User login
Official Newspaper of the American College of Surgeons
Neoadjuvant chemoradiotherapy fails to boost survival
For patients with early-stage esophageal cancer, undergoing chemotherapy and radiotherapy before surgical excision failed to improve the rate of curative resection and, most importantly, failed to boost survival in a phase III clinical trial, according to a report published online June 30 in the Journal of Clinical Oncology.
Unfortunately this treatment strategy also tripled postoperative mortality, making the risk-benefit ratio even more lopsided for this patient population, said Dr. Christophe Mariette of the department of digestive and oncologic surgery, University Hospital Claude Huriez-Regional University Hospital Center, Lille (France), and his associates.
Clinical trials examining neoadjuvant chemoradiotherapy for esophageal cancer have produced conflicting results, with some showing that the approach is effective, in some cases doubling median survival, while others showed no benefit. Most such studies have been limited by small sample sizes, heterogeneity of tumor types, variations in radiation doses and chemotherapy regiments, and differences in preoperative staging techniques and the adequacy of surgical resections. Moreover, the number of study participants with early-stage esophageal cancer has been very small because most patients already have more advanced disease at presentation, the investigators noted.
For their study, Dr. Mariette and his associates confined the cohort to patients younger than 75 years with treatment-naive esophageal adenocarcinoma or squamous-cell carcinoma judged to be stage I or II using thoracoabdominal CT and endoscopic ultrasound; additional preoperative assessments using PET scanning, cervical ultrasound, or radionuclide bone scanning were optional. It required 9 years to enroll 195 patients at 30 French medical centers. These study participants were randomly assigned to receive either neoadjuvant chemotherapy plus radiotherapy before potentially curative surgery (98 subjects) or potentially curative surgery alone (97 subjects).
In the intervention group, radiotherapy involved a total dose of 45 Gy delivered in 25 fractions over the course of 5 weeks. Chemotherapy was administered during the same time period and involved two cycles of fluorouracil and cisplatin infusions. All patients in this group were clinically reevaluated 2-4 weeks after completing this regimen, and surgery was performed soon afterward.
Surgery comprised a transthoracic esophagectomy with extended two-field lymphadenectomy and either high intrathoracic anastomosis (for tumors with an infracarinal proximal margin) or cervical anastomosis (for tumors with a proximal margin above the carina).
Median follow-up was 7.8 years. There were 125 deaths: 62.4% of the intervention group died, as did 66% of the surgery-only group, a nonsignificant difference, the investigators said (J. Clin. Oncol. 2014 June 30 [doi:10.1200/JCO.2013.53.6532]).
Median overall survival was 31.8 months in the intervention group and 41.2 months in the surgery-only group, a nonsignificant difference. Similarly, 3-year overall survival was 47.5% and 5-year overall survival was 41.1% in the intervention group, compared with 53% and 33.8%, respectively, in the surgery-only group, which were also nonsignificant differences.
The rate of curative resection also was not significantly different between the intervention group (93.8%) and the surgery-only group (92.1%), indicating that reducing the tumor with chemotherapy and radiotherapy had no beneficial effect in these early-stage cancers. Previous studies have demonstrated that such downsizing is effective in more advanced esophageal cancers, Dr. Mariette and his associates noted.
Postoperative mortality was more than threefold higher among patients who underwent preoperative chemoradiotherapy (11.1%) than in the surgery-only group (3.4%). The causes of postoperative death included aortic rupture, uncontrollable chylothorax, anastomotic leak, gastric conduit necrosis, mesenteric and lower limb ischemia, and acute RDS in the intervention group, compared with pneumonia and acute RDS in the surgery-only group.
These findings suggest that preoperative chemoradiotherapy "is not the appropriate neoadjuvant therapeutic strategy for stage I or II esophageal cancer," the investigators said.
Since patients with early-stage esophageal cancer don’t appear to benefit from preoperative neoadjuvant chemoradiotherapy, perhaps it is time to consider a different approach: definitive rather than neoadjuvant chemoradiotherapy as the first-line treatment, said Dr. Brian G. Czito, Dr. Manisha Palta, and Dr. Christopher G. Willett.
Some medical centers have already adopted this approach for patients with potentially curable esophageal cancer, reserving surgery as salvage treatment. Compared with surgery as first-line treatment, definitive chemoradiotherapy is associated with a lower rate of treatment-related mortality and similar survival outcomes, they noted.
Dr. Czito, Dr. Palta, and Dr. Willett are in the department of radiation oncology at Duke Cancer Institute, Durham, N.C. They reported no financial conflicts of interest. These remarks were taken from their editorial accompanying Dr. Mariette’s report (J. Clin. Oncol. 2014 June 30 [doi:10.1200/JCO.2013.53.6532]).
Since patients with early-stage esophageal cancer don’t appear to benefit from preoperative neoadjuvant chemoradiotherapy, perhaps it is time to consider a different approach: definitive rather than neoadjuvant chemoradiotherapy as the first-line treatment, said Dr. Brian G. Czito, Dr. Manisha Palta, and Dr. Christopher G. Willett.
Some medical centers have already adopted this approach for patients with potentially curable esophageal cancer, reserving surgery as salvage treatment. Compared with surgery as first-line treatment, definitive chemoradiotherapy is associated with a lower rate of treatment-related mortality and similar survival outcomes, they noted.
Dr. Czito, Dr. Palta, and Dr. Willett are in the department of radiation oncology at Duke Cancer Institute, Durham, N.C. They reported no financial conflicts of interest. These remarks were taken from their editorial accompanying Dr. Mariette’s report (J. Clin. Oncol. 2014 June 30 [doi:10.1200/JCO.2013.53.6532]).
Since patients with early-stage esophageal cancer don’t appear to benefit from preoperative neoadjuvant chemoradiotherapy, perhaps it is time to consider a different approach: definitive rather than neoadjuvant chemoradiotherapy as the first-line treatment, said Dr. Brian G. Czito, Dr. Manisha Palta, and Dr. Christopher G. Willett.
Some medical centers have already adopted this approach for patients with potentially curable esophageal cancer, reserving surgery as salvage treatment. Compared with surgery as first-line treatment, definitive chemoradiotherapy is associated with a lower rate of treatment-related mortality and similar survival outcomes, they noted.
Dr. Czito, Dr. Palta, and Dr. Willett are in the department of radiation oncology at Duke Cancer Institute, Durham, N.C. They reported no financial conflicts of interest. These remarks were taken from their editorial accompanying Dr. Mariette’s report (J. Clin. Oncol. 2014 June 30 [doi:10.1200/JCO.2013.53.6532]).
For patients with early-stage esophageal cancer, undergoing chemotherapy and radiotherapy before surgical excision failed to improve the rate of curative resection and, most importantly, failed to boost survival in a phase III clinical trial, according to a report published online June 30 in the Journal of Clinical Oncology.
Unfortunately this treatment strategy also tripled postoperative mortality, making the risk-benefit ratio even more lopsided for this patient population, said Dr. Christophe Mariette of the department of digestive and oncologic surgery, University Hospital Claude Huriez-Regional University Hospital Center, Lille (France), and his associates.
Clinical trials examining neoadjuvant chemoradiotherapy for esophageal cancer have produced conflicting results, with some showing that the approach is effective, in some cases doubling median survival, while others showed no benefit. Most such studies have been limited by small sample sizes, heterogeneity of tumor types, variations in radiation doses and chemotherapy regiments, and differences in preoperative staging techniques and the adequacy of surgical resections. Moreover, the number of study participants with early-stage esophageal cancer has been very small because most patients already have more advanced disease at presentation, the investigators noted.
For their study, Dr. Mariette and his associates confined the cohort to patients younger than 75 years with treatment-naive esophageal adenocarcinoma or squamous-cell carcinoma judged to be stage I or II using thoracoabdominal CT and endoscopic ultrasound; additional preoperative assessments using PET scanning, cervical ultrasound, or radionuclide bone scanning were optional. It required 9 years to enroll 195 patients at 30 French medical centers. These study participants were randomly assigned to receive either neoadjuvant chemotherapy plus radiotherapy before potentially curative surgery (98 subjects) or potentially curative surgery alone (97 subjects).
In the intervention group, radiotherapy involved a total dose of 45 Gy delivered in 25 fractions over the course of 5 weeks. Chemotherapy was administered during the same time period and involved two cycles of fluorouracil and cisplatin infusions. All patients in this group were clinically reevaluated 2-4 weeks after completing this regimen, and surgery was performed soon afterward.
Surgery comprised a transthoracic esophagectomy with extended two-field lymphadenectomy and either high intrathoracic anastomosis (for tumors with an infracarinal proximal margin) or cervical anastomosis (for tumors with a proximal margin above the carina).
Median follow-up was 7.8 years. There were 125 deaths: 62.4% of the intervention group died, as did 66% of the surgery-only group, a nonsignificant difference, the investigators said (J. Clin. Oncol. 2014 June 30 [doi:10.1200/JCO.2013.53.6532]).
Median overall survival was 31.8 months in the intervention group and 41.2 months in the surgery-only group, a nonsignificant difference. Similarly, 3-year overall survival was 47.5% and 5-year overall survival was 41.1% in the intervention group, compared with 53% and 33.8%, respectively, in the surgery-only group, which were also nonsignificant differences.
The rate of curative resection also was not significantly different between the intervention group (93.8%) and the surgery-only group (92.1%), indicating that reducing the tumor with chemotherapy and radiotherapy had no beneficial effect in these early-stage cancers. Previous studies have demonstrated that such downsizing is effective in more advanced esophageal cancers, Dr. Mariette and his associates noted.
Postoperative mortality was more than threefold higher among patients who underwent preoperative chemoradiotherapy (11.1%) than in the surgery-only group (3.4%). The causes of postoperative death included aortic rupture, uncontrollable chylothorax, anastomotic leak, gastric conduit necrosis, mesenteric and lower limb ischemia, and acute RDS in the intervention group, compared with pneumonia and acute RDS in the surgery-only group.
These findings suggest that preoperative chemoradiotherapy "is not the appropriate neoadjuvant therapeutic strategy for stage I or II esophageal cancer," the investigators said.
For patients with early-stage esophageal cancer, undergoing chemotherapy and radiotherapy before surgical excision failed to improve the rate of curative resection and, most importantly, failed to boost survival in a phase III clinical trial, according to a report published online June 30 in the Journal of Clinical Oncology.
Unfortunately this treatment strategy also tripled postoperative mortality, making the risk-benefit ratio even more lopsided for this patient population, said Dr. Christophe Mariette of the department of digestive and oncologic surgery, University Hospital Claude Huriez-Regional University Hospital Center, Lille (France), and his associates.
Clinical trials examining neoadjuvant chemoradiotherapy for esophageal cancer have produced conflicting results, with some showing that the approach is effective, in some cases doubling median survival, while others showed no benefit. Most such studies have been limited by small sample sizes, heterogeneity of tumor types, variations in radiation doses and chemotherapy regiments, and differences in preoperative staging techniques and the adequacy of surgical resections. Moreover, the number of study participants with early-stage esophageal cancer has been very small because most patients already have more advanced disease at presentation, the investigators noted.
For their study, Dr. Mariette and his associates confined the cohort to patients younger than 75 years with treatment-naive esophageal adenocarcinoma or squamous-cell carcinoma judged to be stage I or II using thoracoabdominal CT and endoscopic ultrasound; additional preoperative assessments using PET scanning, cervical ultrasound, or radionuclide bone scanning were optional. It required 9 years to enroll 195 patients at 30 French medical centers. These study participants were randomly assigned to receive either neoadjuvant chemotherapy plus radiotherapy before potentially curative surgery (98 subjects) or potentially curative surgery alone (97 subjects).
In the intervention group, radiotherapy involved a total dose of 45 Gy delivered in 25 fractions over the course of 5 weeks. Chemotherapy was administered during the same time period and involved two cycles of fluorouracil and cisplatin infusions. All patients in this group were clinically reevaluated 2-4 weeks after completing this regimen, and surgery was performed soon afterward.
Surgery comprised a transthoracic esophagectomy with extended two-field lymphadenectomy and either high intrathoracic anastomosis (for tumors with an infracarinal proximal margin) or cervical anastomosis (for tumors with a proximal margin above the carina).
Median follow-up was 7.8 years. There were 125 deaths: 62.4% of the intervention group died, as did 66% of the surgery-only group, a nonsignificant difference, the investigators said (J. Clin. Oncol. 2014 June 30 [doi:10.1200/JCO.2013.53.6532]).
Median overall survival was 31.8 months in the intervention group and 41.2 months in the surgery-only group, a nonsignificant difference. Similarly, 3-year overall survival was 47.5% and 5-year overall survival was 41.1% in the intervention group, compared with 53% and 33.8%, respectively, in the surgery-only group, which were also nonsignificant differences.
The rate of curative resection also was not significantly different between the intervention group (93.8%) and the surgery-only group (92.1%), indicating that reducing the tumor with chemotherapy and radiotherapy had no beneficial effect in these early-stage cancers. Previous studies have demonstrated that such downsizing is effective in more advanced esophageal cancers, Dr. Mariette and his associates noted.
Postoperative mortality was more than threefold higher among patients who underwent preoperative chemoradiotherapy (11.1%) than in the surgery-only group (3.4%). The causes of postoperative death included aortic rupture, uncontrollable chylothorax, anastomotic leak, gastric conduit necrosis, mesenteric and lower limb ischemia, and acute RDS in the intervention group, compared with pneumonia and acute RDS in the surgery-only group.
These findings suggest that preoperative chemoradiotherapy "is not the appropriate neoadjuvant therapeutic strategy for stage I or II esophageal cancer," the investigators said.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Don’t postpone surgery for esophageal cancer to perform chemoradiotherapy.
Major finding: Median overall survival was 31.8 months in the intervention group and 41.2 months in the surgery-only group; 3-year overall survival was 47.5% and 5-year overall survival was 41.1% in the intervention group, compared with 53% and 33.8%, respectively, in the surgery-only group. All these differences are nonsignificant.
Data source: A multicenter randomized phase III clinical trial involving 98 patients treated with neoadjuvant chemoradiotherapy and 97 treated with surgery alone for early-stage esophageal cancer, who were followed for a median of approximately 8 years.
Disclosures: This study was supported by the French National Cancer Institute’s Programme Hospitalier pour la Recherche Clinque and Lille University Hospital; it received no commercial support. Dr. Mariette reported no financial conflicts of interest; one of his associates reported ties to Roche and Merck.
HHS proposes auto-enrollment for 2015 ACA plans
Federal health officials propose to automatically reenroll consumers in Affordable Care Act health plans for 2015 if they purchased coverage through the federally run marketplace earlier this year.
The auto-enrollment feature is part of an effort by the Health & Human Services department to make the ACA’s second open enrollment period run more smoothly than the first.
The auto-enrollment feature puts the federal marketplace in line with the Federal Employee Health Benefits Program (FEHBP) and many employer-sponsored plans. Close to 90% of federal employees who use the FEHBP system don’t switch plans each year, but instead auto-enroll in their current plan with updated premiums and benefits, according to HHS.
Under the proposed rule, released on June 26, the agency will automatically reenroll consumers in the same plan they had in 2014. If that plan is unavailable, the marketplace will select a similar plan.
During the open enrollment period this fall, consumers who are happy with the selected plan won’t have to make new selections. But they have the option to select a different plan.
The proposed rule notes, however, that even if consumers are auto-enrolled, they may need to provide updated income information to continue to receive a tax credit to subsidize their insurance premiums.
State-run marketplaces can follow the federal government’s lead or propose an alternative, according to HHS.
On Twitter @maryellenny
Federal health officials propose to automatically reenroll consumers in Affordable Care Act health plans for 2015 if they purchased coverage through the federally run marketplace earlier this year.
The auto-enrollment feature is part of an effort by the Health & Human Services department to make the ACA’s second open enrollment period run more smoothly than the first.
The auto-enrollment feature puts the federal marketplace in line with the Federal Employee Health Benefits Program (FEHBP) and many employer-sponsored plans. Close to 90% of federal employees who use the FEHBP system don’t switch plans each year, but instead auto-enroll in their current plan with updated premiums and benefits, according to HHS.
Under the proposed rule, released on June 26, the agency will automatically reenroll consumers in the same plan they had in 2014. If that plan is unavailable, the marketplace will select a similar plan.
During the open enrollment period this fall, consumers who are happy with the selected plan won’t have to make new selections. But they have the option to select a different plan.
The proposed rule notes, however, that even if consumers are auto-enrolled, they may need to provide updated income information to continue to receive a tax credit to subsidize their insurance premiums.
State-run marketplaces can follow the federal government’s lead or propose an alternative, according to HHS.
On Twitter @maryellenny
Federal health officials propose to automatically reenroll consumers in Affordable Care Act health plans for 2015 if they purchased coverage through the federally run marketplace earlier this year.
The auto-enrollment feature is part of an effort by the Health & Human Services department to make the ACA’s second open enrollment period run more smoothly than the first.
The auto-enrollment feature puts the federal marketplace in line with the Federal Employee Health Benefits Program (FEHBP) and many employer-sponsored plans. Close to 90% of federal employees who use the FEHBP system don’t switch plans each year, but instead auto-enroll in their current plan with updated premiums and benefits, according to HHS.
Under the proposed rule, released on June 26, the agency will automatically reenroll consumers in the same plan they had in 2014. If that plan is unavailable, the marketplace will select a similar plan.
During the open enrollment period this fall, consumers who are happy with the selected plan won’t have to make new selections. But they have the option to select a different plan.
The proposed rule notes, however, that even if consumers are auto-enrolled, they may need to provide updated income information to continue to receive a tax credit to subsidize their insurance premiums.
State-run marketplaces can follow the federal government’s lead or propose an alternative, according to HHS.
On Twitter @maryellenny
Reoperative bariatric surgery yields low complication rates, substantial weight loss at 1 year
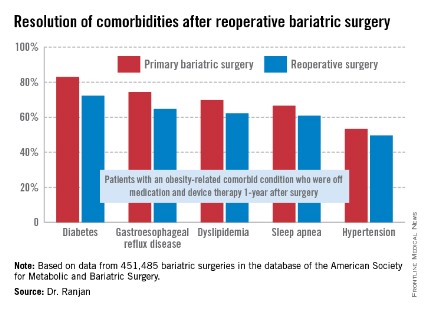
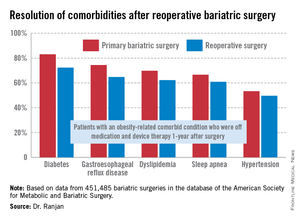
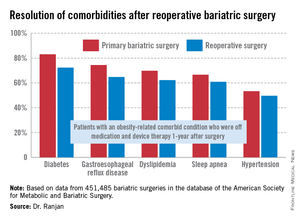
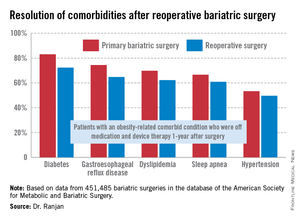
CHICAGO – Reoperative bariatric surgery has impressively low major morbidity and mortality, substantial 1-year weight loss, and a high rate of resolution of the common obesity-linked comorbid conditions, according to an analysis of a large national database.
These data demonstrate that outcomes after contemporary reoperative bariatric surgery are better than believed by insurance carriers, who often deny coverage for these procedures because of a misperception that complication rates are high and benefits uncertain, Dr. Ranjan Sudan said at the annual Digestive Disease Week.
"I think that these data need to get out there to the stakeholders," added Dr. Sudan, a bariatric surgeon and a digestive disorders specialist who is vice chair of education in the department of surgery at Duke University, Durham, N.C.
He presented an analysis of outcomes after reoperative surgery that was carried out by a task force of the American Society for Metabolic and Bariatric Surgery. He and his coinvestigators reviewed all 451,485 bariatric surgery operations entered into the society’s prospective database during a 5-year period ending in spring 2012. The procedures were performed by 1,029 participating surgeons at 709 U.S. hospitals.
The focus of this analysis was on the 6.3% of operations that were reoperations. A total of 70% of the reoperations were corrective operations, essentially redos of the same type of procedure performed initially. The other 30% were conversion procedures, as when a patient who had a gastric band procedure on the first go-round subsequently was converted to a Roux-en-Y gastric bypass or sleeve procedure.
The mean length of stay for primary bariatric operations was 1.78 days, compared with 2.04 days for reoperative corrective procedures and 2.86 days for conversion operations.
The 30-day incidence of serious adverse events, such as leaks, bleeding, or pulmonary embolism, was 1.61% for primary procedures, nearly identical at 1.66% for corrective reoperations, and 3.26% for conversion procedures. The 1-year rate of serious adverse events was 1.87% for primary bariatric operations, 1.9% for corrective procedures, and 3.61% for conversions.
The mortality rate in patients undergoing a primary operation was 0.10% at 30 days and 0.17% at 1 year. Among patients who underwent reoperative bariatric surgery, the 30-day and 1-year mortality rates were 0.14% and 0.26%, respectively.
"Most bariatric surgery patients do not need reoperations. It’s gratifying to see that among those who do, the severe complication rates were low and acceptable and comorbidities often resolved [see chart]," Dr. Sudan declared.
The 1-year rate of excess weight loss following reoperative surgery averaged 36%.
Discussant Dr. Alfons Pomp liked what he saw from the registry.
"Your data show just how good we as bariatric surgeons are to operate on these surgically difficult, very obese, and seriously ill patients, mostly laparoscopically, and get pretty amazing results," commented Dr. Pomp, professor of surgery and chief of GI metabolic and bariatric surgery at Cornell University in New York.
The registry study was funded by Covidien. Dr. Sudan reported having no financial conflicts of interest.
CHICAGO – Reoperative bariatric surgery has impressively low major morbidity and mortality, substantial 1-year weight loss, and a high rate of resolution of the common obesity-linked comorbid conditions, according to an analysis of a large national database.
These data demonstrate that outcomes after contemporary reoperative bariatric surgery are better than believed by insurance carriers, who often deny coverage for these procedures because of a misperception that complication rates are high and benefits uncertain, Dr. Ranjan Sudan said at the annual Digestive Disease Week.
"I think that these data need to get out there to the stakeholders," added Dr. Sudan, a bariatric surgeon and a digestive disorders specialist who is vice chair of education in the department of surgery at Duke University, Durham, N.C.
He presented an analysis of outcomes after reoperative surgery that was carried out by a task force of the American Society for Metabolic and Bariatric Surgery. He and his coinvestigators reviewed all 451,485 bariatric surgery operations entered into the society’s prospective database during a 5-year period ending in spring 2012. The procedures were performed by 1,029 participating surgeons at 709 U.S. hospitals.
The focus of this analysis was on the 6.3% of operations that were reoperations. A total of 70% of the reoperations were corrective operations, essentially redos of the same type of procedure performed initially. The other 30% were conversion procedures, as when a patient who had a gastric band procedure on the first go-round subsequently was converted to a Roux-en-Y gastric bypass or sleeve procedure.
The mean length of stay for primary bariatric operations was 1.78 days, compared with 2.04 days for reoperative corrective procedures and 2.86 days for conversion operations.
The 30-day incidence of serious adverse events, such as leaks, bleeding, or pulmonary embolism, was 1.61% for primary procedures, nearly identical at 1.66% for corrective reoperations, and 3.26% for conversion procedures. The 1-year rate of serious adverse events was 1.87% for primary bariatric operations, 1.9% for corrective procedures, and 3.61% for conversions.
The mortality rate in patients undergoing a primary operation was 0.10% at 30 days and 0.17% at 1 year. Among patients who underwent reoperative bariatric surgery, the 30-day and 1-year mortality rates were 0.14% and 0.26%, respectively.
"Most bariatric surgery patients do not need reoperations. It’s gratifying to see that among those who do, the severe complication rates were low and acceptable and comorbidities often resolved [see chart]," Dr. Sudan declared.
The 1-year rate of excess weight loss following reoperative surgery averaged 36%.
Discussant Dr. Alfons Pomp liked what he saw from the registry.
"Your data show just how good we as bariatric surgeons are to operate on these surgically difficult, very obese, and seriously ill patients, mostly laparoscopically, and get pretty amazing results," commented Dr. Pomp, professor of surgery and chief of GI metabolic and bariatric surgery at Cornell University in New York.
The registry study was funded by Covidien. Dr. Sudan reported having no financial conflicts of interest.
CHICAGO – Reoperative bariatric surgery has impressively low major morbidity and mortality, substantial 1-year weight loss, and a high rate of resolution of the common obesity-linked comorbid conditions, according to an analysis of a large national database.
These data demonstrate that outcomes after contemporary reoperative bariatric surgery are better than believed by insurance carriers, who often deny coverage for these procedures because of a misperception that complication rates are high and benefits uncertain, Dr. Ranjan Sudan said at the annual Digestive Disease Week.
"I think that these data need to get out there to the stakeholders," added Dr. Sudan, a bariatric surgeon and a digestive disorders specialist who is vice chair of education in the department of surgery at Duke University, Durham, N.C.
He presented an analysis of outcomes after reoperative surgery that was carried out by a task force of the American Society for Metabolic and Bariatric Surgery. He and his coinvestigators reviewed all 451,485 bariatric surgery operations entered into the society’s prospective database during a 5-year period ending in spring 2012. The procedures were performed by 1,029 participating surgeons at 709 U.S. hospitals.
The focus of this analysis was on the 6.3% of operations that were reoperations. A total of 70% of the reoperations were corrective operations, essentially redos of the same type of procedure performed initially. The other 30% were conversion procedures, as when a patient who had a gastric band procedure on the first go-round subsequently was converted to a Roux-en-Y gastric bypass or sleeve procedure.
The mean length of stay for primary bariatric operations was 1.78 days, compared with 2.04 days for reoperative corrective procedures and 2.86 days for conversion operations.
The 30-day incidence of serious adverse events, such as leaks, bleeding, or pulmonary embolism, was 1.61% for primary procedures, nearly identical at 1.66% for corrective reoperations, and 3.26% for conversion procedures. The 1-year rate of serious adverse events was 1.87% for primary bariatric operations, 1.9% for corrective procedures, and 3.61% for conversions.
The mortality rate in patients undergoing a primary operation was 0.10% at 30 days and 0.17% at 1 year. Among patients who underwent reoperative bariatric surgery, the 30-day and 1-year mortality rates were 0.14% and 0.26%, respectively.
"Most bariatric surgery patients do not need reoperations. It’s gratifying to see that among those who do, the severe complication rates were low and acceptable and comorbidities often resolved [see chart]," Dr. Sudan declared.
The 1-year rate of excess weight loss following reoperative surgery averaged 36%.
Discussant Dr. Alfons Pomp liked what he saw from the registry.
"Your data show just how good we as bariatric surgeons are to operate on these surgically difficult, very obese, and seriously ill patients, mostly laparoscopically, and get pretty amazing results," commented Dr. Pomp, professor of surgery and chief of GI metabolic and bariatric surgery at Cornell University in New York.
The registry study was funded by Covidien. Dr. Sudan reported having no financial conflicts of interest.
AT DDW 2014
Key clinical point: Reoperative bariatric surgery is considerably safer than previously recognized outside the specialist surgical community. The 1-year excess weight loss is substantial, and common obesity-related comorbidities often resolve.
Major finding: Mortality rates at 30 days and 1-year following reoperative bariatric surgery were just 0.14% and 0. 26%, with an average excess weight loss of 36%at 1 year.
Data source: This was an analysis of more than 450,000 consecutive bariatric surgery operations entered into a prospective national database. Reoperations accounted for 6.3% of the procedures.
Disclosures: The study was funded by Covidien. The presenter reported having no financial conflicts.
Health insurance gap widens between large and small companies
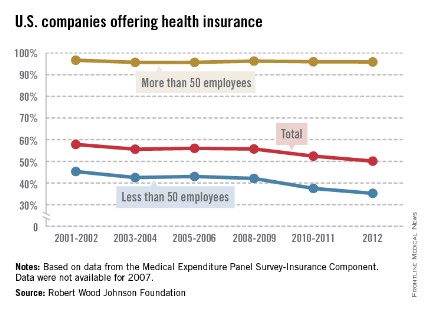
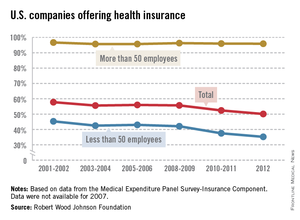
Almost 96% of larger companies still offer health insurance to their employees, but the trend toward smaller companies not providing coverage has accelerated in the last few years, according to the Robert Wood Johnson Foundation.
In 2012, 50.1% of all U.S. firms offered health insurance to their employees, down from 57.8% in 2001-2002. (All estimates represent 2-year averages, except for 2012.) That decline occurred almost entirely among smaller companies – those with fewer than 50 employees – as the percentage offering coverage fell from 45.3% in 2001-2002 to 35.2% in 2012, with two-thirds of the decline occurring after 2008-2009, the RWJF analysis showed.
Among larger companies, the decline was much smaller: from 96.7% in 2001-2002 to 95.9% in 2012.
The data for the analysis came from the Agency for Healthcare Research and Quality’s Medical Expenditure Panel Survey-Insurance Component.
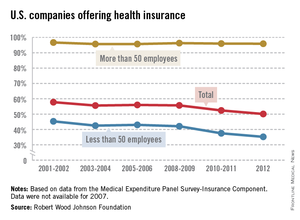
Almost 96% of larger companies still offer health insurance to their employees, but the trend toward smaller companies not providing coverage has accelerated in the last few years, according to the Robert Wood Johnson Foundation.
In 2012, 50.1% of all U.S. firms offered health insurance to their employees, down from 57.8% in 2001-2002. (All estimates represent 2-year averages, except for 2012.) That decline occurred almost entirely among smaller companies – those with fewer than 50 employees – as the percentage offering coverage fell from 45.3% in 2001-2002 to 35.2% in 2012, with two-thirds of the decline occurring after 2008-2009, the RWJF analysis showed.
Among larger companies, the decline was much smaller: from 96.7% in 2001-2002 to 95.9% in 2012.
The data for the analysis came from the Agency for Healthcare Research and Quality’s Medical Expenditure Panel Survey-Insurance Component.
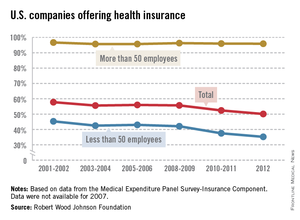
Almost 96% of larger companies still offer health insurance to their employees, but the trend toward smaller companies not providing coverage has accelerated in the last few years, according to the Robert Wood Johnson Foundation.
In 2012, 50.1% of all U.S. firms offered health insurance to their employees, down from 57.8% in 2001-2002. (All estimates represent 2-year averages, except for 2012.) That decline occurred almost entirely among smaller companies – those with fewer than 50 employees – as the percentage offering coverage fell from 45.3% in 2001-2002 to 35.2% in 2012, with two-thirds of the decline occurring after 2008-2009, the RWJF analysis showed.
Among larger companies, the decline was much smaller: from 96.7% in 2001-2002 to 95.9% in 2012.
The data for the analysis came from the Agency for Healthcare Research and Quality’s Medical Expenditure Panel Survey-Insurance Component.
Bariatric surgery/Preventive medicine
Until recently, bariatric surgery was considered a cosmetic operation with little physiologic importance. A series of preliminary randomized clinical trials, however, have suggested that bariatric surgery may have importance in mitigating the adverse pathophysiology associated with obesity, including type 2 diabetes and some cardiovascular risk factors.
The finding of a surgical method of modifying this disease, which has occupied research for the last century, is somewhat unexpected after the many false starts associated with medical interventions. The two most popular surgical procedures, the gastric bypass and the sleeve gastrectomy performed using laparoscopic techniques, are currently being performed in obese patients with BMIs of greater than 35 with very low morbidly and rare mortality events. Several nonrandomized and prospective trials have examined the effect of bariatric surgery and reported beneficial effects on diabetes regression and significant reduction in major cardiovascular disease ( JAMA 2012;307:56-65).
The recent report of the 3-year follow-up of the STAMPEDE (Surgical Therapy And Medications Potentially Eradicate Diabetes Efficiently) trial ( N. Engl. J. Med. 2014;370:2002-13) provides additional physiologic information on the benefits of bariatric surgery in 150 obese diabetic patients aged 20-60 years with BMIs of 27-43, compared with intensive medical therapy. Patients were randomized to three arms: intensive medical therapy, gastric bypass, or sleeve gastrectomy. Most of the patients were white women with a history of diabetes for 8.3 years; the mean hemoglobin A1c was 9.3%. At baseline, 43% of the patients required insulin therapy. The primary endpoint was the achievement of HbA1c of 6% or less, which was achieved in 5% of the medically treated patients, compared with 38% in the gastric bypass group and 24% in the sleeve gastrectomy group. Decrease in BMI was the only measure that predicted the achievement of the HbA1c endpoint. Body weight decreased by 4.5% in the intensive medical group, 24.5% in the gastric bypass group, and 21.1% in the sleeve gastrectomy group. Significant decreases in low-density lipoprotein cholesterol and increases in high-density lipoprotein cholesterol were achieved in both surgical intervention groups, compared with the intensive medical care group. In addition, medical control of diabetes was improved and 69% and 43% of the gastrectomy and sleeve bypass group, respectively, were no longer requiring insulin therapy. There was, however, no significant difference in the change in blood pressure in the three groups. There were no life-threatening complications or deaths in the groups, but there were a number of complications associated with the procedure.
The metabolic changes associated with bariatric surgery reported in STAMPEDE open the door for future randomized studies examining long-term morbidity and mortality benefits that may be attributed to this therapy. Bariatric surgery is being performed widely in the United States with very low mortality and morbidity. Previous short-term studies have reported the benefit of bariatric surgery, compared with intensive medical therapy. The longer duration of follow-up in STAMPEDE emphasizes the need for larger randomized trials of this method of therapy. The study of the surgical patients may also provide new insight into the relationship of body fat to the expression of type 2 diabetes.
The prevention of medical disease using surgical techniques in clinical medicine has not been a particularly fertile road of investigation. Intervention in the treatment of coronary artery disease with bypass surgery although associated with symptomatic benefit and with some exceptions, has not been overwhelmingly successful in affecting the long-term mortality of that disease. Bariatric surgery may be the first surgical intervention that can arrest or even reverse type 2 diabetes and its many sequelae.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
Until recently, bariatric surgery was considered a cosmetic operation with little physiologic importance. A series of preliminary randomized clinical trials, however, have suggested that bariatric surgery may have importance in mitigating the adverse pathophysiology associated with obesity, including type 2 diabetes and some cardiovascular risk factors.
The finding of a surgical method of modifying this disease, which has occupied research for the last century, is somewhat unexpected after the many false starts associated with medical interventions. The two most popular surgical procedures, the gastric bypass and the sleeve gastrectomy performed using laparoscopic techniques, are currently being performed in obese patients with BMIs of greater than 35 with very low morbidly and rare mortality events. Several nonrandomized and prospective trials have examined the effect of bariatric surgery and reported beneficial effects on diabetes regression and significant reduction in major cardiovascular disease ( JAMA 2012;307:56-65).
The recent report of the 3-year follow-up of the STAMPEDE (Surgical Therapy And Medications Potentially Eradicate Diabetes Efficiently) trial ( N. Engl. J. Med. 2014;370:2002-13) provides additional physiologic information on the benefits of bariatric surgery in 150 obese diabetic patients aged 20-60 years with BMIs of 27-43, compared with intensive medical therapy. Patients were randomized to three arms: intensive medical therapy, gastric bypass, or sleeve gastrectomy. Most of the patients were white women with a history of diabetes for 8.3 years; the mean hemoglobin A1c was 9.3%. At baseline, 43% of the patients required insulin therapy. The primary endpoint was the achievement of HbA1c of 6% or less, which was achieved in 5% of the medically treated patients, compared with 38% in the gastric bypass group and 24% in the sleeve gastrectomy group. Decrease in BMI was the only measure that predicted the achievement of the HbA1c endpoint. Body weight decreased by 4.5% in the intensive medical group, 24.5% in the gastric bypass group, and 21.1% in the sleeve gastrectomy group. Significant decreases in low-density lipoprotein cholesterol and increases in high-density lipoprotein cholesterol were achieved in both surgical intervention groups, compared with the intensive medical care group. In addition, medical control of diabetes was improved and 69% and 43% of the gastrectomy and sleeve bypass group, respectively, were no longer requiring insulin therapy. There was, however, no significant difference in the change in blood pressure in the three groups. There were no life-threatening complications or deaths in the groups, but there were a number of complications associated with the procedure.
The metabolic changes associated with bariatric surgery reported in STAMPEDE open the door for future randomized studies examining long-term morbidity and mortality benefits that may be attributed to this therapy. Bariatric surgery is being performed widely in the United States with very low mortality and morbidity. Previous short-term studies have reported the benefit of bariatric surgery, compared with intensive medical therapy. The longer duration of follow-up in STAMPEDE emphasizes the need for larger randomized trials of this method of therapy. The study of the surgical patients may also provide new insight into the relationship of body fat to the expression of type 2 diabetes.
The prevention of medical disease using surgical techniques in clinical medicine has not been a particularly fertile road of investigation. Intervention in the treatment of coronary artery disease with bypass surgery although associated with symptomatic benefit and with some exceptions, has not been overwhelmingly successful in affecting the long-term mortality of that disease. Bariatric surgery may be the first surgical intervention that can arrest or even reverse type 2 diabetes and its many sequelae.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
Until recently, bariatric surgery was considered a cosmetic operation with little physiologic importance. A series of preliminary randomized clinical trials, however, have suggested that bariatric surgery may have importance in mitigating the adverse pathophysiology associated with obesity, including type 2 diabetes and some cardiovascular risk factors.
The finding of a surgical method of modifying this disease, which has occupied research for the last century, is somewhat unexpected after the many false starts associated with medical interventions. The two most popular surgical procedures, the gastric bypass and the sleeve gastrectomy performed using laparoscopic techniques, are currently being performed in obese patients with BMIs of greater than 35 with very low morbidly and rare mortality events. Several nonrandomized and prospective trials have examined the effect of bariatric surgery and reported beneficial effects on diabetes regression and significant reduction in major cardiovascular disease ( JAMA 2012;307:56-65).
The recent report of the 3-year follow-up of the STAMPEDE (Surgical Therapy And Medications Potentially Eradicate Diabetes Efficiently) trial ( N. Engl. J. Med. 2014;370:2002-13) provides additional physiologic information on the benefits of bariatric surgery in 150 obese diabetic patients aged 20-60 years with BMIs of 27-43, compared with intensive medical therapy. Patients were randomized to three arms: intensive medical therapy, gastric bypass, or sleeve gastrectomy. Most of the patients were white women with a history of diabetes for 8.3 years; the mean hemoglobin A1c was 9.3%. At baseline, 43% of the patients required insulin therapy. The primary endpoint was the achievement of HbA1c of 6% or less, which was achieved in 5% of the medically treated patients, compared with 38% in the gastric bypass group and 24% in the sleeve gastrectomy group. Decrease in BMI was the only measure that predicted the achievement of the HbA1c endpoint. Body weight decreased by 4.5% in the intensive medical group, 24.5% in the gastric bypass group, and 21.1% in the sleeve gastrectomy group. Significant decreases in low-density lipoprotein cholesterol and increases in high-density lipoprotein cholesterol were achieved in both surgical intervention groups, compared with the intensive medical care group. In addition, medical control of diabetes was improved and 69% and 43% of the gastrectomy and sleeve bypass group, respectively, were no longer requiring insulin therapy. There was, however, no significant difference in the change in blood pressure in the three groups. There were no life-threatening complications or deaths in the groups, but there were a number of complications associated with the procedure.
The metabolic changes associated with bariatric surgery reported in STAMPEDE open the door for future randomized studies examining long-term morbidity and mortality benefits that may be attributed to this therapy. Bariatric surgery is being performed widely in the United States with very low mortality and morbidity. Previous short-term studies have reported the benefit of bariatric surgery, compared with intensive medical therapy. The longer duration of follow-up in STAMPEDE emphasizes the need for larger randomized trials of this method of therapy. The study of the surgical patients may also provide new insight into the relationship of body fat to the expression of type 2 diabetes.
The prevention of medical disease using surgical techniques in clinical medicine has not been a particularly fertile road of investigation. Intervention in the treatment of coronary artery disease with bypass surgery although associated with symptomatic benefit and with some exceptions, has not been overwhelmingly successful in affecting the long-term mortality of that disease. Bariatric surgery may be the first surgical intervention that can arrest or even reverse type 2 diabetes and its many sequelae.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
SSTI guidelines stress diagnostic skill, careful treatment
New practice guidelines on skin and soft tissue infections from the Infectious Diseases Society of America stress careful clinical attention to the type of infection, the epidemiological setting in which the infection occurred, the health status of the patient, and the selection and dosage of the most appropriate treatment agents.
The guidelines, published online June 18 in Clinical Infectious Diseases (doi:10.1093/cid/ciu296), update those issued by IDSA in 2005 and cover everything from preventing infections caused by animal bites in healthy hosts to life-threatening infections in immunocompromised patients. They also emphasize accurate identification of pathogens, stressing that clinical presentations can be very similar.
"This is not one of those guidelines that boils complex issues down to a choice between a couple of different drugs or combinations of drugs," said Dr. Dennis Stevens of the Department of Veterans Affairs in Boise, Idaho, the guidelines’ lead author. "Skin and soft tissue infections [SSTIs] have multiple causes and different presentations, depending upon the immune status of the host. Here it’s much more complicated and really requires an astute physician to consider a number of things."
The guidelines, drafted by a 10-member panel, offer a novel algorithm for management of nonpurulent and purulent infections that aims to define a pathway for mild, moderate, and severe infections in each category. For example, no antibiotic is recommended for a purulent infection – only incision and drainage – if the patient has no signs of systemic involvement.
For moderate cases of purulent infection with some systemic involvement, incision and drainage should be followed by culture and sensitivity testing, the guidelines say, listing two antibiotics, trimethoprim-sulfamethoxazole and doxycycline, as appropriate for empiric treatment, while trimethoprim-sulfamethoxazole is recommended if the pathogen is found to be methicillin-resistant Staphylococcus aureus (MRSA) and dicloxacillin or cephalexin if it is methicillin-susceptible S. aureus (MSSA).
The purpose of the algorithm, expressed in the guidelines in chart form, "is to make the physician think," Dr. Stevens said in an interview. "There is a huge move to try and monitor antibiotic stewardship to prevent resistance, and we’re just trying to get the clinician to think of tier 1, tier 2, and tier 3 approaches, depending not only on the bug, but on how sick the patient is. Instead of a knee-jerk approach treating everybody with highly expensive IV antibiotics, [the algorithm] provides a clear pathway to treat appropriately."
In people with an abscess who have failed antibiotic treatment, are immunocompromised, or have fever and elevated white blood cell counts or other evidence of severe infection, "we’re not going to gamble," Dr. Stevens said, adding that the guidelines recommend prompt treatment using "an antibiotic that gets all of these organisms, including resistant ones." Newly approved agents dalbavancin and tedizolid are effective in treating SSTIs caused by MRSA, the guidelines note.
The guidelines are intended for use by clinicians in emergency departments, family practice, internal medicine, general surgery, orthopedics, gynecology, dermatology, infectious disease, and oncology.
Another algorithm charted in the guidelines covers wound infections following surgeries, which can involve multiple pathogens. The algorithm provides simple clinical clues as to which require antibiotics, a simple opening of the suture line, "or a full-court press for the kind of devastating infections that occur within the first 48 hours," Dr. Stevens said. Additional recommendations address infections that can occur in individuals receiving treatment for cancer or receiving immunosuppressant medications, or those who have had an organ transplant or who have HIV/AIDS.
Immunocompromised patients, Dr. Stevens said, are among the most challenging to treat because they may have a history of extensive antibiotic exposure, are likely to have infections with resistant bacteria, and often see involvement with fungal and parasitic agents that might be considered innocuous in normal individuals. "This is the first time physicians will have some decent guidelines about how to approach the problem of skin and soft tissue infections in these kinds of patients," he noted.
The guidelines’ development was funded by the IDSA. Dr. Stevens reported no conflicts of interest. Panel member Alan L. Bisno disclosed receiving honoraria from UpToDate, while five other members – Dr. Henry F. Chambers, Dr. E. Patchen Dellinger, Dr. Ellie J. C. Goldstein, Dr. Sherwood L. Gorbach, and Dr. Sheldon L. Kaplan – disclosed financial relationships with pharmaceutical manufacturers.
Skin and soft tissue infections are one of the most common causes for patient evaluation in emergency departments and are common reasons for consultations by surgeons. SSTIs occur across a broad continuum of severity and often require only antimicrobial therapy (such as cellulitis), but they may be fulminate and life-threatening necrotizing infections that require aggressive surgical intervention. The guidelines provided by a distinguished group of clinicians from the Infectious Diseases Society of America provide an excellent organizational framework to understand this heterogenous collection of infections and provide a meaningful structure to direct management.
Several points in these guidelines deserve emphasis. First, considerable discussion in the guidelines has focused on the immunocompromised patient with SSTIs, and appropriately so. A broader consideration might have been to also include those patients with health care-associated exposure in addition to clinical immunosuppression. About 40 million hospitalizations occur annually in the United State, which makes over 3 million patients within 30 days of discharge. A larger number of patients have had recent antibiotic exposure. About 1.5 million patients are in chronic care facilities and nearly 500,000 are receiving chronic hemodialysis. Accordingly, immunocompromised and health care-associated patient exposures require that assumptions about the microbiology of SSTIs have "sensitivity" to the resistant pathogens (such as MRSA) not traditionally typical of community-acquired infections.
Second, the guidelines refer to the use of Gram stains for directing antimicrobial therapy. Although the Gram stain does not have the high-technology flare of contemporary health care, it remains a useful tool in differentiating pathogens, especially in necrotizing SSTIs.
Of the major microbiological presentations of necrotizing SSTIs, Streptococcus pyogenes is a gram-positive cocci in chains, Staphylococcus aureus is a gram-positive cocci in clusters, Clostridium perfringens is a gram-positive rod, and polymicrobial infections will have an assortment of different morphologic and gram-staining characteristics in identified bacteria. Aeromonas hydrophilia and Vibrio vulnificus will appear as gram-negative rods in those necrotizing SSTIs associated with fresh or salt-water recreational exposure. The Gram stain provides immediate direction for therapy when culture results will often be too late for a meaningful impact on patient care. Unfortunately, many hospitals have abandoned the use of Gram stains for clinical specimens.
Finally, prompt diagnosis of necrotizing SSTIs is essential. A cause of potentially preventable morbidity and deaths is a delay in the recognition of necrotizing SSTIs and the need for urgent surgical debridement. Necrotizing SSTIs are common issues in medicolegal actions because of the issue of failure to make the timely diagnosis. The hallmark of necrotizing SSTIs is pain out of proportion to the inciting injury. Trivial cutaneous injuries that are associated with an advancing perimeter of palpable tenderness and induration are necrotizing SSTIs until proven otherwise. Importantly, S. pyogenes in particular is associated with "metastatic" infection. Patients with soft-tissue contusions, joint effusions, and even fractures may have blood-borne streptococcal contamination of the injury site and yield a necrotizing infection without any cutaneous source of microbial contamination.
Because monitoring the progression of SSTIs is so important in differentiating necrotizing infections, I would only take to task the recommendation for the use of corticosteroids in treatment of cellulitic infections. Pharmacologic immunosuppression of the patient with an active SSTI in the interest of providing symptomatic relief compromises the clinical evaluation of disease progression.
In summary, the guidelines and the two algorithms for managing community-acquired and surgical incision infections are very useful for providing surgical clinicians direction in patient management. The increased incidence of S. aureus-associated necrotizing SSTIs and the emergence of community-associated MRSA over the last 20 years indicate that this is a dynamic area with changing characteristics. The changing pattern of pathogens and antimicrobial choices require a more frequent updating of these important guidelines for patient management.
Dr. Donald E. Fry is an ACS Fellow, executive vice-president for clinical outcomes management of MPA Inc. of Chicago, adjunct professor of surgery at the Northwestern University in Chicago, and professor emeritus of surgery at the University of New Mexico. He is a fellow of the Infectious Diseases Society of America, a past president of the Surgical Infection Society, and associate editor of the journal Surgical Infections.
Skin and soft tissue infections are one of the most common causes for patient evaluation in emergency departments and are common reasons for consultations by surgeons. SSTIs occur across a broad continuum of severity and often require only antimicrobial therapy (such as cellulitis), but they may be fulminate and life-threatening necrotizing infections that require aggressive surgical intervention. The guidelines provided by a distinguished group of clinicians from the Infectious Diseases Society of America provide an excellent organizational framework to understand this heterogenous collection of infections and provide a meaningful structure to direct management.
Several points in these guidelines deserve emphasis. First, considerable discussion in the guidelines has focused on the immunocompromised patient with SSTIs, and appropriately so. A broader consideration might have been to also include those patients with health care-associated exposure in addition to clinical immunosuppression. About 40 million hospitalizations occur annually in the United State, which makes over 3 million patients within 30 days of discharge. A larger number of patients have had recent antibiotic exposure. About 1.5 million patients are in chronic care facilities and nearly 500,000 are receiving chronic hemodialysis. Accordingly, immunocompromised and health care-associated patient exposures require that assumptions about the microbiology of SSTIs have "sensitivity" to the resistant pathogens (such as MRSA) not traditionally typical of community-acquired infections.
Second, the guidelines refer to the use of Gram stains for directing antimicrobial therapy. Although the Gram stain does not have the high-technology flare of contemporary health care, it remains a useful tool in differentiating pathogens, especially in necrotizing SSTIs.
Of the major microbiological presentations of necrotizing SSTIs, Streptococcus pyogenes is a gram-positive cocci in chains, Staphylococcus aureus is a gram-positive cocci in clusters, Clostridium perfringens is a gram-positive rod, and polymicrobial infections will have an assortment of different morphologic and gram-staining characteristics in identified bacteria. Aeromonas hydrophilia and Vibrio vulnificus will appear as gram-negative rods in those necrotizing SSTIs associated with fresh or salt-water recreational exposure. The Gram stain provides immediate direction for therapy when culture results will often be too late for a meaningful impact on patient care. Unfortunately, many hospitals have abandoned the use of Gram stains for clinical specimens.
Finally, prompt diagnosis of necrotizing SSTIs is essential. A cause of potentially preventable morbidity and deaths is a delay in the recognition of necrotizing SSTIs and the need for urgent surgical debridement. Necrotizing SSTIs are common issues in medicolegal actions because of the issue of failure to make the timely diagnosis. The hallmark of necrotizing SSTIs is pain out of proportion to the inciting injury. Trivial cutaneous injuries that are associated with an advancing perimeter of palpable tenderness and induration are necrotizing SSTIs until proven otherwise. Importantly, S. pyogenes in particular is associated with "metastatic" infection. Patients with soft-tissue contusions, joint effusions, and even fractures may have blood-borne streptococcal contamination of the injury site and yield a necrotizing infection without any cutaneous source of microbial contamination.
Because monitoring the progression of SSTIs is so important in differentiating necrotizing infections, I would only take to task the recommendation for the use of corticosteroids in treatment of cellulitic infections. Pharmacologic immunosuppression of the patient with an active SSTI in the interest of providing symptomatic relief compromises the clinical evaluation of disease progression.
In summary, the guidelines and the two algorithms for managing community-acquired and surgical incision infections are very useful for providing surgical clinicians direction in patient management. The increased incidence of S. aureus-associated necrotizing SSTIs and the emergence of community-associated MRSA over the last 20 years indicate that this is a dynamic area with changing characteristics. The changing pattern of pathogens and antimicrobial choices require a more frequent updating of these important guidelines for patient management.
Dr. Donald E. Fry is an ACS Fellow, executive vice-president for clinical outcomes management of MPA Inc. of Chicago, adjunct professor of surgery at the Northwestern University in Chicago, and professor emeritus of surgery at the University of New Mexico. He is a fellow of the Infectious Diseases Society of America, a past president of the Surgical Infection Society, and associate editor of the journal Surgical Infections.
Skin and soft tissue infections are one of the most common causes for patient evaluation in emergency departments and are common reasons for consultations by surgeons. SSTIs occur across a broad continuum of severity and often require only antimicrobial therapy (such as cellulitis), but they may be fulminate and life-threatening necrotizing infections that require aggressive surgical intervention. The guidelines provided by a distinguished group of clinicians from the Infectious Diseases Society of America provide an excellent organizational framework to understand this heterogenous collection of infections and provide a meaningful structure to direct management.
Several points in these guidelines deserve emphasis. First, considerable discussion in the guidelines has focused on the immunocompromised patient with SSTIs, and appropriately so. A broader consideration might have been to also include those patients with health care-associated exposure in addition to clinical immunosuppression. About 40 million hospitalizations occur annually in the United State, which makes over 3 million patients within 30 days of discharge. A larger number of patients have had recent antibiotic exposure. About 1.5 million patients are in chronic care facilities and nearly 500,000 are receiving chronic hemodialysis. Accordingly, immunocompromised and health care-associated patient exposures require that assumptions about the microbiology of SSTIs have "sensitivity" to the resistant pathogens (such as MRSA) not traditionally typical of community-acquired infections.
Second, the guidelines refer to the use of Gram stains for directing antimicrobial therapy. Although the Gram stain does not have the high-technology flare of contemporary health care, it remains a useful tool in differentiating pathogens, especially in necrotizing SSTIs.
Of the major microbiological presentations of necrotizing SSTIs, Streptococcus pyogenes is a gram-positive cocci in chains, Staphylococcus aureus is a gram-positive cocci in clusters, Clostridium perfringens is a gram-positive rod, and polymicrobial infections will have an assortment of different morphologic and gram-staining characteristics in identified bacteria. Aeromonas hydrophilia and Vibrio vulnificus will appear as gram-negative rods in those necrotizing SSTIs associated with fresh or salt-water recreational exposure. The Gram stain provides immediate direction for therapy when culture results will often be too late for a meaningful impact on patient care. Unfortunately, many hospitals have abandoned the use of Gram stains for clinical specimens.
Finally, prompt diagnosis of necrotizing SSTIs is essential. A cause of potentially preventable morbidity and deaths is a delay in the recognition of necrotizing SSTIs and the need for urgent surgical debridement. Necrotizing SSTIs are common issues in medicolegal actions because of the issue of failure to make the timely diagnosis. The hallmark of necrotizing SSTIs is pain out of proportion to the inciting injury. Trivial cutaneous injuries that are associated with an advancing perimeter of palpable tenderness and induration are necrotizing SSTIs until proven otherwise. Importantly, S. pyogenes in particular is associated with "metastatic" infection. Patients with soft-tissue contusions, joint effusions, and even fractures may have blood-borne streptococcal contamination of the injury site and yield a necrotizing infection without any cutaneous source of microbial contamination.
Because monitoring the progression of SSTIs is so important in differentiating necrotizing infections, I would only take to task the recommendation for the use of corticosteroids in treatment of cellulitic infections. Pharmacologic immunosuppression of the patient with an active SSTI in the interest of providing symptomatic relief compromises the clinical evaluation of disease progression.
In summary, the guidelines and the two algorithms for managing community-acquired and surgical incision infections are very useful for providing surgical clinicians direction in patient management. The increased incidence of S. aureus-associated necrotizing SSTIs and the emergence of community-associated MRSA over the last 20 years indicate that this is a dynamic area with changing characteristics. The changing pattern of pathogens and antimicrobial choices require a more frequent updating of these important guidelines for patient management.
Dr. Donald E. Fry is an ACS Fellow, executive vice-president for clinical outcomes management of MPA Inc. of Chicago, adjunct professor of surgery at the Northwestern University in Chicago, and professor emeritus of surgery at the University of New Mexico. He is a fellow of the Infectious Diseases Society of America, a past president of the Surgical Infection Society, and associate editor of the journal Surgical Infections.
New practice guidelines on skin and soft tissue infections from the Infectious Diseases Society of America stress careful clinical attention to the type of infection, the epidemiological setting in which the infection occurred, the health status of the patient, and the selection and dosage of the most appropriate treatment agents.
The guidelines, published online June 18 in Clinical Infectious Diseases (doi:10.1093/cid/ciu296), update those issued by IDSA in 2005 and cover everything from preventing infections caused by animal bites in healthy hosts to life-threatening infections in immunocompromised patients. They also emphasize accurate identification of pathogens, stressing that clinical presentations can be very similar.
"This is not one of those guidelines that boils complex issues down to a choice between a couple of different drugs or combinations of drugs," said Dr. Dennis Stevens of the Department of Veterans Affairs in Boise, Idaho, the guidelines’ lead author. "Skin and soft tissue infections [SSTIs] have multiple causes and different presentations, depending upon the immune status of the host. Here it’s much more complicated and really requires an astute physician to consider a number of things."
The guidelines, drafted by a 10-member panel, offer a novel algorithm for management of nonpurulent and purulent infections that aims to define a pathway for mild, moderate, and severe infections in each category. For example, no antibiotic is recommended for a purulent infection – only incision and drainage – if the patient has no signs of systemic involvement.
For moderate cases of purulent infection with some systemic involvement, incision and drainage should be followed by culture and sensitivity testing, the guidelines say, listing two antibiotics, trimethoprim-sulfamethoxazole and doxycycline, as appropriate for empiric treatment, while trimethoprim-sulfamethoxazole is recommended if the pathogen is found to be methicillin-resistant Staphylococcus aureus (MRSA) and dicloxacillin or cephalexin if it is methicillin-susceptible S. aureus (MSSA).
The purpose of the algorithm, expressed in the guidelines in chart form, "is to make the physician think," Dr. Stevens said in an interview. "There is a huge move to try and monitor antibiotic stewardship to prevent resistance, and we’re just trying to get the clinician to think of tier 1, tier 2, and tier 3 approaches, depending not only on the bug, but on how sick the patient is. Instead of a knee-jerk approach treating everybody with highly expensive IV antibiotics, [the algorithm] provides a clear pathway to treat appropriately."
In people with an abscess who have failed antibiotic treatment, are immunocompromised, or have fever and elevated white blood cell counts or other evidence of severe infection, "we’re not going to gamble," Dr. Stevens said, adding that the guidelines recommend prompt treatment using "an antibiotic that gets all of these organisms, including resistant ones." Newly approved agents dalbavancin and tedizolid are effective in treating SSTIs caused by MRSA, the guidelines note.
The guidelines are intended for use by clinicians in emergency departments, family practice, internal medicine, general surgery, orthopedics, gynecology, dermatology, infectious disease, and oncology.
Another algorithm charted in the guidelines covers wound infections following surgeries, which can involve multiple pathogens. The algorithm provides simple clinical clues as to which require antibiotics, a simple opening of the suture line, "or a full-court press for the kind of devastating infections that occur within the first 48 hours," Dr. Stevens said. Additional recommendations address infections that can occur in individuals receiving treatment for cancer or receiving immunosuppressant medications, or those who have had an organ transplant or who have HIV/AIDS.
Immunocompromised patients, Dr. Stevens said, are among the most challenging to treat because they may have a history of extensive antibiotic exposure, are likely to have infections with resistant bacteria, and often see involvement with fungal and parasitic agents that might be considered innocuous in normal individuals. "This is the first time physicians will have some decent guidelines about how to approach the problem of skin and soft tissue infections in these kinds of patients," he noted.
The guidelines’ development was funded by the IDSA. Dr. Stevens reported no conflicts of interest. Panel member Alan L. Bisno disclosed receiving honoraria from UpToDate, while five other members – Dr. Henry F. Chambers, Dr. E. Patchen Dellinger, Dr. Ellie J. C. Goldstein, Dr. Sherwood L. Gorbach, and Dr. Sheldon L. Kaplan – disclosed financial relationships with pharmaceutical manufacturers.
New practice guidelines on skin and soft tissue infections from the Infectious Diseases Society of America stress careful clinical attention to the type of infection, the epidemiological setting in which the infection occurred, the health status of the patient, and the selection and dosage of the most appropriate treatment agents.
The guidelines, published online June 18 in Clinical Infectious Diseases (doi:10.1093/cid/ciu296), update those issued by IDSA in 2005 and cover everything from preventing infections caused by animal bites in healthy hosts to life-threatening infections in immunocompromised patients. They also emphasize accurate identification of pathogens, stressing that clinical presentations can be very similar.
"This is not one of those guidelines that boils complex issues down to a choice between a couple of different drugs or combinations of drugs," said Dr. Dennis Stevens of the Department of Veterans Affairs in Boise, Idaho, the guidelines’ lead author. "Skin and soft tissue infections [SSTIs] have multiple causes and different presentations, depending upon the immune status of the host. Here it’s much more complicated and really requires an astute physician to consider a number of things."
The guidelines, drafted by a 10-member panel, offer a novel algorithm for management of nonpurulent and purulent infections that aims to define a pathway for mild, moderate, and severe infections in each category. For example, no antibiotic is recommended for a purulent infection – only incision and drainage – if the patient has no signs of systemic involvement.
For moderate cases of purulent infection with some systemic involvement, incision and drainage should be followed by culture and sensitivity testing, the guidelines say, listing two antibiotics, trimethoprim-sulfamethoxazole and doxycycline, as appropriate for empiric treatment, while trimethoprim-sulfamethoxazole is recommended if the pathogen is found to be methicillin-resistant Staphylococcus aureus (MRSA) and dicloxacillin or cephalexin if it is methicillin-susceptible S. aureus (MSSA).
The purpose of the algorithm, expressed in the guidelines in chart form, "is to make the physician think," Dr. Stevens said in an interview. "There is a huge move to try and monitor antibiotic stewardship to prevent resistance, and we’re just trying to get the clinician to think of tier 1, tier 2, and tier 3 approaches, depending not only on the bug, but on how sick the patient is. Instead of a knee-jerk approach treating everybody with highly expensive IV antibiotics, [the algorithm] provides a clear pathway to treat appropriately."
In people with an abscess who have failed antibiotic treatment, are immunocompromised, or have fever and elevated white blood cell counts or other evidence of severe infection, "we’re not going to gamble," Dr. Stevens said, adding that the guidelines recommend prompt treatment using "an antibiotic that gets all of these organisms, including resistant ones." Newly approved agents dalbavancin and tedizolid are effective in treating SSTIs caused by MRSA, the guidelines note.
The guidelines are intended for use by clinicians in emergency departments, family practice, internal medicine, general surgery, orthopedics, gynecology, dermatology, infectious disease, and oncology.
Another algorithm charted in the guidelines covers wound infections following surgeries, which can involve multiple pathogens. The algorithm provides simple clinical clues as to which require antibiotics, a simple opening of the suture line, "or a full-court press for the kind of devastating infections that occur within the first 48 hours," Dr. Stevens said. Additional recommendations address infections that can occur in individuals receiving treatment for cancer or receiving immunosuppressant medications, or those who have had an organ transplant or who have HIV/AIDS.
Immunocompromised patients, Dr. Stevens said, are among the most challenging to treat because they may have a history of extensive antibiotic exposure, are likely to have infections with resistant bacteria, and often see involvement with fungal and parasitic agents that might be considered innocuous in normal individuals. "This is the first time physicians will have some decent guidelines about how to approach the problem of skin and soft tissue infections in these kinds of patients," he noted.
The guidelines’ development was funded by the IDSA. Dr. Stevens reported no conflicts of interest. Panel member Alan L. Bisno disclosed receiving honoraria from UpToDate, while five other members – Dr. Henry F. Chambers, Dr. E. Patchen Dellinger, Dr. Ellie J. C. Goldstein, Dr. Sherwood L. Gorbach, and Dr. Sheldon L. Kaplan – disclosed financial relationships with pharmaceutical manufacturers.
FROM CLINICAL INFECTIOUS DISEASES
Bariatric surgery and alcohol use disorder
As obesity continues to ravage the health of the United States, bariatric surgery offers an effective strategy for individual patients suffering from medical complications.
When performed in adults with a body mass index of at least 30 kg/m2, bariatric surgery is associated with a mean weight loss of 20%-35% of baseline weight at 2-3 years. Bariatric surgery is associated with greater reductions in obesity comorbidities, compared with lifestyle intervention and supervised weight loss. Contemporary bariatric surgeries include Roux-en-Y gastric bypass, laparoscopic adjustable gastric banding, biliopancreatic diversion with duodenal switch, sleeve gastrectomy, and mini–gastric bypass.
Bariatric surgical procedures affect weight loss through two mechanisms: malabsorption and restriction. Such alterations in human physiology can change the absorption of common drugs of addiction, such as alcohol. This can increase the risk for problem drinking behaviors.
Wendy C. King, Ph.D., of the department of epidemiology at the University of Pittsburgh and her colleagues conducted an analysis of data from 1,945 patients in a cohort who underwent bariatric surgery in 10 U.S. hospitals. Symptoms of alcohol use disorder (AUD) were assessed pre- and postoperatively (JAMA 2012;307:2516-25).
The prevalence of AUD was significantly higher at 2 years postoperatively (9.6%), compared with the preoperative period (7.6%; P less than .01). Factors associated with a higher risk of postoperative AUD included male gender, younger age, smoking, regular alcohol consumption, a history of AUD, recreational drug use, low social support, and receiving Roux-en-Y gastric bypass.
AUD can disqualify patients from bariatric surgery – but 7.6% of patients in this survey (taken independently of clinical care) reported it. The authors noted that a 2% increase in AUD associated with bariatric surgery translates into 2,000 additional people with AUD each year.
This is particularly problematic for this population, because a large number of calories are associated with alcohol intake, and alcohol intake can lower inhibitions for other types of eating behaviors – all of which can lead to weight regain.
So, what do we do?
I think it may be helpful to take alcohol use histories in the patients we are seeing in bariatric surgery follow-up, especially those who appear to be regaining weight. Some patients may not be aware of this connection. For the patients who I have told about this relationship, they recognize it, which may be the first step toward dealing with it.
Dr. Ebbert is a professor of medicine and a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. He reports no disclosures.
As obesity continues to ravage the health of the United States, bariatric surgery offers an effective strategy for individual patients suffering from medical complications.
When performed in adults with a body mass index of at least 30 kg/m2, bariatric surgery is associated with a mean weight loss of 20%-35% of baseline weight at 2-3 years. Bariatric surgery is associated with greater reductions in obesity comorbidities, compared with lifestyle intervention and supervised weight loss. Contemporary bariatric surgeries include Roux-en-Y gastric bypass, laparoscopic adjustable gastric banding, biliopancreatic diversion with duodenal switch, sleeve gastrectomy, and mini–gastric bypass.
Bariatric surgical procedures affect weight loss through two mechanisms: malabsorption and restriction. Such alterations in human physiology can change the absorption of common drugs of addiction, such as alcohol. This can increase the risk for problem drinking behaviors.
Wendy C. King, Ph.D., of the department of epidemiology at the University of Pittsburgh and her colleagues conducted an analysis of data from 1,945 patients in a cohort who underwent bariatric surgery in 10 U.S. hospitals. Symptoms of alcohol use disorder (AUD) were assessed pre- and postoperatively (JAMA 2012;307:2516-25).
The prevalence of AUD was significantly higher at 2 years postoperatively (9.6%), compared with the preoperative period (7.6%; P less than .01). Factors associated with a higher risk of postoperative AUD included male gender, younger age, smoking, regular alcohol consumption, a history of AUD, recreational drug use, low social support, and receiving Roux-en-Y gastric bypass.
AUD can disqualify patients from bariatric surgery – but 7.6% of patients in this survey (taken independently of clinical care) reported it. The authors noted that a 2% increase in AUD associated with bariatric surgery translates into 2,000 additional people with AUD each year.
This is particularly problematic for this population, because a large number of calories are associated with alcohol intake, and alcohol intake can lower inhibitions for other types of eating behaviors – all of which can lead to weight regain.
So, what do we do?
I think it may be helpful to take alcohol use histories in the patients we are seeing in bariatric surgery follow-up, especially those who appear to be regaining weight. Some patients may not be aware of this connection. For the patients who I have told about this relationship, they recognize it, which may be the first step toward dealing with it.
Dr. Ebbert is a professor of medicine and a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. He reports no disclosures.
As obesity continues to ravage the health of the United States, bariatric surgery offers an effective strategy for individual patients suffering from medical complications.
When performed in adults with a body mass index of at least 30 kg/m2, bariatric surgery is associated with a mean weight loss of 20%-35% of baseline weight at 2-3 years. Bariatric surgery is associated with greater reductions in obesity comorbidities, compared with lifestyle intervention and supervised weight loss. Contemporary bariatric surgeries include Roux-en-Y gastric bypass, laparoscopic adjustable gastric banding, biliopancreatic diversion with duodenal switch, sleeve gastrectomy, and mini–gastric bypass.
Bariatric surgical procedures affect weight loss through two mechanisms: malabsorption and restriction. Such alterations in human physiology can change the absorption of common drugs of addiction, such as alcohol. This can increase the risk for problem drinking behaviors.
Wendy C. King, Ph.D., of the department of epidemiology at the University of Pittsburgh and her colleagues conducted an analysis of data from 1,945 patients in a cohort who underwent bariatric surgery in 10 U.S. hospitals. Symptoms of alcohol use disorder (AUD) were assessed pre- and postoperatively (JAMA 2012;307:2516-25).
The prevalence of AUD was significantly higher at 2 years postoperatively (9.6%), compared with the preoperative period (7.6%; P less than .01). Factors associated with a higher risk of postoperative AUD included male gender, younger age, smoking, regular alcohol consumption, a history of AUD, recreational drug use, low social support, and receiving Roux-en-Y gastric bypass.
AUD can disqualify patients from bariatric surgery – but 7.6% of patients in this survey (taken independently of clinical care) reported it. The authors noted that a 2% increase in AUD associated with bariatric surgery translates into 2,000 additional people with AUD each year.
This is particularly problematic for this population, because a large number of calories are associated with alcohol intake, and alcohol intake can lower inhibitions for other types of eating behaviors – all of which can lead to weight regain.
So, what do we do?
I think it may be helpful to take alcohol use histories in the patients we are seeing in bariatric surgery follow-up, especially those who appear to be regaining weight. Some patients may not be aware of this connection. For the patients who I have told about this relationship, they recognize it, which may be the first step toward dealing with it.
Dr. Ebbert is a professor of medicine and a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. He reports no disclosures.
Adding tomosynthesis improved mammography’s cancer detection
Adding tomosynthesis to screening digital mammography decreases the "recall" rate by 15% while increasing the cancer detection rate by 29%, according to a report published online June 25 in JAMA.
Researchers compared the performance of screening digital mammography alone (281,187 cases) against the performance after tomosynthesis was added to mammography (173,663 cases) at 13 sites in geographically diverse regions across the country. The work was funded primarily by Hologic, maker of the only Food and Drug Administration–approved tomosynthesis equipment at the time of this retrospective study, said Dr. Sarah M. Friedewald of the Caldwell Breast Center, Advocate Lutheran General Hospital, Park Ridge, Ill., and her associates.
The "recall" rate – the proportion of patients requiring additional imaging based on the results of their screening mammography – declined from 107 per 1,000 screens with digital mammography alone to 91 per 1,000 screens when tomosynthesis was added, a relative reduction of 15%. At the same time, the cancer detection rate rose from 4.2 to 5.4 per 1,000 scans, a relative increase of 29%. After tomosynthesis was introduced, the detection rate of invasive cancers rose from 2.9 to 4.1 per 1,000 scans, while that of ductal carcinoma in situ remained unchanged at 1.4 per 1,000, the investigators said (JAMA 2014 June 25 [doi:10.1001/jama.2014.6095]).
It is important to note that this study did not assess clinical outcomes, so it remains to be seen whether these improvements in screening mammography translate into clinically relevant improvements in breast cancer mortality. In addition, this study was limited in that it was retrospective and nonrandomized, they wrote.
This study was funded by tomosynthesis equipment maker Hologic and the National Cancer Institute. Dr. Friedewald and her associates also reported other ties to Hologic.
Tomosynthesis likely represents an advance over digital mammography for breast cancer screening, but only appropriately powered, prospective, randomized, multicenter clinical trials involving all four currently available tomosynthesis systems will answer this question definitively, said Dr. Etta D. Pisano and Martin J. Yaffe, Ph.D.
Despite the promising results of Friedewald et al., it is still uncertain whether women should specifically ask for tomosynthesis or whether screening centers should convert to tomosynthesis. People who believe screening mammography saves lives without undue false-positive results and overdiagnosis will likely advocate the addition of tomosynthesis; those who question the utility of screening mammography will not likely change their views after seeing these results, Dr. Pisano and Dr. Yaffe said.
Dr. Pisano is at the Medical University of South Carolina, Charleston. Dr. Yaffe is at the Ontario Institute for Cancer Research at the University of Toronto. Dr. Pisano reported ties to FujiFilm, Koning Corp., Siemens, Philips, and NextRay Inc.; Dr. Yaffe reported ties to GE Healthcare and Mammographic Physics Inc. These remarks were taken from their editorial accompanying Dr. Friedewald’s report (JAMA 2014;311:2488-9).
Tomosynthesis likely represents an advance over digital mammography for breast cancer screening, but only appropriately powered, prospective, randomized, multicenter clinical trials involving all four currently available tomosynthesis systems will answer this question definitively, said Dr. Etta D. Pisano and Martin J. Yaffe, Ph.D.
Despite the promising results of Friedewald et al., it is still uncertain whether women should specifically ask for tomosynthesis or whether screening centers should convert to tomosynthesis. People who believe screening mammography saves lives without undue false-positive results and overdiagnosis will likely advocate the addition of tomosynthesis; those who question the utility of screening mammography will not likely change their views after seeing these results, Dr. Pisano and Dr. Yaffe said.
Dr. Pisano is at the Medical University of South Carolina, Charleston. Dr. Yaffe is at the Ontario Institute for Cancer Research at the University of Toronto. Dr. Pisano reported ties to FujiFilm, Koning Corp., Siemens, Philips, and NextRay Inc.; Dr. Yaffe reported ties to GE Healthcare and Mammographic Physics Inc. These remarks were taken from their editorial accompanying Dr. Friedewald’s report (JAMA 2014;311:2488-9).
Tomosynthesis likely represents an advance over digital mammography for breast cancer screening, but only appropriately powered, prospective, randomized, multicenter clinical trials involving all four currently available tomosynthesis systems will answer this question definitively, said Dr. Etta D. Pisano and Martin J. Yaffe, Ph.D.
Despite the promising results of Friedewald et al., it is still uncertain whether women should specifically ask for tomosynthesis or whether screening centers should convert to tomosynthesis. People who believe screening mammography saves lives without undue false-positive results and overdiagnosis will likely advocate the addition of tomosynthesis; those who question the utility of screening mammography will not likely change their views after seeing these results, Dr. Pisano and Dr. Yaffe said.
Dr. Pisano is at the Medical University of South Carolina, Charleston. Dr. Yaffe is at the Ontario Institute for Cancer Research at the University of Toronto. Dr. Pisano reported ties to FujiFilm, Koning Corp., Siemens, Philips, and NextRay Inc.; Dr. Yaffe reported ties to GE Healthcare and Mammographic Physics Inc. These remarks were taken from their editorial accompanying Dr. Friedewald’s report (JAMA 2014;311:2488-9).
Adding tomosynthesis to screening digital mammography decreases the "recall" rate by 15% while increasing the cancer detection rate by 29%, according to a report published online June 25 in JAMA.
Researchers compared the performance of screening digital mammography alone (281,187 cases) against the performance after tomosynthesis was added to mammography (173,663 cases) at 13 sites in geographically diverse regions across the country. The work was funded primarily by Hologic, maker of the only Food and Drug Administration–approved tomosynthesis equipment at the time of this retrospective study, said Dr. Sarah M. Friedewald of the Caldwell Breast Center, Advocate Lutheran General Hospital, Park Ridge, Ill., and her associates.
The "recall" rate – the proportion of patients requiring additional imaging based on the results of their screening mammography – declined from 107 per 1,000 screens with digital mammography alone to 91 per 1,000 screens when tomosynthesis was added, a relative reduction of 15%. At the same time, the cancer detection rate rose from 4.2 to 5.4 per 1,000 scans, a relative increase of 29%. After tomosynthesis was introduced, the detection rate of invasive cancers rose from 2.9 to 4.1 per 1,000 scans, while that of ductal carcinoma in situ remained unchanged at 1.4 per 1,000, the investigators said (JAMA 2014 June 25 [doi:10.1001/jama.2014.6095]).
It is important to note that this study did not assess clinical outcomes, so it remains to be seen whether these improvements in screening mammography translate into clinically relevant improvements in breast cancer mortality. In addition, this study was limited in that it was retrospective and nonrandomized, they wrote.
This study was funded by tomosynthesis equipment maker Hologic and the National Cancer Institute. Dr. Friedewald and her associates also reported other ties to Hologic.
Adding tomosynthesis to screening digital mammography decreases the "recall" rate by 15% while increasing the cancer detection rate by 29%, according to a report published online June 25 in JAMA.
Researchers compared the performance of screening digital mammography alone (281,187 cases) against the performance after tomosynthesis was added to mammography (173,663 cases) at 13 sites in geographically diverse regions across the country. The work was funded primarily by Hologic, maker of the only Food and Drug Administration–approved tomosynthesis equipment at the time of this retrospective study, said Dr. Sarah M. Friedewald of the Caldwell Breast Center, Advocate Lutheran General Hospital, Park Ridge, Ill., and her associates.
The "recall" rate – the proportion of patients requiring additional imaging based on the results of their screening mammography – declined from 107 per 1,000 screens with digital mammography alone to 91 per 1,000 screens when tomosynthesis was added, a relative reduction of 15%. At the same time, the cancer detection rate rose from 4.2 to 5.4 per 1,000 scans, a relative increase of 29%. After tomosynthesis was introduced, the detection rate of invasive cancers rose from 2.9 to 4.1 per 1,000 scans, while that of ductal carcinoma in situ remained unchanged at 1.4 per 1,000, the investigators said (JAMA 2014 June 25 [doi:10.1001/jama.2014.6095]).
It is important to note that this study did not assess clinical outcomes, so it remains to be seen whether these improvements in screening mammography translate into clinically relevant improvements in breast cancer mortality. In addition, this study was limited in that it was retrospective and nonrandomized, they wrote.
This study was funded by tomosynthesis equipment maker Hologic and the National Cancer Institute. Dr. Friedewald and her associates also reported other ties to Hologic.
FROM JAMA
Key clinical point: Tomosynthesis may reduce the need for repeat imaging to detect breast cancer.
Major finding: The "recall" rate declined from 107 per 1,000 screens with digital mammography alone to 91 per 1,000 screens when tomosynthesis was added, a relative reduction of 15%; at the same time, the cancer detection rate rose from 4.2 to 5.4 per 1,000 scans, a relative increase of 29%.
Data source: A retrospective multicenter analysis of screening digital mammography’s performance before (281,187 scans) and after (173,663 scans) the introduction of tomosynthesis to improve its accuracy.
Disclosures: This study was funded by Hologic and the National Cancer Institute. Dr. Friedewald and her associates also reported other ties to Hologic, which makes tomosynthesis equipment.
Maintenance of certification took center stage at AMA Congress of Delegates
CHICAGO – The American Medical Association should continue to work with the American Board of Medical Specialties to address physicians’ concerns about Maintenance of Certification – that was the consensus at the annual meeting of the AMA House of Delegates.
The AMA’s delegates defeated a resolution that asked the organization to put a moratorium on MOC until it was proven to improve the quality of care and patient outcomes. However, they did agree to a new policy that directs the AMA to:
• Explore with independent entities the feasibility of conducting a study to evaluate the effect MOC requirements and Maintenance of Licensure principles have on workforce, practice costs, patient outcomes, patient safety, and patient access.
• Work with the American Board of Medical Specialties and its 24 member boards to collect data on why physicians choose to maintain or discontinue their board certification.
• Work with the ABMS and the Federation of State Medical Boards to study whether MOC and the principles of Maintenance of Licensure are important factors to physicians when deciding whether to retire and whether they have a direct effect on workforce.
• Oppose making MOC mandatory as a condition of medical licensure, and encourage physicians to strive constantly to improve their care of patients by the means they find most effective.
The new policy applies to both the ABMS MOC process and the Osteopathic Continuous Certification (OCC) process.
Physicians have increasingly voiced their concerns about MOC. Dr. Paul Teirstein, chief of cardiology and director of interventional cardiology for Scripps Clinic in La Jolla, Calif., launched a petition drive to overhaul the American Board of Internal Medicine’s MOC process. The petition has more than 17,000 signatures.
The ABIM says that it is listening to physicians and is making changes in the process, but also recently said that more than 150,000 physicians had participated in its MOC process – making the May 1 deadline to be listed on the ABIM website as having met the MOC criteria.
But anger is still bubbling up, and was expressed at the AMA’s meeting.
"Practicing physicians on the front lines are increasingly burdened, hassled, and confused by the onerous and expensive process of Maintenance of Certification and Maintenance of Licensure," said Dr. James A. Goodyear, a delegate from Pennsylvania.
Dr. Goodyear introduced the resolution to seek a moratorium on the MOC.
But Dr. Darlyne Menscer, a member of the AMA Council on Medical Education, told the delegates that such a moratorium would put a wedge in the close working relationship the AMA has had with the ABMS. "This is more prescriptive than we can commit to as a council, although we definitely do hear the concerns of the House," added Dr. Menscer.
The AMA has been discussing the concerns about MOC with the ABMS, most recently holding a meeting in Chicago in early June.
Dr. Joshua Cohen, a delegate from the American Academy of Neurology, and a member of the AMA Foundation’s Board of Directors, who attended that meeting, also argued against a moratorium. "It would make it impossible for the AMA to improve the process going forward," said Dr. Cohen.
Dr. Chuck Wilson, a pediatrician and delegate from the North Carolina delegation, also opposed any major change in direction for the AMA. He noted that if the AMA was seen as opposed to MOC, it might not be viewed well. "We all want it to be less onerous," said Dr. Wilson. But, he noted, "the Council on Medical Education is working in that direction. Let’s give them a chance to be successful."
In a statement after the HOD meeting, the AMA said that it "continues to ensure the MOC process does not disrupt physician practice or reduce the capacity of the overall physician workforce." Concerns about MOC "center around the need for relevance to the daily practice of physicians and the better integration into physician practices to optimally support learning and improvement."
On Twitter @aliciaault
CHICAGO – The American Medical Association should continue to work with the American Board of Medical Specialties to address physicians’ concerns about Maintenance of Certification – that was the consensus at the annual meeting of the AMA House of Delegates.
The AMA’s delegates defeated a resolution that asked the organization to put a moratorium on MOC until it was proven to improve the quality of care and patient outcomes. However, they did agree to a new policy that directs the AMA to:
• Explore with independent entities the feasibility of conducting a study to evaluate the effect MOC requirements and Maintenance of Licensure principles have on workforce, practice costs, patient outcomes, patient safety, and patient access.
• Work with the American Board of Medical Specialties and its 24 member boards to collect data on why physicians choose to maintain or discontinue their board certification.
• Work with the ABMS and the Federation of State Medical Boards to study whether MOC and the principles of Maintenance of Licensure are important factors to physicians when deciding whether to retire and whether they have a direct effect on workforce.
• Oppose making MOC mandatory as a condition of medical licensure, and encourage physicians to strive constantly to improve their care of patients by the means they find most effective.
The new policy applies to both the ABMS MOC process and the Osteopathic Continuous Certification (OCC) process.
Physicians have increasingly voiced their concerns about MOC. Dr. Paul Teirstein, chief of cardiology and director of interventional cardiology for Scripps Clinic in La Jolla, Calif., launched a petition drive to overhaul the American Board of Internal Medicine’s MOC process. The petition has more than 17,000 signatures.
The ABIM says that it is listening to physicians and is making changes in the process, but also recently said that more than 150,000 physicians had participated in its MOC process – making the May 1 deadline to be listed on the ABIM website as having met the MOC criteria.
But anger is still bubbling up, and was expressed at the AMA’s meeting.
"Practicing physicians on the front lines are increasingly burdened, hassled, and confused by the onerous and expensive process of Maintenance of Certification and Maintenance of Licensure," said Dr. James A. Goodyear, a delegate from Pennsylvania.
Dr. Goodyear introduced the resolution to seek a moratorium on the MOC.
But Dr. Darlyne Menscer, a member of the AMA Council on Medical Education, told the delegates that such a moratorium would put a wedge in the close working relationship the AMA has had with the ABMS. "This is more prescriptive than we can commit to as a council, although we definitely do hear the concerns of the House," added Dr. Menscer.
The AMA has been discussing the concerns about MOC with the ABMS, most recently holding a meeting in Chicago in early June.
Dr. Joshua Cohen, a delegate from the American Academy of Neurology, and a member of the AMA Foundation’s Board of Directors, who attended that meeting, also argued against a moratorium. "It would make it impossible for the AMA to improve the process going forward," said Dr. Cohen.
Dr. Chuck Wilson, a pediatrician and delegate from the North Carolina delegation, also opposed any major change in direction for the AMA. He noted that if the AMA was seen as opposed to MOC, it might not be viewed well. "We all want it to be less onerous," said Dr. Wilson. But, he noted, "the Council on Medical Education is working in that direction. Let’s give them a chance to be successful."
In a statement after the HOD meeting, the AMA said that it "continues to ensure the MOC process does not disrupt physician practice or reduce the capacity of the overall physician workforce." Concerns about MOC "center around the need for relevance to the daily practice of physicians and the better integration into physician practices to optimally support learning and improvement."
On Twitter @aliciaault
CHICAGO – The American Medical Association should continue to work with the American Board of Medical Specialties to address physicians’ concerns about Maintenance of Certification – that was the consensus at the annual meeting of the AMA House of Delegates.
The AMA’s delegates defeated a resolution that asked the organization to put a moratorium on MOC until it was proven to improve the quality of care and patient outcomes. However, they did agree to a new policy that directs the AMA to:
• Explore with independent entities the feasibility of conducting a study to evaluate the effect MOC requirements and Maintenance of Licensure principles have on workforce, practice costs, patient outcomes, patient safety, and patient access.
• Work with the American Board of Medical Specialties and its 24 member boards to collect data on why physicians choose to maintain or discontinue their board certification.
• Work with the ABMS and the Federation of State Medical Boards to study whether MOC and the principles of Maintenance of Licensure are important factors to physicians when deciding whether to retire and whether they have a direct effect on workforce.
• Oppose making MOC mandatory as a condition of medical licensure, and encourage physicians to strive constantly to improve their care of patients by the means they find most effective.
The new policy applies to both the ABMS MOC process and the Osteopathic Continuous Certification (OCC) process.
Physicians have increasingly voiced their concerns about MOC. Dr. Paul Teirstein, chief of cardiology and director of interventional cardiology for Scripps Clinic in La Jolla, Calif., launched a petition drive to overhaul the American Board of Internal Medicine’s MOC process. The petition has more than 17,000 signatures.
The ABIM says that it is listening to physicians and is making changes in the process, but also recently said that more than 150,000 physicians had participated in its MOC process – making the May 1 deadline to be listed on the ABIM website as having met the MOC criteria.
But anger is still bubbling up, and was expressed at the AMA’s meeting.
"Practicing physicians on the front lines are increasingly burdened, hassled, and confused by the onerous and expensive process of Maintenance of Certification and Maintenance of Licensure," said Dr. James A. Goodyear, a delegate from Pennsylvania.
Dr. Goodyear introduced the resolution to seek a moratorium on the MOC.
But Dr. Darlyne Menscer, a member of the AMA Council on Medical Education, told the delegates that such a moratorium would put a wedge in the close working relationship the AMA has had with the ABMS. "This is more prescriptive than we can commit to as a council, although we definitely do hear the concerns of the House," added Dr. Menscer.
The AMA has been discussing the concerns about MOC with the ABMS, most recently holding a meeting in Chicago in early June.
Dr. Joshua Cohen, a delegate from the American Academy of Neurology, and a member of the AMA Foundation’s Board of Directors, who attended that meeting, also argued against a moratorium. "It would make it impossible for the AMA to improve the process going forward," said Dr. Cohen.
Dr. Chuck Wilson, a pediatrician and delegate from the North Carolina delegation, also opposed any major change in direction for the AMA. He noted that if the AMA was seen as opposed to MOC, it might not be viewed well. "We all want it to be less onerous," said Dr. Wilson. But, he noted, "the Council on Medical Education is working in that direction. Let’s give them a chance to be successful."
In a statement after the HOD meeting, the AMA said that it "continues to ensure the MOC process does not disrupt physician practice or reduce the capacity of the overall physician workforce." Concerns about MOC "center around the need for relevance to the daily practice of physicians and the better integration into physician practices to optimally support learning and improvement."
On Twitter @aliciaault
AT THE AMA HOD MEETING
Survey: Insurance companies, government blamed for cost of health care
When it comes to the increasingly high cost of health care, Americans are most likely to put the blame on health insurance companies and the government, according to a survey from digital media company Morning Consult.
Among all responders, 30% said that insurance companies were most responsible for the high costs of health care, while 25% put the blame on the government and another 12% named the drug companies, Morning Consult reported.
Things change a bit, though, when viewed through a political lens. Among Democrats, 37% said that insurance companies bore the most responsibility, compared with 14% for the government and 14% for drug companies. Republicans saw the situation a bit differently, with government leading the way at 37%, insurance companies at 22%, and drug companies at 10%. Among Independents, 29% put primary responsibility on insurance companies, 25% on the government, and 10% on drug companies, the survey showed.
Among other entities included in the survey, 9% of all respondents said that hospitals were most responsible for the high cost of health care, 7% blamed physicians, and 2% blamed medical device companies.
The survey was conducted online during March 21-23, 2014, and May 2-4, 2014, among a national sample of 3,687 registered voters. It was performed by Survey Sampling International.
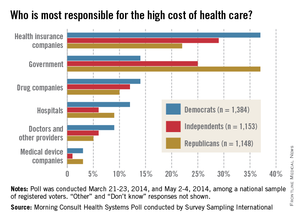
When it comes to the increasingly high cost of health care, Americans are most likely to put the blame on health insurance companies and the government, according to a survey from digital media company Morning Consult.
Among all responders, 30% said that insurance companies were most responsible for the high costs of health care, while 25% put the blame on the government and another 12% named the drug companies, Morning Consult reported.
Things change a bit, though, when viewed through a political lens. Among Democrats, 37% said that insurance companies bore the most responsibility, compared with 14% for the government and 14% for drug companies. Republicans saw the situation a bit differently, with government leading the way at 37%, insurance companies at 22%, and drug companies at 10%. Among Independents, 29% put primary responsibility on insurance companies, 25% on the government, and 10% on drug companies, the survey showed.
Among other entities included in the survey, 9% of all respondents said that hospitals were most responsible for the high cost of health care, 7% blamed physicians, and 2% blamed medical device companies.
The survey was conducted online during March 21-23, 2014, and May 2-4, 2014, among a national sample of 3,687 registered voters. It was performed by Survey Sampling International.
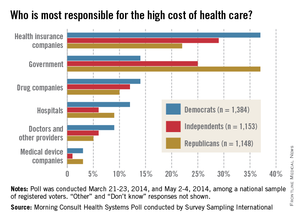
When it comes to the increasingly high cost of health care, Americans are most likely to put the blame on health insurance companies and the government, according to a survey from digital media company Morning Consult.
Among all responders, 30% said that insurance companies were most responsible for the high costs of health care, while 25% put the blame on the government and another 12% named the drug companies, Morning Consult reported.
Things change a bit, though, when viewed through a political lens. Among Democrats, 37% said that insurance companies bore the most responsibility, compared with 14% for the government and 14% for drug companies. Republicans saw the situation a bit differently, with government leading the way at 37%, insurance companies at 22%, and drug companies at 10%. Among Independents, 29% put primary responsibility on insurance companies, 25% on the government, and 10% on drug companies, the survey showed.
Among other entities included in the survey, 9% of all respondents said that hospitals were most responsible for the high cost of health care, 7% blamed physicians, and 2% blamed medical device companies.
The survey was conducted online during March 21-23, 2014, and May 2-4, 2014, among a national sample of 3,687 registered voters. It was performed by Survey Sampling International.