User login
Official Newspaper of the American College of Surgeons
AMA Citizenship and Service award winner named
The American Medical Association (AMA) awarded Kenneth L. Mattox, MD, FACS, the 2013 Benjamin Rush Award for Citizenship and Community Service on November 16, during the opening session of the 2013 Interim Meeting of the AMA House of Delegates in National Harbor, MD. Dr. Mattox, the American College of Surgeons Second Vice-President-Elect, is Distinguished Service Professor, Michael E. DeBakey Department of Surgery, Baylor College of Medicine; and chief of staff and chief of surgery, Ben Taub General Hospital, Houston, TX. The Benjamin Rush Award annually recognizes a physician who has exceeded professional responsibilities and contributed significantly to public service.
Dr. Mattox provided exemplary service in the medical response to several natural disasters, including the 2001 tropical storm Allison and Hurricanes Katrina and Rita in 2005. As part of the Katrina Joint Unified Command, Dr. Mattox helped form an "evacuation city" to house, treat, clothe, and feed more than 27,000 evacuees from New Orleans, LA, in only 18 hours.
Dr. Mattox is a past-president of the American Association for the Surgery of Trauma, past-president of the Harris County Medical Society in Texas, and was the Texas representative to the AMA House of Delegates from 2004 to 2006. He developed the internationally known Ben Taub Hospital Emergency Center and its Trauma Center and currently serves as board chair of the John P. McGovern Museum of Health & Medical Science, Houston. View an AMA press release announcing the award at http://www.ama-assn.org/ama/pub/news/news/2013/2013-11-18-houston-surgeon-receives-award-for-citizenship.page.
The American Medical Association (AMA) awarded Kenneth L. Mattox, MD, FACS, the 2013 Benjamin Rush Award for Citizenship and Community Service on November 16, during the opening session of the 2013 Interim Meeting of the AMA House of Delegates in National Harbor, MD. Dr. Mattox, the American College of Surgeons Second Vice-President-Elect, is Distinguished Service Professor, Michael E. DeBakey Department of Surgery, Baylor College of Medicine; and chief of staff and chief of surgery, Ben Taub General Hospital, Houston, TX. The Benjamin Rush Award annually recognizes a physician who has exceeded professional responsibilities and contributed significantly to public service.
Dr. Mattox provided exemplary service in the medical response to several natural disasters, including the 2001 tropical storm Allison and Hurricanes Katrina and Rita in 2005. As part of the Katrina Joint Unified Command, Dr. Mattox helped form an "evacuation city" to house, treat, clothe, and feed more than 27,000 evacuees from New Orleans, LA, in only 18 hours.
Dr. Mattox is a past-president of the American Association for the Surgery of Trauma, past-president of the Harris County Medical Society in Texas, and was the Texas representative to the AMA House of Delegates from 2004 to 2006. He developed the internationally known Ben Taub Hospital Emergency Center and its Trauma Center and currently serves as board chair of the John P. McGovern Museum of Health & Medical Science, Houston. View an AMA press release announcing the award at http://www.ama-assn.org/ama/pub/news/news/2013/2013-11-18-houston-surgeon-receives-award-for-citizenship.page.
The American Medical Association (AMA) awarded Kenneth L. Mattox, MD, FACS, the 2013 Benjamin Rush Award for Citizenship and Community Service on November 16, during the opening session of the 2013 Interim Meeting of the AMA House of Delegates in National Harbor, MD. Dr. Mattox, the American College of Surgeons Second Vice-President-Elect, is Distinguished Service Professor, Michael E. DeBakey Department of Surgery, Baylor College of Medicine; and chief of staff and chief of surgery, Ben Taub General Hospital, Houston, TX. The Benjamin Rush Award annually recognizes a physician who has exceeded professional responsibilities and contributed significantly to public service.
Dr. Mattox provided exemplary service in the medical response to several natural disasters, including the 2001 tropical storm Allison and Hurricanes Katrina and Rita in 2005. As part of the Katrina Joint Unified Command, Dr. Mattox helped form an "evacuation city" to house, treat, clothe, and feed more than 27,000 evacuees from New Orleans, LA, in only 18 hours.
Dr. Mattox is a past-president of the American Association for the Surgery of Trauma, past-president of the Harris County Medical Society in Texas, and was the Texas representative to the AMA House of Delegates from 2004 to 2006. He developed the internationally known Ben Taub Hospital Emergency Center and its Trauma Center and currently serves as board chair of the John P. McGovern Museum of Health & Medical Science, Houston. View an AMA press release announcing the award at http://www.ama-assn.org/ama/pub/news/news/2013/2013-11-18-houston-surgeon-receives-award-for-citizenship.page.
Members in the News
Joseph B. Cofer, MD, FACS, a general surgeon and program director, department of surgery, and professor of surgery, University of Tennessee College of Medicine, Chattanooga, president of the American College of Surgeons (ACS) Tennessee Chapter, and current chair of the American Board of Surgery, was named a 2014 recipient of the Accreditation Council for Graduate Medical Education’s J. Palmer Courage to Teach Award.
The award honors program directors who find innovative ways to teach residents and remain committed to providing quality patient care.
Stephen R. T. Evans, MD, FACS, has been elected 2014-2015 vice-chair of the American Board of Surgery (ABS) and will serve as chair in 2015-2016. Dr. Evans is executive vice-president for medical affairs and chief medical officer at MedStar Health in Washington, DC. He also is a professor of surgery at Georgetown University. He is a former President of the American College of Surgeons Metropolitan Washington, DC, Chapter and, in 2009, was elected as an ABS director representing the American Medical Association.
David Rothenberger, MD, FACS, on October 1, 2013, became head of the department of surgery at the University of Minnesota (UMN), Minneapolis. He previously held the John P. Delaney Chair of Clinical Surgical Oncology and was deputy chairman of the department of surgery (2006-2013) at UM
Dr. Rothenberger, an internationally known surgical leader, is past-president of the American Society of Colon and Rectal Surgeons, the American Board of Colon and Rectal Surgery, and the Research Foundation of the American Society of Colon and Rectal Surgeons. Dr. Rothenberger is founder and co-director of the UMN Medical School Emerging Physician Leaders Program, which fosters collaboration and develops skills among faculty from all departments.
Arthur J. Vayer, Jr., MD, FACS, recently was installed as vice-speaker of the Medical Society of Virginia (MSV) during the organization’s annual meeting at The Homestead Resort in Hot Springs, VA. Dr. Vayer, a MSV member since 2006 and a general surgeon at Stafford Surgical, Sentara Medical Group, also worked at Robert Cohen, MD, PC, Riverside Gloucester Surgery Associates and in private practice. Dr. Vayer serves as an MSV delegate and associate director, an officer with the Prince William County Medical Society, a committee member at Potomac Hospital, Woodridge, and chairs the performance evaluation committee of Sentara Northern Virginia Medical Center.
Joseph B. Cofer, MD, FACS, a general surgeon and program director, department of surgery, and professor of surgery, University of Tennessee College of Medicine, Chattanooga, president of the American College of Surgeons (ACS) Tennessee Chapter, and current chair of the American Board of Surgery, was named a 2014 recipient of the Accreditation Council for Graduate Medical Education’s J. Palmer Courage to Teach Award.
The award honors program directors who find innovative ways to teach residents and remain committed to providing quality patient care.
Stephen R. T. Evans, MD, FACS, has been elected 2014-2015 vice-chair of the American Board of Surgery (ABS) and will serve as chair in 2015-2016. Dr. Evans is executive vice-president for medical affairs and chief medical officer at MedStar Health in Washington, DC. He also is a professor of surgery at Georgetown University. He is a former President of the American College of Surgeons Metropolitan Washington, DC, Chapter and, in 2009, was elected as an ABS director representing the American Medical Association.
David Rothenberger, MD, FACS, on October 1, 2013, became head of the department of surgery at the University of Minnesota (UMN), Minneapolis. He previously held the John P. Delaney Chair of Clinical Surgical Oncology and was deputy chairman of the department of surgery (2006-2013) at UM
Dr. Rothenberger, an internationally known surgical leader, is past-president of the American Society of Colon and Rectal Surgeons, the American Board of Colon and Rectal Surgery, and the Research Foundation of the American Society of Colon and Rectal Surgeons. Dr. Rothenberger is founder and co-director of the UMN Medical School Emerging Physician Leaders Program, which fosters collaboration and develops skills among faculty from all departments.
Arthur J. Vayer, Jr., MD, FACS, recently was installed as vice-speaker of the Medical Society of Virginia (MSV) during the organization’s annual meeting at The Homestead Resort in Hot Springs, VA. Dr. Vayer, a MSV member since 2006 and a general surgeon at Stafford Surgical, Sentara Medical Group, also worked at Robert Cohen, MD, PC, Riverside Gloucester Surgery Associates and in private practice. Dr. Vayer serves as an MSV delegate and associate director, an officer with the Prince William County Medical Society, a committee member at Potomac Hospital, Woodridge, and chairs the performance evaluation committee of Sentara Northern Virginia Medical Center.
Joseph B. Cofer, MD, FACS, a general surgeon and program director, department of surgery, and professor of surgery, University of Tennessee College of Medicine, Chattanooga, president of the American College of Surgeons (ACS) Tennessee Chapter, and current chair of the American Board of Surgery, was named a 2014 recipient of the Accreditation Council for Graduate Medical Education’s J. Palmer Courage to Teach Award.
The award honors program directors who find innovative ways to teach residents and remain committed to providing quality patient care.
Stephen R. T. Evans, MD, FACS, has been elected 2014-2015 vice-chair of the American Board of Surgery (ABS) and will serve as chair in 2015-2016. Dr. Evans is executive vice-president for medical affairs and chief medical officer at MedStar Health in Washington, DC. He also is a professor of surgery at Georgetown University. He is a former President of the American College of Surgeons Metropolitan Washington, DC, Chapter and, in 2009, was elected as an ABS director representing the American Medical Association.
David Rothenberger, MD, FACS, on October 1, 2013, became head of the department of surgery at the University of Minnesota (UMN), Minneapolis. He previously held the John P. Delaney Chair of Clinical Surgical Oncology and was deputy chairman of the department of surgery (2006-2013) at UM
Dr. Rothenberger, an internationally known surgical leader, is past-president of the American Society of Colon and Rectal Surgeons, the American Board of Colon and Rectal Surgery, and the Research Foundation of the American Society of Colon and Rectal Surgeons. Dr. Rothenberger is founder and co-director of the UMN Medical School Emerging Physician Leaders Program, which fosters collaboration and develops skills among faculty from all departments.
Arthur J. Vayer, Jr., MD, FACS, recently was installed as vice-speaker of the Medical Society of Virginia (MSV) during the organization’s annual meeting at The Homestead Resort in Hot Springs, VA. Dr. Vayer, a MSV member since 2006 and a general surgeon at Stafford Surgical, Sentara Medical Group, also worked at Robert Cohen, MD, PC, Riverside Gloucester Surgery Associates and in private practice. Dr. Vayer serves as an MSV delegate and associate director, an officer with the Prince William County Medical Society, a committee member at Potomac Hospital, Woodridge, and chairs the performance evaluation committee of Sentara Northern Virginia Medical Center.
Introspection – the Next Surgical Time-Out
The Town Hall Meeting held at the Annual Meeting of the American College of Surgeons in Washington, DC, on Oct. 8, entitled, "Introspection – the Next Surgical Time-Out," was cochaired by Geoffrey Dunn, M.D., FACS, and Ann Mosenthal, M.D., FACS, with panelists Dan Hinshaw, M.D., FACS, and David Page, M.D., FACS.
Well-attended, the discussion raised specific issues that addressed the growing need for surgeons to care for themselves in a sometimes chaotic and hostile practice environment. Given a reported 30%-40% burnout rate among surgeons, it was felt prudent to explore a side of the surgical personality too often resistant to self-examination. And like scheduled time-outs before starting a case in the OR, it was felt that a personal time-out before diving into the next procedure or busy office session might blunt the frustration born of time constraints and excessive documentation demands piling up on surgical practitioners of all stripes.
For example, an attendee raised the issue of humanizing the otherwise sterile EHR with personal patient information, perhaps insights about the interior life of the patient unrelated to the diagnosis. Another attendee addressed the need for surgeons to model compassion as well as their reactions to grief for learners at all levels. The notion of using videos to teach introspection was raised and discussed, as was the technique of "reflective" or free (uninhibited) writing and journaling as methods for probing one’s inner landscape and deeper feelings and emotions.
The panel addressed the paradox all surgeons face: the need to confront with objectivity organic surgical disease in all of its anatomic-pathologic complexity, employ technical skills in a time-compressed stressful operating room, interact with other caregivers involved in employing complex technology, and then step away from the operative field and become transformed into a compassionate physician. It is fitting that surgeons understand that draping a patient is both a requirement of sterile technique as well as a metaphorical "hiding of the humanity on the table" in order to shift gears and become engrossed "in the moment," to become focused on the mechanical tasks of cure and not distracted by emotional issues.
What challenges the surgeon in ways he or she may not have anticipated is the act of undraping a wounded human who now needs the surgeon’s empathetic attention as the blood stops flowing. Only self-reflection and a consideration of the profound challenges of these diametrically opposed sides of the surgical personality will sustain surgeons through endless daily lists of complex operations and their associated political, cultural, and psychological burdens. And when cure is no longer possible, confrontation with the patient’s imminent demise too often echoes the confrontation between the surgeon and his or her self-image of invincibility.
Also discussed were two recent changes in the matrix of modern surgical practice that were thought to positively shift the traditional image of surgeons as action hero with relative insensitivity to their patients’ suffering. These features include the minimally invasive surgery revolution which transformed the surgeon from blood-splattered aggressor to a delicate-handed laparoscopic wizard capable of heretofore unseen indirect motor skills maneuvers, a quiet ectomorphic individual rather than the traditional mesomorphic "linebacker" persona. The second change is the rise of women in surgery. Once derided, discouraged, and humiliated at every turn, women are now a valued cohort of colleagues whose innate caregiving skills are matched by an admirable and unflinching work ethic. Introspection seems more natural for women, something the macho surgical male ought to learn from.
Finally, introspection was seen to be somewhat like the "second effect" in opioid administration (hastening death is justifiable if the intent is to reduce suffering, not to cause death). Because although the intent of introspection is ultimately to improve the care of our patients, an unforeseen consequence of introspection may center on the arrival of profound insight into the meaning of the surgeon’s own life.
The potential role of artistic expression by surgeons such as painting or creative writing was entertained and will be further explored in a similar format at next year’s ACS meeting in San Francisco.
Dr. Page is professor of surgery at Tufts University School of Medicine, Boston, and director of Undergraduate Programs in the department of surgery, Baystate Medical Center, Springfield, Mass.
The Town Hall Meeting held at the Annual Meeting of the American College of Surgeons in Washington, DC, on Oct. 8, entitled, "Introspection – the Next Surgical Time-Out," was cochaired by Geoffrey Dunn, M.D., FACS, and Ann Mosenthal, M.D., FACS, with panelists Dan Hinshaw, M.D., FACS, and David Page, M.D., FACS.
Well-attended, the discussion raised specific issues that addressed the growing need for surgeons to care for themselves in a sometimes chaotic and hostile practice environment. Given a reported 30%-40% burnout rate among surgeons, it was felt prudent to explore a side of the surgical personality too often resistant to self-examination. And like scheduled time-outs before starting a case in the OR, it was felt that a personal time-out before diving into the next procedure or busy office session might blunt the frustration born of time constraints and excessive documentation demands piling up on surgical practitioners of all stripes.
For example, an attendee raised the issue of humanizing the otherwise sterile EHR with personal patient information, perhaps insights about the interior life of the patient unrelated to the diagnosis. Another attendee addressed the need for surgeons to model compassion as well as their reactions to grief for learners at all levels. The notion of using videos to teach introspection was raised and discussed, as was the technique of "reflective" or free (uninhibited) writing and journaling as methods for probing one’s inner landscape and deeper feelings and emotions.
The panel addressed the paradox all surgeons face: the need to confront with objectivity organic surgical disease in all of its anatomic-pathologic complexity, employ technical skills in a time-compressed stressful operating room, interact with other caregivers involved in employing complex technology, and then step away from the operative field and become transformed into a compassionate physician. It is fitting that surgeons understand that draping a patient is both a requirement of sterile technique as well as a metaphorical "hiding of the humanity on the table" in order to shift gears and become engrossed "in the moment," to become focused on the mechanical tasks of cure and not distracted by emotional issues.
What challenges the surgeon in ways he or she may not have anticipated is the act of undraping a wounded human who now needs the surgeon’s empathetic attention as the blood stops flowing. Only self-reflection and a consideration of the profound challenges of these diametrically opposed sides of the surgical personality will sustain surgeons through endless daily lists of complex operations and their associated political, cultural, and psychological burdens. And when cure is no longer possible, confrontation with the patient’s imminent demise too often echoes the confrontation between the surgeon and his or her self-image of invincibility.
Also discussed were two recent changes in the matrix of modern surgical practice that were thought to positively shift the traditional image of surgeons as action hero with relative insensitivity to their patients’ suffering. These features include the minimally invasive surgery revolution which transformed the surgeon from blood-splattered aggressor to a delicate-handed laparoscopic wizard capable of heretofore unseen indirect motor skills maneuvers, a quiet ectomorphic individual rather than the traditional mesomorphic "linebacker" persona. The second change is the rise of women in surgery. Once derided, discouraged, and humiliated at every turn, women are now a valued cohort of colleagues whose innate caregiving skills are matched by an admirable and unflinching work ethic. Introspection seems more natural for women, something the macho surgical male ought to learn from.
Finally, introspection was seen to be somewhat like the "second effect" in opioid administration (hastening death is justifiable if the intent is to reduce suffering, not to cause death). Because although the intent of introspection is ultimately to improve the care of our patients, an unforeseen consequence of introspection may center on the arrival of profound insight into the meaning of the surgeon’s own life.
The potential role of artistic expression by surgeons such as painting or creative writing was entertained and will be further explored in a similar format at next year’s ACS meeting in San Francisco.
Dr. Page is professor of surgery at Tufts University School of Medicine, Boston, and director of Undergraduate Programs in the department of surgery, Baystate Medical Center, Springfield, Mass.
The Town Hall Meeting held at the Annual Meeting of the American College of Surgeons in Washington, DC, on Oct. 8, entitled, "Introspection – the Next Surgical Time-Out," was cochaired by Geoffrey Dunn, M.D., FACS, and Ann Mosenthal, M.D., FACS, with panelists Dan Hinshaw, M.D., FACS, and David Page, M.D., FACS.
Well-attended, the discussion raised specific issues that addressed the growing need for surgeons to care for themselves in a sometimes chaotic and hostile practice environment. Given a reported 30%-40% burnout rate among surgeons, it was felt prudent to explore a side of the surgical personality too often resistant to self-examination. And like scheduled time-outs before starting a case in the OR, it was felt that a personal time-out before diving into the next procedure or busy office session might blunt the frustration born of time constraints and excessive documentation demands piling up on surgical practitioners of all stripes.
For example, an attendee raised the issue of humanizing the otherwise sterile EHR with personal patient information, perhaps insights about the interior life of the patient unrelated to the diagnosis. Another attendee addressed the need for surgeons to model compassion as well as their reactions to grief for learners at all levels. The notion of using videos to teach introspection was raised and discussed, as was the technique of "reflective" or free (uninhibited) writing and journaling as methods for probing one’s inner landscape and deeper feelings and emotions.
The panel addressed the paradox all surgeons face: the need to confront with objectivity organic surgical disease in all of its anatomic-pathologic complexity, employ technical skills in a time-compressed stressful operating room, interact with other caregivers involved in employing complex technology, and then step away from the operative field and become transformed into a compassionate physician. It is fitting that surgeons understand that draping a patient is both a requirement of sterile technique as well as a metaphorical "hiding of the humanity on the table" in order to shift gears and become engrossed "in the moment," to become focused on the mechanical tasks of cure and not distracted by emotional issues.
What challenges the surgeon in ways he or she may not have anticipated is the act of undraping a wounded human who now needs the surgeon’s empathetic attention as the blood stops flowing. Only self-reflection and a consideration of the profound challenges of these diametrically opposed sides of the surgical personality will sustain surgeons through endless daily lists of complex operations and their associated political, cultural, and psychological burdens. And when cure is no longer possible, confrontation with the patient’s imminent demise too often echoes the confrontation between the surgeon and his or her self-image of invincibility.
Also discussed were two recent changes in the matrix of modern surgical practice that were thought to positively shift the traditional image of surgeons as action hero with relative insensitivity to their patients’ suffering. These features include the minimally invasive surgery revolution which transformed the surgeon from blood-splattered aggressor to a delicate-handed laparoscopic wizard capable of heretofore unseen indirect motor skills maneuvers, a quiet ectomorphic individual rather than the traditional mesomorphic "linebacker" persona. The second change is the rise of women in surgery. Once derided, discouraged, and humiliated at every turn, women are now a valued cohort of colleagues whose innate caregiving skills are matched by an admirable and unflinching work ethic. Introspection seems more natural for women, something the macho surgical male ought to learn from.
Finally, introspection was seen to be somewhat like the "second effect" in opioid administration (hastening death is justifiable if the intent is to reduce suffering, not to cause death). Because although the intent of introspection is ultimately to improve the care of our patients, an unforeseen consequence of introspection may center on the arrival of profound insight into the meaning of the surgeon’s own life.
The potential role of artistic expression by surgeons such as painting or creative writing was entertained and will be further explored in a similar format at next year’s ACS meeting in San Francisco.
Dr. Page is professor of surgery at Tufts University School of Medicine, Boston, and director of Undergraduate Programs in the department of surgery, Baystate Medical Center, Springfield, Mass.
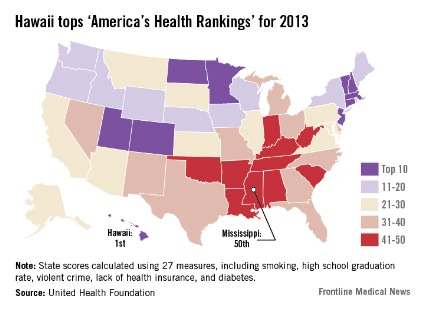
Hawaii named healthiest state in 2013
Residents of Hawaii are living in America’s healthiest state, according to "America's Health Rankings- 2013 Edition."
Hawaii, which has never finished out of the top six since the rankings began in 1990, reclaimed the top spot it last held in 2008. Vermont, which finished first in each of the previous 4 years, was second in 2013, followed by Minnesota, Massachusetts, and New Hampshire.
The bottom five consisted of West Virginia (46) and four states in the Southeast: Alabama (47), Louisiana (48), Arkansas (49), and Mississippi (50). Mississippi has finished "among the bottom three states since the inception of the rankings in 1990," the report said.
For the 2013 report, each state was ranked using 27 measures that represent various aspects of health, grouped into five categories: behaviors, community and environment, policy, clinical care, and outcomes.
"America’s Health Rankings" is published jointly by the United Health Foundation, the American Public Health Association, and the Partnership for Prevention. The private, not-for-profit United Health Foundation was founded in 1999 by UnitedHealth Group, which operates UnitedHealthcare.

Residents of Hawaii are living in America’s healthiest state, according to "America's Health Rankings- 2013 Edition."
Hawaii, which has never finished out of the top six since the rankings began in 1990, reclaimed the top spot it last held in 2008. Vermont, which finished first in each of the previous 4 years, was second in 2013, followed by Minnesota, Massachusetts, and New Hampshire.
The bottom five consisted of West Virginia (46) and four states in the Southeast: Alabama (47), Louisiana (48), Arkansas (49), and Mississippi (50). Mississippi has finished "among the bottom three states since the inception of the rankings in 1990," the report said.
For the 2013 report, each state was ranked using 27 measures that represent various aspects of health, grouped into five categories: behaviors, community and environment, policy, clinical care, and outcomes.
"America’s Health Rankings" is published jointly by the United Health Foundation, the American Public Health Association, and the Partnership for Prevention. The private, not-for-profit United Health Foundation was founded in 1999 by UnitedHealth Group, which operates UnitedHealthcare.

Residents of Hawaii are living in America’s healthiest state, according to "America's Health Rankings- 2013 Edition."
Hawaii, which has never finished out of the top six since the rankings began in 1990, reclaimed the top spot it last held in 2008. Vermont, which finished first in each of the previous 4 years, was second in 2013, followed by Minnesota, Massachusetts, and New Hampshire.
The bottom five consisted of West Virginia (46) and four states in the Southeast: Alabama (47), Louisiana (48), Arkansas (49), and Mississippi (50). Mississippi has finished "among the bottom three states since the inception of the rankings in 1990," the report said.
For the 2013 report, each state was ranked using 27 measures that represent various aspects of health, grouped into five categories: behaviors, community and environment, policy, clinical care, and outcomes.
"America’s Health Rankings" is published jointly by the United Health Foundation, the American Public Health Association, and the Partnership for Prevention. The private, not-for-profit United Health Foundation was founded in 1999 by UnitedHealth Group, which operates UnitedHealthcare.

FDA: Stop prescribing combo drugs with high-dose acetaminophen
The Food and Drug Administration is turning to doctors, dentists, and pharmacists to accomplish what some drug manufacturers won’t help it do.
In 2011, the agency recommended manufacturers cease marketing of acetaminophen/opioid combination products with more than 325 mg of acetaminophen per dose, in an effort to reduce the risk of severe liver injury. Not all manufacturers complied.
Now, the agency on Jan. 14 issued a MedWatch recommendation that health care providers refrain from prescribing combinations with larger acetaminophen doses. The recommendation goes further, urging pharmacists to contact prescribers when they receive a prescription for a combination product with more than 325 mg of acetaminophen per dose to discuss a substitute product with a lower acetaminophen dose.
"Inadvertent overdose from prescription combination drugs containing acetaminophen accounts for nearly half of all cases of acetaminophen-related liver failure in the United States, some of which result in liver transplant or death," the agency said, in a statement.
In the same 2011 notice, the FDA is requiring prescription acetaminophen combinations to carry a boxed warning on the potential for liver damage.
Acetaminophen-containing prescription combinations are among the most-prescribed pharmaceuticals in the United States, and include products such as Vicodin (acetaminophen/hydrocodone), Percocet (acetaminophen/oxycodone), and Tylenol with codeine.
The FDA has been examining acetaminophen since at least 2002. The recommendations of a joint meeting of several advisory committees in 2009 resulted in the 2011 policy changes and recommendations.
The agency now has sent letters to manufacturers that have not lowered the acetaminophen dose warning them that the FDA will withdraw approval of those products.
Physicians can report adverse events or side effects related to the use of acetaminophen products to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program either online or at 800-332-1088.
On Twitter @aliciaault
The Food and Drug Administration is turning to doctors, dentists, and pharmacists to accomplish what some drug manufacturers won’t help it do.
In 2011, the agency recommended manufacturers cease marketing of acetaminophen/opioid combination products with more than 325 mg of acetaminophen per dose, in an effort to reduce the risk of severe liver injury. Not all manufacturers complied.
Now, the agency on Jan. 14 issued a MedWatch recommendation that health care providers refrain from prescribing combinations with larger acetaminophen doses. The recommendation goes further, urging pharmacists to contact prescribers when they receive a prescription for a combination product with more than 325 mg of acetaminophen per dose to discuss a substitute product with a lower acetaminophen dose.
"Inadvertent overdose from prescription combination drugs containing acetaminophen accounts for nearly half of all cases of acetaminophen-related liver failure in the United States, some of which result in liver transplant or death," the agency said, in a statement.
In the same 2011 notice, the FDA is requiring prescription acetaminophen combinations to carry a boxed warning on the potential for liver damage.
Acetaminophen-containing prescription combinations are among the most-prescribed pharmaceuticals in the United States, and include products such as Vicodin (acetaminophen/hydrocodone), Percocet (acetaminophen/oxycodone), and Tylenol with codeine.
The FDA has been examining acetaminophen since at least 2002. The recommendations of a joint meeting of several advisory committees in 2009 resulted in the 2011 policy changes and recommendations.
The agency now has sent letters to manufacturers that have not lowered the acetaminophen dose warning them that the FDA will withdraw approval of those products.
Physicians can report adverse events or side effects related to the use of acetaminophen products to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program either online or at 800-332-1088.
On Twitter @aliciaault
The Food and Drug Administration is turning to doctors, dentists, and pharmacists to accomplish what some drug manufacturers won’t help it do.
In 2011, the agency recommended manufacturers cease marketing of acetaminophen/opioid combination products with more than 325 mg of acetaminophen per dose, in an effort to reduce the risk of severe liver injury. Not all manufacturers complied.
Now, the agency on Jan. 14 issued a MedWatch recommendation that health care providers refrain from prescribing combinations with larger acetaminophen doses. The recommendation goes further, urging pharmacists to contact prescribers when they receive a prescription for a combination product with more than 325 mg of acetaminophen per dose to discuss a substitute product with a lower acetaminophen dose.
"Inadvertent overdose from prescription combination drugs containing acetaminophen accounts for nearly half of all cases of acetaminophen-related liver failure in the United States, some of which result in liver transplant or death," the agency said, in a statement.
In the same 2011 notice, the FDA is requiring prescription acetaminophen combinations to carry a boxed warning on the potential for liver damage.
Acetaminophen-containing prescription combinations are among the most-prescribed pharmaceuticals in the United States, and include products such as Vicodin (acetaminophen/hydrocodone), Percocet (acetaminophen/oxycodone), and Tylenol with codeine.
The FDA has been examining acetaminophen since at least 2002. The recommendations of a joint meeting of several advisory committees in 2009 resulted in the 2011 policy changes and recommendations.
The agency now has sent letters to manufacturers that have not lowered the acetaminophen dose warning them that the FDA will withdraw approval of those products.
Physicians can report adverse events or side effects related to the use of acetaminophen products to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program either online or at 800-332-1088.
On Twitter @aliciaault
Obesity as a disease: Implications for treatment and reimbursement
WASHINGTON – Despite the recent attention given to considering obesity a disease, there are still many limitations to providing treatments for obesity and receiving adequate reimbursement for those treatments, Dr. Lee Kaplan said at a public workshop cosponsored by the Food and Drug Administration and the American Gastroenterological Association.
The American Medical Association resolution to recognize obesity as a disease in 2013 has no legal authority, and therefore does not represent as much progress as suggested by the media attention surrounding the announcement, said Dr. Kaplan, director of the Massachusetts General Hospital Weight Center, Boston.
The AMA resolution was preceded by the Internal Revenue Service’s determination that obesity could qualify as a medical deduction in 2007, and in 2008, the Obesity Society provided support for considering obesity as a medical disorder.
But despite these apparent signs of progress, limitations remain. Weight loss drugs are excluded under Medicare Part D coverage, and while Medicare has started coverage for nutritional counseling, only services provided in a primary care setting are covered, he pointed out. An estimated 1 of every 400 people with obesity in the United States has bariatric surgery every year, but 1 in 100-150 of every 400 meets the criteria for surgery, which "doesn’t sound like we are addressing the problem very seriously," he said.
One problem is that obesity, which has many causes, is lumped together "into one big group," raising the issue of whether treating obesity would require an investment that is so huge, "that even as a society we cannot make it."
A critical issue is how to define obesity, Dr. Kaplan said. A simple definition is excess fat accumulation that presents a risk to health, but this definition does not include ways of measuring excess fat. One measurement, body mass index, is a marker, not a definition of obesity.
A major barrier is the development of an effective therapy, he said, noting that other than gastric bands, there are no devices on the market to treat obesity, and the four drugs approved by the FDA have modest efficacy overall and are not widely used. Another major barrier is "provider utilization," getting the provider to prescribe treatments and obtain reimbursement for the costs of treatment.
"There is also a large gap between the relatively noninvasive treatments and the invasive, more effective therapies, which needs to be filled by midlevel therapies," he said. Those therapies should be gastrointestinal therapies almost exclusively, he added. The current treatment strategy is fairly simplistic: Patients are asked to change their lifestyle and when that does not work, the next step is to see a dietician, psychologist, or another professional to help with their lifestyle changes, followed by the addition of medication if that does not work. Surgery is broached in a small number of patients.
"Obesity is a disease whether we call it one or not, because it behaves like a disease," and there are implications to viewing it as a disease, he said. Therapy should be physiologically based, and the heterogeneity in the underlying causes of obesity, which explains the variable treatment responses, provides an opportunity to benefit selected subpopulations.
Considering the number of disorders that are associated with obesity, it is not surprising that treatment responses vary widely, Dr. Kaplan said. People with one defect may do better than others with gastric bypass, and some people may respond better than others to the approved combination of phentermine and topiramate (Qsymia) – as reflected in the ranges of response rates associated with these therapies, he pointed out.
The average excess weight loss with gastric bypass, the most effective therapy for obesity, is about 65%, but it can be as low as 20% in some people. With banding, some patients lose all or most of their excess weight, but most lose about 25%-30%, he said. Similarly, Dr. Kaplan found some patients responded well to treatment with sibutramine (which is no longer marketed), while others did not respond well; the same pattern was seen with lorcaserin.
"Whether you’re talking about a drug, a device, surgery, or lifestyle modifications, ... you see this very broad response," because there are subtypes of obesity, he said. Identifying the subgroups of patients that are highly responsive to any of these treatments could increase the success rate of the treatment, he noted.
In December 2013, the AGA's Center for Gastrointestinal Innovation and Technology (CGIT), along with the Food and Drug Administration, held a workshop on "Changing Regulatory and Reimbursement Paradigms for Medical Devices in the Treatment of Metabolic Diseases: How to Estimate and Reward True Patient-Centric Value."

|
| Dr. Jay Pasricha |
The theme of the workshop was broad, but obesity and reflux were chosen as representative conditions that highlighted the challenges that companies and innovators face. The FDA showcased some truly innovative GI devices. These initiatives were praised by the other groups, and it is hoped the workshop will inspire similar introspection into coverage policies as well.
It also became clear at the workshop that continuing with current regulatory and reimbursement procedures may result in the throttling of medical innovation. Therefore, taking ownership of the reform process is a task that all parties need to embrace.
The workshop was very successful in bringing together representatives from all walks, and members in the audience enthusiastically joined vigorous discussions by the panel. As a follow-up, the CGIT and FDA are working on a white paper that will lay out a road map for much needed changes.
Dr. Jay Pasricha is director of the Center for Neurogastroenterology and professor (PAR) of medicine at Johns Hopkins University, Baltimore. He has no relevant conflicts of interest.
In December 2013, the AGA's Center for Gastrointestinal Innovation and Technology (CGIT), along with the Food and Drug Administration, held a workshop on "Changing Regulatory and Reimbursement Paradigms for Medical Devices in the Treatment of Metabolic Diseases: How to Estimate and Reward True Patient-Centric Value."

|
| Dr. Jay Pasricha |
The theme of the workshop was broad, but obesity and reflux were chosen as representative conditions that highlighted the challenges that companies and innovators face. The FDA showcased some truly innovative GI devices. These initiatives were praised by the other groups, and it is hoped the workshop will inspire similar introspection into coverage policies as well.
It also became clear at the workshop that continuing with current regulatory and reimbursement procedures may result in the throttling of medical innovation. Therefore, taking ownership of the reform process is a task that all parties need to embrace.
The workshop was very successful in bringing together representatives from all walks, and members in the audience enthusiastically joined vigorous discussions by the panel. As a follow-up, the CGIT and FDA are working on a white paper that will lay out a road map for much needed changes.
Dr. Jay Pasricha is director of the Center for Neurogastroenterology and professor (PAR) of medicine at Johns Hopkins University, Baltimore. He has no relevant conflicts of interest.
In December 2013, the AGA's Center for Gastrointestinal Innovation and Technology (CGIT), along with the Food and Drug Administration, held a workshop on "Changing Regulatory and Reimbursement Paradigms for Medical Devices in the Treatment of Metabolic Diseases: How to Estimate and Reward True Patient-Centric Value."

|
| Dr. Jay Pasricha |
The theme of the workshop was broad, but obesity and reflux were chosen as representative conditions that highlighted the challenges that companies and innovators face. The FDA showcased some truly innovative GI devices. These initiatives were praised by the other groups, and it is hoped the workshop will inspire similar introspection into coverage policies as well.
It also became clear at the workshop that continuing with current regulatory and reimbursement procedures may result in the throttling of medical innovation. Therefore, taking ownership of the reform process is a task that all parties need to embrace.
The workshop was very successful in bringing together representatives from all walks, and members in the audience enthusiastically joined vigorous discussions by the panel. As a follow-up, the CGIT and FDA are working on a white paper that will lay out a road map for much needed changes.
Dr. Jay Pasricha is director of the Center for Neurogastroenterology and professor (PAR) of medicine at Johns Hopkins University, Baltimore. He has no relevant conflicts of interest.
WASHINGTON – Despite the recent attention given to considering obesity a disease, there are still many limitations to providing treatments for obesity and receiving adequate reimbursement for those treatments, Dr. Lee Kaplan said at a public workshop cosponsored by the Food and Drug Administration and the American Gastroenterological Association.
The American Medical Association resolution to recognize obesity as a disease in 2013 has no legal authority, and therefore does not represent as much progress as suggested by the media attention surrounding the announcement, said Dr. Kaplan, director of the Massachusetts General Hospital Weight Center, Boston.
The AMA resolution was preceded by the Internal Revenue Service’s determination that obesity could qualify as a medical deduction in 2007, and in 2008, the Obesity Society provided support for considering obesity as a medical disorder.
But despite these apparent signs of progress, limitations remain. Weight loss drugs are excluded under Medicare Part D coverage, and while Medicare has started coverage for nutritional counseling, only services provided in a primary care setting are covered, he pointed out. An estimated 1 of every 400 people with obesity in the United States has bariatric surgery every year, but 1 in 100-150 of every 400 meets the criteria for surgery, which "doesn’t sound like we are addressing the problem very seriously," he said.
One problem is that obesity, which has many causes, is lumped together "into one big group," raising the issue of whether treating obesity would require an investment that is so huge, "that even as a society we cannot make it."
A critical issue is how to define obesity, Dr. Kaplan said. A simple definition is excess fat accumulation that presents a risk to health, but this definition does not include ways of measuring excess fat. One measurement, body mass index, is a marker, not a definition of obesity.
A major barrier is the development of an effective therapy, he said, noting that other than gastric bands, there are no devices on the market to treat obesity, and the four drugs approved by the FDA have modest efficacy overall and are not widely used. Another major barrier is "provider utilization," getting the provider to prescribe treatments and obtain reimbursement for the costs of treatment.
"There is also a large gap between the relatively noninvasive treatments and the invasive, more effective therapies, which needs to be filled by midlevel therapies," he said. Those therapies should be gastrointestinal therapies almost exclusively, he added. The current treatment strategy is fairly simplistic: Patients are asked to change their lifestyle and when that does not work, the next step is to see a dietician, psychologist, or another professional to help with their lifestyle changes, followed by the addition of medication if that does not work. Surgery is broached in a small number of patients.
"Obesity is a disease whether we call it one or not, because it behaves like a disease," and there are implications to viewing it as a disease, he said. Therapy should be physiologically based, and the heterogeneity in the underlying causes of obesity, which explains the variable treatment responses, provides an opportunity to benefit selected subpopulations.
Considering the number of disorders that are associated with obesity, it is not surprising that treatment responses vary widely, Dr. Kaplan said. People with one defect may do better than others with gastric bypass, and some people may respond better than others to the approved combination of phentermine and topiramate (Qsymia) – as reflected in the ranges of response rates associated with these therapies, he pointed out.
The average excess weight loss with gastric bypass, the most effective therapy for obesity, is about 65%, but it can be as low as 20% in some people. With banding, some patients lose all or most of their excess weight, but most lose about 25%-30%, he said. Similarly, Dr. Kaplan found some patients responded well to treatment with sibutramine (which is no longer marketed), while others did not respond well; the same pattern was seen with lorcaserin.
"Whether you’re talking about a drug, a device, surgery, or lifestyle modifications, ... you see this very broad response," because there are subtypes of obesity, he said. Identifying the subgroups of patients that are highly responsive to any of these treatments could increase the success rate of the treatment, he noted.
WASHINGTON – Despite the recent attention given to considering obesity a disease, there are still many limitations to providing treatments for obesity and receiving adequate reimbursement for those treatments, Dr. Lee Kaplan said at a public workshop cosponsored by the Food and Drug Administration and the American Gastroenterological Association.
The American Medical Association resolution to recognize obesity as a disease in 2013 has no legal authority, and therefore does not represent as much progress as suggested by the media attention surrounding the announcement, said Dr. Kaplan, director of the Massachusetts General Hospital Weight Center, Boston.
The AMA resolution was preceded by the Internal Revenue Service’s determination that obesity could qualify as a medical deduction in 2007, and in 2008, the Obesity Society provided support for considering obesity as a medical disorder.
But despite these apparent signs of progress, limitations remain. Weight loss drugs are excluded under Medicare Part D coverage, and while Medicare has started coverage for nutritional counseling, only services provided in a primary care setting are covered, he pointed out. An estimated 1 of every 400 people with obesity in the United States has bariatric surgery every year, but 1 in 100-150 of every 400 meets the criteria for surgery, which "doesn’t sound like we are addressing the problem very seriously," he said.
One problem is that obesity, which has many causes, is lumped together "into one big group," raising the issue of whether treating obesity would require an investment that is so huge, "that even as a society we cannot make it."
A critical issue is how to define obesity, Dr. Kaplan said. A simple definition is excess fat accumulation that presents a risk to health, but this definition does not include ways of measuring excess fat. One measurement, body mass index, is a marker, not a definition of obesity.
A major barrier is the development of an effective therapy, he said, noting that other than gastric bands, there are no devices on the market to treat obesity, and the four drugs approved by the FDA have modest efficacy overall and are not widely used. Another major barrier is "provider utilization," getting the provider to prescribe treatments and obtain reimbursement for the costs of treatment.
"There is also a large gap between the relatively noninvasive treatments and the invasive, more effective therapies, which needs to be filled by midlevel therapies," he said. Those therapies should be gastrointestinal therapies almost exclusively, he added. The current treatment strategy is fairly simplistic: Patients are asked to change their lifestyle and when that does not work, the next step is to see a dietician, psychologist, or another professional to help with their lifestyle changes, followed by the addition of medication if that does not work. Surgery is broached in a small number of patients.
"Obesity is a disease whether we call it one or not, because it behaves like a disease," and there are implications to viewing it as a disease, he said. Therapy should be physiologically based, and the heterogeneity in the underlying causes of obesity, which explains the variable treatment responses, provides an opportunity to benefit selected subpopulations.
Considering the number of disorders that are associated with obesity, it is not surprising that treatment responses vary widely, Dr. Kaplan said. People with one defect may do better than others with gastric bypass, and some people may respond better than others to the approved combination of phentermine and topiramate (Qsymia) – as reflected in the ranges of response rates associated with these therapies, he pointed out.
The average excess weight loss with gastric bypass, the most effective therapy for obesity, is about 65%, but it can be as low as 20% in some people. With banding, some patients lose all or most of their excess weight, but most lose about 25%-30%, he said. Similarly, Dr. Kaplan found some patients responded well to treatment with sibutramine (which is no longer marketed), while others did not respond well; the same pattern was seen with lorcaserin.
"Whether you’re talking about a drug, a device, surgery, or lifestyle modifications, ... you see this very broad response," because there are subtypes of obesity, he said. Identifying the subgroups of patients that are highly responsive to any of these treatments could increase the success rate of the treatment, he noted.
AT AN FDA/AGA WORKSHOP
Inflammatory markers associated with IBD colon cancer risk
As C-reactive protein levels and erythrocyte sedimentation rates go up in patients with inflammatory bowel disease, the risk of colorectal cancer goes up, too, a finding that suggests a role for both as markers of colon cancer risk, Boston investigators reported in a prospective study published online Jan. 6 in Clinical Gastroenterology and Hepatology.
The team divided 3,145 IBD patients into quartiles based on median C-reactive protein (CRP) levels, and 4,008 others into quartiles based on median erythrocyte sedimentation rates (ESR), then followed them for a median of 6 years.
On multivariate analysis, there was a significant increase in the risk of colorectal cancer (CRC) across quartiles of CRP elevation (P for trend = .017). Higher median ESR was also independently associated with higher risk of CRC across quartiles (P for trend = .007) (Clin. Gastroenterol. Hepatol. 2014 Jan. 6 [doi: 10.1016/j.cgh.2013.12.030]).
"This association adds another clinical variable to help stratify patients into risk categories. There is an important need to identify high-risk subgroups that may benefit from continued intensive surveillance strategies while allowing for less frequent colonoscopies in patients at low risk of CRC. We believe that our findings ... suggest that an individual patient’s severity of inflammation may be helpful in further personalizing surveillance recommendations," and might even help monitor other outcomes, including treatment response, said the authors, led by Dr. Ashwin Ananthakrishnan, a gastroenterologist at Massachusetts General Hospital, Boston.
After adjustment for age, sex, race, IBD type, and other factors, the patients in the highest CRP quartile had more than double the risk of colorectal cancer compared with those in the lowest quartile (OR 2.72, 95% CI 0.95-7.76). The strength of association was similar in men and women, and in Crohn’s disease and ulcerative colitis.
Similarly, patients in the highest ESR quartile had double the risk compared with those in the lowest (OR 2.06, 95% CI 1.14-3.74). The correlation was strongest in ulcerative colitis patients and men.
The median CRP values in each of the quartiles were 0.8, 2.7, 7.5, and 32.8 mg/L. In the ESR group, the median quartile values were 7, 14, 25, and 50 mm/hr.
Overall, 33 patients in the CRP cohort and 102 patients in the ESR cohort developed colorectal cancer at a median age of 55 years. The median number of CRP measurements was three, and median number of ESR measurements six. More than half the subjects were women, most were white, and ulcerative colitis was slightly more common than was Crohn’s disease.
Adjusting for number of colonoscopies, intensity of health care utilization, use of corticosteroids, and other factors did not change results for either the CRP or ESR cohorts.
The National Institutes of Health funded the work. The investigators have no disclosures.
As C-reactive protein levels and erythrocyte sedimentation rates go up in patients with inflammatory bowel disease, the risk of colorectal cancer goes up, too, a finding that suggests a role for both as markers of colon cancer risk, Boston investigators reported in a prospective study published online Jan. 6 in Clinical Gastroenterology and Hepatology.
The team divided 3,145 IBD patients into quartiles based on median C-reactive protein (CRP) levels, and 4,008 others into quartiles based on median erythrocyte sedimentation rates (ESR), then followed them for a median of 6 years.
On multivariate analysis, there was a significant increase in the risk of colorectal cancer (CRC) across quartiles of CRP elevation (P for trend = .017). Higher median ESR was also independently associated with higher risk of CRC across quartiles (P for trend = .007) (Clin. Gastroenterol. Hepatol. 2014 Jan. 6 [doi: 10.1016/j.cgh.2013.12.030]).
"This association adds another clinical variable to help stratify patients into risk categories. There is an important need to identify high-risk subgroups that may benefit from continued intensive surveillance strategies while allowing for less frequent colonoscopies in patients at low risk of CRC. We believe that our findings ... suggest that an individual patient’s severity of inflammation may be helpful in further personalizing surveillance recommendations," and might even help monitor other outcomes, including treatment response, said the authors, led by Dr. Ashwin Ananthakrishnan, a gastroenterologist at Massachusetts General Hospital, Boston.
After adjustment for age, sex, race, IBD type, and other factors, the patients in the highest CRP quartile had more than double the risk of colorectal cancer compared with those in the lowest quartile (OR 2.72, 95% CI 0.95-7.76). The strength of association was similar in men and women, and in Crohn’s disease and ulcerative colitis.
Similarly, patients in the highest ESR quartile had double the risk compared with those in the lowest (OR 2.06, 95% CI 1.14-3.74). The correlation was strongest in ulcerative colitis patients and men.
The median CRP values in each of the quartiles were 0.8, 2.7, 7.5, and 32.8 mg/L. In the ESR group, the median quartile values were 7, 14, 25, and 50 mm/hr.
Overall, 33 patients in the CRP cohort and 102 patients in the ESR cohort developed colorectal cancer at a median age of 55 years. The median number of CRP measurements was three, and median number of ESR measurements six. More than half the subjects were women, most were white, and ulcerative colitis was slightly more common than was Crohn’s disease.
Adjusting for number of colonoscopies, intensity of health care utilization, use of corticosteroids, and other factors did not change results for either the CRP or ESR cohorts.
The National Institutes of Health funded the work. The investigators have no disclosures.
As C-reactive protein levels and erythrocyte sedimentation rates go up in patients with inflammatory bowel disease, the risk of colorectal cancer goes up, too, a finding that suggests a role for both as markers of colon cancer risk, Boston investigators reported in a prospective study published online Jan. 6 in Clinical Gastroenterology and Hepatology.
The team divided 3,145 IBD patients into quartiles based on median C-reactive protein (CRP) levels, and 4,008 others into quartiles based on median erythrocyte sedimentation rates (ESR), then followed them for a median of 6 years.
On multivariate analysis, there was a significant increase in the risk of colorectal cancer (CRC) across quartiles of CRP elevation (P for trend = .017). Higher median ESR was also independently associated with higher risk of CRC across quartiles (P for trend = .007) (Clin. Gastroenterol. Hepatol. 2014 Jan. 6 [doi: 10.1016/j.cgh.2013.12.030]).
"This association adds another clinical variable to help stratify patients into risk categories. There is an important need to identify high-risk subgroups that may benefit from continued intensive surveillance strategies while allowing for less frequent colonoscopies in patients at low risk of CRC. We believe that our findings ... suggest that an individual patient’s severity of inflammation may be helpful in further personalizing surveillance recommendations," and might even help monitor other outcomes, including treatment response, said the authors, led by Dr. Ashwin Ananthakrishnan, a gastroenterologist at Massachusetts General Hospital, Boston.
After adjustment for age, sex, race, IBD type, and other factors, the patients in the highest CRP quartile had more than double the risk of colorectal cancer compared with those in the lowest quartile (OR 2.72, 95% CI 0.95-7.76). The strength of association was similar in men and women, and in Crohn’s disease and ulcerative colitis.
Similarly, patients in the highest ESR quartile had double the risk compared with those in the lowest (OR 2.06, 95% CI 1.14-3.74). The correlation was strongest in ulcerative colitis patients and men.
The median CRP values in each of the quartiles were 0.8, 2.7, 7.5, and 32.8 mg/L. In the ESR group, the median quartile values were 7, 14, 25, and 50 mm/hr.
Overall, 33 patients in the CRP cohort and 102 patients in the ESR cohort developed colorectal cancer at a median age of 55 years. The median number of CRP measurements was three, and median number of ESR measurements six. More than half the subjects were women, most were white, and ulcerative colitis was slightly more common than was Crohn’s disease.
Adjusting for number of colonoscopies, intensity of health care utilization, use of corticosteroids, and other factors did not change results for either the CRP or ESR cohorts.
The National Institutes of Health funded the work. The investigators have no disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Major finding: The risk of colorectal cancer is more than double for IBD patients with the highest quartile values of CRP (P for trend = .017) and ESR (P for trend = .007).
Data Source: Prospective, longitudinal study of 7,153 adult IBD patients.
Disclosures: The work was funded by the National Institutes of Health. The investigators have no disclosures.
Medicare to start releasing individual physician payment data
Reversing more than 30 years of policy, federal officials announced they would soon begin releasing data on how much Medicare pays to individual physicians.
Officials at the Centers for Medicare and Medicaid Services (CMS) announced Jan. 14 that they would take a "case-by-case" approach to the release of individual physician payment information, weighing the right for privacy against the value to the public in each Freedom of Information Act request they receive.
In addition to fielding individual requests for physician data, the agency plans to generate and publish aggregate data sets on physician services.
The policy change will take effect on March 18.
"As CMS makes a determination about how and when to disclose any information on a physician’s Medicare payment, we intend to consider the importance of protecting physicians’ privacy and ensuring the accuracy of any data released as well as appropriate protections to limit potential misuse of the information," Jonathan Blum, CMS Principal Deputy Administrator, wrote in a blog post on Jan. 14.
Last May, a federal judge cleared the way for this policy shift back by lifting an injunction that had previously barred the agency from making public its database of Medicare physician claims.
The new policy has plenty of benefits, Mr. Blum wrote, including allowing providers to collaborate on better care management, giving consumers more reliable measures of quality and performance, and allowing journalists and researchers to identify Medicare waste, fraud, and abuse.
The change is also part of a broader effort at the CMS to make health care prices more transparent.
Last May, the CMS published the average charges for the 100 most common inpatient services at hospitals around the country. And in June, the agency released average charges for 30 selected outpatient procedures, ranging from echocardiograms to pulmonary tests.
Physicians’ groups have been urging caution as the CMS evaluated the release of physician data. In a Sept. 5 letter signed by the American Medical Association as well as several specialty and state medical societies, physicians said that the CMS must educate the public about the limitations of analyzing Medicare claims data. For example, Medicare claims may not include many factors that influence the cost of medical care, including specialty, location, patient mix, other demographics, and practice costs.
In the letter, the physician organizations urged the CMS to provide access to data to organizations that have experience in handling and analyzing Medicare data. And they called for the opportunity to review and correct their information in a timely manner.
"Medicare data is highly susceptible to misleading conclusions," the letter said. "CMS should undertake a detailed educational program to explain any Medicare data release program and openly address its limitations, including that the data may take into account only a small fraction of a physician’s patient population or may be outdated."
Reversing more than 30 years of policy, federal officials announced they would soon begin releasing data on how much Medicare pays to individual physicians.
Officials at the Centers for Medicare and Medicaid Services (CMS) announced Jan. 14 that they would take a "case-by-case" approach to the release of individual physician payment information, weighing the right for privacy against the value to the public in each Freedom of Information Act request they receive.
In addition to fielding individual requests for physician data, the agency plans to generate and publish aggregate data sets on physician services.
The policy change will take effect on March 18.
"As CMS makes a determination about how and when to disclose any information on a physician’s Medicare payment, we intend to consider the importance of protecting physicians’ privacy and ensuring the accuracy of any data released as well as appropriate protections to limit potential misuse of the information," Jonathan Blum, CMS Principal Deputy Administrator, wrote in a blog post on Jan. 14.
Last May, a federal judge cleared the way for this policy shift back by lifting an injunction that had previously barred the agency from making public its database of Medicare physician claims.
The new policy has plenty of benefits, Mr. Blum wrote, including allowing providers to collaborate on better care management, giving consumers more reliable measures of quality and performance, and allowing journalists and researchers to identify Medicare waste, fraud, and abuse.
The change is also part of a broader effort at the CMS to make health care prices more transparent.
Last May, the CMS published the average charges for the 100 most common inpatient services at hospitals around the country. And in June, the agency released average charges for 30 selected outpatient procedures, ranging from echocardiograms to pulmonary tests.
Physicians’ groups have been urging caution as the CMS evaluated the release of physician data. In a Sept. 5 letter signed by the American Medical Association as well as several specialty and state medical societies, physicians said that the CMS must educate the public about the limitations of analyzing Medicare claims data. For example, Medicare claims may not include many factors that influence the cost of medical care, including specialty, location, patient mix, other demographics, and practice costs.
In the letter, the physician organizations urged the CMS to provide access to data to organizations that have experience in handling and analyzing Medicare data. And they called for the opportunity to review and correct their information in a timely manner.
"Medicare data is highly susceptible to misleading conclusions," the letter said. "CMS should undertake a detailed educational program to explain any Medicare data release program and openly address its limitations, including that the data may take into account only a small fraction of a physician’s patient population or may be outdated."
Reversing more than 30 years of policy, federal officials announced they would soon begin releasing data on how much Medicare pays to individual physicians.
Officials at the Centers for Medicare and Medicaid Services (CMS) announced Jan. 14 that they would take a "case-by-case" approach to the release of individual physician payment information, weighing the right for privacy against the value to the public in each Freedom of Information Act request they receive.
In addition to fielding individual requests for physician data, the agency plans to generate and publish aggregate data sets on physician services.
The policy change will take effect on March 18.
"As CMS makes a determination about how and when to disclose any information on a physician’s Medicare payment, we intend to consider the importance of protecting physicians’ privacy and ensuring the accuracy of any data released as well as appropriate protections to limit potential misuse of the information," Jonathan Blum, CMS Principal Deputy Administrator, wrote in a blog post on Jan. 14.
Last May, a federal judge cleared the way for this policy shift back by lifting an injunction that had previously barred the agency from making public its database of Medicare physician claims.
The new policy has plenty of benefits, Mr. Blum wrote, including allowing providers to collaborate on better care management, giving consumers more reliable measures of quality and performance, and allowing journalists and researchers to identify Medicare waste, fraud, and abuse.
The change is also part of a broader effort at the CMS to make health care prices more transparent.
Last May, the CMS published the average charges for the 100 most common inpatient services at hospitals around the country. And in June, the agency released average charges for 30 selected outpatient procedures, ranging from echocardiograms to pulmonary tests.
Physicians’ groups have been urging caution as the CMS evaluated the release of physician data. In a Sept. 5 letter signed by the American Medical Association as well as several specialty and state medical societies, physicians said that the CMS must educate the public about the limitations of analyzing Medicare claims data. For example, Medicare claims may not include many factors that influence the cost of medical care, including specialty, location, patient mix, other demographics, and practice costs.
In the letter, the physician organizations urged the CMS to provide access to data to organizations that have experience in handling and analyzing Medicare data. And they called for the opportunity to review and correct their information in a timely manner.
"Medicare data is highly susceptible to misleading conclusions," the letter said. "CMS should undertake a detailed educational program to explain any Medicare data release program and openly address its limitations, including that the data may take into account only a small fraction of a physician’s patient population or may be outdated."
ACA marketplace enrollment nears 2.2 million
Nearly 2.2 million Americans enrolled in private health plans through federally or state-run insurance marketplaces during the first 3 months of the Affordable Care Act’s open enrollment period, nearly a quarter of whom are aged 18-34 years, according to figures released Jan. 13 by the Health and Human Services department.
"The numbers show that there is a very strong national demand for affordable health care made possible by the Affordable Care Act," Kathleen Sebelius, HHS secretary, said during a press briefing. "Among young adults, the momentum was particularly strong."
More women (54%) than men (46%) enrolled in a health care plan, according to preliminary demographic data provided by HHS. This is the first time demographic information has been released.
More than half of marketplace enrollees are between ages 45 and 64 years, with 22% aged 45-54 years and 33% in aged 55-64 years.
But HHS officials said they were encouraged by the number of younger Americans who had selected a plan through the marketplace. Young, and presumably healthy enrollees, are considered essential to ensuring a favorable risk mix for insurers. Over the first 3 months of open season, individuals aged 18-34 years made up 24% of enrollees. In comparison, 18-34 year olds make up 26% of the U.S. population under age 65 years.
"We think that more and more young people are going to sign up as time goes by, which was the experience in Massachusetts," Gary Cohen, director of the Center for Consumer Information and Insurance Oversight at the Centers for Medicare and Medicaid Services, said during the press briefing.
Overall, enrollment in health plans surged in December, outstripping the slow start of the online insurance marketplaces in October. The number of people enrolling in a health plan through the marketplaces, which HHS defines as selecting but not necessarily paying for a plan, was more than 1.7 million in December alone, up from about 364,000 in October and November.
Another 1.6 million Americans were deemed eligible for Medicaid or the Children’s Health Insurance Program through the marketplaces from Oct. 1 through Dec. 28, according to the report. That figure does not include individuals who applied to the program directly through their state agencies.
Most enrollees selected plans with lower premiums and higher out-of-pocket costs. A total of 60% selected a "silver" plan and another 20% selected a "bronze" plan.
Most enrollees (79%) are receiving some type of financial assistance in paying their premiums, according to the HHS report.
Nearly 2.2 million Americans enrolled in private health plans through federally or state-run insurance marketplaces during the first 3 months of the Affordable Care Act’s open enrollment period, nearly a quarter of whom are aged 18-34 years, according to figures released Jan. 13 by the Health and Human Services department.
"The numbers show that there is a very strong national demand for affordable health care made possible by the Affordable Care Act," Kathleen Sebelius, HHS secretary, said during a press briefing. "Among young adults, the momentum was particularly strong."
More women (54%) than men (46%) enrolled in a health care plan, according to preliminary demographic data provided by HHS. This is the first time demographic information has been released.
More than half of marketplace enrollees are between ages 45 and 64 years, with 22% aged 45-54 years and 33% in aged 55-64 years.
But HHS officials said they were encouraged by the number of younger Americans who had selected a plan through the marketplace. Young, and presumably healthy enrollees, are considered essential to ensuring a favorable risk mix for insurers. Over the first 3 months of open season, individuals aged 18-34 years made up 24% of enrollees. In comparison, 18-34 year olds make up 26% of the U.S. population under age 65 years.
"We think that more and more young people are going to sign up as time goes by, which was the experience in Massachusetts," Gary Cohen, director of the Center for Consumer Information and Insurance Oversight at the Centers for Medicare and Medicaid Services, said during the press briefing.
Overall, enrollment in health plans surged in December, outstripping the slow start of the online insurance marketplaces in October. The number of people enrolling in a health plan through the marketplaces, which HHS defines as selecting but not necessarily paying for a plan, was more than 1.7 million in December alone, up from about 364,000 in October and November.
Another 1.6 million Americans were deemed eligible for Medicaid or the Children’s Health Insurance Program through the marketplaces from Oct. 1 through Dec. 28, according to the report. That figure does not include individuals who applied to the program directly through their state agencies.
Most enrollees selected plans with lower premiums and higher out-of-pocket costs. A total of 60% selected a "silver" plan and another 20% selected a "bronze" plan.
Most enrollees (79%) are receiving some type of financial assistance in paying their premiums, according to the HHS report.
Nearly 2.2 million Americans enrolled in private health plans through federally or state-run insurance marketplaces during the first 3 months of the Affordable Care Act’s open enrollment period, nearly a quarter of whom are aged 18-34 years, according to figures released Jan. 13 by the Health and Human Services department.
"The numbers show that there is a very strong national demand for affordable health care made possible by the Affordable Care Act," Kathleen Sebelius, HHS secretary, said during a press briefing. "Among young adults, the momentum was particularly strong."
More women (54%) than men (46%) enrolled in a health care plan, according to preliminary demographic data provided by HHS. This is the first time demographic information has been released.
More than half of marketplace enrollees are between ages 45 and 64 years, with 22% aged 45-54 years and 33% in aged 55-64 years.
But HHS officials said they were encouraged by the number of younger Americans who had selected a plan through the marketplace. Young, and presumably healthy enrollees, are considered essential to ensuring a favorable risk mix for insurers. Over the first 3 months of open season, individuals aged 18-34 years made up 24% of enrollees. In comparison, 18-34 year olds make up 26% of the U.S. population under age 65 years.
"We think that more and more young people are going to sign up as time goes by, which was the experience in Massachusetts," Gary Cohen, director of the Center for Consumer Information and Insurance Oversight at the Centers for Medicare and Medicaid Services, said during the press briefing.
Overall, enrollment in health plans surged in December, outstripping the slow start of the online insurance marketplaces in October. The number of people enrolling in a health plan through the marketplaces, which HHS defines as selecting but not necessarily paying for a plan, was more than 1.7 million in December alone, up from about 364,000 in October and November.
Another 1.6 million Americans were deemed eligible for Medicaid or the Children’s Health Insurance Program through the marketplaces from Oct. 1 through Dec. 28, according to the report. That figure does not include individuals who applied to the program directly through their state agencies.
Most enrollees selected plans with lower premiums and higher out-of-pocket costs. A total of 60% selected a "silver" plan and another 20% selected a "bronze" plan.
Most enrollees (79%) are receiving some type of financial assistance in paying their premiums, according to the HHS report.
Make the most of nonopioids: Managing acute pain in children
ORLANDO – Effective management of acute pain in children is important not only for improving comfort, but also for improving outcomes, according to Dr. Joseph D. Tobias.
"The important thing to realize is that there are many benefits (of pain management). Although we walk a fine line between adverse effects and benefits, many times with adequate analgesia we put patients in a better place, Dr. Tobias, chief of anesthesiology and pain medicine at Nationwide Children’s Hospital in Columbus, Ohio, said at the annual meeting of the American Academy of Pediatrics.
That’s because with inadequate analgesia there are a host of humoral factors, including increased endogenous catecholamines, that have adverse physiologic effects on oxygen consumption, CO2 production, and on the immune system, he explained.
Multiple studies have demonstrated that aggressive pain management has beneficial immune effects, he added, noting that patients with adequate pain management are less likely to experience infections and that neonates and infants without adequate pain management may experience chronic pain and pain syndromes later in life because of the neuroplasticity of the infant brain.
He recommends the classic "stepwise ladder" approach to pain management in pediatric patients with acute pain following surgery, trauma, or acute illness, for example. Step 1 involves administration of nonopioids and adjuvants.
"But even as we move to step 2 and add opioids, it’s very important to keep the nonopioids and adjuvants going. I don’t think anybody should ever be in the hospital on [patient-controlled analgesia] getting opioids and not getting nonsteroidal [drugs], acetaminophen, and other adjuvants, because what you’re going to do is decrease your opioid requirements, and as you do that, you then decrease opioid-related side effects," he said.
Keep in mind that the maximum dose of oral or rectal acetaminophen has been decreased from 4 to 3 grams, he said, noting that reports of significant toxicity with acetaminophen have been increasing, so it is important to limit the dose.
The same holds true for the new intravenous preparation of acetaminophen, given reports of 10-fold overdose (10 mg/mL concentration).
"We need to be cognizant of that," he said.
A number of salicylates and NSAIDs are also available for use in children. Ibuprofen is among the most commonly used, and also is now available in an intravenous formulation.
Ketorolac is another good treatment option, but intravenous acetaminophen is preferable in children under age 1 year, because of concerns regarding decreased renal perfusion, he said.
Other emerging options that are making their way from the adult to the pediatric pain-management arena are ketamine, gabapentin and pregabalin, dexamethasone, and dexmedetomidine, all of which appear to have some potential benefits for improving pain management and reducing the need for opioids.
Watch for interactions and adverse effects
Be sure to assess for potential drug interactions in children on several medications and to protect against the adverse gastrointestinal tract effects of nonsteroidal drugs, Dr. Tobias advised.
"If you’re using nonsteroidals, especially postoperatively in patients, it’s always a good idea to combine them with a proton pump inhibitor, or an H2 antagonist," he said, noting that that these can generally be discontinued once the patient is tolerating a regular diet.
Effects on renal function are also an important concern, particularly in those with preexisting renal dysfunction, concomitant use of other nephrotoxic agents, hypovolemia, hypoperfusion, and prolonged administration.
Bleeding is another concern, particularly in those receiving ketorolac, which shouldn’t be used in children undergoing tonsillectomy or in other cases involving increased bleeding risk, he said.
As for opioids, morphine and hydromorphone are the most commonly used in children, accounting for about 99% of usage.
Morphine is more often associated with pruritus in older children and adolescents, so hydromorphone may be a better option to start with in these patients.
"As far as dosing guidelines, I think it’s very important to adjust the dose based on the patient’s status and follow pain scores. I think everybody in the hospital needs to have their pain score checked. It doesn’t matter which (pain scale) you use," Dr. Tobias said.
Also, a steady-state serum concentration should be maintained with avoidance of peaks and troughs, and patients on opioids should be monitored for adverse effects, he said, noting that patient-controlled analgesia (PCA) devices are useful – after a loading dose – to maintain those concentrations. PCA devices can be used by children as young as 5 or 6 years of age; nurse-controlled analgesia is best for those who are younger or have cognitive impairment.
A lower basal infusion rate (4-5 mcg/kg per hour) allows for better sleep while reducing side effects, he said.
Among the concerning side effects of opioids are constipation and respiratory depression.
"Remember, you develop tolerance least quickly to their effects on the GI tract ... when you’re sending kids home from the hospital on opioids, make sure you focus on their bowel habits, or they’re going to be back, they’re going to be constipated, they’re not going to be ambulating, they may not be as well hydrated, so we really need to focus on the GI tract," he said.
Respiratory depression is recognized as an increasing concern.
"When these kids are getting PCA on the floor, make sure you have ready access to resuscitation equipment should you need it," he said.
"Especially as the population gets bigger, we may have more undiagnosed OSA [obstructive sleep apnea], so all of our patients get their respiratory rates checked, they’re on pulse oximetry. In really high-risk patients, we’re using end tidal transcutaneous CO2 monitoring," he said, adding: "Remember, hypoxemia is a late finding of opioid-related respiratory depression. You’re going to see a slight elevation in carbon dioxide first."
Adverse effects are most common in those at the extremes of age, in those with underlying systemic diseases, and in those receiving other agents that are central nervous system depressants.
Of course, the best way to limit side effects is to use adjunctive agents, Dr. Tobias said.
"Maximize the use of nonsteroidals and acetaminophen, and you’re going to use a lot less opioid," he said.
Another important approach to reducing opioid use is the perioperative use of regional anesthesia.
"If you’re working in the hospital taking care of kids after major surgical procedures, I think if you partner with the anesthesia team there’s a lot you can do perioperatively to almost eliminate the need for intravenous opioids," he said.
For a femur fracture patient, for example, a catheter can be placed near the femoral nerve to provide analgesia, or the lateral femoral cutaneous nerve can be blocked. Ultrasound has "really opened the door for regional anesthesia."
Home infusion devices are also available.
"So if you’re having your anterior cruciate ligament repaired, where I work, you’re going to go home with a femoral nerve catheter and a home infusion device that will work for 3 days and really limit your need for parenteral and oral opioids," he said.
Outside of the operating room, regional anesthesia can be used to treat pain that is unresponsive to opioids or if the opioids are causing side effects. Cases involving sickle cell vaso-occlusive crisis, multiple trauma, or burns are scenarios in which regional anesthesia can be particularly useful, he said.
Dr. Tobias reported having no disclosures.
ORLANDO – Effective management of acute pain in children is important not only for improving comfort, but also for improving outcomes, according to Dr. Joseph D. Tobias.
"The important thing to realize is that there are many benefits (of pain management). Although we walk a fine line between adverse effects and benefits, many times with adequate analgesia we put patients in a better place, Dr. Tobias, chief of anesthesiology and pain medicine at Nationwide Children’s Hospital in Columbus, Ohio, said at the annual meeting of the American Academy of Pediatrics.
That’s because with inadequate analgesia there are a host of humoral factors, including increased endogenous catecholamines, that have adverse physiologic effects on oxygen consumption, CO2 production, and on the immune system, he explained.
Multiple studies have demonstrated that aggressive pain management has beneficial immune effects, he added, noting that patients with adequate pain management are less likely to experience infections and that neonates and infants without adequate pain management may experience chronic pain and pain syndromes later in life because of the neuroplasticity of the infant brain.
He recommends the classic "stepwise ladder" approach to pain management in pediatric patients with acute pain following surgery, trauma, or acute illness, for example. Step 1 involves administration of nonopioids and adjuvants.
"But even as we move to step 2 and add opioids, it’s very important to keep the nonopioids and adjuvants going. I don’t think anybody should ever be in the hospital on [patient-controlled analgesia] getting opioids and not getting nonsteroidal [drugs], acetaminophen, and other adjuvants, because what you’re going to do is decrease your opioid requirements, and as you do that, you then decrease opioid-related side effects," he said.
Keep in mind that the maximum dose of oral or rectal acetaminophen has been decreased from 4 to 3 grams, he said, noting that reports of significant toxicity with acetaminophen have been increasing, so it is important to limit the dose.
The same holds true for the new intravenous preparation of acetaminophen, given reports of 10-fold overdose (10 mg/mL concentration).
"We need to be cognizant of that," he said.
A number of salicylates and NSAIDs are also available for use in children. Ibuprofen is among the most commonly used, and also is now available in an intravenous formulation.
Ketorolac is another good treatment option, but intravenous acetaminophen is preferable in children under age 1 year, because of concerns regarding decreased renal perfusion, he said.
Other emerging options that are making their way from the adult to the pediatric pain-management arena are ketamine, gabapentin and pregabalin, dexamethasone, and dexmedetomidine, all of which appear to have some potential benefits for improving pain management and reducing the need for opioids.
Watch for interactions and adverse effects
Be sure to assess for potential drug interactions in children on several medications and to protect against the adverse gastrointestinal tract effects of nonsteroidal drugs, Dr. Tobias advised.
"If you’re using nonsteroidals, especially postoperatively in patients, it’s always a good idea to combine them with a proton pump inhibitor, or an H2 antagonist," he said, noting that that these can generally be discontinued once the patient is tolerating a regular diet.
Effects on renal function are also an important concern, particularly in those with preexisting renal dysfunction, concomitant use of other nephrotoxic agents, hypovolemia, hypoperfusion, and prolonged administration.
Bleeding is another concern, particularly in those receiving ketorolac, which shouldn’t be used in children undergoing tonsillectomy or in other cases involving increased bleeding risk, he said.
As for opioids, morphine and hydromorphone are the most commonly used in children, accounting for about 99% of usage.
Morphine is more often associated with pruritus in older children and adolescents, so hydromorphone may be a better option to start with in these patients.
"As far as dosing guidelines, I think it’s very important to adjust the dose based on the patient’s status and follow pain scores. I think everybody in the hospital needs to have their pain score checked. It doesn’t matter which (pain scale) you use," Dr. Tobias said.
Also, a steady-state serum concentration should be maintained with avoidance of peaks and troughs, and patients on opioids should be monitored for adverse effects, he said, noting that patient-controlled analgesia (PCA) devices are useful – after a loading dose – to maintain those concentrations. PCA devices can be used by children as young as 5 or 6 years of age; nurse-controlled analgesia is best for those who are younger or have cognitive impairment.
A lower basal infusion rate (4-5 mcg/kg per hour) allows for better sleep while reducing side effects, he said.
Among the concerning side effects of opioids are constipation and respiratory depression.
"Remember, you develop tolerance least quickly to their effects on the GI tract ... when you’re sending kids home from the hospital on opioids, make sure you focus on their bowel habits, or they’re going to be back, they’re going to be constipated, they’re not going to be ambulating, they may not be as well hydrated, so we really need to focus on the GI tract," he said.
Respiratory depression is recognized as an increasing concern.
"When these kids are getting PCA on the floor, make sure you have ready access to resuscitation equipment should you need it," he said.
"Especially as the population gets bigger, we may have more undiagnosed OSA [obstructive sleep apnea], so all of our patients get their respiratory rates checked, they’re on pulse oximetry. In really high-risk patients, we’re using end tidal transcutaneous CO2 monitoring," he said, adding: "Remember, hypoxemia is a late finding of opioid-related respiratory depression. You’re going to see a slight elevation in carbon dioxide first."
Adverse effects are most common in those at the extremes of age, in those with underlying systemic diseases, and in those receiving other agents that are central nervous system depressants.
Of course, the best way to limit side effects is to use adjunctive agents, Dr. Tobias said.
"Maximize the use of nonsteroidals and acetaminophen, and you’re going to use a lot less opioid," he said.
Another important approach to reducing opioid use is the perioperative use of regional anesthesia.
"If you’re working in the hospital taking care of kids after major surgical procedures, I think if you partner with the anesthesia team there’s a lot you can do perioperatively to almost eliminate the need for intravenous opioids," he said.
For a femur fracture patient, for example, a catheter can be placed near the femoral nerve to provide analgesia, or the lateral femoral cutaneous nerve can be blocked. Ultrasound has "really opened the door for regional anesthesia."
Home infusion devices are also available.
"So if you’re having your anterior cruciate ligament repaired, where I work, you’re going to go home with a femoral nerve catheter and a home infusion device that will work for 3 days and really limit your need for parenteral and oral opioids," he said.
Outside of the operating room, regional anesthesia can be used to treat pain that is unresponsive to opioids or if the opioids are causing side effects. Cases involving sickle cell vaso-occlusive crisis, multiple trauma, or burns are scenarios in which regional anesthesia can be particularly useful, he said.
Dr. Tobias reported having no disclosures.
ORLANDO – Effective management of acute pain in children is important not only for improving comfort, but also for improving outcomes, according to Dr. Joseph D. Tobias.
"The important thing to realize is that there are many benefits (of pain management). Although we walk a fine line between adverse effects and benefits, many times with adequate analgesia we put patients in a better place, Dr. Tobias, chief of anesthesiology and pain medicine at Nationwide Children’s Hospital in Columbus, Ohio, said at the annual meeting of the American Academy of Pediatrics.
That’s because with inadequate analgesia there are a host of humoral factors, including increased endogenous catecholamines, that have adverse physiologic effects on oxygen consumption, CO2 production, and on the immune system, he explained.
Multiple studies have demonstrated that aggressive pain management has beneficial immune effects, he added, noting that patients with adequate pain management are less likely to experience infections and that neonates and infants without adequate pain management may experience chronic pain and pain syndromes later in life because of the neuroplasticity of the infant brain.
He recommends the classic "stepwise ladder" approach to pain management in pediatric patients with acute pain following surgery, trauma, or acute illness, for example. Step 1 involves administration of nonopioids and adjuvants.
"But even as we move to step 2 and add opioids, it’s very important to keep the nonopioids and adjuvants going. I don’t think anybody should ever be in the hospital on [patient-controlled analgesia] getting opioids and not getting nonsteroidal [drugs], acetaminophen, and other adjuvants, because what you’re going to do is decrease your opioid requirements, and as you do that, you then decrease opioid-related side effects," he said.
Keep in mind that the maximum dose of oral or rectal acetaminophen has been decreased from 4 to 3 grams, he said, noting that reports of significant toxicity with acetaminophen have been increasing, so it is important to limit the dose.
The same holds true for the new intravenous preparation of acetaminophen, given reports of 10-fold overdose (10 mg/mL concentration).
"We need to be cognizant of that," he said.
A number of salicylates and NSAIDs are also available for use in children. Ibuprofen is among the most commonly used, and also is now available in an intravenous formulation.
Ketorolac is another good treatment option, but intravenous acetaminophen is preferable in children under age 1 year, because of concerns regarding decreased renal perfusion, he said.
Other emerging options that are making their way from the adult to the pediatric pain-management arena are ketamine, gabapentin and pregabalin, dexamethasone, and dexmedetomidine, all of which appear to have some potential benefits for improving pain management and reducing the need for opioids.
Watch for interactions and adverse effects
Be sure to assess for potential drug interactions in children on several medications and to protect against the adverse gastrointestinal tract effects of nonsteroidal drugs, Dr. Tobias advised.
"If you’re using nonsteroidals, especially postoperatively in patients, it’s always a good idea to combine them with a proton pump inhibitor, or an H2 antagonist," he said, noting that that these can generally be discontinued once the patient is tolerating a regular diet.
Effects on renal function are also an important concern, particularly in those with preexisting renal dysfunction, concomitant use of other nephrotoxic agents, hypovolemia, hypoperfusion, and prolonged administration.
Bleeding is another concern, particularly in those receiving ketorolac, which shouldn’t be used in children undergoing tonsillectomy or in other cases involving increased bleeding risk, he said.
As for opioids, morphine and hydromorphone are the most commonly used in children, accounting for about 99% of usage.
Morphine is more often associated with pruritus in older children and adolescents, so hydromorphone may be a better option to start with in these patients.
"As far as dosing guidelines, I think it’s very important to adjust the dose based on the patient’s status and follow pain scores. I think everybody in the hospital needs to have their pain score checked. It doesn’t matter which (pain scale) you use," Dr. Tobias said.
Also, a steady-state serum concentration should be maintained with avoidance of peaks and troughs, and patients on opioids should be monitored for adverse effects, he said, noting that patient-controlled analgesia (PCA) devices are useful – after a loading dose – to maintain those concentrations. PCA devices can be used by children as young as 5 or 6 years of age; nurse-controlled analgesia is best for those who are younger or have cognitive impairment.
A lower basal infusion rate (4-5 mcg/kg per hour) allows for better sleep while reducing side effects, he said.
Among the concerning side effects of opioids are constipation and respiratory depression.
"Remember, you develop tolerance least quickly to their effects on the GI tract ... when you’re sending kids home from the hospital on opioids, make sure you focus on their bowel habits, or they’re going to be back, they’re going to be constipated, they’re not going to be ambulating, they may not be as well hydrated, so we really need to focus on the GI tract," he said.
Respiratory depression is recognized as an increasing concern.
"When these kids are getting PCA on the floor, make sure you have ready access to resuscitation equipment should you need it," he said.
"Especially as the population gets bigger, we may have more undiagnosed OSA [obstructive sleep apnea], so all of our patients get their respiratory rates checked, they’re on pulse oximetry. In really high-risk patients, we’re using end tidal transcutaneous CO2 monitoring," he said, adding: "Remember, hypoxemia is a late finding of opioid-related respiratory depression. You’re going to see a slight elevation in carbon dioxide first."
Adverse effects are most common in those at the extremes of age, in those with underlying systemic diseases, and in those receiving other agents that are central nervous system depressants.
Of course, the best way to limit side effects is to use adjunctive agents, Dr. Tobias said.
"Maximize the use of nonsteroidals and acetaminophen, and you’re going to use a lot less opioid," he said.
Another important approach to reducing opioid use is the perioperative use of regional anesthesia.
"If you’re working in the hospital taking care of kids after major surgical procedures, I think if you partner with the anesthesia team there’s a lot you can do perioperatively to almost eliminate the need for intravenous opioids," he said.
For a femur fracture patient, for example, a catheter can be placed near the femoral nerve to provide analgesia, or the lateral femoral cutaneous nerve can be blocked. Ultrasound has "really opened the door for regional anesthesia."
Home infusion devices are also available.
"So if you’re having your anterior cruciate ligament repaired, where I work, you’re going to go home with a femoral nerve catheter and a home infusion device that will work for 3 days and really limit your need for parenteral and oral opioids," he said.
Outside of the operating room, regional anesthesia can be used to treat pain that is unresponsive to opioids or if the opioids are causing side effects. Cases involving sickle cell vaso-occlusive crisis, multiple trauma, or burns are scenarios in which regional anesthesia can be particularly useful, he said.
Dr. Tobias reported having no disclosures.
EXPERT ANALYSIS AT THE AAP NATIONAL CONFERENCE