin (198) (Difil-G Forte) (Dilex-G 400) (Dy-G)
This is an OTC liquid drug taken orally. It has not been studied in pregnant animals, and there is no published human pregnancy data. However, these bronchodilator agents probably can be classified as low risk for the embryo and fetus. Dyphylline alone has been removed from the market.
Fluticasone (539) + vilanterol (Breo Ellipta) (775)
Fluticasone is a corticosteroid and vilanterol is a long acting beta2-adrenergic agonist that are given by inhalation. The molecular weights suggest that the two agents will cross the placenta throughout pregnancy. The drug did not cause fetal harm in animals. There is no published human pregnancy data for this fixed combination.
Fluticasone (539) + umeclidinium (509) + vilanterol (Trelegy Ellipta) (776)
The combination of fluticasone (glucocorticoid), umeclidinium, and vilanterol (long-acting beta2-adrenergic agonists) is given by inhalation. The molecular weights suggest that the three agents will cross the placenta throughout pregnancy. Although the three-drug combination has not been studied in pregnant rats and rabbits, the individual agents did not cause embryo-fetal harm in these species. There is no evidence that these agents, when given by inhalation, will harm the human embryo and/or fetus. No published human pregnancy reports for this fixed combination have been located.
Formoterol + mometasone (Dulera Aerosol) (841 / 521)
This combination is an aerosol product. Formoterol is a long-acting beta2-adrenergic agonist and mometasone is a topical corticosteroid. There is no published human pregnancy data for this fixed combination. The molecular weights suggest that both drugs will cross the placenta throughout pregnancy. In animals given high oral doses, both were teratogenic.
Ipratropium (Atrovent) (430)
Inhaled ipratropium, an anticholinergic bronchodilator, is recommended for asthma in patients not responding adequately to other therapy. It was not teratogenic mice, rats, and rabbits. Although the human pregnancy data is limited, there is no evidence that the drug is hazardous to the fetus. It produces fewer systemic effects then atropine and may have an additive bronchodilatory effect to beta2 agonists.
Isoproterenol (211)
Isoproterenol is a sympathomimetic (bronchodilator) with beta-adrenergic effects that is given intravenously. No reports linking this agent with congenital defects have been located. The drug was not teratogenic in rats and rabbits but was in hamsters.
Levalbuterol (Xopenex HFA) (240)
Levalbuterol is the (R)-enantiomer of racemic albuterol. It is given by inhalation. No reports of its use in human pregnancy have been located. However, racemic albuterol is considered compatible in pregnancy, and there is no apparent reason not to classify levalbuterol the same way. The drug, when given orally, is teratogenic in animals. If levalbuterol is used in pregnancy for the treatment of asthma, health care professionals are encouraged to call the toll-free number (1-877-311-8972) for information about patient enrollment in an Organization of Teratology Specialists study.
Mepolizumab (Nucala) (149,000)
Mepolizumab is given by subcutaneous injection. It is not indicated for status asthmaticus. There is no published human pregnancy data but the molecular weight suggests that it will not cross the placenta in the first half of pregnancy. The drug did not cause defects in monkeys and mice. There is a pregnancy exposure registry that monitors pregnancy outcomes in women with asthma exposed to Nucala during pregnancy. Health care providers can enroll patients or encourage patients to enroll themselves by calling 1-877-311-8972 or visiting www.mothertobaby.org/asthma.
Metaproterenol (521)
Metaproterenol, a selective beta2-adrenergic agonist, is a respiratory (bronchodilator) that is given orally. Use of this agent in pregnancy has not been linked with congenital defects. However, the drug is teratogenic in animals.
Methylprednisolone (Medrol) (374)
This is an oral glucocorticoid. The molecular weight suggests that it will cross the placenta throughout pregnancy. No reports relating to its use in human pregnancy or in pregnant animals have been located. However, teratogenicity is a potential problem (see below). If high doses of the drug are used in pregnancy, the newborn infants should be carefully observed for signs of hypoadrenalism. In addition, all corticosteroids increase calcium excretion.
Methylprednisolone acetate (Depo-Medrol) (417)
This is an injectable glucocorticoid. See below.
Methylprednisolone sodium succinate (Solu-Medrol) (497)
Methylprednisolone is a glucocorticoid given parenterally. The molecular weight suggests that it will cross the placenta throughout pregnancy. As with other corticosteroids, the drug was teratogenic, at doses equivalent to the human dose, in mice, rats, and rabbits. If the drug is used in pregnancy, the newborn infant should be carefully observed for signs of hypoadrenalism. In addition, all corticosteroids increase calcium excretion.
Mometasone + formoterol (Dulera) (321 + 841)
Dulera is a combination product of mometasone (corticosteroid) and formoterol (beta2-adrenergic agonist). There is no published human data for Dulera but the molecular weights suggest that the drugs will cross the placenta. Oral doses of formoterol were not teratogenic in animals but were with mometasone. The limited human pregnancy data with formoterol did not suggest a risk of embryo/fetal harm, but there is no human pregnancy data for mometasone.
Montelukast (Singulair) (608)
Montelukast is a leukotriene receptor antagonist that is given orally. Although the human data are limited, the drug does not appear to cause harm to the embryo and/or fetus. The drug was not teratogenic in rats and rabbits. The manufacturer maintains a pregnancy registry for women exposed to montelukast. Health care professionals are encouraged to report pregnancy exposures to the registry by calling the toll-free number 1-800-986-8999.
Omalizumab (Xolair) (149,000)
Omalizumab is a recombinant DNA–derived humanized immunoglobulin (IgG1k) monoclonal antibody that is administered subcutaneously for patients with moderate to severe persistent asthma. In monkeys, the drug did not cause embryotoxicity or teratogenicity. The human pregnancy data is very limited but does not suggest an increased embryo-fetal risk.
Prednisone (Rayos) (358)
The use of oral prednisone appears to represent a small risk to the developing fetus. One of these risks appears to be orofacial clefts. The drug causes birth defects in rats, mice, rabbits, and hamsters. However, the available evidence supports its use to control various maternal diseases, one of which is asthma.
Reslizumab (Cinqair) (147,000)
Reslizumab is given intravenously. Even though the molecular weight is high, the drug crosses the placenta during pregnancy. In placebo-controlled studies, anaphylaxis occurred in 0.3% of patients receiving the drug. No adverse effects were observed when the drug was given to pregnant mice and rabbits.
Salmeterol (Serevent Diskus) (416)
Salmeterol is a long-acting beta2-adrenergic agonist that is given as an aerosol or dry powder for oral inhalation. Because the drug acts locally in the lung, plasma levels are very low or undetectable and are a result of swallowed salmeterol. The limited human pregnancy data does not suggest risk of embryo-fetal harm. High oral doses in animals were not teratogenic.
Theophylline (180)
Oral theophylline is a methylxanthine that is indicated for the treatment of symptoms of chronic asthma and other chronic lung diseases. According to ACOG, theophylline is not a preferred asthma therapy but considered an alternative agent. No published reports linking the use of theophylline with congenital defects have been located. However, the drug is teratogenic in mice, rats, and rabbits at doses close to the human dose.
Tiotropium (Spiriva Respimat) (490)
Tiotropium, an anticholinergic bronchodilator, is given by oral inhalation only. No reports describing the use of tiotropium during human pregnancy have been located. The animal data suggest low risk. However, because of its long elimination half-life (about 25 hours), use of tiotropium immediately before the diagnosis of an inadvertent pregnancy would most likely result in the exposure of a portion of organogenesis.
Triamcinolone (Kenalog-40) (435)
Triamcinolone is an inhaled corticosteroid with potency slightly greater than prednisone. Although the systemic use of the drug has a small absolute risk of oral clefts and fetal growth restriction, inhaled triamcinolone does not appear to cause embryo-fetal harm. The drug is teratogenic when given orally to animals.
Breastfeeding
It is not known if the above drugs are excreted into breast milk. Agents with relatively low molecular weights will probably be in milk. However, if the maternal levels are low, the amount in milk will probably be very small, if at all. Nevertheless, it is doubtful if any of these agents, even if they are excreted into milk, will have a harmful effect on a nursing infant.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
IBD can be treated with diet alone
Dear colleagues and friends,
Thank you for your continued interest and support of the Perspectives debates. In this edition, Dr. Ashwin Ananthakrishnan and Dr. Laura Raffals explore the controversial topic of diet-based therapy in inflammatory bowel disease, highlights of the rationales for and against, and the current state of the evidence. All gastroenterologists frequently face questions pertaining to diet and its purported effects on digestive health. I found the discussion relevant to my own general practice, and I hope you will enjoy reading it as much as I did. As always, I welcome your comments and suggestions for future topics at [email protected].
Charles Kahi, MD, MS, AGAF, professor of medicine, Indiana University, Indianapolis. He is also an associate editor for GI & Hepatology News.
IBD can be treated with diet alone
Inflammatory bowel diseases (IBD), comprising Crohn’s disease and ulcerative colitis, have emerged as global diseases. The past 3 decades have seen a rising incidence of these diseases not just in the Western hemisphere, where their prevalence has been well recognized, but also in regions of the world such as Asia and South America where they were previously rare. Whereas several possible factors have been proposed to explain this rising incidence and globalization of disease with varying degrees of supportive evidence, one of the most likely factors is a changing diet. Over the same period that the disease incidence and prevalence have risen, diets worldwide have converged with several common trends observed across countries and continents. These include reductions in dietary fiber, fruits, and vegetables, and increased intake of processed food, animal protein, fats, and sugary drinks, all of which have been linked epidemiologically to Crohn’s disease.
Treatment of Crohn’s disease and ulcerative colitis over the past 2 decades has focused on the immunologic dysfunction observed in these patients. Successful treatment has relied on suppressing immune responses either broadly or through targeted suppression of specific immunologic pathways. By and large, whereas these approaches have enabled us to make significant progress in reducing disease-related morbidity, success has been moderate at best, with fewer than half of patients in any clinical trial achieving remission at the end of a year. Thus, this approach alone may not be sufficient for most patients with IBD.
Treatment of IBD with diet was long considered out of the mainstream and confined to the realm of anecdotes and message boards. Despite most patients believing that diet played a role in development of IBD and onset of flares and that dietary modification was helpful in relieving symptoms, physicians – who for the most part were not trained in these approaches – were not believers, and probably rightly so in the absence of any supporting data.1 However, the parallel emergence of three bodies of literature has now brought diet back into the mainstream of IBD care (such that not a single IBD conference goes by without at least a session or two on diet). First, large prospective cohorts from Europe and North America provided robust evidence linking long-term adult dietary patterns to disease incidence in adult-onset IBD, which supports many important case-control observations made over the past 2 decades.2 Second, and perhaps most important, we began understanding the role of the microbiome in the development of these diseases and recognizing its centrality to bowel inflammation. One of the key determinants of the microbiome is diet, exerting both short-term and long-term influences on the microbial structure. While microbial changes are by no means the only mechanism through which diet can influence intestinal inflammation, they are among the most important, with broad effects across many dietary components. These findings provided a robust scientific basis for investigating the role of diet. Third, while still far from the high-quality (and expensive) set-up of investigational trials of pharmacologic therapies, dietary therapy studies have also evolved to randomized controlled trial designs and investigation of mechanism-driven dietary combinations. Together, I think these three recent advances, in addition to the wealth of existing literature and anecdotal experience, have been important in moving diet (back) into the IBD mainstream.
So what evidence is there that diet is effective in the treatment of IBD? Randomized controlled trials published more than a decade ago demonstrated that exclusive enteral nutrition, wherein all table foods are eliminated from a diet and the patient relies on an elemental diet alone for nutrition, was effective in not just inducing clinical remission but also improving inflammatory biomarkers.3 With results replicated in several trials, exclusive enteral nutrition is, in many parts of the world, one of the first-line treatments for pediatric Crohn’s disease. That this has not been translated to longer-term maintenance therapy is not necessarily an indicator of lack of durable efficacy, but reflects the challenges of maintaining such a restrictive diet long term while living an active, normal life. However, more recent rigorous studies have demonstrated that the effects of exclusive enteral nutrition can be mimicked either by a selected, less-restrictive diet (such as CD-TREAT4), which is more sustainable, or by combining partial enteral nutrition with an elimination diet that is quite diverse (such as CDED5). The latter two are considerably more promising as longer-term dietary treatments for Crohn’s disease with durable efficacy in open-label studies and randomized trials.
What are my final arguments for diet being used as a treatment for IBD? With the exception of very restrictive ones, diets are generally safe. Of course, patients on restricted diets need monitoring for nutritional deficiencies, but this monitoring is likely less intense than that needed for many of our immunosuppressive therapies. Dietary therapies are not associated with an increase in risk of infections or malignancy (unlike our traditional immunosuppressive therapies), and consequently are much more likely to be accepted by our patients than what we are currently offering. In addition, the existing treatments are expensive and consequently difficult to sustain globally with the increasing burden of these diseases. On the other hand, as eating and dietary choices are a routine part of day-to-day life, dietary therapies are not likely to be associated with any excess costs.
Therefore, treating IBD with diet alone is supported by epidemiologic, mechanistic, and clinical evidence and is a safe, effective, and inexpensive alternative for our patients.
References
1. Zallot C et al. Inflamm Bowel Dis. 2013 Jan;19(1):66-72.
2. Sasson AN et al. Clin Gastroenterol Hepatol. 2019 Dec 5;S1542-3565(19)31394-1.
3. Wall CL et al. World J Gastroenterol. 2013;19:7652-60.
4. Svolos V et al. Gastroenterology. 2019;156:1354-67.e6.
5. Levine A et al. Gastroenterology. 2019;157:440-50.e8.
Dr. Ananthakrishnan is a gastroenterologist in the division of gastroenterology, Crohn’s and Colitis Center, Massachusetts General Hospital and Harvard Medical School, Boston. He is supported by funding from the Crohn’s and Colitis Foundation and the Chleck Family Foundation.
IBD can be treated with diet alone – No, it cannot!
The cause of IBD is not completely understood, but we believe something in our environment triggers a dysregulated immune response in individuals with a genetic predisposition to IBD. Among the environmental triggers commonly recognized, diet is considered an important trigger through its ability to affect the composition and health of the gut microbiome and host barrier function. Epidemiologic data support this assumption. Westernization of diet has been associated with the increasing incidence of IBD across the globe and in immigrants who move from developing countries to an industrialized country. Observational studies have shown diets higher in meat and polyunsaturated fatty acids and omega-6 fatty acids are associated with a higher risk for IBD, whereas diets high in fruits, vegetables, and other sources of dietary fiber have a lower risk of IBD.
A growing body of evidence supports the impact food can have on gut health, specifically in mouse IBD models, but it is challenging to translate findings from animal studies into dietary interventions for IBD patients. Mouse studies help us understand the mechanistic basis of how diet may affect IBD, but randomized clinical trials establishing their role in IBD are lacking. This is not surprising as dietary studies are challenging, particularly if done in a robust manner, given the difficulties of ensuring and measuring dietary compliance.
Exclusive enteral nutrition (EEN) has been studied the most rigorously of all diets in IBD and has demonstrated the greatest benefit, compared with other diet studies in IBD. EEN requires the intake of elemental, semi-elemental, or polymeric formulas to meet all nutritional requirements without additional intake of food for 6-8 weeks. Studies have been performed mostly in pediatric populations and have shown effectiveness in induction of remission with reduction in inflammatory markers, including C-reactive protein, erythrocyte sedimentation rate, and fecal calprotectin, and even mucosal healing. EEN has not worked out as well for adult populations, because of the poor tolerability of exclusive intake of enteral formulas. Because of this limitation, studies of partial enteral nutrition have been performed that generally allow some food intake in addition to the enteral nutrition. When compared with EEN or anti–tumor necrosis factor–alpha therapy, partial enteral nutrition is a less-effective treatment of Crohn’s disease; however, partial enteral nutrition does appear to improve clinical symptoms.
Beyond EEN, there are many diets that have been considered for the treatment of IBD, including the specific carbohydrate diet (SCD), Crohn’s disease exclusion diet, autoimmune diet, low FODMAP (fermentable oligo-, di-, mono-saccharides and polyols), Paleolithic diet, Mediterranean diet, and the semi-vegetarian diet, to name a few. Of these, only the SCD and Crohn’s disease exclusion diets have shown improvement in clinical remission and reduction in inflammatory markers.
The SCD diet is based on the theory that malabsorption of disaccharide and polysaccharide carbohydrates leads to bacterial overgrowth and host barrier dysfunction. This diet eliminates grains, dairy, processed meats, and certain vegetables such as potatoes, yams, and legumes. Small uncontrolled studies have shown improvement in symptoms and endoscopy findings. However, this restrictive diet is nearly impossible to follow long term. The Crohn’s disease exclusion diet is a whole foods diet avoiding all processed foods, animal fats, dairy, and gluten. Small studies of this diet have also shown improvement in clinical symptoms and inflammatory markers.
The plethora of studies and reports of the therapeutic effect of diet on IBD provide some promise of the benefit dietary modifications can bring to our IBD patients. However, most dietary studies are underpowered, lack a control arm, and do not include endoscopic endpoints. The current body of evidence remains insufficient to support the use of diet alone for the treatment of IBD. We need randomized clinical controlled trials that are held to the same rigor as those of our approved medical treatments for IBD. Although such trials are challenging, we’ve seen groups rise to the task to carry out more robust dietary studies in the IBD population, and we await the results of several ongoing trials.
IBD is a challenging disease to live with and often leaves our patients feeling out of control. Dietary choices provide an avenue for patients to have some control of their health. However, current evidence does not support the prescription of dietary interventions alone to treat IBD, particularly when we have known, effective therapies. While I am not ready to prescribe diet as a stand-alone treatment for IBD, I make a point to discuss the role diet may play in helping our patients achieve optimal health. As health care providers, it is our responsibility to provide holistic care to our patients, which includes promotion of a healthy diet, absent processed foods and added sugars. Healthy lifestyle choices combined with effective medical and surgical treatments offer our patients the best shot at sustained disease control.
References
1. Hou JK et al. Am J Gastroenterol. 2011;106(4):563-73.
2. Zachos M et al. Cochrane Database Syst Rev. 2007(1):CD000542.
3. Lee D et al. Inflamm Bowel Dis. 2015;21(8):1786-93.
4. Obih C et al. Nutrition. 2016;32(4):418-25.
5. Sigall Boneh R et al. J Crohns Colitis. 2017;11(10):1205-12.
Dr. Raffals is a gastroenterologist in the division of gastroenterology and hepatology, Mayo Clinic, Rochester, Minn. She has no financial conflicts of interest relevant to this paper.
Dear colleagues and friends,
Thank you for your continued interest and support of the Perspectives debates. In this edition, Dr. Ashwin Ananthakrishnan and Dr. Laura Raffals explore the controversial topic of diet-based therapy in inflammatory bowel disease, highlights of the rationales for and against, and the current state of the evidence. All gastroenterologists frequently face questions pertaining to diet and its purported effects on digestive health. I found the discussion relevant to my own general practice, and I hope you will enjoy reading it as much as I did. As always, I welcome your comments and suggestions for future topics at [email protected].
Charles Kahi, MD, MS, AGAF, professor of medicine, Indiana University, Indianapolis. He is also an associate editor for GI & Hepatology News.
IBD can be treated with diet alone
Inflammatory bowel diseases (IBD), comprising Crohn’s disease and ulcerative colitis, have emerged as global diseases. The past 3 decades have seen a rising incidence of these diseases not just in the Western hemisphere, where their prevalence has been well recognized, but also in regions of the world such as Asia and South America where they were previously rare. Whereas several possible factors have been proposed to explain this rising incidence and globalization of disease with varying degrees of supportive evidence, one of the most likely factors is a changing diet. Over the same period that the disease incidence and prevalence have risen, diets worldwide have converged with several common trends observed across countries and continents. These include reductions in dietary fiber, fruits, and vegetables, and increased intake of processed food, animal protein, fats, and sugary drinks, all of which have been linked epidemiologically to Crohn’s disease.
Treatment of Crohn’s disease and ulcerative colitis over the past 2 decades has focused on the immunologic dysfunction observed in these patients. Successful treatment has relied on suppressing immune responses either broadly or through targeted suppression of specific immunologic pathways. By and large, whereas these approaches have enabled us to make significant progress in reducing disease-related morbidity, success has been moderate at best, with fewer than half of patients in any clinical trial achieving remission at the end of a year. Thus, this approach alone may not be sufficient for most patients with IBD.
Treatment of IBD with diet was long considered out of the mainstream and confined to the realm of anecdotes and message boards. Despite most patients believing that diet played a role in development of IBD and onset of flares and that dietary modification was helpful in relieving symptoms, physicians – who for the most part were not trained in these approaches – were not believers, and probably rightly so in the absence of any supporting data.1 However, the parallel emergence of three bodies of literature has now brought diet back into the mainstream of IBD care (such that not a single IBD conference goes by without at least a session or two on diet). First, large prospective cohorts from Europe and North America provided robust evidence linking long-term adult dietary patterns to disease incidence in adult-onset IBD, which supports many important case-control observations made over the past 2 decades.2 Second, and perhaps most important, we began understanding the role of the microbiome in the development of these diseases and recognizing its centrality to bowel inflammation. One of the key determinants of the microbiome is diet, exerting both short-term and long-term influences on the microbial structure. While microbial changes are by no means the only mechanism through which diet can influence intestinal inflammation, they are among the most important, with broad effects across many dietary components. These findings provided a robust scientific basis for investigating the role of diet. Third, while still far from the high-quality (and expensive) set-up of investigational trials of pharmacologic therapies, dietary therapy studies have also evolved to randomized controlled trial designs and investigation of mechanism-driven dietary combinations. Together, I think these three recent advances, in addition to the wealth of existing literature and anecdotal experience, have been important in moving diet (back) into the IBD mainstream.
So what evidence is there that diet is effective in the treatment of IBD? Randomized controlled trials published more than a decade ago demonstrated that exclusive enteral nutrition, wherein all table foods are eliminated from a diet and the patient relies on an elemental diet alone for nutrition, was effective in not just inducing clinical remission but also improving inflammatory biomarkers.3 With results replicated in several trials, exclusive enteral nutrition is, in many parts of the world, one of the first-line treatments for pediatric Crohn’s disease. That this has not been translated to longer-term maintenance therapy is not necessarily an indicator of lack of durable efficacy, but reflects the challenges of maintaining such a restrictive diet long term while living an active, normal life. However, more recent rigorous studies have demonstrated that the effects of exclusive enteral nutrition can be mimicked either by a selected, less-restrictive diet (such as CD-TREAT4), which is more sustainable, or by combining partial enteral nutrition with an elimination diet that is quite diverse (such as CDED5). The latter two are considerably more promising as longer-term dietary treatments for Crohn’s disease with durable efficacy in open-label studies and randomized trials.
What are my final arguments for diet being used as a treatment for IBD? With the exception of very restrictive ones, diets are generally safe. Of course, patients on restricted diets need monitoring for nutritional deficiencies, but this monitoring is likely less intense than that needed for many of our immunosuppressive therapies. Dietary therapies are not associated with an increase in risk of infections or malignancy (unlike our traditional immunosuppressive therapies), and consequently are much more likely to be accepted by our patients than what we are currently offering. In addition, the existing treatments are expensive and consequently difficult to sustain globally with the increasing burden of these diseases. On the other hand, as eating and dietary choices are a routine part of day-to-day life, dietary therapies are not likely to be associated with any excess costs.
Therefore, treating IBD with diet alone is supported by epidemiologic, mechanistic, and clinical evidence and is a safe, effective, and inexpensive alternative for our patients.
References
1. Zallot C et al. Inflamm Bowel Dis. 2013 Jan;19(1):66-72.
2. Sasson AN et al. Clin Gastroenterol Hepatol. 2019 Dec 5;S1542-3565(19)31394-1.
3. Wall CL et al. World J Gastroenterol. 2013;19:7652-60.
4. Svolos V et al. Gastroenterology. 2019;156:1354-67.e6.
5. Levine A et al. Gastroenterology. 2019;157:440-50.e8.
Dr. Ananthakrishnan is a gastroenterologist in the division of gastroenterology, Crohn’s and Colitis Center, Massachusetts General Hospital and Harvard Medical School, Boston. He is supported by funding from the Crohn’s and Colitis Foundation and the Chleck Family Foundation.
IBD can be treated with diet alone – No, it cannot!
The cause of IBD is not completely understood, but we believe something in our environment triggers a dysregulated immune response in individuals with a genetic predisposition to IBD. Among the environmental triggers commonly recognized, diet is considered an important trigger through its ability to affect the composition and health of the gut microbiome and host barrier function. Epidemiologic data support this assumption. Westernization of diet has been associated with the increasing incidence of IBD across the globe and in immigrants who move from developing countries to an industrialized country. Observational studies have shown diets higher in meat and polyunsaturated fatty acids and omega-6 fatty acids are associated with a higher risk for IBD, whereas diets high in fruits, vegetables, and other sources of dietary fiber have a lower risk of IBD.
A growing body of evidence supports the impact food can have on gut health, specifically in mouse IBD models, but it is challenging to translate findings from animal studies into dietary interventions for IBD patients. Mouse studies help us understand the mechanistic basis of how diet may affect IBD, but randomized clinical trials establishing their role in IBD are lacking. This is not surprising as dietary studies are challenging, particularly if done in a robust manner, given the difficulties of ensuring and measuring dietary compliance.
Exclusive enteral nutrition (EEN) has been studied the most rigorously of all diets in IBD and has demonstrated the greatest benefit, compared with other diet studies in IBD. EEN requires the intake of elemental, semi-elemental, or polymeric formulas to meet all nutritional requirements without additional intake of food for 6-8 weeks. Studies have been performed mostly in pediatric populations and have shown effectiveness in induction of remission with reduction in inflammatory markers, including C-reactive protein, erythrocyte sedimentation rate, and fecal calprotectin, and even mucosal healing. EEN has not worked out as well for adult populations, because of the poor tolerability of exclusive intake of enteral formulas. Because of this limitation, studies of partial enteral nutrition have been performed that generally allow some food intake in addition to the enteral nutrition. When compared with EEN or anti–tumor necrosis factor–alpha therapy, partial enteral nutrition is a less-effective treatment of Crohn’s disease; however, partial enteral nutrition does appear to improve clinical symptoms.
Beyond EEN, there are many diets that have been considered for the treatment of IBD, including the specific carbohydrate diet (SCD), Crohn’s disease exclusion diet, autoimmune diet, low FODMAP (fermentable oligo-, di-, mono-saccharides and polyols), Paleolithic diet, Mediterranean diet, and the semi-vegetarian diet, to name a few. Of these, only the SCD and Crohn’s disease exclusion diets have shown improvement in clinical remission and reduction in inflammatory markers.
The SCD diet is based on the theory that malabsorption of disaccharide and polysaccharide carbohydrates leads to bacterial overgrowth and host barrier dysfunction. This diet eliminates grains, dairy, processed meats, and certain vegetables such as potatoes, yams, and legumes. Small uncontrolled studies have shown improvement in symptoms and endoscopy findings. However, this restrictive diet is nearly impossible to follow long term. The Crohn’s disease exclusion diet is a whole foods diet avoiding all processed foods, animal fats, dairy, and gluten. Small studies of this diet have also shown improvement in clinical symptoms and inflammatory markers.
The plethora of studies and reports of the therapeutic effect of diet on IBD provide some promise of the benefit dietary modifications can bring to our IBD patients. However, most dietary studies are underpowered, lack a control arm, and do not include endoscopic endpoints. The current body of evidence remains insufficient to support the use of diet alone for the treatment of IBD. We need randomized clinical controlled trials that are held to the same rigor as those of our approved medical treatments for IBD. Although such trials are challenging, we’ve seen groups rise to the task to carry out more robust dietary studies in the IBD population, and we await the results of several ongoing trials.
IBD is a challenging disease to live with and often leaves our patients feeling out of control. Dietary choices provide an avenue for patients to have some control of their health. However, current evidence does not support the prescription of dietary interventions alone to treat IBD, particularly when we have known, effective therapies. While I am not ready to prescribe diet as a stand-alone treatment for IBD, I make a point to discuss the role diet may play in helping our patients achieve optimal health. As health care providers, it is our responsibility to provide holistic care to our patients, which includes promotion of a healthy diet, absent processed foods and added sugars. Healthy lifestyle choices combined with effective medical and surgical treatments offer our patients the best shot at sustained disease control.
References
1. Hou JK et al. Am J Gastroenterol. 2011;106(4):563-73.
2. Zachos M et al. Cochrane Database Syst Rev. 2007(1):CD000542.
3. Lee D et al. Inflamm Bowel Dis. 2015;21(8):1786-93.
4. Obih C et al. Nutrition. 2016;32(4):418-25.
5. Sigall Boneh R et al. J Crohns Colitis. 2017;11(10):1205-12.
Dr. Raffals is a gastroenterologist in the division of gastroenterology and hepatology, Mayo Clinic, Rochester, Minn. She has no financial conflicts of interest relevant to this paper.
Dear colleagues and friends,
Thank you for your continued interest and support of the Perspectives debates. In this edition, Dr. Ashwin Ananthakrishnan and Dr. Laura Raffals explore the controversial topic of diet-based therapy in inflammatory bowel disease, highlights of the rationales for and against, and the current state of the evidence. All gastroenterologists frequently face questions pertaining to diet and its purported effects on digestive health. I found the discussion relevant to my own general practice, and I hope you will enjoy reading it as much as I did. As always, I welcome your comments and suggestions for future topics at [email protected].
Charles Kahi, MD, MS, AGAF, professor of medicine, Indiana University, Indianapolis. He is also an associate editor for GI & Hepatology News.
IBD can be treated with diet alone
Inflammatory bowel diseases (IBD), comprising Crohn’s disease and ulcerative colitis, have emerged as global diseases. The past 3 decades have seen a rising incidence of these diseases not just in the Western hemisphere, where their prevalence has been well recognized, but also in regions of the world such as Asia and South America where they were previously rare. Whereas several possible factors have been proposed to explain this rising incidence and globalization of disease with varying degrees of supportive evidence, one of the most likely factors is a changing diet. Over the same period that the disease incidence and prevalence have risen, diets worldwide have converged with several common trends observed across countries and continents. These include reductions in dietary fiber, fruits, and vegetables, and increased intake of processed food, animal protein, fats, and sugary drinks, all of which have been linked epidemiologically to Crohn’s disease.
Treatment of Crohn’s disease and ulcerative colitis over the past 2 decades has focused on the immunologic dysfunction observed in these patients. Successful treatment has relied on suppressing immune responses either broadly or through targeted suppression of specific immunologic pathways. By and large, whereas these approaches have enabled us to make significant progress in reducing disease-related morbidity, success has been moderate at best, with fewer than half of patients in any clinical trial achieving remission at the end of a year. Thus, this approach alone may not be sufficient for most patients with IBD.
Treatment of IBD with diet was long considered out of the mainstream and confined to the realm of anecdotes and message boards. Despite most patients believing that diet played a role in development of IBD and onset of flares and that dietary modification was helpful in relieving symptoms, physicians – who for the most part were not trained in these approaches – were not believers, and probably rightly so in the absence of any supporting data.1 However, the parallel emergence of three bodies of literature has now brought diet back into the mainstream of IBD care (such that not a single IBD conference goes by without at least a session or two on diet). First, large prospective cohorts from Europe and North America provided robust evidence linking long-term adult dietary patterns to disease incidence in adult-onset IBD, which supports many important case-control observations made over the past 2 decades.2 Second, and perhaps most important, we began understanding the role of the microbiome in the development of these diseases and recognizing its centrality to bowel inflammation. One of the key determinants of the microbiome is diet, exerting both short-term and long-term influences on the microbial structure. While microbial changes are by no means the only mechanism through which diet can influence intestinal inflammation, they are among the most important, with broad effects across many dietary components. These findings provided a robust scientific basis for investigating the role of diet. Third, while still far from the high-quality (and expensive) set-up of investigational trials of pharmacologic therapies, dietary therapy studies have also evolved to randomized controlled trial designs and investigation of mechanism-driven dietary combinations. Together, I think these three recent advances, in addition to the wealth of existing literature and anecdotal experience, have been important in moving diet (back) into the IBD mainstream.
So what evidence is there that diet is effective in the treatment of IBD? Randomized controlled trials published more than a decade ago demonstrated that exclusive enteral nutrition, wherein all table foods are eliminated from a diet and the patient relies on an elemental diet alone for nutrition, was effective in not just inducing clinical remission but also improving inflammatory biomarkers.3 With results replicated in several trials, exclusive enteral nutrition is, in many parts of the world, one of the first-line treatments for pediatric Crohn’s disease. That this has not been translated to longer-term maintenance therapy is not necessarily an indicator of lack of durable efficacy, but reflects the challenges of maintaining such a restrictive diet long term while living an active, normal life. However, more recent rigorous studies have demonstrated that the effects of exclusive enteral nutrition can be mimicked either by a selected, less-restrictive diet (such as CD-TREAT4), which is more sustainable, or by combining partial enteral nutrition with an elimination diet that is quite diverse (such as CDED5). The latter two are considerably more promising as longer-term dietary treatments for Crohn’s disease with durable efficacy in open-label studies and randomized trials.
What are my final arguments for diet being used as a treatment for IBD? With the exception of very restrictive ones, diets are generally safe. Of course, patients on restricted diets need monitoring for nutritional deficiencies, but this monitoring is likely less intense than that needed for many of our immunosuppressive therapies. Dietary therapies are not associated with an increase in risk of infections or malignancy (unlike our traditional immunosuppressive therapies), and consequently are much more likely to be accepted by our patients than what we are currently offering. In addition, the existing treatments are expensive and consequently difficult to sustain globally with the increasing burden of these diseases. On the other hand, as eating and dietary choices are a routine part of day-to-day life, dietary therapies are not likely to be associated with any excess costs.
Therefore, treating IBD with diet alone is supported by epidemiologic, mechanistic, and clinical evidence and is a safe, effective, and inexpensive alternative for our patients.
References
1. Zallot C et al. Inflamm Bowel Dis. 2013 Jan;19(1):66-72.
2. Sasson AN et al. Clin Gastroenterol Hepatol. 2019 Dec 5;S1542-3565(19)31394-1.
3. Wall CL et al. World J Gastroenterol. 2013;19:7652-60.
4. Svolos V et al. Gastroenterology. 2019;156:1354-67.e6.
5. Levine A et al. Gastroenterology. 2019;157:440-50.e8.
Dr. Ananthakrishnan is a gastroenterologist in the division of gastroenterology, Crohn’s and Colitis Center, Massachusetts General Hospital and Harvard Medical School, Boston. He is supported by funding from the Crohn’s and Colitis Foundation and the Chleck Family Foundation.
IBD can be treated with diet alone – No, it cannot!
The cause of IBD is not completely understood, but we believe something in our environment triggers a dysregulated immune response in individuals with a genetic predisposition to IBD. Among the environmental triggers commonly recognized, diet is considered an important trigger through its ability to affect the composition and health of the gut microbiome and host barrier function. Epidemiologic data support this assumption. Westernization of diet has been associated with the increasing incidence of IBD across the globe and in immigrants who move from developing countries to an industrialized country. Observational studies have shown diets higher in meat and polyunsaturated fatty acids and omega-6 fatty acids are associated with a higher risk for IBD, whereas diets high in fruits, vegetables, and other sources of dietary fiber have a lower risk of IBD.
A growing body of evidence supports the impact food can have on gut health, specifically in mouse IBD models, but it is challenging to translate findings from animal studies into dietary interventions for IBD patients. Mouse studies help us understand the mechanistic basis of how diet may affect IBD, but randomized clinical trials establishing their role in IBD are lacking. This is not surprising as dietary studies are challenging, particularly if done in a robust manner, given the difficulties of ensuring and measuring dietary compliance.
Exclusive enteral nutrition (EEN) has been studied the most rigorously of all diets in IBD and has demonstrated the greatest benefit, compared with other diet studies in IBD. EEN requires the intake of elemental, semi-elemental, or polymeric formulas to meet all nutritional requirements without additional intake of food for 6-8 weeks. Studies have been performed mostly in pediatric populations and have shown effectiveness in induction of remission with reduction in inflammatory markers, including C-reactive protein, erythrocyte sedimentation rate, and fecal calprotectin, and even mucosal healing. EEN has not worked out as well for adult populations, because of the poor tolerability of exclusive intake of enteral formulas. Because of this limitation, studies of partial enteral nutrition have been performed that generally allow some food intake in addition to the enteral nutrition. When compared with EEN or anti–tumor necrosis factor–alpha therapy, partial enteral nutrition is a less-effective treatment of Crohn’s disease; however, partial enteral nutrition does appear to improve clinical symptoms.
Beyond EEN, there are many diets that have been considered for the treatment of IBD, including the specific carbohydrate diet (SCD), Crohn’s disease exclusion diet, autoimmune diet, low FODMAP (fermentable oligo-, di-, mono-saccharides and polyols), Paleolithic diet, Mediterranean diet, and the semi-vegetarian diet, to name a few. Of these, only the SCD and Crohn’s disease exclusion diets have shown improvement in clinical remission and reduction in inflammatory markers.
The SCD diet is based on the theory that malabsorption of disaccharide and polysaccharide carbohydrates leads to bacterial overgrowth and host barrier dysfunction. This diet eliminates grains, dairy, processed meats, and certain vegetables such as potatoes, yams, and legumes. Small uncontrolled studies have shown improvement in symptoms and endoscopy findings. However, this restrictive diet is nearly impossible to follow long term. The Crohn’s disease exclusion diet is a whole foods diet avoiding all processed foods, animal fats, dairy, and gluten. Small studies of this diet have also shown improvement in clinical symptoms and inflammatory markers.
The plethora of studies and reports of the therapeutic effect of diet on IBD provide some promise of the benefit dietary modifications can bring to our IBD patients. However, most dietary studies are underpowered, lack a control arm, and do not include endoscopic endpoints. The current body of evidence remains insufficient to support the use of diet alone for the treatment of IBD. We need randomized clinical controlled trials that are held to the same rigor as those of our approved medical treatments for IBD. Although such trials are challenging, we’ve seen groups rise to the task to carry out more robust dietary studies in the IBD population, and we await the results of several ongoing trials.
IBD is a challenging disease to live with and often leaves our patients feeling out of control. Dietary choices provide an avenue for patients to have some control of their health. However, current evidence does not support the prescription of dietary interventions alone to treat IBD, particularly when we have known, effective therapies. While I am not ready to prescribe diet as a stand-alone treatment for IBD, I make a point to discuss the role diet may play in helping our patients achieve optimal health. As health care providers, it is our responsibility to provide holistic care to our patients, which includes promotion of a healthy diet, absent processed foods and added sugars. Healthy lifestyle choices combined with effective medical and surgical treatments offer our patients the best shot at sustained disease control.
References
1. Hou JK et al. Am J Gastroenterol. 2011;106(4):563-73.
2. Zachos M et al. Cochrane Database Syst Rev. 2007(1):CD000542.
3. Lee D et al. Inflamm Bowel Dis. 2015;21(8):1786-93.
4. Obih C et al. Nutrition. 2016;32(4):418-25.
5. Sigall Boneh R et al. J Crohns Colitis. 2017;11(10):1205-12.
Dr. Raffals is a gastroenterologist in the division of gastroenterology and hepatology, Mayo Clinic, Rochester, Minn. She has no financial conflicts of interest relevant to this paper.
Direct-acting agents cure hepatitis C in children
Between 23,000 and 46,000 U.S. children live with chronic hepatitis C virus with a prevalence of 0.17% anti–hepatitis C virus (HCV) antibody positivity in those aged 6-11 years and 0.39% among children aged 12-19 years. In the United States, genotype 1 is most frequent, followed by genotypes 2 and 3. About 99% of cases result from vertical transmission; transfusion-related cases have not been observed in recent decades.Only viremic mothers are at risk of transmission as those who have spontaneously cleared HCV viremia or have been treated successfully do not risk transmission. Maternal HCV viral load appears to be a risk factor for HCV transmission, however transmission is reported at all levels of viremia.
In conjunction with the opioid epidemics, the prevalence of HCV infection has increased over the last decade. The Centers for Disease Control and Prevention reported that, between 2009 and 2014, the prevalence of HCV infection increased from 1.8 to 3.4 per 1,000 live births. They identified substantial state-to-state variation with the highest rate in West Virginia (22.6 per 1,000 live births), and the lowest in Hawaii (0.7 per 1,000 live births). The implications are clear that increasing numbers of newborns are exposed to HCV and, if transmission rates are between 1% and 5%, 80-400 U.S. infants each year acquire HCV infection.
HCV in children
HCV in children is almost always associated with persistent transaminitis. Chronic infection is defined as the persistence of HCV RNA for at least 6 months, and clearance of HCV infection is determined by the persistent disappearance of HCV RNA. Regardless of infection status, an infant may have detectable maternal anti-HCV antibody in serum until 18 months of age, resulting from passive transfer. In addition, prolonged infection can lead to cirrhosis, hepatocellular carcinoma, or decompensated liver disease. Potential extrahepatic manifestations including reduced physical and psychosocial health also are linked to chronic HCV. Autoimmune disease also has been reported in children with HCV. As well, the stigma of HCV elicits fear in school and child care settings that is a result of public misunderstanding regarding routes of hepatitis C transmission. No restriction of regular childhood activities is required in the daily life of HCV-infected children.
Taken together, increasing rates of HCV infection in pregnant women, increasing numbers of exposed and infected infants annually, potential for both short- and long-term morbidity, and curative nontoxic treatment,
Screening for HCV
There is considerable discussion about which strategy for screening of at-risk infants is more appropriate. Some groups advocate for HCV-RNA testing within the first year of life. Proponents argue the use of a highly sensitive RNA assay early in life has potential to increase detection of infected infants while a negative result allows the conclusion the infant is not infected. Advocates hypothesize that early identification has potential to improve continued follow-up.
Opponents argue that early testing does not change the need for repeat testing after 18 months to confirm diagnosis. They also argue that HCV RNA is more expensive than an antibody-based testing; and treatment will not begin prior to age 3 as there is still opportunity for viremia to spontaneously clear.
Direct acting agents licensed
Ledipasvir/sofosbuvir (Harvoni) was initially demonstrated as curative for genotype 1, 4, 5, or 6 infection in a phase 2, multicenter, open-label study of 100 adolescents with genotype 1 treated for 12 weeks. Sustained virologic response (SVR) was documented in 98% of participants.The regimen was safe and well tolerated in this population, and the adult dosage formulation resulted in pharmacokinetic characteristics similar to those observed in adults. Two clinical trials supported the efficacy of ledipasvir/sofosbuvir in the pediatric population aged 3-11 years. This regimen also is recommended for interferon-experienced (± ribavirin, with or without an HCV protease inhibitor) children and adolescents aged 3 years or older with genotype 1 or 4. A 12-week course is recommended for patients without cirrhosis; 24 weeks is recommended for those with compensated cirrhosis. The combination of ledipasvir/sofosbuvir is the only treatment option for children aged 3-6 years with genotype 1, 4, 5, or 6 infection.
The efficacy of sofosbuvir/velpatasvir (Epclusa) once daily for 12 weeks was first evaluated in an open-label trial among children aged 6 years and older with genotype 1, 2, 3, 4, or 6 infection, without cirrhosis or with compensated cirrhosis. Subsequently, the “cocktail” was evaluated in children aged 6-12 years, with 76% genotype 1, 3% genotype 2, 15% genotype 3, and 6% genotype 4. SVR12 rates were 93% (50/54) in children with genotype 1, 91% (10/11) in those with genotype 3, and 100% in participants with genotype 2 (2/2) or genotype 4 (4/4). Sofosbuvir/velpatasvir was approved in March 2020 by the Food and Drug Administration for pediatric patients aged 6 years and older. Given its pangenotypic activity, safety, and efficacy, sofosbuvir/velpatasvir is currently recommended as a first choice for HCV treatment in children and adolescents aged at least 6 years.
The daily fixed-dose combination of glecaprevir/pibrentasvir (Mavyret) was approved in April 2019 for adolescents aged 12-17 years, and weighing at least 45 kg.Treatment is for 8 weeks, and includes treatment-naive patients without cirrhosis or those with compensated cirrhosis. SVR12 rates for Mavyret have ranged from 91% to 100 % across clinic trials. FDA approval and HCV guideline treatment recommendations for direct-acting antiviral (DAA)–experienced adolescents are based on clinical trial data from adults. Given its pangenotypic activity, safety, and efficacy record in adult patients, glecaprevir/pibrentasvir is recommended as a first choice for adolescent HCV treatment. Glecaprevir/pibrentasvir once approved for children less than 3 years of age will be safe and efficacious as a pangenotypic treatment option in children with chronic HCV infection.
Current recommendations
Tools for identifying HCV infected infants as early as a few months of age are available, yet studies demonstrate that a minority of at-risk children are tested for HCV using either an HCV polymerase chain reaction strategy early in life or an anti-HCV antibody strategy after 18 months of age.
Therapy with direct-acting agents is now licensed to those aged 3 years and offers the potential for cure, eliminating concern for possible progression after prolonged infection. Such therapy offers the potential to eliminate the stigma faced by many children as well as the hepatic and extrahepatic manifestations observed in children. Medication formulation and the child’s abilities to take the medication needs to be considered when prescribing DAAs. It is important to assess if the child can successfully swallow pills. Currently, Harvoni is the only medication that comes in both pellet and pill formulations. The dose is based on weight. The pellets need to be given in a small amount of nonacidic food; they cannot be chewed.
All children with chronic HCV infection are candidates for treatment. When significant fibrosis and/or cirrhosis is present treatment should not be delayed once the child is age 3 years; when only transaminitis is present, treatment can be delayed. In our experience, parents are eager to complete treatment before starting kindergarten.
Liver biopsy for obtaining liver tissue for histopathologic examination is not routinely indicated in children with chronic HCV infection but should be evaluated case by case. Noninvasive tests of hepatic fibrosis have been used in children, these include serologic markers (i.e., FibroSure) and radiologic tests such as ultrasound-based transient elastography (i.e., Fibroscan). Validation for pediatric patients is variable for the different serologic tests. Studies have shown that Fibroscan using the M probe is feasible for a wide range of ages, but poor patient cooperation may make measurement difficult.
Further details regarding dosing and choice of formulation is available at https://www.hcvguidelines.org/unique-populations/children.
Dr. Sabharwal is assistant professor of pediatrics at Boston University and attending physician in pediatric infectious diseases at Boston Medical Center. Ms. Moloney is an instructor in pediatrics at Boston University and a pediatric nurse practitioner in pediatric infectious diseases at Boston Medicine Center. Dr. Pelton is professor of pediatrics and epidemiology at Boston University and public health and senior attending physician at Boston Medical Center. Boston Medical Center received funding from AbbVie for study of Harvoni in Children 3 years of age and older. Email them at [email protected].
References
MMWR Morb Mortal Wkly Rep. 2017 May 12;66(18):470-3. Hepatol Commun. 2017 March 23. doi: 10.1002/hep4.1028. Hepatology. 2020 Feb;71(2):422-30. Lancet Gastroenterol Hepatol. 2019 Apr 11. doi: 10.1016/S2468-1253(19)30046-9. Arch Dis Child. 2006 Sep;91(9):781-5. J Pediatr Gastroenterol Nutr. 2010 Feb;50(2):123-31.
Between 23,000 and 46,000 U.S. children live with chronic hepatitis C virus with a prevalence of 0.17% anti–hepatitis C virus (HCV) antibody positivity in those aged 6-11 years and 0.39% among children aged 12-19 years. In the United States, genotype 1 is most frequent, followed by genotypes 2 and 3. About 99% of cases result from vertical transmission; transfusion-related cases have not been observed in recent decades.Only viremic mothers are at risk of transmission as those who have spontaneously cleared HCV viremia or have been treated successfully do not risk transmission. Maternal HCV viral load appears to be a risk factor for HCV transmission, however transmission is reported at all levels of viremia.
In conjunction with the opioid epidemics, the prevalence of HCV infection has increased over the last decade. The Centers for Disease Control and Prevention reported that, between 2009 and 2014, the prevalence of HCV infection increased from 1.8 to 3.4 per 1,000 live births. They identified substantial state-to-state variation with the highest rate in West Virginia (22.6 per 1,000 live births), and the lowest in Hawaii (0.7 per 1,000 live births). The implications are clear that increasing numbers of newborns are exposed to HCV and, if transmission rates are between 1% and 5%, 80-400 U.S. infants each year acquire HCV infection.
HCV in children
HCV in children is almost always associated with persistent transaminitis. Chronic infection is defined as the persistence of HCV RNA for at least 6 months, and clearance of HCV infection is determined by the persistent disappearance of HCV RNA. Regardless of infection status, an infant may have detectable maternal anti-HCV antibody in serum until 18 months of age, resulting from passive transfer. In addition, prolonged infection can lead to cirrhosis, hepatocellular carcinoma, or decompensated liver disease. Potential extrahepatic manifestations including reduced physical and psychosocial health also are linked to chronic HCV. Autoimmune disease also has been reported in children with HCV. As well, the stigma of HCV elicits fear in school and child care settings that is a result of public misunderstanding regarding routes of hepatitis C transmission. No restriction of regular childhood activities is required in the daily life of HCV-infected children.
Taken together, increasing rates of HCV infection in pregnant women, increasing numbers of exposed and infected infants annually, potential for both short- and long-term morbidity, and curative nontoxic treatment,
Screening for HCV
There is considerable discussion about which strategy for screening of at-risk infants is more appropriate. Some groups advocate for HCV-RNA testing within the first year of life. Proponents argue the use of a highly sensitive RNA assay early in life has potential to increase detection of infected infants while a negative result allows the conclusion the infant is not infected. Advocates hypothesize that early identification has potential to improve continued follow-up.
Opponents argue that early testing does not change the need for repeat testing after 18 months to confirm diagnosis. They also argue that HCV RNA is more expensive than an antibody-based testing; and treatment will not begin prior to age 3 as there is still opportunity for viremia to spontaneously clear.
Direct acting agents licensed
Ledipasvir/sofosbuvir (Harvoni) was initially demonstrated as curative for genotype 1, 4, 5, or 6 infection in a phase 2, multicenter, open-label study of 100 adolescents with genotype 1 treated for 12 weeks. Sustained virologic response (SVR) was documented in 98% of participants.The regimen was safe and well tolerated in this population, and the adult dosage formulation resulted in pharmacokinetic characteristics similar to those observed in adults. Two clinical trials supported the efficacy of ledipasvir/sofosbuvir in the pediatric population aged 3-11 years. This regimen also is recommended for interferon-experienced (± ribavirin, with or without an HCV protease inhibitor) children and adolescents aged 3 years or older with genotype 1 or 4. A 12-week course is recommended for patients without cirrhosis; 24 weeks is recommended for those with compensated cirrhosis. The combination of ledipasvir/sofosbuvir is the only treatment option for children aged 3-6 years with genotype 1, 4, 5, or 6 infection.
The efficacy of sofosbuvir/velpatasvir (Epclusa) once daily for 12 weeks was first evaluated in an open-label trial among children aged 6 years and older with genotype 1, 2, 3, 4, or 6 infection, without cirrhosis or with compensated cirrhosis. Subsequently, the “cocktail” was evaluated in children aged 6-12 years, with 76% genotype 1, 3% genotype 2, 15% genotype 3, and 6% genotype 4. SVR12 rates were 93% (50/54) in children with genotype 1, 91% (10/11) in those with genotype 3, and 100% in participants with genotype 2 (2/2) or genotype 4 (4/4). Sofosbuvir/velpatasvir was approved in March 2020 by the Food and Drug Administration for pediatric patients aged 6 years and older. Given its pangenotypic activity, safety, and efficacy, sofosbuvir/velpatasvir is currently recommended as a first choice for HCV treatment in children and adolescents aged at least 6 years.
The daily fixed-dose combination of glecaprevir/pibrentasvir (Mavyret) was approved in April 2019 for adolescents aged 12-17 years, and weighing at least 45 kg.Treatment is for 8 weeks, and includes treatment-naive patients without cirrhosis or those with compensated cirrhosis. SVR12 rates for Mavyret have ranged from 91% to 100 % across clinic trials. FDA approval and HCV guideline treatment recommendations for direct-acting antiviral (DAA)–experienced adolescents are based on clinical trial data from adults. Given its pangenotypic activity, safety, and efficacy record in adult patients, glecaprevir/pibrentasvir is recommended as a first choice for adolescent HCV treatment. Glecaprevir/pibrentasvir once approved for children less than 3 years of age will be safe and efficacious as a pangenotypic treatment option in children with chronic HCV infection.
Current recommendations
Tools for identifying HCV infected infants as early as a few months of age are available, yet studies demonstrate that a minority of at-risk children are tested for HCV using either an HCV polymerase chain reaction strategy early in life or an anti-HCV antibody strategy after 18 months of age.
Therapy with direct-acting agents is now licensed to those aged 3 years and offers the potential for cure, eliminating concern for possible progression after prolonged infection. Such therapy offers the potential to eliminate the stigma faced by many children as well as the hepatic and extrahepatic manifestations observed in children. Medication formulation and the child’s abilities to take the medication needs to be considered when prescribing DAAs. It is important to assess if the child can successfully swallow pills. Currently, Harvoni is the only medication that comes in both pellet and pill formulations. The dose is based on weight. The pellets need to be given in a small amount of nonacidic food; they cannot be chewed.
All children with chronic HCV infection are candidates for treatment. When significant fibrosis and/or cirrhosis is present treatment should not be delayed once the child is age 3 years; when only transaminitis is present, treatment can be delayed. In our experience, parents are eager to complete treatment before starting kindergarten.
Liver biopsy for obtaining liver tissue for histopathologic examination is not routinely indicated in children with chronic HCV infection but should be evaluated case by case. Noninvasive tests of hepatic fibrosis have been used in children, these include serologic markers (i.e., FibroSure) and radiologic tests such as ultrasound-based transient elastography (i.e., Fibroscan). Validation for pediatric patients is variable for the different serologic tests. Studies have shown that Fibroscan using the M probe is feasible for a wide range of ages, but poor patient cooperation may make measurement difficult.
Further details regarding dosing and choice of formulation is available at https://www.hcvguidelines.org/unique-populations/children.
Dr. Sabharwal is assistant professor of pediatrics at Boston University and attending physician in pediatric infectious diseases at Boston Medical Center. Ms. Moloney is an instructor in pediatrics at Boston University and a pediatric nurse practitioner in pediatric infectious diseases at Boston Medicine Center. Dr. Pelton is professor of pediatrics and epidemiology at Boston University and public health and senior attending physician at Boston Medical Center. Boston Medical Center received funding from AbbVie for study of Harvoni in Children 3 years of age and older. Email them at [email protected].
References
MMWR Morb Mortal Wkly Rep. 2017 May 12;66(18):470-3. Hepatol Commun. 2017 March 23. doi: 10.1002/hep4.1028. Hepatology. 2020 Feb;71(2):422-30. Lancet Gastroenterol Hepatol. 2019 Apr 11. doi: 10.1016/S2468-1253(19)30046-9. Arch Dis Child. 2006 Sep;91(9):781-5. J Pediatr Gastroenterol Nutr. 2010 Feb;50(2):123-31.
Between 23,000 and 46,000 U.S. children live with chronic hepatitis C virus with a prevalence of 0.17% anti–hepatitis C virus (HCV) antibody positivity in those aged 6-11 years and 0.39% among children aged 12-19 years. In the United States, genotype 1 is most frequent, followed by genotypes 2 and 3. About 99% of cases result from vertical transmission; transfusion-related cases have not been observed in recent decades.Only viremic mothers are at risk of transmission as those who have spontaneously cleared HCV viremia or have been treated successfully do not risk transmission. Maternal HCV viral load appears to be a risk factor for HCV transmission, however transmission is reported at all levels of viremia.
In conjunction with the opioid epidemics, the prevalence of HCV infection has increased over the last decade. The Centers for Disease Control and Prevention reported that, between 2009 and 2014, the prevalence of HCV infection increased from 1.8 to 3.4 per 1,000 live births. They identified substantial state-to-state variation with the highest rate in West Virginia (22.6 per 1,000 live births), and the lowest in Hawaii (0.7 per 1,000 live births). The implications are clear that increasing numbers of newborns are exposed to HCV and, if transmission rates are between 1% and 5%, 80-400 U.S. infants each year acquire HCV infection.
HCV in children
HCV in children is almost always associated with persistent transaminitis. Chronic infection is defined as the persistence of HCV RNA for at least 6 months, and clearance of HCV infection is determined by the persistent disappearance of HCV RNA. Regardless of infection status, an infant may have detectable maternal anti-HCV antibody in serum until 18 months of age, resulting from passive transfer. In addition, prolonged infection can lead to cirrhosis, hepatocellular carcinoma, or decompensated liver disease. Potential extrahepatic manifestations including reduced physical and psychosocial health also are linked to chronic HCV. Autoimmune disease also has been reported in children with HCV. As well, the stigma of HCV elicits fear in school and child care settings that is a result of public misunderstanding regarding routes of hepatitis C transmission. No restriction of regular childhood activities is required in the daily life of HCV-infected children.
Taken together, increasing rates of HCV infection in pregnant women, increasing numbers of exposed and infected infants annually, potential for both short- and long-term morbidity, and curative nontoxic treatment,
Screening for HCV
There is considerable discussion about which strategy for screening of at-risk infants is more appropriate. Some groups advocate for HCV-RNA testing within the first year of life. Proponents argue the use of a highly sensitive RNA assay early in life has potential to increase detection of infected infants while a negative result allows the conclusion the infant is not infected. Advocates hypothesize that early identification has potential to improve continued follow-up.
Opponents argue that early testing does not change the need for repeat testing after 18 months to confirm diagnosis. They also argue that HCV RNA is more expensive than an antibody-based testing; and treatment will not begin prior to age 3 as there is still opportunity for viremia to spontaneously clear.
Direct acting agents licensed
Ledipasvir/sofosbuvir (Harvoni) was initially demonstrated as curative for genotype 1, 4, 5, or 6 infection in a phase 2, multicenter, open-label study of 100 adolescents with genotype 1 treated for 12 weeks. Sustained virologic response (SVR) was documented in 98% of participants.The regimen was safe and well tolerated in this population, and the adult dosage formulation resulted in pharmacokinetic characteristics similar to those observed in adults. Two clinical trials supported the efficacy of ledipasvir/sofosbuvir in the pediatric population aged 3-11 years. This regimen also is recommended for interferon-experienced (± ribavirin, with or without an HCV protease inhibitor) children and adolescents aged 3 years or older with genotype 1 or 4. A 12-week course is recommended for patients without cirrhosis; 24 weeks is recommended for those with compensated cirrhosis. The combination of ledipasvir/sofosbuvir is the only treatment option for children aged 3-6 years with genotype 1, 4, 5, or 6 infection.
The efficacy of sofosbuvir/velpatasvir (Epclusa) once daily for 12 weeks was first evaluated in an open-label trial among children aged 6 years and older with genotype 1, 2, 3, 4, or 6 infection, without cirrhosis or with compensated cirrhosis. Subsequently, the “cocktail” was evaluated in children aged 6-12 years, with 76% genotype 1, 3% genotype 2, 15% genotype 3, and 6% genotype 4. SVR12 rates were 93% (50/54) in children with genotype 1, 91% (10/11) in those with genotype 3, and 100% in participants with genotype 2 (2/2) or genotype 4 (4/4). Sofosbuvir/velpatasvir was approved in March 2020 by the Food and Drug Administration for pediatric patients aged 6 years and older. Given its pangenotypic activity, safety, and efficacy, sofosbuvir/velpatasvir is currently recommended as a first choice for HCV treatment in children and adolescents aged at least 6 years.
The daily fixed-dose combination of glecaprevir/pibrentasvir (Mavyret) was approved in April 2019 for adolescents aged 12-17 years, and weighing at least 45 kg.Treatment is for 8 weeks, and includes treatment-naive patients without cirrhosis or those with compensated cirrhosis. SVR12 rates for Mavyret have ranged from 91% to 100 % across clinic trials. FDA approval and HCV guideline treatment recommendations for direct-acting antiviral (DAA)–experienced adolescents are based on clinical trial data from adults. Given its pangenotypic activity, safety, and efficacy record in adult patients, glecaprevir/pibrentasvir is recommended as a first choice for adolescent HCV treatment. Glecaprevir/pibrentasvir once approved for children less than 3 years of age will be safe and efficacious as a pangenotypic treatment option in children with chronic HCV infection.
Current recommendations
Tools for identifying HCV infected infants as early as a few months of age are available, yet studies demonstrate that a minority of at-risk children are tested for HCV using either an HCV polymerase chain reaction strategy early in life or an anti-HCV antibody strategy after 18 months of age.
Therapy with direct-acting agents is now licensed to those aged 3 years and offers the potential for cure, eliminating concern for possible progression after prolonged infection. Such therapy offers the potential to eliminate the stigma faced by many children as well as the hepatic and extrahepatic manifestations observed in children. Medication formulation and the child’s abilities to take the medication needs to be considered when prescribing DAAs. It is important to assess if the child can successfully swallow pills. Currently, Harvoni is the only medication that comes in both pellet and pill formulations. The dose is based on weight. The pellets need to be given in a small amount of nonacidic food; they cannot be chewed.
All children with chronic HCV infection are candidates for treatment. When significant fibrosis and/or cirrhosis is present treatment should not be delayed once the child is age 3 years; when only transaminitis is present, treatment can be delayed. In our experience, parents are eager to complete treatment before starting kindergarten.
Liver biopsy for obtaining liver tissue for histopathologic examination is not routinely indicated in children with chronic HCV infection but should be evaluated case by case. Noninvasive tests of hepatic fibrosis have been used in children, these include serologic markers (i.e., FibroSure) and radiologic tests such as ultrasound-based transient elastography (i.e., Fibroscan). Validation for pediatric patients is variable for the different serologic tests. Studies have shown that Fibroscan using the M probe is feasible for a wide range of ages, but poor patient cooperation may make measurement difficult.
Further details regarding dosing and choice of formulation is available at https://www.hcvguidelines.org/unique-populations/children.
Dr. Sabharwal is assistant professor of pediatrics at Boston University and attending physician in pediatric infectious diseases at Boston Medical Center. Ms. Moloney is an instructor in pediatrics at Boston University and a pediatric nurse practitioner in pediatric infectious diseases at Boston Medicine Center. Dr. Pelton is professor of pediatrics and epidemiology at Boston University and public health and senior attending physician at Boston Medical Center. Boston Medical Center received funding from AbbVie for study of Harvoni in Children 3 years of age and older. Email them at [email protected].
References
MMWR Morb Mortal Wkly Rep. 2017 May 12;66(18):470-3. Hepatol Commun. 2017 March 23. doi: 10.1002/hep4.1028. Hepatology. 2020 Feb;71(2):422-30. Lancet Gastroenterol Hepatol. 2019 Apr 11. doi: 10.1016/S2468-1253(19)30046-9. Arch Dis Child. 2006 Sep;91(9):781-5. J Pediatr Gastroenterol Nutr. 2010 Feb;50(2):123-31.
Establishing a strong and lasting mentor/mentee relationship
I. Finding a mentor
Case
You are a 27-year-old first-year resident who is seeking mentorship. You are halfway through the year and are thinking about your goals and future. You have a general interest in hematology/oncology but have limited experience and would like to gain more experience with clinically relevant scholarship. However, you do not know anyone in the field and are not sure who to ask for guidance.
Stage 1: Seeking the right mentor
Start first with your area of interest and then look broadly. In this case the resident is interested in heme/onc. The first place to look is on the heme/onc department website or in the faculty directory. It can be helpful to look at what the potential mentor has published recently and/or look at a version of their CV on the faculty directory or website. This can help determine how productive they are and help assess whether you share similar interests, and whether they have worked with many learners in the past.
It is also important to do some background work and ask around about potential mentors. Often resident colleagues and fellows have a good sense of current projects and which faculty work well with learners. Lastly, it is important to also look at non–heme/onc physicians as there may be internal medicine physicians or surgeons who are doing hematology or oncology research that more align with your interests.
After you have assessed whether you think this person would be a strong mentor for you, it is time to reach out. People are flattered to be asked and part of their promotion criteria is their ability to mentor. Do not assume that a potential mentor is too busy! Let him or her make that decision. Remember the worst a mentor can say is “no.” Even if they do not have time or the need for a mentee at the present time, they generally will offer some assistance or direction on who to ask.
Start with a straightforward, but pleasant email. Waiting up to 2 weeks for a response is reasonable. If after 2 weeks you have not received word, feel free to reach out again asking politely if he or she would be willing to work with you. Do not be afraid to ask bluntly for their guidance and mentorship and have a specific project or area of research that you would like their assistance with.
II. Optimizing the mentor/mentee relationship
Case continued
Success! Your email was received with interest by a hematologist who has done several projects, comes highly recommended by other residents, and worked with students and residents in the past. The project involves anticoagulation on the inpatient service. You are set to meet with her next month.
Stage 2: Establishing expectations and goals
Now comes the hard work in establishing an excellent mentor/mentee relationship. Before you meet with your mentor, brainstorm first. What do you want out of the relationship? A publication? Career advice? Attaining a fellowship position? You should feel empowered in knowing that you as the mentee are in the driver seat, but this relationship should be mutually beneficial. Consider basing the relationship and initial discussions on these key questions:
1. My goals
- What are my goals? It is okay not to know but be ready to communicate some information to your mentor.
- Remember to also ask your mentor what their goals are for you as well.
2. Outcome
- What type of outcome are both you and your mentor looking for from the relationship?
3. Expectations
- What mentorship expectations do you have?
- What are your mentor’s expectations of you?
Once you feel you have a sense of what you are looking for out of the relationship, it is important to communicate this with the mentor to establish congruent expectations of one another. For example, think about asking your mentor if the two of you can establish a mentor/mentee contract. This is a written document that can be found online and establishes a mutual agreement of roles, responsibilities, and expectations of one another for the relationship. It can further help to open a line for honest and consistent feedback. This can also give you a formalized endpoint and agreed upon scope for the mentoring relationship. Having a check-in preestablished in a contract reduces any potentially awkward conversations about redefining the relationship down the road. (For example, what if our case resident decides to pursue GI? It could happen.)
Stage 3: Establishing a common goal
After you have determined the goals and expectations of the relationship together (remember, this is a relationship), it is time to start exploring possible projects and establishing goals for those projects. Having a quality improvement or research project will determine a common goal to work towards and help establish and define the relationship.
Once you have delineated broadly what the project(s) should be, develop smaller SMART (specific, measurable, achievable, relevant, time-bound) goals to move the project forward. These goals determine stopping points for evaluation and feedback, which further establish the relationship and keep the project(s) progressing. For example, one goal could be to write the first draft of the proposal for your quality improvement project within 3 weeks.
Stage 4: Continued communication
With any project it is important to stay on the same page as your mentor and be clear to establish “who is doing what by when.” Do not expect accountability to be the mentor’s job. Remember that you are in the driver’s seat and that you should propose how often you need to meet and what those meetings look like by developing an agenda. You can have an open discussion and allow your mentor to help determine a reasonable timeline. Remember, the more you communicate your goals, the better your mentor will be able to address them.
One pro tip is to always exceed your mentor’s expectations – if you think you need 2 weeks to complete a task, ask for 3-4 weeks. This gives you extra padding in case of unforeseen circumstances and makes you look like a “rockstar” if you hit a deadline 1-2 weeks earlier than planned.
III. Ending and/or redefining the relationship
Case continued
You are now a senior resident who’s published multiple articles in the past year, and have completed an anticoagulation project for inpatients with pulmonary emboli. You look back on your experience and what stands out is the extent of your gratitude and appreciation for your incredible mentor. Not only do you feel that your mentor has guided you in your career and with your scholarship, but you feel that he or she has shaped your character and talent set. At this point your mentor is both a teacher and guide, but now also a friend. While you feel there is always more that you can learn from her, you are ready to explore new interests. How do you effectively end or redefine this relationship?
Stage 5: Redefining your mentoring relationship
First, go back to the expectations or contract established early in the relationship. The check-in is a key time in the relationship to reevaluate goals and priorities. At this point you may decide to amicably end the relationship or project, or move on to a new project with a change in your role. For example, the quality improvement project may change to research, or you as the mentee have a change in focus (e.g., change in specialty or scholarly focus).
In summary, the interaction between you and your mentor should be a relationship. And the keys to a great relationship are:
1. Establish clear expectations from the beginning. This clarifies the relationship and helps the mentee and mentor to become more successful.
2. Maintain clear and open communication throughout the relationship.3. Define your goals and discuss them with your mentor early. (Have we mentioned the importance of goals enough?) After all, your goal is the reason you started pursuing this relationship in the first place.
In clinical training having guidance can greatly enhance your experience and direct your future career in unexpected ways. We hope that using these tools will guide you towards forging a strong mentor/mentee relationship.
Dr. Zimmerberg-Helms is a resident physician at the University of New Mexico, Albuquerque. Dr. Rendon is an attending hospitalist at the University of New Mexico.
I. Finding a mentor
Case
You are a 27-year-old first-year resident who is seeking mentorship. You are halfway through the year and are thinking about your goals and future. You have a general interest in hematology/oncology but have limited experience and would like to gain more experience with clinically relevant scholarship. However, you do not know anyone in the field and are not sure who to ask for guidance.
Stage 1: Seeking the right mentor
Start first with your area of interest and then look broadly. In this case the resident is interested in heme/onc. The first place to look is on the heme/onc department website or in the faculty directory. It can be helpful to look at what the potential mentor has published recently and/or look at a version of their CV on the faculty directory or website. This can help determine how productive they are and help assess whether you share similar interests, and whether they have worked with many learners in the past.
It is also important to do some background work and ask around about potential mentors. Often resident colleagues and fellows have a good sense of current projects and which faculty work well with learners. Lastly, it is important to also look at non–heme/onc physicians as there may be internal medicine physicians or surgeons who are doing hematology or oncology research that more align with your interests.
After you have assessed whether you think this person would be a strong mentor for you, it is time to reach out. People are flattered to be asked and part of their promotion criteria is their ability to mentor. Do not assume that a potential mentor is too busy! Let him or her make that decision. Remember the worst a mentor can say is “no.” Even if they do not have time or the need for a mentee at the present time, they generally will offer some assistance or direction on who to ask.
Start with a straightforward, but pleasant email. Waiting up to 2 weeks for a response is reasonable. If after 2 weeks you have not received word, feel free to reach out again asking politely if he or she would be willing to work with you. Do not be afraid to ask bluntly for their guidance and mentorship and have a specific project or area of research that you would like their assistance with.
II. Optimizing the mentor/mentee relationship
Case continued
Success! Your email was received with interest by a hematologist who has done several projects, comes highly recommended by other residents, and worked with students and residents in the past. The project involves anticoagulation on the inpatient service. You are set to meet with her next month.
Stage 2: Establishing expectations and goals
Now comes the hard work in establishing an excellent mentor/mentee relationship. Before you meet with your mentor, brainstorm first. What do you want out of the relationship? A publication? Career advice? Attaining a fellowship position? You should feel empowered in knowing that you as the mentee are in the driver seat, but this relationship should be mutually beneficial. Consider basing the relationship and initial discussions on these key questions:
1. My goals
- What are my goals? It is okay not to know but be ready to communicate some information to your mentor.
- Remember to also ask your mentor what their goals are for you as well.
2. Outcome
- What type of outcome are both you and your mentor looking for from the relationship?
3. Expectations
- What mentorship expectations do you have?
- What are your mentor’s expectations of you?
Once you feel you have a sense of what you are looking for out of the relationship, it is important to communicate this with the mentor to establish congruent expectations of one another. For example, think about asking your mentor if the two of you can establish a mentor/mentee contract. This is a written document that can be found online and establishes a mutual agreement of roles, responsibilities, and expectations of one another for the relationship. It can further help to open a line for honest and consistent feedback. This can also give you a formalized endpoint and agreed upon scope for the mentoring relationship. Having a check-in preestablished in a contract reduces any potentially awkward conversations about redefining the relationship down the road. (For example, what if our case resident decides to pursue GI? It could happen.)
Stage 3: Establishing a common goal
After you have determined the goals and expectations of the relationship together (remember, this is a relationship), it is time to start exploring possible projects and establishing goals for those projects. Having a quality improvement or research project will determine a common goal to work towards and help establish and define the relationship.
Once you have delineated broadly what the project(s) should be, develop smaller SMART (specific, measurable, achievable, relevant, time-bound) goals to move the project forward. These goals determine stopping points for evaluation and feedback, which further establish the relationship and keep the project(s) progressing. For example, one goal could be to write the first draft of the proposal for your quality improvement project within 3 weeks.
Stage 4: Continued communication
With any project it is important to stay on the same page as your mentor and be clear to establish “who is doing what by when.” Do not expect accountability to be the mentor’s job. Remember that you are in the driver’s seat and that you should propose how often you need to meet and what those meetings look like by developing an agenda. You can have an open discussion and allow your mentor to help determine a reasonable timeline. Remember, the more you communicate your goals, the better your mentor will be able to address them.
One pro tip is to always exceed your mentor’s expectations – if you think you need 2 weeks to complete a task, ask for 3-4 weeks. This gives you extra padding in case of unforeseen circumstances and makes you look like a “rockstar” if you hit a deadline 1-2 weeks earlier than planned.
III. Ending and/or redefining the relationship
Case continued
You are now a senior resident who’s published multiple articles in the past year, and have completed an anticoagulation project for inpatients with pulmonary emboli. You look back on your experience and what stands out is the extent of your gratitude and appreciation for your incredible mentor. Not only do you feel that your mentor has guided you in your career and with your scholarship, but you feel that he or she has shaped your character and talent set. At this point your mentor is both a teacher and guide, but now also a friend. While you feel there is always more that you can learn from her, you are ready to explore new interests. How do you effectively end or redefine this relationship?
Stage 5: Redefining your mentoring relationship
First, go back to the expectations or contract established early in the relationship. The check-in is a key time in the relationship to reevaluate goals and priorities. At this point you may decide to amicably end the relationship or project, or move on to a new project with a change in your role. For example, the quality improvement project may change to research, or you as the mentee have a change in focus (e.g., change in specialty or scholarly focus).
In summary, the interaction between you and your mentor should be a relationship. And the keys to a great relationship are:
1. Establish clear expectations from the beginning. This clarifies the relationship and helps the mentee and mentor to become more successful.
2. Maintain clear and open communication throughout the relationship.3. Define your goals and discuss them with your mentor early. (Have we mentioned the importance of goals enough?) After all, your goal is the reason you started pursuing this relationship in the first place.
In clinical training having guidance can greatly enhance your experience and direct your future career in unexpected ways. We hope that using these tools will guide you towards forging a strong mentor/mentee relationship.
Dr. Zimmerberg-Helms is a resident physician at the University of New Mexico, Albuquerque. Dr. Rendon is an attending hospitalist at the University of New Mexico.
I. Finding a mentor
Case
You are a 27-year-old first-year resident who is seeking mentorship. You are halfway through the year and are thinking about your goals and future. You have a general interest in hematology/oncology but have limited experience and would like to gain more experience with clinically relevant scholarship. However, you do not know anyone in the field and are not sure who to ask for guidance.
Stage 1: Seeking the right mentor
Start first with your area of interest and then look broadly. In this case the resident is interested in heme/onc. The first place to look is on the heme/onc department website or in the faculty directory. It can be helpful to look at what the potential mentor has published recently and/or look at a version of their CV on the faculty directory or website. This can help determine how productive they are and help assess whether you share similar interests, and whether they have worked with many learners in the past.
It is also important to do some background work and ask around about potential mentors. Often resident colleagues and fellows have a good sense of current projects and which faculty work well with learners. Lastly, it is important to also look at non–heme/onc physicians as there may be internal medicine physicians or surgeons who are doing hematology or oncology research that more align with your interests.
After you have assessed whether you think this person would be a strong mentor for you, it is time to reach out. People are flattered to be asked and part of their promotion criteria is their ability to mentor. Do not assume that a potential mentor is too busy! Let him or her make that decision. Remember the worst a mentor can say is “no.” Even if they do not have time or the need for a mentee at the present time, they generally will offer some assistance or direction on who to ask.
Start with a straightforward, but pleasant email. Waiting up to 2 weeks for a response is reasonable. If after 2 weeks you have not received word, feel free to reach out again asking politely if he or she would be willing to work with you. Do not be afraid to ask bluntly for their guidance and mentorship and have a specific project or area of research that you would like their assistance with.
II. Optimizing the mentor/mentee relationship
Case continued
Success! Your email was received with interest by a hematologist who has done several projects, comes highly recommended by other residents, and worked with students and residents in the past. The project involves anticoagulation on the inpatient service. You are set to meet with her next month.
Stage 2: Establishing expectations and goals
Now comes the hard work in establishing an excellent mentor/mentee relationship. Before you meet with your mentor, brainstorm first. What do you want out of the relationship? A publication? Career advice? Attaining a fellowship position? You should feel empowered in knowing that you as the mentee are in the driver seat, but this relationship should be mutually beneficial. Consider basing the relationship and initial discussions on these key questions:
1. My goals
- What are my goals? It is okay not to know but be ready to communicate some information to your mentor.
- Remember to also ask your mentor what their goals are for you as well.
2. Outcome
- What type of outcome are both you and your mentor looking for from the relationship?
3. Expectations
- What mentorship expectations do you have?
- What are your mentor’s expectations of you?
Once you feel you have a sense of what you are looking for out of the relationship, it is important to communicate this with the mentor to establish congruent expectations of one another. For example, think about asking your mentor if the two of you can establish a mentor/mentee contract. This is a written document that can be found online and establishes a mutual agreement of roles, responsibilities, and expectations of one another for the relationship. It can further help to open a line for honest and consistent feedback. This can also give you a formalized endpoint and agreed upon scope for the mentoring relationship. Having a check-in preestablished in a contract reduces any potentially awkward conversations about redefining the relationship down the road. (For example, what if our case resident decides to pursue GI? It could happen.)
Stage 3: Establishing a common goal
After you have determined the goals and expectations of the relationship together (remember, this is a relationship), it is time to start exploring possible projects and establishing goals for those projects. Having a quality improvement or research project will determine a common goal to work towards and help establish and define the relationship.
Once you have delineated broadly what the project(s) should be, develop smaller SMART (specific, measurable, achievable, relevant, time-bound) goals to move the project forward. These goals determine stopping points for evaluation and feedback, which further establish the relationship and keep the project(s) progressing. For example, one goal could be to write the first draft of the proposal for your quality improvement project within 3 weeks.
Stage 4: Continued communication
With any project it is important to stay on the same page as your mentor and be clear to establish “who is doing what by when.” Do not expect accountability to be the mentor’s job. Remember that you are in the driver’s seat and that you should propose how often you need to meet and what those meetings look like by developing an agenda. You can have an open discussion and allow your mentor to help determine a reasonable timeline. Remember, the more you communicate your goals, the better your mentor will be able to address them.
One pro tip is to always exceed your mentor’s expectations – if you think you need 2 weeks to complete a task, ask for 3-4 weeks. This gives you extra padding in case of unforeseen circumstances and makes you look like a “rockstar” if you hit a deadline 1-2 weeks earlier than planned.
III. Ending and/or redefining the relationship
Case continued
You are now a senior resident who’s published multiple articles in the past year, and have completed an anticoagulation project for inpatients with pulmonary emboli. You look back on your experience and what stands out is the extent of your gratitude and appreciation for your incredible mentor. Not only do you feel that your mentor has guided you in your career and with your scholarship, but you feel that he or she has shaped your character and talent set. At this point your mentor is both a teacher and guide, but now also a friend. While you feel there is always more that you can learn from her, you are ready to explore new interests. How do you effectively end or redefine this relationship?
Stage 5: Redefining your mentoring relationship
First, go back to the expectations or contract established early in the relationship. The check-in is a key time in the relationship to reevaluate goals and priorities. At this point you may decide to amicably end the relationship or project, or move on to a new project with a change in your role. For example, the quality improvement project may change to research, or you as the mentee have a change in focus (e.g., change in specialty or scholarly focus).
In summary, the interaction between you and your mentor should be a relationship. And the keys to a great relationship are:
1. Establish clear expectations from the beginning. This clarifies the relationship and helps the mentee and mentor to become more successful.
2. Maintain clear and open communication throughout the relationship.3. Define your goals and discuss them with your mentor early. (Have we mentioned the importance of goals enough?) After all, your goal is the reason you started pursuing this relationship in the first place.
In clinical training having guidance can greatly enhance your experience and direct your future career in unexpected ways. We hope that using these tools will guide you towards forging a strong mentor/mentee relationship.
Dr. Zimmerberg-Helms is a resident physician at the University of New Mexico, Albuquerque. Dr. Rendon is an attending hospitalist at the University of New Mexico.
Is ‘Med Ed’ changing for better or worse?
The next generation of physicians is learning much differently from how established doctors once did. Training has shifted from an acute focus on disease to a wider approach that considers patients within the larger context of their community and society. Although many, like myself, see this as progress, others have expressed doubts about this and many other changes.
Amid the madness that is the year 2020, I’m grateful to have a moment to reflect on this subject. Five years ago, in celebration of Medscape’s 20th anniversary, I spoke with various leaders in medical education to learn how med ed had evolved since they were in school. Since then, I’ve gone from student to faculty. This year, for Medscape’s 25th anniversary, I reached out to current medical trainees to reflect on how much things have changed in such a short time.
From adjustments forced on us by COVID-19 to trends that predated the pandemic – including an increased emphasis on social justice and a decreased emphasis on other material – becoming a doctor no longer looks like it did just a half-decade ago.
Social justice is now in the curricula
More than ever, medical training has shifted toward humanism, population health, and social justice. Students are now being shown not only how to treat the patient in front of them but how to “treat” the larger communities they serve. Research skills around social drivers of health, such as structural racism, are increasingly becoming status quo.
In reflecting on her current experience, Emily Kahoud, a third-year medical student at New Jersey Medical School, Newark, told me about a course she took that was devoted to health equity. She applauded how her professors have incorporated this education into their courses. “It’s so nice and refreshing to be in a community that appreciates that.”
I, too, have seen this change firsthand. In addition to caring for patients and teaching at the University of North Carolina at Chapel Hill, I work with a team that develops curricula around social justice. We strive to integrate this material into existing courses and rotations. I believe that this is not only the right thing to teach trainees in order to help their future patients, but that it also reduces harm that many students experience. The “hidden curriculum” of medical school has long marginalized anyone who isn’t White and/or male.
Children, women, and the elderly were often referred to as “special populations” during my training. Even now, content about social and structural drivers of health is still most often relegated to separate courses rather than integrated into existing material. I hope to help improve this at my institution and that others are doing the same elsewhere.
If the current students I spoke with are any indication, further integration will be a welcomed change. Travis Benson, a third-year medical student at Harvard Medical School, Boston, appreciates where medical training is headed. Specifically, he is interested in inequities in the care of transgender patients. He says he has loved what his school has done with education on issues not previously considered part of med ed. “In the first week of school, we go on tours and spend time in community health centers and learn about the ‘Family Van,’ a mobile health care clinic that offers free care. I even had an opportunity to have a longitudinal clinic experience at a jail.”
While some critics argue that this learning goes too far, others argue that it has not gone far enough fast enough. In general, I consider the progress made in this area since my time in med school to be a very good thing. Medical students are now being taught to think about the science of medicine in the context of the larger human condition.
More technology, less preclinical time and cost
Beyond evolution in curricular content, technical and logistical changes have dramatically reshaped med ed. Since I started my training in 2012, most medical schools now no longer formally require students to attend lectures. Instead, they make them available online for students to view on demand. This undoubtedly makes schedules more flexible, allows students to learn at their own pace, and helps accommodate students with different needs.
Another big change: Preclinical years may now be as short as 1.5 years or less. This is a big draw for some students. Most choose to go to medical school to take care of patients. Shortening the preclinical years means students have more time immersed in patient care and less time dealing with medical minutiae.
That also means that they can spend more time thinking about professional development. Ramie Fathy, a fourth-year student, told me, “I came to Penn [University of Pennsylvania in Philadelphia] because of the shortened preclinical curriculum. That allowed more time on the back end to explore different specialties.” Although some established doctors worry about what scientific details may be left out, providing more hands-on experience sure seems like a good thing to me. Learning from textbooks can only take you so far in this profession.
Another, and more expected, development is the use of ever-advancing technology. Some schools now offer 3D virtual modeling for the study of anatomy, as well as a myriad of electronic visual aids for subjects like pathology and microbiology. Adapting to technological changes can be challenging, however, especially because more nontraditional students are being admitted to medical school each year.
Kahoud is one such nontraditional – older – student. She had some concerns about reliance on newer resources going in. “It [medical school] has become increasingly dependent on technology, even before COVID,” she said. “When you are not well versed in these tools it can definitely be a struggle.”
Thanks to the pandemic, remote learning is now the name of the game for many. As a result, instructors have had to amend their teaching styles to suit distance education, various untested applications and programs have been integrated into the curriculum, and students and administrators alike have had to find alternative ways to build a sense of community.
Is this a glimpse at the future for med ed? And if so, what may be lost or gained from this transition? Tino Delamerced, a third-year student at the Brown University, Providence, R.I., shared a likely very widely held hope: “If the preclinical years can be totally remote permanently, then can tuition be cheaper?”
Med ed debt keeps growing and remains a huge deterrent for potential students, especially those who are the first in their family to pursue medicine, come from a disadvantaged background, or have other people for whom they are financially responsible. Is it possible that the restrictions of COVID-19 could finally lead to cost cutting?
A bigger solution – free medical school – predated the pandemic. Institutions such as New York University have completely eliminated tuition, whereas others such as the Icahn School of Medicine at Mount Sinai (my alma mater) have limited the amount of debt with which a student graduates. You can imagine my frustration that the debt limit policy was enacted after I graduated.
Still, as optimistic as some have been at this movement that developed in the past 5 years, many think this specific evolution is little more than a “pipe dream.”
Current students score big with USMLE change
Beyond med school cost, another universally despised part of medical training that has seen a dramatic change is the licensing examination. My dedicated study period for the United States Medical Licensing Examination (USMLE) Step 1 was my worst time of medical school. Well, it was second to holding a retractor in the operating room for hours at a time.
Like everyone, I suspected that Step 1 would not be an accurate indicator of my ability to actually care for patients. As a practicing physician, I can now tell you for sure that this is the case. How lucky for the next generation, then, that the test is going to a pass/fail grading system.
Step 1 has always been important, as residency programs rely on the score to weed out applicants. Even if that screening emphasis simply gets shifted to scores on other examinations, this change still feels like progress. As Fathy told me, “There will likely be more emphasis on USMLE Step 2. But I think, based on practice questions I’ve done, that is more relevant to clinical abilities.” From my new vantage point, I can confirm that.
Not everyone is excited, though. Delamerced told me that he fears that the pass/fail Step 1 score may disparately affect students outside of allopathic medical schools. He said that the new scoring system “does not allow students to distinguish themselves via a standardized test score. That may hurt IMGs or DO students.”
Even then, Delamerced conceded that the change has some clear benefits. “For med students’ mental health, it’s probably a good thing.” From a population-based perspective, a medical student’s mental health often declines throughout school. Standardized exams are not the only cause, but we all know that it is a big contributor. The Step 1 switch can only help with that.
Finish faster or learn more?
In addition to evolution in the content and methods used to teach and assess current med students, the duration of med ed has also changed. Today’s students can choose to complete medical school in less than 4 years.
At the school where I work, the Fully Integrated Readiness for Service Training (FIRST) program allows certain students to complete their education in just 3 years. This program is for students who already know early on that they want to pursue a specialty included on our curated list. The goal of the program is to ultimately train physicians in family medicine, psychiatry, pediatrics, or general surgery in order to provide crucial care to those who need it most in our state.
Other medical schools offer accelerated MD programs for students based on various admissions criteria and specialty interest. The benefit of these programs is that shortening training time cuts down on debt for students.
Accelerated MD programs also aim to quickly increase the number of practicing physicians. This is especially important for primary care, which expects to see a growing gap in the years to come. That aim has come under some criticism, as some believe that the 4-year program was the standard for a reason. But when I reflect on it, I often wonder whether my fourth year was really worth $60,000. I spent a lot of that year traveling for residency interviews and watching Netflix between clinic electives.
Instead of finishing medical school faster, some students now have an opportunity to integrate additional training and education. Benson told me that, at Harvard, many students take a year off to pursue other opportunities. He said, “About 40% of students end up taking a fifth year to do either a master’s degree, global health, or research.” Benson said the additional learning opportunities are broad. “Some classmates even go to other schools altogether to get additional education.” Widened areas of learning are likely to produce better doctors, in my opinion.
This chance to look back on medical education has shown me that the ways in which it has changed rapidly in just the past few years are largely positive. Although COVID-19 has been an unwanted bane, it has also forced schools to integrate new technology and has placed an even brighter spotlight on health inequities and other areas in which education further improved. I hope that, when I look back on med ed in another 5 years, it has grown even more flexible and nimble in meeting the ever-changing needs of students and patients alike.
Alexa Mieses Malchuk, MD, MPH, was born and raised in Queens, New York. Social justice is what drew her to family medicine. As an academic physician at the University of North Carolina, she practices inpatient and outpatient medicine and serves as a medical educator for students and residents.
This article first appeared on Medscape.com.
The next generation of physicians is learning much differently from how established doctors once did. Training has shifted from an acute focus on disease to a wider approach that considers patients within the larger context of their community and society. Although many, like myself, see this as progress, others have expressed doubts about this and many other changes.
Amid the madness that is the year 2020, I’m grateful to have a moment to reflect on this subject. Five years ago, in celebration of Medscape’s 20th anniversary, I spoke with various leaders in medical education to learn how med ed had evolved since they were in school. Since then, I’ve gone from student to faculty. This year, for Medscape’s 25th anniversary, I reached out to current medical trainees to reflect on how much things have changed in such a short time.
From adjustments forced on us by COVID-19 to trends that predated the pandemic – including an increased emphasis on social justice and a decreased emphasis on other material – becoming a doctor no longer looks like it did just a half-decade ago.
Social justice is now in the curricula
More than ever, medical training has shifted toward humanism, population health, and social justice. Students are now being shown not only how to treat the patient in front of them but how to “treat” the larger communities they serve. Research skills around social drivers of health, such as structural racism, are increasingly becoming status quo.
In reflecting on her current experience, Emily Kahoud, a third-year medical student at New Jersey Medical School, Newark, told me about a course she took that was devoted to health equity. She applauded how her professors have incorporated this education into their courses. “It’s so nice and refreshing to be in a community that appreciates that.”
I, too, have seen this change firsthand. In addition to caring for patients and teaching at the University of North Carolina at Chapel Hill, I work with a team that develops curricula around social justice. We strive to integrate this material into existing courses and rotations. I believe that this is not only the right thing to teach trainees in order to help their future patients, but that it also reduces harm that many students experience. The “hidden curriculum” of medical school has long marginalized anyone who isn’t White and/or male.
Children, women, and the elderly were often referred to as “special populations” during my training. Even now, content about social and structural drivers of health is still most often relegated to separate courses rather than integrated into existing material. I hope to help improve this at my institution and that others are doing the same elsewhere.
If the current students I spoke with are any indication, further integration will be a welcomed change. Travis Benson, a third-year medical student at Harvard Medical School, Boston, appreciates where medical training is headed. Specifically, he is interested in inequities in the care of transgender patients. He says he has loved what his school has done with education on issues not previously considered part of med ed. “In the first week of school, we go on tours and spend time in community health centers and learn about the ‘Family Van,’ a mobile health care clinic that offers free care. I even had an opportunity to have a longitudinal clinic experience at a jail.”
While some critics argue that this learning goes too far, others argue that it has not gone far enough fast enough. In general, I consider the progress made in this area since my time in med school to be a very good thing. Medical students are now being taught to think about the science of medicine in the context of the larger human condition.
More technology, less preclinical time and cost
Beyond evolution in curricular content, technical and logistical changes have dramatically reshaped med ed. Since I started my training in 2012, most medical schools now no longer formally require students to attend lectures. Instead, they make them available online for students to view on demand. This undoubtedly makes schedules more flexible, allows students to learn at their own pace, and helps accommodate students with different needs.
Another big change: Preclinical years may now be as short as 1.5 years or less. This is a big draw for some students. Most choose to go to medical school to take care of patients. Shortening the preclinical years means students have more time immersed in patient care and less time dealing with medical minutiae.
That also means that they can spend more time thinking about professional development. Ramie Fathy, a fourth-year student, told me, “I came to Penn [University of Pennsylvania in Philadelphia] because of the shortened preclinical curriculum. That allowed more time on the back end to explore different specialties.” Although some established doctors worry about what scientific details may be left out, providing more hands-on experience sure seems like a good thing to me. Learning from textbooks can only take you so far in this profession.
Another, and more expected, development is the use of ever-advancing technology. Some schools now offer 3D virtual modeling for the study of anatomy, as well as a myriad of electronic visual aids for subjects like pathology and microbiology. Adapting to technological changes can be challenging, however, especially because more nontraditional students are being admitted to medical school each year.
Kahoud is one such nontraditional – older – student. She had some concerns about reliance on newer resources going in. “It [medical school] has become increasingly dependent on technology, even before COVID,” she said. “When you are not well versed in these tools it can definitely be a struggle.”
Thanks to the pandemic, remote learning is now the name of the game for many. As a result, instructors have had to amend their teaching styles to suit distance education, various untested applications and programs have been integrated into the curriculum, and students and administrators alike have had to find alternative ways to build a sense of community.
Is this a glimpse at the future for med ed? And if so, what may be lost or gained from this transition? Tino Delamerced, a third-year student at the Brown University, Providence, R.I., shared a likely very widely held hope: “If the preclinical years can be totally remote permanently, then can tuition be cheaper?”
Med ed debt keeps growing and remains a huge deterrent for potential students, especially those who are the first in their family to pursue medicine, come from a disadvantaged background, or have other people for whom they are financially responsible. Is it possible that the restrictions of COVID-19 could finally lead to cost cutting?
A bigger solution – free medical school – predated the pandemic. Institutions such as New York University have completely eliminated tuition, whereas others such as the Icahn School of Medicine at Mount Sinai (my alma mater) have limited the amount of debt with which a student graduates. You can imagine my frustration that the debt limit policy was enacted after I graduated.
Still, as optimistic as some have been at this movement that developed in the past 5 years, many think this specific evolution is little more than a “pipe dream.”
Current students score big with USMLE change
Beyond med school cost, another universally despised part of medical training that has seen a dramatic change is the licensing examination. My dedicated study period for the United States Medical Licensing Examination (USMLE) Step 1 was my worst time of medical school. Well, it was second to holding a retractor in the operating room for hours at a time.
Like everyone, I suspected that Step 1 would not be an accurate indicator of my ability to actually care for patients. As a practicing physician, I can now tell you for sure that this is the case. How lucky for the next generation, then, that the test is going to a pass/fail grading system.
Step 1 has always been important, as residency programs rely on the score to weed out applicants. Even if that screening emphasis simply gets shifted to scores on other examinations, this change still feels like progress. As Fathy told me, “There will likely be more emphasis on USMLE Step 2. But I think, based on practice questions I’ve done, that is more relevant to clinical abilities.” From my new vantage point, I can confirm that.
Not everyone is excited, though. Delamerced told me that he fears that the pass/fail Step 1 score may disparately affect students outside of allopathic medical schools. He said that the new scoring system “does not allow students to distinguish themselves via a standardized test score. That may hurt IMGs or DO students.”
Even then, Delamerced conceded that the change has some clear benefits. “For med students’ mental health, it’s probably a good thing.” From a population-based perspective, a medical student’s mental health often declines throughout school. Standardized exams are not the only cause, but we all know that it is a big contributor. The Step 1 switch can only help with that.
Finish faster or learn more?
In addition to evolution in the content and methods used to teach and assess current med students, the duration of med ed has also changed. Today’s students can choose to complete medical school in less than 4 years.
At the school where I work, the Fully Integrated Readiness for Service Training (FIRST) program allows certain students to complete their education in just 3 years. This program is for students who already know early on that they want to pursue a specialty included on our curated list. The goal of the program is to ultimately train physicians in family medicine, psychiatry, pediatrics, or general surgery in order to provide crucial care to those who need it most in our state.
Other medical schools offer accelerated MD programs for students based on various admissions criteria and specialty interest. The benefit of these programs is that shortening training time cuts down on debt for students.
Accelerated MD programs also aim to quickly increase the number of practicing physicians. This is especially important for primary care, which expects to see a growing gap in the years to come. That aim has come under some criticism, as some believe that the 4-year program was the standard for a reason. But when I reflect on it, I often wonder whether my fourth year was really worth $60,000. I spent a lot of that year traveling for residency interviews and watching Netflix between clinic electives.
Instead of finishing medical school faster, some students now have an opportunity to integrate additional training and education. Benson told me that, at Harvard, many students take a year off to pursue other opportunities. He said, “About 40% of students end up taking a fifth year to do either a master’s degree, global health, or research.” Benson said the additional learning opportunities are broad. “Some classmates even go to other schools altogether to get additional education.” Widened areas of learning are likely to produce better doctors, in my opinion.
This chance to look back on medical education has shown me that the ways in which it has changed rapidly in just the past few years are largely positive. Although COVID-19 has been an unwanted bane, it has also forced schools to integrate new technology and has placed an even brighter spotlight on health inequities and other areas in which education further improved. I hope that, when I look back on med ed in another 5 years, it has grown even more flexible and nimble in meeting the ever-changing needs of students and patients alike.
Alexa Mieses Malchuk, MD, MPH, was born and raised in Queens, New York. Social justice is what drew her to family medicine. As an academic physician at the University of North Carolina, she practices inpatient and outpatient medicine and serves as a medical educator for students and residents.
This article first appeared on Medscape.com.
The next generation of physicians is learning much differently from how established doctors once did. Training has shifted from an acute focus on disease to a wider approach that considers patients within the larger context of their community and society. Although many, like myself, see this as progress, others have expressed doubts about this and many other changes.
Amid the madness that is the year 2020, I’m grateful to have a moment to reflect on this subject. Five years ago, in celebration of Medscape’s 20th anniversary, I spoke with various leaders in medical education to learn how med ed had evolved since they were in school. Since then, I’ve gone from student to faculty. This year, for Medscape’s 25th anniversary, I reached out to current medical trainees to reflect on how much things have changed in such a short time.
From adjustments forced on us by COVID-19 to trends that predated the pandemic – including an increased emphasis on social justice and a decreased emphasis on other material – becoming a doctor no longer looks like it did just a half-decade ago.
Social justice is now in the curricula
More than ever, medical training has shifted toward humanism, population health, and social justice. Students are now being shown not only how to treat the patient in front of them but how to “treat” the larger communities they serve. Research skills around social drivers of health, such as structural racism, are increasingly becoming status quo.
In reflecting on her current experience, Emily Kahoud, a third-year medical student at New Jersey Medical School, Newark, told me about a course she took that was devoted to health equity. She applauded how her professors have incorporated this education into their courses. “It’s so nice and refreshing to be in a community that appreciates that.”
I, too, have seen this change firsthand. In addition to caring for patients and teaching at the University of North Carolina at Chapel Hill, I work with a team that develops curricula around social justice. We strive to integrate this material into existing courses and rotations. I believe that this is not only the right thing to teach trainees in order to help their future patients, but that it also reduces harm that many students experience. The “hidden curriculum” of medical school has long marginalized anyone who isn’t White and/or male.
Children, women, and the elderly were often referred to as “special populations” during my training. Even now, content about social and structural drivers of health is still most often relegated to separate courses rather than integrated into existing material. I hope to help improve this at my institution and that others are doing the same elsewhere.
If the current students I spoke with are any indication, further integration will be a welcomed change. Travis Benson, a third-year medical student at Harvard Medical School, Boston, appreciates where medical training is headed. Specifically, he is interested in inequities in the care of transgender patients. He says he has loved what his school has done with education on issues not previously considered part of med ed. “In the first week of school, we go on tours and spend time in community health centers and learn about the ‘Family Van,’ a mobile health care clinic that offers free care. I even had an opportunity to have a longitudinal clinic experience at a jail.”
While some critics argue that this learning goes too far, others argue that it has not gone far enough fast enough. In general, I consider the progress made in this area since my time in med school to be a very good thing. Medical students are now being taught to think about the science of medicine in the context of the larger human condition.
More technology, less preclinical time and cost
Beyond evolution in curricular content, technical and logistical changes have dramatically reshaped med ed. Since I started my training in 2012, most medical schools now no longer formally require students to attend lectures. Instead, they make them available online for students to view on demand. This undoubtedly makes schedules more flexible, allows students to learn at their own pace, and helps accommodate students with different needs.
Another big change: Preclinical years may now be as short as 1.5 years or less. This is a big draw for some students. Most choose to go to medical school to take care of patients. Shortening the preclinical years means students have more time immersed in patient care and less time dealing with medical minutiae.
That also means that they can spend more time thinking about professional development. Ramie Fathy, a fourth-year student, told me, “I came to Penn [University of Pennsylvania in Philadelphia] because of the shortened preclinical curriculum. That allowed more time on the back end to explore different specialties.” Although some established doctors worry about what scientific details may be left out, providing more hands-on experience sure seems like a good thing to me. Learning from textbooks can only take you so far in this profession.
Another, and more expected, development is the use of ever-advancing technology. Some schools now offer 3D virtual modeling for the study of anatomy, as well as a myriad of electronic visual aids for subjects like pathology and microbiology. Adapting to technological changes can be challenging, however, especially because more nontraditional students are being admitted to medical school each year.
Kahoud is one such nontraditional – older – student. She had some concerns about reliance on newer resources going in. “It [medical school] has become increasingly dependent on technology, even before COVID,” she said. “When you are not well versed in these tools it can definitely be a struggle.”
Thanks to the pandemic, remote learning is now the name of the game for many. As a result, instructors have had to amend their teaching styles to suit distance education, various untested applications and programs have been integrated into the curriculum, and students and administrators alike have had to find alternative ways to build a sense of community.
Is this a glimpse at the future for med ed? And if so, what may be lost or gained from this transition? Tino Delamerced, a third-year student at the Brown University, Providence, R.I., shared a likely very widely held hope: “If the preclinical years can be totally remote permanently, then can tuition be cheaper?”
Med ed debt keeps growing and remains a huge deterrent for potential students, especially those who are the first in their family to pursue medicine, come from a disadvantaged background, or have other people for whom they are financially responsible. Is it possible that the restrictions of COVID-19 could finally lead to cost cutting?
A bigger solution – free medical school – predated the pandemic. Institutions such as New York University have completely eliminated tuition, whereas others such as the Icahn School of Medicine at Mount Sinai (my alma mater) have limited the amount of debt with which a student graduates. You can imagine my frustration that the debt limit policy was enacted after I graduated.
Still, as optimistic as some have been at this movement that developed in the past 5 years, many think this specific evolution is little more than a “pipe dream.”
Current students score big with USMLE change
Beyond med school cost, another universally despised part of medical training that has seen a dramatic change is the licensing examination. My dedicated study period for the United States Medical Licensing Examination (USMLE) Step 1 was my worst time of medical school. Well, it was second to holding a retractor in the operating room for hours at a time.
Like everyone, I suspected that Step 1 would not be an accurate indicator of my ability to actually care for patients. As a practicing physician, I can now tell you for sure that this is the case. How lucky for the next generation, then, that the test is going to a pass/fail grading system.
Step 1 has always been important, as residency programs rely on the score to weed out applicants. Even if that screening emphasis simply gets shifted to scores on other examinations, this change still feels like progress. As Fathy told me, “There will likely be more emphasis on USMLE Step 2. But I think, based on practice questions I’ve done, that is more relevant to clinical abilities.” From my new vantage point, I can confirm that.
Not everyone is excited, though. Delamerced told me that he fears that the pass/fail Step 1 score may disparately affect students outside of allopathic medical schools. He said that the new scoring system “does not allow students to distinguish themselves via a standardized test score. That may hurt IMGs or DO students.”
Even then, Delamerced conceded that the change has some clear benefits. “For med students’ mental health, it’s probably a good thing.” From a population-based perspective, a medical student’s mental health often declines throughout school. Standardized exams are not the only cause, but we all know that it is a big contributor. The Step 1 switch can only help with that.
Finish faster or learn more?
In addition to evolution in the content and methods used to teach and assess current med students, the duration of med ed has also changed. Today’s students can choose to complete medical school in less than 4 years.
At the school where I work, the Fully Integrated Readiness for Service Training (FIRST) program allows certain students to complete their education in just 3 years. This program is for students who already know early on that they want to pursue a specialty included on our curated list. The goal of the program is to ultimately train physicians in family medicine, psychiatry, pediatrics, or general surgery in order to provide crucial care to those who need it most in our state.
Other medical schools offer accelerated MD programs for students based on various admissions criteria and specialty interest. The benefit of these programs is that shortening training time cuts down on debt for students.
Accelerated MD programs also aim to quickly increase the number of practicing physicians. This is especially important for primary care, which expects to see a growing gap in the years to come. That aim has come under some criticism, as some believe that the 4-year program was the standard for a reason. But when I reflect on it, I often wonder whether my fourth year was really worth $60,000. I spent a lot of that year traveling for residency interviews and watching Netflix between clinic electives.
Instead of finishing medical school faster, some students now have an opportunity to integrate additional training and education. Benson told me that, at Harvard, many students take a year off to pursue other opportunities. He said, “About 40% of students end up taking a fifth year to do either a master’s degree, global health, or research.” Benson said the additional learning opportunities are broad. “Some classmates even go to other schools altogether to get additional education.” Widened areas of learning are likely to produce better doctors, in my opinion.
This chance to look back on medical education has shown me that the ways in which it has changed rapidly in just the past few years are largely positive. Although COVID-19 has been an unwanted bane, it has also forced schools to integrate new technology and has placed an even brighter spotlight on health inequities and other areas in which education further improved. I hope that, when I look back on med ed in another 5 years, it has grown even more flexible and nimble in meeting the ever-changing needs of students and patients alike.
Alexa Mieses Malchuk, MD, MPH, was born and raised in Queens, New York. Social justice is what drew her to family medicine. As an academic physician at the University of North Carolina, she practices inpatient and outpatient medicine and serves as a medical educator for students and residents.
This article first appeared on Medscape.com.
Colorectal cancer screening guidelines: How to make best use of all of them
The recent death of “Black Panther” star Chadwick Boseman has resulted in colorectal cancer (CRC) screening guidelines receiving more attention. Mr. Boseman was diagnosed with Stage 3 CRC in 2016 and underwent treatment. He passed away 4 years later at the young age of 44.
Mr. Boseman’s death has highlighted two important concerns about current screening guidelines for CRC. These include racial disparities in patients with colon cancer and the fact that more younger patients are getting this disease.
There are at least three different sets of CRC screening recommendations from different trusted professional organizations that primary care physicians must decide how to follow. These organizations each published their guidelines indicating review of the best available evidence. On first glance there is discrepancy between these guidelines, but a closer look at them reveals they have a lot of similarities.
The U.S. Multi-Society Task Force of Colorectal Cancer (MSTF), which represents the American College of Gastroenterology, the American Gatroenterological Association, and the American Society for Gastrointestinal Endoscopy, is one of the organizations that offers guidelines. The MSTF recommends CRC screening for non-African American average risked persons at the age of 50 years (strong recommendation; moderate quality evidence). The first-tier options for this recommendation are to have a colonoscopy every 10 years or annual fecal immunochemial test. Additionally, the MSTF recommends beginning screening of African Americans at age 45 years (weak recommendation; very-low-quality evidence). This recommendation cites higher incidence rates, earlier mean age at onset, higher proportion of cancers before age 50 years and late-stage presentation. The MSTF indicates that the increased rate of CRC at an earlier age in African Americans is caused by a combination of biologic and societal factors, but do not point to what those are. This earlier screening is not backed by evidence that it in fact improves morbidity or mortality outcomes. The MSTF also address screening among high-risk individuals. Those with first degree relatives with CRC or advanced adenomas diagnosed before the age of 60 years should be screened beginning at age 40 years or 10 years younger than the age the relative was diagnosed, whichever comes first, according to the MSTF recommendations. These individuals should have a colonoscopy every 5 years, the MSTF says. Those with first degree relatives with CRC or advanced adenomas diagnosed at older than 60 years should have CRC beginning at 40 years, though with the same testing intervals as average-risk individuals.1
The American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP), however, endorse the guidelines set forth by the United States Preventive Services Task Force (USPSTF). These guidelines were published in 2016 in the JAMA and notably are currently under review. These guidelines recommend routine screening for those at average risk at the age of 50 years. In the publication of these guidelines, the increasing incidence of CRC in those under 50 was acknowledged. It is however stated that the modest benefit of earlier diagnosis made via screening is not better than the increased risk of increased lifetime colonoscopy.2
The publication specifically addresses the disparity among Black adults who have the highest incidence and mortality rates in comparison with other racial/ethnic groups. These guidelines specifically state that there are higher rates of colon cancer among black adults. They however clarify that they think it is because of decreased screening and treatment in this group. When compared with other groups and the screening and treatment is controlled for, there is no longer a difference. Lowering the age for starting screening, therefore, won’t help resolve the disparity because the higher cases in Black adults has resulted from not enough Black adults being screened at the recommended age of 50, according to the USPSTF recommendation statement. As such, rather than changing the age of screening for Black adults, this publication recommends efforts to ensure that screening, follow-up, and treatment are received.
The USPSTF specifically did not include adults with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC. They instead refer to other professional organizations for these recommendations.2
The American Cancer Society (ACS) also had a separate guideline published in CA: A Cancer Journal for Clinicians. It provides a qualified recommendation that CRC screening begin at age 45 years for those with average risk. The guideline also includes a strong recommendation for CRC screening beginning at age 50 years. The qualified recommendation for the younger age group is based on the incidence of colorectal cancer being similar between those aged 45-49 and those aged 50-54 years. The ACS also hypothesized that screening at an earlier age will decrease the disparity among population groups with a higher burden. Importantly, this updated guideline prioritized incidence reduction rather than mortality reduction. The ACS also stressed the need for a multipronged approach to mitigate barriers to CRC screening at the individual, provider, organizational, and policy levels. Similar to the USPSTF, the ACS did not address the screening of those with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC.3
In all of the publications discussing CRC screening guidelines, it is stressed that there is not sufficient uptake of any of these recommendations. Rather than conduct earlier screening, in my opinion, we should focus on programmatic ways to ensure that the existing screening recommendations are followed. This is a space in which we can help affect the disparity seen among population groups.
The most important screening test is the one that patients are willing to use. Primary care physicians can use any of these guidelines to have conversations with patients about risk and when to start screening. Although these guidelines may seem to be different from each other, each one includes strong recommendations with the same information.
Additional studies should be done to determine the benefits and harms of screening in patients with known risk factors such as obesity, cigarette smoking, diabetes, high consumption of alcohol, high consumption of red meat and processed food, inactivity, and low intake of dietary fiber, fruits, and vegetables. It is possible that the higher burden of disease among Black adults is related to societal factors leading to increased obesity and dietary habits that increase rates of CRC.
Primary care physicians would be better served by a tool that allows for risk stratification to help guide early screening for all patients. For certain patients, such a tool might result in them qualifying for screening that begins at a later age than the current guidelines recommend. Finally, primary care physicians must remember that these are just the guidelines for screening for CRC. They all specifically exclude patients experiencing any symptoms. As such, patients with unexplained bleeding, anemia, weight loss, and other symptoms should be evaluated fully, including being considered for colonoscopy to diagnose CRC. Primary care physicians should use these guidelines to screen their asymptomatic patients and should ensure that they provide evaluation of any of the symptoms of CRC.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is also program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on editorial advisory board of Family Practice News.
References
1. Rex DK et al. Gastrointest Endosc. 2017;86(1):18-33.
2. US Preventive Services Task Force. JAMA. 2016;315(23):2564-2575.
3. Wolf AMD et al. CA Cancer J Clin. 2018 Jul;68(4):250-281.
The recent death of “Black Panther” star Chadwick Boseman has resulted in colorectal cancer (CRC) screening guidelines receiving more attention. Mr. Boseman was diagnosed with Stage 3 CRC in 2016 and underwent treatment. He passed away 4 years later at the young age of 44.
Mr. Boseman’s death has highlighted two important concerns about current screening guidelines for CRC. These include racial disparities in patients with colon cancer and the fact that more younger patients are getting this disease.
There are at least three different sets of CRC screening recommendations from different trusted professional organizations that primary care physicians must decide how to follow. These organizations each published their guidelines indicating review of the best available evidence. On first glance there is discrepancy between these guidelines, but a closer look at them reveals they have a lot of similarities.
The U.S. Multi-Society Task Force of Colorectal Cancer (MSTF), which represents the American College of Gastroenterology, the American Gatroenterological Association, and the American Society for Gastrointestinal Endoscopy, is one of the organizations that offers guidelines. The MSTF recommends CRC screening for non-African American average risked persons at the age of 50 years (strong recommendation; moderate quality evidence). The first-tier options for this recommendation are to have a colonoscopy every 10 years or annual fecal immunochemial test. Additionally, the MSTF recommends beginning screening of African Americans at age 45 years (weak recommendation; very-low-quality evidence). This recommendation cites higher incidence rates, earlier mean age at onset, higher proportion of cancers before age 50 years and late-stage presentation. The MSTF indicates that the increased rate of CRC at an earlier age in African Americans is caused by a combination of biologic and societal factors, but do not point to what those are. This earlier screening is not backed by evidence that it in fact improves morbidity or mortality outcomes. The MSTF also address screening among high-risk individuals. Those with first degree relatives with CRC or advanced adenomas diagnosed before the age of 60 years should be screened beginning at age 40 years or 10 years younger than the age the relative was diagnosed, whichever comes first, according to the MSTF recommendations. These individuals should have a colonoscopy every 5 years, the MSTF says. Those with first degree relatives with CRC or advanced adenomas diagnosed at older than 60 years should have CRC beginning at 40 years, though with the same testing intervals as average-risk individuals.1
The American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP), however, endorse the guidelines set forth by the United States Preventive Services Task Force (USPSTF). These guidelines were published in 2016 in the JAMA and notably are currently under review. These guidelines recommend routine screening for those at average risk at the age of 50 years. In the publication of these guidelines, the increasing incidence of CRC in those under 50 was acknowledged. It is however stated that the modest benefit of earlier diagnosis made via screening is not better than the increased risk of increased lifetime colonoscopy.2
The publication specifically addresses the disparity among Black adults who have the highest incidence and mortality rates in comparison with other racial/ethnic groups. These guidelines specifically state that there are higher rates of colon cancer among black adults. They however clarify that they think it is because of decreased screening and treatment in this group. When compared with other groups and the screening and treatment is controlled for, there is no longer a difference. Lowering the age for starting screening, therefore, won’t help resolve the disparity because the higher cases in Black adults has resulted from not enough Black adults being screened at the recommended age of 50, according to the USPSTF recommendation statement. As such, rather than changing the age of screening for Black adults, this publication recommends efforts to ensure that screening, follow-up, and treatment are received.
The USPSTF specifically did not include adults with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC. They instead refer to other professional organizations for these recommendations.2
The American Cancer Society (ACS) also had a separate guideline published in CA: A Cancer Journal for Clinicians. It provides a qualified recommendation that CRC screening begin at age 45 years for those with average risk. The guideline also includes a strong recommendation for CRC screening beginning at age 50 years. The qualified recommendation for the younger age group is based on the incidence of colorectal cancer being similar between those aged 45-49 and those aged 50-54 years. The ACS also hypothesized that screening at an earlier age will decrease the disparity among population groups with a higher burden. Importantly, this updated guideline prioritized incidence reduction rather than mortality reduction. The ACS also stressed the need for a multipronged approach to mitigate barriers to CRC screening at the individual, provider, organizational, and policy levels. Similar to the USPSTF, the ACS did not address the screening of those with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC.3
In all of the publications discussing CRC screening guidelines, it is stressed that there is not sufficient uptake of any of these recommendations. Rather than conduct earlier screening, in my opinion, we should focus on programmatic ways to ensure that the existing screening recommendations are followed. This is a space in which we can help affect the disparity seen among population groups.
The most important screening test is the one that patients are willing to use. Primary care physicians can use any of these guidelines to have conversations with patients about risk and when to start screening. Although these guidelines may seem to be different from each other, each one includes strong recommendations with the same information.
Additional studies should be done to determine the benefits and harms of screening in patients with known risk factors such as obesity, cigarette smoking, diabetes, high consumption of alcohol, high consumption of red meat and processed food, inactivity, and low intake of dietary fiber, fruits, and vegetables. It is possible that the higher burden of disease among Black adults is related to societal factors leading to increased obesity and dietary habits that increase rates of CRC.
Primary care physicians would be better served by a tool that allows for risk stratification to help guide early screening for all patients. For certain patients, such a tool might result in them qualifying for screening that begins at a later age than the current guidelines recommend. Finally, primary care physicians must remember that these are just the guidelines for screening for CRC. They all specifically exclude patients experiencing any symptoms. As such, patients with unexplained bleeding, anemia, weight loss, and other symptoms should be evaluated fully, including being considered for colonoscopy to diagnose CRC. Primary care physicians should use these guidelines to screen their asymptomatic patients and should ensure that they provide evaluation of any of the symptoms of CRC.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is also program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on editorial advisory board of Family Practice News.
References
1. Rex DK et al. Gastrointest Endosc. 2017;86(1):18-33.
2. US Preventive Services Task Force. JAMA. 2016;315(23):2564-2575.
3. Wolf AMD et al. CA Cancer J Clin. 2018 Jul;68(4):250-281.
The recent death of “Black Panther” star Chadwick Boseman has resulted in colorectal cancer (CRC) screening guidelines receiving more attention. Mr. Boseman was diagnosed with Stage 3 CRC in 2016 and underwent treatment. He passed away 4 years later at the young age of 44.
Mr. Boseman’s death has highlighted two important concerns about current screening guidelines for CRC. These include racial disparities in patients with colon cancer and the fact that more younger patients are getting this disease.
There are at least three different sets of CRC screening recommendations from different trusted professional organizations that primary care physicians must decide how to follow. These organizations each published their guidelines indicating review of the best available evidence. On first glance there is discrepancy between these guidelines, but a closer look at them reveals they have a lot of similarities.
The U.S. Multi-Society Task Force of Colorectal Cancer (MSTF), which represents the American College of Gastroenterology, the American Gatroenterological Association, and the American Society for Gastrointestinal Endoscopy, is one of the organizations that offers guidelines. The MSTF recommends CRC screening for non-African American average risked persons at the age of 50 years (strong recommendation; moderate quality evidence). The first-tier options for this recommendation are to have a colonoscopy every 10 years or annual fecal immunochemial test. Additionally, the MSTF recommends beginning screening of African Americans at age 45 years (weak recommendation; very-low-quality evidence). This recommendation cites higher incidence rates, earlier mean age at onset, higher proportion of cancers before age 50 years and late-stage presentation. The MSTF indicates that the increased rate of CRC at an earlier age in African Americans is caused by a combination of biologic and societal factors, but do not point to what those are. This earlier screening is not backed by evidence that it in fact improves morbidity or mortality outcomes. The MSTF also address screening among high-risk individuals. Those with first degree relatives with CRC or advanced adenomas diagnosed before the age of 60 years should be screened beginning at age 40 years or 10 years younger than the age the relative was diagnosed, whichever comes first, according to the MSTF recommendations. These individuals should have a colonoscopy every 5 years, the MSTF says. Those with first degree relatives with CRC or advanced adenomas diagnosed at older than 60 years should have CRC beginning at 40 years, though with the same testing intervals as average-risk individuals.1
The American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP), however, endorse the guidelines set forth by the United States Preventive Services Task Force (USPSTF). These guidelines were published in 2016 in the JAMA and notably are currently under review. These guidelines recommend routine screening for those at average risk at the age of 50 years. In the publication of these guidelines, the increasing incidence of CRC in those under 50 was acknowledged. It is however stated that the modest benefit of earlier diagnosis made via screening is not better than the increased risk of increased lifetime colonoscopy.2
The publication specifically addresses the disparity among Black adults who have the highest incidence and mortality rates in comparison with other racial/ethnic groups. These guidelines specifically state that there are higher rates of colon cancer among black adults. They however clarify that they think it is because of decreased screening and treatment in this group. When compared with other groups and the screening and treatment is controlled for, there is no longer a difference. Lowering the age for starting screening, therefore, won’t help resolve the disparity because the higher cases in Black adults has resulted from not enough Black adults being screened at the recommended age of 50, according to the USPSTF recommendation statement. As such, rather than changing the age of screening for Black adults, this publication recommends efforts to ensure that screening, follow-up, and treatment are received.
The USPSTF specifically did not include adults with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC. They instead refer to other professional organizations for these recommendations.2
The American Cancer Society (ACS) also had a separate guideline published in CA: A Cancer Journal for Clinicians. It provides a qualified recommendation that CRC screening begin at age 45 years for those with average risk. The guideline also includes a strong recommendation for CRC screening beginning at age 50 years. The qualified recommendation for the younger age group is based on the incidence of colorectal cancer being similar between those aged 45-49 and those aged 50-54 years. The ACS also hypothesized that screening at an earlier age will decrease the disparity among population groups with a higher burden. Importantly, this updated guideline prioritized incidence reduction rather than mortality reduction. The ACS also stressed the need for a multipronged approach to mitigate barriers to CRC screening at the individual, provider, organizational, and policy levels. Similar to the USPSTF, the ACS did not address the screening of those with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC.3
In all of the publications discussing CRC screening guidelines, it is stressed that there is not sufficient uptake of any of these recommendations. Rather than conduct earlier screening, in my opinion, we should focus on programmatic ways to ensure that the existing screening recommendations are followed. This is a space in which we can help affect the disparity seen among population groups.
The most important screening test is the one that patients are willing to use. Primary care physicians can use any of these guidelines to have conversations with patients about risk and when to start screening. Although these guidelines may seem to be different from each other, each one includes strong recommendations with the same information.
Additional studies should be done to determine the benefits and harms of screening in patients with known risk factors such as obesity, cigarette smoking, diabetes, high consumption of alcohol, high consumption of red meat and processed food, inactivity, and low intake of dietary fiber, fruits, and vegetables. It is possible that the higher burden of disease among Black adults is related to societal factors leading to increased obesity and dietary habits that increase rates of CRC.
Primary care physicians would be better served by a tool that allows for risk stratification to help guide early screening for all patients. For certain patients, such a tool might result in them qualifying for screening that begins at a later age than the current guidelines recommend. Finally, primary care physicians must remember that these are just the guidelines for screening for CRC. They all specifically exclude patients experiencing any symptoms. As such, patients with unexplained bleeding, anemia, weight loss, and other symptoms should be evaluated fully, including being considered for colonoscopy to diagnose CRC. Primary care physicians should use these guidelines to screen their asymptomatic patients and should ensure that they provide evaluation of any of the symptoms of CRC.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is also program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on editorial advisory board of Family Practice News.
References
1. Rex DK et al. Gastrointest Endosc. 2017;86(1):18-33.
2. US Preventive Services Task Force. JAMA. 2016;315(23):2564-2575.
3. Wolf AMD et al. CA Cancer J Clin. 2018 Jul;68(4):250-281.
When the only clinical choices are ‘lose-lose’
Among the many tolls inflicted on health care workers by COVID-19 is one that is not as easily measured as rates of death or disease, but is no less tangible: moral injury. This is the term by which we describe the psychological, social, and spiritual impact of high-stakes situations that lead to the betrayal or transgression of our own deeply held moral beliefs and values.
The current pandemic has provided innumerable such situations that can increase the risk for moral injury, whether we deal directly with patients infected by the coronavirus or not. Telling family members they cannot visit critically ill loved ones. Delaying code activities, even momentarily, to get fully protected with personal protective equipment. Seeing patients who have delayed their necessary or preventive care. Using video rather than touch to reassure people.
Knowing that we are following guidelines from the Centers for Disease Control and Prevention does not stop our feelings of guilt. The longer this pandemic goes on, the more likely it is that these situations will begin to take a toll on us.
For most of us, being exposed to moral injuries is new; they have historically been most associated with severe traumatic wartime experiences. Soldiers, philosophers, and writers have described the ethical dilemmas inherent in war for as long as recorded history. But the use of this term is a more recent development, which the Moral Injury Project at Syracuse (N.Y.) University describes as probably originating in the Vietnam War–era writings of veteran and peace activist Camillo “Mac” Bica and psychiatrist Jonathan Shay. Examples of wartime events that have been thought to lead to moral injury include: causing the harm or death of civilians, knowingly but without alternatives, or accidentally; failing to provide medical aid to an injured civilian or service member; and following orders that were illegal, immoral, and/or against the rules of engagement or the Geneva Conventions.
However, the occurrence of moral injuries in modern health care is increasingly being reported, primarily as an adverse effect of health care inefficiencies that can contribute to burnout. COVID-19 has now provided an array of additional stressors that can cause moral injuries among health care workers. A recent guidance document on moral injury published by the American Psychiatric Association noted that, in the context of a public health disaster, such as COVID-19, it is sometimes necessary to transition from ordinary standards of care to those more appropriate in a crisis, as in wartime. This forces us all to confront challenging questions for which there may be no clear answers, and to make “lose-lose” choices in which no one involved – patients, family, or clinicians – ends up feeling satisfied or even comfortable.
Our lives have been altered significantly, and for many, completely turned upside down by enormous sacrifices and tragic losses. Globally, physicians account for over half of healthcare worker deaths. In the United States alone, over 900 health care workers have died of COVID-19.
Most of us have felt the symptoms of moral injury: frustration, anger, disgust, guilt. A recent report describes three levels of stressors in health care occurring during the pandemic, which are not dissimilar to those wartime events described previously.
- Severe moral stressors, such as the denial of treatment to a COVID-19 patient owing to lack of resources, the inability to provide optimal care to non–COVID-19 patients for many reasons, and concern about passing COVID to loved ones.
- Moderate moral stressors, such as preventing visitors, especially to dying patients, triaging patients for healthcare services with inadequate information, and trying to solve the tension between the need for self-preservation and the need to treat.
- Lower-level but common moral challenges, especially in the community – for example, seeing others not protecting the community by hoarding food, gathering for large parties, and not social distancing or wearing masks. Such stressors lead to frustration and contempt, especially from healthcare workers making personal sacrifices and who may be at risk for infection caused by these behaviors.
Every one of us is affected by these stressors. I certainly am.
What are the outcomes? We know that moral injuries are a risk factor for the development of mental health problems and burnout, and not surprisingly we are seeing that mental health problems, suicidality, and substance use disorders have increased markedly during COVID-19, as recently detailed by the CDC.
Common emotions that occur in response to moral injuries are: feelings of guilt, shame, anger, sadness, anxiety, and disgust; intrapersonal outcomes, including lowered self-esteem, high self-criticism, and beliefs about being bad, damaged, unworthy, failing, or weak; interpersonal outcomes, including loss of faith in people, avoidance of intimacy, and lack of trust in authority figures; and existential and spiritual outcomes, including loss of faith in previous religious beliefs and no longer believing in a just world.
Moral injuries tend to originate primarily from systems-based problems, as we have seen with the lack of concerted national approaches to the pandemic. On the positive side, solutions typically also involve systems-based changes, which in this case may mean changes in leadership styles nationally and locally, as well as changes in the culture of medicine and the way healthcare is practiced and managed in the modern era. We are starting to see some of those changes with the increased use of telemedicine and health technologies, as well as more of a focus on the well-being of health care workers, now deemed “essential.”
As individuals, we are not helpless. There are things we can do in our workplaces to create change. I suggest:
- Acknowledge that you, like me, are affected by these stressors. This is not a secret, and you should not be ashamed of your feelings.
- Talk with your colleagues, loved ones, and friends about how you and they are affected. You are not alone. Encourage others to share their thoughts, stories, and feelings.
- Put this topic on your meeting and departmental agendas and discuss these moral issues openly with your colleagues. Allow sufficient time to engage in open dialogue.
- Work out ways of assisting those who are in high-risk situations, especially for moderate to severe injuries. Be supportive toward those affected.
- Modify policies and change rosters and rotate staff between high- and low-stress roles. Protect and support at-risk colleagues.
- Think about difficult ethical decisions in advance so they can be made by groups, not individuals, and certainly not “on the fly.”
- Keep everyone in your workplace constantly informed, especially of impending staff or equipment shortages.
- Maintain your inherent self-care and resilience with rest, good nutrition, sleep, exercise, love, caring, socialization, and work-life balance.
- Be prepared to access the many professional support services available in our community if you are intensely distressed or if the above suggestions are not enough.
Remember, we are in this together and will find strength in each other. This too will pass.
This article first appeared on Medscape.com.
Among the many tolls inflicted on health care workers by COVID-19 is one that is not as easily measured as rates of death or disease, but is no less tangible: moral injury. This is the term by which we describe the psychological, social, and spiritual impact of high-stakes situations that lead to the betrayal or transgression of our own deeply held moral beliefs and values.
The current pandemic has provided innumerable such situations that can increase the risk for moral injury, whether we deal directly with patients infected by the coronavirus or not. Telling family members they cannot visit critically ill loved ones. Delaying code activities, even momentarily, to get fully protected with personal protective equipment. Seeing patients who have delayed their necessary or preventive care. Using video rather than touch to reassure people.
Knowing that we are following guidelines from the Centers for Disease Control and Prevention does not stop our feelings of guilt. The longer this pandemic goes on, the more likely it is that these situations will begin to take a toll on us.
For most of us, being exposed to moral injuries is new; they have historically been most associated with severe traumatic wartime experiences. Soldiers, philosophers, and writers have described the ethical dilemmas inherent in war for as long as recorded history. But the use of this term is a more recent development, which the Moral Injury Project at Syracuse (N.Y.) University describes as probably originating in the Vietnam War–era writings of veteran and peace activist Camillo “Mac” Bica and psychiatrist Jonathan Shay. Examples of wartime events that have been thought to lead to moral injury include: causing the harm or death of civilians, knowingly but without alternatives, or accidentally; failing to provide medical aid to an injured civilian or service member; and following orders that were illegal, immoral, and/or against the rules of engagement or the Geneva Conventions.
However, the occurrence of moral injuries in modern health care is increasingly being reported, primarily as an adverse effect of health care inefficiencies that can contribute to burnout. COVID-19 has now provided an array of additional stressors that can cause moral injuries among health care workers. A recent guidance document on moral injury published by the American Psychiatric Association noted that, in the context of a public health disaster, such as COVID-19, it is sometimes necessary to transition from ordinary standards of care to those more appropriate in a crisis, as in wartime. This forces us all to confront challenging questions for which there may be no clear answers, and to make “lose-lose” choices in which no one involved – patients, family, or clinicians – ends up feeling satisfied or even comfortable.
Our lives have been altered significantly, and for many, completely turned upside down by enormous sacrifices and tragic losses. Globally, physicians account for over half of healthcare worker deaths. In the United States alone, over 900 health care workers have died of COVID-19.
Most of us have felt the symptoms of moral injury: frustration, anger, disgust, guilt. A recent report describes three levels of stressors in health care occurring during the pandemic, which are not dissimilar to those wartime events described previously.
- Severe moral stressors, such as the denial of treatment to a COVID-19 patient owing to lack of resources, the inability to provide optimal care to non–COVID-19 patients for many reasons, and concern about passing COVID to loved ones.
- Moderate moral stressors, such as preventing visitors, especially to dying patients, triaging patients for healthcare services with inadequate information, and trying to solve the tension between the need for self-preservation and the need to treat.
- Lower-level but common moral challenges, especially in the community – for example, seeing others not protecting the community by hoarding food, gathering for large parties, and not social distancing or wearing masks. Such stressors lead to frustration and contempt, especially from healthcare workers making personal sacrifices and who may be at risk for infection caused by these behaviors.
Every one of us is affected by these stressors. I certainly am.
What are the outcomes? We know that moral injuries are a risk factor for the development of mental health problems and burnout, and not surprisingly we are seeing that mental health problems, suicidality, and substance use disorders have increased markedly during COVID-19, as recently detailed by the CDC.
Common emotions that occur in response to moral injuries are: feelings of guilt, shame, anger, sadness, anxiety, and disgust; intrapersonal outcomes, including lowered self-esteem, high self-criticism, and beliefs about being bad, damaged, unworthy, failing, or weak; interpersonal outcomes, including loss of faith in people, avoidance of intimacy, and lack of trust in authority figures; and existential and spiritual outcomes, including loss of faith in previous religious beliefs and no longer believing in a just world.
Moral injuries tend to originate primarily from systems-based problems, as we have seen with the lack of concerted national approaches to the pandemic. On the positive side, solutions typically also involve systems-based changes, which in this case may mean changes in leadership styles nationally and locally, as well as changes in the culture of medicine and the way healthcare is practiced and managed in the modern era. We are starting to see some of those changes with the increased use of telemedicine and health technologies, as well as more of a focus on the well-being of health care workers, now deemed “essential.”
As individuals, we are not helpless. There are things we can do in our workplaces to create change. I suggest:
- Acknowledge that you, like me, are affected by these stressors. This is not a secret, and you should not be ashamed of your feelings.
- Talk with your colleagues, loved ones, and friends about how you and they are affected. You are not alone. Encourage others to share their thoughts, stories, and feelings.
- Put this topic on your meeting and departmental agendas and discuss these moral issues openly with your colleagues. Allow sufficient time to engage in open dialogue.
- Work out ways of assisting those who are in high-risk situations, especially for moderate to severe injuries. Be supportive toward those affected.
- Modify policies and change rosters and rotate staff between high- and low-stress roles. Protect and support at-risk colleagues.
- Think about difficult ethical decisions in advance so they can be made by groups, not individuals, and certainly not “on the fly.”
- Keep everyone in your workplace constantly informed, especially of impending staff or equipment shortages.
- Maintain your inherent self-care and resilience with rest, good nutrition, sleep, exercise, love, caring, socialization, and work-life balance.
- Be prepared to access the many professional support services available in our community if you are intensely distressed or if the above suggestions are not enough.
Remember, we are in this together and will find strength in each other. This too will pass.
This article first appeared on Medscape.com.
Among the many tolls inflicted on health care workers by COVID-19 is one that is not as easily measured as rates of death or disease, but is no less tangible: moral injury. This is the term by which we describe the psychological, social, and spiritual impact of high-stakes situations that lead to the betrayal or transgression of our own deeply held moral beliefs and values.
The current pandemic has provided innumerable such situations that can increase the risk for moral injury, whether we deal directly with patients infected by the coronavirus or not. Telling family members they cannot visit critically ill loved ones. Delaying code activities, even momentarily, to get fully protected with personal protective equipment. Seeing patients who have delayed their necessary or preventive care. Using video rather than touch to reassure people.
Knowing that we are following guidelines from the Centers for Disease Control and Prevention does not stop our feelings of guilt. The longer this pandemic goes on, the more likely it is that these situations will begin to take a toll on us.
For most of us, being exposed to moral injuries is new; they have historically been most associated with severe traumatic wartime experiences. Soldiers, philosophers, and writers have described the ethical dilemmas inherent in war for as long as recorded history. But the use of this term is a more recent development, which the Moral Injury Project at Syracuse (N.Y.) University describes as probably originating in the Vietnam War–era writings of veteran and peace activist Camillo “Mac” Bica and psychiatrist Jonathan Shay. Examples of wartime events that have been thought to lead to moral injury include: causing the harm or death of civilians, knowingly but without alternatives, or accidentally; failing to provide medical aid to an injured civilian or service member; and following orders that were illegal, immoral, and/or against the rules of engagement or the Geneva Conventions.
However, the occurrence of moral injuries in modern health care is increasingly being reported, primarily as an adverse effect of health care inefficiencies that can contribute to burnout. COVID-19 has now provided an array of additional stressors that can cause moral injuries among health care workers. A recent guidance document on moral injury published by the American Psychiatric Association noted that, in the context of a public health disaster, such as COVID-19, it is sometimes necessary to transition from ordinary standards of care to those more appropriate in a crisis, as in wartime. This forces us all to confront challenging questions for which there may be no clear answers, and to make “lose-lose” choices in which no one involved – patients, family, or clinicians – ends up feeling satisfied or even comfortable.
Our lives have been altered significantly, and for many, completely turned upside down by enormous sacrifices and tragic losses. Globally, physicians account for over half of healthcare worker deaths. In the United States alone, over 900 health care workers have died of COVID-19.
Most of us have felt the symptoms of moral injury: frustration, anger, disgust, guilt. A recent report describes three levels of stressors in health care occurring during the pandemic, which are not dissimilar to those wartime events described previously.
- Severe moral stressors, such as the denial of treatment to a COVID-19 patient owing to lack of resources, the inability to provide optimal care to non–COVID-19 patients for many reasons, and concern about passing COVID to loved ones.
- Moderate moral stressors, such as preventing visitors, especially to dying patients, triaging patients for healthcare services with inadequate information, and trying to solve the tension between the need for self-preservation and the need to treat.
- Lower-level but common moral challenges, especially in the community – for example, seeing others not protecting the community by hoarding food, gathering for large parties, and not social distancing or wearing masks. Such stressors lead to frustration and contempt, especially from healthcare workers making personal sacrifices and who may be at risk for infection caused by these behaviors.
Every one of us is affected by these stressors. I certainly am.
What are the outcomes? We know that moral injuries are a risk factor for the development of mental health problems and burnout, and not surprisingly we are seeing that mental health problems, suicidality, and substance use disorders have increased markedly during COVID-19, as recently detailed by the CDC.
Common emotions that occur in response to moral injuries are: feelings of guilt, shame, anger, sadness, anxiety, and disgust; intrapersonal outcomes, including lowered self-esteem, high self-criticism, and beliefs about being bad, damaged, unworthy, failing, or weak; interpersonal outcomes, including loss of faith in people, avoidance of intimacy, and lack of trust in authority figures; and existential and spiritual outcomes, including loss of faith in previous religious beliefs and no longer believing in a just world.
Moral injuries tend to originate primarily from systems-based problems, as we have seen with the lack of concerted national approaches to the pandemic. On the positive side, solutions typically also involve systems-based changes, which in this case may mean changes in leadership styles nationally and locally, as well as changes in the culture of medicine and the way healthcare is practiced and managed in the modern era. We are starting to see some of those changes with the increased use of telemedicine and health technologies, as well as more of a focus on the well-being of health care workers, now deemed “essential.”
As individuals, we are not helpless. There are things we can do in our workplaces to create change. I suggest:
- Acknowledge that you, like me, are affected by these stressors. This is not a secret, and you should not be ashamed of your feelings.
- Talk with your colleagues, loved ones, and friends about how you and they are affected. You are not alone. Encourage others to share their thoughts, stories, and feelings.
- Put this topic on your meeting and departmental agendas and discuss these moral issues openly with your colleagues. Allow sufficient time to engage in open dialogue.
- Work out ways of assisting those who are in high-risk situations, especially for moderate to severe injuries. Be supportive toward those affected.
- Modify policies and change rosters and rotate staff between high- and low-stress roles. Protect and support at-risk colleagues.
- Think about difficult ethical decisions in advance so they can be made by groups, not individuals, and certainly not “on the fly.”
- Keep everyone in your workplace constantly informed, especially of impending staff or equipment shortages.
- Maintain your inherent self-care and resilience with rest, good nutrition, sleep, exercise, love, caring, socialization, and work-life balance.
- Be prepared to access the many professional support services available in our community if you are intensely distressed or if the above suggestions are not enough.
Remember, we are in this together and will find strength in each other. This too will pass.
This article first appeared on Medscape.com.
Increasing racial diversity in hospital medicine’s leadership ranks
Have you ever done something where you’re not quite sure why you did it at the time, but later on you realize it was part of some larger cosmic purpose, and you go, “Ahhh, now I understand…that’s why!”? Call it a fortuitous coincidence. Or a subconscious act of anticipation. Maybe a little push from God.
Last summer, as SHM’s Practice Analysis Committee was planning the State of Hospital Medicine survey for 2020, we received a request from SHM’s Diversity, Equity & Inclusion (DEI) Special Interest Group (SIG) to include a series of questions related to hospitalist gender, race and ethnic distribution in the new survey. We’ve generally resisted doing things like this because the SoHM is designed to capture data at the group level, not the individual level – and honestly, it’s as much as a lot of groups can do to tell us reliably how many FTEs they have, much less provide details about individual providers. In addition, the survey is already really long, and we are always looking for ways to make it shorter and easier for participants while still collecting the information report users care most about.
But we wanted to take the asks from the DEI SIG seriously, and as we considered their request, we realized that though it wasn’t practical to collect this information for individual hospital medicine group (HMG) members, we could collect it for group leaders. Little did we know last summer that issues of gender and racial diversity and equity would be so front-and-center right now, as we prepare to release the 2020 SoHM Report in early September. Ahhh, now I understand…that’s why – with the prompting of the DEI SIG – we so fortuitously chose to include those questions this year!
Here’s a sneak preview of what we learned. Among SoHM respondents, 57.1% reported that the highest-ranking leader in their HMG is White, and 23.5% of highest-ranking leaders are Asian. Only 5.5% of HMG leaders were Black/African American. Ethnicity was a separate question, and only 2.2% of HMG leaders were reported as Hispanic/Latino.
I have been profoundly moved by the wretched deaths of George Floyd and other people of color at the hands of police in recent months, and by the subsequent protests and our growing national reckoning over issues of racial equity and justice. In my efforts to understand more about race in America, I have been challenged by my friend Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., and others to go beyond just learning about these issues. I want to use my voice to advocate for change, and my actions to participate in effecting change, within the context of my sphere of influence.
So, what does that have to do with the SoHM data on HMG leader demographics? Well, it’s clear that Black and brown people are woefully underrepresented in the ranks of hospital medicine leadership.
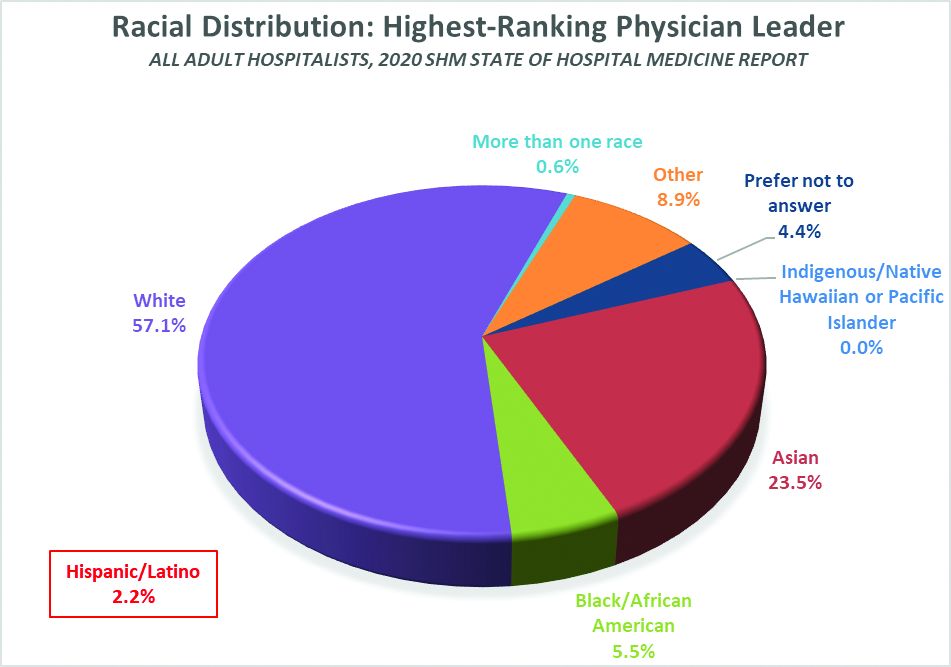
Unfortunately, we don’t have good information on racial diversity for hospitalists as a specialty, though I understand that SHM is working on plans to update membership profiles to begin collecting this information. In searching the Internet, I found a 2018 paper from the Journal of Health Care for the Poor and Underserved that studied racial and ethnic distribution of U.S. primary care physicians (doi: 10.1353/hpu.2018.0036). It reported that, in 2012, 7.8% of general internists were Black, along with 5.8% of family medicine/general practice physicians and 6.8% of pediatricians. A separate data set issued by the Association of American Medical Colleges reported that, in 2019, 6.4% of all actively practicing general internal medicine doctors were Black (5.5% of male IM physicians and 7.9% of female IM physicians). While this doesn’t mean hospitalists have the same racial and ethnic distribution, this is probably the best proxy we can come up with.
At first glance, having 5.5% of HMG leaders who are Black doesn’t seem terribly out of line with the reported range of 6.4 to 7.8% in the general population of internal medicine physicians (apologies to the family medicine and pediatric hospitalists reading this, but I’ll confine my discussion to internists for ease and brevity, since they represent the vast majority of the nation’s hospitalists). But do the math. It means Black hospitalists are likely underrepresented in HMG leadership ranks by something like 14% to 29% compared to their likely presence among hospitalists in general.
The real problem, of course, is that according the U.S. Census Bureau, 13.4% of the U.S. population is Black. So even if the racial distribution of HMG leaders catches up to the general hospitalist population, hospital medicine is still woefully underrepresenting the racial and ethnic distribution of our patient population.
The disconnect between the ethnic distribution of HMG leaders vs. hospitalists (based on general internal medicine distribution) is even more pronounced for Latinos. The JHCPU paper reported that, in 2012, 5.6% of general internists were Hispanic. The AAMC data set reported 5.8% of IM doctors were Hispanic/Latino. But only 2.2% of SoHM respondent HMGs reported a Hispanic/Latino leader, which means Latinos are underrepresented by somewhere around 61% or so relative to the likely hospitalist population, and by a whole lot more considering the fact that Latinos make up about 18.5% of the U.S. population.
I’m not saying that a White or Asian doctor can’t provide skilled, compassionate care to a Black or Latino patient, or vice-versa. It happens every day. I guess what I am saying is that we as a country and in the medical profession need to do a better job of creating pathways and promoting careers in medicine for people of color. A JAMA paper from 2019 reported that while the numbers and proportions of minority medical school matriculants has slowly been increasing from 2002 to 2017, the rate of increase was “slower than their age-matched counterparts in the U.S. population, resulting in increased underrepresentation” (doi:10.1001/jamanetworkopen.2019.10490). This means we’re falling behind, not catching up.
We need to make sure that people like Dr. Ryan Brown aren’t discouraged from pursuing medicine by teachers or school counselors because of their skin color or accent, or their gender or sexual orientation. And among those who become doctors, we need to promote hospital medicine as a desirable specialty for people of color and actively invite them in.
In my view, much of this starts with creating more and better paths to leadership within hospital medicine for people of color. Hospital medicine group leaders wield enormous – and increasing – influence, not only within their HMGs and within SHM, but within their institutions and health care systems. We need their voices and their influence to promote diversity within their groups, their institutions, within hospital medicine, and within medicine and the U.S. health care system more broadly.
The Society of Hospital Medicine is already taking steps to promote diversity, equity and inclusion. These include issuing a formal Diversity and Inclusion Statement, creating the DEI SIG, and the recent formation of a Board-designated DEI task force charged with making recommendations to promote DEI within SHM and in hospital medicine more broadly. But I want to challenge SHM to do more, particularly with regard to promoting diversity in leadership. Here are a few ideas to consider:
- Create and sponsor a mentoring program in which hospitalists volunteer to mentor minority junior high and high school students and help them prepare to pursue a career in medicine.
- Develop a formal, structured advocacy or collaboration effort with organizations like AAMC and the Accreditation Council for Graduate Medical Education designed to promote meaningful increases in the proportion of medical school students and residents who are people of color, and in the proportion who choose primary care – and ultimately, hospital medicine.
- Work hard to collect reliable racial, ethnic and gender information about SHM members and consider collaborating with MGMA to incorporate demographic questions into its survey tool for individual hospitalist compensation and productivity data. Challenge us on the Practice Analysis Committee who are responsible for the SoHM survey to continue surveying leadership demographics, and to consider how we can expand our collection of DEI information in 2022.
- Undertake a public relations campaign to highlight to health systems and other employers the under-representation of Black and Latino hospitalists in leadership positions, and to promote conscious efforts to increase those ranks.
- Create scholarships for hospitalists from underrepresented racial and ethnic groups to attend SHM-sponsored leadership development programs such as Leadership Academy, Academic Hospitalist Academy, and Quality and Safety Educators Academy, with the goal of increasing their ranks in positions of influence throughout healthcare. A scholarship program might even include raising funds to help minority hospitalists pursue Master’s-level programs such as an MBA, MHA, or MMM.
- Develop an educational track, mentoring program, or other support initiative for early-career hospitalist leaders and those interested in developing leadership skills, and ensure it gives specific attention to strategies for increasing the proportion of hospitalists of color in leadership positions.
- Review and revise existing SHM documents such as The Key Principles and Characteristics of an Effective Hospital Medicine Group, the Core Competencies in Hospital Medicine, and various white papers and position statements to ensure they address diversity, equity and inclusion – both with regard to the hospital medicine workforce and leadership, and with regard to patient care and eliminating health disparities.
I’m sure there are plenty of other similar actions we can take that I haven’t thought of. But we need to start the conversation about concrete steps our Society, and the medical specialty we represent, can take to foster real change. And then, we need to follow our words up with actions.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Have you ever done something where you’re not quite sure why you did it at the time, but later on you realize it was part of some larger cosmic purpose, and you go, “Ahhh, now I understand…that’s why!”? Call it a fortuitous coincidence. Or a subconscious act of anticipation. Maybe a little push from God.
Last summer, as SHM’s Practice Analysis Committee was planning the State of Hospital Medicine survey for 2020, we received a request from SHM’s Diversity, Equity & Inclusion (DEI) Special Interest Group (SIG) to include a series of questions related to hospitalist gender, race and ethnic distribution in the new survey. We’ve generally resisted doing things like this because the SoHM is designed to capture data at the group level, not the individual level – and honestly, it’s as much as a lot of groups can do to tell us reliably how many FTEs they have, much less provide details about individual providers. In addition, the survey is already really long, and we are always looking for ways to make it shorter and easier for participants while still collecting the information report users care most about.
But we wanted to take the asks from the DEI SIG seriously, and as we considered their request, we realized that though it wasn’t practical to collect this information for individual hospital medicine group (HMG) members, we could collect it for group leaders. Little did we know last summer that issues of gender and racial diversity and equity would be so front-and-center right now, as we prepare to release the 2020 SoHM Report in early September. Ahhh, now I understand…that’s why – with the prompting of the DEI SIG – we so fortuitously chose to include those questions this year!
Here’s a sneak preview of what we learned. Among SoHM respondents, 57.1% reported that the highest-ranking leader in their HMG is White, and 23.5% of highest-ranking leaders are Asian. Only 5.5% of HMG leaders were Black/African American. Ethnicity was a separate question, and only 2.2% of HMG leaders were reported as Hispanic/Latino.
I have been profoundly moved by the wretched deaths of George Floyd and other people of color at the hands of police in recent months, and by the subsequent protests and our growing national reckoning over issues of racial equity and justice. In my efforts to understand more about race in America, I have been challenged by my friend Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., and others to go beyond just learning about these issues. I want to use my voice to advocate for change, and my actions to participate in effecting change, within the context of my sphere of influence.
So, what does that have to do with the SoHM data on HMG leader demographics? Well, it’s clear that Black and brown people are woefully underrepresented in the ranks of hospital medicine leadership.
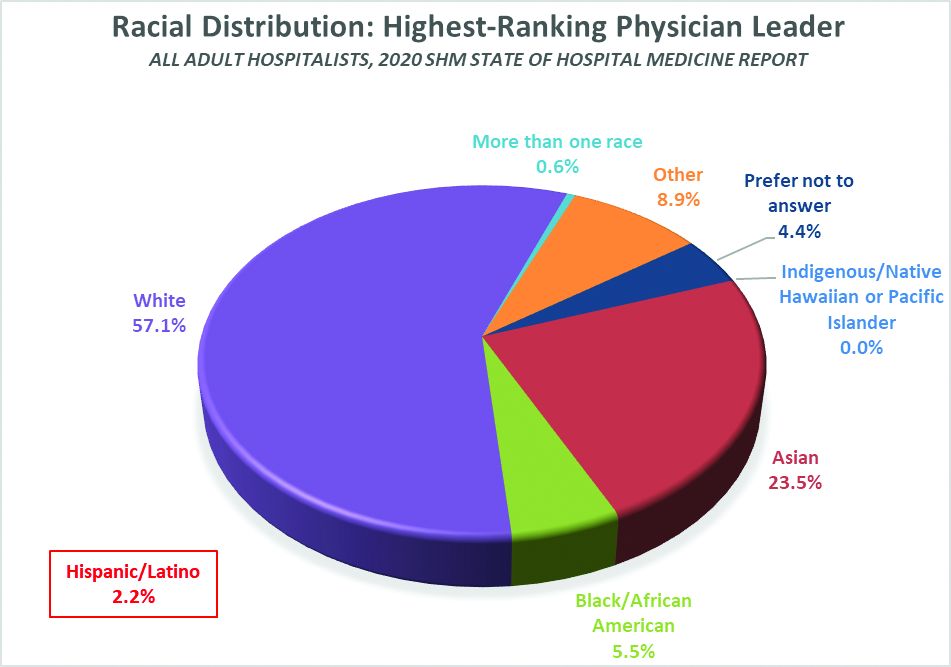
Unfortunately, we don’t have good information on racial diversity for hospitalists as a specialty, though I understand that SHM is working on plans to update membership profiles to begin collecting this information. In searching the Internet, I found a 2018 paper from the Journal of Health Care for the Poor and Underserved that studied racial and ethnic distribution of U.S. primary care physicians (doi: 10.1353/hpu.2018.0036). It reported that, in 2012, 7.8% of general internists were Black, along with 5.8% of family medicine/general practice physicians and 6.8% of pediatricians. A separate data set issued by the Association of American Medical Colleges reported that, in 2019, 6.4% of all actively practicing general internal medicine doctors were Black (5.5% of male IM physicians and 7.9% of female IM physicians). While this doesn’t mean hospitalists have the same racial and ethnic distribution, this is probably the best proxy we can come up with.
At first glance, having 5.5% of HMG leaders who are Black doesn’t seem terribly out of line with the reported range of 6.4 to 7.8% in the general population of internal medicine physicians (apologies to the family medicine and pediatric hospitalists reading this, but I’ll confine my discussion to internists for ease and brevity, since they represent the vast majority of the nation’s hospitalists). But do the math. It means Black hospitalists are likely underrepresented in HMG leadership ranks by something like 14% to 29% compared to their likely presence among hospitalists in general.
The real problem, of course, is that according the U.S. Census Bureau, 13.4% of the U.S. population is Black. So even if the racial distribution of HMG leaders catches up to the general hospitalist population, hospital medicine is still woefully underrepresenting the racial and ethnic distribution of our patient population.
The disconnect between the ethnic distribution of HMG leaders vs. hospitalists (based on general internal medicine distribution) is even more pronounced for Latinos. The JHCPU paper reported that, in 2012, 5.6% of general internists were Hispanic. The AAMC data set reported 5.8% of IM doctors were Hispanic/Latino. But only 2.2% of SoHM respondent HMGs reported a Hispanic/Latino leader, which means Latinos are underrepresented by somewhere around 61% or so relative to the likely hospitalist population, and by a whole lot more considering the fact that Latinos make up about 18.5% of the U.S. population.
I’m not saying that a White or Asian doctor can’t provide skilled, compassionate care to a Black or Latino patient, or vice-versa. It happens every day. I guess what I am saying is that we as a country and in the medical profession need to do a better job of creating pathways and promoting careers in medicine for people of color. A JAMA paper from 2019 reported that while the numbers and proportions of minority medical school matriculants has slowly been increasing from 2002 to 2017, the rate of increase was “slower than their age-matched counterparts in the U.S. population, resulting in increased underrepresentation” (doi:10.1001/jamanetworkopen.2019.10490). This means we’re falling behind, not catching up.
We need to make sure that people like Dr. Ryan Brown aren’t discouraged from pursuing medicine by teachers or school counselors because of their skin color or accent, or their gender or sexual orientation. And among those who become doctors, we need to promote hospital medicine as a desirable specialty for people of color and actively invite them in.
In my view, much of this starts with creating more and better paths to leadership within hospital medicine for people of color. Hospital medicine group leaders wield enormous – and increasing – influence, not only within their HMGs and within SHM, but within their institutions and health care systems. We need their voices and their influence to promote diversity within their groups, their institutions, within hospital medicine, and within medicine and the U.S. health care system more broadly.
The Society of Hospital Medicine is already taking steps to promote diversity, equity and inclusion. These include issuing a formal Diversity and Inclusion Statement, creating the DEI SIG, and the recent formation of a Board-designated DEI task force charged with making recommendations to promote DEI within SHM and in hospital medicine more broadly. But I want to challenge SHM to do more, particularly with regard to promoting diversity in leadership. Here are a few ideas to consider:
- Create and sponsor a mentoring program in which hospitalists volunteer to mentor minority junior high and high school students and help them prepare to pursue a career in medicine.
- Develop a formal, structured advocacy or collaboration effort with organizations like AAMC and the Accreditation Council for Graduate Medical Education designed to promote meaningful increases in the proportion of medical school students and residents who are people of color, and in the proportion who choose primary care – and ultimately, hospital medicine.
- Work hard to collect reliable racial, ethnic and gender information about SHM members and consider collaborating with MGMA to incorporate demographic questions into its survey tool for individual hospitalist compensation and productivity data. Challenge us on the Practice Analysis Committee who are responsible for the SoHM survey to continue surveying leadership demographics, and to consider how we can expand our collection of DEI information in 2022.
- Undertake a public relations campaign to highlight to health systems and other employers the under-representation of Black and Latino hospitalists in leadership positions, and to promote conscious efforts to increase those ranks.
- Create scholarships for hospitalists from underrepresented racial and ethnic groups to attend SHM-sponsored leadership development programs such as Leadership Academy, Academic Hospitalist Academy, and Quality and Safety Educators Academy, with the goal of increasing their ranks in positions of influence throughout healthcare. A scholarship program might even include raising funds to help minority hospitalists pursue Master’s-level programs such as an MBA, MHA, or MMM.
- Develop an educational track, mentoring program, or other support initiative for early-career hospitalist leaders and those interested in developing leadership skills, and ensure it gives specific attention to strategies for increasing the proportion of hospitalists of color in leadership positions.
- Review and revise existing SHM documents such as The Key Principles and Characteristics of an Effective Hospital Medicine Group, the Core Competencies in Hospital Medicine, and various white papers and position statements to ensure they address diversity, equity and inclusion – both with regard to the hospital medicine workforce and leadership, and with regard to patient care and eliminating health disparities.
I’m sure there are plenty of other similar actions we can take that I haven’t thought of. But we need to start the conversation about concrete steps our Society, and the medical specialty we represent, can take to foster real change. And then, we need to follow our words up with actions.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Have you ever done something where you’re not quite sure why you did it at the time, but later on you realize it was part of some larger cosmic purpose, and you go, “Ahhh, now I understand…that’s why!”? Call it a fortuitous coincidence. Or a subconscious act of anticipation. Maybe a little push from God.
Last summer, as SHM’s Practice Analysis Committee was planning the State of Hospital Medicine survey for 2020, we received a request from SHM’s Diversity, Equity & Inclusion (DEI) Special Interest Group (SIG) to include a series of questions related to hospitalist gender, race and ethnic distribution in the new survey. We’ve generally resisted doing things like this because the SoHM is designed to capture data at the group level, not the individual level – and honestly, it’s as much as a lot of groups can do to tell us reliably how many FTEs they have, much less provide details about individual providers. In addition, the survey is already really long, and we are always looking for ways to make it shorter and easier for participants while still collecting the information report users care most about.
But we wanted to take the asks from the DEI SIG seriously, and as we considered their request, we realized that though it wasn’t practical to collect this information for individual hospital medicine group (HMG) members, we could collect it for group leaders. Little did we know last summer that issues of gender and racial diversity and equity would be so front-and-center right now, as we prepare to release the 2020 SoHM Report in early September. Ahhh, now I understand…that’s why – with the prompting of the DEI SIG – we so fortuitously chose to include those questions this year!
Here’s a sneak preview of what we learned. Among SoHM respondents, 57.1% reported that the highest-ranking leader in their HMG is White, and 23.5% of highest-ranking leaders are Asian. Only 5.5% of HMG leaders were Black/African American. Ethnicity was a separate question, and only 2.2% of HMG leaders were reported as Hispanic/Latino.
I have been profoundly moved by the wretched deaths of George Floyd and other people of color at the hands of police in recent months, and by the subsequent protests and our growing national reckoning over issues of racial equity and justice. In my efforts to understand more about race in America, I have been challenged by my friend Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., and others to go beyond just learning about these issues. I want to use my voice to advocate for change, and my actions to participate in effecting change, within the context of my sphere of influence.
So, what does that have to do with the SoHM data on HMG leader demographics? Well, it’s clear that Black and brown people are woefully underrepresented in the ranks of hospital medicine leadership.
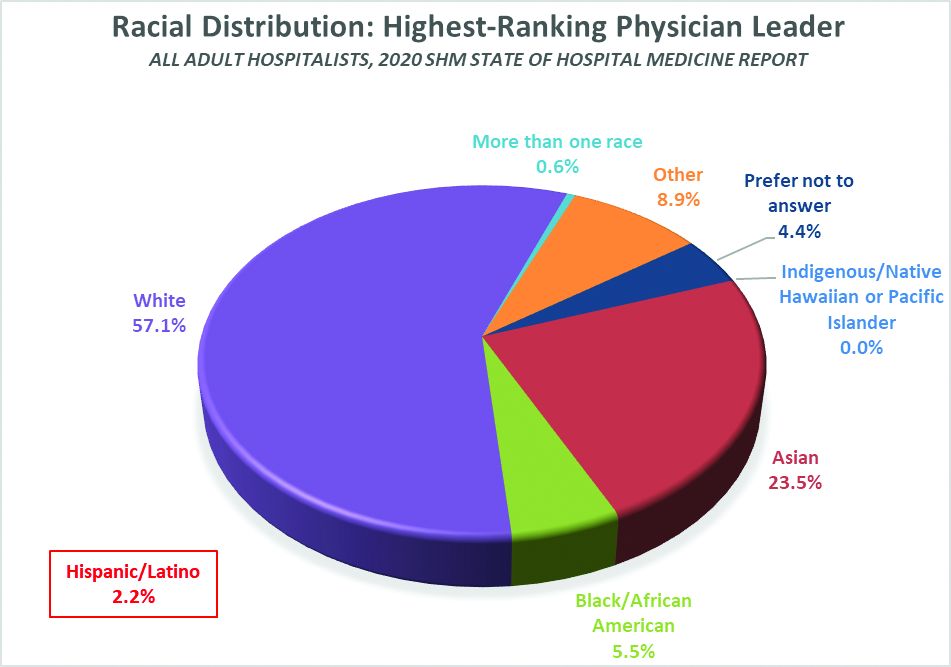
Unfortunately, we don’t have good information on racial diversity for hospitalists as a specialty, though I understand that SHM is working on plans to update membership profiles to begin collecting this information. In searching the Internet, I found a 2018 paper from the Journal of Health Care for the Poor and Underserved that studied racial and ethnic distribution of U.S. primary care physicians (doi: 10.1353/hpu.2018.0036). It reported that, in 2012, 7.8% of general internists were Black, along with 5.8% of family medicine/general practice physicians and 6.8% of pediatricians. A separate data set issued by the Association of American Medical Colleges reported that, in 2019, 6.4% of all actively practicing general internal medicine doctors were Black (5.5% of male IM physicians and 7.9% of female IM physicians). While this doesn’t mean hospitalists have the same racial and ethnic distribution, this is probably the best proxy we can come up with.
At first glance, having 5.5% of HMG leaders who are Black doesn’t seem terribly out of line with the reported range of 6.4 to 7.8% in the general population of internal medicine physicians (apologies to the family medicine and pediatric hospitalists reading this, but I’ll confine my discussion to internists for ease and brevity, since they represent the vast majority of the nation’s hospitalists). But do the math. It means Black hospitalists are likely underrepresented in HMG leadership ranks by something like 14% to 29% compared to their likely presence among hospitalists in general.
The real problem, of course, is that according the U.S. Census Bureau, 13.4% of the U.S. population is Black. So even if the racial distribution of HMG leaders catches up to the general hospitalist population, hospital medicine is still woefully underrepresenting the racial and ethnic distribution of our patient population.
The disconnect between the ethnic distribution of HMG leaders vs. hospitalists (based on general internal medicine distribution) is even more pronounced for Latinos. The JHCPU paper reported that, in 2012, 5.6% of general internists were Hispanic. The AAMC data set reported 5.8% of IM doctors were Hispanic/Latino. But only 2.2% of SoHM respondent HMGs reported a Hispanic/Latino leader, which means Latinos are underrepresented by somewhere around 61% or so relative to the likely hospitalist population, and by a whole lot more considering the fact that Latinos make up about 18.5% of the U.S. population.
I’m not saying that a White or Asian doctor can’t provide skilled, compassionate care to a Black or Latino patient, or vice-versa. It happens every day. I guess what I am saying is that we as a country and in the medical profession need to do a better job of creating pathways and promoting careers in medicine for people of color. A JAMA paper from 2019 reported that while the numbers and proportions of minority medical school matriculants has slowly been increasing from 2002 to 2017, the rate of increase was “slower than their age-matched counterparts in the U.S. population, resulting in increased underrepresentation” (doi:10.1001/jamanetworkopen.2019.10490). This means we’re falling behind, not catching up.
We need to make sure that people like Dr. Ryan Brown aren’t discouraged from pursuing medicine by teachers or school counselors because of their skin color or accent, or their gender or sexual orientation. And among those who become doctors, we need to promote hospital medicine as a desirable specialty for people of color and actively invite them in.
In my view, much of this starts with creating more and better paths to leadership within hospital medicine for people of color. Hospital medicine group leaders wield enormous – and increasing – influence, not only within their HMGs and within SHM, but within their institutions and health care systems. We need their voices and their influence to promote diversity within their groups, their institutions, within hospital medicine, and within medicine and the U.S. health care system more broadly.
The Society of Hospital Medicine is already taking steps to promote diversity, equity and inclusion. These include issuing a formal Diversity and Inclusion Statement, creating the DEI SIG, and the recent formation of a Board-designated DEI task force charged with making recommendations to promote DEI within SHM and in hospital medicine more broadly. But I want to challenge SHM to do more, particularly with regard to promoting diversity in leadership. Here are a few ideas to consider:
- Create and sponsor a mentoring program in which hospitalists volunteer to mentor minority junior high and high school students and help them prepare to pursue a career in medicine.
- Develop a formal, structured advocacy or collaboration effort with organizations like AAMC and the Accreditation Council for Graduate Medical Education designed to promote meaningful increases in the proportion of medical school students and residents who are people of color, and in the proportion who choose primary care – and ultimately, hospital medicine.
- Work hard to collect reliable racial, ethnic and gender information about SHM members and consider collaborating with MGMA to incorporate demographic questions into its survey tool for individual hospitalist compensation and productivity data. Challenge us on the Practice Analysis Committee who are responsible for the SoHM survey to continue surveying leadership demographics, and to consider how we can expand our collection of DEI information in 2022.
- Undertake a public relations campaign to highlight to health systems and other employers the under-representation of Black and Latino hospitalists in leadership positions, and to promote conscious efforts to increase those ranks.
- Create scholarships for hospitalists from underrepresented racial and ethnic groups to attend SHM-sponsored leadership development programs such as Leadership Academy, Academic Hospitalist Academy, and Quality and Safety Educators Academy, with the goal of increasing their ranks in positions of influence throughout healthcare. A scholarship program might even include raising funds to help minority hospitalists pursue Master’s-level programs such as an MBA, MHA, or MMM.
- Develop an educational track, mentoring program, or other support initiative for early-career hospitalist leaders and those interested in developing leadership skills, and ensure it gives specific attention to strategies for increasing the proportion of hospitalists of color in leadership positions.
- Review and revise existing SHM documents such as The Key Principles and Characteristics of an Effective Hospital Medicine Group, the Core Competencies in Hospital Medicine, and various white papers and position statements to ensure they address diversity, equity and inclusion – both with regard to the hospital medicine workforce and leadership, and with regard to patient care and eliminating health disparities.
I’m sure there are plenty of other similar actions we can take that I haven’t thought of. But we need to start the conversation about concrete steps our Society, and the medical specialty we represent, can take to foster real change. And then, we need to follow our words up with actions.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Treating the jowl fat overhang with deoxycholic acid
Rejuvenation of the lower face often involves treatment of the submentum and the jowls. Energy-based devices such as lasers, radiofrequency, radiofrequency microneedling, CoolSculpting, and ultrasound have been used in the tightening of the neck and jowls.
However, the only noninvasive injectable treatment approved for the reduction of submental fat is deoxycholic acid (Kybella). The mechanism of action of deoxycholic acid has been documented as adipocyte lysis, followed by a local tissue response with neutrophil infiltration, septal thickening, neocollagenesis, and neovascularization within the subcutaneous layer, with no adverse changes in the dermis or epidermis. This treatment, which has a dose-dependent response, is highly effective for submental fat reduction and jaw contouring.
In my practice, I have found that multiple consecutive treatments with deoxycholic acid (an off-label use) are effective in permanently reducing the jowl overhang with minimal adverse effects.
Jowl fat is a common cause of sagging of the jowls, and there are few alternatives to treatment with surgery or liposuction. Jowl overhang results from multiple factors related to aging, including skeletal resorption, subcutaneous atrophy, superior and inferior fat pad compartment displacement, or mandibular septum dehiscence, which allows for the accumulation of fat pockets to migrate into the neck.
A prospective study published earlier this year describes results in 66 adults with excess jowl fat, who were treated with 2 mg/cm2 of deoxycholic acid. Injections were done in patients with “pinchable fat on the jawline” and “relatively” minimal skin laxity of 0.2 mL spaced approximately 1 cm apart or 0.1 mL spaced 0.5 cm-0.75 cm apart; the mean injection volume was 0.8 mL. After 6 months, 98% of the patients experienced improvement with a mean of 1.8 treatments. Common injection site adverse events included edema, numbness, tenderness, and bruising.
In my experience, injection volumes from 1.0 mL to 1.5 mL of deoxycholic acid can be used in each jowl with minimal adverse events if proper landmarks are followed. It is crucial that the correct patient is selected (one with minimal skin laxity), and that during injection, the fat and skin are pinched away from the underlying musculature and neurovascular structures to avoid injection near the marginal mandibular nerve. Volumes less than 1.0 mL have minimal visible improvements and will require more than 3-4 treatment sessions for optimal results.
. I often see a marked improvement in patients who present prominent marionette lines who have been unhappy with fillers in the lower face. Often, the marionette lines are a result of significant overhang from jowl fat and hyaluronic acid fillers are a temporary and often unsatisfactory treatment option. The use of deoxycholic acid in the treatment of the jowl fat is a highly effective option to minimize the appearance of marionette lines caused by displaced fat pockets in the aging lower face.
Dr. Talakoub and Dr. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected] . They had no relevant disclosures.
Rejuvenation of the lower face often involves treatment of the submentum and the jowls. Energy-based devices such as lasers, radiofrequency, radiofrequency microneedling, CoolSculpting, and ultrasound have been used in the tightening of the neck and jowls.
However, the only noninvasive injectable treatment approved for the reduction of submental fat is deoxycholic acid (Kybella). The mechanism of action of deoxycholic acid has been documented as adipocyte lysis, followed by a local tissue response with neutrophil infiltration, septal thickening, neocollagenesis, and neovascularization within the subcutaneous layer, with no adverse changes in the dermis or epidermis. This treatment, which has a dose-dependent response, is highly effective for submental fat reduction and jaw contouring.
In my practice, I have found that multiple consecutive treatments with deoxycholic acid (an off-label use) are effective in permanently reducing the jowl overhang with minimal adverse effects.
Jowl fat is a common cause of sagging of the jowls, and there are few alternatives to treatment with surgery or liposuction. Jowl overhang results from multiple factors related to aging, including skeletal resorption, subcutaneous atrophy, superior and inferior fat pad compartment displacement, or mandibular septum dehiscence, which allows for the accumulation of fat pockets to migrate into the neck.
A prospective study published earlier this year describes results in 66 adults with excess jowl fat, who were treated with 2 mg/cm2 of deoxycholic acid. Injections were done in patients with “pinchable fat on the jawline” and “relatively” minimal skin laxity of 0.2 mL spaced approximately 1 cm apart or 0.1 mL spaced 0.5 cm-0.75 cm apart; the mean injection volume was 0.8 mL. After 6 months, 98% of the patients experienced improvement with a mean of 1.8 treatments. Common injection site adverse events included edema, numbness, tenderness, and bruising.
In my experience, injection volumes from 1.0 mL to 1.5 mL of deoxycholic acid can be used in each jowl with minimal adverse events if proper landmarks are followed. It is crucial that the correct patient is selected (one with minimal skin laxity), and that during injection, the fat and skin are pinched away from the underlying musculature and neurovascular structures to avoid injection near the marginal mandibular nerve. Volumes less than 1.0 mL have minimal visible improvements and will require more than 3-4 treatment sessions for optimal results.
. I often see a marked improvement in patients who present prominent marionette lines who have been unhappy with fillers in the lower face. Often, the marionette lines are a result of significant overhang from jowl fat and hyaluronic acid fillers are a temporary and often unsatisfactory treatment option. The use of deoxycholic acid in the treatment of the jowl fat is a highly effective option to minimize the appearance of marionette lines caused by displaced fat pockets in the aging lower face.
Dr. Talakoub and Dr. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected] . They had no relevant disclosures.
Rejuvenation of the lower face often involves treatment of the submentum and the jowls. Energy-based devices such as lasers, radiofrequency, radiofrequency microneedling, CoolSculpting, and ultrasound have been used in the tightening of the neck and jowls.
However, the only noninvasive injectable treatment approved for the reduction of submental fat is deoxycholic acid (Kybella). The mechanism of action of deoxycholic acid has been documented as adipocyte lysis, followed by a local tissue response with neutrophil infiltration, septal thickening, neocollagenesis, and neovascularization within the subcutaneous layer, with no adverse changes in the dermis or epidermis. This treatment, which has a dose-dependent response, is highly effective for submental fat reduction and jaw contouring.
In my practice, I have found that multiple consecutive treatments with deoxycholic acid (an off-label use) are effective in permanently reducing the jowl overhang with minimal adverse effects.
Jowl fat is a common cause of sagging of the jowls, and there are few alternatives to treatment with surgery or liposuction. Jowl overhang results from multiple factors related to aging, including skeletal resorption, subcutaneous atrophy, superior and inferior fat pad compartment displacement, or mandibular septum dehiscence, which allows for the accumulation of fat pockets to migrate into the neck.
A prospective study published earlier this year describes results in 66 adults with excess jowl fat, who were treated with 2 mg/cm2 of deoxycholic acid. Injections were done in patients with “pinchable fat on the jawline” and “relatively” minimal skin laxity of 0.2 mL spaced approximately 1 cm apart or 0.1 mL spaced 0.5 cm-0.75 cm apart; the mean injection volume was 0.8 mL. After 6 months, 98% of the patients experienced improvement with a mean of 1.8 treatments. Common injection site adverse events included edema, numbness, tenderness, and bruising.
In my experience, injection volumes from 1.0 mL to 1.5 mL of deoxycholic acid can be used in each jowl with minimal adverse events if proper landmarks are followed. It is crucial that the correct patient is selected (one with minimal skin laxity), and that during injection, the fat and skin are pinched away from the underlying musculature and neurovascular structures to avoid injection near the marginal mandibular nerve. Volumes less than 1.0 mL have minimal visible improvements and will require more than 3-4 treatment sessions for optimal results.
. I often see a marked improvement in patients who present prominent marionette lines who have been unhappy with fillers in the lower face. Often, the marionette lines are a result of significant overhang from jowl fat and hyaluronic acid fillers are a temporary and often unsatisfactory treatment option. The use of deoxycholic acid in the treatment of the jowl fat is a highly effective option to minimize the appearance of marionette lines caused by displaced fat pockets in the aging lower face.
Dr. Talakoub and Dr. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected] . They had no relevant disclosures.
Conquering the stigma of getting mental health care
Last summer, back when people traveled, I had the pleasure of being in Amsterdam for Pride Week. With a half-million tourists, it was a colorful and costumed display of LGBTQ pride, and both the streets and canals had celebrations with food, drinks, music, and displays beyond anything I could describe.
It was all not that long ago that the American Psychiatric Association classified homosexuality as a psychiatric disorder. Now we have Pride celebrations, and I don’t think twice about mentioning my brother-in-law’s husband, or a female colleague’s wife, nor am I shocked when I hear that the children of my friends are in the process of gender transition. Obviously, the idea that people express both their gender and their sexuality in diverse ways is not accepted by everyone, but we’ve come a long way toward acceptance of people who were once stigmatized and pathologized. I’ll also point out that this shift occurred despite the fact that the gay community was affected by AIDS.
There are many other differences – and illnesses – that our society has come to either accept or sympathize with more graciously over time, and yet both mental illness and substance abuse disorders remain stigmatized and punished. To put it bluntly, we have done a terrible job of making these conditions acceptable illnesses to have, even though we have done a reasonably good job of offering effective treatments. Cancer no longer carries the stigma it once did, even though cancer is a leading cause of death, and the treatments are painful, toxic, and may include the loss of body parts and hair. But if you become ill with cancer, your friends bring casseroles (or perhaps rotisserie chickens), and if you’re hospitalized with bipolar disorder or check into a drug treatment center, you’re more likely to be the recipient of judgment and even scorn.
We have to fix this. We talk about the need to destigmatize mental illness and substance use disorders, and to make these illnesses more on par with other diseases. Maybe that is the wrong call: These disorders sometimes cause people to behave in disruptive, dangerous, and illegal ways that we don’t often see with other illnesses. Frankly psychotic people may be seen as “other,” they may smell bad, they may behave in bizarre ways, and they may be frightening. Their rare acts of violence have been publicized so much that “He’s mentally ill” is accepted by the public as a full explanation for why someone would commit a mass shooting. Depression can cause people to be irritable and unpleasant, and our society equates a lack of motivation with laziness. While people may have sympathy for the suicidal thoughts and feelings of others, completed suicide leaves behind devastated survivors. People with substance use problems may become belligerent or commit crimes to support their addictions. In 2018, over 10,500 people were killed by drivers who were impaired by alcohol. I’m not sure how we destigmatize these conditions, but commercials, billboards, and educational programs aren’t doing it.
Fears around treatment
Perhaps our efforts need to go toward destigmatizing treatment. It is shocking to me how resistant people are to getting help, or having others know they are getting help, when treatment often renders them free from the psychological agony or misbehaviors caused by their condition.
Since I work in an outpatient setting, I see people who have made it beyond the barrier of seeking help. Almost all of my patients are willing to try medications – there is self-selection among those who chose to see a psychiatrist as opposed to another type of psychotherapist. I also believe that direct-to-consumer advertising has helped normalize the use of psychotropic medications.
When it comes to getting a higher level of care, however, the conversations are so much harder. Many of my patients insist they will never be admitted to a psychiatric unit, and when I ask depressed people if they are having suicidal thoughts, some tell me they are afraid to let me know they are for fear I might hospitalize them. This fear of hospitalization is present in people who have never been in a hospital and have only media depictions or their imaginations to go by, but I also see this with patients who have previously been hospitalized and have emerged from their inpatient stays feeling much better. While we know that any type of hospitalization involves a loss of control, unpleasant moments, and sometimes painful procedures, I have never heard anyone say that, if they were to have a second heart attack, they would refuse an admission to the cardiac care unit.
Discussions about treatment for substance use are even more difficult. People with addictions often don’t want to abstain from the substance they are using, and this is an enormous hurdle. Beyond that, they don’t like the labels that come with acknowledging a problem – words like “junkie,” “addict,” “drunk,” and “alcoholic” are hard to escape.
People fear hospitalization for many reasons: They fear losing control, they don’t recognize that they have a problem, or they rationalize their psychosis or substance use as normal. Most of all, they fear what others will think of them and what repercussions this will have for their futures. Patients would rather continue in a state of agony and dysfunction when inpatient treatment would make them better faster. This is nothing short of tragic.
What can we do? The answer is “a lot.” We need to work harder to make the hospital experience a pleasant one for patients. Inpatient units need to be clean, safe places where patients are treated with kindness, dignity, and respect and activities are appropriate, interesting, and promote healing.
Maria, a Maryland attorney, told me about her experience with inpatient treatment. “I experienced my hospitalization as jailing and acutely felt the loss of liberty, especially in the ER, where I was confined to something I recognized from my time visiting incarcerated and detained people as a holding cell, complete with a uniformed guard. I was scared to engage in any kind of meaningful self-advocacy around leaving out of fear for my license to practice law and of lengthening my time as an inpatient. As a result, I found myself concentrating on getting out, and not on getting well. With the benefit of hindsight, I can say now that my hospitalization was a lost opportunity, and the coercive elements were barriers to accessing the treatment that I needed, both at the time and in the years following the hospitalization.”
We have too many policies in place where infractions are met with force, seclusion, and sometimes restraint, and we need to be more flexible with these policies. If a psychiatric unit requires lab work prior to admission and the patient refuses, should force be used in the emergency department if there is nothing to indicate that the patient’s health is in imminent danger? And if the hospital has a policy that all psychiatric patients must disrobe to be examined for preexisting scars or contraband – this is an admission standard for some hospitals, but not others – and the patient refuses, what then? Typically, inpatients are not allowed access to their cell phones or the Internet (for many good reasons), but patients find this very upsetting; might it make sense to allow periods where they can use devices with supervision? Hospitals often forbid smoking, and people with psychiatric disorders may smoke – while it is a wonderful health ideal, is it reasonable to forbid smoking for the course of a hospitalization?
We must work to get questions about psychiatric and substance use disorders removed from any job- or licensure-related forms. There is no reason to believe that people answer these forms truthfully or that including these questions protects the public in any way. What we do know is that people don’t seek help because they, like Maria, are afraid of the consequences of getting care. It doesn’t matter if a surgeon’s abilities are limited because he has episodes of hypoglycemia or past episodes of mania, and the only question on licensing forms should be about current conditions that impair the ability to work. Every district branch of the American Psychiatric Association should be actively speaking with their state professional licensing boards about the harm these questions do.
We need better treatments that have fewer side effects, and we need to acknowledge that, while getting help is the right thing to do, not everyone finds the right treatment with the first attempt and not everyone gets better. Our party line to those who feel suicidal has been “Get Help,” often with a phone number for the National Suicide Prevention Lifeline. While this is an important resource to have readily available, many of the people who die of suicide are already in active treatment. Our party line needs to change to “Get Help, and if it isn’t working, Get Different Help.” We want to be careful that our messaging does not foster a sense of hopelessness in those who have sought care and still suffer.
It’s good to talk about the potential benefits of treatment, but we don’t have enough beds and we don’t have enough mental health clinicians. There are states where psychiatric patients who have committed no crime are held in jail cells while they wait for beds to open – that we allow this is nothing short of a disgrace. The sickest patients with treatment-resistant conditions need access to the best care, and that access should not be limited by finances or networks. And while I’m here: We need our mental health professionals to spend their time working with patients, not computer screens, check boxes, and prior authorization protocols.
Finally, we need to work with the media to show positive and accurate depictions of psychiatric treatment as something that helps. We are still undoing the harm of Nurse Ratched and the depiction of electroconvulsive therapy in the 1975 film “One Flew Over the Cuckoo’s Nest,” and the current focus on mental illness and violence does nothing to help people feel comfortable seeking care.
I’ll end with one more thought from Maria: “Mental health professionals need to talk about hospitalization up front, no matter how uncomfortable, and encourage patients to think about hospitalization as a treatment option on a continuum before it is needed, so they are not approaching hospitalization as an abstract concept, often with a lot of fear and stigma attached to it, but rather as an option that they might explore in a fact-based way.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore. She reported having nothing to disclose.
Last summer, back when people traveled, I had the pleasure of being in Amsterdam for Pride Week. With a half-million tourists, it was a colorful and costumed display of LGBTQ pride, and both the streets and canals had celebrations with food, drinks, music, and displays beyond anything I could describe.
It was all not that long ago that the American Psychiatric Association classified homosexuality as a psychiatric disorder. Now we have Pride celebrations, and I don’t think twice about mentioning my brother-in-law’s husband, or a female colleague’s wife, nor am I shocked when I hear that the children of my friends are in the process of gender transition. Obviously, the idea that people express both their gender and their sexuality in diverse ways is not accepted by everyone, but we’ve come a long way toward acceptance of people who were once stigmatized and pathologized. I’ll also point out that this shift occurred despite the fact that the gay community was affected by AIDS.
There are many other differences – and illnesses – that our society has come to either accept or sympathize with more graciously over time, and yet both mental illness and substance abuse disorders remain stigmatized and punished. To put it bluntly, we have done a terrible job of making these conditions acceptable illnesses to have, even though we have done a reasonably good job of offering effective treatments. Cancer no longer carries the stigma it once did, even though cancer is a leading cause of death, and the treatments are painful, toxic, and may include the loss of body parts and hair. But if you become ill with cancer, your friends bring casseroles (or perhaps rotisserie chickens), and if you’re hospitalized with bipolar disorder or check into a drug treatment center, you’re more likely to be the recipient of judgment and even scorn.
We have to fix this. We talk about the need to destigmatize mental illness and substance use disorders, and to make these illnesses more on par with other diseases. Maybe that is the wrong call: These disorders sometimes cause people to behave in disruptive, dangerous, and illegal ways that we don’t often see with other illnesses. Frankly psychotic people may be seen as “other,” they may smell bad, they may behave in bizarre ways, and they may be frightening. Their rare acts of violence have been publicized so much that “He’s mentally ill” is accepted by the public as a full explanation for why someone would commit a mass shooting. Depression can cause people to be irritable and unpleasant, and our society equates a lack of motivation with laziness. While people may have sympathy for the suicidal thoughts and feelings of others, completed suicide leaves behind devastated survivors. People with substance use problems may become belligerent or commit crimes to support their addictions. In 2018, over 10,500 people were killed by drivers who were impaired by alcohol. I’m not sure how we destigmatize these conditions, but commercials, billboards, and educational programs aren’t doing it.
Fears around treatment
Perhaps our efforts need to go toward destigmatizing treatment. It is shocking to me how resistant people are to getting help, or having others know they are getting help, when treatment often renders them free from the psychological agony or misbehaviors caused by their condition.
Since I work in an outpatient setting, I see people who have made it beyond the barrier of seeking help. Almost all of my patients are willing to try medications – there is self-selection among those who chose to see a psychiatrist as opposed to another type of psychotherapist. I also believe that direct-to-consumer advertising has helped normalize the use of psychotropic medications.
When it comes to getting a higher level of care, however, the conversations are so much harder. Many of my patients insist they will never be admitted to a psychiatric unit, and when I ask depressed people if they are having suicidal thoughts, some tell me they are afraid to let me know they are for fear I might hospitalize them. This fear of hospitalization is present in people who have never been in a hospital and have only media depictions or their imaginations to go by, but I also see this with patients who have previously been hospitalized and have emerged from their inpatient stays feeling much better. While we know that any type of hospitalization involves a loss of control, unpleasant moments, and sometimes painful procedures, I have never heard anyone say that, if they were to have a second heart attack, they would refuse an admission to the cardiac care unit.
Discussions about treatment for substance use are even more difficult. People with addictions often don’t want to abstain from the substance they are using, and this is an enormous hurdle. Beyond that, they don’t like the labels that come with acknowledging a problem – words like “junkie,” “addict,” “drunk,” and “alcoholic” are hard to escape.
People fear hospitalization for many reasons: They fear losing control, they don’t recognize that they have a problem, or they rationalize their psychosis or substance use as normal. Most of all, they fear what others will think of them and what repercussions this will have for their futures. Patients would rather continue in a state of agony and dysfunction when inpatient treatment would make them better faster. This is nothing short of tragic.
What can we do? The answer is “a lot.” We need to work harder to make the hospital experience a pleasant one for patients. Inpatient units need to be clean, safe places where patients are treated with kindness, dignity, and respect and activities are appropriate, interesting, and promote healing.
Maria, a Maryland attorney, told me about her experience with inpatient treatment. “I experienced my hospitalization as jailing and acutely felt the loss of liberty, especially in the ER, where I was confined to something I recognized from my time visiting incarcerated and detained people as a holding cell, complete with a uniformed guard. I was scared to engage in any kind of meaningful self-advocacy around leaving out of fear for my license to practice law and of lengthening my time as an inpatient. As a result, I found myself concentrating on getting out, and not on getting well. With the benefit of hindsight, I can say now that my hospitalization was a lost opportunity, and the coercive elements were barriers to accessing the treatment that I needed, both at the time and in the years following the hospitalization.”
We have too many policies in place where infractions are met with force, seclusion, and sometimes restraint, and we need to be more flexible with these policies. If a psychiatric unit requires lab work prior to admission and the patient refuses, should force be used in the emergency department if there is nothing to indicate that the patient’s health is in imminent danger? And if the hospital has a policy that all psychiatric patients must disrobe to be examined for preexisting scars or contraband – this is an admission standard for some hospitals, but not others – and the patient refuses, what then? Typically, inpatients are not allowed access to their cell phones or the Internet (for many good reasons), but patients find this very upsetting; might it make sense to allow periods where they can use devices with supervision? Hospitals often forbid smoking, and people with psychiatric disorders may smoke – while it is a wonderful health ideal, is it reasonable to forbid smoking for the course of a hospitalization?
We must work to get questions about psychiatric and substance use disorders removed from any job- or licensure-related forms. There is no reason to believe that people answer these forms truthfully or that including these questions protects the public in any way. What we do know is that people don’t seek help because they, like Maria, are afraid of the consequences of getting care. It doesn’t matter if a surgeon’s abilities are limited because he has episodes of hypoglycemia or past episodes of mania, and the only question on licensing forms should be about current conditions that impair the ability to work. Every district branch of the American Psychiatric Association should be actively speaking with their state professional licensing boards about the harm these questions do.
We need better treatments that have fewer side effects, and we need to acknowledge that, while getting help is the right thing to do, not everyone finds the right treatment with the first attempt and not everyone gets better. Our party line to those who feel suicidal has been “Get Help,” often with a phone number for the National Suicide Prevention Lifeline. While this is an important resource to have readily available, many of the people who die of suicide are already in active treatment. Our party line needs to change to “Get Help, and if it isn’t working, Get Different Help.” We want to be careful that our messaging does not foster a sense of hopelessness in those who have sought care and still suffer.
It’s good to talk about the potential benefits of treatment, but we don’t have enough beds and we don’t have enough mental health clinicians. There are states where psychiatric patients who have committed no crime are held in jail cells while they wait for beds to open – that we allow this is nothing short of a disgrace. The sickest patients with treatment-resistant conditions need access to the best care, and that access should not be limited by finances or networks. And while I’m here: We need our mental health professionals to spend their time working with patients, not computer screens, check boxes, and prior authorization protocols.
Finally, we need to work with the media to show positive and accurate depictions of psychiatric treatment as something that helps. We are still undoing the harm of Nurse Ratched and the depiction of electroconvulsive therapy in the 1975 film “One Flew Over the Cuckoo’s Nest,” and the current focus on mental illness and violence does nothing to help people feel comfortable seeking care.
I’ll end with one more thought from Maria: “Mental health professionals need to talk about hospitalization up front, no matter how uncomfortable, and encourage patients to think about hospitalization as a treatment option on a continuum before it is needed, so they are not approaching hospitalization as an abstract concept, often with a lot of fear and stigma attached to it, but rather as an option that they might explore in a fact-based way.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore. She reported having nothing to disclose.
Last summer, back when people traveled, I had the pleasure of being in Amsterdam for Pride Week. With a half-million tourists, it was a colorful and costumed display of LGBTQ pride, and both the streets and canals had celebrations with food, drinks, music, and displays beyond anything I could describe.
It was all not that long ago that the American Psychiatric Association classified homosexuality as a psychiatric disorder. Now we have Pride celebrations, and I don’t think twice about mentioning my brother-in-law’s husband, or a female colleague’s wife, nor am I shocked when I hear that the children of my friends are in the process of gender transition. Obviously, the idea that people express both their gender and their sexuality in diverse ways is not accepted by everyone, but we’ve come a long way toward acceptance of people who were once stigmatized and pathologized. I’ll also point out that this shift occurred despite the fact that the gay community was affected by AIDS.
There are many other differences – and illnesses – that our society has come to either accept or sympathize with more graciously over time, and yet both mental illness and substance abuse disorders remain stigmatized and punished. To put it bluntly, we have done a terrible job of making these conditions acceptable illnesses to have, even though we have done a reasonably good job of offering effective treatments. Cancer no longer carries the stigma it once did, even though cancer is a leading cause of death, and the treatments are painful, toxic, and may include the loss of body parts and hair. But if you become ill with cancer, your friends bring casseroles (or perhaps rotisserie chickens), and if you’re hospitalized with bipolar disorder or check into a drug treatment center, you’re more likely to be the recipient of judgment and even scorn.
We have to fix this. We talk about the need to destigmatize mental illness and substance use disorders, and to make these illnesses more on par with other diseases. Maybe that is the wrong call: These disorders sometimes cause people to behave in disruptive, dangerous, and illegal ways that we don’t often see with other illnesses. Frankly psychotic people may be seen as “other,” they may smell bad, they may behave in bizarre ways, and they may be frightening. Their rare acts of violence have been publicized so much that “He’s mentally ill” is accepted by the public as a full explanation for why someone would commit a mass shooting. Depression can cause people to be irritable and unpleasant, and our society equates a lack of motivation with laziness. While people may have sympathy for the suicidal thoughts and feelings of others, completed suicide leaves behind devastated survivors. People with substance use problems may become belligerent or commit crimes to support their addictions. In 2018, over 10,500 people were killed by drivers who were impaired by alcohol. I’m not sure how we destigmatize these conditions, but commercials, billboards, and educational programs aren’t doing it.
Fears around treatment
Perhaps our efforts need to go toward destigmatizing treatment. It is shocking to me how resistant people are to getting help, or having others know they are getting help, when treatment often renders them free from the psychological agony or misbehaviors caused by their condition.
Since I work in an outpatient setting, I see people who have made it beyond the barrier of seeking help. Almost all of my patients are willing to try medications – there is self-selection among those who chose to see a psychiatrist as opposed to another type of psychotherapist. I also believe that direct-to-consumer advertising has helped normalize the use of psychotropic medications.
When it comes to getting a higher level of care, however, the conversations are so much harder. Many of my patients insist they will never be admitted to a psychiatric unit, and when I ask depressed people if they are having suicidal thoughts, some tell me they are afraid to let me know they are for fear I might hospitalize them. This fear of hospitalization is present in people who have never been in a hospital and have only media depictions or their imaginations to go by, but I also see this with patients who have previously been hospitalized and have emerged from their inpatient stays feeling much better. While we know that any type of hospitalization involves a loss of control, unpleasant moments, and sometimes painful procedures, I have never heard anyone say that, if they were to have a second heart attack, they would refuse an admission to the cardiac care unit.
Discussions about treatment for substance use are even more difficult. People with addictions often don’t want to abstain from the substance they are using, and this is an enormous hurdle. Beyond that, they don’t like the labels that come with acknowledging a problem – words like “junkie,” “addict,” “drunk,” and “alcoholic” are hard to escape.
People fear hospitalization for many reasons: They fear losing control, they don’t recognize that they have a problem, or they rationalize their psychosis or substance use as normal. Most of all, they fear what others will think of them and what repercussions this will have for their futures. Patients would rather continue in a state of agony and dysfunction when inpatient treatment would make them better faster. This is nothing short of tragic.
What can we do? The answer is “a lot.” We need to work harder to make the hospital experience a pleasant one for patients. Inpatient units need to be clean, safe places where patients are treated with kindness, dignity, and respect and activities are appropriate, interesting, and promote healing.
Maria, a Maryland attorney, told me about her experience with inpatient treatment. “I experienced my hospitalization as jailing and acutely felt the loss of liberty, especially in the ER, where I was confined to something I recognized from my time visiting incarcerated and detained people as a holding cell, complete with a uniformed guard. I was scared to engage in any kind of meaningful self-advocacy around leaving out of fear for my license to practice law and of lengthening my time as an inpatient. As a result, I found myself concentrating on getting out, and not on getting well. With the benefit of hindsight, I can say now that my hospitalization was a lost opportunity, and the coercive elements were barriers to accessing the treatment that I needed, both at the time and in the years following the hospitalization.”
We have too many policies in place where infractions are met with force, seclusion, and sometimes restraint, and we need to be more flexible with these policies. If a psychiatric unit requires lab work prior to admission and the patient refuses, should force be used in the emergency department if there is nothing to indicate that the patient’s health is in imminent danger? And if the hospital has a policy that all psychiatric patients must disrobe to be examined for preexisting scars or contraband – this is an admission standard for some hospitals, but not others – and the patient refuses, what then? Typically, inpatients are not allowed access to their cell phones or the Internet (for many good reasons), but patients find this very upsetting; might it make sense to allow periods where they can use devices with supervision? Hospitals often forbid smoking, and people with psychiatric disorders may smoke – while it is a wonderful health ideal, is it reasonable to forbid smoking for the course of a hospitalization?
We must work to get questions about psychiatric and substance use disorders removed from any job- or licensure-related forms. There is no reason to believe that people answer these forms truthfully or that including these questions protects the public in any way. What we do know is that people don’t seek help because they, like Maria, are afraid of the consequences of getting care. It doesn’t matter if a surgeon’s abilities are limited because he has episodes of hypoglycemia or past episodes of mania, and the only question on licensing forms should be about current conditions that impair the ability to work. Every district branch of the American Psychiatric Association should be actively speaking with their state professional licensing boards about the harm these questions do.
We need better treatments that have fewer side effects, and we need to acknowledge that, while getting help is the right thing to do, not everyone finds the right treatment with the first attempt and not everyone gets better. Our party line to those who feel suicidal has been “Get Help,” often with a phone number for the National Suicide Prevention Lifeline. While this is an important resource to have readily available, many of the people who die of suicide are already in active treatment. Our party line needs to change to “Get Help, and if it isn’t working, Get Different Help.” We want to be careful that our messaging does not foster a sense of hopelessness in those who have sought care and still suffer.
It’s good to talk about the potential benefits of treatment, but we don’t have enough beds and we don’t have enough mental health clinicians. There are states where psychiatric patients who have committed no crime are held in jail cells while they wait for beds to open – that we allow this is nothing short of a disgrace. The sickest patients with treatment-resistant conditions need access to the best care, and that access should not be limited by finances or networks. And while I’m here: We need our mental health professionals to spend their time working with patients, not computer screens, check boxes, and prior authorization protocols.
Finally, we need to work with the media to show positive and accurate depictions of psychiatric treatment as something that helps. We are still undoing the harm of Nurse Ratched and the depiction of electroconvulsive therapy in the 1975 film “One Flew Over the Cuckoo’s Nest,” and the current focus on mental illness and violence does nothing to help people feel comfortable seeking care.
I’ll end with one more thought from Maria: “Mental health professionals need to talk about hospitalization up front, no matter how uncomfortable, and encourage patients to think about hospitalization as a treatment option on a continuum before it is needed, so they are not approaching hospitalization as an abstract concept, often with a lot of fear and stigma attached to it, but rather as an option that they might explore in a fact-based way.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore. She reported having nothing to disclose.























