User login
Official Newspaper of the American College of Surgeons
Medicare takes aim at ‘abusive’ prescribing
Medicare officials are seeking new authority to allow them to kick out physicians who engage in "abusive" prescribing practices, according to a newly released proposed rule.
The Centers for Medicare and Medicaid Services (CMS) issued a proposal Jan. 6 with several provisions aimed at rooting out fraud and abuse by physicians. The rule is part of a larger effort to identify Medicare beneficiaries who are potentially overusing opioids, as well as identify prescribers and pharmacies that may be involved in fraudulent activities.
Beginning next year, the proposal would require Medicare Part D prescription drug plans to deny coverage for any drug claim that does not include a prescriber’s National Provider Identifier (NPI). Under the rule, physicians are not required to accept Medicare payments, but they must be enrolled in the program in an approved status or have a valid opt-out affidavit on file with the Medicare fee-for-service program.
The aim, according to CMS, is to ensure that anyone prescribing drugs to Medicare beneficiaries is properly qualified. The Affordable Care Act already requires physicians to be enrolled in the Medicare program for durable medical equipment, prosthetics, orthotics, and supplies, or if they certify home health care for Medicare beneficiaries.
Medicare officials also noted in the proposed rule that they want the right to revoke a physician’s Medicare enrollment if the physician exhibits a pattern of prescribing Part D drugs that is "abusive and represents a threat to the health and safety of Medicare beneficiaries." The agency also would be able to revoke Medicare enrollment if a physician’s Drug Enforcement Administration Certificate of Registration was suspended or revoked, or their state medical license was suspended or revoked.
The decision to revoke enrollment would only be made after a thorough and detailed investigation by CMS, according to the proposed rule.
"Honest physicians and eligible professionals who engage in reasonable prescribing activities would not be impacted by our proposal," the proposed rule states.
But the proposed rule does not define "abusive" or "threat to the health and safety of Medicare beneficiaries."
Instead, it includes a list of criteria for assessing prescribing practices:
• Are there diagnoses to support the indications for which the drugs were prescribed?
• Was the patient deceased or out of state at the time of an alleged office visit?
• Has the physician prescribed controlled substances in excessive dosages linked to patient overdoses?
• Has the physician been subject to disciplinary actions by the state medical board?
• Has the physician been sued for malpractice related to their drug prescribing and been found liable or paid a settlement?
• Has a public insurance program restricted or revoked the physician’s prescribing privileges?
Dr. Ardis Dee Hoven, president of the American Medical Association, said the organization has a zero tolerance policy for irresponsible prescribing that could harm patients and that the proposal is unlikely to affect physicians who are prescribing appropriately.
"The vast majority of physicians who appropriately and safely prescribe medications should not be targets of misguided government enforcement and driven out of practice," she said. "The AMA is carefully examining the details of the newly proposed rule to ensure the [CMS] does not compromise appropriate prescribing or exceed its statutory authority."
But CMS officials will need more data if they plan to identify fraud and abuse by physicians and beneficiaries. As a result, the agency is also proposing to collect information directly from pharmacy benefit managers, pharmacies, and others that contract with Part D drugs plans, rather than going through the drug plan for the information
The proposed rule will be published in the Federal Register on Jan. 10. The agency is accepting public comments at www.regulations.gov until March 7.
Medicare officials are seeking new authority to allow them to kick out physicians who engage in "abusive" prescribing practices, according to a newly released proposed rule.
The Centers for Medicare and Medicaid Services (CMS) issued a proposal Jan. 6 with several provisions aimed at rooting out fraud and abuse by physicians. The rule is part of a larger effort to identify Medicare beneficiaries who are potentially overusing opioids, as well as identify prescribers and pharmacies that may be involved in fraudulent activities.
Beginning next year, the proposal would require Medicare Part D prescription drug plans to deny coverage for any drug claim that does not include a prescriber’s National Provider Identifier (NPI). Under the rule, physicians are not required to accept Medicare payments, but they must be enrolled in the program in an approved status or have a valid opt-out affidavit on file with the Medicare fee-for-service program.
The aim, according to CMS, is to ensure that anyone prescribing drugs to Medicare beneficiaries is properly qualified. The Affordable Care Act already requires physicians to be enrolled in the Medicare program for durable medical equipment, prosthetics, orthotics, and supplies, or if they certify home health care for Medicare beneficiaries.
Medicare officials also noted in the proposed rule that they want the right to revoke a physician’s Medicare enrollment if the physician exhibits a pattern of prescribing Part D drugs that is "abusive and represents a threat to the health and safety of Medicare beneficiaries." The agency also would be able to revoke Medicare enrollment if a physician’s Drug Enforcement Administration Certificate of Registration was suspended or revoked, or their state medical license was suspended or revoked.
The decision to revoke enrollment would only be made after a thorough and detailed investigation by CMS, according to the proposed rule.
"Honest physicians and eligible professionals who engage in reasonable prescribing activities would not be impacted by our proposal," the proposed rule states.
But the proposed rule does not define "abusive" or "threat to the health and safety of Medicare beneficiaries."
Instead, it includes a list of criteria for assessing prescribing practices:
• Are there diagnoses to support the indications for which the drugs were prescribed?
• Was the patient deceased or out of state at the time of an alleged office visit?
• Has the physician prescribed controlled substances in excessive dosages linked to patient overdoses?
• Has the physician been subject to disciplinary actions by the state medical board?
• Has the physician been sued for malpractice related to their drug prescribing and been found liable or paid a settlement?
• Has a public insurance program restricted or revoked the physician’s prescribing privileges?
Dr. Ardis Dee Hoven, president of the American Medical Association, said the organization has a zero tolerance policy for irresponsible prescribing that could harm patients and that the proposal is unlikely to affect physicians who are prescribing appropriately.
"The vast majority of physicians who appropriately and safely prescribe medications should not be targets of misguided government enforcement and driven out of practice," she said. "The AMA is carefully examining the details of the newly proposed rule to ensure the [CMS] does not compromise appropriate prescribing or exceed its statutory authority."
But CMS officials will need more data if they plan to identify fraud and abuse by physicians and beneficiaries. As a result, the agency is also proposing to collect information directly from pharmacy benefit managers, pharmacies, and others that contract with Part D drugs plans, rather than going through the drug plan for the information
The proposed rule will be published in the Federal Register on Jan. 10. The agency is accepting public comments at www.regulations.gov until March 7.
Medicare officials are seeking new authority to allow them to kick out physicians who engage in "abusive" prescribing practices, according to a newly released proposed rule.
The Centers for Medicare and Medicaid Services (CMS) issued a proposal Jan. 6 with several provisions aimed at rooting out fraud and abuse by physicians. The rule is part of a larger effort to identify Medicare beneficiaries who are potentially overusing opioids, as well as identify prescribers and pharmacies that may be involved in fraudulent activities.
Beginning next year, the proposal would require Medicare Part D prescription drug plans to deny coverage for any drug claim that does not include a prescriber’s National Provider Identifier (NPI). Under the rule, physicians are not required to accept Medicare payments, but they must be enrolled in the program in an approved status or have a valid opt-out affidavit on file with the Medicare fee-for-service program.
The aim, according to CMS, is to ensure that anyone prescribing drugs to Medicare beneficiaries is properly qualified. The Affordable Care Act already requires physicians to be enrolled in the Medicare program for durable medical equipment, prosthetics, orthotics, and supplies, or if they certify home health care for Medicare beneficiaries.
Medicare officials also noted in the proposed rule that they want the right to revoke a physician’s Medicare enrollment if the physician exhibits a pattern of prescribing Part D drugs that is "abusive and represents a threat to the health and safety of Medicare beneficiaries." The agency also would be able to revoke Medicare enrollment if a physician’s Drug Enforcement Administration Certificate of Registration was suspended or revoked, or their state medical license was suspended or revoked.
The decision to revoke enrollment would only be made after a thorough and detailed investigation by CMS, according to the proposed rule.
"Honest physicians and eligible professionals who engage in reasonable prescribing activities would not be impacted by our proposal," the proposed rule states.
But the proposed rule does not define "abusive" or "threat to the health and safety of Medicare beneficiaries."
Instead, it includes a list of criteria for assessing prescribing practices:
• Are there diagnoses to support the indications for which the drugs were prescribed?
• Was the patient deceased or out of state at the time of an alleged office visit?
• Has the physician prescribed controlled substances in excessive dosages linked to patient overdoses?
• Has the physician been subject to disciplinary actions by the state medical board?
• Has the physician been sued for malpractice related to their drug prescribing and been found liable or paid a settlement?
• Has a public insurance program restricted or revoked the physician’s prescribing privileges?
Dr. Ardis Dee Hoven, president of the American Medical Association, said the organization has a zero tolerance policy for irresponsible prescribing that could harm patients and that the proposal is unlikely to affect physicians who are prescribing appropriately.
"The vast majority of physicians who appropriately and safely prescribe medications should not be targets of misguided government enforcement and driven out of practice," she said. "The AMA is carefully examining the details of the newly proposed rule to ensure the [CMS] does not compromise appropriate prescribing or exceed its statutory authority."
But CMS officials will need more data if they plan to identify fraud and abuse by physicians and beneficiaries. As a result, the agency is also proposing to collect information directly from pharmacy benefit managers, pharmacies, and others that contract with Part D drugs plans, rather than going through the drug plan for the information
The proposed rule will be published in the Federal Register on Jan. 10. The agency is accepting public comments at www.regulations.gov until March 7.
Extracorporeal shock wave therapy promising for lymphedema
SAN ANTONIO – Extracorporeal shock wave therapy shows early promise for limiting the often-vexing problem of lymphedema arising after axillary lymphadenectomy.
In the first 10 affected patients treated in an ongoing randomized, sham-controlled clinical trial, lymphedema, as measured by median whole-arm water displacement, dropped from 4,200 mL at baseline by 192.5 mL after 10 once-weekly extracorporeal shock wave (ECSW) sessions. Patients who received sham sessions had a 12.5-mL decline from baseline measures, Dr. Sara Imboden reported at the San Antonio Breast Cancer Symposium.
Quantitative CT measures indicated the mean total cross-sectional area of the most swollen part of the arm decreased by 3% in the ECSW group, compared with 1.4% in the control group, added Dr. Imboden of the University of Bern (Switzerland).
A mean of 22 axillary lymph nodes had been removed from the breast cancer patients in the study. The ECSW therapy was performed over the length of the edematous arm at an energy density of 0.25-0.69 mJ/mm2 once per week for 10 weeks. The control group followed the same treatment schedule, but the shock waves were contained inside the probe during their sessions.
None of the patients had to interrupt ECSW therapy due to complications.
The researchers plan to expand the randomized trial to include 30 patients, and to augment the results with patient reports of symptoms based on questionnaires assessing body image and with extended follow-up to evaluate functioning and recurrences.
The likely mechanism of benefit in patients with lymphedema involves ECSW-induced stimulation of angiogenesis and lymphatic vessel regeneration. These results have been demonstrated in animal studies.
No medications have been shown effective in treating lymphedema. Conventional therapy entails repeated manual lymph drainage and compression bandages.
Dr. Imboden reported having no financial conflicts of interest with regard to this university-funded study.
SAN ANTONIO – Extracorporeal shock wave therapy shows early promise for limiting the often-vexing problem of lymphedema arising after axillary lymphadenectomy.
In the first 10 affected patients treated in an ongoing randomized, sham-controlled clinical trial, lymphedema, as measured by median whole-arm water displacement, dropped from 4,200 mL at baseline by 192.5 mL after 10 once-weekly extracorporeal shock wave (ECSW) sessions. Patients who received sham sessions had a 12.5-mL decline from baseline measures, Dr. Sara Imboden reported at the San Antonio Breast Cancer Symposium.
Quantitative CT measures indicated the mean total cross-sectional area of the most swollen part of the arm decreased by 3% in the ECSW group, compared with 1.4% in the control group, added Dr. Imboden of the University of Bern (Switzerland).
A mean of 22 axillary lymph nodes had been removed from the breast cancer patients in the study. The ECSW therapy was performed over the length of the edematous arm at an energy density of 0.25-0.69 mJ/mm2 once per week for 10 weeks. The control group followed the same treatment schedule, but the shock waves were contained inside the probe during their sessions.
None of the patients had to interrupt ECSW therapy due to complications.
The researchers plan to expand the randomized trial to include 30 patients, and to augment the results with patient reports of symptoms based on questionnaires assessing body image and with extended follow-up to evaluate functioning and recurrences.
The likely mechanism of benefit in patients with lymphedema involves ECSW-induced stimulation of angiogenesis and lymphatic vessel regeneration. These results have been demonstrated in animal studies.
No medications have been shown effective in treating lymphedema. Conventional therapy entails repeated manual lymph drainage and compression bandages.
Dr. Imboden reported having no financial conflicts of interest with regard to this university-funded study.
SAN ANTONIO – Extracorporeal shock wave therapy shows early promise for limiting the often-vexing problem of lymphedema arising after axillary lymphadenectomy.
In the first 10 affected patients treated in an ongoing randomized, sham-controlled clinical trial, lymphedema, as measured by median whole-arm water displacement, dropped from 4,200 mL at baseline by 192.5 mL after 10 once-weekly extracorporeal shock wave (ECSW) sessions. Patients who received sham sessions had a 12.5-mL decline from baseline measures, Dr. Sara Imboden reported at the San Antonio Breast Cancer Symposium.
Quantitative CT measures indicated the mean total cross-sectional area of the most swollen part of the arm decreased by 3% in the ECSW group, compared with 1.4% in the control group, added Dr. Imboden of the University of Bern (Switzerland).
A mean of 22 axillary lymph nodes had been removed from the breast cancer patients in the study. The ECSW therapy was performed over the length of the edematous arm at an energy density of 0.25-0.69 mJ/mm2 once per week for 10 weeks. The control group followed the same treatment schedule, but the shock waves were contained inside the probe during their sessions.
None of the patients had to interrupt ECSW therapy due to complications.
The researchers plan to expand the randomized trial to include 30 patients, and to augment the results with patient reports of symptoms based on questionnaires assessing body image and with extended follow-up to evaluate functioning and recurrences.
The likely mechanism of benefit in patients with lymphedema involves ECSW-induced stimulation of angiogenesis and lymphatic vessel regeneration. These results have been demonstrated in animal studies.
No medications have been shown effective in treating lymphedema. Conventional therapy entails repeated manual lymph drainage and compression bandages.
Dr. Imboden reported having no financial conflicts of interest with regard to this university-funded study.
AT SABCS 2013
Major finding: Women with lymphedema following axillary lymphadenectomy had a median 192.5-mL reduction in whole-arm water volume displacement following 10 weekly sessions of extracorporeal shock wave therapy. Controls who underwent sham therapy had a modest 12.5-mL decrease.
Data source: This is an interim report on the first 10 patients in a planned 30-patient, randomized, sham-controlled trial.
Disclosures: Dr. Imboden reported having no financial conflicts of interest with regard to this university-funded study.
FDA approves two-drug combination for advanced melanoma
A combination of two targeted, orally administered drug therapies – trametinib and dabrafenib – has been approved by the Food and Drug Administration for treating patients with unresectable melanoma or metastatic melanoma with BRAF V600E or V600K mutations, manufacturer GlaxoSmithKline announced on Jan. 9.
An FDA-approved test is used to detect the mutations, according to the company statement.
Trametinib, marketed as Mekinist, and dabrafenib, marketed as Tafinlar, were each approved in May 2013 as separate treatments for metastatic or unresectable melanomas that express the mutations – along with a companion test to detect the mutations. Both are kinase inhibitors.
The GSK statement noted that the accelerated approval of the combination therapy is based on the response rate and median duration of response results in a phase I/II study of 108 patients, which compared the combination (150 mg of dabrafenib twice a day and 2 mg of trametinib once a day) to treatment with dabrafenib alone. The overall response rates, as assessed by the investigators, were 76% among those on the combination and 54% for those on dabrafenib alone. The median duration of response was 10.5 months among those on the combination, vs. 5.6 months among those on dabrafenib alone.
The most common adverse events associated with the combination treatment included fever in 71% of patients, chills in 58%, fatigue in 52%, rash in 45%, nausea in 44%, vomiting in 40%, and diarrhea in 36%. Renal failure, pyrexia, back pain, and hemorrhage were among the most common grade-3 or -4 adverse events among those on the combination.
Serious adverse effects associated with treatment, including some potentially fatal effects, are new primary cutaneous skin cancers, tumor promotion in wild-type BRAF melanoma, and hemorrhagic events, according to GSK.
The FDA approval occurred through an accelerated process based on clinical evidence that the treatment has an effect on a surrogate endpoint that is reasonably likely to predict a clinical benefit to patients. As a condition of accelerated approval, manufacturers are required to provide more clinical data confirming benefit, and if the follow-up studies fail to confirm benefit, the FDA can withdraw approval.
Full approval is dependent on the results of an ongoing phase III study, GSK said.
The updated trametinib label states that "improvement in disease-related symptoms or overall survival has not been demonstrated" for the combination treatment.
The prescribing information for Mekinist is available at http://us.gsk.com/products/assets/us_mekinist.pdf. The prescribing information for Tafinlar (which does not yet include the updated information on the combination therapy approval) is available at http://us.gsk.com/products/assets/us_tafinlar.pdf.
A combination of two targeted, orally administered drug therapies – trametinib and dabrafenib – has been approved by the Food and Drug Administration for treating patients with unresectable melanoma or metastatic melanoma with BRAF V600E or V600K mutations, manufacturer GlaxoSmithKline announced on Jan. 9.
An FDA-approved test is used to detect the mutations, according to the company statement.
Trametinib, marketed as Mekinist, and dabrafenib, marketed as Tafinlar, were each approved in May 2013 as separate treatments for metastatic or unresectable melanomas that express the mutations – along with a companion test to detect the mutations. Both are kinase inhibitors.
The GSK statement noted that the accelerated approval of the combination therapy is based on the response rate and median duration of response results in a phase I/II study of 108 patients, which compared the combination (150 mg of dabrafenib twice a day and 2 mg of trametinib once a day) to treatment with dabrafenib alone. The overall response rates, as assessed by the investigators, were 76% among those on the combination and 54% for those on dabrafenib alone. The median duration of response was 10.5 months among those on the combination, vs. 5.6 months among those on dabrafenib alone.
The most common adverse events associated with the combination treatment included fever in 71% of patients, chills in 58%, fatigue in 52%, rash in 45%, nausea in 44%, vomiting in 40%, and diarrhea in 36%. Renal failure, pyrexia, back pain, and hemorrhage were among the most common grade-3 or -4 adverse events among those on the combination.
Serious adverse effects associated with treatment, including some potentially fatal effects, are new primary cutaneous skin cancers, tumor promotion in wild-type BRAF melanoma, and hemorrhagic events, according to GSK.
The FDA approval occurred through an accelerated process based on clinical evidence that the treatment has an effect on a surrogate endpoint that is reasonably likely to predict a clinical benefit to patients. As a condition of accelerated approval, manufacturers are required to provide more clinical data confirming benefit, and if the follow-up studies fail to confirm benefit, the FDA can withdraw approval.
Full approval is dependent on the results of an ongoing phase III study, GSK said.
The updated trametinib label states that "improvement in disease-related symptoms or overall survival has not been demonstrated" for the combination treatment.
The prescribing information for Mekinist is available at http://us.gsk.com/products/assets/us_mekinist.pdf. The prescribing information for Tafinlar (which does not yet include the updated information on the combination therapy approval) is available at http://us.gsk.com/products/assets/us_tafinlar.pdf.
A combination of two targeted, orally administered drug therapies – trametinib and dabrafenib – has been approved by the Food and Drug Administration for treating patients with unresectable melanoma or metastatic melanoma with BRAF V600E or V600K mutations, manufacturer GlaxoSmithKline announced on Jan. 9.
An FDA-approved test is used to detect the mutations, according to the company statement.
Trametinib, marketed as Mekinist, and dabrafenib, marketed as Tafinlar, were each approved in May 2013 as separate treatments for metastatic or unresectable melanomas that express the mutations – along with a companion test to detect the mutations. Both are kinase inhibitors.
The GSK statement noted that the accelerated approval of the combination therapy is based on the response rate and median duration of response results in a phase I/II study of 108 patients, which compared the combination (150 mg of dabrafenib twice a day and 2 mg of trametinib once a day) to treatment with dabrafenib alone. The overall response rates, as assessed by the investigators, were 76% among those on the combination and 54% for those on dabrafenib alone. The median duration of response was 10.5 months among those on the combination, vs. 5.6 months among those on dabrafenib alone.
The most common adverse events associated with the combination treatment included fever in 71% of patients, chills in 58%, fatigue in 52%, rash in 45%, nausea in 44%, vomiting in 40%, and diarrhea in 36%. Renal failure, pyrexia, back pain, and hemorrhage were among the most common grade-3 or -4 adverse events among those on the combination.
Serious adverse effects associated with treatment, including some potentially fatal effects, are new primary cutaneous skin cancers, tumor promotion in wild-type BRAF melanoma, and hemorrhagic events, according to GSK.
The FDA approval occurred through an accelerated process based on clinical evidence that the treatment has an effect on a surrogate endpoint that is reasonably likely to predict a clinical benefit to patients. As a condition of accelerated approval, manufacturers are required to provide more clinical data confirming benefit, and if the follow-up studies fail to confirm benefit, the FDA can withdraw approval.
Full approval is dependent on the results of an ongoing phase III study, GSK said.
The updated trametinib label states that "improvement in disease-related symptoms or overall survival has not been demonstrated" for the combination treatment.
The prescribing information for Mekinist is available at http://us.gsk.com/products/assets/us_mekinist.pdf. The prescribing information for Tafinlar (which does not yet include the updated information on the combination therapy approval) is available at http://us.gsk.com/products/assets/us_tafinlar.pdf.
Two-thirds of women with uterine pathology got pregnant after combined procedure
NATIONAL HARBOR, MD. – More than two-thirds of 30 women with infertility related to uterine pathology achieved pregnancy after a single surgery that combined both hysteroscopy and laparoscopy, a study showed.
"After treatment, many of these patients can achieve pregnancy spontaneously without the use of assisted reproductive technology, and significant cost savings are achieved if the procedures are done at the same time," said Dr. Chris J. Allphin, a gynecologist at the Eastern Idaho Regional Medical Center, Idaho Falls.
The single procedure cost an average of $15,000 less than having sequential procedures.
Dr. Allphin reported a retrospective study of 30 patients treated since 2007 for infertility due to ultrasound-confirmed uterine pathology; 13 women had a uterine septum and 17 had leiomyomata.
Two surgeons simultaneously performed the procedures. Septae were diagnosed laparoscopically and treated with hysteroscopic metroplasty. Leiomyomata were diagnosed laparoscopically and treated with either a hysteroscopic or laparoscopic myomectomy.
Of the 30 patients, 21 women (70%) became pregnant and 5 women conceived twice. Fourteen pregnancies (66%) – including one set of twins – were conceived without assisted reproduction techniques. Four were the result of intrauterine insemination. There were seven in vitro fertilization pregnancies, Dr. Allphin reported at the meeting sponsored by AAGL.
Younger women achieved the best pregnancy rates, with 82% of those younger than 35 years conceiving. The rate was 62% among those aged 35-40 years and 60% in those older than 40 years.
The average cost of having the laparoscopy and hysteroscopy at different admissions is $38,256. The average cost of the dual procedure at a single admission was $23,185. "Thirty patients having the dual procedure saved the system $450,000," according to Dr. Allphin.
Of the nine patients who did not conceive, two had no antral follicles at return to the fertility specialist, two had attempted one in vitro fertilization cycle and then discontinued treatment, one had two intrauterine insemination cycles and then discontinued treatment, three continue to go through in vitro fertilization cycles, and one has postponed trying to conceive.
Dr. Allphin said he had no relevant financial disclosures.
NATIONAL HARBOR, MD. – More than two-thirds of 30 women with infertility related to uterine pathology achieved pregnancy after a single surgery that combined both hysteroscopy and laparoscopy, a study showed.
"After treatment, many of these patients can achieve pregnancy spontaneously without the use of assisted reproductive technology, and significant cost savings are achieved if the procedures are done at the same time," said Dr. Chris J. Allphin, a gynecologist at the Eastern Idaho Regional Medical Center, Idaho Falls.
The single procedure cost an average of $15,000 less than having sequential procedures.
Dr. Allphin reported a retrospective study of 30 patients treated since 2007 for infertility due to ultrasound-confirmed uterine pathology; 13 women had a uterine septum and 17 had leiomyomata.
Two surgeons simultaneously performed the procedures. Septae were diagnosed laparoscopically and treated with hysteroscopic metroplasty. Leiomyomata were diagnosed laparoscopically and treated with either a hysteroscopic or laparoscopic myomectomy.
Of the 30 patients, 21 women (70%) became pregnant and 5 women conceived twice. Fourteen pregnancies (66%) – including one set of twins – were conceived without assisted reproduction techniques. Four were the result of intrauterine insemination. There were seven in vitro fertilization pregnancies, Dr. Allphin reported at the meeting sponsored by AAGL.
Younger women achieved the best pregnancy rates, with 82% of those younger than 35 years conceiving. The rate was 62% among those aged 35-40 years and 60% in those older than 40 years.
The average cost of having the laparoscopy and hysteroscopy at different admissions is $38,256. The average cost of the dual procedure at a single admission was $23,185. "Thirty patients having the dual procedure saved the system $450,000," according to Dr. Allphin.
Of the nine patients who did not conceive, two had no antral follicles at return to the fertility specialist, two had attempted one in vitro fertilization cycle and then discontinued treatment, one had two intrauterine insemination cycles and then discontinued treatment, three continue to go through in vitro fertilization cycles, and one has postponed trying to conceive.
Dr. Allphin said he had no relevant financial disclosures.
NATIONAL HARBOR, MD. – More than two-thirds of 30 women with infertility related to uterine pathology achieved pregnancy after a single surgery that combined both hysteroscopy and laparoscopy, a study showed.
"After treatment, many of these patients can achieve pregnancy spontaneously without the use of assisted reproductive technology, and significant cost savings are achieved if the procedures are done at the same time," said Dr. Chris J. Allphin, a gynecologist at the Eastern Idaho Regional Medical Center, Idaho Falls.
The single procedure cost an average of $15,000 less than having sequential procedures.
Dr. Allphin reported a retrospective study of 30 patients treated since 2007 for infertility due to ultrasound-confirmed uterine pathology; 13 women had a uterine septum and 17 had leiomyomata.
Two surgeons simultaneously performed the procedures. Septae were diagnosed laparoscopically and treated with hysteroscopic metroplasty. Leiomyomata were diagnosed laparoscopically and treated with either a hysteroscopic or laparoscopic myomectomy.
Of the 30 patients, 21 women (70%) became pregnant and 5 women conceived twice. Fourteen pregnancies (66%) – including one set of twins – were conceived without assisted reproduction techniques. Four were the result of intrauterine insemination. There were seven in vitro fertilization pregnancies, Dr. Allphin reported at the meeting sponsored by AAGL.
Younger women achieved the best pregnancy rates, with 82% of those younger than 35 years conceiving. The rate was 62% among those aged 35-40 years and 60% in those older than 40 years.
The average cost of having the laparoscopy and hysteroscopy at different admissions is $38,256. The average cost of the dual procedure at a single admission was $23,185. "Thirty patients having the dual procedure saved the system $450,000," according to Dr. Allphin.
Of the nine patients who did not conceive, two had no antral follicles at return to the fertility specialist, two had attempted one in vitro fertilization cycle and then discontinued treatment, one had two intrauterine insemination cycles and then discontinued treatment, three continue to go through in vitro fertilization cycles, and one has postponed trying to conceive.
Dr. Allphin said he had no relevant financial disclosures.
AT THE AAGL GLOBAL CONGRESS
Major finding: Fourteen pregnancies (66%) – including one set of twins – were conceived without assisted reproduction techniques.
Data source: A retrospective study of 30 patients.
Disclosures: Dr. Allphin said he had no relevant financial disclosures.
Gene panel identifies residual neuroblastoma metastases
BRUSSELS – In advanced-stage neuroblastoma patients with residual metastases in their bone marrow following two cycles of anti-GD2 immunotherapy, another cycle of this treatment is futile and only causes adverse events, based on a review of 343 stage IV patients treated at one U.S. center.
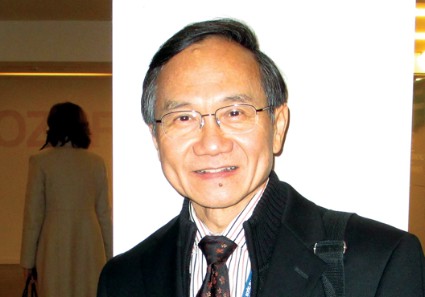
"Bone marrow minimal residual disease [MRD] measured after two cycles of immunotherapy was the strongest predictor of outcome, irrespective of disease status at the start of immunotherapy," Dr. Nai-Kong V. Cheung said at the Markers in Cancer meeting. "If a patient is positive for MRD after two cycles, don’t continue the treatment."
In the series of 343 patients aged 18 months or older with metastatic, stage IV neuroblastoma that he reviewed, all patients with detectable MRD after two cycles of immunotherapy with GD2 antibody eventually relapsed or died within the next 5 years. In contrast, roughly half of the patients who lacked MRD after the first two cycles of anti-GD2 therapy remained progression free and alive during up to 20 years of follow-up.
The full course of anti-GD2 treatment takes 2 years, has the potential to cause adverse effects, and is painful and expensive. "Why continue and subject patients to a treatment that won’t be beneficial?" Dr. Cheung asked during an interview. "We can use [MRD] as a marker to take patients off of a protocol that will not be useful to them and try a different treatment."
Immunotherapy with anti-GD2 is part of standard treatment for patients with advanced neuroblastoma.
Dr. Cheung, a pediatric oncologist and head of the neuroblastoma program at Memorial Sloan-Kettering Cancer Center in New York, and his associates used a four-marker genetic analysis to find evidence of residual, metastatic neuroblastoma cells in patients’ bone marrow. The four markers they used were:
• GD2 synthase, the gene for an enzyme that helps produce a ganglioside-abundant in neuroblastoma cells;
• PHOX2B, the gene for a transcription factor that promotes nerve cell growth and maturation;
• CCND1, the gene for cyclin D1 protein, an oncogene; and
• ISL 1, the gene for islet 1, a transcription factor involved in cell growth.
The database included 169 patients treated during first remission, 69 treated during second or later remission, and 105 with primary refractory disease. The researchers used the four-test genetic panel to screen for MRD in bone marrow specimens taken from these patients after the first two rounds of anti-GD2 treatment with or without granulocyte-macrophage colony-stimulating factor in a series of four treatment protocols. A patient was considered positive for MRD if at least one of the genetic markers was positive for the presence of neuroblastoma cells in the bone marrow.
In a multivariate analysis, patients negative for MRD had about a fourfold increased rate of progression-free survival and about a threefold increased rate of overall survival, compared with patients positive for MRD; both differences were statistically significant.
Dr. Cheung said that the four-gene panel his group used was developed through a project begun 15 years ago to look for the most discriminating gene signatures of metastatic neuroblastoma cells against the background of normal bone marrow cells, the metastatic destination for at least 90% of advanced neuroblastoma tumors. A similar approach could identify genetic tests for treatment response of other metastatic tumor types, he said.
The meeting was sponsored by the American Society of Clinical Oncology, the European Organisation for Research and Treatment of Cancer, and the National Cancer Institute. Dr. Cheung said that he is a coinventor on patents held by Memorial Sloan-Kettering Cancer Center.
On Twitter @mitchelzoler
BRUSSELS – In advanced-stage neuroblastoma patients with residual metastases in their bone marrow following two cycles of anti-GD2 immunotherapy, another cycle of this treatment is futile and only causes adverse events, based on a review of 343 stage IV patients treated at one U.S. center.
"Bone marrow minimal residual disease [MRD] measured after two cycles of immunotherapy was the strongest predictor of outcome, irrespective of disease status at the start of immunotherapy," Dr. Nai-Kong V. Cheung said at the Markers in Cancer meeting. "If a patient is positive for MRD after two cycles, don’t continue the treatment."
In the series of 343 patients aged 18 months or older with metastatic, stage IV neuroblastoma that he reviewed, all patients with detectable MRD after two cycles of immunotherapy with GD2 antibody eventually relapsed or died within the next 5 years. In contrast, roughly half of the patients who lacked MRD after the first two cycles of anti-GD2 therapy remained progression free and alive during up to 20 years of follow-up.
The full course of anti-GD2 treatment takes 2 years, has the potential to cause adverse effects, and is painful and expensive. "Why continue and subject patients to a treatment that won’t be beneficial?" Dr. Cheung asked during an interview. "We can use [MRD] as a marker to take patients off of a protocol that will not be useful to them and try a different treatment."
Immunotherapy with anti-GD2 is part of standard treatment for patients with advanced neuroblastoma.
Dr. Cheung, a pediatric oncologist and head of the neuroblastoma program at Memorial Sloan-Kettering Cancer Center in New York, and his associates used a four-marker genetic analysis to find evidence of residual, metastatic neuroblastoma cells in patients’ bone marrow. The four markers they used were:
• GD2 synthase, the gene for an enzyme that helps produce a ganglioside-abundant in neuroblastoma cells;
• PHOX2B, the gene for a transcription factor that promotes nerve cell growth and maturation;
• CCND1, the gene for cyclin D1 protein, an oncogene; and
• ISL 1, the gene for islet 1, a transcription factor involved in cell growth.
The database included 169 patients treated during first remission, 69 treated during second or later remission, and 105 with primary refractory disease. The researchers used the four-test genetic panel to screen for MRD in bone marrow specimens taken from these patients after the first two rounds of anti-GD2 treatment with or without granulocyte-macrophage colony-stimulating factor in a series of four treatment protocols. A patient was considered positive for MRD if at least one of the genetic markers was positive for the presence of neuroblastoma cells in the bone marrow.
In a multivariate analysis, patients negative for MRD had about a fourfold increased rate of progression-free survival and about a threefold increased rate of overall survival, compared with patients positive for MRD; both differences were statistically significant.
Dr. Cheung said that the four-gene panel his group used was developed through a project begun 15 years ago to look for the most discriminating gene signatures of metastatic neuroblastoma cells against the background of normal bone marrow cells, the metastatic destination for at least 90% of advanced neuroblastoma tumors. A similar approach could identify genetic tests for treatment response of other metastatic tumor types, he said.
The meeting was sponsored by the American Society of Clinical Oncology, the European Organisation for Research and Treatment of Cancer, and the National Cancer Institute. Dr. Cheung said that he is a coinventor on patents held by Memorial Sloan-Kettering Cancer Center.
On Twitter @mitchelzoler
BRUSSELS – In advanced-stage neuroblastoma patients with residual metastases in their bone marrow following two cycles of anti-GD2 immunotherapy, another cycle of this treatment is futile and only causes adverse events, based on a review of 343 stage IV patients treated at one U.S. center.
"Bone marrow minimal residual disease [MRD] measured after two cycles of immunotherapy was the strongest predictor of outcome, irrespective of disease status at the start of immunotherapy," Dr. Nai-Kong V. Cheung said at the Markers in Cancer meeting. "If a patient is positive for MRD after two cycles, don’t continue the treatment."
In the series of 343 patients aged 18 months or older with metastatic, stage IV neuroblastoma that he reviewed, all patients with detectable MRD after two cycles of immunotherapy with GD2 antibody eventually relapsed or died within the next 5 years. In contrast, roughly half of the patients who lacked MRD after the first two cycles of anti-GD2 therapy remained progression free and alive during up to 20 years of follow-up.
The full course of anti-GD2 treatment takes 2 years, has the potential to cause adverse effects, and is painful and expensive. "Why continue and subject patients to a treatment that won’t be beneficial?" Dr. Cheung asked during an interview. "We can use [MRD] as a marker to take patients off of a protocol that will not be useful to them and try a different treatment."
Immunotherapy with anti-GD2 is part of standard treatment for patients with advanced neuroblastoma.
Dr. Cheung, a pediatric oncologist and head of the neuroblastoma program at Memorial Sloan-Kettering Cancer Center in New York, and his associates used a four-marker genetic analysis to find evidence of residual, metastatic neuroblastoma cells in patients’ bone marrow. The four markers they used were:
• GD2 synthase, the gene for an enzyme that helps produce a ganglioside-abundant in neuroblastoma cells;
• PHOX2B, the gene for a transcription factor that promotes nerve cell growth and maturation;
• CCND1, the gene for cyclin D1 protein, an oncogene; and
• ISL 1, the gene for islet 1, a transcription factor involved in cell growth.
The database included 169 patients treated during first remission, 69 treated during second or later remission, and 105 with primary refractory disease. The researchers used the four-test genetic panel to screen for MRD in bone marrow specimens taken from these patients after the first two rounds of anti-GD2 treatment with or without granulocyte-macrophage colony-stimulating factor in a series of four treatment protocols. A patient was considered positive for MRD if at least one of the genetic markers was positive for the presence of neuroblastoma cells in the bone marrow.
In a multivariate analysis, patients negative for MRD had about a fourfold increased rate of progression-free survival and about a threefold increased rate of overall survival, compared with patients positive for MRD; both differences were statistically significant.
Dr. Cheung said that the four-gene panel his group used was developed through a project begun 15 years ago to look for the most discriminating gene signatures of metastatic neuroblastoma cells against the background of normal bone marrow cells, the metastatic destination for at least 90% of advanced neuroblastoma tumors. A similar approach could identify genetic tests for treatment response of other metastatic tumor types, he said.
The meeting was sponsored by the American Society of Clinical Oncology, the European Organisation for Research and Treatment of Cancer, and the National Cancer Institute. Dr. Cheung said that he is a coinventor on patents held by Memorial Sloan-Kettering Cancer Center.
On Twitter @mitchelzoler
AT THE MARKERS IN CANCER MEETING
Major finding: In a multivariate analysis, patients negative for minimal residual disease had about a fourfold increased rate of progression-free survival and about a threefold increased rate of overall survival, compared with patients positive for MRD; both differences were statistically significant.
Data source: A review of 343 patients with stage IV neuroblastoma treated with immunotherapy at one U.S. center.
Disclosures: Dr. Cheung said that he is a coinventor on patents held by Memorial Sloan-Kettering Cancer Center.
The future of meaningful use
By the time you read this, you will be aware of the recent changes in the "meaningful use" timeline announced on Dec. 6, 2013. For those who may have missed it, the Centers for Medicare and Medicaid Services, in conjunction with the Office of the National Coordinator for Health Information Technology, proposed a delay in the meaningful use roll-out in response to mounting concern over the viability of the program deadlines. Essentially, this amounts to an extension of stage 2 through 2016, a hold on initiation of stage 3 criteria until 2017, and a delay in penalties for noncompliance until 2015. In response to the announcement, many physicians are breathing sighs of relief. This additional amnesty promises to ease some concerns, as well as allow for an examination of how far the MU program has come, and where it will be going in the future.
We routinely receive messages from readers outlining their concerns over the practicality of the meaningful use incentive program. We have continued to publish these comments as we feel there is tremendous benefit in giving voice to fellow doctors who are frustrated with EHR technology. We are hopeful that the thoughts expressed in this and other forums are at least partly responsible for the delay announced last week, as the concerns are real and practical. One recent message, which brings criticism (both for EHRs and for us), comes from Dr. Michael Lavery, an internist in Manchester, N.H. Dr. Lavery tells of his own experience with an EHR, which he fails to find "meaningful." He writes:
"Other than the obvious benefits of not needing scribes and paper charts, EHRs have not delivered on their promise of increased efficiency. In our large primary care practice, we are now EHR veterans, having adopted an electronic record several years ago. Since then, we have not had occasion to use the data contained therein for ‘improving population health’ or improving access to care, as those in the government would like. On the contrary, the EHR has only increased the amount of work we all have on a daily basis. I, for one, find myself continuously entering data that may or may not be easy to retrieve and can only hope for improvement in my typing skills. I am bothered when I read your column and see that you are extolling the benefits of Health IT without pointing out the shortcomings. Then, when you do speak of the challenges, you imply they are only due to a poor choice of systems or a fault of the individual physician’s unwillingness to accept the new technology. I resent this. I have always been a champion for change and completely embrace new technology when it becomes available. In the case of EHRs, however, the technology has not delivered on the promise, and our jobs are harder as a result. My experience has not been one of improved patient care, but of diminished physician lifestyle ... "
Dr. Lavery expressed a common reaction to the current state of health information technology, and EHR vendors and the government are taking notice. The change in the meaningful use implementation timeline is an indication of this acknowledgment. Industry experts have observed that the additional time is a great relief to EHR companies, which are struggling to make their products stage-2 compliant. Beyond mere compliance, we are hopeful that the extra time will also lead to improved usability of EHR systems and enhancements that are truly "meaningful" to physicians and patients. This could come in the form of improved clinical decision support, more efficient documentation, or better population management tools. We think vendors are starting to get the message and believe EHR software is maturing to adopt these ideas.
We are also optimistic as we look ahead to the stage 3 criteria. Several influential organizations – including the American Medical Association, the American Academy of Family Physicians, and others – have strongly encouraged the CMS to design the stage 3 criteria around improving patient care and physician efficiency, instead of simply demonstrating data collection capabilities. While this has been the goal of stage 3 all along, the growing pains experienced in implementing the first two stages have given reason for pause; efforts to finalize the official criteria have been put on hold until the first half of 2015. It is the intent of the CMS and the Office of the National Coordinator for Health Information Technology to carefully consider all of the feedback they receive before coming to a conclusion on the measures.
In his comments above, Dr. Lavery took issue – not only with the message – but also with the messengers. He identified columnists like us as cheerleaders for substandard technology who blame the user instead of the EHR software’s lack of usability. In response, we want to assert our fundamental belief that EHR technology only improves care delivery when it complements the "art" of medicine. We feel though that it is important to understand that these early stages of EHR adoption represent a transition point. Just as any child of the 21st century would laugh at the rudimentary nature of a 20th-century video game system, we will all likely one day reflect on this generation of EHRs with incredulity and condescension. One hopes we will also understand this era as the foundation of a new type of medicine – medicine that attends to the needs of – and values – physicians, patients, and populations through high-quality care and "meaningful" technology.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. An avid programmer, he has published software for handheld devices in partnership with national organizations, and he is always looking for new ways to bring evidence-based medicine to the point of care. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is also editor-in-chief of Redi-Reference Inc., a software company that creates mobile apps.
By the time you read this, you will be aware of the recent changes in the "meaningful use" timeline announced on Dec. 6, 2013. For those who may have missed it, the Centers for Medicare and Medicaid Services, in conjunction with the Office of the National Coordinator for Health Information Technology, proposed a delay in the meaningful use roll-out in response to mounting concern over the viability of the program deadlines. Essentially, this amounts to an extension of stage 2 through 2016, a hold on initiation of stage 3 criteria until 2017, and a delay in penalties for noncompliance until 2015. In response to the announcement, many physicians are breathing sighs of relief. This additional amnesty promises to ease some concerns, as well as allow for an examination of how far the MU program has come, and where it will be going in the future.
We routinely receive messages from readers outlining their concerns over the practicality of the meaningful use incentive program. We have continued to publish these comments as we feel there is tremendous benefit in giving voice to fellow doctors who are frustrated with EHR technology. We are hopeful that the thoughts expressed in this and other forums are at least partly responsible for the delay announced last week, as the concerns are real and practical. One recent message, which brings criticism (both for EHRs and for us), comes from Dr. Michael Lavery, an internist in Manchester, N.H. Dr. Lavery tells of his own experience with an EHR, which he fails to find "meaningful." He writes:
"Other than the obvious benefits of not needing scribes and paper charts, EHRs have not delivered on their promise of increased efficiency. In our large primary care practice, we are now EHR veterans, having adopted an electronic record several years ago. Since then, we have not had occasion to use the data contained therein for ‘improving population health’ or improving access to care, as those in the government would like. On the contrary, the EHR has only increased the amount of work we all have on a daily basis. I, for one, find myself continuously entering data that may or may not be easy to retrieve and can only hope for improvement in my typing skills. I am bothered when I read your column and see that you are extolling the benefits of Health IT without pointing out the shortcomings. Then, when you do speak of the challenges, you imply they are only due to a poor choice of systems or a fault of the individual physician’s unwillingness to accept the new technology. I resent this. I have always been a champion for change and completely embrace new technology when it becomes available. In the case of EHRs, however, the technology has not delivered on the promise, and our jobs are harder as a result. My experience has not been one of improved patient care, but of diminished physician lifestyle ... "
Dr. Lavery expressed a common reaction to the current state of health information technology, and EHR vendors and the government are taking notice. The change in the meaningful use implementation timeline is an indication of this acknowledgment. Industry experts have observed that the additional time is a great relief to EHR companies, which are struggling to make their products stage-2 compliant. Beyond mere compliance, we are hopeful that the extra time will also lead to improved usability of EHR systems and enhancements that are truly "meaningful" to physicians and patients. This could come in the form of improved clinical decision support, more efficient documentation, or better population management tools. We think vendors are starting to get the message and believe EHR software is maturing to adopt these ideas.
We are also optimistic as we look ahead to the stage 3 criteria. Several influential organizations – including the American Medical Association, the American Academy of Family Physicians, and others – have strongly encouraged the CMS to design the stage 3 criteria around improving patient care and physician efficiency, instead of simply demonstrating data collection capabilities. While this has been the goal of stage 3 all along, the growing pains experienced in implementing the first two stages have given reason for pause; efforts to finalize the official criteria have been put on hold until the first half of 2015. It is the intent of the CMS and the Office of the National Coordinator for Health Information Technology to carefully consider all of the feedback they receive before coming to a conclusion on the measures.
In his comments above, Dr. Lavery took issue – not only with the message – but also with the messengers. He identified columnists like us as cheerleaders for substandard technology who blame the user instead of the EHR software’s lack of usability. In response, we want to assert our fundamental belief that EHR technology only improves care delivery when it complements the "art" of medicine. We feel though that it is important to understand that these early stages of EHR adoption represent a transition point. Just as any child of the 21st century would laugh at the rudimentary nature of a 20th-century video game system, we will all likely one day reflect on this generation of EHRs with incredulity and condescension. One hopes we will also understand this era as the foundation of a new type of medicine – medicine that attends to the needs of – and values – physicians, patients, and populations through high-quality care and "meaningful" technology.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. An avid programmer, he has published software for handheld devices in partnership with national organizations, and he is always looking for new ways to bring evidence-based medicine to the point of care. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is also editor-in-chief of Redi-Reference Inc., a software company that creates mobile apps.
By the time you read this, you will be aware of the recent changes in the "meaningful use" timeline announced on Dec. 6, 2013. For those who may have missed it, the Centers for Medicare and Medicaid Services, in conjunction with the Office of the National Coordinator for Health Information Technology, proposed a delay in the meaningful use roll-out in response to mounting concern over the viability of the program deadlines. Essentially, this amounts to an extension of stage 2 through 2016, a hold on initiation of stage 3 criteria until 2017, and a delay in penalties for noncompliance until 2015. In response to the announcement, many physicians are breathing sighs of relief. This additional amnesty promises to ease some concerns, as well as allow for an examination of how far the MU program has come, and where it will be going in the future.
We routinely receive messages from readers outlining their concerns over the practicality of the meaningful use incentive program. We have continued to publish these comments as we feel there is tremendous benefit in giving voice to fellow doctors who are frustrated with EHR technology. We are hopeful that the thoughts expressed in this and other forums are at least partly responsible for the delay announced last week, as the concerns are real and practical. One recent message, which brings criticism (both for EHRs and for us), comes from Dr. Michael Lavery, an internist in Manchester, N.H. Dr. Lavery tells of his own experience with an EHR, which he fails to find "meaningful." He writes:
"Other than the obvious benefits of not needing scribes and paper charts, EHRs have not delivered on their promise of increased efficiency. In our large primary care practice, we are now EHR veterans, having adopted an electronic record several years ago. Since then, we have not had occasion to use the data contained therein for ‘improving population health’ or improving access to care, as those in the government would like. On the contrary, the EHR has only increased the amount of work we all have on a daily basis. I, for one, find myself continuously entering data that may or may not be easy to retrieve and can only hope for improvement in my typing skills. I am bothered when I read your column and see that you are extolling the benefits of Health IT without pointing out the shortcomings. Then, when you do speak of the challenges, you imply they are only due to a poor choice of systems or a fault of the individual physician’s unwillingness to accept the new technology. I resent this. I have always been a champion for change and completely embrace new technology when it becomes available. In the case of EHRs, however, the technology has not delivered on the promise, and our jobs are harder as a result. My experience has not been one of improved patient care, but of diminished physician lifestyle ... "
Dr. Lavery expressed a common reaction to the current state of health information technology, and EHR vendors and the government are taking notice. The change in the meaningful use implementation timeline is an indication of this acknowledgment. Industry experts have observed that the additional time is a great relief to EHR companies, which are struggling to make their products stage-2 compliant. Beyond mere compliance, we are hopeful that the extra time will also lead to improved usability of EHR systems and enhancements that are truly "meaningful" to physicians and patients. This could come in the form of improved clinical decision support, more efficient documentation, or better population management tools. We think vendors are starting to get the message and believe EHR software is maturing to adopt these ideas.
We are also optimistic as we look ahead to the stage 3 criteria. Several influential organizations – including the American Medical Association, the American Academy of Family Physicians, and others – have strongly encouraged the CMS to design the stage 3 criteria around improving patient care and physician efficiency, instead of simply demonstrating data collection capabilities. While this has been the goal of stage 3 all along, the growing pains experienced in implementing the first two stages have given reason for pause; efforts to finalize the official criteria have been put on hold until the first half of 2015. It is the intent of the CMS and the Office of the National Coordinator for Health Information Technology to carefully consider all of the feedback they receive before coming to a conclusion on the measures.
In his comments above, Dr. Lavery took issue – not only with the message – but also with the messengers. He identified columnists like us as cheerleaders for substandard technology who blame the user instead of the EHR software’s lack of usability. In response, we want to assert our fundamental belief that EHR technology only improves care delivery when it complements the "art" of medicine. We feel though that it is important to understand that these early stages of EHR adoption represent a transition point. Just as any child of the 21st century would laugh at the rudimentary nature of a 20th-century video game system, we will all likely one day reflect on this generation of EHRs with incredulity and condescension. One hopes we will also understand this era as the foundation of a new type of medicine – medicine that attends to the needs of – and values – physicians, patients, and populations through high-quality care and "meaningful" technology.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. An avid programmer, he has published software for handheld devices in partnership with national organizations, and he is always looking for new ways to bring evidence-based medicine to the point of care. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is also editor-in-chief of Redi-Reference Inc., a software company that creates mobile apps.
CMS: Spending on physician services grew faster in 2012
WASHINGTON - Spending for physician services grew half a percentage point more in 2012 than 2011, according to an annual analysis of health care spending from the National Health Expenditure Accounts Team at the Centers for Medicare and Medicaid Services.
The uptick in spending growth was partially attributable to more physician visits as American pocketbooks began to rebound from the recent recession, Anne B. Martin and her colleagues at the CMS Office of the Actuary said at a briefing Jan. 6.
The impact of the Affordable Care Act on spending growth remained negligible in 2012, as it was in the two prior years, according to their analysis, published simultaneously in the journal Health Affairs (2014;33:67-77 [doi 10/1377/hlthaff.2013.1254]).
The CMS actuaries estimated that, overall, the law increased spending by 0.1% from 2010 to 2012. A few ACA provisions – such as coverage for dependents under age 26 and for patients with pre-existing conditions – increased spending, while others – such as payment cuts to hospitals and rebates for drugs under Medicaid – decreased spending.
Overall, the nation’s health spending – $2.8 *trillion in 2012, the most recent year for which there are accurate and complete data – grew 3.7% in 2012, a historically low rate similar to that seen in the previous 3 years. The flat spending reflects trends seen over the years, in particular with the last three boom-and-bust cycles of the economy, said the CMS actuaries. That is, when the economy does well, health spending rises. When there is a recession, health spending decreases; the rebound in spending often lags an economic recovery by several years, said Aaron Catlin, deputy director of the National Health Statistics Group in the Office of the Actuary.
Certain categories of spending did see growth increases or decreases in 2012 that were the result of one-time events, they said.
Spending on physician services by all payers grew by 4% to $452 billion in 2012. While still not approaching the 5.3% increase in 2008, it’s a rebound from just over 3% growth in 2009 and 2010. Physician services grew 3.5% in 2011 and the upward trend continued in 2012 "primarily because of an increase in visits to doctors’ offices as the economy continued to recover from the recent severe economic recession," Ms. Martin said.
Consumers are shouldering a growing share of their health costs, especially for physician services. Out-of-pocket spending on deductibles and copays grew by 3.8% in 2012. The amount Americans spent on health care, including premiums for private insurance and Medicare, and copays, deductibles, and other uncovered costs, grew 4.3% in 2012, compared to 3.1% in 2011.
Medicare, on the other hand, clamped down on physician pay rates and the volume of care it paid for, even as enrollment grew 4.1% in 2012 – the largest 1-year increase in enrollment in 39 years.
That enrollment growth helped drive an uptick in overall spending on hospital services, which is the largest category of national health expenditures, eating up 32% of the total pie. Hospital spending increased 4.9% in 2012 to $882 billion.
Medicaid spending in 2012 continued a pattern of historically low growth, in part because of slower enrollment as the economy rebounded and also as states continued efforts to rein in the program’s costs. Overall, the Medicaid tab was $421 billion in 2012.
Finally, growth in prescription drug spending slowed precipitously for all Americans – from 2.5% in 2011 to 0.4% in 2012 – even as the number of dispensed prescriptions grew by 1.4%, compared to only a 0.5% increase in 2011. The actuaries noted that this slowing was due in large part to the expanded use of generic drugs. Three top sellers went off patent in late 2011 and 2012: atorvastatin (Lipitor), clopidogrel (Plavix), and montelukast (Singulair). Generic drugs accounted for 77% of all dispensed prescriptions in 2012.
The authors disclosed no relevant conflicts of interest and noted that opinions expressed are their own and not necessarily those of the CMS.
On Twitter @aliciaault
*CORRECTION 1/13/14: A previous version of this article incorrectly reported the cost of the nation's overall health spending. This article has been updated.
WASHINGTON - Spending for physician services grew half a percentage point more in 2012 than 2011, according to an annual analysis of health care spending from the National Health Expenditure Accounts Team at the Centers for Medicare and Medicaid Services.
The uptick in spending growth was partially attributable to more physician visits as American pocketbooks began to rebound from the recent recession, Anne B. Martin and her colleagues at the CMS Office of the Actuary said at a briefing Jan. 6.
The impact of the Affordable Care Act on spending growth remained negligible in 2012, as it was in the two prior years, according to their analysis, published simultaneously in the journal Health Affairs (2014;33:67-77 [doi 10/1377/hlthaff.2013.1254]).
The CMS actuaries estimated that, overall, the law increased spending by 0.1% from 2010 to 2012. A few ACA provisions – such as coverage for dependents under age 26 and for patients with pre-existing conditions – increased spending, while others – such as payment cuts to hospitals and rebates for drugs under Medicaid – decreased spending.
Overall, the nation’s health spending – $2.8 *trillion in 2012, the most recent year for which there are accurate and complete data – grew 3.7% in 2012, a historically low rate similar to that seen in the previous 3 years. The flat spending reflects trends seen over the years, in particular with the last three boom-and-bust cycles of the economy, said the CMS actuaries. That is, when the economy does well, health spending rises. When there is a recession, health spending decreases; the rebound in spending often lags an economic recovery by several years, said Aaron Catlin, deputy director of the National Health Statistics Group in the Office of the Actuary.
Certain categories of spending did see growth increases or decreases in 2012 that were the result of one-time events, they said.
Spending on physician services by all payers grew by 4% to $452 billion in 2012. While still not approaching the 5.3% increase in 2008, it’s a rebound from just over 3% growth in 2009 and 2010. Physician services grew 3.5% in 2011 and the upward trend continued in 2012 "primarily because of an increase in visits to doctors’ offices as the economy continued to recover from the recent severe economic recession," Ms. Martin said.
Consumers are shouldering a growing share of their health costs, especially for physician services. Out-of-pocket spending on deductibles and copays grew by 3.8% in 2012. The amount Americans spent on health care, including premiums for private insurance and Medicare, and copays, deductibles, and other uncovered costs, grew 4.3% in 2012, compared to 3.1% in 2011.
Medicare, on the other hand, clamped down on physician pay rates and the volume of care it paid for, even as enrollment grew 4.1% in 2012 – the largest 1-year increase in enrollment in 39 years.
That enrollment growth helped drive an uptick in overall spending on hospital services, which is the largest category of national health expenditures, eating up 32% of the total pie. Hospital spending increased 4.9% in 2012 to $882 billion.
Medicaid spending in 2012 continued a pattern of historically low growth, in part because of slower enrollment as the economy rebounded and also as states continued efforts to rein in the program’s costs. Overall, the Medicaid tab was $421 billion in 2012.
Finally, growth in prescription drug spending slowed precipitously for all Americans – from 2.5% in 2011 to 0.4% in 2012 – even as the number of dispensed prescriptions grew by 1.4%, compared to only a 0.5% increase in 2011. The actuaries noted that this slowing was due in large part to the expanded use of generic drugs. Three top sellers went off patent in late 2011 and 2012: atorvastatin (Lipitor), clopidogrel (Plavix), and montelukast (Singulair). Generic drugs accounted for 77% of all dispensed prescriptions in 2012.
The authors disclosed no relevant conflicts of interest and noted that opinions expressed are their own and not necessarily those of the CMS.
On Twitter @aliciaault
*CORRECTION 1/13/14: A previous version of this article incorrectly reported the cost of the nation's overall health spending. This article has been updated.
WASHINGTON - Spending for physician services grew half a percentage point more in 2012 than 2011, according to an annual analysis of health care spending from the National Health Expenditure Accounts Team at the Centers for Medicare and Medicaid Services.
The uptick in spending growth was partially attributable to more physician visits as American pocketbooks began to rebound from the recent recession, Anne B. Martin and her colleagues at the CMS Office of the Actuary said at a briefing Jan. 6.
The impact of the Affordable Care Act on spending growth remained negligible in 2012, as it was in the two prior years, according to their analysis, published simultaneously in the journal Health Affairs (2014;33:67-77 [doi 10/1377/hlthaff.2013.1254]).
The CMS actuaries estimated that, overall, the law increased spending by 0.1% from 2010 to 2012. A few ACA provisions – such as coverage for dependents under age 26 and for patients with pre-existing conditions – increased spending, while others – such as payment cuts to hospitals and rebates for drugs under Medicaid – decreased spending.
Overall, the nation’s health spending – $2.8 *trillion in 2012, the most recent year for which there are accurate and complete data – grew 3.7% in 2012, a historically low rate similar to that seen in the previous 3 years. The flat spending reflects trends seen over the years, in particular with the last three boom-and-bust cycles of the economy, said the CMS actuaries. That is, when the economy does well, health spending rises. When there is a recession, health spending decreases; the rebound in spending often lags an economic recovery by several years, said Aaron Catlin, deputy director of the National Health Statistics Group in the Office of the Actuary.
Certain categories of spending did see growth increases or decreases in 2012 that were the result of one-time events, they said.
Spending on physician services by all payers grew by 4% to $452 billion in 2012. While still not approaching the 5.3% increase in 2008, it’s a rebound from just over 3% growth in 2009 and 2010. Physician services grew 3.5% in 2011 and the upward trend continued in 2012 "primarily because of an increase in visits to doctors’ offices as the economy continued to recover from the recent severe economic recession," Ms. Martin said.
Consumers are shouldering a growing share of their health costs, especially for physician services. Out-of-pocket spending on deductibles and copays grew by 3.8% in 2012. The amount Americans spent on health care, including premiums for private insurance and Medicare, and copays, deductibles, and other uncovered costs, grew 4.3% in 2012, compared to 3.1% in 2011.
Medicare, on the other hand, clamped down on physician pay rates and the volume of care it paid for, even as enrollment grew 4.1% in 2012 – the largest 1-year increase in enrollment in 39 years.
That enrollment growth helped drive an uptick in overall spending on hospital services, which is the largest category of national health expenditures, eating up 32% of the total pie. Hospital spending increased 4.9% in 2012 to $882 billion.
Medicaid spending in 2012 continued a pattern of historically low growth, in part because of slower enrollment as the economy rebounded and also as states continued efforts to rein in the program’s costs. Overall, the Medicaid tab was $421 billion in 2012.
Finally, growth in prescription drug spending slowed precipitously for all Americans – from 2.5% in 2011 to 0.4% in 2012 – even as the number of dispensed prescriptions grew by 1.4%, compared to only a 0.5% increase in 2011. The actuaries noted that this slowing was due in large part to the expanded use of generic drugs. Three top sellers went off patent in late 2011 and 2012: atorvastatin (Lipitor), clopidogrel (Plavix), and montelukast (Singulair). Generic drugs accounted for 77% of all dispensed prescriptions in 2012.
The authors disclosed no relevant conflicts of interest and noted that opinions expressed are their own and not necessarily those of the CMS.
On Twitter @aliciaault
*CORRECTION 1/13/14: A previous version of this article incorrectly reported the cost of the nation's overall health spending. This article has been updated.
FROM A HEALTH AFFAIRS BRIEFING
Major finding: Growth in national health care spending for 2012 was 3.7%, a low, but slightly larger rate of growth than in 2011.
Data source: Several federal databases including those managed by the Centers for Medicare and Medicaid Services, the Department of Commerce, the Bureau of Economic Analysis, and the Census Bureau.
Disclosures: The authors disclosed no relevant conflicts of interest and noted that opinions expressed are their own and not necessarily those of the CMS.
Anatomy’s role is elusive in carotid stenting risk
CHICAGO – Pinning down the anatomic characteristics that increase the risk of stroke with carotid artery stenting continues to be a challenge, as demonstrated by a database study and literature review presented at a symposium on vascular surgery sponsored by Northwestern University.
"I am absolutely convinced that certain anatomic and plaque characteristics increase the risk of a stroke for patients with carotid artery stenting," Dr. Melina R. Kibbe said in presenting her study. "The studies are not consistent in the literature, but there is a pattern."
She presented a prospective database review that evaluated no less than a dozen anatomic variables in 381 carotid arteries stented at the university from 2001 to 2010. The mostly male (75%), asymptomatic (70%), and moderate- to high-risk cohort had an average age of 70.5 years.
Within 30 days of carotid stenting, there were six strokes and eight transient ischemic attacks (TIAs), for an overall neurologic event rate of 3.7%, she said. Three patients had a heart attack, and two died.
The risk of perioperative stroke or TIA was significantly increased only in patients with a higher degree of internal carotid artery (ICA) stenosis (87% stenosis vs. 81% stenosis; P = .03).
It also trended higher, but fell short of significance, in those with greater arch calcification (P = .06).
Surprisingly, no statistical association was found between neurologic events and arch type (P = .16), despite the clinical belief that increasing arch type can be associated with more difficulty accessing the target lesion, said Dr. Kibbe, professor of vascular surgery and surgical research at Northwestern University, Chicago.
Other variables with trends that failed to reach statistical significance included internal to common carotid artery angulation, tortuous carotid artery, ipsilateral external carotid artery (ECA) stenosis, plaque calcification, and lesion length.
Turning to the literature for more answers, Dr. Kibbe and her colleagues performed a review of eight carotid stenting studies between 1993 and 2013. These studies included SAPPHIRE, which demonstrated an association between type II and III arches and increased stroke risk. Two other studies implicated type II, type III, and bovine arches, while three other studies, including a systematic review that incorporated the EVA-3S study (Stroke 2011;42:380-8), found no association between arch type and stroke.
Still, Dr. Kibbe said she’s convinced no two patients are alike when it comes to arterial anatomy and called for data from pivotal trials like CREST to be reanalyzed for stroke, based on arch type and plaque characteristics.
"Even better, I’d like to see a prospective, randomized study that excludes patients for carotid artery stenting based on their anatomy; for example, excluding all type III arches," she said. "My own personal bias is that patients with type III arches should not have carotid stenting. We don’t need to push the envelope."
Interestingly, no study in the review has shown ICA stenosis to be a risk factor for stroke or TIA, although lesions with a higher degree of stenosis would be expected to contribute to perioperative stroke risk.
Arch calcification, ECA stenosis, and plaque calcification also failed to register as risk factors, despite their potential to increase the risk of embolization with wire or catheter manipulation, Dr. Kibbe observed.
Two studies found that lesions longer than 1 cm or 1.5 cm were predictive of stroke, while one study (Catheter Cardiovasc. Interv. 2012;80:321-8) linked stroke with ICA tortuosity, defined as a distal ICA angle of more than 60 degrees.
Conventional thinking would suggest that right-sided carotid stenting would also confer a greater stroke risk because selecting the right ICA requires crossing the orifice of the left ICA, but only the SAPPHIRE trial reported more strokes with right-sided lesions, she said.
Finally, Dr. Kibbe highlighted an anatomic scoring system for carotid artery stenting developed by an international panel of seven vascular surgeons and five interventional radiologists (Stroke 2009;40:1698-703). Based on expert consensus, the greatest risk factor is type III arch, followed in descending order of risk by arch atheroma, diseased common carotid artery, ECA disease, angulated distal ICA, bovine arch, and pinhole stenosis. The resulting color-coded, traffic-light scoring system looks rather busy, but is relatively easy to use and provides guidance on carotid stenting suitability for the novice physician, she said.
Dr. Kibbe reported having no financial disclosures.
CHICAGO – Pinning down the anatomic characteristics that increase the risk of stroke with carotid artery stenting continues to be a challenge, as demonstrated by a database study and literature review presented at a symposium on vascular surgery sponsored by Northwestern University.
"I am absolutely convinced that certain anatomic and plaque characteristics increase the risk of a stroke for patients with carotid artery stenting," Dr. Melina R. Kibbe said in presenting her study. "The studies are not consistent in the literature, but there is a pattern."
She presented a prospective database review that evaluated no less than a dozen anatomic variables in 381 carotid arteries stented at the university from 2001 to 2010. The mostly male (75%), asymptomatic (70%), and moderate- to high-risk cohort had an average age of 70.5 years.
Within 30 days of carotid stenting, there were six strokes and eight transient ischemic attacks (TIAs), for an overall neurologic event rate of 3.7%, she said. Three patients had a heart attack, and two died.
The risk of perioperative stroke or TIA was significantly increased only in patients with a higher degree of internal carotid artery (ICA) stenosis (87% stenosis vs. 81% stenosis; P = .03).
It also trended higher, but fell short of significance, in those with greater arch calcification (P = .06).
Surprisingly, no statistical association was found between neurologic events and arch type (P = .16), despite the clinical belief that increasing arch type can be associated with more difficulty accessing the target lesion, said Dr. Kibbe, professor of vascular surgery and surgical research at Northwestern University, Chicago.
Other variables with trends that failed to reach statistical significance included internal to common carotid artery angulation, tortuous carotid artery, ipsilateral external carotid artery (ECA) stenosis, plaque calcification, and lesion length.
Turning to the literature for more answers, Dr. Kibbe and her colleagues performed a review of eight carotid stenting studies between 1993 and 2013. These studies included SAPPHIRE, which demonstrated an association between type II and III arches and increased stroke risk. Two other studies implicated type II, type III, and bovine arches, while three other studies, including a systematic review that incorporated the EVA-3S study (Stroke 2011;42:380-8), found no association between arch type and stroke.
Still, Dr. Kibbe said she’s convinced no two patients are alike when it comes to arterial anatomy and called for data from pivotal trials like CREST to be reanalyzed for stroke, based on arch type and plaque characteristics.
"Even better, I’d like to see a prospective, randomized study that excludes patients for carotid artery stenting based on their anatomy; for example, excluding all type III arches," she said. "My own personal bias is that patients with type III arches should not have carotid stenting. We don’t need to push the envelope."
Interestingly, no study in the review has shown ICA stenosis to be a risk factor for stroke or TIA, although lesions with a higher degree of stenosis would be expected to contribute to perioperative stroke risk.
Arch calcification, ECA stenosis, and plaque calcification also failed to register as risk factors, despite their potential to increase the risk of embolization with wire or catheter manipulation, Dr. Kibbe observed.
Two studies found that lesions longer than 1 cm or 1.5 cm were predictive of stroke, while one study (Catheter Cardiovasc. Interv. 2012;80:321-8) linked stroke with ICA tortuosity, defined as a distal ICA angle of more than 60 degrees.
Conventional thinking would suggest that right-sided carotid stenting would also confer a greater stroke risk because selecting the right ICA requires crossing the orifice of the left ICA, but only the SAPPHIRE trial reported more strokes with right-sided lesions, she said.
Finally, Dr. Kibbe highlighted an anatomic scoring system for carotid artery stenting developed by an international panel of seven vascular surgeons and five interventional radiologists (Stroke 2009;40:1698-703). Based on expert consensus, the greatest risk factor is type III arch, followed in descending order of risk by arch atheroma, diseased common carotid artery, ECA disease, angulated distal ICA, bovine arch, and pinhole stenosis. The resulting color-coded, traffic-light scoring system looks rather busy, but is relatively easy to use and provides guidance on carotid stenting suitability for the novice physician, she said.
Dr. Kibbe reported having no financial disclosures.
CHICAGO – Pinning down the anatomic characteristics that increase the risk of stroke with carotid artery stenting continues to be a challenge, as demonstrated by a database study and literature review presented at a symposium on vascular surgery sponsored by Northwestern University.
"I am absolutely convinced that certain anatomic and plaque characteristics increase the risk of a stroke for patients with carotid artery stenting," Dr. Melina R. Kibbe said in presenting her study. "The studies are not consistent in the literature, but there is a pattern."
She presented a prospective database review that evaluated no less than a dozen anatomic variables in 381 carotid arteries stented at the university from 2001 to 2010. The mostly male (75%), asymptomatic (70%), and moderate- to high-risk cohort had an average age of 70.5 years.
Within 30 days of carotid stenting, there were six strokes and eight transient ischemic attacks (TIAs), for an overall neurologic event rate of 3.7%, she said. Three patients had a heart attack, and two died.
The risk of perioperative stroke or TIA was significantly increased only in patients with a higher degree of internal carotid artery (ICA) stenosis (87% stenosis vs. 81% stenosis; P = .03).
It also trended higher, but fell short of significance, in those with greater arch calcification (P = .06).
Surprisingly, no statistical association was found between neurologic events and arch type (P = .16), despite the clinical belief that increasing arch type can be associated with more difficulty accessing the target lesion, said Dr. Kibbe, professor of vascular surgery and surgical research at Northwestern University, Chicago.
Other variables with trends that failed to reach statistical significance included internal to common carotid artery angulation, tortuous carotid artery, ipsilateral external carotid artery (ECA) stenosis, plaque calcification, and lesion length.
Turning to the literature for more answers, Dr. Kibbe and her colleagues performed a review of eight carotid stenting studies between 1993 and 2013. These studies included SAPPHIRE, which demonstrated an association between type II and III arches and increased stroke risk. Two other studies implicated type II, type III, and bovine arches, while three other studies, including a systematic review that incorporated the EVA-3S study (Stroke 2011;42:380-8), found no association between arch type and stroke.
Still, Dr. Kibbe said she’s convinced no two patients are alike when it comes to arterial anatomy and called for data from pivotal trials like CREST to be reanalyzed for stroke, based on arch type and plaque characteristics.
"Even better, I’d like to see a prospective, randomized study that excludes patients for carotid artery stenting based on their anatomy; for example, excluding all type III arches," she said. "My own personal bias is that patients with type III arches should not have carotid stenting. We don’t need to push the envelope."
Interestingly, no study in the review has shown ICA stenosis to be a risk factor for stroke or TIA, although lesions with a higher degree of stenosis would be expected to contribute to perioperative stroke risk.
Arch calcification, ECA stenosis, and plaque calcification also failed to register as risk factors, despite their potential to increase the risk of embolization with wire or catheter manipulation, Dr. Kibbe observed.
Two studies found that lesions longer than 1 cm or 1.5 cm were predictive of stroke, while one study (Catheter Cardiovasc. Interv. 2012;80:321-8) linked stroke with ICA tortuosity, defined as a distal ICA angle of more than 60 degrees.
Conventional thinking would suggest that right-sided carotid stenting would also confer a greater stroke risk because selecting the right ICA requires crossing the orifice of the left ICA, but only the SAPPHIRE trial reported more strokes with right-sided lesions, she said.
Finally, Dr. Kibbe highlighted an anatomic scoring system for carotid artery stenting developed by an international panel of seven vascular surgeons and five interventional radiologists (Stroke 2009;40:1698-703). Based on expert consensus, the greatest risk factor is type III arch, followed in descending order of risk by arch atheroma, diseased common carotid artery, ECA disease, angulated distal ICA, bovine arch, and pinhole stenosis. The resulting color-coded, traffic-light scoring system looks rather busy, but is relatively easy to use and provides guidance on carotid stenting suitability for the novice physician, she said.
Dr. Kibbe reported having no financial disclosures.
EXPERT ANALYSIS AT A NORTHWESTERN VASCULAR SYMPOSIUM
Major finding: The risk of perioperative stroke or TIA was significantly increased only in patients with a higher degree of internal carotid artery (ICA) stenosis (87% stenosis vs. 81% stenosis; P = .03).
Data source: A retrospective study of 381 carotid arteries and an analysis of eight published studies.
Disclosures: Dr. Kibbe reported having no financial disclosures.
Women physicians weigh work/family life choices
Dr. Phillips and colleagues have identified yet another issue that may add to the complexity of surgical training, i.e., pregnancy. Both surgical training and having children are time-sensitive priorities that may conflict with one another and add extra stress to the decision matrix. There is no perfect answer here. So, even after the decision is made to have a child, there will still be many other conflicts coming down the pike.
The key to managing such issues is to realize the following: Be flexible. You can "do it all" but not all at once. You have a whole lifetime to accomplish goals and from time to time, adjustments in plans have to be made: You lead life, it does not lead you. There is no "yellow brick road." This is where surgeons excel. They exhibit strength and courage when facing such conflicts and recognize that they have the skills and stamina to move their lives forward even in the face of complex challenges.
Grace Rozycki, MD, FACS, is the Willis D. Gatch Professor of Surgery and executive vice chair of the department of surgery, Indiana University, Indianapolis.
It would be interesting to compare female surgeons with other professional women of the same age and generation. Many of my friends from high school and college are not physicians, and they are very accomplished in their chosen fields. Many of these women did not identify a life partner until well into their 30s. I think that getting married and having children in the 30- or even 40-year-old age groups reflects a generational trend, partially, but not entirely, attributable to devoting oneself to a career. In addition, many of my group of friends, including myself, married men who had children from previous marriages. Having an "instant" family may further delay or may encourage childbearing. As expected, several of my friends of advanced maternal age experienced complications in their pregnancies and attempted assisted reproduction. Because I was over 40 years old when my husband and I decided to try to get pregnant, I planned to discuss my fertility with my gynecologist, and we were very blessed to discover that we were already pregnant by the time that appointment was scheduled.
As others have said, there is not a perfect time to have a child. The responsibilities and stresses don’t really get better or worse with career progression; they just change. I think it is the responsibility of all professional women with families to support other women in having families, if that is something they choose to do. This effort involves helping one another and making the workplace family friendly. I don’t schedule my conference calls or research team meetings at times that folks might be picking up their children at school or having dinner with their families. I recently convinced our business manager to get an extra refrigerator in a private room for a nurse practitioner who is returning from maternity leave, wants to breast feed, and will need to pump. The American College of Surgeons has offered all-day child care at their meetings for years, and the Society for American Gastrointestinal and Endoscopic Surgeons (SAGES) has recently followed suit. With such support, I have taken my toddler with me to nearly all my professional meetings during the first 3 years of her life, and I don’t hide the fact that being a wife and mother are priorities for me. These new roles have not significantly compromised my career. In fact, they’ve helped me to focus and set priorities. Since the birth of my child, I have been asked to serve in an institutional leadership role as research director for our patient portal, and my first R01 grant proposal was submitted and successfully funded.
Gretchen Purcell Jackson, M.D, Ph.D., FACS, is assistant professor of surgery, pediatrics, and biomedical informatics, Vanderbilt University, Nashville, Tenn.
The issues of childbearing and fertility are complex for women surgeons. It was not clear from the presentation whether the respondents were all in practice. If the respondents are all primarily from the baby-boomer generation, it may alter the survey results. It would be interesting to see the response of current women surgery trainees and to determine whether this is really more of a generational issue or whether the issues relate to the surgical lifestyle.
Certainly, the knowledge of fertility options, financial stability, and ease of access to specialists may also encourage women surgeons to seek intervention at a higher rate than that of the general population.
There is never a perfect time to have children, but there are certainly times that are not ideal. I am married, and have three children, ages 8, 13, and 18 years. I had no difficulties with any of my pregnancies. I had my first child at the completion of my fellowship, and the other two while in academic practice. I worked up until the day I went into labor during training, and up until 2 weeks prior to my due date when I was in practice. I did modify my surgical schedule to avoid long or complex cases during my last months when I was in practice, whereas, this was not necessary during my training. I was fortunate to have partners who were accommodating.
Comparing surgeons to other professionals from the same generation would give better information as to whether the field itself is the issue, or whether this is more of a generational issue for professionals. Many of my friends both in medical and nonmedical professional fields also waited until early 30s to get married and have children, while others chose not to have any children to prioritize their careers. When I was in training, there were many places in which overt prejudice against women still existed. It was difficult enough to be "equal" to your male colleagues without having to deal with concerns of dumping work on them because of a pregnancy or the potential reaction from your chair or program director. Luckily, not all programs were like that. It was also commonplace to work upward of 100 hours per week.
Finding time for relationships, surviving a pregnancy, surviving a surgical residency, and not putting a pregnancy at risk was more difficult under those conditions.
Times continue to change, and pregnancy during training is becoming more common, especially in larger surgery programs. The acknowledgment that not only women, but also men of the younger generation are not willing to work to the exclusion of family, and outside life is changing the field, as is the fact that 50% of graduating medical students are women.
The ability to have children during training has also been facilitated by the duty hour rules, as well as by having more women faculty. We need to continue to examine ways to encourage the work-life blend in surgical fields, not only for women, but for men as well, or risk losing a large section of the class to "lifestyle fields." Having resources within the institutions such as child care, with hours compatible with working resident schedules would go a long way toward facilitating this blend. The finding that women surgeons availed themselves of fertility specialists more frequently than the general population did is not necessarily a concern. The question is whether the rate of infertility in women surgeons is truly significantly higher than that of their peers in other professional areas. The main issues to address remain how to facilitate childbearing for those women surgeons who wish to have a family, and how to facilitate the work-life blend for ourselves and all of our trainees.
Linda Harris, M.D., FACS, is division chief, vascular surgery, State University of New York at Buffalo.
The decisions about childbearing that women surgeons make are in many ways similar to those of other career-oriented women, as Dr. Harris points out. The dilemmas involved in this area are perhaps more extreme in the field of surgery, compared with other professions because to the pressures and length of training that are associated with surgery. It is a topic that deserves more attention, since from a very general perspective, it is difficult for a trainee to project out the implications of his or her choices in creating a family or having children 5 or more years beyond training. Decisions around childbearing are also complex, nuanced, highly personal, and variable to each person’s life experience. I had one child during my residency and another during my practice, which in each case had its own advantages and challenges. In my case, the most important factor to making it work as well as it has was having a very supportive spouse.
Genevieve Melton-Meaux, M.D., FACS, is an associate professor of surgery, University of Minnesota, Minneapolis.
As a medical student applying into a surgical subspecialty, I am sobered but certainly not surprised by these findings. I approach my career and desire for a family with wary readiness to face a lifetime of setting tough priorities that at times may feel isolating. Is a career as a surgeon incompatible with pregnancy, lasting marriage, and well-behaved children? I would say no, though it depends on who your partner is, where you work, and careful timing. With increasing numbers of females entering surgery who refuse to compromise mothering their own children, the work environment will have to change. Part of this changing landscape may mean that female surgeons will undergo assisted reproductive technologies at higher rates than their non-surgeon counterparts. It may mean that shift work becomes more acceptable. Regardless, the changes we create as a medical community should affect both men and women; we should be wary of designing special tracks or programs that can lend to further isolation and hand-waving of leadership. To ensure gender equity in surgery we are asking for institutional change – something for which there is never a perfect or easy time. Surgeons simply have to make it a priority.
Charlotte R. Gamble is a fourth year medical student at the University of Michigan, Ann Arbor
Dr. Phillips and colleagues have identified yet another issue that may add to the complexity of surgical training, i.e., pregnancy. Both surgical training and having children are time-sensitive priorities that may conflict with one another and add extra stress to the decision matrix. There is no perfect answer here. So, even after the decision is made to have a child, there will still be many other conflicts coming down the pike.
The key to managing such issues is to realize the following: Be flexible. You can "do it all" but not all at once. You have a whole lifetime to accomplish goals and from time to time, adjustments in plans have to be made: You lead life, it does not lead you. There is no "yellow brick road." This is where surgeons excel. They exhibit strength and courage when facing such conflicts and recognize that they have the skills and stamina to move their lives forward even in the face of complex challenges.
Grace Rozycki, MD, FACS, is the Willis D. Gatch Professor of Surgery and executive vice chair of the department of surgery, Indiana University, Indianapolis.
It would be interesting to compare female surgeons with other professional women of the same age and generation. Many of my friends from high school and college are not physicians, and they are very accomplished in their chosen fields. Many of these women did not identify a life partner until well into their 30s. I think that getting married and having children in the 30- or even 40-year-old age groups reflects a generational trend, partially, but not entirely, attributable to devoting oneself to a career. In addition, many of my group of friends, including myself, married men who had children from previous marriages. Having an "instant" family may further delay or may encourage childbearing. As expected, several of my friends of advanced maternal age experienced complications in their pregnancies and attempted assisted reproduction. Because I was over 40 years old when my husband and I decided to try to get pregnant, I planned to discuss my fertility with my gynecologist, and we were very blessed to discover that we were already pregnant by the time that appointment was scheduled.
As others have said, there is not a perfect time to have a child. The responsibilities and stresses don’t really get better or worse with career progression; they just change. I think it is the responsibility of all professional women with families to support other women in having families, if that is something they choose to do. This effort involves helping one another and making the workplace family friendly. I don’t schedule my conference calls or research team meetings at times that folks might be picking up their children at school or having dinner with their families. I recently convinced our business manager to get an extra refrigerator in a private room for a nurse practitioner who is returning from maternity leave, wants to breast feed, and will need to pump. The American College of Surgeons has offered all-day child care at their meetings for years, and the Society for American Gastrointestinal and Endoscopic Surgeons (SAGES) has recently followed suit. With such support, I have taken my toddler with me to nearly all my professional meetings during the first 3 years of her life, and I don’t hide the fact that being a wife and mother are priorities for me. These new roles have not significantly compromised my career. In fact, they’ve helped me to focus and set priorities. Since the birth of my child, I have been asked to serve in an institutional leadership role as research director for our patient portal, and my first R01 grant proposal was submitted and successfully funded.
Gretchen Purcell Jackson, M.D, Ph.D., FACS, is assistant professor of surgery, pediatrics, and biomedical informatics, Vanderbilt University, Nashville, Tenn.
The issues of childbearing and fertility are complex for women surgeons. It was not clear from the presentation whether the respondents were all in practice. If the respondents are all primarily from the baby-boomer generation, it may alter the survey results. It would be interesting to see the response of current women surgery trainees and to determine whether this is really more of a generational issue or whether the issues relate to the surgical lifestyle.
Certainly, the knowledge of fertility options, financial stability, and ease of access to specialists may also encourage women surgeons to seek intervention at a higher rate than that of the general population.
There is never a perfect time to have children, but there are certainly times that are not ideal. I am married, and have three children, ages 8, 13, and 18 years. I had no difficulties with any of my pregnancies. I had my first child at the completion of my fellowship, and the other two while in academic practice. I worked up until the day I went into labor during training, and up until 2 weeks prior to my due date when I was in practice. I did modify my surgical schedule to avoid long or complex cases during my last months when I was in practice, whereas, this was not necessary during my training. I was fortunate to have partners who were accommodating.
Comparing surgeons to other professionals from the same generation would give better information as to whether the field itself is the issue, or whether this is more of a generational issue for professionals. Many of my friends both in medical and nonmedical professional fields also waited until early 30s to get married and have children, while others chose not to have any children to prioritize their careers. When I was in training, there were many places in which overt prejudice against women still existed. It was difficult enough to be "equal" to your male colleagues without having to deal with concerns of dumping work on them because of a pregnancy or the potential reaction from your chair or program director. Luckily, not all programs were like that. It was also commonplace to work upward of 100 hours per week.
Finding time for relationships, surviving a pregnancy, surviving a surgical residency, and not putting a pregnancy at risk was more difficult under those conditions.
Times continue to change, and pregnancy during training is becoming more common, especially in larger surgery programs. The acknowledgment that not only women, but also men of the younger generation are not willing to work to the exclusion of family, and outside life is changing the field, as is the fact that 50% of graduating medical students are women.
The ability to have children during training has also been facilitated by the duty hour rules, as well as by having more women faculty. We need to continue to examine ways to encourage the work-life blend in surgical fields, not only for women, but for men as well, or risk losing a large section of the class to "lifestyle fields." Having resources within the institutions such as child care, with hours compatible with working resident schedules would go a long way toward facilitating this blend. The finding that women surgeons availed themselves of fertility specialists more frequently than the general population did is not necessarily a concern. The question is whether the rate of infertility in women surgeons is truly significantly higher than that of their peers in other professional areas. The main issues to address remain how to facilitate childbearing for those women surgeons who wish to have a family, and how to facilitate the work-life blend for ourselves and all of our trainees.
Linda Harris, M.D., FACS, is division chief, vascular surgery, State University of New York at Buffalo.
The decisions about childbearing that women surgeons make are in many ways similar to those of other career-oriented women, as Dr. Harris points out. The dilemmas involved in this area are perhaps more extreme in the field of surgery, compared with other professions because to the pressures and length of training that are associated with surgery. It is a topic that deserves more attention, since from a very general perspective, it is difficult for a trainee to project out the implications of his or her choices in creating a family or having children 5 or more years beyond training. Decisions around childbearing are also complex, nuanced, highly personal, and variable to each person’s life experience. I had one child during my residency and another during my practice, which in each case had its own advantages and challenges. In my case, the most important factor to making it work as well as it has was having a very supportive spouse.
Genevieve Melton-Meaux, M.D., FACS, is an associate professor of surgery, University of Minnesota, Minneapolis.
As a medical student applying into a surgical subspecialty, I am sobered but certainly not surprised by these findings. I approach my career and desire for a family with wary readiness to face a lifetime of setting tough priorities that at times may feel isolating. Is a career as a surgeon incompatible with pregnancy, lasting marriage, and well-behaved children? I would say no, though it depends on who your partner is, where you work, and careful timing. With increasing numbers of females entering surgery who refuse to compromise mothering their own children, the work environment will have to change. Part of this changing landscape may mean that female surgeons will undergo assisted reproductive technologies at higher rates than their non-surgeon counterparts. It may mean that shift work becomes more acceptable. Regardless, the changes we create as a medical community should affect both men and women; we should be wary of designing special tracks or programs that can lend to further isolation and hand-waving of leadership. To ensure gender equity in surgery we are asking for institutional change – something for which there is never a perfect or easy time. Surgeons simply have to make it a priority.
Charlotte R. Gamble is a fourth year medical student at the University of Michigan, Ann Arbor
Dr. Phillips and colleagues have identified yet another issue that may add to the complexity of surgical training, i.e., pregnancy. Both surgical training and having children are time-sensitive priorities that may conflict with one another and add extra stress to the decision matrix. There is no perfect answer here. So, even after the decision is made to have a child, there will still be many other conflicts coming down the pike.
The key to managing such issues is to realize the following: Be flexible. You can "do it all" but not all at once. You have a whole lifetime to accomplish goals and from time to time, adjustments in plans have to be made: You lead life, it does not lead you. There is no "yellow brick road." This is where surgeons excel. They exhibit strength and courage when facing such conflicts and recognize that they have the skills and stamina to move their lives forward even in the face of complex challenges.
Grace Rozycki, MD, FACS, is the Willis D. Gatch Professor of Surgery and executive vice chair of the department of surgery, Indiana University, Indianapolis.
It would be interesting to compare female surgeons with other professional women of the same age and generation. Many of my friends from high school and college are not physicians, and they are very accomplished in their chosen fields. Many of these women did not identify a life partner until well into their 30s. I think that getting married and having children in the 30- or even 40-year-old age groups reflects a generational trend, partially, but not entirely, attributable to devoting oneself to a career. In addition, many of my group of friends, including myself, married men who had children from previous marriages. Having an "instant" family may further delay or may encourage childbearing. As expected, several of my friends of advanced maternal age experienced complications in their pregnancies and attempted assisted reproduction. Because I was over 40 years old when my husband and I decided to try to get pregnant, I planned to discuss my fertility with my gynecologist, and we were very blessed to discover that we were already pregnant by the time that appointment was scheduled.
As others have said, there is not a perfect time to have a child. The responsibilities and stresses don’t really get better or worse with career progression; they just change. I think it is the responsibility of all professional women with families to support other women in having families, if that is something they choose to do. This effort involves helping one another and making the workplace family friendly. I don’t schedule my conference calls or research team meetings at times that folks might be picking up their children at school or having dinner with their families. I recently convinced our business manager to get an extra refrigerator in a private room for a nurse practitioner who is returning from maternity leave, wants to breast feed, and will need to pump. The American College of Surgeons has offered all-day child care at their meetings for years, and the Society for American Gastrointestinal and Endoscopic Surgeons (SAGES) has recently followed suit. With such support, I have taken my toddler with me to nearly all my professional meetings during the first 3 years of her life, and I don’t hide the fact that being a wife and mother are priorities for me. These new roles have not significantly compromised my career. In fact, they’ve helped me to focus and set priorities. Since the birth of my child, I have been asked to serve in an institutional leadership role as research director for our patient portal, and my first R01 grant proposal was submitted and successfully funded.
Gretchen Purcell Jackson, M.D, Ph.D., FACS, is assistant professor of surgery, pediatrics, and biomedical informatics, Vanderbilt University, Nashville, Tenn.
The issues of childbearing and fertility are complex for women surgeons. It was not clear from the presentation whether the respondents were all in practice. If the respondents are all primarily from the baby-boomer generation, it may alter the survey results. It would be interesting to see the response of current women surgery trainees and to determine whether this is really more of a generational issue or whether the issues relate to the surgical lifestyle.
Certainly, the knowledge of fertility options, financial stability, and ease of access to specialists may also encourage women surgeons to seek intervention at a higher rate than that of the general population.
There is never a perfect time to have children, but there are certainly times that are not ideal. I am married, and have three children, ages 8, 13, and 18 years. I had no difficulties with any of my pregnancies. I had my first child at the completion of my fellowship, and the other two while in academic practice. I worked up until the day I went into labor during training, and up until 2 weeks prior to my due date when I was in practice. I did modify my surgical schedule to avoid long or complex cases during my last months when I was in practice, whereas, this was not necessary during my training. I was fortunate to have partners who were accommodating.
Comparing surgeons to other professionals from the same generation would give better information as to whether the field itself is the issue, or whether this is more of a generational issue for professionals. Many of my friends both in medical and nonmedical professional fields also waited until early 30s to get married and have children, while others chose not to have any children to prioritize their careers. When I was in training, there were many places in which overt prejudice against women still existed. It was difficult enough to be "equal" to your male colleagues without having to deal with concerns of dumping work on them because of a pregnancy or the potential reaction from your chair or program director. Luckily, not all programs were like that. It was also commonplace to work upward of 100 hours per week.
Finding time for relationships, surviving a pregnancy, surviving a surgical residency, and not putting a pregnancy at risk was more difficult under those conditions.
Times continue to change, and pregnancy during training is becoming more common, especially in larger surgery programs. The acknowledgment that not only women, but also men of the younger generation are not willing to work to the exclusion of family, and outside life is changing the field, as is the fact that 50% of graduating medical students are women.
The ability to have children during training has also been facilitated by the duty hour rules, as well as by having more women faculty. We need to continue to examine ways to encourage the work-life blend in surgical fields, not only for women, but for men as well, or risk losing a large section of the class to "lifestyle fields." Having resources within the institutions such as child care, with hours compatible with working resident schedules would go a long way toward facilitating this blend. The finding that women surgeons availed themselves of fertility specialists more frequently than the general population did is not necessarily a concern. The question is whether the rate of infertility in women surgeons is truly significantly higher than that of their peers in other professional areas. The main issues to address remain how to facilitate childbearing for those women surgeons who wish to have a family, and how to facilitate the work-life blend for ourselves and all of our trainees.
Linda Harris, M.D., FACS, is division chief, vascular surgery, State University of New York at Buffalo.
The decisions about childbearing that women surgeons make are in many ways similar to those of other career-oriented women, as Dr. Harris points out. The dilemmas involved in this area are perhaps more extreme in the field of surgery, compared with other professions because to the pressures and length of training that are associated with surgery. It is a topic that deserves more attention, since from a very general perspective, it is difficult for a trainee to project out the implications of his or her choices in creating a family or having children 5 or more years beyond training. Decisions around childbearing are also complex, nuanced, highly personal, and variable to each person’s life experience. I had one child during my residency and another during my practice, which in each case had its own advantages and challenges. In my case, the most important factor to making it work as well as it has was having a very supportive spouse.
Genevieve Melton-Meaux, M.D., FACS, is an associate professor of surgery, University of Minnesota, Minneapolis.
As a medical student applying into a surgical subspecialty, I am sobered but certainly not surprised by these findings. I approach my career and desire for a family with wary readiness to face a lifetime of setting tough priorities that at times may feel isolating. Is a career as a surgeon incompatible with pregnancy, lasting marriage, and well-behaved children? I would say no, though it depends on who your partner is, where you work, and careful timing. With increasing numbers of females entering surgery who refuse to compromise mothering their own children, the work environment will have to change. Part of this changing landscape may mean that female surgeons will undergo assisted reproductive technologies at higher rates than their non-surgeon counterparts. It may mean that shift work becomes more acceptable. Regardless, the changes we create as a medical community should affect both men and women; we should be wary of designing special tracks or programs that can lend to further isolation and hand-waving of leadership. To ensure gender equity in surgery we are asking for institutional change – something for which there is never a perfect or easy time. Surgeons simply have to make it a priority.
Charlotte R. Gamble is a fourth year medical student at the University of Michigan, Ann Arbor
Ten-year outcomes for ablation in atrial fibrillation impressive
DALLAS – At 10 years after their procedures, the rate of freedom from atrial fibrillation and atrial tachycardia was 87% in 513 patients who underwent pulmonary vein antrum isolation for drug-refractory paroxysmal atrial fibrillation at a single high-volume center in Texas.
After a single radiofrequency ablation procedure, 59% of patients remained arrhythmia free for the full decade and another 28% of the cohort was rendered arrhythmia free after an average of two repeat ablation procedures, Dr. Pasquale Santangeli reported at the American Heart Association scientific sessions.
A particularly striking finding in this series was the low 4% rate of recurrent atrial arrhythmias during years 3-6 of follow-up, and the 5% rate between years 6 and 10. Those late recurrence rates are much lower than those in previous reports from other centers. The likely explanation lies in the fact that electrophysiologists at the Austin center routinely extended their pulmonary vein antrum isolation to the posterior wall and performed empiric isolation of the superior vena cava in all patients. Other centers reporting long-term outcomes generally performed segmental or less extensive antral isolation, observed Dr. Santangeli of the Texas Cardiac Arrhythmia Institute at St. David’s Medical Center in Austin, Tex., and the University of Foggia (Italy).
Follow-up, including Holter monitoring, was performed every 3 months during year 1 and every 6-9 months thereafter. The rate of recurrent atrial arrhythmia was 21% at 1 year and 11% during years 1-3.
All patients with a recurrence were offered a repeat procedure, and 74% of them underwent repeat ablation. Reconnection in the pulmonary vein antrum was found in 31% of patients at the time of their first repeat procedure and in no patients who underwent a second repeat ablation.
Patients with recurrent atrial arrhythmia after two failed procedures underwent a high-dose isoproterenol challenge to identify nonpulmonary vein triggers, which were then targeted for ablation. The predictors of very late recurrence due to nonpulmonary vein triggers were increased left atrial size, obesity, and female gender.
Dr. Santangeli reported having no financial conflicts in connection with this study, which was honored as the top presentation by an early career investigator in the core area of heart rhythm disorders and resuscitation science at the annual meeting.
DALLAS – At 10 years after their procedures, the rate of freedom from atrial fibrillation and atrial tachycardia was 87% in 513 patients who underwent pulmonary vein antrum isolation for drug-refractory paroxysmal atrial fibrillation at a single high-volume center in Texas.
After a single radiofrequency ablation procedure, 59% of patients remained arrhythmia free for the full decade and another 28% of the cohort was rendered arrhythmia free after an average of two repeat ablation procedures, Dr. Pasquale Santangeli reported at the American Heart Association scientific sessions.
A particularly striking finding in this series was the low 4% rate of recurrent atrial arrhythmias during years 3-6 of follow-up, and the 5% rate between years 6 and 10. Those late recurrence rates are much lower than those in previous reports from other centers. The likely explanation lies in the fact that electrophysiologists at the Austin center routinely extended their pulmonary vein antrum isolation to the posterior wall and performed empiric isolation of the superior vena cava in all patients. Other centers reporting long-term outcomes generally performed segmental or less extensive antral isolation, observed Dr. Santangeli of the Texas Cardiac Arrhythmia Institute at St. David’s Medical Center in Austin, Tex., and the University of Foggia (Italy).
Follow-up, including Holter monitoring, was performed every 3 months during year 1 and every 6-9 months thereafter. The rate of recurrent atrial arrhythmia was 21% at 1 year and 11% during years 1-3.
All patients with a recurrence were offered a repeat procedure, and 74% of them underwent repeat ablation. Reconnection in the pulmonary vein antrum was found in 31% of patients at the time of their first repeat procedure and in no patients who underwent a second repeat ablation.
Patients with recurrent atrial arrhythmia after two failed procedures underwent a high-dose isoproterenol challenge to identify nonpulmonary vein triggers, which were then targeted for ablation. The predictors of very late recurrence due to nonpulmonary vein triggers were increased left atrial size, obesity, and female gender.
Dr. Santangeli reported having no financial conflicts in connection with this study, which was honored as the top presentation by an early career investigator in the core area of heart rhythm disorders and resuscitation science at the annual meeting.
DALLAS – At 10 years after their procedures, the rate of freedom from atrial fibrillation and atrial tachycardia was 87% in 513 patients who underwent pulmonary vein antrum isolation for drug-refractory paroxysmal atrial fibrillation at a single high-volume center in Texas.
After a single radiofrequency ablation procedure, 59% of patients remained arrhythmia free for the full decade and another 28% of the cohort was rendered arrhythmia free after an average of two repeat ablation procedures, Dr. Pasquale Santangeli reported at the American Heart Association scientific sessions.
A particularly striking finding in this series was the low 4% rate of recurrent atrial arrhythmias during years 3-6 of follow-up, and the 5% rate between years 6 and 10. Those late recurrence rates are much lower than those in previous reports from other centers. The likely explanation lies in the fact that electrophysiologists at the Austin center routinely extended their pulmonary vein antrum isolation to the posterior wall and performed empiric isolation of the superior vena cava in all patients. Other centers reporting long-term outcomes generally performed segmental or less extensive antral isolation, observed Dr. Santangeli of the Texas Cardiac Arrhythmia Institute at St. David’s Medical Center in Austin, Tex., and the University of Foggia (Italy).
Follow-up, including Holter monitoring, was performed every 3 months during year 1 and every 6-9 months thereafter. The rate of recurrent atrial arrhythmia was 21% at 1 year and 11% during years 1-3.
All patients with a recurrence were offered a repeat procedure, and 74% of them underwent repeat ablation. Reconnection in the pulmonary vein antrum was found in 31% of patients at the time of their first repeat procedure and in no patients who underwent a second repeat ablation.
Patients with recurrent atrial arrhythmia after two failed procedures underwent a high-dose isoproterenol challenge to identify nonpulmonary vein triggers, which were then targeted for ablation. The predictors of very late recurrence due to nonpulmonary vein triggers were increased left atrial size, obesity, and female gender.
Dr. Santangeli reported having no financial conflicts in connection with this study, which was honored as the top presentation by an early career investigator in the core area of heart rhythm disorders and resuscitation science at the annual meeting.
AT THE AHA SCIENTIFIC SESSIONS
Major finding: A decade after 513 patients underwent extensive pulmonary vein antrum isolation for drug-resistant paroxysmal atrial fibrillation, 87% were free of atrial fibrillation/atrial tachycardia, including 59% with single-procedure arrhythmia-free survival.
Data source: A retrospective case series involving 513 patients who underwent pulmonary vein antrum isolation during 2000-2002 at a single high-volume center.
Disclosures: The presenter reported having no financial conflicts.