User login
Official Newspaper of the American College of Surgeons
Value-based payment: Time to start getting ready
WASHINGTON– Are physicians ready for the shift toward value-based compensation?
A report from the American Medical Association and the RAND Corporation aims to get physicians thinking about what investments they should expect to make and what obstacles they may encounter as they prepare for the federal government’s switch from fee-for-service to value-based medicine in 2018.
“There is a lot of enthusiasm for change,” Dr. Mark W. Friedberg, senior natural scientist at RAND in Boston and lead researcher on the report, said in an interview. “There is a lot of hope this will result in better patient care and physician success. It’s a matter of the details.”
The report is based on survey data from 34 practices across the country, all of which have some form of alternative payment structure in place, whether it be accountable care or bundled services. Practices were located in rural and urban settings ranging from hospital- to physician-owned or corporately managed, all with varying sizes of patient panels.
The top concern that practice managers faced was matching the appropriate alternative payment model to their particular patient population, researchers found. Other concerns included how best to use incentives without adversely affecting patient care and how to avoid physician burn-out.
These concerns, Dr. Friedberg said, point to a need for payers to offer guidance about what makes sense when and why. “We got the message that more communication between payers and physician practices tends to be a good thing.”
Many of the coming changes will require updated technology. Finding the money for such an overhaul is a universal preoccupation of many practice managers, and another reason some practices have yet to switch. “Some of the time, practices can get a loan, or have the reserves to do it on their own, but sometimes they don’t and they need to partner with a large organization like a hospital or a large physician group,” Dr. Friedberg said.
Payers are not likely to help foot the bill, according to Susan DeVore, president and chief executive officer of Premier Health, a performance improvement alliance of hospitals and other providers.
“It would be wonderful if the health plans would spend hundreds of millions of dollars for the technology enablement of the physician practices and the health systems,” Ms. DeVore said at the press conference. “The truth is, health systems and physicians are [already] spending the billions to build these technology infrastructures, and they need to do that together.”
She called for more systemwide transparent collaboration in how cost is determined and in how quality and outcomes are measured. “It’s not fair to say we need a coordinated system of care, but then we can’t do it for lots of regulatory reasons,” she said noting that ultimately, she believed such information sharing would be determined by Congress.
Payers, should, however, make sure that physicians and other providers have a seat at the table when performance metrics are determined, Dr. Friedberg said.
“Some of the concerns we heard were that, in addition to the number of measures, was also whether individual measures are clinically valid, and do they really reflect true differences in the quality of the patient care. Is it possible that the measure isn’t really reliable and not adequately risk adjusted, and therefore might not be ready for prime time in a payment contract?”
Although the report did not offer specific time frames practice managers could expect before a new structure would take hold, Ms. DeVore said she was aware of some practices that realized more than a third more profits within 3 years of switching to value-based care models.
Chet Burrell, president and CEO of CareFirst BlueCross BlueShield, said his group’s experience was that overall, physicians were not ready for the change to value-based care. This, despite the insurer’s announcement that $1 in every $5 it spends on reimbursement is now tied to quality care.
For physicians who are ready to make the shift to value-based payment, Mr. Burrell said an average of 5 years was necessary to fully integrate. “Each practice is its own ecosystem. Some physicians catch on very quickly, but some are hostile.”
On Twitter @whitneymcknight
WASHINGTON– Are physicians ready for the shift toward value-based compensation?
A report from the American Medical Association and the RAND Corporation aims to get physicians thinking about what investments they should expect to make and what obstacles they may encounter as they prepare for the federal government’s switch from fee-for-service to value-based medicine in 2018.
“There is a lot of enthusiasm for change,” Dr. Mark W. Friedberg, senior natural scientist at RAND in Boston and lead researcher on the report, said in an interview. “There is a lot of hope this will result in better patient care and physician success. It’s a matter of the details.”
The report is based on survey data from 34 practices across the country, all of which have some form of alternative payment structure in place, whether it be accountable care or bundled services. Practices were located in rural and urban settings ranging from hospital- to physician-owned or corporately managed, all with varying sizes of patient panels.
The top concern that practice managers faced was matching the appropriate alternative payment model to their particular patient population, researchers found. Other concerns included how best to use incentives without adversely affecting patient care and how to avoid physician burn-out.
These concerns, Dr. Friedberg said, point to a need for payers to offer guidance about what makes sense when and why. “We got the message that more communication between payers and physician practices tends to be a good thing.”
Many of the coming changes will require updated technology. Finding the money for such an overhaul is a universal preoccupation of many practice managers, and another reason some practices have yet to switch. “Some of the time, practices can get a loan, or have the reserves to do it on their own, but sometimes they don’t and they need to partner with a large organization like a hospital or a large physician group,” Dr. Friedberg said.
Payers are not likely to help foot the bill, according to Susan DeVore, president and chief executive officer of Premier Health, a performance improvement alliance of hospitals and other providers.
“It would be wonderful if the health plans would spend hundreds of millions of dollars for the technology enablement of the physician practices and the health systems,” Ms. DeVore said at the press conference. “The truth is, health systems and physicians are [already] spending the billions to build these technology infrastructures, and they need to do that together.”
She called for more systemwide transparent collaboration in how cost is determined and in how quality and outcomes are measured. “It’s not fair to say we need a coordinated system of care, but then we can’t do it for lots of regulatory reasons,” she said noting that ultimately, she believed such information sharing would be determined by Congress.
Payers, should, however, make sure that physicians and other providers have a seat at the table when performance metrics are determined, Dr. Friedberg said.
“Some of the concerns we heard were that, in addition to the number of measures, was also whether individual measures are clinically valid, and do they really reflect true differences in the quality of the patient care. Is it possible that the measure isn’t really reliable and not adequately risk adjusted, and therefore might not be ready for prime time in a payment contract?”
Although the report did not offer specific time frames practice managers could expect before a new structure would take hold, Ms. DeVore said she was aware of some practices that realized more than a third more profits within 3 years of switching to value-based care models.
Chet Burrell, president and CEO of CareFirst BlueCross BlueShield, said his group’s experience was that overall, physicians were not ready for the change to value-based care. This, despite the insurer’s announcement that $1 in every $5 it spends on reimbursement is now tied to quality care.
For physicians who are ready to make the shift to value-based payment, Mr. Burrell said an average of 5 years was necessary to fully integrate. “Each practice is its own ecosystem. Some physicians catch on very quickly, but some are hostile.”
On Twitter @whitneymcknight
WASHINGTON– Are physicians ready for the shift toward value-based compensation?
A report from the American Medical Association and the RAND Corporation aims to get physicians thinking about what investments they should expect to make and what obstacles they may encounter as they prepare for the federal government’s switch from fee-for-service to value-based medicine in 2018.
“There is a lot of enthusiasm for change,” Dr. Mark W. Friedberg, senior natural scientist at RAND in Boston and lead researcher on the report, said in an interview. “There is a lot of hope this will result in better patient care and physician success. It’s a matter of the details.”
The report is based on survey data from 34 practices across the country, all of which have some form of alternative payment structure in place, whether it be accountable care or bundled services. Practices were located in rural and urban settings ranging from hospital- to physician-owned or corporately managed, all with varying sizes of patient panels.
The top concern that practice managers faced was matching the appropriate alternative payment model to their particular patient population, researchers found. Other concerns included how best to use incentives without adversely affecting patient care and how to avoid physician burn-out.
These concerns, Dr. Friedberg said, point to a need for payers to offer guidance about what makes sense when and why. “We got the message that more communication between payers and physician practices tends to be a good thing.”
Many of the coming changes will require updated technology. Finding the money for such an overhaul is a universal preoccupation of many practice managers, and another reason some practices have yet to switch. “Some of the time, practices can get a loan, or have the reserves to do it on their own, but sometimes they don’t and they need to partner with a large organization like a hospital or a large physician group,” Dr. Friedberg said.
Payers are not likely to help foot the bill, according to Susan DeVore, president and chief executive officer of Premier Health, a performance improvement alliance of hospitals and other providers.
“It would be wonderful if the health plans would spend hundreds of millions of dollars for the technology enablement of the physician practices and the health systems,” Ms. DeVore said at the press conference. “The truth is, health systems and physicians are [already] spending the billions to build these technology infrastructures, and they need to do that together.”
She called for more systemwide transparent collaboration in how cost is determined and in how quality and outcomes are measured. “It’s not fair to say we need a coordinated system of care, but then we can’t do it for lots of regulatory reasons,” she said noting that ultimately, she believed such information sharing would be determined by Congress.
Payers, should, however, make sure that physicians and other providers have a seat at the table when performance metrics are determined, Dr. Friedberg said.
“Some of the concerns we heard were that, in addition to the number of measures, was also whether individual measures are clinically valid, and do they really reflect true differences in the quality of the patient care. Is it possible that the measure isn’t really reliable and not adequately risk adjusted, and therefore might not be ready for prime time in a payment contract?”
Although the report did not offer specific time frames practice managers could expect before a new structure would take hold, Ms. DeVore said she was aware of some practices that realized more than a third more profits within 3 years of switching to value-based care models.
Chet Burrell, president and CEO of CareFirst BlueCross BlueShield, said his group’s experience was that overall, physicians were not ready for the change to value-based care. This, despite the insurer’s announcement that $1 in every $5 it spends on reimbursement is now tied to quality care.
For physicians who are ready to make the shift to value-based payment, Mr. Burrell said an average of 5 years was necessary to fully integrate. “Each practice is its own ecosystem. Some physicians catch on very quickly, but some are hostile.”
On Twitter @whitneymcknight
AT AN AMA/RAND BRIEFING
FAQ: What’s in the House proposal to fix the SGR?
It’s make-or-break time for a Medicare “doc fix” replacement.
The House is likely to vote the week of March 23 on a proposal to scrap Medicare’s troubled physician payment formula, just days before a March 31 deadline when doctors who treat Medicare patients will see a 21% payment cut. Senate action could come this week as well, but probably not until the chamber completes a lengthy series of votes on the GOP’s fiscal 2016 budget package.
After negotiating behind closed doors for more than a week, Republican and Democratic leaders of two key House committees that handle Medicare unveiled details of the package late Friday. According to a summary of the deal, the current system would be scrapped and replaced with payment increases for doctors for the next 5 years as Medicare transitions to a new system focused “on quality, value and accountability.”
There’s enough in the wide-ranging deal for both sides to love or hate.
Senate Democrats have pressed to add to the proposal 4 years of funding for an unrelated program, the Children’s Health Insurance Program (CHIP). The House package extends CHIP for 2 years. In a statement Saturday, Senate Finance Democrats said they were “united by the necessity of extending CHIP funding for another 4 years.”
Their statement also signaled other potential problems for the package in the Senate, including concerns about asking Medicare beneficiaries to pay for more of their medical care, the impact of the package on women’s health services, and cuts to Medicare providers.
Still, some Democratic allies said the CHIP disagreement should not undermine the proposal. Shortly after the package was unveiled Friday, Ron Pollack, executive director of the consumers group Families USA, said in a statement that “while we would have preferred a 4-year extension, the House bill has our full support.”
Some GOP conservatives and Democrats will balk that the package isn’t fully paid for, with policy changes governing Medicare beneficiaries and providers paying for only about $70 billion of the approximately $200 billion package.
For doctors, the package offers an end to a familiar but frustrating rite. Lawmakers have invariably deferred the cuts prescribed by a 1997 reimbursement formula, which everyone agrees is broken beyond repair. But the deferrals have always been temporary because Congress has not agreed to offsetting cuts to pay for a permanent fix. In 2010, Congress delayed scheduled cuts five times. In a statement Sunday, the American Medical Association urged Congress “to seize the moment” to enact the changes.
Here are some answers to frequently asked questions about the proposal and the congressional ritual known as the doc fix.
Q: What are the options that Congress is looking at?
The House package would scrap the Sustainable Growth Rate (SGR) formula and give doctors a 0.5% bump for each of the next 5 years as Medicare transitions to a payment system designed to reward physicians based on the quality of care provided, rather than the quantity of procedures performed, as the current payment formula does.
The measure, which builds upon last year’s legislation from the House Energy and Commerce and Ways and Means Committees and the Senate Finance Committee, would encourage better care coordination and chronic care management, ideas that experts have said are needed in the Medicare program. It would give a 5% payment bonus to providers who receive a “significant portion” of their revenue from an “alternative payment model” or patient-centered medical home. It would also allow broader use of Medicare data for “transparency and quality improvement” purposes.
“The SGR has generated repeated crises for nearly 2 decades,” Energy and Commerce Committee Chairman Fred Upton (R-Mich.), one of the bill’s drafters, said in a statement. “We have a historic opportunity to finally move to a system that promotes quality over quantity and begins the important work of addressing Medicare’s structural issues.”
The package, which House Speaker John Boehner (R-Ohio) and Minority Leader Nancy Pelosi (D-Calif.) began negotiating weeks ago, also includes an additional $7.2 billion for community health centers over the next 2 years. NARAL Pro-Choice America denounced the deal because the health center funding would be subject to the Hyde Amendment, a common legislative provision that says federal money can be used for abortions only when a pregnancy is the result of rape, incest, or to save the life of the mother.
In a letter to Democratic colleagues, Rep. Pelosi said the funding would occur “under the same terms that Members have previously supported and voted on almost every year since 1979.” In a statement, the National Association of Community Health Centers said the proposal “represents no change in current policy for Health Centers, and would not change anything about how Health Centers operate today.”
The “working summary” of the House plan says the package also includes other health measures – known as extenders – that Congress has renewed each year during the SGR debate. The list includes funding for therapy services, ambulance services, and rural hospitals, as well as for continuing a program that allows low-income people to keep their Medicaid coverage as they transition into employment and earn more money. The deal also would permanently extend the Qualifying Individual, or QI, program, which helps low-income seniors pay their Medicare premiums.
Q. What is the plan for CHIP?
The House plan would add 2 years of funding for CHIP, a federal-state program that provides insurance for low-income children whose families earned too much money to qualify for Medicaid. While the health law continues CHIP authorization through 2019, funding for the program has not been extended beyond the end of September.
The length of the proposed extension could cause strains with Senate Democrats beyond those on the Finance panel who have raised objections to the House package. Last month, the Senate Democratic caucus signed on to legislation from Sen. Sherrod Brown (D-Ohio) calling for a 4-year extension of the current CHIP program.
Q: How would Congress pay for all of that?
It might not. That would be a major departure from the GOP’s mantra that all legislation must be financed. Tired of the yearly SGR battle, veteran members in both chambers may be willing to repeal the SGR on the basis that it’s a budget gimmick – the cuts are never made – and therefore financing is unnecessary. But that strategy could run into stiff opposition from Republican lawmakers and some Democrats
Most lawmakers are expected to feel the need to find financing for the Medicare extenders, the CHIP extension, and any increase in physician payments over the current pay schedule. Those items would account for about $70 billion of financing in an approximately $200 billion package.
Conservative groups are urging Republicans to fully finance any SGR repeal. “Americans didn’t hand Republicans a historic House majority to engage in more deficit spending and budget gimmickry,” Dan Holler, communications director of Heritage Action for America, said earlier this month.
Q. Will seniors and Medicare providers have to help pay for the plan?
Starting in 2018, wealthier Medicare beneficiaries (individuals with incomes between $133,500 and $214,000, with thresholds likely higher for couples) would pay more for their Medicare coverage, a provision impacting just 2% of beneficiaries, according to the summary.
Starting in 2020, “first-dollar” supplemental Medicare insurance known as “Medigap” would not be able to cover the Part B deductible for new beneficiaries, which is currently $147 per year but has increased in past years.
But the effect of that change may be mitigated, according to one analysis.
“Because Medigap policies would no longer pay the Part B deductible, Medigap premiums for the affected policies would go down. Most affected beneficiaries would come out ahead – the drop in their Medigap premiums would exceed the increase in their cost sharing for health services,” according to an analysis from the Center on Budget and Policy Priorities, a left-leaning think tank. “Some others would come out behind. In both cases, the effect would be small – generally no more than $100 a year.”
Experts contend that the “first-dollar” plans, which cover nearly all deductibles and copayments, keep beneficiaries from being judicious when making medical decisions. According to lobbyists and aides, an earlier version of the doc fix legislation that negotiators considered would have prohibited first-dollar plans from covering the first $250 in costs for new beneficiaries.
Postacute providers, such as long-term care and inpatient rehabilitation hospitals, skilled nursing facilities, and home health and hospice organizations, would help finance the repeal, receiving base pay increases of 1% in 2018, about half of what was previously expected.
Other changes include phasing in a one-time 3.2 percentage-point boost in the base payment rate for hospitals currently scheduled to take effect in fiscal 2018. The number of years of the phase-in isn’t specified in the bill summary.
Scheduled reductions in Medicaid “disproportionate share” payments to hospitals that care for large numbers of people who are uninsured or covered by Medicaid would be delayed by 1 year to fiscal 2018 but extended for an additional year to fiscal 2025.
Q. How quickly could Congress act?
Legislation to repeal the SGR is expected to move in the House this week. The House is scheduled to begin a 2-week recess March 27.
Senate Democrats and Republicans may want to offer amendments to the emerging House package, which could mean that the chamber does not resolve the SGR issue before the Senate’s 2-week break, which is scheduled to begin starting March 30.
If the SGR issue can’t be resolved by March 31, Congress could pass a temporary patch as negotiations continue or ask the Centers for Medicare & Medicaid Services, which oversees Medicare, to hold the claims in order to avoid physicians seeing their payments cut 21%.
This article is adapted from content created by and first published by Kaiser Health News (KHN), a nonprofit national health policy news service.
It’s make-or-break time for a Medicare “doc fix” replacement.
The House is likely to vote the week of March 23 on a proposal to scrap Medicare’s troubled physician payment formula, just days before a March 31 deadline when doctors who treat Medicare patients will see a 21% payment cut. Senate action could come this week as well, but probably not until the chamber completes a lengthy series of votes on the GOP’s fiscal 2016 budget package.
After negotiating behind closed doors for more than a week, Republican and Democratic leaders of two key House committees that handle Medicare unveiled details of the package late Friday. According to a summary of the deal, the current system would be scrapped and replaced with payment increases for doctors for the next 5 years as Medicare transitions to a new system focused “on quality, value and accountability.”
There’s enough in the wide-ranging deal for both sides to love or hate.
Senate Democrats have pressed to add to the proposal 4 years of funding for an unrelated program, the Children’s Health Insurance Program (CHIP). The House package extends CHIP for 2 years. In a statement Saturday, Senate Finance Democrats said they were “united by the necessity of extending CHIP funding for another 4 years.”
Their statement also signaled other potential problems for the package in the Senate, including concerns about asking Medicare beneficiaries to pay for more of their medical care, the impact of the package on women’s health services, and cuts to Medicare providers.
Still, some Democratic allies said the CHIP disagreement should not undermine the proposal. Shortly after the package was unveiled Friday, Ron Pollack, executive director of the consumers group Families USA, said in a statement that “while we would have preferred a 4-year extension, the House bill has our full support.”
Some GOP conservatives and Democrats will balk that the package isn’t fully paid for, with policy changes governing Medicare beneficiaries and providers paying for only about $70 billion of the approximately $200 billion package.
For doctors, the package offers an end to a familiar but frustrating rite. Lawmakers have invariably deferred the cuts prescribed by a 1997 reimbursement formula, which everyone agrees is broken beyond repair. But the deferrals have always been temporary because Congress has not agreed to offsetting cuts to pay for a permanent fix. In 2010, Congress delayed scheduled cuts five times. In a statement Sunday, the American Medical Association urged Congress “to seize the moment” to enact the changes.
Here are some answers to frequently asked questions about the proposal and the congressional ritual known as the doc fix.
Q: What are the options that Congress is looking at?
The House package would scrap the Sustainable Growth Rate (SGR) formula and give doctors a 0.5% bump for each of the next 5 years as Medicare transitions to a payment system designed to reward physicians based on the quality of care provided, rather than the quantity of procedures performed, as the current payment formula does.
The measure, which builds upon last year’s legislation from the House Energy and Commerce and Ways and Means Committees and the Senate Finance Committee, would encourage better care coordination and chronic care management, ideas that experts have said are needed in the Medicare program. It would give a 5% payment bonus to providers who receive a “significant portion” of their revenue from an “alternative payment model” or patient-centered medical home. It would also allow broader use of Medicare data for “transparency and quality improvement” purposes.
“The SGR has generated repeated crises for nearly 2 decades,” Energy and Commerce Committee Chairman Fred Upton (R-Mich.), one of the bill’s drafters, said in a statement. “We have a historic opportunity to finally move to a system that promotes quality over quantity and begins the important work of addressing Medicare’s structural issues.”
The package, which House Speaker John Boehner (R-Ohio) and Minority Leader Nancy Pelosi (D-Calif.) began negotiating weeks ago, also includes an additional $7.2 billion for community health centers over the next 2 years. NARAL Pro-Choice America denounced the deal because the health center funding would be subject to the Hyde Amendment, a common legislative provision that says federal money can be used for abortions only when a pregnancy is the result of rape, incest, or to save the life of the mother.
In a letter to Democratic colleagues, Rep. Pelosi said the funding would occur “under the same terms that Members have previously supported and voted on almost every year since 1979.” In a statement, the National Association of Community Health Centers said the proposal “represents no change in current policy for Health Centers, and would not change anything about how Health Centers operate today.”
The “working summary” of the House plan says the package also includes other health measures – known as extenders – that Congress has renewed each year during the SGR debate. The list includes funding for therapy services, ambulance services, and rural hospitals, as well as for continuing a program that allows low-income people to keep their Medicaid coverage as they transition into employment and earn more money. The deal also would permanently extend the Qualifying Individual, or QI, program, which helps low-income seniors pay their Medicare premiums.
Q. What is the plan for CHIP?
The House plan would add 2 years of funding for CHIP, a federal-state program that provides insurance for low-income children whose families earned too much money to qualify for Medicaid. While the health law continues CHIP authorization through 2019, funding for the program has not been extended beyond the end of September.
The length of the proposed extension could cause strains with Senate Democrats beyond those on the Finance panel who have raised objections to the House package. Last month, the Senate Democratic caucus signed on to legislation from Sen. Sherrod Brown (D-Ohio) calling for a 4-year extension of the current CHIP program.
Q: How would Congress pay for all of that?
It might not. That would be a major departure from the GOP’s mantra that all legislation must be financed. Tired of the yearly SGR battle, veteran members in both chambers may be willing to repeal the SGR on the basis that it’s a budget gimmick – the cuts are never made – and therefore financing is unnecessary. But that strategy could run into stiff opposition from Republican lawmakers and some Democrats
Most lawmakers are expected to feel the need to find financing for the Medicare extenders, the CHIP extension, and any increase in physician payments over the current pay schedule. Those items would account for about $70 billion of financing in an approximately $200 billion package.
Conservative groups are urging Republicans to fully finance any SGR repeal. “Americans didn’t hand Republicans a historic House majority to engage in more deficit spending and budget gimmickry,” Dan Holler, communications director of Heritage Action for America, said earlier this month.
Q. Will seniors and Medicare providers have to help pay for the plan?
Starting in 2018, wealthier Medicare beneficiaries (individuals with incomes between $133,500 and $214,000, with thresholds likely higher for couples) would pay more for their Medicare coverage, a provision impacting just 2% of beneficiaries, according to the summary.
Starting in 2020, “first-dollar” supplemental Medicare insurance known as “Medigap” would not be able to cover the Part B deductible for new beneficiaries, which is currently $147 per year but has increased in past years.
But the effect of that change may be mitigated, according to one analysis.
“Because Medigap policies would no longer pay the Part B deductible, Medigap premiums for the affected policies would go down. Most affected beneficiaries would come out ahead – the drop in their Medigap premiums would exceed the increase in their cost sharing for health services,” according to an analysis from the Center on Budget and Policy Priorities, a left-leaning think tank. “Some others would come out behind. In both cases, the effect would be small – generally no more than $100 a year.”
Experts contend that the “first-dollar” plans, which cover nearly all deductibles and copayments, keep beneficiaries from being judicious when making medical decisions. According to lobbyists and aides, an earlier version of the doc fix legislation that negotiators considered would have prohibited first-dollar plans from covering the first $250 in costs for new beneficiaries.
Postacute providers, such as long-term care and inpatient rehabilitation hospitals, skilled nursing facilities, and home health and hospice organizations, would help finance the repeal, receiving base pay increases of 1% in 2018, about half of what was previously expected.
Other changes include phasing in a one-time 3.2 percentage-point boost in the base payment rate for hospitals currently scheduled to take effect in fiscal 2018. The number of years of the phase-in isn’t specified in the bill summary.
Scheduled reductions in Medicaid “disproportionate share” payments to hospitals that care for large numbers of people who are uninsured or covered by Medicaid would be delayed by 1 year to fiscal 2018 but extended for an additional year to fiscal 2025.
Q. How quickly could Congress act?
Legislation to repeal the SGR is expected to move in the House this week. The House is scheduled to begin a 2-week recess March 27.
Senate Democrats and Republicans may want to offer amendments to the emerging House package, which could mean that the chamber does not resolve the SGR issue before the Senate’s 2-week break, which is scheduled to begin starting March 30.
If the SGR issue can’t be resolved by March 31, Congress could pass a temporary patch as negotiations continue or ask the Centers for Medicare & Medicaid Services, which oversees Medicare, to hold the claims in order to avoid physicians seeing their payments cut 21%.
This article is adapted from content created by and first published by Kaiser Health News (KHN), a nonprofit national health policy news service.
It’s make-or-break time for a Medicare “doc fix” replacement.
The House is likely to vote the week of March 23 on a proposal to scrap Medicare’s troubled physician payment formula, just days before a March 31 deadline when doctors who treat Medicare patients will see a 21% payment cut. Senate action could come this week as well, but probably not until the chamber completes a lengthy series of votes on the GOP’s fiscal 2016 budget package.
After negotiating behind closed doors for more than a week, Republican and Democratic leaders of two key House committees that handle Medicare unveiled details of the package late Friday. According to a summary of the deal, the current system would be scrapped and replaced with payment increases for doctors for the next 5 years as Medicare transitions to a new system focused “on quality, value and accountability.”
There’s enough in the wide-ranging deal for both sides to love or hate.
Senate Democrats have pressed to add to the proposal 4 years of funding for an unrelated program, the Children’s Health Insurance Program (CHIP). The House package extends CHIP for 2 years. In a statement Saturday, Senate Finance Democrats said they were “united by the necessity of extending CHIP funding for another 4 years.”
Their statement also signaled other potential problems for the package in the Senate, including concerns about asking Medicare beneficiaries to pay for more of their medical care, the impact of the package on women’s health services, and cuts to Medicare providers.
Still, some Democratic allies said the CHIP disagreement should not undermine the proposal. Shortly after the package was unveiled Friday, Ron Pollack, executive director of the consumers group Families USA, said in a statement that “while we would have preferred a 4-year extension, the House bill has our full support.”
Some GOP conservatives and Democrats will balk that the package isn’t fully paid for, with policy changes governing Medicare beneficiaries and providers paying for only about $70 billion of the approximately $200 billion package.
For doctors, the package offers an end to a familiar but frustrating rite. Lawmakers have invariably deferred the cuts prescribed by a 1997 reimbursement formula, which everyone agrees is broken beyond repair. But the deferrals have always been temporary because Congress has not agreed to offsetting cuts to pay for a permanent fix. In 2010, Congress delayed scheduled cuts five times. In a statement Sunday, the American Medical Association urged Congress “to seize the moment” to enact the changes.
Here are some answers to frequently asked questions about the proposal and the congressional ritual known as the doc fix.
Q: What are the options that Congress is looking at?
The House package would scrap the Sustainable Growth Rate (SGR) formula and give doctors a 0.5% bump for each of the next 5 years as Medicare transitions to a payment system designed to reward physicians based on the quality of care provided, rather than the quantity of procedures performed, as the current payment formula does.
The measure, which builds upon last year’s legislation from the House Energy and Commerce and Ways and Means Committees and the Senate Finance Committee, would encourage better care coordination and chronic care management, ideas that experts have said are needed in the Medicare program. It would give a 5% payment bonus to providers who receive a “significant portion” of their revenue from an “alternative payment model” or patient-centered medical home. It would also allow broader use of Medicare data for “transparency and quality improvement” purposes.
“The SGR has generated repeated crises for nearly 2 decades,” Energy and Commerce Committee Chairman Fred Upton (R-Mich.), one of the bill’s drafters, said in a statement. “We have a historic opportunity to finally move to a system that promotes quality over quantity and begins the important work of addressing Medicare’s structural issues.”
The package, which House Speaker John Boehner (R-Ohio) and Minority Leader Nancy Pelosi (D-Calif.) began negotiating weeks ago, also includes an additional $7.2 billion for community health centers over the next 2 years. NARAL Pro-Choice America denounced the deal because the health center funding would be subject to the Hyde Amendment, a common legislative provision that says federal money can be used for abortions only when a pregnancy is the result of rape, incest, or to save the life of the mother.
In a letter to Democratic colleagues, Rep. Pelosi said the funding would occur “under the same terms that Members have previously supported and voted on almost every year since 1979.” In a statement, the National Association of Community Health Centers said the proposal “represents no change in current policy for Health Centers, and would not change anything about how Health Centers operate today.”
The “working summary” of the House plan says the package also includes other health measures – known as extenders – that Congress has renewed each year during the SGR debate. The list includes funding for therapy services, ambulance services, and rural hospitals, as well as for continuing a program that allows low-income people to keep their Medicaid coverage as they transition into employment and earn more money. The deal also would permanently extend the Qualifying Individual, or QI, program, which helps low-income seniors pay their Medicare premiums.
Q. What is the plan for CHIP?
The House plan would add 2 years of funding for CHIP, a federal-state program that provides insurance for low-income children whose families earned too much money to qualify for Medicaid. While the health law continues CHIP authorization through 2019, funding for the program has not been extended beyond the end of September.
The length of the proposed extension could cause strains with Senate Democrats beyond those on the Finance panel who have raised objections to the House package. Last month, the Senate Democratic caucus signed on to legislation from Sen. Sherrod Brown (D-Ohio) calling for a 4-year extension of the current CHIP program.
Q: How would Congress pay for all of that?
It might not. That would be a major departure from the GOP’s mantra that all legislation must be financed. Tired of the yearly SGR battle, veteran members in both chambers may be willing to repeal the SGR on the basis that it’s a budget gimmick – the cuts are never made – and therefore financing is unnecessary. But that strategy could run into stiff opposition from Republican lawmakers and some Democrats
Most lawmakers are expected to feel the need to find financing for the Medicare extenders, the CHIP extension, and any increase in physician payments over the current pay schedule. Those items would account for about $70 billion of financing in an approximately $200 billion package.
Conservative groups are urging Republicans to fully finance any SGR repeal. “Americans didn’t hand Republicans a historic House majority to engage in more deficit spending and budget gimmickry,” Dan Holler, communications director of Heritage Action for America, said earlier this month.
Q. Will seniors and Medicare providers have to help pay for the plan?
Starting in 2018, wealthier Medicare beneficiaries (individuals with incomes between $133,500 and $214,000, with thresholds likely higher for couples) would pay more for their Medicare coverage, a provision impacting just 2% of beneficiaries, according to the summary.
Starting in 2020, “first-dollar” supplemental Medicare insurance known as “Medigap” would not be able to cover the Part B deductible for new beneficiaries, which is currently $147 per year but has increased in past years.
But the effect of that change may be mitigated, according to one analysis.
“Because Medigap policies would no longer pay the Part B deductible, Medigap premiums for the affected policies would go down. Most affected beneficiaries would come out ahead – the drop in their Medigap premiums would exceed the increase in their cost sharing for health services,” according to an analysis from the Center on Budget and Policy Priorities, a left-leaning think tank. “Some others would come out behind. In both cases, the effect would be small – generally no more than $100 a year.”
Experts contend that the “first-dollar” plans, which cover nearly all deductibles and copayments, keep beneficiaries from being judicious when making medical decisions. According to lobbyists and aides, an earlier version of the doc fix legislation that negotiators considered would have prohibited first-dollar plans from covering the first $250 in costs for new beneficiaries.
Postacute providers, such as long-term care and inpatient rehabilitation hospitals, skilled nursing facilities, and home health and hospice organizations, would help finance the repeal, receiving base pay increases of 1% in 2018, about half of what was previously expected.
Other changes include phasing in a one-time 3.2 percentage-point boost in the base payment rate for hospitals currently scheduled to take effect in fiscal 2018. The number of years of the phase-in isn’t specified in the bill summary.
Scheduled reductions in Medicaid “disproportionate share” payments to hospitals that care for large numbers of people who are uninsured or covered by Medicaid would be delayed by 1 year to fiscal 2018 but extended for an additional year to fiscal 2025.
Q. How quickly could Congress act?
Legislation to repeal the SGR is expected to move in the House this week. The House is scheduled to begin a 2-week recess March 27.
Senate Democrats and Republicans may want to offer amendments to the emerging House package, which could mean that the chamber does not resolve the SGR issue before the Senate’s 2-week break, which is scheduled to begin starting March 30.
If the SGR issue can’t be resolved by March 31, Congress could pass a temporary patch as negotiations continue or ask the Centers for Medicare & Medicaid Services, which oversees Medicare, to hold the claims in order to avoid physicians seeing their payments cut 21%.
This article is adapted from content created by and first published by Kaiser Health News (KHN), a nonprofit national health policy news service.
FROM KAISER HEALTH NEWS
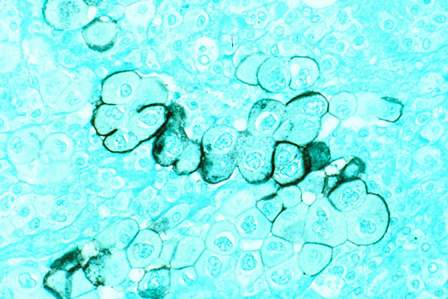
Blood urea nitrogen level and Khorana score predict early pancreatic cancer mortality
Using parameters routinely collected in patients with pancreatic cancer, the Khorana score and the blood urea nitrogen (BUN) level were significantly associated with early mortality in patients with pancreatic cancer who underwent surgical resection, according to a report published in the journal Cancer.
Dr. Davendra P.S. Sohal, an oncologist at Cleveland Clinic, and his colleagues stated that by identifying patients with resectable pancreatic adenocarcinoma who are at high risk of early mortality, the parameters “may be used to stratify patients, and ultimately may be used to select high-risk patients for more aggressive therapies in prospective studies” (Cancer 2015 [doi:10.1002/cncr.29298]).
Multivariate analysis showed the risk for early mortality (before 6 months) increased with high-risk Khorana score (hazard ratio, 2.32; 95% confidence interval, 1.04-5.13; P = .039) and elevated blood urea nitrogen (HR, 4.34; 95% CI, 1.84-10.25; P < .001). The authors noted that other key variables, such as TNM classification of malignant tumor staging, were not associated with early mortality.
The study evaluated 334 patients, median age 67 years, who underwent surgical resection of pancreatic adenocarcinoma during 2006-2013 at the Cleveland Clinic. With a median follow-up time of 39.4 months, there were 205 deaths (61%), and median overall survival was 21.3 months. Within 30 days after surgery, 3 (0.9%) deaths occurred, and within 6 months of surgery, 29 (8.7%) deaths occurred. Most tumors were located in the head of the pancreas (73%); most pathologic stages were T3 (67%) and N1 (63%); median Khorana score was 2; 47% of patients had a score ≥ 3; 59% had comorbidities. Some of the patients received preoperative anticancer therapy, making the study population heterogeneous in that respect.
The Khorana score, a measure of venous thromboembolism risk, combines five items: cancer site, platelet count > 350/nL, white blood cell count > 11/nL, hemoglobin <100 g/L, and body mass index (BMI) ≥ 35 kg/m2; Khorana scores of 3 or greater indicate high risk.
A novel finding in patients with pancreatic cancer, elevated BUN levels have been previously linked to poorer prognosis for patients with non–small cell lung cancer and advanced malignancies who were receiving palliative care. Elevated BUN levels may indicate subclinical renal dysfunction or other comorbidities that influence survival.
Univariate analysis in the current study did not find an association between early mortality and BMI, which may be due to the timing of the measurement. Patients may experience cancer-induced weight loss that renders BMI measures falsely low. The association between BMI and decreased survival after pancreatic cancer diagnosis was found previously to be strongest when BMI was taken 18-20 years prior to diagnosis.
The authors note that although perioperative mortality has improved considerably in recent years, there exists a subgroup of patients who experience early recurrence.
“These patients may not benefit from the current standard of care but to our knowledge, little is known regarding how best to identify such patients at high risk of early mortality,” wrote Dr. Sohal and his associates. The current study identifies a simple set of baseline parameters that may allow for “easy targeting of high-risk patients for specific interventions aimed at improving clinical outcomes.”
Dr. Sohal reported having no disclosures. Dr. Khorana has received fees from several industry sources for work outside of the current study.
Using parameters routinely collected in patients with pancreatic cancer, the Khorana score and the blood urea nitrogen (BUN) level were significantly associated with early mortality in patients with pancreatic cancer who underwent surgical resection, according to a report published in the journal Cancer.
Dr. Davendra P.S. Sohal, an oncologist at Cleveland Clinic, and his colleagues stated that by identifying patients with resectable pancreatic adenocarcinoma who are at high risk of early mortality, the parameters “may be used to stratify patients, and ultimately may be used to select high-risk patients for more aggressive therapies in prospective studies” (Cancer 2015 [doi:10.1002/cncr.29298]).
Multivariate analysis showed the risk for early mortality (before 6 months) increased with high-risk Khorana score (hazard ratio, 2.32; 95% confidence interval, 1.04-5.13; P = .039) and elevated blood urea nitrogen (HR, 4.34; 95% CI, 1.84-10.25; P < .001). The authors noted that other key variables, such as TNM classification of malignant tumor staging, were not associated with early mortality.
The study evaluated 334 patients, median age 67 years, who underwent surgical resection of pancreatic adenocarcinoma during 2006-2013 at the Cleveland Clinic. With a median follow-up time of 39.4 months, there were 205 deaths (61%), and median overall survival was 21.3 months. Within 30 days after surgery, 3 (0.9%) deaths occurred, and within 6 months of surgery, 29 (8.7%) deaths occurred. Most tumors were located in the head of the pancreas (73%); most pathologic stages were T3 (67%) and N1 (63%); median Khorana score was 2; 47% of patients had a score ≥ 3; 59% had comorbidities. Some of the patients received preoperative anticancer therapy, making the study population heterogeneous in that respect.
The Khorana score, a measure of venous thromboembolism risk, combines five items: cancer site, platelet count > 350/nL, white blood cell count > 11/nL, hemoglobin <100 g/L, and body mass index (BMI) ≥ 35 kg/m2; Khorana scores of 3 or greater indicate high risk.
A novel finding in patients with pancreatic cancer, elevated BUN levels have been previously linked to poorer prognosis for patients with non–small cell lung cancer and advanced malignancies who were receiving palliative care. Elevated BUN levels may indicate subclinical renal dysfunction or other comorbidities that influence survival.
Univariate analysis in the current study did not find an association between early mortality and BMI, which may be due to the timing of the measurement. Patients may experience cancer-induced weight loss that renders BMI measures falsely low. The association between BMI and decreased survival after pancreatic cancer diagnosis was found previously to be strongest when BMI was taken 18-20 years prior to diagnosis.
The authors note that although perioperative mortality has improved considerably in recent years, there exists a subgroup of patients who experience early recurrence.
“These patients may not benefit from the current standard of care but to our knowledge, little is known regarding how best to identify such patients at high risk of early mortality,” wrote Dr. Sohal and his associates. The current study identifies a simple set of baseline parameters that may allow for “easy targeting of high-risk patients for specific interventions aimed at improving clinical outcomes.”
Dr. Sohal reported having no disclosures. Dr. Khorana has received fees from several industry sources for work outside of the current study.
Using parameters routinely collected in patients with pancreatic cancer, the Khorana score and the blood urea nitrogen (BUN) level were significantly associated with early mortality in patients with pancreatic cancer who underwent surgical resection, according to a report published in the journal Cancer.
Dr. Davendra P.S. Sohal, an oncologist at Cleveland Clinic, and his colleagues stated that by identifying patients with resectable pancreatic adenocarcinoma who are at high risk of early mortality, the parameters “may be used to stratify patients, and ultimately may be used to select high-risk patients for more aggressive therapies in prospective studies” (Cancer 2015 [doi:10.1002/cncr.29298]).
Multivariate analysis showed the risk for early mortality (before 6 months) increased with high-risk Khorana score (hazard ratio, 2.32; 95% confidence interval, 1.04-5.13; P = .039) and elevated blood urea nitrogen (HR, 4.34; 95% CI, 1.84-10.25; P < .001). The authors noted that other key variables, such as TNM classification of malignant tumor staging, were not associated with early mortality.
The study evaluated 334 patients, median age 67 years, who underwent surgical resection of pancreatic adenocarcinoma during 2006-2013 at the Cleveland Clinic. With a median follow-up time of 39.4 months, there were 205 deaths (61%), and median overall survival was 21.3 months. Within 30 days after surgery, 3 (0.9%) deaths occurred, and within 6 months of surgery, 29 (8.7%) deaths occurred. Most tumors were located in the head of the pancreas (73%); most pathologic stages were T3 (67%) and N1 (63%); median Khorana score was 2; 47% of patients had a score ≥ 3; 59% had comorbidities. Some of the patients received preoperative anticancer therapy, making the study population heterogeneous in that respect.
The Khorana score, a measure of venous thromboembolism risk, combines five items: cancer site, platelet count > 350/nL, white blood cell count > 11/nL, hemoglobin <100 g/L, and body mass index (BMI) ≥ 35 kg/m2; Khorana scores of 3 or greater indicate high risk.
A novel finding in patients with pancreatic cancer, elevated BUN levels have been previously linked to poorer prognosis for patients with non–small cell lung cancer and advanced malignancies who were receiving palliative care. Elevated BUN levels may indicate subclinical renal dysfunction or other comorbidities that influence survival.
Univariate analysis in the current study did not find an association between early mortality and BMI, which may be due to the timing of the measurement. Patients may experience cancer-induced weight loss that renders BMI measures falsely low. The association between BMI and decreased survival after pancreatic cancer diagnosis was found previously to be strongest when BMI was taken 18-20 years prior to diagnosis.
The authors note that although perioperative mortality has improved considerably in recent years, there exists a subgroup of patients who experience early recurrence.
“These patients may not benefit from the current standard of care but to our knowledge, little is known regarding how best to identify such patients at high risk of early mortality,” wrote Dr. Sohal and his associates. The current study identifies a simple set of baseline parameters that may allow for “easy targeting of high-risk patients for specific interventions aimed at improving clinical outcomes.”
Dr. Sohal reported having no disclosures. Dr. Khorana has received fees from several industry sources for work outside of the current study.
FROM CANCER
Key clinical point: High Khorana score and elevated blood urea nitrogen predicted early mortality in patients after surgical resection for pancreatic cancer.
Major finding: For patients with elevated blood urea nitrogen, the early mortality hazard ratio was 4.34 (95% CI, 1.84-10.25), and for high-risk Khorana scores, this was 2.32 (1.04-5.13).
Data source: The retrospective cohort study used medical chart data from 334 consecutive patients who underwent surgical resection at the Cleveland Clinic from 2006 to 2013.
Disclosures: Dr. Sohal reported having no disclosures. Dr. Khorana has received fees from several industry sources for work outside of the current study.
SGR repeal bill reintroduced; payment mechanism not addressed
A bill to repeal the Medicare Sustainable Growth Rate formula was reintroduced into the House and Senate March 19.
H.R. 1470, the SGR Repeal and Medicare Provider Payment Modernization Act, is described as “nearly identical” to the bicameral, bipartisan bill that was passed in the House in April 2014, with a spokesman for the House Ways & Means Committee describing the changes as technical in nature.
The bill’s introduction comes as the latest so-called “doc fix” patch set to expire on March 31, with a physician payment cut of 21% set to go into effect on April 1. Congress previously has passed 17 patches.
In addition to repealing the SGR, the bill includes a 0.5% pay increase per year for the next 5 years; consolidates existing quality programs into a single value-based performance program; incentivizes physicians to use alternate payment models that focus on care coordination and prevention to improve quality and reduce costs; and pushes more transparency of Medicare data for both patients and providers to help them improve care.
It does not address any how to pay for SGR repeal, nor does it include any language to extend funding for the Children’s Health Insurance Program, which expires in 2015.
Dr. David Fleming, president of the American College of Physicians, said in a statement that the bill “achieves ACP’s top priorities for physician payment reform,” and “strongly urges” its passage before the current patch expires.
A March 16 letter, signed by more than 750 organizations, including national and state medical societies, was sent to House Speaker John Boehner (R-Ohio), calling for passage of last year’s SGR repeal.
Rep. Michael C. Burgess (R-Texas) cosponsored the bill in the House with Republican and Democratic leadership in the Ways and Means and Energy and Commerce Committees and the chairmen and ranking members of their health subcommittees. The Senate version of the bill was introduce by Finance Committee Chairman Orrin Hatch (R-Utah).
A bill to repeal the Medicare Sustainable Growth Rate formula was reintroduced into the House and Senate March 19.
H.R. 1470, the SGR Repeal and Medicare Provider Payment Modernization Act, is described as “nearly identical” to the bicameral, bipartisan bill that was passed in the House in April 2014, with a spokesman for the House Ways & Means Committee describing the changes as technical in nature.
The bill’s introduction comes as the latest so-called “doc fix” patch set to expire on March 31, with a physician payment cut of 21% set to go into effect on April 1. Congress previously has passed 17 patches.
In addition to repealing the SGR, the bill includes a 0.5% pay increase per year for the next 5 years; consolidates existing quality programs into a single value-based performance program; incentivizes physicians to use alternate payment models that focus on care coordination and prevention to improve quality and reduce costs; and pushes more transparency of Medicare data for both patients and providers to help them improve care.
It does not address any how to pay for SGR repeal, nor does it include any language to extend funding for the Children’s Health Insurance Program, which expires in 2015.
Dr. David Fleming, president of the American College of Physicians, said in a statement that the bill “achieves ACP’s top priorities for physician payment reform,” and “strongly urges” its passage before the current patch expires.
A March 16 letter, signed by more than 750 organizations, including national and state medical societies, was sent to House Speaker John Boehner (R-Ohio), calling for passage of last year’s SGR repeal.
Rep. Michael C. Burgess (R-Texas) cosponsored the bill in the House with Republican and Democratic leadership in the Ways and Means and Energy and Commerce Committees and the chairmen and ranking members of their health subcommittees. The Senate version of the bill was introduce by Finance Committee Chairman Orrin Hatch (R-Utah).
A bill to repeal the Medicare Sustainable Growth Rate formula was reintroduced into the House and Senate March 19.
H.R. 1470, the SGR Repeal and Medicare Provider Payment Modernization Act, is described as “nearly identical” to the bicameral, bipartisan bill that was passed in the House in April 2014, with a spokesman for the House Ways & Means Committee describing the changes as technical in nature.
The bill’s introduction comes as the latest so-called “doc fix” patch set to expire on March 31, with a physician payment cut of 21% set to go into effect on April 1. Congress previously has passed 17 patches.
In addition to repealing the SGR, the bill includes a 0.5% pay increase per year for the next 5 years; consolidates existing quality programs into a single value-based performance program; incentivizes physicians to use alternate payment models that focus on care coordination and prevention to improve quality and reduce costs; and pushes more transparency of Medicare data for both patients and providers to help them improve care.
It does not address any how to pay for SGR repeal, nor does it include any language to extend funding for the Children’s Health Insurance Program, which expires in 2015.
Dr. David Fleming, president of the American College of Physicians, said in a statement that the bill “achieves ACP’s top priorities for physician payment reform,” and “strongly urges” its passage before the current patch expires.
A March 16 letter, signed by more than 750 organizations, including national and state medical societies, was sent to House Speaker John Boehner (R-Ohio), calling for passage of last year’s SGR repeal.
Rep. Michael C. Burgess (R-Texas) cosponsored the bill in the House with Republican and Democratic leadership in the Ways and Means and Energy and Commerce Committees and the chairmen and ranking members of their health subcommittees. The Senate version of the bill was introduce by Finance Committee Chairman Orrin Hatch (R-Utah).
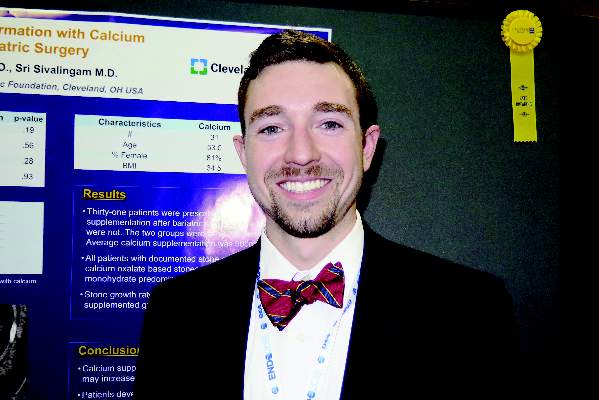
Gastric bypass patients on calcium had higher rates of kidney stone growth
SAN DIEGO – Patients taking calcium supplementation after gastric bypass surgery had higher rates of kidney stone growth, compared with those who received no calcium supplementation, results from a single-center retrospective study showed.
In addition, the majority of stones in patients taking calcium supplementation were comprised of calcium oxalate monohydrate, which is less amenable to extracorporeal shockwave therapy. “You need more invasive procedures to break up these kinds of stones,” lead author Christopher Loftus said in an interview at the meeting of the Endocrine Society, where the study was presented during a late-breaking abstract session.
Though it has been demonstrated that bariatric surgery is associated with an increased risk of kidney stone formation (Kidney Int. 2014 [doi:10.1038/ki.2014.352]), Mr. Loftus, a fourth-year medical student at Cleveland Clinic Lerner College of Medicine, and his associates set out to determine whether calcium supplementation increases the risk of nephrolithiasis in 60 stone-forming patients after gastric bypass surgery performed at the Cleveland Clinic. For each patient, two unenhanced CT scans at least 1 month apart and less than 2 years apart were selected at the start of the supplementation date and after the gastric bypass surgery date. The researchers calculated the rate of stone growth by the change in consecutive stone burden (the sum of maximum diameters of stones) divided by the elapsed time between scans.
Of the 60 patients, 31 received postoperative calcium supplementation (an average of 500 mg/day) and 29 did not. Compared with patients who did not take calcium supplementation, those who did were younger (a mean of 53 years vs. 58 years, respectively), more likely to be female (81% vs. 69%), and had a higher body mass index (34.5 kg/m2 vs. 32.7 kg/m2). In addition, a greater proportion of patients taking calcium supplements underwent Roux-en-Y bypass (83% vs. 64%; P = .19), had stones comprised of calcium oxalate (81% vs. 67%; P = .56), and a higher rate of stone growth (more than 10 mm/year vs. less than 5 mm/year; P = .0004). “We weren’t expecting such a pronounced effect,” Mr. Loftus said.
In their abstract, the researchers said that further studies are required to elucidate the exact role of calcium supplementation on stone disease in this patient population.
The study was funded in part by a grant from the American Society of Nephrology. Mr. Loftus reported having no relevant financial conflicts.
On Twitter @dougbrunk
SAN DIEGO – Patients taking calcium supplementation after gastric bypass surgery had higher rates of kidney stone growth, compared with those who received no calcium supplementation, results from a single-center retrospective study showed.
In addition, the majority of stones in patients taking calcium supplementation were comprised of calcium oxalate monohydrate, which is less amenable to extracorporeal shockwave therapy. “You need more invasive procedures to break up these kinds of stones,” lead author Christopher Loftus said in an interview at the meeting of the Endocrine Society, where the study was presented during a late-breaking abstract session.
Though it has been demonstrated that bariatric surgery is associated with an increased risk of kidney stone formation (Kidney Int. 2014 [doi:10.1038/ki.2014.352]), Mr. Loftus, a fourth-year medical student at Cleveland Clinic Lerner College of Medicine, and his associates set out to determine whether calcium supplementation increases the risk of nephrolithiasis in 60 stone-forming patients after gastric bypass surgery performed at the Cleveland Clinic. For each patient, two unenhanced CT scans at least 1 month apart and less than 2 years apart were selected at the start of the supplementation date and after the gastric bypass surgery date. The researchers calculated the rate of stone growth by the change in consecutive stone burden (the sum of maximum diameters of stones) divided by the elapsed time between scans.
Of the 60 patients, 31 received postoperative calcium supplementation (an average of 500 mg/day) and 29 did not. Compared with patients who did not take calcium supplementation, those who did were younger (a mean of 53 years vs. 58 years, respectively), more likely to be female (81% vs. 69%), and had a higher body mass index (34.5 kg/m2 vs. 32.7 kg/m2). In addition, a greater proportion of patients taking calcium supplements underwent Roux-en-Y bypass (83% vs. 64%; P = .19), had stones comprised of calcium oxalate (81% vs. 67%; P = .56), and a higher rate of stone growth (more than 10 mm/year vs. less than 5 mm/year; P = .0004). “We weren’t expecting such a pronounced effect,” Mr. Loftus said.
In their abstract, the researchers said that further studies are required to elucidate the exact role of calcium supplementation on stone disease in this patient population.
The study was funded in part by a grant from the American Society of Nephrology. Mr. Loftus reported having no relevant financial conflicts.
On Twitter @dougbrunk
SAN DIEGO – Patients taking calcium supplementation after gastric bypass surgery had higher rates of kidney stone growth, compared with those who received no calcium supplementation, results from a single-center retrospective study showed.
In addition, the majority of stones in patients taking calcium supplementation were comprised of calcium oxalate monohydrate, which is less amenable to extracorporeal shockwave therapy. “You need more invasive procedures to break up these kinds of stones,” lead author Christopher Loftus said in an interview at the meeting of the Endocrine Society, where the study was presented during a late-breaking abstract session.
Though it has been demonstrated that bariatric surgery is associated with an increased risk of kidney stone formation (Kidney Int. 2014 [doi:10.1038/ki.2014.352]), Mr. Loftus, a fourth-year medical student at Cleveland Clinic Lerner College of Medicine, and his associates set out to determine whether calcium supplementation increases the risk of nephrolithiasis in 60 stone-forming patients after gastric bypass surgery performed at the Cleveland Clinic. For each patient, two unenhanced CT scans at least 1 month apart and less than 2 years apart were selected at the start of the supplementation date and after the gastric bypass surgery date. The researchers calculated the rate of stone growth by the change in consecutive stone burden (the sum of maximum diameters of stones) divided by the elapsed time between scans.
Of the 60 patients, 31 received postoperative calcium supplementation (an average of 500 mg/day) and 29 did not. Compared with patients who did not take calcium supplementation, those who did were younger (a mean of 53 years vs. 58 years, respectively), more likely to be female (81% vs. 69%), and had a higher body mass index (34.5 kg/m2 vs. 32.7 kg/m2). In addition, a greater proportion of patients taking calcium supplements underwent Roux-en-Y bypass (83% vs. 64%; P = .19), had stones comprised of calcium oxalate (81% vs. 67%; P = .56), and a higher rate of stone growth (more than 10 mm/year vs. less than 5 mm/year; P = .0004). “We weren’t expecting such a pronounced effect,” Mr. Loftus said.
In their abstract, the researchers said that further studies are required to elucidate the exact role of calcium supplementation on stone disease in this patient population.
The study was funded in part by a grant from the American Society of Nephrology. Mr. Loftus reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT ENDO 2015
Key clinical point: Calcium supplementation for post-gastric bypass surgery patients may increase the risk of kidney stone growth.
Major finding: Compared with patients who did not take calcium supplementation, those who did had a higher rate of kidney stone growth (more than 10 mm/year vs. less than 5 mm/year; P = .0004).
Data source: An analysis of 60 stone-forming patients who underwent gastric bypass surgery at the Cleveland Clinic.
Disclosures: The study was funded in part by a grant from the American Society of Nephrology. Mr. Loftus reported having no relevant financial conflicts.
Feds recover $3 billion in health fraud in 2014
The federal government recouped $3 billion in health fraud settlements and judgments in fiscal 2014, down from $4 billion in 2013, according to a March 19 announcement by the Department of Health and Human Services.
The Health Care Fraud and Abuse Control (HCFAC) Program has recovered nearly $30 billion since it began in 1997.
The Department of Justice (DOJ) in 2014 also opened 924 new criminal health care fraud investigations, and federal prosecutors filed criminal charges in 496 cases involving 805 defendants, HHS said in its report. A total of 734 defendants were convicted of health care fraud–related crimes during last year.
Meanwhile, investigations by the HHS Office of Inspector General resulted in 867 criminal actions against individuals or entities that engaged in crimes related to Medicare and Medicaid and 529 civil actions, which include false claims and unjust-enrichment lawsuits. HHS excluded 4,017 health providers from participation in Medicare and Medicaid and other federal health care programs as a result of program violations, criminal actions, and licensure revocations.
The government touted the False Claims Act (FCA) as a leading tool in the fight against health fraud and recoupment of funding.
In 2014, the DOJ civil division, along with state officials, obtained $2.3 billion in settlements and judgments from FCA cases involving fraud and false claims. The department also opened 782 new civil health care fraud investigations under the FCA and had 957 civil health care fraud matters pending at the end of 2014.
For every dollar spent on health care–related fraud and abuse investigations in the last 3 years, HHS officials said they recovered $7.70. This is about $2 higher than the average return on investment when HCFAC was created in 1997.
However, the report noted that there were fewer resources for the federal government to fight health fraud and abuses because of sequestration of mandatory funding in 2014. A total of $32 million was sequestered from the HCFAC program in fiscal 2014, for a combined total of $62 million in the past 2 years.
[email protected]
On Twitter @legal_med
The federal government recouped $3 billion in health fraud settlements and judgments in fiscal 2014, down from $4 billion in 2013, according to a March 19 announcement by the Department of Health and Human Services.
The Health Care Fraud and Abuse Control (HCFAC) Program has recovered nearly $30 billion since it began in 1997.
The Department of Justice (DOJ) in 2014 also opened 924 new criminal health care fraud investigations, and federal prosecutors filed criminal charges in 496 cases involving 805 defendants, HHS said in its report. A total of 734 defendants were convicted of health care fraud–related crimes during last year.
Meanwhile, investigations by the HHS Office of Inspector General resulted in 867 criminal actions against individuals or entities that engaged in crimes related to Medicare and Medicaid and 529 civil actions, which include false claims and unjust-enrichment lawsuits. HHS excluded 4,017 health providers from participation in Medicare and Medicaid and other federal health care programs as a result of program violations, criminal actions, and licensure revocations.
The government touted the False Claims Act (FCA) as a leading tool in the fight against health fraud and recoupment of funding.
In 2014, the DOJ civil division, along with state officials, obtained $2.3 billion in settlements and judgments from FCA cases involving fraud and false claims. The department also opened 782 new civil health care fraud investigations under the FCA and had 957 civil health care fraud matters pending at the end of 2014.
For every dollar spent on health care–related fraud and abuse investigations in the last 3 years, HHS officials said they recovered $7.70. This is about $2 higher than the average return on investment when HCFAC was created in 1997.
However, the report noted that there were fewer resources for the federal government to fight health fraud and abuses because of sequestration of mandatory funding in 2014. A total of $32 million was sequestered from the HCFAC program in fiscal 2014, for a combined total of $62 million in the past 2 years.
[email protected]
On Twitter @legal_med
The federal government recouped $3 billion in health fraud settlements and judgments in fiscal 2014, down from $4 billion in 2013, according to a March 19 announcement by the Department of Health and Human Services.
The Health Care Fraud and Abuse Control (HCFAC) Program has recovered nearly $30 billion since it began in 1997.
The Department of Justice (DOJ) in 2014 also opened 924 new criminal health care fraud investigations, and federal prosecutors filed criminal charges in 496 cases involving 805 defendants, HHS said in its report. A total of 734 defendants were convicted of health care fraud–related crimes during last year.
Meanwhile, investigations by the HHS Office of Inspector General resulted in 867 criminal actions against individuals or entities that engaged in crimes related to Medicare and Medicaid and 529 civil actions, which include false claims and unjust-enrichment lawsuits. HHS excluded 4,017 health providers from participation in Medicare and Medicaid and other federal health care programs as a result of program violations, criminal actions, and licensure revocations.
The government touted the False Claims Act (FCA) as a leading tool in the fight against health fraud and recoupment of funding.
In 2014, the DOJ civil division, along with state officials, obtained $2.3 billion in settlements and judgments from FCA cases involving fraud and false claims. The department also opened 782 new civil health care fraud investigations under the FCA and had 957 civil health care fraud matters pending at the end of 2014.
For every dollar spent on health care–related fraud and abuse investigations in the last 3 years, HHS officials said they recovered $7.70. This is about $2 higher than the average return on investment when HCFAC was created in 1997.
However, the report noted that there were fewer resources for the federal government to fight health fraud and abuses because of sequestration of mandatory funding in 2014. A total of $32 million was sequestered from the HCFAC program in fiscal 2014, for a combined total of $62 million in the past 2 years.
[email protected]
On Twitter @legal_med
Procedure type found to drive readmissions
The type of surgical procedure performed is a significant predictor of hospital readmission, reported Dr. Kevin R. Kasten and his associates at East Carolina University, Greenville, N.C.
In an analysis of 217,389 surgery patients, postoperative adverse events, specifically unplanned operating room return (odds ratio, 8.5; CI, 8.0-9.0), pulmonary embolism (OR, 8.2; CI, 7.1-9.6), deep incisional infection (OR, 7.5; CI, 6.7-8.5), and organ space infection (OR, 5.8; CI, 5.3-6.3), were significantly associated with an increased readmission risk. In addition, specific procedures associated with a higher risk for readmission included cystectomy, proctectomy, pancreatectomy, and lower-extremity vascular interventions.
The findings of this study suggest that “adverse events are a better predictor of 30[-day] readmission than patient comorbidity,” the authors said in the report. “As such, efforts to prevent adverse events such as return to the operating room, pulmonary embolism, surgical site infections, and myocardial infarction are crucial to prevention of readmission.”
Read the full article in the Journal of Surgical Research.
The type of surgical procedure performed is a significant predictor of hospital readmission, reported Dr. Kevin R. Kasten and his associates at East Carolina University, Greenville, N.C.
In an analysis of 217,389 surgery patients, postoperative adverse events, specifically unplanned operating room return (odds ratio, 8.5; CI, 8.0-9.0), pulmonary embolism (OR, 8.2; CI, 7.1-9.6), deep incisional infection (OR, 7.5; CI, 6.7-8.5), and organ space infection (OR, 5.8; CI, 5.3-6.3), were significantly associated with an increased readmission risk. In addition, specific procedures associated with a higher risk for readmission included cystectomy, proctectomy, pancreatectomy, and lower-extremity vascular interventions.
The findings of this study suggest that “adverse events are a better predictor of 30[-day] readmission than patient comorbidity,” the authors said in the report. “As such, efforts to prevent adverse events such as return to the operating room, pulmonary embolism, surgical site infections, and myocardial infarction are crucial to prevention of readmission.”
Read the full article in the Journal of Surgical Research.
The type of surgical procedure performed is a significant predictor of hospital readmission, reported Dr. Kevin R. Kasten and his associates at East Carolina University, Greenville, N.C.
In an analysis of 217,389 surgery patients, postoperative adverse events, specifically unplanned operating room return (odds ratio, 8.5; CI, 8.0-9.0), pulmonary embolism (OR, 8.2; CI, 7.1-9.6), deep incisional infection (OR, 7.5; CI, 6.7-8.5), and organ space infection (OR, 5.8; CI, 5.3-6.3), were significantly associated with an increased readmission risk. In addition, specific procedures associated with a higher risk for readmission included cystectomy, proctectomy, pancreatectomy, and lower-extremity vascular interventions.
The findings of this study suggest that “adverse events are a better predictor of 30[-day] readmission than patient comorbidity,” the authors said in the report. “As such, efforts to prevent adverse events such as return to the operating room, pulmonary embolism, surgical site infections, and myocardial infarction are crucial to prevention of readmission.”
Read the full article in the Journal of Surgical Research.
Most probable postsurgical VTEs diagnosed after hospital discharge
Among surgical patients treated in and discharged from VA hospitals, 49.4% of possible venous thromboembolism s and 47.8% of probable VTEs were diagnosed within 30 days after surgery, and 63.1% of possible VTEs and 62.9% of probable VTEs were diagnosed within 90 days after surgery, according to Dr. Richard E. Nelson of the University of Utah, Salt Lake City.
In a retrospective cohort study, researchers examined medical records from 468,515 operations on 383,551 patients who underwent surgery without prior VTE between Jan. 1, 2005 and Dec. 31, 2010. In total, VTE occurred in 1.3% of surgical admissions for VA patients in the 90 days after surgery. However, the researchers argued that presumed VTE diagnoses should not be monitored based on inpatient records alone.
“Reliable monitoring of postoperative VTE events should incorporate two aspects. First, it should use data sources that allow for extraction of information from unstructured medical records. Second, it should use data sources that have the ability to follow patients after discharge from the hospital,” they said.
Read the full article in Thrombosis Research.
Among surgical patients treated in and discharged from VA hospitals, 49.4% of possible venous thromboembolism s and 47.8% of probable VTEs were diagnosed within 30 days after surgery, and 63.1% of possible VTEs and 62.9% of probable VTEs were diagnosed within 90 days after surgery, according to Dr. Richard E. Nelson of the University of Utah, Salt Lake City.
In a retrospective cohort study, researchers examined medical records from 468,515 operations on 383,551 patients who underwent surgery without prior VTE between Jan. 1, 2005 and Dec. 31, 2010. In total, VTE occurred in 1.3% of surgical admissions for VA patients in the 90 days after surgery. However, the researchers argued that presumed VTE diagnoses should not be monitored based on inpatient records alone.
“Reliable monitoring of postoperative VTE events should incorporate two aspects. First, it should use data sources that allow for extraction of information from unstructured medical records. Second, it should use data sources that have the ability to follow patients after discharge from the hospital,” they said.
Read the full article in Thrombosis Research.
Among surgical patients treated in and discharged from VA hospitals, 49.4% of possible venous thromboembolism s and 47.8% of probable VTEs were diagnosed within 30 days after surgery, and 63.1% of possible VTEs and 62.9% of probable VTEs were diagnosed within 90 days after surgery, according to Dr. Richard E. Nelson of the University of Utah, Salt Lake City.
In a retrospective cohort study, researchers examined medical records from 468,515 operations on 383,551 patients who underwent surgery without prior VTE between Jan. 1, 2005 and Dec. 31, 2010. In total, VTE occurred in 1.3% of surgical admissions for VA patients in the 90 days after surgery. However, the researchers argued that presumed VTE diagnoses should not be monitored based on inpatient records alone.
“Reliable monitoring of postoperative VTE events should incorporate two aspects. First, it should use data sources that allow for extraction of information from unstructured medical records. Second, it should use data sources that have the ability to follow patients after discharge from the hospital,” they said.
Read the full article in Thrombosis Research.
Several factors predict postbariatric surgery readmission
Bariatric surgery is generally safe and readmissions are rare, but prolonged operative time, operation complexity, and major postoperative complications are among several risk factors for readmission identified in a large retrospective cohort.
Of 18,186 patients from the 2012 American College of Surgeons National Surgical Quality Improvement program (ACS NSQIP) database who had bariatric surgery as a primary procedure, 5% were readmitted. Of 815 patients with any major complication, 31% were readmitted. Factors found on multivariate analysis to significantly predict readmission within 30 days were age, sex, body mass index, American Society of Anesthesiology (ASA) risk class, diabetes status, hypertension, and steroid use, Dr. Christa R. Abraham of Albany (N.Y.) Medical College and her colleagues reported online in the Journal of the American College of Surgeons.
Further, all major postoperative complications were significant predictors of readmission, including bleeding requiring transfusion, urinary tract infections, and superficial surgical site infection (SSI). Other significant predictors were deep SSI, organ space SSI, wound disruption, pneumonia, unplanned intubation, mechanical ventilation for more than 48 hours, pulmonary embolism, deep vein thrombosis, and sepsis, the investigators said (J. Am. Coll. Surg. 2015 [doi:10.1016/j.jamcollsurg.2015.02.018]).
Of the patients included in the study, 1,819 had a laparoscopic gastric band, 9,613 had laparoscopic Roux-en-Y gastric bypass, 6,439 had gastroplasties, and 315 had open Roux-en-Y gastric bypass. All had a BMI of at least 30 kg/m2, and had a postsurgery length of stay of 14 days or fewer. Most were ASA risk class 3 or lower, and most were functionally independent.
Complications were more common with laparoscopic and open Roux-en-y gastric bypass (5.5% and 11.8%, respectively) rather than with gastroplasty and sleeve (3.4%) and laparoscopic banding (1.4%).
The findings are of value, because while bariatric surgery is a low-risk procedure, and it is extremely common; in 2013 there were 179,000 such surgeries performed in the United States.

“Bariatric surgery is one of the fastest-growing surgical interest areas, making analysis of patient outcomes and reasons for readmission important,” the investigators explained.
The ability to identify high-risk patients could allow for targeted interventions to prevent readmission, they said.
For example, steroid use, which was identified as a risk factor in the current study, is modifiable.
“In our practice, steroids are discontinued for 6 weeks prior to bariatric surgery and patients who are steroid dependent are unlikely to undergo bariatric surgery,” they said.
Additionally, they “try to minimize readmission for patients with infections by treating with antibiotics following operation and continuing antibiotics at discharge.”
The investigators noted that the ACS NSQIP MORBPROB (estimated probability of morbidity) tool is a good tool for predicting readmission among prospective bariatric patients, although it may not fully capture the effect of preexisting conditions.
“These data led us to change our own practice by risk-stratifying patients with higher ASA and BMI to consider surgical options, and to begin early surveillance soon after discharge,” they said.
The authors reported having no disclosures.
Bariatric surgery is generally safe and readmissions are rare, but prolonged operative time, operation complexity, and major postoperative complications are among several risk factors for readmission identified in a large retrospective cohort.
Of 18,186 patients from the 2012 American College of Surgeons National Surgical Quality Improvement program (ACS NSQIP) database who had bariatric surgery as a primary procedure, 5% were readmitted. Of 815 patients with any major complication, 31% were readmitted. Factors found on multivariate analysis to significantly predict readmission within 30 days were age, sex, body mass index, American Society of Anesthesiology (ASA) risk class, diabetes status, hypertension, and steroid use, Dr. Christa R. Abraham of Albany (N.Y.) Medical College and her colleagues reported online in the Journal of the American College of Surgeons.
Further, all major postoperative complications were significant predictors of readmission, including bleeding requiring transfusion, urinary tract infections, and superficial surgical site infection (SSI). Other significant predictors were deep SSI, organ space SSI, wound disruption, pneumonia, unplanned intubation, mechanical ventilation for more than 48 hours, pulmonary embolism, deep vein thrombosis, and sepsis, the investigators said (J. Am. Coll. Surg. 2015 [doi:10.1016/j.jamcollsurg.2015.02.018]).
Of the patients included in the study, 1,819 had a laparoscopic gastric band, 9,613 had laparoscopic Roux-en-Y gastric bypass, 6,439 had gastroplasties, and 315 had open Roux-en-Y gastric bypass. All had a BMI of at least 30 kg/m2, and had a postsurgery length of stay of 14 days or fewer. Most were ASA risk class 3 or lower, and most were functionally independent.
Complications were more common with laparoscopic and open Roux-en-y gastric bypass (5.5% and 11.8%, respectively) rather than with gastroplasty and sleeve (3.4%) and laparoscopic banding (1.4%).
The findings are of value, because while bariatric surgery is a low-risk procedure, and it is extremely common; in 2013 there were 179,000 such surgeries performed in the United States.

“Bariatric surgery is one of the fastest-growing surgical interest areas, making analysis of patient outcomes and reasons for readmission important,” the investigators explained.
The ability to identify high-risk patients could allow for targeted interventions to prevent readmission, they said.
For example, steroid use, which was identified as a risk factor in the current study, is modifiable.
“In our practice, steroids are discontinued for 6 weeks prior to bariatric surgery and patients who are steroid dependent are unlikely to undergo bariatric surgery,” they said.
Additionally, they “try to minimize readmission for patients with infections by treating with antibiotics following operation and continuing antibiotics at discharge.”
The investigators noted that the ACS NSQIP MORBPROB (estimated probability of morbidity) tool is a good tool for predicting readmission among prospective bariatric patients, although it may not fully capture the effect of preexisting conditions.
“These data led us to change our own practice by risk-stratifying patients with higher ASA and BMI to consider surgical options, and to begin early surveillance soon after discharge,” they said.
The authors reported having no disclosures.
Bariatric surgery is generally safe and readmissions are rare, but prolonged operative time, operation complexity, and major postoperative complications are among several risk factors for readmission identified in a large retrospective cohort.
Of 18,186 patients from the 2012 American College of Surgeons National Surgical Quality Improvement program (ACS NSQIP) database who had bariatric surgery as a primary procedure, 5% were readmitted. Of 815 patients with any major complication, 31% were readmitted. Factors found on multivariate analysis to significantly predict readmission within 30 days were age, sex, body mass index, American Society of Anesthesiology (ASA) risk class, diabetes status, hypertension, and steroid use, Dr. Christa R. Abraham of Albany (N.Y.) Medical College and her colleagues reported online in the Journal of the American College of Surgeons.
Further, all major postoperative complications were significant predictors of readmission, including bleeding requiring transfusion, urinary tract infections, and superficial surgical site infection (SSI). Other significant predictors were deep SSI, organ space SSI, wound disruption, pneumonia, unplanned intubation, mechanical ventilation for more than 48 hours, pulmonary embolism, deep vein thrombosis, and sepsis, the investigators said (J. Am. Coll. Surg. 2015 [doi:10.1016/j.jamcollsurg.2015.02.018]).
Of the patients included in the study, 1,819 had a laparoscopic gastric band, 9,613 had laparoscopic Roux-en-Y gastric bypass, 6,439 had gastroplasties, and 315 had open Roux-en-Y gastric bypass. All had a BMI of at least 30 kg/m2, and had a postsurgery length of stay of 14 days or fewer. Most were ASA risk class 3 or lower, and most were functionally independent.
Complications were more common with laparoscopic and open Roux-en-y gastric bypass (5.5% and 11.8%, respectively) rather than with gastroplasty and sleeve (3.4%) and laparoscopic banding (1.4%).
The findings are of value, because while bariatric surgery is a low-risk procedure, and it is extremely common; in 2013 there were 179,000 such surgeries performed in the United States.

“Bariatric surgery is one of the fastest-growing surgical interest areas, making analysis of patient outcomes and reasons for readmission important,” the investigators explained.
The ability to identify high-risk patients could allow for targeted interventions to prevent readmission, they said.
For example, steroid use, which was identified as a risk factor in the current study, is modifiable.
“In our practice, steroids are discontinued for 6 weeks prior to bariatric surgery and patients who are steroid dependent are unlikely to undergo bariatric surgery,” they said.
Additionally, they “try to minimize readmission for patients with infections by treating with antibiotics following operation and continuing antibiotics at discharge.”
The investigators noted that the ACS NSQIP MORBPROB (estimated probability of morbidity) tool is a good tool for predicting readmission among prospective bariatric patients, although it may not fully capture the effect of preexisting conditions.
“These data led us to change our own practice by risk-stratifying patients with higher ASA and BMI to consider surgical options, and to begin early surveillance soon after discharge,” they said.
The authors reported having no disclosures.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Knowing risk factors for readmission after bariatric surgery can allow for targeted interventions.
Major finding: Steroid use is among several risk factors for readmission following bariatric surgery (incidence rate ratio, 2.07)
Data source: A retrospective cohort study involving 18,186 patients.
Disclosures: The authors reported having no disclosures.
VIDEO: Long-term PARTNER 1 data tip scales toward TAVR
SAN DIEGO – The 5-year results of the PARTNER 1 trial in presented at the annual meeting of the American College of Cardiology were reassuring for clinicians treating patients with severe aortic stenosis at high risk for surgery, said to Dr. Jeffrey J. Popma of Beth Israel DeaconessMedical Center, Boston, in a video interview. The data showed comparable mortality between transcatheter aortic valve replacement (TAVR) and surgical aortic valve replacement (SAVR), as well as long-term durability of the SAPIEN transcatheter valve, he said.
With these similar outcome results, Dr. Popma asks, can the less-invasive TAVR procedure be considered the preferred treatment over SAVR in these very-sick patients?
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – The 5-year results of the PARTNER 1 trial in presented at the annual meeting of the American College of Cardiology were reassuring for clinicians treating patients with severe aortic stenosis at high risk for surgery, said to Dr. Jeffrey J. Popma of Beth Israel DeaconessMedical Center, Boston, in a video interview. The data showed comparable mortality between transcatheter aortic valve replacement (TAVR) and surgical aortic valve replacement (SAVR), as well as long-term durability of the SAPIEN transcatheter valve, he said.
With these similar outcome results, Dr. Popma asks, can the less-invasive TAVR procedure be considered the preferred treatment over SAVR in these very-sick patients?
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – The 5-year results of the PARTNER 1 trial in presented at the annual meeting of the American College of Cardiology were reassuring for clinicians treating patients with severe aortic stenosis at high risk for surgery, said to Dr. Jeffrey J. Popma of Beth Israel DeaconessMedical Center, Boston, in a video interview. The data showed comparable mortality between transcatheter aortic valve replacement (TAVR) and surgical aortic valve replacement (SAVR), as well as long-term durability of the SAPIEN transcatheter valve, he said.
With these similar outcome results, Dr. Popma asks, can the less-invasive TAVR procedure be considered the preferred treatment over SAVR in these very-sick patients?
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ACC 15