User login
Official Newspaper of the American College of Surgeons
Esophagogastric cancer patients on chemotherapy more likely to develop VTE
Incidence rates for developing venous thromboembolism (VTE) among esophagogastric cancer patients undergoing neoadjuvant chemotherapy in combination with curative intended surgery were significantly higher among patients with initial stage III and IV cancers and gastric cancer, according to a new study published in Thrombosis Research.
In the clinical prospective study, 129 patients with lower esophageal, gastroesophageal, and gastric cancer were examined between 2008 and 2011. Baseline assessments were recorded via bilateral compression ultrasound (biCUS) for deep vein thrombosis and computer tomography pulmonary angiography for pulmonary embolism. The patients received a chemotherapy regimen of oxaliplatin, capecitabine, and epirubicin, with curative intended surgery, and were examined before undergoing preoperative chemotherapy, surgery, and postoperative chemotherapy. The researchers encountered 21 VTE cases, or 16% of the total number of patients examined, with VTE incidences twice as likely to be asymptomatic than symptomatic.
The authors noted that state-of-the-art technology helped boost VTE detection rates among asymptomatic patients, and older studies may have underreported incidences of the disease.
“Although our study only included 129 patients, the systematic use of biCUS strongly suggests that the frequency of VTE is much greater than that previously reported for these types of cancer,” wrote Dr. Anders Christian Larsen and his associates at Aalborg University Hospital, Denmark.
Read more here (Thrombosis Research 2015 [doi:10.1016/j.thromres.2015.01.021]).
Incidence rates for developing venous thromboembolism (VTE) among esophagogastric cancer patients undergoing neoadjuvant chemotherapy in combination with curative intended surgery were significantly higher among patients with initial stage III and IV cancers and gastric cancer, according to a new study published in Thrombosis Research.
In the clinical prospective study, 129 patients with lower esophageal, gastroesophageal, and gastric cancer were examined between 2008 and 2011. Baseline assessments were recorded via bilateral compression ultrasound (biCUS) for deep vein thrombosis and computer tomography pulmonary angiography for pulmonary embolism. The patients received a chemotherapy regimen of oxaliplatin, capecitabine, and epirubicin, with curative intended surgery, and were examined before undergoing preoperative chemotherapy, surgery, and postoperative chemotherapy. The researchers encountered 21 VTE cases, or 16% of the total number of patients examined, with VTE incidences twice as likely to be asymptomatic than symptomatic.
The authors noted that state-of-the-art technology helped boost VTE detection rates among asymptomatic patients, and older studies may have underreported incidences of the disease.
“Although our study only included 129 patients, the systematic use of biCUS strongly suggests that the frequency of VTE is much greater than that previously reported for these types of cancer,” wrote Dr. Anders Christian Larsen and his associates at Aalborg University Hospital, Denmark.
Read more here (Thrombosis Research 2015 [doi:10.1016/j.thromres.2015.01.021]).
Incidence rates for developing venous thromboembolism (VTE) among esophagogastric cancer patients undergoing neoadjuvant chemotherapy in combination with curative intended surgery were significantly higher among patients with initial stage III and IV cancers and gastric cancer, according to a new study published in Thrombosis Research.
In the clinical prospective study, 129 patients with lower esophageal, gastroesophageal, and gastric cancer were examined between 2008 and 2011. Baseline assessments were recorded via bilateral compression ultrasound (biCUS) for deep vein thrombosis and computer tomography pulmonary angiography for pulmonary embolism. The patients received a chemotherapy regimen of oxaliplatin, capecitabine, and epirubicin, with curative intended surgery, and were examined before undergoing preoperative chemotherapy, surgery, and postoperative chemotherapy. The researchers encountered 21 VTE cases, or 16% of the total number of patients examined, with VTE incidences twice as likely to be asymptomatic than symptomatic.
The authors noted that state-of-the-art technology helped boost VTE detection rates among asymptomatic patients, and older studies may have underreported incidences of the disease.
“Although our study only included 129 patients, the systematic use of biCUS strongly suggests that the frequency of VTE is much greater than that previously reported for these types of cancer,” wrote Dr. Anders Christian Larsen and his associates at Aalborg University Hospital, Denmark.
Read more here (Thrombosis Research 2015 [doi:10.1016/j.thromres.2015.01.021]).
Rivaroxaban and enoxaparin had comparable rates for VTE prophylaxis after hip and knee surgery
There were no significant differences between the anticoagulants rivaroxaban (Xarelto) and enoxaparin (Lovenox) in terms of venous thromboembolism prophylaxis, infection, reoperation, transfusion, or major bleeding complications after primary hip and knee arthroplasty, according to a study published in the Journal of Arthroplasty.
In a non–industry-funded retrospective cohort study, Dr. Michael A. Charters of Henry Ford Health System in Detroit and his associates looked at 2,406 patients who underwent total hip and knee arthroplasty between 2009 and 2011. Of the 1,762 patients ultimately included in the study, 1,113 (63.2%) received enoxaparin and 649 (36.8%) received rivaroxaban for VTE prophylaxis. The deep venous thrombosis rate of the enoxaparin group was 1.8%, compared with 0.9% in the rivaroxaban group (P = .208) and the pulmonary embolism rate of the enoxaparin group was 0.7%, compared with 0.3% in the rivaroxaban group (P = .437).
“For standard primary THA [total hip arthroplasty] and TKA [total knee arthroplasty], these medications appear to be equally effective without increased adverse events,” the researchers said.
Read the full article at: The Journal of Arthoplasty 2015 (www.arthroplastyjournal.org/article/S0883-5403%2815%2900120-5/abstract).
There were no significant differences between the anticoagulants rivaroxaban (Xarelto) and enoxaparin (Lovenox) in terms of venous thromboembolism prophylaxis, infection, reoperation, transfusion, or major bleeding complications after primary hip and knee arthroplasty, according to a study published in the Journal of Arthroplasty.
In a non–industry-funded retrospective cohort study, Dr. Michael A. Charters of Henry Ford Health System in Detroit and his associates looked at 2,406 patients who underwent total hip and knee arthroplasty between 2009 and 2011. Of the 1,762 patients ultimately included in the study, 1,113 (63.2%) received enoxaparin and 649 (36.8%) received rivaroxaban for VTE prophylaxis. The deep venous thrombosis rate of the enoxaparin group was 1.8%, compared with 0.9% in the rivaroxaban group (P = .208) and the pulmonary embolism rate of the enoxaparin group was 0.7%, compared with 0.3% in the rivaroxaban group (P = .437).
“For standard primary THA [total hip arthroplasty] and TKA [total knee arthroplasty], these medications appear to be equally effective without increased adverse events,” the researchers said.
Read the full article at: The Journal of Arthoplasty 2015 (www.arthroplastyjournal.org/article/S0883-5403%2815%2900120-5/abstract).
There were no significant differences between the anticoagulants rivaroxaban (Xarelto) and enoxaparin (Lovenox) in terms of venous thromboembolism prophylaxis, infection, reoperation, transfusion, or major bleeding complications after primary hip and knee arthroplasty, according to a study published in the Journal of Arthroplasty.
In a non–industry-funded retrospective cohort study, Dr. Michael A. Charters of Henry Ford Health System in Detroit and his associates looked at 2,406 patients who underwent total hip and knee arthroplasty between 2009 and 2011. Of the 1,762 patients ultimately included in the study, 1,113 (63.2%) received enoxaparin and 649 (36.8%) received rivaroxaban for VTE prophylaxis. The deep venous thrombosis rate of the enoxaparin group was 1.8%, compared with 0.9% in the rivaroxaban group (P = .208) and the pulmonary embolism rate of the enoxaparin group was 0.7%, compared with 0.3% in the rivaroxaban group (P = .437).
“For standard primary THA [total hip arthroplasty] and TKA [total knee arthroplasty], these medications appear to be equally effective without increased adverse events,” the researchers said.
Read the full article at: The Journal of Arthoplasty 2015 (www.arthroplastyjournal.org/article/S0883-5403%2815%2900120-5/abstract).
Increase enoxaparin doses to prevent VTEs in trauma patients
PHOENIX – Trauma patients probably need an elevated dose of enoxaparin – perhaps 40 mg twice daily – to prevent venous thromboembolisms, according to a prospective study of 85 trauma patients at the Palmetto Health Richland hospital in Columbia, S.C.
Also, antifactor 10a – a blood test often used in research to gauge how well enoxaparin (Lovenox) is thinning the blood – doesn’t work very well as an empiric measure of anticoagulation; thromboelastography (TEG) may be better, lead investigator Janise Phillips, Pharm.D., said at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.
Her team tracked trauma patients who had at least three consecutive doses of enoxaparin prophylaxis for venous thromboembolism (VTE) and at least one peak antifactor 10a level drawn; enoxaparin doses were adjusted as needed to hit a weekly antifactor 10a level of 0.20-0.40 IU/mL, which is thought to be the therapeutic range for enoxaparin. Patients were in the ICU for a median of about 10 days, and in the hospital for about 2-3 weeks.
The types of trauma were not reported in the study, but the investigation confirms prior findings that critically ill trauma patients – and perhaps burn patients – need higher anticoagulant doses.
Overall, 65% (13) of patients on an initial enoxaparin regimen of 30 mg subcutaneously twice daily were below anti-factor 10a levels of 0.20-0.40 IU/mL after their first dose; 22% (8) were subtherapeutic after an initial dose of 40 mg once daily; and 21% (6) were subtherapeutic after an initial dose of 40 mg twice daily.
Antifactor 10a levels didn’t match well with clinical benefit. VTEs were diagnosed in 15% (4) of patients with an initial subtherapeutic antifactor 10a level, but 15% (4) bled on their subtherapeutic dose; 8.5% (4) of patients with an initial therapeutic level had a VTE, vs. none who were supratherapeutic after their initial dose. However, 9% (1) of supratherapeutic patients had an enoxaparin bleed.
“These were trauma patients in and out of surgery. A lot of the time, we had to stop the dose and hold it, which may” explain why subtherapeutic patients had the highest VTE risk, said Dr. Phillips, now a critical care pharmacist at the Cleveland Clinic hospital in Abu Dhabi, United Arab Emirates.
More than half of the patients were men, and being male was the only factor that seemed to increase the risk of subtherapeutic enoxaparin levels (P = .04). There was a trend for subtherapeutic levels in heavier patients – which might help explain the higher risk in men – and those with diminished kidney function. Even so, the fact that both VTEs and bleeding were most likely in underdosed patients could mean that antifactor 10a “is really not the best marker for VTE risk. At $80 a pop, it isn’t cost-effective, and [even] patients with therapeutic levels ended up with clots. TEG gives you a real time view of the coagulation status of the patient,” and may be the way to go, Dr. Phillips said.
PHOENIX – Trauma patients probably need an elevated dose of enoxaparin – perhaps 40 mg twice daily – to prevent venous thromboembolisms, according to a prospective study of 85 trauma patients at the Palmetto Health Richland hospital in Columbia, S.C.
Also, antifactor 10a – a blood test often used in research to gauge how well enoxaparin (Lovenox) is thinning the blood – doesn’t work very well as an empiric measure of anticoagulation; thromboelastography (TEG) may be better, lead investigator Janise Phillips, Pharm.D., said at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.
Her team tracked trauma patients who had at least three consecutive doses of enoxaparin prophylaxis for venous thromboembolism (VTE) and at least one peak antifactor 10a level drawn; enoxaparin doses were adjusted as needed to hit a weekly antifactor 10a level of 0.20-0.40 IU/mL, which is thought to be the therapeutic range for enoxaparin. Patients were in the ICU for a median of about 10 days, and in the hospital for about 2-3 weeks.
The types of trauma were not reported in the study, but the investigation confirms prior findings that critically ill trauma patients – and perhaps burn patients – need higher anticoagulant doses.
Overall, 65% (13) of patients on an initial enoxaparin regimen of 30 mg subcutaneously twice daily were below anti-factor 10a levels of 0.20-0.40 IU/mL after their first dose; 22% (8) were subtherapeutic after an initial dose of 40 mg once daily; and 21% (6) were subtherapeutic after an initial dose of 40 mg twice daily.
Antifactor 10a levels didn’t match well with clinical benefit. VTEs were diagnosed in 15% (4) of patients with an initial subtherapeutic antifactor 10a level, but 15% (4) bled on their subtherapeutic dose; 8.5% (4) of patients with an initial therapeutic level had a VTE, vs. none who were supratherapeutic after their initial dose. However, 9% (1) of supratherapeutic patients had an enoxaparin bleed.
“These were trauma patients in and out of surgery. A lot of the time, we had to stop the dose and hold it, which may” explain why subtherapeutic patients had the highest VTE risk, said Dr. Phillips, now a critical care pharmacist at the Cleveland Clinic hospital in Abu Dhabi, United Arab Emirates.
More than half of the patients were men, and being male was the only factor that seemed to increase the risk of subtherapeutic enoxaparin levels (P = .04). There was a trend for subtherapeutic levels in heavier patients – which might help explain the higher risk in men – and those with diminished kidney function. Even so, the fact that both VTEs and bleeding were most likely in underdosed patients could mean that antifactor 10a “is really not the best marker for VTE risk. At $80 a pop, it isn’t cost-effective, and [even] patients with therapeutic levels ended up with clots. TEG gives you a real time view of the coagulation status of the patient,” and may be the way to go, Dr. Phillips said.
PHOENIX – Trauma patients probably need an elevated dose of enoxaparin – perhaps 40 mg twice daily – to prevent venous thromboembolisms, according to a prospective study of 85 trauma patients at the Palmetto Health Richland hospital in Columbia, S.C.
Also, antifactor 10a – a blood test often used in research to gauge how well enoxaparin (Lovenox) is thinning the blood – doesn’t work very well as an empiric measure of anticoagulation; thromboelastography (TEG) may be better, lead investigator Janise Phillips, Pharm.D., said at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.
Her team tracked trauma patients who had at least three consecutive doses of enoxaparin prophylaxis for venous thromboembolism (VTE) and at least one peak antifactor 10a level drawn; enoxaparin doses were adjusted as needed to hit a weekly antifactor 10a level of 0.20-0.40 IU/mL, which is thought to be the therapeutic range for enoxaparin. Patients were in the ICU for a median of about 10 days, and in the hospital for about 2-3 weeks.
The types of trauma were not reported in the study, but the investigation confirms prior findings that critically ill trauma patients – and perhaps burn patients – need higher anticoagulant doses.
Overall, 65% (13) of patients on an initial enoxaparin regimen of 30 mg subcutaneously twice daily were below anti-factor 10a levels of 0.20-0.40 IU/mL after their first dose; 22% (8) were subtherapeutic after an initial dose of 40 mg once daily; and 21% (6) were subtherapeutic after an initial dose of 40 mg twice daily.
Antifactor 10a levels didn’t match well with clinical benefit. VTEs were diagnosed in 15% (4) of patients with an initial subtherapeutic antifactor 10a level, but 15% (4) bled on their subtherapeutic dose; 8.5% (4) of patients with an initial therapeutic level had a VTE, vs. none who were supratherapeutic after their initial dose. However, 9% (1) of supratherapeutic patients had an enoxaparin bleed.
“These were trauma patients in and out of surgery. A lot of the time, we had to stop the dose and hold it, which may” explain why subtherapeutic patients had the highest VTE risk, said Dr. Phillips, now a critical care pharmacist at the Cleveland Clinic hospital in Abu Dhabi, United Arab Emirates.
More than half of the patients were men, and being male was the only factor that seemed to increase the risk of subtherapeutic enoxaparin levels (P = .04). There was a trend for subtherapeutic levels in heavier patients – which might help explain the higher risk in men – and those with diminished kidney function. Even so, the fact that both VTEs and bleeding were most likely in underdosed patients could mean that antifactor 10a “is really not the best marker for VTE risk. At $80 a pop, it isn’t cost-effective, and [even] patients with therapeutic levels ended up with clots. TEG gives you a real time view of the coagulation status of the patient,” and may be the way to go, Dr. Phillips said.
AT THE SCCM CRITICAL CARE CONGRESS
Key clinical point: Enoxaparin at 30 mg twice daily isn’t adequate for preventing VTEs in trauma patients.
Major finding: Overall, 65% of patients on an initial enoxaparin regimen of 30 mg subcutaneously twice daily were below anti-factor 10a levels of 0.20-0.40 IU/mL after their first dose; 22% were subtherapeutic after an initial dose of 40 mg once daily; and 21% were subtherapeutic after an initial dose of 40 mg twice daily.
Data source: Prospective study of 85 trauma patients atthe Palmetto Health Richland hospital in Columbia, S.C.
Disclosures: The lead investigator said she has no disclosures, and no outside funding was reported for the work.
Medicare at 50: Is the end near for SGR?
The Sustainable Growth Rate formula. Few aspects of Medicare have been more problematic for physicians.
Designed to control Medicare costs, Congress has spent more since 2003 to delay SGR cuts than it would cost to fund current repeal legislation.
Passed as part of the Balanced Budget Act of 1997, the SGR was designed to make sure Medicare expenditures did not grow faster than the Gross Domestic Product based on four factors: estimated change in physician fees, estimated number of Medicare fee-for-service beneficiaries, estimated 10-year average change in GDP, and estimated changes in expenditures due to law or regulation.
It was not, however, designed to keep up with the Baby Boom. Because it does not adjust for the influx of boomers, it guarantees to produce pay cuts just as demand for physician services grows.
The next pay cut – 21% this time – is slated for April 1.
For doctors, the constant specter of lower payments simply makes it hard to do business.
“Each year, when there is supposedly a cut, it is a consideration for practices that they have to create some contingency thinking, ‘if this were actually to take place, how will I continue to maintain my practice?’ ” Dr. Robert Juhasz, president of the American Osteopathic Association, said in an interview. “If they have a high Medicare population that they take care of, and certainly if there was that kind of a cut, they could not sustain that and would have to make changes.”
Dr. Blase Polite, chair of the American Society of Clinical Oncology Government Relations Committee, agreed. “Ever since the flawed formula was put in place, it has created yearly uncertainty. In recent years, we have had it to the point where the SGR cuts went into effect and then we had to do things like hold bills for a month or 2 months to resubmit them when the SGR would get patched. It became an absolute nightmare from a small business operating standpoint.”
But the tyranny of the SGR may have outgrown itself. In January, the U.S. Department of Health & Human Services announced a major expansion of its efforts to base physicians’ Medicare pay on value instead of volume, calling for half of all Medicare payments to be out of the fee-for-service system by 2018.
“This is the first time in the history of the program that explicit goals for alternative payment models and value-based payment models have been set for Medicare,” HHS Secretary Sylvia Burwell said in an editorial Jan. 26 in the New England Journal of Medicine (doi:10.1056/NEJMp1500445).
The goal is “to move away from the old way of doing things, which amounted to, ‘the more you do, the more you get paid,’ by linking nearly all pay to quality and value in some way to see that we are spending smarter,” Ms. Burwell said in a blog post on the HHS website.
As part of that effort, the department aims to have 30% of Medicare payments tied to quality or value through alternative payment models by the end of 2016.
Further, real efforts to repeal the SGR took hold in the last Congress, with strong support to pass legislation among lawmakers of both parties in the House and in the Senate. H.R. 4015, SGR Repeal and Medicare Provider Payment Modernization Act of 2014, passed the House but was not taken up by the Senate.
“We were cautiously optimistic that this 17th year of trying to repeal the SGR might have been the successful one,” Dr. Patrick T. O’Gara, president of the American College of Cardiology, said in an interview. He said that the sticking point seemed to be that “there was no politically viable way to pay for it.”
Dr. David A. Fleming, president of the American College of Physicians, noted in a statement that finding the money had hung up what otherwise was huge progress: a bill that members of the House and Senate, Republicans and Democrats had put together, and that ultimately passed the House.
Renewed efforts at repeal are underway in the current Congress. The House Energy and Commerce Committee’s Health Subcommittee held 2 days of hearings in January, hearing from doctors and health economists on how to cover the $140 billion cost of SGR repeal. Although experts presented their thoughts on where the health care sector could come up with the money, Rep. Fred Upton (R-Mich.), chairman of the full committee, recently suggested that the funding might come from outside the health care sector, such as from his proposal to legalize Internet poker.
But with time running short, some believe that another SGR patch is in the cards and that repeal will come attached to a broader piece of legislation at the end of the year.
“I don’t think there is any way it gets fixed by the March deadline because the payment offsets are just far too complicated. I think that it has to wait to be incorporated, my guess, in a larger bill,” ASCO’s Dr. Polite said. “That’s how I would do it. You want to include it in a much bigger package of tax reforms, perhaps other entitlement reforms where there’s a lot of pluses and minuses of money flow and the $140 billion for SGR is easy to take care of in that.”
He also cautioned that if it is not taken care of this year, it could be at least another 2 years before the window for repeal is opened.
“There is some talk about it getting delayed 18 months,” Dr. Polite said. “I hope that doesn’t happen because if you kick this can down the road 18 months, you basically put us in the 2016 election cycle and nobody’s coming up with $140 billion during that time. Eighteen months basically means we will see you after the 2016 presidential election. And it would be a shame.”
SGR: A patchwork of fixes
Congress has passed 17 different bills to prevent across-the-board Medicare pay cuts due to the SGR, ranging from 3.3% (2005) to 27.4% (2012). Nearly all have been paid for by some kind of offset. Here’s the sordid history:
• 2003 Consolidated Appropriations Act (4.9%)
• 2004 Medicare Prescription Drug, Improvements, and Modernization Act (4.5%)
• 2005 Medicare Prescription Drug, Improvements, and Modernization Act (3.3%)
• 2006 Deficit Reduction Act of 2005 (4.4%)
• 2007 Tax Relief and Health Care Act (5%)
• 2008 Medicare, Medicaid and SCHIP Extension Act (about 10.%)
• 2009 Medicare Improvements for Patients and Providers Act (16%)
• 2010 DOD Appropriations Act plus two Temporary Extension Acts (21%)
• 2010 Preservation of Access to Care for Medicare Beneficiaries Act (21.2%)
• 2010 Physician Payment and Therapy Relief Act (23% )
• 2011 Medicare and Medicaid Extenders Act (25%)
• 2012 Temporary Payroll Tax Cut Continuation Act (27.4%)
• 2012 Middle Class Tax Relief and Job Creation Act (27.4%)
• 2013 American Tax Payer Relief Act (26.5%)
• 2014 Pathway for SGR Reform Act (20.1%)
• 2014 Protecting Access To Medicare Act (24% )
The Sustainable Growth Rate formula. Few aspects of Medicare have been more problematic for physicians.
Designed to control Medicare costs, Congress has spent more since 2003 to delay SGR cuts than it would cost to fund current repeal legislation.
Passed as part of the Balanced Budget Act of 1997, the SGR was designed to make sure Medicare expenditures did not grow faster than the Gross Domestic Product based on four factors: estimated change in physician fees, estimated number of Medicare fee-for-service beneficiaries, estimated 10-year average change in GDP, and estimated changes in expenditures due to law or regulation.
It was not, however, designed to keep up with the Baby Boom. Because it does not adjust for the influx of boomers, it guarantees to produce pay cuts just as demand for physician services grows.
The next pay cut – 21% this time – is slated for April 1.
For doctors, the constant specter of lower payments simply makes it hard to do business.
“Each year, when there is supposedly a cut, it is a consideration for practices that they have to create some contingency thinking, ‘if this were actually to take place, how will I continue to maintain my practice?’ ” Dr. Robert Juhasz, president of the American Osteopathic Association, said in an interview. “If they have a high Medicare population that they take care of, and certainly if there was that kind of a cut, they could not sustain that and would have to make changes.”
Dr. Blase Polite, chair of the American Society of Clinical Oncology Government Relations Committee, agreed. “Ever since the flawed formula was put in place, it has created yearly uncertainty. In recent years, we have had it to the point where the SGR cuts went into effect and then we had to do things like hold bills for a month or 2 months to resubmit them when the SGR would get patched. It became an absolute nightmare from a small business operating standpoint.”
But the tyranny of the SGR may have outgrown itself. In January, the U.S. Department of Health & Human Services announced a major expansion of its efforts to base physicians’ Medicare pay on value instead of volume, calling for half of all Medicare payments to be out of the fee-for-service system by 2018.
“This is the first time in the history of the program that explicit goals for alternative payment models and value-based payment models have been set for Medicare,” HHS Secretary Sylvia Burwell said in an editorial Jan. 26 in the New England Journal of Medicine (doi:10.1056/NEJMp1500445).
The goal is “to move away from the old way of doing things, which amounted to, ‘the more you do, the more you get paid,’ by linking nearly all pay to quality and value in some way to see that we are spending smarter,” Ms. Burwell said in a blog post on the HHS website.
As part of that effort, the department aims to have 30% of Medicare payments tied to quality or value through alternative payment models by the end of 2016.
Further, real efforts to repeal the SGR took hold in the last Congress, with strong support to pass legislation among lawmakers of both parties in the House and in the Senate. H.R. 4015, SGR Repeal and Medicare Provider Payment Modernization Act of 2014, passed the House but was not taken up by the Senate.
“We were cautiously optimistic that this 17th year of trying to repeal the SGR might have been the successful one,” Dr. Patrick T. O’Gara, president of the American College of Cardiology, said in an interview. He said that the sticking point seemed to be that “there was no politically viable way to pay for it.”
Dr. David A. Fleming, president of the American College of Physicians, noted in a statement that finding the money had hung up what otherwise was huge progress: a bill that members of the House and Senate, Republicans and Democrats had put together, and that ultimately passed the House.
Renewed efforts at repeal are underway in the current Congress. The House Energy and Commerce Committee’s Health Subcommittee held 2 days of hearings in January, hearing from doctors and health economists on how to cover the $140 billion cost of SGR repeal. Although experts presented their thoughts on where the health care sector could come up with the money, Rep. Fred Upton (R-Mich.), chairman of the full committee, recently suggested that the funding might come from outside the health care sector, such as from his proposal to legalize Internet poker.
But with time running short, some believe that another SGR patch is in the cards and that repeal will come attached to a broader piece of legislation at the end of the year.
“I don’t think there is any way it gets fixed by the March deadline because the payment offsets are just far too complicated. I think that it has to wait to be incorporated, my guess, in a larger bill,” ASCO’s Dr. Polite said. “That’s how I would do it. You want to include it in a much bigger package of tax reforms, perhaps other entitlement reforms where there’s a lot of pluses and minuses of money flow and the $140 billion for SGR is easy to take care of in that.”
He also cautioned that if it is not taken care of this year, it could be at least another 2 years before the window for repeal is opened.
“There is some talk about it getting delayed 18 months,” Dr. Polite said. “I hope that doesn’t happen because if you kick this can down the road 18 months, you basically put us in the 2016 election cycle and nobody’s coming up with $140 billion during that time. Eighteen months basically means we will see you after the 2016 presidential election. And it would be a shame.”
SGR: A patchwork of fixes
Congress has passed 17 different bills to prevent across-the-board Medicare pay cuts due to the SGR, ranging from 3.3% (2005) to 27.4% (2012). Nearly all have been paid for by some kind of offset. Here’s the sordid history:
• 2003 Consolidated Appropriations Act (4.9%)
• 2004 Medicare Prescription Drug, Improvements, and Modernization Act (4.5%)
• 2005 Medicare Prescription Drug, Improvements, and Modernization Act (3.3%)
• 2006 Deficit Reduction Act of 2005 (4.4%)
• 2007 Tax Relief and Health Care Act (5%)
• 2008 Medicare, Medicaid and SCHIP Extension Act (about 10.%)
• 2009 Medicare Improvements for Patients and Providers Act (16%)
• 2010 DOD Appropriations Act plus two Temporary Extension Acts (21%)
• 2010 Preservation of Access to Care for Medicare Beneficiaries Act (21.2%)
• 2010 Physician Payment and Therapy Relief Act (23% )
• 2011 Medicare and Medicaid Extenders Act (25%)
• 2012 Temporary Payroll Tax Cut Continuation Act (27.4%)
• 2012 Middle Class Tax Relief and Job Creation Act (27.4%)
• 2013 American Tax Payer Relief Act (26.5%)
• 2014 Pathway for SGR Reform Act (20.1%)
• 2014 Protecting Access To Medicare Act (24% )
The Sustainable Growth Rate formula. Few aspects of Medicare have been more problematic for physicians.
Designed to control Medicare costs, Congress has spent more since 2003 to delay SGR cuts than it would cost to fund current repeal legislation.
Passed as part of the Balanced Budget Act of 1997, the SGR was designed to make sure Medicare expenditures did not grow faster than the Gross Domestic Product based on four factors: estimated change in physician fees, estimated number of Medicare fee-for-service beneficiaries, estimated 10-year average change in GDP, and estimated changes in expenditures due to law or regulation.
It was not, however, designed to keep up with the Baby Boom. Because it does not adjust for the influx of boomers, it guarantees to produce pay cuts just as demand for physician services grows.
The next pay cut – 21% this time – is slated for April 1.
For doctors, the constant specter of lower payments simply makes it hard to do business.
“Each year, when there is supposedly a cut, it is a consideration for practices that they have to create some contingency thinking, ‘if this were actually to take place, how will I continue to maintain my practice?’ ” Dr. Robert Juhasz, president of the American Osteopathic Association, said in an interview. “If they have a high Medicare population that they take care of, and certainly if there was that kind of a cut, they could not sustain that and would have to make changes.”
Dr. Blase Polite, chair of the American Society of Clinical Oncology Government Relations Committee, agreed. “Ever since the flawed formula was put in place, it has created yearly uncertainty. In recent years, we have had it to the point where the SGR cuts went into effect and then we had to do things like hold bills for a month or 2 months to resubmit them when the SGR would get patched. It became an absolute nightmare from a small business operating standpoint.”
But the tyranny of the SGR may have outgrown itself. In January, the U.S. Department of Health & Human Services announced a major expansion of its efforts to base physicians’ Medicare pay on value instead of volume, calling for half of all Medicare payments to be out of the fee-for-service system by 2018.
“This is the first time in the history of the program that explicit goals for alternative payment models and value-based payment models have been set for Medicare,” HHS Secretary Sylvia Burwell said in an editorial Jan. 26 in the New England Journal of Medicine (doi:10.1056/NEJMp1500445).
The goal is “to move away from the old way of doing things, which amounted to, ‘the more you do, the more you get paid,’ by linking nearly all pay to quality and value in some way to see that we are spending smarter,” Ms. Burwell said in a blog post on the HHS website.
As part of that effort, the department aims to have 30% of Medicare payments tied to quality or value through alternative payment models by the end of 2016.
Further, real efforts to repeal the SGR took hold in the last Congress, with strong support to pass legislation among lawmakers of both parties in the House and in the Senate. H.R. 4015, SGR Repeal and Medicare Provider Payment Modernization Act of 2014, passed the House but was not taken up by the Senate.
“We were cautiously optimistic that this 17th year of trying to repeal the SGR might have been the successful one,” Dr. Patrick T. O’Gara, president of the American College of Cardiology, said in an interview. He said that the sticking point seemed to be that “there was no politically viable way to pay for it.”
Dr. David A. Fleming, president of the American College of Physicians, noted in a statement that finding the money had hung up what otherwise was huge progress: a bill that members of the House and Senate, Republicans and Democrats had put together, and that ultimately passed the House.
Renewed efforts at repeal are underway in the current Congress. The House Energy and Commerce Committee’s Health Subcommittee held 2 days of hearings in January, hearing from doctors and health economists on how to cover the $140 billion cost of SGR repeal. Although experts presented their thoughts on where the health care sector could come up with the money, Rep. Fred Upton (R-Mich.), chairman of the full committee, recently suggested that the funding might come from outside the health care sector, such as from his proposal to legalize Internet poker.
But with time running short, some believe that another SGR patch is in the cards and that repeal will come attached to a broader piece of legislation at the end of the year.
“I don’t think there is any way it gets fixed by the March deadline because the payment offsets are just far too complicated. I think that it has to wait to be incorporated, my guess, in a larger bill,” ASCO’s Dr. Polite said. “That’s how I would do it. You want to include it in a much bigger package of tax reforms, perhaps other entitlement reforms where there’s a lot of pluses and minuses of money flow and the $140 billion for SGR is easy to take care of in that.”
He also cautioned that if it is not taken care of this year, it could be at least another 2 years before the window for repeal is opened.
“There is some talk about it getting delayed 18 months,” Dr. Polite said. “I hope that doesn’t happen because if you kick this can down the road 18 months, you basically put us in the 2016 election cycle and nobody’s coming up with $140 billion during that time. Eighteen months basically means we will see you after the 2016 presidential election. And it would be a shame.”
SGR: A patchwork of fixes
Congress has passed 17 different bills to prevent across-the-board Medicare pay cuts due to the SGR, ranging from 3.3% (2005) to 27.4% (2012). Nearly all have been paid for by some kind of offset. Here’s the sordid history:
• 2003 Consolidated Appropriations Act (4.9%)
• 2004 Medicare Prescription Drug, Improvements, and Modernization Act (4.5%)
• 2005 Medicare Prescription Drug, Improvements, and Modernization Act (3.3%)
• 2006 Deficit Reduction Act of 2005 (4.4%)
• 2007 Tax Relief and Health Care Act (5%)
• 2008 Medicare, Medicaid and SCHIP Extension Act (about 10.%)
• 2009 Medicare Improvements for Patients and Providers Act (16%)
• 2010 DOD Appropriations Act plus two Temporary Extension Acts (21%)
• 2010 Preservation of Access to Care for Medicare Beneficiaries Act (21.2%)
• 2010 Physician Payment and Therapy Relief Act (23% )
• 2011 Medicare and Medicaid Extenders Act (25%)
• 2012 Temporary Payroll Tax Cut Continuation Act (27.4%)
• 2012 Middle Class Tax Relief and Job Creation Act (27.4%)
• 2013 American Tax Payer Relief Act (26.5%)
• 2014 Pathway for SGR Reform Act (20.1%)
• 2014 Protecting Access To Medicare Act (24% )
Cost of ACA lowers budget deficit
The Congressional Budget Office (CBO) has reduced its budget deficit estimate over the next decade because of lower projected costs for the Affordable Care Act.
Updated projections released March 9 by the CBO find cumulative deficits between 2016 and 2025 will be $431 billion less than the office’s January projection of $7.6 trillion.
Lower costs for ACA provisions driven by smaller spending growth for insurance subsidies, the Children’s Health Insurance Program (CHIP), and Medicaid drove the reduced figure, the CBO said in an online post.
The total projected cost of ACA provisions to the federal government over the next 9 years is $1.2 billion, 11% less than CBO and the Joint Committee on Taxation estimated in January.
However, CBO predicts the annual budget deficit will rise to $486 billion in fiscal 2015, slightly higher than last year’s shortfall. The latest deficit estimate for 2015 is $18 billion higher than CBO had originally projected.
CBO said the estimated rise stems primarily from a projected rise in spending for student loans, Medicaid, and Medicare. The deficit for 2015 represents a slightly lower percentage of gross domestic product of 2.7%, compared with 2.8% last year.
On Twitter @legal_med
The Congressional Budget Office (CBO) has reduced its budget deficit estimate over the next decade because of lower projected costs for the Affordable Care Act.
Updated projections released March 9 by the CBO find cumulative deficits between 2016 and 2025 will be $431 billion less than the office’s January projection of $7.6 trillion.
Lower costs for ACA provisions driven by smaller spending growth for insurance subsidies, the Children’s Health Insurance Program (CHIP), and Medicaid drove the reduced figure, the CBO said in an online post.
The total projected cost of ACA provisions to the federal government over the next 9 years is $1.2 billion, 11% less than CBO and the Joint Committee on Taxation estimated in January.
However, CBO predicts the annual budget deficit will rise to $486 billion in fiscal 2015, slightly higher than last year’s shortfall. The latest deficit estimate for 2015 is $18 billion higher than CBO had originally projected.
CBO said the estimated rise stems primarily from a projected rise in spending for student loans, Medicaid, and Medicare. The deficit for 2015 represents a slightly lower percentage of gross domestic product of 2.7%, compared with 2.8% last year.
On Twitter @legal_med
The Congressional Budget Office (CBO) has reduced its budget deficit estimate over the next decade because of lower projected costs for the Affordable Care Act.
Updated projections released March 9 by the CBO find cumulative deficits between 2016 and 2025 will be $431 billion less than the office’s January projection of $7.6 trillion.
Lower costs for ACA provisions driven by smaller spending growth for insurance subsidies, the Children’s Health Insurance Program (CHIP), and Medicaid drove the reduced figure, the CBO said in an online post.
The total projected cost of ACA provisions to the federal government over the next 9 years is $1.2 billion, 11% less than CBO and the Joint Committee on Taxation estimated in January.
However, CBO predicts the annual budget deficit will rise to $486 billion in fiscal 2015, slightly higher than last year’s shortfall. The latest deficit estimate for 2015 is $18 billion higher than CBO had originally projected.
CBO said the estimated rise stems primarily from a projected rise in spending for student loans, Medicaid, and Medicare. The deficit for 2015 represents a slightly lower percentage of gross domestic product of 2.7%, compared with 2.8% last year.
On Twitter @legal_med
Scoring system identifies mortality risks in esophagectomy patients
SAN DIEGO – Predictive factors such as Zubrod score, previous cardiothoracic surgery, history of smoking, and hypertension can give health care providers a powerful tool for predicting the likelihood of patient morbidity resulting from esophagectomy, thus allowing accurate stratification of such patients and thereby mitigating morbidity rates, a study showed.
Patients who had previously undergone cardiothoracic surgery, had Zubrod scores of at least 2, had diabetes mellitus requiring insulin therapy, were currently smoking, had hypertension, were female, and had a forced expiratory volume in 1 second (FEV1) score of less than 60% were the most highly predisposed to mortality after undergoing esophagectomy, said Dr. J. Matthew Reinersman of the Mayo Clinic in Rochester, Minn., who presented the findings at the annual meeting of the Society of Thoracic Surgeons.
Dr. Reinersman led a team of investigators in a retrospective analysis of 343 consecutive patients in the STS General Thoracic Surgery Database who underwent esophagectomies for malignancies between August 2009 and December 2012. “Our primary outcome variables were operative mortality, both in-hospital and 30-day mortality, as well as major morbidity, which we defined as anastomotic leak, myocardial infarction, pulmonary embolism, pneumonia, reintubation for respiratory failure, empyema, chylothorax, and any reoperation,” he explained.
Univariate and multivariate analyses, using a chi-square test or Fisher’s exact analyses, were performed to look for predictors within the data set, and were subsequently used to craft the risk-based model that assigned each patient a score for how likely he or she would be to experience morbidity or mortality after undergoing an esophagectomy. Each patient was then assigned to one of four groups based on this score – group A (86 subjects), group B (138 subjects), group C (81 subjects), or group D (38 subjects) – in ascending order of score.
Dr. Reinersman and his coauthors found that 17 subjects (19.8%) in group A had either morbidity or mortality, as did 45 subjects (32.6%) in group B, 61 subjects (75.3%) in group C, and 36 (94.7%) in group D, indicating that the model and scoring system developed by the investigators was successful in predicting likely morbidity and mortality outcomes based on patients’ medical histories.
The mean patient age was 63.2 years, and the majority of subjects were male. Smokers were prevalent in the study population: Roughly 56% were former smokers, and 12% were current smokers. Endocarcinoma was the predominant tissue type observed by the authors, and the most common tumor location was the gastroesophageal junction or lower third of the esophagus. Approximately, 75% of patients received neoadjuvant therapy as well.
“This risk-assessment tool, which uses only seven factors and an easy-to-remember scoring system dividing patients into four risk categories, can be easily integrated into everyday clinical practice,” said Dr. Reinersman. “It can help inform patient selection and education, [and] also identifies smoking as an important but modifiable preoperative risk factor.”
Dr. Reinersman reported no relevant financial conflicts.
SAN DIEGO – Predictive factors such as Zubrod score, previous cardiothoracic surgery, history of smoking, and hypertension can give health care providers a powerful tool for predicting the likelihood of patient morbidity resulting from esophagectomy, thus allowing accurate stratification of such patients and thereby mitigating morbidity rates, a study showed.
Patients who had previously undergone cardiothoracic surgery, had Zubrod scores of at least 2, had diabetes mellitus requiring insulin therapy, were currently smoking, had hypertension, were female, and had a forced expiratory volume in 1 second (FEV1) score of less than 60% were the most highly predisposed to mortality after undergoing esophagectomy, said Dr. J. Matthew Reinersman of the Mayo Clinic in Rochester, Minn., who presented the findings at the annual meeting of the Society of Thoracic Surgeons.
Dr. Reinersman led a team of investigators in a retrospective analysis of 343 consecutive patients in the STS General Thoracic Surgery Database who underwent esophagectomies for malignancies between August 2009 and December 2012. “Our primary outcome variables were operative mortality, both in-hospital and 30-day mortality, as well as major morbidity, which we defined as anastomotic leak, myocardial infarction, pulmonary embolism, pneumonia, reintubation for respiratory failure, empyema, chylothorax, and any reoperation,” he explained.
Univariate and multivariate analyses, using a chi-square test or Fisher’s exact analyses, were performed to look for predictors within the data set, and were subsequently used to craft the risk-based model that assigned each patient a score for how likely he or she would be to experience morbidity or mortality after undergoing an esophagectomy. Each patient was then assigned to one of four groups based on this score – group A (86 subjects), group B (138 subjects), group C (81 subjects), or group D (38 subjects) – in ascending order of score.
Dr. Reinersman and his coauthors found that 17 subjects (19.8%) in group A had either morbidity or mortality, as did 45 subjects (32.6%) in group B, 61 subjects (75.3%) in group C, and 36 (94.7%) in group D, indicating that the model and scoring system developed by the investigators was successful in predicting likely morbidity and mortality outcomes based on patients’ medical histories.
The mean patient age was 63.2 years, and the majority of subjects were male. Smokers were prevalent in the study population: Roughly 56% were former smokers, and 12% were current smokers. Endocarcinoma was the predominant tissue type observed by the authors, and the most common tumor location was the gastroesophageal junction or lower third of the esophagus. Approximately, 75% of patients received neoadjuvant therapy as well.
“This risk-assessment tool, which uses only seven factors and an easy-to-remember scoring system dividing patients into four risk categories, can be easily integrated into everyday clinical practice,” said Dr. Reinersman. “It can help inform patient selection and education, [and] also identifies smoking as an important but modifiable preoperative risk factor.”
Dr. Reinersman reported no relevant financial conflicts.
SAN DIEGO – Predictive factors such as Zubrod score, previous cardiothoracic surgery, history of smoking, and hypertension can give health care providers a powerful tool for predicting the likelihood of patient morbidity resulting from esophagectomy, thus allowing accurate stratification of such patients and thereby mitigating morbidity rates, a study showed.
Patients who had previously undergone cardiothoracic surgery, had Zubrod scores of at least 2, had diabetes mellitus requiring insulin therapy, were currently smoking, had hypertension, were female, and had a forced expiratory volume in 1 second (FEV1) score of less than 60% were the most highly predisposed to mortality after undergoing esophagectomy, said Dr. J. Matthew Reinersman of the Mayo Clinic in Rochester, Minn., who presented the findings at the annual meeting of the Society of Thoracic Surgeons.
Dr. Reinersman led a team of investigators in a retrospective analysis of 343 consecutive patients in the STS General Thoracic Surgery Database who underwent esophagectomies for malignancies between August 2009 and December 2012. “Our primary outcome variables were operative mortality, both in-hospital and 30-day mortality, as well as major morbidity, which we defined as anastomotic leak, myocardial infarction, pulmonary embolism, pneumonia, reintubation for respiratory failure, empyema, chylothorax, and any reoperation,” he explained.
Univariate and multivariate analyses, using a chi-square test or Fisher’s exact analyses, were performed to look for predictors within the data set, and were subsequently used to craft the risk-based model that assigned each patient a score for how likely he or she would be to experience morbidity or mortality after undergoing an esophagectomy. Each patient was then assigned to one of four groups based on this score – group A (86 subjects), group B (138 subjects), group C (81 subjects), or group D (38 subjects) – in ascending order of score.
Dr. Reinersman and his coauthors found that 17 subjects (19.8%) in group A had either morbidity or mortality, as did 45 subjects (32.6%) in group B, 61 subjects (75.3%) in group C, and 36 (94.7%) in group D, indicating that the model and scoring system developed by the investigators was successful in predicting likely morbidity and mortality outcomes based on patients’ medical histories.
The mean patient age was 63.2 years, and the majority of subjects were male. Smokers were prevalent in the study population: Roughly 56% were former smokers, and 12% were current smokers. Endocarcinoma was the predominant tissue type observed by the authors, and the most common tumor location was the gastroesophageal junction or lower third of the esophagus. Approximately, 75% of patients received neoadjuvant therapy as well.
“This risk-assessment tool, which uses only seven factors and an easy-to-remember scoring system dividing patients into four risk categories, can be easily integrated into everyday clinical practice,” said Dr. Reinersman. “It can help inform patient selection and education, [and] also identifies smoking as an important but modifiable preoperative risk factor.”
Dr. Reinersman reported no relevant financial conflicts.
AT THE STS ANNUAL MEETING
Key clinical point: Certain predictive indicators can help stratify esophagectomy patients based on preoperative variables and risk factors so that morbidity rates are mitigated.
Major finding: Of 343 patients studied, morbidity occurred in 159 (45.8%); the combined 30-day and in-hospital mortality in subjects was 12 (3.5%); the most reliable predictors were prior cardiothoracic surgery, Zubrod score ≥ 2, diabetes mellitus requiring insulin therapy, current smoking, hypertension, female gender, and an FEV1 score less than 60% of predicted.
Data source: A retrospective analysis of 343 patients with esophageal cancer who underwent esophagectomy from August 2009 to December 2012.
Disclosures: Dr. Reinersman reported no relevant financial conflicts.
Modified Sugarbaker enhances parastomal hernia repair
CHICAGO – Patients who underwent modified laparoscopic Sugarbaker parastomal hernia repair were a third less likely to experience recurrence as those repaired with other surgical techniques in a multicenter, retrospective study in 62 patients.
The recurrence rate was 16.6% for the modified Sugarbaker technique, compared with 61% for keyhole repair, 69.2% for ostomy relocation, and 33.3% for open repair (P value < .001). Median follow-up was 16.6 months, 19.6 months, 16.4 months, and 27.2 months (P = .748).
In an adjusted Cox proportional hazards regression model, the Sugarbaker technique (hazard ratio, 0.28; P = .021) and body mass index (HR, 1.09; P = .013) were the only significant predictors of time to hernia recurrence.
Using the Kaplan-Meier method, 80% of Sugarbaker patients would be recurrence free at 2 years vs. about 60% of those in the other groups (log-rank P = .021), Mr. Francis DeAsis, a research assistant from NorthShore University Health in Evanston, Ill., reported at the annual meeting of the Central Surgical Association.
The findings are in keeping with prior Sugarbaker studies involving 177 repairs between 2005 and 2013, reporting recurrence rates between 4% and 20% and morbidity of 12%-43%, he said.
Morbidity was 40% among the 25 Sugarbaker repairs in the current analysis, significantly lower than that in the Keyhole, relocation, and open repair groups (40% vs. 83.3%, 61.5%, 83.3%; P = .005).
“Based on our results and others, we’d like to suggest that the Sugarbaker approach should be the primary option for treating parastomal hernia,” Mr. DeAsis said.
The study provides “further proof that no other technique available results in a durable repair compared to the Sugarbaker technique for these challenging hernias,” senior study author Dr. Michael Ujiki, director of minimally invasive surgery at NorthShore, said in an interview.
The Sugarbaker technique typically involves a laparoscopic mesh sublay over the fascial defect and lateralization of the stoma limb. Modifications at NorthShore included use of polytetrafluoroethylene mesh with a 5-cm overlap of the defect and, if possible, primary closure of the defect. A catheter is occasionally used to identify the correct ostomy limb, but most importantly, a laparoscopic approach is utilized in order to decrease wound infections and quicken the return to daily activities, Dr. Ujiki said. “We also avoid cautery and diligently look for other incidental hernias at the prevision incisions.”
Ileus (> 3 days) was the most common complication in all groups: Sugarbaker (4/25), keyhole (9/18), relocation (3/13), and open (1/6). Only one death occurred; in the open group.
Discussant Dr. Matthew Goldblatt, with the Medical College of Wisconsin in Milwaukee, questioned how many patients also had ventral hernias and whether this was a complicating factor in ileus or length of stay and whether the fascia was closed primarily during keyhole repair or the mesh simply placed as a bridge, as this can impact failure rates.
Dr. Ujiki responded that some patients had concomitant ventral hernias and that they simply used a larger piece of mesh to cover both hernias. Primary closure was not part of the keyhole repair early in the 10-year series, spanning 2004 to 2014, but ultimately was performed in about half of patients in the keyhole group.
“I don’t think that there’s going to be a difference between the two in terms of recurrence, but I can’t say for sure,” he added.
At this point, the group does not use prophylactic mesh placement at the time the ostomy is created, to avoid infections.
Finally, the audience asked whether the investigators are willing to accept a 16% recurrence rate, a fourfold increase over the best reported result with a modified Sugarbaker technique.
“With these hernia repairs, to me a 16% recurrence rate is outstanding and I think it will only get better,” Dr. Ujiki said.
The series includes every patient on which they’ve performed a Sugarbaker and thus, represents their learning curve, which may not be the case with other series, he noted.
Dr. Ujiki left the audience with two bits of advice to hasten the learning curve: leave at least 5 cm of overlap because the mesh will shrink down and keep the stitches close to the mesh without cutting off the bowel.
CHICAGO – Patients who underwent modified laparoscopic Sugarbaker parastomal hernia repair were a third less likely to experience recurrence as those repaired with other surgical techniques in a multicenter, retrospective study in 62 patients.
The recurrence rate was 16.6% for the modified Sugarbaker technique, compared with 61% for keyhole repair, 69.2% for ostomy relocation, and 33.3% for open repair (P value < .001). Median follow-up was 16.6 months, 19.6 months, 16.4 months, and 27.2 months (P = .748).
In an adjusted Cox proportional hazards regression model, the Sugarbaker technique (hazard ratio, 0.28; P = .021) and body mass index (HR, 1.09; P = .013) were the only significant predictors of time to hernia recurrence.
Using the Kaplan-Meier method, 80% of Sugarbaker patients would be recurrence free at 2 years vs. about 60% of those in the other groups (log-rank P = .021), Mr. Francis DeAsis, a research assistant from NorthShore University Health in Evanston, Ill., reported at the annual meeting of the Central Surgical Association.
The findings are in keeping with prior Sugarbaker studies involving 177 repairs between 2005 and 2013, reporting recurrence rates between 4% and 20% and morbidity of 12%-43%, he said.
Morbidity was 40% among the 25 Sugarbaker repairs in the current analysis, significantly lower than that in the Keyhole, relocation, and open repair groups (40% vs. 83.3%, 61.5%, 83.3%; P = .005).
“Based on our results and others, we’d like to suggest that the Sugarbaker approach should be the primary option for treating parastomal hernia,” Mr. DeAsis said.
The study provides “further proof that no other technique available results in a durable repair compared to the Sugarbaker technique for these challenging hernias,” senior study author Dr. Michael Ujiki, director of minimally invasive surgery at NorthShore, said in an interview.
The Sugarbaker technique typically involves a laparoscopic mesh sublay over the fascial defect and lateralization of the stoma limb. Modifications at NorthShore included use of polytetrafluoroethylene mesh with a 5-cm overlap of the defect and, if possible, primary closure of the defect. A catheter is occasionally used to identify the correct ostomy limb, but most importantly, a laparoscopic approach is utilized in order to decrease wound infections and quicken the return to daily activities, Dr. Ujiki said. “We also avoid cautery and diligently look for other incidental hernias at the prevision incisions.”
Ileus (> 3 days) was the most common complication in all groups: Sugarbaker (4/25), keyhole (9/18), relocation (3/13), and open (1/6). Only one death occurred; in the open group.
Discussant Dr. Matthew Goldblatt, with the Medical College of Wisconsin in Milwaukee, questioned how many patients also had ventral hernias and whether this was a complicating factor in ileus or length of stay and whether the fascia was closed primarily during keyhole repair or the mesh simply placed as a bridge, as this can impact failure rates.
Dr. Ujiki responded that some patients had concomitant ventral hernias and that they simply used a larger piece of mesh to cover both hernias. Primary closure was not part of the keyhole repair early in the 10-year series, spanning 2004 to 2014, but ultimately was performed in about half of patients in the keyhole group.
“I don’t think that there’s going to be a difference between the two in terms of recurrence, but I can’t say for sure,” he added.
At this point, the group does not use prophylactic mesh placement at the time the ostomy is created, to avoid infections.
Finally, the audience asked whether the investigators are willing to accept a 16% recurrence rate, a fourfold increase over the best reported result with a modified Sugarbaker technique.
“With these hernia repairs, to me a 16% recurrence rate is outstanding and I think it will only get better,” Dr. Ujiki said.
The series includes every patient on which they’ve performed a Sugarbaker and thus, represents their learning curve, which may not be the case with other series, he noted.
Dr. Ujiki left the audience with two bits of advice to hasten the learning curve: leave at least 5 cm of overlap because the mesh will shrink down and keep the stitches close to the mesh without cutting off the bowel.
CHICAGO – Patients who underwent modified laparoscopic Sugarbaker parastomal hernia repair were a third less likely to experience recurrence as those repaired with other surgical techniques in a multicenter, retrospective study in 62 patients.
The recurrence rate was 16.6% for the modified Sugarbaker technique, compared with 61% for keyhole repair, 69.2% for ostomy relocation, and 33.3% for open repair (P value < .001). Median follow-up was 16.6 months, 19.6 months, 16.4 months, and 27.2 months (P = .748).
In an adjusted Cox proportional hazards regression model, the Sugarbaker technique (hazard ratio, 0.28; P = .021) and body mass index (HR, 1.09; P = .013) were the only significant predictors of time to hernia recurrence.
Using the Kaplan-Meier method, 80% of Sugarbaker patients would be recurrence free at 2 years vs. about 60% of those in the other groups (log-rank P = .021), Mr. Francis DeAsis, a research assistant from NorthShore University Health in Evanston, Ill., reported at the annual meeting of the Central Surgical Association.
The findings are in keeping with prior Sugarbaker studies involving 177 repairs between 2005 and 2013, reporting recurrence rates between 4% and 20% and morbidity of 12%-43%, he said.
Morbidity was 40% among the 25 Sugarbaker repairs in the current analysis, significantly lower than that in the Keyhole, relocation, and open repair groups (40% vs. 83.3%, 61.5%, 83.3%; P = .005).
“Based on our results and others, we’d like to suggest that the Sugarbaker approach should be the primary option for treating parastomal hernia,” Mr. DeAsis said.
The study provides “further proof that no other technique available results in a durable repair compared to the Sugarbaker technique for these challenging hernias,” senior study author Dr. Michael Ujiki, director of minimally invasive surgery at NorthShore, said in an interview.
The Sugarbaker technique typically involves a laparoscopic mesh sublay over the fascial defect and lateralization of the stoma limb. Modifications at NorthShore included use of polytetrafluoroethylene mesh with a 5-cm overlap of the defect and, if possible, primary closure of the defect. A catheter is occasionally used to identify the correct ostomy limb, but most importantly, a laparoscopic approach is utilized in order to decrease wound infections and quicken the return to daily activities, Dr. Ujiki said. “We also avoid cautery and diligently look for other incidental hernias at the prevision incisions.”
Ileus (> 3 days) was the most common complication in all groups: Sugarbaker (4/25), keyhole (9/18), relocation (3/13), and open (1/6). Only one death occurred; in the open group.
Discussant Dr. Matthew Goldblatt, with the Medical College of Wisconsin in Milwaukee, questioned how many patients also had ventral hernias and whether this was a complicating factor in ileus or length of stay and whether the fascia was closed primarily during keyhole repair or the mesh simply placed as a bridge, as this can impact failure rates.
Dr. Ujiki responded that some patients had concomitant ventral hernias and that they simply used a larger piece of mesh to cover both hernias. Primary closure was not part of the keyhole repair early in the 10-year series, spanning 2004 to 2014, but ultimately was performed in about half of patients in the keyhole group.
“I don’t think that there’s going to be a difference between the two in terms of recurrence, but I can’t say for sure,” he added.
At this point, the group does not use prophylactic mesh placement at the time the ostomy is created, to avoid infections.
Finally, the audience asked whether the investigators are willing to accept a 16% recurrence rate, a fourfold increase over the best reported result with a modified Sugarbaker technique.
“With these hernia repairs, to me a 16% recurrence rate is outstanding and I think it will only get better,” Dr. Ujiki said.
The series includes every patient on which they’ve performed a Sugarbaker and thus, represents their learning curve, which may not be the case with other series, he noted.
Dr. Ujiki left the audience with two bits of advice to hasten the learning curve: leave at least 5 cm of overlap because the mesh will shrink down and keep the stitches close to the mesh without cutting off the bowel.
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: A modified laparoscopic Sugarbaker parastomal hernia repair had lower rates of recurrence and complications than other surgical repair techniques.
Major finding: The recurrence rate was 16.6% for the modified Sugarbaker technique, 61% for keyhole repair, 69.2% for ostomy relocation, and 33.3% for open repair (P < .001).
Data source: Retrospective study of 62 parastomal hernia repairs.
Disclosures: Mr. DeAsis reported having no financial disclosures. Co-authors Dr. John Linn and Dr. Michael Ujiki reported serving as consultants for Covidien and speakers for Gore.
Hybrid revascularization remains a rare bird
SNOWMASS, COLO. – For all the talk of embracing the heart team approach to coronary revascularization as the new standard, emphasizing interdisciplinary collaboration between cardiologists and surgeons, hybrid coronary revascularization remains a rarely employed strategy.
Hybrid coronary revascularization (HCR) is performed at one-third of U.S. centers providing coronary artery bypass graft (CABG) surgery, but that’s a misleading statistic. A mere handful of the centers have extensive experience with this strategy, according to the first nationwide assessment of HCR in patients with multivessel coronary artery disease.
“Only a very few centers – maybe 5 or 10 – do hybrid procedures as 8%-10% of their volume,” Dr. Vinod H. Thourani* said at the Annual Cardiovascular Conference at Snowmass.
He was a coinvestigator in the analysis of nearly 200,000 CABG procedures in the Society of Thoracic Surgeons (STS) national database for 2011-2013. Hybrid coronary revascularization – a combination of surgical and percutaneous techniques coupling minimally invasive bypass of the left anterior descending (LAD) coronary artery using an internal mammary artery graft along with drug-eluting stents for non-LAD lesions – accounted for just 0.48% of total CABG volume. And no trend for growth in the HCR approach was evident during the study period.
Moreover, even in the one-third of U.S. CABG centers that performed hybrid coronary revascularization, the strategy was used on average in less than 1% of all CABG procedures (Circulation 2014;130:872-9), noted Dr. Thourani, professor of cardiothoracic surgery and codirector of the Structural Heart and Valve Center at Emory University, Atlanta.
In contrast, he and his Emory colleagues have fully embraced HCR. At Emory, even as the annual number of primary isolated CABG procedures with sternotomy fell by 44% from 2005 to 2012, there was a compensatory increase in the number of HCRs.
“We’ve actually maintained our coronary bypass volume based on introducing HCR, unlike a lot of programs,” according to the surgeon.
The appeal of HCR is that it combines the durability of the internal mammary artery-to-LAD graft – long recognized as the main source of the survival advantage CABG holds over percutaneous interventions – with drug-eluting stents as a less invasive alternative to often-unreliable vein grafts in non-LAD target vessels.
The current American College of Cardiology/American Heart Association guidelines on coronary revascularization give HCR a favorable class IIa recommendation. However, since there are few data on clinical outcomes with HCR versus conventional CABG, Dr. Thourani and his coinvestigators compared in-hospital outcomes in the STS database. They found that after adjustment for the higher cardiovascular risk profiles present in patients undergoing HCR, the rates of in-hospital mortality and major morbidity in the two groups were similar, suggesting HCR may offer an equally safe alternative to CABG in selected patients.
Patients want less invasive alternatives to CABG with sternotomy. The three most common minimally invasive, sternal-sparing approaches are minimally invasive direct coronary artery bypass, or MIDCAB; robotic-assisted totally endoscopic coronary artery bypass, or TECAB; and robotic-assisted coronary artery bypass, a favored approach at Emory. In robotic-assisted coronary artery bypass, the harvest of the left internal mammary artery, pericardiotomy, and targeting of the LAD are accomplished with robotic assistance, but the anastomosis is hand sewn under direct vision, off pump, via a non–rib-spreading 3- to 4-cm minithoracotomy.
In a report on 307 consecutive patients who underwent robotic-assisted CABG at the university, including 159 who had HCR for multivessel disease, short-term clinical and angiographic outcomes were excellent (J. Thorac. Cardiovasc. Surg. 2014;147:179-85). Particularly striking, in Dr. Thourani’s view, was that only one postoperative stroke occurred, for a 0.3% incidence. That’s a far lower rate than typical with CABG with vein grafts.
In a more recent, as-yet-unpublished update including 477 consecutive HCR patients at Emory, the stroke rate remained extraordinarily low at 0.2%, he said.
“You can almost eliminate stroke with this procedure,” according to Dr. Thourani.
Thirty-day mortality was 0.8%, with an MI rate of 1.0%, a 3.8% incidence of conversion to sternotomy, and a 1.9% repeat revascularization rate. The rate of Fitzgibbon A patency was 96.2%, he noted.
“Return to work is really at the patient’s discretion. We tell them, ‘when you don’t hurt, you can go back.’ Some people go back 4-5 days after surgery. And there are really zero limitations for the patient – none whatsoever,” the surgeon said.
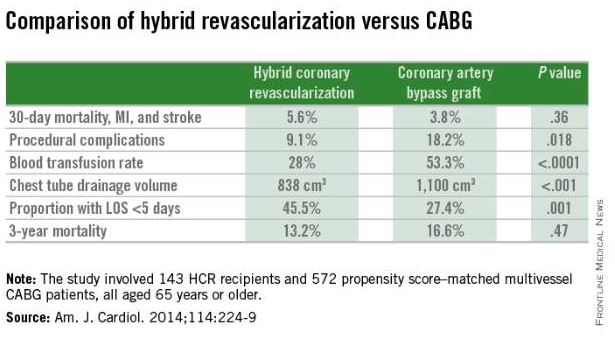
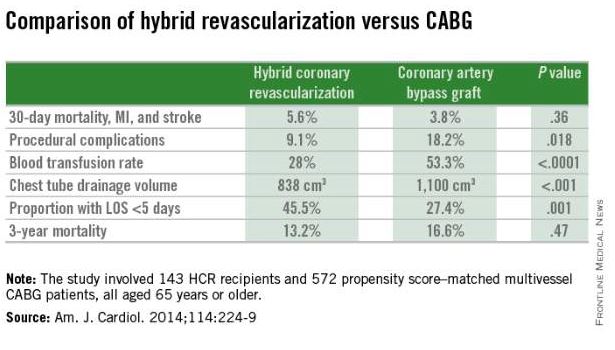
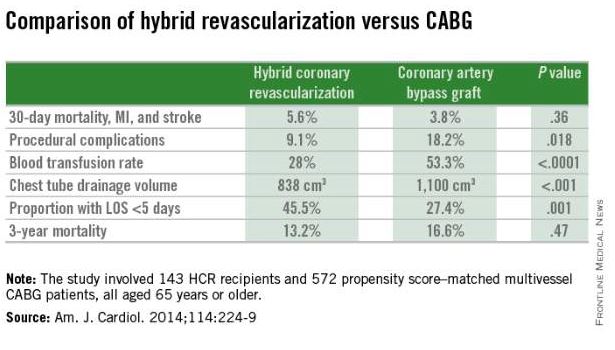
The HCR approach to multivessel revascularization appears to be particularly advantageous in diabetic patients and in older individuals. In a retrospective, nonrandomized single-center comparison of 143 HCR recipients who were propensity score matched to 572 patients who underwent multivessel CABG (Am. J. Cardiol. 2014;114:224-9), the HCR recipients had significantly fewer procedural complications, faster recovery, and similar 3-year mortality (see graphic).
Dr. Thourani said that because of the dirth of randomized trials data, it must be conceded that there is equipoise at present regarding the most effective treatment strategy in patients with multivessel coronary disease. The options are CABG with left internal mammary artery and vein grafts, HCR, medical management, multivessel percutaneous coronary intervention (PCI), and multiarterial CABG. But he added that the available evidence, while not definitive, does point the way forward.
“As we move into 2015 and the future, I think we should be doing less of the left intermal mammary artery with vein grafts, potentially less of the medical therapy, and I think we need to do a lot more multiarterial grafts if we think patients need to be opened up with a sternotomy. And if we don’t think they need to be opened up, we need to think very strongly about hybrid revascularization instead of multivessel PCI, especially in patients who are diabetic or old,” according to the surgeon.
Dr. Thourani reported serving as a consultant to Edwards Lifesciences and St. Jude Medical and receiving research grants from Abbott, Boston Scientific, Medtronic, and Sorin.
*Clarification, 4/20/2015: Dr. Vinod H. Thourani wishes to clarify that, as he stated in his presentation, the current work he reported on from Emory University was performed by Dr. Michael Halkos, who is the leader of hybrid revascularization at Emory, and that Dr. Halkos was lead author and researcher in several of the other studies reported upon.
SNOWMASS, COLO. – For all the talk of embracing the heart team approach to coronary revascularization as the new standard, emphasizing interdisciplinary collaboration between cardiologists and surgeons, hybrid coronary revascularization remains a rarely employed strategy.
Hybrid coronary revascularization (HCR) is performed at one-third of U.S. centers providing coronary artery bypass graft (CABG) surgery, but that’s a misleading statistic. A mere handful of the centers have extensive experience with this strategy, according to the first nationwide assessment of HCR in patients with multivessel coronary artery disease.
“Only a very few centers – maybe 5 or 10 – do hybrid procedures as 8%-10% of their volume,” Dr. Vinod H. Thourani* said at the Annual Cardiovascular Conference at Snowmass.
He was a coinvestigator in the analysis of nearly 200,000 CABG procedures in the Society of Thoracic Surgeons (STS) national database for 2011-2013. Hybrid coronary revascularization – a combination of surgical and percutaneous techniques coupling minimally invasive bypass of the left anterior descending (LAD) coronary artery using an internal mammary artery graft along with drug-eluting stents for non-LAD lesions – accounted for just 0.48% of total CABG volume. And no trend for growth in the HCR approach was evident during the study period.
Moreover, even in the one-third of U.S. CABG centers that performed hybrid coronary revascularization, the strategy was used on average in less than 1% of all CABG procedures (Circulation 2014;130:872-9), noted Dr. Thourani, professor of cardiothoracic surgery and codirector of the Structural Heart and Valve Center at Emory University, Atlanta.
In contrast, he and his Emory colleagues have fully embraced HCR. At Emory, even as the annual number of primary isolated CABG procedures with sternotomy fell by 44% from 2005 to 2012, there was a compensatory increase in the number of HCRs.
“We’ve actually maintained our coronary bypass volume based on introducing HCR, unlike a lot of programs,” according to the surgeon.
The appeal of HCR is that it combines the durability of the internal mammary artery-to-LAD graft – long recognized as the main source of the survival advantage CABG holds over percutaneous interventions – with drug-eluting stents as a less invasive alternative to often-unreliable vein grafts in non-LAD target vessels.
The current American College of Cardiology/American Heart Association guidelines on coronary revascularization give HCR a favorable class IIa recommendation. However, since there are few data on clinical outcomes with HCR versus conventional CABG, Dr. Thourani and his coinvestigators compared in-hospital outcomes in the STS database. They found that after adjustment for the higher cardiovascular risk profiles present in patients undergoing HCR, the rates of in-hospital mortality and major morbidity in the two groups were similar, suggesting HCR may offer an equally safe alternative to CABG in selected patients.
Patients want less invasive alternatives to CABG with sternotomy. The three most common minimally invasive, sternal-sparing approaches are minimally invasive direct coronary artery bypass, or MIDCAB; robotic-assisted totally endoscopic coronary artery bypass, or TECAB; and robotic-assisted coronary artery bypass, a favored approach at Emory. In robotic-assisted coronary artery bypass, the harvest of the left internal mammary artery, pericardiotomy, and targeting of the LAD are accomplished with robotic assistance, but the anastomosis is hand sewn under direct vision, off pump, via a non–rib-spreading 3- to 4-cm minithoracotomy.
In a report on 307 consecutive patients who underwent robotic-assisted CABG at the university, including 159 who had HCR for multivessel disease, short-term clinical and angiographic outcomes were excellent (J. Thorac. Cardiovasc. Surg. 2014;147:179-85). Particularly striking, in Dr. Thourani’s view, was that only one postoperative stroke occurred, for a 0.3% incidence. That’s a far lower rate than typical with CABG with vein grafts.
In a more recent, as-yet-unpublished update including 477 consecutive HCR patients at Emory, the stroke rate remained extraordinarily low at 0.2%, he said.
“You can almost eliminate stroke with this procedure,” according to Dr. Thourani.
Thirty-day mortality was 0.8%, with an MI rate of 1.0%, a 3.8% incidence of conversion to sternotomy, and a 1.9% repeat revascularization rate. The rate of Fitzgibbon A patency was 96.2%, he noted.
“Return to work is really at the patient’s discretion. We tell them, ‘when you don’t hurt, you can go back.’ Some people go back 4-5 days after surgery. And there are really zero limitations for the patient – none whatsoever,” the surgeon said.
The HCR approach to multivessel revascularization appears to be particularly advantageous in diabetic patients and in older individuals. In a retrospective, nonrandomized single-center comparison of 143 HCR recipients who were propensity score matched to 572 patients who underwent multivessel CABG (Am. J. Cardiol. 2014;114:224-9), the HCR recipients had significantly fewer procedural complications, faster recovery, and similar 3-year mortality (see graphic).
Dr. Thourani said that because of the dirth of randomized trials data, it must be conceded that there is equipoise at present regarding the most effective treatment strategy in patients with multivessel coronary disease. The options are CABG with left internal mammary artery and vein grafts, HCR, medical management, multivessel percutaneous coronary intervention (PCI), and multiarterial CABG. But he added that the available evidence, while not definitive, does point the way forward.
“As we move into 2015 and the future, I think we should be doing less of the left intermal mammary artery with vein grafts, potentially less of the medical therapy, and I think we need to do a lot more multiarterial grafts if we think patients need to be opened up with a sternotomy. And if we don’t think they need to be opened up, we need to think very strongly about hybrid revascularization instead of multivessel PCI, especially in patients who are diabetic or old,” according to the surgeon.
Dr. Thourani reported serving as a consultant to Edwards Lifesciences and St. Jude Medical and receiving research grants from Abbott, Boston Scientific, Medtronic, and Sorin.
*Clarification, 4/20/2015: Dr. Vinod H. Thourani wishes to clarify that, as he stated in his presentation, the current work he reported on from Emory University was performed by Dr. Michael Halkos, who is the leader of hybrid revascularization at Emory, and that Dr. Halkos was lead author and researcher in several of the other studies reported upon.
SNOWMASS, COLO. – For all the talk of embracing the heart team approach to coronary revascularization as the new standard, emphasizing interdisciplinary collaboration between cardiologists and surgeons, hybrid coronary revascularization remains a rarely employed strategy.
Hybrid coronary revascularization (HCR) is performed at one-third of U.S. centers providing coronary artery bypass graft (CABG) surgery, but that’s a misleading statistic. A mere handful of the centers have extensive experience with this strategy, according to the first nationwide assessment of HCR in patients with multivessel coronary artery disease.
“Only a very few centers – maybe 5 or 10 – do hybrid procedures as 8%-10% of their volume,” Dr. Vinod H. Thourani* said at the Annual Cardiovascular Conference at Snowmass.
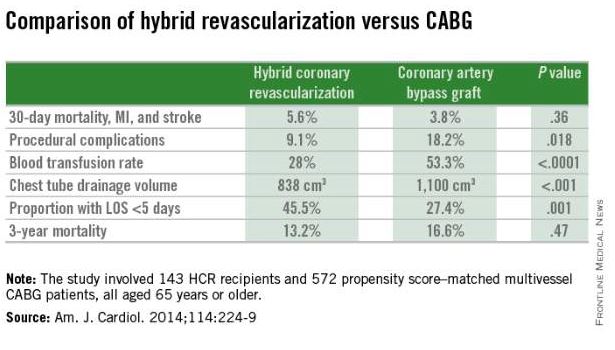
He was a coinvestigator in the analysis of nearly 200,000 CABG procedures in the Society of Thoracic Surgeons (STS) national database for 2011-2013. Hybrid coronary revascularization – a combination of surgical and percutaneous techniques coupling minimally invasive bypass of the left anterior descending (LAD) coronary artery using an internal mammary artery graft along with drug-eluting stents for non-LAD lesions – accounted for just 0.48% of total CABG volume. And no trend for growth in the HCR approach was evident during the study period.
Moreover, even in the one-third of U.S. CABG centers that performed hybrid coronary revascularization, the strategy was used on average in less than 1% of all CABG procedures (Circulation 2014;130:872-9), noted Dr. Thourani, professor of cardiothoracic surgery and codirector of the Structural Heart and Valve Center at Emory University, Atlanta.
In contrast, he and his Emory colleagues have fully embraced HCR. At Emory, even as the annual number of primary isolated CABG procedures with sternotomy fell by 44% from 2005 to 2012, there was a compensatory increase in the number of HCRs.
“We’ve actually maintained our coronary bypass volume based on introducing HCR, unlike a lot of programs,” according to the surgeon.
The appeal of HCR is that it combines the durability of the internal mammary artery-to-LAD graft – long recognized as the main source of the survival advantage CABG holds over percutaneous interventions – with drug-eluting stents as a less invasive alternative to often-unreliable vein grafts in non-LAD target vessels.
The current American College of Cardiology/American Heart Association guidelines on coronary revascularization give HCR a favorable class IIa recommendation. However, since there are few data on clinical outcomes with HCR versus conventional CABG, Dr. Thourani and his coinvestigators compared in-hospital outcomes in the STS database. They found that after adjustment for the higher cardiovascular risk profiles present in patients undergoing HCR, the rates of in-hospital mortality and major morbidity in the two groups were similar, suggesting HCR may offer an equally safe alternative to CABG in selected patients.
Patients want less invasive alternatives to CABG with sternotomy. The three most common minimally invasive, sternal-sparing approaches are minimally invasive direct coronary artery bypass, or MIDCAB; robotic-assisted totally endoscopic coronary artery bypass, or TECAB; and robotic-assisted coronary artery bypass, a favored approach at Emory. In robotic-assisted coronary artery bypass, the harvest of the left internal mammary artery, pericardiotomy, and targeting of the LAD are accomplished with robotic assistance, but the anastomosis is hand sewn under direct vision, off pump, via a non–rib-spreading 3- to 4-cm minithoracotomy.
In a report on 307 consecutive patients who underwent robotic-assisted CABG at the university, including 159 who had HCR for multivessel disease, short-term clinical and angiographic outcomes were excellent (J. Thorac. Cardiovasc. Surg. 2014;147:179-85). Particularly striking, in Dr. Thourani’s view, was that only one postoperative stroke occurred, for a 0.3% incidence. That’s a far lower rate than typical with CABG with vein grafts.
In a more recent, as-yet-unpublished update including 477 consecutive HCR patients at Emory, the stroke rate remained extraordinarily low at 0.2%, he said.
“You can almost eliminate stroke with this procedure,” according to Dr. Thourani.
Thirty-day mortality was 0.8%, with an MI rate of 1.0%, a 3.8% incidence of conversion to sternotomy, and a 1.9% repeat revascularization rate. The rate of Fitzgibbon A patency was 96.2%, he noted.
“Return to work is really at the patient’s discretion. We tell them, ‘when you don’t hurt, you can go back.’ Some people go back 4-5 days after surgery. And there are really zero limitations for the patient – none whatsoever,” the surgeon said.
The HCR approach to multivessel revascularization appears to be particularly advantageous in diabetic patients and in older individuals. In a retrospective, nonrandomized single-center comparison of 143 HCR recipients who were propensity score matched to 572 patients who underwent multivessel CABG (Am. J. Cardiol. 2014;114:224-9), the HCR recipients had significantly fewer procedural complications, faster recovery, and similar 3-year mortality (see graphic).
Dr. Thourani said that because of the dirth of randomized trials data, it must be conceded that there is equipoise at present regarding the most effective treatment strategy in patients with multivessel coronary disease. The options are CABG with left internal mammary artery and vein grafts, HCR, medical management, multivessel percutaneous coronary intervention (PCI), and multiarterial CABG. But he added that the available evidence, while not definitive, does point the way forward.
“As we move into 2015 and the future, I think we should be doing less of the left intermal mammary artery with vein grafts, potentially less of the medical therapy, and I think we need to do a lot more multiarterial grafts if we think patients need to be opened up with a sternotomy. And if we don’t think they need to be opened up, we need to think very strongly about hybrid revascularization instead of multivessel PCI, especially in patients who are diabetic or old,” according to the surgeon.
Dr. Thourani reported serving as a consultant to Edwards Lifesciences and St. Jude Medical and receiving research grants from Abbott, Boston Scientific, Medtronic, and Sorin.
*Clarification, 4/20/2015: Dr. Vinod H. Thourani wishes to clarify that, as he stated in his presentation, the current work he reported on from Emory University was performed by Dr. Michael Halkos, who is the leader of hybrid revascularization at Emory, and that Dr. Halkos was lead author and researcher in several of the other studies reported upon.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
FDA’s mobile app provides real-time drug shortage information
A mobile app that provides up-to-date information on drug shortages has been launched by the Food and Drug Administration, the agency has announced.
The mobile application is “specifically designed to speed public access to valuable information about drug shortages,” namely, current and resolved drug shortages and discontinuations of drug shortages, according to the FDA statement. Clinicians and others can search by a drug’s generic name, active ingredient, or therapeutic category, and also can use the app to report a drug shortage or a supply issue to the FDA.
The app “is an innovative tool that will offer easier and faster access to important drug shortage information,” Capt. Valerie Jensen, R.Ph., associate director of the drug shortages program in the FDA’s Center for Drug Evaluation and Research, said in the statement. “The FDA understands that health care professionals and pharmacists need real-time information about drug shortages to make treatment decisions,” she added.
The app is free and can be downloaded via iTunes for Apple devices and the Google Play store for Android devices, searching for “FDA Drug Shortages.”
More information on drug shortages is available on the FDA’s web site at http://www.accessdata.fda.gov/scripts/drugshortages/default.cfm.
A mobile app that provides up-to-date information on drug shortages has been launched by the Food and Drug Administration, the agency has announced.
The mobile application is “specifically designed to speed public access to valuable information about drug shortages,” namely, current and resolved drug shortages and discontinuations of drug shortages, according to the FDA statement. Clinicians and others can search by a drug’s generic name, active ingredient, or therapeutic category, and also can use the app to report a drug shortage or a supply issue to the FDA.
The app “is an innovative tool that will offer easier and faster access to important drug shortage information,” Capt. Valerie Jensen, R.Ph., associate director of the drug shortages program in the FDA’s Center for Drug Evaluation and Research, said in the statement. “The FDA understands that health care professionals and pharmacists need real-time information about drug shortages to make treatment decisions,” she added.
The app is free and can be downloaded via iTunes for Apple devices and the Google Play store for Android devices, searching for “FDA Drug Shortages.”
More information on drug shortages is available on the FDA’s web site at http://www.accessdata.fda.gov/scripts/drugshortages/default.cfm.
A mobile app that provides up-to-date information on drug shortages has been launched by the Food and Drug Administration, the agency has announced.
The mobile application is “specifically designed to speed public access to valuable information about drug shortages,” namely, current and resolved drug shortages and discontinuations of drug shortages, according to the FDA statement. Clinicians and others can search by a drug’s generic name, active ingredient, or therapeutic category, and also can use the app to report a drug shortage or a supply issue to the FDA.
The app “is an innovative tool that will offer easier and faster access to important drug shortage information,” Capt. Valerie Jensen, R.Ph., associate director of the drug shortages program in the FDA’s Center for Drug Evaluation and Research, said in the statement. “The FDA understands that health care professionals and pharmacists need real-time information about drug shortages to make treatment decisions,” she added.
The app is free and can be downloaded via iTunes for Apple devices and the Google Play store for Android devices, searching for “FDA Drug Shortages.”
More information on drug shortages is available on the FDA’s web site at http://www.accessdata.fda.gov/scripts/drugshortages/default.cfm.
FROM THE FDA
Studies of anesthesia’s effect on upper airway are limited
CORONADO, CALIF. – Studies of the most appropriate anesthetic agents for drug-induced sleep endoscopy are limited, but according to the best available evidence, local anesthetics appear to affect airway reflexes while inhalation anesthetics and opioids exaggerate dynamic airway collapse, so they may not be ideal.
Those are key conclusions from a systematic review of literature on the effects of commonly used anesthetic agents and opioids on the upper airway presented at the Triological Society’s Combined Sections meeting. Drug-induced sleep endoscopy (DISE) “is a great tool to assess upper airway dynamics in order to determine optimal surgical therapy for obstructive sleep apnea,” said Dr. Zarmina Ehsan, a pediatric pulmonary medicine fellow at Cincinnati Children’s Hospital Medical Center. “There’s a lack of understanding regarding how upper airway dynamics are altered by anesthetic agents, compared with normal sleep. This is important because this hinders the development of universal guidelines and protocols for the use of DISE.”
Using PubMed, EMBASE, and other sources, she and her associates conducted a qualitative systematic review of studies related to common anesthetic agents and opioids in the medical literature through September 2014. To be eligible for inclusion, a study must have evaluated the agent’s effect on the upper airway, must have contained an abstract, and must have been published in English. Studies with fewer than seven subjects, no original data, review articles, and those involving animals were excluded. The researchers reviewed 180 abstracts and included 56 full text articles in the final analysis, for a total study population of 8,540 patients. At the meeting Dr. Ehsan summarized the following findings by agent:
• Lidocaine. This agent is safe for topical use, has a rapid onset of action, and an intermediate duration of efficacy. Lidocaine acts on muscles “which are potent dilators and tensors of the pharyngeal and laryngeal structures,” she said. Of 10 studies included in the analysis, 7 assessed the impact of lidocaine on upper airway obstruction. Of these, three showed increased airway obstruction while four showed no significant effects. There were two studies on sleep parameters with conflicting results: One showed an increase in mean apnea duration with lidocaine use while the other did not. From this the researchers concluded that lidocaine does affect upper airway dynamics.
• Propofol. This lipophilic intravenous agent has a quick onset of action and acts by global central nervous system depression. Of 12 studies included in the analysis, 4 examined dose-response characteristics and showed a dose-dependent decrease in airway cross-sectional area with increased dosing of propofol. “So increasing your dose makes airway obstruction more likely,” Dr. Ehsan said. “The levels of obstruction were greatest at the base of tongue, and the closure was primarily in the anterior-posterior direction.” Three studies found that propofol caused a decrease in genioglossus electromyogram activity, while the remaining five studies assessed heterogeneous outcomes. “Overall, the studies showed that propofol had a dose-dependent effect on the upper airway with increasing doses making airway obstruction more likely,” she said.
• Dexmedetomidine (DEX). This agent is an alpha-2 adrenergic agonist with sedative, anxiolytic, and analgesic effects. It’s typically given as a 10-minute loading dose followed by a continuous infusion, and is recommended when you want to preserve spontaneous respiration. Of the four DEX-related studies that were included in the analysis, all demonstrated a minimal effect on upper airway cross-sectional area. “One of the studies looked at sleep parameters and concluded that DEX does approximate non-REM sleep without causing respiratory depression,” Dr. Ehsan added. “So overall, DEX was less likely to result in upper airway obstruction, compared with propofol.”
• Midazolam. This agent is commonly used for procedural sedation, with an onset of action within 1-3 minutes and a duration of 15-60 minutes. Of the six studies involving midazolam, two evaluated sleep staging. One reported lack of REM sleep and increased duration of stage N3 sleep, while the other study found that all sleep stages were observed at a lower dosage. The remaining four studies had heterogeneous outcomes. This led the researchers to conclude that midazolam “may lead to upper airway obstruction,” Dr. Ehsan said. “It’s unclear if this is dose dependent.”
• Pentobarbital. Of the two studies involving this short-acting barbiturate, one showed no effect on pharyngeal critical pressure or respiratory muscle function, while the other found that pentobarbital can increase the upper airway cross-sectional area. “So the effect of pentobarbital is unclear,” she said.
• Ketamine. This N-methyl-D-aspartate receptor has a rapid onset and a minimal effect on the central respiratory drive. Of the three studies involving ketamine, one found a 10% incidence of transient laryngospasm, one found that the incidence of transient laryngospasm was higher when it was delivered intramuscularly vs. intravenously, and one found that ketamine was safe in infants undergoing upper airway endoscopy. The researchers concluded that overall, ketamine “could be useful during DISE.”
• Inhalation anesthetics. There were 11 studies of these agents. Of these, six found that inhalation anesthetics caused upper airway collapse while five had heterogeneous outcomes. “Overall, a majority of studies found that inhalation anesthetics exaggerate dynamic airway collapse,” Dr. Ehsan said.
• Opioids. Of the nine studies involving these agents, six found that opioids caused upper airway obstruction; two found that they caused depression of upper airway reflexes, and one found that they caused a decrease in respiratory compliance. “Overall, opioids increase upper airway obstruction,” she said.
Dr. Ehsan acknowledged certain limitations of the analysis, including the fact that there was little information on sleep state approximated by many of these agents, “which makes it difficult to determine the ideal anesthetic protocol. There was substantial heterogeneity in outcomes, and few prospective studies comparing the ability of anesthetics to approximate natural sleep.” She recommended that future efforts focus on comparative effectiveness studies between the agents, as well as evaluate the impact of combining anesthetic agents. “This is important, because most DISE protocols use a combination of agents,” she said.
The meeting was jointly sponsored by the Triological Society and the American College of Surgeons
Dr. Ehsan reported having no relevant financial conflicts.
On Twitter @dougbrunk
CORONADO, CALIF. – Studies of the most appropriate anesthetic agents for drug-induced sleep endoscopy are limited, but according to the best available evidence, local anesthetics appear to affect airway reflexes while inhalation anesthetics and opioids exaggerate dynamic airway collapse, so they may not be ideal.
Those are key conclusions from a systematic review of literature on the effects of commonly used anesthetic agents and opioids on the upper airway presented at the Triological Society’s Combined Sections meeting. Drug-induced sleep endoscopy (DISE) “is a great tool to assess upper airway dynamics in order to determine optimal surgical therapy for obstructive sleep apnea,” said Dr. Zarmina Ehsan, a pediatric pulmonary medicine fellow at Cincinnati Children’s Hospital Medical Center. “There’s a lack of understanding regarding how upper airway dynamics are altered by anesthetic agents, compared with normal sleep. This is important because this hinders the development of universal guidelines and protocols for the use of DISE.”
Using PubMed, EMBASE, and other sources, she and her associates conducted a qualitative systematic review of studies related to common anesthetic agents and opioids in the medical literature through September 2014. To be eligible for inclusion, a study must have evaluated the agent’s effect on the upper airway, must have contained an abstract, and must have been published in English. Studies with fewer than seven subjects, no original data, review articles, and those involving animals were excluded. The researchers reviewed 180 abstracts and included 56 full text articles in the final analysis, for a total study population of 8,540 patients. At the meeting Dr. Ehsan summarized the following findings by agent:
• Lidocaine. This agent is safe for topical use, has a rapid onset of action, and an intermediate duration of efficacy. Lidocaine acts on muscles “which are potent dilators and tensors of the pharyngeal and laryngeal structures,” she said. Of 10 studies included in the analysis, 7 assessed the impact of lidocaine on upper airway obstruction. Of these, three showed increased airway obstruction while four showed no significant effects. There were two studies on sleep parameters with conflicting results: One showed an increase in mean apnea duration with lidocaine use while the other did not. From this the researchers concluded that lidocaine does affect upper airway dynamics.
• Propofol. This lipophilic intravenous agent has a quick onset of action and acts by global central nervous system depression. Of 12 studies included in the analysis, 4 examined dose-response characteristics and showed a dose-dependent decrease in airway cross-sectional area with increased dosing of propofol. “So increasing your dose makes airway obstruction more likely,” Dr. Ehsan said. “The levels of obstruction were greatest at the base of tongue, and the closure was primarily in the anterior-posterior direction.” Three studies found that propofol caused a decrease in genioglossus electromyogram activity, while the remaining five studies assessed heterogeneous outcomes. “Overall, the studies showed that propofol had a dose-dependent effect on the upper airway with increasing doses making airway obstruction more likely,” she said.
• Dexmedetomidine (DEX). This agent is an alpha-2 adrenergic agonist with sedative, anxiolytic, and analgesic effects. It’s typically given as a 10-minute loading dose followed by a continuous infusion, and is recommended when you want to preserve spontaneous respiration. Of the four DEX-related studies that were included in the analysis, all demonstrated a minimal effect on upper airway cross-sectional area. “One of the studies looked at sleep parameters and concluded that DEX does approximate non-REM sleep without causing respiratory depression,” Dr. Ehsan added. “So overall, DEX was less likely to result in upper airway obstruction, compared with propofol.”
• Midazolam. This agent is commonly used for procedural sedation, with an onset of action within 1-3 minutes and a duration of 15-60 minutes. Of the six studies involving midazolam, two evaluated sleep staging. One reported lack of REM sleep and increased duration of stage N3 sleep, while the other study found that all sleep stages were observed at a lower dosage. The remaining four studies had heterogeneous outcomes. This led the researchers to conclude that midazolam “may lead to upper airway obstruction,” Dr. Ehsan said. “It’s unclear if this is dose dependent.”
• Pentobarbital. Of the two studies involving this short-acting barbiturate, one showed no effect on pharyngeal critical pressure or respiratory muscle function, while the other found that pentobarbital can increase the upper airway cross-sectional area. “So the effect of pentobarbital is unclear,” she said.
• Ketamine. This N-methyl-D-aspartate receptor has a rapid onset and a minimal effect on the central respiratory drive. Of the three studies involving ketamine, one found a 10% incidence of transient laryngospasm, one found that the incidence of transient laryngospasm was higher when it was delivered intramuscularly vs. intravenously, and one found that ketamine was safe in infants undergoing upper airway endoscopy. The researchers concluded that overall, ketamine “could be useful during DISE.”
• Inhalation anesthetics. There were 11 studies of these agents. Of these, six found that inhalation anesthetics caused upper airway collapse while five had heterogeneous outcomes. “Overall, a majority of studies found that inhalation anesthetics exaggerate dynamic airway collapse,” Dr. Ehsan said.
• Opioids. Of the nine studies involving these agents, six found that opioids caused upper airway obstruction; two found that they caused depression of upper airway reflexes, and one found that they caused a decrease in respiratory compliance. “Overall, opioids increase upper airway obstruction,” she said.
Dr. Ehsan acknowledged certain limitations of the analysis, including the fact that there was little information on sleep state approximated by many of these agents, “which makes it difficult to determine the ideal anesthetic protocol. There was substantial heterogeneity in outcomes, and few prospective studies comparing the ability of anesthetics to approximate natural sleep.” She recommended that future efforts focus on comparative effectiveness studies between the agents, as well as evaluate the impact of combining anesthetic agents. “This is important, because most DISE protocols use a combination of agents,” she said.
The meeting was jointly sponsored by the Triological Society and the American College of Surgeons
Dr. Ehsan reported having no relevant financial conflicts.
On Twitter @dougbrunk
CORONADO, CALIF. – Studies of the most appropriate anesthetic agents for drug-induced sleep endoscopy are limited, but according to the best available evidence, local anesthetics appear to affect airway reflexes while inhalation anesthetics and opioids exaggerate dynamic airway collapse, so they may not be ideal.
Those are key conclusions from a systematic review of literature on the effects of commonly used anesthetic agents and opioids on the upper airway presented at the Triological Society’s Combined Sections meeting. Drug-induced sleep endoscopy (DISE) “is a great tool to assess upper airway dynamics in order to determine optimal surgical therapy for obstructive sleep apnea,” said Dr. Zarmina Ehsan, a pediatric pulmonary medicine fellow at Cincinnati Children’s Hospital Medical Center. “There’s a lack of understanding regarding how upper airway dynamics are altered by anesthetic agents, compared with normal sleep. This is important because this hinders the development of universal guidelines and protocols for the use of DISE.”
Using PubMed, EMBASE, and other sources, she and her associates conducted a qualitative systematic review of studies related to common anesthetic agents and opioids in the medical literature through September 2014. To be eligible for inclusion, a study must have evaluated the agent’s effect on the upper airway, must have contained an abstract, and must have been published in English. Studies with fewer than seven subjects, no original data, review articles, and those involving animals were excluded. The researchers reviewed 180 abstracts and included 56 full text articles in the final analysis, for a total study population of 8,540 patients. At the meeting Dr. Ehsan summarized the following findings by agent:
• Lidocaine. This agent is safe for topical use, has a rapid onset of action, and an intermediate duration of efficacy. Lidocaine acts on muscles “which are potent dilators and tensors of the pharyngeal and laryngeal structures,” she said. Of 10 studies included in the analysis, 7 assessed the impact of lidocaine on upper airway obstruction. Of these, three showed increased airway obstruction while four showed no significant effects. There were two studies on sleep parameters with conflicting results: One showed an increase in mean apnea duration with lidocaine use while the other did not. From this the researchers concluded that lidocaine does affect upper airway dynamics.
• Propofol. This lipophilic intravenous agent has a quick onset of action and acts by global central nervous system depression. Of 12 studies included in the analysis, 4 examined dose-response characteristics and showed a dose-dependent decrease in airway cross-sectional area with increased dosing of propofol. “So increasing your dose makes airway obstruction more likely,” Dr. Ehsan said. “The levels of obstruction were greatest at the base of tongue, and the closure was primarily in the anterior-posterior direction.” Three studies found that propofol caused a decrease in genioglossus electromyogram activity, while the remaining five studies assessed heterogeneous outcomes. “Overall, the studies showed that propofol had a dose-dependent effect on the upper airway with increasing doses making airway obstruction more likely,” she said.
• Dexmedetomidine (DEX). This agent is an alpha-2 adrenergic agonist with sedative, anxiolytic, and analgesic effects. It’s typically given as a 10-minute loading dose followed by a continuous infusion, and is recommended when you want to preserve spontaneous respiration. Of the four DEX-related studies that were included in the analysis, all demonstrated a minimal effect on upper airway cross-sectional area. “One of the studies looked at sleep parameters and concluded that DEX does approximate non-REM sleep without causing respiratory depression,” Dr. Ehsan added. “So overall, DEX was less likely to result in upper airway obstruction, compared with propofol.”
• Midazolam. This agent is commonly used for procedural sedation, with an onset of action within 1-3 minutes and a duration of 15-60 minutes. Of the six studies involving midazolam, two evaluated sleep staging. One reported lack of REM sleep and increased duration of stage N3 sleep, while the other study found that all sleep stages were observed at a lower dosage. The remaining four studies had heterogeneous outcomes. This led the researchers to conclude that midazolam “may lead to upper airway obstruction,” Dr. Ehsan said. “It’s unclear if this is dose dependent.”
• Pentobarbital. Of the two studies involving this short-acting barbiturate, one showed no effect on pharyngeal critical pressure or respiratory muscle function, while the other found that pentobarbital can increase the upper airway cross-sectional area. “So the effect of pentobarbital is unclear,” she said.
• Ketamine. This N-methyl-D-aspartate receptor has a rapid onset and a minimal effect on the central respiratory drive. Of the three studies involving ketamine, one found a 10% incidence of transient laryngospasm, one found that the incidence of transient laryngospasm was higher when it was delivered intramuscularly vs. intravenously, and one found that ketamine was safe in infants undergoing upper airway endoscopy. The researchers concluded that overall, ketamine “could be useful during DISE.”
• Inhalation anesthetics. There were 11 studies of these agents. Of these, six found that inhalation anesthetics caused upper airway collapse while five had heterogeneous outcomes. “Overall, a majority of studies found that inhalation anesthetics exaggerate dynamic airway collapse,” Dr. Ehsan said.
• Opioids. Of the nine studies involving these agents, six found that opioids caused upper airway obstruction; two found that they caused depression of upper airway reflexes, and one found that they caused a decrease in respiratory compliance. “Overall, opioids increase upper airway obstruction,” she said.
Dr. Ehsan acknowledged certain limitations of the analysis, including the fact that there was little information on sleep state approximated by many of these agents, “which makes it difficult to determine the ideal anesthetic protocol. There was substantial heterogeneity in outcomes, and few prospective studies comparing the ability of anesthetics to approximate natural sleep.” She recommended that future efforts focus on comparative effectiveness studies between the agents, as well as evaluate the impact of combining anesthetic agents. “This is important, because most DISE protocols use a combination of agents,” she said.
The meeting was jointly sponsored by the Triological Society and the American College of Surgeons
Dr. Ehsan reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT THE COMBINED SECTIONS WINTER MEETING
Key clinical point: Choice of an appropriate anesthetic protocol for drug-induced sleep endoscopy must be based on a limited number of comparative studies.
Major finding: Local anesthetics appear to affect upper airway reflexes while inhalation anesthetics and opioids exaggerate dynamic airway collapse.
Data source: A qualitative systematic review of 56 studies related to common anesthetic agents and opioids published in the medical literature through September 2014.
Disclosures: Dr. Ehsan reported having no financial disclosures.