User login
Official Newspaper of the American College of Surgeons
Point/Counterpoint: Should FEVAR be used for a short neck?
FEVAR is generally the best option
The advent of endovascular aortic aneurysm repair (EVAR) has steadily become the standard of care in the management of infrarenal abdominal aortic aneurysms (AAAs). In fact, it has now surpassed open surgical repair and is the predominant therapeutic modality in managing this disease entity. Clearly, there are specific anatomic and technical factors that may preclude the use of traditional EVAR – most notably, challenging proximal neck anatomy, be it insufficient length or severe angulation.
It is estimated that up to 30%-40% of patients are unsuitable candidates because of these concerns.1 Such patients are thus relegated to traditional open repair with the associated concerns for supravisceral clamping, including dramatic changes in hemodynamics and prolonged ICU and hospital stays.
Open surgical repair of pararenal, juxtarenal, and suprarenal AAAs is tried, tested, and durable. Knott and the group from Mayo Clinic reviewed their repair of 126 consecutive elective juxtarenal AAAs requiring suprarenal aortic clamping noting a 30-day mortality of .8%.2 More recent data from Kabbani and the Henry Ford group involved their 27-year clinical experience suggesting that open repair of complex proximal aortic aneurysms can be performed with clinical outcomes that are similar to those of open infrarenal repair.3 I respectfully accept this traditional – and historic – treatment modality.
However, we vascular surgeons are progressive and resilient in our quest to innovate and modernize – some of us even modified the traditional endografts on the back table. We charged forward despite the initial paucity of data on infrarenal EVAR compared to traditional open repair of aneurysms in the past. Now, a large percentage of infrarenal AAA repairs are performed via EVAR. In fact, our steadfast progression to advanced endovascular techniques has raised the concern that our graduating trainees are no longer proficient, competent, or even capable, in open complex aneurysm repair!
Tsilimparis and colleagues reported the first outcomes comparing open repair and FEVAR.4 They queried the NSQIP database comparing 1,091 patients undergoing open repair with 264 in the FEVAR group. There was an increased risk of morbidity in all combined endpoints including pulmonary and cardiovascular complications as well as length of stay in patients undergoing the open repair group. A larger comprehensive review pooled the results from 8 FEVAR and 12 open repair series. Analysis of the data found the groups to be identical. Open repair, however, was found to have an increased 30-day mortality when compared to FEVAR (relative risk 1.03, 2% increased absolute mortality).5
Gupta and colleagues reported the latest multi-institutional data noting that open repair was associated with higher risk than FEVAR for 30-day mortality, cardiac and pulmonary complications, renal failure requiring dialysis, return to the operating room, and in this age of cost-containment, length of stay (2 days vs. 7 days; P less than .0001).6
A further study by Donas and colleagues evaluated 90 consecutive patients with primary degenerative juxtarenal AAAs to different operative strategies based on morphologic and clinical characteristics – 29 FEVAR, 30 chEVAR, and 31 open repair.7 Early procedure-related and all-cause 30-day mortality was 0% in the endovascular group and 6.4% in the open group.
Although open repair for juxtarenal AAAs is the gold standard, short- and mid-term data on the outcomes for complex endovascular repair are excellent. Data on long-term durability, graft fixation/migration as well as the integrity of the graft and concerns for endoleaks and branch vessel patency, however, are limited. We do not have long-term data because we have not been doing these newer procedures for that long – but the data thus far show great promise.
We need to continue to challenge the status quo, particularly when the current data are satisfactory and the procedure feasible. With our continued appraisal of the data we publish as vascular surgeons, we can then identify if these innovations and techniques will withstand the test of time. After all, we are vascular surgeons (particularly those of us who have trained extensively in open repair) – and if open repair is necessary, then we will be ready.
But, if I can avoid a thoracoabdominal incision for a few percutaneous access sites, then sign me up!
Dr. Mouawad is chief of vascular and endovascular surgery, medical director of the vascular laboratory, and vice-chair of the department of surgery at McLaren Bay Region, Bay City, Mich. He is assistant professor of surgery at Michigan State University and Central Michigan University.
References
1. Perspect Vasc Surg Endovasc Ther. 2009;21:13-8.
2. J Vasc Surg. 2008;47:695-701.
3. J Vasc Surg. 2014;59:1488-94.
4. Ann Vasc Surg. 2013;27(3):267-73.
5. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
6. J Vasc Surg. 2017 Dec;66(6):1653-8.
7. J Vasc Surg. 2012 Aug;56(2):285-90.
FEVAR may not be the best choice
Over the past 3 decades, EVAR, with its very low periprocedural morbidity and mortality, and satisfactory long-term results, has become the primary treatment modality for the majority of infrarenal AAAs. The success of stent grafts for the repair of AAA relies heavily on satisfactory proximal and distal seal zones. Each commercially available standard EVAR graft has a manufacturer’s instructions for use requiring a proximal landing zone length of between 10 and 15 mm. Patients with less than this required length are considered to have “short necks.” Evaluation of this group of patients has demonstrated that this is not an uncommon finding and that EVAR performed outside the instructions for use has been associated with an increased risk of intraoperative failure, aneurysm expansion, and later complications.1-3
Current treatment options for patients with short necks include open surgical repair (OSR), FEVAR, and EVAR with the chimney graft technique (Ch-EVAR).
Thus, current knowledge acquired from case series, registries, and clinical experience must be used in deciding which therapeutic option to offer patients. Relevant factors influencing this decision include the availability and adaptability of the technique, early outcomes including technical success, morbidity and mortality, and late outcomes including survival, need for reintervention, and other late morbidity. Finally, in an era of value-based medical care, cost also must be considered.
Currently there is only one Food and Drug Administration–approved fenestrated graft. When used in properly selected patients, excellent periprocedural results have been reported approaching those of standard EVAR. However, there are limitations in both the availability and adaptability of FEVAR. These grafts are custom made for each patient, often requiring several weeks of lead time. Adaptability also has its limitations, including access vessels, severe neck angulation, calcification, mural thrombus, and branch vessel size, number, location, and associated arterial disease. Any of these factors may preclude the use of this technology. Open repair, on the other hand, is not limited by graft availability and allows for custom modification for each patient’s specific disease morphology. The essential limitation for open repair is the patient’s physiological ability to withstand the operation.
Several studies attempting to compare the early outcomes of FEVAR versus comparable patients undergoing OSR of similar aneurysms have reported significantly lower 30-day mortality and major morbidity rates for FEVAR.4,5 However, Rao et al., in a recent systematic review and meta-analysis that included data on 2,326 patients from 35 case series reporting on elective repair of juxtarenal aneurysms by either OSR or FEVAR, found perioperative mortality to not be significantly different (4.1% for both). Also, no significant difference was found between the two groups when evaluating postoperative renal insufficiency and need for permanent dialysis. However, OSR did have significantly higher major complication rates (25% vs. 15.7%).6 These findings suggest that both modalities can be performed successfully, but that long term outcomes need to be considered to determine if the increased initial morbidity of OSR is justified by differences in long term results between the two modalities.
Open surgical repair of juxtarenal AAA has been shown to be a durable repair.7 While early and even intermediate results of FEVAR appear to be satisfactory, long-term durability has yet to be determined.4,8 Along with continuing to exclude the aneurysm sac, as with standard EVAR, there is the additional concern regarding the outcome of the organs supplied by the fenestrated/stent-grafted branches with FEVAR. Longer-term follow-up in the same review by Rao et al. showed that significantly more FEVAR patients developed renal failure compared with OSR patients (19.7% vs. 7.7%). FEVAR patients also had a higher rate of reintervention.
And finally, long-term survival was significantly greater in OSR patients compared to FEVAR at 3 and 5 years (80% vs. 74% vs. 73% vs. 55%). These authors concluded that open repair remains the gold standard while FEVAR is a favorable option for high risk patients.6
These new and innovative stent graft devices come at considerable expense. While this aspect of FEVAR has not been extensively studied, Michel et al., in their report from the multicenter prospective Windows registry, attempted to evaluate the economic aspect of FEVAR. They compared a group of patients who underwent FEVAR to patients from a large national hospital discharge database who underwent OSR. No difference in 30-day mortality was noted between these two groups; however, there was a significantly greater cost with FEVAR. The authors concluded that FEVAR did not appear to be justified for patients fit for open surgery with juxtarenal AAA.9
For now, the roles of OSR and FEVAR would appear to be complementary. Current evidence suggests that OSR is the most appropriate intervention for good risk patients with an anticipated longer life expectancy. Patients with appropriate anatomy for FEVAR and who are at higher risk for open repair would benefit from FEVAR. As further experience and outcomes are accumulated, our ability to select the appropriate therapy for individual patients should improve.
Dr. Weaver is an assistant clinical professor for surgery at Wayne State School of Medicine, Detroit, and an attending in the division of vascular surgery, Henry Ford Hospital.
References
1. Ir J Med Sci. 2015;184(1):249-55.
2. Circulation. 2011;123(24):2848-55.
3. J Endovasc Therapy. 2001;8(5):457-64.
4. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
5. Ann Vasc Surg. 2013;27(3):267-73.
6. J Vasc Surg. 2015;61(1):242-55.
7. J Vasc Surg. 2012;56(1):2-7.
8. J Cardiovasc Surg. 2015;56(3):331-7.
9. Eur J Vasc Endovasc Surg. 2015;50(2):189-96.
FEVAR is generally the best option
The advent of endovascular aortic aneurysm repair (EVAR) has steadily become the standard of care in the management of infrarenal abdominal aortic aneurysms (AAAs). In fact, it has now surpassed open surgical repair and is the predominant therapeutic modality in managing this disease entity. Clearly, there are specific anatomic and technical factors that may preclude the use of traditional EVAR – most notably, challenging proximal neck anatomy, be it insufficient length or severe angulation.
It is estimated that up to 30%-40% of patients are unsuitable candidates because of these concerns.1 Such patients are thus relegated to traditional open repair with the associated concerns for supravisceral clamping, including dramatic changes in hemodynamics and prolonged ICU and hospital stays.
Open surgical repair of pararenal, juxtarenal, and suprarenal AAAs is tried, tested, and durable. Knott and the group from Mayo Clinic reviewed their repair of 126 consecutive elective juxtarenal AAAs requiring suprarenal aortic clamping noting a 30-day mortality of .8%.2 More recent data from Kabbani and the Henry Ford group involved their 27-year clinical experience suggesting that open repair of complex proximal aortic aneurysms can be performed with clinical outcomes that are similar to those of open infrarenal repair.3 I respectfully accept this traditional – and historic – treatment modality.
However, we vascular surgeons are progressive and resilient in our quest to innovate and modernize – some of us even modified the traditional endografts on the back table. We charged forward despite the initial paucity of data on infrarenal EVAR compared to traditional open repair of aneurysms in the past. Now, a large percentage of infrarenal AAA repairs are performed via EVAR. In fact, our steadfast progression to advanced endovascular techniques has raised the concern that our graduating trainees are no longer proficient, competent, or even capable, in open complex aneurysm repair!
Tsilimparis and colleagues reported the first outcomes comparing open repair and FEVAR.4 They queried the NSQIP database comparing 1,091 patients undergoing open repair with 264 in the FEVAR group. There was an increased risk of morbidity in all combined endpoints including pulmonary and cardiovascular complications as well as length of stay in patients undergoing the open repair group. A larger comprehensive review pooled the results from 8 FEVAR and 12 open repair series. Analysis of the data found the groups to be identical. Open repair, however, was found to have an increased 30-day mortality when compared to FEVAR (relative risk 1.03, 2% increased absolute mortality).5
Gupta and colleagues reported the latest multi-institutional data noting that open repair was associated with higher risk than FEVAR for 30-day mortality, cardiac and pulmonary complications, renal failure requiring dialysis, return to the operating room, and in this age of cost-containment, length of stay (2 days vs. 7 days; P less than .0001).6
A further study by Donas and colleagues evaluated 90 consecutive patients with primary degenerative juxtarenal AAAs to different operative strategies based on morphologic and clinical characteristics – 29 FEVAR, 30 chEVAR, and 31 open repair.7 Early procedure-related and all-cause 30-day mortality was 0% in the endovascular group and 6.4% in the open group.
Although open repair for juxtarenal AAAs is the gold standard, short- and mid-term data on the outcomes for complex endovascular repair are excellent. Data on long-term durability, graft fixation/migration as well as the integrity of the graft and concerns for endoleaks and branch vessel patency, however, are limited. We do not have long-term data because we have not been doing these newer procedures for that long – but the data thus far show great promise.
We need to continue to challenge the status quo, particularly when the current data are satisfactory and the procedure feasible. With our continued appraisal of the data we publish as vascular surgeons, we can then identify if these innovations and techniques will withstand the test of time. After all, we are vascular surgeons (particularly those of us who have trained extensively in open repair) – and if open repair is necessary, then we will be ready.
But, if I can avoid a thoracoabdominal incision for a few percutaneous access sites, then sign me up!
Dr. Mouawad is chief of vascular and endovascular surgery, medical director of the vascular laboratory, and vice-chair of the department of surgery at McLaren Bay Region, Bay City, Mich. He is assistant professor of surgery at Michigan State University and Central Michigan University.
References
1. Perspect Vasc Surg Endovasc Ther. 2009;21:13-8.
2. J Vasc Surg. 2008;47:695-701.
3. J Vasc Surg. 2014;59:1488-94.
4. Ann Vasc Surg. 2013;27(3):267-73.
5. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
6. J Vasc Surg. 2017 Dec;66(6):1653-8.
7. J Vasc Surg. 2012 Aug;56(2):285-90.
FEVAR may not be the best choice
Over the past 3 decades, EVAR, with its very low periprocedural morbidity and mortality, and satisfactory long-term results, has become the primary treatment modality for the majority of infrarenal AAAs. The success of stent grafts for the repair of AAA relies heavily on satisfactory proximal and distal seal zones. Each commercially available standard EVAR graft has a manufacturer’s instructions for use requiring a proximal landing zone length of between 10 and 15 mm. Patients with less than this required length are considered to have “short necks.” Evaluation of this group of patients has demonstrated that this is not an uncommon finding and that EVAR performed outside the instructions for use has been associated with an increased risk of intraoperative failure, aneurysm expansion, and later complications.1-3
Current treatment options for patients with short necks include open surgical repair (OSR), FEVAR, and EVAR with the chimney graft technique (Ch-EVAR).
Thus, current knowledge acquired from case series, registries, and clinical experience must be used in deciding which therapeutic option to offer patients. Relevant factors influencing this decision include the availability and adaptability of the technique, early outcomes including technical success, morbidity and mortality, and late outcomes including survival, need for reintervention, and other late morbidity. Finally, in an era of value-based medical care, cost also must be considered.
Currently there is only one Food and Drug Administration–approved fenestrated graft. When used in properly selected patients, excellent periprocedural results have been reported approaching those of standard EVAR. However, there are limitations in both the availability and adaptability of FEVAR. These grafts are custom made for each patient, often requiring several weeks of lead time. Adaptability also has its limitations, including access vessels, severe neck angulation, calcification, mural thrombus, and branch vessel size, number, location, and associated arterial disease. Any of these factors may preclude the use of this technology. Open repair, on the other hand, is not limited by graft availability and allows for custom modification for each patient’s specific disease morphology. The essential limitation for open repair is the patient’s physiological ability to withstand the operation.
Several studies attempting to compare the early outcomes of FEVAR versus comparable patients undergoing OSR of similar aneurysms have reported significantly lower 30-day mortality and major morbidity rates for FEVAR.4,5 However, Rao et al., in a recent systematic review and meta-analysis that included data on 2,326 patients from 35 case series reporting on elective repair of juxtarenal aneurysms by either OSR or FEVAR, found perioperative mortality to not be significantly different (4.1% for both). Also, no significant difference was found between the two groups when evaluating postoperative renal insufficiency and need for permanent dialysis. However, OSR did have significantly higher major complication rates (25% vs. 15.7%).6 These findings suggest that both modalities can be performed successfully, but that long term outcomes need to be considered to determine if the increased initial morbidity of OSR is justified by differences in long term results between the two modalities.
Open surgical repair of juxtarenal AAA has been shown to be a durable repair.7 While early and even intermediate results of FEVAR appear to be satisfactory, long-term durability has yet to be determined.4,8 Along with continuing to exclude the aneurysm sac, as with standard EVAR, there is the additional concern regarding the outcome of the organs supplied by the fenestrated/stent-grafted branches with FEVAR. Longer-term follow-up in the same review by Rao et al. showed that significantly more FEVAR patients developed renal failure compared with OSR patients (19.7% vs. 7.7%). FEVAR patients also had a higher rate of reintervention.
And finally, long-term survival was significantly greater in OSR patients compared to FEVAR at 3 and 5 years (80% vs. 74% vs. 73% vs. 55%). These authors concluded that open repair remains the gold standard while FEVAR is a favorable option for high risk patients.6
These new and innovative stent graft devices come at considerable expense. While this aspect of FEVAR has not been extensively studied, Michel et al., in their report from the multicenter prospective Windows registry, attempted to evaluate the economic aspect of FEVAR. They compared a group of patients who underwent FEVAR to patients from a large national hospital discharge database who underwent OSR. No difference in 30-day mortality was noted between these two groups; however, there was a significantly greater cost with FEVAR. The authors concluded that FEVAR did not appear to be justified for patients fit for open surgery with juxtarenal AAA.9
For now, the roles of OSR and FEVAR would appear to be complementary. Current evidence suggests that OSR is the most appropriate intervention for good risk patients with an anticipated longer life expectancy. Patients with appropriate anatomy for FEVAR and who are at higher risk for open repair would benefit from FEVAR. As further experience and outcomes are accumulated, our ability to select the appropriate therapy for individual patients should improve.
Dr. Weaver is an assistant clinical professor for surgery at Wayne State School of Medicine, Detroit, and an attending in the division of vascular surgery, Henry Ford Hospital.
References
1. Ir J Med Sci. 2015;184(1):249-55.
2. Circulation. 2011;123(24):2848-55.
3. J Endovasc Therapy. 2001;8(5):457-64.
4. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
5. Ann Vasc Surg. 2013;27(3):267-73.
6. J Vasc Surg. 2015;61(1):242-55.
7. J Vasc Surg. 2012;56(1):2-7.
8. J Cardiovasc Surg. 2015;56(3):331-7.
9. Eur J Vasc Endovasc Surg. 2015;50(2):189-96.
FEVAR is generally the best option
The advent of endovascular aortic aneurysm repair (EVAR) has steadily become the standard of care in the management of infrarenal abdominal aortic aneurysms (AAAs). In fact, it has now surpassed open surgical repair and is the predominant therapeutic modality in managing this disease entity. Clearly, there are specific anatomic and technical factors that may preclude the use of traditional EVAR – most notably, challenging proximal neck anatomy, be it insufficient length or severe angulation.
It is estimated that up to 30%-40% of patients are unsuitable candidates because of these concerns.1 Such patients are thus relegated to traditional open repair with the associated concerns for supravisceral clamping, including dramatic changes in hemodynamics and prolonged ICU and hospital stays.
Open surgical repair of pararenal, juxtarenal, and suprarenal AAAs is tried, tested, and durable. Knott and the group from Mayo Clinic reviewed their repair of 126 consecutive elective juxtarenal AAAs requiring suprarenal aortic clamping noting a 30-day mortality of .8%.2 More recent data from Kabbani and the Henry Ford group involved their 27-year clinical experience suggesting that open repair of complex proximal aortic aneurysms can be performed with clinical outcomes that are similar to those of open infrarenal repair.3 I respectfully accept this traditional – and historic – treatment modality.
However, we vascular surgeons are progressive and resilient in our quest to innovate and modernize – some of us even modified the traditional endografts on the back table. We charged forward despite the initial paucity of data on infrarenal EVAR compared to traditional open repair of aneurysms in the past. Now, a large percentage of infrarenal AAA repairs are performed via EVAR. In fact, our steadfast progression to advanced endovascular techniques has raised the concern that our graduating trainees are no longer proficient, competent, or even capable, in open complex aneurysm repair!
Tsilimparis and colleagues reported the first outcomes comparing open repair and FEVAR.4 They queried the NSQIP database comparing 1,091 patients undergoing open repair with 264 in the FEVAR group. There was an increased risk of morbidity in all combined endpoints including pulmonary and cardiovascular complications as well as length of stay in patients undergoing the open repair group. A larger comprehensive review pooled the results from 8 FEVAR and 12 open repair series. Analysis of the data found the groups to be identical. Open repair, however, was found to have an increased 30-day mortality when compared to FEVAR (relative risk 1.03, 2% increased absolute mortality).5
Gupta and colleagues reported the latest multi-institutional data noting that open repair was associated with higher risk than FEVAR for 30-day mortality, cardiac and pulmonary complications, renal failure requiring dialysis, return to the operating room, and in this age of cost-containment, length of stay (2 days vs. 7 days; P less than .0001).6
A further study by Donas and colleagues evaluated 90 consecutive patients with primary degenerative juxtarenal AAAs to different operative strategies based on morphologic and clinical characteristics – 29 FEVAR, 30 chEVAR, and 31 open repair.7 Early procedure-related and all-cause 30-day mortality was 0% in the endovascular group and 6.4% in the open group.
Although open repair for juxtarenal AAAs is the gold standard, short- and mid-term data on the outcomes for complex endovascular repair are excellent. Data on long-term durability, graft fixation/migration as well as the integrity of the graft and concerns for endoleaks and branch vessel patency, however, are limited. We do not have long-term data because we have not been doing these newer procedures for that long – but the data thus far show great promise.
We need to continue to challenge the status quo, particularly when the current data are satisfactory and the procedure feasible. With our continued appraisal of the data we publish as vascular surgeons, we can then identify if these innovations and techniques will withstand the test of time. After all, we are vascular surgeons (particularly those of us who have trained extensively in open repair) – and if open repair is necessary, then we will be ready.
But, if I can avoid a thoracoabdominal incision for a few percutaneous access sites, then sign me up!
Dr. Mouawad is chief of vascular and endovascular surgery, medical director of the vascular laboratory, and vice-chair of the department of surgery at McLaren Bay Region, Bay City, Mich. He is assistant professor of surgery at Michigan State University and Central Michigan University.
References
1. Perspect Vasc Surg Endovasc Ther. 2009;21:13-8.
2. J Vasc Surg. 2008;47:695-701.
3. J Vasc Surg. 2014;59:1488-94.
4. Ann Vasc Surg. 2013;27(3):267-73.
5. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
6. J Vasc Surg. 2017 Dec;66(6):1653-8.
7. J Vasc Surg. 2012 Aug;56(2):285-90.
FEVAR may not be the best choice
Over the past 3 decades, EVAR, with its very low periprocedural morbidity and mortality, and satisfactory long-term results, has become the primary treatment modality for the majority of infrarenal AAAs. The success of stent grafts for the repair of AAA relies heavily on satisfactory proximal and distal seal zones. Each commercially available standard EVAR graft has a manufacturer’s instructions for use requiring a proximal landing zone length of between 10 and 15 mm. Patients with less than this required length are considered to have “short necks.” Evaluation of this group of patients has demonstrated that this is not an uncommon finding and that EVAR performed outside the instructions for use has been associated with an increased risk of intraoperative failure, aneurysm expansion, and later complications.1-3
Current treatment options for patients with short necks include open surgical repair (OSR), FEVAR, and EVAR with the chimney graft technique (Ch-EVAR).
Thus, current knowledge acquired from case series, registries, and clinical experience must be used in deciding which therapeutic option to offer patients. Relevant factors influencing this decision include the availability and adaptability of the technique, early outcomes including technical success, morbidity and mortality, and late outcomes including survival, need for reintervention, and other late morbidity. Finally, in an era of value-based medical care, cost also must be considered.
Currently there is only one Food and Drug Administration–approved fenestrated graft. When used in properly selected patients, excellent periprocedural results have been reported approaching those of standard EVAR. However, there are limitations in both the availability and adaptability of FEVAR. These grafts are custom made for each patient, often requiring several weeks of lead time. Adaptability also has its limitations, including access vessels, severe neck angulation, calcification, mural thrombus, and branch vessel size, number, location, and associated arterial disease. Any of these factors may preclude the use of this technology. Open repair, on the other hand, is not limited by graft availability and allows for custom modification for each patient’s specific disease morphology. The essential limitation for open repair is the patient’s physiological ability to withstand the operation.
Several studies attempting to compare the early outcomes of FEVAR versus comparable patients undergoing OSR of similar aneurysms have reported significantly lower 30-day mortality and major morbidity rates for FEVAR.4,5 However, Rao et al., in a recent systematic review and meta-analysis that included data on 2,326 patients from 35 case series reporting on elective repair of juxtarenal aneurysms by either OSR or FEVAR, found perioperative mortality to not be significantly different (4.1% for both). Also, no significant difference was found between the two groups when evaluating postoperative renal insufficiency and need for permanent dialysis. However, OSR did have significantly higher major complication rates (25% vs. 15.7%).6 These findings suggest that both modalities can be performed successfully, but that long term outcomes need to be considered to determine if the increased initial morbidity of OSR is justified by differences in long term results between the two modalities.
Open surgical repair of juxtarenal AAA has been shown to be a durable repair.7 While early and even intermediate results of FEVAR appear to be satisfactory, long-term durability has yet to be determined.4,8 Along with continuing to exclude the aneurysm sac, as with standard EVAR, there is the additional concern regarding the outcome of the organs supplied by the fenestrated/stent-grafted branches with FEVAR. Longer-term follow-up in the same review by Rao et al. showed that significantly more FEVAR patients developed renal failure compared with OSR patients (19.7% vs. 7.7%). FEVAR patients also had a higher rate of reintervention.
And finally, long-term survival was significantly greater in OSR patients compared to FEVAR at 3 and 5 years (80% vs. 74% vs. 73% vs. 55%). These authors concluded that open repair remains the gold standard while FEVAR is a favorable option for high risk patients.6
These new and innovative stent graft devices come at considerable expense. While this aspect of FEVAR has not been extensively studied, Michel et al., in their report from the multicenter prospective Windows registry, attempted to evaluate the economic aspect of FEVAR. They compared a group of patients who underwent FEVAR to patients from a large national hospital discharge database who underwent OSR. No difference in 30-day mortality was noted between these two groups; however, there was a significantly greater cost with FEVAR. The authors concluded that FEVAR did not appear to be justified for patients fit for open surgery with juxtarenal AAA.9
For now, the roles of OSR and FEVAR would appear to be complementary. Current evidence suggests that OSR is the most appropriate intervention for good risk patients with an anticipated longer life expectancy. Patients with appropriate anatomy for FEVAR and who are at higher risk for open repair would benefit from FEVAR. As further experience and outcomes are accumulated, our ability to select the appropriate therapy for individual patients should improve.
Dr. Weaver is an assistant clinical professor for surgery at Wayne State School of Medicine, Detroit, and an attending in the division of vascular surgery, Henry Ford Hospital.
References
1. Ir J Med Sci. 2015;184(1):249-55.
2. Circulation. 2011;123(24):2848-55.
3. J Endovasc Therapy. 2001;8(5):457-64.
4. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
5. Ann Vasc Surg. 2013;27(3):267-73.
6. J Vasc Surg. 2015;61(1):242-55.
7. J Vasc Surg. 2012;56(1):2-7.
8. J Cardiovasc Surg. 2015;56(3):331-7.
9. Eur J Vasc Endovasc Surg. 2015;50(2):189-96.
EndoPredict results reflected tumor response to neoadjuvant therapy
SAN ANTONIO – The results of the EndoPredict test appear to predict tumor response in patients with early hormone receptor–positive, HER2-negative breast cancer given neoadjuvant therapy, based on results of a study conducted by the Austrian Breast & Colorectal Cancer Study Group (ABCSG).
“Very good tumor shrinkage in estrogen receptor–positive, HER2-negative disease is going to happen only in a minority of patients, and biomarkers that would predict excellent tumor shrinkage are an unmet medical need,” commented lead investigator Peter Dubsky, MD, PhD, who is head of the Breast Center at Hirslanden Klinik St. Anna, Lucerne, Switzerland. “As a surgeon, that would help me to predict breast conservation at diagnosis, but as a surgical oncologist, I would also recognize that tumor response is an important component of future survival.”
The ABCSG findings suggest expanded utility for EndoPredict. The test’s molecular score is currently used along with tumor size and nodal status to predict the 10-year distant recurrence rate, and whether patients may safely forgo chemotherapy or are at high risk and may need adjuvant chemotherapy in addition to endocrine therapy.
Dr. Dubsky and his coinvestigators assessed performance of the EndoPredict test among 217 patients treated on ABCSG 34, a randomized phase 2 neoadjuvant trial. Findings showed that among patients given neoadjuvant endocrine therapy because they had less aggressive disease features, an EndoPredict high-risk result was associated with poor response (negative predictive value of 92%), defined as a residual cancer burden (RCB) of II or III, he reported at the San Antonio Breast Cancer Symposium.
On the other hand, among patients given neoadjuvant chemotherapy because they had more aggressive disease features, a low-risk result was associated with poor response (negative predictive value of 100%).
“Clinicians really gave us two distinct cohorts within ABCSG 34. In the luminal A–type patients who were treated with neoendocrine therapy, a high EndoPredict score predicted a low chance of tumor shrinkage. In the more aggressive ER-positive tumors, so-called luminal B type, treated with neoadjuvant chemotherapy, there was absolutely no excellent response in the low-risk group,” Dr. Dubsky summarized. “We believe that this molecular score may contribute to patient selection for biomarker-driven studies, especially in the neoadjuvant setting.”
Session attendee Steven Vogl, MD, a medical oncologist with the Montefiore Medical Center in New York, commented, “I have trouble correlating an RCB of 0 or I with what you as a surgeon do for the patient, because you are talking about pathologic complete response or just a few cells there. That’s not what determines how much breast you take off: It’s determined by the total size of the tumor and the size of the breast. So if it’s less than a few centimeters, I’m sure you can do a lumpectomy in every patient. Tell me why I should care that you are getting an RCB of 0 or I in these endocrine patients.”
“Because it’s more likely that these patients will have a smaller tumor and better tumor shrinkage,” Dr. Dubsky replied. “You are of course right, RCB 0 or I was not designed to help surgeons. But it helps me as a translational scientist to have a surrogate and an exact classification for good tumor shrinkage. That’s how I used it.”
C. Kent Osborne, MD, codirector of SABCS and director of the Dan L. Duncan Cancer Center at Baylor College of Medicine in Houston, asked, “We see it in the clinic, and I’m sure you have as well, patients whose tumor doesn’t shrink very much, but the Ki-67 really drops. And that may or may not be a better factor than the actual tumor shrinkage. So how many patients who had tumors that didn’t shrink, which was your endpoint, had a reduction in Ki-67 that was, say, 5%?”
“We haven’t looked at that specifically, but we will do so as we carry on with the follow-up of these patients. Then we can learn more about the prognosis,” Dr. Dubsky replied.
Study details
ABCSG 34 was a randomized phase 2 trial testing addition of the cancer vaccine tecemotide (Stimuvax) to neoadjuvant standard of care among patients with HER2-negative early breast cancer.
Dr. Dubsky and coinvestigators restricted analyses to patients with hormone receptor–positive disease who, depending on clinical and pathologic factors, received neoadjuvant chemotherapy (eight cycles of epirubicin-cyclophosphamide and docetaxel) or neoadjuvant endocrine therapy (6 months of letrozole [Femara]) as standard of care. They were then randomized to additionally receive tecemotide or not before undergoing surgery.
Overall, 25% of the 134 patients in the neoadjuvant chemotherapy group had a good tumor response, defined as pathologic complete response in both breast and nodes (RCB of 0) or minimal residual disease (RCB of I).
Higher EndoPredict score was associated with greater likelihood of good response to chemotherapy. EndoPredict risk group (high vs. low) had a negative predictive value of 100%, a positive predictive value of 26.4%, a true-positive rate of 100%, and a true-negative rate of 8.9% for predicting response (P = .112).
Area under the receiver operating characteristic curve was 0.736.
In a multivariate model, EndoPredict score as a continuous variable was not an independent predictor of response. “The good response was largely driven by covariates that included cell proliferation, and it was Ki-67 that was significant,” Dr. Dubsky noted.
Overall, 18% of the 83 patients in the neoadjuvant endocrine therapy group had a good tumor response (RCB of 0 or I). Here, lower EndoPredict score was associated with greater likelihood of good response. EndoPredict risk group (high vs. low) had a negative predictive value of 92.3%, a positive predictive value of 27.3%, a true-positive rate of 80.0%, and a true-negative rate of 52.9% for predicting response (P = .024). Area under the curve was 0.726.
In a multivariate model here, EndoPredict score as a continuous variable, its estrogen receptor–signaling/differentiation component, and Ki-67 did not independently predict response. “It was maybe a bit surprising that T stage was the strongest factor, possibly indicating that we should have simply treated those women longer than 6 months,” Dr. Dubsky commented. The EndoPredict proliferation component was also a significant predictor.
“Possibly, the very narrow distribution of Ki-67 [among patients given neoendocrine therapy] may have prevented this factor from playing a bigger role in this particular model,” he speculated.
Dr. Dubsky disclosed that he receives consulting fees from Myriad, the maker of EndoPredict, and from Cepheid, Nanostring, and Amgen.
SOURCE: Dubsky P et al. SABCS 2017 Abstract GS6-04.
SAN ANTONIO – The results of the EndoPredict test appear to predict tumor response in patients with early hormone receptor–positive, HER2-negative breast cancer given neoadjuvant therapy, based on results of a study conducted by the Austrian Breast & Colorectal Cancer Study Group (ABCSG).
“Very good tumor shrinkage in estrogen receptor–positive, HER2-negative disease is going to happen only in a minority of patients, and biomarkers that would predict excellent tumor shrinkage are an unmet medical need,” commented lead investigator Peter Dubsky, MD, PhD, who is head of the Breast Center at Hirslanden Klinik St. Anna, Lucerne, Switzerland. “As a surgeon, that would help me to predict breast conservation at diagnosis, but as a surgical oncologist, I would also recognize that tumor response is an important component of future survival.”
The ABCSG findings suggest expanded utility for EndoPredict. The test’s molecular score is currently used along with tumor size and nodal status to predict the 10-year distant recurrence rate, and whether patients may safely forgo chemotherapy or are at high risk and may need adjuvant chemotherapy in addition to endocrine therapy.
Dr. Dubsky and his coinvestigators assessed performance of the EndoPredict test among 217 patients treated on ABCSG 34, a randomized phase 2 neoadjuvant trial. Findings showed that among patients given neoadjuvant endocrine therapy because they had less aggressive disease features, an EndoPredict high-risk result was associated with poor response (negative predictive value of 92%), defined as a residual cancer burden (RCB) of II or III, he reported at the San Antonio Breast Cancer Symposium.
On the other hand, among patients given neoadjuvant chemotherapy because they had more aggressive disease features, a low-risk result was associated with poor response (negative predictive value of 100%).
“Clinicians really gave us two distinct cohorts within ABCSG 34. In the luminal A–type patients who were treated with neoendocrine therapy, a high EndoPredict score predicted a low chance of tumor shrinkage. In the more aggressive ER-positive tumors, so-called luminal B type, treated with neoadjuvant chemotherapy, there was absolutely no excellent response in the low-risk group,” Dr. Dubsky summarized. “We believe that this molecular score may contribute to patient selection for biomarker-driven studies, especially in the neoadjuvant setting.”
Session attendee Steven Vogl, MD, a medical oncologist with the Montefiore Medical Center in New York, commented, “I have trouble correlating an RCB of 0 or I with what you as a surgeon do for the patient, because you are talking about pathologic complete response or just a few cells there. That’s not what determines how much breast you take off: It’s determined by the total size of the tumor and the size of the breast. So if it’s less than a few centimeters, I’m sure you can do a lumpectomy in every patient. Tell me why I should care that you are getting an RCB of 0 or I in these endocrine patients.”
“Because it’s more likely that these patients will have a smaller tumor and better tumor shrinkage,” Dr. Dubsky replied. “You are of course right, RCB 0 or I was not designed to help surgeons. But it helps me as a translational scientist to have a surrogate and an exact classification for good tumor shrinkage. That’s how I used it.”
C. Kent Osborne, MD, codirector of SABCS and director of the Dan L. Duncan Cancer Center at Baylor College of Medicine in Houston, asked, “We see it in the clinic, and I’m sure you have as well, patients whose tumor doesn’t shrink very much, but the Ki-67 really drops. And that may or may not be a better factor than the actual tumor shrinkage. So how many patients who had tumors that didn’t shrink, which was your endpoint, had a reduction in Ki-67 that was, say, 5%?”
“We haven’t looked at that specifically, but we will do so as we carry on with the follow-up of these patients. Then we can learn more about the prognosis,” Dr. Dubsky replied.
Study details
ABCSG 34 was a randomized phase 2 trial testing addition of the cancer vaccine tecemotide (Stimuvax) to neoadjuvant standard of care among patients with HER2-negative early breast cancer.
Dr. Dubsky and coinvestigators restricted analyses to patients with hormone receptor–positive disease who, depending on clinical and pathologic factors, received neoadjuvant chemotherapy (eight cycles of epirubicin-cyclophosphamide and docetaxel) or neoadjuvant endocrine therapy (6 months of letrozole [Femara]) as standard of care. They were then randomized to additionally receive tecemotide or not before undergoing surgery.
Overall, 25% of the 134 patients in the neoadjuvant chemotherapy group had a good tumor response, defined as pathologic complete response in both breast and nodes (RCB of 0) or minimal residual disease (RCB of I).
Higher EndoPredict score was associated with greater likelihood of good response to chemotherapy. EndoPredict risk group (high vs. low) had a negative predictive value of 100%, a positive predictive value of 26.4%, a true-positive rate of 100%, and a true-negative rate of 8.9% for predicting response (P = .112).
Area under the receiver operating characteristic curve was 0.736.
In a multivariate model, EndoPredict score as a continuous variable was not an independent predictor of response. “The good response was largely driven by covariates that included cell proliferation, and it was Ki-67 that was significant,” Dr. Dubsky noted.
Overall, 18% of the 83 patients in the neoadjuvant endocrine therapy group had a good tumor response (RCB of 0 or I). Here, lower EndoPredict score was associated with greater likelihood of good response. EndoPredict risk group (high vs. low) had a negative predictive value of 92.3%, a positive predictive value of 27.3%, a true-positive rate of 80.0%, and a true-negative rate of 52.9% for predicting response (P = .024). Area under the curve was 0.726.
In a multivariate model here, EndoPredict score as a continuous variable, its estrogen receptor–signaling/differentiation component, and Ki-67 did not independently predict response. “It was maybe a bit surprising that T stage was the strongest factor, possibly indicating that we should have simply treated those women longer than 6 months,” Dr. Dubsky commented. The EndoPredict proliferation component was also a significant predictor.
“Possibly, the very narrow distribution of Ki-67 [among patients given neoendocrine therapy] may have prevented this factor from playing a bigger role in this particular model,” he speculated.
Dr. Dubsky disclosed that he receives consulting fees from Myriad, the maker of EndoPredict, and from Cepheid, Nanostring, and Amgen.
SOURCE: Dubsky P et al. SABCS 2017 Abstract GS6-04.
SAN ANTONIO – The results of the EndoPredict test appear to predict tumor response in patients with early hormone receptor–positive, HER2-negative breast cancer given neoadjuvant therapy, based on results of a study conducted by the Austrian Breast & Colorectal Cancer Study Group (ABCSG).
“Very good tumor shrinkage in estrogen receptor–positive, HER2-negative disease is going to happen only in a minority of patients, and biomarkers that would predict excellent tumor shrinkage are an unmet medical need,” commented lead investigator Peter Dubsky, MD, PhD, who is head of the Breast Center at Hirslanden Klinik St. Anna, Lucerne, Switzerland. “As a surgeon, that would help me to predict breast conservation at diagnosis, but as a surgical oncologist, I would also recognize that tumor response is an important component of future survival.”
The ABCSG findings suggest expanded utility for EndoPredict. The test’s molecular score is currently used along with tumor size and nodal status to predict the 10-year distant recurrence rate, and whether patients may safely forgo chemotherapy or are at high risk and may need adjuvant chemotherapy in addition to endocrine therapy.
Dr. Dubsky and his coinvestigators assessed performance of the EndoPredict test among 217 patients treated on ABCSG 34, a randomized phase 2 neoadjuvant trial. Findings showed that among patients given neoadjuvant endocrine therapy because they had less aggressive disease features, an EndoPredict high-risk result was associated with poor response (negative predictive value of 92%), defined as a residual cancer burden (RCB) of II or III, he reported at the San Antonio Breast Cancer Symposium.
On the other hand, among patients given neoadjuvant chemotherapy because they had more aggressive disease features, a low-risk result was associated with poor response (negative predictive value of 100%).
“Clinicians really gave us two distinct cohorts within ABCSG 34. In the luminal A–type patients who were treated with neoendocrine therapy, a high EndoPredict score predicted a low chance of tumor shrinkage. In the more aggressive ER-positive tumors, so-called luminal B type, treated with neoadjuvant chemotherapy, there was absolutely no excellent response in the low-risk group,” Dr. Dubsky summarized. “We believe that this molecular score may contribute to patient selection for biomarker-driven studies, especially in the neoadjuvant setting.”
Session attendee Steven Vogl, MD, a medical oncologist with the Montefiore Medical Center in New York, commented, “I have trouble correlating an RCB of 0 or I with what you as a surgeon do for the patient, because you are talking about pathologic complete response or just a few cells there. That’s not what determines how much breast you take off: It’s determined by the total size of the tumor and the size of the breast. So if it’s less than a few centimeters, I’m sure you can do a lumpectomy in every patient. Tell me why I should care that you are getting an RCB of 0 or I in these endocrine patients.”
“Because it’s more likely that these patients will have a smaller tumor and better tumor shrinkage,” Dr. Dubsky replied. “You are of course right, RCB 0 or I was not designed to help surgeons. But it helps me as a translational scientist to have a surrogate and an exact classification for good tumor shrinkage. That’s how I used it.”
C. Kent Osborne, MD, codirector of SABCS and director of the Dan L. Duncan Cancer Center at Baylor College of Medicine in Houston, asked, “We see it in the clinic, and I’m sure you have as well, patients whose tumor doesn’t shrink very much, but the Ki-67 really drops. And that may or may not be a better factor than the actual tumor shrinkage. So how many patients who had tumors that didn’t shrink, which was your endpoint, had a reduction in Ki-67 that was, say, 5%?”
“We haven’t looked at that specifically, but we will do so as we carry on with the follow-up of these patients. Then we can learn more about the prognosis,” Dr. Dubsky replied.
Study details
ABCSG 34 was a randomized phase 2 trial testing addition of the cancer vaccine tecemotide (Stimuvax) to neoadjuvant standard of care among patients with HER2-negative early breast cancer.
Dr. Dubsky and coinvestigators restricted analyses to patients with hormone receptor–positive disease who, depending on clinical and pathologic factors, received neoadjuvant chemotherapy (eight cycles of epirubicin-cyclophosphamide and docetaxel) or neoadjuvant endocrine therapy (6 months of letrozole [Femara]) as standard of care. They were then randomized to additionally receive tecemotide or not before undergoing surgery.
Overall, 25% of the 134 patients in the neoadjuvant chemotherapy group had a good tumor response, defined as pathologic complete response in both breast and nodes (RCB of 0) or minimal residual disease (RCB of I).
Higher EndoPredict score was associated with greater likelihood of good response to chemotherapy. EndoPredict risk group (high vs. low) had a negative predictive value of 100%, a positive predictive value of 26.4%, a true-positive rate of 100%, and a true-negative rate of 8.9% for predicting response (P = .112).
Area under the receiver operating characteristic curve was 0.736.
In a multivariate model, EndoPredict score as a continuous variable was not an independent predictor of response. “The good response was largely driven by covariates that included cell proliferation, and it was Ki-67 that was significant,” Dr. Dubsky noted.
Overall, 18% of the 83 patients in the neoadjuvant endocrine therapy group had a good tumor response (RCB of 0 or I). Here, lower EndoPredict score was associated with greater likelihood of good response. EndoPredict risk group (high vs. low) had a negative predictive value of 92.3%, a positive predictive value of 27.3%, a true-positive rate of 80.0%, and a true-negative rate of 52.9% for predicting response (P = .024). Area under the curve was 0.726.
In a multivariate model here, EndoPredict score as a continuous variable, its estrogen receptor–signaling/differentiation component, and Ki-67 did not independently predict response. “It was maybe a bit surprising that T stage was the strongest factor, possibly indicating that we should have simply treated those women longer than 6 months,” Dr. Dubsky commented. The EndoPredict proliferation component was also a significant predictor.
“Possibly, the very narrow distribution of Ki-67 [among patients given neoendocrine therapy] may have prevented this factor from playing a bigger role in this particular model,” he speculated.
Dr. Dubsky disclosed that he receives consulting fees from Myriad, the maker of EndoPredict, and from Cepheid, Nanostring, and Amgen.
SOURCE: Dubsky P et al. SABCS 2017 Abstract GS6-04.
REPORTING FROM SABCS 2017
Key clinical point:
Major finding: EndoPredict predicted poor tumor shrinkage in patients given neoadjuvant endocrine therapy (high-risk test result NPV, 92%) or neoadjuvant chemotherapy (low-risk test result NPV, 100%).
Data source: A cohort study of 217 patients with HR–positive, HER2-negative breast cancer enrolled in a phase 2 trial of neoadjuvant therapy (ABCSG 34).
Disclosures: Dr. Dubsky disclosed that he receives consulting fees from Cepheid, Myriad, Nanostring, and Amgen.
Burnout among surgical residents mitigated by traits of mindfulness
General surgery residents reported high levels of stress linked to burnout, but those who exhibited characteristics of mindfulness were less likely to experience this dynamic, a survey-based study has found.
Carter C. Lebares, MD, of the department of surgery at the University of California, San Francisco, and her colleagues wrote, “Stress is a double-edged sword, with a dose-response relationship between stress and performance described as an ‘inverted U-shaped curve.’ Although stress is initially stimulating, there is a tipping point when demands outstrip resources and stress becomes overwhelming,” the researchers wrote. Surgical trainees purposefully join a high-stress profession and presumably thrive on a demanding environment, but “that does not make individuals immune to the effects of overwhelming stress.”
The investigative team aimed to assess the prevalence and root causes of burnout among surgical trainees. They sent a survey questionnaire to 246 general surgery training program directors and asked them to distribute the survey to their residents (J Am Coll Surg. 2018 Jan;226[1]:80-90. doi: 10.1016/j.jamcollsurg.2017.10.010). The investigators focused on the components of burnout identified in the literature (emotional exhaustion, depersonalization, perceived stress, depression, anxiety, and alcohol misuse/abuse).
The survey, a voluntary and confidential exercise, was based on scales and tools to assess symptoms of burnout (Maslach Burnout Inventory), stress (Cohen’s Perceived Stress Scale), anxiety (Spielberger’s State Trait Anxiety Index), and depression/suicidal ideation (Patient Health Questionnaire).
The researchers also looked at personality traits that could make the difference between the usual stress of residency and burnout in individual trainees. Mindfulness was studied using the Cognitive Affective Mindfulness Scale–Revised. A personality characteristic “trait resilience” was captured in a 10-item Block Ego-Resiliency Scale, which measured ability to adapt to a demanding and changing environment. “Dispositional mindfulness, that is, the innate ability to pay attention to one’s thoughts, emotions, and experiences in a nonreactive way, has been shown to have a buffering effect against perceived stress and burnout among healthcare workers and trainees,” they wrote.
A total of 566 surgery residents responded to the survey; 51% were female and 76% were based in an academic training program. Overall, the survey found that burnout prevalence among general surgery residents was 69%, which confirms the findings of earlier studies of this population, and was significantly higher than rates seen in age-matched peers in the general population and among practicing surgeons. Burnout was equally prevalent among men and women, but men appeared more likely to experience depersonalization (62% vs. 51%). Emotional exhaustion was lower among lab trainees. Alcohol misuse and abuse was somewhat higher in women (58% vs. 41% and 40% vs. 26%, respectively). Although symptoms of burnout were not strongly associated with training level, PGY3 residents experienced the most (58% reported higher stress, 16% suicidal ideation, 50% high anxiety, and 61% alcohol abuse). A high level of stress was reported significantly less often by lab trainees, but alcohol misuse was significantly greater. A high level of stress and emotional exhaustion and depersonalization were strongly linked. And all of these elements were strongly associated with moderate to severe depressive symptoms, suicidal ideation, and high anxiety.
The study is limited by potential biases in the responses, inevitable in a voluntary, self-selected sample. The survey was sent to ACGME-accredited program directors who may or may not have distributed it to their trainees. The investigators suggested that whereas the findings of this study in general confirm earlier research on trainee burnout, the perception of lack personal accomplishment in this sample was less dominant in this sample. “Although this might be because we included residents in lab/research years (widely thought to be a time of very high productivity), it is more likely due to our use of an abbreviated (9-item) form of the Maslach Burnout Inventory-Human Services Survey” and therefore underreported the personal accomplishment factor.
The impact that personality traits (mindfulness and trait resilience) on burnout risk was notable in this sample. “Greater dispositional mindfulness was associated with an 85% decrease in the risk of high stress, and a greater trait resilience was associated with a 65% decrease in the risk of high stress.” Some individuals have traits to help them cope better with stress but the investigators stated that mindfulness and resilience can be taught and fostered in trainees.
The current research on burnout has identified both institutional factors and personal factors. This study suggests that strategies to address both, simultaneously, are needed to truly change the current burnout risk prevalence among surgical trainees. They concluded: “Our findings demonstrate that inherent mindfulness is already in use to combat stress and burnout in surgical trainees and, more importantly, it appears to work. Based on this evidence, mindfulness training can be a critical component of any intervention aimed at enhancing stress resilience and preventing or treating burnout in surgical trainees.”
The researchers reported no relevant financial conflicts.
SOURCE: J Am Coll Surg. 2018 Jan;226(1):80-90. doi: 10.1016/j.jamcollsurg.2017.10.010)
General surgery residents reported high levels of stress linked to burnout, but those who exhibited characteristics of mindfulness were less likely to experience this dynamic, a survey-based study has found.
Carter C. Lebares, MD, of the department of surgery at the University of California, San Francisco, and her colleagues wrote, “Stress is a double-edged sword, with a dose-response relationship between stress and performance described as an ‘inverted U-shaped curve.’ Although stress is initially stimulating, there is a tipping point when demands outstrip resources and stress becomes overwhelming,” the researchers wrote. Surgical trainees purposefully join a high-stress profession and presumably thrive on a demanding environment, but “that does not make individuals immune to the effects of overwhelming stress.”
The investigative team aimed to assess the prevalence and root causes of burnout among surgical trainees. They sent a survey questionnaire to 246 general surgery training program directors and asked them to distribute the survey to their residents (J Am Coll Surg. 2018 Jan;226[1]:80-90. doi: 10.1016/j.jamcollsurg.2017.10.010). The investigators focused on the components of burnout identified in the literature (emotional exhaustion, depersonalization, perceived stress, depression, anxiety, and alcohol misuse/abuse).
The survey, a voluntary and confidential exercise, was based on scales and tools to assess symptoms of burnout (Maslach Burnout Inventory), stress (Cohen’s Perceived Stress Scale), anxiety (Spielberger’s State Trait Anxiety Index), and depression/suicidal ideation (Patient Health Questionnaire).
The researchers also looked at personality traits that could make the difference between the usual stress of residency and burnout in individual trainees. Mindfulness was studied using the Cognitive Affective Mindfulness Scale–Revised. A personality characteristic “trait resilience” was captured in a 10-item Block Ego-Resiliency Scale, which measured ability to adapt to a demanding and changing environment. “Dispositional mindfulness, that is, the innate ability to pay attention to one’s thoughts, emotions, and experiences in a nonreactive way, has been shown to have a buffering effect against perceived stress and burnout among healthcare workers and trainees,” they wrote.
A total of 566 surgery residents responded to the survey; 51% were female and 76% were based in an academic training program. Overall, the survey found that burnout prevalence among general surgery residents was 69%, which confirms the findings of earlier studies of this population, and was significantly higher than rates seen in age-matched peers in the general population and among practicing surgeons. Burnout was equally prevalent among men and women, but men appeared more likely to experience depersonalization (62% vs. 51%). Emotional exhaustion was lower among lab trainees. Alcohol misuse and abuse was somewhat higher in women (58% vs. 41% and 40% vs. 26%, respectively). Although symptoms of burnout were not strongly associated with training level, PGY3 residents experienced the most (58% reported higher stress, 16% suicidal ideation, 50% high anxiety, and 61% alcohol abuse). A high level of stress was reported significantly less often by lab trainees, but alcohol misuse was significantly greater. A high level of stress and emotional exhaustion and depersonalization were strongly linked. And all of these elements were strongly associated with moderate to severe depressive symptoms, suicidal ideation, and high anxiety.
The study is limited by potential biases in the responses, inevitable in a voluntary, self-selected sample. The survey was sent to ACGME-accredited program directors who may or may not have distributed it to their trainees. The investigators suggested that whereas the findings of this study in general confirm earlier research on trainee burnout, the perception of lack personal accomplishment in this sample was less dominant in this sample. “Although this might be because we included residents in lab/research years (widely thought to be a time of very high productivity), it is more likely due to our use of an abbreviated (9-item) form of the Maslach Burnout Inventory-Human Services Survey” and therefore underreported the personal accomplishment factor.
The impact that personality traits (mindfulness and trait resilience) on burnout risk was notable in this sample. “Greater dispositional mindfulness was associated with an 85% decrease in the risk of high stress, and a greater trait resilience was associated with a 65% decrease in the risk of high stress.” Some individuals have traits to help them cope better with stress but the investigators stated that mindfulness and resilience can be taught and fostered in trainees.
The current research on burnout has identified both institutional factors and personal factors. This study suggests that strategies to address both, simultaneously, are needed to truly change the current burnout risk prevalence among surgical trainees. They concluded: “Our findings demonstrate that inherent mindfulness is already in use to combat stress and burnout in surgical trainees and, more importantly, it appears to work. Based on this evidence, mindfulness training can be a critical component of any intervention aimed at enhancing stress resilience and preventing or treating burnout in surgical trainees.”
The researchers reported no relevant financial conflicts.
SOURCE: J Am Coll Surg. 2018 Jan;226(1):80-90. doi: 10.1016/j.jamcollsurg.2017.10.010)
General surgery residents reported high levels of stress linked to burnout, but those who exhibited characteristics of mindfulness were less likely to experience this dynamic, a survey-based study has found.
Carter C. Lebares, MD, of the department of surgery at the University of California, San Francisco, and her colleagues wrote, “Stress is a double-edged sword, with a dose-response relationship between stress and performance described as an ‘inverted U-shaped curve.’ Although stress is initially stimulating, there is a tipping point when demands outstrip resources and stress becomes overwhelming,” the researchers wrote. Surgical trainees purposefully join a high-stress profession and presumably thrive on a demanding environment, but “that does not make individuals immune to the effects of overwhelming stress.”
The investigative team aimed to assess the prevalence and root causes of burnout among surgical trainees. They sent a survey questionnaire to 246 general surgery training program directors and asked them to distribute the survey to their residents (J Am Coll Surg. 2018 Jan;226[1]:80-90. doi: 10.1016/j.jamcollsurg.2017.10.010). The investigators focused on the components of burnout identified in the literature (emotional exhaustion, depersonalization, perceived stress, depression, anxiety, and alcohol misuse/abuse).
The survey, a voluntary and confidential exercise, was based on scales and tools to assess symptoms of burnout (Maslach Burnout Inventory), stress (Cohen’s Perceived Stress Scale), anxiety (Spielberger’s State Trait Anxiety Index), and depression/suicidal ideation (Patient Health Questionnaire).
The researchers also looked at personality traits that could make the difference between the usual stress of residency and burnout in individual trainees. Mindfulness was studied using the Cognitive Affective Mindfulness Scale–Revised. A personality characteristic “trait resilience” was captured in a 10-item Block Ego-Resiliency Scale, which measured ability to adapt to a demanding and changing environment. “Dispositional mindfulness, that is, the innate ability to pay attention to one’s thoughts, emotions, and experiences in a nonreactive way, has been shown to have a buffering effect against perceived stress and burnout among healthcare workers and trainees,” they wrote.
A total of 566 surgery residents responded to the survey; 51% were female and 76% were based in an academic training program. Overall, the survey found that burnout prevalence among general surgery residents was 69%, which confirms the findings of earlier studies of this population, and was significantly higher than rates seen in age-matched peers in the general population and among practicing surgeons. Burnout was equally prevalent among men and women, but men appeared more likely to experience depersonalization (62% vs. 51%). Emotional exhaustion was lower among lab trainees. Alcohol misuse and abuse was somewhat higher in women (58% vs. 41% and 40% vs. 26%, respectively). Although symptoms of burnout were not strongly associated with training level, PGY3 residents experienced the most (58% reported higher stress, 16% suicidal ideation, 50% high anxiety, and 61% alcohol abuse). A high level of stress was reported significantly less often by lab trainees, but alcohol misuse was significantly greater. A high level of stress and emotional exhaustion and depersonalization were strongly linked. And all of these elements were strongly associated with moderate to severe depressive symptoms, suicidal ideation, and high anxiety.
The study is limited by potential biases in the responses, inevitable in a voluntary, self-selected sample. The survey was sent to ACGME-accredited program directors who may or may not have distributed it to their trainees. The investigators suggested that whereas the findings of this study in general confirm earlier research on trainee burnout, the perception of lack personal accomplishment in this sample was less dominant in this sample. “Although this might be because we included residents in lab/research years (widely thought to be a time of very high productivity), it is more likely due to our use of an abbreviated (9-item) form of the Maslach Burnout Inventory-Human Services Survey” and therefore underreported the personal accomplishment factor.
The impact that personality traits (mindfulness and trait resilience) on burnout risk was notable in this sample. “Greater dispositional mindfulness was associated with an 85% decrease in the risk of high stress, and a greater trait resilience was associated with a 65% decrease in the risk of high stress.” Some individuals have traits to help them cope better with stress but the investigators stated that mindfulness and resilience can be taught and fostered in trainees.
The current research on burnout has identified both institutional factors and personal factors. This study suggests that strategies to address both, simultaneously, are needed to truly change the current burnout risk prevalence among surgical trainees. They concluded: “Our findings demonstrate that inherent mindfulness is already in use to combat stress and burnout in surgical trainees and, more importantly, it appears to work. Based on this evidence, mindfulness training can be a critical component of any intervention aimed at enhancing stress resilience and preventing or treating burnout in surgical trainees.”
The researchers reported no relevant financial conflicts.
SOURCE: J Am Coll Surg. 2018 Jan;226(1):80-90. doi: 10.1016/j.jamcollsurg.2017.10.010)
FROM JOURNAL OF THE AMERICAN COLLEGE OF SURGERY
Key clinical point: Burnout prevalence is high among surgical trainees, but individual traits such as mindfulness are linked to a lower risk of burnout.
Major finding: Among surgery residents, the total prevalence of burnout was 69%.
Study details: 566 responses to a voluntary and confidential survey of general surgery residents.
Disclosures: Investigators had no relevant financial disclosures.
Source: J Am Coll Surg. 2018 Jan;226(1):80-90. doi: 10.1016/j.jamcollsurg.2017.10.010.
FDA bans 24 ingredients from OTC health care antiseptic products
in hospital settings and other health care situations outside the hospital, the U.S. Food and Drug Administration announced in a final rule.
The affected products include health care personnel hand washes and hand rubs, surgical hand scrubs and hand rubs, and patient antiseptic skin preparations. The final rule was published Dec. 20 in the Federal Register and becomes effective in December 2018.
The agency determined that a deferral is warranted for six health care antiseptic active ingredients – benzalkonium chloride, benzethonium chloride, chloroxylenol, alcohol, isopropyl alcohol, and povidone-iodine – to allow more time for interested parties to complete the studies necessary to fill the safety and effectiveness data gaps identified for these ingredients.
“The FDA expects that this information may help better inform us on antiseptic resistance and antibiotic cross-resistance in the health care setting,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “Importantly, this doesn’t mean that products containing these six ingredients are ineffective or unsafe. These antiseptic products remain an important resource in health care settings. Personnel should continue to use these products consistent with infection control guidelines while the additional data are gathered.”
No additional data was provided for another 24 products, which were deemed not generally recognized as safe and effective. The minimum data needed to demonstrate safety for all health care antiseptic active ingredients fall into four broad categories: human safety studies, nonclinical safety studies (developmental and reproductive toxicity studies and carcinogenicity studies), data to characterize potential hormonal effects, and data to evaluate the development of antimicrobial resistance, the final rule states.
The FDA noted that manufacturers started to remove nearly all of these 24 active ingredients from their products following a 2015 proposed rule. Triclosan is currently being used in available products.
The active ingredients affected are chlorhexidine gluconate; cloflucarban; fluorosalan; hexachlorophene; hexylresorcinol; iodophors (iodine-containing ingredients including iodine complex [ammonium ether sulfate and polyoxyethylene sorbitan monolaurate], iodine complex [phosphate ester of alkylaryloxy polyethylene glycol], iodine tincture USP, iodine topical solution USP, nonylphenoxypoly [ethyleneoxy] ethanoliodine, poloxamer–iodine complex, undecoylium chloride iodine complex); mercufenol chloride; methylbenzethonium chloride; phenol; secondary amyltricresols; sodium oxychlorosene; tribromsalan; triclocarban; triclosan; triple dye; combination of calomel, oxyquinoline benzoate, triethanolamine, and phenol derivative; and combination of mercufenol chloride and secondary amyltricresols in 50% alcohol.
If manufacturers want to use one or more of these 24 active ingredients in future OTC health care antiseptic drug products, those products will be considered new drugs for which a new drug application approval will be required, the agency said.
The rule does not affect health care antiseptics that are currently marketed under new drug applications and abbreviated new drug applications.
FDA’s action follows a similar final rule published Sept. 6, 2016, which removed triclosan and 18 other active ingredients from consumer antiseptic products.
in hospital settings and other health care situations outside the hospital, the U.S. Food and Drug Administration announced in a final rule.
The affected products include health care personnel hand washes and hand rubs, surgical hand scrubs and hand rubs, and patient antiseptic skin preparations. The final rule was published Dec. 20 in the Federal Register and becomes effective in December 2018.
The agency determined that a deferral is warranted for six health care antiseptic active ingredients – benzalkonium chloride, benzethonium chloride, chloroxylenol, alcohol, isopropyl alcohol, and povidone-iodine – to allow more time for interested parties to complete the studies necessary to fill the safety and effectiveness data gaps identified for these ingredients.
“The FDA expects that this information may help better inform us on antiseptic resistance and antibiotic cross-resistance in the health care setting,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “Importantly, this doesn’t mean that products containing these six ingredients are ineffective or unsafe. These antiseptic products remain an important resource in health care settings. Personnel should continue to use these products consistent with infection control guidelines while the additional data are gathered.”
No additional data was provided for another 24 products, which were deemed not generally recognized as safe and effective. The minimum data needed to demonstrate safety for all health care antiseptic active ingredients fall into four broad categories: human safety studies, nonclinical safety studies (developmental and reproductive toxicity studies and carcinogenicity studies), data to characterize potential hormonal effects, and data to evaluate the development of antimicrobial resistance, the final rule states.
The FDA noted that manufacturers started to remove nearly all of these 24 active ingredients from their products following a 2015 proposed rule. Triclosan is currently being used in available products.
The active ingredients affected are chlorhexidine gluconate; cloflucarban; fluorosalan; hexachlorophene; hexylresorcinol; iodophors (iodine-containing ingredients including iodine complex [ammonium ether sulfate and polyoxyethylene sorbitan monolaurate], iodine complex [phosphate ester of alkylaryloxy polyethylene glycol], iodine tincture USP, iodine topical solution USP, nonylphenoxypoly [ethyleneoxy] ethanoliodine, poloxamer–iodine complex, undecoylium chloride iodine complex); mercufenol chloride; methylbenzethonium chloride; phenol; secondary amyltricresols; sodium oxychlorosene; tribromsalan; triclocarban; triclosan; triple dye; combination of calomel, oxyquinoline benzoate, triethanolamine, and phenol derivative; and combination of mercufenol chloride and secondary amyltricresols in 50% alcohol.
If manufacturers want to use one or more of these 24 active ingredients in future OTC health care antiseptic drug products, those products will be considered new drugs for which a new drug application approval will be required, the agency said.
The rule does not affect health care antiseptics that are currently marketed under new drug applications and abbreviated new drug applications.
FDA’s action follows a similar final rule published Sept. 6, 2016, which removed triclosan and 18 other active ingredients from consumer antiseptic products.
in hospital settings and other health care situations outside the hospital, the U.S. Food and Drug Administration announced in a final rule.
The affected products include health care personnel hand washes and hand rubs, surgical hand scrubs and hand rubs, and patient antiseptic skin preparations. The final rule was published Dec. 20 in the Federal Register and becomes effective in December 2018.
The agency determined that a deferral is warranted for six health care antiseptic active ingredients – benzalkonium chloride, benzethonium chloride, chloroxylenol, alcohol, isopropyl alcohol, and povidone-iodine – to allow more time for interested parties to complete the studies necessary to fill the safety and effectiveness data gaps identified for these ingredients.
“The FDA expects that this information may help better inform us on antiseptic resistance and antibiotic cross-resistance in the health care setting,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “Importantly, this doesn’t mean that products containing these six ingredients are ineffective or unsafe. These antiseptic products remain an important resource in health care settings. Personnel should continue to use these products consistent with infection control guidelines while the additional data are gathered.”
No additional data was provided for another 24 products, which were deemed not generally recognized as safe and effective. The minimum data needed to demonstrate safety for all health care antiseptic active ingredients fall into four broad categories: human safety studies, nonclinical safety studies (developmental and reproductive toxicity studies and carcinogenicity studies), data to characterize potential hormonal effects, and data to evaluate the development of antimicrobial resistance, the final rule states.
The FDA noted that manufacturers started to remove nearly all of these 24 active ingredients from their products following a 2015 proposed rule. Triclosan is currently being used in available products.
The active ingredients affected are chlorhexidine gluconate; cloflucarban; fluorosalan; hexachlorophene; hexylresorcinol; iodophors (iodine-containing ingredients including iodine complex [ammonium ether sulfate and polyoxyethylene sorbitan monolaurate], iodine complex [phosphate ester of alkylaryloxy polyethylene glycol], iodine tincture USP, iodine topical solution USP, nonylphenoxypoly [ethyleneoxy] ethanoliodine, poloxamer–iodine complex, undecoylium chloride iodine complex); mercufenol chloride; methylbenzethonium chloride; phenol; secondary amyltricresols; sodium oxychlorosene; tribromsalan; triclocarban; triclosan; triple dye; combination of calomel, oxyquinoline benzoate, triethanolamine, and phenol derivative; and combination of mercufenol chloride and secondary amyltricresols in 50% alcohol.
If manufacturers want to use one or more of these 24 active ingredients in future OTC health care antiseptic drug products, those products will be considered new drugs for which a new drug application approval will be required, the agency said.
The rule does not affect health care antiseptics that are currently marketed under new drug applications and abbreviated new drug applications.
FDA’s action follows a similar final rule published Sept. 6, 2016, which removed triclosan and 18 other active ingredients from consumer antiseptic products.
Drug price increases far outpaced inflation in 2015
The retail price for a set of 768 prescription drugs rose by 6.4% in 2015, while the general inflation rate increased by just 0.1%, according to the AARP Public Policy Institute and the PRIME Institute at the University of Minnesota in Minneapolis.
One year, of course, does not make a trend, but how about 10 years? The average increase in the price of the “market basket” of 768 drugs widely used by older Americans has exceeded the rate of inflation every year since the AARP started tracking costs in 2004. This is “attributable entirely to drug price growth among brand name and specialty drugs, which more than offset often substantial price decreases among generic drugs,” Leigh Purvis of AARP and Stephen Schondelmeyer, PharmD, PhD, of the Prime Institute, said in an Rx Price Watch report.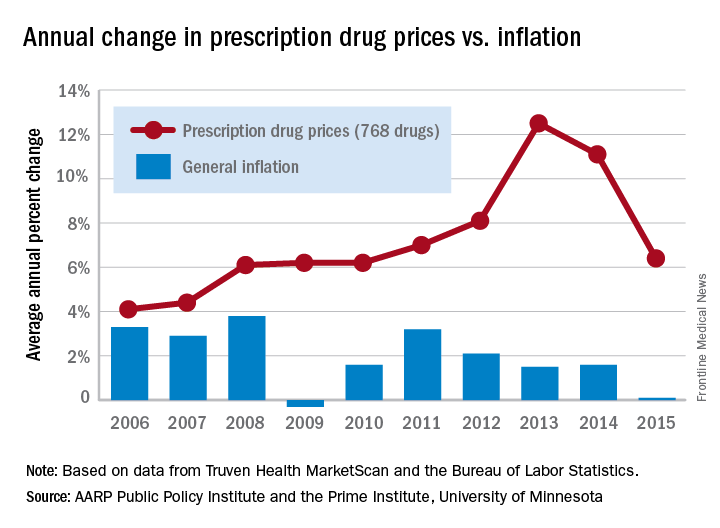
In terms of actual cost, however, the specialty drugs were far ahead of the other two segments. The average cost of a year of treatment with a specialty drug was more than $52,000 in 2015, which was nine times higher than the brand-name drugs ($5,800) and 100 times higher than the generics ($523), they said.
The Rx Price Watch reports are based on retail-level prescription prices from the Truven Health MarketScan Research Databases. The general inflation rate is based on the Consumer Price Index–All Urban Consumers for All Items, which is measured by the Bureau of Labor Statistics.
The retail price for a set of 768 prescription drugs rose by 6.4% in 2015, while the general inflation rate increased by just 0.1%, according to the AARP Public Policy Institute and the PRIME Institute at the University of Minnesota in Minneapolis.
One year, of course, does not make a trend, but how about 10 years? The average increase in the price of the “market basket” of 768 drugs widely used by older Americans has exceeded the rate of inflation every year since the AARP started tracking costs in 2004. This is “attributable entirely to drug price growth among brand name and specialty drugs, which more than offset often substantial price decreases among generic drugs,” Leigh Purvis of AARP and Stephen Schondelmeyer, PharmD, PhD, of the Prime Institute, said in an Rx Price Watch report.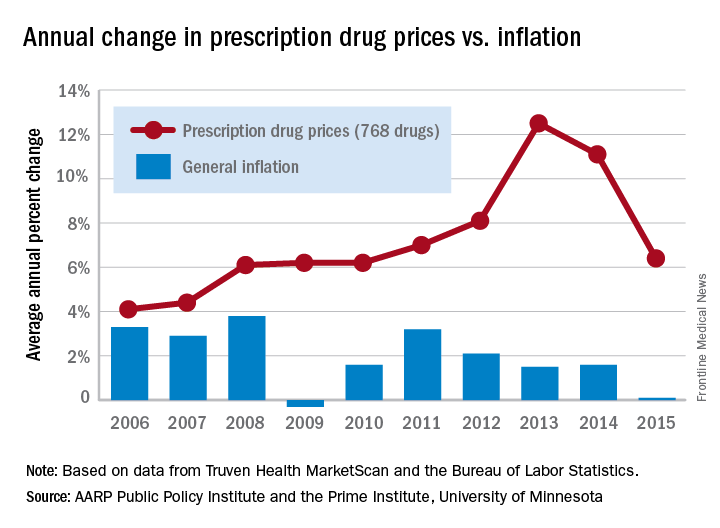
In terms of actual cost, however, the specialty drugs were far ahead of the other two segments. The average cost of a year of treatment with a specialty drug was more than $52,000 in 2015, which was nine times higher than the brand-name drugs ($5,800) and 100 times higher than the generics ($523), they said.
The Rx Price Watch reports are based on retail-level prescription prices from the Truven Health MarketScan Research Databases. The general inflation rate is based on the Consumer Price Index–All Urban Consumers for All Items, which is measured by the Bureau of Labor Statistics.
The retail price for a set of 768 prescription drugs rose by 6.4% in 2015, while the general inflation rate increased by just 0.1%, according to the AARP Public Policy Institute and the PRIME Institute at the University of Minnesota in Minneapolis.
One year, of course, does not make a trend, but how about 10 years? The average increase in the price of the “market basket” of 768 drugs widely used by older Americans has exceeded the rate of inflation every year since the AARP started tracking costs in 2004. This is “attributable entirely to drug price growth among brand name and specialty drugs, which more than offset often substantial price decreases among generic drugs,” Leigh Purvis of AARP and Stephen Schondelmeyer, PharmD, PhD, of the Prime Institute, said in an Rx Price Watch report.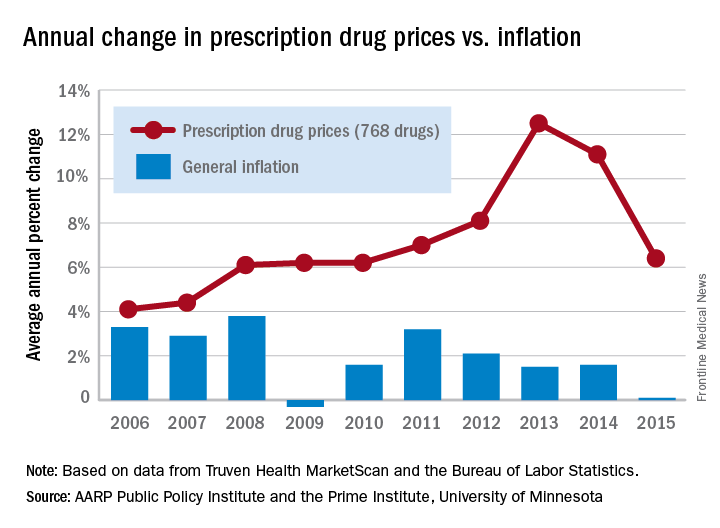
In terms of actual cost, however, the specialty drugs were far ahead of the other two segments. The average cost of a year of treatment with a specialty drug was more than $52,000 in 2015, which was nine times higher than the brand-name drugs ($5,800) and 100 times higher than the generics ($523), they said.
The Rx Price Watch reports are based on retail-level prescription prices from the Truven Health MarketScan Research Databases. The general inflation rate is based on the Consumer Price Index–All Urban Consumers for All Items, which is measured by the Bureau of Labor Statistics.
Test storyHeadline – 7 words, sentence case, active verb, include best SEO terms
Body text starts here….
Second and subsequent grafs
Doctor’s Name and Bio
Body text starts here….
Second and subsequent grafs
Doctor’s Name and Bio
Body text starts here….
Second and subsequent grafs
Doctor’s Name and Bio
Key clinical point:
Major finding: Key numerical finding (e.g., number needed to treat to prevent one death/event; number lived or died as result of intervention). Maximum 10 words/1 sentence.
Data source: Include type of study (e.g., randomized, placebo controlled trial; retrospective case-control study). Include number in the study.
Disclosures: Sponsor of study, funding source, relevant disclosures. If author has no relevant disclosures, “Dr. X reported having no financial disclosures.” If necessary, “Meeting Y did not require reports of financial disclosures.” Check meeting website because many list disclosures. Written in sentence form.
HealthCare.gov enrollment for 2018 nearly doubled in final week
A busy final week of open enrollment at HealthCare.gov almost doubled the total number of health insurance plans selected and nearly equaled the total for last year’s much longer period, according to data from the Centers for Medicare & Medicaid Services.
After the first 6 weeks of enrollment, the total number of plans selected for 2018 stood at 4.68 million. Just 1 week later, . That works out to 6.43 million plans selected by consumers who renewed their coverage on 1 of the 39 state exchanges that use the HealthCare.gov platform and 2.39 million plans selected by new consumers (those who did not have coverage in 2017), the CMS reported.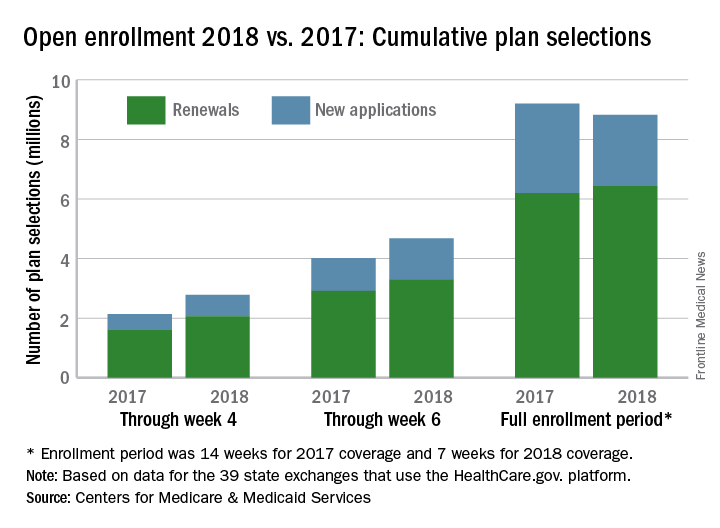
The CMS noted that the numbers for 2018 are estimates that represent plans selected and not the number of consumers who have paid premiums to effectuate their enrollment.
SOURCE: CMS.gov Fact Sheet
A busy final week of open enrollment at HealthCare.gov almost doubled the total number of health insurance plans selected and nearly equaled the total for last year’s much longer period, according to data from the Centers for Medicare & Medicaid Services.
After the first 6 weeks of enrollment, the total number of plans selected for 2018 stood at 4.68 million. Just 1 week later, . That works out to 6.43 million plans selected by consumers who renewed their coverage on 1 of the 39 state exchanges that use the HealthCare.gov platform and 2.39 million plans selected by new consumers (those who did not have coverage in 2017), the CMS reported.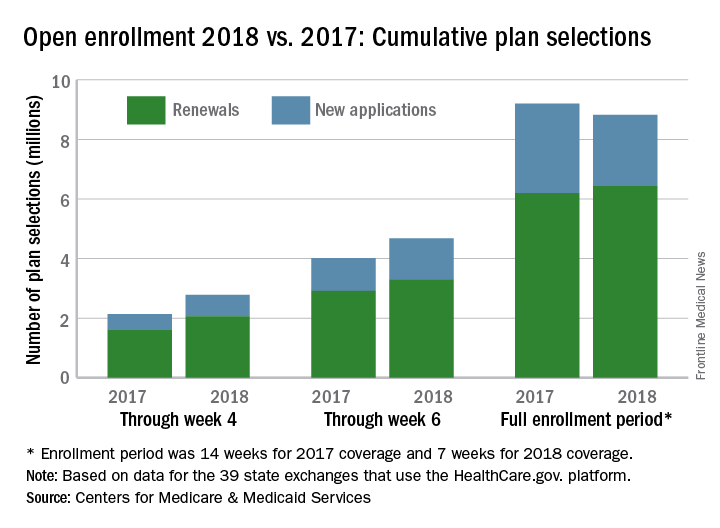
The CMS noted that the numbers for 2018 are estimates that represent plans selected and not the number of consumers who have paid premiums to effectuate their enrollment.
SOURCE: CMS.gov Fact Sheet
A busy final week of open enrollment at HealthCare.gov almost doubled the total number of health insurance plans selected and nearly equaled the total for last year’s much longer period, according to data from the Centers for Medicare & Medicaid Services.
After the first 6 weeks of enrollment, the total number of plans selected for 2018 stood at 4.68 million. Just 1 week later, . That works out to 6.43 million plans selected by consumers who renewed their coverage on 1 of the 39 state exchanges that use the HealthCare.gov platform and 2.39 million plans selected by new consumers (those who did not have coverage in 2017), the CMS reported.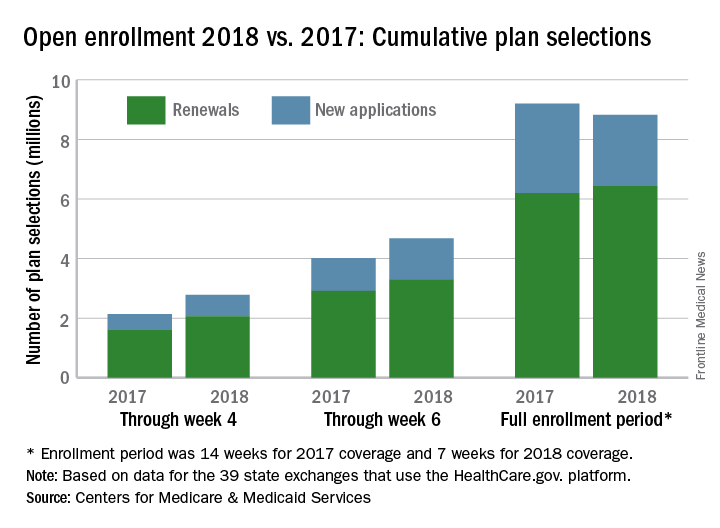
The CMS noted that the numbers for 2018 are estimates that represent plans selected and not the number of consumers who have paid premiums to effectuate their enrollment.
SOURCE: CMS.gov Fact Sheet
Enhanced recovery protocols after colectomy safely cut LOS
, at 15 hospitals in a pilot study of the Enhanced Recovery in National Surgical Quality Improvement Program.
Guidance from experts, engaged multidisciplinary team leadership, continuous data collection and auditing, and collaboration across institutions were all key to success. “The pilot may serve to inform future implementation efforts across hospitals varied in size, location, and resource availability,” investigators led by Julia R. Berian, MD, a surgery resident at the University of Chicago, wrote in a study published online in JAMA Surgery.
The program suggested 13 measures aimed at improved pain control, reduced gut dysfunction, and early nutrition and physical activity. Recommendations included shorter fluid fasts and better preop patient counseling; discontinuation of IV fluids and mobilization of patients within 24 hours of surgery; and solid diets within 24-48 hours.
The measures weren’t mandatory; each hospital tailored its protocols, and timing of implementation was at their discretion.
The report didn’t name the 15 hospitals, but they varied by size and academic status. Hospitals were selected for the program because they were outliers on elective colectomy LOS. The study ran during 2013-2015.
There were 3,437 colectomies at the hospitals before implementation, and 1,538 after. Results were compared with those of 9,950 colectomies over the study period at hospitals not involved in the efforts. Emergency and septic cases were excluded.
ERPs decreased mean LOS by 1.7 days, from 6.9 to 5.2 days. After taking patient characteristics and other matters into account, the adjusted decrease was 1.1 days. LOS fell by 0.4 days in the control hospitals (P less than .001).
Serious morbidity or mortality in the ERP hospitals decreased from 485 cases (14.1%) before implementation to 162 (10.5%) afterward (P less than .001); there was no change in the control hospitals. After implementation, serious morbidity or mortality was significantly less likely in ERP hospitals (adjusted odds ratio, 0.76; 95% confidence interval, 0.60-0.96).
Meanwhile, there was no difference in readmission rates before and after implementation.
“The ERIN pilot study included hospitals of various sizes, indicating that both small and large hospitals can successfully decrease LOS with implementation of an ERP. ... Regardless of resource limitations, small hospitals may have the advantage of decreased bureaucracy and improved communication and collaboration across disciplines. ... We strongly believe that surgeon engagement and leadership in such initiatives are critical to sustained success,” the investigators wrote.
The ACS; Johns Hopkins’ Armstrong Institute for Patient Safety and Quality, Baltimore; and the Agency for Healthcare Research and Quality have recently launched the “Improving Surgical Care and Recovery” program to provide more than 750 hospitals with tools, experts, and other resources for implementing ERPs. “The program is one opportunity for hospitals seeking implementation guidance,” the investigators noted.
Dr. Berian reported receiving salary support from the John A. Hartford Foundation. Her coinvestigators reported receiving grant or salary support from the foundation and the Agency for Healthcare Research and Quality. One investigator reported relationships with a variety of drug and device companies.
SOURCE: Berian J et. al. JAMA Surg. 2017 Dec 20. doi: 10.1001/jamasurg.2017.4906
, at 15 hospitals in a pilot study of the Enhanced Recovery in National Surgical Quality Improvement Program.
Guidance from experts, engaged multidisciplinary team leadership, continuous data collection and auditing, and collaboration across institutions were all key to success. “The pilot may serve to inform future implementation efforts across hospitals varied in size, location, and resource availability,” investigators led by Julia R. Berian, MD, a surgery resident at the University of Chicago, wrote in a study published online in JAMA Surgery.
The program suggested 13 measures aimed at improved pain control, reduced gut dysfunction, and early nutrition and physical activity. Recommendations included shorter fluid fasts and better preop patient counseling; discontinuation of IV fluids and mobilization of patients within 24 hours of surgery; and solid diets within 24-48 hours.
The measures weren’t mandatory; each hospital tailored its protocols, and timing of implementation was at their discretion.
The report didn’t name the 15 hospitals, but they varied by size and academic status. Hospitals were selected for the program because they were outliers on elective colectomy LOS. The study ran during 2013-2015.
There were 3,437 colectomies at the hospitals before implementation, and 1,538 after. Results were compared with those of 9,950 colectomies over the study period at hospitals not involved in the efforts. Emergency and septic cases were excluded.
ERPs decreased mean LOS by 1.7 days, from 6.9 to 5.2 days. After taking patient characteristics and other matters into account, the adjusted decrease was 1.1 days. LOS fell by 0.4 days in the control hospitals (P less than .001).
Serious morbidity or mortality in the ERP hospitals decreased from 485 cases (14.1%) before implementation to 162 (10.5%) afterward (P less than .001); there was no change in the control hospitals. After implementation, serious morbidity or mortality was significantly less likely in ERP hospitals (adjusted odds ratio, 0.76; 95% confidence interval, 0.60-0.96).
Meanwhile, there was no difference in readmission rates before and after implementation.
“The ERIN pilot study included hospitals of various sizes, indicating that both small and large hospitals can successfully decrease LOS with implementation of an ERP. ... Regardless of resource limitations, small hospitals may have the advantage of decreased bureaucracy and improved communication and collaboration across disciplines. ... We strongly believe that surgeon engagement and leadership in such initiatives are critical to sustained success,” the investigators wrote.
The ACS; Johns Hopkins’ Armstrong Institute for Patient Safety and Quality, Baltimore; and the Agency for Healthcare Research and Quality have recently launched the “Improving Surgical Care and Recovery” program to provide more than 750 hospitals with tools, experts, and other resources for implementing ERPs. “The program is one opportunity for hospitals seeking implementation guidance,” the investigators noted.
Dr. Berian reported receiving salary support from the John A. Hartford Foundation. Her coinvestigators reported receiving grant or salary support from the foundation and the Agency for Healthcare Research and Quality. One investigator reported relationships with a variety of drug and device companies.
SOURCE: Berian J et. al. JAMA Surg. 2017 Dec 20. doi: 10.1001/jamasurg.2017.4906
, at 15 hospitals in a pilot study of the Enhanced Recovery in National Surgical Quality Improvement Program.
Guidance from experts, engaged multidisciplinary team leadership, continuous data collection and auditing, and collaboration across institutions were all key to success. “The pilot may serve to inform future implementation efforts across hospitals varied in size, location, and resource availability,” investigators led by Julia R. Berian, MD, a surgery resident at the University of Chicago, wrote in a study published online in JAMA Surgery.
The program suggested 13 measures aimed at improved pain control, reduced gut dysfunction, and early nutrition and physical activity. Recommendations included shorter fluid fasts and better preop patient counseling; discontinuation of IV fluids and mobilization of patients within 24 hours of surgery; and solid diets within 24-48 hours.
The measures weren’t mandatory; each hospital tailored its protocols, and timing of implementation was at their discretion.
The report didn’t name the 15 hospitals, but they varied by size and academic status. Hospitals were selected for the program because they were outliers on elective colectomy LOS. The study ran during 2013-2015.
There were 3,437 colectomies at the hospitals before implementation, and 1,538 after. Results were compared with those of 9,950 colectomies over the study period at hospitals not involved in the efforts. Emergency and septic cases were excluded.
ERPs decreased mean LOS by 1.7 days, from 6.9 to 5.2 days. After taking patient characteristics and other matters into account, the adjusted decrease was 1.1 days. LOS fell by 0.4 days in the control hospitals (P less than .001).
Serious morbidity or mortality in the ERP hospitals decreased from 485 cases (14.1%) before implementation to 162 (10.5%) afterward (P less than .001); there was no change in the control hospitals. After implementation, serious morbidity or mortality was significantly less likely in ERP hospitals (adjusted odds ratio, 0.76; 95% confidence interval, 0.60-0.96).
Meanwhile, there was no difference in readmission rates before and after implementation.
“The ERIN pilot study included hospitals of various sizes, indicating that both small and large hospitals can successfully decrease LOS with implementation of an ERP. ... Regardless of resource limitations, small hospitals may have the advantage of decreased bureaucracy and improved communication and collaboration across disciplines. ... We strongly believe that surgeon engagement and leadership in such initiatives are critical to sustained success,” the investigators wrote.
The ACS; Johns Hopkins’ Armstrong Institute for Patient Safety and Quality, Baltimore; and the Agency for Healthcare Research and Quality have recently launched the “Improving Surgical Care and Recovery” program to provide more than 750 hospitals with tools, experts, and other resources for implementing ERPs. “The program is one opportunity for hospitals seeking implementation guidance,” the investigators noted.
Dr. Berian reported receiving salary support from the John A. Hartford Foundation. Her coinvestigators reported receiving grant or salary support from the foundation and the Agency for Healthcare Research and Quality. One investigator reported relationships with a variety of drug and device companies.
SOURCE: Berian J et. al. JAMA Surg. 2017 Dec 20. doi: 10.1001/jamasurg.2017.4906
FROM JAMA SURGERY
Key clinical point: With the help of the Enhanced Recovery in National Surgical Quality Improvement Program, 15 hospitals enacted enhanced recovery protocols for elective colectomy that shortened length of stay and decreased complications, without increasing readmissions.
Major finding: After taking patient characteristics and other matters into account, the adjusted decrease in LOS was 1.1 days, versus 0.4 days in control hospitals (P less than .001).
Study details: The study compared 3,437 colectomies at 15 hospitals before ERP implementation to 1,538 after.
Disclosures: Dr. Berian reported receiving salary support from the John A. Hartford Foundation. Her coinvestigators reported receiving grant or salary support from the foundation and the Agency for Healthcare Research and Quality. One investigator reported relationships with a variety of drug and device companies.
Source: Berian J et. al. JAMA Surg. 2017 Dec 20. doi: 10.1001/jamasurg.2017.4906
Palliative care underutilized in dementia patients with acute abdomen
Despite high rates of in-hospital mortality and nonroutine discharge, palliative care is underutilized in patients with dementia and acute abdominal emergency, according to findings published in Surgery.
“Currently little is known about palliative care utilization among patients with dementia in possible need of surgical intervention. This raises the question of whether the acute surgical emergency represents an appropriate episode during which to introduce palliative care for patients with dementia,” wrote Ana Berlin, MD, FACS, of the department of surgery at New Jersey Medical School, Newark, N.J., and her coauthors (Surgery. 2017 Dec 4. doi: 10.1016/j.surg.2017.09.048).
Of 15,209 patients aged 50 years and older with dementia and acute abdomen, 7.5% received palliative care. Patients discharged nonroutinely and patients treated operatively were less likely to receive palliative care, the researchers reported.
Dr. Berlin and her colleagues used the National Inpatient Sample database to identify patients with dementia and acute abdomen who were admitted nonelectively between 2009 and 2013. They used ICD-9 primary and secondary codes to limit surgical diagnoses to gastrointestinal obstruction, ischemia, and perforation.
Overall, 50.9% of patients were admitted for gastrointestinal obstruction, 39.8% for perforation, 5.1% for bowel ischemia, and 4.3% for mixed pathology; 17.8% of patients were managed operatively.
Patients with intestinal ischemia had the highest rate of both operation and mortality, at 22.8% and 27.6%, respectively. These patients also had the lowest rate of routine discharge, at 15.9%, the authors said. In comparison, patients with obstruction had surgical intervention and in-hospital mortality rates of 17% and 10.1%, respectively, and a routine discharge rate of 20.9%. Patients with perforation had an operation rate of 13.8%, in-hospital mortality rate of 6.8%, and routine discharge rate of 26.9%.
The palliative care utilization rate overall was 7.5%. Patients with mixed pathology who did not have surgery were most likely to receive palliative care, at 21.1%, noted Dr. Berlin and her coauthors.
Patients who died postoperatively were less likely than were those who died without surgical intervention to have received palliative care (20.9% vs. 31.4%; odds ratio = 0.63, 95% confidence interval, 0.46-0.86; P = .0039), and those who were discharged nonroutinely after an operation were less likely than were patients who were discharged nonroutinely without an operation to receive palliative care (3.7% vs. 7.0%; OR = 0.44, 95% CI, 0.34-0.57; P less than .0001).
Lastly, patients who received palliative care had shorter median hospital stays than did those who did not receive palliative care (5 days vs. 6 days; P less than .0001). These patients also had lower median hospital charges ($29,500 vs. $31,600; P = .0403).
The results identify two subsets of patients with unmet palliative care needs: patients requiring operative intervention, and patients with a diagnosis of intestinal ischemia, the authors said. In addition, the findings suggest that “surgeons should consider initiating palliative care … early in the hospital course for patients with dementia presenting with acute surgical abdomen,” they wrote.
“Both hip fracture and intensive care unit admission in patients with dementia have been described as appropriate triggers for palliative care assessment. ... Acute abdominal emergency [may also represent] an appropriate episode during which to introduce palliative care for patients with dementia,” they concluded.
The study was funded by the Rutgers New Jersey Medical School department of surgery and the New Jersey Medical School Hispanic Center of Excellence, Health Resources, and Services Administration. No other disclosures were reported.
SOURCE: Surgery. 2017 Dec 4. doi: 10.1016/j.surg.2017.09.048.
Few surgeons would argue that a patient with dementia and an acute abdomen would be less appropriate for a palliative care consultation than demented patients with a hip fracture or ICU admission who have been shown to benefit from triggered palliative care consults. However, the dynamic interaction between patient, family, and surgeon, described by Thomas Miner as the “palliative triangle,” will likely prevent universal acceptance of triggered consults (Ann Surg Oncol. 2002;9[7]:696-709). Despite the current trend of increasingly algorithmic care, there is still a need for surgeon autonomy for treatment decisions even when the recommended triggered intervention is highly appropriate. A mentor of mine put it, “I never do things routinely, but there are some things I do all the time.” As the benefits of palliative care become more evident, the referrals for palliative care for this latest indication will become “some things I do all the time” just as pharmacokinetics referrals have become for antibiotics, anticoagulation, and total parenteral nutrition.
Few surgeons would argue that a patient with dementia and an acute abdomen would be less appropriate for a palliative care consultation than demented patients with a hip fracture or ICU admission who have been shown to benefit from triggered palliative care consults. However, the dynamic interaction between patient, family, and surgeon, described by Thomas Miner as the “palliative triangle,” will likely prevent universal acceptance of triggered consults (Ann Surg Oncol. 2002;9[7]:696-709). Despite the current trend of increasingly algorithmic care, there is still a need for surgeon autonomy for treatment decisions even when the recommended triggered intervention is highly appropriate. A mentor of mine put it, “I never do things routinely, but there are some things I do all the time.” As the benefits of palliative care become more evident, the referrals for palliative care for this latest indication will become “some things I do all the time” just as pharmacokinetics referrals have become for antibiotics, anticoagulation, and total parenteral nutrition.
Few surgeons would argue that a patient with dementia and an acute abdomen would be less appropriate for a palliative care consultation than demented patients with a hip fracture or ICU admission who have been shown to benefit from triggered palliative care consults. However, the dynamic interaction between patient, family, and surgeon, described by Thomas Miner as the “palliative triangle,” will likely prevent universal acceptance of triggered consults (Ann Surg Oncol. 2002;9[7]:696-709). Despite the current trend of increasingly algorithmic care, there is still a need for surgeon autonomy for treatment decisions even when the recommended triggered intervention is highly appropriate. A mentor of mine put it, “I never do things routinely, but there are some things I do all the time.” As the benefits of palliative care become more evident, the referrals for palliative care for this latest indication will become “some things I do all the time” just as pharmacokinetics referrals have become for antibiotics, anticoagulation, and total parenteral nutrition.
Despite high rates of in-hospital mortality and nonroutine discharge, palliative care is underutilized in patients with dementia and acute abdominal emergency, according to findings published in Surgery.
“Currently little is known about palliative care utilization among patients with dementia in possible need of surgical intervention. This raises the question of whether the acute surgical emergency represents an appropriate episode during which to introduce palliative care for patients with dementia,” wrote Ana Berlin, MD, FACS, of the department of surgery at New Jersey Medical School, Newark, N.J., and her coauthors (Surgery. 2017 Dec 4. doi: 10.1016/j.surg.2017.09.048).
Of 15,209 patients aged 50 years and older with dementia and acute abdomen, 7.5% received palliative care. Patients discharged nonroutinely and patients treated operatively were less likely to receive palliative care, the researchers reported.
Dr. Berlin and her colleagues used the National Inpatient Sample database to identify patients with dementia and acute abdomen who were admitted nonelectively between 2009 and 2013. They used ICD-9 primary and secondary codes to limit surgical diagnoses to gastrointestinal obstruction, ischemia, and perforation.
Overall, 50.9% of patients were admitted for gastrointestinal obstruction, 39.8% for perforation, 5.1% for bowel ischemia, and 4.3% for mixed pathology; 17.8% of patients were managed operatively.
Patients with intestinal ischemia had the highest rate of both operation and mortality, at 22.8% and 27.6%, respectively. These patients also had the lowest rate of routine discharge, at 15.9%, the authors said. In comparison, patients with obstruction had surgical intervention and in-hospital mortality rates of 17% and 10.1%, respectively, and a routine discharge rate of 20.9%. Patients with perforation had an operation rate of 13.8%, in-hospital mortality rate of 6.8%, and routine discharge rate of 26.9%.
The palliative care utilization rate overall was 7.5%. Patients with mixed pathology who did not have surgery were most likely to receive palliative care, at 21.1%, noted Dr. Berlin and her coauthors.
Patients who died postoperatively were less likely than were those who died without surgical intervention to have received palliative care (20.9% vs. 31.4%; odds ratio = 0.63, 95% confidence interval, 0.46-0.86; P = .0039), and those who were discharged nonroutinely after an operation were less likely than were patients who were discharged nonroutinely without an operation to receive palliative care (3.7% vs. 7.0%; OR = 0.44, 95% CI, 0.34-0.57; P less than .0001).
Lastly, patients who received palliative care had shorter median hospital stays than did those who did not receive palliative care (5 days vs. 6 days; P less than .0001). These patients also had lower median hospital charges ($29,500 vs. $31,600; P = .0403).
The results identify two subsets of patients with unmet palliative care needs: patients requiring operative intervention, and patients with a diagnosis of intestinal ischemia, the authors said. In addition, the findings suggest that “surgeons should consider initiating palliative care … early in the hospital course for patients with dementia presenting with acute surgical abdomen,” they wrote.
“Both hip fracture and intensive care unit admission in patients with dementia have been described as appropriate triggers for palliative care assessment. ... Acute abdominal emergency [may also represent] an appropriate episode during which to introduce palliative care for patients with dementia,” they concluded.
The study was funded by the Rutgers New Jersey Medical School department of surgery and the New Jersey Medical School Hispanic Center of Excellence, Health Resources, and Services Administration. No other disclosures were reported.
SOURCE: Surgery. 2017 Dec 4. doi: 10.1016/j.surg.2017.09.048.
Despite high rates of in-hospital mortality and nonroutine discharge, palliative care is underutilized in patients with dementia and acute abdominal emergency, according to findings published in Surgery.
“Currently little is known about palliative care utilization among patients with dementia in possible need of surgical intervention. This raises the question of whether the acute surgical emergency represents an appropriate episode during which to introduce palliative care for patients with dementia,” wrote Ana Berlin, MD, FACS, of the department of surgery at New Jersey Medical School, Newark, N.J., and her coauthors (Surgery. 2017 Dec 4. doi: 10.1016/j.surg.2017.09.048).
Of 15,209 patients aged 50 years and older with dementia and acute abdomen, 7.5% received palliative care. Patients discharged nonroutinely and patients treated operatively were less likely to receive palliative care, the researchers reported.
Dr. Berlin and her colleagues used the National Inpatient Sample database to identify patients with dementia and acute abdomen who were admitted nonelectively between 2009 and 2013. They used ICD-9 primary and secondary codes to limit surgical diagnoses to gastrointestinal obstruction, ischemia, and perforation.
Overall, 50.9% of patients were admitted for gastrointestinal obstruction, 39.8% for perforation, 5.1% for bowel ischemia, and 4.3% for mixed pathology; 17.8% of patients were managed operatively.
Patients with intestinal ischemia had the highest rate of both operation and mortality, at 22.8% and 27.6%, respectively. These patients also had the lowest rate of routine discharge, at 15.9%, the authors said. In comparison, patients with obstruction had surgical intervention and in-hospital mortality rates of 17% and 10.1%, respectively, and a routine discharge rate of 20.9%. Patients with perforation had an operation rate of 13.8%, in-hospital mortality rate of 6.8%, and routine discharge rate of 26.9%.
The palliative care utilization rate overall was 7.5%. Patients with mixed pathology who did not have surgery were most likely to receive palliative care, at 21.1%, noted Dr. Berlin and her coauthors.
Patients who died postoperatively were less likely than were those who died without surgical intervention to have received palliative care (20.9% vs. 31.4%; odds ratio = 0.63, 95% confidence interval, 0.46-0.86; P = .0039), and those who were discharged nonroutinely after an operation were less likely than were patients who were discharged nonroutinely without an operation to receive palliative care (3.7% vs. 7.0%; OR = 0.44, 95% CI, 0.34-0.57; P less than .0001).
Lastly, patients who received palliative care had shorter median hospital stays than did those who did not receive palliative care (5 days vs. 6 days; P less than .0001). These patients also had lower median hospital charges ($29,500 vs. $31,600; P = .0403).
The results identify two subsets of patients with unmet palliative care needs: patients requiring operative intervention, and patients with a diagnosis of intestinal ischemia, the authors said. In addition, the findings suggest that “surgeons should consider initiating palliative care … early in the hospital course for patients with dementia presenting with acute surgical abdomen,” they wrote.
“Both hip fracture and intensive care unit admission in patients with dementia have been described as appropriate triggers for palliative care assessment. ... Acute abdominal emergency [may also represent] an appropriate episode during which to introduce palliative care for patients with dementia,” they concluded.
The study was funded by the Rutgers New Jersey Medical School department of surgery and the New Jersey Medical School Hispanic Center of Excellence, Health Resources, and Services Administration. No other disclosures were reported.
SOURCE: Surgery. 2017 Dec 4. doi: 10.1016/j.surg.2017.09.048.
FROM SURGERY
Key clinical point: Despite high mortality and frequent nonroutine discharges, palliative care is underutilized in dementia patients with acute abdominal emergency.
Major finding: Among dementia patients with acute abdominal emergency, 7.5% received palliative care.
Data source: A retrospective analysis of 15,209 patients aged 50 years and older from the National Inpatient Sample, for the period of 2009-2013.
Disclosures: The study was funded by the Rutgers New Jersey Medical School Department of Surgery and the New Jersey Medical School Hispanic Center of Excellence, Health Resources, and Services Administration.
SOURCE: Surgery. 2017 Dec 4. doi: http://dx.doi.org/10.1016/j.surg.2017.09.048.
Think before you Tweet: Social media guidelines for surgeons aim to prevent Internet regret
Think before you tweet. That’s what surgeons should remember before they express themselves on social media.
Anger and frustration can prompt ill-advised social media postings that have a big potential for blowback, Heather J. Logghe, MD, FACS, and her colleagues wrote in the Journal of the American College of Surgeons. But so can enthusiasm about posting about a new device or procedure, a fascination with a difficult case, the sense of relief that a patient made it though a harrowing period, or even just the simple joy of tossing back a beer or two with pals at the local watering hole (J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.11.022).
“In a survey of 48 state medical boards, 44 (92%) reported online-related misbehavior with serious disciplinary consequences leading to license restriction, suspension, or revocation. A 2011 study of ‘Physicians on Twitter’ revealed that 10% of the physicians sampled had tweeted potential patient privacy violations. A 2014 study of publicly available Facebook profiles of 319 Midwest residents found 14% had ‘potentially unprofessional content’ and 12.2% had ‘clearly unprofessional’ content, the latter including references to binge drinking, sexually suggestive photos, and HIPAA violations.”
Dr. Logghe, of Thomas Jefferson University, Philadelphia, is a member of the American College of Surgeons’ (ACS’s) social media committee tasked with creating practice recommendations for clinicians’ use of social media. Conducting a literature review was the first step to creating a surgeon-specific document, and the team found seven online behavior guidelines directed at physicians. Groups authoring these papers included the American Medical Association, the Federation of State Medical Boards, the American Congress of Obstetricians and Gynecologists, and several international groups.
Dr. Logghe and her colleagues reviewed each one, synthesized the information, and created a practice recommendation statement specific to the ACS. While not encoded in any professional ethics requirements, “Best Practices for Surgeons’ Social Media Use: Statement of the Resident and Associate Society of the American College of Surgeons” does lay out some common, potentially problematic scenarios and offers some suggestions about how to avoid Internet regret.
Everything discussed in the paper revolves around maintaining a decorous public persona. Professionalism on and off the clock is a key tenet of the recommendations. Definitions of key terms like “professionalism” are an important basis for any practice guideline, but sometimes concepts are not easy to define, the team wrote. “Perhaps the limitation most difficult to address in any formalized guideline is the necessary subjectivity in interpreting what is ‘appropriate’ or ‘professional’ online – or in any other setting,” the authors wrote. The ACS Code of Professional Conduct does not explicitly define either of those terms or discuss the appearance of unprofessional behavior.
In the absence of a plain-and-simple definition, the authors attempted to couch the social media recommendations in terms of ACS’s commitment to maintaining the patient trust. It urges surgeons to “avoid even the appearance of impropriety.”
The practice recommendations touch on a number of areas that are potentially problematic for surgeons, including confidentiality, financial conflicts, collegial support, and general social responsibility.
Confidentiality
Maintaining privacy is more than a courtesy to patients: It’s a federally mandated law with serious punitive repercussions if violated. Blogs, YouTube, Twitter, and Facebook offer a vast potential for sharing information with and educating the public, but postings can also easily violate HIPPA standards, the team wrote.
“In general, most social media platforms are not HIPPA-compliant,” no matter how the privacy settings are adjusted. These modes of communication are never appropriate for patient-physician communication: They can’t be archived in an electronic health record, and it is ill advised to give any medical advice by using these channels.
Discussing a particular case online, even with the usual defining details omitted, can be a bad idea.“Simply de-identifying patient information may not be sufficient. When posting information online, one must be cognizant of the context of other information available online. Such information includes the poster’s place of employment, news media, and publicly available vital statistics. Therefore even when posting general comments about hospital events, surgical cases, or patients under one’s care, it is essential to consider the sum of information available to the reader, rather than simply the information shared in the isolated post.”
Employment
Most employers have social media guidelines and don’t take kindly to violations – which can affect both current and future job postings. “A strong social media presence can be of benefit to one’s employer, [but] content that portrays a surgeon in an unprofessional or controversial light can be detrimental and even career-damaging.”
This reaches beyond professional communications online and deep into a surgeon’s personal life, the team noted, so exercise caution when “friending.”
“While this practice is inevitable, surgeons should be aware of potential conflicts. Connecting with or accepting friend requests from some but not all coworkers or coresidents could be interpreted as favoritism and may create a problematic work relationship. … Surgeons should consider primarily connecting with coworkers on professional websites if they have little contact with them outside the workplace.”
As for friending patients – just don’t, for both your sake and theirs. “Accepting a patient’s Facebook friend request may allow them access to events, details, and commentary not traditionally appropriate for the patient-physician relationship. Accepting such requests is strongly discouraged. If concerned about appearing rude or rejecting a patient’s request to be Facebook friends, the patient can be referred to society guidelines or best practices such as these.” One helpful alternative to such a request may be to invite patients to follow a practice website or other professional page.
Conflicts of interest
Online friends might not require disclosures when a surgeon posts about an exciting procedure or piece of equipment, such as whether there is a financial interest in doing so, but it’s important to be proactive. “As always, it is the physician’s responsibility to avoid even the appearance of impropriety. If it is not feasible to include a relevant conflict of interest within a post, the post should not be made.”
Defamation
Irritated about a colleague? Keep it to yourself – especially if you’ve had a beer. “It is never appropriate to post derogatory comments about patients or colleagues. Surgeons should be careful not to post in anger or under the influence of any substance. Statements about a colleague’s abilities, experience, or outcomes intended in jest may be appropriate for the surgeon’s lounge, yet entirely inappropriate for public consumption. Again, the ‘pause-before-posting’ practice is likely to prevent regretful posts in this vein.”
Privacy and Permanence
The Internet goes everywhere and lasts forever. A snappy quote that’s funny at 2 a.m. might not seem so hilarious in the light of day – or even in the light of a day 5 years yet to come.
The delete key is a false friend, and that clever pseudonym you dreamed up is probably as crackable as the classic “Pa55word” password. “One should presume that all content posted online will remain there forever and may be seen by anyone. Again, ‘pause-before-posting’ is a recommended practice.”
Privacy settings should be viewed as an illusion, the team noted. In this era of face recognition and tagging, images carry just as much risk as words.
Collegial support
Maybe your mother was right when she said, “This is for your own good.” If a colleague’s postings are getting out of hand, a tactful heart-to-heart might be the best course of action. “As coined by Dr. Sarah Mansfield, ‘Looking after colleagues is an integral element of professional conduct.’ Surgeons who notice colleagues posting unprofessional content that could be damaging to both the colleague and the public’s trust in the profession should discreetly express their concern to the individual, who should then take any appropriate corrective actions. … If the action is in violation of the law or medical board regulations, it should be reported to the appropriate governing bodies.”
Physician, Google Thyself
The team acknowledged that an online presence is virtually a must for professional development. And even if you don’t create a web page, chances are your university or hospital has done it for you. The media is interested in your life, too, and may make mention of your activities – both positive or negative.
“To better understand and control this publicly accessible information, surgeons are encouraged to periodically self-audit themselves online and taking measures to ensure that the information present is accurate and professional.” Some professional service websites are more trustworthy than others. The team encouraged physicians to participate in the ACS professional pages, LinkedIn, Doximity, and ResearchGate.
Not rules – just recommendations
The team stressed that their recommendations aren’t meant to stifle personal expression. Instead, their aim is to prompt a more conscious use of what can be a very powerful tool for both self-expression and professional development.
“The authors recommend no punitive action based on a perceived ‘violation’ of these recommendations alone. While they refer to other guidelines, including laws such as HIPAA, that must be appropriately enforced, these best practices are intended to guide the practicing surgeon in the use of social media rather than act as regulations or encourage reprimand. Rather than encouraging a social media landscape as sterile as the operating theater, the authors hope these recommendations lead to conscious consideration of online behavior, to avoidance of preventable harm, and to recognition of others’ views of their posts.”
None of the authors reported any financial disclosures.
SOURCE: Logghe HJ et al. J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.11.022.
As Editor of the ACS Communities, I am thrilled to see the RAS paper of social media recommendations. We who did not grow up with a keyboard in our hands can learn valuable and career-saving lessons from our younger colleagues who have had a lifetime of experience with social media.
There’s nothing like social media to get your thoughts “out there,” but the other side of the sword is excellently described in this article. I have seen or had to intervene on each of the subjects mentioned in it while reading through the thousands of posts that the ACS Communities’ users have generated over the last three-and-a-half years. When sitting in front of a screen, we can easily lose sight of the fact that our comments are going out into the real world and how rapidly they might reflect back on us and affect friends, relatives, employers, patients, foreign governments, cultures vastly different from our own, and other breathing, feeling human beings – in short, the entire universe hears regardless of whether the site is “password protected.”
I urge everyone using social media to read these guidelines, laminate them, and put them in their wallets, purses, or somewhere else that’s handy. Being self-aware and insightful in your posts can do a world of good, but a lack thereof can result in an avalanche of harm to yourself or others.
Tyler G. Hughes, MD, FACS, is a clinical professor in the department of surgery and the director of medical education at the Kansas University in Salina, Kan., as well as a Co-Editor of ACS Surgery News.
As Editor of the ACS Communities, I am thrilled to see the RAS paper of social media recommendations. We who did not grow up with a keyboard in our hands can learn valuable and career-saving lessons from our younger colleagues who have had a lifetime of experience with social media.
There’s nothing like social media to get your thoughts “out there,” but the other side of the sword is excellently described in this article. I have seen or had to intervene on each of the subjects mentioned in it while reading through the thousands of posts that the ACS Communities’ users have generated over the last three-and-a-half years. When sitting in front of a screen, we can easily lose sight of the fact that our comments are going out into the real world and how rapidly they might reflect back on us and affect friends, relatives, employers, patients, foreign governments, cultures vastly different from our own, and other breathing, feeling human beings – in short, the entire universe hears regardless of whether the site is “password protected.”
I urge everyone using social media to read these guidelines, laminate them, and put them in their wallets, purses, or somewhere else that’s handy. Being self-aware and insightful in your posts can do a world of good, but a lack thereof can result in an avalanche of harm to yourself or others.
Tyler G. Hughes, MD, FACS, is a clinical professor in the department of surgery and the director of medical education at the Kansas University in Salina, Kan., as well as a Co-Editor of ACS Surgery News.
As Editor of the ACS Communities, I am thrilled to see the RAS paper of social media recommendations. We who did not grow up with a keyboard in our hands can learn valuable and career-saving lessons from our younger colleagues who have had a lifetime of experience with social media.
There’s nothing like social media to get your thoughts “out there,” but the other side of the sword is excellently described in this article. I have seen or had to intervene on each of the subjects mentioned in it while reading through the thousands of posts that the ACS Communities’ users have generated over the last three-and-a-half years. When sitting in front of a screen, we can easily lose sight of the fact that our comments are going out into the real world and how rapidly they might reflect back on us and affect friends, relatives, employers, patients, foreign governments, cultures vastly different from our own, and other breathing, feeling human beings – in short, the entire universe hears regardless of whether the site is “password protected.”
I urge everyone using social media to read these guidelines, laminate them, and put them in their wallets, purses, or somewhere else that’s handy. Being self-aware and insightful in your posts can do a world of good, but a lack thereof can result in an avalanche of harm to yourself or others.
Tyler G. Hughes, MD, FACS, is a clinical professor in the department of surgery and the director of medical education at the Kansas University in Salina, Kan., as well as a Co-Editor of ACS Surgery News.
Think before you tweet. That’s what surgeons should remember before they express themselves on social media.
Anger and frustration can prompt ill-advised social media postings that have a big potential for blowback, Heather J. Logghe, MD, FACS, and her colleagues wrote in the Journal of the American College of Surgeons. But so can enthusiasm about posting about a new device or procedure, a fascination with a difficult case, the sense of relief that a patient made it though a harrowing period, or even just the simple joy of tossing back a beer or two with pals at the local watering hole (J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.11.022).
“In a survey of 48 state medical boards, 44 (92%) reported online-related misbehavior with serious disciplinary consequences leading to license restriction, suspension, or revocation. A 2011 study of ‘Physicians on Twitter’ revealed that 10% of the physicians sampled had tweeted potential patient privacy violations. A 2014 study of publicly available Facebook profiles of 319 Midwest residents found 14% had ‘potentially unprofessional content’ and 12.2% had ‘clearly unprofessional’ content, the latter including references to binge drinking, sexually suggestive photos, and HIPAA violations.”
Dr. Logghe, of Thomas Jefferson University, Philadelphia, is a member of the American College of Surgeons’ (ACS’s) social media committee tasked with creating practice recommendations for clinicians’ use of social media. Conducting a literature review was the first step to creating a surgeon-specific document, and the team found seven online behavior guidelines directed at physicians. Groups authoring these papers included the American Medical Association, the Federation of State Medical Boards, the American Congress of Obstetricians and Gynecologists, and several international groups.
Dr. Logghe and her colleagues reviewed each one, synthesized the information, and created a practice recommendation statement specific to the ACS. While not encoded in any professional ethics requirements, “Best Practices for Surgeons’ Social Media Use: Statement of the Resident and Associate Society of the American College of Surgeons” does lay out some common, potentially problematic scenarios and offers some suggestions about how to avoid Internet regret.
Everything discussed in the paper revolves around maintaining a decorous public persona. Professionalism on and off the clock is a key tenet of the recommendations. Definitions of key terms like “professionalism” are an important basis for any practice guideline, but sometimes concepts are not easy to define, the team wrote. “Perhaps the limitation most difficult to address in any formalized guideline is the necessary subjectivity in interpreting what is ‘appropriate’ or ‘professional’ online – or in any other setting,” the authors wrote. The ACS Code of Professional Conduct does not explicitly define either of those terms or discuss the appearance of unprofessional behavior.
In the absence of a plain-and-simple definition, the authors attempted to couch the social media recommendations in terms of ACS’s commitment to maintaining the patient trust. It urges surgeons to “avoid even the appearance of impropriety.”
The practice recommendations touch on a number of areas that are potentially problematic for surgeons, including confidentiality, financial conflicts, collegial support, and general social responsibility.
Confidentiality
Maintaining privacy is more than a courtesy to patients: It’s a federally mandated law with serious punitive repercussions if violated. Blogs, YouTube, Twitter, and Facebook offer a vast potential for sharing information with and educating the public, but postings can also easily violate HIPPA standards, the team wrote.
“In general, most social media platforms are not HIPPA-compliant,” no matter how the privacy settings are adjusted. These modes of communication are never appropriate for patient-physician communication: They can’t be archived in an electronic health record, and it is ill advised to give any medical advice by using these channels.
Discussing a particular case online, even with the usual defining details omitted, can be a bad idea.“Simply de-identifying patient information may not be sufficient. When posting information online, one must be cognizant of the context of other information available online. Such information includes the poster’s place of employment, news media, and publicly available vital statistics. Therefore even when posting general comments about hospital events, surgical cases, or patients under one’s care, it is essential to consider the sum of information available to the reader, rather than simply the information shared in the isolated post.”
Employment
Most employers have social media guidelines and don’t take kindly to violations – which can affect both current and future job postings. “A strong social media presence can be of benefit to one’s employer, [but] content that portrays a surgeon in an unprofessional or controversial light can be detrimental and even career-damaging.”
This reaches beyond professional communications online and deep into a surgeon’s personal life, the team noted, so exercise caution when “friending.”
“While this practice is inevitable, surgeons should be aware of potential conflicts. Connecting with or accepting friend requests from some but not all coworkers or coresidents could be interpreted as favoritism and may create a problematic work relationship. … Surgeons should consider primarily connecting with coworkers on professional websites if they have little contact with them outside the workplace.”
As for friending patients – just don’t, for both your sake and theirs. “Accepting a patient’s Facebook friend request may allow them access to events, details, and commentary not traditionally appropriate for the patient-physician relationship. Accepting such requests is strongly discouraged. If concerned about appearing rude or rejecting a patient’s request to be Facebook friends, the patient can be referred to society guidelines or best practices such as these.” One helpful alternative to such a request may be to invite patients to follow a practice website or other professional page.
Conflicts of interest
Online friends might not require disclosures when a surgeon posts about an exciting procedure or piece of equipment, such as whether there is a financial interest in doing so, but it’s important to be proactive. “As always, it is the physician’s responsibility to avoid even the appearance of impropriety. If it is not feasible to include a relevant conflict of interest within a post, the post should not be made.”
Defamation
Irritated about a colleague? Keep it to yourself – especially if you’ve had a beer. “It is never appropriate to post derogatory comments about patients or colleagues. Surgeons should be careful not to post in anger or under the influence of any substance. Statements about a colleague’s abilities, experience, or outcomes intended in jest may be appropriate for the surgeon’s lounge, yet entirely inappropriate for public consumption. Again, the ‘pause-before-posting’ practice is likely to prevent regretful posts in this vein.”
Privacy and Permanence
The Internet goes everywhere and lasts forever. A snappy quote that’s funny at 2 a.m. might not seem so hilarious in the light of day – or even in the light of a day 5 years yet to come.
The delete key is a false friend, and that clever pseudonym you dreamed up is probably as crackable as the classic “Pa55word” password. “One should presume that all content posted online will remain there forever and may be seen by anyone. Again, ‘pause-before-posting’ is a recommended practice.”
Privacy settings should be viewed as an illusion, the team noted. In this era of face recognition and tagging, images carry just as much risk as words.
Collegial support
Maybe your mother was right when she said, “This is for your own good.” If a colleague’s postings are getting out of hand, a tactful heart-to-heart might be the best course of action. “As coined by Dr. Sarah Mansfield, ‘Looking after colleagues is an integral element of professional conduct.’ Surgeons who notice colleagues posting unprofessional content that could be damaging to both the colleague and the public’s trust in the profession should discreetly express their concern to the individual, who should then take any appropriate corrective actions. … If the action is in violation of the law or medical board regulations, it should be reported to the appropriate governing bodies.”
Physician, Google Thyself
The team acknowledged that an online presence is virtually a must for professional development. And even if you don’t create a web page, chances are your university or hospital has done it for you. The media is interested in your life, too, and may make mention of your activities – both positive or negative.
“To better understand and control this publicly accessible information, surgeons are encouraged to periodically self-audit themselves online and taking measures to ensure that the information present is accurate and professional.” Some professional service websites are more trustworthy than others. The team encouraged physicians to participate in the ACS professional pages, LinkedIn, Doximity, and ResearchGate.
Not rules – just recommendations
The team stressed that their recommendations aren’t meant to stifle personal expression. Instead, their aim is to prompt a more conscious use of what can be a very powerful tool for both self-expression and professional development.
“The authors recommend no punitive action based on a perceived ‘violation’ of these recommendations alone. While they refer to other guidelines, including laws such as HIPAA, that must be appropriately enforced, these best practices are intended to guide the practicing surgeon in the use of social media rather than act as regulations or encourage reprimand. Rather than encouraging a social media landscape as sterile as the operating theater, the authors hope these recommendations lead to conscious consideration of online behavior, to avoidance of preventable harm, and to recognition of others’ views of their posts.”
None of the authors reported any financial disclosures.
SOURCE: Logghe HJ et al. J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.11.022.
Think before you tweet. That’s what surgeons should remember before they express themselves on social media.
Anger and frustration can prompt ill-advised social media postings that have a big potential for blowback, Heather J. Logghe, MD, FACS, and her colleagues wrote in the Journal of the American College of Surgeons. But so can enthusiasm about posting about a new device or procedure, a fascination with a difficult case, the sense of relief that a patient made it though a harrowing period, or even just the simple joy of tossing back a beer or two with pals at the local watering hole (J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.11.022).
“In a survey of 48 state medical boards, 44 (92%) reported online-related misbehavior with serious disciplinary consequences leading to license restriction, suspension, or revocation. A 2011 study of ‘Physicians on Twitter’ revealed that 10% of the physicians sampled had tweeted potential patient privacy violations. A 2014 study of publicly available Facebook profiles of 319 Midwest residents found 14% had ‘potentially unprofessional content’ and 12.2% had ‘clearly unprofessional’ content, the latter including references to binge drinking, sexually suggestive photos, and HIPAA violations.”
Dr. Logghe, of Thomas Jefferson University, Philadelphia, is a member of the American College of Surgeons’ (ACS’s) social media committee tasked with creating practice recommendations for clinicians’ use of social media. Conducting a literature review was the first step to creating a surgeon-specific document, and the team found seven online behavior guidelines directed at physicians. Groups authoring these papers included the American Medical Association, the Federation of State Medical Boards, the American Congress of Obstetricians and Gynecologists, and several international groups.
Dr. Logghe and her colleagues reviewed each one, synthesized the information, and created a practice recommendation statement specific to the ACS. While not encoded in any professional ethics requirements, “Best Practices for Surgeons’ Social Media Use: Statement of the Resident and Associate Society of the American College of Surgeons” does lay out some common, potentially problematic scenarios and offers some suggestions about how to avoid Internet regret.
Everything discussed in the paper revolves around maintaining a decorous public persona. Professionalism on and off the clock is a key tenet of the recommendations. Definitions of key terms like “professionalism” are an important basis for any practice guideline, but sometimes concepts are not easy to define, the team wrote. “Perhaps the limitation most difficult to address in any formalized guideline is the necessary subjectivity in interpreting what is ‘appropriate’ or ‘professional’ online – or in any other setting,” the authors wrote. The ACS Code of Professional Conduct does not explicitly define either of those terms or discuss the appearance of unprofessional behavior.
In the absence of a plain-and-simple definition, the authors attempted to couch the social media recommendations in terms of ACS’s commitment to maintaining the patient trust. It urges surgeons to “avoid even the appearance of impropriety.”
The practice recommendations touch on a number of areas that are potentially problematic for surgeons, including confidentiality, financial conflicts, collegial support, and general social responsibility.
Confidentiality
Maintaining privacy is more than a courtesy to patients: It’s a federally mandated law with serious punitive repercussions if violated. Blogs, YouTube, Twitter, and Facebook offer a vast potential for sharing information with and educating the public, but postings can also easily violate HIPPA standards, the team wrote.
“In general, most social media platforms are not HIPPA-compliant,” no matter how the privacy settings are adjusted. These modes of communication are never appropriate for patient-physician communication: They can’t be archived in an electronic health record, and it is ill advised to give any medical advice by using these channels.
Discussing a particular case online, even with the usual defining details omitted, can be a bad idea.“Simply de-identifying patient information may not be sufficient. When posting information online, one must be cognizant of the context of other information available online. Such information includes the poster’s place of employment, news media, and publicly available vital statistics. Therefore even when posting general comments about hospital events, surgical cases, or patients under one’s care, it is essential to consider the sum of information available to the reader, rather than simply the information shared in the isolated post.”
Employment
Most employers have social media guidelines and don’t take kindly to violations – which can affect both current and future job postings. “A strong social media presence can be of benefit to one’s employer, [but] content that portrays a surgeon in an unprofessional or controversial light can be detrimental and even career-damaging.”
This reaches beyond professional communications online and deep into a surgeon’s personal life, the team noted, so exercise caution when “friending.”
“While this practice is inevitable, surgeons should be aware of potential conflicts. Connecting with or accepting friend requests from some but not all coworkers or coresidents could be interpreted as favoritism and may create a problematic work relationship. … Surgeons should consider primarily connecting with coworkers on professional websites if they have little contact with them outside the workplace.”
As for friending patients – just don’t, for both your sake and theirs. “Accepting a patient’s Facebook friend request may allow them access to events, details, and commentary not traditionally appropriate for the patient-physician relationship. Accepting such requests is strongly discouraged. If concerned about appearing rude or rejecting a patient’s request to be Facebook friends, the patient can be referred to society guidelines or best practices such as these.” One helpful alternative to such a request may be to invite patients to follow a practice website or other professional page.
Conflicts of interest
Online friends might not require disclosures when a surgeon posts about an exciting procedure or piece of equipment, such as whether there is a financial interest in doing so, but it’s important to be proactive. “As always, it is the physician’s responsibility to avoid even the appearance of impropriety. If it is not feasible to include a relevant conflict of interest within a post, the post should not be made.”
Defamation
Irritated about a colleague? Keep it to yourself – especially if you’ve had a beer. “It is never appropriate to post derogatory comments about patients or colleagues. Surgeons should be careful not to post in anger or under the influence of any substance. Statements about a colleague’s abilities, experience, or outcomes intended in jest may be appropriate for the surgeon’s lounge, yet entirely inappropriate for public consumption. Again, the ‘pause-before-posting’ practice is likely to prevent regretful posts in this vein.”
Privacy and Permanence
The Internet goes everywhere and lasts forever. A snappy quote that’s funny at 2 a.m. might not seem so hilarious in the light of day – or even in the light of a day 5 years yet to come.
The delete key is a false friend, and that clever pseudonym you dreamed up is probably as crackable as the classic “Pa55word” password. “One should presume that all content posted online will remain there forever and may be seen by anyone. Again, ‘pause-before-posting’ is a recommended practice.”
Privacy settings should be viewed as an illusion, the team noted. In this era of face recognition and tagging, images carry just as much risk as words.
Collegial support
Maybe your mother was right when she said, “This is for your own good.” If a colleague’s postings are getting out of hand, a tactful heart-to-heart might be the best course of action. “As coined by Dr. Sarah Mansfield, ‘Looking after colleagues is an integral element of professional conduct.’ Surgeons who notice colleagues posting unprofessional content that could be damaging to both the colleague and the public’s trust in the profession should discreetly express their concern to the individual, who should then take any appropriate corrective actions. … If the action is in violation of the law or medical board regulations, it should be reported to the appropriate governing bodies.”
Physician, Google Thyself
The team acknowledged that an online presence is virtually a must for professional development. And even if you don’t create a web page, chances are your university or hospital has done it for you. The media is interested in your life, too, and may make mention of your activities – both positive or negative.
“To better understand and control this publicly accessible information, surgeons are encouraged to periodically self-audit themselves online and taking measures to ensure that the information present is accurate and professional.” Some professional service websites are more trustworthy than others. The team encouraged physicians to participate in the ACS professional pages, LinkedIn, Doximity, and ResearchGate.
Not rules – just recommendations
The team stressed that their recommendations aren’t meant to stifle personal expression. Instead, their aim is to prompt a more conscious use of what can be a very powerful tool for both self-expression and professional development.
“The authors recommend no punitive action based on a perceived ‘violation’ of these recommendations alone. While they refer to other guidelines, including laws such as HIPAA, that must be appropriately enforced, these best practices are intended to guide the practicing surgeon in the use of social media rather than act as regulations or encourage reprimand. Rather than encouraging a social media landscape as sterile as the operating theater, the authors hope these recommendations lead to conscious consideration of online behavior, to avoidance of preventable harm, and to recognition of others’ views of their posts.”
None of the authors reported any financial disclosures.
SOURCE: Logghe HJ et al. J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.11.022.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS










