User login
Official Newspaper of the American College of Surgeons
Survey: Pediatric hospitalists are treating more acutely ill children
SAN DIEGO – Pediatric hospitalists are treating a greater proportion of acutely ill children than ever before, results from the largest and most up-to-date national survey suggests.
“What we’re seeing is that our colleagues in ambulatory medicine are treating a large swath of patients that used to spend 1, 2, 3, or even more days in the hospital,” Dr. Erin Stucky Fisher said in an interview at the annual meeting of the American Academy of Pediatrics. “Given that those patients are no longer being hospitalized, and given that our emergency room colleagues stabilize and discharge yet another group of ill patients, patients who are admitted require a higher level of acute care thinking. More often the skill sets required for hospital medicine will require clinicians to be able to care for patients that require multiple visits daily and acute care decision making 24/7.”
In an effort to describe current pediatric hospitalist work trends, Dr. Fisher and her associates sent a survey to 1,260 members of the AAP’s Section of Hospital Medicine during the winter of 2012-2013. A total of 542 completed the survey for a response rate of 43%, making it the largest cohort of pediatric hospitalists surveyed to date. Of these, 64% were female and 85% were white.
Slightly more than half of respondents (51%) reported working 6-7 or 8-14 consecutive days when on service, with 57% spending 40-60 hours of on-site time per service week, and 28% spending more than 60 hours. Fewer than half (43%) provide 24/7 in-house coverage, 34% take call from home, and 23% use a hybrid model for after-hours coverage.
Nearly all respondents (97%) cover general pediatric units, and 49% consult in emergency medicine departments. Other common areas of coverage include the observation unit (36%), well baby nursery (34%), intermediate care/step-down unit (27%), and the pediatric intensive care unit (9%).
More than two-third of respondents (43%) routinely comanage surgery patients, 23% provide consultation to surgery patients, and nearly one-third (29%) participate in rapid response teams. In addition, 21% provide a sedation service and 11% provide a diagnostic referral service. While only 6% currently provide patient emergency transport, this is of interest as a partnership opportunity with critical care colleagues.
The most common procedure performed by respondents are lumbar puncture (88%), followed by arterial puncture (29%), intubation of children without teeth (29%), venipuncture (28%), peripheral IV placement (26%), and bladder catheterization (20%).
Findings “not surprising but notable – as the field has evolved – are that there is increasing provision of critical care and emergency level services,” said Dr. Fisher, a pediatric hospitalist at Rady Children’s Hospital–San Diego and professor of clinical pediatrics at the University of California, San Diego. “This reflects both the need for these services and a fact reported in other studies on hospitalized patients over the years: In all hospital settings, patients that are admitted – particularly children – are sicker. Many leaders and clinicians in hospital settings state that hospitals are or soon will be in essence a high-end critical care ICU, a step-down ICU, and an emergency department. Nowadays there are fewer patients admitted who are what would be considered standard ward patients. For community sites that’s particularly telling, because hospitalists in those settings are having to care for many sicker patients because there aren’t [enough] critical care physicians available in those environments.”
The study’s lead author is Dr. Daniel A. Rauch, a pediatrician based in Elmhurst, N.Y. Dr. Fisher reported having no financial disclosures.
On Twitter @dougbrunk
SAN DIEGO – Pediatric hospitalists are treating a greater proportion of acutely ill children than ever before, results from the largest and most up-to-date national survey suggests.
“What we’re seeing is that our colleagues in ambulatory medicine are treating a large swath of patients that used to spend 1, 2, 3, or even more days in the hospital,” Dr. Erin Stucky Fisher said in an interview at the annual meeting of the American Academy of Pediatrics. “Given that those patients are no longer being hospitalized, and given that our emergency room colleagues stabilize and discharge yet another group of ill patients, patients who are admitted require a higher level of acute care thinking. More often the skill sets required for hospital medicine will require clinicians to be able to care for patients that require multiple visits daily and acute care decision making 24/7.”
In an effort to describe current pediatric hospitalist work trends, Dr. Fisher and her associates sent a survey to 1,260 members of the AAP’s Section of Hospital Medicine during the winter of 2012-2013. A total of 542 completed the survey for a response rate of 43%, making it the largest cohort of pediatric hospitalists surveyed to date. Of these, 64% were female and 85% were white.
Slightly more than half of respondents (51%) reported working 6-7 or 8-14 consecutive days when on service, with 57% spending 40-60 hours of on-site time per service week, and 28% spending more than 60 hours. Fewer than half (43%) provide 24/7 in-house coverage, 34% take call from home, and 23% use a hybrid model for after-hours coverage.
Nearly all respondents (97%) cover general pediatric units, and 49% consult in emergency medicine departments. Other common areas of coverage include the observation unit (36%), well baby nursery (34%), intermediate care/step-down unit (27%), and the pediatric intensive care unit (9%).
More than two-third of respondents (43%) routinely comanage surgery patients, 23% provide consultation to surgery patients, and nearly one-third (29%) participate in rapid response teams. In addition, 21% provide a sedation service and 11% provide a diagnostic referral service. While only 6% currently provide patient emergency transport, this is of interest as a partnership opportunity with critical care colleagues.
The most common procedure performed by respondents are lumbar puncture (88%), followed by arterial puncture (29%), intubation of children without teeth (29%), venipuncture (28%), peripheral IV placement (26%), and bladder catheterization (20%).
Findings “not surprising but notable – as the field has evolved – are that there is increasing provision of critical care and emergency level services,” said Dr. Fisher, a pediatric hospitalist at Rady Children’s Hospital–San Diego and professor of clinical pediatrics at the University of California, San Diego. “This reflects both the need for these services and a fact reported in other studies on hospitalized patients over the years: In all hospital settings, patients that are admitted – particularly children – are sicker. Many leaders and clinicians in hospital settings state that hospitals are or soon will be in essence a high-end critical care ICU, a step-down ICU, and an emergency department. Nowadays there are fewer patients admitted who are what would be considered standard ward patients. For community sites that’s particularly telling, because hospitalists in those settings are having to care for many sicker patients because there aren’t [enough] critical care physicians available in those environments.”
The study’s lead author is Dr. Daniel A. Rauch, a pediatrician based in Elmhurst, N.Y. Dr. Fisher reported having no financial disclosures.
On Twitter @dougbrunk
SAN DIEGO – Pediatric hospitalists are treating a greater proportion of acutely ill children than ever before, results from the largest and most up-to-date national survey suggests.
“What we’re seeing is that our colleagues in ambulatory medicine are treating a large swath of patients that used to spend 1, 2, 3, or even more days in the hospital,” Dr. Erin Stucky Fisher said in an interview at the annual meeting of the American Academy of Pediatrics. “Given that those patients are no longer being hospitalized, and given that our emergency room colleagues stabilize and discharge yet another group of ill patients, patients who are admitted require a higher level of acute care thinking. More often the skill sets required for hospital medicine will require clinicians to be able to care for patients that require multiple visits daily and acute care decision making 24/7.”
In an effort to describe current pediatric hospitalist work trends, Dr. Fisher and her associates sent a survey to 1,260 members of the AAP’s Section of Hospital Medicine during the winter of 2012-2013. A total of 542 completed the survey for a response rate of 43%, making it the largest cohort of pediatric hospitalists surveyed to date. Of these, 64% were female and 85% were white.
Slightly more than half of respondents (51%) reported working 6-7 or 8-14 consecutive days when on service, with 57% spending 40-60 hours of on-site time per service week, and 28% spending more than 60 hours. Fewer than half (43%) provide 24/7 in-house coverage, 34% take call from home, and 23% use a hybrid model for after-hours coverage.
Nearly all respondents (97%) cover general pediatric units, and 49% consult in emergency medicine departments. Other common areas of coverage include the observation unit (36%), well baby nursery (34%), intermediate care/step-down unit (27%), and the pediatric intensive care unit (9%).
More than two-third of respondents (43%) routinely comanage surgery patients, 23% provide consultation to surgery patients, and nearly one-third (29%) participate in rapid response teams. In addition, 21% provide a sedation service and 11% provide a diagnostic referral service. While only 6% currently provide patient emergency transport, this is of interest as a partnership opportunity with critical care colleagues.
The most common procedure performed by respondents are lumbar puncture (88%), followed by arterial puncture (29%), intubation of children without teeth (29%), venipuncture (28%), peripheral IV placement (26%), and bladder catheterization (20%).
Findings “not surprising but notable – as the field has evolved – are that there is increasing provision of critical care and emergency level services,” said Dr. Fisher, a pediatric hospitalist at Rady Children’s Hospital–San Diego and professor of clinical pediatrics at the University of California, San Diego. “This reflects both the need for these services and a fact reported in other studies on hospitalized patients over the years: In all hospital settings, patients that are admitted – particularly children – are sicker. Many leaders and clinicians in hospital settings state that hospitals are or soon will be in essence a high-end critical care ICU, a step-down ICU, and an emergency department. Nowadays there are fewer patients admitted who are what would be considered standard ward patients. For community sites that’s particularly telling, because hospitalists in those settings are having to care for many sicker patients because there aren’t [enough] critical care physicians available in those environments.”
The study’s lead author is Dr. Daniel A. Rauch, a pediatrician based in Elmhurst, N.Y. Dr. Fisher reported having no financial disclosures.
On Twitter @dougbrunk
AT THE AAP NATIONAL CONFERENCE
Key clinical point: Pediatric hospitalists are treating more acutely ill children than ever before.
Major finding: Nearly half of pediatric hospitalists (49%) consult in emergency medicine departments, 43% routinely comanage surgery patients, 23% provide consultation to surgery patients, and nearly one-third (29%) participate in rapid response teams.
Data source: Responses from a survey sent to 1,260 members of the AAP’s Section of Hospital Medicine during the winter of 2012-2013.
Disclosures: Dr. Fisher reported having no financial disclosures.
Postdiagnosis imaging common in thyroid cancer
CORONADO, CALIF.– Today’s clinicians are ordering more postdiagnosis imaging tests in patients with thyroid cancer than they did in the early 1990s, results from the largest study of its kind showed.
“There is very little data on surveillance imaging for cancers in general, and especially for thyroid cancer,” lead author Dr. Jaime L. Wiebel said in an interview in advance of at the annual meeting of the American Thyroid Association, where the work was presented. “This study revealed that, over time, there has been an increase in all postdiagnosis imaging studies: ultrasound, I-131 [radioactive iodine] scans, and PET scans.”
Dr. Wiebel of the University of Michigan’s metabolism, endocrinology, and diabetes clinic, Ann Arbor, and her associates used records from the linked database to identify patients diagnosed with localized, regional, or distant well-differentiated thyroid cancer between 1991 and 2009. Next, they reviewed medical claims and determined the use of thyroid ultrasound, I-131 scan, or PET scan within 3 years post diagnosis. The researchers used linear regression analysis to evaluate imaging trends during the study period and multivariate logistic regression to estimate the likelihood of imaging use based on patient characteristics.
In all, 23,669 patients with well-differentiated thyroid cancer were included in the analysis. Most (79%) were younger than age 75 years, and 70% were female. Dr. Wiebel and her associates observed an increased use of both thyroid ultrasound and I-131 among patients with localized disease (P < .001 and P = .003, respectively). Use of the two modalities also increased among patients with regional disease (both P < .001) as well as among patients with distant disease (P = .001 and P = .015).
After controlling for patient characteristics, the researchers found that patients diagnosed during 2001-2009 were 2.15 times more likely to undergo a thyroid ultrasound, compared with those diagnosed during 1991-2000. In addition, PET scan use during 2005-2009, compared with 1996-2004, increased 32.4-fold among those with localized disease, 13.1-fold among those with regional disease, and 33.4-fold among those with distant disease (all significant at P < .001). Patients diagnosed with thyroid cancer after the year 2000 were more likely to have smaller, localized cancer.
“A few of our findings were unexpected,” Dr. Wiebel said. “We had anticipated that since more low-risk thyroid cancer is being diagnosed in the United States, that postdiagnosis surveillance imaging would decrease over time. We found the exact opposite. Despite the rise in low-risk thyroid cancer, there has been an increase in postdiagnosis imaging in the United States. Especially surprising was the very large increase in PET scan use.”
She acknowledged certain limitations of the analysis, including lack of data regarding indications for the imaging studies, “including iodine avidity of the tumor, disease recurrence, or patient preferences,” and the fact that most of the patients were over age 65 years. “However, we suspect that imaging practices in younger patients are similar,” she said.
Dr. Wiebel reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF.– Today’s clinicians are ordering more postdiagnosis imaging tests in patients with thyroid cancer than they did in the early 1990s, results from the largest study of its kind showed.
“There is very little data on surveillance imaging for cancers in general, and especially for thyroid cancer,” lead author Dr. Jaime L. Wiebel said in an interview in advance of at the annual meeting of the American Thyroid Association, where the work was presented. “This study revealed that, over time, there has been an increase in all postdiagnosis imaging studies: ultrasound, I-131 [radioactive iodine] scans, and PET scans.”
Dr. Wiebel of the University of Michigan’s metabolism, endocrinology, and diabetes clinic, Ann Arbor, and her associates used records from the linked database to identify patients diagnosed with localized, regional, or distant well-differentiated thyroid cancer between 1991 and 2009. Next, they reviewed medical claims and determined the use of thyroid ultrasound, I-131 scan, or PET scan within 3 years post diagnosis. The researchers used linear regression analysis to evaluate imaging trends during the study period and multivariate logistic regression to estimate the likelihood of imaging use based on patient characteristics.
In all, 23,669 patients with well-differentiated thyroid cancer were included in the analysis. Most (79%) were younger than age 75 years, and 70% were female. Dr. Wiebel and her associates observed an increased use of both thyroid ultrasound and I-131 among patients with localized disease (P < .001 and P = .003, respectively). Use of the two modalities also increased among patients with regional disease (both P < .001) as well as among patients with distant disease (P = .001 and P = .015).
After controlling for patient characteristics, the researchers found that patients diagnosed during 2001-2009 were 2.15 times more likely to undergo a thyroid ultrasound, compared with those diagnosed during 1991-2000. In addition, PET scan use during 2005-2009, compared with 1996-2004, increased 32.4-fold among those with localized disease, 13.1-fold among those with regional disease, and 33.4-fold among those with distant disease (all significant at P < .001). Patients diagnosed with thyroid cancer after the year 2000 were more likely to have smaller, localized cancer.
“A few of our findings were unexpected,” Dr. Wiebel said. “We had anticipated that since more low-risk thyroid cancer is being diagnosed in the United States, that postdiagnosis surveillance imaging would decrease over time. We found the exact opposite. Despite the rise in low-risk thyroid cancer, there has been an increase in postdiagnosis imaging in the United States. Especially surprising was the very large increase in PET scan use.”
She acknowledged certain limitations of the analysis, including lack of data regarding indications for the imaging studies, “including iodine avidity of the tumor, disease recurrence, or patient preferences,” and the fact that most of the patients were over age 65 years. “However, we suspect that imaging practices in younger patients are similar,” she said.
Dr. Wiebel reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF.– Today’s clinicians are ordering more postdiagnosis imaging tests in patients with thyroid cancer than they did in the early 1990s, results from the largest study of its kind showed.
“There is very little data on surveillance imaging for cancers in general, and especially for thyroid cancer,” lead author Dr. Jaime L. Wiebel said in an interview in advance of at the annual meeting of the American Thyroid Association, where the work was presented. “This study revealed that, over time, there has been an increase in all postdiagnosis imaging studies: ultrasound, I-131 [radioactive iodine] scans, and PET scans.”
Dr. Wiebel of the University of Michigan’s metabolism, endocrinology, and diabetes clinic, Ann Arbor, and her associates used records from the linked database to identify patients diagnosed with localized, regional, or distant well-differentiated thyroid cancer between 1991 and 2009. Next, they reviewed medical claims and determined the use of thyroid ultrasound, I-131 scan, or PET scan within 3 years post diagnosis. The researchers used linear regression analysis to evaluate imaging trends during the study period and multivariate logistic regression to estimate the likelihood of imaging use based on patient characteristics.
In all, 23,669 patients with well-differentiated thyroid cancer were included in the analysis. Most (79%) were younger than age 75 years, and 70% were female. Dr. Wiebel and her associates observed an increased use of both thyroid ultrasound and I-131 among patients with localized disease (P < .001 and P = .003, respectively). Use of the two modalities also increased among patients with regional disease (both P < .001) as well as among patients with distant disease (P = .001 and P = .015).
After controlling for patient characteristics, the researchers found that patients diagnosed during 2001-2009 were 2.15 times more likely to undergo a thyroid ultrasound, compared with those diagnosed during 1991-2000. In addition, PET scan use during 2005-2009, compared with 1996-2004, increased 32.4-fold among those with localized disease, 13.1-fold among those with regional disease, and 33.4-fold among those with distant disease (all significant at P < .001). Patients diagnosed with thyroid cancer after the year 2000 were more likely to have smaller, localized cancer.
“A few of our findings were unexpected,” Dr. Wiebel said. “We had anticipated that since more low-risk thyroid cancer is being diagnosed in the United States, that postdiagnosis surveillance imaging would decrease over time. We found the exact opposite. Despite the rise in low-risk thyroid cancer, there has been an increase in postdiagnosis imaging in the United States. Especially surprising was the very large increase in PET scan use.”
She acknowledged certain limitations of the analysis, including lack of data regarding indications for the imaging studies, “including iodine avidity of the tumor, disease recurrence, or patient preferences,” and the fact that most of the patients were over age 65 years. “However, we suspect that imaging practices in younger patients are similar,” she said.
Dr. Wiebel reported having no financial disclosures.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: Regardless of stage, clinicians are doing more postdiagnosis imaging of thyroid cancer patients than they were in the 1990s.
Major finding: Between 1991 and 2009, the use of both thyroid ultrasound and I-131 scans increased significantly among patients with localized thyroid disease. Imaging also increased among those with regional and distant disease.
Data source: An analysis of 23,669 patients diagnosed with localized, regional, or distant well-differentiated thyroid cancer between 1991 and 2009 who were identified from the linked SEER-Medicare database.
Disclosures: Dr. Wiebel reported having no financial disclosures.
Decompression can save lives in ventricular trapping
BALTIMORE –Aggressive decompression dramatically improved survival in patients who had trapped ventricle syndrome as a result of tumor or intracerebral hemorrhage in a retrospective study.
Overall mortality in the cohort was 70% among those who had no decompression, Dr. Gabriel L. Pagani-Estevez said at the annual meeting of the American Neurological Association. But it dropped to 19% among those who underwent some form of decompression therapy. Even after controlling for confounding factors like age, etiology, and hemorrhage volume, decompression remained a significant independent predictor of survival, said Dr. Pagani-Estevez, a neurology resident at the Mayo Clinic, Rochester, Minn.
Despite all the methodological issues inherent in a retrospective study, the findings “provide at least a suggestion that neurosurgical intervention can markedly reduce mortality in trapped ventricle syndrome,” he said. “Now, research needs to clarify the ideal intervention, the effect of decompression on functional outcome, and which patients might derive the most benefit from treatment.”
The cohort comprised 392 patients who developed ventricular trapping and were treated during 2002-2010. They were a mean of 58 years old. Most (223) were not on anticoagulation therapy. A total of 80 patients were taking aspirin, and the remainder were taking other anticoagulants. The median midline shift was about 10 mm.
Trapping was caused by a tumor in 177 patients. Other etiologies included intracerebral hemorrhage (80), subdural hematoma (55), trauma (26), and stroke (18). Unspecified causes made up the remainder.
The left lateral ventricle was most often involved (176). The right lateral ventricle was trapped in 159 patients and both were involved in 32. Thirteen patients had a trapped fourth ventricle, and 12 had unspecified trapping.
Some kind of decompression procedure was performed on 221 patients. These included craniotomy (126), craniectomy (26), external ventricular drain (30), ventricular-peritoneal shunt (23), and endoscopic septum pellucidum fenestration (16).
Comparisons showed significantly decreased mortality for intervention vs. nonintervention in groups with various causes of ventricular trapping: intracerebral hemorrhage (48% vs. 95%), tumor (12% vs. 47%), and subdural hematoma (20% vs. 90%).
There were nonsignificant declines in mortality among patients who underwent intervention for ventricular trapping caused by trauma or ischemic stroke, but the number of patients in those subgroups were small, which probably confounded the results, Dr. Pagani-Estevez said.
He then conducted a multivariate analysis to determine patient characteristics that might have contributed to survival. Patients who had a decompression procedure were 87% less likely to die than were those who had not – a highly significant finding (P = .0001). A midline shift conferred a slight increase in the risk of death, while having intracerebral hemorrhage as the trapping etiology increased the risk fourfold.
Trapped ventricle carries a notoriously poor prognosis, said Dr. Alejandro A. Rabinstein, a coauthor on the study. “By the time you develop it, it’s a very bad situation, so whatever way you can achieve decompression may improve the situation,” said Dr. Rabinstein, a critical care neurologist who is also at the Mayo Clinic in Rochester. “If you don’t think the patient has enough left to merit the intervention, then you just don’t do it. But despite that limitation, if you think the patient can recover some function, it’s appropriate. An intervention will make patients survive way more often than no intervention. Without something, though, the prospect of survival is bleak.”
Neither Dr. Pagani-Estevez nor Dr. Rabinstein had any financial disclosures.
On Twitter @alz_gal
BALTIMORE –Aggressive decompression dramatically improved survival in patients who had trapped ventricle syndrome as a result of tumor or intracerebral hemorrhage in a retrospective study.
Overall mortality in the cohort was 70% among those who had no decompression, Dr. Gabriel L. Pagani-Estevez said at the annual meeting of the American Neurological Association. But it dropped to 19% among those who underwent some form of decompression therapy. Even after controlling for confounding factors like age, etiology, and hemorrhage volume, decompression remained a significant independent predictor of survival, said Dr. Pagani-Estevez, a neurology resident at the Mayo Clinic, Rochester, Minn.
Despite all the methodological issues inherent in a retrospective study, the findings “provide at least a suggestion that neurosurgical intervention can markedly reduce mortality in trapped ventricle syndrome,” he said. “Now, research needs to clarify the ideal intervention, the effect of decompression on functional outcome, and which patients might derive the most benefit from treatment.”
The cohort comprised 392 patients who developed ventricular trapping and were treated during 2002-2010. They were a mean of 58 years old. Most (223) were not on anticoagulation therapy. A total of 80 patients were taking aspirin, and the remainder were taking other anticoagulants. The median midline shift was about 10 mm.
Trapping was caused by a tumor in 177 patients. Other etiologies included intracerebral hemorrhage (80), subdural hematoma (55), trauma (26), and stroke (18). Unspecified causes made up the remainder.
The left lateral ventricle was most often involved (176). The right lateral ventricle was trapped in 159 patients and both were involved in 32. Thirteen patients had a trapped fourth ventricle, and 12 had unspecified trapping.
Some kind of decompression procedure was performed on 221 patients. These included craniotomy (126), craniectomy (26), external ventricular drain (30), ventricular-peritoneal shunt (23), and endoscopic septum pellucidum fenestration (16).
Comparisons showed significantly decreased mortality for intervention vs. nonintervention in groups with various causes of ventricular trapping: intracerebral hemorrhage (48% vs. 95%), tumor (12% vs. 47%), and subdural hematoma (20% vs. 90%).
There were nonsignificant declines in mortality among patients who underwent intervention for ventricular trapping caused by trauma or ischemic stroke, but the number of patients in those subgroups were small, which probably confounded the results, Dr. Pagani-Estevez said.
He then conducted a multivariate analysis to determine patient characteristics that might have contributed to survival. Patients who had a decompression procedure were 87% less likely to die than were those who had not – a highly significant finding (P = .0001). A midline shift conferred a slight increase in the risk of death, while having intracerebral hemorrhage as the trapping etiology increased the risk fourfold.
Trapped ventricle carries a notoriously poor prognosis, said Dr. Alejandro A. Rabinstein, a coauthor on the study. “By the time you develop it, it’s a very bad situation, so whatever way you can achieve decompression may improve the situation,” said Dr. Rabinstein, a critical care neurologist who is also at the Mayo Clinic in Rochester. “If you don’t think the patient has enough left to merit the intervention, then you just don’t do it. But despite that limitation, if you think the patient can recover some function, it’s appropriate. An intervention will make patients survive way more often than no intervention. Without something, though, the prospect of survival is bleak.”
Neither Dr. Pagani-Estevez nor Dr. Rabinstein had any financial disclosures.
On Twitter @alz_gal
BALTIMORE –Aggressive decompression dramatically improved survival in patients who had trapped ventricle syndrome as a result of tumor or intracerebral hemorrhage in a retrospective study.
Overall mortality in the cohort was 70% among those who had no decompression, Dr. Gabriel L. Pagani-Estevez said at the annual meeting of the American Neurological Association. But it dropped to 19% among those who underwent some form of decompression therapy. Even after controlling for confounding factors like age, etiology, and hemorrhage volume, decompression remained a significant independent predictor of survival, said Dr. Pagani-Estevez, a neurology resident at the Mayo Clinic, Rochester, Minn.
Despite all the methodological issues inherent in a retrospective study, the findings “provide at least a suggestion that neurosurgical intervention can markedly reduce mortality in trapped ventricle syndrome,” he said. “Now, research needs to clarify the ideal intervention, the effect of decompression on functional outcome, and which patients might derive the most benefit from treatment.”
The cohort comprised 392 patients who developed ventricular trapping and were treated during 2002-2010. They were a mean of 58 years old. Most (223) were not on anticoagulation therapy. A total of 80 patients were taking aspirin, and the remainder were taking other anticoagulants. The median midline shift was about 10 mm.
Trapping was caused by a tumor in 177 patients. Other etiologies included intracerebral hemorrhage (80), subdural hematoma (55), trauma (26), and stroke (18). Unspecified causes made up the remainder.
The left lateral ventricle was most often involved (176). The right lateral ventricle was trapped in 159 patients and both were involved in 32. Thirteen patients had a trapped fourth ventricle, and 12 had unspecified trapping.
Some kind of decompression procedure was performed on 221 patients. These included craniotomy (126), craniectomy (26), external ventricular drain (30), ventricular-peritoneal shunt (23), and endoscopic septum pellucidum fenestration (16).
Comparisons showed significantly decreased mortality for intervention vs. nonintervention in groups with various causes of ventricular trapping: intracerebral hemorrhage (48% vs. 95%), tumor (12% vs. 47%), and subdural hematoma (20% vs. 90%).
There were nonsignificant declines in mortality among patients who underwent intervention for ventricular trapping caused by trauma or ischemic stroke, but the number of patients in those subgroups were small, which probably confounded the results, Dr. Pagani-Estevez said.
He then conducted a multivariate analysis to determine patient characteristics that might have contributed to survival. Patients who had a decompression procedure were 87% less likely to die than were those who had not – a highly significant finding (P = .0001). A midline shift conferred a slight increase in the risk of death, while having intracerebral hemorrhage as the trapping etiology increased the risk fourfold.
Trapped ventricle carries a notoriously poor prognosis, said Dr. Alejandro A. Rabinstein, a coauthor on the study. “By the time you develop it, it’s a very bad situation, so whatever way you can achieve decompression may improve the situation,” said Dr. Rabinstein, a critical care neurologist who is also at the Mayo Clinic in Rochester. “If you don’t think the patient has enough left to merit the intervention, then you just don’t do it. But despite that limitation, if you think the patient can recover some function, it’s appropriate. An intervention will make patients survive way more often than no intervention. Without something, though, the prospect of survival is bleak.”
Neither Dr. Pagani-Estevez nor Dr. Rabinstein had any financial disclosures.
On Twitter @alz_gal
AT ANA 2014
Key clinical point: Decompression for a trapped ventricle can be a life-saving procedure.
Major finding: Mortality significantly declined from 70% in patients without decompression to 19% in those who underwent decompression via a variety of methods.
Data source: The retrospective study comprised 392 patients.
Disclosures: Neither Dr. Pagani-Estevez nor Dr. Rabinstein had any financial disclosures.
DeSalvo to stay involved in health IT work
Dr. Karen DeSalvo, recently named acting assistant secretary for health and charged with helping to form and run the federal government’s Ebola response efforts, will remain involved in a federal health information technology efforts as well.
Officials clarified on Oct. 29 that Dr. DeSalvo will continue to have a leadership role at the Office of the National Coordinator for Health Information Technology (ONC). Specifically, she will continue to chair the Health IT Policy Committee, lead the development and finalization of the Interoperability Roadmap, and remain involved in policymaking related to physicians’ meaningful use of electronic health records.
Lisa Lewis, who was named the Acting National Coordinator, will handle the day-to-day running of the ONC during Dr. DeSalvo’s “deployment” to the Office of the Assistant Secretary for Health, according to a blog post clarifying Dr. DeSalvo’s new role.
The news was welcomed by the American Medical Association, which had raised concerns that Dr. DeSalvo’s departure would create a “leadership gap” at a time when the ONC was tackling a number of important issues, from meaningful use of EHRs to interoperability of the systems.
“The AMA hopes Dr. DeSalvo’s continued presence will further advance efforts to improve the regulatory framework for health information technology and patient care,” Dr. Steven J. Stack, the AMA’s president-elect, said in a statement.
On Twitter @maryellenny
Dr. Karen DeSalvo, recently named acting assistant secretary for health and charged with helping to form and run the federal government’s Ebola response efforts, will remain involved in a federal health information technology efforts as well.
Officials clarified on Oct. 29 that Dr. DeSalvo will continue to have a leadership role at the Office of the National Coordinator for Health Information Technology (ONC). Specifically, she will continue to chair the Health IT Policy Committee, lead the development and finalization of the Interoperability Roadmap, and remain involved in policymaking related to physicians’ meaningful use of electronic health records.
Lisa Lewis, who was named the Acting National Coordinator, will handle the day-to-day running of the ONC during Dr. DeSalvo’s “deployment” to the Office of the Assistant Secretary for Health, according to a blog post clarifying Dr. DeSalvo’s new role.
The news was welcomed by the American Medical Association, which had raised concerns that Dr. DeSalvo’s departure would create a “leadership gap” at a time when the ONC was tackling a number of important issues, from meaningful use of EHRs to interoperability of the systems.
“The AMA hopes Dr. DeSalvo’s continued presence will further advance efforts to improve the regulatory framework for health information technology and patient care,” Dr. Steven J. Stack, the AMA’s president-elect, said in a statement.
On Twitter @maryellenny
Dr. Karen DeSalvo, recently named acting assistant secretary for health and charged with helping to form and run the federal government’s Ebola response efforts, will remain involved in a federal health information technology efforts as well.
Officials clarified on Oct. 29 that Dr. DeSalvo will continue to have a leadership role at the Office of the National Coordinator for Health Information Technology (ONC). Specifically, she will continue to chair the Health IT Policy Committee, lead the development and finalization of the Interoperability Roadmap, and remain involved in policymaking related to physicians’ meaningful use of electronic health records.
Lisa Lewis, who was named the Acting National Coordinator, will handle the day-to-day running of the ONC during Dr. DeSalvo’s “deployment” to the Office of the Assistant Secretary for Health, according to a blog post clarifying Dr. DeSalvo’s new role.
The news was welcomed by the American Medical Association, which had raised concerns that Dr. DeSalvo’s departure would create a “leadership gap” at a time when the ONC was tackling a number of important issues, from meaningful use of EHRs to interoperability of the systems.
“The AMA hopes Dr. DeSalvo’s continued presence will further advance efforts to improve the regulatory framework for health information technology and patient care,” Dr. Steven J. Stack, the AMA’s president-elect, said in a statement.
On Twitter @maryellenny
Lungs donated after cardiac arrest, brain death yield similar survival rates
AUSTIN, TEX. – The risk of death at 1 year after lung transplantation with organs donated either after cardiac arrest or after brain death was virtually the same, an analysis of the literature has shown.
“Donation after cardiac death appears to be a safe and effective method to expand the donor pool,” said Dr. Dustin Krutsinger of the University of Iowa, Iowa City, who presented the findings during the Hot Topics in Pulmonary Critical Care session at the annual meeting of the American College of Chest Physicians.
Over the years, the demand for organ donations for lung transplant candidates has steadily increased while the number of available organs has remained static. This is due, in part, to physicians being concerned about injury to the organs during the ischemic period, as well as what can often be as much as an hour before organ procurement after withdrawal of life support. However, Dr. Krutsinger said the similarities between the two cohorts could result from the fact that before procurement, systemic circulation allows the lungs to oxygenate by perfusion, and so there is less impact during the ischemic period.
“There is also a thought that the ischemic period might actually protect the lungs and the liver from reperfusion injury. And we’re avoiding brain death, which is not a completely benign state,” he told the audience.
After conducting an extensive review of the literature for 1-year survival rates post lung transplantation, the investigators found 519 unique citations, including 58 citations selected for full text review, 10 observational cohort studies for systematic review, and another 5 such studies for meta-analysis.
Dr. Krutsinger and his colleagues found no significant difference in 1-year survival rates between the donation after cardiac death and the donation after brain death cohorts (P = .658). In a pooled analysis of the five studies, no significant difference in risk of death was found at 1 year after either transplantation procedure (relative risk, 0.66; 95% confidence interval, 0.38-1.15; P = .15). Although he thought the findings were limited by shortcomings in the data, such as the fact that the study was a retrospective analysis of unmatched cohorts and that the follow-up period was short, Dr. Krutsinger said in an interview that he thought the data were compelling enough for institutions to begin rethinking organ procurement and transplantation protocols. In addition to his own study, he cited a 2013 study which he said indicated that if lungs donated after cardiac arrest were included, the pool of available organs would increase by as much as 50% (Ann. Am. Thorac. Soc. 2013;10:73-80).
But challenges remain.
“There are some things you can do to the potential donors that are questionable ethicswise, such as administering heparin premortem, which would be beneficial to the actual recipients. But, up until they are pronounced dead, they are still a patient. You don’t really have that complication with a donation after brain death, since once brain death is determined, the person is officially dead. Things you then do to them to benefit the eventual recipients aren’t being done to a ‘patient.’ ”
Still, Dr. Krutsinger said that if organs procured after cardiac arrest were to become more common than after brain death, he would be “disappointed” since the data showed “the outcomes are similar, not inferior.”
Dr. Krutsinger said he had no relevant disclosures.
On Twitter @whitneymcknight
AUSTIN, TEX. – The risk of death at 1 year after lung transplantation with organs donated either after cardiac arrest or after brain death was virtually the same, an analysis of the literature has shown.
“Donation after cardiac death appears to be a safe and effective method to expand the donor pool,” said Dr. Dustin Krutsinger of the University of Iowa, Iowa City, who presented the findings during the Hot Topics in Pulmonary Critical Care session at the annual meeting of the American College of Chest Physicians.
Over the years, the demand for organ donations for lung transplant candidates has steadily increased while the number of available organs has remained static. This is due, in part, to physicians being concerned about injury to the organs during the ischemic period, as well as what can often be as much as an hour before organ procurement after withdrawal of life support. However, Dr. Krutsinger said the similarities between the two cohorts could result from the fact that before procurement, systemic circulation allows the lungs to oxygenate by perfusion, and so there is less impact during the ischemic period.
“There is also a thought that the ischemic period might actually protect the lungs and the liver from reperfusion injury. And we’re avoiding brain death, which is not a completely benign state,” he told the audience.
After conducting an extensive review of the literature for 1-year survival rates post lung transplantation, the investigators found 519 unique citations, including 58 citations selected for full text review, 10 observational cohort studies for systematic review, and another 5 such studies for meta-analysis.
Dr. Krutsinger and his colleagues found no significant difference in 1-year survival rates between the donation after cardiac death and the donation after brain death cohorts (P = .658). In a pooled analysis of the five studies, no significant difference in risk of death was found at 1 year after either transplantation procedure (relative risk, 0.66; 95% confidence interval, 0.38-1.15; P = .15). Although he thought the findings were limited by shortcomings in the data, such as the fact that the study was a retrospective analysis of unmatched cohorts and that the follow-up period was short, Dr. Krutsinger said in an interview that he thought the data were compelling enough for institutions to begin rethinking organ procurement and transplantation protocols. In addition to his own study, he cited a 2013 study which he said indicated that if lungs donated after cardiac arrest were included, the pool of available organs would increase by as much as 50% (Ann. Am. Thorac. Soc. 2013;10:73-80).
But challenges remain.
“There are some things you can do to the potential donors that are questionable ethicswise, such as administering heparin premortem, which would be beneficial to the actual recipients. But, up until they are pronounced dead, they are still a patient. You don’t really have that complication with a donation after brain death, since once brain death is determined, the person is officially dead. Things you then do to them to benefit the eventual recipients aren’t being done to a ‘patient.’ ”
Still, Dr. Krutsinger said that if organs procured after cardiac arrest were to become more common than after brain death, he would be “disappointed” since the data showed “the outcomes are similar, not inferior.”
Dr. Krutsinger said he had no relevant disclosures.
On Twitter @whitneymcknight
AUSTIN, TEX. – The risk of death at 1 year after lung transplantation with organs donated either after cardiac arrest or after brain death was virtually the same, an analysis of the literature has shown.
“Donation after cardiac death appears to be a safe and effective method to expand the donor pool,” said Dr. Dustin Krutsinger of the University of Iowa, Iowa City, who presented the findings during the Hot Topics in Pulmonary Critical Care session at the annual meeting of the American College of Chest Physicians.
Over the years, the demand for organ donations for lung transplant candidates has steadily increased while the number of available organs has remained static. This is due, in part, to physicians being concerned about injury to the organs during the ischemic period, as well as what can often be as much as an hour before organ procurement after withdrawal of life support. However, Dr. Krutsinger said the similarities between the two cohorts could result from the fact that before procurement, systemic circulation allows the lungs to oxygenate by perfusion, and so there is less impact during the ischemic period.
“There is also a thought that the ischemic period might actually protect the lungs and the liver from reperfusion injury. And we’re avoiding brain death, which is not a completely benign state,” he told the audience.
After conducting an extensive review of the literature for 1-year survival rates post lung transplantation, the investigators found 519 unique citations, including 58 citations selected for full text review, 10 observational cohort studies for systematic review, and another 5 such studies for meta-analysis.
Dr. Krutsinger and his colleagues found no significant difference in 1-year survival rates between the donation after cardiac death and the donation after brain death cohorts (P = .658). In a pooled analysis of the five studies, no significant difference in risk of death was found at 1 year after either transplantation procedure (relative risk, 0.66; 95% confidence interval, 0.38-1.15; P = .15). Although he thought the findings were limited by shortcomings in the data, such as the fact that the study was a retrospective analysis of unmatched cohorts and that the follow-up period was short, Dr. Krutsinger said in an interview that he thought the data were compelling enough for institutions to begin rethinking organ procurement and transplantation protocols. In addition to his own study, he cited a 2013 study which he said indicated that if lungs donated after cardiac arrest were included, the pool of available organs would increase by as much as 50% (Ann. Am. Thorac. Soc. 2013;10:73-80).
But challenges remain.
“There are some things you can do to the potential donors that are questionable ethicswise, such as administering heparin premortem, which would be beneficial to the actual recipients. But, up until they are pronounced dead, they are still a patient. You don’t really have that complication with a donation after brain death, since once brain death is determined, the person is officially dead. Things you then do to them to benefit the eventual recipients aren’t being done to a ‘patient.’ ”
Still, Dr. Krutsinger said that if organs procured after cardiac arrest were to become more common than after brain death, he would be “disappointed” since the data showed “the outcomes are similar, not inferior.”
Dr. Krutsinger said he had no relevant disclosures.
On Twitter @whitneymcknight
AT CHEST 2014
Key clinical point: Expansion of organ donation programs to include organs donated after cardiac death could help meet a growing demand for donated lungs.
Major finding: No significant difference was seen in lung transplantation 1-year survival rates between donation after cardiac arrest and donation after brain death.
Data source: A systematic review of 10 observational cohort studies and a meta-analysis of 5 studies, chosen from more than 500 citations that included 1-year survival data for lung transplantation occuring after either cardiac arrest or brain death.
Disclosures: Dr. Krutsinger said he had no relevant disclosures.
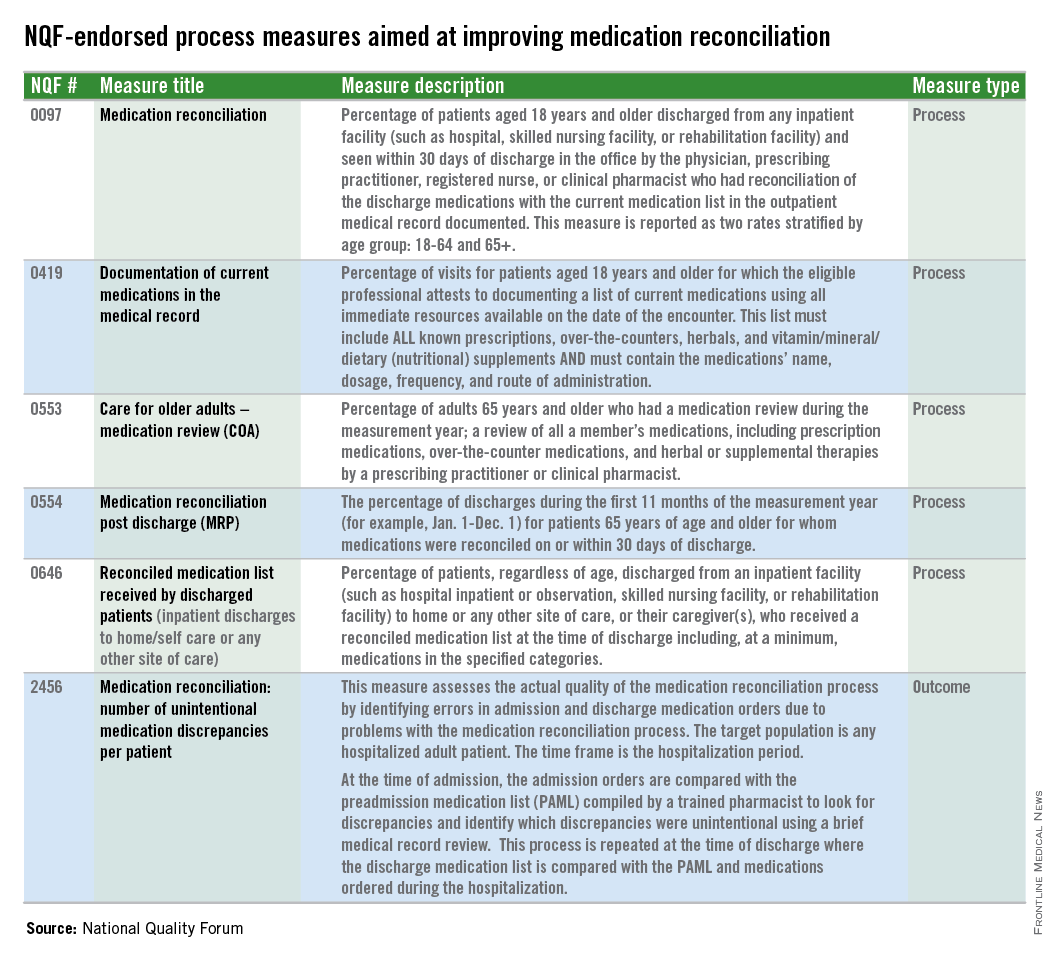
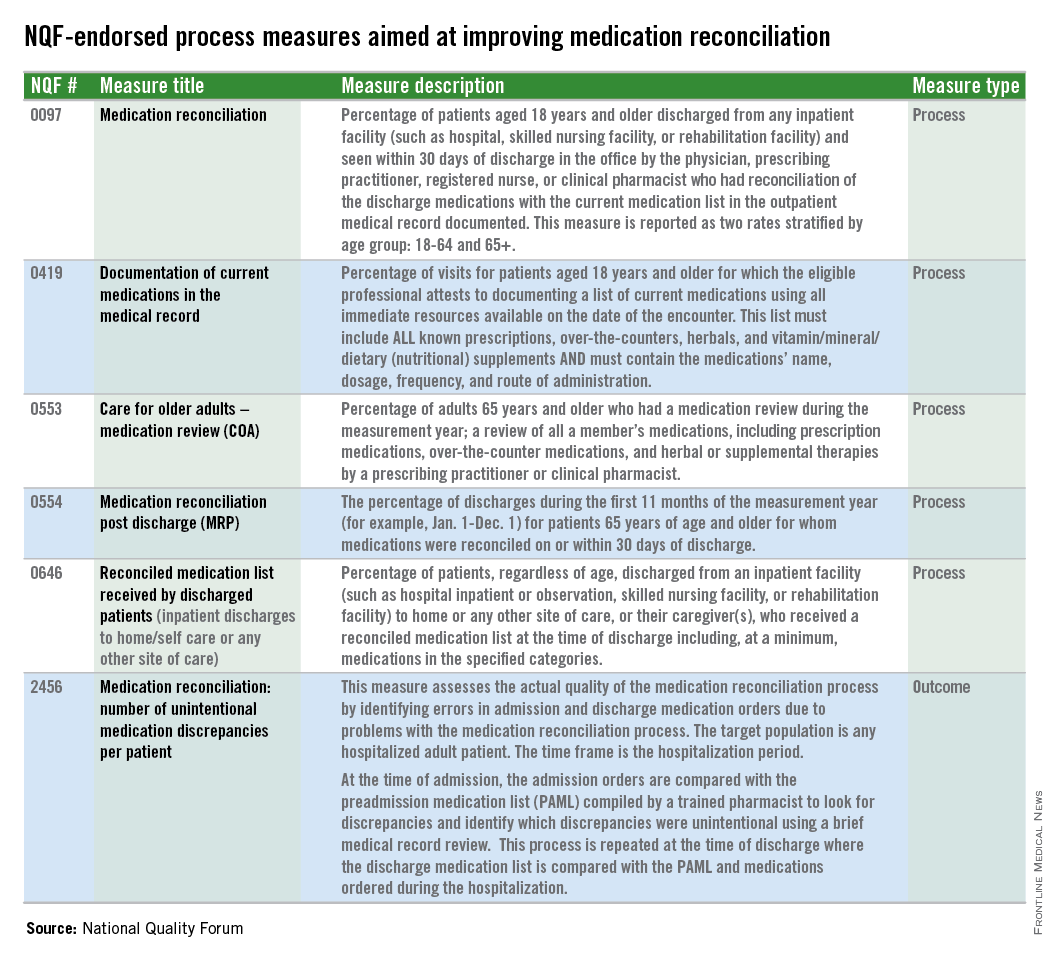
NQF endorses hospital medication reconciliation measure
Is a lax medication reconciliation process producing errors at your hospital? The National Quality Forum has endorsed a new quality measure aimed at identifying medication discrepancies and the process gaps that caused them. Measure #2456, officially endorsed by the NQF in September, assesses the quality of a hospital’s medication reconciliation process by identifying errors in admission and discharge orders. Here’s how it works: At the time of admission, hospital medication orders are compared with the preadmission medication list, which is compiled by a pharmacist. At discharge, the pharmacist repeats the process using both the preadmission list and any medications ordered during the hospitalization.
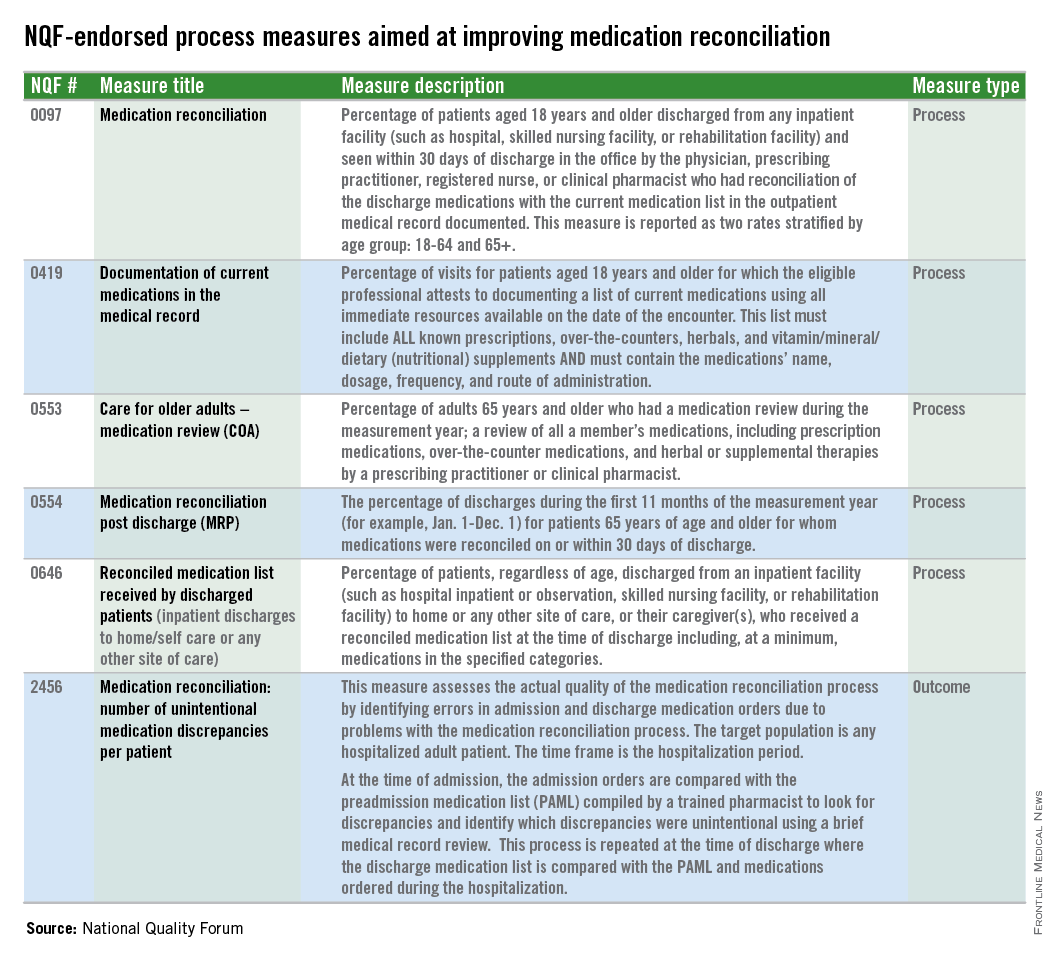
This type of review can help identify both history errors and reconciliation errors. History errors occur when a mistake in the history leads to an error in the medication order. For instance, if the clinical team in the hospital didn’t know a patient was on aspirin when they were admitted, they wouldn’t order it at admission.
If the history is correct, but the medication orders don’t match the preadmission medication list, that could be an intentional change by the care team or a reconciliation error.
The pharmacist can usually determine which one it is by reviewing the chart or consulting the care team, said Dr. Jeffrey L. Schnipper, a hospitalist at Brigham and Women’s Hospital in Boston, who proposed the new NQF measure.
The new measure joins five NQF-endorsed process measures aimed at improving medication reconciliation. But the new measure is the first outcome measure.
The Joint Commission also requires hospitals to engage in medication reconciliation, but that mandate is mostly pro forma, Dr. Schnipper said.
“It’s very much a process measure,” he said. “You say that you have a med rec process. You say that you’ve done med rec. Therefore, med rec is done. There really has been no national measure out there that looks at the actual quality of the med rec process you’re doing. Are you taking accurate medication histories and are you writing the correct orders based on those histories?”
Dr. Schnipper and his colleagues have been studying the issue of unintentional medication discrepancies for the last 5 years as part of the Multi-Center Medication Reconciliation Quality Improvement Study (MARQUIS). They found that there are about three unintentional medical discrepancies per patient on average, making reconciliation errors a larger source of medication errors than those caused by prescribing, transcribing, or administration. The error rate for potentially harmful medication discrepancies is about one-half per patient.
“There aren’t a whole lot of things out there where we tolerate a potentially harmful error in every other patient,” Dr. Schnipper said.
Hospitals won’t be required to take on the new measure right away. The measure will continue to be studied and tested over the next couple of years. But Dr. Schnipper said he’s hopeful that at the end of about 5 years, the measure could become part of some federal measurement programs, with financial incentives attached to performance on it.
One of the questions that still has to be studied is whether the measure will be adjusted for risk. More data will be available once the MARQUIS study is complete, Dr. Schnipper said, but early data suggests that it would need to be adjusted for patient age and the number of medications that a patient is taking.
Another question is whether hospitals will be evaluated based on the absolute number of medication discrepancies per patient or on their relative improvement over time. The final MARQUIS data are also expected to shed light on that issue.
Dr. Schnipper said he does not expect the new measure to be a drain on hospitals or physicians. As currently crafted, the measure would be used for about 22 patients per month and he estimates that it would take one full-time pharmacist or less to take a “gold standard” medication history and compare it with the preadmission and discharge medication lists. It would be no more labor intensive than the chart reviews undertaken by nurses to comply with the National Surgical Quality Improvement Program measures, he said.
Is a lax medication reconciliation process producing errors at your hospital? The National Quality Forum has endorsed a new quality measure aimed at identifying medication discrepancies and the process gaps that caused them. Measure #2456, officially endorsed by the NQF in September, assesses the quality of a hospital’s medication reconciliation process by identifying errors in admission and discharge orders. Here’s how it works: At the time of admission, hospital medication orders are compared with the preadmission medication list, which is compiled by a pharmacist. At discharge, the pharmacist repeats the process using both the preadmission list and any medications ordered during the hospitalization.
This type of review can help identify both history errors and reconciliation errors. History errors occur when a mistake in the history leads to an error in the medication order. For instance, if the clinical team in the hospital didn’t know a patient was on aspirin when they were admitted, they wouldn’t order it at admission.
If the history is correct, but the medication orders don’t match the preadmission medication list, that could be an intentional change by the care team or a reconciliation error.
The pharmacist can usually determine which one it is by reviewing the chart or consulting the care team, said Dr. Jeffrey L. Schnipper, a hospitalist at Brigham and Women’s Hospital in Boston, who proposed the new NQF measure.
The new measure joins five NQF-endorsed process measures aimed at improving medication reconciliation. But the new measure is the first outcome measure.
The Joint Commission also requires hospitals to engage in medication reconciliation, but that mandate is mostly pro forma, Dr. Schnipper said.
“It’s very much a process measure,” he said. “You say that you have a med rec process. You say that you’ve done med rec. Therefore, med rec is done. There really has been no national measure out there that looks at the actual quality of the med rec process you’re doing. Are you taking accurate medication histories and are you writing the correct orders based on those histories?”
Dr. Schnipper and his colleagues have been studying the issue of unintentional medication discrepancies for the last 5 years as part of the Multi-Center Medication Reconciliation Quality Improvement Study (MARQUIS). They found that there are about three unintentional medical discrepancies per patient on average, making reconciliation errors a larger source of medication errors than those caused by prescribing, transcribing, or administration. The error rate for potentially harmful medication discrepancies is about one-half per patient.
“There aren’t a whole lot of things out there where we tolerate a potentially harmful error in every other patient,” Dr. Schnipper said.
Hospitals won’t be required to take on the new measure right away. The measure will continue to be studied and tested over the next couple of years. But Dr. Schnipper said he’s hopeful that at the end of about 5 years, the measure could become part of some federal measurement programs, with financial incentives attached to performance on it.
One of the questions that still has to be studied is whether the measure will be adjusted for risk. More data will be available once the MARQUIS study is complete, Dr. Schnipper said, but early data suggests that it would need to be adjusted for patient age and the number of medications that a patient is taking.
Another question is whether hospitals will be evaluated based on the absolute number of medication discrepancies per patient or on their relative improvement over time. The final MARQUIS data are also expected to shed light on that issue.
Dr. Schnipper said he does not expect the new measure to be a drain on hospitals or physicians. As currently crafted, the measure would be used for about 22 patients per month and he estimates that it would take one full-time pharmacist or less to take a “gold standard” medication history and compare it with the preadmission and discharge medication lists. It would be no more labor intensive than the chart reviews undertaken by nurses to comply with the National Surgical Quality Improvement Program measures, he said.
Is a lax medication reconciliation process producing errors at your hospital? The National Quality Forum has endorsed a new quality measure aimed at identifying medication discrepancies and the process gaps that caused them. Measure #2456, officially endorsed by the NQF in September, assesses the quality of a hospital’s medication reconciliation process by identifying errors in admission and discharge orders. Here’s how it works: At the time of admission, hospital medication orders are compared with the preadmission medication list, which is compiled by a pharmacist. At discharge, the pharmacist repeats the process using both the preadmission list and any medications ordered during the hospitalization.
This type of review can help identify both history errors and reconciliation errors. History errors occur when a mistake in the history leads to an error in the medication order. For instance, if the clinical team in the hospital didn’t know a patient was on aspirin when they were admitted, they wouldn’t order it at admission.
If the history is correct, but the medication orders don’t match the preadmission medication list, that could be an intentional change by the care team or a reconciliation error.
The pharmacist can usually determine which one it is by reviewing the chart or consulting the care team, said Dr. Jeffrey L. Schnipper, a hospitalist at Brigham and Women’s Hospital in Boston, who proposed the new NQF measure.
The new measure joins five NQF-endorsed process measures aimed at improving medication reconciliation. But the new measure is the first outcome measure.
The Joint Commission also requires hospitals to engage in medication reconciliation, but that mandate is mostly pro forma, Dr. Schnipper said.
“It’s very much a process measure,” he said. “You say that you have a med rec process. You say that you’ve done med rec. Therefore, med rec is done. There really has been no national measure out there that looks at the actual quality of the med rec process you’re doing. Are you taking accurate medication histories and are you writing the correct orders based on those histories?”
Dr. Schnipper and his colleagues have been studying the issue of unintentional medication discrepancies for the last 5 years as part of the Multi-Center Medication Reconciliation Quality Improvement Study (MARQUIS). They found that there are about three unintentional medical discrepancies per patient on average, making reconciliation errors a larger source of medication errors than those caused by prescribing, transcribing, or administration. The error rate for potentially harmful medication discrepancies is about one-half per patient.
“There aren’t a whole lot of things out there where we tolerate a potentially harmful error in every other patient,” Dr. Schnipper said.
Hospitals won’t be required to take on the new measure right away. The measure will continue to be studied and tested over the next couple of years. But Dr. Schnipper said he’s hopeful that at the end of about 5 years, the measure could become part of some federal measurement programs, with financial incentives attached to performance on it.
One of the questions that still has to be studied is whether the measure will be adjusted for risk. More data will be available once the MARQUIS study is complete, Dr. Schnipper said, but early data suggests that it would need to be adjusted for patient age and the number of medications that a patient is taking.
Another question is whether hospitals will be evaluated based on the absolute number of medication discrepancies per patient or on their relative improvement over time. The final MARQUIS data are also expected to shed light on that issue.
Dr. Schnipper said he does not expect the new measure to be a drain on hospitals or physicians. As currently crafted, the measure would be used for about 22 patients per month and he estimates that it would take one full-time pharmacist or less to take a “gold standard” medication history and compare it with the preadmission and discharge medication lists. It would be no more labor intensive than the chart reviews undertaken by nurses to comply with the National Surgical Quality Improvement Program measures, he said.
DeSalvo leaves post to focus on Ebola response
Dr. Karen DeSalvo, who has served as National Coordinator for Health Information Technology for less than a year, is leaving her position to aid in public health efforts to contain Ebola in the United States.
On Oct. 23, the Office of the National Coordinator for Health IT (ONC) announced that effective immediately, Dr. DeSalvo would serve as acting assistant secretary for health at the Health and Human Services department.
Dr. DeSalvo will work with HHS Secretary Sylvia Burwell on “pressing public health issues, including becoming a part of the department’s team responding to Ebola,” according to Peter Ashkenaz, an ONC spokesman.
Lisa Lewis, ONC’s chief operating officer, will take the reins at ONC as acting national coordinator. But Dr. DeSalvo will continue to be available to the ONC team to support their work, Mr. Ashkenaz said.
Before coming to HHS, Dr. DeSalvo served as health commissioner for the City of New Orleans, where she helped modernize the city’s health department and helped establish a public hospital. Before working for the city, she was a professor of medicine and vice dean for community affairs and health policy at Tulane University, New Orleans.
On Twitter @maryellenny
Dr. Karen DeSalvo, who has served as National Coordinator for Health Information Technology for less than a year, is leaving her position to aid in public health efforts to contain Ebola in the United States.
On Oct. 23, the Office of the National Coordinator for Health IT (ONC) announced that effective immediately, Dr. DeSalvo would serve as acting assistant secretary for health at the Health and Human Services department.
Dr. DeSalvo will work with HHS Secretary Sylvia Burwell on “pressing public health issues, including becoming a part of the department’s team responding to Ebola,” according to Peter Ashkenaz, an ONC spokesman.
Lisa Lewis, ONC’s chief operating officer, will take the reins at ONC as acting national coordinator. But Dr. DeSalvo will continue to be available to the ONC team to support their work, Mr. Ashkenaz said.
Before coming to HHS, Dr. DeSalvo served as health commissioner for the City of New Orleans, where she helped modernize the city’s health department and helped establish a public hospital. Before working for the city, she was a professor of medicine and vice dean for community affairs and health policy at Tulane University, New Orleans.
On Twitter @maryellenny
Dr. Karen DeSalvo, who has served as National Coordinator for Health Information Technology for less than a year, is leaving her position to aid in public health efforts to contain Ebola in the United States.
On Oct. 23, the Office of the National Coordinator for Health IT (ONC) announced that effective immediately, Dr. DeSalvo would serve as acting assistant secretary for health at the Health and Human Services department.
Dr. DeSalvo will work with HHS Secretary Sylvia Burwell on “pressing public health issues, including becoming a part of the department’s team responding to Ebola,” according to Peter Ashkenaz, an ONC spokesman.
Lisa Lewis, ONC’s chief operating officer, will take the reins at ONC as acting national coordinator. But Dr. DeSalvo will continue to be available to the ONC team to support their work, Mr. Ashkenaz said.
Before coming to HHS, Dr. DeSalvo served as health commissioner for the City of New Orleans, where she helped modernize the city’s health department and helped establish a public hospital. Before working for the city, she was a professor of medicine and vice dean for community affairs and health policy at Tulane University, New Orleans.
On Twitter @maryellenny
Regurgitation controlled by transoral fundoplication
PHILADELPHIA – The first trial conducted in gastroesophageal reflux diseases that employed control of regurgitation as a primary endpoint found a significant advantage for transoral fundoplication over a sham procedure, according to the results presented at the American College of Gastroenterology (ACG).
On the basis of these results “TF [transoral fundoplication] should be considered in GERD [gastroesophageal reflux disease] patients with small or absent hiatal hernia who suffer from troublesome regurgitation despite PPI therapy,” reported Dr. Peter J. Kahrilas, the Gilbert H. Marquardt Professor of Medicine, a professor of medicine, gastroenterology, and hepatology, at Northwestern University, Chicago*.
The focus on regurgitation in this trial was partially driven by the lack of previous evidence for an effective therapy. In those trials that have included change in regurgitation among secondary endpoints, Dr. Kahrilas said control on this symptom has typically been “significantly less” than that observed with heartburn.
In this study, called RESPECT, 129 patients were randomized in a 2:1 ratio to TF performed with the Esophyx device or to a sham procedure. Both groups were initiated on a standard dose of proton pump inhibitors (PPIs), but PPIs were discontinued in the TF arm 2 weeks after the procedure. In the sham group, an increase in PPI dose was permitted at the 2-week and 12-week assessments in those not already at the maximum double the standard dose limit.
The primary endpoint was elimination of troublesome regurgitation based on the regurgitation-related fields from the Reflux Disease Questionnaire (RDQ), which is a validated tool for GERD assessment. On this basis, symptoms at the final 26-week assessment had resolved in 67% of patients randomized to TF and 25% (P = .023) randomized to the sham procedure. Early failure rates were also significantly lower in the TF group (11% vs. 36%; P = .002).
Intraesophageal acid levels assessed with 48-hour pH monitoring at the end of the study “were improved but not normalized in the TF group and unchanged in the sham group,” Dr. Kahrilas reported.
Adverse events, although more common in the TF group, were infrequent in both arms, and none were serious. Summarizing risk of adverse events, Dr. Kahrilas said, “TF appears safe without typical fundoplication side effects.”
The specific mechanism of benefit for controlling regurgitation has not been defined, but Dr. Kahrilas suggested, “We think we are restricting the volume of reflux.”
Regurgitation is “the ignored symptom of GERD,” according to Dr. Kahrilas. Although this symptom can be significant to patients, clinicians have had limited treatment options.
This point was emphasized by Dr. Nicholas Shaheen, director, Center for Esophageal Diseases and Swallowing, University of North Carolina, Chapel Hill. In an interview, Dr. Shaheen said effective therapy for regurgitation is an unmet need.
“Patients with predominant regurgitation are not uncommon and PPIs do appear to be less effective for this symptom,” Dr. Shaheen reported. “Having a treatment option with efficacy specific for this symptom could be helpful.”
Dr. Peter Kahrilas has numerous financial relationships with pharmaceutical companies including EndoGastric, the sponsor of this trial.
*Correction, 10/27/2014: An earlier version of this article misstated Dr. Kahrilas' position.
PHILADELPHIA – The first trial conducted in gastroesophageal reflux diseases that employed control of regurgitation as a primary endpoint found a significant advantage for transoral fundoplication over a sham procedure, according to the results presented at the American College of Gastroenterology (ACG).
On the basis of these results “TF [transoral fundoplication] should be considered in GERD [gastroesophageal reflux disease] patients with small or absent hiatal hernia who suffer from troublesome regurgitation despite PPI therapy,” reported Dr. Peter J. Kahrilas, the Gilbert H. Marquardt Professor of Medicine, a professor of medicine, gastroenterology, and hepatology, at Northwestern University, Chicago*.
The focus on regurgitation in this trial was partially driven by the lack of previous evidence for an effective therapy. In those trials that have included change in regurgitation among secondary endpoints, Dr. Kahrilas said control on this symptom has typically been “significantly less” than that observed with heartburn.
In this study, called RESPECT, 129 patients were randomized in a 2:1 ratio to TF performed with the Esophyx device or to a sham procedure. Both groups were initiated on a standard dose of proton pump inhibitors (PPIs), but PPIs were discontinued in the TF arm 2 weeks after the procedure. In the sham group, an increase in PPI dose was permitted at the 2-week and 12-week assessments in those not already at the maximum double the standard dose limit.
The primary endpoint was elimination of troublesome regurgitation based on the regurgitation-related fields from the Reflux Disease Questionnaire (RDQ), which is a validated tool for GERD assessment. On this basis, symptoms at the final 26-week assessment had resolved in 67% of patients randomized to TF and 25% (P = .023) randomized to the sham procedure. Early failure rates were also significantly lower in the TF group (11% vs. 36%; P = .002).
Intraesophageal acid levels assessed with 48-hour pH monitoring at the end of the study “were improved but not normalized in the TF group and unchanged in the sham group,” Dr. Kahrilas reported.
Adverse events, although more common in the TF group, were infrequent in both arms, and none were serious. Summarizing risk of adverse events, Dr. Kahrilas said, “TF appears safe without typical fundoplication side effects.”
The specific mechanism of benefit for controlling regurgitation has not been defined, but Dr. Kahrilas suggested, “We think we are restricting the volume of reflux.”
Regurgitation is “the ignored symptom of GERD,” according to Dr. Kahrilas. Although this symptom can be significant to patients, clinicians have had limited treatment options.
This point was emphasized by Dr. Nicholas Shaheen, director, Center for Esophageal Diseases and Swallowing, University of North Carolina, Chapel Hill. In an interview, Dr. Shaheen said effective therapy for regurgitation is an unmet need.
“Patients with predominant regurgitation are not uncommon and PPIs do appear to be less effective for this symptom,” Dr. Shaheen reported. “Having a treatment option with efficacy specific for this symptom could be helpful.”
Dr. Peter Kahrilas has numerous financial relationships with pharmaceutical companies including EndoGastric, the sponsor of this trial.
*Correction, 10/27/2014: An earlier version of this article misstated Dr. Kahrilas' position.
PHILADELPHIA – The first trial conducted in gastroesophageal reflux diseases that employed control of regurgitation as a primary endpoint found a significant advantage for transoral fundoplication over a sham procedure, according to the results presented at the American College of Gastroenterology (ACG).
On the basis of these results “TF [transoral fundoplication] should be considered in GERD [gastroesophageal reflux disease] patients with small or absent hiatal hernia who suffer from troublesome regurgitation despite PPI therapy,” reported Dr. Peter J. Kahrilas, the Gilbert H. Marquardt Professor of Medicine, a professor of medicine, gastroenterology, and hepatology, at Northwestern University, Chicago*.
The focus on regurgitation in this trial was partially driven by the lack of previous evidence for an effective therapy. In those trials that have included change in regurgitation among secondary endpoints, Dr. Kahrilas said control on this symptom has typically been “significantly less” than that observed with heartburn.
In this study, called RESPECT, 129 patients were randomized in a 2:1 ratio to TF performed with the Esophyx device or to a sham procedure. Both groups were initiated on a standard dose of proton pump inhibitors (PPIs), but PPIs were discontinued in the TF arm 2 weeks after the procedure. In the sham group, an increase in PPI dose was permitted at the 2-week and 12-week assessments in those not already at the maximum double the standard dose limit.
The primary endpoint was elimination of troublesome regurgitation based on the regurgitation-related fields from the Reflux Disease Questionnaire (RDQ), which is a validated tool for GERD assessment. On this basis, symptoms at the final 26-week assessment had resolved in 67% of patients randomized to TF and 25% (P = .023) randomized to the sham procedure. Early failure rates were also significantly lower in the TF group (11% vs. 36%; P = .002).
Intraesophageal acid levels assessed with 48-hour pH monitoring at the end of the study “were improved but not normalized in the TF group and unchanged in the sham group,” Dr. Kahrilas reported.
Adverse events, although more common in the TF group, were infrequent in both arms, and none were serious. Summarizing risk of adverse events, Dr. Kahrilas said, “TF appears safe without typical fundoplication side effects.”
The specific mechanism of benefit for controlling regurgitation has not been defined, but Dr. Kahrilas suggested, “We think we are restricting the volume of reflux.”
Regurgitation is “the ignored symptom of GERD,” according to Dr. Kahrilas. Although this symptom can be significant to patients, clinicians have had limited treatment options.
This point was emphasized by Dr. Nicholas Shaheen, director, Center for Esophageal Diseases and Swallowing, University of North Carolina, Chapel Hill. In an interview, Dr. Shaheen said effective therapy for regurgitation is an unmet need.
“Patients with predominant regurgitation are not uncommon and PPIs do appear to be less effective for this symptom,” Dr. Shaheen reported. “Having a treatment option with efficacy specific for this symptom could be helpful.”
Dr. Peter Kahrilas has numerous financial relationships with pharmaceutical companies including EndoGastric, the sponsor of this trial.
*Correction, 10/27/2014: An earlier version of this article misstated Dr. Kahrilas' position.
ANNUAL SCIENTIFIC MEETING AND POSTGRADUATE COURSE OF THE AMERICAN COLLEGE OF GASTROENTEROLOGY
Key clinical point: In patients with gastroesophageal reflux disease (GERD), transoral fundoplication (TF) is effective for controlling the specific complaint of regurgitation uncontrolled with proton pump inhibitors.
Major finding: At 6 months, troublesome regurgitation was eliminated in 67% of GERD patients undergoing TF vs. 25% (P = .023) in those randomized to a sham procedure.
Data source: Prospective, multicenter, randomized, controlled trial.
Disclosures: Dr. Peter Kahrilas has numerous financial relationships with pharmaceutical companies including EndoGastric, the sponsor of this trial.
Incidence of cranial nerve injury after CEA is low
CORONADO, CALIF. – Cranial nerve injury occurred in 4.6% of patients who participated in the Carotid Revascularization Endarterectomy versus Stenting Trial (CREST), with 34% resolution at 1 month and 80.8% at 1 year, a detailed analysis demonstrated.
While cranial nerve injury (CNI) is the most common neurologic complication of carotid endarterectomy, its reported incidence “is highly variable, ranging from 3% to 30% and depends on the intensity and the methods that are used for evaluation,” Dr. Robert J. Hye said at the annual meeting of the Western Vascular Society. “When using clinical criteria as in CREST, the incidence varies from 5% to 8%, and most injuries resolve in a few weeks. But in rare cases it can result in significant long-term disability.”
Most publications that have evaluated CNI discuss the frequency of nerve injury, not resolution or the time to healing. “Previous publications have identified prolonged operations, urgent operations, and re-exploration as predictors of CNI,” said Dr. Hye of the department of general and vascular surgery at Kaiser Permanente, San Diego. “Advocates of CAS [carotid artery stenting] have equated CNI with minor stroke, mitigating some of the benefit of CEA over CAS.”
He and his associates conducted the present study in an effort to evaluate the incidence, predictive factors, and resolution and also to compare health-related quality of life in patients with and without CNI in CREST, a trial conducted at 117 centers in the United States and Canada in which 2,502 patients were randomized to receive either CAS or CEA. Researchers in that trial observed no difference in outcome in the combined primary endpoint of stroke, MI, and death, but periprocedural stroke was significantly more common in the CAS group and periprocedural MI in the CEA group. Quality of life analyses were performed at 2 weeks, 1 month, and 12 months after the interventions (N. Engl. J. Med. 2010;363:11-23).
For the current analysis, patients with CNI were identified from the CREST database and classified using case report forms, adverse event reports, and clinical follow-up notes. Adjudication of the CNIs was performed by two neurologists and one vascular surgeon. Patients with only cutaneous sensory symptoms were excluded from analysis, and postprocedural outcomes were assessed at 30 days and 12 months. The researchers used the SF-36 and disease-specific Likert scales to measure health-related quality of life.
The mean age of patients at baseline was 68 years. Dr. Hye reported that CNI occurred in 53 of 1,151 (4.6%) randomized to CEA who received their operation within 30 days. CNIs were also noted in five additional patients: three who crossed over from CAS to CEA and two who did not undergo CEA within 30 days of randomization. In contrast to prior studies, CNI was significantly more common when general anesthesia was used, but there were no other demographic or procedural characteristics that were predictive of CNI. About one-third of CNIs (34%) were resolved at 30 days, and 80.8% were resolved at 1 year. CNI had a small effect on quality of life, negatively impacting only swallowing and eating at 2 and 4 weeks but not at 1 year (P less than .001).
Injuries to cranial nerves IX and X were most common, followed by injuries to the marginal mandibular branch of the facial nerve and the hypoglossal nerves. All of the hypoglossal injuries resolved, while injuries involving cranial nerves IX and X were least likely to resolve.
Dr. Hye acknowledged certain limitations of the trial, including the fact that CNI diagnosis was made from a clinical standpoint, and there were no routine otolaryngologic exams. “It’s likely that some of the subtle injuries were missed and that the incidence of cranial nerve injury is underestimated,” he added. “On the other hand, patients did have postoperative exams by experienced neurologists and vascular surgeons, so not many of the injuries should have been missed. Another unique thing about the study is the [quality of life] tools [we used]. They may be insufficiently sensitive to detect the consequences of CNI.”
Dr. Hye went on to note that the persistence of CNI at 1 year in CREST is higher than in most other reports available in the medical literature (19.2% vs. 7%-12%, respectively). “We’re not really sure why this is the case,” he said. “It may be that the postoperative assessment in CREST was more detailed and detected more subtle residual deficits from the CNIs.”
The study was funded by the National Institutes of Health, with supplemental funding from Abbott Vascular Inc. Dr. Hye reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – Cranial nerve injury occurred in 4.6% of patients who participated in the Carotid Revascularization Endarterectomy versus Stenting Trial (CREST), with 34% resolution at 1 month and 80.8% at 1 year, a detailed analysis demonstrated.
While cranial nerve injury (CNI) is the most common neurologic complication of carotid endarterectomy, its reported incidence “is highly variable, ranging from 3% to 30% and depends on the intensity and the methods that are used for evaluation,” Dr. Robert J. Hye said at the annual meeting of the Western Vascular Society. “When using clinical criteria as in CREST, the incidence varies from 5% to 8%, and most injuries resolve in a few weeks. But in rare cases it can result in significant long-term disability.”
Most publications that have evaluated CNI discuss the frequency of nerve injury, not resolution or the time to healing. “Previous publications have identified prolonged operations, urgent operations, and re-exploration as predictors of CNI,” said Dr. Hye of the department of general and vascular surgery at Kaiser Permanente, San Diego. “Advocates of CAS [carotid artery stenting] have equated CNI with minor stroke, mitigating some of the benefit of CEA over CAS.”
He and his associates conducted the present study in an effort to evaluate the incidence, predictive factors, and resolution and also to compare health-related quality of life in patients with and without CNI in CREST, a trial conducted at 117 centers in the United States and Canada in which 2,502 patients were randomized to receive either CAS or CEA. Researchers in that trial observed no difference in outcome in the combined primary endpoint of stroke, MI, and death, but periprocedural stroke was significantly more common in the CAS group and periprocedural MI in the CEA group. Quality of life analyses were performed at 2 weeks, 1 month, and 12 months after the interventions (N. Engl. J. Med. 2010;363:11-23).
For the current analysis, patients with CNI were identified from the CREST database and classified using case report forms, adverse event reports, and clinical follow-up notes. Adjudication of the CNIs was performed by two neurologists and one vascular surgeon. Patients with only cutaneous sensory symptoms were excluded from analysis, and postprocedural outcomes were assessed at 30 days and 12 months. The researchers used the SF-36 and disease-specific Likert scales to measure health-related quality of life.
The mean age of patients at baseline was 68 years. Dr. Hye reported that CNI occurred in 53 of 1,151 (4.6%) randomized to CEA who received their operation within 30 days. CNIs were also noted in five additional patients: three who crossed over from CAS to CEA and two who did not undergo CEA within 30 days of randomization. In contrast to prior studies, CNI was significantly more common when general anesthesia was used, but there were no other demographic or procedural characteristics that were predictive of CNI. About one-third of CNIs (34%) were resolved at 30 days, and 80.8% were resolved at 1 year. CNI had a small effect on quality of life, negatively impacting only swallowing and eating at 2 and 4 weeks but not at 1 year (P less than .001).
Injuries to cranial nerves IX and X were most common, followed by injuries to the marginal mandibular branch of the facial nerve and the hypoglossal nerves. All of the hypoglossal injuries resolved, while injuries involving cranial nerves IX and X were least likely to resolve.
Dr. Hye acknowledged certain limitations of the trial, including the fact that CNI diagnosis was made from a clinical standpoint, and there were no routine otolaryngologic exams. “It’s likely that some of the subtle injuries were missed and that the incidence of cranial nerve injury is underestimated,” he added. “On the other hand, patients did have postoperative exams by experienced neurologists and vascular surgeons, so not many of the injuries should have been missed. Another unique thing about the study is the [quality of life] tools [we used]. They may be insufficiently sensitive to detect the consequences of CNI.”
Dr. Hye went on to note that the persistence of CNI at 1 year in CREST is higher than in most other reports available in the medical literature (19.2% vs. 7%-12%, respectively). “We’re not really sure why this is the case,” he said. “It may be that the postoperative assessment in CREST was more detailed and detected more subtle residual deficits from the CNIs.”
The study was funded by the National Institutes of Health, with supplemental funding from Abbott Vascular Inc. Dr. Hye reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – Cranial nerve injury occurred in 4.6% of patients who participated in the Carotid Revascularization Endarterectomy versus Stenting Trial (CREST), with 34% resolution at 1 month and 80.8% at 1 year, a detailed analysis demonstrated.
While cranial nerve injury (CNI) is the most common neurologic complication of carotid endarterectomy, its reported incidence “is highly variable, ranging from 3% to 30% and depends on the intensity and the methods that are used for evaluation,” Dr. Robert J. Hye said at the annual meeting of the Western Vascular Society. “When using clinical criteria as in CREST, the incidence varies from 5% to 8%, and most injuries resolve in a few weeks. But in rare cases it can result in significant long-term disability.”
Most publications that have evaluated CNI discuss the frequency of nerve injury, not resolution or the time to healing. “Previous publications have identified prolonged operations, urgent operations, and re-exploration as predictors of CNI,” said Dr. Hye of the department of general and vascular surgery at Kaiser Permanente, San Diego. “Advocates of CAS [carotid artery stenting] have equated CNI with minor stroke, mitigating some of the benefit of CEA over CAS.”
He and his associates conducted the present study in an effort to evaluate the incidence, predictive factors, and resolution and also to compare health-related quality of life in patients with and without CNI in CREST, a trial conducted at 117 centers in the United States and Canada in which 2,502 patients were randomized to receive either CAS or CEA. Researchers in that trial observed no difference in outcome in the combined primary endpoint of stroke, MI, and death, but periprocedural stroke was significantly more common in the CAS group and periprocedural MI in the CEA group. Quality of life analyses were performed at 2 weeks, 1 month, and 12 months after the interventions (N. Engl. J. Med. 2010;363:11-23).
For the current analysis, patients with CNI were identified from the CREST database and classified using case report forms, adverse event reports, and clinical follow-up notes. Adjudication of the CNIs was performed by two neurologists and one vascular surgeon. Patients with only cutaneous sensory symptoms were excluded from analysis, and postprocedural outcomes were assessed at 30 days and 12 months. The researchers used the SF-36 and disease-specific Likert scales to measure health-related quality of life.
The mean age of patients at baseline was 68 years. Dr. Hye reported that CNI occurred in 53 of 1,151 (4.6%) randomized to CEA who received their operation within 30 days. CNIs were also noted in five additional patients: three who crossed over from CAS to CEA and two who did not undergo CEA within 30 days of randomization. In contrast to prior studies, CNI was significantly more common when general anesthesia was used, but there were no other demographic or procedural characteristics that were predictive of CNI. About one-third of CNIs (34%) were resolved at 30 days, and 80.8% were resolved at 1 year. CNI had a small effect on quality of life, negatively impacting only swallowing and eating at 2 and 4 weeks but not at 1 year (P less than .001).
Injuries to cranial nerves IX and X were most common, followed by injuries to the marginal mandibular branch of the facial nerve and the hypoglossal nerves. All of the hypoglossal injuries resolved, while injuries involving cranial nerves IX and X were least likely to resolve.
Dr. Hye acknowledged certain limitations of the trial, including the fact that CNI diagnosis was made from a clinical standpoint, and there were no routine otolaryngologic exams. “It’s likely that some of the subtle injuries were missed and that the incidence of cranial nerve injury is underestimated,” he added. “On the other hand, patients did have postoperative exams by experienced neurologists and vascular surgeons, so not many of the injuries should have been missed. Another unique thing about the study is the [quality of life] tools [we used]. They may be insufficiently sensitive to detect the consequences of CNI.”
Dr. Hye went on to note that the persistence of CNI at 1 year in CREST is higher than in most other reports available in the medical literature (19.2% vs. 7%-12%, respectively). “We’re not really sure why this is the case,” he said. “It may be that the postoperative assessment in CREST was more detailed and detected more subtle residual deficits from the CNIs.”
The study was funded by the National Institutes of Health, with supplemental funding from Abbott Vascular Inc. Dr. Hye reported having no financial disclosures.
On Twitter @dougbrunk
AT THE WESTERN VASCULAR SOCIETY ANNUAL MEETING
Key clinical point: Cranial nerve injury occurred in fewer than 5% of patients undergoing carotid endarterectomy.
Major finding: About one-third of CNIs sustained by patients who underwent CEA resolved within 30 days (34%), and 80.8% resolved at 1 year.
Data source: An analysis of 1,151 patients who were randomized to carotid revascularization endarterectomy in the Carotid Revascularization Endarterectomy versus Stenting Trial (CREST).
Disclosures: The study was funded by the National Institutes of Health, with supplemental funding from Abbott Vascular Inc. Dr. Hye reported having no financial disclosures.
Uncomplicated diverticulitis patients safely avoid routine antibiotics
VIENNA – Patients with first-episode, uncomplicated diverticulitis can safely be managed by observation alone without routine antibiotic treatment, based on results from a prospective, controlled, multicenter Dutch trial with 528 patients.
Coupled with similar results from a 2012 Swedish randomized trial, the new findings show that an observational approach without up-front antibiotic treatment is safe and effective for routine practice for patients with a modified Hinchey stage 1 classification, the most common diverticulitis presentation, Dr. Lidewine Daniels said at the United European Gastroenterology Global Congress.
The 2012 trial, done in Sweden and Iceland, randomized 623 patients with acute, uncomplicated diverticulitis, and found no statistically significant difference in the rate of recovery without complications during 12 months of follow-up, regardless of whether or not patients received routine antibiotic treatment at the time of initial diagnosis (Br. J. Surg. 2012;99:532-9).
This approach “can now be adopted into guidelines,” said Dr. Daniels, a researcher in the surgery department at the Academic Medical Center in Amsterdam. This would shift current practice recommendations, such as those published earlier this year by the American College of Colon and Rectal Surgeons (Dis. Colon Rectum 2014;57:284-94), which have generally called for routine antibiotic management of these types of diverticulitis patients, Dr. Daniels said.
The DIABOLO (Multicenter Randomized Clinical Trial Investigating the Cost-effectiveness of Treatment Strategies With or Without Antibiotics for Uncomplicated Acute Diverticulitis) trial enrolled patients with CT-proven, left-sided, first-episode, uncomplicated diverticulitis at 22 Dutch centers. All patients were classified as having stage 1 disease by the modified Hinchey criteria (Int. J. Colorectal Dis. 2012;27:207-14), with about 92% of patients classified as Hinchey 1a.
The 266 patients randomized to initial antibiotic treatment began at least 2 days on intravenous treatment with amoxicillin and clavulanic acid, followed by a switch to oral delivery of the same combination when appropriate for a total of 10 days on the antibiotic.
Patients remained hospitalized until they switched from intravenous to oral treatment. The 262 patients randomized to no initial antibiotic treatment were hospitalized and observed, and received supportive treatment until they were judged ready for discharge by being able to eat a normal diet, had a temperature of less than 38 °C, and had a self-rated pain score of less than 4 on a visual analog scale of 0-10 without use of pain medication; in addition, the patient’s agreement was needed for discharge.
During 6 months of follow-up, the median time to complete recovery – defined as the criteria for hospital discharge plus a return to normal activity – occurred after a median of 12 days among patients in the antibiotic group and 14 days among those in the observation group, a difference that was not statistically significant for the study’s primary endpoint.
The results also showed no statistically significant differences between the two study arms for almost all the other outcomes assessed, including need for readmission, complications, need for surgery, morbidities, serious morbidities, and deaths. The only significant differences in outcomes were a decreased rate of hospitalization at the time of initial treatment among patients in the observation-only arm, and fewer hospitalized days among the observation-only patients.
“Observational treatment is without short- or long-term repercussions,” Dr. Daniels concluded.
Dr. Daniels had no disclosures.
On Twitter @mitchelzoler
VIENNA – Patients with first-episode, uncomplicated diverticulitis can safely be managed by observation alone without routine antibiotic treatment, based on results from a prospective, controlled, multicenter Dutch trial with 528 patients.
Coupled with similar results from a 2012 Swedish randomized trial, the new findings show that an observational approach without up-front antibiotic treatment is safe and effective for routine practice for patients with a modified Hinchey stage 1 classification, the most common diverticulitis presentation, Dr. Lidewine Daniels said at the United European Gastroenterology Global Congress.
The 2012 trial, done in Sweden and Iceland, randomized 623 patients with acute, uncomplicated diverticulitis, and found no statistically significant difference in the rate of recovery without complications during 12 months of follow-up, regardless of whether or not patients received routine antibiotic treatment at the time of initial diagnosis (Br. J. Surg. 2012;99:532-9).
This approach “can now be adopted into guidelines,” said Dr. Daniels, a researcher in the surgery department at the Academic Medical Center in Amsterdam. This would shift current practice recommendations, such as those published earlier this year by the American College of Colon and Rectal Surgeons (Dis. Colon Rectum 2014;57:284-94), which have generally called for routine antibiotic management of these types of diverticulitis patients, Dr. Daniels said.
The DIABOLO (Multicenter Randomized Clinical Trial Investigating the Cost-effectiveness of Treatment Strategies With or Without Antibiotics for Uncomplicated Acute Diverticulitis) trial enrolled patients with CT-proven, left-sided, first-episode, uncomplicated diverticulitis at 22 Dutch centers. All patients were classified as having stage 1 disease by the modified Hinchey criteria (Int. J. Colorectal Dis. 2012;27:207-14), with about 92% of patients classified as Hinchey 1a.
The 266 patients randomized to initial antibiotic treatment began at least 2 days on intravenous treatment with amoxicillin and clavulanic acid, followed by a switch to oral delivery of the same combination when appropriate for a total of 10 days on the antibiotic.
Patients remained hospitalized until they switched from intravenous to oral treatment. The 262 patients randomized to no initial antibiotic treatment were hospitalized and observed, and received supportive treatment until they were judged ready for discharge by being able to eat a normal diet, had a temperature of less than 38 °C, and had a self-rated pain score of less than 4 on a visual analog scale of 0-10 without use of pain medication; in addition, the patient’s agreement was needed for discharge.
During 6 months of follow-up, the median time to complete recovery – defined as the criteria for hospital discharge plus a return to normal activity – occurred after a median of 12 days among patients in the antibiotic group and 14 days among those in the observation group, a difference that was not statistically significant for the study’s primary endpoint.
The results also showed no statistically significant differences between the two study arms for almost all the other outcomes assessed, including need for readmission, complications, need for surgery, morbidities, serious morbidities, and deaths. The only significant differences in outcomes were a decreased rate of hospitalization at the time of initial treatment among patients in the observation-only arm, and fewer hospitalized days among the observation-only patients.
“Observational treatment is without short- or long-term repercussions,” Dr. Daniels concluded.
Dr. Daniels had no disclosures.
On Twitter @mitchelzoler
VIENNA – Patients with first-episode, uncomplicated diverticulitis can safely be managed by observation alone without routine antibiotic treatment, based on results from a prospective, controlled, multicenter Dutch trial with 528 patients.
Coupled with similar results from a 2012 Swedish randomized trial, the new findings show that an observational approach without up-front antibiotic treatment is safe and effective for routine practice for patients with a modified Hinchey stage 1 classification, the most common diverticulitis presentation, Dr. Lidewine Daniels said at the United European Gastroenterology Global Congress.
The 2012 trial, done in Sweden and Iceland, randomized 623 patients with acute, uncomplicated diverticulitis, and found no statistically significant difference in the rate of recovery without complications during 12 months of follow-up, regardless of whether or not patients received routine antibiotic treatment at the time of initial diagnosis (Br. J. Surg. 2012;99:532-9).
This approach “can now be adopted into guidelines,” said Dr. Daniels, a researcher in the surgery department at the Academic Medical Center in Amsterdam. This would shift current practice recommendations, such as those published earlier this year by the American College of Colon and Rectal Surgeons (Dis. Colon Rectum 2014;57:284-94), which have generally called for routine antibiotic management of these types of diverticulitis patients, Dr. Daniels said.
The DIABOLO (Multicenter Randomized Clinical Trial Investigating the Cost-effectiveness of Treatment Strategies With or Without Antibiotics for Uncomplicated Acute Diverticulitis) trial enrolled patients with CT-proven, left-sided, first-episode, uncomplicated diverticulitis at 22 Dutch centers. All patients were classified as having stage 1 disease by the modified Hinchey criteria (Int. J. Colorectal Dis. 2012;27:207-14), with about 92% of patients classified as Hinchey 1a.
The 266 patients randomized to initial antibiotic treatment began at least 2 days on intravenous treatment with amoxicillin and clavulanic acid, followed by a switch to oral delivery of the same combination when appropriate for a total of 10 days on the antibiotic.
Patients remained hospitalized until they switched from intravenous to oral treatment. The 262 patients randomized to no initial antibiotic treatment were hospitalized and observed, and received supportive treatment until they were judged ready for discharge by being able to eat a normal diet, had a temperature of less than 38 °C, and had a self-rated pain score of less than 4 on a visual analog scale of 0-10 without use of pain medication; in addition, the patient’s agreement was needed for discharge.
During 6 months of follow-up, the median time to complete recovery – defined as the criteria for hospital discharge plus a return to normal activity – occurred after a median of 12 days among patients in the antibiotic group and 14 days among those in the observation group, a difference that was not statistically significant for the study’s primary endpoint.
The results also showed no statistically significant differences between the two study arms for almost all the other outcomes assessed, including need for readmission, complications, need for surgery, morbidities, serious morbidities, and deaths. The only significant differences in outcomes were a decreased rate of hospitalization at the time of initial treatment among patients in the observation-only arm, and fewer hospitalized days among the observation-only patients.
“Observational treatment is without short- or long-term repercussions,” Dr. Daniels concluded.
Dr. Daniels had no disclosures.
On Twitter @mitchelzoler
AT UEG WEEK VIENNA 2014
Key clinical point: Observation-only worked as well as routine antibiotic treatment for patients with uncomplicated diverticulitis.
Major finding: Median time to full recovery was 12 days for antibiotic-treated patients and 14 days for observation-only patients.
Data source: The DIABOLO study, which randomized 528 patients with first-time, CT-proven, acute, uncomplicated diverticulitis at 22 Dutch centers.
Disclosures: Dr. Daniels had no disclosures.