User login
Flattening the hierarchy
What fellows can learn about leadership from aircraft crews
Fellowship is a time of great growth for pediatric hospital medicine fellows as clinicians, educators, scholars, and as leaders. Leadership is a crucial skill for hospitalists that is cultivated throughout fellowship. As fellows, we step into the role of clinical team leader for the first time and it is our responsibility to create a clinical and educational environment that is safe, inviting and engaging.
For possibly the first time in our careers, pediatric hospital medicine fellows are expected to make final decisions, big and small. We are faced with high-pressure situations almost daily, whether it is a rapid response on a patient, tough diagnostic and therapeutic decisions, difficult conversations with families, or dealing with challenging team members.
Soon after starting fellowship I was faced with a such a situation. The patient was a 6-month-old infant with trisomy 21 who was admitted because of feeding difficulties. They were working on oral feeds but required nasogastric (NG) feeds to meet caloric needs. On my first day on service, the residents indicated that the medical team desired the patient to have a gastrostomy tube (G-tube) placed. I was hoping to send the patient home for a few weeks with the NG tube to see if they were making progress on their oral feeds before deciding on the need for a G-tube. However, the patient’s parents pulled me aside in the hallway and said they were considering a third possibility.
The parents felt strongly about a trial period of a few weeks without the NG tube to see if the patient was able to maintain adequate weight gain with just oral feeds. The bedside nurse reiterated that the family felt their concerns had not been considered up until this point. As the fellow and team leader, it was my job to navigate between my resident team, myself, and the family in order to make a final decision. Through a bedside meeting and shared decision making, we were able to compromise and negotiate a decision, allowing the patient to go home on just oral feeds with close follow-up with their pediatrician. Afterwards, I found myself searching for strategies to be a better leader in these situations.
I found a potential answer in a recent article from the Harvard Business Review titled “What Aircraft Crews Know About Managing High-Pressure Situations.”1 The article discusses crew resource management (CRM), which was developed in the 1980s and is used in civil and military aviation worldwide. CRM is based on two principles to improve crisis management: The hierarchy on the flight deck must be flattened, and crew members must be actively integrated into the flight’s work flows and decision-making processes.
The authors of the article conducted two different studies to further understand CRM and its effects. The first study included observing 11 flight crews in emergency simulations. In the study, the flight crew had to react to an emergency, and then conduct a landing of the aircraft. What the authors found was that the captain’s style of communication had a major impact on crew performance in two major ways: Crews performed consistently better under times of pressure when the copilot was included in the decision-making process, and captains who asked open-ended questions (“How do you assess the situation”) came up with better solutions than captains who asked “yes or no” questions.
The authors conclude that “involving colleagues as equal decision partners by asking them questions…aids constructive, factual information exchange.” The second study consisted of conducting 61 interviews with flight crew members to better understand crisis management. In the interviews, the same theme occurred, that open-ended questions are vital in all decision-making processes and may be preventative against dangerous or imperfect outcomes. As fellows and team leaders we can learn from CRM and these studies. We need to flatten the hierarchy and ask open-ended questions.
To flatten the hierarchy, we should value the thoughts and opinions of all our team members. Now more than ever in this current COVID-19 pandemic with many hospitals instituting telehealth/telerounding for some or all team members, it is essential to utilize our entire “flight crew” (physicians, nurses, therapists, subspecialists, social worker, case managers, etc.) during routine decisions and high-stake decisions. We should make sure our flight crew, especially the bedside nurse is part of the decision-making process.2 This means we need to ensure they are present and given a voice on clinical rounds. To flatten the hierarchy, we must take pride in eliciting other team member’s opinions. We must realize that we alone do not have all the answers, and other team members may have different frameworks in which they process a decision.
Finally, in medicine, our patients and families are included in our flight crew. They too must have a voice in the decision-making process. Previous studies have shown that patients and families desire to be included in the decision-making process, and opportunities exist to improve shared decision-making in pediatrics.3-5 Lastly, we should commit to asking open-ended questions from our team and our patients. We should value their input and use their answers and frameworks to make the best decision for our patients.
I wasn’t aware at the time, but I was using some of the principles of CRM while navigating my high-pressure situation. A bedside meeting with all team members and the patient’s family helped to flatten the hierarchy by understanding and valuing each team member’s input. Asking open-ended questions of the different team members led to a more inviting and engaging clinical and learning environment. These strategies helped to lead our team into a clinical decision that wasn’t entirely clear at first but ended up being the best decision for the patient, as they are now thriving without ever requiring supplemental nutrition after discharge.
As physicians, we have learned a lot from the airline industry about wellness and the effect of fatigue on performance. It is clear now that we can also learn from them about clinical decision-making and leadership strategies. When adopted for health care, CRM principles have been shown to result in a culture of safety and long-term behavioral change.6,7 If we can model ourselves after the airline industry by following the principles of CRM, then we will be better clinicians, educators, and leaders.
Dr. Palmer is a second-year pediatric hospital medicine fellow at Children’s Hospital Los Angeles and is working toward a masters in academic medicine at the University of Southern California, Los Angeles, with a focus on curriculum development and educational scholarship production.
References
1. Hagan J et al. What Aircraft Crews Know About Managing High-Pressure Situations. Harvard Business Review. 2019 Dec. https://hbr.org/2019/12/what-aircraft-crews-know-about-managing-high-pressure-situations
2. Erickson J. Bedside nurse involvement in end-of-life decision-making: A brief review of the literature. Dimens Crit Care Nurs. 2013;32(2):65-8.
3. Richards CA et al. Physicians perceptions of shared decision-making in neonatal and pediatric critical care. Am J Hosp Palliat Care. 2018;35(4):669-76.
4. Boland L et al. Barriers and facilitators of pediatric shared decision-making: A systematic review. Implement Sci. 2019 Jan 18. doi: 10.1186/s13012-018-0851-5.
5. Blankenburg R et al. Shared decision-making during inpatient rounds: Opportunities for improvement in patient engagement and communication. J Hosp Med. 2018;13(7):453-61.
6. Kemper PF et al. Crew resource management training in the intensive care unit. A multisite controlled before-after study. BMJ Qual Saf. 2016;25(8):577-87.
7. Sax HC et al. Can aviation-based team training elicit sustainable behavioral change? Arch Surg. 2009;144(12):1133-7.
What fellows can learn about leadership from aircraft crews
What fellows can learn about leadership from aircraft crews
Fellowship is a time of great growth for pediatric hospital medicine fellows as clinicians, educators, scholars, and as leaders. Leadership is a crucial skill for hospitalists that is cultivated throughout fellowship. As fellows, we step into the role of clinical team leader for the first time and it is our responsibility to create a clinical and educational environment that is safe, inviting and engaging.
For possibly the first time in our careers, pediatric hospital medicine fellows are expected to make final decisions, big and small. We are faced with high-pressure situations almost daily, whether it is a rapid response on a patient, tough diagnostic and therapeutic decisions, difficult conversations with families, or dealing with challenging team members.
Soon after starting fellowship I was faced with a such a situation. The patient was a 6-month-old infant with trisomy 21 who was admitted because of feeding difficulties. They were working on oral feeds but required nasogastric (NG) feeds to meet caloric needs. On my first day on service, the residents indicated that the medical team desired the patient to have a gastrostomy tube (G-tube) placed. I was hoping to send the patient home for a few weeks with the NG tube to see if they were making progress on their oral feeds before deciding on the need for a G-tube. However, the patient’s parents pulled me aside in the hallway and said they were considering a third possibility.
The parents felt strongly about a trial period of a few weeks without the NG tube to see if the patient was able to maintain adequate weight gain with just oral feeds. The bedside nurse reiterated that the family felt their concerns had not been considered up until this point. As the fellow and team leader, it was my job to navigate between my resident team, myself, and the family in order to make a final decision. Through a bedside meeting and shared decision making, we were able to compromise and negotiate a decision, allowing the patient to go home on just oral feeds with close follow-up with their pediatrician. Afterwards, I found myself searching for strategies to be a better leader in these situations.
I found a potential answer in a recent article from the Harvard Business Review titled “What Aircraft Crews Know About Managing High-Pressure Situations.”1 The article discusses crew resource management (CRM), which was developed in the 1980s and is used in civil and military aviation worldwide. CRM is based on two principles to improve crisis management: The hierarchy on the flight deck must be flattened, and crew members must be actively integrated into the flight’s work flows and decision-making processes.
The authors of the article conducted two different studies to further understand CRM and its effects. The first study included observing 11 flight crews in emergency simulations. In the study, the flight crew had to react to an emergency, and then conduct a landing of the aircraft. What the authors found was that the captain’s style of communication had a major impact on crew performance in two major ways: Crews performed consistently better under times of pressure when the copilot was included in the decision-making process, and captains who asked open-ended questions (“How do you assess the situation”) came up with better solutions than captains who asked “yes or no” questions.
The authors conclude that “involving colleagues as equal decision partners by asking them questions…aids constructive, factual information exchange.” The second study consisted of conducting 61 interviews with flight crew members to better understand crisis management. In the interviews, the same theme occurred, that open-ended questions are vital in all decision-making processes and may be preventative against dangerous or imperfect outcomes. As fellows and team leaders we can learn from CRM and these studies. We need to flatten the hierarchy and ask open-ended questions.
To flatten the hierarchy, we should value the thoughts and opinions of all our team members. Now more than ever in this current COVID-19 pandemic with many hospitals instituting telehealth/telerounding for some or all team members, it is essential to utilize our entire “flight crew” (physicians, nurses, therapists, subspecialists, social worker, case managers, etc.) during routine decisions and high-stake decisions. We should make sure our flight crew, especially the bedside nurse is part of the decision-making process.2 This means we need to ensure they are present and given a voice on clinical rounds. To flatten the hierarchy, we must take pride in eliciting other team member’s opinions. We must realize that we alone do not have all the answers, and other team members may have different frameworks in which they process a decision.
Finally, in medicine, our patients and families are included in our flight crew. They too must have a voice in the decision-making process. Previous studies have shown that patients and families desire to be included in the decision-making process, and opportunities exist to improve shared decision-making in pediatrics.3-5 Lastly, we should commit to asking open-ended questions from our team and our patients. We should value their input and use their answers and frameworks to make the best decision for our patients.
I wasn’t aware at the time, but I was using some of the principles of CRM while navigating my high-pressure situation. A bedside meeting with all team members and the patient’s family helped to flatten the hierarchy by understanding and valuing each team member’s input. Asking open-ended questions of the different team members led to a more inviting and engaging clinical and learning environment. These strategies helped to lead our team into a clinical decision that wasn’t entirely clear at first but ended up being the best decision for the patient, as they are now thriving without ever requiring supplemental nutrition after discharge.
As physicians, we have learned a lot from the airline industry about wellness and the effect of fatigue on performance. It is clear now that we can also learn from them about clinical decision-making and leadership strategies. When adopted for health care, CRM principles have been shown to result in a culture of safety and long-term behavioral change.6,7 If we can model ourselves after the airline industry by following the principles of CRM, then we will be better clinicians, educators, and leaders.
Dr. Palmer is a second-year pediatric hospital medicine fellow at Children’s Hospital Los Angeles and is working toward a masters in academic medicine at the University of Southern California, Los Angeles, with a focus on curriculum development and educational scholarship production.
References
1. Hagan J et al. What Aircraft Crews Know About Managing High-Pressure Situations. Harvard Business Review. 2019 Dec. https://hbr.org/2019/12/what-aircraft-crews-know-about-managing-high-pressure-situations
2. Erickson J. Bedside nurse involvement in end-of-life decision-making: A brief review of the literature. Dimens Crit Care Nurs. 2013;32(2):65-8.
3. Richards CA et al. Physicians perceptions of shared decision-making in neonatal and pediatric critical care. Am J Hosp Palliat Care. 2018;35(4):669-76.
4. Boland L et al. Barriers and facilitators of pediatric shared decision-making: A systematic review. Implement Sci. 2019 Jan 18. doi: 10.1186/s13012-018-0851-5.
5. Blankenburg R et al. Shared decision-making during inpatient rounds: Opportunities for improvement in patient engagement and communication. J Hosp Med. 2018;13(7):453-61.
6. Kemper PF et al. Crew resource management training in the intensive care unit. A multisite controlled before-after study. BMJ Qual Saf. 2016;25(8):577-87.
7. Sax HC et al. Can aviation-based team training elicit sustainable behavioral change? Arch Surg. 2009;144(12):1133-7.
Fellowship is a time of great growth for pediatric hospital medicine fellows as clinicians, educators, scholars, and as leaders. Leadership is a crucial skill for hospitalists that is cultivated throughout fellowship. As fellows, we step into the role of clinical team leader for the first time and it is our responsibility to create a clinical and educational environment that is safe, inviting and engaging.
For possibly the first time in our careers, pediatric hospital medicine fellows are expected to make final decisions, big and small. We are faced with high-pressure situations almost daily, whether it is a rapid response on a patient, tough diagnostic and therapeutic decisions, difficult conversations with families, or dealing with challenging team members.
Soon after starting fellowship I was faced with a such a situation. The patient was a 6-month-old infant with trisomy 21 who was admitted because of feeding difficulties. They were working on oral feeds but required nasogastric (NG) feeds to meet caloric needs. On my first day on service, the residents indicated that the medical team desired the patient to have a gastrostomy tube (G-tube) placed. I was hoping to send the patient home for a few weeks with the NG tube to see if they were making progress on their oral feeds before deciding on the need for a G-tube. However, the patient’s parents pulled me aside in the hallway and said they were considering a third possibility.
The parents felt strongly about a trial period of a few weeks without the NG tube to see if the patient was able to maintain adequate weight gain with just oral feeds. The bedside nurse reiterated that the family felt their concerns had not been considered up until this point. As the fellow and team leader, it was my job to navigate between my resident team, myself, and the family in order to make a final decision. Through a bedside meeting and shared decision making, we were able to compromise and negotiate a decision, allowing the patient to go home on just oral feeds with close follow-up with their pediatrician. Afterwards, I found myself searching for strategies to be a better leader in these situations.
I found a potential answer in a recent article from the Harvard Business Review titled “What Aircraft Crews Know About Managing High-Pressure Situations.”1 The article discusses crew resource management (CRM), which was developed in the 1980s and is used in civil and military aviation worldwide. CRM is based on two principles to improve crisis management: The hierarchy on the flight deck must be flattened, and crew members must be actively integrated into the flight’s work flows and decision-making processes.
The authors of the article conducted two different studies to further understand CRM and its effects. The first study included observing 11 flight crews in emergency simulations. In the study, the flight crew had to react to an emergency, and then conduct a landing of the aircraft. What the authors found was that the captain’s style of communication had a major impact on crew performance in two major ways: Crews performed consistently better under times of pressure when the copilot was included in the decision-making process, and captains who asked open-ended questions (“How do you assess the situation”) came up with better solutions than captains who asked “yes or no” questions.
The authors conclude that “involving colleagues as equal decision partners by asking them questions…aids constructive, factual information exchange.” The second study consisted of conducting 61 interviews with flight crew members to better understand crisis management. In the interviews, the same theme occurred, that open-ended questions are vital in all decision-making processes and may be preventative against dangerous or imperfect outcomes. As fellows and team leaders we can learn from CRM and these studies. We need to flatten the hierarchy and ask open-ended questions.
To flatten the hierarchy, we should value the thoughts and opinions of all our team members. Now more than ever in this current COVID-19 pandemic with many hospitals instituting telehealth/telerounding for some or all team members, it is essential to utilize our entire “flight crew” (physicians, nurses, therapists, subspecialists, social worker, case managers, etc.) during routine decisions and high-stake decisions. We should make sure our flight crew, especially the bedside nurse is part of the decision-making process.2 This means we need to ensure they are present and given a voice on clinical rounds. To flatten the hierarchy, we must take pride in eliciting other team member’s opinions. We must realize that we alone do not have all the answers, and other team members may have different frameworks in which they process a decision.
Finally, in medicine, our patients and families are included in our flight crew. They too must have a voice in the decision-making process. Previous studies have shown that patients and families desire to be included in the decision-making process, and opportunities exist to improve shared decision-making in pediatrics.3-5 Lastly, we should commit to asking open-ended questions from our team and our patients. We should value their input and use their answers and frameworks to make the best decision for our patients.
I wasn’t aware at the time, but I was using some of the principles of CRM while navigating my high-pressure situation. A bedside meeting with all team members and the patient’s family helped to flatten the hierarchy by understanding and valuing each team member’s input. Asking open-ended questions of the different team members led to a more inviting and engaging clinical and learning environment. These strategies helped to lead our team into a clinical decision that wasn’t entirely clear at first but ended up being the best decision for the patient, as they are now thriving without ever requiring supplemental nutrition after discharge.
As physicians, we have learned a lot from the airline industry about wellness and the effect of fatigue on performance. It is clear now that we can also learn from them about clinical decision-making and leadership strategies. When adopted for health care, CRM principles have been shown to result in a culture of safety and long-term behavioral change.6,7 If we can model ourselves after the airline industry by following the principles of CRM, then we will be better clinicians, educators, and leaders.
Dr. Palmer is a second-year pediatric hospital medicine fellow at Children’s Hospital Los Angeles and is working toward a masters in academic medicine at the University of Southern California, Los Angeles, with a focus on curriculum development and educational scholarship production.
References
1. Hagan J et al. What Aircraft Crews Know About Managing High-Pressure Situations. Harvard Business Review. 2019 Dec. https://hbr.org/2019/12/what-aircraft-crews-know-about-managing-high-pressure-situations
2. Erickson J. Bedside nurse involvement in end-of-life decision-making: A brief review of the literature. Dimens Crit Care Nurs. 2013;32(2):65-8.
3. Richards CA et al. Physicians perceptions of shared decision-making in neonatal and pediatric critical care. Am J Hosp Palliat Care. 2018;35(4):669-76.
4. Boland L et al. Barriers and facilitators of pediatric shared decision-making: A systematic review. Implement Sci. 2019 Jan 18. doi: 10.1186/s13012-018-0851-5.
5. Blankenburg R et al. Shared decision-making during inpatient rounds: Opportunities for improvement in patient engagement and communication. J Hosp Med. 2018;13(7):453-61.
6. Kemper PF et al. Crew resource management training in the intensive care unit. A multisite controlled before-after study. BMJ Qual Saf. 2016;25(8):577-87.
7. Sax HC et al. Can aviation-based team training elicit sustainable behavioral change? Arch Surg. 2009;144(12):1133-7.
Should I be afraid of getting COVID again?
Is it over or do I have to brace myself for the possibility of a reinfection? Moreover, could the second time potentially be worse than the first?
I was diagnosed with COVID in March of this year. After spending 10 days in the hospital, and one night in the ICU, it took another 2 months for the air-hunger, headaches, and fatigue to completely resolve. Compared with many other unfortunate victims, I did all right – and I am very grateful for the care I received.
Now, as the surge in cases takes new life, I will be on the front lines taking care of patients. Having had an eventful personal encounter with the virus, I now have a unique vantage point and remain fully committed to paying my fortunate circumstances forward. Although I can’t help but have the same question faced by millions of others: Am I safe now?
It is no surprise that studies have shown health care workers comprising 6% of COVID hospital admissions, with one-third of these admissions being nurses. Recently, we heard that over 900 health care workers at Mayo Clinic had acquired the infection in the first 2 weeks of the ongoing second COVID surge. Are these frontline workers protected? Can they return to work with no fear of a rerun? Or, for that matter, anyone who has been afflicted by COVID – are they now forever immune?
There are no clear answers here. But to understand this a little, let’s quickly revisit some basic principles of immunity.
Innate and adaptive immunity
Simply put, there are two forms of immunity: innate and adaptive. Innate immunity encompasses our body’s natural protective mechanisms that come into play almost immediately. This enables recognition of the virus and activates an immediate antiviral defense and attempt at removal of the infective agent. This, however, does not always do the job. Accordingly, a couple weeks after the initial exposure to the pathogen, adaptive immunity is invoked. Circulating white blood cells within our body recognize the virus and set off an immune response, involving the activation of T and B cells that actively attack the infective agent. It is this T- and B-cell–mediated immunity that should protect one against a second infection with the same agent.
What about herd immunity?
Herd immunity is defined as essentially yielding to the virus and letting it spread naturally in order to develop community-wide immunity. By consequence of a large proportion of the population becoming immune after exposure to the disease, person-to-person spread can potentially be mitigated. This does not confer immunity to the virus at the individual level; rather, it reduces the risk of vulnerable people coming in contact with the pathogen.
Unfortunately, depending on herd immunity as a way to deal with COVID-19 has not worked well, even in well-contained countries like Sweden, where a disproportionate number of their most vulnerable populations have died. It is self-evident that containment strategies with vaccination may be our best way forward to achieve herd immunity. Not surrendering to the virus.
Am I safe from reinfection?
In all honesty, we’re not entirely sure. But it is important to recognize a few points when considering your relative safety.
- The immune system is far from perfect. Not everyone has a robust immune response. And in those who do, the immune response can wane over time, potentially allowing for reinfection. While rare, there have already been some clearly documented reinfections, four that have been confirmed and published; two patients (in Nevada and Ecuador) actually fared worse the second time around.
- The virus can mutate and escape detection by the immune system. One could still be susceptible to reinfection from a different strain. (At least, this remains the case with the influenza virus.) There is some evidence that SARS-CoV-2 does not mutate rapidly, and hence this may not be a problem. But we don’t know for certain, at least as of yet.
- Even a vigorous immune response can be overwhelmed by the virus. It is unclear whether the relative length of time and the amount of virus exposure could undermine a previously primed immune system.
A prior infection and a consequent healthy immunity may help you combat a reinfection but it does not prevent you from harboring or carrying the virus. You may be asymptomatic, but you can still be a carrier and spread the infection. I am a strong advocate for limiting your exposure to others no matter your previous exposure status, in order to limit the spread of the virus.
So, what should I do?
I guess the answer is that you can’t be too careful. Not everyone has had their antibody levels tested, and even if positive, it is unclear how well that affords protection. It is best to presume that you are vulnerable for a reinfection and that you can still carry and spread the virus. This may be the safest approach until we actually achieve herd immunity through vaccination.
Even then, for a period of time, there will remain a sense of uncertainty. So, containment strategies inclusive of distancing and masking will and should remain a way of life at least until mid-2021, when we will be in a better position to reassess the landscape.
The surge is back. As I repay my debt and get back to the front line, I will continue to mask up and practice distancing. I am taking no chances of getting reinfected or being an asymptomatic carrier.
I had COVID, I also have antibodies, and I will be taking the vaccine. I implore you all to do the same.
Jag Singh is a physician, scientist, and professor at Harvard. He is passionate about social issues, leadership, digital health, and medical innovations. You can follow him on Twitter @JagSinghMD.
A version of this article first appeared on Medscape.com.
Is it over or do I have to brace myself for the possibility of a reinfection? Moreover, could the second time potentially be worse than the first?
I was diagnosed with COVID in March of this year. After spending 10 days in the hospital, and one night in the ICU, it took another 2 months for the air-hunger, headaches, and fatigue to completely resolve. Compared with many other unfortunate victims, I did all right – and I am very grateful for the care I received.
Now, as the surge in cases takes new life, I will be on the front lines taking care of patients. Having had an eventful personal encounter with the virus, I now have a unique vantage point and remain fully committed to paying my fortunate circumstances forward. Although I can’t help but have the same question faced by millions of others: Am I safe now?
It is no surprise that studies have shown health care workers comprising 6% of COVID hospital admissions, with one-third of these admissions being nurses. Recently, we heard that over 900 health care workers at Mayo Clinic had acquired the infection in the first 2 weeks of the ongoing second COVID surge. Are these frontline workers protected? Can they return to work with no fear of a rerun? Or, for that matter, anyone who has been afflicted by COVID – are they now forever immune?
There are no clear answers here. But to understand this a little, let’s quickly revisit some basic principles of immunity.
Innate and adaptive immunity
Simply put, there are two forms of immunity: innate and adaptive. Innate immunity encompasses our body’s natural protective mechanisms that come into play almost immediately. This enables recognition of the virus and activates an immediate antiviral defense and attempt at removal of the infective agent. This, however, does not always do the job. Accordingly, a couple weeks after the initial exposure to the pathogen, adaptive immunity is invoked. Circulating white blood cells within our body recognize the virus and set off an immune response, involving the activation of T and B cells that actively attack the infective agent. It is this T- and B-cell–mediated immunity that should protect one against a second infection with the same agent.
What about herd immunity?
Herd immunity is defined as essentially yielding to the virus and letting it spread naturally in order to develop community-wide immunity. By consequence of a large proportion of the population becoming immune after exposure to the disease, person-to-person spread can potentially be mitigated. This does not confer immunity to the virus at the individual level; rather, it reduces the risk of vulnerable people coming in contact with the pathogen.
Unfortunately, depending on herd immunity as a way to deal with COVID-19 has not worked well, even in well-contained countries like Sweden, where a disproportionate number of their most vulnerable populations have died. It is self-evident that containment strategies with vaccination may be our best way forward to achieve herd immunity. Not surrendering to the virus.
Am I safe from reinfection?
In all honesty, we’re not entirely sure. But it is important to recognize a few points when considering your relative safety.
- The immune system is far from perfect. Not everyone has a robust immune response. And in those who do, the immune response can wane over time, potentially allowing for reinfection. While rare, there have already been some clearly documented reinfections, four that have been confirmed and published; two patients (in Nevada and Ecuador) actually fared worse the second time around.
- The virus can mutate and escape detection by the immune system. One could still be susceptible to reinfection from a different strain. (At least, this remains the case with the influenza virus.) There is some evidence that SARS-CoV-2 does not mutate rapidly, and hence this may not be a problem. But we don’t know for certain, at least as of yet.
- Even a vigorous immune response can be overwhelmed by the virus. It is unclear whether the relative length of time and the amount of virus exposure could undermine a previously primed immune system.
A prior infection and a consequent healthy immunity may help you combat a reinfection but it does not prevent you from harboring or carrying the virus. You may be asymptomatic, but you can still be a carrier and spread the infection. I am a strong advocate for limiting your exposure to others no matter your previous exposure status, in order to limit the spread of the virus.
So, what should I do?
I guess the answer is that you can’t be too careful. Not everyone has had their antibody levels tested, and even if positive, it is unclear how well that affords protection. It is best to presume that you are vulnerable for a reinfection and that you can still carry and spread the virus. This may be the safest approach until we actually achieve herd immunity through vaccination.
Even then, for a period of time, there will remain a sense of uncertainty. So, containment strategies inclusive of distancing and masking will and should remain a way of life at least until mid-2021, when we will be in a better position to reassess the landscape.
The surge is back. As I repay my debt and get back to the front line, I will continue to mask up and practice distancing. I am taking no chances of getting reinfected or being an asymptomatic carrier.
I had COVID, I also have antibodies, and I will be taking the vaccine. I implore you all to do the same.
Jag Singh is a physician, scientist, and professor at Harvard. He is passionate about social issues, leadership, digital health, and medical innovations. You can follow him on Twitter @JagSinghMD.
A version of this article first appeared on Medscape.com.
Is it over or do I have to brace myself for the possibility of a reinfection? Moreover, could the second time potentially be worse than the first?
I was diagnosed with COVID in March of this year. After spending 10 days in the hospital, and one night in the ICU, it took another 2 months for the air-hunger, headaches, and fatigue to completely resolve. Compared with many other unfortunate victims, I did all right – and I am very grateful for the care I received.
Now, as the surge in cases takes new life, I will be on the front lines taking care of patients. Having had an eventful personal encounter with the virus, I now have a unique vantage point and remain fully committed to paying my fortunate circumstances forward. Although I can’t help but have the same question faced by millions of others: Am I safe now?
It is no surprise that studies have shown health care workers comprising 6% of COVID hospital admissions, with one-third of these admissions being nurses. Recently, we heard that over 900 health care workers at Mayo Clinic had acquired the infection in the first 2 weeks of the ongoing second COVID surge. Are these frontline workers protected? Can they return to work with no fear of a rerun? Or, for that matter, anyone who has been afflicted by COVID – are they now forever immune?
There are no clear answers here. But to understand this a little, let’s quickly revisit some basic principles of immunity.
Innate and adaptive immunity
Simply put, there are two forms of immunity: innate and adaptive. Innate immunity encompasses our body’s natural protective mechanisms that come into play almost immediately. This enables recognition of the virus and activates an immediate antiviral defense and attempt at removal of the infective agent. This, however, does not always do the job. Accordingly, a couple weeks after the initial exposure to the pathogen, adaptive immunity is invoked. Circulating white blood cells within our body recognize the virus and set off an immune response, involving the activation of T and B cells that actively attack the infective agent. It is this T- and B-cell–mediated immunity that should protect one against a second infection with the same agent.
What about herd immunity?
Herd immunity is defined as essentially yielding to the virus and letting it spread naturally in order to develop community-wide immunity. By consequence of a large proportion of the population becoming immune after exposure to the disease, person-to-person spread can potentially be mitigated. This does not confer immunity to the virus at the individual level; rather, it reduces the risk of vulnerable people coming in contact with the pathogen.
Unfortunately, depending on herd immunity as a way to deal with COVID-19 has not worked well, even in well-contained countries like Sweden, where a disproportionate number of their most vulnerable populations have died. It is self-evident that containment strategies with vaccination may be our best way forward to achieve herd immunity. Not surrendering to the virus.
Am I safe from reinfection?
In all honesty, we’re not entirely sure. But it is important to recognize a few points when considering your relative safety.
- The immune system is far from perfect. Not everyone has a robust immune response. And in those who do, the immune response can wane over time, potentially allowing for reinfection. While rare, there have already been some clearly documented reinfections, four that have been confirmed and published; two patients (in Nevada and Ecuador) actually fared worse the second time around.
- The virus can mutate and escape detection by the immune system. One could still be susceptible to reinfection from a different strain. (At least, this remains the case with the influenza virus.) There is some evidence that SARS-CoV-2 does not mutate rapidly, and hence this may not be a problem. But we don’t know for certain, at least as of yet.
- Even a vigorous immune response can be overwhelmed by the virus. It is unclear whether the relative length of time and the amount of virus exposure could undermine a previously primed immune system.
A prior infection and a consequent healthy immunity may help you combat a reinfection but it does not prevent you from harboring or carrying the virus. You may be asymptomatic, but you can still be a carrier and spread the infection. I am a strong advocate for limiting your exposure to others no matter your previous exposure status, in order to limit the spread of the virus.
So, what should I do?
I guess the answer is that you can’t be too careful. Not everyone has had their antibody levels tested, and even if positive, it is unclear how well that affords protection. It is best to presume that you are vulnerable for a reinfection and that you can still carry and spread the virus. This may be the safest approach until we actually achieve herd immunity through vaccination.
Even then, for a period of time, there will remain a sense of uncertainty. So, containment strategies inclusive of distancing and masking will and should remain a way of life at least until mid-2021, when we will be in a better position to reassess the landscape.
The surge is back. As I repay my debt and get back to the front line, I will continue to mask up and practice distancing. I am taking no chances of getting reinfected or being an asymptomatic carrier.
I had COVID, I also have antibodies, and I will be taking the vaccine. I implore you all to do the same.
Jag Singh is a physician, scientist, and professor at Harvard. He is passionate about social issues, leadership, digital health, and medical innovations. You can follow him on Twitter @JagSinghMD.
A version of this article first appeared on Medscape.com.
13 best practices to increase hospitalist billing efficiency
As an aspiring physician, I like learning about how things work. Since medical students learn very little about the “business” of medicine in school, this led me to pioneer a project on missed billing by hospitalists at a medium-sized hospital in the northeastern US. Although hospitalists do a tremendous amount of work, they do not always bill for what they are doing. The question became: Why are hospitalists missing charges and what can we do to stop it?
Shortly into my study, I recognized there was little daily communication between the administrators and the hospitalists; neither the hospitalists nor administrators understood the different dynamics that the others faced in their own workplace. It became apparent that administrators needed to learn what was important to hospitalists and to address them at their level in order to bring about change.
Some trending themes emerged as I started shadowing the hospitalists. Many of them asked how this project would benefit them. They argued that administrative needs should be dealt with at the administrative level. A major point was made that current incentives, such as the bonuses given for exceeding a certain number of RVUs, were not the motivating force behind their work ethics. From my observations, the motivating factors were the quality of their patient care, the needs of their patients, and teaching. The hospitalists also were eager to teach and continually instructed me on clinical skills and how to be a better medical student.
Bonuses or notoriety didn’t seem to be the main incentives for them. However, efficiency – especially in rounding – was important, and that became the focal point of the project. I found several studies that showed that improvements in aspects of rounding led to increased quality of patient care, decreased burnout, increased patient satisfaction, and decreased workload and discussed some of those findings with the hospitalists.1-10 When the hospitalists felt that their concerns were being heard, they became even more involved in the project, and the administrators and hospitalists started working together as a team.
One hospitalist spent two hours helping me design the platform that would be used for hospitalists to report barriers in their rounding process that may cause them to miss a charge. Once we identified those barriers, we discussed the possibility of standardizing their workflow based off these data. Many hospitalists argued that each physician has unique skills and practices that make them successful; therefore, the disruption of an already established workflow may cause a decrease in efficiency.
The hospitalists and I talked a lot about the importance of them rounding more efficiently and how that could positively affect the time that they have with their patients and themselves. We discussed that due to the additional work missed billing causes, minimizing this burden can possibly help decrease burnout. As a result, seven hospitalists, the administrative staff, and I met and created thirteen best practices, six of which they were able to get approved to use immediately. To note, hospitalists bill differently; some use a software company, fill out paper forms still or have integration within their EMR. Although these solutions were made for a program which has the ability to bill within the EMR, many of the principles will apply to your program too.
The 13 best practices that the seven hospitalists agreed upon are the following:
When a doctor signs a note, it opens a charge option or there is a hard stop.
Charge delinquencies are sent via email to the hospitalist.
Standardize that hospitalists charge directly after writing a note consistently as part of their workflow.*
Prioritize discharges before rounding.*
Standardize the use of the “my prof charges” column, a feature of this hospital’s EMR system that tells them if they had made a charge to a patient or not, in order to remind them to/confirm billing a patient.*
Create reports by the EMR system to provide charge data for individual providers.
Create a report for bill vs note to help providers self-audit. At this hospital, this feature was offered to the administrators as a way to audit their providers and doctors.
Ensure that when a patient is seen by a physician hospitalist as well as an NP/PA hospitalist, the appropriate charge for the physician is entered.
Notifications get sent to the physician hospitalist if a charge gets deleted by another person (e.g., NP/PA hospitalist).
Handoff of daily rounding sheets, or a paper copy of the patients assigned to a hospitalist for his/her shift, at the end of the shift to the project specialist.*
To keep the rounding sheets a complete and accurate account of the patients seen by the hospitalist.*
Hospitalists are to complete and check all billing at the end of their shift at the latest.*
Hospitalists are to participate on Provider Efficiency Training to optimize workflow, by creating more efficient note-writing behavior using Dragon.
*Indicates the practices the hospitalists were able to implement immediately. Practices 1, 2, 6, 7, and 9 request EMR changes. Practice 8 was already an established practice the hospitalists wished to continue. Practice 13 was suggested by the Lean Director for the continuation of a previous project.
Six of the best practices were easier to implement right away because they were at the discretion of the hospitalists. We found that the hospitalists who had the highest billing performances were more likely to start writing notes and charge earlier while rounding. Those who had poorer billing performances were more likely to leave all note writing and billing towards the end of their shift. The few exceptions (hospitalists who left all note writing and charging to the end of their shift yet had high billing performances) were found to have a consistent and standardized workflow. This was unlike the hospitalists who had the lowest billing performances. Having practices that help remind hospitalists to bill will surely help prevent missed billing, but because of the findings from this project, it was important to have consistent and standardized practices to additionally improve missed billing.
When we followed up with the hospitalist division two months later, we learned they were making great progress. Not only were hospitalists using their best practices, but in working with the administrators, they were designing sessions to further educate fellow hospitalists to prevent further missed billing. These sessions outlined shortcuts, resources and ways hospitalists may modify their personal EMR accounts to prevent missed billing. None of the progress could have been made without first understanding and addressing what is truly important to the hospitalists.
In summary, we noted these general observations in this project:
- Hospitalists favor solutions that benefit them or their patients.
- Hospitalists want to be part of the solution process.
- Hospitalists were more likely to accept ideas to improve their rounding if it meant they could keep their routine.
Obstacles exist in our health care system that prevent administrators and hospitalists from working together as a team. The more we are able to communicate and collaborate to fix problems in the health system, the more we can use the system to our mutual advantage. With the ongoing changes in medicine, especially during uncertain times, better communication needs be a major priority to affect positive change.
Ms. Mirabella attends the Frank H. Netter MD School of Medicine at Quinnipiac University, Hamden, Conn., in the class of 2022. She has interests in internal/hospital medicine, primary care, and health management and leadership. Dr. Rosenberg is associate professor at the Frank H. Netter MD School of Medicine at Quinnipiac University where she is director of clinical skills coaching. Dr. Kiassat is associate dean of the School of Engineering and associate clinical professor at Frank H. Netter MD School of Medicine, at Quinnipiac University. His research interests are in process improvement in health care, using Lean Six Sigma.
References
1. Burdick K, et al. Bedside interprofessional rounding. J Patient Exp. 2017;4(1):22-27. doi: 10.1177/2374373517692910.
2. Patel CR. Improving communication between hospitalists and consultants. The Hospital Leader. 2018. https://thehospitalleader.org/improving-communication-between-hospitalists-and-consultants/.
3. Adams TN, et al. Hospitalist perspective of interactions with medicine subspecialty consult services. J Hosp Med. 2018;13(5):318-323. doi: 10.12788/jhm.2882.
4. Michtalik HJ, et al. Impact of attending physician workload on patient care: A survey of hospitalists. JAMA Intern Med. 2013;173(5):375-377. doi: 10.1001/jamainternmed.2013.1864.
5. Chandra R, et al. How hospitalists can improve efficiency on inpatient wards. The Hospitalist. 2014. https://www.the-hospitalist.org/hospitalist/article/126231/how-hospitalists-can-improve-efficiency-inpatient-wards.
6. Chand DV. Observational study using the tools of lean six sigma to improve the efficiency of the resident rounding process. J Grad Med Educ. 2011;3(2):144-150. doi: 10.4300/JGME-D-10-00116.1.
7. O’Leary KJ, et al. How hospitalists spend their time: Insights on efficiency and safety. J Hosp Med. 2006;1(2):88-93. doi: 10.1002/jhm.88.
8. Wachter RM. Hospitalist workload: The search for the magic number. JAMA Intern Med. 2014;174(5):794-795. doi: 10.1001/jamainternmed.2014.18.
9. Bryson C, et al. Geographical assignment of hospitalists in an urban teaching hospital: Feasibility and impact on efficiency and provider satisfaction. Hospital Practice. 2017;45(4):135-142. doi: 10.1080/21548331.2017.1353884.
10. Calderon AS, et al. Transforming ward rounds through rounding-in-flow. J Grad Med Educ. 2014 Dec;6(4):750-5. doi: 10.4300/JGME-D-13-00324.1.
As an aspiring physician, I like learning about how things work. Since medical students learn very little about the “business” of medicine in school, this led me to pioneer a project on missed billing by hospitalists at a medium-sized hospital in the northeastern US. Although hospitalists do a tremendous amount of work, they do not always bill for what they are doing. The question became: Why are hospitalists missing charges and what can we do to stop it?
Shortly into my study, I recognized there was little daily communication between the administrators and the hospitalists; neither the hospitalists nor administrators understood the different dynamics that the others faced in their own workplace. It became apparent that administrators needed to learn what was important to hospitalists and to address them at their level in order to bring about change.
Some trending themes emerged as I started shadowing the hospitalists. Many of them asked how this project would benefit them. They argued that administrative needs should be dealt with at the administrative level. A major point was made that current incentives, such as the bonuses given for exceeding a certain number of RVUs, were not the motivating force behind their work ethics. From my observations, the motivating factors were the quality of their patient care, the needs of their patients, and teaching. The hospitalists also were eager to teach and continually instructed me on clinical skills and how to be a better medical student.
Bonuses or notoriety didn’t seem to be the main incentives for them. However, efficiency – especially in rounding – was important, and that became the focal point of the project. I found several studies that showed that improvements in aspects of rounding led to increased quality of patient care, decreased burnout, increased patient satisfaction, and decreased workload and discussed some of those findings with the hospitalists.1-10 When the hospitalists felt that their concerns were being heard, they became even more involved in the project, and the administrators and hospitalists started working together as a team.
One hospitalist spent two hours helping me design the platform that would be used for hospitalists to report barriers in their rounding process that may cause them to miss a charge. Once we identified those barriers, we discussed the possibility of standardizing their workflow based off these data. Many hospitalists argued that each physician has unique skills and practices that make them successful; therefore, the disruption of an already established workflow may cause a decrease in efficiency.
The hospitalists and I talked a lot about the importance of them rounding more efficiently and how that could positively affect the time that they have with their patients and themselves. We discussed that due to the additional work missed billing causes, minimizing this burden can possibly help decrease burnout. As a result, seven hospitalists, the administrative staff, and I met and created thirteen best practices, six of which they were able to get approved to use immediately. To note, hospitalists bill differently; some use a software company, fill out paper forms still or have integration within their EMR. Although these solutions were made for a program which has the ability to bill within the EMR, many of the principles will apply to your program too.
The 13 best practices that the seven hospitalists agreed upon are the following:
When a doctor signs a note, it opens a charge option or there is a hard stop.
Charge delinquencies are sent via email to the hospitalist.
Standardize that hospitalists charge directly after writing a note consistently as part of their workflow.*
Prioritize discharges before rounding.*
Standardize the use of the “my prof charges” column, a feature of this hospital’s EMR system that tells them if they had made a charge to a patient or not, in order to remind them to/confirm billing a patient.*
Create reports by the EMR system to provide charge data for individual providers.
Create a report for bill vs note to help providers self-audit. At this hospital, this feature was offered to the administrators as a way to audit their providers and doctors.
Ensure that when a patient is seen by a physician hospitalist as well as an NP/PA hospitalist, the appropriate charge for the physician is entered.
Notifications get sent to the physician hospitalist if a charge gets deleted by another person (e.g., NP/PA hospitalist).
Handoff of daily rounding sheets, or a paper copy of the patients assigned to a hospitalist for his/her shift, at the end of the shift to the project specialist.*
To keep the rounding sheets a complete and accurate account of the patients seen by the hospitalist.*
Hospitalists are to complete and check all billing at the end of their shift at the latest.*
Hospitalists are to participate on Provider Efficiency Training to optimize workflow, by creating more efficient note-writing behavior using Dragon.
*Indicates the practices the hospitalists were able to implement immediately. Practices 1, 2, 6, 7, and 9 request EMR changes. Practice 8 was already an established practice the hospitalists wished to continue. Practice 13 was suggested by the Lean Director for the continuation of a previous project.
Six of the best practices were easier to implement right away because they were at the discretion of the hospitalists. We found that the hospitalists who had the highest billing performances were more likely to start writing notes and charge earlier while rounding. Those who had poorer billing performances were more likely to leave all note writing and billing towards the end of their shift. The few exceptions (hospitalists who left all note writing and charging to the end of their shift yet had high billing performances) were found to have a consistent and standardized workflow. This was unlike the hospitalists who had the lowest billing performances. Having practices that help remind hospitalists to bill will surely help prevent missed billing, but because of the findings from this project, it was important to have consistent and standardized practices to additionally improve missed billing.
When we followed up with the hospitalist division two months later, we learned they were making great progress. Not only were hospitalists using their best practices, but in working with the administrators, they were designing sessions to further educate fellow hospitalists to prevent further missed billing. These sessions outlined shortcuts, resources and ways hospitalists may modify their personal EMR accounts to prevent missed billing. None of the progress could have been made without first understanding and addressing what is truly important to the hospitalists.
In summary, we noted these general observations in this project:
- Hospitalists favor solutions that benefit them or their patients.
- Hospitalists want to be part of the solution process.
- Hospitalists were more likely to accept ideas to improve their rounding if it meant they could keep their routine.
Obstacles exist in our health care system that prevent administrators and hospitalists from working together as a team. The more we are able to communicate and collaborate to fix problems in the health system, the more we can use the system to our mutual advantage. With the ongoing changes in medicine, especially during uncertain times, better communication needs be a major priority to affect positive change.
Ms. Mirabella attends the Frank H. Netter MD School of Medicine at Quinnipiac University, Hamden, Conn., in the class of 2022. She has interests in internal/hospital medicine, primary care, and health management and leadership. Dr. Rosenberg is associate professor at the Frank H. Netter MD School of Medicine at Quinnipiac University where she is director of clinical skills coaching. Dr. Kiassat is associate dean of the School of Engineering and associate clinical professor at Frank H. Netter MD School of Medicine, at Quinnipiac University. His research interests are in process improvement in health care, using Lean Six Sigma.
References
1. Burdick K, et al. Bedside interprofessional rounding. J Patient Exp. 2017;4(1):22-27. doi: 10.1177/2374373517692910.
2. Patel CR. Improving communication between hospitalists and consultants. The Hospital Leader. 2018. https://thehospitalleader.org/improving-communication-between-hospitalists-and-consultants/.
3. Adams TN, et al. Hospitalist perspective of interactions with medicine subspecialty consult services. J Hosp Med. 2018;13(5):318-323. doi: 10.12788/jhm.2882.
4. Michtalik HJ, et al. Impact of attending physician workload on patient care: A survey of hospitalists. JAMA Intern Med. 2013;173(5):375-377. doi: 10.1001/jamainternmed.2013.1864.
5. Chandra R, et al. How hospitalists can improve efficiency on inpatient wards. The Hospitalist. 2014. https://www.the-hospitalist.org/hospitalist/article/126231/how-hospitalists-can-improve-efficiency-inpatient-wards.
6. Chand DV. Observational study using the tools of lean six sigma to improve the efficiency of the resident rounding process. J Grad Med Educ. 2011;3(2):144-150. doi: 10.4300/JGME-D-10-00116.1.
7. O’Leary KJ, et al. How hospitalists spend their time: Insights on efficiency and safety. J Hosp Med. 2006;1(2):88-93. doi: 10.1002/jhm.88.
8. Wachter RM. Hospitalist workload: The search for the magic number. JAMA Intern Med. 2014;174(5):794-795. doi: 10.1001/jamainternmed.2014.18.
9. Bryson C, et al. Geographical assignment of hospitalists in an urban teaching hospital: Feasibility and impact on efficiency and provider satisfaction. Hospital Practice. 2017;45(4):135-142. doi: 10.1080/21548331.2017.1353884.
10. Calderon AS, et al. Transforming ward rounds through rounding-in-flow. J Grad Med Educ. 2014 Dec;6(4):750-5. doi: 10.4300/JGME-D-13-00324.1.
As an aspiring physician, I like learning about how things work. Since medical students learn very little about the “business” of medicine in school, this led me to pioneer a project on missed billing by hospitalists at a medium-sized hospital in the northeastern US. Although hospitalists do a tremendous amount of work, they do not always bill for what they are doing. The question became: Why are hospitalists missing charges and what can we do to stop it?
Shortly into my study, I recognized there was little daily communication between the administrators and the hospitalists; neither the hospitalists nor administrators understood the different dynamics that the others faced in their own workplace. It became apparent that administrators needed to learn what was important to hospitalists and to address them at their level in order to bring about change.
Some trending themes emerged as I started shadowing the hospitalists. Many of them asked how this project would benefit them. They argued that administrative needs should be dealt with at the administrative level. A major point was made that current incentives, such as the bonuses given for exceeding a certain number of RVUs, were not the motivating force behind their work ethics. From my observations, the motivating factors were the quality of their patient care, the needs of their patients, and teaching. The hospitalists also were eager to teach and continually instructed me on clinical skills and how to be a better medical student.
Bonuses or notoriety didn’t seem to be the main incentives for them. However, efficiency – especially in rounding – was important, and that became the focal point of the project. I found several studies that showed that improvements in aspects of rounding led to increased quality of patient care, decreased burnout, increased patient satisfaction, and decreased workload and discussed some of those findings with the hospitalists.1-10 When the hospitalists felt that their concerns were being heard, they became even more involved in the project, and the administrators and hospitalists started working together as a team.
One hospitalist spent two hours helping me design the platform that would be used for hospitalists to report barriers in their rounding process that may cause them to miss a charge. Once we identified those barriers, we discussed the possibility of standardizing their workflow based off these data. Many hospitalists argued that each physician has unique skills and practices that make them successful; therefore, the disruption of an already established workflow may cause a decrease in efficiency.
The hospitalists and I talked a lot about the importance of them rounding more efficiently and how that could positively affect the time that they have with their patients and themselves. We discussed that due to the additional work missed billing causes, minimizing this burden can possibly help decrease burnout. As a result, seven hospitalists, the administrative staff, and I met and created thirteen best practices, six of which they were able to get approved to use immediately. To note, hospitalists bill differently; some use a software company, fill out paper forms still or have integration within their EMR. Although these solutions were made for a program which has the ability to bill within the EMR, many of the principles will apply to your program too.
The 13 best practices that the seven hospitalists agreed upon are the following:
When a doctor signs a note, it opens a charge option or there is a hard stop.
Charge delinquencies are sent via email to the hospitalist.
Standardize that hospitalists charge directly after writing a note consistently as part of their workflow.*
Prioritize discharges before rounding.*
Standardize the use of the “my prof charges” column, a feature of this hospital’s EMR system that tells them if they had made a charge to a patient or not, in order to remind them to/confirm billing a patient.*
Create reports by the EMR system to provide charge data for individual providers.
Create a report for bill vs note to help providers self-audit. At this hospital, this feature was offered to the administrators as a way to audit their providers and doctors.
Ensure that when a patient is seen by a physician hospitalist as well as an NP/PA hospitalist, the appropriate charge for the physician is entered.
Notifications get sent to the physician hospitalist if a charge gets deleted by another person (e.g., NP/PA hospitalist).
Handoff of daily rounding sheets, or a paper copy of the patients assigned to a hospitalist for his/her shift, at the end of the shift to the project specialist.*
To keep the rounding sheets a complete and accurate account of the patients seen by the hospitalist.*
Hospitalists are to complete and check all billing at the end of their shift at the latest.*
Hospitalists are to participate on Provider Efficiency Training to optimize workflow, by creating more efficient note-writing behavior using Dragon.
*Indicates the practices the hospitalists were able to implement immediately. Practices 1, 2, 6, 7, and 9 request EMR changes. Practice 8 was already an established practice the hospitalists wished to continue. Practice 13 was suggested by the Lean Director for the continuation of a previous project.
Six of the best practices were easier to implement right away because they were at the discretion of the hospitalists. We found that the hospitalists who had the highest billing performances were more likely to start writing notes and charge earlier while rounding. Those who had poorer billing performances were more likely to leave all note writing and billing towards the end of their shift. The few exceptions (hospitalists who left all note writing and charging to the end of their shift yet had high billing performances) were found to have a consistent and standardized workflow. This was unlike the hospitalists who had the lowest billing performances. Having practices that help remind hospitalists to bill will surely help prevent missed billing, but because of the findings from this project, it was important to have consistent and standardized practices to additionally improve missed billing.
When we followed up with the hospitalist division two months later, we learned they were making great progress. Not only were hospitalists using their best practices, but in working with the administrators, they were designing sessions to further educate fellow hospitalists to prevent further missed billing. These sessions outlined shortcuts, resources and ways hospitalists may modify their personal EMR accounts to prevent missed billing. None of the progress could have been made without first understanding and addressing what is truly important to the hospitalists.
In summary, we noted these general observations in this project:
- Hospitalists favor solutions that benefit them or their patients.
- Hospitalists want to be part of the solution process.
- Hospitalists were more likely to accept ideas to improve their rounding if it meant they could keep their routine.
Obstacles exist in our health care system that prevent administrators and hospitalists from working together as a team. The more we are able to communicate and collaborate to fix problems in the health system, the more we can use the system to our mutual advantage. With the ongoing changes in medicine, especially during uncertain times, better communication needs be a major priority to affect positive change.
Ms. Mirabella attends the Frank H. Netter MD School of Medicine at Quinnipiac University, Hamden, Conn., in the class of 2022. She has interests in internal/hospital medicine, primary care, and health management and leadership. Dr. Rosenberg is associate professor at the Frank H. Netter MD School of Medicine at Quinnipiac University where she is director of clinical skills coaching. Dr. Kiassat is associate dean of the School of Engineering and associate clinical professor at Frank H. Netter MD School of Medicine, at Quinnipiac University. His research interests are in process improvement in health care, using Lean Six Sigma.
References
1. Burdick K, et al. Bedside interprofessional rounding. J Patient Exp. 2017;4(1):22-27. doi: 10.1177/2374373517692910.
2. Patel CR. Improving communication between hospitalists and consultants. The Hospital Leader. 2018. https://thehospitalleader.org/improving-communication-between-hospitalists-and-consultants/.
3. Adams TN, et al. Hospitalist perspective of interactions with medicine subspecialty consult services. J Hosp Med. 2018;13(5):318-323. doi: 10.12788/jhm.2882.
4. Michtalik HJ, et al. Impact of attending physician workload on patient care: A survey of hospitalists. JAMA Intern Med. 2013;173(5):375-377. doi: 10.1001/jamainternmed.2013.1864.
5. Chandra R, et al. How hospitalists can improve efficiency on inpatient wards. The Hospitalist. 2014. https://www.the-hospitalist.org/hospitalist/article/126231/how-hospitalists-can-improve-efficiency-inpatient-wards.
6. Chand DV. Observational study using the tools of lean six sigma to improve the efficiency of the resident rounding process. J Grad Med Educ. 2011;3(2):144-150. doi: 10.4300/JGME-D-10-00116.1.
7. O’Leary KJ, et al. How hospitalists spend their time: Insights on efficiency and safety. J Hosp Med. 2006;1(2):88-93. doi: 10.1002/jhm.88.
8. Wachter RM. Hospitalist workload: The search for the magic number. JAMA Intern Med. 2014;174(5):794-795. doi: 10.1001/jamainternmed.2014.18.
9. Bryson C, et al. Geographical assignment of hospitalists in an urban teaching hospital: Feasibility and impact on efficiency and provider satisfaction. Hospital Practice. 2017;45(4):135-142. doi: 10.1080/21548331.2017.1353884.
10. Calderon AS, et al. Transforming ward rounds through rounding-in-flow. J Grad Med Educ. 2014 Dec;6(4):750-5. doi: 10.4300/JGME-D-13-00324.1.
Distinguishing between joy and pleasure during the pandemic
You can now buy vegan eggnog, made from almond milk. The fact that someone created this wasn’t a surprise – plant milks are taking over. That it gave me such pleasure was. It’s rich, and if you love eggnog, like all normal people, it’s amazingly satisfying when mixed in a Nespresso latte swirled creamy white and brown. It seems some things, like Netflix’s The Crown, my Peloton spin classes, long Sunday walks on the beach, and the best mushroom risotto I ever made were still pleasurable this year, despite all. I’d daresay, there was joy even in the time of COVID.
.
Pleasure is pretty constant. It pops up even in the worst times. It seems, there’s plenty to be found even now. Unless, perhaps it’s just me. The label my mother pinned on me as a boy has remained into adulthood: “Easy to please.” There’s hardly a movie I’ve seen that I didn’t like. I’m quite comfortable in the middle seat. I thought the EPIC updates this year were nice. I’ve liked the vast majority of pizzas I’ve ever eaten – even those contaminated with Truffle salt. Easy to please is a gift, not something I’ve acquired through hours of meditation or aesthetic fasts. But surely pleasure isn’t the same as joy. No one has tears of pleasure. (Not to mention, pleasure as a verb has obvious NSFW connotations; not true of joy).
No, joy is waaay bigger. Joy is shared. Joy is to the whole world. Joy is what happens when you have a baby. Pleasure is what happens when you remembered to put a burp cloth in the car. Pleasure is when three patients in a row take merely 5 minutes each. Joy is when an itchy patient is cured.
2020 was one of the most miserable years in the last century. We didn’t expect it, but we ought to have. I mean really, how many plagues have we endured? How many times has inequality led to social unrest? Many times. We, by luck and dint of hard work, have always managed to get through. Although suffering would surely have been greater during those times of sickness and loss, I don’t believe joy would have been less. Indeed, maybe it is those difficulties and that suffering that allows us to feel joy in the first place. It is only once you summit that you experience joy. The run-up is just pain.
It is no coincidence that it is now during this cold, dark, difficult part of the year that we wish joy. We’ve made it. We light the darkness with candles to joyously celebrate Mawlid, Diwali, then Hanukkah and Christmas. Had malls been open now, you’d hear amongst the din of ringing bells Rejoice! Rejoice! O Emmanuel! You’d sing along, “Joy to the world, now we sing, let the Angel voices ring.” Joy: A pleasure so great and so deserved, it is shared by all. It is good news, hope, gratitude.
A joy shared amongst us all is also coming. Through the wrenching pain of watching patients suffocate, fogged shields, and bleached masks, through canceled Thanksgivings, through weekends spent in the OR on the backlog of patients, after months spent sitting in empty clinics, though the long, orange-cone-winding lines of testing, at last, at last a vaccine is here to light the darkness.
Let the sea resound, and everything in it,
Let the rivers clap their hands,
let the mountains sing together for joy.
Joy to the world.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
You can now buy vegan eggnog, made from almond milk. The fact that someone created this wasn’t a surprise – plant milks are taking over. That it gave me such pleasure was. It’s rich, and if you love eggnog, like all normal people, it’s amazingly satisfying when mixed in a Nespresso latte swirled creamy white and brown. It seems some things, like Netflix’s The Crown, my Peloton spin classes, long Sunday walks on the beach, and the best mushroom risotto I ever made were still pleasurable this year, despite all. I’d daresay, there was joy even in the time of COVID.
.
Pleasure is pretty constant. It pops up even in the worst times. It seems, there’s plenty to be found even now. Unless, perhaps it’s just me. The label my mother pinned on me as a boy has remained into adulthood: “Easy to please.” There’s hardly a movie I’ve seen that I didn’t like. I’m quite comfortable in the middle seat. I thought the EPIC updates this year were nice. I’ve liked the vast majority of pizzas I’ve ever eaten – even those contaminated with Truffle salt. Easy to please is a gift, not something I’ve acquired through hours of meditation or aesthetic fasts. But surely pleasure isn’t the same as joy. No one has tears of pleasure. (Not to mention, pleasure as a verb has obvious NSFW connotations; not true of joy).
No, joy is waaay bigger. Joy is shared. Joy is to the whole world. Joy is what happens when you have a baby. Pleasure is what happens when you remembered to put a burp cloth in the car. Pleasure is when three patients in a row take merely 5 minutes each. Joy is when an itchy patient is cured.
2020 was one of the most miserable years in the last century. We didn’t expect it, but we ought to have. I mean really, how many plagues have we endured? How many times has inequality led to social unrest? Many times. We, by luck and dint of hard work, have always managed to get through. Although suffering would surely have been greater during those times of sickness and loss, I don’t believe joy would have been less. Indeed, maybe it is those difficulties and that suffering that allows us to feel joy in the first place. It is only once you summit that you experience joy. The run-up is just pain.
It is no coincidence that it is now during this cold, dark, difficult part of the year that we wish joy. We’ve made it. We light the darkness with candles to joyously celebrate Mawlid, Diwali, then Hanukkah and Christmas. Had malls been open now, you’d hear amongst the din of ringing bells Rejoice! Rejoice! O Emmanuel! You’d sing along, “Joy to the world, now we sing, let the Angel voices ring.” Joy: A pleasure so great and so deserved, it is shared by all. It is good news, hope, gratitude.
A joy shared amongst us all is also coming. Through the wrenching pain of watching patients suffocate, fogged shields, and bleached masks, through canceled Thanksgivings, through weekends spent in the OR on the backlog of patients, after months spent sitting in empty clinics, though the long, orange-cone-winding lines of testing, at last, at last a vaccine is here to light the darkness.
Let the sea resound, and everything in it,
Let the rivers clap their hands,
let the mountains sing together for joy.
Joy to the world.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
You can now buy vegan eggnog, made from almond milk. The fact that someone created this wasn’t a surprise – plant milks are taking over. That it gave me such pleasure was. It’s rich, and if you love eggnog, like all normal people, it’s amazingly satisfying when mixed in a Nespresso latte swirled creamy white and brown. It seems some things, like Netflix’s The Crown, my Peloton spin classes, long Sunday walks on the beach, and the best mushroom risotto I ever made were still pleasurable this year, despite all. I’d daresay, there was joy even in the time of COVID.
.
Pleasure is pretty constant. It pops up even in the worst times. It seems, there’s plenty to be found even now. Unless, perhaps it’s just me. The label my mother pinned on me as a boy has remained into adulthood: “Easy to please.” There’s hardly a movie I’ve seen that I didn’t like. I’m quite comfortable in the middle seat. I thought the EPIC updates this year were nice. I’ve liked the vast majority of pizzas I’ve ever eaten – even those contaminated with Truffle salt. Easy to please is a gift, not something I’ve acquired through hours of meditation or aesthetic fasts. But surely pleasure isn’t the same as joy. No one has tears of pleasure. (Not to mention, pleasure as a verb has obvious NSFW connotations; not true of joy).
No, joy is waaay bigger. Joy is shared. Joy is to the whole world. Joy is what happens when you have a baby. Pleasure is what happens when you remembered to put a burp cloth in the car. Pleasure is when three patients in a row take merely 5 minutes each. Joy is when an itchy patient is cured.
2020 was one of the most miserable years in the last century. We didn’t expect it, but we ought to have. I mean really, how many plagues have we endured? How many times has inequality led to social unrest? Many times. We, by luck and dint of hard work, have always managed to get through. Although suffering would surely have been greater during those times of sickness and loss, I don’t believe joy would have been less. Indeed, maybe it is those difficulties and that suffering that allows us to feel joy in the first place. It is only once you summit that you experience joy. The run-up is just pain.
It is no coincidence that it is now during this cold, dark, difficult part of the year that we wish joy. We’ve made it. We light the darkness with candles to joyously celebrate Mawlid, Diwali, then Hanukkah and Christmas. Had malls been open now, you’d hear amongst the din of ringing bells Rejoice! Rejoice! O Emmanuel! You’d sing along, “Joy to the world, now we sing, let the Angel voices ring.” Joy: A pleasure so great and so deserved, it is shared by all. It is good news, hope, gratitude.
A joy shared amongst us all is also coming. Through the wrenching pain of watching patients suffocate, fogged shields, and bleached masks, through canceled Thanksgivings, through weekends spent in the OR on the backlog of patients, after months spent sitting in empty clinics, though the long, orange-cone-winding lines of testing, at last, at last a vaccine is here to light the darkness.
Let the sea resound, and everything in it,
Let the rivers clap their hands,
let the mountains sing together for joy.
Joy to the world.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Can patients record office visits?
Recently I posted a simple question on several social media pages and internet blogs populated exclusively by board-certified dermatologists and dermatologic surgeons: How would you respond to a patient asking (or demanding) to record all or part of their office visit? (Or, if you have encountered such a situation, how did you respond?)
The question was simple, but the answers were somewhat complicated.
First, I noticed a fundamental misunderstanding of applicable laws: Many practitioners apparently believe that taping or recording a private conversation is per se illegal. Perhaps they are conflating with wiretapping laws, which don’t apply in this situation. HIPAA laws don’t apply either, because the patient, by definition, is waiving the right to privacy by initiating the recording in the first place.
In fact, and only 11 states (California, Florida, Illinois, Maryland, Massachusetts, Michigan, Montana, New Hampshire, Oregon, Pennsylvania, and Washington) require the consent of both parties. All other states and territories actually allow it even if one party has not given consent. And some patients don’t ask permission at all; they just do it.
Another misconception was the perceived frequency of such situations. Recordings of conversations in the doctor’s office are by no means rare. A 2014 survey in the United Kingdom revealed that 15% of the public had secretly recorded a clinic visit, and a further 11% were aware of someone else doing the same, a topic discussed by a Dartmouth group in the Aug. 8, 2017, issue of JAMA.
In general, younger respondents to my (admittedly unscientific) informal survey tended to be less receptive to being recorded. “I do not allow recordings by patients because I can’t control how they may be used later and it’s just creepy,” wrote one. “It just seems a strange way to begin a trusting, transparent patient/doctor relationship … this is not Instagram.”
“I will sometimes let them take a photo of a specimen or a defect but I don’t allow recording,” wrote another. “Same reasons; creepy and out of my control. I worry about it happening surreptitiously, but what can you do?”
You can proactively prohibit all office recordings by posting a “no recording” sign in your waiting room in the name of confidentiality and privacy. Should a patient initiate a covert recording anyway, you have the option of terminating the visit with a warning that a repeat attempt will result in discharge. If you practice in one of the 39 one-party states, the recording would still be admissible, but your notice gives your attorney an argument – specifically, that the patient made the recording after being expressly directed not to do so – if anyone ever tries to use the recording against you, or without your permission.
Older, more experienced practitioners in the survey tended to be more sanguine about recordings. “I have allowed patients to record all or parts of the visit,” wrote one. “I even allowed a patient to film a [liposuction] procedure. My decision … was that the patient might think I had something to hide, which I [did not].”
Another reported, “I have no problem with patients or family recording office visits or procedures. When someone is recording a procedure, I have no problem ignoring them.”
“We don’t have anything to hide, after all,” affirmed another. “In the era of telemedicine, many things can be recorded, even without permission.”
Several other veteran practitioners summarized my own philosophy on the subject: Patients have a right to record visits in my state (New Jersey), whether I like it or not, so I simply assume I’m being recorded during every visit, and conduct myself accordingly.
Risk managers and malpractice carriers are divided on recordings. At one neurology clinic in Arizona, patients are routinely offered videos of their visits, and clinicians who participate in these recordings receive a 10% reduction in the cost of their medical defense and extra liability coverage. There are clear advantages to having a permanent record of a doctor’s professional opinion. Other carriers are not as supportive, discouraging their insureds from allowing recordings to be made.
In the end, like it or not, recordings are here to stay, and the omnipresence of modern communications devices such as smartphones, tablets, etc., will only increase their prevalence. My advice: Familiarize yourself with the laws in your state, and never say anything during an office visit that you would not stand behind, if it ever turns out to have been recorded.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Recently I posted a simple question on several social media pages and internet blogs populated exclusively by board-certified dermatologists and dermatologic surgeons: How would you respond to a patient asking (or demanding) to record all or part of their office visit? (Or, if you have encountered such a situation, how did you respond?)
The question was simple, but the answers were somewhat complicated.
First, I noticed a fundamental misunderstanding of applicable laws: Many practitioners apparently believe that taping or recording a private conversation is per se illegal. Perhaps they are conflating with wiretapping laws, which don’t apply in this situation. HIPAA laws don’t apply either, because the patient, by definition, is waiving the right to privacy by initiating the recording in the first place.
In fact, and only 11 states (California, Florida, Illinois, Maryland, Massachusetts, Michigan, Montana, New Hampshire, Oregon, Pennsylvania, and Washington) require the consent of both parties. All other states and territories actually allow it even if one party has not given consent. And some patients don’t ask permission at all; they just do it.
Another misconception was the perceived frequency of such situations. Recordings of conversations in the doctor’s office are by no means rare. A 2014 survey in the United Kingdom revealed that 15% of the public had secretly recorded a clinic visit, and a further 11% were aware of someone else doing the same, a topic discussed by a Dartmouth group in the Aug. 8, 2017, issue of JAMA.
In general, younger respondents to my (admittedly unscientific) informal survey tended to be less receptive to being recorded. “I do not allow recordings by patients because I can’t control how they may be used later and it’s just creepy,” wrote one. “It just seems a strange way to begin a trusting, transparent patient/doctor relationship … this is not Instagram.”
“I will sometimes let them take a photo of a specimen or a defect but I don’t allow recording,” wrote another. “Same reasons; creepy and out of my control. I worry about it happening surreptitiously, but what can you do?”
You can proactively prohibit all office recordings by posting a “no recording” sign in your waiting room in the name of confidentiality and privacy. Should a patient initiate a covert recording anyway, you have the option of terminating the visit with a warning that a repeat attempt will result in discharge. If you practice in one of the 39 one-party states, the recording would still be admissible, but your notice gives your attorney an argument – specifically, that the patient made the recording after being expressly directed not to do so – if anyone ever tries to use the recording against you, or without your permission.
Older, more experienced practitioners in the survey tended to be more sanguine about recordings. “I have allowed patients to record all or parts of the visit,” wrote one. “I even allowed a patient to film a [liposuction] procedure. My decision … was that the patient might think I had something to hide, which I [did not].”
Another reported, “I have no problem with patients or family recording office visits or procedures. When someone is recording a procedure, I have no problem ignoring them.”
“We don’t have anything to hide, after all,” affirmed another. “In the era of telemedicine, many things can be recorded, even without permission.”
Several other veteran practitioners summarized my own philosophy on the subject: Patients have a right to record visits in my state (New Jersey), whether I like it or not, so I simply assume I’m being recorded during every visit, and conduct myself accordingly.
Risk managers and malpractice carriers are divided on recordings. At one neurology clinic in Arizona, patients are routinely offered videos of their visits, and clinicians who participate in these recordings receive a 10% reduction in the cost of their medical defense and extra liability coverage. There are clear advantages to having a permanent record of a doctor’s professional opinion. Other carriers are not as supportive, discouraging their insureds from allowing recordings to be made.
In the end, like it or not, recordings are here to stay, and the omnipresence of modern communications devices such as smartphones, tablets, etc., will only increase their prevalence. My advice: Familiarize yourself with the laws in your state, and never say anything during an office visit that you would not stand behind, if it ever turns out to have been recorded.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Recently I posted a simple question on several social media pages and internet blogs populated exclusively by board-certified dermatologists and dermatologic surgeons: How would you respond to a patient asking (or demanding) to record all or part of their office visit? (Or, if you have encountered such a situation, how did you respond?)
The question was simple, but the answers were somewhat complicated.
First, I noticed a fundamental misunderstanding of applicable laws: Many practitioners apparently believe that taping or recording a private conversation is per se illegal. Perhaps they are conflating with wiretapping laws, which don’t apply in this situation. HIPAA laws don’t apply either, because the patient, by definition, is waiving the right to privacy by initiating the recording in the first place.
In fact, and only 11 states (California, Florida, Illinois, Maryland, Massachusetts, Michigan, Montana, New Hampshire, Oregon, Pennsylvania, and Washington) require the consent of both parties. All other states and territories actually allow it even if one party has not given consent. And some patients don’t ask permission at all; they just do it.
Another misconception was the perceived frequency of such situations. Recordings of conversations in the doctor’s office are by no means rare. A 2014 survey in the United Kingdom revealed that 15% of the public had secretly recorded a clinic visit, and a further 11% were aware of someone else doing the same, a topic discussed by a Dartmouth group in the Aug. 8, 2017, issue of JAMA.
In general, younger respondents to my (admittedly unscientific) informal survey tended to be less receptive to being recorded. “I do not allow recordings by patients because I can’t control how they may be used later and it’s just creepy,” wrote one. “It just seems a strange way to begin a trusting, transparent patient/doctor relationship … this is not Instagram.”
“I will sometimes let them take a photo of a specimen or a defect but I don’t allow recording,” wrote another. “Same reasons; creepy and out of my control. I worry about it happening surreptitiously, but what can you do?”
You can proactively prohibit all office recordings by posting a “no recording” sign in your waiting room in the name of confidentiality and privacy. Should a patient initiate a covert recording anyway, you have the option of terminating the visit with a warning that a repeat attempt will result in discharge. If you practice in one of the 39 one-party states, the recording would still be admissible, but your notice gives your attorney an argument – specifically, that the patient made the recording after being expressly directed not to do so – if anyone ever tries to use the recording against you, or without your permission.
Older, more experienced practitioners in the survey tended to be more sanguine about recordings. “I have allowed patients to record all or parts of the visit,” wrote one. “I even allowed a patient to film a [liposuction] procedure. My decision … was that the patient might think I had something to hide, which I [did not].”
Another reported, “I have no problem with patients or family recording office visits or procedures. When someone is recording a procedure, I have no problem ignoring them.”
“We don’t have anything to hide, after all,” affirmed another. “In the era of telemedicine, many things can be recorded, even without permission.”
Several other veteran practitioners summarized my own philosophy on the subject: Patients have a right to record visits in my state (New Jersey), whether I like it or not, so I simply assume I’m being recorded during every visit, and conduct myself accordingly.
Risk managers and malpractice carriers are divided on recordings. At one neurology clinic in Arizona, patients are routinely offered videos of their visits, and clinicians who participate in these recordings receive a 10% reduction in the cost of their medical defense and extra liability coverage. There are clear advantages to having a permanent record of a doctor’s professional opinion. Other carriers are not as supportive, discouraging their insureds from allowing recordings to be made.
In the end, like it or not, recordings are here to stay, and the omnipresence of modern communications devices such as smartphones, tablets, etc., will only increase their prevalence. My advice: Familiarize yourself with the laws in your state, and never say anything during an office visit that you would not stand behind, if it ever turns out to have been recorded.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Six big changes coming for office-visit coding
Betsy Nicoletti, MS, a nationally recognized coding expert, will take your coding questions via email and provide guidance on how to code properly to maximize reimbursement. Have a question about coding? Send it to [email protected].
thanks to the American Medical Association.
The first major changes to the definitions for E/M services will be in effect as of Jan. 1, 2021, with all payers expected to adopt these new guidelines. In particular, the AMA has revised the definitions for E/M codes 99202-99215 in the Current Procedural Terminology (CPT) 2021 codebook. The existing guidelines were developed in 1995 and 1997 and remain in effect for all other E/M services determined by history, exam, and medical decision-making (MDM).
What do the new changes mean to you? In 2021, for new and established office and other outpatient services reported with codes 99202-99215, a clinician may select the code on the basis of time or MDM.
There are three elements in MDM, and two of three are required. These elements are the number and complexity of problems addressed, amount and/or complexity of data to be reviewed and analyzed, and risk of complications and/or morbidity or mortality of patient management.
Make sure you familiarize yourself with these six big changes. It may take a bit of time to integrate these new processes into your daily routine, but wrapping your head around them as soon as possible can help boost your bottom line:
1. History and exam don’t count toward level of service
Physicians, advanced practice registered nurses, and physician assistants won’t use history or exam to select what level of code to bill for office visits 99202-99215, as they did in the past. They need only document a medically appropriate history and exam. The history may be obtained by staff members and reviewed by the billing practitioner.
While specific history and exam requirements disappear for office visit codes, they remain for all other types of visits, selected on the basis of history, exam, and MDM, such as hospital services, nursing facility services, and home and domiciliary care. So, say goodbye to “all other systems reviewed and negative” in office notes, but keep it handy for those other E/M codes.
2. All time spent caring for the patient on a particular day counts
This includes all time spent on the day of service, including preparing to see the patient, seeing the patient, phone calls or other work done after the visit (if not billed with a care management or other CPT code), and documenting in the medical record. The AMA developed new guidelines for using time for office and other outpatient services. For codes 99202-99215, count all of the face-to-face and non–face-to-face time spent by the billing clinician on the day of the visit. Counseling does not need to be more than 50% of the total time.
Do not include any staff time or time spent on any days before or after the visit. This allows clinicians to capture the work when a significant amount of it takes place before or after the visit with the patient, and to bill for it on the day of the visit.
According to the 2021 CPT codebook, physician or other qualified health care professional time includes the following activities:
- Preparing to see the patient (e.g., review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests, or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the electronic or other health record.
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
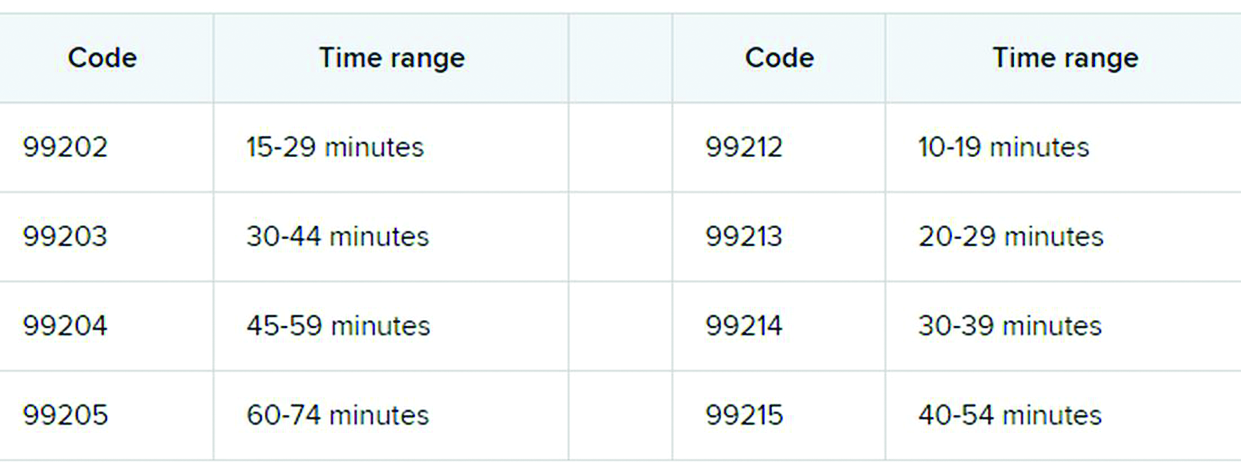
3. Soon to be gone: ‘new to the examiner’ and ‘workup planned’
The current guidelines don’t differentiate between a new problem to the clinician or an established problem to the clinician. So it doesn’t matter whether you’re hearing about a particular problem for the first time or the fifth time. The new office and outpatient services guidelines define problems only as they relate to the patient. For example, when selecting a level of service, a chronic problem with a mild exacerbation is the same level whether it’s the primary care physician seeing the patient for the 10th time to help manage her diabetes or the endocrinologist seeing the patient for the first time.
In the current guidelines (1995 and 1997), additional weight is given in selecting the level of MDM for a problem that’s new to the examiner with a workup planned, yet when the diagnostic test couldn’t be completed at the visit. This concept is gone from element of number and complexity of new problems. Ordering diagnostic tests is part of the second element, the amount and/or complexity of data to be reviewed.
4. Different guidelines if you need a history from a parent or other source
The new guidelines recognize the additional work required by the clinician when the patient is unable to give a history or when the practitioner doesn’t find the history to be reliable.
For example, in the case of a baby or child who is unable to give a history, the parent counts as an “independent historian,” according to the new guidelines. Likewise, for a patient with dementia, the caregiver counts as a historian. Note, however, that the criteria is not met simply because the patient is accompanied by another person. The additional weight in selecting the level of service is based on the patient being unable to give a reliable history.
Bottom line: In cases where patients are unable to communicate clearly, physicians or other providers should document the necessity of getting a complete history and who provided it.
5. A new spin on social determinants of health (SDoH)
In the risk of morbidity and/or mortality element, conditions described as “social determinants of health” are considered moderate complexity. SDoH are social and environmental factors that affect a patient’s health and medical outcomes. These include homelessness, inability to afford medications, food insecurity, and occupational exposure to risk factors. These circumstances are reported with codes in categories Z55-Z65.
In the past, physicians often documented this information in their office notes but rarely added a diagnosis code that described the patient’s situation. The ICD-10-CM code set includes codes that describe these factors. Using them allows the practice to track patients who have increased needs, and it communicates to payers the complexity of caring for these patients.
6. Risks related to surgery are defined
The current guidelines assign different levels of risk to minor and major surgery. They also include differentiation for “minor surgery with no identified risk factors,” “minor surgery with identified risk factors,” “elective major surgery with no identified risk factors,” and “elective major surgery with identified risk factors.” The old guidelines didn’t state whether the risk factors pertained to the patient – such as smoking, heart disease, or high body mass index – or to the procedure itself.
The new guidelines specifically say that it’s both. In the risk column, “decision regarding minor surgery with identified patient or procedure risk factors” and “decision regarding elective major surgery without patient or procedure risk factors” are both considered moderate. “Decision regarding elective major surgery with identified patient or procedure risk factors” and “decision regarding emergency major surgery” are in the high complexity column for risk.
Keep in mind that two of three elements are required: the number and complexity of problems, amount of data, and morbidity/mortality risk. Risk of morbidity/mortality alone doesn’t count as the basis for selecting the code. Of course, when surgeons see this, they ask, “What major procedures don’t have identified risk factors?”
Note, too, that these new CPT guidelines do not define the terms “minor” and “major” surgery. For payment reasons related to the postop period, the Centers for Medicare & Medicaid Services defines minor surgery as a procedure with 0-10 global days and a major surgery as a procedure with 90 global days. However, there are many procedures with 0 global days (endoscopy, cardiac catheterization) that are not minor procedures. Hopefully, the AMA will clarify this in 2021.
What’s the take-away for clinicians?
There are sure to be shifts in coding patterns based on these new guidelines. Some specialties will find that not being able to select a service based on history and exam alone will lower the level of service for which they can bill. Some practices, on the other hand, will be able to code for more high-level visits, without the need for a complete review of systems or a comprehensive exam.
The biggest challenge will be for practices that provide services both in the hospital and in the office, because they’ll have to use both sets of guidelines, depending on which type of service they’re performing.
For more details on what’s coming your way beginning on New Year’s Day, you may want to read the 16-page AMA document .
A version of this article first appeared on Medscape.com.
Betsy Nicoletti, MS, a nationally recognized coding expert, will take your coding questions via email and provide guidance on how to code properly to maximize reimbursement. Have a question about coding? Send it to [email protected].
thanks to the American Medical Association.
The first major changes to the definitions for E/M services will be in effect as of Jan. 1, 2021, with all payers expected to adopt these new guidelines. In particular, the AMA has revised the definitions for E/M codes 99202-99215 in the Current Procedural Terminology (CPT) 2021 codebook. The existing guidelines were developed in 1995 and 1997 and remain in effect for all other E/M services determined by history, exam, and medical decision-making (MDM).
What do the new changes mean to you? In 2021, for new and established office and other outpatient services reported with codes 99202-99215, a clinician may select the code on the basis of time or MDM.
There are three elements in MDM, and two of three are required. These elements are the number and complexity of problems addressed, amount and/or complexity of data to be reviewed and analyzed, and risk of complications and/or morbidity or mortality of patient management.
Make sure you familiarize yourself with these six big changes. It may take a bit of time to integrate these new processes into your daily routine, but wrapping your head around them as soon as possible can help boost your bottom line:
1. History and exam don’t count toward level of service
Physicians, advanced practice registered nurses, and physician assistants won’t use history or exam to select what level of code to bill for office visits 99202-99215, as they did in the past. They need only document a medically appropriate history and exam. The history may be obtained by staff members and reviewed by the billing practitioner.
While specific history and exam requirements disappear for office visit codes, they remain for all other types of visits, selected on the basis of history, exam, and MDM, such as hospital services, nursing facility services, and home and domiciliary care. So, say goodbye to “all other systems reviewed and negative” in office notes, but keep it handy for those other E/M codes.
2. All time spent caring for the patient on a particular day counts
This includes all time spent on the day of service, including preparing to see the patient, seeing the patient, phone calls or other work done after the visit (if not billed with a care management or other CPT code), and documenting in the medical record. The AMA developed new guidelines for using time for office and other outpatient services. For codes 99202-99215, count all of the face-to-face and non–face-to-face time spent by the billing clinician on the day of the visit. Counseling does not need to be more than 50% of the total time.
Do not include any staff time or time spent on any days before or after the visit. This allows clinicians to capture the work when a significant amount of it takes place before or after the visit with the patient, and to bill for it on the day of the visit.
According to the 2021 CPT codebook, physician or other qualified health care professional time includes the following activities:
- Preparing to see the patient (e.g., review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests, or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the electronic or other health record.
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
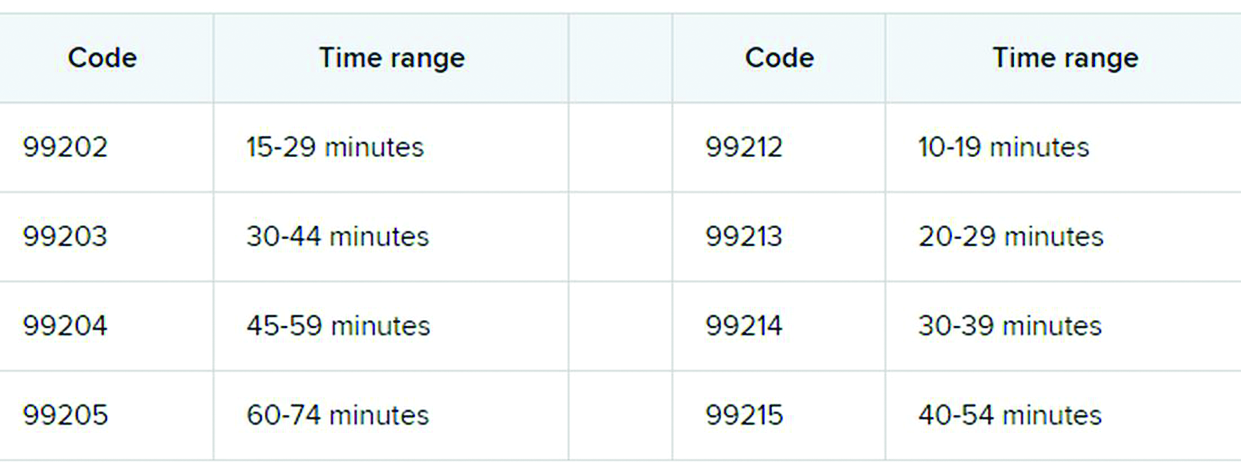
3. Soon to be gone: ‘new to the examiner’ and ‘workup planned’
The current guidelines don’t differentiate between a new problem to the clinician or an established problem to the clinician. So it doesn’t matter whether you’re hearing about a particular problem for the first time or the fifth time. The new office and outpatient services guidelines define problems only as they relate to the patient. For example, when selecting a level of service, a chronic problem with a mild exacerbation is the same level whether it’s the primary care physician seeing the patient for the 10th time to help manage her diabetes or the endocrinologist seeing the patient for the first time.
In the current guidelines (1995 and 1997), additional weight is given in selecting the level of MDM for a problem that’s new to the examiner with a workup planned, yet when the diagnostic test couldn’t be completed at the visit. This concept is gone from element of number and complexity of new problems. Ordering diagnostic tests is part of the second element, the amount and/or complexity of data to be reviewed.
4. Different guidelines if you need a history from a parent or other source
The new guidelines recognize the additional work required by the clinician when the patient is unable to give a history or when the practitioner doesn’t find the history to be reliable.
For example, in the case of a baby or child who is unable to give a history, the parent counts as an “independent historian,” according to the new guidelines. Likewise, for a patient with dementia, the caregiver counts as a historian. Note, however, that the criteria is not met simply because the patient is accompanied by another person. The additional weight in selecting the level of service is based on the patient being unable to give a reliable history.
Bottom line: In cases where patients are unable to communicate clearly, physicians or other providers should document the necessity of getting a complete history and who provided it.
5. A new spin on social determinants of health (SDoH)
In the risk of morbidity and/or mortality element, conditions described as “social determinants of health” are considered moderate complexity. SDoH are social and environmental factors that affect a patient’s health and medical outcomes. These include homelessness, inability to afford medications, food insecurity, and occupational exposure to risk factors. These circumstances are reported with codes in categories Z55-Z65.
In the past, physicians often documented this information in their office notes but rarely added a diagnosis code that described the patient’s situation. The ICD-10-CM code set includes codes that describe these factors. Using them allows the practice to track patients who have increased needs, and it communicates to payers the complexity of caring for these patients.
6. Risks related to surgery are defined
The current guidelines assign different levels of risk to minor and major surgery. They also include differentiation for “minor surgery with no identified risk factors,” “minor surgery with identified risk factors,” “elective major surgery with no identified risk factors,” and “elective major surgery with identified risk factors.” The old guidelines didn’t state whether the risk factors pertained to the patient – such as smoking, heart disease, or high body mass index – or to the procedure itself.
The new guidelines specifically say that it’s both. In the risk column, “decision regarding minor surgery with identified patient or procedure risk factors” and “decision regarding elective major surgery without patient or procedure risk factors” are both considered moderate. “Decision regarding elective major surgery with identified patient or procedure risk factors” and “decision regarding emergency major surgery” are in the high complexity column for risk.
Keep in mind that two of three elements are required: the number and complexity of problems, amount of data, and morbidity/mortality risk. Risk of morbidity/mortality alone doesn’t count as the basis for selecting the code. Of course, when surgeons see this, they ask, “What major procedures don’t have identified risk factors?”
Note, too, that these new CPT guidelines do not define the terms “minor” and “major” surgery. For payment reasons related to the postop period, the Centers for Medicare & Medicaid Services defines minor surgery as a procedure with 0-10 global days and a major surgery as a procedure with 90 global days. However, there are many procedures with 0 global days (endoscopy, cardiac catheterization) that are not minor procedures. Hopefully, the AMA will clarify this in 2021.
What’s the take-away for clinicians?
There are sure to be shifts in coding patterns based on these new guidelines. Some specialties will find that not being able to select a service based on history and exam alone will lower the level of service for which they can bill. Some practices, on the other hand, will be able to code for more high-level visits, without the need for a complete review of systems or a comprehensive exam.
The biggest challenge will be for practices that provide services both in the hospital and in the office, because they’ll have to use both sets of guidelines, depending on which type of service they’re performing.
For more details on what’s coming your way beginning on New Year’s Day, you may want to read the 16-page AMA document .
A version of this article first appeared on Medscape.com.
Betsy Nicoletti, MS, a nationally recognized coding expert, will take your coding questions via email and provide guidance on how to code properly to maximize reimbursement. Have a question about coding? Send it to [email protected].
thanks to the American Medical Association.
The first major changes to the definitions for E/M services will be in effect as of Jan. 1, 2021, with all payers expected to adopt these new guidelines. In particular, the AMA has revised the definitions for E/M codes 99202-99215 in the Current Procedural Terminology (CPT) 2021 codebook. The existing guidelines were developed in 1995 and 1997 and remain in effect for all other E/M services determined by history, exam, and medical decision-making (MDM).
What do the new changes mean to you? In 2021, for new and established office and other outpatient services reported with codes 99202-99215, a clinician may select the code on the basis of time or MDM.
There are three elements in MDM, and two of three are required. These elements are the number and complexity of problems addressed, amount and/or complexity of data to be reviewed and analyzed, and risk of complications and/or morbidity or mortality of patient management.
Make sure you familiarize yourself with these six big changes. It may take a bit of time to integrate these new processes into your daily routine, but wrapping your head around them as soon as possible can help boost your bottom line:
1. History and exam don’t count toward level of service
Physicians, advanced practice registered nurses, and physician assistants won’t use history or exam to select what level of code to bill for office visits 99202-99215, as they did in the past. They need only document a medically appropriate history and exam. The history may be obtained by staff members and reviewed by the billing practitioner.
While specific history and exam requirements disappear for office visit codes, they remain for all other types of visits, selected on the basis of history, exam, and MDM, such as hospital services, nursing facility services, and home and domiciliary care. So, say goodbye to “all other systems reviewed and negative” in office notes, but keep it handy for those other E/M codes.
2. All time spent caring for the patient on a particular day counts
This includes all time spent on the day of service, including preparing to see the patient, seeing the patient, phone calls or other work done after the visit (if not billed with a care management or other CPT code), and documenting in the medical record. The AMA developed new guidelines for using time for office and other outpatient services. For codes 99202-99215, count all of the face-to-face and non–face-to-face time spent by the billing clinician on the day of the visit. Counseling does not need to be more than 50% of the total time.
Do not include any staff time or time spent on any days before or after the visit. This allows clinicians to capture the work when a significant amount of it takes place before or after the visit with the patient, and to bill for it on the day of the visit.
According to the 2021 CPT codebook, physician or other qualified health care professional time includes the following activities:
- Preparing to see the patient (e.g., review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests, or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the electronic or other health record.
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
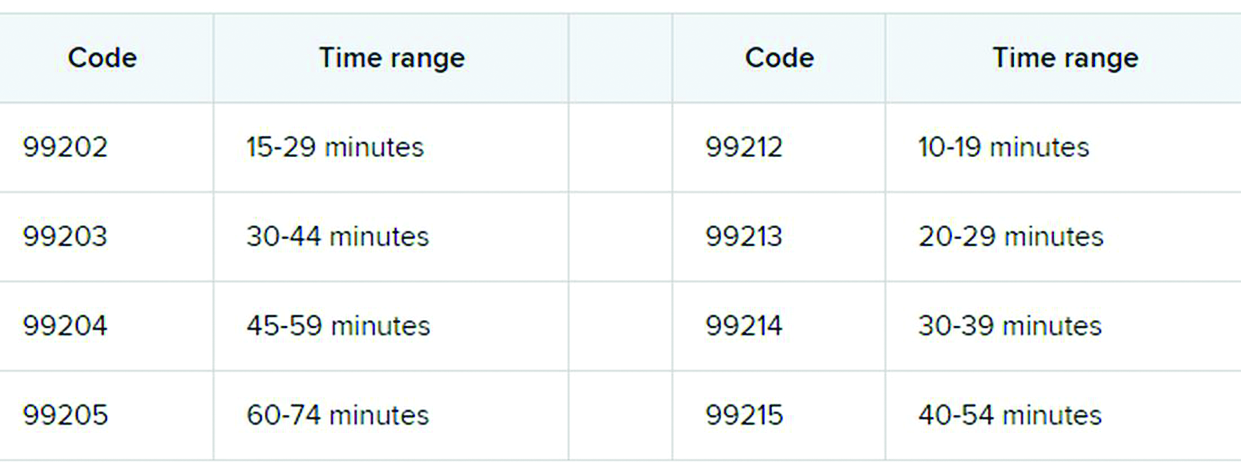
3. Soon to be gone: ‘new to the examiner’ and ‘workup planned’
The current guidelines don’t differentiate between a new problem to the clinician or an established problem to the clinician. So it doesn’t matter whether you’re hearing about a particular problem for the first time or the fifth time. The new office and outpatient services guidelines define problems only as they relate to the patient. For example, when selecting a level of service, a chronic problem with a mild exacerbation is the same level whether it’s the primary care physician seeing the patient for the 10th time to help manage her diabetes or the endocrinologist seeing the patient for the first time.
In the current guidelines (1995 and 1997), additional weight is given in selecting the level of MDM for a problem that’s new to the examiner with a workup planned, yet when the diagnostic test couldn’t be completed at the visit. This concept is gone from element of number and complexity of new problems. Ordering diagnostic tests is part of the second element, the amount and/or complexity of data to be reviewed.
4. Different guidelines if you need a history from a parent or other source
The new guidelines recognize the additional work required by the clinician when the patient is unable to give a history or when the practitioner doesn’t find the history to be reliable.
For example, in the case of a baby or child who is unable to give a history, the parent counts as an “independent historian,” according to the new guidelines. Likewise, for a patient with dementia, the caregiver counts as a historian. Note, however, that the criteria is not met simply because the patient is accompanied by another person. The additional weight in selecting the level of service is based on the patient being unable to give a reliable history.
Bottom line: In cases where patients are unable to communicate clearly, physicians or other providers should document the necessity of getting a complete history and who provided it.
5. A new spin on social determinants of health (SDoH)
In the risk of morbidity and/or mortality element, conditions described as “social determinants of health” are considered moderate complexity. SDoH are social and environmental factors that affect a patient’s health and medical outcomes. These include homelessness, inability to afford medications, food insecurity, and occupational exposure to risk factors. These circumstances are reported with codes in categories Z55-Z65.
In the past, physicians often documented this information in their office notes but rarely added a diagnosis code that described the patient’s situation. The ICD-10-CM code set includes codes that describe these factors. Using them allows the practice to track patients who have increased needs, and it communicates to payers the complexity of caring for these patients.
6. Risks related to surgery are defined
The current guidelines assign different levels of risk to minor and major surgery. They also include differentiation for “minor surgery with no identified risk factors,” “minor surgery with identified risk factors,” “elective major surgery with no identified risk factors,” and “elective major surgery with identified risk factors.” The old guidelines didn’t state whether the risk factors pertained to the patient – such as smoking, heart disease, or high body mass index – or to the procedure itself.
The new guidelines specifically say that it’s both. In the risk column, “decision regarding minor surgery with identified patient or procedure risk factors” and “decision regarding elective major surgery without patient or procedure risk factors” are both considered moderate. “Decision regarding elective major surgery with identified patient or procedure risk factors” and “decision regarding emergency major surgery” are in the high complexity column for risk.
Keep in mind that two of three elements are required: the number and complexity of problems, amount of data, and morbidity/mortality risk. Risk of morbidity/mortality alone doesn’t count as the basis for selecting the code. Of course, when surgeons see this, they ask, “What major procedures don’t have identified risk factors?”
Note, too, that these new CPT guidelines do not define the terms “minor” and “major” surgery. For payment reasons related to the postop period, the Centers for Medicare & Medicaid Services defines minor surgery as a procedure with 0-10 global days and a major surgery as a procedure with 90 global days. However, there are many procedures with 0 global days (endoscopy, cardiac catheterization) that are not minor procedures. Hopefully, the AMA will clarify this in 2021.
What’s the take-away for clinicians?
There are sure to be shifts in coding patterns based on these new guidelines. Some specialties will find that not being able to select a service based on history and exam alone will lower the level of service for which they can bill. Some practices, on the other hand, will be able to code for more high-level visits, without the need for a complete review of systems or a comprehensive exam.
The biggest challenge will be for practices that provide services both in the hospital and in the office, because they’ll have to use both sets of guidelines, depending on which type of service they’re performing.
For more details on what’s coming your way beginning on New Year’s Day, you may want to read the 16-page AMA document .
A version of this article first appeared on Medscape.com.
COVID-19 and patient safety in the medical office
Editor’s note: This article has been provided by The Doctors Company, the exclusively endorsed medical malpractice carrier for the Society of Hospital Medicine.
As the pandemic hits its third nationwide surge, families are gathering for the holidays, and medical practices are preparing for a potential increase in cases. Medical offices in states that were not strongly affected by the first and second waves of the virus may now be facing an influx of COVID-19 patients. Therefore, medical offices must remain very attentive to the widespread outbreak of COVID-19, continuing to proactively take steps to safely manage patients while protecting clinical staff.
Here are tips and resources for this season of the pandemic:
- Documentation: Maintain administrative records of how you have adapted to the evolving crisis, including the challenges you faced. For details, see Keep a COVID-19 Diary: Document Now in Case of Future Lawsuits.
- Legislation and Guidance: Reference the CDC; your state medical board; professional societies; and federal, state, and local authorities daily for public health guidance and new legislation, as this continues to be a fluid situation.
- Screening Criteria: Follow the CDC’s patient assessment protocol for early disease detection for patients presenting to your practice. Patients should be screened using these guidelines: Overview of Testing for SARS-CoV-2 (COVID-19). Essential visitors to your facility should also be assessed for symptoms of coronavirus and contact exposure and redirected to remain outside if suspect.
- Accepting Patients: Do not turn patients away simply because a patient calls with acute respiratory symptoms. Refusing assessment/care may lead to concerns of patient abandonment.
- Designated Triage Location: Check with your local public health authorities for locations designated to triage suspected patients, so exposure is limited in general medical offices.
- Telehealth Triage: Licensed staff should be trained in triage protocol to determine which patients can be managed safely at home. See Healthcare Facilities: Managing Operations During the COVID-19 Pandemic. The Doctors Company offers resources on telemedicine in our COVID-19 Telehealth Resource Center.
- Patient Testing: When there is a reasonable presumption that a patient may have been exposed to COVID-19, contact the local or state health department to coordinate testing using available community resources. See the CDC’s Testing for COVID-19 , the COVID-19 Testing Overview, and the Clinician Call Center.
- Elective Services: Check with regional governmental and health authorities on the provision of nonessential and elective health care visits and group-related activities. Many states continue or have reinstated restrictions on the provision of nonurgent, elective surgeries and procedures.
- Patient Precautions: Educational resources, including posters for use in the medical office, are available from the WHO and for health care workers from the CDC (Contact Precautions, Droplet Precautions, and Airborne Precautions). Reference the CDC’s and Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19) for patient management guidance.
- Provider/Staff Precautions: Follow Standard Precautions and Transmission-Based Precautions, including gloves, gowns, protective eyewear, and NIOSH-certified N95 respirators that have been properly fit-tested. If there is a shortage of N95 respirators in your facility, access current CDC respirator recommendations and review Optimizing Personal Protective Equipment (PPE) Supplies.
- Limit Exposure: Limit staff exposure to suspected patients, with the exam room door kept closed. Ideally, the designated exam room should be at the back of the office, far away from other staff and patients.
- Surface Disinfection: Once the patient exits the room, conduct surface disinfection while staff continues to wear PPE.
- Patient Education: Provide up-to-date, factual information on the virus to suspected COVID-19–positive patients and their close contacts.
- Provider/Staff Exposure: Screen health care personnel daily for symptoms/contacts relevant to COVID-19. Any unprotected occupational exposure by staff members should be assessed and monitored. See Interim U.S. Guidance for Risk Assessment and Work Restrictions for Healthcare Personnel with Potential Exposure to COVID-19. Should providers and/or staff test positive within your facility, conduct and document a risk assessment identifying contacts, type of interaction, and PPE in use, then contact local health authorities for additional instruction. The CDC provides guidance here under the section “Infection Control.” The health department may assist with patient notification if determined to be necessary. For return-to-work guidance, review the Criteria for Return to Work for Healthcare Personnel with SARS-CoV-2 Infection (Interim Guidance).
- Staff Training: Provide and document additional staff training as protocols change. Maintain training records in administrative files.
Ms. Hill is senior patient safety risk manager at The Doctors Company. The guidelines suggested here are not rules, do not constitute legal advice, and do not ensure a successful outcome. The ultimate decision regarding the appropriateness of any treatment must be made by each health care provider considering the circumstances of the individual situation and in accordance with the laws of the jurisdiction in which the care is rendered.
Editor’s note: This article has been provided by The Doctors Company, the exclusively endorsed medical malpractice carrier for the Society of Hospital Medicine.
As the pandemic hits its third nationwide surge, families are gathering for the holidays, and medical practices are preparing for a potential increase in cases. Medical offices in states that were not strongly affected by the first and second waves of the virus may now be facing an influx of COVID-19 patients. Therefore, medical offices must remain very attentive to the widespread outbreak of COVID-19, continuing to proactively take steps to safely manage patients while protecting clinical staff.
Here are tips and resources for this season of the pandemic:
- Documentation: Maintain administrative records of how you have adapted to the evolving crisis, including the challenges you faced. For details, see Keep a COVID-19 Diary: Document Now in Case of Future Lawsuits.
- Legislation and Guidance: Reference the CDC; your state medical board; professional societies; and federal, state, and local authorities daily for public health guidance and new legislation, as this continues to be a fluid situation.
- Screening Criteria: Follow the CDC’s patient assessment protocol for early disease detection for patients presenting to your practice. Patients should be screened using these guidelines: Overview of Testing for SARS-CoV-2 (COVID-19). Essential visitors to your facility should also be assessed for symptoms of coronavirus and contact exposure and redirected to remain outside if suspect.
- Accepting Patients: Do not turn patients away simply because a patient calls with acute respiratory symptoms. Refusing assessment/care may lead to concerns of patient abandonment.
- Designated Triage Location: Check with your local public health authorities for locations designated to triage suspected patients, so exposure is limited in general medical offices.
- Telehealth Triage: Licensed staff should be trained in triage protocol to determine which patients can be managed safely at home. See Healthcare Facilities: Managing Operations During the COVID-19 Pandemic. The Doctors Company offers resources on telemedicine in our COVID-19 Telehealth Resource Center.
- Patient Testing: When there is a reasonable presumption that a patient may have been exposed to COVID-19, contact the local or state health department to coordinate testing using available community resources. See the CDC’s Testing for COVID-19 , the COVID-19 Testing Overview, and the Clinician Call Center.
- Elective Services: Check with regional governmental and health authorities on the provision of nonessential and elective health care visits and group-related activities. Many states continue or have reinstated restrictions on the provision of nonurgent, elective surgeries and procedures.
- Patient Precautions: Educational resources, including posters for use in the medical office, are available from the WHO and for health care workers from the CDC (Contact Precautions, Droplet Precautions, and Airborne Precautions). Reference the CDC’s and Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19) for patient management guidance.
- Provider/Staff Precautions: Follow Standard Precautions and Transmission-Based Precautions, including gloves, gowns, protective eyewear, and NIOSH-certified N95 respirators that have been properly fit-tested. If there is a shortage of N95 respirators in your facility, access current CDC respirator recommendations and review Optimizing Personal Protective Equipment (PPE) Supplies.
- Limit Exposure: Limit staff exposure to suspected patients, with the exam room door kept closed. Ideally, the designated exam room should be at the back of the office, far away from other staff and patients.
- Surface Disinfection: Once the patient exits the room, conduct surface disinfection while staff continues to wear PPE.
- Patient Education: Provide up-to-date, factual information on the virus to suspected COVID-19–positive patients and their close contacts.
- Provider/Staff Exposure: Screen health care personnel daily for symptoms/contacts relevant to COVID-19. Any unprotected occupational exposure by staff members should be assessed and monitored. See Interim U.S. Guidance for Risk Assessment and Work Restrictions for Healthcare Personnel with Potential Exposure to COVID-19. Should providers and/or staff test positive within your facility, conduct and document a risk assessment identifying contacts, type of interaction, and PPE in use, then contact local health authorities for additional instruction. The CDC provides guidance here under the section “Infection Control.” The health department may assist with patient notification if determined to be necessary. For return-to-work guidance, review the Criteria for Return to Work for Healthcare Personnel with SARS-CoV-2 Infection (Interim Guidance).
- Staff Training: Provide and document additional staff training as protocols change. Maintain training records in administrative files.
Ms. Hill is senior patient safety risk manager at The Doctors Company. The guidelines suggested here are not rules, do not constitute legal advice, and do not ensure a successful outcome. The ultimate decision regarding the appropriateness of any treatment must be made by each health care provider considering the circumstances of the individual situation and in accordance with the laws of the jurisdiction in which the care is rendered.
Editor’s note: This article has been provided by The Doctors Company, the exclusively endorsed medical malpractice carrier for the Society of Hospital Medicine.
As the pandemic hits its third nationwide surge, families are gathering for the holidays, and medical practices are preparing for a potential increase in cases. Medical offices in states that were not strongly affected by the first and second waves of the virus may now be facing an influx of COVID-19 patients. Therefore, medical offices must remain very attentive to the widespread outbreak of COVID-19, continuing to proactively take steps to safely manage patients while protecting clinical staff.
Here are tips and resources for this season of the pandemic:
- Documentation: Maintain administrative records of how you have adapted to the evolving crisis, including the challenges you faced. For details, see Keep a COVID-19 Diary: Document Now in Case of Future Lawsuits.
- Legislation and Guidance: Reference the CDC; your state medical board; professional societies; and federal, state, and local authorities daily for public health guidance and new legislation, as this continues to be a fluid situation.
- Screening Criteria: Follow the CDC’s patient assessment protocol for early disease detection for patients presenting to your practice. Patients should be screened using these guidelines: Overview of Testing for SARS-CoV-2 (COVID-19). Essential visitors to your facility should also be assessed for symptoms of coronavirus and contact exposure and redirected to remain outside if suspect.
- Accepting Patients: Do not turn patients away simply because a patient calls with acute respiratory symptoms. Refusing assessment/care may lead to concerns of patient abandonment.
- Designated Triage Location: Check with your local public health authorities for locations designated to triage suspected patients, so exposure is limited in general medical offices.
- Telehealth Triage: Licensed staff should be trained in triage protocol to determine which patients can be managed safely at home. See Healthcare Facilities: Managing Operations During the COVID-19 Pandemic. The Doctors Company offers resources on telemedicine in our COVID-19 Telehealth Resource Center.
- Patient Testing: When there is a reasonable presumption that a patient may have been exposed to COVID-19, contact the local or state health department to coordinate testing using available community resources. See the CDC’s Testing for COVID-19 , the COVID-19 Testing Overview, and the Clinician Call Center.
- Elective Services: Check with regional governmental and health authorities on the provision of nonessential and elective health care visits and group-related activities. Many states continue or have reinstated restrictions on the provision of nonurgent, elective surgeries and procedures.
- Patient Precautions: Educational resources, including posters for use in the medical office, are available from the WHO and for health care workers from the CDC (Contact Precautions, Droplet Precautions, and Airborne Precautions). Reference the CDC’s and Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19) for patient management guidance.
- Provider/Staff Precautions: Follow Standard Precautions and Transmission-Based Precautions, including gloves, gowns, protective eyewear, and NIOSH-certified N95 respirators that have been properly fit-tested. If there is a shortage of N95 respirators in your facility, access current CDC respirator recommendations and review Optimizing Personal Protective Equipment (PPE) Supplies.
- Limit Exposure: Limit staff exposure to suspected patients, with the exam room door kept closed. Ideally, the designated exam room should be at the back of the office, far away from other staff and patients.
- Surface Disinfection: Once the patient exits the room, conduct surface disinfection while staff continues to wear PPE.
- Patient Education: Provide up-to-date, factual information on the virus to suspected COVID-19–positive patients and their close contacts.
- Provider/Staff Exposure: Screen health care personnel daily for symptoms/contacts relevant to COVID-19. Any unprotected occupational exposure by staff members should be assessed and monitored. See Interim U.S. Guidance for Risk Assessment and Work Restrictions for Healthcare Personnel with Potential Exposure to COVID-19. Should providers and/or staff test positive within your facility, conduct and document a risk assessment identifying contacts, type of interaction, and PPE in use, then contact local health authorities for additional instruction. The CDC provides guidance here under the section “Infection Control.” The health department may assist with patient notification if determined to be necessary. For return-to-work guidance, review the Criteria for Return to Work for Healthcare Personnel with SARS-CoV-2 Infection (Interim Guidance).
- Staff Training: Provide and document additional staff training as protocols change. Maintain training records in administrative files.
Ms. Hill is senior patient safety risk manager at The Doctors Company. The guidelines suggested here are not rules, do not constitute legal advice, and do not ensure a successful outcome. The ultimate decision regarding the appropriateness of any treatment must be made by each health care provider considering the circumstances of the individual situation and in accordance with the laws of the jurisdiction in which the care is rendered.
Etonogestrel implants may be bent, fractured by trauma or during sports
In 2017, Global Pediatric Health published a case report series associated with the use of long-acting reversible contraceptives, specifically the etonogestrel implant.
In November 2020, the makers of the etonogestrel implant (Merck) recommended a change in practice with the release of a notice to health care providers certified in the training of this product. This mass marketing blast included an updated warning and cautions for prescribers as well as patient information on the potential risks of migration, fracture, and bent devices attributable to trauma or sports. “Broken or Bent Implant (Section 5.16). The addition of the following underlined language: “There have been reports of broken or bent implants, which may be related to external forces (e.g., manipulation of the implant or contact sports) while in the patient’s arm. There have also been reports of migration of a broken implant fragment within the arm.”
Clearly the etonogestrel subdermal hormonal implant is an effective form of contraception and particularly beneficial in nonadherent sexually active teens who struggle to remember oral contraceptives. But it is important to be aware of this alert. Little is known about the type of trauma or rate of external force required to cause migration, fracture, or bend implants. This update requires adequate counseling of potential risks and complications of the etonogestrel implant, including the risk of migration, fracture, or bent devices specifically in the event of contact sports and trauma.
Ms. Thew is medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She is a member of the Pediatric News editorial advisory board. She had no relevant financial disclosures. Email Ms. Thew at [email protected].
In 2017, Global Pediatric Health published a case report series associated with the use of long-acting reversible contraceptives, specifically the etonogestrel implant.
In November 2020, the makers of the etonogestrel implant (Merck) recommended a change in practice with the release of a notice to health care providers certified in the training of this product. This mass marketing blast included an updated warning and cautions for prescribers as well as patient information on the potential risks of migration, fracture, and bent devices attributable to trauma or sports. “Broken or Bent Implant (Section 5.16). The addition of the following underlined language: “There have been reports of broken or bent implants, which may be related to external forces (e.g., manipulation of the implant or contact sports) while in the patient’s arm. There have also been reports of migration of a broken implant fragment within the arm.”
Clearly the etonogestrel subdermal hormonal implant is an effective form of contraception and particularly beneficial in nonadherent sexually active teens who struggle to remember oral contraceptives. But it is important to be aware of this alert. Little is known about the type of trauma or rate of external force required to cause migration, fracture, or bend implants. This update requires adequate counseling of potential risks and complications of the etonogestrel implant, including the risk of migration, fracture, or bent devices specifically in the event of contact sports and trauma.
Ms. Thew is medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She is a member of the Pediatric News editorial advisory board. She had no relevant financial disclosures. Email Ms. Thew at [email protected].
In 2017, Global Pediatric Health published a case report series associated with the use of long-acting reversible contraceptives, specifically the etonogestrel implant.
In November 2020, the makers of the etonogestrel implant (Merck) recommended a change in practice with the release of a notice to health care providers certified in the training of this product. This mass marketing blast included an updated warning and cautions for prescribers as well as patient information on the potential risks of migration, fracture, and bent devices attributable to trauma or sports. “Broken or Bent Implant (Section 5.16). The addition of the following underlined language: “There have been reports of broken or bent implants, which may be related to external forces (e.g., manipulation of the implant or contact sports) while in the patient’s arm. There have also been reports of migration of a broken implant fragment within the arm.”
Clearly the etonogestrel subdermal hormonal implant is an effective form of contraception and particularly beneficial in nonadherent sexually active teens who struggle to remember oral contraceptives. But it is important to be aware of this alert. Little is known about the type of trauma or rate of external force required to cause migration, fracture, or bend implants. This update requires adequate counseling of potential risks and complications of the etonogestrel implant, including the risk of migration, fracture, or bent devices specifically in the event of contact sports and trauma.
Ms. Thew is medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She is a member of the Pediatric News editorial advisory board. She had no relevant financial disclosures. Email Ms. Thew at [email protected].
To vape or not to vape: Is that really a question?
All pediatricians are relieved that the rates of children smoking cigarettes has dropped steadily since 2011. This decline seems to be associated with education on the dangers of cigarettes and fewer parents smoking. Perhaps less modeling of cigarette use in movies (although it increased again from 2010 to 2019) and lawsuits against advertisements targeting children also has helped.
“Whew,” we may have said, “we can relax our efforts to convince children to avoid smoking.” But, as is commonly true in medicine, the next threat was right around the corner – in this case vaping or e-cigarettes, also called vapes, e-hookahs, vape pens, tank systems, mods, and electronic nicotine delivery systems. And the size of the problem is huge – over 20% of high school students report using e-cigarettes – and immediate, as vaping can kill in the short term as well as causing long-term harm.
“E-cigarette, or vaping, product use–associated Lung Injury” – EVALI for short – has killed 68 vapers and hospitalized thousands. EVALI is thought to be caused by a vitamin E acetate additive used when vaping marijuana, particularly from informal sources like friends, family, or in-person or online dealers.
Vaping increases the risk of severe COVID-19 disease
While EVALI deaths dropped in months after being explained, the COVID-19 epidemic is now a much greater threat to vapers. Vaping increases risk of severe COVID-19 disease because of its immediate paralysis of lung cilia. Sharing vape devices and touching one’s lips while using also increase the risk of virus transmission. Vaping and smoking increase the number of ACE2 receptors to which the SARS-CoV-2 virus attaches causing the characteristic cell damage, and suppresses macrophages and neutrophils, resulting in more smokers testing positive, being twice as likely to develop a severe illness and get hospitalized because of pneumonia from COVID-19, and being less likely to recover. Unfortunately, addressing this new threat to the immediate and long-term health of our patients appears to be more complicated than for addressing smoking tobacco. First of all, vaping is much more difficult to detect than smelly cigarettes sending smoke signals from behind the garage or in the school bathrooms. Many, if not most, adults do not recognize the vaping devices when they see them, as many are tiny and some look like computer thumb drives. The aerosol emitted when in use, while containing dangerous toxins, has less odor than tobacco smoke. Vaping equipment and ads have been designed to attract youth, including linking them to sports and music events. Vaping has been advertised as a way to wean off nicotine addiction, a claim that has some scientific evidence in adults, but at a lower dose of nicotine. Warning children about the dangers of marijuana vaping has been made less credible by the rapid expansion of legalization of marijuana around the United States, eliciting “I told you it was fine” reactions from youth. And the person vaping does not know what or how much of the psychoactive components are being delivered into their bodies. One Juul pod, for example, has the equivalent in nicotine of an entire pack of 20 cigarettes. They are highly addictive, especially to the developing brain, such that youth who vape are more likely to become addicted and to smoke cigarettes in the future.
Help from federal regulation has been weak
While all 50 states ban sales to youth, adults can still buy. Food and Drug Administration limitations on kid-friendly ads, and use of sweet, fruity, and mint flavorings that are most preferred by children, apply only to new producers. The FDA does not yet regulate content of vaping solutions.
So we pediatricians are on the front line for this new threat to prevent vaping or convince youth to cut down or quit. The first step in addressing vaping is being knowledgeable about its many known and emerging health risks. It may seem obvious that the dangers of vaping microscopic particles depends on the contents. Water vapor alone is not dangerous; in fact, we prescribe it in nebulizers. Unfortunately, the contents of different vaping products vary and are not well defined in different vape products. The process of using an electric current to vaporize a substance can make it more toxic than the precursor, and teens have little idea about the substances they are inhaling. The psychoactive components vary from nicotine to tetrahydrocannabinol in varying amounts. These have the well known effects of stimulation or a high, but also the potential adverse effects of poor concentration, agitation, and even psychosis. Most e-cigarettes contain nicotine, which is highly addictive and can harm adolescent brain development, which continues into the early- to mid-20s. About two-thirds of Juul users aged 15-24 years did not know that it always contains nicotine, as do 99% of all vape solutions (Centers for Disease Control and Prevention, 2020). Earlier use of nicotine is more highly associated with later addiction to tobacco products that cause lung damage, acid reflux, insulin resistance, harm to the testes, harm to fetuses, cancer, and heart disease.
E-cigarette aerosols also contain dozens of other harmful substances besides nicotine ranging from acetone, propylene glycol, and metals to formaldehyde and ethyl benzene. These same chemicals are part of familiar toxic substances such as antifreeze, paint thinner, and pesticides. These cause ear, eye and throat irritation, and impairments in the cardiovascular system reducing athletic ability – at the least. Some flavorings in vape fluids also are toxic. Even the residual left on furniture and floors is harmful to those coming in contact, including pets.
How to encourage teens not to vaping
Trying to scare youth about health hazards is not generally effective in stopping risk behaviors since adolescence is a time of perceived singularity (it does not apply to me) and even a sense of immortality. Teens also see peers who vape as being unaffected and decide on using based on this small personal sample instead of valid statistics.
But teens do pay some attention to peer models or influencers saying why they do not use. One source of such testimony you can refer to is videos of inspiring athletes, musicians, and other “cool” young adults found on the naturalhigh.org website. You may know other examples of community teens desisting you can reference.
Parent rules, and less so advice, against smoking have been shown to be effective in deterring youth cigarette smoking. Because parents are less aware of vaping and its dangers, another step we can take is educating parents in our practices about vaping, its variable forms, its effects, and dangers, supplying authoritative materials, and advising them to talk with their children. Other steps the American Academy of Pediatrics recommends regarding smoking is for parents to be a role model of not using or try to quit, designate the house and car as smoking free, avoid children viewing smoking in media, tell their children about the side effects, and encourage their children who use to quit. Parents also can encourage schools to teach and have rules about smoking and vaping (e.g., med.stanford.edu/tobaccopreventiontoolkit.html).
Another approach we have been using is to not only screen for all substance use, but also to gather information about the teen’s strengths, activities, and life goals both to enhance rapport and to reference during motivational interviewing as reasons to avoid, reduce, or quit vaping. Motivational interviewing has been shown to help patients make healthier lifestyle choices by nonjudgmentally exploring their pros and cons in a conversation that takes into account readiness to change. This fits well with the stage of developing autonomy when teens want above all to make their own decisions. The cons of using can be discussed as including the effects and side effects of vaping interfering with their favored activities and moving towards their identified goals. Praising abstinence and asking them to show you how they could decline offers to vape are valuable reinforcement you can provide.
Finally, we all know that teens hate being manipulated. Vaping education we provide can make it clear that youth are being tricked by companies – most being large cigarette producers who know the dangers of vaping – into getting addicted so these companies can get rich on their money.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She has no other relevant disclosures. Dr. Howard’s contribution to this publication is as a paid expert to MDedge News. Email her at [email protected].
All pediatricians are relieved that the rates of children smoking cigarettes has dropped steadily since 2011. This decline seems to be associated with education on the dangers of cigarettes and fewer parents smoking. Perhaps less modeling of cigarette use in movies (although it increased again from 2010 to 2019) and lawsuits against advertisements targeting children also has helped.
“Whew,” we may have said, “we can relax our efforts to convince children to avoid smoking.” But, as is commonly true in medicine, the next threat was right around the corner – in this case vaping or e-cigarettes, also called vapes, e-hookahs, vape pens, tank systems, mods, and electronic nicotine delivery systems. And the size of the problem is huge – over 20% of high school students report using e-cigarettes – and immediate, as vaping can kill in the short term as well as causing long-term harm.
“E-cigarette, or vaping, product use–associated Lung Injury” – EVALI for short – has killed 68 vapers and hospitalized thousands. EVALI is thought to be caused by a vitamin E acetate additive used when vaping marijuana, particularly from informal sources like friends, family, or in-person or online dealers.
Vaping increases the risk of severe COVID-19 disease
While EVALI deaths dropped in months after being explained, the COVID-19 epidemic is now a much greater threat to vapers. Vaping increases risk of severe COVID-19 disease because of its immediate paralysis of lung cilia. Sharing vape devices and touching one’s lips while using also increase the risk of virus transmission. Vaping and smoking increase the number of ACE2 receptors to which the SARS-CoV-2 virus attaches causing the characteristic cell damage, and suppresses macrophages and neutrophils, resulting in more smokers testing positive, being twice as likely to develop a severe illness and get hospitalized because of pneumonia from COVID-19, and being less likely to recover. Unfortunately, addressing this new threat to the immediate and long-term health of our patients appears to be more complicated than for addressing smoking tobacco. First of all, vaping is much more difficult to detect than smelly cigarettes sending smoke signals from behind the garage or in the school bathrooms. Many, if not most, adults do not recognize the vaping devices when they see them, as many are tiny and some look like computer thumb drives. The aerosol emitted when in use, while containing dangerous toxins, has less odor than tobacco smoke. Vaping equipment and ads have been designed to attract youth, including linking them to sports and music events. Vaping has been advertised as a way to wean off nicotine addiction, a claim that has some scientific evidence in adults, but at a lower dose of nicotine. Warning children about the dangers of marijuana vaping has been made less credible by the rapid expansion of legalization of marijuana around the United States, eliciting “I told you it was fine” reactions from youth. And the person vaping does not know what or how much of the psychoactive components are being delivered into their bodies. One Juul pod, for example, has the equivalent in nicotine of an entire pack of 20 cigarettes. They are highly addictive, especially to the developing brain, such that youth who vape are more likely to become addicted and to smoke cigarettes in the future.
Help from federal regulation has been weak
While all 50 states ban sales to youth, adults can still buy. Food and Drug Administration limitations on kid-friendly ads, and use of sweet, fruity, and mint flavorings that are most preferred by children, apply only to new producers. The FDA does not yet regulate content of vaping solutions.
So we pediatricians are on the front line for this new threat to prevent vaping or convince youth to cut down or quit. The first step in addressing vaping is being knowledgeable about its many known and emerging health risks. It may seem obvious that the dangers of vaping microscopic particles depends on the contents. Water vapor alone is not dangerous; in fact, we prescribe it in nebulizers. Unfortunately, the contents of different vaping products vary and are not well defined in different vape products. The process of using an electric current to vaporize a substance can make it more toxic than the precursor, and teens have little idea about the substances they are inhaling. The psychoactive components vary from nicotine to tetrahydrocannabinol in varying amounts. These have the well known effects of stimulation or a high, but also the potential adverse effects of poor concentration, agitation, and even psychosis. Most e-cigarettes contain nicotine, which is highly addictive and can harm adolescent brain development, which continues into the early- to mid-20s. About two-thirds of Juul users aged 15-24 years did not know that it always contains nicotine, as do 99% of all vape solutions (Centers for Disease Control and Prevention, 2020). Earlier use of nicotine is more highly associated with later addiction to tobacco products that cause lung damage, acid reflux, insulin resistance, harm to the testes, harm to fetuses, cancer, and heart disease.
E-cigarette aerosols also contain dozens of other harmful substances besides nicotine ranging from acetone, propylene glycol, and metals to formaldehyde and ethyl benzene. These same chemicals are part of familiar toxic substances such as antifreeze, paint thinner, and pesticides. These cause ear, eye and throat irritation, and impairments in the cardiovascular system reducing athletic ability – at the least. Some flavorings in vape fluids also are toxic. Even the residual left on furniture and floors is harmful to those coming in contact, including pets.
How to encourage teens not to vaping
Trying to scare youth about health hazards is not generally effective in stopping risk behaviors since adolescence is a time of perceived singularity (it does not apply to me) and even a sense of immortality. Teens also see peers who vape as being unaffected and decide on using based on this small personal sample instead of valid statistics.
But teens do pay some attention to peer models or influencers saying why they do not use. One source of such testimony you can refer to is videos of inspiring athletes, musicians, and other “cool” young adults found on the naturalhigh.org website. You may know other examples of community teens desisting you can reference.
Parent rules, and less so advice, against smoking have been shown to be effective in deterring youth cigarette smoking. Because parents are less aware of vaping and its dangers, another step we can take is educating parents in our practices about vaping, its variable forms, its effects, and dangers, supplying authoritative materials, and advising them to talk with their children. Other steps the American Academy of Pediatrics recommends regarding smoking is for parents to be a role model of not using or try to quit, designate the house and car as smoking free, avoid children viewing smoking in media, tell their children about the side effects, and encourage their children who use to quit. Parents also can encourage schools to teach and have rules about smoking and vaping (e.g., med.stanford.edu/tobaccopreventiontoolkit.html).
Another approach we have been using is to not only screen for all substance use, but also to gather information about the teen’s strengths, activities, and life goals both to enhance rapport and to reference during motivational interviewing as reasons to avoid, reduce, or quit vaping. Motivational interviewing has been shown to help patients make healthier lifestyle choices by nonjudgmentally exploring their pros and cons in a conversation that takes into account readiness to change. This fits well with the stage of developing autonomy when teens want above all to make their own decisions. The cons of using can be discussed as including the effects and side effects of vaping interfering with their favored activities and moving towards their identified goals. Praising abstinence and asking them to show you how they could decline offers to vape are valuable reinforcement you can provide.
Finally, we all know that teens hate being manipulated. Vaping education we provide can make it clear that youth are being tricked by companies – most being large cigarette producers who know the dangers of vaping – into getting addicted so these companies can get rich on their money.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She has no other relevant disclosures. Dr. Howard’s contribution to this publication is as a paid expert to MDedge News. Email her at [email protected].
All pediatricians are relieved that the rates of children smoking cigarettes has dropped steadily since 2011. This decline seems to be associated with education on the dangers of cigarettes and fewer parents smoking. Perhaps less modeling of cigarette use in movies (although it increased again from 2010 to 2019) and lawsuits against advertisements targeting children also has helped.
“Whew,” we may have said, “we can relax our efforts to convince children to avoid smoking.” But, as is commonly true in medicine, the next threat was right around the corner – in this case vaping or e-cigarettes, also called vapes, e-hookahs, vape pens, tank systems, mods, and electronic nicotine delivery systems. And the size of the problem is huge – over 20% of high school students report using e-cigarettes – and immediate, as vaping can kill in the short term as well as causing long-term harm.
“E-cigarette, or vaping, product use–associated Lung Injury” – EVALI for short – has killed 68 vapers and hospitalized thousands. EVALI is thought to be caused by a vitamin E acetate additive used when vaping marijuana, particularly from informal sources like friends, family, or in-person or online dealers.
Vaping increases the risk of severe COVID-19 disease
While EVALI deaths dropped in months after being explained, the COVID-19 epidemic is now a much greater threat to vapers. Vaping increases risk of severe COVID-19 disease because of its immediate paralysis of lung cilia. Sharing vape devices and touching one’s lips while using also increase the risk of virus transmission. Vaping and smoking increase the number of ACE2 receptors to which the SARS-CoV-2 virus attaches causing the characteristic cell damage, and suppresses macrophages and neutrophils, resulting in more smokers testing positive, being twice as likely to develop a severe illness and get hospitalized because of pneumonia from COVID-19, and being less likely to recover. Unfortunately, addressing this new threat to the immediate and long-term health of our patients appears to be more complicated than for addressing smoking tobacco. First of all, vaping is much more difficult to detect than smelly cigarettes sending smoke signals from behind the garage or in the school bathrooms. Many, if not most, adults do not recognize the vaping devices when they see them, as many are tiny and some look like computer thumb drives. The aerosol emitted when in use, while containing dangerous toxins, has less odor than tobacco smoke. Vaping equipment and ads have been designed to attract youth, including linking them to sports and music events. Vaping has been advertised as a way to wean off nicotine addiction, a claim that has some scientific evidence in adults, but at a lower dose of nicotine. Warning children about the dangers of marijuana vaping has been made less credible by the rapid expansion of legalization of marijuana around the United States, eliciting “I told you it was fine” reactions from youth. And the person vaping does not know what or how much of the psychoactive components are being delivered into their bodies. One Juul pod, for example, has the equivalent in nicotine of an entire pack of 20 cigarettes. They are highly addictive, especially to the developing brain, such that youth who vape are more likely to become addicted and to smoke cigarettes in the future.
Help from federal regulation has been weak
While all 50 states ban sales to youth, adults can still buy. Food and Drug Administration limitations on kid-friendly ads, and use of sweet, fruity, and mint flavorings that are most preferred by children, apply only to new producers. The FDA does not yet regulate content of vaping solutions.
So we pediatricians are on the front line for this new threat to prevent vaping or convince youth to cut down or quit. The first step in addressing vaping is being knowledgeable about its many known and emerging health risks. It may seem obvious that the dangers of vaping microscopic particles depends on the contents. Water vapor alone is not dangerous; in fact, we prescribe it in nebulizers. Unfortunately, the contents of different vaping products vary and are not well defined in different vape products. The process of using an electric current to vaporize a substance can make it more toxic than the precursor, and teens have little idea about the substances they are inhaling. The psychoactive components vary from nicotine to tetrahydrocannabinol in varying amounts. These have the well known effects of stimulation or a high, but also the potential adverse effects of poor concentration, agitation, and even psychosis. Most e-cigarettes contain nicotine, which is highly addictive and can harm adolescent brain development, which continues into the early- to mid-20s. About two-thirds of Juul users aged 15-24 years did not know that it always contains nicotine, as do 99% of all vape solutions (Centers for Disease Control and Prevention, 2020). Earlier use of nicotine is more highly associated with later addiction to tobacco products that cause lung damage, acid reflux, insulin resistance, harm to the testes, harm to fetuses, cancer, and heart disease.
E-cigarette aerosols also contain dozens of other harmful substances besides nicotine ranging from acetone, propylene glycol, and metals to formaldehyde and ethyl benzene. These same chemicals are part of familiar toxic substances such as antifreeze, paint thinner, and pesticides. These cause ear, eye and throat irritation, and impairments in the cardiovascular system reducing athletic ability – at the least. Some flavorings in vape fluids also are toxic. Even the residual left on furniture and floors is harmful to those coming in contact, including pets.
How to encourage teens not to vaping
Trying to scare youth about health hazards is not generally effective in stopping risk behaviors since adolescence is a time of perceived singularity (it does not apply to me) and even a sense of immortality. Teens also see peers who vape as being unaffected and decide on using based on this small personal sample instead of valid statistics.
But teens do pay some attention to peer models or influencers saying why they do not use. One source of such testimony you can refer to is videos of inspiring athletes, musicians, and other “cool” young adults found on the naturalhigh.org website. You may know other examples of community teens desisting you can reference.
Parent rules, and less so advice, against smoking have been shown to be effective in deterring youth cigarette smoking. Because parents are less aware of vaping and its dangers, another step we can take is educating parents in our practices about vaping, its variable forms, its effects, and dangers, supplying authoritative materials, and advising them to talk with their children. Other steps the American Academy of Pediatrics recommends regarding smoking is for parents to be a role model of not using or try to quit, designate the house and car as smoking free, avoid children viewing smoking in media, tell their children about the side effects, and encourage their children who use to quit. Parents also can encourage schools to teach and have rules about smoking and vaping (e.g., med.stanford.edu/tobaccopreventiontoolkit.html).
Another approach we have been using is to not only screen for all substance use, but also to gather information about the teen’s strengths, activities, and life goals both to enhance rapport and to reference during motivational interviewing as reasons to avoid, reduce, or quit vaping. Motivational interviewing has been shown to help patients make healthier lifestyle choices by nonjudgmentally exploring their pros and cons in a conversation that takes into account readiness to change. This fits well with the stage of developing autonomy when teens want above all to make their own decisions. The cons of using can be discussed as including the effects and side effects of vaping interfering with their favored activities and moving towards their identified goals. Praising abstinence and asking them to show you how they could decline offers to vape are valuable reinforcement you can provide.
Finally, we all know that teens hate being manipulated. Vaping education we provide can make it clear that youth are being tricked by companies – most being large cigarette producers who know the dangers of vaping – into getting addicted so these companies can get rich on their money.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She has no other relevant disclosures. Dr. Howard’s contribution to this publication is as a paid expert to MDedge News. Email her at [email protected].
A girl presents with blotchy, slightly itchy spots on her chest, back
On close evaluation of the picture on her chest, she has pale macules and patches surrounded by erythematous ill-defined patches consistent with nevus anemicus. The findings of the picture raise the suspicion for neurofibromatosis, and it was recommended for her to be evaluated in person.
She comes several days later to the clinic. The caretaker, who is her aunt, reports she does not know much of the girl’s medical history as she recently moved from South America to live with her. The girl is a very nice and pleasant 8-year-old. She reports noticing the spots on her chest for about a year and that they seem to get a little itchier and more noticeable when she is hot or when she is running. She also reports increasing headaches for several months. She is being home schooled, and according to her aunt she is at par with her cousins who are about the same age. There is no history of seizures. She has had back surgery in the past. There is no history of hypertension. There is no family history of any genetic disorder or similar lesions.
On physical exam, her vital signs are normal, but her head circumference is over the 90th percentile. She is pleasant and interactive. On skin examination, she has slightly noticeable pale macules and patches on the chest and back that become more apparent after rubbing her skin. She has multiple light brown macules and oval patches on the chest, back, and neck. She has no axillary or inguinal freckling. She has scars on the back from her prior surgery.
As she was having worsening headaches, an MRI of the brain was ordered, which showed a left optic glioma. She was then referred to ophthalmology, neurology, and genetics.
Neurofibromatosis type 1 (NF1) is a common genetic autosomal dominant disorder cause by mutations on the NF1 gene on chromosome 17, which encodes for the protein neurofibromin. This protein works in the Ras-mitogen–activated protein kinase pathway as a negative regulator. Based on the National Institute of Health criteria, children need two or more of the following to be diagnosed with NF1: more than six café au lait macules larger than 5 mm in prepubescent children and 2.5 cm after puberty; axillary or inguinal freckling; two or more Lisch nodules; optic gliomas; two or more neurofibromas or one plexiform neurofibroma; or a first degree relative with a diagnosis of NF1. With these criteria, about 70% of the children can be diagnosed before the age of 1 year.1
Nevus anemicus is an uncommon birthmark, sometimes overlooked, that is characterized by pale, hypopigmented, well-defined macules and patches that do not turn red after trauma or changes in temperature. Nevus anemicus is usually localized on the torso but can be seen on the face, neck, and extremities. These lesions are present in 1%-2% of the general population. They are thought to occur because of increased sensitivity of the affected blood vessels to catecholamines, which causes permanent vasoconstriction, which leads to hypopigmentation on the area.2 These lesions are usually present at birth and have been described in patients with tuberous sclerosis, neurofibromatosis, and phakomatosis pigmentovascularis.
Recent studies of patients with neurofibromatosis and other RASopathies have noticed that nevus anemicus is present in about 8.8%-51% of the patients studied with a diagnosis NF1, compared with only 2% of the controls.3,4 The studies failed to report any cases of nevus anemicus in patients with other RASopathies associated with café au lait macules. Bulteel and colleagues recently reported two cases of non-NF1 RASopathies also associated with nevus anemicus in a patient with Legius syndrome and a patient with Noonan syndrome with multiple lentigines.5 The nevus anemicus was reported to occur most commonly on the anterior chest and be multiple, as seen in our patient.
The authors of the published studies advocate for the introduction of nevus anemicus as part of the diagnostic criteria for NF1, especially because it can be an early finding seen in babies, which can aid in early diagnosis of NF1.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. She has no relevant financial disclosures. Email Dr. Matiz at [email protected].
References
1. Pediatrics. 2000 Mar. doi: 10.1542/peds.105.3.608.
2. Nevus Anemicus. StatPearls [Internet] (Treasure Island, Fla.: StatPearls Publishing; 2020 Jan).
3. J Am Acad Dermatol. 2013 Nov. doi: 10.1016/j.jaad.2013.06.039.
4. Pediatr Dermatol. 2015 May-Jun. doi: 10.1111/pde.12525.
5. JAAD Case Rep. 2018 Apr 5. doi: 10.1016/j.jdcr.2017.09.037.
On close evaluation of the picture on her chest, she has pale macules and patches surrounded by erythematous ill-defined patches consistent with nevus anemicus. The findings of the picture raise the suspicion for neurofibromatosis, and it was recommended for her to be evaluated in person.
She comes several days later to the clinic. The caretaker, who is her aunt, reports she does not know much of the girl’s medical history as she recently moved from South America to live with her. The girl is a very nice and pleasant 8-year-old. She reports noticing the spots on her chest for about a year and that they seem to get a little itchier and more noticeable when she is hot or when she is running. She also reports increasing headaches for several months. She is being home schooled, and according to her aunt she is at par with her cousins who are about the same age. There is no history of seizures. She has had back surgery in the past. There is no history of hypertension. There is no family history of any genetic disorder or similar lesions.
On physical exam, her vital signs are normal, but her head circumference is over the 90th percentile. She is pleasant and interactive. On skin examination, she has slightly noticeable pale macules and patches on the chest and back that become more apparent after rubbing her skin. She has multiple light brown macules and oval patches on the chest, back, and neck. She has no axillary or inguinal freckling. She has scars on the back from her prior surgery.
As she was having worsening headaches, an MRI of the brain was ordered, which showed a left optic glioma. She was then referred to ophthalmology, neurology, and genetics.
Neurofibromatosis type 1 (NF1) is a common genetic autosomal dominant disorder cause by mutations on the NF1 gene on chromosome 17, which encodes for the protein neurofibromin. This protein works in the Ras-mitogen–activated protein kinase pathway as a negative regulator. Based on the National Institute of Health criteria, children need two or more of the following to be diagnosed with NF1: more than six café au lait macules larger than 5 mm in prepubescent children and 2.5 cm after puberty; axillary or inguinal freckling; two or more Lisch nodules; optic gliomas; two or more neurofibromas or one plexiform neurofibroma; or a first degree relative with a diagnosis of NF1. With these criteria, about 70% of the children can be diagnosed before the age of 1 year.1
Nevus anemicus is an uncommon birthmark, sometimes overlooked, that is characterized by pale, hypopigmented, well-defined macules and patches that do not turn red after trauma or changes in temperature. Nevus anemicus is usually localized on the torso but can be seen on the face, neck, and extremities. These lesions are present in 1%-2% of the general population. They are thought to occur because of increased sensitivity of the affected blood vessels to catecholamines, which causes permanent vasoconstriction, which leads to hypopigmentation on the area.2 These lesions are usually present at birth and have been described in patients with tuberous sclerosis, neurofibromatosis, and phakomatosis pigmentovascularis.
Recent studies of patients with neurofibromatosis and other RASopathies have noticed that nevus anemicus is present in about 8.8%-51% of the patients studied with a diagnosis NF1, compared with only 2% of the controls.3,4 The studies failed to report any cases of nevus anemicus in patients with other RASopathies associated with café au lait macules. Bulteel and colleagues recently reported two cases of non-NF1 RASopathies also associated with nevus anemicus in a patient with Legius syndrome and a patient with Noonan syndrome with multiple lentigines.5 The nevus anemicus was reported to occur most commonly on the anterior chest and be multiple, as seen in our patient.
The authors of the published studies advocate for the introduction of nevus anemicus as part of the diagnostic criteria for NF1, especially because it can be an early finding seen in babies, which can aid in early diagnosis of NF1.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. She has no relevant financial disclosures. Email Dr. Matiz at [email protected].
References
1. Pediatrics. 2000 Mar. doi: 10.1542/peds.105.3.608.
2. Nevus Anemicus. StatPearls [Internet] (Treasure Island, Fla.: StatPearls Publishing; 2020 Jan).
3. J Am Acad Dermatol. 2013 Nov. doi: 10.1016/j.jaad.2013.06.039.
4. Pediatr Dermatol. 2015 May-Jun. doi: 10.1111/pde.12525.
5. JAAD Case Rep. 2018 Apr 5. doi: 10.1016/j.jdcr.2017.09.037.
On close evaluation of the picture on her chest, she has pale macules and patches surrounded by erythematous ill-defined patches consistent with nevus anemicus. The findings of the picture raise the suspicion for neurofibromatosis, and it was recommended for her to be evaluated in person.
She comes several days later to the clinic. The caretaker, who is her aunt, reports she does not know much of the girl’s medical history as she recently moved from South America to live with her. The girl is a very nice and pleasant 8-year-old. She reports noticing the spots on her chest for about a year and that they seem to get a little itchier and more noticeable when she is hot or when she is running. She also reports increasing headaches for several months. She is being home schooled, and according to her aunt she is at par with her cousins who are about the same age. There is no history of seizures. She has had back surgery in the past. There is no history of hypertension. There is no family history of any genetic disorder or similar lesions.
On physical exam, her vital signs are normal, but her head circumference is over the 90th percentile. She is pleasant and interactive. On skin examination, she has slightly noticeable pale macules and patches on the chest and back that become more apparent after rubbing her skin. She has multiple light brown macules and oval patches on the chest, back, and neck. She has no axillary or inguinal freckling. She has scars on the back from her prior surgery.
As she was having worsening headaches, an MRI of the brain was ordered, which showed a left optic glioma. She was then referred to ophthalmology, neurology, and genetics.
Neurofibromatosis type 1 (NF1) is a common genetic autosomal dominant disorder cause by mutations on the NF1 gene on chromosome 17, which encodes for the protein neurofibromin. This protein works in the Ras-mitogen–activated protein kinase pathway as a negative regulator. Based on the National Institute of Health criteria, children need two or more of the following to be diagnosed with NF1: more than six café au lait macules larger than 5 mm in prepubescent children and 2.5 cm after puberty; axillary or inguinal freckling; two or more Lisch nodules; optic gliomas; two or more neurofibromas or one plexiform neurofibroma; or a first degree relative with a diagnosis of NF1. With these criteria, about 70% of the children can be diagnosed before the age of 1 year.1
Nevus anemicus is an uncommon birthmark, sometimes overlooked, that is characterized by pale, hypopigmented, well-defined macules and patches that do not turn red after trauma or changes in temperature. Nevus anemicus is usually localized on the torso but can be seen on the face, neck, and extremities. These lesions are present in 1%-2% of the general population. They are thought to occur because of increased sensitivity of the affected blood vessels to catecholamines, which causes permanent vasoconstriction, which leads to hypopigmentation on the area.2 These lesions are usually present at birth and have been described in patients with tuberous sclerosis, neurofibromatosis, and phakomatosis pigmentovascularis.
Recent studies of patients with neurofibromatosis and other RASopathies have noticed that nevus anemicus is present in about 8.8%-51% of the patients studied with a diagnosis NF1, compared with only 2% of the controls.3,4 The studies failed to report any cases of nevus anemicus in patients with other RASopathies associated with café au lait macules. Bulteel and colleagues recently reported two cases of non-NF1 RASopathies also associated with nevus anemicus in a patient with Legius syndrome and a patient with Noonan syndrome with multiple lentigines.5 The nevus anemicus was reported to occur most commonly on the anterior chest and be multiple, as seen in our patient.
The authors of the published studies advocate for the introduction of nevus anemicus as part of the diagnostic criteria for NF1, especially because it can be an early finding seen in babies, which can aid in early diagnosis of NF1.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. She has no relevant financial disclosures. Email Dr. Matiz at [email protected].
References
1. Pediatrics. 2000 Mar. doi: 10.1542/peds.105.3.608.
2. Nevus Anemicus. StatPearls [Internet] (Treasure Island, Fla.: StatPearls Publishing; 2020 Jan).
3. J Am Acad Dermatol. 2013 Nov. doi: 10.1016/j.jaad.2013.06.039.
4. Pediatr Dermatol. 2015 May-Jun. doi: 10.1111/pde.12525.
5. JAAD Case Rep. 2018 Apr 5. doi: 10.1016/j.jdcr.2017.09.037.
















