User login
Official Newspaper of the American College of Surgeons
FDA: Laparoscopic power morcellators can spread malignant cells when used in women with occult uterine cancers*
Laparoscopic power morcellation appears capable of spreading fulminant uterine malignancies when used to remove uterine fibroids from women who have unsuspected uterine cancers.
A new Food and Drug Administration literature review of 23 studies found consistent evidence that women who undergo surgery using laparoscopic power morcellators (LPMs) for fibroids that were assumed to be benign may have an occult uterine sarcoma or leiomyosarcoma. In the FDA’s literature review of 12 studies from 2014 to 2016, women who received power morcellation were at a significantly increased risk of death, compared with those whose fibroids were removed by other methods.
The findings reaffirm the agency’s 2014 warnings about LPMs:
• LPMs are contraindicated in gynecologic surgery in which the tissue to be morcellated is known or suspected to contain malignancy.
• LPMs are contraindicated for removal of uterine tissue containing suspected fibroids in patients who are peri- or postmenopausal, or in candidates for en bloc tissue removal.
• Boxed warning: Uterine tissue may contain unsuspected cancer. The use of LPMs during fibroid surgery may spread cancer and decrease long-term survival of patients. This information should be shared with patients when considering surgery with the use of these devices.
“We recognize that some health organizations have reported a lower estimate of risk and that some groups continue to request that we scale back our recommendations. However, after looking at all the relevant data, we believe our estimates remain accurate, and our recommendation against the use of this device to remove fibroids in the vast majority of women is appropriate and critical to better protecting these women. We are committed to continuing to review new relevant data to assure patient safety.”
The review determined that 1 in 350 women undergoing hysterectomy or myomectomy for fibroids may have an occult uterine sarcoma, and that 1 in about 500 have an unsuspected leiomyosarcoma. The literature review clearly identified increased risk of uterine cancers and decreased survival when these women are treated with an LPM, as opposed to manual morcellation or en bloc removal.
Twelve studies of women with uterine cancers examined this outcome in comparison groups. LPMs were associated with a 2- to 3-times increased risk of disease recurrence, compared with manual morcellation or other fibroid removal methods. In some studies, disease-free survival was significantly shorter among those who had undergone an LPM procedure; others found a higher risk of death – including, in one study, almost a quintupling of mortality risk by 1 year (crude risk ratio, 4.75).
Device-related malignancies began appearing in 2013; since then, 262 cases have been reported. But after the 2014 warning, use of LPMs in this application has decreased sharply. Two studies examined this, one finding that LPM use in fibroid surgery dropped from 14% to 3% and the other, that it dropped from 11% to 0.02%.
“The agency also continues to recommend that the advantages and risks of using LPMs during fibroid surgery be thoroughly discussed between the patient and physician before surgery,” the paper concluded. “FDA continues to actively encourage and engage in research to evaluate outcomes for a range of treatment options for fibroids and support the development of safer alternatives for providing a minimally invasive approach.”
[email protected]
Laparoscopic power morcellation appears capable of spreading fulminant uterine malignancies when used to remove uterine fibroids from women who have unsuspected uterine cancers.
A new Food and Drug Administration literature review of 23 studies found consistent evidence that women who undergo surgery using laparoscopic power morcellators (LPMs) for fibroids that were assumed to be benign may have an occult uterine sarcoma or leiomyosarcoma. In the FDA’s literature review of 12 studies from 2014 to 2016, women who received power morcellation were at a significantly increased risk of death, compared with those whose fibroids were removed by other methods.
The findings reaffirm the agency’s 2014 warnings about LPMs:
• LPMs are contraindicated in gynecologic surgery in which the tissue to be morcellated is known or suspected to contain malignancy.
• LPMs are contraindicated for removal of uterine tissue containing suspected fibroids in patients who are peri- or postmenopausal, or in candidates for en bloc tissue removal.
• Boxed warning: Uterine tissue may contain unsuspected cancer. The use of LPMs during fibroid surgery may spread cancer and decrease long-term survival of patients. This information should be shared with patients when considering surgery with the use of these devices.
“We recognize that some health organizations have reported a lower estimate of risk and that some groups continue to request that we scale back our recommendations. However, after looking at all the relevant data, we believe our estimates remain accurate, and our recommendation against the use of this device to remove fibroids in the vast majority of women is appropriate and critical to better protecting these women. We are committed to continuing to review new relevant data to assure patient safety.”
The review determined that 1 in 350 women undergoing hysterectomy or myomectomy for fibroids may have an occult uterine sarcoma, and that 1 in about 500 have an unsuspected leiomyosarcoma. The literature review clearly identified increased risk of uterine cancers and decreased survival when these women are treated with an LPM, as opposed to manual morcellation or en bloc removal.
Twelve studies of women with uterine cancers examined this outcome in comparison groups. LPMs were associated with a 2- to 3-times increased risk of disease recurrence, compared with manual morcellation or other fibroid removal methods. In some studies, disease-free survival was significantly shorter among those who had undergone an LPM procedure; others found a higher risk of death – including, in one study, almost a quintupling of mortality risk by 1 year (crude risk ratio, 4.75).
Device-related malignancies began appearing in 2013; since then, 262 cases have been reported. But after the 2014 warning, use of LPMs in this application has decreased sharply. Two studies examined this, one finding that LPM use in fibroid surgery dropped from 14% to 3% and the other, that it dropped from 11% to 0.02%.
“The agency also continues to recommend that the advantages and risks of using LPMs during fibroid surgery be thoroughly discussed between the patient and physician before surgery,” the paper concluded. “FDA continues to actively encourage and engage in research to evaluate outcomes for a range of treatment options for fibroids and support the development of safer alternatives for providing a minimally invasive approach.”
[email protected]
Laparoscopic power morcellation appears capable of spreading fulminant uterine malignancies when used to remove uterine fibroids from women who have unsuspected uterine cancers.
A new Food and Drug Administration literature review of 23 studies found consistent evidence that women who undergo surgery using laparoscopic power morcellators (LPMs) for fibroids that were assumed to be benign may have an occult uterine sarcoma or leiomyosarcoma. In the FDA’s literature review of 12 studies from 2014 to 2016, women who received power morcellation were at a significantly increased risk of death, compared with those whose fibroids were removed by other methods.
The findings reaffirm the agency’s 2014 warnings about LPMs:
• LPMs are contraindicated in gynecologic surgery in which the tissue to be morcellated is known or suspected to contain malignancy.
• LPMs are contraindicated for removal of uterine tissue containing suspected fibroids in patients who are peri- or postmenopausal, or in candidates for en bloc tissue removal.
• Boxed warning: Uterine tissue may contain unsuspected cancer. The use of LPMs during fibroid surgery may spread cancer and decrease long-term survival of patients. This information should be shared with patients when considering surgery with the use of these devices.
“We recognize that some health organizations have reported a lower estimate of risk and that some groups continue to request that we scale back our recommendations. However, after looking at all the relevant data, we believe our estimates remain accurate, and our recommendation against the use of this device to remove fibroids in the vast majority of women is appropriate and critical to better protecting these women. We are committed to continuing to review new relevant data to assure patient safety.”
The review determined that 1 in 350 women undergoing hysterectomy or myomectomy for fibroids may have an occult uterine sarcoma, and that 1 in about 500 have an unsuspected leiomyosarcoma. The literature review clearly identified increased risk of uterine cancers and decreased survival when these women are treated with an LPM, as opposed to manual morcellation or en bloc removal.
Twelve studies of women with uterine cancers examined this outcome in comparison groups. LPMs were associated with a 2- to 3-times increased risk of disease recurrence, compared with manual morcellation or other fibroid removal methods. In some studies, disease-free survival was significantly shorter among those who had undergone an LPM procedure; others found a higher risk of death – including, in one study, almost a quintupling of mortality risk by 1 year (crude risk ratio, 4.75).
Device-related malignancies began appearing in 2013; since then, 262 cases have been reported. But after the 2014 warning, use of LPMs in this application has decreased sharply. Two studies examined this, one finding that LPM use in fibroid surgery dropped from 14% to 3% and the other, that it dropped from 11% to 0.02%.
“The agency also continues to recommend that the advantages and risks of using LPMs during fibroid surgery be thoroughly discussed between the patient and physician before surgery,” the paper concluded. “FDA continues to actively encourage and engage in research to evaluate outcomes for a range of treatment options for fibroids and support the development of safer alternatives for providing a minimally invasive approach.”
[email protected]
New anticoagulants pose challenges for surgeons
SAN DIEGO – A new class of is now commonly seen in patients and can require new strategies for management in the surgical setting. New drugs to reverse anticoagulation agents now need to be routinely considered in advance of surgery.
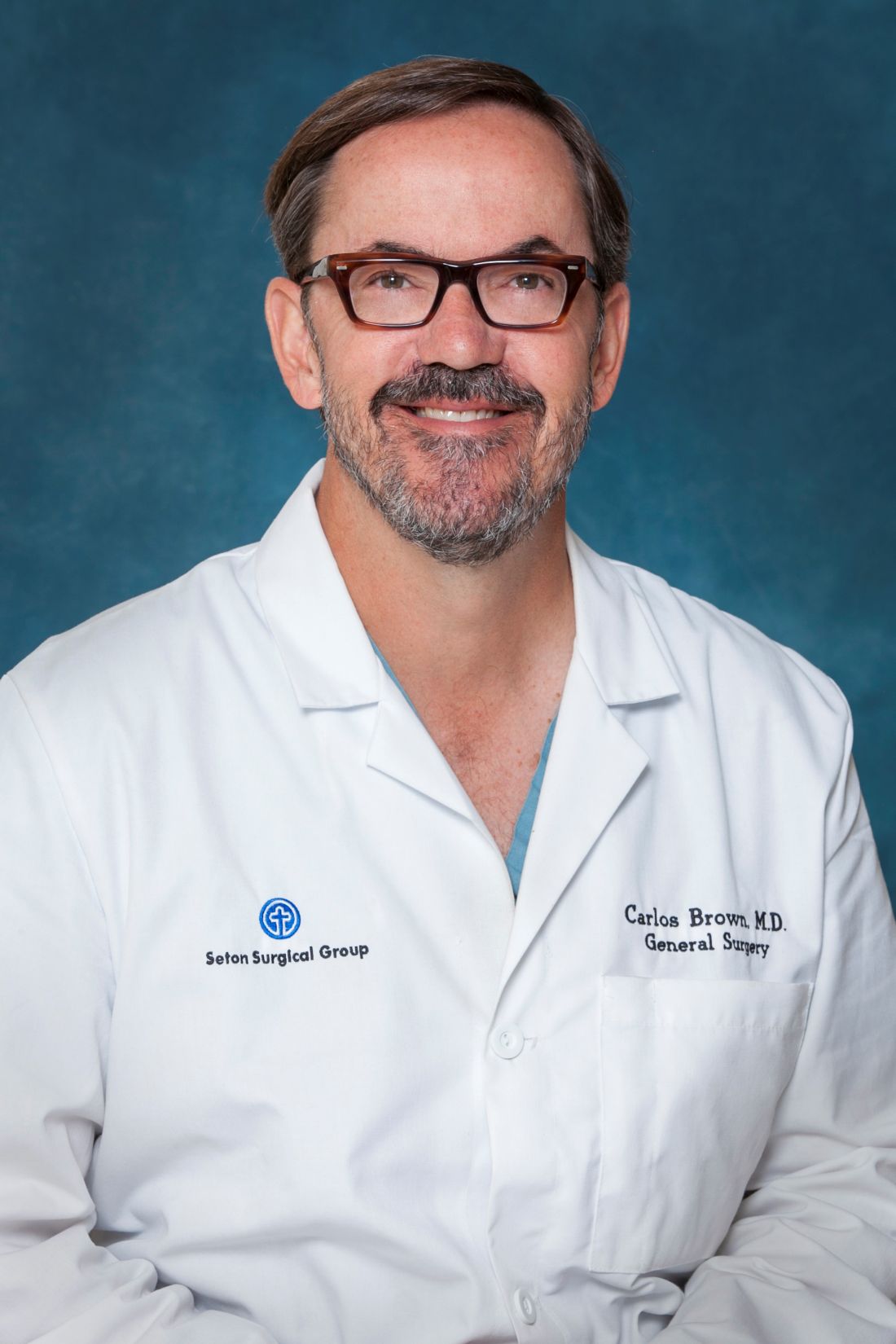
“They’re all over the place. It feels like everyone I see is on an anticoagulant, especially the new anticoagulants,” said Carlos V.R. Brown, MD, FACS, associate professor of surgery and chief of the division of acute care surgery at the University of Texas at Austin. “There’s a lot more learning that has to take place into how these medications work and how to take care of patients who use them.”
“Warfarin is slow, unpredictable, and requires monitoring and dose adjustment,” he said. In addition, interactions with food and other medications can be problematic, he said. The injectable drug heparin, meanwhile, requires monitoring and frequent dose adjustments, he said. “We’re in search of the ideal anticoagulant – one that’s oral, has a wide therapeutic window, is very predictable with rapid onset, and has minimal interaction with other food or drugs.”
Here’s the hitch, he said: “It probably doesn’t exist.”
There are now several alternatives to the old standbys on the market. One class, the direct thrombin inhibitor, is led by dabigatran etexilate (Pradaxa). Another class, the factor Xa inhibitors, includes rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa). From an elective surgery standpoint, Dr. Brown said in an interview, it has become important to understand how to reverse the effects of anticoagulants before a procedure.
To determine levels of the drugs, a TT (thrombin time) screening test is recommended for dabigatran and an anti-Xa test for rivaroxaban, apixaban, and edoxaban said Dr. Brown, referring to a 2017 study published in Critical Care Clinics. The paper summarized the available evidence and provided the optimal reversal strategy for bleeding patients with trauma on novel oral anticoagulants. The report also noted that newer blood thinners have a half-life of 7 or 12 hours and reach peak plasma level at 1-4 hours, depending on the medication (Crit Care Clin. 2017;33[1]135-52).
There may be no time to determine blood thinner levels in emergency situations. In those cases, patient or caregiver history about recent doses can be crucial, Dr. Brown said. “Knowing the patient’s history is going to be a key component,” he said.
Surgeons can turn to a variety of options to reverse the newer anticoagulants in an emergent setting, but only dabigatran has a Food and Drug Administration–approved reversal agent. Activated charcoal, PCC (Kcentra) and aPCC (FEIBA) can reverse dabigatran and oral factor Xa inhibitors, Dr. Brown said. Dialysis is also an option for dabigatran.
Another option to reverse dabigatran may be idarucizumab (Praxbind), a reversal agent. A 2017 industry-funded, open-label study reported successful results. It has been shown to work rapidly, Dr. Brown said, and the drug is now FDA approved (N Engl J Med. 2017 Aug 3;377[5]:431-41).
For oral factor Xa inhibitors, Dr. Brown said, andexanet alfa is now in a trial and doesn’t yet have FDA approval. “Presumably, it will provide a benefit over PCC because it’s directed at that specific medication,” he said.
Dr. Brown cautioned about the risks of reversing anticoagulants. “Any time you’re reversing an anticoagulant, the side effect is going to be clotting,” boosting the likelihood of events such as heart attack or stroke, he said. “You’re always weighing the risk versus the benefit of reversing.”
Dr. Brown has no relevant disclosures.
SAN DIEGO – A new class of is now commonly seen in patients and can require new strategies for management in the surgical setting. New drugs to reverse anticoagulation agents now need to be routinely considered in advance of surgery.
“They’re all over the place. It feels like everyone I see is on an anticoagulant, especially the new anticoagulants,” said Carlos V.R. Brown, MD, FACS, associate professor of surgery and chief of the division of acute care surgery at the University of Texas at Austin. “There’s a lot more learning that has to take place into how these medications work and how to take care of patients who use them.”
“Warfarin is slow, unpredictable, and requires monitoring and dose adjustment,” he said. In addition, interactions with food and other medications can be problematic, he said. The injectable drug heparin, meanwhile, requires monitoring and frequent dose adjustments, he said. “We’re in search of the ideal anticoagulant – one that’s oral, has a wide therapeutic window, is very predictable with rapid onset, and has minimal interaction with other food or drugs.”
Here’s the hitch, he said: “It probably doesn’t exist.”
There are now several alternatives to the old standbys on the market. One class, the direct thrombin inhibitor, is led by dabigatran etexilate (Pradaxa). Another class, the factor Xa inhibitors, includes rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa). From an elective surgery standpoint, Dr. Brown said in an interview, it has become important to understand how to reverse the effects of anticoagulants before a procedure.
To determine levels of the drugs, a TT (thrombin time) screening test is recommended for dabigatran and an anti-Xa test for rivaroxaban, apixaban, and edoxaban said Dr. Brown, referring to a 2017 study published in Critical Care Clinics. The paper summarized the available evidence and provided the optimal reversal strategy for bleeding patients with trauma on novel oral anticoagulants. The report also noted that newer blood thinners have a half-life of 7 or 12 hours and reach peak plasma level at 1-4 hours, depending on the medication (Crit Care Clin. 2017;33[1]135-52).
There may be no time to determine blood thinner levels in emergency situations. In those cases, patient or caregiver history about recent doses can be crucial, Dr. Brown said. “Knowing the patient’s history is going to be a key component,” he said.
Surgeons can turn to a variety of options to reverse the newer anticoagulants in an emergent setting, but only dabigatran has a Food and Drug Administration–approved reversal agent. Activated charcoal, PCC (Kcentra) and aPCC (FEIBA) can reverse dabigatran and oral factor Xa inhibitors, Dr. Brown said. Dialysis is also an option for dabigatran.
Another option to reverse dabigatran may be idarucizumab (Praxbind), a reversal agent. A 2017 industry-funded, open-label study reported successful results. It has been shown to work rapidly, Dr. Brown said, and the drug is now FDA approved (N Engl J Med. 2017 Aug 3;377[5]:431-41).
For oral factor Xa inhibitors, Dr. Brown said, andexanet alfa is now in a trial and doesn’t yet have FDA approval. “Presumably, it will provide a benefit over PCC because it’s directed at that specific medication,” he said.
Dr. Brown cautioned about the risks of reversing anticoagulants. “Any time you’re reversing an anticoagulant, the side effect is going to be clotting,” boosting the likelihood of events such as heart attack or stroke, he said. “You’re always weighing the risk versus the benefit of reversing.”
Dr. Brown has no relevant disclosures.
SAN DIEGO – A new class of is now commonly seen in patients and can require new strategies for management in the surgical setting. New drugs to reverse anticoagulation agents now need to be routinely considered in advance of surgery.
“They’re all over the place. It feels like everyone I see is on an anticoagulant, especially the new anticoagulants,” said Carlos V.R. Brown, MD, FACS, associate professor of surgery and chief of the division of acute care surgery at the University of Texas at Austin. “There’s a lot more learning that has to take place into how these medications work and how to take care of patients who use them.”
“Warfarin is slow, unpredictable, and requires monitoring and dose adjustment,” he said. In addition, interactions with food and other medications can be problematic, he said. The injectable drug heparin, meanwhile, requires monitoring and frequent dose adjustments, he said. “We’re in search of the ideal anticoagulant – one that’s oral, has a wide therapeutic window, is very predictable with rapid onset, and has minimal interaction with other food or drugs.”
Here’s the hitch, he said: “It probably doesn’t exist.”
There are now several alternatives to the old standbys on the market. One class, the direct thrombin inhibitor, is led by dabigatran etexilate (Pradaxa). Another class, the factor Xa inhibitors, includes rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa). From an elective surgery standpoint, Dr. Brown said in an interview, it has become important to understand how to reverse the effects of anticoagulants before a procedure.
To determine levels of the drugs, a TT (thrombin time) screening test is recommended for dabigatran and an anti-Xa test for rivaroxaban, apixaban, and edoxaban said Dr. Brown, referring to a 2017 study published in Critical Care Clinics. The paper summarized the available evidence and provided the optimal reversal strategy for bleeding patients with trauma on novel oral anticoagulants. The report also noted that newer blood thinners have a half-life of 7 or 12 hours and reach peak plasma level at 1-4 hours, depending on the medication (Crit Care Clin. 2017;33[1]135-52).
There may be no time to determine blood thinner levels in emergency situations. In those cases, patient or caregiver history about recent doses can be crucial, Dr. Brown said. “Knowing the patient’s history is going to be a key component,” he said.
Surgeons can turn to a variety of options to reverse the newer anticoagulants in an emergent setting, but only dabigatran has a Food and Drug Administration–approved reversal agent. Activated charcoal, PCC (Kcentra) and aPCC (FEIBA) can reverse dabigatran and oral factor Xa inhibitors, Dr. Brown said. Dialysis is also an option for dabigatran.
Another option to reverse dabigatran may be idarucizumab (Praxbind), a reversal agent. A 2017 industry-funded, open-label study reported successful results. It has been shown to work rapidly, Dr. Brown said, and the drug is now FDA approved (N Engl J Med. 2017 Aug 3;377[5]:431-41).
For oral factor Xa inhibitors, Dr. Brown said, andexanet alfa is now in a trial and doesn’t yet have FDA approval. “Presumably, it will provide a benefit over PCC because it’s directed at that specific medication,” he said.
Dr. Brown cautioned about the risks of reversing anticoagulants. “Any time you’re reversing an anticoagulant, the side effect is going to be clotting,” boosting the likelihood of events such as heart attack or stroke, he said. “You’re always weighing the risk versus the benefit of reversing.”
Dr. Brown has no relevant disclosures.
EXPERT OPINION FROM THE ACS CLINICAL CONGRESS
High rate of arm morbidity in young breast cancer survivors
SAN ANTONIO – as compared with having a sentinel lymph node biopsy (SLNB), according to new findings.
In a large prospective cohort study that included 1,302 breast cancer patients aged 40 or younger, the incidence of arm swelling 1 year after diagnosis among women who underwent breast-conserving surgery was 6% for the SLNB group versus 24% for those who had ALND. Among patients who had a mastectomy, the rates were similar; 6% versus 23% for SLNB or ALND, respectively.
“Young breast cancer survivors report high rates of arm morbidity in the first year of follow-up,” said lead author Anne Kuijer, MD, of Dana-Farber Cancer Institute/Brigham and Women’s Hospital in Boston. “Axillary node dissection, increased BMI [body mass index] and socioeconomic status were all independently associated with an increased risk of arm swelling,” she said at the San Antonio Breast Cancer Symposium.
She noted that patients who received mastectomy with radiation therapy were twice as likely to have decreased range of motion at 1 year, compared with patients treated with breast-conserving treatment.
In this study, the authors evaluated the incidence of arm morbidity associated with both ALND and SLNB in patients who were enrolled in the Young Women’s Breast Cancer Study. This multicenter prospective cohort study was designed to explore biological, medical, and psychosocial issues experienced by young breast cancer patients.
Within this large cohort, 55% had undergone an SLNB only, and 41% an ALND. The remaining patients did not undergo either procedure.
The primary endpoint of this study was to examine the incidence of patient-reported arm swelling or decreased range of motion at 1 year after their breast cancer diagnosis. Patients used the Cancer Rehabilitation Evaluation System (CARES-SF) to measure their symptoms.
Overall, at 1 year, 13% of the cohort reported arm swelling, and 40% reported decreased range of motion in the ipsilateral arm.
Several factors were associated with a higher risk of arm morbidity. Patients with a BMI of greater than 25 were more likely to report arm swelling vs. those with lower BMI (odds ratio, 1.7; P = .03) as well as have less range of motion (OR, 1.5; P = .05). Women who reported feeling financially comfortable were 40% less likely to report swelling (P = .02) and 90% less likely to report decreased range of motion (P = .67).
In addition, those who underwent ALND were 3.4 times more likely to report swelling, compared with women who had SLNB, but it was not associated with a reduction in range of motion.
One limitation of the study is that the cohort included patients who had received treatment at large cancer centers in the Northeast, suggesting that they may have been of higher socioeconomic status and may have led more active lifestyles, compared with the general population. Another limitation is that arm morbidity was self-reported and not objectively measured.
“I think our findings highlight opportunities for preoperative counseling, early referral of patients to physical therapy, and identification of resources for support of those at increased risk,” said Dr. Kuijer.
SOURCE: Kuijer et al. SABCS Abstract GS5-03
SAN ANTONIO – as compared with having a sentinel lymph node biopsy (SLNB), according to new findings.
In a large prospective cohort study that included 1,302 breast cancer patients aged 40 or younger, the incidence of arm swelling 1 year after diagnosis among women who underwent breast-conserving surgery was 6% for the SLNB group versus 24% for those who had ALND. Among patients who had a mastectomy, the rates were similar; 6% versus 23% for SLNB or ALND, respectively.
“Young breast cancer survivors report high rates of arm morbidity in the first year of follow-up,” said lead author Anne Kuijer, MD, of Dana-Farber Cancer Institute/Brigham and Women’s Hospital in Boston. “Axillary node dissection, increased BMI [body mass index] and socioeconomic status were all independently associated with an increased risk of arm swelling,” she said at the San Antonio Breast Cancer Symposium.
She noted that patients who received mastectomy with radiation therapy were twice as likely to have decreased range of motion at 1 year, compared with patients treated with breast-conserving treatment.
In this study, the authors evaluated the incidence of arm morbidity associated with both ALND and SLNB in patients who were enrolled in the Young Women’s Breast Cancer Study. This multicenter prospective cohort study was designed to explore biological, medical, and psychosocial issues experienced by young breast cancer patients.
Within this large cohort, 55% had undergone an SLNB only, and 41% an ALND. The remaining patients did not undergo either procedure.
The primary endpoint of this study was to examine the incidence of patient-reported arm swelling or decreased range of motion at 1 year after their breast cancer diagnosis. Patients used the Cancer Rehabilitation Evaluation System (CARES-SF) to measure their symptoms.
Overall, at 1 year, 13% of the cohort reported arm swelling, and 40% reported decreased range of motion in the ipsilateral arm.
Several factors were associated with a higher risk of arm morbidity. Patients with a BMI of greater than 25 were more likely to report arm swelling vs. those with lower BMI (odds ratio, 1.7; P = .03) as well as have less range of motion (OR, 1.5; P = .05). Women who reported feeling financially comfortable were 40% less likely to report swelling (P = .02) and 90% less likely to report decreased range of motion (P = .67).
In addition, those who underwent ALND were 3.4 times more likely to report swelling, compared with women who had SLNB, but it was not associated with a reduction in range of motion.
One limitation of the study is that the cohort included patients who had received treatment at large cancer centers in the Northeast, suggesting that they may have been of higher socioeconomic status and may have led more active lifestyles, compared with the general population. Another limitation is that arm morbidity was self-reported and not objectively measured.
“I think our findings highlight opportunities for preoperative counseling, early referral of patients to physical therapy, and identification of resources for support of those at increased risk,” said Dr. Kuijer.
SOURCE: Kuijer et al. SABCS Abstract GS5-03
SAN ANTONIO – as compared with having a sentinel lymph node biopsy (SLNB), according to new findings.
In a large prospective cohort study that included 1,302 breast cancer patients aged 40 or younger, the incidence of arm swelling 1 year after diagnosis among women who underwent breast-conserving surgery was 6% for the SLNB group versus 24% for those who had ALND. Among patients who had a mastectomy, the rates were similar; 6% versus 23% for SLNB or ALND, respectively.
“Young breast cancer survivors report high rates of arm morbidity in the first year of follow-up,” said lead author Anne Kuijer, MD, of Dana-Farber Cancer Institute/Brigham and Women’s Hospital in Boston. “Axillary node dissection, increased BMI [body mass index] and socioeconomic status were all independently associated with an increased risk of arm swelling,” she said at the San Antonio Breast Cancer Symposium.
She noted that patients who received mastectomy with radiation therapy were twice as likely to have decreased range of motion at 1 year, compared with patients treated with breast-conserving treatment.
In this study, the authors evaluated the incidence of arm morbidity associated with both ALND and SLNB in patients who were enrolled in the Young Women’s Breast Cancer Study. This multicenter prospective cohort study was designed to explore biological, medical, and psychosocial issues experienced by young breast cancer patients.
Within this large cohort, 55% had undergone an SLNB only, and 41% an ALND. The remaining patients did not undergo either procedure.
The primary endpoint of this study was to examine the incidence of patient-reported arm swelling or decreased range of motion at 1 year after their breast cancer diagnosis. Patients used the Cancer Rehabilitation Evaluation System (CARES-SF) to measure their symptoms.
Overall, at 1 year, 13% of the cohort reported arm swelling, and 40% reported decreased range of motion in the ipsilateral arm.
Several factors were associated with a higher risk of arm morbidity. Patients with a BMI of greater than 25 were more likely to report arm swelling vs. those with lower BMI (odds ratio, 1.7; P = .03) as well as have less range of motion (OR, 1.5; P = .05). Women who reported feeling financially comfortable were 40% less likely to report swelling (P = .02) and 90% less likely to report decreased range of motion (P = .67).
In addition, those who underwent ALND were 3.4 times more likely to report swelling, compared with women who had SLNB, but it was not associated with a reduction in range of motion.
One limitation of the study is that the cohort included patients who had received treatment at large cancer centers in the Northeast, suggesting that they may have been of higher socioeconomic status and may have led more active lifestyles, compared with the general population. Another limitation is that arm morbidity was self-reported and not objectively measured.
“I think our findings highlight opportunities for preoperative counseling, early referral of patients to physical therapy, and identification of resources for support of those at increased risk,” said Dr. Kuijer.
SOURCE: Kuijer et al. SABCS Abstract GS5-03
REPORTING FROM SABCS 2017
Key clinical point: A significant rate of arm swelling and decreased range of motion was seen in young breast cancer patients 1 year after undergoing surgery.
Major finding: At 1 year, 13% of a large cohort of breast cancer patients aged 40 years or younger reported arm swelling, and 40% reported decreased range of motion in the ipsilateral arm.
Data source: Large prospective cohort study that included 1,302 breast cancer patients aged 40 or younger.
Disclosures:. This study was funded by the National Institutes of Health, the Susan G. Komen Foundation, The Pink Agenda, and the Breast Cancer Research Foundation. Dr. Kuijer and her colleagues declare no conflicts of interest.
Source: Kuijer et al. SABCS 2017 Abstract GS5-03.
Surgery residents cite time challenges to robotics training
Although a majority of surgical residents plan to incorporate robotics in practice, 80% cited time commitment as a barrier to completing a nonmandatory robotics curriculum, according to a survey published online in the American Journal of Surgery.
Most surgery residents agree that robotics training is important, but most academic institutions have not yet established a mandatory training program, wrote Vernissia Tam, MD, of the University of Pittsburgh and her colleagues (Am J Surg. 2017. doi: 10.1016/j.amjsurg.2017.08.051).
To determine resident attitudes about robotics and the impact of a robotics curriculum, the researchers surveyed 48 general surgery residents in 2014-2015 and 49 residents in 2016-2017 at a single academic center. Overall, 98% and 96% of the two groups, respectively, reported high interest improving robotic skills, and more than two-thirds reported plans to use robotics in their practices.
The introduction of a voluntary, structured robotics program yielded significant improvements in the percentage of residents using both a robotic backpack simulator (from 18% to 39%) and an inanimate box trainer (increased from 20% to 41%).
However, of 60 unique residents between the two survey time points, only 24 began the robotics curriculum (40%) and only 11 (18%) completed it. In a follow-up survey of residents who had not yet completed the robotics training, 80% said that “time away from clinical responsibilities and/or research was the most commonly cited barrier to curriculum completion,” Dr. Tam and her associates noted.
The study was limited in part by the use of data from a single center over a short period of time, but “we believe these results provide a broad needs assessment for a structured robotics program and identify barriers to implementing a novel curriculum,” the researchers wrote. Many health professionals argue that a competence-based program, rather than time-based, would be more effective and accessible to students, so “development of an inanimate deliberate practice system with weekly opportunities is a viable avenue to increase technical skills and learn surgical procedures,” they said.
The researchers had no financial conflicts to disclose. The study was supported in part by an Intuitive Surgical Education Grant.
SOURCE: Tam V et al. Am J Surg. 2017. doi: 10.1016/j.amjsurg.2017.08.051.
Although a majority of surgical residents plan to incorporate robotics in practice, 80% cited time commitment as a barrier to completing a nonmandatory robotics curriculum, according to a survey published online in the American Journal of Surgery.
Most surgery residents agree that robotics training is important, but most academic institutions have not yet established a mandatory training program, wrote Vernissia Tam, MD, of the University of Pittsburgh and her colleagues (Am J Surg. 2017. doi: 10.1016/j.amjsurg.2017.08.051).
To determine resident attitudes about robotics and the impact of a robotics curriculum, the researchers surveyed 48 general surgery residents in 2014-2015 and 49 residents in 2016-2017 at a single academic center. Overall, 98% and 96% of the two groups, respectively, reported high interest improving robotic skills, and more than two-thirds reported plans to use robotics in their practices.
The introduction of a voluntary, structured robotics program yielded significant improvements in the percentage of residents using both a robotic backpack simulator (from 18% to 39%) and an inanimate box trainer (increased from 20% to 41%).
However, of 60 unique residents between the two survey time points, only 24 began the robotics curriculum (40%) and only 11 (18%) completed it. In a follow-up survey of residents who had not yet completed the robotics training, 80% said that “time away from clinical responsibilities and/or research was the most commonly cited barrier to curriculum completion,” Dr. Tam and her associates noted.
The study was limited in part by the use of data from a single center over a short period of time, but “we believe these results provide a broad needs assessment for a structured robotics program and identify barriers to implementing a novel curriculum,” the researchers wrote. Many health professionals argue that a competence-based program, rather than time-based, would be more effective and accessible to students, so “development of an inanimate deliberate practice system with weekly opportunities is a viable avenue to increase technical skills and learn surgical procedures,” they said.
The researchers had no financial conflicts to disclose. The study was supported in part by an Intuitive Surgical Education Grant.
SOURCE: Tam V et al. Am J Surg. 2017. doi: 10.1016/j.amjsurg.2017.08.051.
Although a majority of surgical residents plan to incorporate robotics in practice, 80% cited time commitment as a barrier to completing a nonmandatory robotics curriculum, according to a survey published online in the American Journal of Surgery.
Most surgery residents agree that robotics training is important, but most academic institutions have not yet established a mandatory training program, wrote Vernissia Tam, MD, of the University of Pittsburgh and her colleagues (Am J Surg. 2017. doi: 10.1016/j.amjsurg.2017.08.051).
To determine resident attitudes about robotics and the impact of a robotics curriculum, the researchers surveyed 48 general surgery residents in 2014-2015 and 49 residents in 2016-2017 at a single academic center. Overall, 98% and 96% of the two groups, respectively, reported high interest improving robotic skills, and more than two-thirds reported plans to use robotics in their practices.
The introduction of a voluntary, structured robotics program yielded significant improvements in the percentage of residents using both a robotic backpack simulator (from 18% to 39%) and an inanimate box trainer (increased from 20% to 41%).
However, of 60 unique residents between the two survey time points, only 24 began the robotics curriculum (40%) and only 11 (18%) completed it. In a follow-up survey of residents who had not yet completed the robotics training, 80% said that “time away from clinical responsibilities and/or research was the most commonly cited barrier to curriculum completion,” Dr. Tam and her associates noted.
The study was limited in part by the use of data from a single center over a short period of time, but “we believe these results provide a broad needs assessment for a structured robotics program and identify barriers to implementing a novel curriculum,” the researchers wrote. Many health professionals argue that a competence-based program, rather than time-based, would be more effective and accessible to students, so “development of an inanimate deliberate practice system with weekly opportunities is a viable avenue to increase technical skills and learn surgical procedures,” they said.
The researchers had no financial conflicts to disclose. The study was supported in part by an Intuitive Surgical Education Grant.
SOURCE: Tam V et al. Am J Surg. 2017. doi: 10.1016/j.amjsurg.2017.08.051.
FROM THE AMERICAN JOURNAL OF SURGERY
Key clinical point: .
Major finding: 80% of surgical residents said that the length of time needed to complete a robotics curriculum was a barrier to doing so.
Data source: Survey of 97 general surgery residents conducted in 2014-2015 and 2016-2017.
Disclosures: The researchers had no financial conflicts to disclose. The study was supported in part by an Intuitive Surgical Education Grant.
Source: Tam V et al. Am J Surg. 2017. doi: 10.1016/j.amjsurg.2017.08.051.
Survey: Safety, rather than ethics, tops concerns about uterine transplantation
Uterine transplantation is generally seen as ethical, with acceptable risk levels for both donors and recipients, according to two parallel surveys given to women’s health physicians and to the general public.
The results, presented at the annual meeting of the American Society for Reproductive Medicine (ASRM), showed that “the majority of gynecologists surveyed find uterine transplantation to be an acceptable and ethical option for patients with uterine factor infertility,” wrote Pietro Bortoletto, MD, and his coauthors.
Similarly, about two-thirds of the general public found uterine transplantation permissible and ethical, according to responses from an age- and gender-balanced nationally representative survey.
The web-based surveys were designed to assess the personal beliefs of both the public and of physicians about the permissibility of uterine transplantation, and to evaluate respondents’ concerns about perceived risks associated with the procedure. Respondents in each survey were also asked to identify any ethical concerns they might have; recipients of both surveys received background information about uterine transplantation.
Dr. Bortoletto and his colleagues sent the survey by email to physicians who were members of ASRM and AAGL. Of the 4,216 physicians who were invited to take the survey, 447 (28.4%) completed it, though results were tallied just for the 414 respondents who were United States–based physicians.
Physician respondents, when asked whether women should be allowed to donate or receive a transplanted uterus, responded mostly in the affirmative: 20% strongly agreed and 36% agreed, while 23% were neutral. The remainder disagreed or strongly disagreed.
The possibility of complications for the recipient was identified as the top concern by about 50% of physician respondents. Next most concerning was fetal outcomes, of primary concern for about 28%, followed by complications to the donor and cost, each of which was of primary concern to 10% or fewer of the physician respondents.
The risk to donors of uterine transplantation was seen as acceptable by 73.7% of AAGL members and 71.7% of ASRM members; just over half of each group saw the risk as acceptable for the recipients and the infants, however.
Though over half of physician respondents (57.9% of AAGL members and 59.5% of ASRM members) felt that uterine transplantation should be a potential treatment option for women with absolute uterine factor infertility, fewer felt it should be covered by health insurance – 35.4% of AAGL members and 40.5% of ASRM members held this opinion.
Among the general public, over three quarters (78%) felt that women should be allowed to undergo uterine transplantation. Slightly fewer (67%) respondents to the public survey felt that uterine transplantation is ethical; those who agreed had slightly higher incomes and education levels (relative risk, 1.11 and 1.09, respectively). A similar number (66%) felt that uterine transplantation was an acceptable alternative to using a gestational carrier.
As was the case for physicians, fewer members of the general public (45%) agreed that health insurance should cover the procedure; here, women and Hispanics were more likely to agree (relative risk, 1.11 and 1.18, respectively).
The results of the survey of the general public were presented by first author Eduardo Hariton, MD, a coauthor of Dr. Bortoletto’s in the study of physician survey results. Both Dr. Hariton and Dr. Bortoletto are resident physicians in the department of obstetrics, gynecology, and reproductive biology at Brigham and Women’s Hospital, Boston.
The public survey was sent to a nationally representative sample, balanced by gender and age. Of 1,444 individuals who were recruited to receive the survey, 1,337 completed it. Ninety respondents reported that they found in vitro fertilization unacceptable; these responses were excluded, Dr. Hariton said in an interview. “We wanted to get at uterine transplantation per se,” rather than assisted reproductive technology in general.
Placing the ethics of uterine transplantation in a broader context, Dr. Bortoletto said in an interview that the United States is one of just a few countries that permit gestational surrogacy, with regulations varying by state. To his knowledge, he said, Ukraine and Russia are the only other two nations that permit compensation for surrogacy. Greece and the United Kingdom permit altruistic surrogacy, while gestational surrogacy of any sort is forbidden in the European Union. Thus, in those nations, uterine transplantation will be the only option for women who wish to bear their biological children.
“I think the main takeaway is that for people who had hesitation about [uterine transplantation], it was mainly around safety,” and not ethical concerns, said Dr. Hariton. “I was a bit surprised, but also encouraged, by the degree of support.”
Neither Dr. Hariton nor Dr. Bortoletto reported any conflicts of interest. The public opinion study was funded by an Expanding the Boundaries grant.
Uterine transplantation is generally seen as ethical, with acceptable risk levels for both donors and recipients, according to two parallel surveys given to women’s health physicians and to the general public.
The results, presented at the annual meeting of the American Society for Reproductive Medicine (ASRM), showed that “the majority of gynecologists surveyed find uterine transplantation to be an acceptable and ethical option for patients with uterine factor infertility,” wrote Pietro Bortoletto, MD, and his coauthors.
Similarly, about two-thirds of the general public found uterine transplantation permissible and ethical, according to responses from an age- and gender-balanced nationally representative survey.
The web-based surveys were designed to assess the personal beliefs of both the public and of physicians about the permissibility of uterine transplantation, and to evaluate respondents’ concerns about perceived risks associated with the procedure. Respondents in each survey were also asked to identify any ethical concerns they might have; recipients of both surveys received background information about uterine transplantation.
Dr. Bortoletto and his colleagues sent the survey by email to physicians who were members of ASRM and AAGL. Of the 4,216 physicians who were invited to take the survey, 447 (28.4%) completed it, though results were tallied just for the 414 respondents who were United States–based physicians.
Physician respondents, when asked whether women should be allowed to donate or receive a transplanted uterus, responded mostly in the affirmative: 20% strongly agreed and 36% agreed, while 23% were neutral. The remainder disagreed or strongly disagreed.
The possibility of complications for the recipient was identified as the top concern by about 50% of physician respondents. Next most concerning was fetal outcomes, of primary concern for about 28%, followed by complications to the donor and cost, each of which was of primary concern to 10% or fewer of the physician respondents.
The risk to donors of uterine transplantation was seen as acceptable by 73.7% of AAGL members and 71.7% of ASRM members; just over half of each group saw the risk as acceptable for the recipients and the infants, however.
Though over half of physician respondents (57.9% of AAGL members and 59.5% of ASRM members) felt that uterine transplantation should be a potential treatment option for women with absolute uterine factor infertility, fewer felt it should be covered by health insurance – 35.4% of AAGL members and 40.5% of ASRM members held this opinion.
Among the general public, over three quarters (78%) felt that women should be allowed to undergo uterine transplantation. Slightly fewer (67%) respondents to the public survey felt that uterine transplantation is ethical; those who agreed had slightly higher incomes and education levels (relative risk, 1.11 and 1.09, respectively). A similar number (66%) felt that uterine transplantation was an acceptable alternative to using a gestational carrier.
As was the case for physicians, fewer members of the general public (45%) agreed that health insurance should cover the procedure; here, women and Hispanics were more likely to agree (relative risk, 1.11 and 1.18, respectively).
The results of the survey of the general public were presented by first author Eduardo Hariton, MD, a coauthor of Dr. Bortoletto’s in the study of physician survey results. Both Dr. Hariton and Dr. Bortoletto are resident physicians in the department of obstetrics, gynecology, and reproductive biology at Brigham and Women’s Hospital, Boston.
The public survey was sent to a nationally representative sample, balanced by gender and age. Of 1,444 individuals who were recruited to receive the survey, 1,337 completed it. Ninety respondents reported that they found in vitro fertilization unacceptable; these responses were excluded, Dr. Hariton said in an interview. “We wanted to get at uterine transplantation per se,” rather than assisted reproductive technology in general.
Placing the ethics of uterine transplantation in a broader context, Dr. Bortoletto said in an interview that the United States is one of just a few countries that permit gestational surrogacy, with regulations varying by state. To his knowledge, he said, Ukraine and Russia are the only other two nations that permit compensation for surrogacy. Greece and the United Kingdom permit altruistic surrogacy, while gestational surrogacy of any sort is forbidden in the European Union. Thus, in those nations, uterine transplantation will be the only option for women who wish to bear their biological children.
“I think the main takeaway is that for people who had hesitation about [uterine transplantation], it was mainly around safety,” and not ethical concerns, said Dr. Hariton. “I was a bit surprised, but also encouraged, by the degree of support.”
Neither Dr. Hariton nor Dr. Bortoletto reported any conflicts of interest. The public opinion study was funded by an Expanding the Boundaries grant.
Uterine transplantation is generally seen as ethical, with acceptable risk levels for both donors and recipients, according to two parallel surveys given to women’s health physicians and to the general public.
The results, presented at the annual meeting of the American Society for Reproductive Medicine (ASRM), showed that “the majority of gynecologists surveyed find uterine transplantation to be an acceptable and ethical option for patients with uterine factor infertility,” wrote Pietro Bortoletto, MD, and his coauthors.
Similarly, about two-thirds of the general public found uterine transplantation permissible and ethical, according to responses from an age- and gender-balanced nationally representative survey.
The web-based surveys were designed to assess the personal beliefs of both the public and of physicians about the permissibility of uterine transplantation, and to evaluate respondents’ concerns about perceived risks associated with the procedure. Respondents in each survey were also asked to identify any ethical concerns they might have; recipients of both surveys received background information about uterine transplantation.
Dr. Bortoletto and his colleagues sent the survey by email to physicians who were members of ASRM and AAGL. Of the 4,216 physicians who were invited to take the survey, 447 (28.4%) completed it, though results were tallied just for the 414 respondents who were United States–based physicians.
Physician respondents, when asked whether women should be allowed to donate or receive a transplanted uterus, responded mostly in the affirmative: 20% strongly agreed and 36% agreed, while 23% were neutral. The remainder disagreed or strongly disagreed.
The possibility of complications for the recipient was identified as the top concern by about 50% of physician respondents. Next most concerning was fetal outcomes, of primary concern for about 28%, followed by complications to the donor and cost, each of which was of primary concern to 10% or fewer of the physician respondents.
The risk to donors of uterine transplantation was seen as acceptable by 73.7% of AAGL members and 71.7% of ASRM members; just over half of each group saw the risk as acceptable for the recipients and the infants, however.
Though over half of physician respondents (57.9% of AAGL members and 59.5% of ASRM members) felt that uterine transplantation should be a potential treatment option for women with absolute uterine factor infertility, fewer felt it should be covered by health insurance – 35.4% of AAGL members and 40.5% of ASRM members held this opinion.
Among the general public, over three quarters (78%) felt that women should be allowed to undergo uterine transplantation. Slightly fewer (67%) respondents to the public survey felt that uterine transplantation is ethical; those who agreed had slightly higher incomes and education levels (relative risk, 1.11 and 1.09, respectively). A similar number (66%) felt that uterine transplantation was an acceptable alternative to using a gestational carrier.
As was the case for physicians, fewer members of the general public (45%) agreed that health insurance should cover the procedure; here, women and Hispanics were more likely to agree (relative risk, 1.11 and 1.18, respectively).
The results of the survey of the general public were presented by first author Eduardo Hariton, MD, a coauthor of Dr. Bortoletto’s in the study of physician survey results. Both Dr. Hariton and Dr. Bortoletto are resident physicians in the department of obstetrics, gynecology, and reproductive biology at Brigham and Women’s Hospital, Boston.
The public survey was sent to a nationally representative sample, balanced by gender and age. Of 1,444 individuals who were recruited to receive the survey, 1,337 completed it. Ninety respondents reported that they found in vitro fertilization unacceptable; these responses were excluded, Dr. Hariton said in an interview. “We wanted to get at uterine transplantation per se,” rather than assisted reproductive technology in general.
Placing the ethics of uterine transplantation in a broader context, Dr. Bortoletto said in an interview that the United States is one of just a few countries that permit gestational surrogacy, with regulations varying by state. To his knowledge, he said, Ukraine and Russia are the only other two nations that permit compensation for surrogacy. Greece and the United Kingdom permit altruistic surrogacy, while gestational surrogacy of any sort is forbidden in the European Union. Thus, in those nations, uterine transplantation will be the only option for women who wish to bear their biological children.
“I think the main takeaway is that for people who had hesitation about [uterine transplantation], it was mainly around safety,” and not ethical concerns, said Dr. Hariton. “I was a bit surprised, but also encouraged, by the degree of support.”
Neither Dr. Hariton nor Dr. Bortoletto reported any conflicts of interest. The public opinion study was funded by an Expanding the Boundaries grant.
Medicaid’s share of state budgets continues to grow
State spending on Medicaid in fiscal 2017 was up 6.1% over 2016, and the program’s share of state budgets increased for the fifth year in a row, according to the National Association of State Budget Officers.
Total spending by the states on Medicaid benefits for more than 74 million individuals was an estimated $574 billion in 2017, which represented 29% of all expenditures. That compares with 28.7% in 2016 and 23.6% in 2012 – the last year that Medicaid’s share of state spending decreased, NASBO said in its annual State Expenditure Report.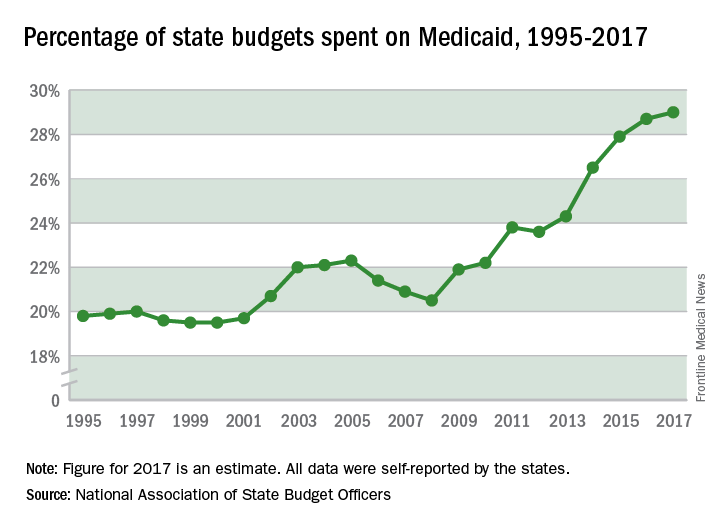
Enrollment rose by 2.9% from 2016 to 2017, which was down from the 3.9% increase seen from 2015 to 2016. Since October 2013, Medicaid enrollment is up 38% in expansion states and 12% in nonexpansion states, the report noted.
Enrollment increases are “the major driver” of spending growth, NASBO said, and “Medicaid’s annual spending growth from all fund sources has averaged 8.1% over the past 5 years, while the rest of total spending growth has averaged 2.2% annually.”
State spending on Medicaid in fiscal 2017 was up 6.1% over 2016, and the program’s share of state budgets increased for the fifth year in a row, according to the National Association of State Budget Officers.
Total spending by the states on Medicaid benefits for more than 74 million individuals was an estimated $574 billion in 2017, which represented 29% of all expenditures. That compares with 28.7% in 2016 and 23.6% in 2012 – the last year that Medicaid’s share of state spending decreased, NASBO said in its annual State Expenditure Report.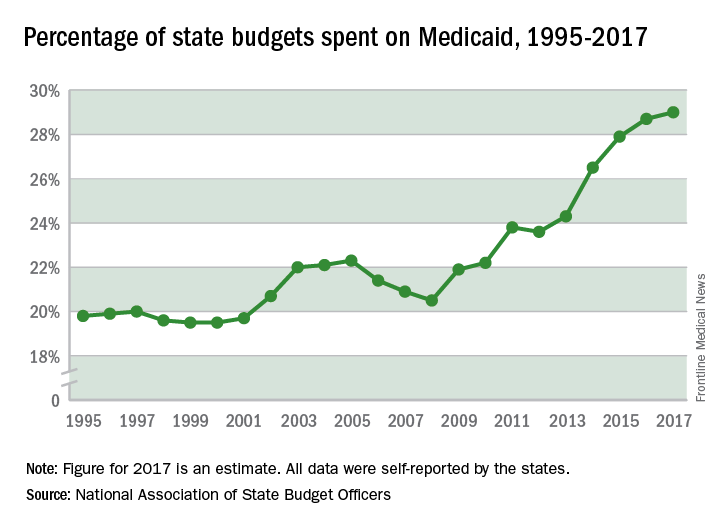
Enrollment rose by 2.9% from 2016 to 2017, which was down from the 3.9% increase seen from 2015 to 2016. Since October 2013, Medicaid enrollment is up 38% in expansion states and 12% in nonexpansion states, the report noted.
Enrollment increases are “the major driver” of spending growth, NASBO said, and “Medicaid’s annual spending growth from all fund sources has averaged 8.1% over the past 5 years, while the rest of total spending growth has averaged 2.2% annually.”
State spending on Medicaid in fiscal 2017 was up 6.1% over 2016, and the program’s share of state budgets increased for the fifth year in a row, according to the National Association of State Budget Officers.
Total spending by the states on Medicaid benefits for more than 74 million individuals was an estimated $574 billion in 2017, which represented 29% of all expenditures. That compares with 28.7% in 2016 and 23.6% in 2012 – the last year that Medicaid’s share of state spending decreased, NASBO said in its annual State Expenditure Report.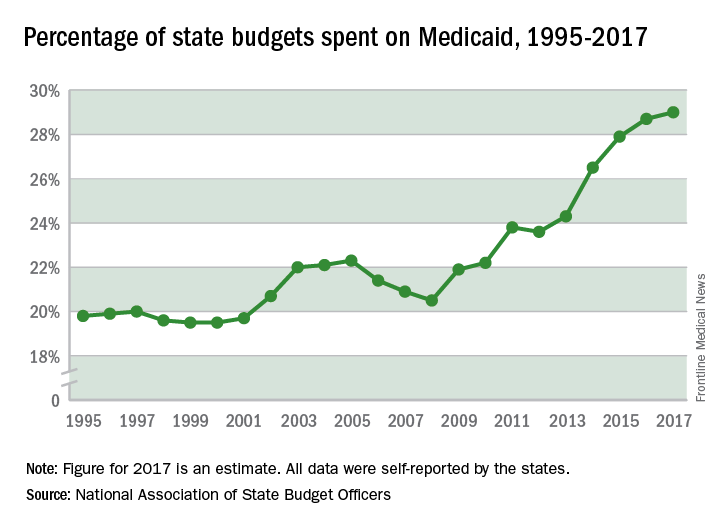
Enrollment rose by 2.9% from 2016 to 2017, which was down from the 3.9% increase seen from 2015 to 2016. Since October 2013, Medicaid enrollment is up 38% in expansion states and 12% in nonexpansion states, the report noted.
Enrollment increases are “the major driver” of spending growth, NASBO said, and “Medicaid’s annual spending growth from all fund sources has averaged 8.1% over the past 5 years, while the rest of total spending growth has averaged 2.2% annually.”
After 6 weeks, HealthCare.gov activity still ahead of last year
compared with the total at the end of week 4, according to the Centers for Medicare & Medicaid Services.
The 1.89 million plans that consumers selected over the 2-week period ending Dec. 9 brought this year’s total to 4.68 million after 6 weeks. That’s 16.5% higher than last year’s 6-week total of 4.02 million, but the difference has been getting smaller: After week 2 (enrollment figures were released only biweekly last year), the 2018 open season’s tally was higher than the 2017 open season’s week 2 tally by almost 47%, but after 4 weeks, the difference was only 30%, the CMS data show.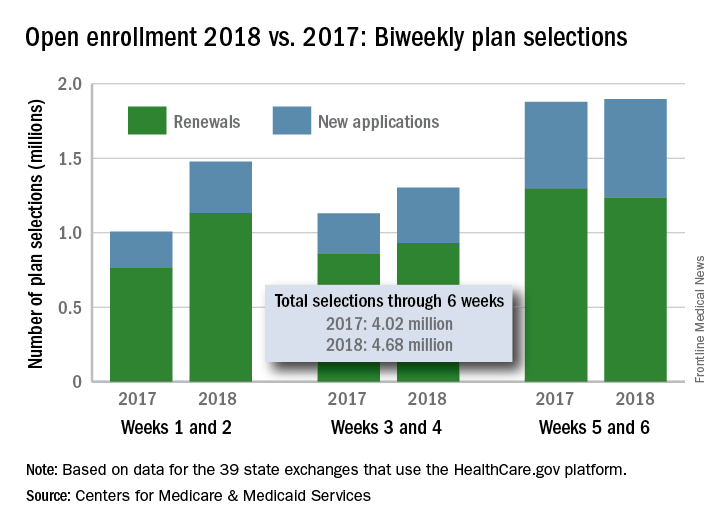
compared with the total at the end of week 4, according to the Centers for Medicare & Medicaid Services.
The 1.89 million plans that consumers selected over the 2-week period ending Dec. 9 brought this year’s total to 4.68 million after 6 weeks. That’s 16.5% higher than last year’s 6-week total of 4.02 million, but the difference has been getting smaller: After week 2 (enrollment figures were released only biweekly last year), the 2018 open season’s tally was higher than the 2017 open season’s week 2 tally by almost 47%, but after 4 weeks, the difference was only 30%, the CMS data show.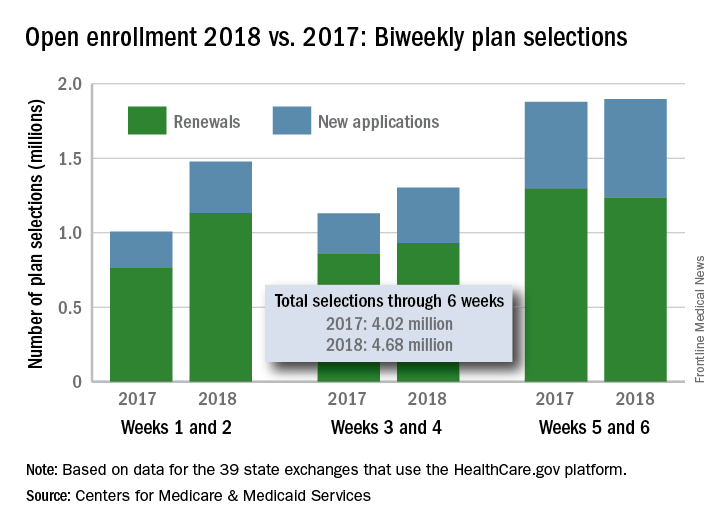
compared with the total at the end of week 4, according to the Centers for Medicare & Medicaid Services.
The 1.89 million plans that consumers selected over the 2-week period ending Dec. 9 brought this year’s total to 4.68 million after 6 weeks. That’s 16.5% higher than last year’s 6-week total of 4.02 million, but the difference has been getting smaller: After week 2 (enrollment figures were released only biweekly last year), the 2018 open season’s tally was higher than the 2017 open season’s week 2 tally by almost 47%, but after 4 weeks, the difference was only 30%, the CMS data show.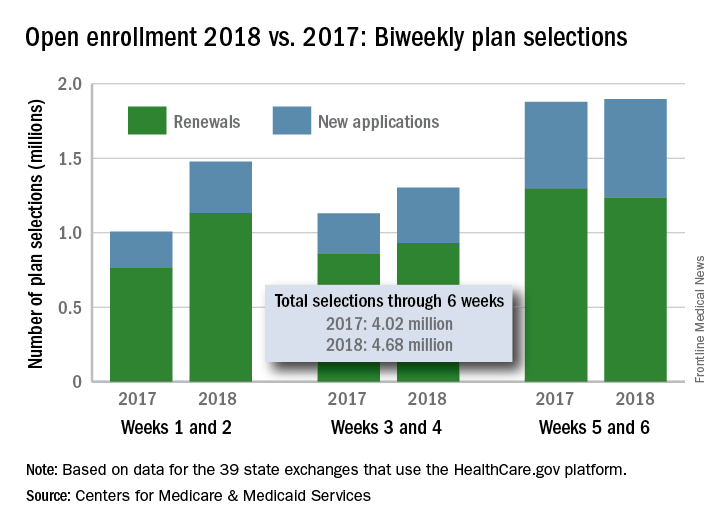
Recommended Reading: Best of 2017
Recommended Reading lists are something of a tradition for ACS Surgery News. This feature has appeared several times over the years and it has always proved among the most popular items in the publication. But the project hinges on input from our Editorial Advisory Board, the members of which are already regularly called upon to help vet the publication’s content and give their advice. They have gone the extra mile and have once again chosen their “Best of 2017” studies in their own specialty areas, along with commentary on why their choices should be of interest to all surgeons. We hope our readers will find the list and the comments of interest.
General surgery
Cogbill TH et al. Rural general surgery: A 38-year experience with a regional network established by an integrated health system in the Midwestern United States. J Am Coll Surg. 2017;225(1):115-24.
This article is of particular interest because it provides details of an innovative, regional system of surgical care at the critical access hospitals and referral centers that cooperate seamlessly to improve quality of care and quality of practice for rural surgeons. It could serve as a model for similar independent hospitals and practices in a region to improve the practice lives of the surgeons in rural communities and preserve access to local care for rural patients.
Dimou FM et al. Outcomes in older patients with grade III cholecystitis and cholecystostomy tube placement: A propensity score analysis. J Am Coll Surg. 2017;224(4):502-14.This study is valuable because it sheds light on the current status of treatment of severe acute cholecystitis in the United States and reports outcomes of patients who get initial tube cholecystostomy. It demonstrates potential drawbacks of following the Tokyo Guidelines: fewer patients receiving definitive treatment (cholecystectomy) and higher mortality rates and readmissions.
Karen E. Deveney, MD, FACS
Palliative Care
Gani F et al. Palliative care utilization among patients admitted for gastrointestinal and thoracic cancers. J Palliat Med. 2017 Nov 3; doi: 10.1089/jpm.2017.0295; epub ahead of print.
Is this a matter of “too little too late”? This retrospective cross-sectional analysis of patients identified in the National Inpatient Sample database admitted with a primary diagnosis of gastrointestinal and/or thoracic cancer determined that only 8.5% of patients admitted received palliative care services. Surgical patients were 79% less likely to have received a palliative care consultation, and then only after a prolonged length of stay or postoperative complication. Is referral to palliative care services hindered by its stigmatization with these outcomes?
Taylor LJ et al. A framework to improve surgeon communication in high-stakes surgical decisions: Best Case/Worst Case. JAMA Surgery. 2017;152(6):531-8.
My chief used to say, “You might not be teachable, but you are trainable!” After surgeons received training in the Best Case/Worst Case framework described in this paper, they demonstrated that it was possible to successfully change the focus of decision-making conversations from an isolated surgical problem – with its menu of technical solutions – instead into a discussion about treatment alternatives and outcomes. This intervention is a useful tool for one of the most invasive procedures of all – an exploration of a patient’s preferences and values that is necessary for shared decision making within the acute setting.
Makhani SS et al. Cognitive impairment and overall survival in frail surgical patients. J Amer Coll Surg. 2017 Nov;225(5):590-600.
In my preoperative discussions with families of frail patients, it is often quite evident that the factor driving their decision is the cognitive state of the patient and the consequences of its further decline, even when they are willing to accept the risks of physical frailty. This study in a large multidisciplinary cohort of patients undergoing major operations determined that a combined frailty (Fried frailty score) and cognitive assessment score (Emory Clock Draw Test) has a more powerful potential to predict adult patients at higher risk of overall survival than does either measurement alone. Dual frailty and cognitive screening appears to be a promising adjunct to the shared decision-making process.
Geoffrey P. Dunn, MD, FACS
Wilson DG et al. Patterns of care in hospitalized vascular patients at end of life. JAMA Surg. 2017;152(2):183-90.
This thoughtful study and the excellent accompanying invited commentary by William Schecter, MD, FACS, address a major, difficult issue that faces all physicians as our patients become older and sicker and our ability to keep them alive expands: How do we speak honestly with patients about their prognosis and likely outcomes and honor their autonomy in decision making?
Karen E. Deveney, MD, FACS
Practice Management
Robinson JR et al. Complexity of medical decision making in care provided by surgeons through patient portals. Surg Res. 2017;214:93-101.
This article describes an analysis of the content of patient portal messages exchanged between surgical providers and patients. The study demonstrates that more than 90% of these exchanges involved the delivery of medical care, and more than two-thirds of the messages contained medical decision making, which might have generated charges if done in a face-to-face outpatient encounter. The articles argues that surgeons are providing substantial medical care to their patients through patient portal message exchanges and suggests that models for compensation of this type of online care should be developed.
Gretchen Purcell Jackson, MD, FACS
Vascular Surgery
Bennett KM et al. Carotid artery stenting is associated with a higher incidence of major adverse clinical events than carotid endarterectomy in female patients. J Vasc Surg. 2017 Sep;66(3):794-801.
This article uses the ACS NSQIP database to assess outcomes of women undergoing intervention for carotid stenosis in a real-world setting and finds that major adverse cardiac events in the first 30 days is higher for carotid artery stenting (12.2%), compared with carotid endarterectomy (5.2%). What we need to keep in mind is that the practice of any intervention for asymptomatic carotid stenosis is being reevaluated in the new CREST study, which will compare current best medical management with carotid stenting and carotid endarterectomy. The indications are likely to change for all, but because women had less relative risk reduction in the early studies, we can expect that the benefits for intervention for women will continue to be less than those for men, calling to question when we should truly intervene, and how best to do so.
Gargiulo M et al. Outcomes of endovascular aneurysm repair performed in abdominal aortic aneurysms with large infrarenal necks. J Vasc Surg. 2017 Oct;66(4);1065-72.
This study found that endovascular aneurysm repair, performed in patients with large necks (greater than 28 mm), was associated with further neck enlargement at 2 years, and a higher risk of proximal type I endoleak, with the need for reintervention. This is one of many recent studies, all with similar findings. The issue becomes how we can best address larger infrarenal necks, whether by use of fenestrated grafts, snorkels/chimneys with extension of the seal zone, aptus, or other technologies. The question of whether all grafts have equal impacts on these more dilated necks has still to be elucidated. Nonetheless, when we stretch the instructions for use, there is an increased likelihood for more interventions.
Zettervall SL et al. Renal complications after EVAR with suprarenal versus infrarenal fixation among all users and routine users. J Vasc Surg. 2017 Oct;66(4):1305.
This study found that endografts with suprarenal fixation were associated with a greater decline in renal function, compared with those with infrarenal fixation, as well as with a longer length of stay. The reasons for the renal function decline are not entirely clear, and there was a slight increase in contrast use for those with suprarenal fixation but were otherwise similar when comparing comorbidities. Clearly, assessment of any impact on long-term renal function is important, and may affect future choice of endografts.
Linda Harris, MD, FACS
Bariatric Surgery
Rosenthal RJ et al. Obesity in America. Surg Obes Relat Dis. 2017 Oct;13(10):1643-50.
Although much has been reported on the dramatic benefits of bariatric surgery, it remains a matter of deep disappointment that only 1%-2% of the eligible population is receiving this life-saving therapy. This is a paper that reports and analyzes the results of a national survey that was conducted on behalf of the American Society for Metabolic & Bariatric Surgery, in an attempt to identify barriers to access, public misconceptions on obesity and its consequences, and other pertinent factors. Survey results included the findings that, although 80% of Americans considered obesity as the most serious health risk problem, there was a clear overestimation of the effectiveness of diet and exercise alone. The importance of this paper lies in the persistent lack of recognition and/or awareness of proven, safe, and durable medical and surgical options in the lay population, highlighting the importance of aligning efforts and resources toward educating both the public and referring physicians.
Adams TD et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017 Sep 21;377(12):1143-55
This paper reports the results of an observational, prospective study that followed patients who received gastric bypass, in comparison with a group of patients who desired but did not receive gastric bypass, and a third group of obese patients who did not seek surgery. The authors concluded that gastric bypass provided durable, 12-year remission and prevention of such lethal diseases as diabetes, hypertension, and dyslipidemia. The importance of this study is in its detailed follow-up, the exceedingly high retention rate of 90% at 12 years, and the comparisons made between surgical and nonsurgical groups, demonstrating not only the benefits of gastric bypass, but as importantly, the hazards of not receiving this treatment.
Schauer PR et al. Bariatric surgery versus intensive medical therapy for diabetes – 5-year outcomes. N Engl J Med. 2017 Feb 16;376(7):641-51.This paper is the latest installment of the long-term results from the STAMPEDE trial conducted at the Cleveland Clinic. STAMPEDE is a randomized, controlled trial that compared the best, most “intensive” medical therapy for type 2 diabetes vs. bariatric surgery (comprising a mix of gastric bypass and sleeve gastrectomy). Prior publications from this group reported 1- and 3-year results, and this paper reported the 5-year results, demonstrating the persistent superiority of bariatric surgery over the most rigorous intensive medical therapy in the resolution or improvement of hyperglycemia in patients with BMI ranges of 27 kg/m2 to 43 kg/m2. Of further significance was the fact that there were no major late surgical complications except for one reoperation.
Samer Mattar, MD, FACS
Colon & Rectal Surgery
Jayne D et al. Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: The ROLARR randomized clinical trial. JAMA. 2017;318(16):1569-80.
This trial of 471 rectal cancer patients demonstrated similar conversion rates for robotic (8.1%) and laparoscopic (12.2%) surgery. Of the other secondary end points, including intraoperative complications, postoperative complications, plane of surgery, 30-day mortality, bladder dysfunction, and sexual dysfunction, none showed a statistically significant difference between groups.
Marshall JR et al. Laparoscopic lavage in the management of Hinchey grade III diverticulitis: A systematic review. Ann Surg. 2017;265(4):670-6.While there have been a number of groups using laparoscopic lavage in the setting of acute diverticulitis, including Hinchey grade III disease, several recent studies question this approach. This meta-analysis includes three recent randomized, controlled trials and analysis of 48 studies – demonstrating that rates of reintervention within 30 days to be 28.3% in the lavage group and 8.8% in the resection group. Other outcomes – including ICU admissions, 30- and 90-day mortality, or stoma rates at 12 months – were similar between groups.
Denost Q et al. To drain or not to drain infraperitoneal anastomosis after rectal excision for cancer: The GRECCAR 5 randomized trial. Ann Surg. 2017;365(3):474-80.
While many studies have confirmed infectiveness of drainage after colectomy, there is still some controversy of the role of pelvic drainage after rectal surgery. A multicenter randomized, controlled trial with two parallel arms (drain vs. no drain) was conducted in 469 patients after rectal surgery for cancer. Primary endpoint was postoperative pelvic sepsis within 30 postoperative days, including anastomotic leakage, pelvic abscess, and peritonitis. Rates of pelvic sepsis were similar between drain and no drain: 16.1% vs. 18.0% (P = .58), and there was no difference in surgical morbidity, rate of reoperation, length of hospital stay, and rate of stoma closure between groups. Overall, this trial suggests that the use of a pelvic drain after rectal excision for rectal cancer did not confer any benefit.
Genevieve Melton-Meaux, MD, FACS
Breast Surgery
Giuliano AE et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: The ACOSOG Z0011 randomized clinical trial. JAMA. 2017 Sep 12;318(10):918-926.
Long-term outcomes from the practice-changing ACOSOG Z0011 (Alliance) trial confirming the safety of omitting completion axillary lymph node dissection in women with T1/T2 tumors treated by lumpectomy and whole-breast radiation when metastatic disease is identified in one or two sentinel nodes.
Masuda N et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med. 2017 Jun 1;376(22):2147-59.
Breast cancer patients that achieve a complete pathologic response after receiving neoadjuvant chemotherapy have a survival advantage, and patients found to have residual disease represent a higher-risk population subset. This prospective randomized clinical trial (known as the CREATE-X study) revealed that adjuvant capecitabine can significantly mitigate this risk, especially for patients with triple-negative breast cancer.
Curigliano G et al. De-escalating and escalating treatments for early stage breast cancer: the St. Gallen International Expert Consensus Conference on the Primary Therapy of Early Breast Cancer 2017. Ann Oncol. 2017 Aug 1;28(8):1700-12.
This summary of the 2017 St. Gallen Conference proceedings provides a comprehensive yet concise review of contemporary standards of care in managing early stage breast cancer. Issues reviewed include lumpectomy margins, extent of breast/axillary surgery following neoadjuvant chemotherapy, options for breast radiation schedules following lumpectomy, and application of currently available gene expression profiles.
Troester MA et al. Racial differences in PAM50 subtypes in the Carolina Breast Cancer Study. J Natl Cancer Inst. 2018 Feb 1;110(2);doi: 10.1093/jnci/djx135; epub ahead of print (Aug 2017).
Breast cancer outcome disparities related to racial/ethnic identity are well documented, with African American patients experiencing higher mortality rates, compared with White Americans. This disparity is partly explained by differences in tumor biology, since triple-negative breast cancer (TNBC) is twice as common in African American patients. Troester et al. conducted RNA expression-based PAM-50 tumor subtyping to demonstrate significantly higher rates of biologically aggressive tumor subtypes among African Americans breast cancer patients, compared with white Americans.
Lisa Newman, MD, FACS
Foregut
Teitelbaum EN et al. Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg Endosc. 2017 Jun 29. doi: 10.1007/s00464-017-5699-2 ; epub ahead of print.
This provides the longest follow-up to date regarding clinical efficacy of peroral endoscopic myotomy (POEM) in the United States. Although not a panacea, POEM appears to provide substantial durable clinical improvement in patients suffering from esophageal motility disorders.
Kevin Reavis, MD, FACS
Yufei Chen et al. Primary lymph node gastrinoma: A single institution experience. Surgery 2017 Nov;162(5):1088-94
This article retrospectively review a rare neuroendocrine (gastrinoma) tumor over a 25-year period at a single institution, noting all demographics and outcomes. Great update and refresher. The article then went farther, evaluating an even rarer occurrence of a primary lymph node gastrinoma within this patient population and followed those patients outcomes as well. Two “values” for the “price of one.”
Haisley KR et al. Twenty-year trends in the utilization of Heller myotomy for achalasia in the United States. Am J Surg. 2017 Aug;214(2):299-302.
Gary Timmerman, MD, FACS
Recommended Reading lists are something of a tradition for ACS Surgery News. This feature has appeared several times over the years and it has always proved among the most popular items in the publication. But the project hinges on input from our Editorial Advisory Board, the members of which are already regularly called upon to help vet the publication’s content and give their advice. They have gone the extra mile and have once again chosen their “Best of 2017” studies in their own specialty areas, along with commentary on why their choices should be of interest to all surgeons. We hope our readers will find the list and the comments of interest.
General surgery
Cogbill TH et al. Rural general surgery: A 38-year experience with a regional network established by an integrated health system in the Midwestern United States. J Am Coll Surg. 2017;225(1):115-24.
This article is of particular interest because it provides details of an innovative, regional system of surgical care at the critical access hospitals and referral centers that cooperate seamlessly to improve quality of care and quality of practice for rural surgeons. It could serve as a model for similar independent hospitals and practices in a region to improve the practice lives of the surgeons in rural communities and preserve access to local care for rural patients.
Dimou FM et al. Outcomes in older patients with grade III cholecystitis and cholecystostomy tube placement: A propensity score analysis. J Am Coll Surg. 2017;224(4):502-14.This study is valuable because it sheds light on the current status of treatment of severe acute cholecystitis in the United States and reports outcomes of patients who get initial tube cholecystostomy. It demonstrates potential drawbacks of following the Tokyo Guidelines: fewer patients receiving definitive treatment (cholecystectomy) and higher mortality rates and readmissions.
Karen E. Deveney, MD, FACS
Palliative Care
Gani F et al. Palliative care utilization among patients admitted for gastrointestinal and thoracic cancers. J Palliat Med. 2017 Nov 3; doi: 10.1089/jpm.2017.0295; epub ahead of print.
Is this a matter of “too little too late”? This retrospective cross-sectional analysis of patients identified in the National Inpatient Sample database admitted with a primary diagnosis of gastrointestinal and/or thoracic cancer determined that only 8.5% of patients admitted received palliative care services. Surgical patients were 79% less likely to have received a palliative care consultation, and then only after a prolonged length of stay or postoperative complication. Is referral to palliative care services hindered by its stigmatization with these outcomes?
Taylor LJ et al. A framework to improve surgeon communication in high-stakes surgical decisions: Best Case/Worst Case. JAMA Surgery. 2017;152(6):531-8.
My chief used to say, “You might not be teachable, but you are trainable!” After surgeons received training in the Best Case/Worst Case framework described in this paper, they demonstrated that it was possible to successfully change the focus of decision-making conversations from an isolated surgical problem – with its menu of technical solutions – instead into a discussion about treatment alternatives and outcomes. This intervention is a useful tool for one of the most invasive procedures of all – an exploration of a patient’s preferences and values that is necessary for shared decision making within the acute setting.
Makhani SS et al. Cognitive impairment and overall survival in frail surgical patients. J Amer Coll Surg. 2017 Nov;225(5):590-600.
In my preoperative discussions with families of frail patients, it is often quite evident that the factor driving their decision is the cognitive state of the patient and the consequences of its further decline, even when they are willing to accept the risks of physical frailty. This study in a large multidisciplinary cohort of patients undergoing major operations determined that a combined frailty (Fried frailty score) and cognitive assessment score (Emory Clock Draw Test) has a more powerful potential to predict adult patients at higher risk of overall survival than does either measurement alone. Dual frailty and cognitive screening appears to be a promising adjunct to the shared decision-making process.
Geoffrey P. Dunn, MD, FACS
Wilson DG et al. Patterns of care in hospitalized vascular patients at end of life. JAMA Surg. 2017;152(2):183-90.
This thoughtful study and the excellent accompanying invited commentary by William Schecter, MD, FACS, address a major, difficult issue that faces all physicians as our patients become older and sicker and our ability to keep them alive expands: How do we speak honestly with patients about their prognosis and likely outcomes and honor their autonomy in decision making?
Karen E. Deveney, MD, FACS
Practice Management
Robinson JR et al. Complexity of medical decision making in care provided by surgeons through patient portals. Surg Res. 2017;214:93-101.
This article describes an analysis of the content of patient portal messages exchanged between surgical providers and patients. The study demonstrates that more than 90% of these exchanges involved the delivery of medical care, and more than two-thirds of the messages contained medical decision making, which might have generated charges if done in a face-to-face outpatient encounter. The articles argues that surgeons are providing substantial medical care to their patients through patient portal message exchanges and suggests that models for compensation of this type of online care should be developed.
Gretchen Purcell Jackson, MD, FACS
Vascular Surgery
Bennett KM et al. Carotid artery stenting is associated with a higher incidence of major adverse clinical events than carotid endarterectomy in female patients. J Vasc Surg. 2017 Sep;66(3):794-801.
This article uses the ACS NSQIP database to assess outcomes of women undergoing intervention for carotid stenosis in a real-world setting and finds that major adverse cardiac events in the first 30 days is higher for carotid artery stenting (12.2%), compared with carotid endarterectomy (5.2%). What we need to keep in mind is that the practice of any intervention for asymptomatic carotid stenosis is being reevaluated in the new CREST study, which will compare current best medical management with carotid stenting and carotid endarterectomy. The indications are likely to change for all, but because women had less relative risk reduction in the early studies, we can expect that the benefits for intervention for women will continue to be less than those for men, calling to question when we should truly intervene, and how best to do so.
Gargiulo M et al. Outcomes of endovascular aneurysm repair performed in abdominal aortic aneurysms with large infrarenal necks. J Vasc Surg. 2017 Oct;66(4);1065-72.
This study found that endovascular aneurysm repair, performed in patients with large necks (greater than 28 mm), was associated with further neck enlargement at 2 years, and a higher risk of proximal type I endoleak, with the need for reintervention. This is one of many recent studies, all with similar findings. The issue becomes how we can best address larger infrarenal necks, whether by use of fenestrated grafts, snorkels/chimneys with extension of the seal zone, aptus, or other technologies. The question of whether all grafts have equal impacts on these more dilated necks has still to be elucidated. Nonetheless, when we stretch the instructions for use, there is an increased likelihood for more interventions.
Zettervall SL et al. Renal complications after EVAR with suprarenal versus infrarenal fixation among all users and routine users. J Vasc Surg. 2017 Oct;66(4):1305.
This study found that endografts with suprarenal fixation were associated with a greater decline in renal function, compared with those with infrarenal fixation, as well as with a longer length of stay. The reasons for the renal function decline are not entirely clear, and there was a slight increase in contrast use for those with suprarenal fixation but were otherwise similar when comparing comorbidities. Clearly, assessment of any impact on long-term renal function is important, and may affect future choice of endografts.
Linda Harris, MD, FACS
Bariatric Surgery
Rosenthal RJ et al. Obesity in America. Surg Obes Relat Dis. 2017 Oct;13(10):1643-50.
Although much has been reported on the dramatic benefits of bariatric surgery, it remains a matter of deep disappointment that only 1%-2% of the eligible population is receiving this life-saving therapy. This is a paper that reports and analyzes the results of a national survey that was conducted on behalf of the American Society for Metabolic & Bariatric Surgery, in an attempt to identify barriers to access, public misconceptions on obesity and its consequences, and other pertinent factors. Survey results included the findings that, although 80% of Americans considered obesity as the most serious health risk problem, there was a clear overestimation of the effectiveness of diet and exercise alone. The importance of this paper lies in the persistent lack of recognition and/or awareness of proven, safe, and durable medical and surgical options in the lay population, highlighting the importance of aligning efforts and resources toward educating both the public and referring physicians.
Adams TD et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017 Sep 21;377(12):1143-55
This paper reports the results of an observational, prospective study that followed patients who received gastric bypass, in comparison with a group of patients who desired but did not receive gastric bypass, and a third group of obese patients who did not seek surgery. The authors concluded that gastric bypass provided durable, 12-year remission and prevention of such lethal diseases as diabetes, hypertension, and dyslipidemia. The importance of this study is in its detailed follow-up, the exceedingly high retention rate of 90% at 12 years, and the comparisons made between surgical and nonsurgical groups, demonstrating not only the benefits of gastric bypass, but as importantly, the hazards of not receiving this treatment.
Schauer PR et al. Bariatric surgery versus intensive medical therapy for diabetes – 5-year outcomes. N Engl J Med. 2017 Feb 16;376(7):641-51.This paper is the latest installment of the long-term results from the STAMPEDE trial conducted at the Cleveland Clinic. STAMPEDE is a randomized, controlled trial that compared the best, most “intensive” medical therapy for type 2 diabetes vs. bariatric surgery (comprising a mix of gastric bypass and sleeve gastrectomy). Prior publications from this group reported 1- and 3-year results, and this paper reported the 5-year results, demonstrating the persistent superiority of bariatric surgery over the most rigorous intensive medical therapy in the resolution or improvement of hyperglycemia in patients with BMI ranges of 27 kg/m2 to 43 kg/m2. Of further significance was the fact that there were no major late surgical complications except for one reoperation.
Samer Mattar, MD, FACS
Colon & Rectal Surgery
Jayne D et al. Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: The ROLARR randomized clinical trial. JAMA. 2017;318(16):1569-80.
This trial of 471 rectal cancer patients demonstrated similar conversion rates for robotic (8.1%) and laparoscopic (12.2%) surgery. Of the other secondary end points, including intraoperative complications, postoperative complications, plane of surgery, 30-day mortality, bladder dysfunction, and sexual dysfunction, none showed a statistically significant difference between groups.
Marshall JR et al. Laparoscopic lavage in the management of Hinchey grade III diverticulitis: A systematic review. Ann Surg. 2017;265(4):670-6.While there have been a number of groups using laparoscopic lavage in the setting of acute diverticulitis, including Hinchey grade III disease, several recent studies question this approach. This meta-analysis includes three recent randomized, controlled trials and analysis of 48 studies – demonstrating that rates of reintervention within 30 days to be 28.3% in the lavage group and 8.8% in the resection group. Other outcomes – including ICU admissions, 30- and 90-day mortality, or stoma rates at 12 months – were similar between groups.
Denost Q et al. To drain or not to drain infraperitoneal anastomosis after rectal excision for cancer: The GRECCAR 5 randomized trial. Ann Surg. 2017;365(3):474-80.
While many studies have confirmed infectiveness of drainage after colectomy, there is still some controversy of the role of pelvic drainage after rectal surgery. A multicenter randomized, controlled trial with two parallel arms (drain vs. no drain) was conducted in 469 patients after rectal surgery for cancer. Primary endpoint was postoperative pelvic sepsis within 30 postoperative days, including anastomotic leakage, pelvic abscess, and peritonitis. Rates of pelvic sepsis were similar between drain and no drain: 16.1% vs. 18.0% (P = .58), and there was no difference in surgical morbidity, rate of reoperation, length of hospital stay, and rate of stoma closure between groups. Overall, this trial suggests that the use of a pelvic drain after rectal excision for rectal cancer did not confer any benefit.
Genevieve Melton-Meaux, MD, FACS
Breast Surgery
Giuliano AE et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: The ACOSOG Z0011 randomized clinical trial. JAMA. 2017 Sep 12;318(10):918-926.
Long-term outcomes from the practice-changing ACOSOG Z0011 (Alliance) trial confirming the safety of omitting completion axillary lymph node dissection in women with T1/T2 tumors treated by lumpectomy and whole-breast radiation when metastatic disease is identified in one or two sentinel nodes.
Masuda N et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med. 2017 Jun 1;376(22):2147-59.
Breast cancer patients that achieve a complete pathologic response after receiving neoadjuvant chemotherapy have a survival advantage, and patients found to have residual disease represent a higher-risk population subset. This prospective randomized clinical trial (known as the CREATE-X study) revealed that adjuvant capecitabine can significantly mitigate this risk, especially for patients with triple-negative breast cancer.
Curigliano G et al. De-escalating and escalating treatments for early stage breast cancer: the St. Gallen International Expert Consensus Conference on the Primary Therapy of Early Breast Cancer 2017. Ann Oncol. 2017 Aug 1;28(8):1700-12.
This summary of the 2017 St. Gallen Conference proceedings provides a comprehensive yet concise review of contemporary standards of care in managing early stage breast cancer. Issues reviewed include lumpectomy margins, extent of breast/axillary surgery following neoadjuvant chemotherapy, options for breast radiation schedules following lumpectomy, and application of currently available gene expression profiles.
Troester MA et al. Racial differences in PAM50 subtypes in the Carolina Breast Cancer Study. J Natl Cancer Inst. 2018 Feb 1;110(2);doi: 10.1093/jnci/djx135; epub ahead of print (Aug 2017).
Breast cancer outcome disparities related to racial/ethnic identity are well documented, with African American patients experiencing higher mortality rates, compared with White Americans. This disparity is partly explained by differences in tumor biology, since triple-negative breast cancer (TNBC) is twice as common in African American patients. Troester et al. conducted RNA expression-based PAM-50 tumor subtyping to demonstrate significantly higher rates of biologically aggressive tumor subtypes among African Americans breast cancer patients, compared with white Americans.
Lisa Newman, MD, FACS
Foregut
Teitelbaum EN et al. Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg Endosc. 2017 Jun 29. doi: 10.1007/s00464-017-5699-2 ; epub ahead of print.
This provides the longest follow-up to date regarding clinical efficacy of peroral endoscopic myotomy (POEM) in the United States. Although not a panacea, POEM appears to provide substantial durable clinical improvement in patients suffering from esophageal motility disorders.
Kevin Reavis, MD, FACS
Yufei Chen et al. Primary lymph node gastrinoma: A single institution experience. Surgery 2017 Nov;162(5):1088-94
This article retrospectively review a rare neuroendocrine (gastrinoma) tumor over a 25-year period at a single institution, noting all demographics and outcomes. Great update and refresher. The article then went farther, evaluating an even rarer occurrence of a primary lymph node gastrinoma within this patient population and followed those patients outcomes as well. Two “values” for the “price of one.”
Haisley KR et al. Twenty-year trends in the utilization of Heller myotomy for achalasia in the United States. Am J Surg. 2017 Aug;214(2):299-302.
Gary Timmerman, MD, FACS
Recommended Reading lists are something of a tradition for ACS Surgery News. This feature has appeared several times over the years and it has always proved among the most popular items in the publication. But the project hinges on input from our Editorial Advisory Board, the members of which are already regularly called upon to help vet the publication’s content and give their advice. They have gone the extra mile and have once again chosen their “Best of 2017” studies in their own specialty areas, along with commentary on why their choices should be of interest to all surgeons. We hope our readers will find the list and the comments of interest.
General surgery
Cogbill TH et al. Rural general surgery: A 38-year experience with a regional network established by an integrated health system in the Midwestern United States. J Am Coll Surg. 2017;225(1):115-24.
This article is of particular interest because it provides details of an innovative, regional system of surgical care at the critical access hospitals and referral centers that cooperate seamlessly to improve quality of care and quality of practice for rural surgeons. It could serve as a model for similar independent hospitals and practices in a region to improve the practice lives of the surgeons in rural communities and preserve access to local care for rural patients.
Dimou FM et al. Outcomes in older patients with grade III cholecystitis and cholecystostomy tube placement: A propensity score analysis. J Am Coll Surg. 2017;224(4):502-14.This study is valuable because it sheds light on the current status of treatment of severe acute cholecystitis in the United States and reports outcomes of patients who get initial tube cholecystostomy. It demonstrates potential drawbacks of following the Tokyo Guidelines: fewer patients receiving definitive treatment (cholecystectomy) and higher mortality rates and readmissions.
Karen E. Deveney, MD, FACS
Palliative Care
Gani F et al. Palliative care utilization among patients admitted for gastrointestinal and thoracic cancers. J Palliat Med. 2017 Nov 3; doi: 10.1089/jpm.2017.0295; epub ahead of print.
Is this a matter of “too little too late”? This retrospective cross-sectional analysis of patients identified in the National Inpatient Sample database admitted with a primary diagnosis of gastrointestinal and/or thoracic cancer determined that only 8.5% of patients admitted received palliative care services. Surgical patients were 79% less likely to have received a palliative care consultation, and then only after a prolonged length of stay or postoperative complication. Is referral to palliative care services hindered by its stigmatization with these outcomes?
Taylor LJ et al. A framework to improve surgeon communication in high-stakes surgical decisions: Best Case/Worst Case. JAMA Surgery. 2017;152(6):531-8.
My chief used to say, “You might not be teachable, but you are trainable!” After surgeons received training in the Best Case/Worst Case framework described in this paper, they demonstrated that it was possible to successfully change the focus of decision-making conversations from an isolated surgical problem – with its menu of technical solutions – instead into a discussion about treatment alternatives and outcomes. This intervention is a useful tool for one of the most invasive procedures of all – an exploration of a patient’s preferences and values that is necessary for shared decision making within the acute setting.
Makhani SS et al. Cognitive impairment and overall survival in frail surgical patients. J Amer Coll Surg. 2017 Nov;225(5):590-600.
In my preoperative discussions with families of frail patients, it is often quite evident that the factor driving their decision is the cognitive state of the patient and the consequences of its further decline, even when they are willing to accept the risks of physical frailty. This study in a large multidisciplinary cohort of patients undergoing major operations determined that a combined frailty (Fried frailty score) and cognitive assessment score (Emory Clock Draw Test) has a more powerful potential to predict adult patients at higher risk of overall survival than does either measurement alone. Dual frailty and cognitive screening appears to be a promising adjunct to the shared decision-making process.
Geoffrey P. Dunn, MD, FACS
Wilson DG et al. Patterns of care in hospitalized vascular patients at end of life. JAMA Surg. 2017;152(2):183-90.
This thoughtful study and the excellent accompanying invited commentary by William Schecter, MD, FACS, address a major, difficult issue that faces all physicians as our patients become older and sicker and our ability to keep them alive expands: How do we speak honestly with patients about their prognosis and likely outcomes and honor their autonomy in decision making?
Karen E. Deveney, MD, FACS
Practice Management
Robinson JR et al. Complexity of medical decision making in care provided by surgeons through patient portals. Surg Res. 2017;214:93-101.
This article describes an analysis of the content of patient portal messages exchanged between surgical providers and patients. The study demonstrates that more than 90% of these exchanges involved the delivery of medical care, and more than two-thirds of the messages contained medical decision making, which might have generated charges if done in a face-to-face outpatient encounter. The articles argues that surgeons are providing substantial medical care to their patients through patient portal message exchanges and suggests that models for compensation of this type of online care should be developed.
Gretchen Purcell Jackson, MD, FACS
Vascular Surgery
Bennett KM et al. Carotid artery stenting is associated with a higher incidence of major adverse clinical events than carotid endarterectomy in female patients. J Vasc Surg. 2017 Sep;66(3):794-801.
This article uses the ACS NSQIP database to assess outcomes of women undergoing intervention for carotid stenosis in a real-world setting and finds that major adverse cardiac events in the first 30 days is higher for carotid artery stenting (12.2%), compared with carotid endarterectomy (5.2%). What we need to keep in mind is that the practice of any intervention for asymptomatic carotid stenosis is being reevaluated in the new CREST study, which will compare current best medical management with carotid stenting and carotid endarterectomy. The indications are likely to change for all, but because women had less relative risk reduction in the early studies, we can expect that the benefits for intervention for women will continue to be less than those for men, calling to question when we should truly intervene, and how best to do so.
Gargiulo M et al. Outcomes of endovascular aneurysm repair performed in abdominal aortic aneurysms with large infrarenal necks. J Vasc Surg. 2017 Oct;66(4);1065-72.
This study found that endovascular aneurysm repair, performed in patients with large necks (greater than 28 mm), was associated with further neck enlargement at 2 years, and a higher risk of proximal type I endoleak, with the need for reintervention. This is one of many recent studies, all with similar findings. The issue becomes how we can best address larger infrarenal necks, whether by use of fenestrated grafts, snorkels/chimneys with extension of the seal zone, aptus, or other technologies. The question of whether all grafts have equal impacts on these more dilated necks has still to be elucidated. Nonetheless, when we stretch the instructions for use, there is an increased likelihood for more interventions.
Zettervall SL et al. Renal complications after EVAR with suprarenal versus infrarenal fixation among all users and routine users. J Vasc Surg. 2017 Oct;66(4):1305.
This study found that endografts with suprarenal fixation were associated with a greater decline in renal function, compared with those with infrarenal fixation, as well as with a longer length of stay. The reasons for the renal function decline are not entirely clear, and there was a slight increase in contrast use for those with suprarenal fixation but were otherwise similar when comparing comorbidities. Clearly, assessment of any impact on long-term renal function is important, and may affect future choice of endografts.
Linda Harris, MD, FACS
Bariatric Surgery
Rosenthal RJ et al. Obesity in America. Surg Obes Relat Dis. 2017 Oct;13(10):1643-50.
Although much has been reported on the dramatic benefits of bariatric surgery, it remains a matter of deep disappointment that only 1%-2% of the eligible population is receiving this life-saving therapy. This is a paper that reports and analyzes the results of a national survey that was conducted on behalf of the American Society for Metabolic & Bariatric Surgery, in an attempt to identify barriers to access, public misconceptions on obesity and its consequences, and other pertinent factors. Survey results included the findings that, although 80% of Americans considered obesity as the most serious health risk problem, there was a clear overestimation of the effectiveness of diet and exercise alone. The importance of this paper lies in the persistent lack of recognition and/or awareness of proven, safe, and durable medical and surgical options in the lay population, highlighting the importance of aligning efforts and resources toward educating both the public and referring physicians.
Adams TD et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017 Sep 21;377(12):1143-55
This paper reports the results of an observational, prospective study that followed patients who received gastric bypass, in comparison with a group of patients who desired but did not receive gastric bypass, and a third group of obese patients who did not seek surgery. The authors concluded that gastric bypass provided durable, 12-year remission and prevention of such lethal diseases as diabetes, hypertension, and dyslipidemia. The importance of this study is in its detailed follow-up, the exceedingly high retention rate of 90% at 12 years, and the comparisons made between surgical and nonsurgical groups, demonstrating not only the benefits of gastric bypass, but as importantly, the hazards of not receiving this treatment.
Schauer PR et al. Bariatric surgery versus intensive medical therapy for diabetes – 5-year outcomes. N Engl J Med. 2017 Feb 16;376(7):641-51.This paper is the latest installment of the long-term results from the STAMPEDE trial conducted at the Cleveland Clinic. STAMPEDE is a randomized, controlled trial that compared the best, most “intensive” medical therapy for type 2 diabetes vs. bariatric surgery (comprising a mix of gastric bypass and sleeve gastrectomy). Prior publications from this group reported 1- and 3-year results, and this paper reported the 5-year results, demonstrating the persistent superiority of bariatric surgery over the most rigorous intensive medical therapy in the resolution or improvement of hyperglycemia in patients with BMI ranges of 27 kg/m2 to 43 kg/m2. Of further significance was the fact that there were no major late surgical complications except for one reoperation.
Samer Mattar, MD, FACS
Colon & Rectal Surgery
Jayne D et al. Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: The ROLARR randomized clinical trial. JAMA. 2017;318(16):1569-80.
This trial of 471 rectal cancer patients demonstrated similar conversion rates for robotic (8.1%) and laparoscopic (12.2%) surgery. Of the other secondary end points, including intraoperative complications, postoperative complications, plane of surgery, 30-day mortality, bladder dysfunction, and sexual dysfunction, none showed a statistically significant difference between groups.
Marshall JR et al. Laparoscopic lavage in the management of Hinchey grade III diverticulitis: A systematic review. Ann Surg. 2017;265(4):670-6.While there have been a number of groups using laparoscopic lavage in the setting of acute diverticulitis, including Hinchey grade III disease, several recent studies question this approach. This meta-analysis includes three recent randomized, controlled trials and analysis of 48 studies – demonstrating that rates of reintervention within 30 days to be 28.3% in the lavage group and 8.8% in the resection group. Other outcomes – including ICU admissions, 30- and 90-day mortality, or stoma rates at 12 months – were similar between groups.
Denost Q et al. To drain or not to drain infraperitoneal anastomosis after rectal excision for cancer: The GRECCAR 5 randomized trial. Ann Surg. 2017;365(3):474-80.
While many studies have confirmed infectiveness of drainage after colectomy, there is still some controversy of the role of pelvic drainage after rectal surgery. A multicenter randomized, controlled trial with two parallel arms (drain vs. no drain) was conducted in 469 patients after rectal surgery for cancer. Primary endpoint was postoperative pelvic sepsis within 30 postoperative days, including anastomotic leakage, pelvic abscess, and peritonitis. Rates of pelvic sepsis were similar between drain and no drain: 16.1% vs. 18.0% (P = .58), and there was no difference in surgical morbidity, rate of reoperation, length of hospital stay, and rate of stoma closure between groups. Overall, this trial suggests that the use of a pelvic drain after rectal excision for rectal cancer did not confer any benefit.
Genevieve Melton-Meaux, MD, FACS
Breast Surgery
Giuliano AE et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: The ACOSOG Z0011 randomized clinical trial. JAMA. 2017 Sep 12;318(10):918-926.
Long-term outcomes from the practice-changing ACOSOG Z0011 (Alliance) trial confirming the safety of omitting completion axillary lymph node dissection in women with T1/T2 tumors treated by lumpectomy and whole-breast radiation when metastatic disease is identified in one or two sentinel nodes.
Masuda N et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med. 2017 Jun 1;376(22):2147-59.
Breast cancer patients that achieve a complete pathologic response after receiving neoadjuvant chemotherapy have a survival advantage, and patients found to have residual disease represent a higher-risk population subset. This prospective randomized clinical trial (known as the CREATE-X study) revealed that adjuvant capecitabine can significantly mitigate this risk, especially for patients with triple-negative breast cancer.
Curigliano G et al. De-escalating and escalating treatments for early stage breast cancer: the St. Gallen International Expert Consensus Conference on the Primary Therapy of Early Breast Cancer 2017. Ann Oncol. 2017 Aug 1;28(8):1700-12.
This summary of the 2017 St. Gallen Conference proceedings provides a comprehensive yet concise review of contemporary standards of care in managing early stage breast cancer. Issues reviewed include lumpectomy margins, extent of breast/axillary surgery following neoadjuvant chemotherapy, options for breast radiation schedules following lumpectomy, and application of currently available gene expression profiles.
Troester MA et al. Racial differences in PAM50 subtypes in the Carolina Breast Cancer Study. J Natl Cancer Inst. 2018 Feb 1;110(2);doi: 10.1093/jnci/djx135; epub ahead of print (Aug 2017).
Breast cancer outcome disparities related to racial/ethnic identity are well documented, with African American patients experiencing higher mortality rates, compared with White Americans. This disparity is partly explained by differences in tumor biology, since triple-negative breast cancer (TNBC) is twice as common in African American patients. Troester et al. conducted RNA expression-based PAM-50 tumor subtyping to demonstrate significantly higher rates of biologically aggressive tumor subtypes among African Americans breast cancer patients, compared with white Americans.
Lisa Newman, MD, FACS
Foregut
Teitelbaum EN et al. Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg Endosc. 2017 Jun 29. doi: 10.1007/s00464-017-5699-2 ; epub ahead of print.
This provides the longest follow-up to date regarding clinical efficacy of peroral endoscopic myotomy (POEM) in the United States. Although not a panacea, POEM appears to provide substantial durable clinical improvement in patients suffering from esophageal motility disorders.
Kevin Reavis, MD, FACS
Yufei Chen et al. Primary lymph node gastrinoma: A single institution experience. Surgery 2017 Nov;162(5):1088-94
This article retrospectively review a rare neuroendocrine (gastrinoma) tumor over a 25-year period at a single institution, noting all demographics and outcomes. Great update and refresher. The article then went farther, evaluating an even rarer occurrence of a primary lymph node gastrinoma within this patient population and followed those patients outcomes as well. Two “values” for the “price of one.”
Haisley KR et al. Twenty-year trends in the utilization of Heller myotomy for achalasia in the United States. Am J Surg. 2017 Aug;214(2):299-302.
Gary Timmerman, MD, FACS
Clinical trial: The Role of the Robotic Platform in Inguinal Hernia Repair Surgery
The Role of the Robotic Platform in Inguinal Hernia Repair Surgery is an interventional trial currently recruiting patients who require inguinal hernia repair surgery.
The trial will compare postoperative pain in patients undergoing laparoscopic inguinal hernia surgery repair or robotic inguinal hernia repair surgery. The laparoscopic approach has been used frequently and has several advantages. However, it has several disadvantages that the robotic approach may address. As such, the study investigators have hypothesized that the robotic approach will result in less postoperative pain than the laparoscopic approach.
The primary outcome measure is the difference in postoperative pain between patients who undergo robotic inguinal hernia repair and those who undergo laparoscopic inguinal hernia repair during the 2 years following surgery. Secondary outcome measures include differences in surgeon ergonomics between the two approaches, institution cost analysis, and long-term recurrence rate differences, all within 2 years of surgery.
The study will end in May 2019. About 100 people are expected to be included in the final analysis.
Find more information on the study page at Clinicaltrials.gov.
SOURCE: Clinicaltrials.gov. NCT02816658.
The Role of the Robotic Platform in Inguinal Hernia Repair Surgery is an interventional trial currently recruiting patients who require inguinal hernia repair surgery.
The trial will compare postoperative pain in patients undergoing laparoscopic inguinal hernia surgery repair or robotic inguinal hernia repair surgery. The laparoscopic approach has been used frequently and has several advantages. However, it has several disadvantages that the robotic approach may address. As such, the study investigators have hypothesized that the robotic approach will result in less postoperative pain than the laparoscopic approach.
The primary outcome measure is the difference in postoperative pain between patients who undergo robotic inguinal hernia repair and those who undergo laparoscopic inguinal hernia repair during the 2 years following surgery. Secondary outcome measures include differences in surgeon ergonomics between the two approaches, institution cost analysis, and long-term recurrence rate differences, all within 2 years of surgery.
The study will end in May 2019. About 100 people are expected to be included in the final analysis.
Find more information on the study page at Clinicaltrials.gov.
SOURCE: Clinicaltrials.gov. NCT02816658.
The Role of the Robotic Platform in Inguinal Hernia Repair Surgery is an interventional trial currently recruiting patients who require inguinal hernia repair surgery.
The trial will compare postoperative pain in patients undergoing laparoscopic inguinal hernia surgery repair or robotic inguinal hernia repair surgery. The laparoscopic approach has been used frequently and has several advantages. However, it has several disadvantages that the robotic approach may address. As such, the study investigators have hypothesized that the robotic approach will result in less postoperative pain than the laparoscopic approach.
The primary outcome measure is the difference in postoperative pain between patients who undergo robotic inguinal hernia repair and those who undergo laparoscopic inguinal hernia repair during the 2 years following surgery. Secondary outcome measures include differences in surgeon ergonomics between the two approaches, institution cost analysis, and long-term recurrence rate differences, all within 2 years of surgery.
The study will end in May 2019. About 100 people are expected to be included in the final analysis.
Find more information on the study page at Clinicaltrials.gov.
SOURCE: Clinicaltrials.gov. NCT02816658.
FROM CLINICALTRIALS.GOV
Cancer Care Facilities Receive CoC Outstanding Achievement Award
The Commission on Cancer (CoC) of the American College of Surgeons (ACS) has granted its mid-year 2017 Outstanding Achievement Award to a select group of 16 accredited cancer programs throughout the U.S. Award criteria are based on qualitative and quantitative surveys conducted in the first half of 2017. Visit the ACS website for a list of these award-winning cancer programs at facs.org/quality-programs/cancer/coc/info/outstanding/2017-part-1.
The purpose of the award is to raise the bar on quality cancer care, with the ultimate goal of increasing awareness about quality care choices among cancer patients and their loved ones. In addition, the award is intended to fulfill the following goals:
• Recognize those cancer programs that achieve excellence in providing quality care to cancer patients
• Motivate other cancer programs to work toward improving their level of care
• Facilitate dialogue between award recipients and health care professionals at other cancer facilities for the purpose of sharing best practices
• Encourage honorees to serve as quality care resources to other cancer programs
“More and more, we’re finding that patients and their families want to know how the health care institutions in their communities compare with one another,” said Lawrence N. Shulman, MD, FACP, Chair of the CoC. “They want access to information in terms of who’s providing the best quality of care, and they want to know about overall patient outcomes. Through this recognition program, I’d like to think we’re playing a small, but vital, role in helping them make informed decisions on their cancer care. ”The 16 award-winning cancer care programs represent approximately six percent of programs surveyed by the CoC January 1–June 30, 2017. “These cancer programs currently represent the best of the best when it comes to cancer care,” Dr. Shulman added.
The Commission on Cancer (CoC) of the American College of Surgeons (ACS) has granted its mid-year 2017 Outstanding Achievement Award to a select group of 16 accredited cancer programs throughout the U.S. Award criteria are based on qualitative and quantitative surveys conducted in the first half of 2017. Visit the ACS website for a list of these award-winning cancer programs at facs.org/quality-programs/cancer/coc/info/outstanding/2017-part-1.
The purpose of the award is to raise the bar on quality cancer care, with the ultimate goal of increasing awareness about quality care choices among cancer patients and their loved ones. In addition, the award is intended to fulfill the following goals:
• Recognize those cancer programs that achieve excellence in providing quality care to cancer patients
• Motivate other cancer programs to work toward improving their level of care
• Facilitate dialogue between award recipients and health care professionals at other cancer facilities for the purpose of sharing best practices
• Encourage honorees to serve as quality care resources to other cancer programs
“More and more, we’re finding that patients and their families want to know how the health care institutions in their communities compare with one another,” said Lawrence N. Shulman, MD, FACP, Chair of the CoC. “They want access to information in terms of who’s providing the best quality of care, and they want to know about overall patient outcomes. Through this recognition program, I’d like to think we’re playing a small, but vital, role in helping them make informed decisions on their cancer care. ”The 16 award-winning cancer care programs represent approximately six percent of programs surveyed by the CoC January 1–June 30, 2017. “These cancer programs currently represent the best of the best when it comes to cancer care,” Dr. Shulman added.
The Commission on Cancer (CoC) of the American College of Surgeons (ACS) has granted its mid-year 2017 Outstanding Achievement Award to a select group of 16 accredited cancer programs throughout the U.S. Award criteria are based on qualitative and quantitative surveys conducted in the first half of 2017. Visit the ACS website for a list of these award-winning cancer programs at facs.org/quality-programs/cancer/coc/info/outstanding/2017-part-1.
The purpose of the award is to raise the bar on quality cancer care, with the ultimate goal of increasing awareness about quality care choices among cancer patients and their loved ones. In addition, the award is intended to fulfill the following goals:
• Recognize those cancer programs that achieve excellence in providing quality care to cancer patients
• Motivate other cancer programs to work toward improving their level of care
• Facilitate dialogue between award recipients and health care professionals at other cancer facilities for the purpose of sharing best practices
• Encourage honorees to serve as quality care resources to other cancer programs
“More and more, we’re finding that patients and their families want to know how the health care institutions in their communities compare with one another,” said Lawrence N. Shulman, MD, FACP, Chair of the CoC. “They want access to information in terms of who’s providing the best quality of care, and they want to know about overall patient outcomes. Through this recognition program, I’d like to think we’re playing a small, but vital, role in helping them make informed decisions on their cancer care. ”The 16 award-winning cancer care programs represent approximately six percent of programs surveyed by the CoC January 1–June 30, 2017. “These cancer programs currently represent the best of the best when it comes to cancer care,” Dr. Shulman added.