User login
Official Newspaper of the American College of Surgeons
Case studies highlight HCV health care transmission risk
Hospitals should carefully monitor equipment for hepatitis C virus contamination and the possibility of health care transmission, according to a Feb. 27 report from the Centers for Disease Control and Prevention.
The CDC report focuses on two specific cases of health care–transmitted HCV. In 2010, a patient without HCV in a New Jersey hospital was treated by an anesthesiologist who had immediately beforehand treated someone with HCV. Despite the single commonality between the two patients, patient A contracted HCV.
In 2011, a patient in Wisconsin with a history of diabetes and chronic renal disease was diagnosed with HCV-4, a subtype of the disease that is rare in that part of the world. The infection occurred in 2009, when this patient had a kidney transplant at the same time as a patient with HCV-4 also was having a kidney transplant. The two transplants shared a surgeon, but the source of infection was likely a perfusion machine where an HCV-positive kidney and an HCV-negative kidney were both stored without cleaning the machine.
“These cases illustrate the importance of partnerships and communication between public health and health care professionals to ensure that basic infection control and injection safety practices are optimized wherever health care is delivered,” the CDC investigators concluded.
Read the full report in the MMWR (2015;64:165-70).
Hospitals should carefully monitor equipment for hepatitis C virus contamination and the possibility of health care transmission, according to a Feb. 27 report from the Centers for Disease Control and Prevention.
The CDC report focuses on two specific cases of health care–transmitted HCV. In 2010, a patient without HCV in a New Jersey hospital was treated by an anesthesiologist who had immediately beforehand treated someone with HCV. Despite the single commonality between the two patients, patient A contracted HCV.
In 2011, a patient in Wisconsin with a history of diabetes and chronic renal disease was diagnosed with HCV-4, a subtype of the disease that is rare in that part of the world. The infection occurred in 2009, when this patient had a kidney transplant at the same time as a patient with HCV-4 also was having a kidney transplant. The two transplants shared a surgeon, but the source of infection was likely a perfusion machine where an HCV-positive kidney and an HCV-negative kidney were both stored without cleaning the machine.
“These cases illustrate the importance of partnerships and communication between public health and health care professionals to ensure that basic infection control and injection safety practices are optimized wherever health care is delivered,” the CDC investigators concluded.
Read the full report in the MMWR (2015;64:165-70).
Hospitals should carefully monitor equipment for hepatitis C virus contamination and the possibility of health care transmission, according to a Feb. 27 report from the Centers for Disease Control and Prevention.
The CDC report focuses on two specific cases of health care–transmitted HCV. In 2010, a patient without HCV in a New Jersey hospital was treated by an anesthesiologist who had immediately beforehand treated someone with HCV. Despite the single commonality between the two patients, patient A contracted HCV.
In 2011, a patient in Wisconsin with a history of diabetes and chronic renal disease was diagnosed with HCV-4, a subtype of the disease that is rare in that part of the world. The infection occurred in 2009, when this patient had a kidney transplant at the same time as a patient with HCV-4 also was having a kidney transplant. The two transplants shared a surgeon, but the source of infection was likely a perfusion machine where an HCV-positive kidney and an HCV-negative kidney were both stored without cleaning the machine.
“These cases illustrate the importance of partnerships and communication between public health and health care professionals to ensure that basic infection control and injection safety practices are optimized wherever health care is delivered,” the CDC investigators concluded.
Read the full report in the MMWR (2015;64:165-70).
FDA approves antibacterial combo drug Avycaz
The Food and Drug Administration has approved the antibacterial drug ceftazidime-avibactam (Avycaz) on Feb. 25 for complicated intra-abdominal infections in combination with metronidazole, and for complicated urinary tract infections including pyelonephritis in adults.
“It is important that the use of Avycaz be reserved for situations where there are limited or no alternative antibacterial drugs for treating a patient’s infection,” Dr. Edward Cox, director of the FDA’s Office of Antimicrobial Products in the Center for Drug Evaluation and Research, said in a statement.
Avycaz is a fixed-combination drug containing ceftazidime, a previously approved cephalosporin with in vitro activity against certain gram-negative and gram-positive bacteria, and avibactam, a beta-lactamase inhibitor.
The addition of avibactam to ceftazidime protects ceftazidime from breakdown by extended spectrum beta-lactamases, Klebsiella pneumoniae carbapenemase (KPC), and AmpC-producing pathogens, according to David Nicholson, Ph.D., executive vice president of branded research and development at Actavis, which is jointly developing the drug with AstraZeneca.
“The FDA approval of Avycaz is an important step forward in enhancing our ability to respond to serious pathogens caused by difficult-to-treat gram-negative pathogens,” he said in a statement.
The recent rise in the incidence of multidrug-resistant gram-negative pathogens poses a significant threat to patients and places a tremendous strain on the U.S. health care system, Dr. Jose Vazquez, chief of infectious disease at Georgia Regents University in Augusta, Ga., commented in the same statement.
“The increasing prevalence of KPC-producing Enterobacteriaceae in particular, has become a major therapeutic challenge for physicians managing these infections. Unfortunately, there are currently a limited number of safe and effective antimicrobials to treat these serious infections,” he said.
Avycaz was granted priority review and named a Qualified Infectious Disease Product (QIDP), a designation given to antibacterial products to treat serious or life-threatening infections.
Its efficacy was supported in part by findings of the efficacy and safety of ceftazidime for the treatment of complicated intra-abdominal infections (cIAI) and complicated urinary tract infections (cUTI). The contribution of avibactam to Avycaz was based on data from in vitro studies and animal models of infection. Avycaz was also studied in two phase II trials, one each in cIAI and cUTI.
The most common side effects are vomiting, nausea, constipation, and anxiety. The FDA advises health care professionals to inform patients of these risks and that decreased efficacy, seizures, and other neurologic events were seen in patients with renal impairment. Serious skin reactions and anaphylaxis may occur in patients with penicillin allergies.
The recommended dosage for patients with normal renal function is 2.5 g administered every 8 hours by intravenous infusion over 2 hours in adults aged 18 years and older. For patients with changing or impaired renal function (creatinine clearance < 50 mL/min), CrCL should be monitored at least daily and the dosage adjusted accordingly.
In a phase III trial of intra-abdominal infections, clinical cure rates were lower in the subgroup of patients with CrCL of 30-50 mL/min, compared with those with CrCL greater than 50 mL/min, according to the company. The reduction in cure rates was more marked in patients treated with Avycaz plus metronidazole vs. meropenem-treated patients.
Avycaz will be available in the second quarter of 2015, according to the company. Phase III studies evaluating Avycaz for the treatment of cIAI and cUTI are ongoing and targeted for completion in late 2015.
The Food and Drug Administration has approved the antibacterial drug ceftazidime-avibactam (Avycaz) on Feb. 25 for complicated intra-abdominal infections in combination with metronidazole, and for complicated urinary tract infections including pyelonephritis in adults.
“It is important that the use of Avycaz be reserved for situations where there are limited or no alternative antibacterial drugs for treating a patient’s infection,” Dr. Edward Cox, director of the FDA’s Office of Antimicrobial Products in the Center for Drug Evaluation and Research, said in a statement.
Avycaz is a fixed-combination drug containing ceftazidime, a previously approved cephalosporin with in vitro activity against certain gram-negative and gram-positive bacteria, and avibactam, a beta-lactamase inhibitor.
The addition of avibactam to ceftazidime protects ceftazidime from breakdown by extended spectrum beta-lactamases, Klebsiella pneumoniae carbapenemase (KPC), and AmpC-producing pathogens, according to David Nicholson, Ph.D., executive vice president of branded research and development at Actavis, which is jointly developing the drug with AstraZeneca.
“The FDA approval of Avycaz is an important step forward in enhancing our ability to respond to serious pathogens caused by difficult-to-treat gram-negative pathogens,” he said in a statement.
The recent rise in the incidence of multidrug-resistant gram-negative pathogens poses a significant threat to patients and places a tremendous strain on the U.S. health care system, Dr. Jose Vazquez, chief of infectious disease at Georgia Regents University in Augusta, Ga., commented in the same statement.
“The increasing prevalence of KPC-producing Enterobacteriaceae in particular, has become a major therapeutic challenge for physicians managing these infections. Unfortunately, there are currently a limited number of safe and effective antimicrobials to treat these serious infections,” he said.
Avycaz was granted priority review and named a Qualified Infectious Disease Product (QIDP), a designation given to antibacterial products to treat serious or life-threatening infections.
Its efficacy was supported in part by findings of the efficacy and safety of ceftazidime for the treatment of complicated intra-abdominal infections (cIAI) and complicated urinary tract infections (cUTI). The contribution of avibactam to Avycaz was based on data from in vitro studies and animal models of infection. Avycaz was also studied in two phase II trials, one each in cIAI and cUTI.
The most common side effects are vomiting, nausea, constipation, and anxiety. The FDA advises health care professionals to inform patients of these risks and that decreased efficacy, seizures, and other neurologic events were seen in patients with renal impairment. Serious skin reactions and anaphylaxis may occur in patients with penicillin allergies.
The recommended dosage for patients with normal renal function is 2.5 g administered every 8 hours by intravenous infusion over 2 hours in adults aged 18 years and older. For patients with changing or impaired renal function (creatinine clearance < 50 mL/min), CrCL should be monitored at least daily and the dosage adjusted accordingly.
In a phase III trial of intra-abdominal infections, clinical cure rates were lower in the subgroup of patients with CrCL of 30-50 mL/min, compared with those with CrCL greater than 50 mL/min, according to the company. The reduction in cure rates was more marked in patients treated with Avycaz plus metronidazole vs. meropenem-treated patients.
Avycaz will be available in the second quarter of 2015, according to the company. Phase III studies evaluating Avycaz for the treatment of cIAI and cUTI are ongoing and targeted for completion in late 2015.
The Food and Drug Administration has approved the antibacterial drug ceftazidime-avibactam (Avycaz) on Feb. 25 for complicated intra-abdominal infections in combination with metronidazole, and for complicated urinary tract infections including pyelonephritis in adults.
“It is important that the use of Avycaz be reserved for situations where there are limited or no alternative antibacterial drugs for treating a patient’s infection,” Dr. Edward Cox, director of the FDA’s Office of Antimicrobial Products in the Center for Drug Evaluation and Research, said in a statement.
Avycaz is a fixed-combination drug containing ceftazidime, a previously approved cephalosporin with in vitro activity against certain gram-negative and gram-positive bacteria, and avibactam, a beta-lactamase inhibitor.
The addition of avibactam to ceftazidime protects ceftazidime from breakdown by extended spectrum beta-lactamases, Klebsiella pneumoniae carbapenemase (KPC), and AmpC-producing pathogens, according to David Nicholson, Ph.D., executive vice president of branded research and development at Actavis, which is jointly developing the drug with AstraZeneca.
“The FDA approval of Avycaz is an important step forward in enhancing our ability to respond to serious pathogens caused by difficult-to-treat gram-negative pathogens,” he said in a statement.
The recent rise in the incidence of multidrug-resistant gram-negative pathogens poses a significant threat to patients and places a tremendous strain on the U.S. health care system, Dr. Jose Vazquez, chief of infectious disease at Georgia Regents University in Augusta, Ga., commented in the same statement.
“The increasing prevalence of KPC-producing Enterobacteriaceae in particular, has become a major therapeutic challenge for physicians managing these infections. Unfortunately, there are currently a limited number of safe and effective antimicrobials to treat these serious infections,” he said.
Avycaz was granted priority review and named a Qualified Infectious Disease Product (QIDP), a designation given to antibacterial products to treat serious or life-threatening infections.
Its efficacy was supported in part by findings of the efficacy and safety of ceftazidime for the treatment of complicated intra-abdominal infections (cIAI) and complicated urinary tract infections (cUTI). The contribution of avibactam to Avycaz was based on data from in vitro studies and animal models of infection. Avycaz was also studied in two phase II trials, one each in cIAI and cUTI.
The most common side effects are vomiting, nausea, constipation, and anxiety. The FDA advises health care professionals to inform patients of these risks and that decreased efficacy, seizures, and other neurologic events were seen in patients with renal impairment. Serious skin reactions and anaphylaxis may occur in patients with penicillin allergies.
The recommended dosage for patients with normal renal function is 2.5 g administered every 8 hours by intravenous infusion over 2 hours in adults aged 18 years and older. For patients with changing or impaired renal function (creatinine clearance < 50 mL/min), CrCL should be monitored at least daily and the dosage adjusted accordingly.
In a phase III trial of intra-abdominal infections, clinical cure rates were lower in the subgroup of patients with CrCL of 30-50 mL/min, compared with those with CrCL greater than 50 mL/min, according to the company. The reduction in cure rates was more marked in patients treated with Avycaz plus metronidazole vs. meropenem-treated patients.
Avycaz will be available in the second quarter of 2015, according to the company. Phase III studies evaluating Avycaz for the treatment of cIAI and cUTI are ongoing and targeted for completion in late 2015.
Do complications muddle NSQIP risk calculator validity?
The American College of Surgeons’ NSQIP surgical risk calculator was effective for evaluating patients at average surgical risk undergoing laparoscopic colectomy at a single institution, but did not accurately predict outcomes in a small percentage of patients when one or more serious complications occurred, a new study has found.
Specifically, the actual length of stay (LOS) was significantly longer than predicted by the calculator (4.22 days vs. 4.11 days; P = .0001), with four outliers with multiple complications having an LOS more than 3 standard deviations from the mean. After removing the outliers, the actual LOS was significantly shorter than that predicted (3.31 days vs. 4.05 days; P = .002). Occurrence of any complication was also significantly lower than predicted (17.3% vs. 19.4%; P = .05).
“Addition of surgeon- and patient-specific data via the American College of Surgeons case-logging system could better adjust for these areas,” study author Dr. Kyle Cologne and his colleagues recommend.
Read the full article at J. Am. Coll. Surg. 2015;220:281-6.
The American College of Surgeons’ NSQIP surgical risk calculator was effective for evaluating patients at average surgical risk undergoing laparoscopic colectomy at a single institution, but did not accurately predict outcomes in a small percentage of patients when one or more serious complications occurred, a new study has found.
Specifically, the actual length of stay (LOS) was significantly longer than predicted by the calculator (4.22 days vs. 4.11 days; P = .0001), with four outliers with multiple complications having an LOS more than 3 standard deviations from the mean. After removing the outliers, the actual LOS was significantly shorter than that predicted (3.31 days vs. 4.05 days; P = .002). Occurrence of any complication was also significantly lower than predicted (17.3% vs. 19.4%; P = .05).
“Addition of surgeon- and patient-specific data via the American College of Surgeons case-logging system could better adjust for these areas,” study author Dr. Kyle Cologne and his colleagues recommend.
Read the full article at J. Am. Coll. Surg. 2015;220:281-6.
The American College of Surgeons’ NSQIP surgical risk calculator was effective for evaluating patients at average surgical risk undergoing laparoscopic colectomy at a single institution, but did not accurately predict outcomes in a small percentage of patients when one or more serious complications occurred, a new study has found.
Specifically, the actual length of stay (LOS) was significantly longer than predicted by the calculator (4.22 days vs. 4.11 days; P = .0001), with four outliers with multiple complications having an LOS more than 3 standard deviations from the mean. After removing the outliers, the actual LOS was significantly shorter than that predicted (3.31 days vs. 4.05 days; P = .002). Occurrence of any complication was also significantly lower than predicted (17.3% vs. 19.4%; P = .05).
“Addition of surgeon- and patient-specific data via the American College of Surgeons case-logging system could better adjust for these areas,” study author Dr. Kyle Cologne and his colleagues recommend.
Read the full article at J. Am. Coll. Surg. 2015;220:281-6.
Guidelines updated for postoperative delirium in geriatric patients
The American Geriatrics Society has released its new Clinical Practice Guideline for Postoperative Delirium in Older Adults, which the society hopes will enable health care professionals to improve delirium prevention and treatment through evidence-based measures.
Among the recommendations for treating delirium in geriatric postsurgical patients are nonpharmacologic interventions such as mobility and walking, avoiding physical restraints, and assuring adequate oxygen, fluids, and nutrition; pain management, preferably with nonopioid medications; and avoidance of certain medications such as antipsychotics, benzodiazepines, and cholinesterase inhibitors.
The guidelines are part of a larger package that includes patient resources, evidence tables and journal articles, and other companion public education materials, available on the AGS website.
The American Geriatrics Society has released its new Clinical Practice Guideline for Postoperative Delirium in Older Adults, which the society hopes will enable health care professionals to improve delirium prevention and treatment through evidence-based measures.
Among the recommendations for treating delirium in geriatric postsurgical patients are nonpharmacologic interventions such as mobility and walking, avoiding physical restraints, and assuring adequate oxygen, fluids, and nutrition; pain management, preferably with nonopioid medications; and avoidance of certain medications such as antipsychotics, benzodiazepines, and cholinesterase inhibitors.
The guidelines are part of a larger package that includes patient resources, evidence tables and journal articles, and other companion public education materials, available on the AGS website.
The American Geriatrics Society has released its new Clinical Practice Guideline for Postoperative Delirium in Older Adults, which the society hopes will enable health care professionals to improve delirium prevention and treatment through evidence-based measures.
Among the recommendations for treating delirium in geriatric postsurgical patients are nonpharmacologic interventions such as mobility and walking, avoiding physical restraints, and assuring adequate oxygen, fluids, and nutrition; pain management, preferably with nonopioid medications; and avoidance of certain medications such as antipsychotics, benzodiazepines, and cholinesterase inhibitors.
The guidelines are part of a larger package that includes patient resources, evidence tables and journal articles, and other companion public education materials, available on the AGS website.
Surgical wound classification unreliable
Surgical wound classification is frequently unreliable, according to a multicenter review of 2,034 cases.
Overall concordance between surgical wound classification (SWC) from the electronic medical record and SWC from operative note review was only 56%, ranging from 47% to 66% across 11 participating institutions.
The degree of discordance also varied according to the specific operation, with inguinal hernia repair having the highest overall median concordance at 92% and appendectomy having the lowest at just 12%.
“Using unreliable measures, such as current SWC assignment methods, can lead to biased study results and misleading portrayals of hospital quality. Surgical wound classification should not be used for SSI [surgical site infection] risk stratification until a more consistent process can be developed and validated,” Dr. Shauna M. Levy, lead study author, concluded.
Read the full article: J. Am. Coll. Surg. 2015;220;323-9.
Surgical wound classification is frequently unreliable, according to a multicenter review of 2,034 cases.
Overall concordance between surgical wound classification (SWC) from the electronic medical record and SWC from operative note review was only 56%, ranging from 47% to 66% across 11 participating institutions.
The degree of discordance also varied according to the specific operation, with inguinal hernia repair having the highest overall median concordance at 92% and appendectomy having the lowest at just 12%.
“Using unreliable measures, such as current SWC assignment methods, can lead to biased study results and misleading portrayals of hospital quality. Surgical wound classification should not be used for SSI [surgical site infection] risk stratification until a more consistent process can be developed and validated,” Dr. Shauna M. Levy, lead study author, concluded.
Read the full article: J. Am. Coll. Surg. 2015;220;323-9.
Surgical wound classification is frequently unreliable, according to a multicenter review of 2,034 cases.
Overall concordance between surgical wound classification (SWC) from the electronic medical record and SWC from operative note review was only 56%, ranging from 47% to 66% across 11 participating institutions.
The degree of discordance also varied according to the specific operation, with inguinal hernia repair having the highest overall median concordance at 92% and appendectomy having the lowest at just 12%.
“Using unreliable measures, such as current SWC assignment methods, can lead to biased study results and misleading portrayals of hospital quality. Surgical wound classification should not be used for SSI [surgical site infection] risk stratification until a more consistent process can be developed and validated,” Dr. Shauna M. Levy, lead study author, concluded.
Read the full article: J. Am. Coll. Surg. 2015;220;323-9.
AGA guideline addresses asymptomatic neoplastic pancreatic cysts
For asymptomatic neoplastic pancreatic cysts discovered incidentally on abdominal imaging, surgery is warranted only if both a solid component and a dilated pancreatic duct are shown and/or if endoscopic* ultrasound with or without fine-needle aspiration has detected “concerning features,” according to a clinical practice guideline published in the April issue of Gastroenterology (doi:10.1053/j.gastro.2015.01.015).
Even then, patients should be referred for the procedure only to centers that perform high volumes of pancreatic surgery, so as to minimize the relatively high rates of morbidity and mortality associated with these invasive, expensive, and potentially harmful surgeries.
These are 2 of the 10 recommendations and “suggestions” in the American Gastroenterological Association guideline, which is the first such guideline to be based on a systematic evaluation of the available evidence, said Dr. Santhi Swaroop Vege of the division of gastroenterology and hepatology, Mayo Clinic, Rochester, Minn., and his associates.
Incidental discovery of asymptomatic pancreatic cysts is common with the increasing use of sophisticated abdominal imaging techniques. For example, approximately 15% of patients undergoing abdominal MRI for other indications are found to have them. Clinical management is very difficult because only a small fraction of these lesions prove to be malignant, and the data to guide diagnostic and treatment decisions are sparse and of very low quality, based almost entirely on retrospective case series. Nevertheless, Dr. Vege and his associates developed the guideline from the limited evidence that is available, because of the seriousness of the outcomes for that minority of cancers and the complexity of management strategies.
“These recommendations may result in significant controversy, as they advocate less frequent follow-up and a higher threshold before offering endoscopic ultrasound and/or surgery. However, consistent utilization should decrease inadvertent harm to patients and reduce the costs of health care delivery,” they noted.
After reviewing the literature, the investigators estimated that an asymptomatic cyst found incidentally on MRI has only a 10 in 100,000 chance of being a mucinous invasive malignancy and a 17 in 100,000 chance of being a ductal cancer. The guideline therefore suggests that surveillance is sufficient for asymptomatic pancreatic cysts smaller than 3 cm that don’t have a solid component or a dilated pancreatic duct. The preferred imaging modality is MRI, and the preferred surveillance interval is at 1 year after discovery. If no change is noted, surveillance every 2 years for a total of 5 years should be sufficient.
The risk of malignant transformation is estimated to be only 0.24% per year, and is even lower among cysts that show no changes over time. “The small risk of malignant progression in stable cysts is likely outweighed by the costs of surveillance and the risks of surgery,” so the guideline suggests that surveillance can be discontinued if no change has occurred after 5 years or if the patient is no longer a candidate for surgery. However, some patients, such as those with a family history of pancreatic cancer, may opt to continue surveillance.
In contrast, asymptomatic pancreatic cysts that have at least two high-risk features should be assessed using endoscopic ultrasound, with or without fine-needle aspiration. If these procedures reveal “concerning features,” the benefits of surgery probably outweigh the risks, and surgical excision/resection is conditionally recommended. However, even in these “suspect” lesions only an estimated 17% are found to harbor high-grade dysplasia. Any benefit ascribed to surgery must be balanced against “an overall postoperative mortality of 2% and major morbidity of 30% from our review of the literature,” Dr. Vege and his associates said.
In contrast to its suggestions and conditional recommendations, the AGA guideline strongly recommends that if surgery is being considered, patients be referred to “a center with demonstrated expertise in pancreatic surgery.” Their investigation showed that in the U.S. overall, all pancreatic surgeries carry a postoperative mortality of 6.6%, while in centers of excellence, the postoperative mortality is only 2%.
The guideline conditionally suggests that patients found to have invasive cancer or dysplasia in a resected cyst can undergo MRI surveillance of any remaining pancreas every 2 years, for as long as the patient remains a good candidate for further surgery.
Another recommendation is that patients be given a clear understanding of the benefits and risks of any surveillance program, because surveillance may not be appropriate for some. Certain patients have a high tolerance for risk and may decide against surveillance once the small risk of malignancy is explained to them. Others have a limited life expectancy and are unlikely to benefit from surveillance or surgery, and still others who are poor surgical candidates because of age or comorbidities shouldn’t be subjected to surveillance.
Finally, this AGA guideline pertains only to asymptomatic neoplastic pancreatic cysts. It doesn’t address lesions such as solid papillary neoplasms, cystic degeneration of adenocarcinomas, neuroendocrine tumors, or main duct intraductal papillary mucinous neoplasms without side-branch involvement, because identification of these lesions is more straightforward and the accepted management approach is surgical resection, Dr. Vege and his associates added.
*A correction was made on April 29, 2015.
For asymptomatic neoplastic pancreatic cysts discovered incidentally on abdominal imaging, surgery is warranted only if both a solid component and a dilated pancreatic duct are shown and/or if endoscopic* ultrasound with or without fine-needle aspiration has detected “concerning features,” according to a clinical practice guideline published in the April issue of Gastroenterology (doi:10.1053/j.gastro.2015.01.015).
Even then, patients should be referred for the procedure only to centers that perform high volumes of pancreatic surgery, so as to minimize the relatively high rates of morbidity and mortality associated with these invasive, expensive, and potentially harmful surgeries.
These are 2 of the 10 recommendations and “suggestions” in the American Gastroenterological Association guideline, which is the first such guideline to be based on a systematic evaluation of the available evidence, said Dr. Santhi Swaroop Vege of the division of gastroenterology and hepatology, Mayo Clinic, Rochester, Minn., and his associates.
Incidental discovery of asymptomatic pancreatic cysts is common with the increasing use of sophisticated abdominal imaging techniques. For example, approximately 15% of patients undergoing abdominal MRI for other indications are found to have them. Clinical management is very difficult because only a small fraction of these lesions prove to be malignant, and the data to guide diagnostic and treatment decisions are sparse and of very low quality, based almost entirely on retrospective case series. Nevertheless, Dr. Vege and his associates developed the guideline from the limited evidence that is available, because of the seriousness of the outcomes for that minority of cancers and the complexity of management strategies.
“These recommendations may result in significant controversy, as they advocate less frequent follow-up and a higher threshold before offering endoscopic ultrasound and/or surgery. However, consistent utilization should decrease inadvertent harm to patients and reduce the costs of health care delivery,” they noted.
After reviewing the literature, the investigators estimated that an asymptomatic cyst found incidentally on MRI has only a 10 in 100,000 chance of being a mucinous invasive malignancy and a 17 in 100,000 chance of being a ductal cancer. The guideline therefore suggests that surveillance is sufficient for asymptomatic pancreatic cysts smaller than 3 cm that don’t have a solid component or a dilated pancreatic duct. The preferred imaging modality is MRI, and the preferred surveillance interval is at 1 year after discovery. If no change is noted, surveillance every 2 years for a total of 5 years should be sufficient.
The risk of malignant transformation is estimated to be only 0.24% per year, and is even lower among cysts that show no changes over time. “The small risk of malignant progression in stable cysts is likely outweighed by the costs of surveillance and the risks of surgery,” so the guideline suggests that surveillance can be discontinued if no change has occurred after 5 years or if the patient is no longer a candidate for surgery. However, some patients, such as those with a family history of pancreatic cancer, may opt to continue surveillance.
In contrast, asymptomatic pancreatic cysts that have at least two high-risk features should be assessed using endoscopic ultrasound, with or without fine-needle aspiration. If these procedures reveal “concerning features,” the benefits of surgery probably outweigh the risks, and surgical excision/resection is conditionally recommended. However, even in these “suspect” lesions only an estimated 17% are found to harbor high-grade dysplasia. Any benefit ascribed to surgery must be balanced against “an overall postoperative mortality of 2% and major morbidity of 30% from our review of the literature,” Dr. Vege and his associates said.
In contrast to its suggestions and conditional recommendations, the AGA guideline strongly recommends that if surgery is being considered, patients be referred to “a center with demonstrated expertise in pancreatic surgery.” Their investigation showed that in the U.S. overall, all pancreatic surgeries carry a postoperative mortality of 6.6%, while in centers of excellence, the postoperative mortality is only 2%.
The guideline conditionally suggests that patients found to have invasive cancer or dysplasia in a resected cyst can undergo MRI surveillance of any remaining pancreas every 2 years, for as long as the patient remains a good candidate for further surgery.
Another recommendation is that patients be given a clear understanding of the benefits and risks of any surveillance program, because surveillance may not be appropriate for some. Certain patients have a high tolerance for risk and may decide against surveillance once the small risk of malignancy is explained to them. Others have a limited life expectancy and are unlikely to benefit from surveillance or surgery, and still others who are poor surgical candidates because of age or comorbidities shouldn’t be subjected to surveillance.
Finally, this AGA guideline pertains only to asymptomatic neoplastic pancreatic cysts. It doesn’t address lesions such as solid papillary neoplasms, cystic degeneration of adenocarcinomas, neuroendocrine tumors, or main duct intraductal papillary mucinous neoplasms without side-branch involvement, because identification of these lesions is more straightforward and the accepted management approach is surgical resection, Dr. Vege and his associates added.
*A correction was made on April 29, 2015.
For asymptomatic neoplastic pancreatic cysts discovered incidentally on abdominal imaging, surgery is warranted only if both a solid component and a dilated pancreatic duct are shown and/or if endoscopic* ultrasound with or without fine-needle aspiration has detected “concerning features,” according to a clinical practice guideline published in the April issue of Gastroenterology (doi:10.1053/j.gastro.2015.01.015).
Even then, patients should be referred for the procedure only to centers that perform high volumes of pancreatic surgery, so as to minimize the relatively high rates of morbidity and mortality associated with these invasive, expensive, and potentially harmful surgeries.
These are 2 of the 10 recommendations and “suggestions” in the American Gastroenterological Association guideline, which is the first such guideline to be based on a systematic evaluation of the available evidence, said Dr. Santhi Swaroop Vege of the division of gastroenterology and hepatology, Mayo Clinic, Rochester, Minn., and his associates.
Incidental discovery of asymptomatic pancreatic cysts is common with the increasing use of sophisticated abdominal imaging techniques. For example, approximately 15% of patients undergoing abdominal MRI for other indications are found to have them. Clinical management is very difficult because only a small fraction of these lesions prove to be malignant, and the data to guide diagnostic and treatment decisions are sparse and of very low quality, based almost entirely on retrospective case series. Nevertheless, Dr. Vege and his associates developed the guideline from the limited evidence that is available, because of the seriousness of the outcomes for that minority of cancers and the complexity of management strategies.
“These recommendations may result in significant controversy, as they advocate less frequent follow-up and a higher threshold before offering endoscopic ultrasound and/or surgery. However, consistent utilization should decrease inadvertent harm to patients and reduce the costs of health care delivery,” they noted.
After reviewing the literature, the investigators estimated that an asymptomatic cyst found incidentally on MRI has only a 10 in 100,000 chance of being a mucinous invasive malignancy and a 17 in 100,000 chance of being a ductal cancer. The guideline therefore suggests that surveillance is sufficient for asymptomatic pancreatic cysts smaller than 3 cm that don’t have a solid component or a dilated pancreatic duct. The preferred imaging modality is MRI, and the preferred surveillance interval is at 1 year after discovery. If no change is noted, surveillance every 2 years for a total of 5 years should be sufficient.
The risk of malignant transformation is estimated to be only 0.24% per year, and is even lower among cysts that show no changes over time. “The small risk of malignant progression in stable cysts is likely outweighed by the costs of surveillance and the risks of surgery,” so the guideline suggests that surveillance can be discontinued if no change has occurred after 5 years or if the patient is no longer a candidate for surgery. However, some patients, such as those with a family history of pancreatic cancer, may opt to continue surveillance.
In contrast, asymptomatic pancreatic cysts that have at least two high-risk features should be assessed using endoscopic ultrasound, with or without fine-needle aspiration. If these procedures reveal “concerning features,” the benefits of surgery probably outweigh the risks, and surgical excision/resection is conditionally recommended. However, even in these “suspect” lesions only an estimated 17% are found to harbor high-grade dysplasia. Any benefit ascribed to surgery must be balanced against “an overall postoperative mortality of 2% and major morbidity of 30% from our review of the literature,” Dr. Vege and his associates said.
In contrast to its suggestions and conditional recommendations, the AGA guideline strongly recommends that if surgery is being considered, patients be referred to “a center with demonstrated expertise in pancreatic surgery.” Their investigation showed that in the U.S. overall, all pancreatic surgeries carry a postoperative mortality of 6.6%, while in centers of excellence, the postoperative mortality is only 2%.
The guideline conditionally suggests that patients found to have invasive cancer or dysplasia in a resected cyst can undergo MRI surveillance of any remaining pancreas every 2 years, for as long as the patient remains a good candidate for further surgery.
Another recommendation is that patients be given a clear understanding of the benefits and risks of any surveillance program, because surveillance may not be appropriate for some. Certain patients have a high tolerance for risk and may decide against surveillance once the small risk of malignancy is explained to them. Others have a limited life expectancy and are unlikely to benefit from surveillance or surgery, and still others who are poor surgical candidates because of age or comorbidities shouldn’t be subjected to surveillance.
Finally, this AGA guideline pertains only to asymptomatic neoplastic pancreatic cysts. It doesn’t address lesions such as solid papillary neoplasms, cystic degeneration of adenocarcinomas, neuroendocrine tumors, or main duct intraductal papillary mucinous neoplasms without side-branch involvement, because identification of these lesions is more straightforward and the accepted management approach is surgical resection, Dr. Vege and his associates added.
*A correction was made on April 29, 2015.
Key clinical point: A new AGA clinical practice guideline suggests surgery is warranted only if asymptomatic neoplastic pancreatic cysts have both a solid component and a dilated pancreatic duct and/or concerning features on endoscopic ultrasound with or without fine-needle aspiration.
Major finding: An asymptomatic pancreatic cyst found incidentally on MRI is estimated to have only a 10 in 100,000 chance of being a mucinous invasive malignancy and a 17 in 100,000 chance of being a ductal cancer.
Data source: A review and summary of the available evidence regarding management of asymptomatic neoplastic pancreatic cysts, and a compilation of recommendations for clinicians.
Disclosures: Dr. Vege and his associates’ disclosures are available at the American Gastroenterological Association, Bethesda, Md.
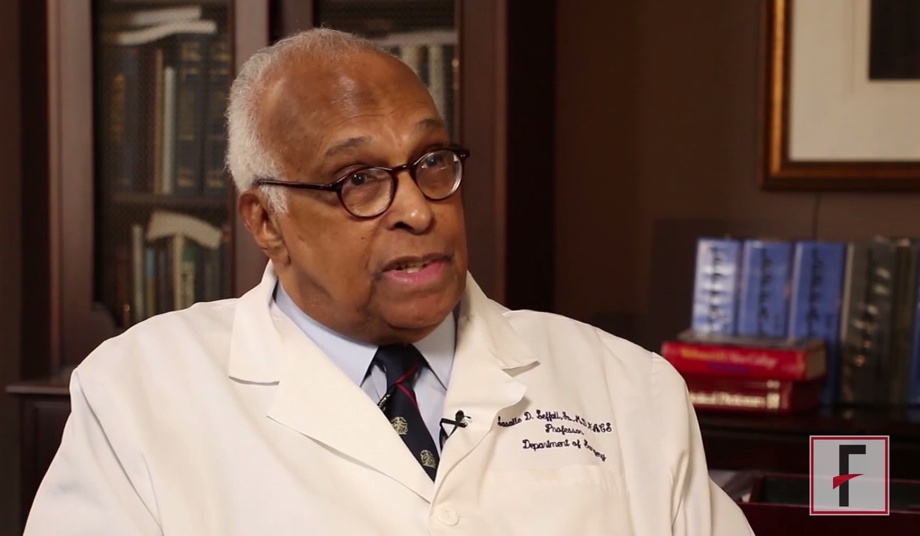
VIDEO: Eminent surgeon Dr. LaSalle D. Leffall reflects on his journey
LaSalle D. Leffall, Jr., M.D., FACS, is the Charles R. Drew Professor of Surgery, Howard University College of Medicine, Washington DC.
Dr. Leffall has had a long and distinguished career and has served as President of the American Cancer Society, the Society of Surgical Oncology, the Society of Surgical Chairmen, the Washington Academy of Surgery, the Society of Black Academic Surgeons, and the American College of Surgeons. He reflects on his career, the role of the American College of Surgeons in promoting diversity in the surgical field, and the Society for Black Academic Surgeons.
LaSalle D. Leffall, Jr., M.D., FACS, is the Charles R. Drew Professor of Surgery, Howard University College of Medicine, Washington DC.
Dr. Leffall has had a long and distinguished career and has served as President of the American Cancer Society, the Society of Surgical Oncology, the Society of Surgical Chairmen, the Washington Academy of Surgery, the Society of Black Academic Surgeons, and the American College of Surgeons. He reflects on his career, the role of the American College of Surgeons in promoting diversity in the surgical field, and the Society for Black Academic Surgeons.
LaSalle D. Leffall, Jr., M.D., FACS, is the Charles R. Drew Professor of Surgery, Howard University College of Medicine, Washington DC.
Dr. Leffall has had a long and distinguished career and has served as President of the American Cancer Society, the Society of Surgical Oncology, the Society of Surgical Chairmen, the Washington Academy of Surgery, the Society of Black Academic Surgeons, and the American College of Surgeons. He reflects on his career, the role of the American College of Surgeons in promoting diversity in the surgical field, and the Society for Black Academic Surgeons.
Supreme Court’s ruling could jeopardize state medical board regulation
A U.S. Supreme Court ruling against a local dental board that attempted to stop nonprofessionals from whitening teeth could alter state medical boards’ ability to regulate the practice of medicine, some physician groups warn.
The federal high court ruled Feb. 25 that North Carolina’s state board of dental examiners violated federal antitrust laws when it tried to prevent nondentists from offering teeth-whitening services. State professional boards that regulate their competitors are only protected from antitrust scrutiny when supervised by state government, the court said in its 6-3 decision.
The ruling in North Carolina State Board of Dental Examiners v. Federal Trade Commission is disappointing and will have a broad impact on how regulatory boards function nationwide, said Bobby D. White, chief operations officer for the North Carolina Board of Dental Examiners.
“Virtually every professional regulatory board in the country will eventually have to change the way it’s structured, change the way it’s supervised, or change the activities it performs,” Mr. White said in an interview. “And since all of those changes will take time – and often legislative activity – the opinion threatens to massively disrupt professional regulation.”
Federal Trade Commission Chair Edith Ramirez said the decision correctly affirms that a state may not give private market participants unsupervised authority to suppress competition, even if they act through a formally designated “state agency.”
“We are pleased with the Supreme Court’s recognition that the antitrust laws limit the ability of market incumbents to suppress competition through state professional boards,” Ms. Ramirez said in a statement. “We will remain vigilant through our enforcement initiatives and advocacy to safeguard competition and ensure that American consumers benefit from entrepreneurial initiative.”
The ruling stems from a dispute between the North Carolina State Board of Dental Examiners and a group of unlicensed teeth whiteners who were providing services at shopping malls. From 2006 to 2009, the board issued cease-and-desist letters to the nondentists, warning them about a state ban against stain removal by unlicensed practitioners.
The nondentists contacted the FTC, and an administrative law judge found that the board’s conduct constituted an unreasonable restraint of trade. The board argued its conduct was protected from antitrust oversight by the state action doctrine, a legal rule that applies to some state board conduct. The doctrine exempts from federal antitrust scrutiny state agencies that are actively supervised by a state.
But the FTC said the board’s activities fell outside the doctrine because it is made up of market participants – dentists – and is not actively supervised by a sovereign part of the state government. The 4th U.S. Circuit Court of Appeals in 2013 ruled in favor of the FTC, and the dental board appealed to the U.S. Supreme Court.
Physician leaders, including the American Medical Association and the American Academy of Family Physicians, issued a joint brief to the high court in support of the dental board.
If the appellate ruling stands, the decisions of state medical and dental boards will be distorted by considerations of federal competition policy, to the detriment of public health, the AMA said in its brief. In addition, highly qualified practitioners who would otherwise be willing to serve on boards would likely resign or refuse to accept office to avoid personal antitrust exposure, the brief argued.
But in its opinion, the Supreme Court majority said if a state wants to rely on active market participants as regulators, it must provide active supervision to achieve antitrust immunity. The North Carolina Board of Dental Examiners did not have such supervision, the court said.
“When a state empowers a group of active market participants to decide who can participate in its market, and on what terms, the need for supervision is manifest,” the majority justices said in their opinion. “The court holds today that a state board on which a controlling number of decision makers are active market participants in the occupation the board regulates must satisfy active supervision requirement(s) in order to invoke state action antitrust immunity.”
The American Association of Nurse Anesthetists praised the decision, calling it a win for patients’ access to care. The AANA filed a joint brief to the high court in support of the FTC with several other organizations, including the American Nurses Association.
“The AANA and its co-amici had a strong interest in this case, because unnecessary restrictions on the practice of any qualified health care provider limit patient access to quality care, may increase cost, and can compromise the quality of health care delivery,” AANA President Sharon Pearce said in an interview.
“The Supreme Court decision is consistent with the arguments made by the AANA and its co-amici who urged the Supreme Court to affirm the appellate court’s decision for a number of reasons, including concerns that unsupervised state regulatory boards comprised mostly of practicing professionals have the potential of acting in their own economic self-interest by protecting their competitive position in ways not intended or authorized by the state, thus warranting oversight.”
The North Carolina Medical Society said the Supreme Court decision runs contrary to the time-tested regulatory model used nationwide by states to regulate learned professions.
“The decision focuses narrowly on antitrust law, not on the broader and far more important issue of protecting the public through effective regulation of medical practice,” the medical society said.
State medical boards will need to time to analyze the decision and decide how the ruling might affect the way in which they operate, said Dr. Humayun J. Chaudhry, president and CEO of the Federation of State Medical Boards. The FSMB plans to hold a webinar March 5 to address how state medical boards should apply the ruling.
“We recognize the importance of this decision and will now begin to make better sense of it and begin to address the open-ended questions” left by the ruling, he said in an interview. “What kind of impact [the decision has] remains to be seen.”
The AMA expressed disappointment with the decision.
“State medical boards are authorized by state governments to regulate medical licensing and medical practice in the interest of patient safety,” noted AMA President Robert M. Wah in a statement. “The AMA agrees with Justice [Samuel] Alito, speaking for the three dissenting justices, that today’s decision ‘will spawn confusion’ by creating far-reaching effects on the jurisdiction of states to regulate medicine and protect patient safety.
“The AMA will work with other physician groups to secure policy changes to reinforce long-held antitrust protections for activities conducted under state authority to protect patients,” Dr. Wah said.
On Twitter @legal_med
A U.S. Supreme Court ruling against a local dental board that attempted to stop nonprofessionals from whitening teeth could alter state medical boards’ ability to regulate the practice of medicine, some physician groups warn.
The federal high court ruled Feb. 25 that North Carolina’s state board of dental examiners violated federal antitrust laws when it tried to prevent nondentists from offering teeth-whitening services. State professional boards that regulate their competitors are only protected from antitrust scrutiny when supervised by state government, the court said in its 6-3 decision.
The ruling in North Carolina State Board of Dental Examiners v. Federal Trade Commission is disappointing and will have a broad impact on how regulatory boards function nationwide, said Bobby D. White, chief operations officer for the North Carolina Board of Dental Examiners.
“Virtually every professional regulatory board in the country will eventually have to change the way it’s structured, change the way it’s supervised, or change the activities it performs,” Mr. White said in an interview. “And since all of those changes will take time – and often legislative activity – the opinion threatens to massively disrupt professional regulation.”
Federal Trade Commission Chair Edith Ramirez said the decision correctly affirms that a state may not give private market participants unsupervised authority to suppress competition, even if they act through a formally designated “state agency.”
“We are pleased with the Supreme Court’s recognition that the antitrust laws limit the ability of market incumbents to suppress competition through state professional boards,” Ms. Ramirez said in a statement. “We will remain vigilant through our enforcement initiatives and advocacy to safeguard competition and ensure that American consumers benefit from entrepreneurial initiative.”
The ruling stems from a dispute between the North Carolina State Board of Dental Examiners and a group of unlicensed teeth whiteners who were providing services at shopping malls. From 2006 to 2009, the board issued cease-and-desist letters to the nondentists, warning them about a state ban against stain removal by unlicensed practitioners.
The nondentists contacted the FTC, and an administrative law judge found that the board’s conduct constituted an unreasonable restraint of trade. The board argued its conduct was protected from antitrust oversight by the state action doctrine, a legal rule that applies to some state board conduct. The doctrine exempts from federal antitrust scrutiny state agencies that are actively supervised by a state.
But the FTC said the board’s activities fell outside the doctrine because it is made up of market participants – dentists – and is not actively supervised by a sovereign part of the state government. The 4th U.S. Circuit Court of Appeals in 2013 ruled in favor of the FTC, and the dental board appealed to the U.S. Supreme Court.
Physician leaders, including the American Medical Association and the American Academy of Family Physicians, issued a joint brief to the high court in support of the dental board.
If the appellate ruling stands, the decisions of state medical and dental boards will be distorted by considerations of federal competition policy, to the detriment of public health, the AMA said in its brief. In addition, highly qualified practitioners who would otherwise be willing to serve on boards would likely resign or refuse to accept office to avoid personal antitrust exposure, the brief argued.
But in its opinion, the Supreme Court majority said if a state wants to rely on active market participants as regulators, it must provide active supervision to achieve antitrust immunity. The North Carolina Board of Dental Examiners did not have such supervision, the court said.
“When a state empowers a group of active market participants to decide who can participate in its market, and on what terms, the need for supervision is manifest,” the majority justices said in their opinion. “The court holds today that a state board on which a controlling number of decision makers are active market participants in the occupation the board regulates must satisfy active supervision requirement(s) in order to invoke state action antitrust immunity.”
The American Association of Nurse Anesthetists praised the decision, calling it a win for patients’ access to care. The AANA filed a joint brief to the high court in support of the FTC with several other organizations, including the American Nurses Association.
“The AANA and its co-amici had a strong interest in this case, because unnecessary restrictions on the practice of any qualified health care provider limit patient access to quality care, may increase cost, and can compromise the quality of health care delivery,” AANA President Sharon Pearce said in an interview.
“The Supreme Court decision is consistent with the arguments made by the AANA and its co-amici who urged the Supreme Court to affirm the appellate court’s decision for a number of reasons, including concerns that unsupervised state regulatory boards comprised mostly of practicing professionals have the potential of acting in their own economic self-interest by protecting their competitive position in ways not intended or authorized by the state, thus warranting oversight.”
The North Carolina Medical Society said the Supreme Court decision runs contrary to the time-tested regulatory model used nationwide by states to regulate learned professions.
“The decision focuses narrowly on antitrust law, not on the broader and far more important issue of protecting the public through effective regulation of medical practice,” the medical society said.
State medical boards will need to time to analyze the decision and decide how the ruling might affect the way in which they operate, said Dr. Humayun J. Chaudhry, president and CEO of the Federation of State Medical Boards. The FSMB plans to hold a webinar March 5 to address how state medical boards should apply the ruling.
“We recognize the importance of this decision and will now begin to make better sense of it and begin to address the open-ended questions” left by the ruling, he said in an interview. “What kind of impact [the decision has] remains to be seen.”
The AMA expressed disappointment with the decision.
“State medical boards are authorized by state governments to regulate medical licensing and medical practice in the interest of patient safety,” noted AMA President Robert M. Wah in a statement. “The AMA agrees with Justice [Samuel] Alito, speaking for the three dissenting justices, that today’s decision ‘will spawn confusion’ by creating far-reaching effects on the jurisdiction of states to regulate medicine and protect patient safety.
“The AMA will work with other physician groups to secure policy changes to reinforce long-held antitrust protections for activities conducted under state authority to protect patients,” Dr. Wah said.
On Twitter @legal_med
A U.S. Supreme Court ruling against a local dental board that attempted to stop nonprofessionals from whitening teeth could alter state medical boards’ ability to regulate the practice of medicine, some physician groups warn.
The federal high court ruled Feb. 25 that North Carolina’s state board of dental examiners violated federal antitrust laws when it tried to prevent nondentists from offering teeth-whitening services. State professional boards that regulate their competitors are only protected from antitrust scrutiny when supervised by state government, the court said in its 6-3 decision.
The ruling in North Carolina State Board of Dental Examiners v. Federal Trade Commission is disappointing and will have a broad impact on how regulatory boards function nationwide, said Bobby D. White, chief operations officer for the North Carolina Board of Dental Examiners.
“Virtually every professional regulatory board in the country will eventually have to change the way it’s structured, change the way it’s supervised, or change the activities it performs,” Mr. White said in an interview. “And since all of those changes will take time – and often legislative activity – the opinion threatens to massively disrupt professional regulation.”
Federal Trade Commission Chair Edith Ramirez said the decision correctly affirms that a state may not give private market participants unsupervised authority to suppress competition, even if they act through a formally designated “state agency.”
“We are pleased with the Supreme Court’s recognition that the antitrust laws limit the ability of market incumbents to suppress competition through state professional boards,” Ms. Ramirez said in a statement. “We will remain vigilant through our enforcement initiatives and advocacy to safeguard competition and ensure that American consumers benefit from entrepreneurial initiative.”
The ruling stems from a dispute between the North Carolina State Board of Dental Examiners and a group of unlicensed teeth whiteners who were providing services at shopping malls. From 2006 to 2009, the board issued cease-and-desist letters to the nondentists, warning them about a state ban against stain removal by unlicensed practitioners.
The nondentists contacted the FTC, and an administrative law judge found that the board’s conduct constituted an unreasonable restraint of trade. The board argued its conduct was protected from antitrust oversight by the state action doctrine, a legal rule that applies to some state board conduct. The doctrine exempts from federal antitrust scrutiny state agencies that are actively supervised by a state.
But the FTC said the board’s activities fell outside the doctrine because it is made up of market participants – dentists – and is not actively supervised by a sovereign part of the state government. The 4th U.S. Circuit Court of Appeals in 2013 ruled in favor of the FTC, and the dental board appealed to the U.S. Supreme Court.
Physician leaders, including the American Medical Association and the American Academy of Family Physicians, issued a joint brief to the high court in support of the dental board.
If the appellate ruling stands, the decisions of state medical and dental boards will be distorted by considerations of federal competition policy, to the detriment of public health, the AMA said in its brief. In addition, highly qualified practitioners who would otherwise be willing to serve on boards would likely resign or refuse to accept office to avoid personal antitrust exposure, the brief argued.
But in its opinion, the Supreme Court majority said if a state wants to rely on active market participants as regulators, it must provide active supervision to achieve antitrust immunity. The North Carolina Board of Dental Examiners did not have such supervision, the court said.
“When a state empowers a group of active market participants to decide who can participate in its market, and on what terms, the need for supervision is manifest,” the majority justices said in their opinion. “The court holds today that a state board on which a controlling number of decision makers are active market participants in the occupation the board regulates must satisfy active supervision requirement(s) in order to invoke state action antitrust immunity.”
The American Association of Nurse Anesthetists praised the decision, calling it a win for patients’ access to care. The AANA filed a joint brief to the high court in support of the FTC with several other organizations, including the American Nurses Association.
“The AANA and its co-amici had a strong interest in this case, because unnecessary restrictions on the practice of any qualified health care provider limit patient access to quality care, may increase cost, and can compromise the quality of health care delivery,” AANA President Sharon Pearce said in an interview.
“The Supreme Court decision is consistent with the arguments made by the AANA and its co-amici who urged the Supreme Court to affirm the appellate court’s decision for a number of reasons, including concerns that unsupervised state regulatory boards comprised mostly of practicing professionals have the potential of acting in their own economic self-interest by protecting their competitive position in ways not intended or authorized by the state, thus warranting oversight.”
The North Carolina Medical Society said the Supreme Court decision runs contrary to the time-tested regulatory model used nationwide by states to regulate learned professions.
“The decision focuses narrowly on antitrust law, not on the broader and far more important issue of protecting the public through effective regulation of medical practice,” the medical society said.
State medical boards will need to time to analyze the decision and decide how the ruling might affect the way in which they operate, said Dr. Humayun J. Chaudhry, president and CEO of the Federation of State Medical Boards. The FSMB plans to hold a webinar March 5 to address how state medical boards should apply the ruling.
“We recognize the importance of this decision and will now begin to make better sense of it and begin to address the open-ended questions” left by the ruling, he said in an interview. “What kind of impact [the decision has] remains to be seen.”
The AMA expressed disappointment with the decision.
“State medical boards are authorized by state governments to regulate medical licensing and medical practice in the interest of patient safety,” noted AMA President Robert M. Wah in a statement. “The AMA agrees with Justice [Samuel] Alito, speaking for the three dissenting justices, that today’s decision ‘will spawn confusion’ by creating far-reaching effects on the jurisdiction of states to regulate medicine and protect patient safety.
“The AMA will work with other physician groups to secure policy changes to reinforce long-held antitrust protections for activities conducted under state authority to protect patients,” Dr. Wah said.
On Twitter @legal_med
C. difficile burden in U.S. documented in 2011 estimates of infections, deaths
The estimated 453,000 infections and 29,300 deaths caused by Clostridium difficile in the United States in 2011 underline the importance of appropriate use of antibiotics and rigorous infection control measures in health care settings, Dr. Michael Bell, an official at the Centers for Disease Control and Prevention, said during a CDC telebriefing.
“To reduce the majority of C. difficile infections, we will need to improve how antibiotics are being prescribed in hospitals and throughout health care,” said Dr. Bell, deputy director of the division of health care quality promotion, at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases. Early diagnosis is also critical to prevent spread of C. difficile. Many infections are community acquired, and “it is essential that patients and their clinicians be aware that they need to take any diarrhea following antibiotic use very seriously,” he added.
The briefing was held to discuss the results and implications of the study published in the New England Journal of Medicine, which was supported by the CDC and the Emerging Infections Program (EIP) Cooperative Agreement between the 10 EIP sites and the CDC. In the study of 10 geographic regions in the United States in 2011, 15,461 cases were confirmed, with the estimated incidence of the infection being 453,000 (95% confidence interval, 397,100-508,500) after predictors of incidence were adjusted for, the investigators found. The estimated number of deaths from C. difficile was 29,300 (95% CI, 16,500-42,100).
Estimates for disease incidence were higher among women, whites, and patients 65 years of age or older, wrote Dr. Fernanda Lessa of the CDC, and her associates. Future efforts should focus on antibiotic use, the proper management of which may be effective in decreasing infection rates, the authors said in the report.
“Antibiotics clearly are driving this whole epidemic,” one of the study authors, Dr. Clifford McDonald of the CDC, said during the briefing. The epidemic strain in the United States, which emerged in 2000 in Pittsburgh and Montreal, is now spread globally, and accounted for about 30% of cases in this study, he added. It is transmitted more easily than other strains and causes more severe disease.
Dr. Bell said that to reduce the rate of these infections, antibiotics should be used only when needed and for as long as necessary, “and to ensure rigorous infection control in all health care settings.” The CDC’s National Strategy to Combat Antibiotic Resistant Bacteria has the potential to reduce C. difficile infections by 50%, he added.
“There’s no room for error” when infection control is considered, he added, pointing out that hand sanitizers do not kill C. difficile spores, which spread easily and are durable, “so that any breach in correct glove use, hand hygiene, or cleaning protocol can allow the spores to spread.”
The study also estimated that more than 150,000 infections were community acquired, with no documentation of inpatient exposure in the hospital. “Nonetheless, as we showed in another recent CDC study, 80% of patients with community-associated C. difficile infections did, in fact, have contact with a health care setting like a doctor’s office or a dental clinic,” generally during the 3-month period before being diagnosed, and most of the patients had also been treated with antibiotics, Dr. Bell said.
Future efforts should focus on antibiotic use, which may be effective in decreasing infection rates, Dr. Fernanda C. Lessa and her coauthors at the Centers for Disease Control and Prevention reported in The New England Journal of Medicine.
In a study of 10 geographic regions in the United States in 2011, 15,461 cases were confirmed, with the estimated incidence of the infection being 453,000 (95% confidence interval, 397,100-508,500) after predictors of incidence were adjusted for, the investigators found. The estimated number of deaths from C. difficile was 29,300 (95% CI, 16,500-42,100). Estimates for disease incidence were higher among women, whites, and patients 65 years of age or older, wrote Dr. Lessa and associates.
National efforts to address the increase in C. difficile infections include the requirement since 2013 that hospitals participating in the Centers for Medicare & Medicaid Services’ Hospital Inpatient Quality Reporting Program data on C. difficile infections to the CDC’s National Healthcare Safety Network, which has shown at least a 10% drop since 2013, Dr Bell said. Targets for reducing C. difficile infections in the United States by 2020 are being established in the National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination.
Madhu Rajaraman contributed to this report.
The estimated 453,000 infections and 29,300 deaths caused by Clostridium difficile in the United States in 2011 underline the importance of appropriate use of antibiotics and rigorous infection control measures in health care settings, Dr. Michael Bell, an official at the Centers for Disease Control and Prevention, said during a CDC telebriefing.
“To reduce the majority of C. difficile infections, we will need to improve how antibiotics are being prescribed in hospitals and throughout health care,” said Dr. Bell, deputy director of the division of health care quality promotion, at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases. Early diagnosis is also critical to prevent spread of C. difficile. Many infections are community acquired, and “it is essential that patients and their clinicians be aware that they need to take any diarrhea following antibiotic use very seriously,” he added.
The briefing was held to discuss the results and implications of the study published in the New England Journal of Medicine, which was supported by the CDC and the Emerging Infections Program (EIP) Cooperative Agreement between the 10 EIP sites and the CDC. In the study of 10 geographic regions in the United States in 2011, 15,461 cases were confirmed, with the estimated incidence of the infection being 453,000 (95% confidence interval, 397,100-508,500) after predictors of incidence were adjusted for, the investigators found. The estimated number of deaths from C. difficile was 29,300 (95% CI, 16,500-42,100).
Estimates for disease incidence were higher among women, whites, and patients 65 years of age or older, wrote Dr. Fernanda Lessa of the CDC, and her associates. Future efforts should focus on antibiotic use, the proper management of which may be effective in decreasing infection rates, the authors said in the report.
“Antibiotics clearly are driving this whole epidemic,” one of the study authors, Dr. Clifford McDonald of the CDC, said during the briefing. The epidemic strain in the United States, which emerged in 2000 in Pittsburgh and Montreal, is now spread globally, and accounted for about 30% of cases in this study, he added. It is transmitted more easily than other strains and causes more severe disease.
Dr. Bell said that to reduce the rate of these infections, antibiotics should be used only when needed and for as long as necessary, “and to ensure rigorous infection control in all health care settings.” The CDC’s National Strategy to Combat Antibiotic Resistant Bacteria has the potential to reduce C. difficile infections by 50%, he added.
“There’s no room for error” when infection control is considered, he added, pointing out that hand sanitizers do not kill C. difficile spores, which spread easily and are durable, “so that any breach in correct glove use, hand hygiene, or cleaning protocol can allow the spores to spread.”
The study also estimated that more than 150,000 infections were community acquired, with no documentation of inpatient exposure in the hospital. “Nonetheless, as we showed in another recent CDC study, 80% of patients with community-associated C. difficile infections did, in fact, have contact with a health care setting like a doctor’s office or a dental clinic,” generally during the 3-month period before being diagnosed, and most of the patients had also been treated with antibiotics, Dr. Bell said.
Future efforts should focus on antibiotic use, which may be effective in decreasing infection rates, Dr. Fernanda C. Lessa and her coauthors at the Centers for Disease Control and Prevention reported in The New England Journal of Medicine.
In a study of 10 geographic regions in the United States in 2011, 15,461 cases were confirmed, with the estimated incidence of the infection being 453,000 (95% confidence interval, 397,100-508,500) after predictors of incidence were adjusted for, the investigators found. The estimated number of deaths from C. difficile was 29,300 (95% CI, 16,500-42,100). Estimates for disease incidence were higher among women, whites, and patients 65 years of age or older, wrote Dr. Lessa and associates.
National efforts to address the increase in C. difficile infections include the requirement since 2013 that hospitals participating in the Centers for Medicare & Medicaid Services’ Hospital Inpatient Quality Reporting Program data on C. difficile infections to the CDC’s National Healthcare Safety Network, which has shown at least a 10% drop since 2013, Dr Bell said. Targets for reducing C. difficile infections in the United States by 2020 are being established in the National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination.
Madhu Rajaraman contributed to this report.
The estimated 453,000 infections and 29,300 deaths caused by Clostridium difficile in the United States in 2011 underline the importance of appropriate use of antibiotics and rigorous infection control measures in health care settings, Dr. Michael Bell, an official at the Centers for Disease Control and Prevention, said during a CDC telebriefing.
“To reduce the majority of C. difficile infections, we will need to improve how antibiotics are being prescribed in hospitals and throughout health care,” said Dr. Bell, deputy director of the division of health care quality promotion, at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases. Early diagnosis is also critical to prevent spread of C. difficile. Many infections are community acquired, and “it is essential that patients and their clinicians be aware that they need to take any diarrhea following antibiotic use very seriously,” he added.
The briefing was held to discuss the results and implications of the study published in the New England Journal of Medicine, which was supported by the CDC and the Emerging Infections Program (EIP) Cooperative Agreement between the 10 EIP sites and the CDC. In the study of 10 geographic regions in the United States in 2011, 15,461 cases were confirmed, with the estimated incidence of the infection being 453,000 (95% confidence interval, 397,100-508,500) after predictors of incidence were adjusted for, the investigators found. The estimated number of deaths from C. difficile was 29,300 (95% CI, 16,500-42,100).
Estimates for disease incidence were higher among women, whites, and patients 65 years of age or older, wrote Dr. Fernanda Lessa of the CDC, and her associates. Future efforts should focus on antibiotic use, the proper management of which may be effective in decreasing infection rates, the authors said in the report.
“Antibiotics clearly are driving this whole epidemic,” one of the study authors, Dr. Clifford McDonald of the CDC, said during the briefing. The epidemic strain in the United States, which emerged in 2000 in Pittsburgh and Montreal, is now spread globally, and accounted for about 30% of cases in this study, he added. It is transmitted more easily than other strains and causes more severe disease.
Dr. Bell said that to reduce the rate of these infections, antibiotics should be used only when needed and for as long as necessary, “and to ensure rigorous infection control in all health care settings.” The CDC’s National Strategy to Combat Antibiotic Resistant Bacteria has the potential to reduce C. difficile infections by 50%, he added.
“There’s no room for error” when infection control is considered, he added, pointing out that hand sanitizers do not kill C. difficile spores, which spread easily and are durable, “so that any breach in correct glove use, hand hygiene, or cleaning protocol can allow the spores to spread.”
The study also estimated that more than 150,000 infections were community acquired, with no documentation of inpatient exposure in the hospital. “Nonetheless, as we showed in another recent CDC study, 80% of patients with community-associated C. difficile infections did, in fact, have contact with a health care setting like a doctor’s office or a dental clinic,” generally during the 3-month period before being diagnosed, and most of the patients had also been treated with antibiotics, Dr. Bell said.
Future efforts should focus on antibiotic use, which may be effective in decreasing infection rates, Dr. Fernanda C. Lessa and her coauthors at the Centers for Disease Control and Prevention reported in The New England Journal of Medicine.
In a study of 10 geographic regions in the United States in 2011, 15,461 cases were confirmed, with the estimated incidence of the infection being 453,000 (95% confidence interval, 397,100-508,500) after predictors of incidence were adjusted for, the investigators found. The estimated number of deaths from C. difficile was 29,300 (95% CI, 16,500-42,100). Estimates for disease incidence were higher among women, whites, and patients 65 years of age or older, wrote Dr. Lessa and associates.
National efforts to address the increase in C. difficile infections include the requirement since 2013 that hospitals participating in the Centers for Medicare & Medicaid Services’ Hospital Inpatient Quality Reporting Program data on C. difficile infections to the CDC’s National Healthcare Safety Network, which has shown at least a 10% drop since 2013, Dr Bell said. Targets for reducing C. difficile infections in the United States by 2020 are being established in the National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination.
Madhu Rajaraman contributed to this report.
FROM A CDC TELEBRIEFING
Broadly implementing stroke embolectomy faces hurdles
NASHVILLE, TENN. – Results from three randomized controlled trials presented at the International Stroke Conference, plus the outcomes from a fourth trial first reported last fall, immediately established embolectomy as standard-of-care treatment for selected patients with acute ischemic stroke.
Stroke experts interviewed during the conference, however, said that making embolectomy routinely available to most U.S. stroke patients who would be candidates for the intervention will take months, if not years.
They envision challenges involving the availability of trained interventionalists, triage of patients to the right centers, and reimbursement issues as some of the obstacles to be dealt with before endovascular embolectomy aimed at removing intracerebral-artery occlusions in acute ischemic stroke patients becomes uniformly available.
Yet another challenge will arise when stroke-treatment groups that did not participate in the trials strive to replicate the success their colleagues reported by implementing the highly streamlined systems that were used in the trials for identifying appropriate stroke patients and for delivering treatment. Those systems were cited as an important reason why those studies succeeded in producing positive outcomes when similar embolectomy trials without the same efficiencies reported just a year or two ago failed to show benefit.
“The evidence makes it standard of care, but the challenge is that our systems are not set up. This is the big thing we will all go home to work on,” said Dr. Pooja Khatri, professor of neurology and director of acute stroke at the University of Cincinnati.
“You talk to everyone at this meeting, and what they want to go home and figure out is how can we deliver this care. It’s really challenging, at a myriad of levels,” said Dr. Colin P. Derdeyn, professor of neurology and director of the Center for Stroke and Cerebrovascular Disease at Washington University in St. Louis.
Growing endovascular availability
Arguably the most critical issue in rolling out endovascular stroke interventions more broadly is scaling up the number of centers that have the staff and systems in place to perform them. Clearly, the scope of providers able to deliver this treatment currently falls substantially short of what will be needed. “It’s kind of daunting to think about the [workforce] needs,” Dr. Khatri said in a talk at the conference, which was sponsored by the American Heart Association.
“In the United States, we’ve been building out a two-tier system, with comprehensive stroke centers capable of delivering this [endovascular embolectomy] treatment” and primary stroke centers capable of administering intravenous treatment with tissue plasminogen activator (TPA), the first treatment that patients eligible for embolectomy should receive, said Dr. Jeffrey L. Saver, professor of neurology and director of the stroke center at the University of California, Los Angeles, and lead investigator for one of the new embolectomy studies.
“Work groups have suggested about 60,000 U.S. stroke patients could potentially be treated with endovascular therapy, and we’d need about 300 comprehensive stroke centers to do this.” Dr. Saver estimated the current total of U.S. comprehensive stroke centers to be 75, a number that several others at the meeting pegged as more like 80, and they also noted that some centers are endovascular ready but have not received official comprehensive stroke center certification from the Joint Commission.
The extent to which availability of U.S. embolectomy remained limited through most of 2013 was apparent in data reported at the conference by Dr. Opeolu M. Adeoye, an emergency medicine physician and medical director of the telestroke program of the University of Cincinnati. During fiscal year 2013 (Oct. 2012 to Sept. 2013), 386,144 Medicare patients either older than 65 years or totally disabled had a primary hospital discharge diagnosis of stroke; of those, 5.1% had received thrombolytic therapy with intravenous TPA and 0.8% had undergone embolectomy. In a second analysis, he looked at stroke discharges and reperfusion treatments used in the 214 U.S. acute-care hospitals currently enrolled in StrokeNet, a program begun in 2013 by the National Institute of Neurological Disorders and Stroke to organize U.S. centers interested in participating in stroke trials.
During the same period, the 214 StrokeNet hospitals discharged 44,282 Medicare eligible patients who met the same age or disability criteria, with a TPA-treatment rate of 7.9% and an endovascular treatment rate of 2.2%. Although the StrokeNet hospitals treated roughly 11% of U.S. stroke patients in the specified demographic, they administered about 20% of the reperfusion treatment, Dr. Adeoye reported. He also highlighted that the 7.9% rate of TPA treatment among the StrokeNet hospitals correlated well with prior estimates that 6%-11% of stroke patients fulfill existing criteria for TPA treatment
A wide disparity existed in the rate of reperfusion use among StrokeNet hospitals. Sixty-seven hospitals, 31% of the StrokeNet group, treated at least 20 stroke patients with TPA during the study period, while 100 (47%) of the StrokeNet hospitals treated fewer than 10 acute stroke patients. The rate of those doing embolectomies was substantially lower, with 10 hospitals (5%) doing at least 20 endovascular procedures while 90% did fewer than 10.
Although Dr. Adeoye expressed confidence that the number of U.S. centers doing embolectomy cases will “change rapidly” following the new reports documenting the efficacy of the approach, he also acknowledged the challenges of growing the number of high-volume endovascular centers.
Centers that have been equivocal about embolectomy will now start doing it in a more concerted way, he predicted, but if cases get spread out and some sites do only a few patients a year, the quality of the procedures may suffer. “The more cases a site does, the better,” he noted, adding that regions that funnel all their stroke patients to a single endovascular site “do really well.”
“Right now, many hospitals want to do everything to get [fully] reimbursed and not send their patients down the line. There is a financial incentive to build up the stroke service at every hospital,” Dr. Derdeyn noted.
Another aspect to sorting out which centers start offering endovascular treatment will be the need to locate them in a rational way, as happened with trauma centers. Until now, placement of comprehensive stroke centers often depended on hospitals developing the capability as a marketing tool, noted Dr. Larry B. Goldstein, professor of neurology and director of the stroke center at Duke University in Durham, N.C. A hospital might achieve comprehensive stroke center certification, so a second center a few blocks away then follows suit seemingly to keep pace in a public-relations battle for cachet. The result has been an irrational clustering of centers with endovascular capability. He cited the situation in Cleveland, where comprehensive centers run by the Cleveland Clinic and Case Western stand a few dozen feet apart.
Challenges for triage
An analysis published last year by Dr. Adeoye and his colleagues showed that 56% of the U.S. population lived within a 60-minute drive of a hospital able to administer endovascular stroke treatment; by air, 85% had that access (Stroke 2014;45:3019-24). For TPA, 81% of people lived within a 60-minute drive of a center able to administer intravenous lytic treatment and 97% could reach these hospitals within an hour by air. While those numbers sound promising, though, fulfilling that potential depends on getting the right patients to the right hospitals.
Patient triage is perhaps the most vexing issue created by embolectomy’s success. For at least the short term, a limited number of centers will have the staffing and capacity to deliver endovascular embolectomy on a 24/7 basis to acute ischemic stroke patients who have a proximal blockage in a large cerebral artery. The relatively small number of sites able to offer embolectomy, and the much larger number of sites able to administer thrombolytic therapy with TPA, set the stage for some possible tension, or at least confusion, within communities over where an ambulance should bring an acute ischemic stroke patient.
“In some places they have trained the EMS [emergency medical services] to recognize severe strokes that are likely to benefit [from embolectomy], and they take those patients to places with endovascular capability. But there are some states with laws against doing this. There are major issues when EMS bypasses hospitals,” Dr. Derdeyn noted. “That’s the million-dollar question: How do you identify the stroke patients [with severe strokes who would benefit from embolectomy] and get them to where they need to go.” Like Dr. Adeoye, Dr. Derdeyn believes that endovascular treatment for stroke needs to be centralized at a relatively small number of high-volume centers.
“You can imagine that the fastest way to get stroke patients treated is to have them all go to one place, but that is much easier said than done,” Dr. Khatri said.
“Stent retrievers get cerebral arteries open, but that is not the biggest challenge. For the short term, the key issue is to get the correct patients to the correct hospitals where they can be treated by the correct team,” said Dr. Mayank Goyal, professor of diagnostic imaging at the University of Calgary (Alta.) and lead investigator for two of the three trials presented at the conference.
“You need a neurologist capable of deciding whether it really is a stroke, and pretty high-level imaging to identify the large-vessel occlusions that will benefit. Acquiring a CT angiography (CTA) image of the brain is a push-button process, but figuring out what the CTA says is not push button, especially the more sophisticated perfusion CT imaging to assess collateral circulation. I don’t see this capability happening in every catheterization laboratory,” Dr. Derdeyn said in an interview.
Another issue is volume. “Telemedicine may allow broader use of [more sophisticated] imaging, but if a place is only doing 20 endovascular procedures a year, they won’t have the best outcomes. Most small hospitals that today give patients TPA see 20 cases or fewer a year, and perhaps 5 patients will have a large-vessel occlusion,” Dr. Derdeyn said.
Before the new reports documenting the safety and efficacy of endovascular treatment, “we did not have the justification to bypass primary stroke centers and take patients directly to comprehensive stroke centers,” Dr. Khatri said. Now, “there is clear evidence that patients with severe strokes should not go to the nearby primary stroke center” but instead head directly for the centers capable of performing embolectomy. But Dr. Khatri also acknowledged that a complex calculation is needed to balance the trade off: Is it better to take a stroke patient more quickly to a nearby hospital that can only start TPA and perhaps later forward the patient to an embolectomy-ready hospital, or to transport the patient somewhat further to a facility able to deliver both TPA and embolectomy?
Dr. Khatri said that, in the Cincinnati area, “we have scheduled a retreat for March to start to plan how this will happen.” Her region includes just one comprehensive stroke center that already performs endovascular treatments for stroke, at the University of Cincinnati, which sits amid 16 other hospitals that perform acute stroke care and can administer TPA. “Ambulance-based triage will be a big issue,” she predicted.
Other aspects of improved triage will be training ambulance personal to better identify the more severe stroke patients who will most likely need endovascular treatment and improving communication between ambulance crews and receiving hospitals to further speed up a process that depends on quick treatment to get the best outcomes.
The ideal is “having paramedics call and tell us what is happening [in their ambulance] and give us as much information as possible so we can start planning for the patient’s arrival. Most hospitals don’t do this now; relatively few have their system well organized,” Dr. Goyal said in an interview. A finely orchestrated emergency transport system and hospital-based stroke team was part of the program developed at the University of Calgary by Dr. Goyal and his associates and which they credited with contributing to the successful embolectomy trial they led, called ESCAPE (Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times)(N. Engl. J. Med. 2015 Feb. 11 [doi:10.1056/NEJMoa1414905]). Dr. Goyal said that he is now visiting hospitals around the world to assist them in setting up stroke-response systems that mimic what was successful in Calgary and the other centers that participated in ESCAPE.
Improving triage with better screening
A key to improved ambulance triage will be identifying a simple, evidence-based method for assessing stroke severity that ambulance personnel can use to determine what sort of care a patient needs and where the patient needs to go to. Although a couple of U.S. sites have begun pilot studies of field-based CT units that allow stroke patients to undergo imaging-based assessment in the field, clinical evaluation remains the main tool used in the ambulance.
One possible tool is the Los Angeles Motor Scale (LAMS), a stroke-assessment scoring system developed by Dr. Saver and his associates for ambulance use about a decade ago (Prehosp. Emerg. Care 2004;8:46-50). “A LAMS score of 4 or 5 [on a scale of 0-5] is a good starting point, and with time it might improve,” Dr. Goyal said.
The National Institutes of Health Stroke Scale (NIHSS) is a clinical assessment tool not designed for prehospital use, but a new analysis reported at the meeting showed value in using the NIHSS to identify stroke patients who are good candidates for endovascular treatment, further suggesting that a simple screening tool could potentially work in the ambulance to identify patients who probably need embolectomy.
The new analysis combined data from two randomized trials: The IMS (Interventional Management of Stroke) III trial, the results of which, published in early 2013, showed no incremental benefit of endovascular therapy plus TPA over TPA alone for patients with acute ischemic stroke (N. Engl. J. Med. 2013;368:893-903); and the MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) trial, the results of which, published in January, showed a significant incremental benefit from endovascular treatment – it was the first of the four studies recently reported to show this benefit (N. Engl. J. Med. 2015;372:11-20).
The combined data included all patients from both studies with a NIHSS score of at least 20, indicating a very severe stroke. This produced a total of 342 patients, of whom 191 received intravenous TPA plus endovascular treatment and 152 received only TPA. After 90 days, 24% of the patients treated with endovascular treatment and 14% of those treated only with TPA had a modified Rankin Scale score of 0-2, indicating no or limited disability, Dr. Joseph P. Broderick reported at the conference. After adjustments for age and other potential confounders, treatment with endovascular therapy produced a statistically significant 85% improvement in patients achieving an acceptable modified Rankin Scale score at 90 days, said Dr. Broderick, professor of neurology and director of the neuroscience institute at the University of Cincinnati.
“The NIHSS score is a surrogate for clot size. It is an imperfect measure, especially at lower levels, but when the score is 20 or higher it means the patient has a big clot” that will likely not fully respond to TPA but potentially will respond to embolectomy, Dr. Broderick said in an interview. “A patient with a NIHSS score of 20 or higher has about a 95% risk of having an ongoing major artery occlusion despite TPA treatment.”
“The challenge is that we don’t have a fully validated [prehospital] scoring system. Several groups are trying to create one; in the meantime we may come up with certain clinical thresholds” that can reliably guide ambulance crews on the best place to take each stroke patient, Dr. Khatri said.
Dr. Khatri has received research support from Penumbra and Genentech. Dr. Derdeyn has received honoraria from Penumbra and holds equity in Pulse Therapeutics. Dr. Saver has been a consultant to and received research support from Covidien. Dr. Adeoye has been a speaker for Genentech. Dr. Goldstein had no disclosures. Dr. Goyal has been a consultant to and received research support from Covidien and holds a patent on using CT angiography to diagnose stroke. Dr. Broderick has received research support from Genentech.
[email protected]
On Twitter @mitchelzoler
NASHVILLE, TENN. – Results from three randomized controlled trials presented at the International Stroke Conference, plus the outcomes from a fourth trial first reported last fall, immediately established embolectomy as standard-of-care treatment for selected patients with acute ischemic stroke.
Stroke experts interviewed during the conference, however, said that making embolectomy routinely available to most U.S. stroke patients who would be candidates for the intervention will take months, if not years.
They envision challenges involving the availability of trained interventionalists, triage of patients to the right centers, and reimbursement issues as some of the obstacles to be dealt with before endovascular embolectomy aimed at removing intracerebral-artery occlusions in acute ischemic stroke patients becomes uniformly available.
Yet another challenge will arise when stroke-treatment groups that did not participate in the trials strive to replicate the success their colleagues reported by implementing the highly streamlined systems that were used in the trials for identifying appropriate stroke patients and for delivering treatment. Those systems were cited as an important reason why those studies succeeded in producing positive outcomes when similar embolectomy trials without the same efficiencies reported just a year or two ago failed to show benefit.
“The evidence makes it standard of care, but the challenge is that our systems are not set up. This is the big thing we will all go home to work on,” said Dr. Pooja Khatri, professor of neurology and director of acute stroke at the University of Cincinnati.
“You talk to everyone at this meeting, and what they want to go home and figure out is how can we deliver this care. It’s really challenging, at a myriad of levels,” said Dr. Colin P. Derdeyn, professor of neurology and director of the Center for Stroke and Cerebrovascular Disease at Washington University in St. Louis.
Growing endovascular availability
Arguably the most critical issue in rolling out endovascular stroke interventions more broadly is scaling up the number of centers that have the staff and systems in place to perform them. Clearly, the scope of providers able to deliver this treatment currently falls substantially short of what will be needed. “It’s kind of daunting to think about the [workforce] needs,” Dr. Khatri said in a talk at the conference, which was sponsored by the American Heart Association.
“In the United States, we’ve been building out a two-tier system, with comprehensive stroke centers capable of delivering this [endovascular embolectomy] treatment” and primary stroke centers capable of administering intravenous treatment with tissue plasminogen activator (TPA), the first treatment that patients eligible for embolectomy should receive, said Dr. Jeffrey L. Saver, professor of neurology and director of the stroke center at the University of California, Los Angeles, and lead investigator for one of the new embolectomy studies.
“Work groups have suggested about 60,000 U.S. stroke patients could potentially be treated with endovascular therapy, and we’d need about 300 comprehensive stroke centers to do this.” Dr. Saver estimated the current total of U.S. comprehensive stroke centers to be 75, a number that several others at the meeting pegged as more like 80, and they also noted that some centers are endovascular ready but have not received official comprehensive stroke center certification from the Joint Commission.
The extent to which availability of U.S. embolectomy remained limited through most of 2013 was apparent in data reported at the conference by Dr. Opeolu M. Adeoye, an emergency medicine physician and medical director of the telestroke program of the University of Cincinnati. During fiscal year 2013 (Oct. 2012 to Sept. 2013), 386,144 Medicare patients either older than 65 years or totally disabled had a primary hospital discharge diagnosis of stroke; of those, 5.1% had received thrombolytic therapy with intravenous TPA and 0.8% had undergone embolectomy. In a second analysis, he looked at stroke discharges and reperfusion treatments used in the 214 U.S. acute-care hospitals currently enrolled in StrokeNet, a program begun in 2013 by the National Institute of Neurological Disorders and Stroke to organize U.S. centers interested in participating in stroke trials.
During the same period, the 214 StrokeNet hospitals discharged 44,282 Medicare eligible patients who met the same age or disability criteria, with a TPA-treatment rate of 7.9% and an endovascular treatment rate of 2.2%. Although the StrokeNet hospitals treated roughly 11% of U.S. stroke patients in the specified demographic, they administered about 20% of the reperfusion treatment, Dr. Adeoye reported. He also highlighted that the 7.9% rate of TPA treatment among the StrokeNet hospitals correlated well with prior estimates that 6%-11% of stroke patients fulfill existing criteria for TPA treatment
A wide disparity existed in the rate of reperfusion use among StrokeNet hospitals. Sixty-seven hospitals, 31% of the StrokeNet group, treated at least 20 stroke patients with TPA during the study period, while 100 (47%) of the StrokeNet hospitals treated fewer than 10 acute stroke patients. The rate of those doing embolectomies was substantially lower, with 10 hospitals (5%) doing at least 20 endovascular procedures while 90% did fewer than 10.
Although Dr. Adeoye expressed confidence that the number of U.S. centers doing embolectomy cases will “change rapidly” following the new reports documenting the efficacy of the approach, he also acknowledged the challenges of growing the number of high-volume endovascular centers.
Centers that have been equivocal about embolectomy will now start doing it in a more concerted way, he predicted, but if cases get spread out and some sites do only a few patients a year, the quality of the procedures may suffer. “The more cases a site does, the better,” he noted, adding that regions that funnel all their stroke patients to a single endovascular site “do really well.”
“Right now, many hospitals want to do everything to get [fully] reimbursed and not send their patients down the line. There is a financial incentive to build up the stroke service at every hospital,” Dr. Derdeyn noted.
Another aspect to sorting out which centers start offering endovascular treatment will be the need to locate them in a rational way, as happened with trauma centers. Until now, placement of comprehensive stroke centers often depended on hospitals developing the capability as a marketing tool, noted Dr. Larry B. Goldstein, professor of neurology and director of the stroke center at Duke University in Durham, N.C. A hospital might achieve comprehensive stroke center certification, so a second center a few blocks away then follows suit seemingly to keep pace in a public-relations battle for cachet. The result has been an irrational clustering of centers with endovascular capability. He cited the situation in Cleveland, where comprehensive centers run by the Cleveland Clinic and Case Western stand a few dozen feet apart.
Challenges for triage
An analysis published last year by Dr. Adeoye and his colleagues showed that 56% of the U.S. population lived within a 60-minute drive of a hospital able to administer endovascular stroke treatment; by air, 85% had that access (Stroke 2014;45:3019-24). For TPA, 81% of people lived within a 60-minute drive of a center able to administer intravenous lytic treatment and 97% could reach these hospitals within an hour by air. While those numbers sound promising, though, fulfilling that potential depends on getting the right patients to the right hospitals.
Patient triage is perhaps the most vexing issue created by embolectomy’s success. For at least the short term, a limited number of centers will have the staffing and capacity to deliver endovascular embolectomy on a 24/7 basis to acute ischemic stroke patients who have a proximal blockage in a large cerebral artery. The relatively small number of sites able to offer embolectomy, and the much larger number of sites able to administer thrombolytic therapy with TPA, set the stage for some possible tension, or at least confusion, within communities over where an ambulance should bring an acute ischemic stroke patient.
“In some places they have trained the EMS [emergency medical services] to recognize severe strokes that are likely to benefit [from embolectomy], and they take those patients to places with endovascular capability. But there are some states with laws against doing this. There are major issues when EMS bypasses hospitals,” Dr. Derdeyn noted. “That’s the million-dollar question: How do you identify the stroke patients [with severe strokes who would benefit from embolectomy] and get them to where they need to go.” Like Dr. Adeoye, Dr. Derdeyn believes that endovascular treatment for stroke needs to be centralized at a relatively small number of high-volume centers.
“You can imagine that the fastest way to get stroke patients treated is to have them all go to one place, but that is much easier said than done,” Dr. Khatri said.
“Stent retrievers get cerebral arteries open, but that is not the biggest challenge. For the short term, the key issue is to get the correct patients to the correct hospitals where they can be treated by the correct team,” said Dr. Mayank Goyal, professor of diagnostic imaging at the University of Calgary (Alta.) and lead investigator for two of the three trials presented at the conference.
“You need a neurologist capable of deciding whether it really is a stroke, and pretty high-level imaging to identify the large-vessel occlusions that will benefit. Acquiring a CT angiography (CTA) image of the brain is a push-button process, but figuring out what the CTA says is not push button, especially the more sophisticated perfusion CT imaging to assess collateral circulation. I don’t see this capability happening in every catheterization laboratory,” Dr. Derdeyn said in an interview.
Another issue is volume. “Telemedicine may allow broader use of [more sophisticated] imaging, but if a place is only doing 20 endovascular procedures a year, they won’t have the best outcomes. Most small hospitals that today give patients TPA see 20 cases or fewer a year, and perhaps 5 patients will have a large-vessel occlusion,” Dr. Derdeyn said.
Before the new reports documenting the safety and efficacy of endovascular treatment, “we did not have the justification to bypass primary stroke centers and take patients directly to comprehensive stroke centers,” Dr. Khatri said. Now, “there is clear evidence that patients with severe strokes should not go to the nearby primary stroke center” but instead head directly for the centers capable of performing embolectomy. But Dr. Khatri also acknowledged that a complex calculation is needed to balance the trade off: Is it better to take a stroke patient more quickly to a nearby hospital that can only start TPA and perhaps later forward the patient to an embolectomy-ready hospital, or to transport the patient somewhat further to a facility able to deliver both TPA and embolectomy?
Dr. Khatri said that, in the Cincinnati area, “we have scheduled a retreat for March to start to plan how this will happen.” Her region includes just one comprehensive stroke center that already performs endovascular treatments for stroke, at the University of Cincinnati, which sits amid 16 other hospitals that perform acute stroke care and can administer TPA. “Ambulance-based triage will be a big issue,” she predicted.
Other aspects of improved triage will be training ambulance personal to better identify the more severe stroke patients who will most likely need endovascular treatment and improving communication between ambulance crews and receiving hospitals to further speed up a process that depends on quick treatment to get the best outcomes.
The ideal is “having paramedics call and tell us what is happening [in their ambulance] and give us as much information as possible so we can start planning for the patient’s arrival. Most hospitals don’t do this now; relatively few have their system well organized,” Dr. Goyal said in an interview. A finely orchestrated emergency transport system and hospital-based stroke team was part of the program developed at the University of Calgary by Dr. Goyal and his associates and which they credited with contributing to the successful embolectomy trial they led, called ESCAPE (Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times)(N. Engl. J. Med. 2015 Feb. 11 [doi:10.1056/NEJMoa1414905]). Dr. Goyal said that he is now visiting hospitals around the world to assist them in setting up stroke-response systems that mimic what was successful in Calgary and the other centers that participated in ESCAPE.
Improving triage with better screening
A key to improved ambulance triage will be identifying a simple, evidence-based method for assessing stroke severity that ambulance personnel can use to determine what sort of care a patient needs and where the patient needs to go to. Although a couple of U.S. sites have begun pilot studies of field-based CT units that allow stroke patients to undergo imaging-based assessment in the field, clinical evaluation remains the main tool used in the ambulance.
One possible tool is the Los Angeles Motor Scale (LAMS), a stroke-assessment scoring system developed by Dr. Saver and his associates for ambulance use about a decade ago (Prehosp. Emerg. Care 2004;8:46-50). “A LAMS score of 4 or 5 [on a scale of 0-5] is a good starting point, and with time it might improve,” Dr. Goyal said.
The National Institutes of Health Stroke Scale (NIHSS) is a clinical assessment tool not designed for prehospital use, but a new analysis reported at the meeting showed value in using the NIHSS to identify stroke patients who are good candidates for endovascular treatment, further suggesting that a simple screening tool could potentially work in the ambulance to identify patients who probably need embolectomy.
The new analysis combined data from two randomized trials: The IMS (Interventional Management of Stroke) III trial, the results of which, published in early 2013, showed no incremental benefit of endovascular therapy plus TPA over TPA alone for patients with acute ischemic stroke (N. Engl. J. Med. 2013;368:893-903); and the MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) trial, the results of which, published in January, showed a significant incremental benefit from endovascular treatment – it was the first of the four studies recently reported to show this benefit (N. Engl. J. Med. 2015;372:11-20).
The combined data included all patients from both studies with a NIHSS score of at least 20, indicating a very severe stroke. This produced a total of 342 patients, of whom 191 received intravenous TPA plus endovascular treatment and 152 received only TPA. After 90 days, 24% of the patients treated with endovascular treatment and 14% of those treated only with TPA had a modified Rankin Scale score of 0-2, indicating no or limited disability, Dr. Joseph P. Broderick reported at the conference. After adjustments for age and other potential confounders, treatment with endovascular therapy produced a statistically significant 85% improvement in patients achieving an acceptable modified Rankin Scale score at 90 days, said Dr. Broderick, professor of neurology and director of the neuroscience institute at the University of Cincinnati.
“The NIHSS score is a surrogate for clot size. It is an imperfect measure, especially at lower levels, but when the score is 20 or higher it means the patient has a big clot” that will likely not fully respond to TPA but potentially will respond to embolectomy, Dr. Broderick said in an interview. “A patient with a NIHSS score of 20 or higher has about a 95% risk of having an ongoing major artery occlusion despite TPA treatment.”
“The challenge is that we don’t have a fully validated [prehospital] scoring system. Several groups are trying to create one; in the meantime we may come up with certain clinical thresholds” that can reliably guide ambulance crews on the best place to take each stroke patient, Dr. Khatri said.
Dr. Khatri has received research support from Penumbra and Genentech. Dr. Derdeyn has received honoraria from Penumbra and holds equity in Pulse Therapeutics. Dr. Saver has been a consultant to and received research support from Covidien. Dr. Adeoye has been a speaker for Genentech. Dr. Goldstein had no disclosures. Dr. Goyal has been a consultant to and received research support from Covidien and holds a patent on using CT angiography to diagnose stroke. Dr. Broderick has received research support from Genentech.
[email protected]
On Twitter @mitchelzoler
NASHVILLE, TENN. – Results from three randomized controlled trials presented at the International Stroke Conference, plus the outcomes from a fourth trial first reported last fall, immediately established embolectomy as standard-of-care treatment for selected patients with acute ischemic stroke.
Stroke experts interviewed during the conference, however, said that making embolectomy routinely available to most U.S. stroke patients who would be candidates for the intervention will take months, if not years.
They envision challenges involving the availability of trained interventionalists, triage of patients to the right centers, and reimbursement issues as some of the obstacles to be dealt with before endovascular embolectomy aimed at removing intracerebral-artery occlusions in acute ischemic stroke patients becomes uniformly available.
Yet another challenge will arise when stroke-treatment groups that did not participate in the trials strive to replicate the success their colleagues reported by implementing the highly streamlined systems that were used in the trials for identifying appropriate stroke patients and for delivering treatment. Those systems were cited as an important reason why those studies succeeded in producing positive outcomes when similar embolectomy trials without the same efficiencies reported just a year or two ago failed to show benefit.
“The evidence makes it standard of care, but the challenge is that our systems are not set up. This is the big thing we will all go home to work on,” said Dr. Pooja Khatri, professor of neurology and director of acute stroke at the University of Cincinnati.
“You talk to everyone at this meeting, and what they want to go home and figure out is how can we deliver this care. It’s really challenging, at a myriad of levels,” said Dr. Colin P. Derdeyn, professor of neurology and director of the Center for Stroke and Cerebrovascular Disease at Washington University in St. Louis.
Growing endovascular availability
Arguably the most critical issue in rolling out endovascular stroke interventions more broadly is scaling up the number of centers that have the staff and systems in place to perform them. Clearly, the scope of providers able to deliver this treatment currently falls substantially short of what will be needed. “It’s kind of daunting to think about the [workforce] needs,” Dr. Khatri said in a talk at the conference, which was sponsored by the American Heart Association.
“In the United States, we’ve been building out a two-tier system, with comprehensive stroke centers capable of delivering this [endovascular embolectomy] treatment” and primary stroke centers capable of administering intravenous treatment with tissue plasminogen activator (TPA), the first treatment that patients eligible for embolectomy should receive, said Dr. Jeffrey L. Saver, professor of neurology and director of the stroke center at the University of California, Los Angeles, and lead investigator for one of the new embolectomy studies.
“Work groups have suggested about 60,000 U.S. stroke patients could potentially be treated with endovascular therapy, and we’d need about 300 comprehensive stroke centers to do this.” Dr. Saver estimated the current total of U.S. comprehensive stroke centers to be 75, a number that several others at the meeting pegged as more like 80, and they also noted that some centers are endovascular ready but have not received official comprehensive stroke center certification from the Joint Commission.
The extent to which availability of U.S. embolectomy remained limited through most of 2013 was apparent in data reported at the conference by Dr. Opeolu M. Adeoye, an emergency medicine physician and medical director of the telestroke program of the University of Cincinnati. During fiscal year 2013 (Oct. 2012 to Sept. 2013), 386,144 Medicare patients either older than 65 years or totally disabled had a primary hospital discharge diagnosis of stroke; of those, 5.1% had received thrombolytic therapy with intravenous TPA and 0.8% had undergone embolectomy. In a second analysis, he looked at stroke discharges and reperfusion treatments used in the 214 U.S. acute-care hospitals currently enrolled in StrokeNet, a program begun in 2013 by the National Institute of Neurological Disorders and Stroke to organize U.S. centers interested in participating in stroke trials.
During the same period, the 214 StrokeNet hospitals discharged 44,282 Medicare eligible patients who met the same age or disability criteria, with a TPA-treatment rate of 7.9% and an endovascular treatment rate of 2.2%. Although the StrokeNet hospitals treated roughly 11% of U.S. stroke patients in the specified demographic, they administered about 20% of the reperfusion treatment, Dr. Adeoye reported. He also highlighted that the 7.9% rate of TPA treatment among the StrokeNet hospitals correlated well with prior estimates that 6%-11% of stroke patients fulfill existing criteria for TPA treatment
A wide disparity existed in the rate of reperfusion use among StrokeNet hospitals. Sixty-seven hospitals, 31% of the StrokeNet group, treated at least 20 stroke patients with TPA during the study period, while 100 (47%) of the StrokeNet hospitals treated fewer than 10 acute stroke patients. The rate of those doing embolectomies was substantially lower, with 10 hospitals (5%) doing at least 20 endovascular procedures while 90% did fewer than 10.
Although Dr. Adeoye expressed confidence that the number of U.S. centers doing embolectomy cases will “change rapidly” following the new reports documenting the efficacy of the approach, he also acknowledged the challenges of growing the number of high-volume endovascular centers.
Centers that have been equivocal about embolectomy will now start doing it in a more concerted way, he predicted, but if cases get spread out and some sites do only a few patients a year, the quality of the procedures may suffer. “The more cases a site does, the better,” he noted, adding that regions that funnel all their stroke patients to a single endovascular site “do really well.”
“Right now, many hospitals want to do everything to get [fully] reimbursed and not send their patients down the line. There is a financial incentive to build up the stroke service at every hospital,” Dr. Derdeyn noted.
Another aspect to sorting out which centers start offering endovascular treatment will be the need to locate them in a rational way, as happened with trauma centers. Until now, placement of comprehensive stroke centers often depended on hospitals developing the capability as a marketing tool, noted Dr. Larry B. Goldstein, professor of neurology and director of the stroke center at Duke University in Durham, N.C. A hospital might achieve comprehensive stroke center certification, so a second center a few blocks away then follows suit seemingly to keep pace in a public-relations battle for cachet. The result has been an irrational clustering of centers with endovascular capability. He cited the situation in Cleveland, where comprehensive centers run by the Cleveland Clinic and Case Western stand a few dozen feet apart.
Challenges for triage
An analysis published last year by Dr. Adeoye and his colleagues showed that 56% of the U.S. population lived within a 60-minute drive of a hospital able to administer endovascular stroke treatment; by air, 85% had that access (Stroke 2014;45:3019-24). For TPA, 81% of people lived within a 60-minute drive of a center able to administer intravenous lytic treatment and 97% could reach these hospitals within an hour by air. While those numbers sound promising, though, fulfilling that potential depends on getting the right patients to the right hospitals.
Patient triage is perhaps the most vexing issue created by embolectomy’s success. For at least the short term, a limited number of centers will have the staffing and capacity to deliver endovascular embolectomy on a 24/7 basis to acute ischemic stroke patients who have a proximal blockage in a large cerebral artery. The relatively small number of sites able to offer embolectomy, and the much larger number of sites able to administer thrombolytic therapy with TPA, set the stage for some possible tension, or at least confusion, within communities over where an ambulance should bring an acute ischemic stroke patient.
“In some places they have trained the EMS [emergency medical services] to recognize severe strokes that are likely to benefit [from embolectomy], and they take those patients to places with endovascular capability. But there are some states with laws against doing this. There are major issues when EMS bypasses hospitals,” Dr. Derdeyn noted. “That’s the million-dollar question: How do you identify the stroke patients [with severe strokes who would benefit from embolectomy] and get them to where they need to go.” Like Dr. Adeoye, Dr. Derdeyn believes that endovascular treatment for stroke needs to be centralized at a relatively small number of high-volume centers.
“You can imagine that the fastest way to get stroke patients treated is to have them all go to one place, but that is much easier said than done,” Dr. Khatri said.
“Stent retrievers get cerebral arteries open, but that is not the biggest challenge. For the short term, the key issue is to get the correct patients to the correct hospitals where they can be treated by the correct team,” said Dr. Mayank Goyal, professor of diagnostic imaging at the University of Calgary (Alta.) and lead investigator for two of the three trials presented at the conference.
“You need a neurologist capable of deciding whether it really is a stroke, and pretty high-level imaging to identify the large-vessel occlusions that will benefit. Acquiring a CT angiography (CTA) image of the brain is a push-button process, but figuring out what the CTA says is not push button, especially the more sophisticated perfusion CT imaging to assess collateral circulation. I don’t see this capability happening in every catheterization laboratory,” Dr. Derdeyn said in an interview.
Another issue is volume. “Telemedicine may allow broader use of [more sophisticated] imaging, but if a place is only doing 20 endovascular procedures a year, they won’t have the best outcomes. Most small hospitals that today give patients TPA see 20 cases or fewer a year, and perhaps 5 patients will have a large-vessel occlusion,” Dr. Derdeyn said.
Before the new reports documenting the safety and efficacy of endovascular treatment, “we did not have the justification to bypass primary stroke centers and take patients directly to comprehensive stroke centers,” Dr. Khatri said. Now, “there is clear evidence that patients with severe strokes should not go to the nearby primary stroke center” but instead head directly for the centers capable of performing embolectomy. But Dr. Khatri also acknowledged that a complex calculation is needed to balance the trade off: Is it better to take a stroke patient more quickly to a nearby hospital that can only start TPA and perhaps later forward the patient to an embolectomy-ready hospital, or to transport the patient somewhat further to a facility able to deliver both TPA and embolectomy?
Dr. Khatri said that, in the Cincinnati area, “we have scheduled a retreat for March to start to plan how this will happen.” Her region includes just one comprehensive stroke center that already performs endovascular treatments for stroke, at the University of Cincinnati, which sits amid 16 other hospitals that perform acute stroke care and can administer TPA. “Ambulance-based triage will be a big issue,” she predicted.
Other aspects of improved triage will be training ambulance personal to better identify the more severe stroke patients who will most likely need endovascular treatment and improving communication between ambulance crews and receiving hospitals to further speed up a process that depends on quick treatment to get the best outcomes.
The ideal is “having paramedics call and tell us what is happening [in their ambulance] and give us as much information as possible so we can start planning for the patient’s arrival. Most hospitals don’t do this now; relatively few have their system well organized,” Dr. Goyal said in an interview. A finely orchestrated emergency transport system and hospital-based stroke team was part of the program developed at the University of Calgary by Dr. Goyal and his associates and which they credited with contributing to the successful embolectomy trial they led, called ESCAPE (Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times)(N. Engl. J. Med. 2015 Feb. 11 [doi:10.1056/NEJMoa1414905]). Dr. Goyal said that he is now visiting hospitals around the world to assist them in setting up stroke-response systems that mimic what was successful in Calgary and the other centers that participated in ESCAPE.
Improving triage with better screening
A key to improved ambulance triage will be identifying a simple, evidence-based method for assessing stroke severity that ambulance personnel can use to determine what sort of care a patient needs and where the patient needs to go to. Although a couple of U.S. sites have begun pilot studies of field-based CT units that allow stroke patients to undergo imaging-based assessment in the field, clinical evaluation remains the main tool used in the ambulance.
One possible tool is the Los Angeles Motor Scale (LAMS), a stroke-assessment scoring system developed by Dr. Saver and his associates for ambulance use about a decade ago (Prehosp. Emerg. Care 2004;8:46-50). “A LAMS score of 4 or 5 [on a scale of 0-5] is a good starting point, and with time it might improve,” Dr. Goyal said.
The National Institutes of Health Stroke Scale (NIHSS) is a clinical assessment tool not designed for prehospital use, but a new analysis reported at the meeting showed value in using the NIHSS to identify stroke patients who are good candidates for endovascular treatment, further suggesting that a simple screening tool could potentially work in the ambulance to identify patients who probably need embolectomy.
The new analysis combined data from two randomized trials: The IMS (Interventional Management of Stroke) III trial, the results of which, published in early 2013, showed no incremental benefit of endovascular therapy plus TPA over TPA alone for patients with acute ischemic stroke (N. Engl. J. Med. 2013;368:893-903); and the MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) trial, the results of which, published in January, showed a significant incremental benefit from endovascular treatment – it was the first of the four studies recently reported to show this benefit (N. Engl. J. Med. 2015;372:11-20).
The combined data included all patients from both studies with a NIHSS score of at least 20, indicating a very severe stroke. This produced a total of 342 patients, of whom 191 received intravenous TPA plus endovascular treatment and 152 received only TPA. After 90 days, 24% of the patients treated with endovascular treatment and 14% of those treated only with TPA had a modified Rankin Scale score of 0-2, indicating no or limited disability, Dr. Joseph P. Broderick reported at the conference. After adjustments for age and other potential confounders, treatment with endovascular therapy produced a statistically significant 85% improvement in patients achieving an acceptable modified Rankin Scale score at 90 days, said Dr. Broderick, professor of neurology and director of the neuroscience institute at the University of Cincinnati.
“The NIHSS score is a surrogate for clot size. It is an imperfect measure, especially at lower levels, but when the score is 20 or higher it means the patient has a big clot” that will likely not fully respond to TPA but potentially will respond to embolectomy, Dr. Broderick said in an interview. “A patient with a NIHSS score of 20 or higher has about a 95% risk of having an ongoing major artery occlusion despite TPA treatment.”
“The challenge is that we don’t have a fully validated [prehospital] scoring system. Several groups are trying to create one; in the meantime we may come up with certain clinical thresholds” that can reliably guide ambulance crews on the best place to take each stroke patient, Dr. Khatri said.
Dr. Khatri has received research support from Penumbra and Genentech. Dr. Derdeyn has received honoraria from Penumbra and holds equity in Pulse Therapeutics. Dr. Saver has been a consultant to and received research support from Covidien. Dr. Adeoye has been a speaker for Genentech. Dr. Goldstein had no disclosures. Dr. Goyal has been a consultant to and received research support from Covidien and holds a patent on using CT angiography to diagnose stroke. Dr. Broderick has received research support from Genentech.
[email protected]
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE INTERNATIONAL STROKE CONFERENCE