User login
Official Newspaper of the American College of Surgeons
Supreme Court justices appear split on ACA tax subsidies
Supreme Court justices appear to differ over whether the Affordable Care Act allows tax subsidies for patients who purchase insurance through the federal exchange.
During oral arguments March 4 in King v. Burwell, justices expressed mixed perspective not only on the ACA language on tax credits, but also on the ramifications of striking down use of the subsidies in states that rely on the federal exchange.
“One thing that was surprising was that the justices spent a lot of time asking questions about the consequences of agreeing with the petitioners,” said Brian M. Pinheiro, a Philadelphia-based health care and employee benefits attorney who attended the oral arguments. He said that some justices asked questions to find out “ ‘if the court struck down subsidies in the 34 states that had federal exchanges, what would that do to that law? What would that do to the health system, and could Congress have intended that result?’ I think that did trouble several of the justices who were thinking of the ultimate consequences of the decision.”
King v. Burwell centers on whether people who live in states that rely on the federal marketplace are eligible for tax credits to purchase insurance or whether such assistance can go only to residents whose states run their own marketplaces. The ACA states that tax credits apply to insurance purchased through an exchange “established by the state.” Challengers argue the law does not mention the federal exchange. The government interprets the ACA to allow subsidies whenever patients buys insurance on any exchange. Only 16 states and the District of Columbia have established a state-based exchange.
Recent research from the Urban Institute predicts that as many as 6 million Americans could lose their insurance coverage if the court rules against the government and strikes down the federal subsidies. Further, analysts from consultancy Avalere Health predict also that patients could see significant premium increases and health care providers could lose billions due to increased uncompensated care.
During the March 4 debate, the court’s four liberal justices appeared to side with the government’s reading of the law, including Justice Ruth Bader-Ginsberg and Justice Sonia Sotomayor, said Eric J. Segall, professor of law at Georgia State University, Atlanta. Justice Sotomayor said the plaintiffs’ interpretation of the ACA would mean Congress intended to coerce states into creating exchanges.
“The choice the state had was establish your own exchange or let the federal government establish it for you,” Justice Sotomayor said to plaintiff’s attorney Michael Carvin. “If we read it the way you’re saying, then we’re going to read a statute as intruding on the federal/state relationship because then the states are going to be coerced into establishing their own exchanges. In those states that don’t, their citizens don’t receive subsidies. We’re going to have the death spiral that this system was created to avoid.”
But the high court’s more conservative judges, including Justice Samuel Alito and Justice Antonin Scalia, appeared to agree with the plaintiff’s reading. Justice Scalia noted that whether the ACA functions well or not based on King’s interpretation should not be the issue.
“Is it not the case that if the only reasonable interpretation of a particular provision produces disastrous consequences in the rest of the statute, it nonetheless means what it says?” Justice Scalia asked Solicitor General Donald B. Verrilli Jr., who represented the government. Justice Scalia stressed that addressing flaws within a law is the business of legislators. “You really think Congress is just going to sit there while all of these disastrous consequences ensue?”
Justices also grilled attorneys about whether the plaintiffs in the case have standing to sue, an issue that arose late in the litigation. The question surrounds whether all four plaintiffs have legal authority to challenge the ACA since some, or all, may not be penalized if they do not buy health insurance. Mr. Carvin argued the plaintiffs have clear standing to sue, while Mr. Verrilli indicated that the government was not interested in having the case decided on the basis of standing.
Although dismissing the case based on standing would be an easy out for the Supreme Court, the outcome is highly unlikely, Mr. Segall said.
“The court will do what it wants, regardless of the law of standing,” he said in an interview. “It felt like nobody wanted to get rid of this case based on standing. They’re going to basically ignore” the issue.
Mr. Pinheiro said that he believed the government had the stronger case. He predicted the Supreme Court will rule 6-3 in favor of the government.
Ilya Shapiro of the Cato Institute had originally predicted a 6-3 rule in favor of the challengers. However, after the arguments, he now says it’s anyone’s call.
“My only prediction is that it’s a complete toss-up,” he said in an interview. “Whichever side anyone thought had the edge before argument has to temper their expectations, because I would give each side an even 50-50 shot at this point.”
The Justices’ decision is expected in June.
On Twitter @legal_med
Supreme Court justices appear to differ over whether the Affordable Care Act allows tax subsidies for patients who purchase insurance through the federal exchange.
During oral arguments March 4 in King v. Burwell, justices expressed mixed perspective not only on the ACA language on tax credits, but also on the ramifications of striking down use of the subsidies in states that rely on the federal exchange.
“One thing that was surprising was that the justices spent a lot of time asking questions about the consequences of agreeing with the petitioners,” said Brian M. Pinheiro, a Philadelphia-based health care and employee benefits attorney who attended the oral arguments. He said that some justices asked questions to find out “ ‘if the court struck down subsidies in the 34 states that had federal exchanges, what would that do to that law? What would that do to the health system, and could Congress have intended that result?’ I think that did trouble several of the justices who were thinking of the ultimate consequences of the decision.”
King v. Burwell centers on whether people who live in states that rely on the federal marketplace are eligible for tax credits to purchase insurance or whether such assistance can go only to residents whose states run their own marketplaces. The ACA states that tax credits apply to insurance purchased through an exchange “established by the state.” Challengers argue the law does not mention the federal exchange. The government interprets the ACA to allow subsidies whenever patients buys insurance on any exchange. Only 16 states and the District of Columbia have established a state-based exchange.
Recent research from the Urban Institute predicts that as many as 6 million Americans could lose their insurance coverage if the court rules against the government and strikes down the federal subsidies. Further, analysts from consultancy Avalere Health predict also that patients could see significant premium increases and health care providers could lose billions due to increased uncompensated care.
During the March 4 debate, the court’s four liberal justices appeared to side with the government’s reading of the law, including Justice Ruth Bader-Ginsberg and Justice Sonia Sotomayor, said Eric J. Segall, professor of law at Georgia State University, Atlanta. Justice Sotomayor said the plaintiffs’ interpretation of the ACA would mean Congress intended to coerce states into creating exchanges.
“The choice the state had was establish your own exchange or let the federal government establish it for you,” Justice Sotomayor said to plaintiff’s attorney Michael Carvin. “If we read it the way you’re saying, then we’re going to read a statute as intruding on the federal/state relationship because then the states are going to be coerced into establishing their own exchanges. In those states that don’t, their citizens don’t receive subsidies. We’re going to have the death spiral that this system was created to avoid.”
But the high court’s more conservative judges, including Justice Samuel Alito and Justice Antonin Scalia, appeared to agree with the plaintiff’s reading. Justice Scalia noted that whether the ACA functions well or not based on King’s interpretation should not be the issue.
“Is it not the case that if the only reasonable interpretation of a particular provision produces disastrous consequences in the rest of the statute, it nonetheless means what it says?” Justice Scalia asked Solicitor General Donald B. Verrilli Jr., who represented the government. Justice Scalia stressed that addressing flaws within a law is the business of legislators. “You really think Congress is just going to sit there while all of these disastrous consequences ensue?”
Justices also grilled attorneys about whether the plaintiffs in the case have standing to sue, an issue that arose late in the litigation. The question surrounds whether all four plaintiffs have legal authority to challenge the ACA since some, or all, may not be penalized if they do not buy health insurance. Mr. Carvin argued the plaintiffs have clear standing to sue, while Mr. Verrilli indicated that the government was not interested in having the case decided on the basis of standing.
Although dismissing the case based on standing would be an easy out for the Supreme Court, the outcome is highly unlikely, Mr. Segall said.
“The court will do what it wants, regardless of the law of standing,” he said in an interview. “It felt like nobody wanted to get rid of this case based on standing. They’re going to basically ignore” the issue.
Mr. Pinheiro said that he believed the government had the stronger case. He predicted the Supreme Court will rule 6-3 in favor of the government.
Ilya Shapiro of the Cato Institute had originally predicted a 6-3 rule in favor of the challengers. However, after the arguments, he now says it’s anyone’s call.
“My only prediction is that it’s a complete toss-up,” he said in an interview. “Whichever side anyone thought had the edge before argument has to temper their expectations, because I would give each side an even 50-50 shot at this point.”
The Justices’ decision is expected in June.
On Twitter @legal_med
Supreme Court justices appear to differ over whether the Affordable Care Act allows tax subsidies for patients who purchase insurance through the federal exchange.
During oral arguments March 4 in King v. Burwell, justices expressed mixed perspective not only on the ACA language on tax credits, but also on the ramifications of striking down use of the subsidies in states that rely on the federal exchange.
“One thing that was surprising was that the justices spent a lot of time asking questions about the consequences of agreeing with the petitioners,” said Brian M. Pinheiro, a Philadelphia-based health care and employee benefits attorney who attended the oral arguments. He said that some justices asked questions to find out “ ‘if the court struck down subsidies in the 34 states that had federal exchanges, what would that do to that law? What would that do to the health system, and could Congress have intended that result?’ I think that did trouble several of the justices who were thinking of the ultimate consequences of the decision.”
King v. Burwell centers on whether people who live in states that rely on the federal marketplace are eligible for tax credits to purchase insurance or whether such assistance can go only to residents whose states run their own marketplaces. The ACA states that tax credits apply to insurance purchased through an exchange “established by the state.” Challengers argue the law does not mention the federal exchange. The government interprets the ACA to allow subsidies whenever patients buys insurance on any exchange. Only 16 states and the District of Columbia have established a state-based exchange.
Recent research from the Urban Institute predicts that as many as 6 million Americans could lose their insurance coverage if the court rules against the government and strikes down the federal subsidies. Further, analysts from consultancy Avalere Health predict also that patients could see significant premium increases and health care providers could lose billions due to increased uncompensated care.
During the March 4 debate, the court’s four liberal justices appeared to side with the government’s reading of the law, including Justice Ruth Bader-Ginsberg and Justice Sonia Sotomayor, said Eric J. Segall, professor of law at Georgia State University, Atlanta. Justice Sotomayor said the plaintiffs’ interpretation of the ACA would mean Congress intended to coerce states into creating exchanges.
“The choice the state had was establish your own exchange or let the federal government establish it for you,” Justice Sotomayor said to plaintiff’s attorney Michael Carvin. “If we read it the way you’re saying, then we’re going to read a statute as intruding on the federal/state relationship because then the states are going to be coerced into establishing their own exchanges. In those states that don’t, their citizens don’t receive subsidies. We’re going to have the death spiral that this system was created to avoid.”
But the high court’s more conservative judges, including Justice Samuel Alito and Justice Antonin Scalia, appeared to agree with the plaintiff’s reading. Justice Scalia noted that whether the ACA functions well or not based on King’s interpretation should not be the issue.
“Is it not the case that if the only reasonable interpretation of a particular provision produces disastrous consequences in the rest of the statute, it nonetheless means what it says?” Justice Scalia asked Solicitor General Donald B. Verrilli Jr., who represented the government. Justice Scalia stressed that addressing flaws within a law is the business of legislators. “You really think Congress is just going to sit there while all of these disastrous consequences ensue?”
Justices also grilled attorneys about whether the plaintiffs in the case have standing to sue, an issue that arose late in the litigation. The question surrounds whether all four plaintiffs have legal authority to challenge the ACA since some, or all, may not be penalized if they do not buy health insurance. Mr. Carvin argued the plaintiffs have clear standing to sue, while Mr. Verrilli indicated that the government was not interested in having the case decided on the basis of standing.
Although dismissing the case based on standing would be an easy out for the Supreme Court, the outcome is highly unlikely, Mr. Segall said.
“The court will do what it wants, regardless of the law of standing,” he said in an interview. “It felt like nobody wanted to get rid of this case based on standing. They’re going to basically ignore” the issue.
Mr. Pinheiro said that he believed the government had the stronger case. He predicted the Supreme Court will rule 6-3 in favor of the government.
Ilya Shapiro of the Cato Institute had originally predicted a 6-3 rule in favor of the challengers. However, after the arguments, he now says it’s anyone’s call.
“My only prediction is that it’s a complete toss-up,” he said in an interview. “Whichever side anyone thought had the edge before argument has to temper their expectations, because I would give each side an even 50-50 shot at this point.”
The Justices’ decision is expected in June.
On Twitter @legal_med
ACS NSQIP hospitals steadily improve surgical outcomes
Surgical performance data gathered within the American College of Surgeons, National Surgical Quality Improvement Program (ACS NSQIP) from the period of 2006-2013 indicate improved performance by most participating hospitals over time. In the categories of mortality, morbidity, and surgical site infections (SSI), the ratio of observed to expected surgery-related adverse events declined over time, showing that with increasing years of participation in ACS NSQIP, hospitals saw cumulative reductions in observed/expected ratios.
Dr. Clifford Y. Ko, coauthor of the report, an ACS Fellow and professor of surgery at David Geffen School of Medicine, University of California Los Angeles, spoke in an interview about the results, which were published in Annals of Surgery.
“An important finding from our study is that hospitals get better when they participate in ACS NSQIP, and the longer they are in the program, the better they get. It means that if hospitals commit to going on the journey of quality improvement, the longer they are on that journey, the better they get, the more experience they get in quality improvement, and the more their outcomes improve.
“Another important point that became evident from the analysis was that the biggest area for improvement is in the rate of complications, more so than mortality. The mortality rate is already low, and the number of preventable deaths is low. There are many more preventable complications than preventable deaths. The data show that risk-adjusted complications decrease over time because many opportunities lie in decreasing rates of infection, blood clot, pneumonia, urinary tract infection, and others. Whatever rate the hospital starts in ACS NSQIP, there is more opportunity to realize improvements in the number of complications than in mortality.”
The researchers used clinical data collected from 2006 to 2013 from 515 hospitals participating in ACS NSQIP.
Hospitals participating in the program receive semiannual reports that benchmark performance compared to other similar institutions. But the performance benchmarks are continuously updated to reflect current practices across groups of similar institutions, so individual hospitals cannot gauge whether their performance improves over time relative to fixed standard.
“The aim of the study was to determine if over several years hospitals who participated in ACS NSQIP got better. Benchmarking data provides feedback, but does not indicate whether over time hospitals improve. Our analysis looked at hospital performance longitudinally to evaluate if they got better from year to year,” said Dr. Ko.
To make meaningful comparisons of surgical outcomes, expected outcomes were calculated based on risk adjustments to compensate for differences in patient characteristics and the risk profile of procedures performed. Dr. Ko explained, “Large, tertiary institutions that care for very sick patients, or very complex cases, are expected to have worse outcomes than hospitals that perform more common procedures with lower expected event rates. In this analysis, the results of interest are the trends in observed/expected (O/E) event rates, which adjust for these risks.”
For all hospitals, 62%, 70%, and 65% had negative slopes for mortality, morbidity, and any SSI, respectively. The O/E ratios for mortality, morbidity, and SSI declined with each year of participation in the program, and the slope of the decline was steepest for morbidity and SSI. SSI is the most common complication and largely mirrors morbidity. For hospitals in the program at least 3 years, annual reductions in mortality, morbidity, and SSI were estimated to be 0.8%, 3.1%, and 2.6%, respectively.
One of the hallmarks of ACS NSQIP is the accuracy of the data, which come directly from medical records. In a large study comparing clinical with billing (or administrative) data, Dr. Ko and colleagues found the accuracy of billing data to be low.
“In a 2-year study we merged clinical and administrative data from over 100,000 patients and found the agreement to be poor. Billing data had a detection rate for SSI of 25% and a false-positive rate of 70%,” he said.
“In developing programs to improve patient care, we want to base our work on the most accurate data possible. Our analysis shows that hospitals committed to using ACS NSQIP improve over time.”
The authors reported having no financial disclosures.
Surgical performance data gathered within the American College of Surgeons, National Surgical Quality Improvement Program (ACS NSQIP) from the period of 2006-2013 indicate improved performance by most participating hospitals over time. In the categories of mortality, morbidity, and surgical site infections (SSI), the ratio of observed to expected surgery-related adverse events declined over time, showing that with increasing years of participation in ACS NSQIP, hospitals saw cumulative reductions in observed/expected ratios.
Dr. Clifford Y. Ko, coauthor of the report, an ACS Fellow and professor of surgery at David Geffen School of Medicine, University of California Los Angeles, spoke in an interview about the results, which were published in Annals of Surgery.
“An important finding from our study is that hospitals get better when they participate in ACS NSQIP, and the longer they are in the program, the better they get. It means that if hospitals commit to going on the journey of quality improvement, the longer they are on that journey, the better they get, the more experience they get in quality improvement, and the more their outcomes improve.
“Another important point that became evident from the analysis was that the biggest area for improvement is in the rate of complications, more so than mortality. The mortality rate is already low, and the number of preventable deaths is low. There are many more preventable complications than preventable deaths. The data show that risk-adjusted complications decrease over time because many opportunities lie in decreasing rates of infection, blood clot, pneumonia, urinary tract infection, and others. Whatever rate the hospital starts in ACS NSQIP, there is more opportunity to realize improvements in the number of complications than in mortality.”
The researchers used clinical data collected from 2006 to 2013 from 515 hospitals participating in ACS NSQIP.
Hospitals participating in the program receive semiannual reports that benchmark performance compared to other similar institutions. But the performance benchmarks are continuously updated to reflect current practices across groups of similar institutions, so individual hospitals cannot gauge whether their performance improves over time relative to fixed standard.
“The aim of the study was to determine if over several years hospitals who participated in ACS NSQIP got better. Benchmarking data provides feedback, but does not indicate whether over time hospitals improve. Our analysis looked at hospital performance longitudinally to evaluate if they got better from year to year,” said Dr. Ko.
To make meaningful comparisons of surgical outcomes, expected outcomes were calculated based on risk adjustments to compensate for differences in patient characteristics and the risk profile of procedures performed. Dr. Ko explained, “Large, tertiary institutions that care for very sick patients, or very complex cases, are expected to have worse outcomes than hospitals that perform more common procedures with lower expected event rates. In this analysis, the results of interest are the trends in observed/expected (O/E) event rates, which adjust for these risks.”
For all hospitals, 62%, 70%, and 65% had negative slopes for mortality, morbidity, and any SSI, respectively. The O/E ratios for mortality, morbidity, and SSI declined with each year of participation in the program, and the slope of the decline was steepest for morbidity and SSI. SSI is the most common complication and largely mirrors morbidity. For hospitals in the program at least 3 years, annual reductions in mortality, morbidity, and SSI were estimated to be 0.8%, 3.1%, and 2.6%, respectively.
One of the hallmarks of ACS NSQIP is the accuracy of the data, which come directly from medical records. In a large study comparing clinical with billing (or administrative) data, Dr. Ko and colleagues found the accuracy of billing data to be low.
“In a 2-year study we merged clinical and administrative data from over 100,000 patients and found the agreement to be poor. Billing data had a detection rate for SSI of 25% and a false-positive rate of 70%,” he said.
“In developing programs to improve patient care, we want to base our work on the most accurate data possible. Our analysis shows that hospitals committed to using ACS NSQIP improve over time.”
The authors reported having no financial disclosures.
Surgical performance data gathered within the American College of Surgeons, National Surgical Quality Improvement Program (ACS NSQIP) from the period of 2006-2013 indicate improved performance by most participating hospitals over time. In the categories of mortality, morbidity, and surgical site infections (SSI), the ratio of observed to expected surgery-related adverse events declined over time, showing that with increasing years of participation in ACS NSQIP, hospitals saw cumulative reductions in observed/expected ratios.
Dr. Clifford Y. Ko, coauthor of the report, an ACS Fellow and professor of surgery at David Geffen School of Medicine, University of California Los Angeles, spoke in an interview about the results, which were published in Annals of Surgery.
“An important finding from our study is that hospitals get better when they participate in ACS NSQIP, and the longer they are in the program, the better they get. It means that if hospitals commit to going on the journey of quality improvement, the longer they are on that journey, the better they get, the more experience they get in quality improvement, and the more their outcomes improve.
“Another important point that became evident from the analysis was that the biggest area for improvement is in the rate of complications, more so than mortality. The mortality rate is already low, and the number of preventable deaths is low. There are many more preventable complications than preventable deaths. The data show that risk-adjusted complications decrease over time because many opportunities lie in decreasing rates of infection, blood clot, pneumonia, urinary tract infection, and others. Whatever rate the hospital starts in ACS NSQIP, there is more opportunity to realize improvements in the number of complications than in mortality.”
The researchers used clinical data collected from 2006 to 2013 from 515 hospitals participating in ACS NSQIP.
Hospitals participating in the program receive semiannual reports that benchmark performance compared to other similar institutions. But the performance benchmarks are continuously updated to reflect current practices across groups of similar institutions, so individual hospitals cannot gauge whether their performance improves over time relative to fixed standard.
“The aim of the study was to determine if over several years hospitals who participated in ACS NSQIP got better. Benchmarking data provides feedback, but does not indicate whether over time hospitals improve. Our analysis looked at hospital performance longitudinally to evaluate if they got better from year to year,” said Dr. Ko.
To make meaningful comparisons of surgical outcomes, expected outcomes were calculated based on risk adjustments to compensate for differences in patient characteristics and the risk profile of procedures performed. Dr. Ko explained, “Large, tertiary institutions that care for very sick patients, or very complex cases, are expected to have worse outcomes than hospitals that perform more common procedures with lower expected event rates. In this analysis, the results of interest are the trends in observed/expected (O/E) event rates, which adjust for these risks.”
For all hospitals, 62%, 70%, and 65% had negative slopes for mortality, morbidity, and any SSI, respectively. The O/E ratios for mortality, morbidity, and SSI declined with each year of participation in the program, and the slope of the decline was steepest for morbidity and SSI. SSI is the most common complication and largely mirrors morbidity. For hospitals in the program at least 3 years, annual reductions in mortality, morbidity, and SSI were estimated to be 0.8%, 3.1%, and 2.6%, respectively.
One of the hallmarks of ACS NSQIP is the accuracy of the data, which come directly from medical records. In a large study comparing clinical with billing (or administrative) data, Dr. Ko and colleagues found the accuracy of billing data to be low.
“In a 2-year study we merged clinical and administrative data from over 100,000 patients and found the agreement to be poor. Billing data had a detection rate for SSI of 25% and a false-positive rate of 70%,” he said.
“In developing programs to improve patient care, we want to base our work on the most accurate data possible. Our analysis shows that hospitals committed to using ACS NSQIP improve over time.”
The authors reported having no financial disclosures.
FROM ANNALS OF SURGERY
Key clinical point: As length of hospital participation in ACS NSQIP increased, the ratio of observed/expected surgery-related adverse events declined.
Major finding: Improvements in morbidity were observed in 70% of participating hospitals; for surgical site infections, in 65% of hospitals; for mortality, in 62% of hospitals.
Data source: Clinical data from 2006 to 2013 from 515 hospitals participating in ACS NSQIP.
Disclosures: The authors reported having no financial disclosures.
PQRS participation varies by specialty
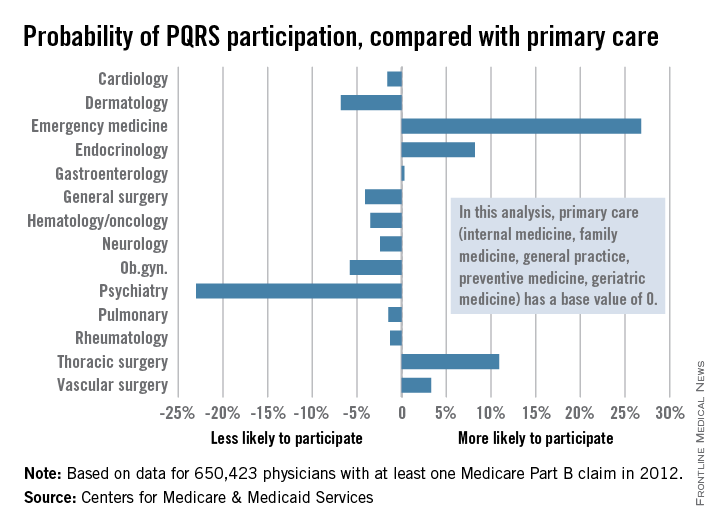
Participation in the Physician Quality Reporting System (PQRS) varies considerably by specialty, according to an new analysis of 2012 data using primary care physicians as the base, the Centers for Medicare & Medicaid Services reported.
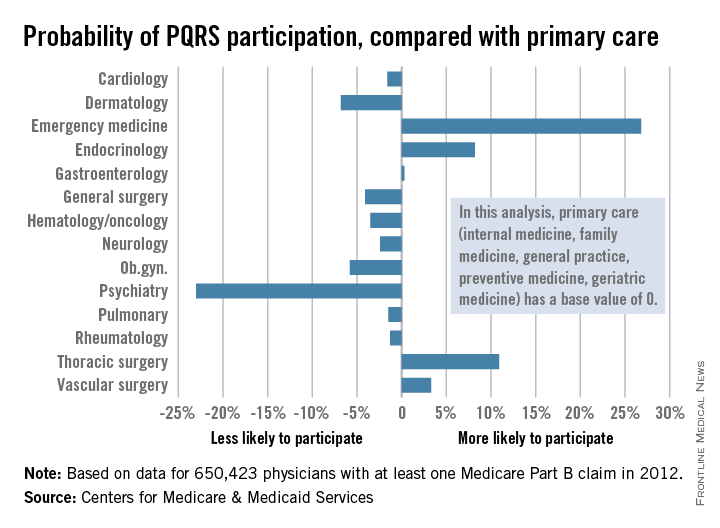
Emergency medicine physicians were almost 27% more likely to participate in PQRS than were physicians in primary care (internal medicine, family medicine, general practice, preventive medicine, and geriatrics). On the other end of the scale were psychiatrists, who were 23% less likely than were primary care physicians to participate in PQRS, according to the CMS.
Among surgical specialties, general surgeons were 4% less likely to participate in PQRS, but thoracic surgeons and vascular surgeons were 11% and 3%, respectively, more likely to participate, compared with primary care physicians.
The PQRS participation rate in 2012 was 41.3% overall for the 650,423 MDs/DOs who submitted at least one Medicare Part B claim that year. Other health care professionals – including podiatrists, chiropractors, nurse practitioners, psychologists, and physical therapists – are eligible for PQRS but were not included in this analysis, the CMS said.
Participation in the Physician Quality Reporting System (PQRS) varies considerably by specialty, according to an new analysis of 2012 data using primary care physicians as the base, the Centers for Medicare & Medicaid Services reported.
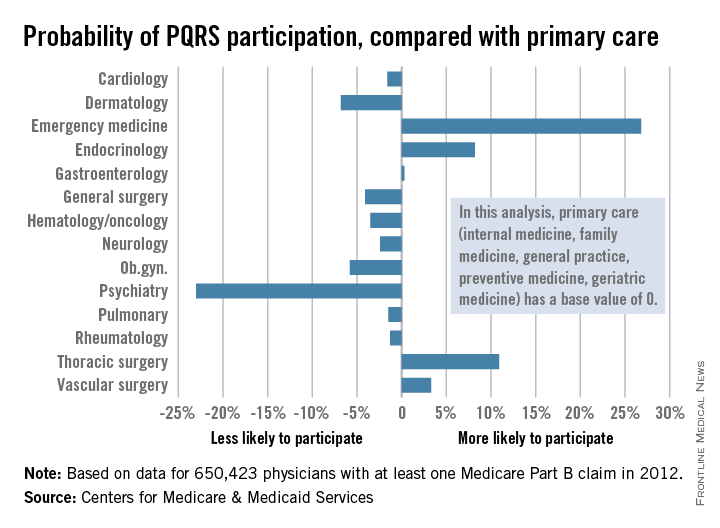
Emergency medicine physicians were almost 27% more likely to participate in PQRS than were physicians in primary care (internal medicine, family medicine, general practice, preventive medicine, and geriatrics). On the other end of the scale were psychiatrists, who were 23% less likely than were primary care physicians to participate in PQRS, according to the CMS.
Among surgical specialties, general surgeons were 4% less likely to participate in PQRS, but thoracic surgeons and vascular surgeons were 11% and 3%, respectively, more likely to participate, compared with primary care physicians.
The PQRS participation rate in 2012 was 41.3% overall for the 650,423 MDs/DOs who submitted at least one Medicare Part B claim that year. Other health care professionals – including podiatrists, chiropractors, nurse practitioners, psychologists, and physical therapists – are eligible for PQRS but were not included in this analysis, the CMS said.
Participation in the Physician Quality Reporting System (PQRS) varies considerably by specialty, according to an new analysis of 2012 data using primary care physicians as the base, the Centers for Medicare & Medicaid Services reported.
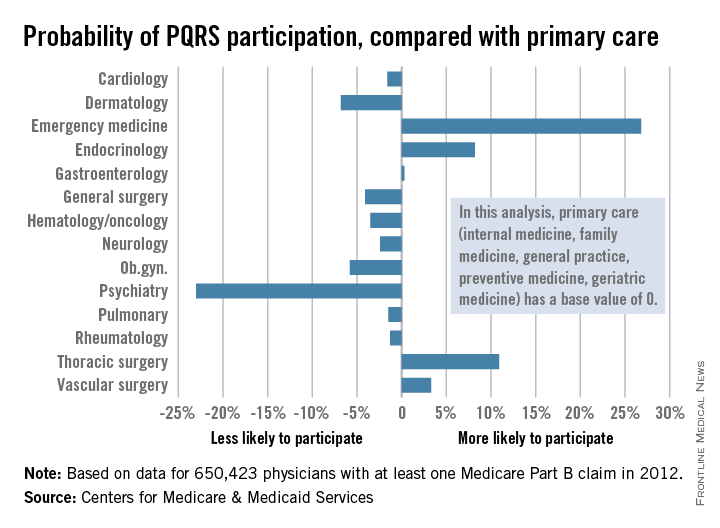
Emergency medicine physicians were almost 27% more likely to participate in PQRS than were physicians in primary care (internal medicine, family medicine, general practice, preventive medicine, and geriatrics). On the other end of the scale were psychiatrists, who were 23% less likely than were primary care physicians to participate in PQRS, according to the CMS.
Among surgical specialties, general surgeons were 4% less likely to participate in PQRS, but thoracic surgeons and vascular surgeons were 11% and 3%, respectively, more likely to participate, compared with primary care physicians.
The PQRS participation rate in 2012 was 41.3% overall for the 650,423 MDs/DOs who submitted at least one Medicare Part B claim that year. Other health care professionals – including podiatrists, chiropractors, nurse practitioners, psychologists, and physical therapists – are eligible for PQRS but were not included in this analysis, the CMS said.
Meticulous planning, creativity key to management of EVAR infections
CHICAGO – Successful management of infected aortic endovascular grafts requires careful operative planning and execution, meticulous postoperative care, and a fair bit of creativity.
“Each patient is different, so surgeons have to tailor the reconstructions to the individual patient and with these specific infections, have to be creative,” Dr. Thomas C. Bower, chair of vascular and endovascular surgery at Mayo Clinic, Rochester, Minn., said. “I’ve found the operations to be more challenging and more difficult than explanting portions or total graft excision when the infection has occurred in a hand-sewn graft.”
Unlike the typical bimodal distribution seen with hand-sewn graft infections, infection following endovascular repair of aortic aneurysms (EVAR) occurs from days up to 3 years after implantation. At the Mayo Clinic, a 79-year-old man presented with an infected endograft, psoas abscess, and Salmonella septicemia 4 years after EVAR.
“These infections are uncommon, but we are seeing more of them,” Dr. Bower said at a symposium on vascular surgery sponsored by Northwestern University.
Roughly two-thirds of patients will present with fever, nonspecific abdominal or back pain, malaise, weight loss or night sweats. If time permits, preoperative assessments include echocardiography for left ventricular function, arterial blood gases for pulmonary function since many patients are smokers, and renal ultrasound if creatinine is ≥ 1.5 mg/dL after rehydration. These tests are important because preoperative chronic obstructive pulmonary disease and renal dysfunction correlate with worse postoperative outcomes, he said.
Computed tomography angiography (CTA), however, stands as the single most important step of preoperative preparation, with the sine qua non of infection being air around the graft. Unlike hand-sewn grafts where infections can be localized, typically there is total graft involvement in these cases because the device is left inside the aneurysm sac. Aneurysms or pseudoaneurysms also have been seen above the infected device, including at the top end of suprarenal stents.
“This clearly has an impact on how we approach patients, but what’s become very apparent to me is that CTA often underestimates the amount of periaortic inflammation, especially at the juxta- and pararenal locations,” Dr. Bower said.
The Mayo group initially used in situ antibiotic-soaked prosthetic grafts for explanting EVAR devices, which yielded “acceptable mortality and reinfection rates, but primarily outstanding patency rates.” However, cryopreserved aortoiliac grafts have now become their first choice, Dr. Bower said. An ABO match is not imperative, preparation takes roughly 45 minutes, branch closures done in the lab are buttressed with sutures, and the graft is turned over to keep the lumbar arteries anterior, which offers an easy fix if there is bleeding, rather than having it on the posterior wall. Cryopreserved grafts, however, can dilate 40% and lengthen 10% under pressure.
“I’ve been burned more than once where the graft elongates more than I think, and I end up having to cut a small piece out to foreshorten it,” he said.
Reconstructions are tailored to patient anatomy. Surgeons should have several plans for reconstruction, including routing a graft through a remote path, remembering that CTA will underestimate the amount of periaortic inflammation. Separate bypasses of the renal or visceral arteries are performed first before the aortic clamp is applied to reduce physiologic stress. This requires knowledge of the supraceliac and pararenal aorta exposures, which really begins with the correct choice of incisions, Dr. Bower said. This is based on the aortic segment to be treated, position of the new graft, the aortic clamp site, and patient body habitus.
Most patients with EVAR infections are approached with a midline abdominal incision extended along the xiphoid process, which is the lynch pin for allowing upward and lateral retraction of the abdominal wall, he said. Choosing an incision that allows a more vertical orientation to where the new aortic anastomosis and clamp site will be, rather than operating in a keyhole, is important.
The second step is to open up the pararenal space by moving the viscera out of the way. This begins by ligating the inferior mesenteric vein and adjacent lymphatics, which allows incision of an avascular plane along the base of the left transverse colon. Retractor blades are set to allow the upward and lateral retraction of the small bowel, the left colon, and pancreas. Exposure of the suprarenal or supramesenteric aorta requires mobilization of the left renal vein after ligation and division of its branches.
“If that vein is intensely involved in inflammation, don’t ligate the branches in case you have to divide that vein at the caval confluence. Otherwise, you’ll run into some dysfunction of that left kidney,” Dr. Bower cautioned.
To have a secure place for the aortic cross clamp, the crura must be divided on either side of the diaphragm at or above the supramesenteric aorta, he added.
Key steps in total graft explantation are to drain abscesses prior to surgery to lower the bacterial burden and thus reduce the postoperative inflammatory response, bypass renal/visceral arteries first, if needed, remove the infected graft, debride the aorta to healthy tissue, place the new graft and cover it with omentum, and repair the bowel, if needed.
A piece of the proximal aortic wall should be sent to pathology to ensure the absence of bacteria or microabscesses. Organism-specific antibiotics are administered intravenously for 6-8 weeks followed by lifelong oral antibiotics, he said.
An earlier report involving 24 patients with infected aortic endografts (21 EVARs and 3 thoracic EVARs) treated at Mayo Clinic between 1997 and 2012 revealed polymicrobial infection in 11 patients, with methicillin-resistant Staphylococcus aureus being common. Potential contributors to infection were endovascular reintervention in eight, aortoenteric fistula/erosion in four, and various remote infections (J. Vasc. Surg. 2013;58:371-9).
Rifampin-soaked grafts were used in 15 patients, cryopreserved grafts in 4, femoral vein in 2, and axillofemoral grafts in 3. At a median of 14 months follow-up, patient survival, graft-related complications, and reinfection rates were 79%, 13%, and 4%, respectively, Dr. Bower said.
Dr. Bower reported having no financial disclosures.
The expert opinion from the Northwestern Vascular Symposium regarding the management of EVAR infections reminds us of the importance of appropriate patient selection, proper performance of the planned procedure, and long-term follow-up. As EVAR has become the treatment of choice for more than 80% of patients with infrarenal AAAs in the United States, the rate of patients that return with EVAR infections, although rare, is increasing and their management can be more challenging than that of a primary or aortic graft infection as suggested by Dr. Thomas C. Bower in this opinion. The planning for these cases is critical with multiple options for treatment currently available and endorsed by a variety of investigators. From an evaluation standpoint, CTA is critical for diagnosis and case planning. Air around the graft is considered the “sine qua non” of infection but if it presents in the first month after EVAR it can be due to trapped air introduced into the sac during the intervention.

|
Dr. Luis A. Sanchez |
Patients with air in the sac at the initial postprocedure evaluation should be considered for early follow-up to make sure this finding resolves. Further assessment that will change the management of the patient includes the type of EVAR device, infra- or suprarenal, since the entire removal of a suprarenal device usually requires supraceliac cross-clamping with its associated morbidity and mortality. Drainage of the infected cavity, as suggested by Dr. Bower, can help lower the bacterial burden and provide information regarding the offending organism. That information will help the vascular surgeon decide if an in-line reconstruction or an extra-anatomical one is more appropriate in the patient’s situation as more virulent organisms tend to be associated with higher reinfection and complication rates when in-line reconstructions are performed.
The different options for aortic access need to be evaluated based on the anatomy of the patient. A transabdominal approach is best for most patients as it allows access to the iliac arteries bilaterally for removal of the entire graft, debridement of the infected bed, aortic and/or visceral reconstruction, and omental coverage of the in-line graft or aortic stump if an extra-anatomical reconstruction is selected. The retroperitoneal approach should be considered for patients that will require extensive perivisceral work, as may be necessary from suprarenal or fenestrated devices, but limitations exist accessing the right iliac system and potentially intraabdominal targets for visceral or renal reconstructions.
The best configuration to reconstruct these patients remains largely undetermined based on the literature. The published experience from the Mayo Clinic (J. Vasc. Surg. 2013;58:371-9), in which some of the opinions of Dr. Bower are based, suggested excellent results in 24 patients mostly treated with rifampin-soaked in-line reconstructions with a periprocedural mortality of 4%. Cryopreserved aortic grafts “have become the conduit of choice for the group at this time,” stated Dr. Bower, to try to further decrease the reinfection rates in their patient population. There are limited data regarding the use of cryopreserved aortoiliac segments for aortic infections and less for EVAR infections. The most recent and largest series (J. Vasc. Surg. 2014;59:669-74) included 220 patients with aortic infections with a perioperative mortality of 9% and cryopreserved graft complications in another 12%-15% of patients.
In summary, aortic infections associated with EVAR are challenging problems that should be addressed in regional centers with experience. Renal and visceral reconstructions as well as supravisceral clamping are associated with significantly higher periprocedural morbidity and mortality based on the extensive experience at the Cleveland Clinic with EVAR explants (J. Vasc. Surg. 2014;59:886-93). The choice of the reconstruction and the material used should be based on the offending organism, type of EVAR device, extent of the infectious process, and the expertise of the treating physician.
Dr. Luis A. Sanchez is chief, section of vascular surgery and Gregorio A. Sicard Distinguished Professor of Surgery and Radiology, Washington University, St. Louis, and an associate medical editor for Vascular Specialist. He had no relevant disclosures.
The expert opinion from the Northwestern Vascular Symposium regarding the management of EVAR infections reminds us of the importance of appropriate patient selection, proper performance of the planned procedure, and long-term follow-up. As EVAR has become the treatment of choice for more than 80% of patients with infrarenal AAAs in the United States, the rate of patients that return with EVAR infections, although rare, is increasing and their management can be more challenging than that of a primary or aortic graft infection as suggested by Dr. Thomas C. Bower in this opinion. The planning for these cases is critical with multiple options for treatment currently available and endorsed by a variety of investigators. From an evaluation standpoint, CTA is critical for diagnosis and case planning. Air around the graft is considered the “sine qua non” of infection but if it presents in the first month after EVAR it can be due to trapped air introduced into the sac during the intervention.

|
Dr. Luis A. Sanchez |
Patients with air in the sac at the initial postprocedure evaluation should be considered for early follow-up to make sure this finding resolves. Further assessment that will change the management of the patient includes the type of EVAR device, infra- or suprarenal, since the entire removal of a suprarenal device usually requires supraceliac cross-clamping with its associated morbidity and mortality. Drainage of the infected cavity, as suggested by Dr. Bower, can help lower the bacterial burden and provide information regarding the offending organism. That information will help the vascular surgeon decide if an in-line reconstruction or an extra-anatomical one is more appropriate in the patient’s situation as more virulent organisms tend to be associated with higher reinfection and complication rates when in-line reconstructions are performed.
The different options for aortic access need to be evaluated based on the anatomy of the patient. A transabdominal approach is best for most patients as it allows access to the iliac arteries bilaterally for removal of the entire graft, debridement of the infected bed, aortic and/or visceral reconstruction, and omental coverage of the in-line graft or aortic stump if an extra-anatomical reconstruction is selected. The retroperitoneal approach should be considered for patients that will require extensive perivisceral work, as may be necessary from suprarenal or fenestrated devices, but limitations exist accessing the right iliac system and potentially intraabdominal targets for visceral or renal reconstructions.
The best configuration to reconstruct these patients remains largely undetermined based on the literature. The published experience from the Mayo Clinic (J. Vasc. Surg. 2013;58:371-9), in which some of the opinions of Dr. Bower are based, suggested excellent results in 24 patients mostly treated with rifampin-soaked in-line reconstructions with a periprocedural mortality of 4%. Cryopreserved aortic grafts “have become the conduit of choice for the group at this time,” stated Dr. Bower, to try to further decrease the reinfection rates in their patient population. There are limited data regarding the use of cryopreserved aortoiliac segments for aortic infections and less for EVAR infections. The most recent and largest series (J. Vasc. Surg. 2014;59:669-74) included 220 patients with aortic infections with a perioperative mortality of 9% and cryopreserved graft complications in another 12%-15% of patients.
In summary, aortic infections associated with EVAR are challenging problems that should be addressed in regional centers with experience. Renal and visceral reconstructions as well as supravisceral clamping are associated with significantly higher periprocedural morbidity and mortality based on the extensive experience at the Cleveland Clinic with EVAR explants (J. Vasc. Surg. 2014;59:886-93). The choice of the reconstruction and the material used should be based on the offending organism, type of EVAR device, extent of the infectious process, and the expertise of the treating physician.
Dr. Luis A. Sanchez is chief, section of vascular surgery and Gregorio A. Sicard Distinguished Professor of Surgery and Radiology, Washington University, St. Louis, and an associate medical editor for Vascular Specialist. He had no relevant disclosures.
The expert opinion from the Northwestern Vascular Symposium regarding the management of EVAR infections reminds us of the importance of appropriate patient selection, proper performance of the planned procedure, and long-term follow-up. As EVAR has become the treatment of choice for more than 80% of patients with infrarenal AAAs in the United States, the rate of patients that return with EVAR infections, although rare, is increasing and their management can be more challenging than that of a primary or aortic graft infection as suggested by Dr. Thomas C. Bower in this opinion. The planning for these cases is critical with multiple options for treatment currently available and endorsed by a variety of investigators. From an evaluation standpoint, CTA is critical for diagnosis and case planning. Air around the graft is considered the “sine qua non” of infection but if it presents in the first month after EVAR it can be due to trapped air introduced into the sac during the intervention.

|
Dr. Luis A. Sanchez |
Patients with air in the sac at the initial postprocedure evaluation should be considered for early follow-up to make sure this finding resolves. Further assessment that will change the management of the patient includes the type of EVAR device, infra- or suprarenal, since the entire removal of a suprarenal device usually requires supraceliac cross-clamping with its associated morbidity and mortality. Drainage of the infected cavity, as suggested by Dr. Bower, can help lower the bacterial burden and provide information regarding the offending organism. That information will help the vascular surgeon decide if an in-line reconstruction or an extra-anatomical one is more appropriate in the patient’s situation as more virulent organisms tend to be associated with higher reinfection and complication rates when in-line reconstructions are performed.
The different options for aortic access need to be evaluated based on the anatomy of the patient. A transabdominal approach is best for most patients as it allows access to the iliac arteries bilaterally for removal of the entire graft, debridement of the infected bed, aortic and/or visceral reconstruction, and omental coverage of the in-line graft or aortic stump if an extra-anatomical reconstruction is selected. The retroperitoneal approach should be considered for patients that will require extensive perivisceral work, as may be necessary from suprarenal or fenestrated devices, but limitations exist accessing the right iliac system and potentially intraabdominal targets for visceral or renal reconstructions.
The best configuration to reconstruct these patients remains largely undetermined based on the literature. The published experience from the Mayo Clinic (J. Vasc. Surg. 2013;58:371-9), in which some of the opinions of Dr. Bower are based, suggested excellent results in 24 patients mostly treated with rifampin-soaked in-line reconstructions with a periprocedural mortality of 4%. Cryopreserved aortic grafts “have become the conduit of choice for the group at this time,” stated Dr. Bower, to try to further decrease the reinfection rates in their patient population. There are limited data regarding the use of cryopreserved aortoiliac segments for aortic infections and less for EVAR infections. The most recent and largest series (J. Vasc. Surg. 2014;59:669-74) included 220 patients with aortic infections with a perioperative mortality of 9% and cryopreserved graft complications in another 12%-15% of patients.
In summary, aortic infections associated with EVAR are challenging problems that should be addressed in regional centers with experience. Renal and visceral reconstructions as well as supravisceral clamping are associated with significantly higher periprocedural morbidity and mortality based on the extensive experience at the Cleveland Clinic with EVAR explants (J. Vasc. Surg. 2014;59:886-93). The choice of the reconstruction and the material used should be based on the offending organism, type of EVAR device, extent of the infectious process, and the expertise of the treating physician.
Dr. Luis A. Sanchez is chief, section of vascular surgery and Gregorio A. Sicard Distinguished Professor of Surgery and Radiology, Washington University, St. Louis, and an associate medical editor for Vascular Specialist. He had no relevant disclosures.
CHICAGO – Successful management of infected aortic endovascular grafts requires careful operative planning and execution, meticulous postoperative care, and a fair bit of creativity.
“Each patient is different, so surgeons have to tailor the reconstructions to the individual patient and with these specific infections, have to be creative,” Dr. Thomas C. Bower, chair of vascular and endovascular surgery at Mayo Clinic, Rochester, Minn., said. “I’ve found the operations to be more challenging and more difficult than explanting portions or total graft excision when the infection has occurred in a hand-sewn graft.”
Unlike the typical bimodal distribution seen with hand-sewn graft infections, infection following endovascular repair of aortic aneurysms (EVAR) occurs from days up to 3 years after implantation. At the Mayo Clinic, a 79-year-old man presented with an infected endograft, psoas abscess, and Salmonella septicemia 4 years after EVAR.
“These infections are uncommon, but we are seeing more of them,” Dr. Bower said at a symposium on vascular surgery sponsored by Northwestern University.
Roughly two-thirds of patients will present with fever, nonspecific abdominal or back pain, malaise, weight loss or night sweats. If time permits, preoperative assessments include echocardiography for left ventricular function, arterial blood gases for pulmonary function since many patients are smokers, and renal ultrasound if creatinine is ≥ 1.5 mg/dL after rehydration. These tests are important because preoperative chronic obstructive pulmonary disease and renal dysfunction correlate with worse postoperative outcomes, he said.
Computed tomography angiography (CTA), however, stands as the single most important step of preoperative preparation, with the sine qua non of infection being air around the graft. Unlike hand-sewn grafts where infections can be localized, typically there is total graft involvement in these cases because the device is left inside the aneurysm sac. Aneurysms or pseudoaneurysms also have been seen above the infected device, including at the top end of suprarenal stents.
“This clearly has an impact on how we approach patients, but what’s become very apparent to me is that CTA often underestimates the amount of periaortic inflammation, especially at the juxta- and pararenal locations,” Dr. Bower said.
The Mayo group initially used in situ antibiotic-soaked prosthetic grafts for explanting EVAR devices, which yielded “acceptable mortality and reinfection rates, but primarily outstanding patency rates.” However, cryopreserved aortoiliac grafts have now become their first choice, Dr. Bower said. An ABO match is not imperative, preparation takes roughly 45 minutes, branch closures done in the lab are buttressed with sutures, and the graft is turned over to keep the lumbar arteries anterior, which offers an easy fix if there is bleeding, rather than having it on the posterior wall. Cryopreserved grafts, however, can dilate 40% and lengthen 10% under pressure.
“I’ve been burned more than once where the graft elongates more than I think, and I end up having to cut a small piece out to foreshorten it,” he said.
Reconstructions are tailored to patient anatomy. Surgeons should have several plans for reconstruction, including routing a graft through a remote path, remembering that CTA will underestimate the amount of periaortic inflammation. Separate bypasses of the renal or visceral arteries are performed first before the aortic clamp is applied to reduce physiologic stress. This requires knowledge of the supraceliac and pararenal aorta exposures, which really begins with the correct choice of incisions, Dr. Bower said. This is based on the aortic segment to be treated, position of the new graft, the aortic clamp site, and patient body habitus.
Most patients with EVAR infections are approached with a midline abdominal incision extended along the xiphoid process, which is the lynch pin for allowing upward and lateral retraction of the abdominal wall, he said. Choosing an incision that allows a more vertical orientation to where the new aortic anastomosis and clamp site will be, rather than operating in a keyhole, is important.
The second step is to open up the pararenal space by moving the viscera out of the way. This begins by ligating the inferior mesenteric vein and adjacent lymphatics, which allows incision of an avascular plane along the base of the left transverse colon. Retractor blades are set to allow the upward and lateral retraction of the small bowel, the left colon, and pancreas. Exposure of the suprarenal or supramesenteric aorta requires mobilization of the left renal vein after ligation and division of its branches.
“If that vein is intensely involved in inflammation, don’t ligate the branches in case you have to divide that vein at the caval confluence. Otherwise, you’ll run into some dysfunction of that left kidney,” Dr. Bower cautioned.
To have a secure place for the aortic cross clamp, the crura must be divided on either side of the diaphragm at or above the supramesenteric aorta, he added.
Key steps in total graft explantation are to drain abscesses prior to surgery to lower the bacterial burden and thus reduce the postoperative inflammatory response, bypass renal/visceral arteries first, if needed, remove the infected graft, debride the aorta to healthy tissue, place the new graft and cover it with omentum, and repair the bowel, if needed.
A piece of the proximal aortic wall should be sent to pathology to ensure the absence of bacteria or microabscesses. Organism-specific antibiotics are administered intravenously for 6-8 weeks followed by lifelong oral antibiotics, he said.
An earlier report involving 24 patients with infected aortic endografts (21 EVARs and 3 thoracic EVARs) treated at Mayo Clinic between 1997 and 2012 revealed polymicrobial infection in 11 patients, with methicillin-resistant Staphylococcus aureus being common. Potential contributors to infection were endovascular reintervention in eight, aortoenteric fistula/erosion in four, and various remote infections (J. Vasc. Surg. 2013;58:371-9).
Rifampin-soaked grafts were used in 15 patients, cryopreserved grafts in 4, femoral vein in 2, and axillofemoral grafts in 3. At a median of 14 months follow-up, patient survival, graft-related complications, and reinfection rates were 79%, 13%, and 4%, respectively, Dr. Bower said.
Dr. Bower reported having no financial disclosures.
CHICAGO – Successful management of infected aortic endovascular grafts requires careful operative planning and execution, meticulous postoperative care, and a fair bit of creativity.
“Each patient is different, so surgeons have to tailor the reconstructions to the individual patient and with these specific infections, have to be creative,” Dr. Thomas C. Bower, chair of vascular and endovascular surgery at Mayo Clinic, Rochester, Minn., said. “I’ve found the operations to be more challenging and more difficult than explanting portions or total graft excision when the infection has occurred in a hand-sewn graft.”
Unlike the typical bimodal distribution seen with hand-sewn graft infections, infection following endovascular repair of aortic aneurysms (EVAR) occurs from days up to 3 years after implantation. At the Mayo Clinic, a 79-year-old man presented with an infected endograft, psoas abscess, and Salmonella septicemia 4 years after EVAR.
“These infections are uncommon, but we are seeing more of them,” Dr. Bower said at a symposium on vascular surgery sponsored by Northwestern University.
Roughly two-thirds of patients will present with fever, nonspecific abdominal or back pain, malaise, weight loss or night sweats. If time permits, preoperative assessments include echocardiography for left ventricular function, arterial blood gases for pulmonary function since many patients are smokers, and renal ultrasound if creatinine is ≥ 1.5 mg/dL after rehydration. These tests are important because preoperative chronic obstructive pulmonary disease and renal dysfunction correlate with worse postoperative outcomes, he said.
Computed tomography angiography (CTA), however, stands as the single most important step of preoperative preparation, with the sine qua non of infection being air around the graft. Unlike hand-sewn grafts where infections can be localized, typically there is total graft involvement in these cases because the device is left inside the aneurysm sac. Aneurysms or pseudoaneurysms also have been seen above the infected device, including at the top end of suprarenal stents.
“This clearly has an impact on how we approach patients, but what’s become very apparent to me is that CTA often underestimates the amount of periaortic inflammation, especially at the juxta- and pararenal locations,” Dr. Bower said.
The Mayo group initially used in situ antibiotic-soaked prosthetic grafts for explanting EVAR devices, which yielded “acceptable mortality and reinfection rates, but primarily outstanding patency rates.” However, cryopreserved aortoiliac grafts have now become their first choice, Dr. Bower said. An ABO match is not imperative, preparation takes roughly 45 minutes, branch closures done in the lab are buttressed with sutures, and the graft is turned over to keep the lumbar arteries anterior, which offers an easy fix if there is bleeding, rather than having it on the posterior wall. Cryopreserved grafts, however, can dilate 40% and lengthen 10% under pressure.
“I’ve been burned more than once where the graft elongates more than I think, and I end up having to cut a small piece out to foreshorten it,” he said.
Reconstructions are tailored to patient anatomy. Surgeons should have several plans for reconstruction, including routing a graft through a remote path, remembering that CTA will underestimate the amount of periaortic inflammation. Separate bypasses of the renal or visceral arteries are performed first before the aortic clamp is applied to reduce physiologic stress. This requires knowledge of the supraceliac and pararenal aorta exposures, which really begins with the correct choice of incisions, Dr. Bower said. This is based on the aortic segment to be treated, position of the new graft, the aortic clamp site, and patient body habitus.
Most patients with EVAR infections are approached with a midline abdominal incision extended along the xiphoid process, which is the lynch pin for allowing upward and lateral retraction of the abdominal wall, he said. Choosing an incision that allows a more vertical orientation to where the new aortic anastomosis and clamp site will be, rather than operating in a keyhole, is important.
The second step is to open up the pararenal space by moving the viscera out of the way. This begins by ligating the inferior mesenteric vein and adjacent lymphatics, which allows incision of an avascular plane along the base of the left transverse colon. Retractor blades are set to allow the upward and lateral retraction of the small bowel, the left colon, and pancreas. Exposure of the suprarenal or supramesenteric aorta requires mobilization of the left renal vein after ligation and division of its branches.
“If that vein is intensely involved in inflammation, don’t ligate the branches in case you have to divide that vein at the caval confluence. Otherwise, you’ll run into some dysfunction of that left kidney,” Dr. Bower cautioned.
To have a secure place for the aortic cross clamp, the crura must be divided on either side of the diaphragm at or above the supramesenteric aorta, he added.
Key steps in total graft explantation are to drain abscesses prior to surgery to lower the bacterial burden and thus reduce the postoperative inflammatory response, bypass renal/visceral arteries first, if needed, remove the infected graft, debride the aorta to healthy tissue, place the new graft and cover it with omentum, and repair the bowel, if needed.
A piece of the proximal aortic wall should be sent to pathology to ensure the absence of bacteria or microabscesses. Organism-specific antibiotics are administered intravenously for 6-8 weeks followed by lifelong oral antibiotics, he said.
An earlier report involving 24 patients with infected aortic endografts (21 EVARs and 3 thoracic EVARs) treated at Mayo Clinic between 1997 and 2012 revealed polymicrobial infection in 11 patients, with methicillin-resistant Staphylococcus aureus being common. Potential contributors to infection were endovascular reintervention in eight, aortoenteric fistula/erosion in four, and various remote infections (J. Vasc. Surg. 2013;58:371-9).
Rifampin-soaked grafts were used in 15 patients, cryopreserved grafts in 4, femoral vein in 2, and axillofemoral grafts in 3. At a median of 14 months follow-up, patient survival, graft-related complications, and reinfection rates were 79%, 13%, and 4%, respectively, Dr. Bower said.
Dr. Bower reported having no financial disclosures.
EXPERT OPINION FROM THE NORTHWESTERN VASCULAR SYMPOSIUM
Hybrid carotid stents eyed with cautious optimism
CHICAGO – The next generation of hybrid carotid stents is slowly breathing life into the stagnant field of carotid artery stenting.
The new hybrid stents combine the flexibility of a traditional open-cell, nitinol stent with the stabilization typically offered by a closed-cell stent design. The initial clinical experience is limited, but shows promising results against embolization, Dr. Claudio Schönholz said at a symposium on vascular surgery sponsored by Northwestern University.
Last year, Dr. Schönholz and his colleagues at the Medical University of South Carolina in Charleston reported the first-in-man use of the investigational Gore Carotid Stent (W.L. Gore & Associates) (J. Endovasc. Thera. 2014 Aug;21:601-4).
As part of the Gore Carotid Stent Clinical Study for the Treatment of Carotid Artery Stenosis in Patients at Increased Risk for Adverse Events from Carotid Endarterectomy (SCAFFOLD) study, the team has successfully treated another four patients with no evidence of peri- or postprocedural neurological events. This included a case with such severe high-grade stenosis and slow flow that the external carotid artery was not even visible on imaging before the stent was placed, Dr. Schönholz said.
The Food and Drug Administration recently reviewed unreleased data for the first 100 patients enrolled in SCAFFOLD and given the green light for the multicenter, 312-patient study to resume with the start of the new year, he said.
Medtronic’s Cristallo Ideale hybrid stent is already approved outside the United States and was associated with no major neurological events and two cases of transient ischemic attack in 124 patients treated at four expert centers in Italy and Germany in the Cristallo study (J. Endovasc. Ther. 2008;15:186-92).
A more recent retrospective study revealed only one minor stroke in the perioperative period and during the first 30 days in 68 patients with symptomatic carotid stenosis treated by Turkish surgeons with the Cristallo Ideale stent and a proximal protection device (MO.MA, Invatec s.r.l., Medtronic, Italy) (Int. Angiol. 2014 Nov. 14. [Epub ahead of print]).
Better patient selection, increased operator experience, and use of embolic protection devices has reduced neurological events associated with carotid artery stenting, but embolization still occurs after protection devices are removed due to plaque protrusion through the stent struts, Dr. Schönholz said.
The unique design of the hybrid stents “may prevent plaque protrusion, eliminating peri- and postprocedural events,” he said.
The Cristallo Ideale hybrid stent is a nitinol-based stent that has a closed-cell portion at its center and an open-cell configuration on the distal and proximal sections.
In contrast, the Gore Carotid Stent has a closed-cell component throughout the entire device length that is created by placing an expanded polytetrafluoroethylene lattice with 500-micron pores over an open-cell frame. Once combined, both the stent frame and lattice are coated on all surfaces with Carmeda Bioactive Surface (CBAS) heparin. It’s action is limited only to the device surface and has no systemic anticoagulation effects, said Dr. Schönholz, who disclosed serving on Gore’s scientific advisory board.
The open-cell frame allows a high degree of flexibility and conformity to the native anatomy, while the stent lattice provides a high degree of plaque scaffolding that can reduce plaque prolapse, he said. The lattice also reduces the amount of emboli released during and after stent deployment and stabilizes the stent frame by resisting elongation as well as “fish-scaling,” or the misalignment of stent struts that protrude into the vessel wall, particularly when stents are deployed in tortuous anatomy.
When asked during a discussion whether the same results couldn’t be achieved by simply putting in another covered stent like a Viabahn, Dr. Schönholz replied that the Gore Stent isn’t a true covered stent because the 500-micron pores allow perfusion to be maintained to the external carotid artery. “It was intended to prevent plaque profusion, but at the same time allowing perfusion of the external carotid,” he said.
So far, the investigators have not incorporated intravascular ultrasound during stent placement, as it was not part of the SCAFFOLD protocol, but this will likely be used once the device is approved, he added.
Course director Dr. Mark K. Eskandari, chief of vascular surgery at Northwestern University in Chicago, said the results show that “carotid stenting isn’t dead yet and we can persevere. Advances in technology, both in regards to mechanical embolic protection devices and stent design systems, continue to improve the already great results of carotid artery stenting.”
CHICAGO – The next generation of hybrid carotid stents is slowly breathing life into the stagnant field of carotid artery stenting.
The new hybrid stents combine the flexibility of a traditional open-cell, nitinol stent with the stabilization typically offered by a closed-cell stent design. The initial clinical experience is limited, but shows promising results against embolization, Dr. Claudio Schönholz said at a symposium on vascular surgery sponsored by Northwestern University.
Last year, Dr. Schönholz and his colleagues at the Medical University of South Carolina in Charleston reported the first-in-man use of the investigational Gore Carotid Stent (W.L. Gore & Associates) (J. Endovasc. Thera. 2014 Aug;21:601-4).
As part of the Gore Carotid Stent Clinical Study for the Treatment of Carotid Artery Stenosis in Patients at Increased Risk for Adverse Events from Carotid Endarterectomy (SCAFFOLD) study, the team has successfully treated another four patients with no evidence of peri- or postprocedural neurological events. This included a case with such severe high-grade stenosis and slow flow that the external carotid artery was not even visible on imaging before the stent was placed, Dr. Schönholz said.
The Food and Drug Administration recently reviewed unreleased data for the first 100 patients enrolled in SCAFFOLD and given the green light for the multicenter, 312-patient study to resume with the start of the new year, he said.
Medtronic’s Cristallo Ideale hybrid stent is already approved outside the United States and was associated with no major neurological events and two cases of transient ischemic attack in 124 patients treated at four expert centers in Italy and Germany in the Cristallo study (J. Endovasc. Ther. 2008;15:186-92).
A more recent retrospective study revealed only one minor stroke in the perioperative period and during the first 30 days in 68 patients with symptomatic carotid stenosis treated by Turkish surgeons with the Cristallo Ideale stent and a proximal protection device (MO.MA, Invatec s.r.l., Medtronic, Italy) (Int. Angiol. 2014 Nov. 14. [Epub ahead of print]).
Better patient selection, increased operator experience, and use of embolic protection devices has reduced neurological events associated with carotid artery stenting, but embolization still occurs after protection devices are removed due to plaque protrusion through the stent struts, Dr. Schönholz said.
The unique design of the hybrid stents “may prevent plaque protrusion, eliminating peri- and postprocedural events,” he said.
The Cristallo Ideale hybrid stent is a nitinol-based stent that has a closed-cell portion at its center and an open-cell configuration on the distal and proximal sections.
In contrast, the Gore Carotid Stent has a closed-cell component throughout the entire device length that is created by placing an expanded polytetrafluoroethylene lattice with 500-micron pores over an open-cell frame. Once combined, both the stent frame and lattice are coated on all surfaces with Carmeda Bioactive Surface (CBAS) heparin. It’s action is limited only to the device surface and has no systemic anticoagulation effects, said Dr. Schönholz, who disclosed serving on Gore’s scientific advisory board.
The open-cell frame allows a high degree of flexibility and conformity to the native anatomy, while the stent lattice provides a high degree of plaque scaffolding that can reduce plaque prolapse, he said. The lattice also reduces the amount of emboli released during and after stent deployment and stabilizes the stent frame by resisting elongation as well as “fish-scaling,” or the misalignment of stent struts that protrude into the vessel wall, particularly when stents are deployed in tortuous anatomy.
When asked during a discussion whether the same results couldn’t be achieved by simply putting in another covered stent like a Viabahn, Dr. Schönholz replied that the Gore Stent isn’t a true covered stent because the 500-micron pores allow perfusion to be maintained to the external carotid artery. “It was intended to prevent plaque profusion, but at the same time allowing perfusion of the external carotid,” he said.
So far, the investigators have not incorporated intravascular ultrasound during stent placement, as it was not part of the SCAFFOLD protocol, but this will likely be used once the device is approved, he added.
Course director Dr. Mark K. Eskandari, chief of vascular surgery at Northwestern University in Chicago, said the results show that “carotid stenting isn’t dead yet and we can persevere. Advances in technology, both in regards to mechanical embolic protection devices and stent design systems, continue to improve the already great results of carotid artery stenting.”
CHICAGO – The next generation of hybrid carotid stents is slowly breathing life into the stagnant field of carotid artery stenting.
The new hybrid stents combine the flexibility of a traditional open-cell, nitinol stent with the stabilization typically offered by a closed-cell stent design. The initial clinical experience is limited, but shows promising results against embolization, Dr. Claudio Schönholz said at a symposium on vascular surgery sponsored by Northwestern University.
Last year, Dr. Schönholz and his colleagues at the Medical University of South Carolina in Charleston reported the first-in-man use of the investigational Gore Carotid Stent (W.L. Gore & Associates) (J. Endovasc. Thera. 2014 Aug;21:601-4).
As part of the Gore Carotid Stent Clinical Study for the Treatment of Carotid Artery Stenosis in Patients at Increased Risk for Adverse Events from Carotid Endarterectomy (SCAFFOLD) study, the team has successfully treated another four patients with no evidence of peri- or postprocedural neurological events. This included a case with such severe high-grade stenosis and slow flow that the external carotid artery was not even visible on imaging before the stent was placed, Dr. Schönholz said.
The Food and Drug Administration recently reviewed unreleased data for the first 100 patients enrolled in SCAFFOLD and given the green light for the multicenter, 312-patient study to resume with the start of the new year, he said.
Medtronic’s Cristallo Ideale hybrid stent is already approved outside the United States and was associated with no major neurological events and two cases of transient ischemic attack in 124 patients treated at four expert centers in Italy and Germany in the Cristallo study (J. Endovasc. Ther. 2008;15:186-92).
A more recent retrospective study revealed only one minor stroke in the perioperative period and during the first 30 days in 68 patients with symptomatic carotid stenosis treated by Turkish surgeons with the Cristallo Ideale stent and a proximal protection device (MO.MA, Invatec s.r.l., Medtronic, Italy) (Int. Angiol. 2014 Nov. 14. [Epub ahead of print]).
Better patient selection, increased operator experience, and use of embolic protection devices has reduced neurological events associated with carotid artery stenting, but embolization still occurs after protection devices are removed due to plaque protrusion through the stent struts, Dr. Schönholz said.
The unique design of the hybrid stents “may prevent plaque protrusion, eliminating peri- and postprocedural events,” he said.
The Cristallo Ideale hybrid stent is a nitinol-based stent that has a closed-cell portion at its center and an open-cell configuration on the distal and proximal sections.
In contrast, the Gore Carotid Stent has a closed-cell component throughout the entire device length that is created by placing an expanded polytetrafluoroethylene lattice with 500-micron pores over an open-cell frame. Once combined, both the stent frame and lattice are coated on all surfaces with Carmeda Bioactive Surface (CBAS) heparin. It’s action is limited only to the device surface and has no systemic anticoagulation effects, said Dr. Schönholz, who disclosed serving on Gore’s scientific advisory board.
The open-cell frame allows a high degree of flexibility and conformity to the native anatomy, while the stent lattice provides a high degree of plaque scaffolding that can reduce plaque prolapse, he said. The lattice also reduces the amount of emboli released during and after stent deployment and stabilizes the stent frame by resisting elongation as well as “fish-scaling,” or the misalignment of stent struts that protrude into the vessel wall, particularly when stents are deployed in tortuous anatomy.
When asked during a discussion whether the same results couldn’t be achieved by simply putting in another covered stent like a Viabahn, Dr. Schönholz replied that the Gore Stent isn’t a true covered stent because the 500-micron pores allow perfusion to be maintained to the external carotid artery. “It was intended to prevent plaque profusion, but at the same time allowing perfusion of the external carotid,” he said.
So far, the investigators have not incorporated intravascular ultrasound during stent placement, as it was not part of the SCAFFOLD protocol, but this will likely be used once the device is approved, he added.
Course director Dr. Mark K. Eskandari, chief of vascular surgery at Northwestern University in Chicago, said the results show that “carotid stenting isn’t dead yet and we can persevere. Advances in technology, both in regards to mechanical embolic protection devices and stent design systems, continue to improve the already great results of carotid artery stenting.”
EXPERT ANALYSIS FROM THE NORTHWESTERN VASCULAR SYMPOSIUM
Most thyroid nodules have favorable prognosis
During 5 years of follow-up, cancer arose in only 0.3% of thyroid nodules that were cytologically and sonographically benign at baseline, according to a large prospective study published online March 3 in JAMA.
Furthermore, only two of the five nodules that became cancerous had grown beforehand, reported Dr. Cosimo Durante of the Sapienza University of Rome and his associates. “These data suggest that the American Thyroid Association’s recommendation for indication for repeat cytology should be revised. Clinical and sonographic findings should probably play larger roles in the decision-making process,” the researchers said (JAMA 2015;313:926-35).
Advances in diagnostic imaging have increased the detection of thyroid nodules, the great majority of which are found to be benign. For such nodules, the ATA recommends repeating thyroid ultrasonography at 6-18 months and then every 3-5 years thereafter, as long as nodules do not significantly grow (defined as at least a 20% increase in two nodule diameters, with a minimum increase of at least 2 mm [Thyroid 2009;19:1167-214]). But little is known about rate, extent, or predictors of nodule growth, the researchers noted. Therefore, they performed annual thyroid ultrasound examinations on 992 patients who had one to four asymptomatic subcentimeter thyroid modules that were cytologically or sonographically benign at baseline.
After 5 years of follow-up, just 15.4% of patients had experienced significant nodule growth according to the ATA definition, the researchers reported. Average growth was 4.9 mm, and 9.3% of patients developed new nodules, of which one was found to be cancerous. Growth was least likely when a patient’s largest nodule measured 7.5 mm or less and was significantly more likely when patients had multiple nodules instead of one; had baseline nodule volume greater than 0.2 mL; were up to 45 years old, compared with at least 60 years of age; and were male, the investigators said.
Among older patients, having a body mass index of 28.6 kg/m2 more than doubled the odds of nodule growth, in keeping with recent reports linking obesity and insulin resistance with nodular thyroid disease, they added.
The findings suggest that repeat thyroid ultrasonography could be safely extended to 12 months for initial follow-up and to every 5 years thereafter for most patients, as long as nodule size remained stable, Dr. Durante and his associates said. “This approach should be suitable for about 85% of patients, whose risk of disease progression is low. Closer surveillance may be appropriate for nodules occurring in younger patients or older overweight individuals with multiple nodules, large nodules (greater than 7.5 mm), or both,” they added.
The Umberto Di Mario Foundation, Banca d’Italia, and the Italian Thyroid Cancer Observatory Foundation funded the study. The authors reported having no conflicts of interest.
Thyroid nodules are pervasive, whereas thyroid cancer is not. The findings from Durante et al represent an important step in improving the efficiency and mitigating the expense of follow-up for the vast majority of thyroid nodules that are either cytologically or sonographically benign.
These prospective data provide reassurance about the validity of a benign cytology result obtained by ultrasound-guided fine-needle aspiration and confirm a very low false-negative rate, at 1.1%. The practice of routine sonographic surveillance with repeat fine-needle aspiration for growth, as recommended by published guidelines, is not the most efficient strategy to detect the very small number of missed cancers among previously sampled cytologically benign nodules. The one-size-fits-all approach simply does not work. Instead, surveillance strategies should be individualized based on a nodule’s sonographic appearance.
Many nodules detected on ultrasound are small (less than 1 cm) and not sonographically suspicious. In the study by Durante et al, only one cancer was diagnosed during follow-up among the 852 sonographically benign nodules that were smaller than 1 cm. Of note, the trigger for fine-needle aspiration for this nodule was development of hypoechogenicity and irregular margins, not growth.
Although 69% of nodules [in the study] remained stable in size, size increase was not a harbinger of malignancy, especially if the nodule had no sonographically suspicious features.
Anne R. Cappola, M.D., Sc.M., and Susan J. Mandel, M.D., M.P.H., are with the University of Pennsylvania, Philadelphia. Dr. Cappola is also an associate editor of JAMA. These comments are based on their accompanying editorial (JAMA 2015 March 3 [doi:10.1001/jama.2015.0836]).
Thyroid nodules are pervasive, whereas thyroid cancer is not. The findings from Durante et al represent an important step in improving the efficiency and mitigating the expense of follow-up for the vast majority of thyroid nodules that are either cytologically or sonographically benign.
These prospective data provide reassurance about the validity of a benign cytology result obtained by ultrasound-guided fine-needle aspiration and confirm a very low false-negative rate, at 1.1%. The practice of routine sonographic surveillance with repeat fine-needle aspiration for growth, as recommended by published guidelines, is not the most efficient strategy to detect the very small number of missed cancers among previously sampled cytologically benign nodules. The one-size-fits-all approach simply does not work. Instead, surveillance strategies should be individualized based on a nodule’s sonographic appearance.
Many nodules detected on ultrasound are small (less than 1 cm) and not sonographically suspicious. In the study by Durante et al, only one cancer was diagnosed during follow-up among the 852 sonographically benign nodules that were smaller than 1 cm. Of note, the trigger for fine-needle aspiration for this nodule was development of hypoechogenicity and irregular margins, not growth.
Although 69% of nodules [in the study] remained stable in size, size increase was not a harbinger of malignancy, especially if the nodule had no sonographically suspicious features.
Anne R. Cappola, M.D., Sc.M., and Susan J. Mandel, M.D., M.P.H., are with the University of Pennsylvania, Philadelphia. Dr. Cappola is also an associate editor of JAMA. These comments are based on their accompanying editorial (JAMA 2015 March 3 [doi:10.1001/jama.2015.0836]).
Thyroid nodules are pervasive, whereas thyroid cancer is not. The findings from Durante et al represent an important step in improving the efficiency and mitigating the expense of follow-up for the vast majority of thyroid nodules that are either cytologically or sonographically benign.
These prospective data provide reassurance about the validity of a benign cytology result obtained by ultrasound-guided fine-needle aspiration and confirm a very low false-negative rate, at 1.1%. The practice of routine sonographic surveillance with repeat fine-needle aspiration for growth, as recommended by published guidelines, is not the most efficient strategy to detect the very small number of missed cancers among previously sampled cytologically benign nodules. The one-size-fits-all approach simply does not work. Instead, surveillance strategies should be individualized based on a nodule’s sonographic appearance.
Many nodules detected on ultrasound are small (less than 1 cm) and not sonographically suspicious. In the study by Durante et al, only one cancer was diagnosed during follow-up among the 852 sonographically benign nodules that were smaller than 1 cm. Of note, the trigger for fine-needle aspiration for this nodule was development of hypoechogenicity and irregular margins, not growth.
Although 69% of nodules [in the study] remained stable in size, size increase was not a harbinger of malignancy, especially if the nodule had no sonographically suspicious features.
Anne R. Cappola, M.D., Sc.M., and Susan J. Mandel, M.D., M.P.H., are with the University of Pennsylvania, Philadelphia. Dr. Cappola is also an associate editor of JAMA. These comments are based on their accompanying editorial (JAMA 2015 March 3 [doi:10.1001/jama.2015.0836]).
During 5 years of follow-up, cancer arose in only 0.3% of thyroid nodules that were cytologically and sonographically benign at baseline, according to a large prospective study published online March 3 in JAMA.
Furthermore, only two of the five nodules that became cancerous had grown beforehand, reported Dr. Cosimo Durante of the Sapienza University of Rome and his associates. “These data suggest that the American Thyroid Association’s recommendation for indication for repeat cytology should be revised. Clinical and sonographic findings should probably play larger roles in the decision-making process,” the researchers said (JAMA 2015;313:926-35).
Advances in diagnostic imaging have increased the detection of thyroid nodules, the great majority of which are found to be benign. For such nodules, the ATA recommends repeating thyroid ultrasonography at 6-18 months and then every 3-5 years thereafter, as long as nodules do not significantly grow (defined as at least a 20% increase in two nodule diameters, with a minimum increase of at least 2 mm [Thyroid 2009;19:1167-214]). But little is known about rate, extent, or predictors of nodule growth, the researchers noted. Therefore, they performed annual thyroid ultrasound examinations on 992 patients who had one to four asymptomatic subcentimeter thyroid modules that were cytologically or sonographically benign at baseline.
After 5 years of follow-up, just 15.4% of patients had experienced significant nodule growth according to the ATA definition, the researchers reported. Average growth was 4.9 mm, and 9.3% of patients developed new nodules, of which one was found to be cancerous. Growth was least likely when a patient’s largest nodule measured 7.5 mm or less and was significantly more likely when patients had multiple nodules instead of one; had baseline nodule volume greater than 0.2 mL; were up to 45 years old, compared with at least 60 years of age; and were male, the investigators said.
Among older patients, having a body mass index of 28.6 kg/m2 more than doubled the odds of nodule growth, in keeping with recent reports linking obesity and insulin resistance with nodular thyroid disease, they added.
The findings suggest that repeat thyroid ultrasonography could be safely extended to 12 months for initial follow-up and to every 5 years thereafter for most patients, as long as nodule size remained stable, Dr. Durante and his associates said. “This approach should be suitable for about 85% of patients, whose risk of disease progression is low. Closer surveillance may be appropriate for nodules occurring in younger patients or older overweight individuals with multiple nodules, large nodules (greater than 7.5 mm), or both,” they added.
The Umberto Di Mario Foundation, Banca d’Italia, and the Italian Thyroid Cancer Observatory Foundation funded the study. The authors reported having no conflicts of interest.
During 5 years of follow-up, cancer arose in only 0.3% of thyroid nodules that were cytologically and sonographically benign at baseline, according to a large prospective study published online March 3 in JAMA.
Furthermore, only two of the five nodules that became cancerous had grown beforehand, reported Dr. Cosimo Durante of the Sapienza University of Rome and his associates. “These data suggest that the American Thyroid Association’s recommendation for indication for repeat cytology should be revised. Clinical and sonographic findings should probably play larger roles in the decision-making process,” the researchers said (JAMA 2015;313:926-35).
Advances in diagnostic imaging have increased the detection of thyroid nodules, the great majority of which are found to be benign. For such nodules, the ATA recommends repeating thyroid ultrasonography at 6-18 months and then every 3-5 years thereafter, as long as nodules do not significantly grow (defined as at least a 20% increase in two nodule diameters, with a minimum increase of at least 2 mm [Thyroid 2009;19:1167-214]). But little is known about rate, extent, or predictors of nodule growth, the researchers noted. Therefore, they performed annual thyroid ultrasound examinations on 992 patients who had one to four asymptomatic subcentimeter thyroid modules that were cytologically or sonographically benign at baseline.
After 5 years of follow-up, just 15.4% of patients had experienced significant nodule growth according to the ATA definition, the researchers reported. Average growth was 4.9 mm, and 9.3% of patients developed new nodules, of which one was found to be cancerous. Growth was least likely when a patient’s largest nodule measured 7.5 mm or less and was significantly more likely when patients had multiple nodules instead of one; had baseline nodule volume greater than 0.2 mL; were up to 45 years old, compared with at least 60 years of age; and were male, the investigators said.
Among older patients, having a body mass index of 28.6 kg/m2 more than doubled the odds of nodule growth, in keeping with recent reports linking obesity and insulin resistance with nodular thyroid disease, they added.
The findings suggest that repeat thyroid ultrasonography could be safely extended to 12 months for initial follow-up and to every 5 years thereafter for most patients, as long as nodule size remained stable, Dr. Durante and his associates said. “This approach should be suitable for about 85% of patients, whose risk of disease progression is low. Closer surveillance may be appropriate for nodules occurring in younger patients or older overweight individuals with multiple nodules, large nodules (greater than 7.5 mm), or both,” they added.
The Umberto Di Mario Foundation, Banca d’Italia, and the Italian Thyroid Cancer Observatory Foundation funded the study. The authors reported having no conflicts of interest.
FROM JAMA
Key clinical point: The vast majority of thyroid nodules found to be benign at baseline remained so 5 years later.
Major finding: Cancer arose in only 0.3% of nodules in 5 years of follow-up.
Data source: Prospective, multicenter, observational study of 992 patients with 1,567 asymptomatic thyroid nodules.
Disclosures: The Umberto Di Mario Foundation, Banca d’Italia, and the Italian Thyroid Cancer Observatory Foundation funded the study. The authors reported having no conflicts of interest.
ACP guidelines for preventing, treating pressure ulcers
Alternating-air and low-air-loss mattresses and overlays have little data to support their use for preventing or treating pressure ulcers, the Clinical Guidelines Committee of the American College of Physicians has concluded.
Many U.S. acute-care hospitals, home caregivers, and long-term nursing facilities use alternating-air and low-air-loss mattresses and overlays, even though the evidence in favor of using these surfaces is sparse and of poor quality, the guideline writers said.
The devices have not been show to actually reduce pressure ulcers. The harms have been poorly reported but could be significant. “Using these support systems is expensive and adds unnecessary burden on the health care system. Based on a review of the current evidence, lower-cost support surfaces should be the preferred approach to care,” Dr. Amir Qaseem, of the ACP, Philadelphia, and his associates wrote.
The committee performed an extensive review of the literature on pressure ulcers and compiled two Clinical Practice Guidelines – one concerning prevention (Ann. Intern. Med. 2015;162 [doi:10.7326/M14-1567]) and the other concerning treatment (Ann. Intern. Med. 2015;162 [doi:10.7326/M14-1568]) – in part because “a growing industry” has developed in recent years and aggressively pitches a wide array of products for this patient population. The guidelines present the available evidence on the comparative effectiveness of tools and strategies but state repeatedly that evidence regarding pressure ulcers is sparse and of poor quality.
The prevention guideline strongly recommends that clinicians choose advanced static mattresses or advanced static overlays rather than standard hospital mattresses for at-risk patients. Static mattresses and advanced static overlays provide a constant level of inflation or support and evenly distribute body weight. These products are among the few actually shown to reduce the incidence of pressure ulcers. They are also preferable to alternating-air mattresses and overlays, which change the distribution of pressure by inflating or deflating cells within the devices, and to low-air-loss mattresses and overlays, which use flowing air to regulate heat and humidity and adjust pressure.
Evidence is similarly poor or lacking concerning the use of other support surfaces such as heel supports or boots and a variety of wheelchair cushions. Also lacking evidence are other preventive interventions that extend beyond “usual care,” such as different types of repositioning schemes, a variety of leg elevations, various nutritional supplements, and a wide variety of skin care strategies and topical treatments.
The prevention guideline advises patient assessments to identify those at risk of developing pressure ulcers. However, there is not enough evidence to demonstrate that any one of the many risk assessment tools for this purpose is superior to the others, nor that any of these tools is superior to simple clinical judgment. Risk factors for pressure ulcers include older age; black race or Hispanic ethnicity; low body weight; cognitive impairment; physical impairments; and comorbid conditions that may affect soft-tissue integrity and healing, such as urinary or fecal incontinence, diabetes, edema, impaired microcirculation, hypoalbuminemia, and malnutrition, Dr. Qaseem and his associates wrote (Ann. Intern. Med. 2015 March 2 [doi:10.7326/M14-1567]).
The treatment guideline for patients who already have pressure ulcers similarly notes that the lack of evidence for advanced support surfaces such as alternating-air and low-air-loss mattresses and overlays. It similarly recommends advanced static mattresses or overlays for these patients.
The treatment guideline recommends protein or amino acid supplements as well as hydrocolloid or foam dressings to reduce wound size, and electrical stimulation to accelerate wound healing. The evidence for these recommendations is “weak” and of low- to moderate-quality, Dr. Qaseem and his associates said (Ann. Intern. Med. 2015 March 2 [doi:10.7326/M14-1568]).
The evidence for the safety and efficacy of hyperbaric oxygen therapy, even though it is often used to treat pressure ulcers in hospitals, is similarly inconclusive. Also lacking good-quality evidence are the use of alternating-air chair cushions, three-dimensional polyester overlays, zinc supplements, L-carnosine supplements, wound dressings other than the ones already discussed, debriding enzymes, topical phenytoin, maggot therapy, biological agents other than platelet-derived growth factor, or hydrotherapy in which wounds are cleaned using a whirlpool or pulsed lavage.
These guidelines emphasize the dire need for good science to guide both prevention and treatment of pressure ulcers. Despite the ubiquity of pressure ulcers and their potential to threaten life and limb, clinical management varies greatly. Most of the research in this field to date has been underpowered and focused on early signs of healing rather than on more definitive outcomes.
Joyce Black, Ph.D., R.N., is at the University of Nebraska Medical Center, Omaha. Her financial disclosures are available at www.acponline.org. Dr. Black made these remarks in an editorial accompanying the ACP Clinical Practice Guidelines on prevention and treatment of pressure ulcers (Ann. Intern. Med. 2015 March 2 [doi:10.1326/M15-0190]).
These guidelines emphasize the dire need for good science to guide both prevention and treatment of pressure ulcers. Despite the ubiquity of pressure ulcers and their potential to threaten life and limb, clinical management varies greatly. Most of the research in this field to date has been underpowered and focused on early signs of healing rather than on more definitive outcomes.
Joyce Black, Ph.D., R.N., is at the University of Nebraska Medical Center, Omaha. Her financial disclosures are available at www.acponline.org. Dr. Black made these remarks in an editorial accompanying the ACP Clinical Practice Guidelines on prevention and treatment of pressure ulcers (Ann. Intern. Med. 2015 March 2 [doi:10.1326/M15-0190]).
These guidelines emphasize the dire need for good science to guide both prevention and treatment of pressure ulcers. Despite the ubiquity of pressure ulcers and their potential to threaten life and limb, clinical management varies greatly. Most of the research in this field to date has been underpowered and focused on early signs of healing rather than on more definitive outcomes.
Joyce Black, Ph.D., R.N., is at the University of Nebraska Medical Center, Omaha. Her financial disclosures are available at www.acponline.org. Dr. Black made these remarks in an editorial accompanying the ACP Clinical Practice Guidelines on prevention and treatment of pressure ulcers (Ann. Intern. Med. 2015 March 2 [doi:10.1326/M15-0190]).
Alternating-air and low-air-loss mattresses and overlays have little data to support their use for preventing or treating pressure ulcers, the Clinical Guidelines Committee of the American College of Physicians has concluded.
Many U.S. acute-care hospitals, home caregivers, and long-term nursing facilities use alternating-air and low-air-loss mattresses and overlays, even though the evidence in favor of using these surfaces is sparse and of poor quality, the guideline writers said.
The devices have not been show to actually reduce pressure ulcers. The harms have been poorly reported but could be significant. “Using these support systems is expensive and adds unnecessary burden on the health care system. Based on a review of the current evidence, lower-cost support surfaces should be the preferred approach to care,” Dr. Amir Qaseem, of the ACP, Philadelphia, and his associates wrote.
The committee performed an extensive review of the literature on pressure ulcers and compiled two Clinical Practice Guidelines – one concerning prevention (Ann. Intern. Med. 2015;162 [doi:10.7326/M14-1567]) and the other concerning treatment (Ann. Intern. Med. 2015;162 [doi:10.7326/M14-1568]) – in part because “a growing industry” has developed in recent years and aggressively pitches a wide array of products for this patient population. The guidelines present the available evidence on the comparative effectiveness of tools and strategies but state repeatedly that evidence regarding pressure ulcers is sparse and of poor quality.
The prevention guideline strongly recommends that clinicians choose advanced static mattresses or advanced static overlays rather than standard hospital mattresses for at-risk patients. Static mattresses and advanced static overlays provide a constant level of inflation or support and evenly distribute body weight. These products are among the few actually shown to reduce the incidence of pressure ulcers. They are also preferable to alternating-air mattresses and overlays, which change the distribution of pressure by inflating or deflating cells within the devices, and to low-air-loss mattresses and overlays, which use flowing air to regulate heat and humidity and adjust pressure.
Evidence is similarly poor or lacking concerning the use of other support surfaces such as heel supports or boots and a variety of wheelchair cushions. Also lacking evidence are other preventive interventions that extend beyond “usual care,” such as different types of repositioning schemes, a variety of leg elevations, various nutritional supplements, and a wide variety of skin care strategies and topical treatments.
The prevention guideline advises patient assessments to identify those at risk of developing pressure ulcers. However, there is not enough evidence to demonstrate that any one of the many risk assessment tools for this purpose is superior to the others, nor that any of these tools is superior to simple clinical judgment. Risk factors for pressure ulcers include older age; black race or Hispanic ethnicity; low body weight; cognitive impairment; physical impairments; and comorbid conditions that may affect soft-tissue integrity and healing, such as urinary or fecal incontinence, diabetes, edema, impaired microcirculation, hypoalbuminemia, and malnutrition, Dr. Qaseem and his associates wrote (Ann. Intern. Med. 2015 March 2 [doi:10.7326/M14-1567]).
The treatment guideline for patients who already have pressure ulcers similarly notes that the lack of evidence for advanced support surfaces such as alternating-air and low-air-loss mattresses and overlays. It similarly recommends advanced static mattresses or overlays for these patients.
The treatment guideline recommends protein or amino acid supplements as well as hydrocolloid or foam dressings to reduce wound size, and electrical stimulation to accelerate wound healing. The evidence for these recommendations is “weak” and of low- to moderate-quality, Dr. Qaseem and his associates said (Ann. Intern. Med. 2015 March 2 [doi:10.7326/M14-1568]).
The evidence for the safety and efficacy of hyperbaric oxygen therapy, even though it is often used to treat pressure ulcers in hospitals, is similarly inconclusive. Also lacking good-quality evidence are the use of alternating-air chair cushions, three-dimensional polyester overlays, zinc supplements, L-carnosine supplements, wound dressings other than the ones already discussed, debriding enzymes, topical phenytoin, maggot therapy, biological agents other than platelet-derived growth factor, or hydrotherapy in which wounds are cleaned using a whirlpool or pulsed lavage.
Alternating-air and low-air-loss mattresses and overlays have little data to support their use for preventing or treating pressure ulcers, the Clinical Guidelines Committee of the American College of Physicians has concluded.
Many U.S. acute-care hospitals, home caregivers, and long-term nursing facilities use alternating-air and low-air-loss mattresses and overlays, even though the evidence in favor of using these surfaces is sparse and of poor quality, the guideline writers said.
The devices have not been show to actually reduce pressure ulcers. The harms have been poorly reported but could be significant. “Using these support systems is expensive and adds unnecessary burden on the health care system. Based on a review of the current evidence, lower-cost support surfaces should be the preferred approach to care,” Dr. Amir Qaseem, of the ACP, Philadelphia, and his associates wrote.
The committee performed an extensive review of the literature on pressure ulcers and compiled two Clinical Practice Guidelines – one concerning prevention (Ann. Intern. Med. 2015;162 [doi:10.7326/M14-1567]) and the other concerning treatment (Ann. Intern. Med. 2015;162 [doi:10.7326/M14-1568]) – in part because “a growing industry” has developed in recent years and aggressively pitches a wide array of products for this patient population. The guidelines present the available evidence on the comparative effectiveness of tools and strategies but state repeatedly that evidence regarding pressure ulcers is sparse and of poor quality.
The prevention guideline strongly recommends that clinicians choose advanced static mattresses or advanced static overlays rather than standard hospital mattresses for at-risk patients. Static mattresses and advanced static overlays provide a constant level of inflation or support and evenly distribute body weight. These products are among the few actually shown to reduce the incidence of pressure ulcers. They are also preferable to alternating-air mattresses and overlays, which change the distribution of pressure by inflating or deflating cells within the devices, and to low-air-loss mattresses and overlays, which use flowing air to regulate heat and humidity and adjust pressure.
Evidence is similarly poor or lacking concerning the use of other support surfaces such as heel supports or boots and a variety of wheelchair cushions. Also lacking evidence are other preventive interventions that extend beyond “usual care,” such as different types of repositioning schemes, a variety of leg elevations, various nutritional supplements, and a wide variety of skin care strategies and topical treatments.
The prevention guideline advises patient assessments to identify those at risk of developing pressure ulcers. However, there is not enough evidence to demonstrate that any one of the many risk assessment tools for this purpose is superior to the others, nor that any of these tools is superior to simple clinical judgment. Risk factors for pressure ulcers include older age; black race or Hispanic ethnicity; low body weight; cognitive impairment; physical impairments; and comorbid conditions that may affect soft-tissue integrity and healing, such as urinary or fecal incontinence, diabetes, edema, impaired microcirculation, hypoalbuminemia, and malnutrition, Dr. Qaseem and his associates wrote (Ann. Intern. Med. 2015 March 2 [doi:10.7326/M14-1567]).
The treatment guideline for patients who already have pressure ulcers similarly notes that the lack of evidence for advanced support surfaces such as alternating-air and low-air-loss mattresses and overlays. It similarly recommends advanced static mattresses or overlays for these patients.
The treatment guideline recommends protein or amino acid supplements as well as hydrocolloid or foam dressings to reduce wound size, and electrical stimulation to accelerate wound healing. The evidence for these recommendations is “weak” and of low- to moderate-quality, Dr. Qaseem and his associates said (Ann. Intern. Med. 2015 March 2 [doi:10.7326/M14-1568]).
The evidence for the safety and efficacy of hyperbaric oxygen therapy, even though it is often used to treat pressure ulcers in hospitals, is similarly inconclusive. Also lacking good-quality evidence are the use of alternating-air chair cushions, three-dimensional polyester overlays, zinc supplements, L-carnosine supplements, wound dressings other than the ones already discussed, debriding enzymes, topical phenytoin, maggot therapy, biological agents other than platelet-derived growth factor, or hydrotherapy in which wounds are cleaned using a whirlpool or pulsed lavage.
STS releases public surgical outcomes report
The Society of Thoracic Surgeons has released a public online report of national surgical outcomes from its Congenital Heart Surgery Database, the association has announced.
The STS report focuses on pediatric and congenital cardiac malformations, and includes 4-year observed, expected, and risk-adjusted mortality rates, the society said in a statement.
Twenty-five sites participated in the first round of STS public online reporting, similar to the observed participation in the first round of public reporting in the STS Adult Cardiac Surgery Database, which started in 2010.
“Reporting hospital surgical outcomes using risk-adjusted analysis is extremely important because it allows for a fair assessment, on a level playing field, of outcomes across hospitals that treat different populations of patients,” Dr. Marshall L. Jacobs, STS CHSD Task Force chair, said in the statement.
For more information, visit http://www.sts.org/quality-research-patient-safety/sts-public-reporting-online.
The Society of Thoracic Surgeons has released a public online report of national surgical outcomes from its Congenital Heart Surgery Database, the association has announced.
The STS report focuses on pediatric and congenital cardiac malformations, and includes 4-year observed, expected, and risk-adjusted mortality rates, the society said in a statement.
Twenty-five sites participated in the first round of STS public online reporting, similar to the observed participation in the first round of public reporting in the STS Adult Cardiac Surgery Database, which started in 2010.
“Reporting hospital surgical outcomes using risk-adjusted analysis is extremely important because it allows for a fair assessment, on a level playing field, of outcomes across hospitals that treat different populations of patients,” Dr. Marshall L. Jacobs, STS CHSD Task Force chair, said in the statement.
For more information, visit http://www.sts.org/quality-research-patient-safety/sts-public-reporting-online.
The Society of Thoracic Surgeons has released a public online report of national surgical outcomes from its Congenital Heart Surgery Database, the association has announced.
The STS report focuses on pediatric and congenital cardiac malformations, and includes 4-year observed, expected, and risk-adjusted mortality rates, the society said in a statement.
Twenty-five sites participated in the first round of STS public online reporting, similar to the observed participation in the first round of public reporting in the STS Adult Cardiac Surgery Database, which started in 2010.
“Reporting hospital surgical outcomes using risk-adjusted analysis is extremely important because it allows for a fair assessment, on a level playing field, of outcomes across hospitals that treat different populations of patients,” Dr. Marshall L. Jacobs, STS CHSD Task Force chair, said in the statement.
For more information, visit http://www.sts.org/quality-research-patient-safety/sts-public-reporting-online.
Justices gear up to hear arguments in ACA subsidy case
The showdown over federal subsidies under the Affordable Care Act commences March 4 as Supreme Court justices prepare to hear arguments in King v. Burwell. The outcome could significantly alter the ACA and impact millions of patients and their physicians.
“King v. Burwell is extremely important to patients and physicians alike,” said Danielle C. Gray, a New York attorney and coauthor of a brief on behalf of the American Academy of Pediatrics (AAP), the American Academy of Family Physicians (AAFP), and other groups in support of the government. “All told, studies predict that a ruling in petitioners’ favor would leave 8 million Americans uninsured and cause premiums to rise by almost 50% for those who continue to purchase insurance on federally facilitated exchanges. Physicians would likely see a significant drop in the number of insured patients, which would affect their treatment options and protocol.”
King supporters argue that the basis of the case is being lost in impact studies and outcome projections. The case is about the meaning of ACA language concerning subsidies and whether the executive branch has the authority to change laws as it sees fit, said Ilya Shapiro a senior fellow in constitutional studies at the Cato Institute, a libertarian public policy organization. The group issued a brief to the high court in support of King.
“A lot of arguments in the litigation and the media concern these sort of nightmare scenarios about people losing coverage. … You see some of that in the amicus briefs supporting the government,” Mr. Shapiro said in an interview. “A lot of them are … just kind of painting nightmare policy scenarios, which really should play no role in how you interpret the law.”
King v. Burwell centers on whether residents in states that rely on the federal marketplace are eligible for tax credits to purchase insurance or whether such assistance can go only to residents who purchase insurance via a state-run marketplace. The ACA states that tax credits apply to insurance purchased through an exchange “established by the state.” Challengers argue the law does not mention the federal exchange and that the subsidies are available only for purchases through state exchanges. The government interprets the ACA to allow subsidies whenever patients buys insurance on any exchange.
The future of the ACA depends on the Supreme Court’s interpretation of the language, said Eric J. Segall, professor of law at Georgia State University, Atlanta. Mr. Segall has written on the merits of King v. Burwell, including a recent opinion in the University of Pennsylvania Law Review.
The basis of the ACA comprises three key components: that insurers provide health insurance without denying coverage to patients with preexisting conditions; that the individual mandate that requires all Americans buy insurance; and that the availability of tax subsidies that ensures lower- and middle-income residents can afford to comply with the mandate.
“That third leg, the subsidies, is just as important as the first two legs,” he said in an interview. “If you cut off any of the three legs, the entire purpose of the Affordable Care Act is undercut and the law would be in serious danger.”
Mr. Segall said that he believes the plaintiffs cannot legally demonstrate that the ACA as a whole, clearly and unambiguously precludes tax credits to people who buy health insurance from federal exchanges. If a law is ambiguous or unclear, an agency’s decision must be upheld if it is reasonable, he notes. Given the structure of the ACA and its reliance on the three essential components, it is a reasonable interpretation that the statute allows for subsidies on both state and federal exchanges, Mr. Segall said.
However, King supporters argue the case should turn on the constitutional principle that neither a federal court nor an executive agency can ignore or override a law’s plain meaning.
“The U.S. Supreme Court believes in clear language, and the language in the law clearly states that the subsidies were available only to an exchange established by the state,” said Sally C. Pipes, president and CEO of the Pacific Research Institute, a San Francisco-based think tank and public policy research institute. The Institute issued a brief in support of King. “By giving subsidies [to] the 37 states that have federal exchanges or exchanges that are jointly operated, it goes against the written intent of the law.”
More than 50 friend of the court briefs have been sent to the high court in support or opposition of King, including comments from the American College of Physicians, the American Thoracic Society and the American Hospital Association. The ACP and its allies urged the court to uphold the premium subsidies created by the ACA in all states.
A Supreme Court ruling to overturn the subsidies would not only disrupt care for millions of patients, but also harm the physician-patient relationship and fuel uncompensated care, said Robert B. Doherty, ACP’s senior vice president for governmental affairs and public policy.
“On a practical level, it would introduce chaos in the patient-physician relationship, especially if an adverse ruling by the Supreme Court took effect immediately, as people – including people, such as cancer patients, who are currently undergoing treatment – immediately lost their coverage, and their physicians and hospitals then have to figure out how to continue to get them the care they need without insurance,” Mr. Doherty said in an interview.
Estimates vary on how many Americans could lose subsidies in 2016 if the high court strikes down the financial assistance. An Urban Institute analysis estimated that just over 6 million people would lose coverage; one from RAND finds that individual-market enrollment would decline by an estimated 10 million people (70%). AvalereHealth found 7.5 million Americans could face a 255% rise in premiums if the Supreme Court strikes down the subsidies, according to a Feb. 26 analysis.
If the Supreme Court sides with King, a congressional fix would be imperative, ACP’s Mr. Doherty said. Another option would be for states that rely on the federal exchange to form their own exchanges in order to retain the subsidies and keep patients covered. But both options pose cost, procedural, and political challenges, Mr. Doherty said in an interview.
“The problem will be that it is hard to envision a fix that a majority of Republicans could support and that would be acceptable to Democrats and President Obama,” he said. “ ... Politics being politics, we could end up with a ‘blame game’ with both sides trying to blame the other for millions of people losing health insurance coverage.”
On Twitter@legal_med
The showdown over federal subsidies under the Affordable Care Act commences March 4 as Supreme Court justices prepare to hear arguments in King v. Burwell. The outcome could significantly alter the ACA and impact millions of patients and their physicians.
“King v. Burwell is extremely important to patients and physicians alike,” said Danielle C. Gray, a New York attorney and coauthor of a brief on behalf of the American Academy of Pediatrics (AAP), the American Academy of Family Physicians (AAFP), and other groups in support of the government. “All told, studies predict that a ruling in petitioners’ favor would leave 8 million Americans uninsured and cause premiums to rise by almost 50% for those who continue to purchase insurance on federally facilitated exchanges. Physicians would likely see a significant drop in the number of insured patients, which would affect their treatment options and protocol.”
King supporters argue that the basis of the case is being lost in impact studies and outcome projections. The case is about the meaning of ACA language concerning subsidies and whether the executive branch has the authority to change laws as it sees fit, said Ilya Shapiro a senior fellow in constitutional studies at the Cato Institute, a libertarian public policy organization. The group issued a brief to the high court in support of King.
“A lot of arguments in the litigation and the media concern these sort of nightmare scenarios about people losing coverage. … You see some of that in the amicus briefs supporting the government,” Mr. Shapiro said in an interview. “A lot of them are … just kind of painting nightmare policy scenarios, which really should play no role in how you interpret the law.”
King v. Burwell centers on whether residents in states that rely on the federal marketplace are eligible for tax credits to purchase insurance or whether such assistance can go only to residents who purchase insurance via a state-run marketplace. The ACA states that tax credits apply to insurance purchased through an exchange “established by the state.” Challengers argue the law does not mention the federal exchange and that the subsidies are available only for purchases through state exchanges. The government interprets the ACA to allow subsidies whenever patients buys insurance on any exchange.
The future of the ACA depends on the Supreme Court’s interpretation of the language, said Eric J. Segall, professor of law at Georgia State University, Atlanta. Mr. Segall has written on the merits of King v. Burwell, including a recent opinion in the University of Pennsylvania Law Review.
The basis of the ACA comprises three key components: that insurers provide health insurance without denying coverage to patients with preexisting conditions; that the individual mandate that requires all Americans buy insurance; and that the availability of tax subsidies that ensures lower- and middle-income residents can afford to comply with the mandate.
“That third leg, the subsidies, is just as important as the first two legs,” he said in an interview. “If you cut off any of the three legs, the entire purpose of the Affordable Care Act is undercut and the law would be in serious danger.”
Mr. Segall said that he believes the plaintiffs cannot legally demonstrate that the ACA as a whole, clearly and unambiguously precludes tax credits to people who buy health insurance from federal exchanges. If a law is ambiguous or unclear, an agency’s decision must be upheld if it is reasonable, he notes. Given the structure of the ACA and its reliance on the three essential components, it is a reasonable interpretation that the statute allows for subsidies on both state and federal exchanges, Mr. Segall said.
However, King supporters argue the case should turn on the constitutional principle that neither a federal court nor an executive agency can ignore or override a law’s plain meaning.
“The U.S. Supreme Court believes in clear language, and the language in the law clearly states that the subsidies were available only to an exchange established by the state,” said Sally C. Pipes, president and CEO of the Pacific Research Institute, a San Francisco-based think tank and public policy research institute. The Institute issued a brief in support of King. “By giving subsidies [to] the 37 states that have federal exchanges or exchanges that are jointly operated, it goes against the written intent of the law.”
More than 50 friend of the court briefs have been sent to the high court in support or opposition of King, including comments from the American College of Physicians, the American Thoracic Society and the American Hospital Association. The ACP and its allies urged the court to uphold the premium subsidies created by the ACA in all states.
A Supreme Court ruling to overturn the subsidies would not only disrupt care for millions of patients, but also harm the physician-patient relationship and fuel uncompensated care, said Robert B. Doherty, ACP’s senior vice president for governmental affairs and public policy.
“On a practical level, it would introduce chaos in the patient-physician relationship, especially if an adverse ruling by the Supreme Court took effect immediately, as people – including people, such as cancer patients, who are currently undergoing treatment – immediately lost their coverage, and their physicians and hospitals then have to figure out how to continue to get them the care they need without insurance,” Mr. Doherty said in an interview.
Estimates vary on how many Americans could lose subsidies in 2016 if the high court strikes down the financial assistance. An Urban Institute analysis estimated that just over 6 million people would lose coverage; one from RAND finds that individual-market enrollment would decline by an estimated 10 million people (70%). AvalereHealth found 7.5 million Americans could face a 255% rise in premiums if the Supreme Court strikes down the subsidies, according to a Feb. 26 analysis.
If the Supreme Court sides with King, a congressional fix would be imperative, ACP’s Mr. Doherty said. Another option would be for states that rely on the federal exchange to form their own exchanges in order to retain the subsidies and keep patients covered. But both options pose cost, procedural, and political challenges, Mr. Doherty said in an interview.
“The problem will be that it is hard to envision a fix that a majority of Republicans could support and that would be acceptable to Democrats and President Obama,” he said. “ ... Politics being politics, we could end up with a ‘blame game’ with both sides trying to blame the other for millions of people losing health insurance coverage.”
On Twitter@legal_med
The showdown over federal subsidies under the Affordable Care Act commences March 4 as Supreme Court justices prepare to hear arguments in King v. Burwell. The outcome could significantly alter the ACA and impact millions of patients and their physicians.
“King v. Burwell is extremely important to patients and physicians alike,” said Danielle C. Gray, a New York attorney and coauthor of a brief on behalf of the American Academy of Pediatrics (AAP), the American Academy of Family Physicians (AAFP), and other groups in support of the government. “All told, studies predict that a ruling in petitioners’ favor would leave 8 million Americans uninsured and cause premiums to rise by almost 50% for those who continue to purchase insurance on federally facilitated exchanges. Physicians would likely see a significant drop in the number of insured patients, which would affect their treatment options and protocol.”
King supporters argue that the basis of the case is being lost in impact studies and outcome projections. The case is about the meaning of ACA language concerning subsidies and whether the executive branch has the authority to change laws as it sees fit, said Ilya Shapiro a senior fellow in constitutional studies at the Cato Institute, a libertarian public policy organization. The group issued a brief to the high court in support of King.
“A lot of arguments in the litigation and the media concern these sort of nightmare scenarios about people losing coverage. … You see some of that in the amicus briefs supporting the government,” Mr. Shapiro said in an interview. “A lot of them are … just kind of painting nightmare policy scenarios, which really should play no role in how you interpret the law.”
King v. Burwell centers on whether residents in states that rely on the federal marketplace are eligible for tax credits to purchase insurance or whether such assistance can go only to residents who purchase insurance via a state-run marketplace. The ACA states that tax credits apply to insurance purchased through an exchange “established by the state.” Challengers argue the law does not mention the federal exchange and that the subsidies are available only for purchases through state exchanges. The government interprets the ACA to allow subsidies whenever patients buys insurance on any exchange.
The future of the ACA depends on the Supreme Court’s interpretation of the language, said Eric J. Segall, professor of law at Georgia State University, Atlanta. Mr. Segall has written on the merits of King v. Burwell, including a recent opinion in the University of Pennsylvania Law Review.
The basis of the ACA comprises three key components: that insurers provide health insurance without denying coverage to patients with preexisting conditions; that the individual mandate that requires all Americans buy insurance; and that the availability of tax subsidies that ensures lower- and middle-income residents can afford to comply with the mandate.
“That third leg, the subsidies, is just as important as the first two legs,” he said in an interview. “If you cut off any of the three legs, the entire purpose of the Affordable Care Act is undercut and the law would be in serious danger.”
Mr. Segall said that he believes the plaintiffs cannot legally demonstrate that the ACA as a whole, clearly and unambiguously precludes tax credits to people who buy health insurance from federal exchanges. If a law is ambiguous or unclear, an agency’s decision must be upheld if it is reasonable, he notes. Given the structure of the ACA and its reliance on the three essential components, it is a reasonable interpretation that the statute allows for subsidies on both state and federal exchanges, Mr. Segall said.
However, King supporters argue the case should turn on the constitutional principle that neither a federal court nor an executive agency can ignore or override a law’s plain meaning.
“The U.S. Supreme Court believes in clear language, and the language in the law clearly states that the subsidies were available only to an exchange established by the state,” said Sally C. Pipes, president and CEO of the Pacific Research Institute, a San Francisco-based think tank and public policy research institute. The Institute issued a brief in support of King. “By giving subsidies [to] the 37 states that have federal exchanges or exchanges that are jointly operated, it goes against the written intent of the law.”
More than 50 friend of the court briefs have been sent to the high court in support or opposition of King, including comments from the American College of Physicians, the American Thoracic Society and the American Hospital Association. The ACP and its allies urged the court to uphold the premium subsidies created by the ACA in all states.
A Supreme Court ruling to overturn the subsidies would not only disrupt care for millions of patients, but also harm the physician-patient relationship and fuel uncompensated care, said Robert B. Doherty, ACP’s senior vice president for governmental affairs and public policy.
“On a practical level, it would introduce chaos in the patient-physician relationship, especially if an adverse ruling by the Supreme Court took effect immediately, as people – including people, such as cancer patients, who are currently undergoing treatment – immediately lost their coverage, and their physicians and hospitals then have to figure out how to continue to get them the care they need without insurance,” Mr. Doherty said in an interview.
Estimates vary on how many Americans could lose subsidies in 2016 if the high court strikes down the financial assistance. An Urban Institute analysis estimated that just over 6 million people would lose coverage; one from RAND finds that individual-market enrollment would decline by an estimated 10 million people (70%). AvalereHealth found 7.5 million Americans could face a 255% rise in premiums if the Supreme Court strikes down the subsidies, according to a Feb. 26 analysis.
If the Supreme Court sides with King, a congressional fix would be imperative, ACP’s Mr. Doherty said. Another option would be for states that rely on the federal exchange to form their own exchanges in order to retain the subsidies and keep patients covered. But both options pose cost, procedural, and political challenges, Mr. Doherty said in an interview.
“The problem will be that it is hard to envision a fix that a majority of Republicans could support and that would be acceptable to Democrats and President Obama,” he said. “ ... Politics being politics, we could end up with a ‘blame game’ with both sides trying to blame the other for millions of people losing health insurance coverage.”
On Twitter@legal_med
Nonclinical interventions enhance care and outcomes for vascular patients
SCOTTSDALE, ARIZ. – The application of simple low-cost interventions and hands-on care, as well as enlisting the patient to participate in care for him or herself, can help vascular specialists achieve favorable outcomes when managing patients in an era of increased regulation.
That was the message of an expert panel assembled to deliver “clinically pertinent information in the midst of a regulatory system that is driving us down a [certain] pathway whether or not we want to go,” panelist Dr. Bruce H. Gray, a vascular surgeon at Greenville (S.C.) Health System, told the audience at this year’s annual meeting of the Southern Association for Vascular Surgery.
Under the Affordable Care Act, there has been “a shift from structure and process to now just outcomes,” according to panelist Dr. John W. Hallett Jr., a clinical professor of surgery at the Medical University of South Carolina and chief medical officer at the Roper St. Francis Vascular Care Center, both in Charleston.
Incentives now penalties
The Patient Quality Reporting System (formerly called the Physicians Quality Reporting Initiative) was the first national program designed by the Centers for Medicare & Medicaid Services to link the reporting of quality data to physician payment. There are six quality strategy domains in the PQRS: effective clinical care; patient safety; communication and care coordination; person- and caregiver-centered experience and outcomes; efficiency and cost reduction; and community and population health. Physicians must satisfy at least three of the six or risk penalties.
Initially intended as an incentive program when it was launched as part of the Tax Relief and Health Care Act of 2006, physicians who voluntarily reported their quality data were awarded a 2% bonus on their yearly CMS payment. Although still referred to by CMS as an incentive program, beginning this year, physician-reported quality data considered by the PQRS criteria as negative will be used to assess a penalty up to 1.5% against their expected CMS payment for that year. In 2016, the penalty is set to increase to 2% of the physician’s CMS payment. “They call the reporting voluntary but now there’s a penalty if you don’t report it,” said panelist Dr. Adam W. Beck, a vascular surgeon at the University of Florida.
Searching for evidence
However, much of the criteria used by the PRQS to evaluate a vascular surgeon’s performance, and thus what he or she will be paid, is not evidence based, according to Dr. Beck. For example, one CMS vascular surgery quality measure in place considers that open repair of a 6 cm or less nonruptured abdominal aortic aneurysm without major complications should result in the patient being discharged postoperatively on day 7.
“The idea is that this is a purely elective operation so in theory, that patient should not die, and should not have major complications, and so can go home on day 7,” Dr. Beck said. “But we don’t really know if that’s true. Some of us are working on figuring out if any of these [measures] are useful or not.”
Similarly, Dr. Gray said that, since its publication in 2005, the BASIL (Bypass vs. Angioplasty in Severe Ischemia of the Leg) trial, which supported surgery over balloon angioplasty for improved long-term outcomes in patients with peripheral artery disease, has been the de facto benchmark for predicting death in this patient cohort, a necessary consideration when choosing a treatment algorithm.
This, despite what he suggested were generalizations gleaned from the data that are not always appropriate, particularly when considering claudication. “Only 11% of those critical limb ischemia patients who were eligible for the trial were randomized to any of the study’s six sites. This trial cannot be extrapolated to our entire heterogeneous CLI population,” Dr. Gray said.
This was true, too, he said, not only because a minority of the patients had angioplasty at multiple levels, but because the patient assessment and mortality rate criteria in the study may not actually coincide with how other specialists assess their patients and predict mortality, as evidenced by a number of studies that have been published since BASIL, all of which relied on different criteria for determining two-year mortality rates.
“The BASIL trial recommendation that we should know the life expectancy of our patients has popped up in the literature more and more, and I have thought long and hard about how that impacts my clinical practice decision tree,” Dr. Gray said, concluding that ultimately, predicting mortality is beside the point. “Mortality is inevitable and sooner in CLI patients. The best care has less to do with predicting mortality, but requires ... the integrity to choose the right procedure for the right patient at the right time.”
Assessing how much muscle and functional mobility a patient has in order to help determine which treatment is best, and not overrelying on electronic health records can also impact outcomes. “You don’t need too many fancy tests to tell what a patient’s functional level is,” he said, adding “there is no substitute for putting your own eyes on the patient.”
Patient participation
Despite the pressure on physicians to perform well on the PQRS, there are many factors beyond their control, such as a patient’s choice to smoke. That’s why using “teachable moments” that remind patients of their own power to improve their chances for recovery is more important than ever, as is clear communication with the patient about what they can expect both pre- and post-surgery, according to Dr. Hallett. “The challenge of taking care of these patients is much more than our technical skill.”
Combining a medical tobacco-cessation program with teletherapeutic programs such as the federally funded 1-800-QUIT-NOW line can be of support to patients, as are phone-based counseling sessions to remind patients to fill their prescriptions and to take them once they do, said Dr. Hallett.
Motivating patients to participate in their recovery should not be left to others, however. Dr. Hallett said has found that leaning on his authority as the surgeon is more effective than leaving the role of adviser to “physician extenders.”
“I can do a teachable moment in less than 5 minutes,” he said in an interview. “For me to say to the patient, ‘Smoking is one of the reasons you have this bad leg. I would really like to help you with stopping. Are you interested?’ Coming from me, it’s much more powerful than from anyone else [on my staff].”
In addition, adhering to low- or no-cost postoperative protocols such as keeping patients warm, and administering both aspirin and a statin at discharge can help improve patient outcomes by as much as 20%, according to Dr. Hallett.
Above all else, Dr. Hallett urged vascular surgeons to focus on the long-term care of patients, or risk not only poor outcomes and lower reimbursements, but also loss of control over the patient’s care.
“If we don’t take care of them, they lose the integrated care they need,” Dr. Hallett said in an interview. “The primary care doctors are too frappin’ busy. I see 15-18 patients a day; they’ll see twice that.”
To that end, he recommended giving patients a thorough cardiovascular exam that includes a complete lipid profile and a review of their medications, particularly since the patient’s primary care doctors aren’t always as attentive to vascular concerns. “You are the long-term cardiovascular doc for these patients. You give the advice, you check their drugs, and you, the surgeon, needs to set their expectations, not someone else,” Dr. Hallett concluded.
On Twitter @whitneymcknight
SCOTTSDALE, ARIZ. – The application of simple low-cost interventions and hands-on care, as well as enlisting the patient to participate in care for him or herself, can help vascular specialists achieve favorable outcomes when managing patients in an era of increased regulation.
That was the message of an expert panel assembled to deliver “clinically pertinent information in the midst of a regulatory system that is driving us down a [certain] pathway whether or not we want to go,” panelist Dr. Bruce H. Gray, a vascular surgeon at Greenville (S.C.) Health System, told the audience at this year’s annual meeting of the Southern Association for Vascular Surgery.
Under the Affordable Care Act, there has been “a shift from structure and process to now just outcomes,” according to panelist Dr. John W. Hallett Jr., a clinical professor of surgery at the Medical University of South Carolina and chief medical officer at the Roper St. Francis Vascular Care Center, both in Charleston.
Incentives now penalties
The Patient Quality Reporting System (formerly called the Physicians Quality Reporting Initiative) was the first national program designed by the Centers for Medicare & Medicaid Services to link the reporting of quality data to physician payment. There are six quality strategy domains in the PQRS: effective clinical care; patient safety; communication and care coordination; person- and caregiver-centered experience and outcomes; efficiency and cost reduction; and community and population health. Physicians must satisfy at least three of the six or risk penalties.
Initially intended as an incentive program when it was launched as part of the Tax Relief and Health Care Act of 2006, physicians who voluntarily reported their quality data were awarded a 2% bonus on their yearly CMS payment. Although still referred to by CMS as an incentive program, beginning this year, physician-reported quality data considered by the PQRS criteria as negative will be used to assess a penalty up to 1.5% against their expected CMS payment for that year. In 2016, the penalty is set to increase to 2% of the physician’s CMS payment. “They call the reporting voluntary but now there’s a penalty if you don’t report it,” said panelist Dr. Adam W. Beck, a vascular surgeon at the University of Florida.
Searching for evidence
However, much of the criteria used by the PRQS to evaluate a vascular surgeon’s performance, and thus what he or she will be paid, is not evidence based, according to Dr. Beck. For example, one CMS vascular surgery quality measure in place considers that open repair of a 6 cm or less nonruptured abdominal aortic aneurysm without major complications should result in the patient being discharged postoperatively on day 7.
“The idea is that this is a purely elective operation so in theory, that patient should not die, and should not have major complications, and so can go home on day 7,” Dr. Beck said. “But we don’t really know if that’s true. Some of us are working on figuring out if any of these [measures] are useful or not.”
Similarly, Dr. Gray said that, since its publication in 2005, the BASIL (Bypass vs. Angioplasty in Severe Ischemia of the Leg) trial, which supported surgery over balloon angioplasty for improved long-term outcomes in patients with peripheral artery disease, has been the de facto benchmark for predicting death in this patient cohort, a necessary consideration when choosing a treatment algorithm.
This, despite what he suggested were generalizations gleaned from the data that are not always appropriate, particularly when considering claudication. “Only 11% of those critical limb ischemia patients who were eligible for the trial were randomized to any of the study’s six sites. This trial cannot be extrapolated to our entire heterogeneous CLI population,” Dr. Gray said.
This was true, too, he said, not only because a minority of the patients had angioplasty at multiple levels, but because the patient assessment and mortality rate criteria in the study may not actually coincide with how other specialists assess their patients and predict mortality, as evidenced by a number of studies that have been published since BASIL, all of which relied on different criteria for determining two-year mortality rates.
“The BASIL trial recommendation that we should know the life expectancy of our patients has popped up in the literature more and more, and I have thought long and hard about how that impacts my clinical practice decision tree,” Dr. Gray said, concluding that ultimately, predicting mortality is beside the point. “Mortality is inevitable and sooner in CLI patients. The best care has less to do with predicting mortality, but requires ... the integrity to choose the right procedure for the right patient at the right time.”
Assessing how much muscle and functional mobility a patient has in order to help determine which treatment is best, and not overrelying on electronic health records can also impact outcomes. “You don’t need too many fancy tests to tell what a patient’s functional level is,” he said, adding “there is no substitute for putting your own eyes on the patient.”
Patient participation
Despite the pressure on physicians to perform well on the PQRS, there are many factors beyond their control, such as a patient’s choice to smoke. That’s why using “teachable moments” that remind patients of their own power to improve their chances for recovery is more important than ever, as is clear communication with the patient about what they can expect both pre- and post-surgery, according to Dr. Hallett. “The challenge of taking care of these patients is much more than our technical skill.”
Combining a medical tobacco-cessation program with teletherapeutic programs such as the federally funded 1-800-QUIT-NOW line can be of support to patients, as are phone-based counseling sessions to remind patients to fill their prescriptions and to take them once they do, said Dr. Hallett.
Motivating patients to participate in their recovery should not be left to others, however. Dr. Hallett said has found that leaning on his authority as the surgeon is more effective than leaving the role of adviser to “physician extenders.”
“I can do a teachable moment in less than 5 minutes,” he said in an interview. “For me to say to the patient, ‘Smoking is one of the reasons you have this bad leg. I would really like to help you with stopping. Are you interested?’ Coming from me, it’s much more powerful than from anyone else [on my staff].”
In addition, adhering to low- or no-cost postoperative protocols such as keeping patients warm, and administering both aspirin and a statin at discharge can help improve patient outcomes by as much as 20%, according to Dr. Hallett.
Above all else, Dr. Hallett urged vascular surgeons to focus on the long-term care of patients, or risk not only poor outcomes and lower reimbursements, but also loss of control over the patient’s care.
“If we don’t take care of them, they lose the integrated care they need,” Dr. Hallett said in an interview. “The primary care doctors are too frappin’ busy. I see 15-18 patients a day; they’ll see twice that.”
To that end, he recommended giving patients a thorough cardiovascular exam that includes a complete lipid profile and a review of their medications, particularly since the patient’s primary care doctors aren’t always as attentive to vascular concerns. “You are the long-term cardiovascular doc for these patients. You give the advice, you check their drugs, and you, the surgeon, needs to set their expectations, not someone else,” Dr. Hallett concluded.
On Twitter @whitneymcknight
SCOTTSDALE, ARIZ. – The application of simple low-cost interventions and hands-on care, as well as enlisting the patient to participate in care for him or herself, can help vascular specialists achieve favorable outcomes when managing patients in an era of increased regulation.
That was the message of an expert panel assembled to deliver “clinically pertinent information in the midst of a regulatory system that is driving us down a [certain] pathway whether or not we want to go,” panelist Dr. Bruce H. Gray, a vascular surgeon at Greenville (S.C.) Health System, told the audience at this year’s annual meeting of the Southern Association for Vascular Surgery.
Under the Affordable Care Act, there has been “a shift from structure and process to now just outcomes,” according to panelist Dr. John W. Hallett Jr., a clinical professor of surgery at the Medical University of South Carolina and chief medical officer at the Roper St. Francis Vascular Care Center, both in Charleston.
Incentives now penalties
The Patient Quality Reporting System (formerly called the Physicians Quality Reporting Initiative) was the first national program designed by the Centers for Medicare & Medicaid Services to link the reporting of quality data to physician payment. There are six quality strategy domains in the PQRS: effective clinical care; patient safety; communication and care coordination; person- and caregiver-centered experience and outcomes; efficiency and cost reduction; and community and population health. Physicians must satisfy at least three of the six or risk penalties.
Initially intended as an incentive program when it was launched as part of the Tax Relief and Health Care Act of 2006, physicians who voluntarily reported their quality data were awarded a 2% bonus on their yearly CMS payment. Although still referred to by CMS as an incentive program, beginning this year, physician-reported quality data considered by the PQRS criteria as negative will be used to assess a penalty up to 1.5% against their expected CMS payment for that year. In 2016, the penalty is set to increase to 2% of the physician’s CMS payment. “They call the reporting voluntary but now there’s a penalty if you don’t report it,” said panelist Dr. Adam W. Beck, a vascular surgeon at the University of Florida.
Searching for evidence
However, much of the criteria used by the PRQS to evaluate a vascular surgeon’s performance, and thus what he or she will be paid, is not evidence based, according to Dr. Beck. For example, one CMS vascular surgery quality measure in place considers that open repair of a 6 cm or less nonruptured abdominal aortic aneurysm without major complications should result in the patient being discharged postoperatively on day 7.
“The idea is that this is a purely elective operation so in theory, that patient should not die, and should not have major complications, and so can go home on day 7,” Dr. Beck said. “But we don’t really know if that’s true. Some of us are working on figuring out if any of these [measures] are useful or not.”
Similarly, Dr. Gray said that, since its publication in 2005, the BASIL (Bypass vs. Angioplasty in Severe Ischemia of the Leg) trial, which supported surgery over balloon angioplasty for improved long-term outcomes in patients with peripheral artery disease, has been the de facto benchmark for predicting death in this patient cohort, a necessary consideration when choosing a treatment algorithm.
This, despite what he suggested were generalizations gleaned from the data that are not always appropriate, particularly when considering claudication. “Only 11% of those critical limb ischemia patients who were eligible for the trial were randomized to any of the study’s six sites. This trial cannot be extrapolated to our entire heterogeneous CLI population,” Dr. Gray said.
This was true, too, he said, not only because a minority of the patients had angioplasty at multiple levels, but because the patient assessment and mortality rate criteria in the study may not actually coincide with how other specialists assess their patients and predict mortality, as evidenced by a number of studies that have been published since BASIL, all of which relied on different criteria for determining two-year mortality rates.
“The BASIL trial recommendation that we should know the life expectancy of our patients has popped up in the literature more and more, and I have thought long and hard about how that impacts my clinical practice decision tree,” Dr. Gray said, concluding that ultimately, predicting mortality is beside the point. “Mortality is inevitable and sooner in CLI patients. The best care has less to do with predicting mortality, but requires ... the integrity to choose the right procedure for the right patient at the right time.”
Assessing how much muscle and functional mobility a patient has in order to help determine which treatment is best, and not overrelying on electronic health records can also impact outcomes. “You don’t need too many fancy tests to tell what a patient’s functional level is,” he said, adding “there is no substitute for putting your own eyes on the patient.”
Patient participation
Despite the pressure on physicians to perform well on the PQRS, there are many factors beyond their control, such as a patient’s choice to smoke. That’s why using “teachable moments” that remind patients of their own power to improve their chances for recovery is more important than ever, as is clear communication with the patient about what they can expect both pre- and post-surgery, according to Dr. Hallett. “The challenge of taking care of these patients is much more than our technical skill.”
Combining a medical tobacco-cessation program with teletherapeutic programs such as the federally funded 1-800-QUIT-NOW line can be of support to patients, as are phone-based counseling sessions to remind patients to fill their prescriptions and to take them once they do, said Dr. Hallett.
Motivating patients to participate in their recovery should not be left to others, however. Dr. Hallett said has found that leaning on his authority as the surgeon is more effective than leaving the role of adviser to “physician extenders.”
“I can do a teachable moment in less than 5 minutes,” he said in an interview. “For me to say to the patient, ‘Smoking is one of the reasons you have this bad leg. I would really like to help you with stopping. Are you interested?’ Coming from me, it’s much more powerful than from anyone else [on my staff].”
In addition, adhering to low- or no-cost postoperative protocols such as keeping patients warm, and administering both aspirin and a statin at discharge can help improve patient outcomes by as much as 20%, according to Dr. Hallett.
Above all else, Dr. Hallett urged vascular surgeons to focus on the long-term care of patients, or risk not only poor outcomes and lower reimbursements, but also loss of control over the patient’s care.
“If we don’t take care of them, they lose the integrated care they need,” Dr. Hallett said in an interview. “The primary care doctors are too frappin’ busy. I see 15-18 patients a day; they’ll see twice that.”
To that end, he recommended giving patients a thorough cardiovascular exam that includes a complete lipid profile and a review of their medications, particularly since the patient’s primary care doctors aren’t always as attentive to vascular concerns. “You are the long-term cardiovascular doc for these patients. You give the advice, you check their drugs, and you, the surgeon, needs to set their expectations, not someone else,” Dr. Hallett concluded.
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM THE SAVS 2015 ANNUAL MEETING