User login
Official Newspaper of the American College of Surgeons
Laparoscopic surgery cut length of hospital stay in colorectal cancer
In patients with colorectal cancer, laparoscopic resection reduced total hospital stay by a median of 2 days, compared with open surgery, researchers reported online May 5 in the Journal of Clinical Oncology.
However, laparoscopy did not significantly improve physical fatigue at 1 month, compared with open surgery, and it did not affect other secondary clinical outcomes, said Prof. Robin Kennedy of St. Mark’s Hospital, Harrow, England, and his associates.
The researchers conducted a multicenter, randomized trial of 204 patients with colorectal cancer, of whom 103 underwent laparoscopic resection and 101 had open surgery within a standardized enhanced recovery program (J. Clin. Oncol. 2014 May 5 [doi: 10.1200/JCO.2013.54.3694]).
Median total hospital stay was significantly shorter in the laparoscopy group (5 days; interquartile range, 4-9 days) vs. the open surgery group (7 days; IQR, 5-11 days; P = .033), the investigators reported. However, 1-month physical fatigue scores on the Multidimensional Fatigue Inventory 20 were similar between the two groups (mean for laparoscopy patients, 12.28; 95% confidence interval, 11.37-13.19; mean for open surgery patients, 12.05; 95% CI, 11.14-12.96; adjusted mean difference, –0.23; 95% CI, –1.52-1.07), the researchers reported. Other outcomes also were similar, including quality of the specimens based on central pathologic review, the researchers said.
The findings contradicted those of prior studies in which shorter duration of hospital stay correlated with less "pain, ileus, and other complications, leading to earlier mobilization, feeding, and recovery," the researchers noted. They recommended more studies to determine whether the similarities between other outcomes were due to a lack of power or truly indicated comparable short-term recoveries.
The research was funded by Cancer Research UK, the National Institute for Health Research, Ethicon Endo-Surgery Europe, the Medical Research Council ConDuCT Hub, and Yorkshire Cancer Research. The authors reported that they had no relevant conflicts of interest.
In patients with colorectal cancer, laparoscopic resection reduced total hospital stay by a median of 2 days, compared with open surgery, researchers reported online May 5 in the Journal of Clinical Oncology.
However, laparoscopy did not significantly improve physical fatigue at 1 month, compared with open surgery, and it did not affect other secondary clinical outcomes, said Prof. Robin Kennedy of St. Mark’s Hospital, Harrow, England, and his associates.
The researchers conducted a multicenter, randomized trial of 204 patients with colorectal cancer, of whom 103 underwent laparoscopic resection and 101 had open surgery within a standardized enhanced recovery program (J. Clin. Oncol. 2014 May 5 [doi: 10.1200/JCO.2013.54.3694]).
Median total hospital stay was significantly shorter in the laparoscopy group (5 days; interquartile range, 4-9 days) vs. the open surgery group (7 days; IQR, 5-11 days; P = .033), the investigators reported. However, 1-month physical fatigue scores on the Multidimensional Fatigue Inventory 20 were similar between the two groups (mean for laparoscopy patients, 12.28; 95% confidence interval, 11.37-13.19; mean for open surgery patients, 12.05; 95% CI, 11.14-12.96; adjusted mean difference, –0.23; 95% CI, –1.52-1.07), the researchers reported. Other outcomes also were similar, including quality of the specimens based on central pathologic review, the researchers said.
The findings contradicted those of prior studies in which shorter duration of hospital stay correlated with less "pain, ileus, and other complications, leading to earlier mobilization, feeding, and recovery," the researchers noted. They recommended more studies to determine whether the similarities between other outcomes were due to a lack of power or truly indicated comparable short-term recoveries.
The research was funded by Cancer Research UK, the National Institute for Health Research, Ethicon Endo-Surgery Europe, the Medical Research Council ConDuCT Hub, and Yorkshire Cancer Research. The authors reported that they had no relevant conflicts of interest.
In patients with colorectal cancer, laparoscopic resection reduced total hospital stay by a median of 2 days, compared with open surgery, researchers reported online May 5 in the Journal of Clinical Oncology.
However, laparoscopy did not significantly improve physical fatigue at 1 month, compared with open surgery, and it did not affect other secondary clinical outcomes, said Prof. Robin Kennedy of St. Mark’s Hospital, Harrow, England, and his associates.
The researchers conducted a multicenter, randomized trial of 204 patients with colorectal cancer, of whom 103 underwent laparoscopic resection and 101 had open surgery within a standardized enhanced recovery program (J. Clin. Oncol. 2014 May 5 [doi: 10.1200/JCO.2013.54.3694]).
Median total hospital stay was significantly shorter in the laparoscopy group (5 days; interquartile range, 4-9 days) vs. the open surgery group (7 days; IQR, 5-11 days; P = .033), the investigators reported. However, 1-month physical fatigue scores on the Multidimensional Fatigue Inventory 20 were similar between the two groups (mean for laparoscopy patients, 12.28; 95% confidence interval, 11.37-13.19; mean for open surgery patients, 12.05; 95% CI, 11.14-12.96; adjusted mean difference, –0.23; 95% CI, –1.52-1.07), the researchers reported. Other outcomes also were similar, including quality of the specimens based on central pathologic review, the researchers said.
The findings contradicted those of prior studies in which shorter duration of hospital stay correlated with less "pain, ileus, and other complications, leading to earlier mobilization, feeding, and recovery," the researchers noted. They recommended more studies to determine whether the similarities between other outcomes were due to a lack of power or truly indicated comparable short-term recoveries.
The research was funded by Cancer Research UK, the National Institute for Health Research, Ethicon Endo-Surgery Europe, the Medical Research Council ConDuCT Hub, and Yorkshire Cancer Research. The authors reported that they had no relevant conflicts of interest.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical finding: Laparoscopy should be considered over open surgery for colorectal cancer.
Major finding: Median total hospital stay was significantly shorter when patients underwent laparoscopy (5 days; interquartile range, 4-9 days) vs. open surgery (7 days; IQR, 5-11 days; P = .033).
Data source: Multicenter randomized trial of 204 patients with colorectal cancer, of whom 103 underwent laparoscopic resection and 101 had open surgery.
Disclosures: The research was funded by Cancer Research UK, the National Institute for Health Research, Ethicon Endo-Surgery Europe, the Medical Research Council ConDuCT Hub, and Yorkshire Cancer Research. The authors reported that they had no relevant conflicts of interest.
VIDEO: Statins flop in COPD, but hope remains
SAN DIEGO – Two randomized, controlled trials presented at the American Thoracic Society international conference reported that statins did not improve pulmonary function or reduce exacerbations in patients with chronic obstructive pulmonary disease. But not everyone has given up on statins.
When a drug that showed promise in large observational studies doesn’t pan out in randomized, controlled trials, physicians start looking for subgroups of patients that still might benefit, Dr. Nicholas Gross told us. Hear his perspective on the STATCOPE trial (in which simvastatin did not prevent exacerbations in moderate to severe COPD) and the RODEO trial (in which rosuvastatin improved endothelial function only in a subset of patients with evidence of systemic inflammation.)
Dr. Gross is an emeritus professor of medicine and molecular biochemistry at Stritch-Loyola University, Chicago. He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN DIEGO – Two randomized, controlled trials presented at the American Thoracic Society international conference reported that statins did not improve pulmonary function or reduce exacerbations in patients with chronic obstructive pulmonary disease. But not everyone has given up on statins.
When a drug that showed promise in large observational studies doesn’t pan out in randomized, controlled trials, physicians start looking for subgroups of patients that still might benefit, Dr. Nicholas Gross told us. Hear his perspective on the STATCOPE trial (in which simvastatin did not prevent exacerbations in moderate to severe COPD) and the RODEO trial (in which rosuvastatin improved endothelial function only in a subset of patients with evidence of systemic inflammation.)
Dr. Gross is an emeritus professor of medicine and molecular biochemistry at Stritch-Loyola University, Chicago. He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN DIEGO – Two randomized, controlled trials presented at the American Thoracic Society international conference reported that statins did not improve pulmonary function or reduce exacerbations in patients with chronic obstructive pulmonary disease. But not everyone has given up on statins.
When a drug that showed promise in large observational studies doesn’t pan out in randomized, controlled trials, physicians start looking for subgroups of patients that still might benefit, Dr. Nicholas Gross told us. Hear his perspective on the STATCOPE trial (in which simvastatin did not prevent exacerbations in moderate to severe COPD) and the RODEO trial (in which rosuvastatin improved endothelial function only in a subset of patients with evidence of systemic inflammation.)
Dr. Gross is an emeritus professor of medicine and molecular biochemistry at Stritch-Loyola University, Chicago. He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT ATS 2014
VIDEO: PTSD common in survivors of critical illness
SAN DIEGO – Following an ICU stay, about one-fourth of critical illness survivors are affected by symptoms of posttraumatic stress disorder, a meta-analysis of studies representing 3,437 patients demonstrated.
During a press briefing at an international conference of the American Thoracic Society, Dr. Ann Parker, a fellow in pulmonary and critical care medicine at Johns Hopkins University, Baltimore, discussed the findings and noted that certain patient-related risk factors influenced the association, including younger age, preexisting mental health problems, and post-ICU memories of frightening experiences in the ICU.
On Twitter @dougbrunk
SAN DIEGO – Following an ICU stay, about one-fourth of critical illness survivors are affected by symptoms of posttraumatic stress disorder, a meta-analysis of studies representing 3,437 patients demonstrated.
During a press briefing at an international conference of the American Thoracic Society, Dr. Ann Parker, a fellow in pulmonary and critical care medicine at Johns Hopkins University, Baltimore, discussed the findings and noted that certain patient-related risk factors influenced the association, including younger age, preexisting mental health problems, and post-ICU memories of frightening experiences in the ICU.
On Twitter @dougbrunk
SAN DIEGO – Following an ICU stay, about one-fourth of critical illness survivors are affected by symptoms of posttraumatic stress disorder, a meta-analysis of studies representing 3,437 patients demonstrated.
During a press briefing at an international conference of the American Thoracic Society, Dr. Ann Parker, a fellow in pulmonary and critical care medicine at Johns Hopkins University, Baltimore, discussed the findings and noted that certain patient-related risk factors influenced the association, including younger age, preexisting mental health problems, and post-ICU memories of frightening experiences in the ICU.
On Twitter @dougbrunk
AT ATS 2014
A fatal ‘never event’
DB was a 22-year-old man who was brought to the hospital after he was found down in the street by police. Witnesses confirmed that DB was a pedestrian involved in a hit-and-run accident with a motor vehicle.
Upon initial assessment at the hospital, DB was awake and alert. Imaging confirmed several rib fractures, a broken right humerus, and two burst fractures of the thoracic spine. In addition, DB had evidence of a pulmonary contusion and a pneumothorax. DB went to the operating room for his spinal injuries and was subsequently admitted by Dr. Hospitalist 1 to the trauma intensive care unit. DB remained intubated and sedated. Dr. Hospitalist 1 documented that DB was at high risk for venous thromboembolism (VTE) and DB received bilateral intermittent pneumatic compression (IPC) of his legs and subcutaneous unfractionated heparin (UFH), 5,000 units every 8 hours, for VTE prophylaxis.
Over the next week, DB underwent open reduction and internal fixation of his right humerus fracture, along with an additional neurosurgical procedure to further stabilize his spine. DB made progress with respect to his pneumothorax and his chest tubes were eventually discontinued. DB was extubated on hospital day 5. On hospital day 7, DB was transferred out of the trauma ICU. For unclear reasons, DB’s prophylactic UFH was discontinued at the time of transfer. DB continued to wear bilateral IPC devices on his legs while he was in bed.
DB began physical therapy, but he had significant pain control issues. On hospital day 11, Dr. Hospitalist 2 restarted UFH, 5,000 units every 8 hours, for VTE prophylaxis. Two days later, DB was noted to have asymmetric edema of his right lower extremity and Dr. Hospitalist 3 obtained a vascular ultrasound. DB was diagnosed with an acute right femoral deep vein thrombosis. Dr. Hospitalist 3 ordered intravenous UFH 80 units/kg bolus followed by an intravenous infusion at 18 units/kg per hour.
The following morning (hospital day 14), the activated partial thromboplastin time was noted to be 82 seconds (1.5-2.5 thromboplastin time control). At approximately 10 a.m. that same day, DB collapsed while he was up to the commode. A code blue was called, but DB did not respond to resuscitation and was pronounced dead at 10:45 a.m. Autopsy confirmed the cause of death as a large saddle pulmonary embolism.
Complaint
DB’s mother was a flight attendant and very familiar with the concept of VTE and VTE prevention. According to her research on the internet, pulmonary embolism (PE) was a "never event" for hospitals and she immediately sought DB’s medical records to ascertain whether appropriate VTE prophylaxis had occurred. Once she discovered that DB had his prophylactic UFH discontinued for 4 days (12 doses of heparin missed), she contacted an attorney and a complaint was filed.
The complaint alleged that the physicians caring for DB failed to apply appropriate VTE prophylaxis commensurate with his high risk, and their collective failure in this regard was the proximate cause for his acute deep vein thrombosis and fatal PE.
Scientific principles
Trauma patients are considered to be at high risk for the development of VTE and some form of prophylaxis is universally recommended. Low-dose UFH given subcutaneously has been shown in multiple studies to safely and effectively decrease the incidence of VTE in high-risk groups. For those patients deemed to be at prohibitive risk for bleeding, nonpharmacologic methods of prevention are recommended. IPC prevents venous thrombosis by enhancing blood flow in the deep veins of the legs, thereby preventing venous stasis. IPC also reduces plasminogen activator inhibitor-1 (PAI-1), thereby increasing endogenous fibrinolytic activity.
Despite appropriate prophylaxis, acute VTE can still occur. Full-dose anticoagulant therapy is indicated for patients with symptomatic VTE, and anticoagulation is usually achieved initially with intravenous UFH or weight-adjusted doses of subcutaneous low-molecular-weight heparin. A 2010 meta-analysis of 13 prospective cohort studies and 56 randomized clinical trials demonstrated that the rate of recurrent fatal VTE following the appropriate initiation of full-dose anticoagulant therapy was just 0.4% (Ann. Intern. Med.2010;152:578-89).
Complaint rebuttal and discussion
The defense argued that the approach to VTE prophylaxis in a patient such as DB was a matter of clinical judgment and that, regardless of the strategy applied, acute events can and do occur. The defense highlighted the fact that DB was persistently anemic following his ICU transfer and that the physicians were concerned about possible hemorrhage. The defense also pointed out that DB continued to receive mechanical prophylaxis, which was appropriate.
In addition, the defense explained that DB had his acute DVT diagnosed immediately and he received appropriate full-dose anticoagulation prior to his death; DB therefore had less than a 0.4% chance of dying from VTE, according to the literature. Defense experts opined that, since DB went on to succumb to fatal PE despite adequate therapy, he was somehow different than those who typically respond to treatment and/or VTE prevention. In other words, the defense experts opined that DB would have developed and ultimately died from VTE regardless of what the physicians did or didn’t do in this case.
Conclusion
At the time of DB’s transition of care from the ICU to the regular nursing floor, there was no chart documentation to support the notion that his physicians were concerned about hemorrhage. It is more likely than not that DB had his subcutaneous UFH discontinued for several days by mistake.
Whether DB would still have suffered an acute DVT (along with a fatal PE) had the UFH prophylaxis not been interrupted is unknown. Sadly, DB defied the odds when he did not respond to treatment following the diagnosis of his acute DVT. At the end of the day, the plaintiffs were unable to find an expert to rebut the opinions of the defense in this case and, as a result, the case was dismissed without prejudice.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
DB was a 22-year-old man who was brought to the hospital after he was found down in the street by police. Witnesses confirmed that DB was a pedestrian involved in a hit-and-run accident with a motor vehicle.
Upon initial assessment at the hospital, DB was awake and alert. Imaging confirmed several rib fractures, a broken right humerus, and two burst fractures of the thoracic spine. In addition, DB had evidence of a pulmonary contusion and a pneumothorax. DB went to the operating room for his spinal injuries and was subsequently admitted by Dr. Hospitalist 1 to the trauma intensive care unit. DB remained intubated and sedated. Dr. Hospitalist 1 documented that DB was at high risk for venous thromboembolism (VTE) and DB received bilateral intermittent pneumatic compression (IPC) of his legs and subcutaneous unfractionated heparin (UFH), 5,000 units every 8 hours, for VTE prophylaxis.
Over the next week, DB underwent open reduction and internal fixation of his right humerus fracture, along with an additional neurosurgical procedure to further stabilize his spine. DB made progress with respect to his pneumothorax and his chest tubes were eventually discontinued. DB was extubated on hospital day 5. On hospital day 7, DB was transferred out of the trauma ICU. For unclear reasons, DB’s prophylactic UFH was discontinued at the time of transfer. DB continued to wear bilateral IPC devices on his legs while he was in bed.
DB began physical therapy, but he had significant pain control issues. On hospital day 11, Dr. Hospitalist 2 restarted UFH, 5,000 units every 8 hours, for VTE prophylaxis. Two days later, DB was noted to have asymmetric edema of his right lower extremity and Dr. Hospitalist 3 obtained a vascular ultrasound. DB was diagnosed with an acute right femoral deep vein thrombosis. Dr. Hospitalist 3 ordered intravenous UFH 80 units/kg bolus followed by an intravenous infusion at 18 units/kg per hour.
The following morning (hospital day 14), the activated partial thromboplastin time was noted to be 82 seconds (1.5-2.5 thromboplastin time control). At approximately 10 a.m. that same day, DB collapsed while he was up to the commode. A code blue was called, but DB did not respond to resuscitation and was pronounced dead at 10:45 a.m. Autopsy confirmed the cause of death as a large saddle pulmonary embolism.
Complaint
DB’s mother was a flight attendant and very familiar with the concept of VTE and VTE prevention. According to her research on the internet, pulmonary embolism (PE) was a "never event" for hospitals and she immediately sought DB’s medical records to ascertain whether appropriate VTE prophylaxis had occurred. Once she discovered that DB had his prophylactic UFH discontinued for 4 days (12 doses of heparin missed), she contacted an attorney and a complaint was filed.
The complaint alleged that the physicians caring for DB failed to apply appropriate VTE prophylaxis commensurate with his high risk, and their collective failure in this regard was the proximate cause for his acute deep vein thrombosis and fatal PE.
Scientific principles
Trauma patients are considered to be at high risk for the development of VTE and some form of prophylaxis is universally recommended. Low-dose UFH given subcutaneously has been shown in multiple studies to safely and effectively decrease the incidence of VTE in high-risk groups. For those patients deemed to be at prohibitive risk for bleeding, nonpharmacologic methods of prevention are recommended. IPC prevents venous thrombosis by enhancing blood flow in the deep veins of the legs, thereby preventing venous stasis. IPC also reduces plasminogen activator inhibitor-1 (PAI-1), thereby increasing endogenous fibrinolytic activity.
Despite appropriate prophylaxis, acute VTE can still occur. Full-dose anticoagulant therapy is indicated for patients with symptomatic VTE, and anticoagulation is usually achieved initially with intravenous UFH or weight-adjusted doses of subcutaneous low-molecular-weight heparin. A 2010 meta-analysis of 13 prospective cohort studies and 56 randomized clinical trials demonstrated that the rate of recurrent fatal VTE following the appropriate initiation of full-dose anticoagulant therapy was just 0.4% (Ann. Intern. Med.2010;152:578-89).
Complaint rebuttal and discussion
The defense argued that the approach to VTE prophylaxis in a patient such as DB was a matter of clinical judgment and that, regardless of the strategy applied, acute events can and do occur. The defense highlighted the fact that DB was persistently anemic following his ICU transfer and that the physicians were concerned about possible hemorrhage. The defense also pointed out that DB continued to receive mechanical prophylaxis, which was appropriate.
In addition, the defense explained that DB had his acute DVT diagnosed immediately and he received appropriate full-dose anticoagulation prior to his death; DB therefore had less than a 0.4% chance of dying from VTE, according to the literature. Defense experts opined that, since DB went on to succumb to fatal PE despite adequate therapy, he was somehow different than those who typically respond to treatment and/or VTE prevention. In other words, the defense experts opined that DB would have developed and ultimately died from VTE regardless of what the physicians did or didn’t do in this case.
Conclusion
At the time of DB’s transition of care from the ICU to the regular nursing floor, there was no chart documentation to support the notion that his physicians were concerned about hemorrhage. It is more likely than not that DB had his subcutaneous UFH discontinued for several days by mistake.
Whether DB would still have suffered an acute DVT (along with a fatal PE) had the UFH prophylaxis not been interrupted is unknown. Sadly, DB defied the odds when he did not respond to treatment following the diagnosis of his acute DVT. At the end of the day, the plaintiffs were unable to find an expert to rebut the opinions of the defense in this case and, as a result, the case was dismissed without prejudice.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
DB was a 22-year-old man who was brought to the hospital after he was found down in the street by police. Witnesses confirmed that DB was a pedestrian involved in a hit-and-run accident with a motor vehicle.
Upon initial assessment at the hospital, DB was awake and alert. Imaging confirmed several rib fractures, a broken right humerus, and two burst fractures of the thoracic spine. In addition, DB had evidence of a pulmonary contusion and a pneumothorax. DB went to the operating room for his spinal injuries and was subsequently admitted by Dr. Hospitalist 1 to the trauma intensive care unit. DB remained intubated and sedated. Dr. Hospitalist 1 documented that DB was at high risk for venous thromboembolism (VTE) and DB received bilateral intermittent pneumatic compression (IPC) of his legs and subcutaneous unfractionated heparin (UFH), 5,000 units every 8 hours, for VTE prophylaxis.
Over the next week, DB underwent open reduction and internal fixation of his right humerus fracture, along with an additional neurosurgical procedure to further stabilize his spine. DB made progress with respect to his pneumothorax and his chest tubes were eventually discontinued. DB was extubated on hospital day 5. On hospital day 7, DB was transferred out of the trauma ICU. For unclear reasons, DB’s prophylactic UFH was discontinued at the time of transfer. DB continued to wear bilateral IPC devices on his legs while he was in bed.
DB began physical therapy, but he had significant pain control issues. On hospital day 11, Dr. Hospitalist 2 restarted UFH, 5,000 units every 8 hours, for VTE prophylaxis. Two days later, DB was noted to have asymmetric edema of his right lower extremity and Dr. Hospitalist 3 obtained a vascular ultrasound. DB was diagnosed with an acute right femoral deep vein thrombosis. Dr. Hospitalist 3 ordered intravenous UFH 80 units/kg bolus followed by an intravenous infusion at 18 units/kg per hour.
The following morning (hospital day 14), the activated partial thromboplastin time was noted to be 82 seconds (1.5-2.5 thromboplastin time control). At approximately 10 a.m. that same day, DB collapsed while he was up to the commode. A code blue was called, but DB did not respond to resuscitation and was pronounced dead at 10:45 a.m. Autopsy confirmed the cause of death as a large saddle pulmonary embolism.
Complaint
DB’s mother was a flight attendant and very familiar with the concept of VTE and VTE prevention. According to her research on the internet, pulmonary embolism (PE) was a "never event" for hospitals and she immediately sought DB’s medical records to ascertain whether appropriate VTE prophylaxis had occurred. Once she discovered that DB had his prophylactic UFH discontinued for 4 days (12 doses of heparin missed), she contacted an attorney and a complaint was filed.
The complaint alleged that the physicians caring for DB failed to apply appropriate VTE prophylaxis commensurate with his high risk, and their collective failure in this regard was the proximate cause for his acute deep vein thrombosis and fatal PE.
Scientific principles
Trauma patients are considered to be at high risk for the development of VTE and some form of prophylaxis is universally recommended. Low-dose UFH given subcutaneously has been shown in multiple studies to safely and effectively decrease the incidence of VTE in high-risk groups. For those patients deemed to be at prohibitive risk for bleeding, nonpharmacologic methods of prevention are recommended. IPC prevents venous thrombosis by enhancing blood flow in the deep veins of the legs, thereby preventing venous stasis. IPC also reduces plasminogen activator inhibitor-1 (PAI-1), thereby increasing endogenous fibrinolytic activity.
Despite appropriate prophylaxis, acute VTE can still occur. Full-dose anticoagulant therapy is indicated for patients with symptomatic VTE, and anticoagulation is usually achieved initially with intravenous UFH or weight-adjusted doses of subcutaneous low-molecular-weight heparin. A 2010 meta-analysis of 13 prospective cohort studies and 56 randomized clinical trials demonstrated that the rate of recurrent fatal VTE following the appropriate initiation of full-dose anticoagulant therapy was just 0.4% (Ann. Intern. Med.2010;152:578-89).
Complaint rebuttal and discussion
The defense argued that the approach to VTE prophylaxis in a patient such as DB was a matter of clinical judgment and that, regardless of the strategy applied, acute events can and do occur. The defense highlighted the fact that DB was persistently anemic following his ICU transfer and that the physicians were concerned about possible hemorrhage. The defense also pointed out that DB continued to receive mechanical prophylaxis, which was appropriate.
In addition, the defense explained that DB had his acute DVT diagnosed immediately and he received appropriate full-dose anticoagulation prior to his death; DB therefore had less than a 0.4% chance of dying from VTE, according to the literature. Defense experts opined that, since DB went on to succumb to fatal PE despite adequate therapy, he was somehow different than those who typically respond to treatment and/or VTE prevention. In other words, the defense experts opined that DB would have developed and ultimately died from VTE regardless of what the physicians did or didn’t do in this case.
Conclusion
At the time of DB’s transition of care from the ICU to the regular nursing floor, there was no chart documentation to support the notion that his physicians were concerned about hemorrhage. It is more likely than not that DB had his subcutaneous UFH discontinued for several days by mistake.
Whether DB would still have suffered an acute DVT (along with a fatal PE) had the UFH prophylaxis not been interrupted is unknown. Sadly, DB defied the odds when he did not respond to treatment following the diagnosis of his acute DVT. At the end of the day, the plaintiffs were unable to find an expert to rebut the opinions of the defense in this case and, as a result, the case was dismissed without prejudice.
Dr. Michota is director of academic affairs in the hospital medicine department at the Cleveland Clinic and medical editor of Hospitalist News. He has been involved in peer review both within and outside the legal system.
Patient outcomes not affected by attendings running ‘simultaneous’ ORs
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs.
However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single-institution review presented by Dr. Kenan W. Yount at the annual meeting of the American Association for Thoracic Surgery.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon to operating room.
In his presentation, Dr. Yount discussed the results of their review, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two operations. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates of postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 types of surgery, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically impact operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also, operations being scheduled in separate rooms must be done so with reasonable foresight." As long as institutions are following these practices, he concluded, "it would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs.
However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single-institution review presented by Dr. Kenan W. Yount at the annual meeting of the American Association for Thoracic Surgery.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon to operating room.
In his presentation, Dr. Yount discussed the results of their review, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two operations. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates of postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 types of surgery, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically impact operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also, operations being scheduled in separate rooms must be done so with reasonable foresight." As long as institutions are following these practices, he concluded, "it would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs.
However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single-institution review presented by Dr. Kenan W. Yount at the annual meeting of the American Association for Thoracic Surgery.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon to operating room.
In his presentation, Dr. Yount discussed the results of their review, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two operations. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates of postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 types of surgery, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically impact operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also, operations being scheduled in separate rooms must be done so with reasonable foresight." As long as institutions are following these practices, he concluded, "it would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
AT THE AATS ANNUAL MEETING
Major finding: Running two rooms was not associated with any differences in operative duration, morbidity, or mortality in multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category.
Data source: The study reviewed 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two operations.
Disclosures: Dr. Yount had no disclosures.
VIDEO: It's time to focus on less severe sepsis
SAN DIEGO – About half of sepsis-related deaths are in people with normal blood pressure and normal or intermediate serum lactate levels (less than 4 mmol/L) on admission, suggesting that perhaps in some cases, sepsis that could have been extinguished early got out of hand before it was recognized, according to a review of about 7 million adult hospital admissions by Kaiser Permanente researchers.
In other words, even though death rates have come down for patients with severe sepsis, there’s still a ways to go to recognize and treat less severe cases in time. Lead investigator Dr. Vincent Liu of the Kaiser Permanente division of research, Oakland, Calif., explained the problem – and what Kaiser’s doing about it – at an international conference of the American Thoracic Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – About half of sepsis-related deaths are in people with normal blood pressure and normal or intermediate serum lactate levels (less than 4 mmol/L) on admission, suggesting that perhaps in some cases, sepsis that could have been extinguished early got out of hand before it was recognized, according to a review of about 7 million adult hospital admissions by Kaiser Permanente researchers.
In other words, even though death rates have come down for patients with severe sepsis, there’s still a ways to go to recognize and treat less severe cases in time. Lead investigator Dr. Vincent Liu of the Kaiser Permanente division of research, Oakland, Calif., explained the problem – and what Kaiser’s doing about it – at an international conference of the American Thoracic Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – About half of sepsis-related deaths are in people with normal blood pressure and normal or intermediate serum lactate levels (less than 4 mmol/L) on admission, suggesting that perhaps in some cases, sepsis that could have been extinguished early got out of hand before it was recognized, according to a review of about 7 million adult hospital admissions by Kaiser Permanente researchers.
In other words, even though death rates have come down for patients with severe sepsis, there’s still a ways to go to recognize and treat less severe cases in time. Lead investigator Dr. Vincent Liu of the Kaiser Permanente division of research, Oakland, Calif., explained the problem – and what Kaiser’s doing about it – at an international conference of the American Thoracic Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ATS 2014
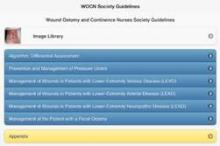
Reference apps bring the evidence to you
There are at least two ways to consider the meaning of evidence-based apps. One is a category of apps that have clinical trial evidence showing that they are useful, a topic we cover regularly in this column.
Another category, though, is apps that take existing evidence-based guidelines or already-vetted medical information and deliver that to you in a more efficient, convenient package.
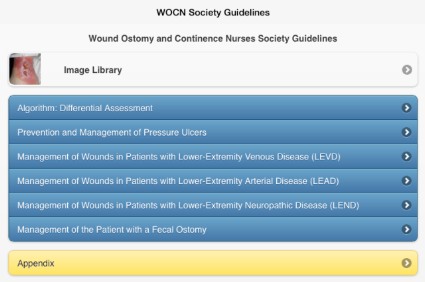
One of the latest examples of the latter is the new Evidence-Based Wound Care Guidelines and Fecal Ostomy Best Practice app, sold by the Wound, Ostomy and Continence Nurses Society (WOCN) for iPhones, iPads, or iPod Touch devices. Is it worth the $60 price?
It would cost you at least $160 to buy print copies from the WOCN of the five guidelines included in the app, on management of patients with pressure ulcers, lower-extremity arterial disease (LEAD), lower-extremity neuropathic disease (LEND), lower-extremity venous disease (LEVD), and fecal ostomy.
Or, you could spend a fair amount of time finding and printing the equivalent guidelines in the archives of medical journals or online. The Agency for Healthcare Research and Quality (AHRQ) provides detailed summaries of most of these guidelines on its website, including the major recommendations in each guideline and ratings of the evidence behind those recommendations. You can find the AHRQ pages on management of pressure ulcers, LEND, LEVD, and fecal ostomy, for example. They’re free, but it’s a time-consuming process that leaves you with bulky printouts.
Alternatively, the WOCN offers a free, 12-page, quick-reference guide for management of lower-extremity venous, arterial, or neuropathic wounds that you can download and print for free or, alternatively, consult without printing.
All in all, that’s a lot of dead trees to carry around if you want to consult these guidelines while treating patients, unless you have a bulky desktop computer handy. Compare that with the convenience of pulling out your smartphone or tablet to consult the literature on best practices at the bedside, and you can see why knowledge-delivering apps have caught physicians’ imaginations.
How can you know that an app is delivering credible information? The easiest way is to choose an app from a credible organization, such as the Cancer.Net app for patients with cancer, from the American Society of Clinical Oncology. Apps that have been vetted by the likes of the Cleveland Clinic, Mayo Clinic, or Veterans Affairs Healthcare System, for example, typically have been assessed with some quality-control measures. Every app has its flaws, however, so it’s usually worth searching for reviews online to gauge the strengths and weaknesses of various apps, especially when there is more than one available on a particular topic.
For-profit companies have developed some of the most popular evidence-driven apps for physicians. UpToDate claims that its physicians, authors, and editors synthesize the available medical evidence so the app can provide recommendations in primary care, ob.gyn., pediatrics, general surgery, emergency medicine, internal medicine, and all of the internal medicine subspecialties, among others. An individual subscription costs $499/year.
Epocrates offers a free app that provides medication information and lets you look up drug interactions and more, with additional services for a fee. Other apps do the same – Lexicomp is one subscription-based app that allows a 30-day free trial.
How to choose? Again, reviews may be helpful. The physician-run site iMedicalApps compared several medical drug reference apps in a 2010 review, but in app development time, that already seems light-years ago.
If you don’t recognize a company as a credible player in delivering mobile medical information, you can take several steps to assess the app’s trustworthiness. When you look at the app’s description online or in your mobile device’s app store, often the description is short and doesn’t list the reference information that the app relies on, though that’s often included in the app itself.
You’ll find reviews and ratings in the app description, but take these with a grain of salt. These can be anonymous, reflect anecdotal experiences, and may be planted by the developer of the app to make it look good.
Click on the tab for the developer in the app description, and if you don’t recognize the name, make sure there’s a link to a website or at least an e-mail address so you can assess whether the developer has health care expertise.
It’s also worth clicking on the Updates or Version History tab to see if it’s been updated, because good-quality apps usually get frequent updates, typically at least every 6 months, several app consultants said in interviews.
Are you already using evidence-delivering apps? Which are your favorites? Let us know, and we may highlight them in a future column.
On Twitter @sherryboschert
There are at least two ways to consider the meaning of evidence-based apps. One is a category of apps that have clinical trial evidence showing that they are useful, a topic we cover regularly in this column.
Another category, though, is apps that take existing evidence-based guidelines or already-vetted medical information and deliver that to you in a more efficient, convenient package.
One of the latest examples of the latter is the new Evidence-Based Wound Care Guidelines and Fecal Ostomy Best Practice app, sold by the Wound, Ostomy and Continence Nurses Society (WOCN) for iPhones, iPads, or iPod Touch devices. Is it worth the $60 price?
It would cost you at least $160 to buy print copies from the WOCN of the five guidelines included in the app, on management of patients with pressure ulcers, lower-extremity arterial disease (LEAD), lower-extremity neuropathic disease (LEND), lower-extremity venous disease (LEVD), and fecal ostomy.
Or, you could spend a fair amount of time finding and printing the equivalent guidelines in the archives of medical journals or online. The Agency for Healthcare Research and Quality (AHRQ) provides detailed summaries of most of these guidelines on its website, including the major recommendations in each guideline and ratings of the evidence behind those recommendations. You can find the AHRQ pages on management of pressure ulcers, LEND, LEVD, and fecal ostomy, for example. They’re free, but it’s a time-consuming process that leaves you with bulky printouts.
Alternatively, the WOCN offers a free, 12-page, quick-reference guide for management of lower-extremity venous, arterial, or neuropathic wounds that you can download and print for free or, alternatively, consult without printing.
All in all, that’s a lot of dead trees to carry around if you want to consult these guidelines while treating patients, unless you have a bulky desktop computer handy. Compare that with the convenience of pulling out your smartphone or tablet to consult the literature on best practices at the bedside, and you can see why knowledge-delivering apps have caught physicians’ imaginations.
How can you know that an app is delivering credible information? The easiest way is to choose an app from a credible organization, such as the Cancer.Net app for patients with cancer, from the American Society of Clinical Oncology. Apps that have been vetted by the likes of the Cleveland Clinic, Mayo Clinic, or Veterans Affairs Healthcare System, for example, typically have been assessed with some quality-control measures. Every app has its flaws, however, so it’s usually worth searching for reviews online to gauge the strengths and weaknesses of various apps, especially when there is more than one available on a particular topic.
For-profit companies have developed some of the most popular evidence-driven apps for physicians. UpToDate claims that its physicians, authors, and editors synthesize the available medical evidence so the app can provide recommendations in primary care, ob.gyn., pediatrics, general surgery, emergency medicine, internal medicine, and all of the internal medicine subspecialties, among others. An individual subscription costs $499/year.
Epocrates offers a free app that provides medication information and lets you look up drug interactions and more, with additional services for a fee. Other apps do the same – Lexicomp is one subscription-based app that allows a 30-day free trial.
How to choose? Again, reviews may be helpful. The physician-run site iMedicalApps compared several medical drug reference apps in a 2010 review, but in app development time, that already seems light-years ago.
If you don’t recognize a company as a credible player in delivering mobile medical information, you can take several steps to assess the app’s trustworthiness. When you look at the app’s description online or in your mobile device’s app store, often the description is short and doesn’t list the reference information that the app relies on, though that’s often included in the app itself.
You’ll find reviews and ratings in the app description, but take these with a grain of salt. These can be anonymous, reflect anecdotal experiences, and may be planted by the developer of the app to make it look good.
Click on the tab for the developer in the app description, and if you don’t recognize the name, make sure there’s a link to a website or at least an e-mail address so you can assess whether the developer has health care expertise.
It’s also worth clicking on the Updates or Version History tab to see if it’s been updated, because good-quality apps usually get frequent updates, typically at least every 6 months, several app consultants said in interviews.
Are you already using evidence-delivering apps? Which are your favorites? Let us know, and we may highlight them in a future column.
On Twitter @sherryboschert
There are at least two ways to consider the meaning of evidence-based apps. One is a category of apps that have clinical trial evidence showing that they are useful, a topic we cover regularly in this column.
Another category, though, is apps that take existing evidence-based guidelines or already-vetted medical information and deliver that to you in a more efficient, convenient package.
One of the latest examples of the latter is the new Evidence-Based Wound Care Guidelines and Fecal Ostomy Best Practice app, sold by the Wound, Ostomy and Continence Nurses Society (WOCN) for iPhones, iPads, or iPod Touch devices. Is it worth the $60 price?
It would cost you at least $160 to buy print copies from the WOCN of the five guidelines included in the app, on management of patients with pressure ulcers, lower-extremity arterial disease (LEAD), lower-extremity neuropathic disease (LEND), lower-extremity venous disease (LEVD), and fecal ostomy.
Or, you could spend a fair amount of time finding and printing the equivalent guidelines in the archives of medical journals or online. The Agency for Healthcare Research and Quality (AHRQ) provides detailed summaries of most of these guidelines on its website, including the major recommendations in each guideline and ratings of the evidence behind those recommendations. You can find the AHRQ pages on management of pressure ulcers, LEND, LEVD, and fecal ostomy, for example. They’re free, but it’s a time-consuming process that leaves you with bulky printouts.
Alternatively, the WOCN offers a free, 12-page, quick-reference guide for management of lower-extremity venous, arterial, or neuropathic wounds that you can download and print for free or, alternatively, consult without printing.
All in all, that’s a lot of dead trees to carry around if you want to consult these guidelines while treating patients, unless you have a bulky desktop computer handy. Compare that with the convenience of pulling out your smartphone or tablet to consult the literature on best practices at the bedside, and you can see why knowledge-delivering apps have caught physicians’ imaginations.
How can you know that an app is delivering credible information? The easiest way is to choose an app from a credible organization, such as the Cancer.Net app for patients with cancer, from the American Society of Clinical Oncology. Apps that have been vetted by the likes of the Cleveland Clinic, Mayo Clinic, or Veterans Affairs Healthcare System, for example, typically have been assessed with some quality-control measures. Every app has its flaws, however, so it’s usually worth searching for reviews online to gauge the strengths and weaknesses of various apps, especially when there is more than one available on a particular topic.
For-profit companies have developed some of the most popular evidence-driven apps for physicians. UpToDate claims that its physicians, authors, and editors synthesize the available medical evidence so the app can provide recommendations in primary care, ob.gyn., pediatrics, general surgery, emergency medicine, internal medicine, and all of the internal medicine subspecialties, among others. An individual subscription costs $499/year.
Epocrates offers a free app that provides medication information and lets you look up drug interactions and more, with additional services for a fee. Other apps do the same – Lexicomp is one subscription-based app that allows a 30-day free trial.
How to choose? Again, reviews may be helpful. The physician-run site iMedicalApps compared several medical drug reference apps in a 2010 review, but in app development time, that already seems light-years ago.
If you don’t recognize a company as a credible player in delivering mobile medical information, you can take several steps to assess the app’s trustworthiness. When you look at the app’s description online or in your mobile device’s app store, often the description is short and doesn’t list the reference information that the app relies on, though that’s often included in the app itself.
You’ll find reviews and ratings in the app description, but take these with a grain of salt. These can be anonymous, reflect anecdotal experiences, and may be planted by the developer of the app to make it look good.
Click on the tab for the developer in the app description, and if you don’t recognize the name, make sure there’s a link to a website or at least an e-mail address so you can assess whether the developer has health care expertise.
It’s also worth clicking on the Updates or Version History tab to see if it’s been updated, because good-quality apps usually get frequent updates, typically at least every 6 months, several app consultants said in interviews.
Are you already using evidence-delivering apps? Which are your favorites? Let us know, and we may highlight them in a future column.
On Twitter @sherryboschert
RKV/BSA ratio predicted decline of renal function after radical nephrectomy
ORLANDO – Absence of comorbidities, larger remnant kidney volume/body surface area ratio, and larger tumor diameter were significant predictors of mild renal insufficiency following radical nephrectomy, and smaller tumor diameter was a significant predictor of severe renal insufficiency in an analysis of 53 cases.
"This is the first report to identify the remnant kidney volume/body surface area (RKV/BSA) ratio as a promising predictor of post–radical nephrectomy renal functional decline," according to Dr. Takehiro Sejima, a urologist at Tottori University, Yonago, Japan, whose research was featured in an "Outstanding Posters" session at the annual meeting of the American Urological Association.
At a cutoff value of 115, the RKV/BSA ratio had 47.6% sensitivity and 79.2% specificity for predicting mild renal insufficiency using a receiver operating characteristic curve, Dr. Sejima said.
A total of 21 patients categorized as having mild renal insufficiency and 32 patients categorized as having severe renal insufficiency were included in the study. Those with severe renal insufficiency had a significantly greater extent of global glomerulosclerosis, compared with those with mild renal insufficiency. Also, cardiovascular disease events occurred in 11 patients with severe renal insufficiency during up to 122.5 months of follow-up; no cardiovascular disease events occurred in those with mild renal insufficiency, he said.
Estimated glomerular filtration rates were measured preoperatively, and at 6-12 months after radical nephrectomy in 175 patients. Those with a greater than 20% drop in estimated glomerular filtration rates were classified as having mild renal insufficiency, and those with a percentage decline above 40% were classified as having severe renal insufficiency.
"Our results provide physicians and patients with a useful predictor of renal functional outcomes preoperatively. The consideration of post–radical nephrectomy medical management for the prevention of cardiovascular disease, except in mild renal insufficiency patients, should be a future step toward improving the overall survival of post–radical nephrectomy patients," he concluded.
Dr. Sejima reported having no disclosures.
ORLANDO – Absence of comorbidities, larger remnant kidney volume/body surface area ratio, and larger tumor diameter were significant predictors of mild renal insufficiency following radical nephrectomy, and smaller tumor diameter was a significant predictor of severe renal insufficiency in an analysis of 53 cases.
"This is the first report to identify the remnant kidney volume/body surface area (RKV/BSA) ratio as a promising predictor of post–radical nephrectomy renal functional decline," according to Dr. Takehiro Sejima, a urologist at Tottori University, Yonago, Japan, whose research was featured in an "Outstanding Posters" session at the annual meeting of the American Urological Association.
At a cutoff value of 115, the RKV/BSA ratio had 47.6% sensitivity and 79.2% specificity for predicting mild renal insufficiency using a receiver operating characteristic curve, Dr. Sejima said.
A total of 21 patients categorized as having mild renal insufficiency and 32 patients categorized as having severe renal insufficiency were included in the study. Those with severe renal insufficiency had a significantly greater extent of global glomerulosclerosis, compared with those with mild renal insufficiency. Also, cardiovascular disease events occurred in 11 patients with severe renal insufficiency during up to 122.5 months of follow-up; no cardiovascular disease events occurred in those with mild renal insufficiency, he said.
Estimated glomerular filtration rates were measured preoperatively, and at 6-12 months after radical nephrectomy in 175 patients. Those with a greater than 20% drop in estimated glomerular filtration rates were classified as having mild renal insufficiency, and those with a percentage decline above 40% were classified as having severe renal insufficiency.
"Our results provide physicians and patients with a useful predictor of renal functional outcomes preoperatively. The consideration of post–radical nephrectomy medical management for the prevention of cardiovascular disease, except in mild renal insufficiency patients, should be a future step toward improving the overall survival of post–radical nephrectomy patients," he concluded.
Dr. Sejima reported having no disclosures.
ORLANDO – Absence of comorbidities, larger remnant kidney volume/body surface area ratio, and larger tumor diameter were significant predictors of mild renal insufficiency following radical nephrectomy, and smaller tumor diameter was a significant predictor of severe renal insufficiency in an analysis of 53 cases.
"This is the first report to identify the remnant kidney volume/body surface area (RKV/BSA) ratio as a promising predictor of post–radical nephrectomy renal functional decline," according to Dr. Takehiro Sejima, a urologist at Tottori University, Yonago, Japan, whose research was featured in an "Outstanding Posters" session at the annual meeting of the American Urological Association.
At a cutoff value of 115, the RKV/BSA ratio had 47.6% sensitivity and 79.2% specificity for predicting mild renal insufficiency using a receiver operating characteristic curve, Dr. Sejima said.
A total of 21 patients categorized as having mild renal insufficiency and 32 patients categorized as having severe renal insufficiency were included in the study. Those with severe renal insufficiency had a significantly greater extent of global glomerulosclerosis, compared with those with mild renal insufficiency. Also, cardiovascular disease events occurred in 11 patients with severe renal insufficiency during up to 122.5 months of follow-up; no cardiovascular disease events occurred in those with mild renal insufficiency, he said.
Estimated glomerular filtration rates were measured preoperatively, and at 6-12 months after radical nephrectomy in 175 patients. Those with a greater than 20% drop in estimated glomerular filtration rates were classified as having mild renal insufficiency, and those with a percentage decline above 40% were classified as having severe renal insufficiency.
"Our results provide physicians and patients with a useful predictor of renal functional outcomes preoperatively. The consideration of post–radical nephrectomy medical management for the prevention of cardiovascular disease, except in mild renal insufficiency patients, should be a future step toward improving the overall survival of post–radical nephrectomy patients," he concluded.
Dr. Sejima reported having no disclosures.
AT THE AUA ANNUAL MEETING
Key clinical finding: A simple to calculate ratio predicts who will fare best after radical nephrectomy.
Major finding: At a cutoff value of 115, the RKV/BSA ratio had 47.6% sensitivity and 79.2% specificity for predicting mild renal insufficiency.
Data source: An analysis of 53 cases.
Disclosures: Dr. Sejima reported having no disclosures.
Longer laparoscopic and robotic hysterectomy time ups perioperative risk
CHICAGO – Longer operative time is independently associated with perioperative morbidity after laparoscopic and robotic hysterectomy, according to a review of cases from the American College of Surgeons National Surgical Quality Improvement Program.
The overall complication rate in the 9,064 laparoscopic and robotic hysterectomies recorded in the database (ACS NSQIP) increased significantly and in tandem with increasing operative time, Dr. Tatiana L. Catanzarite reported in a blue ribbon poster at the annual meeting of the American Congress of Obstetricians and Gynecologists.
For example, the overall complication rate was 2.79% for operative time of 20-59 minutes and 18.75% for operative time greater than 360 minutes, according to Dr. Catanzarite of Northwestern University, Chicago.
Operative time of 240 minutes or longer was associated with increased overall complications, medical complications, surgical complications, reoperation, transfusion, urinary tract infection, and deep vein thrombosis/pulmonary embolism on both bivariate and multivariable regression analysis. Factors associated with operative time of 240 minutes or longer included age over 50 years, obesity, nonsmoking status, hypertension, history of stroke or transient ischemic attack, and American Anesthesiologists Society (ASA) class greater than 3, she noted.
Patients included in the database, which contains prospectively collected data for more than 240 variables from more than 460 participating institutions, underwent total or subtotal laparoscopic hysterectomy between 2006 and 2011. Patients with concomitant procedures, emergency surgery, gynecologic cancer, ASA class 5, or operative time less than 20 minutes were excluded from the analysis.
Similar findings have been reported for general surgery, but studies in gynecology have been conflicting, Dr. Catanzarite noted.
"Future research should aim to identify risk factors for excessive operative time in order to select appropriate candidates for minimally invasive approaches and maximize surgical efficiency," she wrote.
Dr. Catanzarite reported having no relevant financial disclosures.
CHICAGO – Longer operative time is independently associated with perioperative morbidity after laparoscopic and robotic hysterectomy, according to a review of cases from the American College of Surgeons National Surgical Quality Improvement Program.
The overall complication rate in the 9,064 laparoscopic and robotic hysterectomies recorded in the database (ACS NSQIP) increased significantly and in tandem with increasing operative time, Dr. Tatiana L. Catanzarite reported in a blue ribbon poster at the annual meeting of the American Congress of Obstetricians and Gynecologists.
For example, the overall complication rate was 2.79% for operative time of 20-59 minutes and 18.75% for operative time greater than 360 minutes, according to Dr. Catanzarite of Northwestern University, Chicago.
Operative time of 240 minutes or longer was associated with increased overall complications, medical complications, surgical complications, reoperation, transfusion, urinary tract infection, and deep vein thrombosis/pulmonary embolism on both bivariate and multivariable regression analysis. Factors associated with operative time of 240 minutes or longer included age over 50 years, obesity, nonsmoking status, hypertension, history of stroke or transient ischemic attack, and American Anesthesiologists Society (ASA) class greater than 3, she noted.
Patients included in the database, which contains prospectively collected data for more than 240 variables from more than 460 participating institutions, underwent total or subtotal laparoscopic hysterectomy between 2006 and 2011. Patients with concomitant procedures, emergency surgery, gynecologic cancer, ASA class 5, or operative time less than 20 minutes were excluded from the analysis.
Similar findings have been reported for general surgery, but studies in gynecology have been conflicting, Dr. Catanzarite noted.
"Future research should aim to identify risk factors for excessive operative time in order to select appropriate candidates for minimally invasive approaches and maximize surgical efficiency," she wrote.
Dr. Catanzarite reported having no relevant financial disclosures.
CHICAGO – Longer operative time is independently associated with perioperative morbidity after laparoscopic and robotic hysterectomy, according to a review of cases from the American College of Surgeons National Surgical Quality Improvement Program.
The overall complication rate in the 9,064 laparoscopic and robotic hysterectomies recorded in the database (ACS NSQIP) increased significantly and in tandem with increasing operative time, Dr. Tatiana L. Catanzarite reported in a blue ribbon poster at the annual meeting of the American Congress of Obstetricians and Gynecologists.
For example, the overall complication rate was 2.79% for operative time of 20-59 minutes and 18.75% for operative time greater than 360 minutes, according to Dr. Catanzarite of Northwestern University, Chicago.
Operative time of 240 minutes or longer was associated with increased overall complications, medical complications, surgical complications, reoperation, transfusion, urinary tract infection, and deep vein thrombosis/pulmonary embolism on both bivariate and multivariable regression analysis. Factors associated with operative time of 240 minutes or longer included age over 50 years, obesity, nonsmoking status, hypertension, history of stroke or transient ischemic attack, and American Anesthesiologists Society (ASA) class greater than 3, she noted.
Patients included in the database, which contains prospectively collected data for more than 240 variables from more than 460 participating institutions, underwent total or subtotal laparoscopic hysterectomy between 2006 and 2011. Patients with concomitant procedures, emergency surgery, gynecologic cancer, ASA class 5, or operative time less than 20 minutes were excluded from the analysis.
Similar findings have been reported for general surgery, but studies in gynecology have been conflicting, Dr. Catanzarite noted.
"Future research should aim to identify risk factors for excessive operative time in order to select appropriate candidates for minimally invasive approaches and maximize surgical efficiency," she wrote.
Dr. Catanzarite reported having no relevant financial disclosures.
AT THE ACOG ANNUAL CLINICAL MEETING
Key clinical point: Future research should aim to identify risk factors for excessive operative time in order to select appropriate candidates for minimally invasive approaches and maximize surgical efficiency.
Major finding: The overall complication rate was 2.79% for operative time of 20-59 minutes and 18.75% for operative time greater than 360 minutes.
Data source: A retrospective study of more than 9,000 cases.
Disclosures: Dr. Catanzarite reported having no relevant financial disclosures.
PTSD symptoms a common complication of critical illness
SAN DIEGO – About one-fourth of survivors after critical illness are substantially affected by symptoms of posttraumatic stress syndrome up to 1 year after discharge from the ICU, results from a large meta-analysis demonstrated.
"This incidence is as high as PTSD following other traumatic exposures, such as wartime combat," Dr. Ann Parker said in an interview in advance of an international conference of the American Thoracic Society, where the research was presented. "It is important for clinicians to recognize that patients with preexisting psychological symptoms, receiving benzodiazepines for sedation in the ICU or reporting memories of ‘frightening’ ICU experiences are at increased risk of developing PTSD following critical illness."
In a study led by Dr. Dale M. Needham, medical director of Johns Hopkins University’s critical care physical medicine and rehabilitation program, Dr. Parker and fellow first author Dr. Thiti Sricharoenchai searched PubMed and four other databases to perform a systematic review and meta-analysis of the prevalence of and risk factors for PTSD in survivors of critical illness.
"The number of studies investigating PTSD among critical illness survivors has doubled since the publication of prior reviews [in 2007 and 2008]," said Dr. Parker, who is a fellow in pulmonary and critical care medicine at Johns Hopkins University, Baltimore. "With these additional publications, there is greater similarity between studies regarding the timing of and instruments used for PTSD symptom assessment. As a result, we provide the first meta-analysis yielding a pooled prevalence of clinically important PTSD symptoms."
The researchers evaluated the databases from inception through July 15, 2012, for studies that included adult ICU survivors, used a validated PTSD instrument 1 month or more post-ICU discharge, focused on general ICU populations, and included at least 10 patients with substantial PTSD symptoms. In all, 28 articles on 25 unique cohorts representing a total of 3,437 patients were identified. The most common validated PTSD instrument used in the studies was the Impact of Events Scale (IES), a scoring system that ranges from 0-75, with higher scores indicating greater symptoms.
Dr. Parker reported that among 429 patients who were assessed 1-6 months post-ICU discharge, the pooled mean IES score was 19 and the pooled prevalence of clinically important PTSD symptoms ranged from 23% to 42%. Among 698 patients who were assessed 7-12 months post-ICU discharge, the pooled mean IES score was 17 and the pooled prevalence of clinically important PTSD symptoms ranged from 17% to 34%. In other studies the prevalence of PTSD symptoms ranged from 5% to 62%.
Risk factors for PTSD in critical illness survivors included patient-specific factors, such as younger age and preexisting mental health disorders, as well as ICU-specific factors, including sedation with benzodiazepines and memories of "frightening" experiences in the ICU. In addition, PTSD symptoms were associated with worse quality of life.
"It seems that patients’ memories of their ICU experiences after ICU discharge may play a more important role than the duration of their stay in the ICU or the severity of their illness," Dr. Parker said. "Patients who recalled ‘frightening’ memories were more likely to have substantial PTSD symptoms. These memories may be related to delirium in the ICU, but few studies have attempted to evaluate this theory. There are very few interventions with proven efficacy for reducing PTSD symptoms in critical illness survivors. One intervention that has shown promising results in two European studies is the ICU diary, which has not been rigorously evaluated in North America."
She acknowledged certain limitations of the study, including the fact that differences between studies regarding sample populations and PTSD symptom instruments "make direct comparison difficult. However, the use of meta-analysis to pool the results of the 10 studies using the IES for PTSD symptom assessment strengthens the assertion that PTSD symptoms are highly prevalent among general critical illness survivors."
Neither Dr. Parker nor her associates had relevant financial disclosures.
SAN DIEGO – About one-fourth of survivors after critical illness are substantially affected by symptoms of posttraumatic stress syndrome up to 1 year after discharge from the ICU, results from a large meta-analysis demonstrated.
"This incidence is as high as PTSD following other traumatic exposures, such as wartime combat," Dr. Ann Parker said in an interview in advance of an international conference of the American Thoracic Society, where the research was presented. "It is important for clinicians to recognize that patients with preexisting psychological symptoms, receiving benzodiazepines for sedation in the ICU or reporting memories of ‘frightening’ ICU experiences are at increased risk of developing PTSD following critical illness."
In a study led by Dr. Dale M. Needham, medical director of Johns Hopkins University’s critical care physical medicine and rehabilitation program, Dr. Parker and fellow first author Dr. Thiti Sricharoenchai searched PubMed and four other databases to perform a systematic review and meta-analysis of the prevalence of and risk factors for PTSD in survivors of critical illness.
"The number of studies investigating PTSD among critical illness survivors has doubled since the publication of prior reviews [in 2007 and 2008]," said Dr. Parker, who is a fellow in pulmonary and critical care medicine at Johns Hopkins University, Baltimore. "With these additional publications, there is greater similarity between studies regarding the timing of and instruments used for PTSD symptom assessment. As a result, we provide the first meta-analysis yielding a pooled prevalence of clinically important PTSD symptoms."
The researchers evaluated the databases from inception through July 15, 2012, for studies that included adult ICU survivors, used a validated PTSD instrument 1 month or more post-ICU discharge, focused on general ICU populations, and included at least 10 patients with substantial PTSD symptoms. In all, 28 articles on 25 unique cohorts representing a total of 3,437 patients were identified. The most common validated PTSD instrument used in the studies was the Impact of Events Scale (IES), a scoring system that ranges from 0-75, with higher scores indicating greater symptoms.
Dr. Parker reported that among 429 patients who were assessed 1-6 months post-ICU discharge, the pooled mean IES score was 19 and the pooled prevalence of clinically important PTSD symptoms ranged from 23% to 42%. Among 698 patients who were assessed 7-12 months post-ICU discharge, the pooled mean IES score was 17 and the pooled prevalence of clinically important PTSD symptoms ranged from 17% to 34%. In other studies the prevalence of PTSD symptoms ranged from 5% to 62%.
Risk factors for PTSD in critical illness survivors included patient-specific factors, such as younger age and preexisting mental health disorders, as well as ICU-specific factors, including sedation with benzodiazepines and memories of "frightening" experiences in the ICU. In addition, PTSD symptoms were associated with worse quality of life.
"It seems that patients’ memories of their ICU experiences after ICU discharge may play a more important role than the duration of their stay in the ICU or the severity of their illness," Dr. Parker said. "Patients who recalled ‘frightening’ memories were more likely to have substantial PTSD symptoms. These memories may be related to delirium in the ICU, but few studies have attempted to evaluate this theory. There are very few interventions with proven efficacy for reducing PTSD symptoms in critical illness survivors. One intervention that has shown promising results in two European studies is the ICU diary, which has not been rigorously evaluated in North America."
She acknowledged certain limitations of the study, including the fact that differences between studies regarding sample populations and PTSD symptom instruments "make direct comparison difficult. However, the use of meta-analysis to pool the results of the 10 studies using the IES for PTSD symptom assessment strengthens the assertion that PTSD symptoms are highly prevalent among general critical illness survivors."
Neither Dr. Parker nor her associates had relevant financial disclosures.
SAN DIEGO – About one-fourth of survivors after critical illness are substantially affected by symptoms of posttraumatic stress syndrome up to 1 year after discharge from the ICU, results from a large meta-analysis demonstrated.
"This incidence is as high as PTSD following other traumatic exposures, such as wartime combat," Dr. Ann Parker said in an interview in advance of an international conference of the American Thoracic Society, where the research was presented. "It is important for clinicians to recognize that patients with preexisting psychological symptoms, receiving benzodiazepines for sedation in the ICU or reporting memories of ‘frightening’ ICU experiences are at increased risk of developing PTSD following critical illness."
In a study led by Dr. Dale M. Needham, medical director of Johns Hopkins University’s critical care physical medicine and rehabilitation program, Dr. Parker and fellow first author Dr. Thiti Sricharoenchai searched PubMed and four other databases to perform a systematic review and meta-analysis of the prevalence of and risk factors for PTSD in survivors of critical illness.
"The number of studies investigating PTSD among critical illness survivors has doubled since the publication of prior reviews [in 2007 and 2008]," said Dr. Parker, who is a fellow in pulmonary and critical care medicine at Johns Hopkins University, Baltimore. "With these additional publications, there is greater similarity between studies regarding the timing of and instruments used for PTSD symptom assessment. As a result, we provide the first meta-analysis yielding a pooled prevalence of clinically important PTSD symptoms."
The researchers evaluated the databases from inception through July 15, 2012, for studies that included adult ICU survivors, used a validated PTSD instrument 1 month or more post-ICU discharge, focused on general ICU populations, and included at least 10 patients with substantial PTSD symptoms. In all, 28 articles on 25 unique cohorts representing a total of 3,437 patients were identified. The most common validated PTSD instrument used in the studies was the Impact of Events Scale (IES), a scoring system that ranges from 0-75, with higher scores indicating greater symptoms.
Dr. Parker reported that among 429 patients who were assessed 1-6 months post-ICU discharge, the pooled mean IES score was 19 and the pooled prevalence of clinically important PTSD symptoms ranged from 23% to 42%. Among 698 patients who were assessed 7-12 months post-ICU discharge, the pooled mean IES score was 17 and the pooled prevalence of clinically important PTSD symptoms ranged from 17% to 34%. In other studies the prevalence of PTSD symptoms ranged from 5% to 62%.
Risk factors for PTSD in critical illness survivors included patient-specific factors, such as younger age and preexisting mental health disorders, as well as ICU-specific factors, including sedation with benzodiazepines and memories of "frightening" experiences in the ICU. In addition, PTSD symptoms were associated with worse quality of life.
"It seems that patients’ memories of their ICU experiences after ICU discharge may play a more important role than the duration of their stay in the ICU or the severity of their illness," Dr. Parker said. "Patients who recalled ‘frightening’ memories were more likely to have substantial PTSD symptoms. These memories may be related to delirium in the ICU, but few studies have attempted to evaluate this theory. There are very few interventions with proven efficacy for reducing PTSD symptoms in critical illness survivors. One intervention that has shown promising results in two European studies is the ICU diary, which has not been rigorously evaluated in North America."
She acknowledged certain limitations of the study, including the fact that differences between studies regarding sample populations and PTSD symptom instruments "make direct comparison difficult. However, the use of meta-analysis to pool the results of the 10 studies using the IES for PTSD symptom assessment strengthens the assertion that PTSD symptoms are highly prevalent among general critical illness survivors."
Neither Dr. Parker nor her associates had relevant financial disclosures.
AT ATS 2014
Key clinical point: PTSD symptoms affect 25% or more of patients up to a year after a critical illness.
Major finding: Among 429 survivors of critical illness who were assessed 1-6 months post-ICU discharge, the prevalence of clinically important PTSD symptoms ranged from 23% to 42%. Among 698 patients who were assessed 7-12 months post-ICU discharge, prevalence of clinically important PTSD symptoms ranged from 17% to 34%.
Data source: A meta-analysis of 28 articles in the medical literature on 25 unique cohorts representing a total of 3,437 patients.
Disclosures: Neither Dr. Parker nor her associates had relevant financial disclosures.