User login
Official Newspaper of the American College of Surgeons
Factual and proximate cause
Question: Mrs. P sustained multiple fractures after a drunk driver struck her car. The orthopedic surgeon accidentally nicked her femoral artery during surgery, which resulted in profuse hemorrhage requiring six units of packed red blood cells. Although she survived, Mrs. P was left with irreversible renal failure, and she now requires lifelong dialysis. Which of the following is correct?
A. The drunk driver’s negligence may be both a factual and proximate cause of all of Mrs. P’s injuries.
B. The surgeon’s action may be deemed a factual, a concurring, or a superseding cause.
C. The surgeon will be successfully sued for malpractice.
D. Only A and B are correct.
E. All are correct.
Answer: D. The surgeon may be successfully sued for malpractice if the nicking of the artery is shown to be a negligent act. This is by no means a foregone conclusion, as a bad outcome is not necessarily indicative of negligence. The measure of legal negligence is what is to be ordinarily expected of a surgeon under similar situations.
For example, expert testimony may establish exculpatory circumstances such as an obscured surgical field, anomalous anatomy, emergency conditions, etc., that would free the surgeon from liability.
Causation issues have long plagued courts and scholars, earning epithets like "a thicket of complexities" and "a simplicity that is deceptive." Causation inquires into both factual and proximate cause. Factual cause deals with whether there is a physical and sequential cause-effect relationship between a defendant’s negligence and a plaintiff’s injuries. It uses the "but-for" test, which stipulates that the defendant’s conduct is a factual cause of a plaintiff’s injuries if the plaintiff’s harm would not have occurred but for defendant’s conduct, i.e., in the absence of the defendant’s tortious conduct.
A recent case is illustrative (BNM v. National University of Singapore, [2014] SGHC 05). An obese, middle-aged man drowned while swimming in the university pool. Lifeguards were on duty, but they were neither aware of where the emergency equipment was kept nor adequately trained in cardiopulmonary resuscitation. Efforts to revive the swimmer failed.
At autopsy, the victim was found to have cardiomegaly and advanced coronary artery disease, with old foci of myocardial scarring. The coroner testified that the victim probably suffered a major cardiac event, such as an arrhythmia, prior to drowning.
On the issue of causation, the court held that because of his severe underlying heart disease, the deceased was not likely to have survived, even if the lifeguards had acted more promptly, i.e., the negligent lifeguards did not factually cause the victim’s death.
A more important inquiry into causal connectivity is captured in the term "proximate cause," which is meant to prevent indeterminate liability. It is sometimes referred to as legal cause.
Unfortunately, there is no bright line to define what constitutes a sufficient causal nexus, and courts are therefore occasionally forced to base their decision on their sense of practical policy and justice. In some cases, an intervening event results in causing, or aggravating, harm suffered by the victim, but the original defendant may be freed of liability if the intervening event constitutes a superseding cause, i.e. unforeseeable event with unforeseeable results.
The opposite is a concurring cause. For example, rescuers may sometimes act negligently following a tortious event leading to aggravated injuries. If such conduct and damages were deemed foreseeable, that would constitute a concurring cause, and the initial wrongdoer then becomes liable for both the original and any aggravated injuries.
A variant of proximate cause is when the harm suffered is a natural expectation of the underlying condition, and the wrongdoer’s negligence simply deprived the victim of some chance of reducing that risk. This is known as the "loss of a chance" doctrine, which has been variously considered a part of causation analysis, a separate tort, or a means to apportion damages.
It asserts that the damage or loss that will materialize or had already materialized, could have been prevented or improved upon – had the victim not been deprived of an opportunity. Loss of a chance is simply another way of saying that the defendant’s conduct has increased the risk of harm to the plaintiff.
The doctrine is well established in contract law, especially where only economic losses are at issue, the key requirement there being that the lost opportunity be real or substantial, and not speculative. The seminal case, Chaplin v. Hicks ([1911] 2 KB 786), dealt with a late notification in a competition, which caused a plaintiff to lose her chance as a finalist to win a prize. The court ruled that the damage was not too remote, and the plaintiff did not have to prove that she would have won the competition.
In clinical negligence, allegations of loss of a chance often arise from an omission to treat or a failure to diagnose, which in turn may deprive the patient of an opportunity of a better outcome. In some U.S. and most Commonwealth jurisdictions, its successful application requires that the underlying condition prior to an individual’s negligence be associated with a better than even chance of cure to begin with.
The controversy arises over what level of risk reduction or lost opportunity is necessary to constitute proximate causation. How large the chance of an adverse outcome and how much of a reduction in that chance are required as a matter of law? Some courts assert that the lost opportunity is relevant only if the plaintiff’s prognosis for survival is better than 50% to begin with, whereas others reject this numerical imperative, especially in cases alleging a delayed diagnosis of cancer.
Proximate cause is the law’s intended mechanism to limit indeterminate liability. Thus, whether a defendant’s negligent conduct constitutes proximate cause is often dispositive in personal injury litigation. However, the term is frequently misunderstood, and has caused much confusion because it has sometimes been used interchangeably with legal cause, or used to include factual cause. And, of course, there can be more than one proximate cause for any given injury.
Reflecting this complexity, the California Supreme Court now disallows confusing jury instructions regarding proximate cause, suggesting instead that the jury be simply directed to determine whether the defendant’s conduct was a contributory factor in the plaintiff’s injury (Mitchell v. Gonzales, 819 P.2d 872 [Cal. 1991]).
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical or legal advice. It is adapted from the author’s book, "Medical Malpractice: Understanding the Law, Managing the Risk" (2006) and his Halsbury treatise, "Medical Negligence and Professional Misconduct" (2012). For additional information, readers may contact the author at [email protected].
Question: Mrs. P sustained multiple fractures after a drunk driver struck her car. The orthopedic surgeon accidentally nicked her femoral artery during surgery, which resulted in profuse hemorrhage requiring six units of packed red blood cells. Although she survived, Mrs. P was left with irreversible renal failure, and she now requires lifelong dialysis. Which of the following is correct?
A. The drunk driver’s negligence may be both a factual and proximate cause of all of Mrs. P’s injuries.
B. The surgeon’s action may be deemed a factual, a concurring, or a superseding cause.
C. The surgeon will be successfully sued for malpractice.
D. Only A and B are correct.
E. All are correct.
Answer: D. The surgeon may be successfully sued for malpractice if the nicking of the artery is shown to be a negligent act. This is by no means a foregone conclusion, as a bad outcome is not necessarily indicative of negligence. The measure of legal negligence is what is to be ordinarily expected of a surgeon under similar situations.
For example, expert testimony may establish exculpatory circumstances such as an obscured surgical field, anomalous anatomy, emergency conditions, etc., that would free the surgeon from liability.
Causation issues have long plagued courts and scholars, earning epithets like "a thicket of complexities" and "a simplicity that is deceptive." Causation inquires into both factual and proximate cause. Factual cause deals with whether there is a physical and sequential cause-effect relationship between a defendant’s negligence and a plaintiff’s injuries. It uses the "but-for" test, which stipulates that the defendant’s conduct is a factual cause of a plaintiff’s injuries if the plaintiff’s harm would not have occurred but for defendant’s conduct, i.e., in the absence of the defendant’s tortious conduct.
A recent case is illustrative (BNM v. National University of Singapore, [2014] SGHC 05). An obese, middle-aged man drowned while swimming in the university pool. Lifeguards were on duty, but they were neither aware of where the emergency equipment was kept nor adequately trained in cardiopulmonary resuscitation. Efforts to revive the swimmer failed.
At autopsy, the victim was found to have cardiomegaly and advanced coronary artery disease, with old foci of myocardial scarring. The coroner testified that the victim probably suffered a major cardiac event, such as an arrhythmia, prior to drowning.
On the issue of causation, the court held that because of his severe underlying heart disease, the deceased was not likely to have survived, even if the lifeguards had acted more promptly, i.e., the negligent lifeguards did not factually cause the victim’s death.
A more important inquiry into causal connectivity is captured in the term "proximate cause," which is meant to prevent indeterminate liability. It is sometimes referred to as legal cause.
Unfortunately, there is no bright line to define what constitutes a sufficient causal nexus, and courts are therefore occasionally forced to base their decision on their sense of practical policy and justice. In some cases, an intervening event results in causing, or aggravating, harm suffered by the victim, but the original defendant may be freed of liability if the intervening event constitutes a superseding cause, i.e. unforeseeable event with unforeseeable results.
The opposite is a concurring cause. For example, rescuers may sometimes act negligently following a tortious event leading to aggravated injuries. If such conduct and damages were deemed foreseeable, that would constitute a concurring cause, and the initial wrongdoer then becomes liable for both the original and any aggravated injuries.
A variant of proximate cause is when the harm suffered is a natural expectation of the underlying condition, and the wrongdoer’s negligence simply deprived the victim of some chance of reducing that risk. This is known as the "loss of a chance" doctrine, which has been variously considered a part of causation analysis, a separate tort, or a means to apportion damages.
It asserts that the damage or loss that will materialize or had already materialized, could have been prevented or improved upon – had the victim not been deprived of an opportunity. Loss of a chance is simply another way of saying that the defendant’s conduct has increased the risk of harm to the plaintiff.
The doctrine is well established in contract law, especially where only economic losses are at issue, the key requirement there being that the lost opportunity be real or substantial, and not speculative. The seminal case, Chaplin v. Hicks ([1911] 2 KB 786), dealt with a late notification in a competition, which caused a plaintiff to lose her chance as a finalist to win a prize. The court ruled that the damage was not too remote, and the plaintiff did not have to prove that she would have won the competition.
In clinical negligence, allegations of loss of a chance often arise from an omission to treat or a failure to diagnose, which in turn may deprive the patient of an opportunity of a better outcome. In some U.S. and most Commonwealth jurisdictions, its successful application requires that the underlying condition prior to an individual’s negligence be associated with a better than even chance of cure to begin with.
The controversy arises over what level of risk reduction or lost opportunity is necessary to constitute proximate causation. How large the chance of an adverse outcome and how much of a reduction in that chance are required as a matter of law? Some courts assert that the lost opportunity is relevant only if the plaintiff’s prognosis for survival is better than 50% to begin with, whereas others reject this numerical imperative, especially in cases alleging a delayed diagnosis of cancer.
Proximate cause is the law’s intended mechanism to limit indeterminate liability. Thus, whether a defendant’s negligent conduct constitutes proximate cause is often dispositive in personal injury litigation. However, the term is frequently misunderstood, and has caused much confusion because it has sometimes been used interchangeably with legal cause, or used to include factual cause. And, of course, there can be more than one proximate cause for any given injury.
Reflecting this complexity, the California Supreme Court now disallows confusing jury instructions regarding proximate cause, suggesting instead that the jury be simply directed to determine whether the defendant’s conduct was a contributory factor in the plaintiff’s injury (Mitchell v. Gonzales, 819 P.2d 872 [Cal. 1991]).
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical or legal advice. It is adapted from the author’s book, "Medical Malpractice: Understanding the Law, Managing the Risk" (2006) and his Halsbury treatise, "Medical Negligence and Professional Misconduct" (2012). For additional information, readers may contact the author at [email protected].
Question: Mrs. P sustained multiple fractures after a drunk driver struck her car. The orthopedic surgeon accidentally nicked her femoral artery during surgery, which resulted in profuse hemorrhage requiring six units of packed red blood cells. Although she survived, Mrs. P was left with irreversible renal failure, and she now requires lifelong dialysis. Which of the following is correct?
A. The drunk driver’s negligence may be both a factual and proximate cause of all of Mrs. P’s injuries.
B. The surgeon’s action may be deemed a factual, a concurring, or a superseding cause.
C. The surgeon will be successfully sued for malpractice.
D. Only A and B are correct.
E. All are correct.
Answer: D. The surgeon may be successfully sued for malpractice if the nicking of the artery is shown to be a negligent act. This is by no means a foregone conclusion, as a bad outcome is not necessarily indicative of negligence. The measure of legal negligence is what is to be ordinarily expected of a surgeon under similar situations.
For example, expert testimony may establish exculpatory circumstances such as an obscured surgical field, anomalous anatomy, emergency conditions, etc., that would free the surgeon from liability.
Causation issues have long plagued courts and scholars, earning epithets like "a thicket of complexities" and "a simplicity that is deceptive." Causation inquires into both factual and proximate cause. Factual cause deals with whether there is a physical and sequential cause-effect relationship between a defendant’s negligence and a plaintiff’s injuries. It uses the "but-for" test, which stipulates that the defendant’s conduct is a factual cause of a plaintiff’s injuries if the plaintiff’s harm would not have occurred but for defendant’s conduct, i.e., in the absence of the defendant’s tortious conduct.
A recent case is illustrative (BNM v. National University of Singapore, [2014] SGHC 05). An obese, middle-aged man drowned while swimming in the university pool. Lifeguards were on duty, but they were neither aware of where the emergency equipment was kept nor adequately trained in cardiopulmonary resuscitation. Efforts to revive the swimmer failed.
At autopsy, the victim was found to have cardiomegaly and advanced coronary artery disease, with old foci of myocardial scarring. The coroner testified that the victim probably suffered a major cardiac event, such as an arrhythmia, prior to drowning.
On the issue of causation, the court held that because of his severe underlying heart disease, the deceased was not likely to have survived, even if the lifeguards had acted more promptly, i.e., the negligent lifeguards did not factually cause the victim’s death.
A more important inquiry into causal connectivity is captured in the term "proximate cause," which is meant to prevent indeterminate liability. It is sometimes referred to as legal cause.
Unfortunately, there is no bright line to define what constitutes a sufficient causal nexus, and courts are therefore occasionally forced to base their decision on their sense of practical policy and justice. In some cases, an intervening event results in causing, or aggravating, harm suffered by the victim, but the original defendant may be freed of liability if the intervening event constitutes a superseding cause, i.e. unforeseeable event with unforeseeable results.
The opposite is a concurring cause. For example, rescuers may sometimes act negligently following a tortious event leading to aggravated injuries. If such conduct and damages were deemed foreseeable, that would constitute a concurring cause, and the initial wrongdoer then becomes liable for both the original and any aggravated injuries.
A variant of proximate cause is when the harm suffered is a natural expectation of the underlying condition, and the wrongdoer’s negligence simply deprived the victim of some chance of reducing that risk. This is known as the "loss of a chance" doctrine, which has been variously considered a part of causation analysis, a separate tort, or a means to apportion damages.
It asserts that the damage or loss that will materialize or had already materialized, could have been prevented or improved upon – had the victim not been deprived of an opportunity. Loss of a chance is simply another way of saying that the defendant’s conduct has increased the risk of harm to the plaintiff.
The doctrine is well established in contract law, especially where only economic losses are at issue, the key requirement there being that the lost opportunity be real or substantial, and not speculative. The seminal case, Chaplin v. Hicks ([1911] 2 KB 786), dealt with a late notification in a competition, which caused a plaintiff to lose her chance as a finalist to win a prize. The court ruled that the damage was not too remote, and the plaintiff did not have to prove that she would have won the competition.
In clinical negligence, allegations of loss of a chance often arise from an omission to treat or a failure to diagnose, which in turn may deprive the patient of an opportunity of a better outcome. In some U.S. and most Commonwealth jurisdictions, its successful application requires that the underlying condition prior to an individual’s negligence be associated with a better than even chance of cure to begin with.
The controversy arises over what level of risk reduction or lost opportunity is necessary to constitute proximate causation. How large the chance of an adverse outcome and how much of a reduction in that chance are required as a matter of law? Some courts assert that the lost opportunity is relevant only if the plaintiff’s prognosis for survival is better than 50% to begin with, whereas others reject this numerical imperative, especially in cases alleging a delayed diagnosis of cancer.
Proximate cause is the law’s intended mechanism to limit indeterminate liability. Thus, whether a defendant’s negligent conduct constitutes proximate cause is often dispositive in personal injury litigation. However, the term is frequently misunderstood, and has caused much confusion because it has sometimes been used interchangeably with legal cause, or used to include factual cause. And, of course, there can be more than one proximate cause for any given injury.
Reflecting this complexity, the California Supreme Court now disallows confusing jury instructions regarding proximate cause, suggesting instead that the jury be simply directed to determine whether the defendant’s conduct was a contributory factor in the plaintiff’s injury (Mitchell v. Gonzales, 819 P.2d 872 [Cal. 1991]).
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical or legal advice. It is adapted from the author’s book, "Medical Malpractice: Understanding the Law, Managing the Risk" (2006) and his Halsbury treatise, "Medical Negligence and Professional Misconduct" (2012). For additional information, readers may contact the author at [email protected].
The future of obesity treatments could include endoscopically placed devices
WASHINGTON – Endoscopically placed devices that include intragastric balloons and gastrointestinal liners are being evaluated for the treatment of obesity and could eventually fill some of the current void in treatment options that fall between lifestyle changes and surgical treatments.
These types of devices are the new paradigm for obesity treatments, and many are already available in Europe and elsewhere, Dr. Richard Rothstein said at a public workshop cosponsored by the Food and Drug Administration and the American Gastroenterological Association. Some have been evaluated in studies that use diabetes control measures as the main outcome endpoint, rather than weight loss, he noted.
Dr. Rothstein, the Joseph M. Huber Professor of Medicine and chair of the department of medicine, Geisel School of Medicine at Dartmouth, Hanover, N.H., provided an overview of some of the devices, which include sleeves, techniques, and devices used to reduce gastric volume such as balloons, and surgical tools used to sew or staple the stomach together.
Endoscopic treatments for obesity are less invasive, less expensive, reversible, and are performed as outpatient procedures, he said, noting that patients may be willing to pay for these procedures out of pocket.
In early studies, the endoscopically delivered EndoBarrier resulted in weight loss and was well tolerated, said Dr. Rothstein, who is an adviser to the manufacturer, GI Dynamics. This is a flexible, tube-shaped liner that forms a physical barrier between food and the intestinal wall, according to the manufacturer. The device, which mimics malabsorptive surgical procedures, has been available for 3 years in Europe, Australia, and South America and is being evaluated in a pivotal U.S. study, the ENDO trial, for treating patients who are obese and have uncontrolled type 2 diabetes.
Andy Levine, who was chief technology officer at GI Dynamics and is now an adviser to the company, said that to date, the EndoBarrier, which completely covers the duodenum and the proximal jejunum and is anchored in the duodenal bulb distal to the pylorus, has been placed in more than 1,300 people worldwide. The device creates a "a complete bypass," so the food from the stomach goes through the flexible soft liner, driven by peristalsis, and the bile and pancreatic enzymes pass on the outside of the liner, with all mixing in the bowel, said Mr. Levine, who is now the leader of business development for medical devices and robotics at the Wyss Institute for Biologically Inspired Engineering at Harvard University, Boston.
In studies, improvements in type 2 diabetes measures are being used as endpoints, since showing improvement in obesity comorbidities was determined to be important for reimbursement, "and the technology had a unique impact on diabetes."
Based on experience with the device to date, Mr. Levine said that for the first 9-10 months, patients lose about 10%-20% of their body weight and many have been able to discontinue insulin and stay on oral therapy. Following removal of the device at 1 year, there is a slow rebound in weight and hemoglobin A1c values. While this might appear to be a temporary solution for a chronic problem, "we’re certainly treating it, and in some ways may be reversing the disease at least for awhile," he said, pointing out that the device addresses the need to break the cycle of continuing weight gain and helps patients discontinue diabetes medications, especially insulin.
A variety of newer, improved versions of endoscopically placed balloons are also being studied, including the ReShape, a double balloon device, Dr. Rothstein said.
During the same session, Richard Thompson, president and CEO of ReShape Medical, a small venture capital–funded company, said that the ReShape Duo intragastric device is made up of two balloons that contain a total of about 900 mL of fluid, which occupy space in the stomach without the discomfort and distension that can occur with one large balloon. This device is designed to reduce the risk of migration, which can occurs when a balloon deflates and migrates to the intestine where it can cause a blockage. If one balloon deflates the other remains inflated, and because there is blue dye in the balloons, when one deflates, the dye is visible in urine to alert the patient, he noted. ReShape Duo has been available in Europe for more than 2 years.
The U.S. trial evaluating the device in 325 patients is almost completed, and the company recently announced that the primary endpoints that assessed weight loss and responder rates had been met. The company plans to file for FDA approval in the second quarter of 2014.
Dr. Rothstein said that other nonsurgical devices being developed include those that do not require endoscopic placement, such as bezoars or balloons that are swallowed by the patient and function as temporary "space-occupying devices," he said. One example is a capsule that contains beads, which swell up in the stomach and take up space after the capsule is swallowed – which may affect satiety and result in weight loss if ingested before a meal, he said.
Techniques that bring aspects of the proximal stomach together represent another approach, using devices to sew and stitch up the stomach, compartmentalizing the stomach, creating "if you will, an endoscopic gastric sleeve," he said, noting there are not much data available on this approach.
Data from studies that are sham-controlled and have adequate sample sizes are needed to determine the role of these therapies, as they are developed, and they need to be shown to have "reasonable durability," and a safety profile with minimal complications, with cost-effectiveness data, Dr. Rothstein said. And as they become available, it will be necessary to "tease out" which patient groups respond best to which therapy, such as balloons or bezoars, or gastric bypass surgery, he added.
WASHINGTON – Endoscopically placed devices that include intragastric balloons and gastrointestinal liners are being evaluated for the treatment of obesity and could eventually fill some of the current void in treatment options that fall between lifestyle changes and surgical treatments.
These types of devices are the new paradigm for obesity treatments, and many are already available in Europe and elsewhere, Dr. Richard Rothstein said at a public workshop cosponsored by the Food and Drug Administration and the American Gastroenterological Association. Some have been evaluated in studies that use diabetes control measures as the main outcome endpoint, rather than weight loss, he noted.
Dr. Rothstein, the Joseph M. Huber Professor of Medicine and chair of the department of medicine, Geisel School of Medicine at Dartmouth, Hanover, N.H., provided an overview of some of the devices, which include sleeves, techniques, and devices used to reduce gastric volume such as balloons, and surgical tools used to sew or staple the stomach together.
Endoscopic treatments for obesity are less invasive, less expensive, reversible, and are performed as outpatient procedures, he said, noting that patients may be willing to pay for these procedures out of pocket.
In early studies, the endoscopically delivered EndoBarrier resulted in weight loss and was well tolerated, said Dr. Rothstein, who is an adviser to the manufacturer, GI Dynamics. This is a flexible, tube-shaped liner that forms a physical barrier between food and the intestinal wall, according to the manufacturer. The device, which mimics malabsorptive surgical procedures, has been available for 3 years in Europe, Australia, and South America and is being evaluated in a pivotal U.S. study, the ENDO trial, for treating patients who are obese and have uncontrolled type 2 diabetes.
Andy Levine, who was chief technology officer at GI Dynamics and is now an adviser to the company, said that to date, the EndoBarrier, which completely covers the duodenum and the proximal jejunum and is anchored in the duodenal bulb distal to the pylorus, has been placed in more than 1,300 people worldwide. The device creates a "a complete bypass," so the food from the stomach goes through the flexible soft liner, driven by peristalsis, and the bile and pancreatic enzymes pass on the outside of the liner, with all mixing in the bowel, said Mr. Levine, who is now the leader of business development for medical devices and robotics at the Wyss Institute for Biologically Inspired Engineering at Harvard University, Boston.
In studies, improvements in type 2 diabetes measures are being used as endpoints, since showing improvement in obesity comorbidities was determined to be important for reimbursement, "and the technology had a unique impact on diabetes."
Based on experience with the device to date, Mr. Levine said that for the first 9-10 months, patients lose about 10%-20% of their body weight and many have been able to discontinue insulin and stay on oral therapy. Following removal of the device at 1 year, there is a slow rebound in weight and hemoglobin A1c values. While this might appear to be a temporary solution for a chronic problem, "we’re certainly treating it, and in some ways may be reversing the disease at least for awhile," he said, pointing out that the device addresses the need to break the cycle of continuing weight gain and helps patients discontinue diabetes medications, especially insulin.
A variety of newer, improved versions of endoscopically placed balloons are also being studied, including the ReShape, a double balloon device, Dr. Rothstein said.
During the same session, Richard Thompson, president and CEO of ReShape Medical, a small venture capital–funded company, said that the ReShape Duo intragastric device is made up of two balloons that contain a total of about 900 mL of fluid, which occupy space in the stomach without the discomfort and distension that can occur with one large balloon. This device is designed to reduce the risk of migration, which can occurs when a balloon deflates and migrates to the intestine where it can cause a blockage. If one balloon deflates the other remains inflated, and because there is blue dye in the balloons, when one deflates, the dye is visible in urine to alert the patient, he noted. ReShape Duo has been available in Europe for more than 2 years.
The U.S. trial evaluating the device in 325 patients is almost completed, and the company recently announced that the primary endpoints that assessed weight loss and responder rates had been met. The company plans to file for FDA approval in the second quarter of 2014.
Dr. Rothstein said that other nonsurgical devices being developed include those that do not require endoscopic placement, such as bezoars or balloons that are swallowed by the patient and function as temporary "space-occupying devices," he said. One example is a capsule that contains beads, which swell up in the stomach and take up space after the capsule is swallowed – which may affect satiety and result in weight loss if ingested before a meal, he said.
Techniques that bring aspects of the proximal stomach together represent another approach, using devices to sew and stitch up the stomach, compartmentalizing the stomach, creating "if you will, an endoscopic gastric sleeve," he said, noting there are not much data available on this approach.
Data from studies that are sham-controlled and have adequate sample sizes are needed to determine the role of these therapies, as they are developed, and they need to be shown to have "reasonable durability," and a safety profile with minimal complications, with cost-effectiveness data, Dr. Rothstein said. And as they become available, it will be necessary to "tease out" which patient groups respond best to which therapy, such as balloons or bezoars, or gastric bypass surgery, he added.
WASHINGTON – Endoscopically placed devices that include intragastric balloons and gastrointestinal liners are being evaluated for the treatment of obesity and could eventually fill some of the current void in treatment options that fall between lifestyle changes and surgical treatments.
These types of devices are the new paradigm for obesity treatments, and many are already available in Europe and elsewhere, Dr. Richard Rothstein said at a public workshop cosponsored by the Food and Drug Administration and the American Gastroenterological Association. Some have been evaluated in studies that use diabetes control measures as the main outcome endpoint, rather than weight loss, he noted.
Dr. Rothstein, the Joseph M. Huber Professor of Medicine and chair of the department of medicine, Geisel School of Medicine at Dartmouth, Hanover, N.H., provided an overview of some of the devices, which include sleeves, techniques, and devices used to reduce gastric volume such as balloons, and surgical tools used to sew or staple the stomach together.
Endoscopic treatments for obesity are less invasive, less expensive, reversible, and are performed as outpatient procedures, he said, noting that patients may be willing to pay for these procedures out of pocket.
In early studies, the endoscopically delivered EndoBarrier resulted in weight loss and was well tolerated, said Dr. Rothstein, who is an adviser to the manufacturer, GI Dynamics. This is a flexible, tube-shaped liner that forms a physical barrier between food and the intestinal wall, according to the manufacturer. The device, which mimics malabsorptive surgical procedures, has been available for 3 years in Europe, Australia, and South America and is being evaluated in a pivotal U.S. study, the ENDO trial, for treating patients who are obese and have uncontrolled type 2 diabetes.
Andy Levine, who was chief technology officer at GI Dynamics and is now an adviser to the company, said that to date, the EndoBarrier, which completely covers the duodenum and the proximal jejunum and is anchored in the duodenal bulb distal to the pylorus, has been placed in more than 1,300 people worldwide. The device creates a "a complete bypass," so the food from the stomach goes through the flexible soft liner, driven by peristalsis, and the bile and pancreatic enzymes pass on the outside of the liner, with all mixing in the bowel, said Mr. Levine, who is now the leader of business development for medical devices and robotics at the Wyss Institute for Biologically Inspired Engineering at Harvard University, Boston.
In studies, improvements in type 2 diabetes measures are being used as endpoints, since showing improvement in obesity comorbidities was determined to be important for reimbursement, "and the technology had a unique impact on diabetes."
Based on experience with the device to date, Mr. Levine said that for the first 9-10 months, patients lose about 10%-20% of their body weight and many have been able to discontinue insulin and stay on oral therapy. Following removal of the device at 1 year, there is a slow rebound in weight and hemoglobin A1c values. While this might appear to be a temporary solution for a chronic problem, "we’re certainly treating it, and in some ways may be reversing the disease at least for awhile," he said, pointing out that the device addresses the need to break the cycle of continuing weight gain and helps patients discontinue diabetes medications, especially insulin.
A variety of newer, improved versions of endoscopically placed balloons are also being studied, including the ReShape, a double balloon device, Dr. Rothstein said.
During the same session, Richard Thompson, president and CEO of ReShape Medical, a small venture capital–funded company, said that the ReShape Duo intragastric device is made up of two balloons that contain a total of about 900 mL of fluid, which occupy space in the stomach without the discomfort and distension that can occur with one large balloon. This device is designed to reduce the risk of migration, which can occurs when a balloon deflates and migrates to the intestine where it can cause a blockage. If one balloon deflates the other remains inflated, and because there is blue dye in the balloons, when one deflates, the dye is visible in urine to alert the patient, he noted. ReShape Duo has been available in Europe for more than 2 years.
The U.S. trial evaluating the device in 325 patients is almost completed, and the company recently announced that the primary endpoints that assessed weight loss and responder rates had been met. The company plans to file for FDA approval in the second quarter of 2014.
Dr. Rothstein said that other nonsurgical devices being developed include those that do not require endoscopic placement, such as bezoars or balloons that are swallowed by the patient and function as temporary "space-occupying devices," he said. One example is a capsule that contains beads, which swell up in the stomach and take up space after the capsule is swallowed – which may affect satiety and result in weight loss if ingested before a meal, he said.
Techniques that bring aspects of the proximal stomach together represent another approach, using devices to sew and stitch up the stomach, compartmentalizing the stomach, creating "if you will, an endoscopic gastric sleeve," he said, noting there are not much data available on this approach.
Data from studies that are sham-controlled and have adequate sample sizes are needed to determine the role of these therapies, as they are developed, and they need to be shown to have "reasonable durability," and a safety profile with minimal complications, with cost-effectiveness data, Dr. Rothstein said. And as they become available, it will be necessary to "tease out" which patient groups respond best to which therapy, such as balloons or bezoars, or gastric bypass surgery, he added.
AT AN FDA/AGA WORKSHOP
VIDEO: How to improve cancer survivorship planning
BRUSSELS – National Cancer Institute Director Catherine Alfano, Ph.D., summarizes the institute’s work on improving cancer survivor planning, better coordinating survivor care, and gathering new data on long-term outcomes. She made her remarks during the Cancer Survivorship Summit in a video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
BRUSSELS – National Cancer Institute Director Catherine Alfano, Ph.D., summarizes the institute’s work on improving cancer survivor planning, better coordinating survivor care, and gathering new data on long-term outcomes. She made her remarks during the Cancer Survivorship Summit in a video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
BRUSSELS – National Cancer Institute Director Catherine Alfano, Ph.D., summarizes the institute’s work on improving cancer survivor planning, better coordinating survivor care, and gathering new data on long-term outcomes. She made her remarks during the Cancer Survivorship Summit in a video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE CANCER SURVIVORSHIP SUMMIT
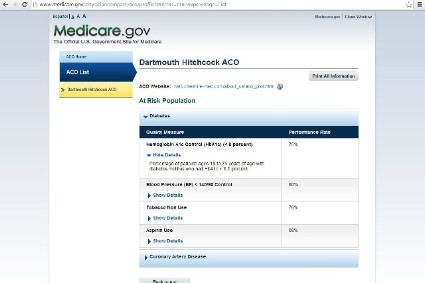
Physician Compare site adds quality scores
Physician Compare, Medicare’s online portal for checking on physician qualifications, has added quality scores for physicians in some group practices and Accountable Care Organizations.
The site now displays how a group of physicians has performed on five quality indicators related to management of diabetes and heart disease.
The website will display the ratings using stars, as well as the actual percentage score on the measure.
"This is an important first step in publicly reporting quality measures on Physician Compare," Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Centers for Medicare and Medicaid Services, said in a statement. "Offering a strong set of meaningful quality measures on the site will ultimately help consumers make decisions and it will encourage quality improvement among the clinician community, who shares CMS’s strong commitment to the best possible patient care."
The Physician Compare site, which was created under the Affordable Care Act, already displays the specialties offered by physicians, their board certification, and hospital affiliations. It also displays whether physicians participate in Medicare quality programs such as the Physician Quality Reporting System, the Electronic Prescribing Incentive Program, and the Electronic Health Records Incentive Program.
The information comes primarily from the Provider, Enrollment, Chain, and Ownership System (PECOS) and is checked against Medicare claims data. The site includes information on physicians enrolled in the Medicare program only.
This year, CMS is posting quality data from 66 group practices and 141 ACOs. The data is reported at the group practice and ACO level.
The quality measures include:
• Controlling hemoglobin A1c in patients with diabetes.
• Controlling blood pressure in patients with diabetes.
• Prescribing aspirin to patients with diabetes and heart disease.
• Reporting the number of diabetic patients who do not use tobacco.
• Prescribing medicine to improve the pumping action of the heart in patients who have both heart disease and certain other conditions.
On Twitter @maryellenny
Physician Compare, Medicare’s online portal for checking on physician qualifications, has added quality scores for physicians in some group practices and Accountable Care Organizations.
The site now displays how a group of physicians has performed on five quality indicators related to management of diabetes and heart disease.
The website will display the ratings using stars, as well as the actual percentage score on the measure.
"This is an important first step in publicly reporting quality measures on Physician Compare," Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Centers for Medicare and Medicaid Services, said in a statement. "Offering a strong set of meaningful quality measures on the site will ultimately help consumers make decisions and it will encourage quality improvement among the clinician community, who shares CMS’s strong commitment to the best possible patient care."
The Physician Compare site, which was created under the Affordable Care Act, already displays the specialties offered by physicians, their board certification, and hospital affiliations. It also displays whether physicians participate in Medicare quality programs such as the Physician Quality Reporting System, the Electronic Prescribing Incentive Program, and the Electronic Health Records Incentive Program.
The information comes primarily from the Provider, Enrollment, Chain, and Ownership System (PECOS) and is checked against Medicare claims data. The site includes information on physicians enrolled in the Medicare program only.
This year, CMS is posting quality data from 66 group practices and 141 ACOs. The data is reported at the group practice and ACO level.
The quality measures include:
• Controlling hemoglobin A1c in patients with diabetes.
• Controlling blood pressure in patients with diabetes.
• Prescribing aspirin to patients with diabetes and heart disease.
• Reporting the number of diabetic patients who do not use tobacco.
• Prescribing medicine to improve the pumping action of the heart in patients who have both heart disease and certain other conditions.
On Twitter @maryellenny
Physician Compare, Medicare’s online portal for checking on physician qualifications, has added quality scores for physicians in some group practices and Accountable Care Organizations.
The site now displays how a group of physicians has performed on five quality indicators related to management of diabetes and heart disease.
The website will display the ratings using stars, as well as the actual percentage score on the measure.
"This is an important first step in publicly reporting quality measures on Physician Compare," Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Centers for Medicare and Medicaid Services, said in a statement. "Offering a strong set of meaningful quality measures on the site will ultimately help consumers make decisions and it will encourage quality improvement among the clinician community, who shares CMS’s strong commitment to the best possible patient care."
The Physician Compare site, which was created under the Affordable Care Act, already displays the specialties offered by physicians, their board certification, and hospital affiliations. It also displays whether physicians participate in Medicare quality programs such as the Physician Quality Reporting System, the Electronic Prescribing Incentive Program, and the Electronic Health Records Incentive Program.
The information comes primarily from the Provider, Enrollment, Chain, and Ownership System (PECOS) and is checked against Medicare claims data. The site includes information on physicians enrolled in the Medicare program only.
This year, CMS is posting quality data from 66 group practices and 141 ACOs. The data is reported at the group practice and ACO level.
The quality measures include:
• Controlling hemoglobin A1c in patients with diabetes.
• Controlling blood pressure in patients with diabetes.
• Prescribing aspirin to patients with diabetes and heart disease.
• Reporting the number of diabetic patients who do not use tobacco.
• Prescribing medicine to improve the pumping action of the heart in patients who have both heart disease and certain other conditions.
On Twitter @maryellenny
ICD-10: CMS to hold end-to-end testing
To address concerns about the upcoming transition to ICD-10, the Centers for Medicare and Medicaid Services announced Feb. 20 that it would conduct full end-to-end testing this summer.
End-to-end testing will allow selected physicians, health care providers, hospitals, clearing houses, and billing agents to submit claims with ICD-10 codes, have those claims processed, and receive accurate remittance advice regarding payment.
The test will be conducted by a statistically significant sample of providers gleaned from a pool of volunteers, CMS officials said during a webinar on ICD-10.
Providers can apply to participate through one of the 16 Medicare Administrative Contractors (MACs) in March; the agency will announce those selected sometime in April. More details will be available on the CMS ICD-10 website in a few weeks, CMS officials said.
Physician groups have sought such thorough testing and heralded the CMS announcement.
"The AMA believes end-to-end testing is essential for ensuring the health care industry will not suffer massive disruptions in claims and payment processing and ultimately risk physicians’ ability to care for their patients," said Dr. Ardis Dee Hoven, president of the American Medical Association, in a statement. "The AMA urges CMS to conduct the testing as soon as possible and to ensure that there is an adequate sample which includes a variety of different-sized medical practices and specialties."
The Medical Group Management Association also supports end-to-end testing, according to Dr. Susan Turney, president and CEO. However, the MGMA would like to see the CMS expand the scope of the testing "to include any provider who wishes to test with them," Dr. Turney said in a statement. That would minimize the possibility of "potential operational problems similar to what was experienced with the rollout of healthcare.gov," and "help to decrease the potential of catastrophic cash flow disruption that could impact the ability of practices to treat patients."
The AMA said that it continues to seek a delay in the Oct. 1 implementation of the new coding set, but CMS officials said that would not happen.
"I want to make really clear that the Oct. 1, 2014, date is firm," said Robert Tagalicod, director of the Office of eHealth Standards and Services at the CMS. "If you are a medical practice and haven’t talked with your vendors, clearing houses, and payers, now is the time to act."
CMS officials also noted that acknowledgment testing for interested providers starts soon. The first official period will be March 3-7. The test will let physicians determine whether their ICD-10 coded claims would be accepted or rejected. The claims will not be adjudicated. Doctors can apply through their MAC website for the testing; so far, some 2,500 have signed up for the March dates.
The agency will offer more official test periods, and will provide information on those soon, officials said. Physicians also can request unofficial testing with their MAC any time between March and October. The results of those tests won’t be included as part of the CMS’s official statistics.
Denesecia Green, of the CMS Office of eHealth Standards and Services, said that the agency wanted to reach out more to small physician practices. The agency is collaborating with state medical societies and national physician organizations to do so.
She also said that the CMS offers specific training for physician offices, and free billing software. More information about those programs can be found on the ICD-10 website.
Both the AMA and the MGMA also provide tools to help physicians make the transition.
But, Dr. Hoven said, although adopting the new code set "may provide benefits to others in the health care system, [it] is unlikely to improve the care physicians provide their patients and takes valuable resources away from implementing delivery reforms and health information technology."
On Twitter @aliciaault
To address concerns about the upcoming transition to ICD-10, the Centers for Medicare and Medicaid Services announced Feb. 20 that it would conduct full end-to-end testing this summer.
End-to-end testing will allow selected physicians, health care providers, hospitals, clearing houses, and billing agents to submit claims with ICD-10 codes, have those claims processed, and receive accurate remittance advice regarding payment.
The test will be conducted by a statistically significant sample of providers gleaned from a pool of volunteers, CMS officials said during a webinar on ICD-10.
Providers can apply to participate through one of the 16 Medicare Administrative Contractors (MACs) in March; the agency will announce those selected sometime in April. More details will be available on the CMS ICD-10 website in a few weeks, CMS officials said.
Physician groups have sought such thorough testing and heralded the CMS announcement.
"The AMA believes end-to-end testing is essential for ensuring the health care industry will not suffer massive disruptions in claims and payment processing and ultimately risk physicians’ ability to care for their patients," said Dr. Ardis Dee Hoven, president of the American Medical Association, in a statement. "The AMA urges CMS to conduct the testing as soon as possible and to ensure that there is an adequate sample which includes a variety of different-sized medical practices and specialties."
The Medical Group Management Association also supports end-to-end testing, according to Dr. Susan Turney, president and CEO. However, the MGMA would like to see the CMS expand the scope of the testing "to include any provider who wishes to test with them," Dr. Turney said in a statement. That would minimize the possibility of "potential operational problems similar to what was experienced with the rollout of healthcare.gov," and "help to decrease the potential of catastrophic cash flow disruption that could impact the ability of practices to treat patients."
The AMA said that it continues to seek a delay in the Oct. 1 implementation of the new coding set, but CMS officials said that would not happen.
"I want to make really clear that the Oct. 1, 2014, date is firm," said Robert Tagalicod, director of the Office of eHealth Standards and Services at the CMS. "If you are a medical practice and haven’t talked with your vendors, clearing houses, and payers, now is the time to act."
CMS officials also noted that acknowledgment testing for interested providers starts soon. The first official period will be March 3-7. The test will let physicians determine whether their ICD-10 coded claims would be accepted or rejected. The claims will not be adjudicated. Doctors can apply through their MAC website for the testing; so far, some 2,500 have signed up for the March dates.
The agency will offer more official test periods, and will provide information on those soon, officials said. Physicians also can request unofficial testing with their MAC any time between March and October. The results of those tests won’t be included as part of the CMS’s official statistics.
Denesecia Green, of the CMS Office of eHealth Standards and Services, said that the agency wanted to reach out more to small physician practices. The agency is collaborating with state medical societies and national physician organizations to do so.
She also said that the CMS offers specific training for physician offices, and free billing software. More information about those programs can be found on the ICD-10 website.
Both the AMA and the MGMA also provide tools to help physicians make the transition.
But, Dr. Hoven said, although adopting the new code set "may provide benefits to others in the health care system, [it] is unlikely to improve the care physicians provide their patients and takes valuable resources away from implementing delivery reforms and health information technology."
On Twitter @aliciaault
To address concerns about the upcoming transition to ICD-10, the Centers for Medicare and Medicaid Services announced Feb. 20 that it would conduct full end-to-end testing this summer.
End-to-end testing will allow selected physicians, health care providers, hospitals, clearing houses, and billing agents to submit claims with ICD-10 codes, have those claims processed, and receive accurate remittance advice regarding payment.
The test will be conducted by a statistically significant sample of providers gleaned from a pool of volunteers, CMS officials said during a webinar on ICD-10.
Providers can apply to participate through one of the 16 Medicare Administrative Contractors (MACs) in March; the agency will announce those selected sometime in April. More details will be available on the CMS ICD-10 website in a few weeks, CMS officials said.
Physician groups have sought such thorough testing and heralded the CMS announcement.
"The AMA believes end-to-end testing is essential for ensuring the health care industry will not suffer massive disruptions in claims and payment processing and ultimately risk physicians’ ability to care for their patients," said Dr. Ardis Dee Hoven, president of the American Medical Association, in a statement. "The AMA urges CMS to conduct the testing as soon as possible and to ensure that there is an adequate sample which includes a variety of different-sized medical practices and specialties."
The Medical Group Management Association also supports end-to-end testing, according to Dr. Susan Turney, president and CEO. However, the MGMA would like to see the CMS expand the scope of the testing "to include any provider who wishes to test with them," Dr. Turney said in a statement. That would minimize the possibility of "potential operational problems similar to what was experienced with the rollout of healthcare.gov," and "help to decrease the potential of catastrophic cash flow disruption that could impact the ability of practices to treat patients."
The AMA said that it continues to seek a delay in the Oct. 1 implementation of the new coding set, but CMS officials said that would not happen.
"I want to make really clear that the Oct. 1, 2014, date is firm," said Robert Tagalicod, director of the Office of eHealth Standards and Services at the CMS. "If you are a medical practice and haven’t talked with your vendors, clearing houses, and payers, now is the time to act."
CMS officials also noted that acknowledgment testing for interested providers starts soon. The first official period will be March 3-7. The test will let physicians determine whether their ICD-10 coded claims would be accepted or rejected. The claims will not be adjudicated. Doctors can apply through their MAC website for the testing; so far, some 2,500 have signed up for the March dates.
The agency will offer more official test periods, and will provide information on those soon, officials said. Physicians also can request unofficial testing with their MAC any time between March and October. The results of those tests won’t be included as part of the CMS’s official statistics.
Denesecia Green, of the CMS Office of eHealth Standards and Services, said that the agency wanted to reach out more to small physician practices. The agency is collaborating with state medical societies and national physician organizations to do so.
She also said that the CMS offers specific training for physician offices, and free billing software. More information about those programs can be found on the ICD-10 website.
Both the AMA and the MGMA also provide tools to help physicians make the transition.
But, Dr. Hoven said, although adopting the new code set "may provide benefits to others in the health care system, [it] is unlikely to improve the care physicians provide their patients and takes valuable resources away from implementing delivery reforms and health information technology."
On Twitter @aliciaault
FROM A CMS WEBINAR ON ICD-10
Renal insufficiency tied to risk of post–liver surgery problems
MIAMI BEACH – Renal insufficiency significantly increased the risk of major complications after liver surgery.
However, it wasn’t associated with an increased risk of 90-day mortality, suggesting that patients with poor renal function shouldn’t be ruled out as surgical candidates, Dr. Malcolm Squires III said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
"While they may be at a potential risk of major complications – renal failure and respiratory failure – we are ultimately able to get these patients through the postoperative period without any significant increase in mortality," said Dr. Squires of Emory University, Atlanta.
He presented a large retrospective study that examined postoperative outcomes in 1,170 patients (mean age, 57 years) who underwent major hepatectomy at three national academic hospitals from 2000 to 2012. The study determined the link between major complications and preoperative serum creatinine levels. These levels were dichotomized as normal (1.8 mg/dL or less) and elevated (greater than 1.8 mg/dL).
Most patients (1,148) had normal levels; only 22 had elevated serum creatinine, considered to be reflective of chronic renal insufficiency.
Pathology included cholangiocarcinoma, hepatocellular carcinoma, metastatic colorectal cancer, other cancers, and benign lesions. Cirrhosis was present in 4% and steatosis in 39%.
Most (83%) had open surgery; 17% had a laparoscopic procedure. The mean blood loss was 510 cc; 25% needed an intraoperative blood transfusion.
Postoperative complications arose in 56% of the group. A quarter (24%) had a major complication, including renal failure (3%) and respiratory failure (5%). Three-month mortality in the entire group was 5%.
In a multivariate model, preoperative renal insufficiency conferred a fourfold increased risk of developing a major postoperative complication. Other significant predictors were a high American Society of Anesthesiologists classification score (odds ratio, 1.6), having a bile duct resection (OR, 1.7), and a low preoperative albumin level (OR, 1.6).
Renal insufficiency also significantly predicted postoperative respiratory failure (OR, 4.4). Other predictors of respiratory failure were older age (OR, 1.06) and cirrhosis (OR, 6.6).
Renal insufficiency was also a significant risk factor for renal failure, increasing the odds by 4.6.
The biggest predictor of 90-day mortality was hepatitis C, which conferred a ninefold increased risk. Cardiac disease also significantly increased the risk (OR, 2), as did bile duct resection (OR, 2.3), intraoperative transfusion (OR, 2) and cirrhosis (OR, 4.7).
Preoperative renal insufficiency did not significantly increase the risk of death, Dr. Squires noted.
"These findings should be taken into consideration when evaluating patients with preoperative renal insufficiency for hepatic resection," he said. "Careful patient selection and appropriate preoperative counseling are critical."
Dr. Squires had no financial disclosures.
MIAMI BEACH – Renal insufficiency significantly increased the risk of major complications after liver surgery.
However, it wasn’t associated with an increased risk of 90-day mortality, suggesting that patients with poor renal function shouldn’t be ruled out as surgical candidates, Dr. Malcolm Squires III said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
"While they may be at a potential risk of major complications – renal failure and respiratory failure – we are ultimately able to get these patients through the postoperative period without any significant increase in mortality," said Dr. Squires of Emory University, Atlanta.
He presented a large retrospective study that examined postoperative outcomes in 1,170 patients (mean age, 57 years) who underwent major hepatectomy at three national academic hospitals from 2000 to 2012. The study determined the link between major complications and preoperative serum creatinine levels. These levels were dichotomized as normal (1.8 mg/dL or less) and elevated (greater than 1.8 mg/dL).
Most patients (1,148) had normal levels; only 22 had elevated serum creatinine, considered to be reflective of chronic renal insufficiency.
Pathology included cholangiocarcinoma, hepatocellular carcinoma, metastatic colorectal cancer, other cancers, and benign lesions. Cirrhosis was present in 4% and steatosis in 39%.
Most (83%) had open surgery; 17% had a laparoscopic procedure. The mean blood loss was 510 cc; 25% needed an intraoperative blood transfusion.
Postoperative complications arose in 56% of the group. A quarter (24%) had a major complication, including renal failure (3%) and respiratory failure (5%). Three-month mortality in the entire group was 5%.
In a multivariate model, preoperative renal insufficiency conferred a fourfold increased risk of developing a major postoperative complication. Other significant predictors were a high American Society of Anesthesiologists classification score (odds ratio, 1.6), having a bile duct resection (OR, 1.7), and a low preoperative albumin level (OR, 1.6).
Renal insufficiency also significantly predicted postoperative respiratory failure (OR, 4.4). Other predictors of respiratory failure were older age (OR, 1.06) and cirrhosis (OR, 6.6).
Renal insufficiency was also a significant risk factor for renal failure, increasing the odds by 4.6.
The biggest predictor of 90-day mortality was hepatitis C, which conferred a ninefold increased risk. Cardiac disease also significantly increased the risk (OR, 2), as did bile duct resection (OR, 2.3), intraoperative transfusion (OR, 2) and cirrhosis (OR, 4.7).
Preoperative renal insufficiency did not significantly increase the risk of death, Dr. Squires noted.
"These findings should be taken into consideration when evaluating patients with preoperative renal insufficiency for hepatic resection," he said. "Careful patient selection and appropriate preoperative counseling are critical."
Dr. Squires had no financial disclosures.
MIAMI BEACH – Renal insufficiency significantly increased the risk of major complications after liver surgery.
However, it wasn’t associated with an increased risk of 90-day mortality, suggesting that patients with poor renal function shouldn’t be ruled out as surgical candidates, Dr. Malcolm Squires III said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
"While they may be at a potential risk of major complications – renal failure and respiratory failure – we are ultimately able to get these patients through the postoperative period without any significant increase in mortality," said Dr. Squires of Emory University, Atlanta.
He presented a large retrospective study that examined postoperative outcomes in 1,170 patients (mean age, 57 years) who underwent major hepatectomy at three national academic hospitals from 2000 to 2012. The study determined the link between major complications and preoperative serum creatinine levels. These levels were dichotomized as normal (1.8 mg/dL or less) and elevated (greater than 1.8 mg/dL).
Most patients (1,148) had normal levels; only 22 had elevated serum creatinine, considered to be reflective of chronic renal insufficiency.
Pathology included cholangiocarcinoma, hepatocellular carcinoma, metastatic colorectal cancer, other cancers, and benign lesions. Cirrhosis was present in 4% and steatosis in 39%.
Most (83%) had open surgery; 17% had a laparoscopic procedure. The mean blood loss was 510 cc; 25% needed an intraoperative blood transfusion.
Postoperative complications arose in 56% of the group. A quarter (24%) had a major complication, including renal failure (3%) and respiratory failure (5%). Three-month mortality in the entire group was 5%.
In a multivariate model, preoperative renal insufficiency conferred a fourfold increased risk of developing a major postoperative complication. Other significant predictors were a high American Society of Anesthesiologists classification score (odds ratio, 1.6), having a bile duct resection (OR, 1.7), and a low preoperative albumin level (OR, 1.6).
Renal insufficiency also significantly predicted postoperative respiratory failure (OR, 4.4). Other predictors of respiratory failure were older age (OR, 1.06) and cirrhosis (OR, 6.6).
Renal insufficiency was also a significant risk factor for renal failure, increasing the odds by 4.6.
The biggest predictor of 90-day mortality was hepatitis C, which conferred a ninefold increased risk. Cardiac disease also significantly increased the risk (OR, 2), as did bile duct resection (OR, 2.3), intraoperative transfusion (OR, 2) and cirrhosis (OR, 4.7).
Preoperative renal insufficiency did not significantly increase the risk of death, Dr. Squires noted.
"These findings should be taken into consideration when evaluating patients with preoperative renal insufficiency for hepatic resection," he said. "Careful patient selection and appropriate preoperative counseling are critical."
Dr. Squires had no financial disclosures.
AT AHPBA 2014
Major finding: Chronic preoperative renal insufficiency confers a fourfold increase in the risk of major complications after hepatic resection, although it did not increase the risk of 90-day mortality.
Data source: The retrospective study looked at postoperative outcomes in 1,170 patients.
Disclosures: Dr. Squires had no financial disclosures.
Thyroid cancer rise mostly overdiagnosis
The incidence of thyroid cancer has nearly tripled in the United States since the 1970s. However, this is mainly an epidemic of diagnosis, researchers reported.
Small papillary cancers are not likely to cause death or disease, and women are four times more likely to receive a diagnosis than men, even though autopsy findings show that these cancers occur more frequently in men.
For the research, published online Feb. 20 in JAMA Otolaryngology–Head & Neck Surgery, Dr. Louise Davies and Dr. H. Gilbert Welch reviewed diagnostic trends from the population-based Surveillance, Epidemiology, and End Results (SEER) 9 program, which covers four large U.S. metropolitan areas along with five states. They also reviewed mortality records from the National Vital Statistics System between 1975 and 2009 for the same areas, reported Dr. Davies of the Veterans Affairs Medical Center in White River Junction, Vt., and Dr. Welch of the Dartmouth Institute for Health Policy and Clinical Practice in Hanover, N.H.
The researchers found that thyroid cancer incidence nearly tripled, from 4.9 to 14.3 per 100,000 individuals, in that time period (relative rate, 2.9) and that nearly all of the increase was attributable to diagnoses of small papillary cancers, the least aggressive form of thyroid cancer. The mortality rate from thyroid cancer remained stable – at 0.5 deaths per 100,000 – during the same time, Dr. Davies and Dr. Welch reported (JAMA Otolaryngol. Head Neck Surg. 2014 Feb. 20 [doi: 10.1001/jamaoto.2014.1]).
The investigators saw a much greater absolute increase in thyroid cancer in women, at 3.3-fold (from 6.5 to 21.4 cases per 100,000), than in men, at 2.2-fold (from 3.1 to 6.9), during the study period, which suggests that the burden of overdiagnosis fell heavily on women, they wrote.
Moreover, most thyroid cancers are treated "as though they are destined to cause real problems for the people who have them," Dr. Davies and Dr. Welch wrote, usually with total thyroidectomy, radiation, or both, putting patients at risk for complications and secondary cancers.
Patients – particularly women – might be better served with a less intensive diagnostic and treatment approach to these cancers, and even by relabeling them using a term other than cancer. Clinicians should take care to advise patients of the uncertainty surrounding the small papillary cancers and encourage them to consider the risks of treatment compared with active surveillance, the researchers said.
Dr. Davies and Dr. Welch received support from their institutions for their research; neither declared conflicts of interest.
This is an interesting and important study, but one that is difficult to interpret. We don't yet know which of these cancers, no matter what size, will ultimately prove to be important. Once a diagnosis of cancer is made, it is difficult for patients and doctors to simply continue to observe the cancer. Most patients and doctors are uncomfortable with that.
In addition, the follow-up itself becomes burdensome, with annual ultrasounds and, possibly, multiple needle biopsies over time. Although much of this increased incidence seems related to increased use of imaging studies, several authors have also reported an absolute increase in the incidence of thyroid cancer.
Other issues related to this topic are the extent of surgery that is necessary for these small early cancers. The authors point out that many surgeons perform total thyroidectomy and postoperative radioactive iodine ablation, but there are some who advocate for lesser surgery. This becomes problematic when patients have other smaller nodules in the opposite lobe of the thyroid of uncertain significance. Some national guidelines recommend total or near-total thyroidectomy for T1 and T2 well-differentiated thyroid cancers, and it is difficult to go against these guidelines. What is really needed are better molecular and genetic tests to better define which well-differentiated thyroid cancers are likely to act in a more aggressive manner, and which are not.
Mark C. Weissler, M.D., FACS, is the J.P. Riddle Distinguished Professor of Otolaryngology-Head and Neck Surgery at the University of North Carolina, Chapel Hill. Dr. Weissler had no disclosures.
This is an interesting and important study, but one that is difficult to interpret. We don't yet know which of these cancers, no matter what size, will ultimately prove to be important. Once a diagnosis of cancer is made, it is difficult for patients and doctors to simply continue to observe the cancer. Most patients and doctors are uncomfortable with that.
In addition, the follow-up itself becomes burdensome, with annual ultrasounds and, possibly, multiple needle biopsies over time. Although much of this increased incidence seems related to increased use of imaging studies, several authors have also reported an absolute increase in the incidence of thyroid cancer.
Other issues related to this topic are the extent of surgery that is necessary for these small early cancers. The authors point out that many surgeons perform total thyroidectomy and postoperative radioactive iodine ablation, but there are some who advocate for lesser surgery. This becomes problematic when patients have other smaller nodules in the opposite lobe of the thyroid of uncertain significance. Some national guidelines recommend total or near-total thyroidectomy for T1 and T2 well-differentiated thyroid cancers, and it is difficult to go against these guidelines. What is really needed are better molecular and genetic tests to better define which well-differentiated thyroid cancers are likely to act in a more aggressive manner, and which are not.
Mark C. Weissler, M.D., FACS, is the J.P. Riddle Distinguished Professor of Otolaryngology-Head and Neck Surgery at the University of North Carolina, Chapel Hill. Dr. Weissler had no disclosures.
This is an interesting and important study, but one that is difficult to interpret. We don't yet know which of these cancers, no matter what size, will ultimately prove to be important. Once a diagnosis of cancer is made, it is difficult for patients and doctors to simply continue to observe the cancer. Most patients and doctors are uncomfortable with that.
In addition, the follow-up itself becomes burdensome, with annual ultrasounds and, possibly, multiple needle biopsies over time. Although much of this increased incidence seems related to increased use of imaging studies, several authors have also reported an absolute increase in the incidence of thyroid cancer.
Other issues related to this topic are the extent of surgery that is necessary for these small early cancers. The authors point out that many surgeons perform total thyroidectomy and postoperative radioactive iodine ablation, but there are some who advocate for lesser surgery. This becomes problematic when patients have other smaller nodules in the opposite lobe of the thyroid of uncertain significance. Some national guidelines recommend total or near-total thyroidectomy for T1 and T2 well-differentiated thyroid cancers, and it is difficult to go against these guidelines. What is really needed are better molecular and genetic tests to better define which well-differentiated thyroid cancers are likely to act in a more aggressive manner, and which are not.
Mark C. Weissler, M.D., FACS, is the J.P. Riddle Distinguished Professor of Otolaryngology-Head and Neck Surgery at the University of North Carolina, Chapel Hill. Dr. Weissler had no disclosures.
The incidence of thyroid cancer has nearly tripled in the United States since the 1970s. However, this is mainly an epidemic of diagnosis, researchers reported.
Small papillary cancers are not likely to cause death or disease, and women are four times more likely to receive a diagnosis than men, even though autopsy findings show that these cancers occur more frequently in men.
For the research, published online Feb. 20 in JAMA Otolaryngology–Head & Neck Surgery, Dr. Louise Davies and Dr. H. Gilbert Welch reviewed diagnostic trends from the population-based Surveillance, Epidemiology, and End Results (SEER) 9 program, which covers four large U.S. metropolitan areas along with five states. They also reviewed mortality records from the National Vital Statistics System between 1975 and 2009 for the same areas, reported Dr. Davies of the Veterans Affairs Medical Center in White River Junction, Vt., and Dr. Welch of the Dartmouth Institute for Health Policy and Clinical Practice in Hanover, N.H.
The researchers found that thyroid cancer incidence nearly tripled, from 4.9 to 14.3 per 100,000 individuals, in that time period (relative rate, 2.9) and that nearly all of the increase was attributable to diagnoses of small papillary cancers, the least aggressive form of thyroid cancer. The mortality rate from thyroid cancer remained stable – at 0.5 deaths per 100,000 – during the same time, Dr. Davies and Dr. Welch reported (JAMA Otolaryngol. Head Neck Surg. 2014 Feb. 20 [doi: 10.1001/jamaoto.2014.1]).
The investigators saw a much greater absolute increase in thyroid cancer in women, at 3.3-fold (from 6.5 to 21.4 cases per 100,000), than in men, at 2.2-fold (from 3.1 to 6.9), during the study period, which suggests that the burden of overdiagnosis fell heavily on women, they wrote.
Moreover, most thyroid cancers are treated "as though they are destined to cause real problems for the people who have them," Dr. Davies and Dr. Welch wrote, usually with total thyroidectomy, radiation, or both, putting patients at risk for complications and secondary cancers.
Patients – particularly women – might be better served with a less intensive diagnostic and treatment approach to these cancers, and even by relabeling them using a term other than cancer. Clinicians should take care to advise patients of the uncertainty surrounding the small papillary cancers and encourage them to consider the risks of treatment compared with active surveillance, the researchers said.
Dr. Davies and Dr. Welch received support from their institutions for their research; neither declared conflicts of interest.
The incidence of thyroid cancer has nearly tripled in the United States since the 1970s. However, this is mainly an epidemic of diagnosis, researchers reported.
Small papillary cancers are not likely to cause death or disease, and women are four times more likely to receive a diagnosis than men, even though autopsy findings show that these cancers occur more frequently in men.
For the research, published online Feb. 20 in JAMA Otolaryngology–Head & Neck Surgery, Dr. Louise Davies and Dr. H. Gilbert Welch reviewed diagnostic trends from the population-based Surveillance, Epidemiology, and End Results (SEER) 9 program, which covers four large U.S. metropolitan areas along with five states. They also reviewed mortality records from the National Vital Statistics System between 1975 and 2009 for the same areas, reported Dr. Davies of the Veterans Affairs Medical Center in White River Junction, Vt., and Dr. Welch of the Dartmouth Institute for Health Policy and Clinical Practice in Hanover, N.H.
The researchers found that thyroid cancer incidence nearly tripled, from 4.9 to 14.3 per 100,000 individuals, in that time period (relative rate, 2.9) and that nearly all of the increase was attributable to diagnoses of small papillary cancers, the least aggressive form of thyroid cancer. The mortality rate from thyroid cancer remained stable – at 0.5 deaths per 100,000 – during the same time, Dr. Davies and Dr. Welch reported (JAMA Otolaryngol. Head Neck Surg. 2014 Feb. 20 [doi: 10.1001/jamaoto.2014.1]).
The investigators saw a much greater absolute increase in thyroid cancer in women, at 3.3-fold (from 6.5 to 21.4 cases per 100,000), than in men, at 2.2-fold (from 3.1 to 6.9), during the study period, which suggests that the burden of overdiagnosis fell heavily on women, they wrote.
Moreover, most thyroid cancers are treated "as though they are destined to cause real problems for the people who have them," Dr. Davies and Dr. Welch wrote, usually with total thyroidectomy, radiation, or both, putting patients at risk for complications and secondary cancers.
Patients – particularly women – might be better served with a less intensive diagnostic and treatment approach to these cancers, and even by relabeling them using a term other than cancer. Clinicians should take care to advise patients of the uncertainty surrounding the small papillary cancers and encourage them to consider the risks of treatment compared with active surveillance, the researchers said.
Dr. Davies and Dr. Welch received support from their institutions for their research; neither declared conflicts of interest.
FROM JAMA OTOLARYNGOLOGY – HEAD & NECK SURGERY
ACA hassles, payment cuts are top reasons physicians sell practices
When a hospital approached Georgia surgeon Ian Hamilton Jr. about buying his vascular surgery practice, the proposal was too appealing for him to turn down. At the time, Dr. Hamilton’s practice was facing the challenges of meeting new regulatory and business requirements, including the need for a new electronic health record system that would meet meaningful use requirements.
"I didn’t feel that I was going to be able to maintain a solo practice indefinitely," said Dr. Hamilton, who sold his practice in 2013. "I felt something was going to have to change. The reality of what’s happening in American medicine right now makes it very difficult for a solo practitioner at many different levels. It’s become very expensive to be compliant with the Affordable Care Act and the other regulations that are associated with it."
Dr. Hamilton is far from alone in closing up shop because of a more complex and changing health care landscape. Thirty-two percent of physicians who sold their practice within the past 3 years cited the complexities of the ACA as a primary motivator for the sale, according to a nationwide survey by Jackson Healthcare, a health care staffing firm. Of physicians who sold their practices more than 3 years ago, 10% said the law was a factor, according to the survey.
A second survey by Jackson Healthcare found 60% of practice acquisitions by hospitals in 2013 were initiated by the sellers.
"The practice of medicine has increasingly become more complex," said Sheri Sorrell, director of market research for Jackson Healthcare. This includes "getting reimbursement and the amount of paperwork and the amount of regulations [doctors] have to deal with. They can’t keep up with all the regulations. At least if they are selling to a hospital, the hospital has those resources" to comply.
Budding and completed practice acquisitions varied by specialty, the survey found. Nearly 25% of physicians actively seeking to sell their practices described themselves as internal medicine subspecialists, 14% as primary care physicians, and 12% as surgeons. Of the internal medicine subspecialists seeking to sell, 23% described themselves as otolaryngologists, 17% as urologists, and 13% as cardiologists, the survey found.
Hospitals are keen to acquire primary care practices, the second survey found. Family medicine practices made up 58% of practices acquired by hospitals in 2013, while internal medicine made up 40%.
Cardiology practices also are being acquired as physicians seek to avoid significant reimbursement gaps, Dallas health law attorney Cheryl Camin Murray said. Ms. Murray is a shareholder in the health care industry group and corporate securities/mergers and acquisitions practice group of Texas law firm Winstead PC. Hospitals are paid at a higher rate by Medicare than cardiology practices for the same procedures, Ms. Murray said.
While physicians who sell their practices face their share of challenges, the Jackson Healthcare survey found that the majority of doctors who sold are happy with their decision. Fifty-five percent of physicians who sold said they do not miss private practice, and 60% said they are satisfied or very satisfied. Overall, 76% of physician sellers said they would make the same choice again.
One of those physicians is Dr. Hamilton. In the end, he chose not to become an employee of the hospital he sold his practice to, and he is job hunting for nonclinical positions. The sale came at the right time in his practice and career, Dr. Hamilton said.
"For me it was a very good decision," he said. "I’m very happy I was able to get the equity out of my practice that I built over 11 years. For me it was a very timely and very wonderful opportunity."
Data in the first survey were collected from 536 physicians across the United States who responded to a survey about practice acquisitions in 2013. The second survey analyzed responses from 123 hospital executives who had completed acquisitions in 2013 or had acquisitions planned for 2014.
When a hospital approached Georgia surgeon Ian Hamilton Jr. about buying his vascular surgery practice, the proposal was too appealing for him to turn down. At the time, Dr. Hamilton’s practice was facing the challenges of meeting new regulatory and business requirements, including the need for a new electronic health record system that would meet meaningful use requirements.
"I didn’t feel that I was going to be able to maintain a solo practice indefinitely," said Dr. Hamilton, who sold his practice in 2013. "I felt something was going to have to change. The reality of what’s happening in American medicine right now makes it very difficult for a solo practitioner at many different levels. It’s become very expensive to be compliant with the Affordable Care Act and the other regulations that are associated with it."
Dr. Hamilton is far from alone in closing up shop because of a more complex and changing health care landscape. Thirty-two percent of physicians who sold their practice within the past 3 years cited the complexities of the ACA as a primary motivator for the sale, according to a nationwide survey by Jackson Healthcare, a health care staffing firm. Of physicians who sold their practices more than 3 years ago, 10% said the law was a factor, according to the survey.
A second survey by Jackson Healthcare found 60% of practice acquisitions by hospitals in 2013 were initiated by the sellers.
"The practice of medicine has increasingly become more complex," said Sheri Sorrell, director of market research for Jackson Healthcare. This includes "getting reimbursement and the amount of paperwork and the amount of regulations [doctors] have to deal with. They can’t keep up with all the regulations. At least if they are selling to a hospital, the hospital has those resources" to comply.
Budding and completed practice acquisitions varied by specialty, the survey found. Nearly 25% of physicians actively seeking to sell their practices described themselves as internal medicine subspecialists, 14% as primary care physicians, and 12% as surgeons. Of the internal medicine subspecialists seeking to sell, 23% described themselves as otolaryngologists, 17% as urologists, and 13% as cardiologists, the survey found.
Hospitals are keen to acquire primary care practices, the second survey found. Family medicine practices made up 58% of practices acquired by hospitals in 2013, while internal medicine made up 40%.
Cardiology practices also are being acquired as physicians seek to avoid significant reimbursement gaps, Dallas health law attorney Cheryl Camin Murray said. Ms. Murray is a shareholder in the health care industry group and corporate securities/mergers and acquisitions practice group of Texas law firm Winstead PC. Hospitals are paid at a higher rate by Medicare than cardiology practices for the same procedures, Ms. Murray said.
While physicians who sell their practices face their share of challenges, the Jackson Healthcare survey found that the majority of doctors who sold are happy with their decision. Fifty-five percent of physicians who sold said they do not miss private practice, and 60% said they are satisfied or very satisfied. Overall, 76% of physician sellers said they would make the same choice again.
One of those physicians is Dr. Hamilton. In the end, he chose not to become an employee of the hospital he sold his practice to, and he is job hunting for nonclinical positions. The sale came at the right time in his practice and career, Dr. Hamilton said.
"For me it was a very good decision," he said. "I’m very happy I was able to get the equity out of my practice that I built over 11 years. For me it was a very timely and very wonderful opportunity."
Data in the first survey were collected from 536 physicians across the United States who responded to a survey about practice acquisitions in 2013. The second survey analyzed responses from 123 hospital executives who had completed acquisitions in 2013 or had acquisitions planned for 2014.
When a hospital approached Georgia surgeon Ian Hamilton Jr. about buying his vascular surgery practice, the proposal was too appealing for him to turn down. At the time, Dr. Hamilton’s practice was facing the challenges of meeting new regulatory and business requirements, including the need for a new electronic health record system that would meet meaningful use requirements.
"I didn’t feel that I was going to be able to maintain a solo practice indefinitely," said Dr. Hamilton, who sold his practice in 2013. "I felt something was going to have to change. The reality of what’s happening in American medicine right now makes it very difficult for a solo practitioner at many different levels. It’s become very expensive to be compliant with the Affordable Care Act and the other regulations that are associated with it."
Dr. Hamilton is far from alone in closing up shop because of a more complex and changing health care landscape. Thirty-two percent of physicians who sold their practice within the past 3 years cited the complexities of the ACA as a primary motivator for the sale, according to a nationwide survey by Jackson Healthcare, a health care staffing firm. Of physicians who sold their practices more than 3 years ago, 10% said the law was a factor, according to the survey.
A second survey by Jackson Healthcare found 60% of practice acquisitions by hospitals in 2013 were initiated by the sellers.
"The practice of medicine has increasingly become more complex," said Sheri Sorrell, director of market research for Jackson Healthcare. This includes "getting reimbursement and the amount of paperwork and the amount of regulations [doctors] have to deal with. They can’t keep up with all the regulations. At least if they are selling to a hospital, the hospital has those resources" to comply.
Budding and completed practice acquisitions varied by specialty, the survey found. Nearly 25% of physicians actively seeking to sell their practices described themselves as internal medicine subspecialists, 14% as primary care physicians, and 12% as surgeons. Of the internal medicine subspecialists seeking to sell, 23% described themselves as otolaryngologists, 17% as urologists, and 13% as cardiologists, the survey found.
Hospitals are keen to acquire primary care practices, the second survey found. Family medicine practices made up 58% of practices acquired by hospitals in 2013, while internal medicine made up 40%.
Cardiology practices also are being acquired as physicians seek to avoid significant reimbursement gaps, Dallas health law attorney Cheryl Camin Murray said. Ms. Murray is a shareholder in the health care industry group and corporate securities/mergers and acquisitions practice group of Texas law firm Winstead PC. Hospitals are paid at a higher rate by Medicare than cardiology practices for the same procedures, Ms. Murray said.
While physicians who sell their practices face their share of challenges, the Jackson Healthcare survey found that the majority of doctors who sold are happy with their decision. Fifty-five percent of physicians who sold said they do not miss private practice, and 60% said they are satisfied or very satisfied. Overall, 76% of physician sellers said they would make the same choice again.
One of those physicians is Dr. Hamilton. In the end, he chose not to become an employee of the hospital he sold his practice to, and he is job hunting for nonclinical positions. The sale came at the right time in his practice and career, Dr. Hamilton said.
"For me it was a very good decision," he said. "I’m very happy I was able to get the equity out of my practice that I built over 11 years. For me it was a very timely and very wonderful opportunity."
Data in the first survey were collected from 536 physicians across the United States who responded to a survey about practice acquisitions in 2013. The second survey analyzed responses from 123 hospital executives who had completed acquisitions in 2013 or had acquisitions planned for 2014.
Medicare to cover cardiac rehab for some HF patients
Medicare will begin covering cardiac rehabilitation for patients with stable, chronic heart failure with a left ventricular ejection fraction of 35% or less.
The Centers for Medicare & Medicaid Services announced the new policy on Feb. 18.
About 5 million Americans have heart failure, but only half have an ejection fraction of less than 35%, Dr. Joseph A. Hill, chief of cardiology at the University of Texas Southwestern Medical Center, Dallas, said in an interview. Dr. Hill is chairman of the Heart Failure Society of America’s advocacy committee.
The HFSA, along with the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR), the American College of Cardiology (ACC), and the American Heart Association (AHA), submitted a formal request to the CMS to add heart failure to the list of approved indications for coverage for cardiac rehabilitation. The agency began its analysis process in June 2013.
At that time, cardiac rehab was covered only for acute myocardial infarction within the preceding 12 months, coronary artery bypass surgery, current stable angina pectoris, heart valve repair or replacement, percutaneous transluminal coronary angioplasty or coronary stenting, and a heart or heart-lung transplant. Cardiac rehab includes physician prescribed exercise; risk factor modification, including education, counseling, and behavioral intervention; psychosocial assessment; and outcomes assessment.
Physician supervision is required for coverage.
The CMS said it had reconsidered coverage for some heart failure patients as a result of the HF-Action study, published in 2009 (JAMA 2009;301:1439-50). That study "provided the best evidence of benefit" in the HF patient group, but in particular for patients with an ejection fraction of 35% or less and New York Heart Association (NYHA) class II-IV symptoms.
Specifically, the coverage is extended to "beneficiaries with stable, chronic heart failure defined as patients with left ventricular ejection fraction of 35% or less and [NYHA] class II to IV symptoms despite being on optimal heart failure therapy for at least six weeks." The decision defines stable patients as those who have not had recent (within the past 6 weeks) or planned (within the past 6 months) major cardiovascular hospitalizations or procedures.
"We conclude that the evidence that supports the clinical benefits of the individual components of CR programs is sufficient to determine that participation in these programs improves health outcomes for Medicare beneficiaries with chronic HF," the CMS noted in its analysis.
"We’re very pleased," with the CMS decision, said Dr. Hill.
The ACC said it was still evaluating the decision. But Dr. M. Eugene Sherman, chairman of the ACC’s Advocacy Steering Committee, added that "we are pleased to see Medicare expand coverage of cardiac rehabilitation services, as the ACC requested, to a new patient population where medical and scientific literature demonstrates a medical benefit."
Dr. Hill said that the HFSA and others were hopeful that the CMS would eventually expand coverage of rehab to the remainder of HF patients.
On Twitter @aliciaault
Medicare will begin covering cardiac rehabilitation for patients with stable, chronic heart failure with a left ventricular ejection fraction of 35% or less.
The Centers for Medicare & Medicaid Services announced the new policy on Feb. 18.
About 5 million Americans have heart failure, but only half have an ejection fraction of less than 35%, Dr. Joseph A. Hill, chief of cardiology at the University of Texas Southwestern Medical Center, Dallas, said in an interview. Dr. Hill is chairman of the Heart Failure Society of America’s advocacy committee.
The HFSA, along with the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR), the American College of Cardiology (ACC), and the American Heart Association (AHA), submitted a formal request to the CMS to add heart failure to the list of approved indications for coverage for cardiac rehabilitation. The agency began its analysis process in June 2013.
At that time, cardiac rehab was covered only for acute myocardial infarction within the preceding 12 months, coronary artery bypass surgery, current stable angina pectoris, heart valve repair or replacement, percutaneous transluminal coronary angioplasty or coronary stenting, and a heart or heart-lung transplant. Cardiac rehab includes physician prescribed exercise; risk factor modification, including education, counseling, and behavioral intervention; psychosocial assessment; and outcomes assessment.
Physician supervision is required for coverage.
The CMS said it had reconsidered coverage for some heart failure patients as a result of the HF-Action study, published in 2009 (JAMA 2009;301:1439-50). That study "provided the best evidence of benefit" in the HF patient group, but in particular for patients with an ejection fraction of 35% or less and New York Heart Association (NYHA) class II-IV symptoms.
Specifically, the coverage is extended to "beneficiaries with stable, chronic heart failure defined as patients with left ventricular ejection fraction of 35% or less and [NYHA] class II to IV symptoms despite being on optimal heart failure therapy for at least six weeks." The decision defines stable patients as those who have not had recent (within the past 6 weeks) or planned (within the past 6 months) major cardiovascular hospitalizations or procedures.
"We conclude that the evidence that supports the clinical benefits of the individual components of CR programs is sufficient to determine that participation in these programs improves health outcomes for Medicare beneficiaries with chronic HF," the CMS noted in its analysis.
"We’re very pleased," with the CMS decision, said Dr. Hill.
The ACC said it was still evaluating the decision. But Dr. M. Eugene Sherman, chairman of the ACC’s Advocacy Steering Committee, added that "we are pleased to see Medicare expand coverage of cardiac rehabilitation services, as the ACC requested, to a new patient population where medical and scientific literature demonstrates a medical benefit."
Dr. Hill said that the HFSA and others were hopeful that the CMS would eventually expand coverage of rehab to the remainder of HF patients.
On Twitter @aliciaault
Medicare will begin covering cardiac rehabilitation for patients with stable, chronic heart failure with a left ventricular ejection fraction of 35% or less.
The Centers for Medicare & Medicaid Services announced the new policy on Feb. 18.
About 5 million Americans have heart failure, but only half have an ejection fraction of less than 35%, Dr. Joseph A. Hill, chief of cardiology at the University of Texas Southwestern Medical Center, Dallas, said in an interview. Dr. Hill is chairman of the Heart Failure Society of America’s advocacy committee.
The HFSA, along with the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR), the American College of Cardiology (ACC), and the American Heart Association (AHA), submitted a formal request to the CMS to add heart failure to the list of approved indications for coverage for cardiac rehabilitation. The agency began its analysis process in June 2013.
At that time, cardiac rehab was covered only for acute myocardial infarction within the preceding 12 months, coronary artery bypass surgery, current stable angina pectoris, heart valve repair or replacement, percutaneous transluminal coronary angioplasty or coronary stenting, and a heart or heart-lung transplant. Cardiac rehab includes physician prescribed exercise; risk factor modification, including education, counseling, and behavioral intervention; psychosocial assessment; and outcomes assessment.
Physician supervision is required for coverage.
The CMS said it had reconsidered coverage for some heart failure patients as a result of the HF-Action study, published in 2009 (JAMA 2009;301:1439-50). That study "provided the best evidence of benefit" in the HF patient group, but in particular for patients with an ejection fraction of 35% or less and New York Heart Association (NYHA) class II-IV symptoms.
Specifically, the coverage is extended to "beneficiaries with stable, chronic heart failure defined as patients with left ventricular ejection fraction of 35% or less and [NYHA] class II to IV symptoms despite being on optimal heart failure therapy for at least six weeks." The decision defines stable patients as those who have not had recent (within the past 6 weeks) or planned (within the past 6 months) major cardiovascular hospitalizations or procedures.
"We conclude that the evidence that supports the clinical benefits of the individual components of CR programs is sufficient to determine that participation in these programs improves health outcomes for Medicare beneficiaries with chronic HF," the CMS noted in its analysis.
"We’re very pleased," with the CMS decision, said Dr. Hill.
The ACC said it was still evaluating the decision. But Dr. M. Eugene Sherman, chairman of the ACC’s Advocacy Steering Committee, added that "we are pleased to see Medicare expand coverage of cardiac rehabilitation services, as the ACC requested, to a new patient population where medical and scientific literature demonstrates a medical benefit."
Dr. Hill said that the HFSA and others were hopeful that the CMS would eventually expand coverage of rehab to the remainder of HF patients.
On Twitter @aliciaault
Multiple gut operations tip scale against laparoscopic gall bladder surgery
NAPLES, FLA. – Only fewer prior abdominal surgeries predicted successful laparoscopic gall bladder surgery after percutaneous cholecystostomy tube placement in a review of 245 patients.
Notably, the degree of illness at the time of percutaneous cholecystostomy tube (PCT) placement did not seem to influence the rate of laparoscopy, Dr. Mohammad Khasawneh reported at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
"Our data suggest that having three or more prior abdominal operations seemed to reliably lean toward conversion to an open cholecystectomy," he said in an interview.
Many patients with high operative morbidity and mortality risk developing cholecystitis and are treated with PCT drainage. Cholecystectomy after PCT placement is the definitive treatment for cholecystitis among patients whose risk profile improves, but it is unclear which patients will be able to have a laparoscopic cholecystectomy, explained Dr. Khasawneh, with the department of surgery at the Mayo Clinic, Rochester, Minn.
The investigators reviewed 245 patients who had a PCT placed at the clinic from 2009 to 2011. Their median age was 71 years, and two-thirds were male. Of these, 43 patients died, 131 were not surgical candidates, and 71 went on to interval cholecystectomy in a median of 55 days (range, 42-75 days).
Laparoscopy was planned for 63 patients (89%) and successfully completed in 50 (79%), with 13 converted to open surgery. Eight cases were originally planned for open surgery.
The high mortality rate after PCT placement (17.5%) was due to the presence of comorbid conditions, according to Dr. Khasawneh.
Index admission comorbidities among cholecystectomy and non-cholecystectomy patients were prior abdominal surgeries (44% vs. 55%, respectively), mechanical ventilation (8% vs. 16%), steroid use (8.5% vs. 15%), anticoagulation use (28% vs. 32%), vasopressor use (10% both), and dysrhythmia (23% vs. 27%).
Interval cholecystectomy patients had a significantly lower overall Charlson Comorbidity Index (5 vs. 6; P = .005) and spent significantly less time in the intensive care unit (3 vs. 7 days; P less than .01) and hospital (6 vs. 9 days; P less than .01), he reported.
In multivariable regression analysis, comorbidity index and number of prior abdominal operations significantly predicted interval cholecystectomy, whereas age (odds ratio, 1.1; P = .39), presence of stones (OR, 1.7; P = .11), and mechanical ventilation at the time of PCT drainage (OR, 0.55; P = .12) did not.
Only the number of prior abdominal operations significantly predicted laparoscopic cholecystectomy (OR, 0.52; P = .02), Dr. Khasawneh reported.
"Patients who are medically cleared for cholecystectomy should have an attempt at laparoscopic cholecystectomy unless they have multiple prior operations," the authors concluded.
Dr. Khasawneh and his coauthors reported having no financial disclosures.
NAPLES, FLA. – Only fewer prior abdominal surgeries predicted successful laparoscopic gall bladder surgery after percutaneous cholecystostomy tube placement in a review of 245 patients.
Notably, the degree of illness at the time of percutaneous cholecystostomy tube (PCT) placement did not seem to influence the rate of laparoscopy, Dr. Mohammad Khasawneh reported at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
"Our data suggest that having three or more prior abdominal operations seemed to reliably lean toward conversion to an open cholecystectomy," he said in an interview.
Many patients with high operative morbidity and mortality risk developing cholecystitis and are treated with PCT drainage. Cholecystectomy after PCT placement is the definitive treatment for cholecystitis among patients whose risk profile improves, but it is unclear which patients will be able to have a laparoscopic cholecystectomy, explained Dr. Khasawneh, with the department of surgery at the Mayo Clinic, Rochester, Minn.
The investigators reviewed 245 patients who had a PCT placed at the clinic from 2009 to 2011. Their median age was 71 years, and two-thirds were male. Of these, 43 patients died, 131 were not surgical candidates, and 71 went on to interval cholecystectomy in a median of 55 days (range, 42-75 days).
Laparoscopy was planned for 63 patients (89%) and successfully completed in 50 (79%), with 13 converted to open surgery. Eight cases were originally planned for open surgery.
The high mortality rate after PCT placement (17.5%) was due to the presence of comorbid conditions, according to Dr. Khasawneh.
Index admission comorbidities among cholecystectomy and non-cholecystectomy patients were prior abdominal surgeries (44% vs. 55%, respectively), mechanical ventilation (8% vs. 16%), steroid use (8.5% vs. 15%), anticoagulation use (28% vs. 32%), vasopressor use (10% both), and dysrhythmia (23% vs. 27%).
Interval cholecystectomy patients had a significantly lower overall Charlson Comorbidity Index (5 vs. 6; P = .005) and spent significantly less time in the intensive care unit (3 vs. 7 days; P less than .01) and hospital (6 vs. 9 days; P less than .01), he reported.
In multivariable regression analysis, comorbidity index and number of prior abdominal operations significantly predicted interval cholecystectomy, whereas age (odds ratio, 1.1; P = .39), presence of stones (OR, 1.7; P = .11), and mechanical ventilation at the time of PCT drainage (OR, 0.55; P = .12) did not.
Only the number of prior abdominal operations significantly predicted laparoscopic cholecystectomy (OR, 0.52; P = .02), Dr. Khasawneh reported.
"Patients who are medically cleared for cholecystectomy should have an attempt at laparoscopic cholecystectomy unless they have multiple prior operations," the authors concluded.
Dr. Khasawneh and his coauthors reported having no financial disclosures.
NAPLES, FLA. – Only fewer prior abdominal surgeries predicted successful laparoscopic gall bladder surgery after percutaneous cholecystostomy tube placement in a review of 245 patients.
Notably, the degree of illness at the time of percutaneous cholecystostomy tube (PCT) placement did not seem to influence the rate of laparoscopy, Dr. Mohammad Khasawneh reported at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
"Our data suggest that having three or more prior abdominal operations seemed to reliably lean toward conversion to an open cholecystectomy," he said in an interview.
Many patients with high operative morbidity and mortality risk developing cholecystitis and are treated with PCT drainage. Cholecystectomy after PCT placement is the definitive treatment for cholecystitis among patients whose risk profile improves, but it is unclear which patients will be able to have a laparoscopic cholecystectomy, explained Dr. Khasawneh, with the department of surgery at the Mayo Clinic, Rochester, Minn.
The investigators reviewed 245 patients who had a PCT placed at the clinic from 2009 to 2011. Their median age was 71 years, and two-thirds were male. Of these, 43 patients died, 131 were not surgical candidates, and 71 went on to interval cholecystectomy in a median of 55 days (range, 42-75 days).
Laparoscopy was planned for 63 patients (89%) and successfully completed in 50 (79%), with 13 converted to open surgery. Eight cases were originally planned for open surgery.
The high mortality rate after PCT placement (17.5%) was due to the presence of comorbid conditions, according to Dr. Khasawneh.
Index admission comorbidities among cholecystectomy and non-cholecystectomy patients were prior abdominal surgeries (44% vs. 55%, respectively), mechanical ventilation (8% vs. 16%), steroid use (8.5% vs. 15%), anticoagulation use (28% vs. 32%), vasopressor use (10% both), and dysrhythmia (23% vs. 27%).
Interval cholecystectomy patients had a significantly lower overall Charlson Comorbidity Index (5 vs. 6; P = .005) and spent significantly less time in the intensive care unit (3 vs. 7 days; P less than .01) and hospital (6 vs. 9 days; P less than .01), he reported.
In multivariable regression analysis, comorbidity index and number of prior abdominal operations significantly predicted interval cholecystectomy, whereas age (odds ratio, 1.1; P = .39), presence of stones (OR, 1.7; P = .11), and mechanical ventilation at the time of PCT drainage (OR, 0.55; P = .12) did not.
Only the number of prior abdominal operations significantly predicted laparoscopic cholecystectomy (OR, 0.52; P = .02), Dr. Khasawneh reported.
"Patients who are medically cleared for cholecystectomy should have an attempt at laparoscopic cholecystectomy unless they have multiple prior operations," the authors concluded.
Dr. Khasawneh and his coauthors reported having no financial disclosures.
AT THE EAST SCIENTIFIC ASSEMBLY
Major finding: Fewer prior abdominal operations significantly predict successful laparoscopic cholecystectomy (OR, 0.52; P = .02).
Data source: A retrospective study of 245 patients with a percutaneous cholecystostomy tube.
Disclosures: Dr. Khasawneh and his coauthors reported having no financial disclosures.