User login
Official Newspaper of the American College of Surgeons
USPSTF goes neutral on adolescent scoliosis screening
The U.S. Preventive Services Task Force neither recommended for nor recommended against routine screening for adolescent idiopathic scoliosis in new guidelines published Jan. 9 in JAMA.
The determination applies to asymptomatic adolescents 10-18 years old; it does not apply to children and adolescents who present with back pain, breathing difficulties, obvious spine deformities, or abnormal imaging.
Studies since then, however, have shifted the calculus a bit so that the group “no longer has moderate certainty that the harms of treatment outweigh the benefits ... As a result, the USPSTF has determined that the current evidence is insufficient to assess the balance of benefits and harms of screening for adolescent idiopathic scoliosis,” which led the group to issue an “I statement” for “insufficient evidence,” David C. Grossman, MD, MPH, of Kaiser Permanente
Washington Health Research Institute, Seattle, and the other members of the task force wrote.
An I statement means that “if the service is offered, patients should understand the uncertainty about the balance of benefits and harms ... The USPSTF recognizes that clinical decisions involve more considerations than evidence alone. Clinicians should understand the evidence but individualize decision making to the specific patient or situation.”
The task force did find that screening using the forward bend test, scoliometer, or both with radiologic confirmation does a good job at detecting scoliosis. It also found a growing body of evidence that bracing can interrupt or slow scoliosis progression; “however, evidence on whether reducing spinal curvature in adolescence has a long-term effect on health in adulthood is inadequate,” and “evidence on the effects of exercise and surgery on health or spinal curvature in childhood or adulthood is insufficient.” Also, the majority of individuals identified through screening will never require treatment, the task force said.
The guidance is based on a review of 448,276 subjects in 14 studies, more than half of which were published after the last guidance.
USPSTF noted that limited new evidence suggests curves “may respond similarly to physiotherapeutic, scoliosis-specific exercise treatment; if confirmed, this may represent a treatment option for mild curves before bracing is recommended.”
Meanwhile, “surgical treatment remains the standard of care for curves that progress to greater than 40-50 degrees; however, there are no controlled studies of surgical [versus] nonsurgical treatment in individuals with lower degrees of curvature,” the task force said in an evidence review that was also published Jan. 9 in JAMA and was led by pediatrician John Dunn, MD, of Kaiser Permanente Washington Health Research Institute, Seattle.
More than half of US states either mandate or recommend school-based screening for scoliosis. The American Academy of Orthopaedic Surgeons, the Scoliosis Research Society, the Pediatric Orthopaedic Society of North America, and the American Academy of Pediatrics advocate screening for scoliosis in girls at 10 and 12 years and in male adolescents at either 13 or 14 years as part of medical home preventive services. The United Kingdom National Screening Society does not recommend screening for scoliosis given the uncertainty surrounding the effectiveness of screening and treatment.
The work was funded by the Agency for Healthcare Research and Quality. The authors had no relevant disclosures.
SOURCE: US Preventive Services Task Force. JAMA. 2018 Jan 9;319(2):165-72; Dunn J et al. JAMA. 2018;319(2):173-87.
Twenty or more states, including highly populous states such as California, New York, Ohio, and Texas, mandate or strongly recommend school-based screening for scoliosis ... Given the new USPSTF recommendations and the I statement [suggesting insufficient evidence], it would be appropriate for states to advise students and parents of the insufficient data about benefits and harms of screening, while also sharing more recent evidence that bracing and exercise therapies may be helpful if scoliosis is clinically diagnosed in screen-positive youth.
The broad lack of evidence regarding the short-term effect of screening for adolescents and long-term health outcomes in later adolescence and into adulthood is a clear obstacle to moving adolescent idiopathic scoliosis recommendations beyond the I rating. Consequently, the gaps in current understanding serve to highlight immediate opportunities for clinical and health services research. For example, a multisite, multiyear observational study could provide evidence about the association between reduction in spinal curvature in adolescence and long-term health outcomes.
John Sarwark, MD , is head of orthopedic surgery at Ann & Robert H. Lurie Children’s Hospital and a professor of orthopedic surgery at Northwestern University, both in Chicago. Matthew Davis, MD , is head of academic general pediatrics and primary care at Lurie and a pediatrics professor at Northwestern. They made their comments in an editorial published Jan. 9 in JAMA and were not involved with the work ( 2018;319(2):127-129) .
Twenty or more states, including highly populous states such as California, New York, Ohio, and Texas, mandate or strongly recommend school-based screening for scoliosis ... Given the new USPSTF recommendations and the I statement [suggesting insufficient evidence], it would be appropriate for states to advise students and parents of the insufficient data about benefits and harms of screening, while also sharing more recent evidence that bracing and exercise therapies may be helpful if scoliosis is clinically diagnosed in screen-positive youth.
The broad lack of evidence regarding the short-term effect of screening for adolescents and long-term health outcomes in later adolescence and into adulthood is a clear obstacle to moving adolescent idiopathic scoliosis recommendations beyond the I rating. Consequently, the gaps in current understanding serve to highlight immediate opportunities for clinical and health services research. For example, a multisite, multiyear observational study could provide evidence about the association between reduction in spinal curvature in adolescence and long-term health outcomes.
John Sarwark, MD , is head of orthopedic surgery at Ann & Robert H. Lurie Children’s Hospital and a professor of orthopedic surgery at Northwestern University, both in Chicago. Matthew Davis, MD , is head of academic general pediatrics and primary care at Lurie and a pediatrics professor at Northwestern. They made their comments in an editorial published Jan. 9 in JAMA and were not involved with the work ( 2018;319(2):127-129) .
Twenty or more states, including highly populous states such as California, New York, Ohio, and Texas, mandate or strongly recommend school-based screening for scoliosis ... Given the new USPSTF recommendations and the I statement [suggesting insufficient evidence], it would be appropriate for states to advise students and parents of the insufficient data about benefits and harms of screening, while also sharing more recent evidence that bracing and exercise therapies may be helpful if scoliosis is clinically diagnosed in screen-positive youth.
The broad lack of evidence regarding the short-term effect of screening for adolescents and long-term health outcomes in later adolescence and into adulthood is a clear obstacle to moving adolescent idiopathic scoliosis recommendations beyond the I rating. Consequently, the gaps in current understanding serve to highlight immediate opportunities for clinical and health services research. For example, a multisite, multiyear observational study could provide evidence about the association between reduction in spinal curvature in adolescence and long-term health outcomes.
John Sarwark, MD , is head of orthopedic surgery at Ann & Robert H. Lurie Children’s Hospital and a professor of orthopedic surgery at Northwestern University, both in Chicago. Matthew Davis, MD , is head of academic general pediatrics and primary care at Lurie and a pediatrics professor at Northwestern. They made their comments in an editorial published Jan. 9 in JAMA and were not involved with the work ( 2018;319(2):127-129) .
The U.S. Preventive Services Task Force neither recommended for nor recommended against routine screening for adolescent idiopathic scoliosis in new guidelines published Jan. 9 in JAMA.
The determination applies to asymptomatic adolescents 10-18 years old; it does not apply to children and adolescents who present with back pain, breathing difficulties, obvious spine deformities, or abnormal imaging.
Studies since then, however, have shifted the calculus a bit so that the group “no longer has moderate certainty that the harms of treatment outweigh the benefits ... As a result, the USPSTF has determined that the current evidence is insufficient to assess the balance of benefits and harms of screening for adolescent idiopathic scoliosis,” which led the group to issue an “I statement” for “insufficient evidence,” David C. Grossman, MD, MPH, of Kaiser Permanente
Washington Health Research Institute, Seattle, and the other members of the task force wrote.
An I statement means that “if the service is offered, patients should understand the uncertainty about the balance of benefits and harms ... The USPSTF recognizes that clinical decisions involve more considerations than evidence alone. Clinicians should understand the evidence but individualize decision making to the specific patient or situation.”
The task force did find that screening using the forward bend test, scoliometer, or both with radiologic confirmation does a good job at detecting scoliosis. It also found a growing body of evidence that bracing can interrupt or slow scoliosis progression; “however, evidence on whether reducing spinal curvature in adolescence has a long-term effect on health in adulthood is inadequate,” and “evidence on the effects of exercise and surgery on health or spinal curvature in childhood or adulthood is insufficient.” Also, the majority of individuals identified through screening will never require treatment, the task force said.
The guidance is based on a review of 448,276 subjects in 14 studies, more than half of which were published after the last guidance.
USPSTF noted that limited new evidence suggests curves “may respond similarly to physiotherapeutic, scoliosis-specific exercise treatment; if confirmed, this may represent a treatment option for mild curves before bracing is recommended.”
Meanwhile, “surgical treatment remains the standard of care for curves that progress to greater than 40-50 degrees; however, there are no controlled studies of surgical [versus] nonsurgical treatment in individuals with lower degrees of curvature,” the task force said in an evidence review that was also published Jan. 9 in JAMA and was led by pediatrician John Dunn, MD, of Kaiser Permanente Washington Health Research Institute, Seattle.
More than half of US states either mandate or recommend school-based screening for scoliosis. The American Academy of Orthopaedic Surgeons, the Scoliosis Research Society, the Pediatric Orthopaedic Society of North America, and the American Academy of Pediatrics advocate screening for scoliosis in girls at 10 and 12 years and in male adolescents at either 13 or 14 years as part of medical home preventive services. The United Kingdom National Screening Society does not recommend screening for scoliosis given the uncertainty surrounding the effectiveness of screening and treatment.
The work was funded by the Agency for Healthcare Research and Quality. The authors had no relevant disclosures.
SOURCE: US Preventive Services Task Force. JAMA. 2018 Jan 9;319(2):165-72; Dunn J et al. JAMA. 2018;319(2):173-87.
The U.S. Preventive Services Task Force neither recommended for nor recommended against routine screening for adolescent idiopathic scoliosis in new guidelines published Jan. 9 in JAMA.
The determination applies to asymptomatic adolescents 10-18 years old; it does not apply to children and adolescents who present with back pain, breathing difficulties, obvious spine deformities, or abnormal imaging.
Studies since then, however, have shifted the calculus a bit so that the group “no longer has moderate certainty that the harms of treatment outweigh the benefits ... As a result, the USPSTF has determined that the current evidence is insufficient to assess the balance of benefits and harms of screening for adolescent idiopathic scoliosis,” which led the group to issue an “I statement” for “insufficient evidence,” David C. Grossman, MD, MPH, of Kaiser Permanente
Washington Health Research Institute, Seattle, and the other members of the task force wrote.
An I statement means that “if the service is offered, patients should understand the uncertainty about the balance of benefits and harms ... The USPSTF recognizes that clinical decisions involve more considerations than evidence alone. Clinicians should understand the evidence but individualize decision making to the specific patient or situation.”
The task force did find that screening using the forward bend test, scoliometer, or both with radiologic confirmation does a good job at detecting scoliosis. It also found a growing body of evidence that bracing can interrupt or slow scoliosis progression; “however, evidence on whether reducing spinal curvature in adolescence has a long-term effect on health in adulthood is inadequate,” and “evidence on the effects of exercise and surgery on health or spinal curvature in childhood or adulthood is insufficient.” Also, the majority of individuals identified through screening will never require treatment, the task force said.
The guidance is based on a review of 448,276 subjects in 14 studies, more than half of which were published after the last guidance.
USPSTF noted that limited new evidence suggests curves “may respond similarly to physiotherapeutic, scoliosis-specific exercise treatment; if confirmed, this may represent a treatment option for mild curves before bracing is recommended.”
Meanwhile, “surgical treatment remains the standard of care for curves that progress to greater than 40-50 degrees; however, there are no controlled studies of surgical [versus] nonsurgical treatment in individuals with lower degrees of curvature,” the task force said in an evidence review that was also published Jan. 9 in JAMA and was led by pediatrician John Dunn, MD, of Kaiser Permanente Washington Health Research Institute, Seattle.
More than half of US states either mandate or recommend school-based screening for scoliosis. The American Academy of Orthopaedic Surgeons, the Scoliosis Research Society, the Pediatric Orthopaedic Society of North America, and the American Academy of Pediatrics advocate screening for scoliosis in girls at 10 and 12 years and in male adolescents at either 13 or 14 years as part of medical home preventive services. The United Kingdom National Screening Society does not recommend screening for scoliosis given the uncertainty surrounding the effectiveness of screening and treatment.
The work was funded by the Agency for Healthcare Research and Quality. The authors had no relevant disclosures.
SOURCE: US Preventive Services Task Force. JAMA. 2018 Jan 9;319(2):165-72; Dunn J et al. JAMA. 2018;319(2):173-87.
FROM JAMA
Clinical Trial: The Checklist to Prevent MRSA Surgical Site Infections
who are undergoing or have undergone cardiac surgery or total joint arthroplasty.
The Department of Veteran Affairs has previously implemented the VA MRSA Prevention Initiative, which successfully reduced patient-to-patient MRSA transmission; however, this initiative does not prevent most MRSA surgical site infections, which are spread differently. The VA has developed a new checklist which will be tested in this study aimed at reducing MRSA surgical site infections (SSIs), and will be implemented at 10 VA medical centers.
The primary outcome measure is superficial and deep/organ space MRSA infections within 90 days of operation. Secondary outcome measures include superficial and deep/organ space MRSA infections within 1 year of operation, presurgical bundle and individual bundle components compliance for 30 days prior to operation, length of postoperative stay, all-cause mortality 1 year after surgery, readmission within 90 days of surgery, and mupirocin and chlorhexidine resistance 30 days presurgery to 90 days postsurgery.
The study will end in April 2019. More than 10,000 people are expected to be included in the final analysis.
Find more information on the study page at Clinicaltrials.gov.
who are undergoing or have undergone cardiac surgery or total joint arthroplasty.
The Department of Veteran Affairs has previously implemented the VA MRSA Prevention Initiative, which successfully reduced patient-to-patient MRSA transmission; however, this initiative does not prevent most MRSA surgical site infections, which are spread differently. The VA has developed a new checklist which will be tested in this study aimed at reducing MRSA surgical site infections (SSIs), and will be implemented at 10 VA medical centers.
The primary outcome measure is superficial and deep/organ space MRSA infections within 90 days of operation. Secondary outcome measures include superficial and deep/organ space MRSA infections within 1 year of operation, presurgical bundle and individual bundle components compliance for 30 days prior to operation, length of postoperative stay, all-cause mortality 1 year after surgery, readmission within 90 days of surgery, and mupirocin and chlorhexidine resistance 30 days presurgery to 90 days postsurgery.
The study will end in April 2019. More than 10,000 people are expected to be included in the final analysis.
Find more information on the study page at Clinicaltrials.gov.
who are undergoing or have undergone cardiac surgery or total joint arthroplasty.
The Department of Veteran Affairs has previously implemented the VA MRSA Prevention Initiative, which successfully reduced patient-to-patient MRSA transmission; however, this initiative does not prevent most MRSA surgical site infections, which are spread differently. The VA has developed a new checklist which will be tested in this study aimed at reducing MRSA surgical site infections (SSIs), and will be implemented at 10 VA medical centers.
The primary outcome measure is superficial and deep/organ space MRSA infections within 90 days of operation. Secondary outcome measures include superficial and deep/organ space MRSA infections within 1 year of operation, presurgical bundle and individual bundle components compliance for 30 days prior to operation, length of postoperative stay, all-cause mortality 1 year after surgery, readmission within 90 days of surgery, and mupirocin and chlorhexidine resistance 30 days presurgery to 90 days postsurgery.
The study will end in April 2019. More than 10,000 people are expected to be included in the final analysis.
Find more information on the study page at Clinicaltrials.gov.
FROM CLINICALTRIALS.GOV
MSQC quality recommendations improve SSI in colectomy patients
The rate of patients decreased as hospitals implemented three specific care measures promoted by the Michigan Surgical Quality Collaborative, according to a study funded by the Blue Cross Blue Shield of Michigan.
With surgical site infections (SSIs) after colectomy associated with high morbidity as the second leading hospital acquired infection, and costing the health care system approximately $315 million annually, investment in this quality improvement program could ease a tremendous burden, according to Joceline V. Vu, MD, general surgery resident at the University of Michigan, Ann Arbor, and fellow investigators. The study was published in the Journal of the American College of Surgeons (2018 Jan;226[1]:91-99).
The study cohort included 5,742 colectomy patients at 1 of 52 hospitals associated with the Michigan Surgical Quality Collaborative (MSQC) between 2012 and 2016. Investigators assessed the use of the MSQC-recommended care bundle – cefazolin/metronidazole, oral antibiotics with mechanical bowel preparation, and postoperative day-1 glucose less than or equal to 140 mg/dL – and the impact of the bundle components on surgical site infection (SSI).
Patients were also split into groups based on the use of perioperative treatments previously found to be associated with SSI improvement, which included the three treatments in the care bundle as well as postoperative normothermia, minimally invasive surgery, and operative duration defined as either less than or greater than 100 minutes.
Those who had received these perioperative measures were given one point for each measure received.
Of the total, 8.1% of patients received 0-1 point, 22.2% received 2 points, 31.7% received 3 points, 27.2% received 4 points, and 10.7% received 5-6 points.
Patients were split relatively evenly between male and female, and the majority of patients were white across all six SSI perioperative groups.
Patients with 0-1 point were more likely to be older than 65 years (56.4%), while those who received 5-6 points were more likely to be between 45 and 64 years old (45.6% [P less than .001]).
Hospitals increased the use of three of the promoted processes (cefazolin/metronidazole, oral antibiotics with mechanical bowel preparation, and normoglycemia) during 2012-2016, and average use scores for patients went from 1.1 to 1.5 (P less than .001), according to investigators. As the rate of cefazolin/metronidazole and oral antibiotics with mechanical bowel preparation use rose from 18.6% and 42.9%, respectively, to 32.3% and 62.0% (P less than .001), SSI rates fell from 6.7% to 3.9% (P = .012) during the same period. The change in the normoglycemia rate (48.9% to 57.7%) was not significant (P = .112).
Hospitals that used all six recommended items saw a slightly decreased rate of SSI (r = –.39) between 2012 and 2016, according to Dr. Vu and her colleagues. Patients who received more measures had lower rates of complications, with SSI rates at 5.7% for those with 0-1 point, compared with 1.1% in those with 5-6 (P less than .001).
Rates of sepsis, pneumonia, emergency department visits, readmission, reoperation, and morbidity were also significantly lower.
“The MSQC and other collaborative quality improvement organizations represent a step toward this vision [of a learning health care system],” according to Dr. Vu and her colleagues. “Collaborating organizations can identify problems in care, adopt practice changes, and analyze the effect of those changes in a timely fashion.”
The findings of this study may be limited by a selection bias of how many bundle procedures a patient received based on comorbidities such as chronic obstructive pulmonary disease, hypertension, and obesity, which were all higher among those with fewer points. Investigators were also unable to discern causality of certain results because of the observational nature of the study. Hospitals included in the cohort volunteered to use the MSQC infrastructure, which may have limited the generalizability of the study,
Investigators reported no relevant financial disclosures. The study was funded by the Blue Cross Blue Shield of Michigan.
SOURCE: Vu, J V et al. J Am Coll Surg. 2018 Jan;226(1):91-9.
The rate of patients decreased as hospitals implemented three specific care measures promoted by the Michigan Surgical Quality Collaborative, according to a study funded by the Blue Cross Blue Shield of Michigan.
With surgical site infections (SSIs) after colectomy associated with high morbidity as the second leading hospital acquired infection, and costing the health care system approximately $315 million annually, investment in this quality improvement program could ease a tremendous burden, according to Joceline V. Vu, MD, general surgery resident at the University of Michigan, Ann Arbor, and fellow investigators. The study was published in the Journal of the American College of Surgeons (2018 Jan;226[1]:91-99).
The study cohort included 5,742 colectomy patients at 1 of 52 hospitals associated with the Michigan Surgical Quality Collaborative (MSQC) between 2012 and 2016. Investigators assessed the use of the MSQC-recommended care bundle – cefazolin/metronidazole, oral antibiotics with mechanical bowel preparation, and postoperative day-1 glucose less than or equal to 140 mg/dL – and the impact of the bundle components on surgical site infection (SSI).
Patients were also split into groups based on the use of perioperative treatments previously found to be associated with SSI improvement, which included the three treatments in the care bundle as well as postoperative normothermia, minimally invasive surgery, and operative duration defined as either less than or greater than 100 minutes.
Those who had received these perioperative measures were given one point for each measure received.
Of the total, 8.1% of patients received 0-1 point, 22.2% received 2 points, 31.7% received 3 points, 27.2% received 4 points, and 10.7% received 5-6 points.
Patients were split relatively evenly between male and female, and the majority of patients were white across all six SSI perioperative groups.
Patients with 0-1 point were more likely to be older than 65 years (56.4%), while those who received 5-6 points were more likely to be between 45 and 64 years old (45.6% [P less than .001]).
Hospitals increased the use of three of the promoted processes (cefazolin/metronidazole, oral antibiotics with mechanical bowel preparation, and normoglycemia) during 2012-2016, and average use scores for patients went from 1.1 to 1.5 (P less than .001), according to investigators. As the rate of cefazolin/metronidazole and oral antibiotics with mechanical bowel preparation use rose from 18.6% and 42.9%, respectively, to 32.3% and 62.0% (P less than .001), SSI rates fell from 6.7% to 3.9% (P = .012) during the same period. The change in the normoglycemia rate (48.9% to 57.7%) was not significant (P = .112).
Hospitals that used all six recommended items saw a slightly decreased rate of SSI (r = –.39) between 2012 and 2016, according to Dr. Vu and her colleagues. Patients who received more measures had lower rates of complications, with SSI rates at 5.7% for those with 0-1 point, compared with 1.1% in those with 5-6 (P less than .001).
Rates of sepsis, pneumonia, emergency department visits, readmission, reoperation, and morbidity were also significantly lower.
“The MSQC and other collaborative quality improvement organizations represent a step toward this vision [of a learning health care system],” according to Dr. Vu and her colleagues. “Collaborating organizations can identify problems in care, adopt practice changes, and analyze the effect of those changes in a timely fashion.”
The findings of this study may be limited by a selection bias of how many bundle procedures a patient received based on comorbidities such as chronic obstructive pulmonary disease, hypertension, and obesity, which were all higher among those with fewer points. Investigators were also unable to discern causality of certain results because of the observational nature of the study. Hospitals included in the cohort volunteered to use the MSQC infrastructure, which may have limited the generalizability of the study,
Investigators reported no relevant financial disclosures. The study was funded by the Blue Cross Blue Shield of Michigan.
SOURCE: Vu, J V et al. J Am Coll Surg. 2018 Jan;226(1):91-9.
The rate of patients decreased as hospitals implemented three specific care measures promoted by the Michigan Surgical Quality Collaborative, according to a study funded by the Blue Cross Blue Shield of Michigan.
With surgical site infections (SSIs) after colectomy associated with high morbidity as the second leading hospital acquired infection, and costing the health care system approximately $315 million annually, investment in this quality improvement program could ease a tremendous burden, according to Joceline V. Vu, MD, general surgery resident at the University of Michigan, Ann Arbor, and fellow investigators. The study was published in the Journal of the American College of Surgeons (2018 Jan;226[1]:91-99).
The study cohort included 5,742 colectomy patients at 1 of 52 hospitals associated with the Michigan Surgical Quality Collaborative (MSQC) between 2012 and 2016. Investigators assessed the use of the MSQC-recommended care bundle – cefazolin/metronidazole, oral antibiotics with mechanical bowel preparation, and postoperative day-1 glucose less than or equal to 140 mg/dL – and the impact of the bundle components on surgical site infection (SSI).
Patients were also split into groups based on the use of perioperative treatments previously found to be associated with SSI improvement, which included the three treatments in the care bundle as well as postoperative normothermia, minimally invasive surgery, and operative duration defined as either less than or greater than 100 minutes.
Those who had received these perioperative measures were given one point for each measure received.
Of the total, 8.1% of patients received 0-1 point, 22.2% received 2 points, 31.7% received 3 points, 27.2% received 4 points, and 10.7% received 5-6 points.
Patients were split relatively evenly between male and female, and the majority of patients were white across all six SSI perioperative groups.
Patients with 0-1 point were more likely to be older than 65 years (56.4%), while those who received 5-6 points were more likely to be between 45 and 64 years old (45.6% [P less than .001]).
Hospitals increased the use of three of the promoted processes (cefazolin/metronidazole, oral antibiotics with mechanical bowel preparation, and normoglycemia) during 2012-2016, and average use scores for patients went from 1.1 to 1.5 (P less than .001), according to investigators. As the rate of cefazolin/metronidazole and oral antibiotics with mechanical bowel preparation use rose from 18.6% and 42.9%, respectively, to 32.3% and 62.0% (P less than .001), SSI rates fell from 6.7% to 3.9% (P = .012) during the same period. The change in the normoglycemia rate (48.9% to 57.7%) was not significant (P = .112).
Hospitals that used all six recommended items saw a slightly decreased rate of SSI (r = –.39) between 2012 and 2016, according to Dr. Vu and her colleagues. Patients who received more measures had lower rates of complications, with SSI rates at 5.7% for those with 0-1 point, compared with 1.1% in those with 5-6 (P less than .001).
Rates of sepsis, pneumonia, emergency department visits, readmission, reoperation, and morbidity were also significantly lower.
“The MSQC and other collaborative quality improvement organizations represent a step toward this vision [of a learning health care system],” according to Dr. Vu and her colleagues. “Collaborating organizations can identify problems in care, adopt practice changes, and analyze the effect of those changes in a timely fashion.”
The findings of this study may be limited by a selection bias of how many bundle procedures a patient received based on comorbidities such as chronic obstructive pulmonary disease, hypertension, and obesity, which were all higher among those with fewer points. Investigators were also unable to discern causality of certain results because of the observational nature of the study. Hospitals included in the cohort volunteered to use the MSQC infrastructure, which may have limited the generalizability of the study,
Investigators reported no relevant financial disclosures. The study was funded by the Blue Cross Blue Shield of Michigan.
SOURCE: Vu, J V et al. J Am Coll Surg. 2018 Jan;226(1):91-9.
Key clinical point: Promotion of quality improvement bundled process measures by regional programs is associated with lower SSI in colectomy patients.
Major finding: As use of bundled care processes increased, surgical site infections (SSI) decreased from 6.7% to 3.9% (P = .012) across 52 hospitals.
Study details: Observational study of 5,742 colectomy patients at 1 of 52 hospitals in the Michigan Surgical Quality Collaborative system between 2012 and 2016.
Disclosures: Investigators reported no relevant financial disclosures. The study was funded by the Blue Cross Blue Shield of Michigan.
Source: Vu, J V et al. J Am Coll Surg. 2018 Jan;226(1):91-99.
Metabolic and bariatric surgery reduces CVD risk in severely obese adolescents
Weight loss caused by metabolic and bariatric surgery (MBS) independently predicts the normalization of dyslipidemia, elevated blood pressure (EPB), hyperinsulinemia, diabetes, and elevated high-sensitivity C-reactive protein (hs-CRP) in severely obese adolescents, according to results of a longitudinal, multicenter prospective study.
In the study of 242 severely obese adolescents undergoing MBS between Feb. 28, 2007, and Dec. 30, 2011, Marc Michalsky, MD, of Nationwide Children’s Hospital, Columbus, Ohio, and his colleagues found that with every 10% increase in weight loss, patients were 24%, 11%, 14%, 13%, and 19% more likely to resolve dyslipidemia, EBP, hyperinsulinemia, diabetes, and elevated hs-CRP, respectively.
One of the most important facets of this study is the predictive nature of different patient risk factors on the future remission of cardiovascular disease symptoms.
For example, “the evidence suggests that better long-term outcomes may be anticipated among individuals undergoing MBS at lower BMI levels (i.e., less than 50),” they reported in the journal Pediatrics. “Increasing age at the time of MBS was associated with a reduced likelihood of dyslipidemia remission and normalization of hs-CRP,” which was true even in the narrow age range of this group of adolescents.
“The identification of specific predictors of CVD-RF [cardiovascular disease risk factors] normalization and/or remission on the basis of sex, race, preoperative BMI, and age at surgery may serve to improve future study design and insights regarding the optimization of treatment strategies,” wrote Dr. Michalsky and his colleagues. “Collectively, these data demonstrate a reduction in the risk for development of CVD in adulthood and offer additional, compelling support for MBS in adolescents.”
Dr. Inge has worked as a consultant for Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services; all of these companies are unrelated to this research. John B. Dixon, PhD, has received support for his research through a National Health and Medical Research Council research fellowship. Anita Courcoulas, MD, has received grants from various health care groups and companies. All other authors had no relevant financial disclosures. The study was funded by a variety of institutional grants and the National Institutes of Health.
SOURCE: M Michalsky et al. Pediatrics. 2018 Jan 8. doi: 10.1542/peds.2017-2485.
Weight loss caused by metabolic and bariatric surgery (MBS) independently predicts the normalization of dyslipidemia, elevated blood pressure (EPB), hyperinsulinemia, diabetes, and elevated high-sensitivity C-reactive protein (hs-CRP) in severely obese adolescents, according to results of a longitudinal, multicenter prospective study.
In the study of 242 severely obese adolescents undergoing MBS between Feb. 28, 2007, and Dec. 30, 2011, Marc Michalsky, MD, of Nationwide Children’s Hospital, Columbus, Ohio, and his colleagues found that with every 10% increase in weight loss, patients were 24%, 11%, 14%, 13%, and 19% more likely to resolve dyslipidemia, EBP, hyperinsulinemia, diabetes, and elevated hs-CRP, respectively.
One of the most important facets of this study is the predictive nature of different patient risk factors on the future remission of cardiovascular disease symptoms.
For example, “the evidence suggests that better long-term outcomes may be anticipated among individuals undergoing MBS at lower BMI levels (i.e., less than 50),” they reported in the journal Pediatrics. “Increasing age at the time of MBS was associated with a reduced likelihood of dyslipidemia remission and normalization of hs-CRP,” which was true even in the narrow age range of this group of adolescents.
“The identification of specific predictors of CVD-RF [cardiovascular disease risk factors] normalization and/or remission on the basis of sex, race, preoperative BMI, and age at surgery may serve to improve future study design and insights regarding the optimization of treatment strategies,” wrote Dr. Michalsky and his colleagues. “Collectively, these data demonstrate a reduction in the risk for development of CVD in adulthood and offer additional, compelling support for MBS in adolescents.”
Dr. Inge has worked as a consultant for Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services; all of these companies are unrelated to this research. John B. Dixon, PhD, has received support for his research through a National Health and Medical Research Council research fellowship. Anita Courcoulas, MD, has received grants from various health care groups and companies. All other authors had no relevant financial disclosures. The study was funded by a variety of institutional grants and the National Institutes of Health.
SOURCE: M Michalsky et al. Pediatrics. 2018 Jan 8. doi: 10.1542/peds.2017-2485.
Weight loss caused by metabolic and bariatric surgery (MBS) independently predicts the normalization of dyslipidemia, elevated blood pressure (EPB), hyperinsulinemia, diabetes, and elevated high-sensitivity C-reactive protein (hs-CRP) in severely obese adolescents, according to results of a longitudinal, multicenter prospective study.
In the study of 242 severely obese adolescents undergoing MBS between Feb. 28, 2007, and Dec. 30, 2011, Marc Michalsky, MD, of Nationwide Children’s Hospital, Columbus, Ohio, and his colleagues found that with every 10% increase in weight loss, patients were 24%, 11%, 14%, 13%, and 19% more likely to resolve dyslipidemia, EBP, hyperinsulinemia, diabetes, and elevated hs-CRP, respectively.
One of the most important facets of this study is the predictive nature of different patient risk factors on the future remission of cardiovascular disease symptoms.
For example, “the evidence suggests that better long-term outcomes may be anticipated among individuals undergoing MBS at lower BMI levels (i.e., less than 50),” they reported in the journal Pediatrics. “Increasing age at the time of MBS was associated with a reduced likelihood of dyslipidemia remission and normalization of hs-CRP,” which was true even in the narrow age range of this group of adolescents.
“The identification of specific predictors of CVD-RF [cardiovascular disease risk factors] normalization and/or remission on the basis of sex, race, preoperative BMI, and age at surgery may serve to improve future study design and insights regarding the optimization of treatment strategies,” wrote Dr. Michalsky and his colleagues. “Collectively, these data demonstrate a reduction in the risk for development of CVD in adulthood and offer additional, compelling support for MBS in adolescents.”
Dr. Inge has worked as a consultant for Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services; all of these companies are unrelated to this research. John B. Dixon, PhD, has received support for his research through a National Health and Medical Research Council research fellowship. Anita Courcoulas, MD, has received grants from various health care groups and companies. All other authors had no relevant financial disclosures. The study was funded by a variety of institutional grants and the National Institutes of Health.
SOURCE: M Michalsky et al. Pediatrics. 2018 Jan 8. doi: 10.1542/peds.2017-2485.
FROM PEDIATRICS
Key clinical point:
Major finding: With every 10% increase in weight loss, patients were 24%, 11%, 14%, 13%, and 19% more likely to resolve dyslipidemia, elevated BP, hyperinsulinemia, diabetes and elevated high-sensitivity C-reactive protein, respectively.
Study details: This study was a longitudinal, multicenter prospective study of 242 severely obese adolescents undergoing metabolic and bariatric surgery between February 28, 2007 and December 30, 2011.
Disclosures: Dr. Inge has worked as a consultant for Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services; all of these companies are unrelated to this research. John B. Dixon, PhD, has received support for his research through a National Health and Medical Research Council research fellowship. Anita Courcoulas, MD, has received grants from various healthcare groups and companies. All other authors had no relevant financial disclosures. The study was funded by a variety of institutional grants and the National Institutes of Health.
Source: M Michalsky et al. Pediatrics. 2018 Jan 8. doi: 10.1542/peds.2017-2485
Model validates use of HCV+ livers for transplant
As the evidence supporting the idea of transplanting livers infected with hepatitis C into patients who do not have the disease continues to mount, a multi-institutional team of researchers has developed a mathematical model that shows when hepatitis C–positive-to-negative transplant may improve survival for patients who might otherwise die awaiting a disease-free liver.
In a report published in the journal Hepatology (doi: 10.1002/hep.29723), the researchers noted how direct-acting antivirals (DAAs) have changed the calculus of hepatitis C (HCV) status in liver transplant by reducing the number of HCV-positive patients on the wait list and providing treatment for HCV-negative patients who receive HCV-positive livers. “It is important that further research in this area continues, as we expect that the supply of HCV-positive organs may continue to increase in light of the growing opioid epidemic,” said lead author Jagpreet Chhatwal, PhD, of Massachusetts General Hospital Institute for Technology Assessment in Boston.
Dr. Chhatwal and coauthors claimed their study provides some of the first empirical data for transplanting livers from patients with HCV into patients who do not have the disease.
The researchers performed their analysis using a Markov-based mathematical model known as Simulation of Liver Transplant Candidates (SIM-LT). The model had been validated in previous studies that Dr. Chhatwal and some coauthors had published (Hepatology. 2017;65:777-88; Clin Gastroenterol Hepatol 2018;16:115-22). Dr. Chhatwal and coauthors revised the SIM-LT model to simulate a virtual trial of HCV-negative patients on the liver transplant waiting list to compare outcomes in patients willing to accept any liver to those willing to accept only HCV-negative livers.
The patients willing to receive HCV-positive livers were given 12 weeks of DAA therapy preemptively and had a higher risk of graft failure. The model incorporated data from published studies using the United Network for Organ Sharing (UNOS) and used reported outcomes of the Organ Procurement and Transplantation Network to validate the findings.
The study showed that the clinical benefits of an HCV-negative patient receiving an HCV-positive liver depend on the patient’s Model for End-Stage Liver Disease (MELD) score. Using the measured change in life-years, the researchers found that patients with a MELD score below 20 actually witnessed reduction in life-years when accepting any liver, but that the benefits of accepting any liver started to accrue at MELD score 20. The benefit topped out at MELD 28, with 0.172 life years gained, but even sustained at 0.06 life years gained at MELD 40.
The effectiveness of using HCV-positive livers may also depend on region. UNOS Region 1 – essentially New England minus western Vermont – has the highest rate of HCV-positive organs, and a patient there with MELD 28 would gain 0.36 life-years by accepting any liver regardless of HCV status. However, Region 7 – the Dakotas and upper Midwest plus Illinois – has the lowest HCV-positive organ rate, and a MELD 28 patient there would gain only 0.1 life-year accepting any liver.
“Transplanting HCV-positive livers into HCV-negative patients receiving preemptive DAA therapy could be a viable option for improving patient survival on the LT waiting list, especially in UNOS regions with high HCV-positive donor organ rates,” said Dr. Chhatwal and coauthors. They concluded that their analysis could help direct future clinical trials evaluating the effectiveness of DAA therapy in liver transplant by recognizing patients who could benefit most from accepting HCV-positive donor organs.
The study authors reported having no financial disclosures. The study was supported by grants from the American Cancer Society, Health Resources and Services Administration, National Institutes of Health, National Science Foundation, and Massachusetts General Hospital Research Scholars Program. Coauthor Fasiha Kanwal, MD, received support from the Veterans Administration Health Services, Research & Development Center for Innovations in Quality, Effectiveness and Safety and Public Health Service.
SOURCE: Chhatwal J et al. Hepatology. doi:10.1002/hep.29723.
As the evidence supporting the idea of transplanting livers infected with hepatitis C into patients who do not have the disease continues to mount, a multi-institutional team of researchers has developed a mathematical model that shows when hepatitis C–positive-to-negative transplant may improve survival for patients who might otherwise die awaiting a disease-free liver.
In a report published in the journal Hepatology (doi: 10.1002/hep.29723), the researchers noted how direct-acting antivirals (DAAs) have changed the calculus of hepatitis C (HCV) status in liver transplant by reducing the number of HCV-positive patients on the wait list and providing treatment for HCV-negative patients who receive HCV-positive livers. “It is important that further research in this area continues, as we expect that the supply of HCV-positive organs may continue to increase in light of the growing opioid epidemic,” said lead author Jagpreet Chhatwal, PhD, of Massachusetts General Hospital Institute for Technology Assessment in Boston.
Dr. Chhatwal and coauthors claimed their study provides some of the first empirical data for transplanting livers from patients with HCV into patients who do not have the disease.
The researchers performed their analysis using a Markov-based mathematical model known as Simulation of Liver Transplant Candidates (SIM-LT). The model had been validated in previous studies that Dr. Chhatwal and some coauthors had published (Hepatology. 2017;65:777-88; Clin Gastroenterol Hepatol 2018;16:115-22). Dr. Chhatwal and coauthors revised the SIM-LT model to simulate a virtual trial of HCV-negative patients on the liver transplant waiting list to compare outcomes in patients willing to accept any liver to those willing to accept only HCV-negative livers.
The patients willing to receive HCV-positive livers were given 12 weeks of DAA therapy preemptively and had a higher risk of graft failure. The model incorporated data from published studies using the United Network for Organ Sharing (UNOS) and used reported outcomes of the Organ Procurement and Transplantation Network to validate the findings.
The study showed that the clinical benefits of an HCV-negative patient receiving an HCV-positive liver depend on the patient’s Model for End-Stage Liver Disease (MELD) score. Using the measured change in life-years, the researchers found that patients with a MELD score below 20 actually witnessed reduction in life-years when accepting any liver, but that the benefits of accepting any liver started to accrue at MELD score 20. The benefit topped out at MELD 28, with 0.172 life years gained, but even sustained at 0.06 life years gained at MELD 40.
The effectiveness of using HCV-positive livers may also depend on region. UNOS Region 1 – essentially New England minus western Vermont – has the highest rate of HCV-positive organs, and a patient there with MELD 28 would gain 0.36 life-years by accepting any liver regardless of HCV status. However, Region 7 – the Dakotas and upper Midwest plus Illinois – has the lowest HCV-positive organ rate, and a MELD 28 patient there would gain only 0.1 life-year accepting any liver.
“Transplanting HCV-positive livers into HCV-negative patients receiving preemptive DAA therapy could be a viable option for improving patient survival on the LT waiting list, especially in UNOS regions with high HCV-positive donor organ rates,” said Dr. Chhatwal and coauthors. They concluded that their analysis could help direct future clinical trials evaluating the effectiveness of DAA therapy in liver transplant by recognizing patients who could benefit most from accepting HCV-positive donor organs.
The study authors reported having no financial disclosures. The study was supported by grants from the American Cancer Society, Health Resources and Services Administration, National Institutes of Health, National Science Foundation, and Massachusetts General Hospital Research Scholars Program. Coauthor Fasiha Kanwal, MD, received support from the Veterans Administration Health Services, Research & Development Center for Innovations in Quality, Effectiveness and Safety and Public Health Service.
SOURCE: Chhatwal J et al. Hepatology. doi:10.1002/hep.29723.
As the evidence supporting the idea of transplanting livers infected with hepatitis C into patients who do not have the disease continues to mount, a multi-institutional team of researchers has developed a mathematical model that shows when hepatitis C–positive-to-negative transplant may improve survival for patients who might otherwise die awaiting a disease-free liver.
In a report published in the journal Hepatology (doi: 10.1002/hep.29723), the researchers noted how direct-acting antivirals (DAAs) have changed the calculus of hepatitis C (HCV) status in liver transplant by reducing the number of HCV-positive patients on the wait list and providing treatment for HCV-negative patients who receive HCV-positive livers. “It is important that further research in this area continues, as we expect that the supply of HCV-positive organs may continue to increase in light of the growing opioid epidemic,” said lead author Jagpreet Chhatwal, PhD, of Massachusetts General Hospital Institute for Technology Assessment in Boston.
Dr. Chhatwal and coauthors claimed their study provides some of the first empirical data for transplanting livers from patients with HCV into patients who do not have the disease.
The researchers performed their analysis using a Markov-based mathematical model known as Simulation of Liver Transplant Candidates (SIM-LT). The model had been validated in previous studies that Dr. Chhatwal and some coauthors had published (Hepatology. 2017;65:777-88; Clin Gastroenterol Hepatol 2018;16:115-22). Dr. Chhatwal and coauthors revised the SIM-LT model to simulate a virtual trial of HCV-negative patients on the liver transplant waiting list to compare outcomes in patients willing to accept any liver to those willing to accept only HCV-negative livers.
The patients willing to receive HCV-positive livers were given 12 weeks of DAA therapy preemptively and had a higher risk of graft failure. The model incorporated data from published studies using the United Network for Organ Sharing (UNOS) and used reported outcomes of the Organ Procurement and Transplantation Network to validate the findings.
The study showed that the clinical benefits of an HCV-negative patient receiving an HCV-positive liver depend on the patient’s Model for End-Stage Liver Disease (MELD) score. Using the measured change in life-years, the researchers found that patients with a MELD score below 20 actually witnessed reduction in life-years when accepting any liver, but that the benefits of accepting any liver started to accrue at MELD score 20. The benefit topped out at MELD 28, with 0.172 life years gained, but even sustained at 0.06 life years gained at MELD 40.
The effectiveness of using HCV-positive livers may also depend on region. UNOS Region 1 – essentially New England minus western Vermont – has the highest rate of HCV-positive organs, and a patient there with MELD 28 would gain 0.36 life-years by accepting any liver regardless of HCV status. However, Region 7 – the Dakotas and upper Midwest plus Illinois – has the lowest HCV-positive organ rate, and a MELD 28 patient there would gain only 0.1 life-year accepting any liver.
“Transplanting HCV-positive livers into HCV-negative patients receiving preemptive DAA therapy could be a viable option for improving patient survival on the LT waiting list, especially in UNOS regions with high HCV-positive donor organ rates,” said Dr. Chhatwal and coauthors. They concluded that their analysis could help direct future clinical trials evaluating the effectiveness of DAA therapy in liver transplant by recognizing patients who could benefit most from accepting HCV-positive donor organs.
The study authors reported having no financial disclosures. The study was supported by grants from the American Cancer Society, Health Resources and Services Administration, National Institutes of Health, National Science Foundation, and Massachusetts General Hospital Research Scholars Program. Coauthor Fasiha Kanwal, MD, received support from the Veterans Administration Health Services, Research & Development Center for Innovations in Quality, Effectiveness and Safety and Public Health Service.
SOURCE: Chhatwal J et al. Hepatology. doi:10.1002/hep.29723.
FROM HEPATOLOGY
Key clinical point: Making hepatitis C virus–positive livers available to HCV-negative patients awaiting liver transplant could improve survival of patients on the liver transplant waiting list.
Major finding: Patients with a Model for End-Stage Liver Disease score of 28 willing to receive any liver gained 0.172 life-years.
Data source: Simulated trial using Markov-based mathematical model and data from published studies and the United Network for Organ Sharing.
Disclosures: Dr. Chhatwal and coauthors reported having no financial disclosures. The study was supported by grants from the American Cancer Society, Health Resources and Services Administration, National Institutes of Health, National Science Foundation, and Massachusetts General Hospital Research Scholars Program. Coauthor Fasiha Kanwal, MD, received support from the Veterans Administration Health Services, Research & Development Center for Innovations in Quality, Effectiveness and Safety and Public Health Service.
Source: Chhatwal J et al. Hepatology. doi:10.1002/hep.29723.
Gastrointestinal complications are a key risk factor for death after AEF repair
Aortoenteric fistulas (AEFs) are an uncommon but lethal form of aortic graft infection with morbidity and mortality rates reported in the literature to range from 14% to 75%. Over a 20-year period, researchers found that nearly half of their patients undergoing repair of their aortoenteric fistulas died within 60 days. The presence of gastrointestinal complications increased the risk of mortality more than threefold, according to the results of a single-center retrospective review of consecutive AEF repairs.
The researchers assessed 50 patients who presented with AEF and had repair during 1995-2014. Sixty percent of the patients were men, and the overall median age was 70 years. The median follow-up for the entire cohort was 14 months. The duodenum was the most common location of the enteric defect, found in 80% of the infections. Overall, 23 patients (46%) died by day 60, according to the report published in the July Journal of the American College of Surgeons.
Univariate analysis showed that advanced age, chronic renal insufficiency, any complications, and GI complications in particular (occurring in 26% of patients) were all associated with an increase in overall mortality (P less than .05). But upon multivariate analysis, gastrointestinal complications (hazard ratio, 3.23; P = .015) and advanced age (HR, 1.07; P = .01) were the only independent predictors of mortality, Atish Chopra, MD, of the division of vascular surgery, Oregon Health & Science University, Portland, and his colleagues wrote.
The institution changed operative procedures in 2007, based upon an earlier assessment of the importance of GI complications performed by the researchers, with greater emphasis placed on ensuring a viable GI reconstruction, and early intervention for mesenteric ischemia. In addition, they surmised that, after 2007, there was improved adherence to achieving wide debridement of nonviable and infected tissue, and to creating a tension-free anastomosis to healthy tissue edges while optimizing nutritional, medical, and antibiotic therapy, according to the researchers.
“When comparing the patients undergoing repair before 2007 with those compared after 2007 [38 and 12 AEF patients, respectively], we found that in-hospitality mortality decreased from 37% to 8% (P = .08), 60-day mortality decreased from 53% to 8% (P less than .01), and mortality at last follow-up decreased from 55% to 17% (P = .02). Dr. Chopra and his colleagues also found that mortality after GI complications decreased from 90% for those operated on before 2007 to 33% in those operated on after 2007 (P = .01).
“Methods to decrease and improvement management of GI complications may prove most effective at improving mortality rates for this lethal pathology,” the researchers concluded.
The authors reported that they had nothing to disclose.
SOURCE: Chopra A et al. J Am Coll Surg 2017 Jul;225(1):9-18.
While secondary aortoenteric fistulas fortunately are a rare occurrence after open aortic repair (less than 1%), the reported results of treatment are disappointing (up to 75% mortality). The authors have demonstrated significant improvement in overall mortality in their series by paying more attention to the GI component of the procedure and postoperative management of the patient.
When we published our institutions experience with AEFs from 1991 to 2004, the study included 29 patients with one-third of patients presenting in shock. Extra-anatomic repair was performed in 86% (68% single stage). Mortality was 24%, with shock, blood transfusions, and suprarenal clamping associated with a worse outcome. Our 5-year survival was 61% and freedom from recurrent infection or amputation was 86% and 88% respectively. While our experience favors an extra-anatomic reconstruction, there has been increased utilization of in-situ repair in recent years. The current authors have extensive experience with the Neoaortoiliac System (NAIS) procedure and have had minimal complications associated with the extensive vein harvest necessary for NAIS; however, this is not universal. Wound complications, compartment syndrome, and chronic venous insufficiency are not uncommon complications. Improved results using cryopreserved aortoiliac allografts (CAA) were reported by The Vascular Low-Frequency Disease Consortium. In a 2014 publication on 220 patients receiving CAA for aortic reconstruction for aortic graft infection, freedom from graft-related complications, graft explant, and limb loss was 80%, 88%, and 97%, respectively, at 5 years. This compares favorably with extra-anatomic reconstruction and other techniques. In suprarenal reconstructions, allografts have been favored since the natural branches can be used to simplify multiple vessel reconstruction. In cases of low-grade infection (Staphylococcus epidermidis), excellent results have been demonstrated with wide debridement, in-situ replacement with rifampin-bonded grafts and omental coverage.
AEF can also occur after endovascular abdominal aortic aneurysm (AAA) repair and a management strategy for removing the endograft should be considered in the planning of these cases. The authors describe their technique, which involves constraining the endograft using an umbilical tape. Another technique that I prefer uses a 20-cc syringe with the tip cut off. The endograft is constrained by advancing the syringe proximally over the endograft. The syringe collapses the device and can be used to constrain the proximal fixation stents of a suprarenal graft, simplifying removal of the stent graft. Infected EVAR will likely become more common as an etiology as we continue to expand EVAR utilization for AAA repair. Another Low-Frequency Consortium paper reviewed the treatment and outcome of EVAR infection. In that report of 206 infected EVAR (endovascular aneurysm repair) and TEVAR (thoracic endovascular aortic repair) patients, 90% had in situ replacement with a 30-day mortality of 11% and morbidity of 35%.
As in previous reports on AEF, the authors highlight the importance of high clinical suspicion in making an expeditious diagnosis. Many imaging modalities can be used, but often operative exploration is required for a definitive diagnosis. Complete graft excision and wide debridement are critical to minimize the risk of recurrent infection. Optimal revascularization techniques should be determined by the experience of the operator, current experience demonstrating nearly equivalent outcomes with extra-anatomic and in situ replacement. Careful GI reconstruction and post-operative nutrition, culture-specific antibiotics, and ICU care are likely more important than the mode of reconstruction. Lifelong surveillance to detect recurrent infections also is recommended.
Murray L. Shames, MD , is professor of surgery and radiology and chief of the division of vascular surgery at the University of South Florida, Tampa, and director of the Tampa General Hospital aortic program.
While secondary aortoenteric fistulas fortunately are a rare occurrence after open aortic repair (less than 1%), the reported results of treatment are disappointing (up to 75% mortality). The authors have demonstrated significant improvement in overall mortality in their series by paying more attention to the GI component of the procedure and postoperative management of the patient.
When we published our institutions experience with AEFs from 1991 to 2004, the study included 29 patients with one-third of patients presenting in shock. Extra-anatomic repair was performed in 86% (68% single stage). Mortality was 24%, with shock, blood transfusions, and suprarenal clamping associated with a worse outcome. Our 5-year survival was 61% and freedom from recurrent infection or amputation was 86% and 88% respectively. While our experience favors an extra-anatomic reconstruction, there has been increased utilization of in-situ repair in recent years. The current authors have extensive experience with the Neoaortoiliac System (NAIS) procedure and have had minimal complications associated with the extensive vein harvest necessary for NAIS; however, this is not universal. Wound complications, compartment syndrome, and chronic venous insufficiency are not uncommon complications. Improved results using cryopreserved aortoiliac allografts (CAA) were reported by The Vascular Low-Frequency Disease Consortium. In a 2014 publication on 220 patients receiving CAA for aortic reconstruction for aortic graft infection, freedom from graft-related complications, graft explant, and limb loss was 80%, 88%, and 97%, respectively, at 5 years. This compares favorably with extra-anatomic reconstruction and other techniques. In suprarenal reconstructions, allografts have been favored since the natural branches can be used to simplify multiple vessel reconstruction. In cases of low-grade infection (Staphylococcus epidermidis), excellent results have been demonstrated with wide debridement, in-situ replacement with rifampin-bonded grafts and omental coverage.
AEF can also occur after endovascular abdominal aortic aneurysm (AAA) repair and a management strategy for removing the endograft should be considered in the planning of these cases. The authors describe their technique, which involves constraining the endograft using an umbilical tape. Another technique that I prefer uses a 20-cc syringe with the tip cut off. The endograft is constrained by advancing the syringe proximally over the endograft. The syringe collapses the device and can be used to constrain the proximal fixation stents of a suprarenal graft, simplifying removal of the stent graft. Infected EVAR will likely become more common as an etiology as we continue to expand EVAR utilization for AAA repair. Another Low-Frequency Consortium paper reviewed the treatment and outcome of EVAR infection. In that report of 206 infected EVAR (endovascular aneurysm repair) and TEVAR (thoracic endovascular aortic repair) patients, 90% had in situ replacement with a 30-day mortality of 11% and morbidity of 35%.
As in previous reports on AEF, the authors highlight the importance of high clinical suspicion in making an expeditious diagnosis. Many imaging modalities can be used, but often operative exploration is required for a definitive diagnosis. Complete graft excision and wide debridement are critical to minimize the risk of recurrent infection. Optimal revascularization techniques should be determined by the experience of the operator, current experience demonstrating nearly equivalent outcomes with extra-anatomic and in situ replacement. Careful GI reconstruction and post-operative nutrition, culture-specific antibiotics, and ICU care are likely more important than the mode of reconstruction. Lifelong surveillance to detect recurrent infections also is recommended.
Murray L. Shames, MD , is professor of surgery and radiology and chief of the division of vascular surgery at the University of South Florida, Tampa, and director of the Tampa General Hospital aortic program.
While secondary aortoenteric fistulas fortunately are a rare occurrence after open aortic repair (less than 1%), the reported results of treatment are disappointing (up to 75% mortality). The authors have demonstrated significant improvement in overall mortality in their series by paying more attention to the GI component of the procedure and postoperative management of the patient.
When we published our institutions experience with AEFs from 1991 to 2004, the study included 29 patients with one-third of patients presenting in shock. Extra-anatomic repair was performed in 86% (68% single stage). Mortality was 24%, with shock, blood transfusions, and suprarenal clamping associated with a worse outcome. Our 5-year survival was 61% and freedom from recurrent infection or amputation was 86% and 88% respectively. While our experience favors an extra-anatomic reconstruction, there has been increased utilization of in-situ repair in recent years. The current authors have extensive experience with the Neoaortoiliac System (NAIS) procedure and have had minimal complications associated with the extensive vein harvest necessary for NAIS; however, this is not universal. Wound complications, compartment syndrome, and chronic venous insufficiency are not uncommon complications. Improved results using cryopreserved aortoiliac allografts (CAA) were reported by The Vascular Low-Frequency Disease Consortium. In a 2014 publication on 220 patients receiving CAA for aortic reconstruction for aortic graft infection, freedom from graft-related complications, graft explant, and limb loss was 80%, 88%, and 97%, respectively, at 5 years. This compares favorably with extra-anatomic reconstruction and other techniques. In suprarenal reconstructions, allografts have been favored since the natural branches can be used to simplify multiple vessel reconstruction. In cases of low-grade infection (Staphylococcus epidermidis), excellent results have been demonstrated with wide debridement, in-situ replacement with rifampin-bonded grafts and omental coverage.
AEF can also occur after endovascular abdominal aortic aneurysm (AAA) repair and a management strategy for removing the endograft should be considered in the planning of these cases. The authors describe their technique, which involves constraining the endograft using an umbilical tape. Another technique that I prefer uses a 20-cc syringe with the tip cut off. The endograft is constrained by advancing the syringe proximally over the endograft. The syringe collapses the device and can be used to constrain the proximal fixation stents of a suprarenal graft, simplifying removal of the stent graft. Infected EVAR will likely become more common as an etiology as we continue to expand EVAR utilization for AAA repair. Another Low-Frequency Consortium paper reviewed the treatment and outcome of EVAR infection. In that report of 206 infected EVAR (endovascular aneurysm repair) and TEVAR (thoracic endovascular aortic repair) patients, 90% had in situ replacement with a 30-day mortality of 11% and morbidity of 35%.
As in previous reports on AEF, the authors highlight the importance of high clinical suspicion in making an expeditious diagnosis. Many imaging modalities can be used, but often operative exploration is required for a definitive diagnosis. Complete graft excision and wide debridement are critical to minimize the risk of recurrent infection. Optimal revascularization techniques should be determined by the experience of the operator, current experience demonstrating nearly equivalent outcomes with extra-anatomic and in situ replacement. Careful GI reconstruction and post-operative nutrition, culture-specific antibiotics, and ICU care are likely more important than the mode of reconstruction. Lifelong surveillance to detect recurrent infections also is recommended.
Murray L. Shames, MD , is professor of surgery and radiology and chief of the division of vascular surgery at the University of South Florida, Tampa, and director of the Tampa General Hospital aortic program.
Aortoenteric fistulas (AEFs) are an uncommon but lethal form of aortic graft infection with morbidity and mortality rates reported in the literature to range from 14% to 75%. Over a 20-year period, researchers found that nearly half of their patients undergoing repair of their aortoenteric fistulas died within 60 days. The presence of gastrointestinal complications increased the risk of mortality more than threefold, according to the results of a single-center retrospective review of consecutive AEF repairs.
The researchers assessed 50 patients who presented with AEF and had repair during 1995-2014. Sixty percent of the patients were men, and the overall median age was 70 years. The median follow-up for the entire cohort was 14 months. The duodenum was the most common location of the enteric defect, found in 80% of the infections. Overall, 23 patients (46%) died by day 60, according to the report published in the July Journal of the American College of Surgeons.
Univariate analysis showed that advanced age, chronic renal insufficiency, any complications, and GI complications in particular (occurring in 26% of patients) were all associated with an increase in overall mortality (P less than .05). But upon multivariate analysis, gastrointestinal complications (hazard ratio, 3.23; P = .015) and advanced age (HR, 1.07; P = .01) were the only independent predictors of mortality, Atish Chopra, MD, of the division of vascular surgery, Oregon Health & Science University, Portland, and his colleagues wrote.
The institution changed operative procedures in 2007, based upon an earlier assessment of the importance of GI complications performed by the researchers, with greater emphasis placed on ensuring a viable GI reconstruction, and early intervention for mesenteric ischemia. In addition, they surmised that, after 2007, there was improved adherence to achieving wide debridement of nonviable and infected tissue, and to creating a tension-free anastomosis to healthy tissue edges while optimizing nutritional, medical, and antibiotic therapy, according to the researchers.
“When comparing the patients undergoing repair before 2007 with those compared after 2007 [38 and 12 AEF patients, respectively], we found that in-hospitality mortality decreased from 37% to 8% (P = .08), 60-day mortality decreased from 53% to 8% (P less than .01), and mortality at last follow-up decreased from 55% to 17% (P = .02). Dr. Chopra and his colleagues also found that mortality after GI complications decreased from 90% for those operated on before 2007 to 33% in those operated on after 2007 (P = .01).
“Methods to decrease and improvement management of GI complications may prove most effective at improving mortality rates for this lethal pathology,” the researchers concluded.
The authors reported that they had nothing to disclose.
SOURCE: Chopra A et al. J Am Coll Surg 2017 Jul;225(1):9-18.
Aortoenteric fistulas (AEFs) are an uncommon but lethal form of aortic graft infection with morbidity and mortality rates reported in the literature to range from 14% to 75%. Over a 20-year period, researchers found that nearly half of their patients undergoing repair of their aortoenteric fistulas died within 60 days. The presence of gastrointestinal complications increased the risk of mortality more than threefold, according to the results of a single-center retrospective review of consecutive AEF repairs.
The researchers assessed 50 patients who presented with AEF and had repair during 1995-2014. Sixty percent of the patients were men, and the overall median age was 70 years. The median follow-up for the entire cohort was 14 months. The duodenum was the most common location of the enteric defect, found in 80% of the infections. Overall, 23 patients (46%) died by day 60, according to the report published in the July Journal of the American College of Surgeons.
Univariate analysis showed that advanced age, chronic renal insufficiency, any complications, and GI complications in particular (occurring in 26% of patients) were all associated with an increase in overall mortality (P less than .05). But upon multivariate analysis, gastrointestinal complications (hazard ratio, 3.23; P = .015) and advanced age (HR, 1.07; P = .01) were the only independent predictors of mortality, Atish Chopra, MD, of the division of vascular surgery, Oregon Health & Science University, Portland, and his colleagues wrote.
The institution changed operative procedures in 2007, based upon an earlier assessment of the importance of GI complications performed by the researchers, with greater emphasis placed on ensuring a viable GI reconstruction, and early intervention for mesenteric ischemia. In addition, they surmised that, after 2007, there was improved adherence to achieving wide debridement of nonviable and infected tissue, and to creating a tension-free anastomosis to healthy tissue edges while optimizing nutritional, medical, and antibiotic therapy, according to the researchers.
“When comparing the patients undergoing repair before 2007 with those compared after 2007 [38 and 12 AEF patients, respectively], we found that in-hospitality mortality decreased from 37% to 8% (P = .08), 60-day mortality decreased from 53% to 8% (P less than .01), and mortality at last follow-up decreased from 55% to 17% (P = .02). Dr. Chopra and his colleagues also found that mortality after GI complications decreased from 90% for those operated on before 2007 to 33% in those operated on after 2007 (P = .01).
“Methods to decrease and improvement management of GI complications may prove most effective at improving mortality rates for this lethal pathology,” the researchers concluded.
The authors reported that they had nothing to disclose.
SOURCE: Chopra A et al. J Am Coll Surg 2017 Jul;225(1):9-18.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Nearly half of patients undergoing aortoenteric fistula repair died within 60 days.
Major finding: The presence of gastrointestinal complications increased the risk of mortality for AEF repair more than threefold.
Study details: A single center, retrospective review of 50 consecutive patients with AEF repairs during 1995-2014.
Disclosures: The authors reported that they had nothing to disclose.
Source: Chopra A et al. J Am Coll Surg. 2017 Jul;225:9-18.
Analysis: Hospital pay for performance not significantly improving Medicare outcomes
for Medicare beneficiaries, according to an analysis of Medicare claims data.
“No evidence that hospitals [that were] operating under pay for performance programs for more than a decade had better process scores or lower mortality than other hospitals was found,” Igna Bonfrer, PhD, of Erasmus University, Rotterdam, the Netherlands, and colleagues wrote in a study published Jan. 4, 2018, in BMJ.
Researchers looked at Medicare claims data from nearly 1.4 million patients aged 65 years and older across 1,189 hospitals. That total included 214 hospitals that were early adopters of pay for performance (PFP) programs, including the Hospital Quality Incentive Demonstration (HQID) and the current Hospital Value-Based Purchasing (HVBP) program, and 975 hospitals that adopted the programs at a later date. The study authors examined clinical process scores and 30-day mortality rates from 2003 to 2013.
Hospitals that were early adopters of a PFP program typically started from a higher baseline process measure score (91.5), compared with late adopters (89.9).
However, improvements among the early adopters “were smaller during the HQID period, although early adopters continued to perform at a slightly higher level than the late adopters during the pre-HVBP period,” the researchers explained. “Over the HVBP period, early and late adopters no longer differed in their clinical process scores.”
Indeed, a ceiling was ultimately reached, with early and late adopters approaching the same level (98.5 vs. 98.2).
For the 30-day mortality rates, both groups “started from a similar baseline (14.9% and 14.8% for the early and late adopters in the fourth quarter of 2003) and ended at the same rate of 9.9% for both groups in the fourth quarter of 2013,” Dr. Bonfrer and colleagues wrote.
The researchers suggested that the programs did not yield better results because of small financial incentives, coupled with program complexities that made it “difficult for hospitals to meaningfully engage in the program.” They also suggested that having to wait until year end to receive any financial incentives could have limited the impact.
“We found that hospitals that have been under financial incentives for more than a decade have not been able to reduce patient mortality more than late adopters, which had only been under financial incentives for less than 3 years,” the researchers concluded. “Given its cost, policymakers in the [United States] should consider one of two things: revise the current program or potentially end it.”
The changes suggested include increasing financial incentives and focusing on process measures that matter most to patients (mortality, patient experience, and functional status), rather than the current measure set that is larger and more difficult to track.
The researchers did not report any financial conflicts of interest.
SOURCE: Dr. Igna Bonfrer et al. BMJ 2018;360:j5622.
for Medicare beneficiaries, according to an analysis of Medicare claims data.
“No evidence that hospitals [that were] operating under pay for performance programs for more than a decade had better process scores or lower mortality than other hospitals was found,” Igna Bonfrer, PhD, of Erasmus University, Rotterdam, the Netherlands, and colleagues wrote in a study published Jan. 4, 2018, in BMJ.
Researchers looked at Medicare claims data from nearly 1.4 million patients aged 65 years and older across 1,189 hospitals. That total included 214 hospitals that were early adopters of pay for performance (PFP) programs, including the Hospital Quality Incentive Demonstration (HQID) and the current Hospital Value-Based Purchasing (HVBP) program, and 975 hospitals that adopted the programs at a later date. The study authors examined clinical process scores and 30-day mortality rates from 2003 to 2013.
Hospitals that were early adopters of a PFP program typically started from a higher baseline process measure score (91.5), compared with late adopters (89.9).
However, improvements among the early adopters “were smaller during the HQID period, although early adopters continued to perform at a slightly higher level than the late adopters during the pre-HVBP period,” the researchers explained. “Over the HVBP period, early and late adopters no longer differed in their clinical process scores.”
Indeed, a ceiling was ultimately reached, with early and late adopters approaching the same level (98.5 vs. 98.2).
For the 30-day mortality rates, both groups “started from a similar baseline (14.9% and 14.8% for the early and late adopters in the fourth quarter of 2003) and ended at the same rate of 9.9% for both groups in the fourth quarter of 2013,” Dr. Bonfrer and colleagues wrote.
The researchers suggested that the programs did not yield better results because of small financial incentives, coupled with program complexities that made it “difficult for hospitals to meaningfully engage in the program.” They also suggested that having to wait until year end to receive any financial incentives could have limited the impact.
“We found that hospitals that have been under financial incentives for more than a decade have not been able to reduce patient mortality more than late adopters, which had only been under financial incentives for less than 3 years,” the researchers concluded. “Given its cost, policymakers in the [United States] should consider one of two things: revise the current program or potentially end it.”
The changes suggested include increasing financial incentives and focusing on process measures that matter most to patients (mortality, patient experience, and functional status), rather than the current measure set that is larger and more difficult to track.
The researchers did not report any financial conflicts of interest.
SOURCE: Dr. Igna Bonfrer et al. BMJ 2018;360:j5622.
for Medicare beneficiaries, according to an analysis of Medicare claims data.
“No evidence that hospitals [that were] operating under pay for performance programs for more than a decade had better process scores or lower mortality than other hospitals was found,” Igna Bonfrer, PhD, of Erasmus University, Rotterdam, the Netherlands, and colleagues wrote in a study published Jan. 4, 2018, in BMJ.
Researchers looked at Medicare claims data from nearly 1.4 million patients aged 65 years and older across 1,189 hospitals. That total included 214 hospitals that were early adopters of pay for performance (PFP) programs, including the Hospital Quality Incentive Demonstration (HQID) and the current Hospital Value-Based Purchasing (HVBP) program, and 975 hospitals that adopted the programs at a later date. The study authors examined clinical process scores and 30-day mortality rates from 2003 to 2013.
Hospitals that were early adopters of a PFP program typically started from a higher baseline process measure score (91.5), compared with late adopters (89.9).
However, improvements among the early adopters “were smaller during the HQID period, although early adopters continued to perform at a slightly higher level than the late adopters during the pre-HVBP period,” the researchers explained. “Over the HVBP period, early and late adopters no longer differed in their clinical process scores.”
Indeed, a ceiling was ultimately reached, with early and late adopters approaching the same level (98.5 vs. 98.2).
For the 30-day mortality rates, both groups “started from a similar baseline (14.9% and 14.8% for the early and late adopters in the fourth quarter of 2003) and ended at the same rate of 9.9% for both groups in the fourth quarter of 2013,” Dr. Bonfrer and colleagues wrote.
The researchers suggested that the programs did not yield better results because of small financial incentives, coupled with program complexities that made it “difficult for hospitals to meaningfully engage in the program.” They also suggested that having to wait until year end to receive any financial incentives could have limited the impact.
“We found that hospitals that have been under financial incentives for more than a decade have not been able to reduce patient mortality more than late adopters, which had only been under financial incentives for less than 3 years,” the researchers concluded. “Given its cost, policymakers in the [United States] should consider one of two things: revise the current program or potentially end it.”
The changes suggested include increasing financial incentives and focusing on process measures that matter most to patients (mortality, patient experience, and functional status), rather than the current measure set that is larger and more difficult to track.
The researchers did not report any financial conflicts of interest.
SOURCE: Dr. Igna Bonfrer et al. BMJ 2018;360:j5622.
FROM BMJ
C7 nerve transfer shows promising results for spastic arm paralysis
Patients with spastic arm paralysis who received a contralateral C7 nerve graft from their nonparalyzed side to their paralyzed side led to greater improvement in arm function and reduction in spasticity after a year, compared with rehabilitation alone, investigators from Huashan Hospital in China reported online Jan. 3 in the New England Journal of Medicine.
The researchers randomly assigned 36 patients who had unilateral arm paralysis for at least 5 years to either surgical C7 nerve transfer plus rehabilitation or rehabilitation only. Results of the trial’s primary outcome – arm function using the Fugl-Meyer score – showed that those in the surgery group had an average increase of 17.7, while those in the rehabilitation-only group had an average increase of 2.6 (P less than .001). This 15.1-point difference had a 95% confidence interval ranging from 12.2 to 17.9.
To evaluate spasticity, the researchers used the Modified Ashworth Scale, which is a 0-5 scale to score spasticity; a higher score means more spasticity. Surgery patients saw improvement from baseline in all five areas measured across the board, and none saw worsening in scores. The smallest difference between the two groups was in thumb extension, with 15 surgery patients having a 1- and 2-unit improvement and 3 having no change, while 7 controls showed a 1- or 2-unit improvement, another 7 showed no improvement, and 4 had a 1-unit worsening in score (P less than .001). At 1 year, 16 (89%) of surgery patients could accomplish three or more of the functional tasks researchers gave them, whereas none of the controls could.
“The majority of clinical improvements coincided with physiological evidence of connectivity between the hemisphere on the side of the donor nerve and the paralyzed arm,” said lead author Mou-Xiong Zheng, MD, PhD, of the department of hand surgery at Huashan Hospital at Fudan University in Shanghai, and colleagues.
The research by Dr. Zheng and coauthors arises from what is known about hand paralysis after stroke, that damage to the contralateral cerebral hemisphere arises from interruption of the inhibitory activity of upper motor neurons, which causes spasticity, along with hand weakness and loss of fractionated fine motor control. Other studies have noted activity in the cerebral hemisphere on the same side of paralysis during recovery (Neuroimage. 2004;22:1775-83; J Neurophysiol. 2005;93:1209-22; J Neurosci. 2006;26:6096-102; Front Neurol. 2015;6:214), but Dr. Zheng and coauthors noted “sparse” connections between the hand and that part of the brain limit the body’s ability to compensate for spasticity and functional loss.
The latest study followed earlier studies, including one by Dr. Zheng’s coauthors (J Hand Surg Br. 1992;17:518-21), that reported the paralyzed hand could be connected to the unaffected hemisphere by transferring a cervical spine nerve from the nonparalyzed side, a treatment previously reported for injuries of the brachial plexus. Of the five nerves of the brachial plexus, Dr. Zheng and coauthors chose the C7 nerve because it accounts for about 20% of the nerve fibers in the brachial bundle and severing the nerve typically results in transient weakness and numbness in the arm or leg on the same side. Hence, when evaluating the hand on the side of the donor graft, the researchers found no significant changes in power, tactile threshold, or two-point discrimination as a result of surgery.
Their surgical approach was a modification of the C7 nerve transfer method that Dr. Zheng and coauthors had previously reported (Microsurgery. 2011;31:404-8; Neurosurgery. 2015;76:187-95). The operation involved making an incision at the superior aspect of the sternum, mobilizing the donor C7 nerve on the nonparalyzed side, and routing it between the spinal column and esophagus. Then, an anastomosis was performed directly with the C7 nerve on the paralyzed side.
Rehabilitation therapy for both the surgery group and controls was identical, administered four times weekly for 12 months at a single facility, although surgery patients wore an immobilizing cast after their operations.
The nature of the study population – men of varying ages with varying causes of the underlying cerebral lesions – makes it difficult to generalize the findings, Dr. Zheng and coauthors noted. “A larger cohort, followed for a longer period, would be necessary to determine whether cervical nerve transfer results in safe, consistent, and long-term improvements in the function of an arm that is chronically paralyzed as a result of a cerebral lesion,” the authors concluded.
Grants from the following supported the study: National Natural Science Foundation of China; Science and Technology Commission of Shanghai Municipality; Health and Family Planning Commission of Shanghai; and Shanghai Shen-Kang Hospital Development Center.
The results that Dr. Zheng and coauthors reported “are exciting,” said Robert J. Spinner, MD, Alexander Y. Shin, MD, and Allen T. Bishop, MD, in an accompanying editorial, “but need clarification and confirmation” (N Engl J Med. 2017 Dec 20. doi: 10.1056/NEJMe1713313).
Among questions Dr. Spinner and coauthors raised about the study is whether distal muscles can functionally reinnervate in a year, and if C7 neurotomy on the paralyzed side led to improvements in spasticity and function. “The C7 neurotomy itself, associated with an immediate reduction in spasticity, represents a major advance for some patients with brain injury who have poor function and spasticity,” the authors of the editorial noted. Improvement of the damaged motor cortex, which ongoing physical therapy may enhance, may also contribute to a reduction in spasticity.
Dr. Spinner and coauthors also cited a previous trial by some of Dr. Zheng’s coauthors that showed 49% of patients with brachial plexus injury had motor recovery within 7 years (Chin Med J [Engl]. 2013;126:3865-8). “The presence of physiological connectivity observed in the trials does not necessarily equate with functional recovery,” the authors stated.
Future studies of surgical C7 nerve transfer in patients with one-sided arm paralysis should include patients who have C7 neurotomy without nerve transfer, Dr. Spinner and coauthors said. They also noted that Dr. Zheng and coauthors perform a relatively high volume of these operations, so their results may not be easy to reproduce elsewhere.
“Factors other than technical ones, including differences in body-mass index and limb length across different populations, may lead to different surgical outcomes,” Dr. Spinner and coauthors said. Future research should focus on ways to enhance or speed up nerve regeneration, improve plasticity, and maximize rehabilitation, they added.
Dr. Spinner, Dr. Shin, and Dr. Bishop are with the departments of neurologic surgery and orthopedics, division of hand surgery, at the Mayo Clinic in Rochester, Minn.
The results that Dr. Zheng and coauthors reported “are exciting,” said Robert J. Spinner, MD, Alexander Y. Shin, MD, and Allen T. Bishop, MD, in an accompanying editorial, “but need clarification and confirmation” (N Engl J Med. 2017 Dec 20. doi: 10.1056/NEJMe1713313).
Among questions Dr. Spinner and coauthors raised about the study is whether distal muscles can functionally reinnervate in a year, and if C7 neurotomy on the paralyzed side led to improvements in spasticity and function. “The C7 neurotomy itself, associated with an immediate reduction in spasticity, represents a major advance for some patients with brain injury who have poor function and spasticity,” the authors of the editorial noted. Improvement of the damaged motor cortex, which ongoing physical therapy may enhance, may also contribute to a reduction in spasticity.
Dr. Spinner and coauthors also cited a previous trial by some of Dr. Zheng’s coauthors that showed 49% of patients with brachial plexus injury had motor recovery within 7 years (Chin Med J [Engl]. 2013;126:3865-8). “The presence of physiological connectivity observed in the trials does not necessarily equate with functional recovery,” the authors stated.
Future studies of surgical C7 nerve transfer in patients with one-sided arm paralysis should include patients who have C7 neurotomy without nerve transfer, Dr. Spinner and coauthors said. They also noted that Dr. Zheng and coauthors perform a relatively high volume of these operations, so their results may not be easy to reproduce elsewhere.
“Factors other than technical ones, including differences in body-mass index and limb length across different populations, may lead to different surgical outcomes,” Dr. Spinner and coauthors said. Future research should focus on ways to enhance or speed up nerve regeneration, improve plasticity, and maximize rehabilitation, they added.
Dr. Spinner, Dr. Shin, and Dr. Bishop are with the departments of neurologic surgery and orthopedics, division of hand surgery, at the Mayo Clinic in Rochester, Minn.
The results that Dr. Zheng and coauthors reported “are exciting,” said Robert J. Spinner, MD, Alexander Y. Shin, MD, and Allen T. Bishop, MD, in an accompanying editorial, “but need clarification and confirmation” (N Engl J Med. 2017 Dec 20. doi: 10.1056/NEJMe1713313).
Among questions Dr. Spinner and coauthors raised about the study is whether distal muscles can functionally reinnervate in a year, and if C7 neurotomy on the paralyzed side led to improvements in spasticity and function. “The C7 neurotomy itself, associated with an immediate reduction in spasticity, represents a major advance for some patients with brain injury who have poor function and spasticity,” the authors of the editorial noted. Improvement of the damaged motor cortex, which ongoing physical therapy may enhance, may also contribute to a reduction in spasticity.
Dr. Spinner and coauthors also cited a previous trial by some of Dr. Zheng’s coauthors that showed 49% of patients with brachial plexus injury had motor recovery within 7 years (Chin Med J [Engl]. 2013;126:3865-8). “The presence of physiological connectivity observed in the trials does not necessarily equate with functional recovery,” the authors stated.
Future studies of surgical C7 nerve transfer in patients with one-sided arm paralysis should include patients who have C7 neurotomy without nerve transfer, Dr. Spinner and coauthors said. They also noted that Dr. Zheng and coauthors perform a relatively high volume of these operations, so their results may not be easy to reproduce elsewhere.
“Factors other than technical ones, including differences in body-mass index and limb length across different populations, may lead to different surgical outcomes,” Dr. Spinner and coauthors said. Future research should focus on ways to enhance or speed up nerve regeneration, improve plasticity, and maximize rehabilitation, they added.
Dr. Spinner, Dr. Shin, and Dr. Bishop are with the departments of neurologic surgery and orthopedics, division of hand surgery, at the Mayo Clinic in Rochester, Minn.
Patients with spastic arm paralysis who received a contralateral C7 nerve graft from their nonparalyzed side to their paralyzed side led to greater improvement in arm function and reduction in spasticity after a year, compared with rehabilitation alone, investigators from Huashan Hospital in China reported online Jan. 3 in the New England Journal of Medicine.
The researchers randomly assigned 36 patients who had unilateral arm paralysis for at least 5 years to either surgical C7 nerve transfer plus rehabilitation or rehabilitation only. Results of the trial’s primary outcome – arm function using the Fugl-Meyer score – showed that those in the surgery group had an average increase of 17.7, while those in the rehabilitation-only group had an average increase of 2.6 (P less than .001). This 15.1-point difference had a 95% confidence interval ranging from 12.2 to 17.9.
To evaluate spasticity, the researchers used the Modified Ashworth Scale, which is a 0-5 scale to score spasticity; a higher score means more spasticity. Surgery patients saw improvement from baseline in all five areas measured across the board, and none saw worsening in scores. The smallest difference between the two groups was in thumb extension, with 15 surgery patients having a 1- and 2-unit improvement and 3 having no change, while 7 controls showed a 1- or 2-unit improvement, another 7 showed no improvement, and 4 had a 1-unit worsening in score (P less than .001). At 1 year, 16 (89%) of surgery patients could accomplish three or more of the functional tasks researchers gave them, whereas none of the controls could.
“The majority of clinical improvements coincided with physiological evidence of connectivity between the hemisphere on the side of the donor nerve and the paralyzed arm,” said lead author Mou-Xiong Zheng, MD, PhD, of the department of hand surgery at Huashan Hospital at Fudan University in Shanghai, and colleagues.
The research by Dr. Zheng and coauthors arises from what is known about hand paralysis after stroke, that damage to the contralateral cerebral hemisphere arises from interruption of the inhibitory activity of upper motor neurons, which causes spasticity, along with hand weakness and loss of fractionated fine motor control. Other studies have noted activity in the cerebral hemisphere on the same side of paralysis during recovery (Neuroimage. 2004;22:1775-83; J Neurophysiol. 2005;93:1209-22; J Neurosci. 2006;26:6096-102; Front Neurol. 2015;6:214), but Dr. Zheng and coauthors noted “sparse” connections between the hand and that part of the brain limit the body’s ability to compensate for spasticity and functional loss.
The latest study followed earlier studies, including one by Dr. Zheng’s coauthors (J Hand Surg Br. 1992;17:518-21), that reported the paralyzed hand could be connected to the unaffected hemisphere by transferring a cervical spine nerve from the nonparalyzed side, a treatment previously reported for injuries of the brachial plexus. Of the five nerves of the brachial plexus, Dr. Zheng and coauthors chose the C7 nerve because it accounts for about 20% of the nerve fibers in the brachial bundle and severing the nerve typically results in transient weakness and numbness in the arm or leg on the same side. Hence, when evaluating the hand on the side of the donor graft, the researchers found no significant changes in power, tactile threshold, or two-point discrimination as a result of surgery.
Their surgical approach was a modification of the C7 nerve transfer method that Dr. Zheng and coauthors had previously reported (Microsurgery. 2011;31:404-8; Neurosurgery. 2015;76:187-95). The operation involved making an incision at the superior aspect of the sternum, mobilizing the donor C7 nerve on the nonparalyzed side, and routing it between the spinal column and esophagus. Then, an anastomosis was performed directly with the C7 nerve on the paralyzed side.
Rehabilitation therapy for both the surgery group and controls was identical, administered four times weekly for 12 months at a single facility, although surgery patients wore an immobilizing cast after their operations.
The nature of the study population – men of varying ages with varying causes of the underlying cerebral lesions – makes it difficult to generalize the findings, Dr. Zheng and coauthors noted. “A larger cohort, followed for a longer period, would be necessary to determine whether cervical nerve transfer results in safe, consistent, and long-term improvements in the function of an arm that is chronically paralyzed as a result of a cerebral lesion,” the authors concluded.
Grants from the following supported the study: National Natural Science Foundation of China; Science and Technology Commission of Shanghai Municipality; Health and Family Planning Commission of Shanghai; and Shanghai Shen-Kang Hospital Development Center.
Patients with spastic arm paralysis who received a contralateral C7 nerve graft from their nonparalyzed side to their paralyzed side led to greater improvement in arm function and reduction in spasticity after a year, compared with rehabilitation alone, investigators from Huashan Hospital in China reported online Jan. 3 in the New England Journal of Medicine.
The researchers randomly assigned 36 patients who had unilateral arm paralysis for at least 5 years to either surgical C7 nerve transfer plus rehabilitation or rehabilitation only. Results of the trial’s primary outcome – arm function using the Fugl-Meyer score – showed that those in the surgery group had an average increase of 17.7, while those in the rehabilitation-only group had an average increase of 2.6 (P less than .001). This 15.1-point difference had a 95% confidence interval ranging from 12.2 to 17.9.
To evaluate spasticity, the researchers used the Modified Ashworth Scale, which is a 0-5 scale to score spasticity; a higher score means more spasticity. Surgery patients saw improvement from baseline in all five areas measured across the board, and none saw worsening in scores. The smallest difference between the two groups was in thumb extension, with 15 surgery patients having a 1- and 2-unit improvement and 3 having no change, while 7 controls showed a 1- or 2-unit improvement, another 7 showed no improvement, and 4 had a 1-unit worsening in score (P less than .001). At 1 year, 16 (89%) of surgery patients could accomplish three or more of the functional tasks researchers gave them, whereas none of the controls could.
“The majority of clinical improvements coincided with physiological evidence of connectivity between the hemisphere on the side of the donor nerve and the paralyzed arm,” said lead author Mou-Xiong Zheng, MD, PhD, of the department of hand surgery at Huashan Hospital at Fudan University in Shanghai, and colleagues.
The research by Dr. Zheng and coauthors arises from what is known about hand paralysis after stroke, that damage to the contralateral cerebral hemisphere arises from interruption of the inhibitory activity of upper motor neurons, which causes spasticity, along with hand weakness and loss of fractionated fine motor control. Other studies have noted activity in the cerebral hemisphere on the same side of paralysis during recovery (Neuroimage. 2004;22:1775-83; J Neurophysiol. 2005;93:1209-22; J Neurosci. 2006;26:6096-102; Front Neurol. 2015;6:214), but Dr. Zheng and coauthors noted “sparse” connections between the hand and that part of the brain limit the body’s ability to compensate for spasticity and functional loss.
The latest study followed earlier studies, including one by Dr. Zheng’s coauthors (J Hand Surg Br. 1992;17:518-21), that reported the paralyzed hand could be connected to the unaffected hemisphere by transferring a cervical spine nerve from the nonparalyzed side, a treatment previously reported for injuries of the brachial plexus. Of the five nerves of the brachial plexus, Dr. Zheng and coauthors chose the C7 nerve because it accounts for about 20% of the nerve fibers in the brachial bundle and severing the nerve typically results in transient weakness and numbness in the arm or leg on the same side. Hence, when evaluating the hand on the side of the donor graft, the researchers found no significant changes in power, tactile threshold, or two-point discrimination as a result of surgery.
Their surgical approach was a modification of the C7 nerve transfer method that Dr. Zheng and coauthors had previously reported (Microsurgery. 2011;31:404-8; Neurosurgery. 2015;76:187-95). The operation involved making an incision at the superior aspect of the sternum, mobilizing the donor C7 nerve on the nonparalyzed side, and routing it between the spinal column and esophagus. Then, an anastomosis was performed directly with the C7 nerve on the paralyzed side.
Rehabilitation therapy for both the surgery group and controls was identical, administered four times weekly for 12 months at a single facility, although surgery patients wore an immobilizing cast after their operations.
The nature of the study population – men of varying ages with varying causes of the underlying cerebral lesions – makes it difficult to generalize the findings, Dr. Zheng and coauthors noted. “A larger cohort, followed for a longer period, would be necessary to determine whether cervical nerve transfer results in safe, consistent, and long-term improvements in the function of an arm that is chronically paralyzed as a result of a cerebral lesion,” the authors concluded.
Grants from the following supported the study: National Natural Science Foundation of China; Science and Technology Commission of Shanghai Municipality; Health and Family Planning Commission of Shanghai; and Shanghai Shen-Kang Hospital Development Center.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Mean increase in Fugl-Meyer score in the paralyzed arm was 17.7 in the surgery group and 2.6 in the control group at 12 months (P less than .001).
Data source: Thirty-six patients with unilateral arm paralysis randomly assigned to C7 nerve transfer plus rehabilitation or rehabilitation alone.
Disclosures: The National Natural Science Foundation of China, the Science and Technology Commission of Shanghai Municipality, the Health and Family Planning Commission of Shanghai, and the Shanghai Shen-Kang Hospital Development Center provided funding for the study.
Source: Zheng M et al. N Engl J Med. 2018;378:22-34
Massachusetts named healthiest state for 2017
A year of surprises ended with one more bit of unexpected news:
Massachusetts’ win may have knocked Hawaii out of the top spot for the first time since 2011, but the Aloha State was still second out of 50 in 2017. Two other New England states were in the top five: Vermont in third and Connecticut in fifth, with Utah sandwiched between them in fourth, the United Health Foundation said in its latest report.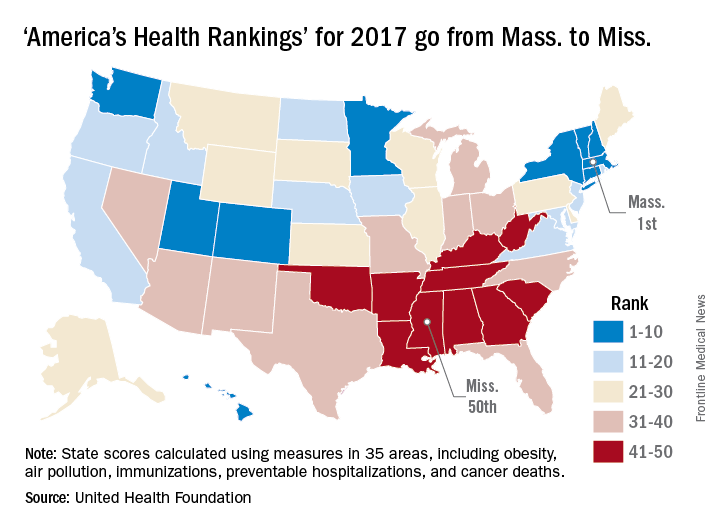
The report ranks states using 35 measures in five broad areas: behaviors, community and environment, policy, clinical care, and outcomes. The measures include drug-related death rate, percentage of children in poverty, public health funding per person, mental health provider rate, and diabetes rate.
“America’s Health Rankings” is funded entirely by the private, not-for-profit United Health Foundation, founded by UnitedHealth Group, which operates UnitedHealthcare.
A year of surprises ended with one more bit of unexpected news:
Massachusetts’ win may have knocked Hawaii out of the top spot for the first time since 2011, but the Aloha State was still second out of 50 in 2017. Two other New England states were in the top five: Vermont in third and Connecticut in fifth, with Utah sandwiched between them in fourth, the United Health Foundation said in its latest report.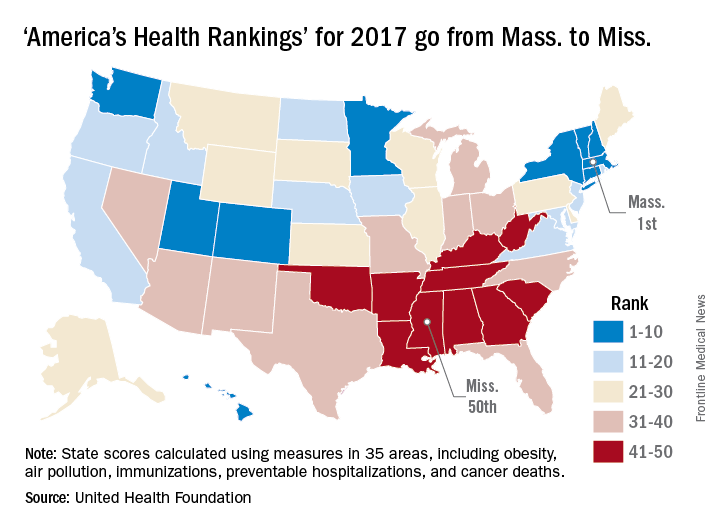
The report ranks states using 35 measures in five broad areas: behaviors, community and environment, policy, clinical care, and outcomes. The measures include drug-related death rate, percentage of children in poverty, public health funding per person, mental health provider rate, and diabetes rate.
“America’s Health Rankings” is funded entirely by the private, not-for-profit United Health Foundation, founded by UnitedHealth Group, which operates UnitedHealthcare.
A year of surprises ended with one more bit of unexpected news:
Massachusetts’ win may have knocked Hawaii out of the top spot for the first time since 2011, but the Aloha State was still second out of 50 in 2017. Two other New England states were in the top five: Vermont in third and Connecticut in fifth, with Utah sandwiched between them in fourth, the United Health Foundation said in its latest report.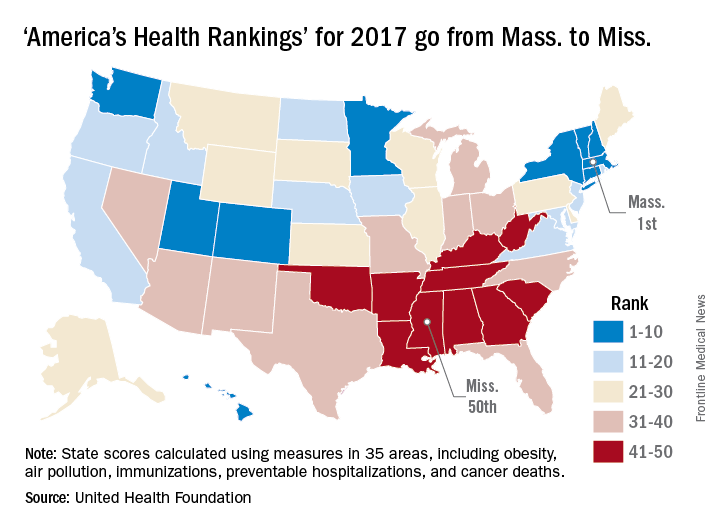
The report ranks states using 35 measures in five broad areas: behaviors, community and environment, policy, clinical care, and outcomes. The measures include drug-related death rate, percentage of children in poverty, public health funding per person, mental health provider rate, and diabetes rate.
“America’s Health Rankings” is funded entirely by the private, not-for-profit United Health Foundation, founded by UnitedHealth Group, which operates UnitedHealthcare.
Withholding elective surgery in smokers, obese patients
No one will argue that obesity and tobacco aren’t serious public health issues, underlying many causes of morbidity and mortality. As a result, they’re driving factors behind a fair amount of health care spending.
In England, the county of Hertfordshire recently adopted a new approach to this: a ban on routine, nonurgent surgeries for both. Those with a body mass index of 30-40 kg/m2 must lose 10% of their weight over 9 months to qualify for a procedure, while those with a BMI above 40 must lose 15%. Smokers have to go 8 weeks without a cigarette and take breath tests to prove it.
The group that formulated the plan noted that resources to help these groups achieve such goals are (and will continue to be) freely available.
Not unexpectedly, the plan is controversial. Robert West, MD, a professor of health psychology and director of tobacco studies at the University College London, told CNN that “rationing treatment on the basis of unhealthy behaviors betrays an extraordinary naivety about what drives those behaviors.”
Of course, this debate is nothing new. In December 2014, I wrote about surgeons in the United States who were refusing to do elective hernia repairs on smokers because of their higher complication rates.
A lot of this is framed in terms of money, since that’s the driving factor. Obese patients and smokers do have higher rates of surgical complications in general, with longer recoveries and, hence, higher costs. This policy tries to put greater responsibility on patients to maintain their own health and well-being. After all, financial resources are a finite, shared commodity.
Like everything in modern health care, there’s no easy answer. Insurers and doctors try to balance better outcomes vs. greater good and cost savings.
Medicine is, and always will be, an ongoing experiment, where some things work, some don’t, and we learn from time and experience.
Unfortunately, patients and their doctors are often caught in the middle, trapped between market and political forces on one side and caring for those who need us on the other. That’s never good, or easy, for those directly involved with individual patients on the front lines of medical care.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
No one will argue that obesity and tobacco aren’t serious public health issues, underlying many causes of morbidity and mortality. As a result, they’re driving factors behind a fair amount of health care spending.
In England, the county of Hertfordshire recently adopted a new approach to this: a ban on routine, nonurgent surgeries for both. Those with a body mass index of 30-40 kg/m2 must lose 10% of their weight over 9 months to qualify for a procedure, while those with a BMI above 40 must lose 15%. Smokers have to go 8 weeks without a cigarette and take breath tests to prove it.
The group that formulated the plan noted that resources to help these groups achieve such goals are (and will continue to be) freely available.
Not unexpectedly, the plan is controversial. Robert West, MD, a professor of health psychology and director of tobacco studies at the University College London, told CNN that “rationing treatment on the basis of unhealthy behaviors betrays an extraordinary naivety about what drives those behaviors.”
Of course, this debate is nothing new. In December 2014, I wrote about surgeons in the United States who were refusing to do elective hernia repairs on smokers because of their higher complication rates.
A lot of this is framed in terms of money, since that’s the driving factor. Obese patients and smokers do have higher rates of surgical complications in general, with longer recoveries and, hence, higher costs. This policy tries to put greater responsibility on patients to maintain their own health and well-being. After all, financial resources are a finite, shared commodity.
Like everything in modern health care, there’s no easy answer. Insurers and doctors try to balance better outcomes vs. greater good and cost savings.
Medicine is, and always will be, an ongoing experiment, where some things work, some don’t, and we learn from time and experience.
Unfortunately, patients and their doctors are often caught in the middle, trapped between market and political forces on one side and caring for those who need us on the other. That’s never good, or easy, for those directly involved with individual patients on the front lines of medical care.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
No one will argue that obesity and tobacco aren’t serious public health issues, underlying many causes of morbidity and mortality. As a result, they’re driving factors behind a fair amount of health care spending.
In England, the county of Hertfordshire recently adopted a new approach to this: a ban on routine, nonurgent surgeries for both. Those with a body mass index of 30-40 kg/m2 must lose 10% of their weight over 9 months to qualify for a procedure, while those with a BMI above 40 must lose 15%. Smokers have to go 8 weeks without a cigarette and take breath tests to prove it.
The group that formulated the plan noted that resources to help these groups achieve such goals are (and will continue to be) freely available.
Not unexpectedly, the plan is controversial. Robert West, MD, a professor of health psychology and director of tobacco studies at the University College London, told CNN that “rationing treatment on the basis of unhealthy behaviors betrays an extraordinary naivety about what drives those behaviors.”
Of course, this debate is nothing new. In December 2014, I wrote about surgeons in the United States who were refusing to do elective hernia repairs on smokers because of their higher complication rates.
A lot of this is framed in terms of money, since that’s the driving factor. Obese patients and smokers do have higher rates of surgical complications in general, with longer recoveries and, hence, higher costs. This policy tries to put greater responsibility on patients to maintain their own health and well-being. After all, financial resources are a finite, shared commodity.
Like everything in modern health care, there’s no easy answer. Insurers and doctors try to balance better outcomes vs. greater good and cost savings.
Medicine is, and always will be, an ongoing experiment, where some things work, some don’t, and we learn from time and experience.
Unfortunately, patients and their doctors are often caught in the middle, trapped between market and political forces on one side and caring for those who need us on the other. That’s never good, or easy, for those directly involved with individual patients on the front lines of medical care.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.













