User login
Official Newspaper of the American College of Surgeons
HALS and LAP colectomy each offer unique benefits
CHICAGO – A nationwide analysis comparing straight versus hand-assisted laparoscopic colectomy appears to have resulted in a draw.
Despite being used more commonly in patients with higher body mass index and comorbidities, hand-assisted laparoscopic surgery (HALS) resulted in a significantly shorter operative time than did straight laparoscopic surgery (LAP) (171 minutes vs. 178.8 minutes; P < .001).
On the other hand, LAP was associated with a significantly shorter length of stay (5.9 days vs. 6.0 days; P < .001), fewer complications (15.9% vs. 18.2%; P = .006), fewer specifically superficial skin infections (4.1% vs. 5.4%; P = .007), and less prolonged postoperative ileus (7.5% vs. 9.1%; P = .01).
The differences were statistically significant likely because of the high volume of patients in each group, but are unlikely to be clinically significant in terms of patient care, senior study author Dr. I. Emre Gorgun said at the annual meeting of the Central Surgical Association.
CSA incoming president Dr. Scott A. Gruber, chief of staff at the John D. Dingell VA Medical Center in Detroit, agreed. “There were very, very small differences. I think they were trying to show that the two [approaches] are virtually equivalent,” he said in an interview. “Each has its advantages and disadvantages, but the HALS technique was used in more complex, more high-risk patients,” Dr. Gruber said.
HALS bridges the learning gap between open and straight laparoscopic surgery, which has been slow to gain adoption in colorectal surgery because it is technically demanding and has a steep learning curve, said Dr. Gorgun, a colorectal surgeon at the Cleveland Clinic. HALS allows surgeons to regain tactile sensation and manual retraction, enabling them to perform even more complex operations more effectively.
Studies also suggest that HALS reduces conversion rates and preserves the short-term benefits of LAP, though a nationwide comparison of short-term outcomes using the two techniques has been absent.
To fill this knowledge gap, the investigators used the 2012 colectomy-targeted American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP
At baseline, the HALS group was significantly older than the LAP group (61.5 years vs. 60 years), had a higher body mass index (28.6 kg/m2 vs. 28 kg/m2), was more likely to be hypertensive (49.8% vs. 45.1%), and to be American Society of Anesthesiologists class III (42% vs. 37.4%) and class IV (2.8% vs. 2.7%). Steroid use for inflammatory bowel disease was significantly higher in the LAP group (6.5% vs. 5.4%).
Mortality rates were similar in the LAP and HALS groups (0.52% vs. 0.50%; P = .94), Dr. Gorgun reported.
Multivariate logistic regression adjusted for comorbid conditions lessened the degree of differences between the two groups, but continued to favor HALS for shorter operative time (odds ratio, 0.94) and favor LAP for shorter hospital stays (OR, 1.05) and less superficial surgical site infections (OR, 1.31), less prolonged post-operative ileus (OR, 1.25), and overall morbidity (OR, 1.16).
“Both LAP and HALS approaches are used in minimally invasive colorectal surgery based on their respective contributions and complement each other,” Dr. Gorgun concluded. “Implementing the best approach to decrease postoperative complication rates and increase use of MIS [minimally invasive surgery] will play a role in improving patient care and overall quality of health care.”
Dr. Gorgun, his coauthors, and Dr. Gruber reported having no financial conflicts
CHICAGO – A nationwide analysis comparing straight versus hand-assisted laparoscopic colectomy appears to have resulted in a draw.
Despite being used more commonly in patients with higher body mass index and comorbidities, hand-assisted laparoscopic surgery (HALS) resulted in a significantly shorter operative time than did straight laparoscopic surgery (LAP) (171 minutes vs. 178.8 minutes; P < .001).
On the other hand, LAP was associated with a significantly shorter length of stay (5.9 days vs. 6.0 days; P < .001), fewer complications (15.9% vs. 18.2%; P = .006), fewer specifically superficial skin infections (4.1% vs. 5.4%; P = .007), and less prolonged postoperative ileus (7.5% vs. 9.1%; P = .01).
The differences were statistically significant likely because of the high volume of patients in each group, but are unlikely to be clinically significant in terms of patient care, senior study author Dr. I. Emre Gorgun said at the annual meeting of the Central Surgical Association.
CSA incoming president Dr. Scott A. Gruber, chief of staff at the John D. Dingell VA Medical Center in Detroit, agreed. “There were very, very small differences. I think they were trying to show that the two [approaches] are virtually equivalent,” he said in an interview. “Each has its advantages and disadvantages, but the HALS technique was used in more complex, more high-risk patients,” Dr. Gruber said.
HALS bridges the learning gap between open and straight laparoscopic surgery, which has been slow to gain adoption in colorectal surgery because it is technically demanding and has a steep learning curve, said Dr. Gorgun, a colorectal surgeon at the Cleveland Clinic. HALS allows surgeons to regain tactile sensation and manual retraction, enabling them to perform even more complex operations more effectively.
Studies also suggest that HALS reduces conversion rates and preserves the short-term benefits of LAP, though a nationwide comparison of short-term outcomes using the two techniques has been absent.
To fill this knowledge gap, the investigators used the 2012 colectomy-targeted American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP
At baseline, the HALS group was significantly older than the LAP group (61.5 years vs. 60 years), had a higher body mass index (28.6 kg/m2 vs. 28 kg/m2), was more likely to be hypertensive (49.8% vs. 45.1%), and to be American Society of Anesthesiologists class III (42% vs. 37.4%) and class IV (2.8% vs. 2.7%). Steroid use for inflammatory bowel disease was significantly higher in the LAP group (6.5% vs. 5.4%).
Mortality rates were similar in the LAP and HALS groups (0.52% vs. 0.50%; P = .94), Dr. Gorgun reported.
Multivariate logistic regression adjusted for comorbid conditions lessened the degree of differences between the two groups, but continued to favor HALS for shorter operative time (odds ratio, 0.94) and favor LAP for shorter hospital stays (OR, 1.05) and less superficial surgical site infections (OR, 1.31), less prolonged post-operative ileus (OR, 1.25), and overall morbidity (OR, 1.16).
“Both LAP and HALS approaches are used in minimally invasive colorectal surgery based on their respective contributions and complement each other,” Dr. Gorgun concluded. “Implementing the best approach to decrease postoperative complication rates and increase use of MIS [minimally invasive surgery] will play a role in improving patient care and overall quality of health care.”
Dr. Gorgun, his coauthors, and Dr. Gruber reported having no financial conflicts
CHICAGO – A nationwide analysis comparing straight versus hand-assisted laparoscopic colectomy appears to have resulted in a draw.
Despite being used more commonly in patients with higher body mass index and comorbidities, hand-assisted laparoscopic surgery (HALS) resulted in a significantly shorter operative time than did straight laparoscopic surgery (LAP) (171 minutes vs. 178.8 minutes; P < .001).
On the other hand, LAP was associated with a significantly shorter length of stay (5.9 days vs. 6.0 days; P < .001), fewer complications (15.9% vs. 18.2%; P = .006), fewer specifically superficial skin infections (4.1% vs. 5.4%; P = .007), and less prolonged postoperative ileus (7.5% vs. 9.1%; P = .01).
The differences were statistically significant likely because of the high volume of patients in each group, but are unlikely to be clinically significant in terms of patient care, senior study author Dr. I. Emre Gorgun said at the annual meeting of the Central Surgical Association.
CSA incoming president Dr. Scott A. Gruber, chief of staff at the John D. Dingell VA Medical Center in Detroit, agreed. “There were very, very small differences. I think they were trying to show that the two [approaches] are virtually equivalent,” he said in an interview. “Each has its advantages and disadvantages, but the HALS technique was used in more complex, more high-risk patients,” Dr. Gruber said.
HALS bridges the learning gap between open and straight laparoscopic surgery, which has been slow to gain adoption in colorectal surgery because it is technically demanding and has a steep learning curve, said Dr. Gorgun, a colorectal surgeon at the Cleveland Clinic. HALS allows surgeons to regain tactile sensation and manual retraction, enabling them to perform even more complex operations more effectively.
Studies also suggest that HALS reduces conversion rates and preserves the short-term benefits of LAP, though a nationwide comparison of short-term outcomes using the two techniques has been absent.
To fill this knowledge gap, the investigators used the 2012 colectomy-targeted American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP
At baseline, the HALS group was significantly older than the LAP group (61.5 years vs. 60 years), had a higher body mass index (28.6 kg/m2 vs. 28 kg/m2), was more likely to be hypertensive (49.8% vs. 45.1%), and to be American Society of Anesthesiologists class III (42% vs. 37.4%) and class IV (2.8% vs. 2.7%). Steroid use for inflammatory bowel disease was significantly higher in the LAP group (6.5% vs. 5.4%).
Mortality rates were similar in the LAP and HALS groups (0.52% vs. 0.50%; P = .94), Dr. Gorgun reported.
Multivariate logistic regression adjusted for comorbid conditions lessened the degree of differences between the two groups, but continued to favor HALS for shorter operative time (odds ratio, 0.94) and favor LAP for shorter hospital stays (OR, 1.05) and less superficial surgical site infections (OR, 1.31), less prolonged post-operative ileus (OR, 1.25), and overall morbidity (OR, 1.16).
“Both LAP and HALS approaches are used in minimally invasive colorectal surgery based on their respective contributions and complement each other,” Dr. Gorgun concluded. “Implementing the best approach to decrease postoperative complication rates and increase use of MIS [minimally invasive surgery] will play a role in improving patient care and overall quality of health care.”
Dr. Gorgun, his coauthors, and Dr. Gruber reported having no financial conflicts
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: Straight and hand-assisted laparoscopic colectomy offer unique benefits, and HALS is a good option in more complex patients.
Major finding: Surgery was 7 minutes shorter with HALS, while complications were down 2.3% with LAP.
Data source: Retrospective study of 7,843 patients undergoing colectomy in the ACS NSQIP database.
Disclosures: Dr. Gorgun, his coauthors, and Dr. Gruber reported having no financial conflicts.
Novel Watchman device approved as warfarin alternative in atrial fib
The Watchman left atrial appendage (LAA) closure device has been approved in the United States as an alternative to warfarin for patients with nonvalvular atrial fibrillation, for a narrower indication than the one submitted for approval to the Food and Drug Administration.
The device is a percutaneously delivered permanent cardiac implant placed in the LAA to prevent the embolization of thrombi formed in the LAA, and is manufactured by Boston Scientific. The FDA approved the Watchman for reducing the risk of thromboembolism from the LAA in patients with nonvalvular atrial fibrillation “who are at increased risk for stroke and systemic embolism based on CHADS2 or CHA2DS2-VASc scores, are deemed by their physicians to be suitable for warfarin; and have an appropriate rationale to seek a nonpharmacologic alternative to warfarin, taking into account the safety and effectiveness of the device, compared to warfarin,” according to a statement issued by the company on March 13.
The approved indication is worded differently than the proposed indication that was submitted to the FDA for approval and discussed at an FDA panel meeting in October, to “prevent thromboembolism from the left atrial appendage.” The changes in the indication include the replacement of “prevent” with “reduce the risk” of thromboembolism, and the addition of the following qualifiers: In patients who “are deemed by their physicians to be suitable for warfarin,” and who have “an appropriate rationale to seek a nonpharmacologic alternative to warfarin, taking into account the safety and effectiveness of the device compared to warfarin.”
“These changes were made to more accurately reflect the appropriate patient population for this device,” according to an FDA spokesperson.
At a meeting in October 2014, the FDA’s Circulatory System Devices Panel voted 6-5 with one abstention that the benefits of the device outweighed its risks for the proposed indication, but several panelists who voted no said they would support approval of a second-line indication. In addition, panelists voting on both sides of this question said that the indication was too broad and should be revised to describe the device as a second-line alternative to warfarin, making clear it is not appropriate for all warfarin-eligible patients. (At the meeting, the panel unanimously agreed that there was “reasonable assurance” that the device was safe for use in this population.)
At the first advisory panel meeting on the device, in December 2013, the panel voted 13-1 to recommend approval, based on data from the PREVAIL and PROTECT-AF studies, which compared the device to chronic warfarin, and information from the Continued Access to PREVAIL (CAP2) registry.PREVAIL compared implantation of the device – with 45 days of warfarin plus 81 mg of aspirin for 45 days, followed by 325 mg of aspirin and 75 mg of clopidogrel through 6 months, followed by 325 mg of aspirin a day indefinitely – to chronic warfarin.
The October meeting was convened by the FDA to review longer follow-up data from PREVAIL, which found additional cases of ischemic strokes in the Watchman group and none in the warfarin-treated group.
The Watchman device has been available outside of the United States since 2009, is registered in 75 countries, and has been used to treat more than 10,000 patients, according to Boston Scientific.
The Watchman left atrial appendage (LAA) closure device has been approved in the United States as an alternative to warfarin for patients with nonvalvular atrial fibrillation, for a narrower indication than the one submitted for approval to the Food and Drug Administration.
The device is a percutaneously delivered permanent cardiac implant placed in the LAA to prevent the embolization of thrombi formed in the LAA, and is manufactured by Boston Scientific. The FDA approved the Watchman for reducing the risk of thromboembolism from the LAA in patients with nonvalvular atrial fibrillation “who are at increased risk for stroke and systemic embolism based on CHADS2 or CHA2DS2-VASc scores, are deemed by their physicians to be suitable for warfarin; and have an appropriate rationale to seek a nonpharmacologic alternative to warfarin, taking into account the safety and effectiveness of the device, compared to warfarin,” according to a statement issued by the company on March 13.
The approved indication is worded differently than the proposed indication that was submitted to the FDA for approval and discussed at an FDA panel meeting in October, to “prevent thromboembolism from the left atrial appendage.” The changes in the indication include the replacement of “prevent” with “reduce the risk” of thromboembolism, and the addition of the following qualifiers: In patients who “are deemed by their physicians to be suitable for warfarin,” and who have “an appropriate rationale to seek a nonpharmacologic alternative to warfarin, taking into account the safety and effectiveness of the device compared to warfarin.”
“These changes were made to more accurately reflect the appropriate patient population for this device,” according to an FDA spokesperson.
At a meeting in October 2014, the FDA’s Circulatory System Devices Panel voted 6-5 with one abstention that the benefits of the device outweighed its risks for the proposed indication, but several panelists who voted no said they would support approval of a second-line indication. In addition, panelists voting on both sides of this question said that the indication was too broad and should be revised to describe the device as a second-line alternative to warfarin, making clear it is not appropriate for all warfarin-eligible patients. (At the meeting, the panel unanimously agreed that there was “reasonable assurance” that the device was safe for use in this population.)
At the first advisory panel meeting on the device, in December 2013, the panel voted 13-1 to recommend approval, based on data from the PREVAIL and PROTECT-AF studies, which compared the device to chronic warfarin, and information from the Continued Access to PREVAIL (CAP2) registry.PREVAIL compared implantation of the device – with 45 days of warfarin plus 81 mg of aspirin for 45 days, followed by 325 mg of aspirin and 75 mg of clopidogrel through 6 months, followed by 325 mg of aspirin a day indefinitely – to chronic warfarin.
The October meeting was convened by the FDA to review longer follow-up data from PREVAIL, which found additional cases of ischemic strokes in the Watchman group and none in the warfarin-treated group.
The Watchman device has been available outside of the United States since 2009, is registered in 75 countries, and has been used to treat more than 10,000 patients, according to Boston Scientific.
The Watchman left atrial appendage (LAA) closure device has been approved in the United States as an alternative to warfarin for patients with nonvalvular atrial fibrillation, for a narrower indication than the one submitted for approval to the Food and Drug Administration.
The device is a percutaneously delivered permanent cardiac implant placed in the LAA to prevent the embolization of thrombi formed in the LAA, and is manufactured by Boston Scientific. The FDA approved the Watchman for reducing the risk of thromboembolism from the LAA in patients with nonvalvular atrial fibrillation “who are at increased risk for stroke and systemic embolism based on CHADS2 or CHA2DS2-VASc scores, are deemed by their physicians to be suitable for warfarin; and have an appropriate rationale to seek a nonpharmacologic alternative to warfarin, taking into account the safety and effectiveness of the device, compared to warfarin,” according to a statement issued by the company on March 13.
The approved indication is worded differently than the proposed indication that was submitted to the FDA for approval and discussed at an FDA panel meeting in October, to “prevent thromboembolism from the left atrial appendage.” The changes in the indication include the replacement of “prevent” with “reduce the risk” of thromboembolism, and the addition of the following qualifiers: In patients who “are deemed by their physicians to be suitable for warfarin,” and who have “an appropriate rationale to seek a nonpharmacologic alternative to warfarin, taking into account the safety and effectiveness of the device compared to warfarin.”
“These changes were made to more accurately reflect the appropriate patient population for this device,” according to an FDA spokesperson.
At a meeting in October 2014, the FDA’s Circulatory System Devices Panel voted 6-5 with one abstention that the benefits of the device outweighed its risks for the proposed indication, but several panelists who voted no said they would support approval of a second-line indication. In addition, panelists voting on both sides of this question said that the indication was too broad and should be revised to describe the device as a second-line alternative to warfarin, making clear it is not appropriate for all warfarin-eligible patients. (At the meeting, the panel unanimously agreed that there was “reasonable assurance” that the device was safe for use in this population.)
At the first advisory panel meeting on the device, in December 2013, the panel voted 13-1 to recommend approval, based on data from the PREVAIL and PROTECT-AF studies, which compared the device to chronic warfarin, and information from the Continued Access to PREVAIL (CAP2) registry.PREVAIL compared implantation of the device – with 45 days of warfarin plus 81 mg of aspirin for 45 days, followed by 325 mg of aspirin and 75 mg of clopidogrel through 6 months, followed by 325 mg of aspirin a day indefinitely – to chronic warfarin.
The October meeting was convened by the FDA to review longer follow-up data from PREVAIL, which found additional cases of ischemic strokes in the Watchman group and none in the warfarin-treated group.
The Watchman device has been available outside of the United States since 2009, is registered in 75 countries, and has been used to treat more than 10,000 patients, according to Boston Scientific.
Addressing pain at the end of life
A few months ago, a colleague asked me about treating a patient’s pain that he was managing for months both in and out of the hospital for what was now an incurable condition. This very skilled surgeon believed that the patient should “not require” such high doses of opioids based on the clinical picture of a healed surgical wound but felt at a loss of what else to do. He did not want to abandon his relationship with the patient. He considered referral to the anesthesia pain clinic as escalating pain requirements were exceeding his comfort level.
Alternatively, he considered deferring pain management to the patient’s primary care provider. Instead, we worked together through a rational pain approach and explored external factors that may have been contributing to the patient’s total pain experience. This brief vignette is not atypical and sheds light onto the ongoing need to fill an education gap for surgeons who deal with patients at the end of life.
It has been almost 25 years since the term “pain as the fifth vital sign” was first introduced into the lexicon of clinical practice. The idea was to provide as much zeal to the topic of pain as we do to a patient’s other vital physiological measures. Yet, seriously ill patients with potential life-limiting conditions continue to experience significant pain, especially at the end of life. Among patients with nonmalignant diagnoses, more than 40% experience severe pain within days of their death. For those with malignant conditions, 15%-75% report moderate to severe pain during the final weeks of life. Whether in the ICU, hospital ward, or outpatient setting, our surgical community struggles to provide effective symptomatic pain control in many patients who have transitioned from a curative pathway to one of comfort.
Although we never intend to allow patients to suffer at the end of life, barriers to appropriate pain control persist. In some case cases, patients may feel embarrassed or ashamed to accept escalating opioid doses. In other cases, patients and families may possess misconceptions about addiction to pain medication. It is important to dispel such myths and distinguish tolerance from dependence. Among opioid-naive patients, the risk of dependence (in other words, addiction) is estimated to be 0.1%. Among patients with a history of opioid abuse, the risk of addiction is still only 1%.
Large proportions of physicians continue to report inadequate training in pain control and are reluctant to prescribe high-enough doses of opioids to relieve pain, even at the end of life. One well-described reason has been physician fear of regulatory action and possible litigation for higher than typical opioid dosing.
This was the case for my colleague who was reluctant to escalate pain control.
This in turn leads to undertreating pain which, in fact, has been a source of successful litigation. Because undertreatment of pain may be akin to patient negligence, we should strive to become more comfortable with optimal pain treatment strategies. But pain control is not merely about intravenous opioids or pain tablets. Surgeons should at least have an appreciation for, if not a better understanding, of the modern palliative care approach to “total pain.” This construct consists of four interrelated pain domains: physical, psychological (emotional), spiritual, and social.
Although we tend to focus on physical pain, other domains are influenced by anxiety, depression, and fear. If such an approach seems a bridge too far, optimal care should involve a multidisciplinary team that touches on such areas. This may be most efficiently achieved through consultation and coordination with palliative care services when available. This patient’s surgeon soon discovered that family financial concerns were contributing to the patient’s sleepless nights and worsening somatic pain.
Somewhat outside the scope of typical postoperative care, pain relief at the end of life requires dosing and medication choices for extended periods of time. When establishing a treatment strategy, the surgeon should consider the feasibility and efficacy (half-life, duration, bioavailability, active metabolites) of each modality. In our patient, standard dosing was inadequate; for some, basal doses may increase by 25%-100% for progressive disease. To support the surgeon in learning more about this important area of care, multiple online tools and websites are available to assist with pain management choices. A short while ago, I learned from my colleague that this patient died comfortably and essentially pain free for the last months of his life.
Dr. Zonies is an associate professor of surgery in the trauma/critical care division at Oregon Health & Science University, Portland. He is board certified in hospice and palliative medicine.
A few months ago, a colleague asked me about treating a patient’s pain that he was managing for months both in and out of the hospital for what was now an incurable condition. This very skilled surgeon believed that the patient should “not require” such high doses of opioids based on the clinical picture of a healed surgical wound but felt at a loss of what else to do. He did not want to abandon his relationship with the patient. He considered referral to the anesthesia pain clinic as escalating pain requirements were exceeding his comfort level.
Alternatively, he considered deferring pain management to the patient’s primary care provider. Instead, we worked together through a rational pain approach and explored external factors that may have been contributing to the patient’s total pain experience. This brief vignette is not atypical and sheds light onto the ongoing need to fill an education gap for surgeons who deal with patients at the end of life.
It has been almost 25 years since the term “pain as the fifth vital sign” was first introduced into the lexicon of clinical practice. The idea was to provide as much zeal to the topic of pain as we do to a patient’s other vital physiological measures. Yet, seriously ill patients with potential life-limiting conditions continue to experience significant pain, especially at the end of life. Among patients with nonmalignant diagnoses, more than 40% experience severe pain within days of their death. For those with malignant conditions, 15%-75% report moderate to severe pain during the final weeks of life. Whether in the ICU, hospital ward, or outpatient setting, our surgical community struggles to provide effective symptomatic pain control in many patients who have transitioned from a curative pathway to one of comfort.
Although we never intend to allow patients to suffer at the end of life, barriers to appropriate pain control persist. In some case cases, patients may feel embarrassed or ashamed to accept escalating opioid doses. In other cases, patients and families may possess misconceptions about addiction to pain medication. It is important to dispel such myths and distinguish tolerance from dependence. Among opioid-naive patients, the risk of dependence (in other words, addiction) is estimated to be 0.1%. Among patients with a history of opioid abuse, the risk of addiction is still only 1%.
Large proportions of physicians continue to report inadequate training in pain control and are reluctant to prescribe high-enough doses of opioids to relieve pain, even at the end of life. One well-described reason has been physician fear of regulatory action and possible litigation for higher than typical opioid dosing.
This was the case for my colleague who was reluctant to escalate pain control.
This in turn leads to undertreating pain which, in fact, has been a source of successful litigation. Because undertreatment of pain may be akin to patient negligence, we should strive to become more comfortable with optimal pain treatment strategies. But pain control is not merely about intravenous opioids or pain tablets. Surgeons should at least have an appreciation for, if not a better understanding, of the modern palliative care approach to “total pain.” This construct consists of four interrelated pain domains: physical, psychological (emotional), spiritual, and social.
Although we tend to focus on physical pain, other domains are influenced by anxiety, depression, and fear. If such an approach seems a bridge too far, optimal care should involve a multidisciplinary team that touches on such areas. This may be most efficiently achieved through consultation and coordination with palliative care services when available. This patient’s surgeon soon discovered that family financial concerns were contributing to the patient’s sleepless nights and worsening somatic pain.
Somewhat outside the scope of typical postoperative care, pain relief at the end of life requires dosing and medication choices for extended periods of time. When establishing a treatment strategy, the surgeon should consider the feasibility and efficacy (half-life, duration, bioavailability, active metabolites) of each modality. In our patient, standard dosing was inadequate; for some, basal doses may increase by 25%-100% for progressive disease. To support the surgeon in learning more about this important area of care, multiple online tools and websites are available to assist with pain management choices. A short while ago, I learned from my colleague that this patient died comfortably and essentially pain free for the last months of his life.
Dr. Zonies is an associate professor of surgery in the trauma/critical care division at Oregon Health & Science University, Portland. He is board certified in hospice and palliative medicine.
A few months ago, a colleague asked me about treating a patient’s pain that he was managing for months both in and out of the hospital for what was now an incurable condition. This very skilled surgeon believed that the patient should “not require” such high doses of opioids based on the clinical picture of a healed surgical wound but felt at a loss of what else to do. He did not want to abandon his relationship with the patient. He considered referral to the anesthesia pain clinic as escalating pain requirements were exceeding his comfort level.
Alternatively, he considered deferring pain management to the patient’s primary care provider. Instead, we worked together through a rational pain approach and explored external factors that may have been contributing to the patient’s total pain experience. This brief vignette is not atypical and sheds light onto the ongoing need to fill an education gap for surgeons who deal with patients at the end of life.
It has been almost 25 years since the term “pain as the fifth vital sign” was first introduced into the lexicon of clinical practice. The idea was to provide as much zeal to the topic of pain as we do to a patient’s other vital physiological measures. Yet, seriously ill patients with potential life-limiting conditions continue to experience significant pain, especially at the end of life. Among patients with nonmalignant diagnoses, more than 40% experience severe pain within days of their death. For those with malignant conditions, 15%-75% report moderate to severe pain during the final weeks of life. Whether in the ICU, hospital ward, or outpatient setting, our surgical community struggles to provide effective symptomatic pain control in many patients who have transitioned from a curative pathway to one of comfort.
Although we never intend to allow patients to suffer at the end of life, barriers to appropriate pain control persist. In some case cases, patients may feel embarrassed or ashamed to accept escalating opioid doses. In other cases, patients and families may possess misconceptions about addiction to pain medication. It is important to dispel such myths and distinguish tolerance from dependence. Among opioid-naive patients, the risk of dependence (in other words, addiction) is estimated to be 0.1%. Among patients with a history of opioid abuse, the risk of addiction is still only 1%.
Large proportions of physicians continue to report inadequate training in pain control and are reluctant to prescribe high-enough doses of opioids to relieve pain, even at the end of life. One well-described reason has been physician fear of regulatory action and possible litigation for higher than typical opioid dosing.
This was the case for my colleague who was reluctant to escalate pain control.
This in turn leads to undertreating pain which, in fact, has been a source of successful litigation. Because undertreatment of pain may be akin to patient negligence, we should strive to become more comfortable with optimal pain treatment strategies. But pain control is not merely about intravenous opioids or pain tablets. Surgeons should at least have an appreciation for, if not a better understanding, of the modern palliative care approach to “total pain.” This construct consists of four interrelated pain domains: physical, psychological (emotional), spiritual, and social.
Although we tend to focus on physical pain, other domains are influenced by anxiety, depression, and fear. If such an approach seems a bridge too far, optimal care should involve a multidisciplinary team that touches on such areas. This may be most efficiently achieved through consultation and coordination with palliative care services when available. This patient’s surgeon soon discovered that family financial concerns were contributing to the patient’s sleepless nights and worsening somatic pain.
Somewhat outside the scope of typical postoperative care, pain relief at the end of life requires dosing and medication choices for extended periods of time. When establishing a treatment strategy, the surgeon should consider the feasibility and efficacy (half-life, duration, bioavailability, active metabolites) of each modality. In our patient, standard dosing was inadequate; for some, basal doses may increase by 25%-100% for progressive disease. To support the surgeon in learning more about this important area of care, multiple online tools and websites are available to assist with pain management choices. A short while ago, I learned from my colleague that this patient died comfortably and essentially pain free for the last months of his life.
Dr. Zonies is an associate professor of surgery in the trauma/critical care division at Oregon Health & Science University, Portland. He is board certified in hospice and palliative medicine.
From the Washington Office
In November 2014, the Centers for Medicare & Medicaid Services finalized a policy that will transition all 10-day and 90-day global codes to 0-day global codes in 2017 and 2018, respectively.
As most surgeons will know, global codes include all necessary services normally furnished before, during, and after a surgical procedure. Approximately 4,200 of the more than 9,900 Current Procedural Terminology codes are 10-day or 90-day global codes. The CMS claims the transition is necessary, in part, to increase the accuracy of payment for these codes. Despite the fact that the policy for the 10-day codes will be put into effect in 2017, the CMS has yet to develop a methodology for making this transition.
Prior to the release of the final rule, the ACS sent a detailed letter to the CMS asserting that the agency should postpone moving forward with this proposal until a comprehensive analysis of the effect on surgical patients and access to surgical care was completed. The ACS included recommendations on a number of issues that the CMS must resolve before moving forward with the proposed policy and stressed, above all, that the CMS should not make policy changes that infringe on surgeons’ ability to provide high-quality care to surgical patients. Despite the ACS regulatory advocacy efforts and those similar from other surgical and medical specialty groups, the CMS finalized the rule and continues to indicate that it plans to move forward.
During the lame duck session of Congress following the November election, a coalition of surgical groups led by the ACS drafted and provided to Congress legislative language the effect of which would be to preclude the CMS from moving forward with its plan to transition the 10-day and 90-day global codes to 0-day global codes.
The groups involved mounted an aggressive campaign, strongly advocating for the inclusion of the legislative language in the “CRomnibus” bill. Despite strong support from the Congressional “Doc Caucus” and other members of Congress, no language addressing transitioning of the global codes was included in the “CRomnibus” bill, which passed both chambers at the conclusion of the 113th Congress.
Now that the 114th Congress has begun, the ACS, working again in concert with the aforementioned coalition of other surgical and medical specialty groups, is taking a variety of strategic actions on both the legislative and regulatory fronts. Working with key members of Congress including Rep. Larry Bucshon, MD, FACS, Rep. Tom Price, MD, FACS, and Rep. Dan Benishek, MD, FACS, the ACS will continue to oppose implementation of the policy change by seeking congressional intervention to rescind the rule until such time as the CMS can ensure that the transition will not have a negative impact on patients and can be implemented in a way that accurately accounts for the care that surgeons provide.
Revised legislative language has been provided to Congress. Members of the ACS DAHP legislative affairs staff are engaged in daily advocacy efforts for inclusion of that language in legislation. ACS leaders and DAHP regulatory affairs staff have met with the CMS in an attempt to provide education concerning what is believed will be significant, negative impact of the policy on both patients and surgeons.
Fellows are encouraged to augment the efforts of the DAHP by personally contacting their senators and representatives to educate them about the following negative potential consequences the implementation of this policy would be expected to have:
1. Reduces patient access and quality of care. If 10-day and 90-day global codes are transitioned to 0-day global codes, patients will have a copay for the procedure and additional, separate copays for other services including each of the follow-up visits. Patients may also be responsible for separate payment of supplies and drugs necessary during postop visits currently bundled into the global payment, but not bundled into visit codes. This could considerably increase the financial burden on patients, or worse, discourage them from returning for follow-up care.
2. Undermines the current SGR legislation and other Medicare reform initiatives. The CMS initiatives for payment are all moving toward larger bundled payments. Deconstruction of the current payment structure for physicians is counterintuitive to the end goal of providing more comprehensive and coordinated care for patients.
3. Increases administrative burden. The administrative burden on surgical practices, the CMS, and its contractors will be significant. The American Medical Association estimates that eliminating the global package will result in 63 million additional claims per year to account for postsurgical evaluation and management services. This will add unnecessary costs to the claims processing system.
4. Obstructs clinical registry data collection and quality improvement. If patients forgo follow-up treatment or seek it from other providers, the policy would have a deleterious effect on surgeons’ ability to collect information on patient outcomes in clinical registries and undermine many meaningful quality improvement initiatives.
Staff members of the DC office are available to assist surgeons interested in contacting their individual senators and representatives to assist in the advocacy efforts relative to this policy. I can be reached by phone at 202-337-2701 or by e-mail at [email protected].
Until next month …
Dr. Bailey is a pediatric surgeon and Medical Director, Advocacy for the Division of Advocacy and Health Policy in the ACS offices in Washington, DC.
In November 2014, the Centers for Medicare & Medicaid Services finalized a policy that will transition all 10-day and 90-day global codes to 0-day global codes in 2017 and 2018, respectively.
As most surgeons will know, global codes include all necessary services normally furnished before, during, and after a surgical procedure. Approximately 4,200 of the more than 9,900 Current Procedural Terminology codes are 10-day or 90-day global codes. The CMS claims the transition is necessary, in part, to increase the accuracy of payment for these codes. Despite the fact that the policy for the 10-day codes will be put into effect in 2017, the CMS has yet to develop a methodology for making this transition.
Prior to the release of the final rule, the ACS sent a detailed letter to the CMS asserting that the agency should postpone moving forward with this proposal until a comprehensive analysis of the effect on surgical patients and access to surgical care was completed. The ACS included recommendations on a number of issues that the CMS must resolve before moving forward with the proposed policy and stressed, above all, that the CMS should not make policy changes that infringe on surgeons’ ability to provide high-quality care to surgical patients. Despite the ACS regulatory advocacy efforts and those similar from other surgical and medical specialty groups, the CMS finalized the rule and continues to indicate that it plans to move forward.
During the lame duck session of Congress following the November election, a coalition of surgical groups led by the ACS drafted and provided to Congress legislative language the effect of which would be to preclude the CMS from moving forward with its plan to transition the 10-day and 90-day global codes to 0-day global codes.
The groups involved mounted an aggressive campaign, strongly advocating for the inclusion of the legislative language in the “CRomnibus” bill. Despite strong support from the Congressional “Doc Caucus” and other members of Congress, no language addressing transitioning of the global codes was included in the “CRomnibus” bill, which passed both chambers at the conclusion of the 113th Congress.
Now that the 114th Congress has begun, the ACS, working again in concert with the aforementioned coalition of other surgical and medical specialty groups, is taking a variety of strategic actions on both the legislative and regulatory fronts. Working with key members of Congress including Rep. Larry Bucshon, MD, FACS, Rep. Tom Price, MD, FACS, and Rep. Dan Benishek, MD, FACS, the ACS will continue to oppose implementation of the policy change by seeking congressional intervention to rescind the rule until such time as the CMS can ensure that the transition will not have a negative impact on patients and can be implemented in a way that accurately accounts for the care that surgeons provide.
Revised legislative language has been provided to Congress. Members of the ACS DAHP legislative affairs staff are engaged in daily advocacy efforts for inclusion of that language in legislation. ACS leaders and DAHP regulatory affairs staff have met with the CMS in an attempt to provide education concerning what is believed will be significant, negative impact of the policy on both patients and surgeons.
Fellows are encouraged to augment the efforts of the DAHP by personally contacting their senators and representatives to educate them about the following negative potential consequences the implementation of this policy would be expected to have:
1. Reduces patient access and quality of care. If 10-day and 90-day global codes are transitioned to 0-day global codes, patients will have a copay for the procedure and additional, separate copays for other services including each of the follow-up visits. Patients may also be responsible for separate payment of supplies and drugs necessary during postop visits currently bundled into the global payment, but not bundled into visit codes. This could considerably increase the financial burden on patients, or worse, discourage them from returning for follow-up care.
2. Undermines the current SGR legislation and other Medicare reform initiatives. The CMS initiatives for payment are all moving toward larger bundled payments. Deconstruction of the current payment structure for physicians is counterintuitive to the end goal of providing more comprehensive and coordinated care for patients.
3. Increases administrative burden. The administrative burden on surgical practices, the CMS, and its contractors will be significant. The American Medical Association estimates that eliminating the global package will result in 63 million additional claims per year to account for postsurgical evaluation and management services. This will add unnecessary costs to the claims processing system.
4. Obstructs clinical registry data collection and quality improvement. If patients forgo follow-up treatment or seek it from other providers, the policy would have a deleterious effect on surgeons’ ability to collect information on patient outcomes in clinical registries and undermine many meaningful quality improvement initiatives.
Staff members of the DC office are available to assist surgeons interested in contacting their individual senators and representatives to assist in the advocacy efforts relative to this policy. I can be reached by phone at 202-337-2701 or by e-mail at [email protected].
Until next month …
Dr. Bailey is a pediatric surgeon and Medical Director, Advocacy for the Division of Advocacy and Health Policy in the ACS offices in Washington, DC.
In November 2014, the Centers for Medicare & Medicaid Services finalized a policy that will transition all 10-day and 90-day global codes to 0-day global codes in 2017 and 2018, respectively.
As most surgeons will know, global codes include all necessary services normally furnished before, during, and after a surgical procedure. Approximately 4,200 of the more than 9,900 Current Procedural Terminology codes are 10-day or 90-day global codes. The CMS claims the transition is necessary, in part, to increase the accuracy of payment for these codes. Despite the fact that the policy for the 10-day codes will be put into effect in 2017, the CMS has yet to develop a methodology for making this transition.
Prior to the release of the final rule, the ACS sent a detailed letter to the CMS asserting that the agency should postpone moving forward with this proposal until a comprehensive analysis of the effect on surgical patients and access to surgical care was completed. The ACS included recommendations on a number of issues that the CMS must resolve before moving forward with the proposed policy and stressed, above all, that the CMS should not make policy changes that infringe on surgeons’ ability to provide high-quality care to surgical patients. Despite the ACS regulatory advocacy efforts and those similar from other surgical and medical specialty groups, the CMS finalized the rule and continues to indicate that it plans to move forward.
During the lame duck session of Congress following the November election, a coalition of surgical groups led by the ACS drafted and provided to Congress legislative language the effect of which would be to preclude the CMS from moving forward with its plan to transition the 10-day and 90-day global codes to 0-day global codes.
The groups involved mounted an aggressive campaign, strongly advocating for the inclusion of the legislative language in the “CRomnibus” bill. Despite strong support from the Congressional “Doc Caucus” and other members of Congress, no language addressing transitioning of the global codes was included in the “CRomnibus” bill, which passed both chambers at the conclusion of the 113th Congress.
Now that the 114th Congress has begun, the ACS, working again in concert with the aforementioned coalition of other surgical and medical specialty groups, is taking a variety of strategic actions on both the legislative and regulatory fronts. Working with key members of Congress including Rep. Larry Bucshon, MD, FACS, Rep. Tom Price, MD, FACS, and Rep. Dan Benishek, MD, FACS, the ACS will continue to oppose implementation of the policy change by seeking congressional intervention to rescind the rule until such time as the CMS can ensure that the transition will not have a negative impact on patients and can be implemented in a way that accurately accounts for the care that surgeons provide.
Revised legislative language has been provided to Congress. Members of the ACS DAHP legislative affairs staff are engaged in daily advocacy efforts for inclusion of that language in legislation. ACS leaders and DAHP regulatory affairs staff have met with the CMS in an attempt to provide education concerning what is believed will be significant, negative impact of the policy on both patients and surgeons.
Fellows are encouraged to augment the efforts of the DAHP by personally contacting their senators and representatives to educate them about the following negative potential consequences the implementation of this policy would be expected to have:
1. Reduces patient access and quality of care. If 10-day and 90-day global codes are transitioned to 0-day global codes, patients will have a copay for the procedure and additional, separate copays for other services including each of the follow-up visits. Patients may also be responsible for separate payment of supplies and drugs necessary during postop visits currently bundled into the global payment, but not bundled into visit codes. This could considerably increase the financial burden on patients, or worse, discourage them from returning for follow-up care.
2. Undermines the current SGR legislation and other Medicare reform initiatives. The CMS initiatives for payment are all moving toward larger bundled payments. Deconstruction of the current payment structure for physicians is counterintuitive to the end goal of providing more comprehensive and coordinated care for patients.
3. Increases administrative burden. The administrative burden on surgical practices, the CMS, and its contractors will be significant. The American Medical Association estimates that eliminating the global package will result in 63 million additional claims per year to account for postsurgical evaluation and management services. This will add unnecessary costs to the claims processing system.
4. Obstructs clinical registry data collection and quality improvement. If patients forgo follow-up treatment or seek it from other providers, the policy would have a deleterious effect on surgeons’ ability to collect information on patient outcomes in clinical registries and undermine many meaningful quality improvement initiatives.
Staff members of the DC office are available to assist surgeons interested in contacting their individual senators and representatives to assist in the advocacy efforts relative to this policy. I can be reached by phone at 202-337-2701 or by e-mail at [email protected].
Until next month …
Dr. Bailey is a pediatric surgeon and Medical Director, Advocacy for the Division of Advocacy and Health Policy in the ACS offices in Washington, DC.
Practicing surgery and having a life
For those who have chosen the surgeon’s path, finding a sustainable work/life balance is challenging. For surgeons with young families and spousal responsibilities, achieving that balance may seem like an unattainable goal. As a rural surgeon with a spouse and children, I am here to say that rural practice has many benefits to those who love their work and also want a balanced life. I recommend that young surgeons, women in particular, consider this path for both the professional and personal advantages it offers.
I always tell the medical students that rotate with me, “When it is 4 o’clock in the morning and you forgot to go home ... be that.” That is to say, whatever rotation they are on when they have that feeling, that is the specialty they should choose. That was us when it came to surgery. When we were students going through surgical rotations we could not get enough. We wanted to see everything, do everything, and we didn’t want to miss anything. Many of our colleagues recommended against choosing surgery. We were told, “You’ll never have a life or a family;” “Your life will be horrible,” etc.
Now, many years later, I still love what I do as a surgeon. But I also love the other half of my life. I chose to practice rural surgery because I sensed that a balanced life would be possible in the rural setting. So I offer the following 10 tips for young surgeons who might be considering a rural practice:
1. Pick a good small town
Sit down and write out a list of all the things you want in a small town. My list, of course, will be different from your list but most importantly, make the list! It is no use taking a job in rural Colorado if you hate to hunt and fish. Consider the town and the job equally. For women surgeons, you may want to look for a place where there are women in upper administrative roles and other female physicians on staff. All small towns are definitely not alike and if you pick one for the hospital or the job without considering your surroundings, you will not likely be happy.
2. Don’t commute
Some people take a job in a small town or a rural setting but choose to live 30 miles away in the next larger town. I suggest living in the town you practice in. If at all possible, live close to the hospital. Every minute that you spend on the road is a minute away from your family. Living far away makes that 2 a.m. call from the ER that much more painful. You also miss out on the opportunity to become a real part of your community.
3. Choose the right partner
Small town physicians are tough to keep. Rural practice turnover is high. One of the most common reasons I hear for why a physician has left the area is because his or her spouse wasn’t happy. No matter how appealing the job seems, no matter how much bonus money they offer, no matter how great the hospital appears, if your spouse doesn’t like it there, you’ll be leaving. You may love your job and back country camping every weekend, but if your spouse pines for Whole Foods and the opera, you will be moving on eventually.
A large part of rural life revolves around events in the school system, and even if you have no young children of your own, it is helpful to make an effort to attend some of these events, if only to support your neighbor’s kids. It goes a long way to establish you as someone who is involved in the community and who cares. Remember, it is the mothers young and old who make many of the health care decisions for their families. Volunteer for events or get involved in the science program at the high school. You may find that you are a unique role model for teenagers in your community.
4. Choose the right partners
Rural general surgery is challenging enough without having to compete with those around you. Surgery in the small town setting becomes infinitely more pleasant when you have good partners. Is the practice set up to help and support each partner, or are you pitted against one another, competing for RVUs? Would your partners tolerate covering your call for 3 months of maternity leave or would this cause resentment? Look for a practice where the surgeons work together and cover for each other, and your small town life will be greatly enhanced.
5. Live within your means
A small town surgical practice can make for a very comfortable life. The cost of living is less, which means that your money goes further, with more left over for expenses such as saving for your kids’ college education. In addition, when you live in rural America, you won’t likely feel pressured to join the super expensive country club, send your kids to an expensive school, or drive a six-figure car. Although we may not make quite as much as the big city folk, when you account for the cost of living, rural surgeons do quite well.
6. Hire help
My husband is a firefighter, and at one point early in our marriage he was working night shift. With me on call and small children at home, that presented somewhat of a problem. But we solved it with a live-in nanny. Some people say, “I don’t want someone else raising my children,” and then they spend all their free time washing baby’s laundry and cleaning house instead of playing with the baby and having family meals and other family time together. How you utilize a nanny or any other help you hire is determined by you. But the idea is to hire help to do the mundane things so that you can do the fun things.
7. Learn to charm a rock
Small towns can be tough. Make one mistake, make one person angry, and before you eat your breakfast the next morning, the whole town knows about it. A very wise mentor of mine once said, “You catch more flies with honey.” Of course, he was absolutely right. When we work in bigger places, we tend to become numb to our own behavior because outbursts and conflicts are so common that our own little outbursts get lost in the mix. Such is not the case in a small town.
In rural America, people stop their cars to let you pull out. This can be very shocking when you come from New York and your first thought is …am I being carjacked? In a rural town, if you walk around with a Band-Aid on your face, every single person you pass on the street will ask if you are ok. It teaches you to treat other people well, even if you are having an absolutely terrible day. You can’t get away with taking your mood out on other people in a small town.
One very nice thing about working in a rural community is that people are grateful and have a very long memory for whatever you’ve done for them. Whether you’ve cured their colon cancer or removed a lipoma, they will stop you on the street to thank you or tell their friends for years afterward about how wonderful you were.
8. Get a hobby
Although life as a small town general surgeon can seem like a 24/7 occupation, careful time management and household support can create space for a hobby. And you need one. No matter how much we all love surgery, it is essential that we cultivate the ability to leave it be for a time here and there. A hobby (preferably one that helps alleviate stress) can help stave off burnout.
9. Don’t forget to sleep
This much-neglected survival tip is so important. We all have to be on call, some more than others. But most of us also have nights where we are not on call. These should not be the nights where we stay up until 3 a.m. watching every episode of the latest Netflix series. You must resist that temptation. The older you get, the harder it is to recover from a night out operating.
10. Never forget the 4 a.m. feeling
So you may learn to adjust to the small town and then to love it fiercely and protectively. You may even buy your own cow once a year or join a shooting range. You may learn to discuss the fall elk hunt, ice fishing, ranching, and the best place to buy ammunition with your patients. You walk through the hospital and you know every single person you pass in the hallway as well as their kids.
Let us never forget why we chose to be surgeons. Most of us would weather any challenge to continue to do what we love. And choosing a rural practice is one way to practice surgery and also achieve a satisfying work/life balance.
Dr. Long is an ACS Fellow and a general surgeon in rural West Virginia. She is the mother of five and an ironman triathlete. She is currently preparing for her 18th surgical mission trip to Central America in April. Dr. Justine Gavagan and Dr. Catherine O’Connor contributed to this article.
For those who have chosen the surgeon’s path, finding a sustainable work/life balance is challenging. For surgeons with young families and spousal responsibilities, achieving that balance may seem like an unattainable goal. As a rural surgeon with a spouse and children, I am here to say that rural practice has many benefits to those who love their work and also want a balanced life. I recommend that young surgeons, women in particular, consider this path for both the professional and personal advantages it offers.
I always tell the medical students that rotate with me, “When it is 4 o’clock in the morning and you forgot to go home ... be that.” That is to say, whatever rotation they are on when they have that feeling, that is the specialty they should choose. That was us when it came to surgery. When we were students going through surgical rotations we could not get enough. We wanted to see everything, do everything, and we didn’t want to miss anything. Many of our colleagues recommended against choosing surgery. We were told, “You’ll never have a life or a family;” “Your life will be horrible,” etc.
Now, many years later, I still love what I do as a surgeon. But I also love the other half of my life. I chose to practice rural surgery because I sensed that a balanced life would be possible in the rural setting. So I offer the following 10 tips for young surgeons who might be considering a rural practice:
1. Pick a good small town
Sit down and write out a list of all the things you want in a small town. My list, of course, will be different from your list but most importantly, make the list! It is no use taking a job in rural Colorado if you hate to hunt and fish. Consider the town and the job equally. For women surgeons, you may want to look for a place where there are women in upper administrative roles and other female physicians on staff. All small towns are definitely not alike and if you pick one for the hospital or the job without considering your surroundings, you will not likely be happy.
2. Don’t commute
Some people take a job in a small town or a rural setting but choose to live 30 miles away in the next larger town. I suggest living in the town you practice in. If at all possible, live close to the hospital. Every minute that you spend on the road is a minute away from your family. Living far away makes that 2 a.m. call from the ER that much more painful. You also miss out on the opportunity to become a real part of your community.
3. Choose the right partner
Small town physicians are tough to keep. Rural practice turnover is high. One of the most common reasons I hear for why a physician has left the area is because his or her spouse wasn’t happy. No matter how appealing the job seems, no matter how much bonus money they offer, no matter how great the hospital appears, if your spouse doesn’t like it there, you’ll be leaving. You may love your job and back country camping every weekend, but if your spouse pines for Whole Foods and the opera, you will be moving on eventually.
A large part of rural life revolves around events in the school system, and even if you have no young children of your own, it is helpful to make an effort to attend some of these events, if only to support your neighbor’s kids. It goes a long way to establish you as someone who is involved in the community and who cares. Remember, it is the mothers young and old who make many of the health care decisions for their families. Volunteer for events or get involved in the science program at the high school. You may find that you are a unique role model for teenagers in your community.
4. Choose the right partners
Rural general surgery is challenging enough without having to compete with those around you. Surgery in the small town setting becomes infinitely more pleasant when you have good partners. Is the practice set up to help and support each partner, or are you pitted against one another, competing for RVUs? Would your partners tolerate covering your call for 3 months of maternity leave or would this cause resentment? Look for a practice where the surgeons work together and cover for each other, and your small town life will be greatly enhanced.
5. Live within your means
A small town surgical practice can make for a very comfortable life. The cost of living is less, which means that your money goes further, with more left over for expenses such as saving for your kids’ college education. In addition, when you live in rural America, you won’t likely feel pressured to join the super expensive country club, send your kids to an expensive school, or drive a six-figure car. Although we may not make quite as much as the big city folk, when you account for the cost of living, rural surgeons do quite well.
6. Hire help
My husband is a firefighter, and at one point early in our marriage he was working night shift. With me on call and small children at home, that presented somewhat of a problem. But we solved it with a live-in nanny. Some people say, “I don’t want someone else raising my children,” and then they spend all their free time washing baby’s laundry and cleaning house instead of playing with the baby and having family meals and other family time together. How you utilize a nanny or any other help you hire is determined by you. But the idea is to hire help to do the mundane things so that you can do the fun things.
7. Learn to charm a rock
Small towns can be tough. Make one mistake, make one person angry, and before you eat your breakfast the next morning, the whole town knows about it. A very wise mentor of mine once said, “You catch more flies with honey.” Of course, he was absolutely right. When we work in bigger places, we tend to become numb to our own behavior because outbursts and conflicts are so common that our own little outbursts get lost in the mix. Such is not the case in a small town.
In rural America, people stop their cars to let you pull out. This can be very shocking when you come from New York and your first thought is …am I being carjacked? In a rural town, if you walk around with a Band-Aid on your face, every single person you pass on the street will ask if you are ok. It teaches you to treat other people well, even if you are having an absolutely terrible day. You can’t get away with taking your mood out on other people in a small town.
One very nice thing about working in a rural community is that people are grateful and have a very long memory for whatever you’ve done for them. Whether you’ve cured their colon cancer or removed a lipoma, they will stop you on the street to thank you or tell their friends for years afterward about how wonderful you were.
8. Get a hobby
Although life as a small town general surgeon can seem like a 24/7 occupation, careful time management and household support can create space for a hobby. And you need one. No matter how much we all love surgery, it is essential that we cultivate the ability to leave it be for a time here and there. A hobby (preferably one that helps alleviate stress) can help stave off burnout.
9. Don’t forget to sleep
This much-neglected survival tip is so important. We all have to be on call, some more than others. But most of us also have nights where we are not on call. These should not be the nights where we stay up until 3 a.m. watching every episode of the latest Netflix series. You must resist that temptation. The older you get, the harder it is to recover from a night out operating.
10. Never forget the 4 a.m. feeling
So you may learn to adjust to the small town and then to love it fiercely and protectively. You may even buy your own cow once a year or join a shooting range. You may learn to discuss the fall elk hunt, ice fishing, ranching, and the best place to buy ammunition with your patients. You walk through the hospital and you know every single person you pass in the hallway as well as their kids.
Let us never forget why we chose to be surgeons. Most of us would weather any challenge to continue to do what we love. And choosing a rural practice is one way to practice surgery and also achieve a satisfying work/life balance.
Dr. Long is an ACS Fellow and a general surgeon in rural West Virginia. She is the mother of five and an ironman triathlete. She is currently preparing for her 18th surgical mission trip to Central America in April. Dr. Justine Gavagan and Dr. Catherine O’Connor contributed to this article.
For those who have chosen the surgeon’s path, finding a sustainable work/life balance is challenging. For surgeons with young families and spousal responsibilities, achieving that balance may seem like an unattainable goal. As a rural surgeon with a spouse and children, I am here to say that rural practice has many benefits to those who love their work and also want a balanced life. I recommend that young surgeons, women in particular, consider this path for both the professional and personal advantages it offers.
I always tell the medical students that rotate with me, “When it is 4 o’clock in the morning and you forgot to go home ... be that.” That is to say, whatever rotation they are on when they have that feeling, that is the specialty they should choose. That was us when it came to surgery. When we were students going through surgical rotations we could not get enough. We wanted to see everything, do everything, and we didn’t want to miss anything. Many of our colleagues recommended against choosing surgery. We were told, “You’ll never have a life or a family;” “Your life will be horrible,” etc.
Now, many years later, I still love what I do as a surgeon. But I also love the other half of my life. I chose to practice rural surgery because I sensed that a balanced life would be possible in the rural setting. So I offer the following 10 tips for young surgeons who might be considering a rural practice:
1. Pick a good small town
Sit down and write out a list of all the things you want in a small town. My list, of course, will be different from your list but most importantly, make the list! It is no use taking a job in rural Colorado if you hate to hunt and fish. Consider the town and the job equally. For women surgeons, you may want to look for a place where there are women in upper administrative roles and other female physicians on staff. All small towns are definitely not alike and if you pick one for the hospital or the job without considering your surroundings, you will not likely be happy.
2. Don’t commute
Some people take a job in a small town or a rural setting but choose to live 30 miles away in the next larger town. I suggest living in the town you practice in. If at all possible, live close to the hospital. Every minute that you spend on the road is a minute away from your family. Living far away makes that 2 a.m. call from the ER that much more painful. You also miss out on the opportunity to become a real part of your community.
3. Choose the right partner
Small town physicians are tough to keep. Rural practice turnover is high. One of the most common reasons I hear for why a physician has left the area is because his or her spouse wasn’t happy. No matter how appealing the job seems, no matter how much bonus money they offer, no matter how great the hospital appears, if your spouse doesn’t like it there, you’ll be leaving. You may love your job and back country camping every weekend, but if your spouse pines for Whole Foods and the opera, you will be moving on eventually.
A large part of rural life revolves around events in the school system, and even if you have no young children of your own, it is helpful to make an effort to attend some of these events, if only to support your neighbor’s kids. It goes a long way to establish you as someone who is involved in the community and who cares. Remember, it is the mothers young and old who make many of the health care decisions for their families. Volunteer for events or get involved in the science program at the high school. You may find that you are a unique role model for teenagers in your community.
4. Choose the right partners
Rural general surgery is challenging enough without having to compete with those around you. Surgery in the small town setting becomes infinitely more pleasant when you have good partners. Is the practice set up to help and support each partner, or are you pitted against one another, competing for RVUs? Would your partners tolerate covering your call for 3 months of maternity leave or would this cause resentment? Look for a practice where the surgeons work together and cover for each other, and your small town life will be greatly enhanced.
5. Live within your means
A small town surgical practice can make for a very comfortable life. The cost of living is less, which means that your money goes further, with more left over for expenses such as saving for your kids’ college education. In addition, when you live in rural America, you won’t likely feel pressured to join the super expensive country club, send your kids to an expensive school, or drive a six-figure car. Although we may not make quite as much as the big city folk, when you account for the cost of living, rural surgeons do quite well.
6. Hire help
My husband is a firefighter, and at one point early in our marriage he was working night shift. With me on call and small children at home, that presented somewhat of a problem. But we solved it with a live-in nanny. Some people say, “I don’t want someone else raising my children,” and then they spend all their free time washing baby’s laundry and cleaning house instead of playing with the baby and having family meals and other family time together. How you utilize a nanny or any other help you hire is determined by you. But the idea is to hire help to do the mundane things so that you can do the fun things.
7. Learn to charm a rock
Small towns can be tough. Make one mistake, make one person angry, and before you eat your breakfast the next morning, the whole town knows about it. A very wise mentor of mine once said, “You catch more flies with honey.” Of course, he was absolutely right. When we work in bigger places, we tend to become numb to our own behavior because outbursts and conflicts are so common that our own little outbursts get lost in the mix. Such is not the case in a small town.
In rural America, people stop their cars to let you pull out. This can be very shocking when you come from New York and your first thought is …am I being carjacked? In a rural town, if you walk around with a Band-Aid on your face, every single person you pass on the street will ask if you are ok. It teaches you to treat other people well, even if you are having an absolutely terrible day. You can’t get away with taking your mood out on other people in a small town.
One very nice thing about working in a rural community is that people are grateful and have a very long memory for whatever you’ve done for them. Whether you’ve cured their colon cancer or removed a lipoma, they will stop you on the street to thank you or tell their friends for years afterward about how wonderful you were.
8. Get a hobby
Although life as a small town general surgeon can seem like a 24/7 occupation, careful time management and household support can create space for a hobby. And you need one. No matter how much we all love surgery, it is essential that we cultivate the ability to leave it be for a time here and there. A hobby (preferably one that helps alleviate stress) can help stave off burnout.
9. Don’t forget to sleep
This much-neglected survival tip is so important. We all have to be on call, some more than others. But most of us also have nights where we are not on call. These should not be the nights where we stay up until 3 a.m. watching every episode of the latest Netflix series. You must resist that temptation. The older you get, the harder it is to recover from a night out operating.
10. Never forget the 4 a.m. feeling
So you may learn to adjust to the small town and then to love it fiercely and protectively. You may even buy your own cow once a year or join a shooting range. You may learn to discuss the fall elk hunt, ice fishing, ranching, and the best place to buy ammunition with your patients. You walk through the hospital and you know every single person you pass in the hallway as well as their kids.
Let us never forget why we chose to be surgeons. Most of us would weather any challenge to continue to do what we love. And choosing a rural practice is one way to practice surgery and also achieve a satisfying work/life balance.
Dr. Long is an ACS Fellow and a general surgeon in rural West Virginia. She is the mother of five and an ironman triathlete. She is currently preparing for her 18th surgical mission trip to Central America in April. Dr. Justine Gavagan and Dr. Catherine O’Connor contributed to this article.
ACS poised to lead change in health care delivery
The American College of Surgeons (ACS) had another successful year in 2014, and the College leadership and staff are working to ensure that we make even greater strides in 2015.
The ACS Division of Advocacy and Health Policy got a boost in June 2014 when Frank Opelka, MD, FACS, and Patrick Bailey, MD, FACS, joined the Washington Office team as Medical Directors of Quality and Advocacy, respectively. These surgeons are playing a leading role in positioning the ACS as a leader in the health policy, legislative, and regulatory arenas.
To address surgeons’ ongoing concerns regarding Medicare physician payment, the ACS has worked closely with Congress to develop legislation that would repeal the sustainable growth rate (SGR) formula. More than 200 ACS members from 44 states participated in 229 meetings on Capitol Hill April 1, 2014, as part of Leadership & Advocacy Summit, and the SGR was a key topic of discussion. Unfortunately, passage of the SGR Repeal Act was derailed because of funding challenges, and another temporary patch, which expires April 1, 2015, was put in place. The ACS continues to urge Congress to pass the SGR Repeal Act in this legislative session.
Other issues on the ACS health policy agenda include averting a provision in the final rule on the Medicare physician fee schedule that would convert 10- and 90-day global codes to 0-day codes, medical liability reform, and graduate medical education.
We are looking forward to taking Operation Giving Back in a new direction under the leadership of Medical Director Girma Tefera, MD, FACS. Dr. Tefera will be responsible for coordinating the College’s response to disasters worldwide, developing programs and opportunities for surgeon volunteers, communicating the work of the OGB, and increasing the College’s recognition among other global organizations.
In addition, the ACS and the U.S. Military Health System have entered into a 3-year strategic partnership that will encourage collaboration with respect to training and education, research, quality improvement, and combat readiness and disaster preparedness. M. Margaret (Peggy) Knudson, MD, FACS, is the Medical Director of this initiative.
Enthusiasm for leadership training among young surgeons and chapter officers remains high, More than 425 of these individuals participated in the leadership portion of the 2014 Leadership & Advocacy Summit, which featured sessions on best practices for chapters, mentoring, and emotional intelligence The next Summit will take place April 18-21.
The 2014 Initiates class was one of the College’s largest, totaling 1,640. To further boost membership, we have launched a Young Surgeons Marketing Campaign – Realize the Potential of Your Profession – and a Show Your Pride campaign.
The College also has launched a nationwide ACS Education and Training Campaign to communicate that ACS Education and Training are the cornerstones of excellence, transform possibilities into realities, and instill the joy of lifelong learning.
Many of the College’s recent education efforts have centered on assisting surgeons – particularly young surgeons – in career transitions. To address ongoing concerns regarding surgical training, the ACS has appointed a Committee on Residency Training (“Fix the Five”).
To help young surgeons shift from residency to practice, the ACS has developed the Transition to Practice (TTP) Program, which provides individuals who have completed five years of general surgery training with the opportunity to serve as a junior partner in a surgical practice. Presently, the TTP Program is being pilot-tested at 10 sites. In addition, the ACS has partnered with the Association of Program Directors in Surgery and the Association for Surgical Education to create a Surgery Resident Prep Curriculum for medical students transitioning to residency.
The ACS National Surgical Quality Improvement Program (ACS NSQIP®) celebrated its 10th anniversary in July 2014 at its annual conference in New York. A record-breaking 1,200 representatives from nearly 600 hospitals attended. Furthermore, the Joint Commission and the National Quality Forum (NQF) will honor ACS NSQIP® with the 2014 John M. Eisenberg Patient Safety and Quality Award later this month. The Eisenberg Award recognizes the major achievements of individuals and organizations in advancing patient safety and quality of care.
Another quality improvement activity has now been completed after three years of work – the development of comprehensive guidelines that define the resources needed to perform safe, effective pediatric operations. These standards were published in the March 2014 issue of the Journal of the American College of Surgeons. The College also is developing a Quality Manual that will be useful in guiding chief surgical quality officers as they attempt to implement quality improvement and patient safety programs in their institutions. Additionally, the ACS Clinical Research Program (ACS CRP) has completed the manuscript for Operative Standards for Cancer Surgery.
The Committee on Trauma has been actively involved in government efforts to establish guidelines for emergency medical services in mass-casualty events, including hemorrhage control. In a related effort, the Hartford Consensus, led by ACS Regent Lenworth Jacobs, Jr., MD, FACS, has articulated a framework for increasing survivability in mass shootings, known as THREAT: 1) threat suppression, 2) hemorrhage control, 3) rapid extrication to safety, 4) assessment by medical providers, and 5) transport to definitive care.
Among the Commission on Cancer’s (COC’s) most significant accomplishments in 2014 was the development of a framework for oncology medical home standards. In addition, the COC held its first legislative briefing in 2014 and issued a written response to the Institutes of Medicine report, Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis.
The College is providing more opportunities for surgeons to communicate with each other and for the ACS to communicate with the membership. The ACS Communities, now totaling 92, launched in July 2014, providing an interactive platform for surgeons to share their views, interests, and concerns. Shortly thereafter, the College launched a new, easy-to-navigate website, www.facs.org, which has been well-received.
In 2014-2015, the ACS Inspiring Quality tour has made stops in Northern California, North Carolina, Ohio, South Carolina, Iowa, Utah, and Sacramento, CA. At these meetings, we have continued to communicate to policymakers how ACS Quality Programs reduce spending and improve outcomes.
With these programs and solid leadership, the College is well-positioned to lead efforts to ensure that surgical patients receive optimal care. Your continued support is appreciated and your active involvement is strongly encouraged.
Dr. Hoyt is the Executive Director of the American College of Surgeons, Chicago.
The American College of Surgeons (ACS) had another successful year in 2014, and the College leadership and staff are working to ensure that we make even greater strides in 2015.
The ACS Division of Advocacy and Health Policy got a boost in June 2014 when Frank Opelka, MD, FACS, and Patrick Bailey, MD, FACS, joined the Washington Office team as Medical Directors of Quality and Advocacy, respectively. These surgeons are playing a leading role in positioning the ACS as a leader in the health policy, legislative, and regulatory arenas.
To address surgeons’ ongoing concerns regarding Medicare physician payment, the ACS has worked closely with Congress to develop legislation that would repeal the sustainable growth rate (SGR) formula. More than 200 ACS members from 44 states participated in 229 meetings on Capitol Hill April 1, 2014, as part of Leadership & Advocacy Summit, and the SGR was a key topic of discussion. Unfortunately, passage of the SGR Repeal Act was derailed because of funding challenges, and another temporary patch, which expires April 1, 2015, was put in place. The ACS continues to urge Congress to pass the SGR Repeal Act in this legislative session.
Other issues on the ACS health policy agenda include averting a provision in the final rule on the Medicare physician fee schedule that would convert 10- and 90-day global codes to 0-day codes, medical liability reform, and graduate medical education.
We are looking forward to taking Operation Giving Back in a new direction under the leadership of Medical Director Girma Tefera, MD, FACS. Dr. Tefera will be responsible for coordinating the College’s response to disasters worldwide, developing programs and opportunities for surgeon volunteers, communicating the work of the OGB, and increasing the College’s recognition among other global organizations.
In addition, the ACS and the U.S. Military Health System have entered into a 3-year strategic partnership that will encourage collaboration with respect to training and education, research, quality improvement, and combat readiness and disaster preparedness. M. Margaret (Peggy) Knudson, MD, FACS, is the Medical Director of this initiative.
Enthusiasm for leadership training among young surgeons and chapter officers remains high, More than 425 of these individuals participated in the leadership portion of the 2014 Leadership & Advocacy Summit, which featured sessions on best practices for chapters, mentoring, and emotional intelligence The next Summit will take place April 18-21.
The 2014 Initiates class was one of the College’s largest, totaling 1,640. To further boost membership, we have launched a Young Surgeons Marketing Campaign – Realize the Potential of Your Profession – and a Show Your Pride campaign.
The College also has launched a nationwide ACS Education and Training Campaign to communicate that ACS Education and Training are the cornerstones of excellence, transform possibilities into realities, and instill the joy of lifelong learning.
Many of the College’s recent education efforts have centered on assisting surgeons – particularly young surgeons – in career transitions. To address ongoing concerns regarding surgical training, the ACS has appointed a Committee on Residency Training (“Fix the Five”).
To help young surgeons shift from residency to practice, the ACS has developed the Transition to Practice (TTP) Program, which provides individuals who have completed five years of general surgery training with the opportunity to serve as a junior partner in a surgical practice. Presently, the TTP Program is being pilot-tested at 10 sites. In addition, the ACS has partnered with the Association of Program Directors in Surgery and the Association for Surgical Education to create a Surgery Resident Prep Curriculum for medical students transitioning to residency.
The ACS National Surgical Quality Improvement Program (ACS NSQIP®) celebrated its 10th anniversary in July 2014 at its annual conference in New York. A record-breaking 1,200 representatives from nearly 600 hospitals attended. Furthermore, the Joint Commission and the National Quality Forum (NQF) will honor ACS NSQIP® with the 2014 John M. Eisenberg Patient Safety and Quality Award later this month. The Eisenberg Award recognizes the major achievements of individuals and organizations in advancing patient safety and quality of care.
Another quality improvement activity has now been completed after three years of work – the development of comprehensive guidelines that define the resources needed to perform safe, effective pediatric operations. These standards were published in the March 2014 issue of the Journal of the American College of Surgeons. The College also is developing a Quality Manual that will be useful in guiding chief surgical quality officers as they attempt to implement quality improvement and patient safety programs in their institutions. Additionally, the ACS Clinical Research Program (ACS CRP) has completed the manuscript for Operative Standards for Cancer Surgery.
The Committee on Trauma has been actively involved in government efforts to establish guidelines for emergency medical services in mass-casualty events, including hemorrhage control. In a related effort, the Hartford Consensus, led by ACS Regent Lenworth Jacobs, Jr., MD, FACS, has articulated a framework for increasing survivability in mass shootings, known as THREAT: 1) threat suppression, 2) hemorrhage control, 3) rapid extrication to safety, 4) assessment by medical providers, and 5) transport to definitive care.
Among the Commission on Cancer’s (COC’s) most significant accomplishments in 2014 was the development of a framework for oncology medical home standards. In addition, the COC held its first legislative briefing in 2014 and issued a written response to the Institutes of Medicine report, Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis.
The College is providing more opportunities for surgeons to communicate with each other and for the ACS to communicate with the membership. The ACS Communities, now totaling 92, launched in July 2014, providing an interactive platform for surgeons to share their views, interests, and concerns. Shortly thereafter, the College launched a new, easy-to-navigate website, www.facs.org, which has been well-received.
In 2014-2015, the ACS Inspiring Quality tour has made stops in Northern California, North Carolina, Ohio, South Carolina, Iowa, Utah, and Sacramento, CA. At these meetings, we have continued to communicate to policymakers how ACS Quality Programs reduce spending and improve outcomes.
With these programs and solid leadership, the College is well-positioned to lead efforts to ensure that surgical patients receive optimal care. Your continued support is appreciated and your active involvement is strongly encouraged.
Dr. Hoyt is the Executive Director of the American College of Surgeons, Chicago.
The American College of Surgeons (ACS) had another successful year in 2014, and the College leadership and staff are working to ensure that we make even greater strides in 2015.
The ACS Division of Advocacy and Health Policy got a boost in June 2014 when Frank Opelka, MD, FACS, and Patrick Bailey, MD, FACS, joined the Washington Office team as Medical Directors of Quality and Advocacy, respectively. These surgeons are playing a leading role in positioning the ACS as a leader in the health policy, legislative, and regulatory arenas.
To address surgeons’ ongoing concerns regarding Medicare physician payment, the ACS has worked closely with Congress to develop legislation that would repeal the sustainable growth rate (SGR) formula. More than 200 ACS members from 44 states participated in 229 meetings on Capitol Hill April 1, 2014, as part of Leadership & Advocacy Summit, and the SGR was a key topic of discussion. Unfortunately, passage of the SGR Repeal Act was derailed because of funding challenges, and another temporary patch, which expires April 1, 2015, was put in place. The ACS continues to urge Congress to pass the SGR Repeal Act in this legislative session.
Other issues on the ACS health policy agenda include averting a provision in the final rule on the Medicare physician fee schedule that would convert 10- and 90-day global codes to 0-day codes, medical liability reform, and graduate medical education.
We are looking forward to taking Operation Giving Back in a new direction under the leadership of Medical Director Girma Tefera, MD, FACS. Dr. Tefera will be responsible for coordinating the College’s response to disasters worldwide, developing programs and opportunities for surgeon volunteers, communicating the work of the OGB, and increasing the College’s recognition among other global organizations.
In addition, the ACS and the U.S. Military Health System have entered into a 3-year strategic partnership that will encourage collaboration with respect to training and education, research, quality improvement, and combat readiness and disaster preparedness. M. Margaret (Peggy) Knudson, MD, FACS, is the Medical Director of this initiative.
Enthusiasm for leadership training among young surgeons and chapter officers remains high, More than 425 of these individuals participated in the leadership portion of the 2014 Leadership & Advocacy Summit, which featured sessions on best practices for chapters, mentoring, and emotional intelligence The next Summit will take place April 18-21.
The 2014 Initiates class was one of the College’s largest, totaling 1,640. To further boost membership, we have launched a Young Surgeons Marketing Campaign – Realize the Potential of Your Profession – and a Show Your Pride campaign.
The College also has launched a nationwide ACS Education and Training Campaign to communicate that ACS Education and Training are the cornerstones of excellence, transform possibilities into realities, and instill the joy of lifelong learning.
Many of the College’s recent education efforts have centered on assisting surgeons – particularly young surgeons – in career transitions. To address ongoing concerns regarding surgical training, the ACS has appointed a Committee on Residency Training (“Fix the Five”).
To help young surgeons shift from residency to practice, the ACS has developed the Transition to Practice (TTP) Program, which provides individuals who have completed five years of general surgery training with the opportunity to serve as a junior partner in a surgical practice. Presently, the TTP Program is being pilot-tested at 10 sites. In addition, the ACS has partnered with the Association of Program Directors in Surgery and the Association for Surgical Education to create a Surgery Resident Prep Curriculum for medical students transitioning to residency.
The ACS National Surgical Quality Improvement Program (ACS NSQIP®) celebrated its 10th anniversary in July 2014 at its annual conference in New York. A record-breaking 1,200 representatives from nearly 600 hospitals attended. Furthermore, the Joint Commission and the National Quality Forum (NQF) will honor ACS NSQIP® with the 2014 John M. Eisenberg Patient Safety and Quality Award later this month. The Eisenberg Award recognizes the major achievements of individuals and organizations in advancing patient safety and quality of care.
Another quality improvement activity has now been completed after three years of work – the development of comprehensive guidelines that define the resources needed to perform safe, effective pediatric operations. These standards were published in the March 2014 issue of the Journal of the American College of Surgeons. The College also is developing a Quality Manual that will be useful in guiding chief surgical quality officers as they attempt to implement quality improvement and patient safety programs in their institutions. Additionally, the ACS Clinical Research Program (ACS CRP) has completed the manuscript for Operative Standards for Cancer Surgery.
The Committee on Trauma has been actively involved in government efforts to establish guidelines for emergency medical services in mass-casualty events, including hemorrhage control. In a related effort, the Hartford Consensus, led by ACS Regent Lenworth Jacobs, Jr., MD, FACS, has articulated a framework for increasing survivability in mass shootings, known as THREAT: 1) threat suppression, 2) hemorrhage control, 3) rapid extrication to safety, 4) assessment by medical providers, and 5) transport to definitive care.
Among the Commission on Cancer’s (COC’s) most significant accomplishments in 2014 was the development of a framework for oncology medical home standards. In addition, the COC held its first legislative briefing in 2014 and issued a written response to the Institutes of Medicine report, Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis.
The College is providing more opportunities for surgeons to communicate with each other and for the ACS to communicate with the membership. The ACS Communities, now totaling 92, launched in July 2014, providing an interactive platform for surgeons to share their views, interests, and concerns. Shortly thereafter, the College launched a new, easy-to-navigate website, www.facs.org, which has been well-received.
In 2014-2015, the ACS Inspiring Quality tour has made stops in Northern California, North Carolina, Ohio, South Carolina, Iowa, Utah, and Sacramento, CA. At these meetings, we have continued to communicate to policymakers how ACS Quality Programs reduce spending and improve outcomes.
With these programs and solid leadership, the College is well-positioned to lead efforts to ensure that surgical patients receive optimal care. Your continued support is appreciated and your active involvement is strongly encouraged.
Dr. Hoyt is the Executive Director of the American College of Surgeons, Chicago.
Fresh red blood cells add no advantages for critically ill
The use of fresh red blood cells for transfusion did not reduce mortality or improve other outcomes, compared with older standard-issue red cells, according to results of a multicenter, blinded, randomized prospective study presented at the annual meeting of the International Society on Intensive Care and Emergency Medicine.
In the Age of Blood Evaluation (ABLE) study, researchers randomized 1,211 critically ill patients to red blood cells stored for less than 8 days and 1,219 patients to standard-issue cells stored for a mean of 22.4 days. The study was conducted at 64 centers in Europe and Canada, where all blood units were leukoreduced and SAGM (saline-adenine-glucose-mannitol) suspended. Similar products are supplied in the United States, but red cells are suspended in additive solution 3 (AS3) rather than SAGM.
At 90 days, 37% of patients in the fresh-blood group and 35.3% of patients in the standard blood group had died. The survival analysis of the time to death showed a hazard ratio of those in the fresh-blood group was 1.1, compared with those in the standard blood group (95% confidence interval, 0.9-1.2; P = .38).
There were no significant differences in the rates of death, organ failure, acute respiratory distress, cardiovascular complications, thrombosis, infection, or acute transfusion reaction.
There also were no significant differences between the two groups in length of hospital stay or duration of supportive care such as mechanical ventilation, as was simultaneously reported in the March 17 edition of the New England Journal of Medicine (doi:10.1056/NEJMoa1500704).
“Although [other] initial studies showed an association between longer red-cell storage and adverse outcomes, these associations may have been spurious owing to sicker patients receiving more units with longer storage, the overlap between comparison groups in the age of the red cells transfused, and the inclusion of transfusions that occurred after the clinical events,” Dr. Jacque Lacroix of University of Montreal and his coauthors wrote.
The study was supported by the Canadian Institutes of Health Research, Fonds de Recherche du Québec–Santé, the National Institute for Health Research Evaluation, the French Ministry of Health, and the Etablissement Français du Sang, and Sanquin Blood Supply. Two authors reported grants and personal fees from pharmaceutical companies outside the submitted work, while others reported financial support from the study funding sources.
The use of fresh red blood cells for transfusion did not reduce mortality or improve other outcomes, compared with older standard-issue red cells, according to results of a multicenter, blinded, randomized prospective study presented at the annual meeting of the International Society on Intensive Care and Emergency Medicine.
In the Age of Blood Evaluation (ABLE) study, researchers randomized 1,211 critically ill patients to red blood cells stored for less than 8 days and 1,219 patients to standard-issue cells stored for a mean of 22.4 days. The study was conducted at 64 centers in Europe and Canada, where all blood units were leukoreduced and SAGM (saline-adenine-glucose-mannitol) suspended. Similar products are supplied in the United States, but red cells are suspended in additive solution 3 (AS3) rather than SAGM.
At 90 days, 37% of patients in the fresh-blood group and 35.3% of patients in the standard blood group had died. The survival analysis of the time to death showed a hazard ratio of those in the fresh-blood group was 1.1, compared with those in the standard blood group (95% confidence interval, 0.9-1.2; P = .38).
There were no significant differences in the rates of death, organ failure, acute respiratory distress, cardiovascular complications, thrombosis, infection, or acute transfusion reaction.
There also were no significant differences between the two groups in length of hospital stay or duration of supportive care such as mechanical ventilation, as was simultaneously reported in the March 17 edition of the New England Journal of Medicine (doi:10.1056/NEJMoa1500704).
“Although [other] initial studies showed an association between longer red-cell storage and adverse outcomes, these associations may have been spurious owing to sicker patients receiving more units with longer storage, the overlap between comparison groups in the age of the red cells transfused, and the inclusion of transfusions that occurred after the clinical events,” Dr. Jacque Lacroix of University of Montreal and his coauthors wrote.
The study was supported by the Canadian Institutes of Health Research, Fonds de Recherche du Québec–Santé, the National Institute for Health Research Evaluation, the French Ministry of Health, and the Etablissement Français du Sang, and Sanquin Blood Supply. Two authors reported grants and personal fees from pharmaceutical companies outside the submitted work, while others reported financial support from the study funding sources.
The use of fresh red blood cells for transfusion did not reduce mortality or improve other outcomes, compared with older standard-issue red cells, according to results of a multicenter, blinded, randomized prospective study presented at the annual meeting of the International Society on Intensive Care and Emergency Medicine.
In the Age of Blood Evaluation (ABLE) study, researchers randomized 1,211 critically ill patients to red blood cells stored for less than 8 days and 1,219 patients to standard-issue cells stored for a mean of 22.4 days. The study was conducted at 64 centers in Europe and Canada, where all blood units were leukoreduced and SAGM (saline-adenine-glucose-mannitol) suspended. Similar products are supplied in the United States, but red cells are suspended in additive solution 3 (AS3) rather than SAGM.
At 90 days, 37% of patients in the fresh-blood group and 35.3% of patients in the standard blood group had died. The survival analysis of the time to death showed a hazard ratio of those in the fresh-blood group was 1.1, compared with those in the standard blood group (95% confidence interval, 0.9-1.2; P = .38).
There were no significant differences in the rates of death, organ failure, acute respiratory distress, cardiovascular complications, thrombosis, infection, or acute transfusion reaction.
There also were no significant differences between the two groups in length of hospital stay or duration of supportive care such as mechanical ventilation, as was simultaneously reported in the March 17 edition of the New England Journal of Medicine (doi:10.1056/NEJMoa1500704).
“Although [other] initial studies showed an association between longer red-cell storage and adverse outcomes, these associations may have been spurious owing to sicker patients receiving more units with longer storage, the overlap between comparison groups in the age of the red cells transfused, and the inclusion of transfusions that occurred after the clinical events,” Dr. Jacque Lacroix of University of Montreal and his coauthors wrote.
The study was supported by the Canadian Institutes of Health Research, Fonds de Recherche du Québec–Santé, the National Institute for Health Research Evaluation, the French Ministry of Health, and the Etablissement Français du Sang, and Sanquin Blood Supply. Two authors reported grants and personal fees from pharmaceutical companies outside the submitted work, while others reported financial support from the study funding sources.
Key clinical point: Fresh red blood cells didn’t provide any additional gains in outcomes or reduce mortality at 90 days.
Major finding: The survival analysis of the time to death showed a hazard ratio of those in the fresh-blood group was 1.1, compared to those in the standard blood group (95% confidence interval, 0.9-1.2) (P = .38).
Data source: A multicenter, blinded, randomized prospective study in 2,430 patients receiving red blood cell transfusions.
Disclosures: The study was supported by the Canadian Institutes of Health Research, Fonds de Recherche du Québec–Santé, the National Institute for Health Research Evaluation, the French Ministry of Health, and the Etablissement Français du Sang, and Sanquin Blood Supply. Two authors reported grants and personal fees from pharmaceutical companies outside the submitted work, while others reported financial support from the study funding sources.
States expand Medicaid through unique approaches
State government officials are getting creative in their efforts to expand Medicaid under the Affordable Care Act.
After the 2014 election, some states sought to expand their Medicaid programs “with some kind of special arrangement in an attempt to fine tune it to their specific state needs and political objectives,” James F. Blumstein, a constitutional and health law professor at Vanderbilt University in Nashville, said in an interview. The Republican-controlled Congress is a key reason why, he said. “The Obama [administration] realized if they didn’t make some substantial concessions [in the form of Medicaid waivers] to various local political needs and goals, that those states would not have expanded.”
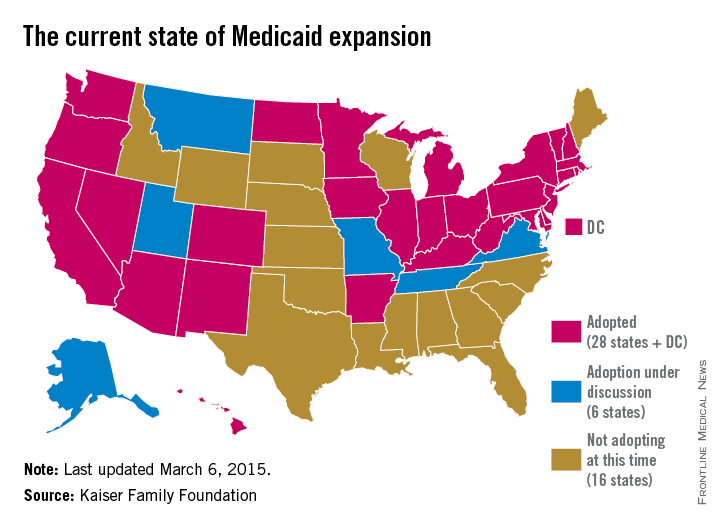
While at least 12 states chose to expand Medicaid in the 2 years immediately after ACA enactment, others held back.
Debate over the ideal expansion plan – and refusal by some states to expand – is largely based on political views, budget concerns, and resistance to federal programs, Robin Rudowitz, associate director for the Kaiser Commission on Medicaid and the Uninsured said during a webinar.
“Some of the states that have opposed have certainly [refused to expand] on ideological grounds,” she said during the presentation. “Some states have cited concerns about cost. Some states are concerned about the federal government’s commitment to maintain the high match.”
So far, six states have earned a federal waiver to create their own brand of Medicaid reform; New Hampshire is the latest. Gov. Maggie Hassan (D) announced on March 5 that the Centers for Medicare & Medicaid Services approved her state’s waiver to expand the New Hampshire Health Protection Program. New Hampshire’s plan implements mandatory qualified health plan (QHP) premium assistance for new patients to purchase coverage. QHPs refer to health plans that are certified by the federal health insurance marketplace, provide essential health benefits, follow established limits on cost-sharing, and meet other federal requirements. New Hampshire’s plan also includes the authority to waive retroactive coverage, a provision that has not been approved in other states.
Expansion waivers approved in Arkansas and Iowa follow similar QHP approaches. Arkansas’s expansion program, approved by CMS through December 2016, allows the state to implement Medicaid expansion through a premium assistance model that uses federal Medicaid funds to purchase coverage through QHPs. Iowa is using the same premium assistance model and also received approval for another option that provides Medicaid coverage through a medical home model for patients with incomes up to 100% of the federal poverty line (FPL) and for medically frail patients up to 138% of the FPL. Meanwhile, Michigan’s alternative program, called Healthy Michigan allows patients to participate in health savings accounts that can be used for required cost-sharing payments. Pennsylvania is transitioning from an approved alternative model to a traditional expansion approach. Former Pennsylvania Gov. Tom Corbett’s (R) Healthy PA program was undone when Gov. Tom Wolf (D) took office. Gov. Wolf plans to move the state to a traditional expansion by Sept. 1.
Indiana’s expansion approach is perhaps the most unique. Similar to other waivers, the state’s plan includes premium assistance and monthly contributions by patients to a personal health savings account. However, unlike other states, Indiana can prevent beneficiaries from reenrolling in coverage for 6 months if they are disenrolled for nonpayment of premiums. The plan also provides a less-generous benefit package to newly eligible beneficiaries at or below the federal poverty level who do not pay premiums. To receive the more generous benefit package, even patients with very little or no income must pay premiums of $1 per month, and medically frail patients above the federal poverty level who do not pay premiums must pay state plan copayments.
Indiana’s expansion encourages personal responsibility by patients, Gov. Mike Pence(R) said in a statement. “We have worked hard to ensure that low-income Hoosiers have access to a health care plan that empowers them to take charge of their health and prepares them to move to private insurance as they improve their lives.”
But constitutional and health law professor David Orentlicher of Indiana University, Indianapolis, said that he believes the expansion may backfire.
“When patients are expected to pay more for their health care, whether through increases in premiums, deductibles, or copayments, they are less able to afford health care,” Mr. Orentlicher said in an interview. “For low-income persons, that can mean not filling prescriptions or seeing a physician when sick. As a result, the health of poor patients may suffer.”
Indiana’s expansion could encourage more states to adopt similar approaches. “It’s important to understand what CMS has approved and what they have said they would deny because these actions set the guideposts and parameters for other states that are considering waiver approaches to implement the expansion,” Ms. Rudowitz said during the webinar.
Traditional Medicaid expansion bills are currently under consideration in Florida, Montana, and Alaska. In other states, alternative Medicaid expansions has been voted down. The Utah House on March 5 killed Gov. Gary Herbert’s (R) Healthy Utah plan in a 16-56 vote. The proposal would have covered residents earning up to 138% of the poverty line. Instead, the Utah House on Mar. 6 passed Utah Cares, an expansion plan that would use traditional Medicaid and the state’s Primary Care Network to provide limited health care to Utahans earning up to 100% of the poverty line. That bill, sponsored by House Majority Leader Jim Dunnigan (R), has been sent on to the state senate.
And in February, a Senate panel defeated Tennessee Gov. Bill Haslam’s alternative plan to expand Medicaid under the ACA. Tennessee was widely seen as the next Republican state that could expand Medicaid, with Gov. Haslam negotiating for months with the federal government for a plan that included conservative policy elements. The governor’s Insure Tennessee plan had included two coverage tracks for patients making less than 138% of the poverty level. One plan included defined contributions for beneficiaries with employer-sponsored plans to help them pay for premiums and copays. The other option would have created health savings accounts for consumers who can earn credits to pay for health care costs by engaging in healthy behaviors.
A wild card in the future of Medicaid expansions is the case of King v. Burwell before the Supreme Court, Mr. Blumstein said. Justices are weighing whether patients in states that use the federal exchange can receive federal tax credits to buy insurance or whether the credits apply only in state-run exchanges The high court heard oral arguments in the case March 4. Some states, such as North Carolina, will not consider expanding until after the court rules.
If the court rules for the plaintiffs, “there’s going to have to be a reassessment,” Mr. Blumstein said. “The Legislature and various states will have to figure out how they want to handle Medicaid expansion and whether they want to get into the business of handling an exchange. It adds a level of complexity.”
On Twitter @legal_med
State government officials are getting creative in their efforts to expand Medicaid under the Affordable Care Act.
After the 2014 election, some states sought to expand their Medicaid programs “with some kind of special arrangement in an attempt to fine tune it to their specific state needs and political objectives,” James F. Blumstein, a constitutional and health law professor at Vanderbilt University in Nashville, said in an interview. The Republican-controlled Congress is a key reason why, he said. “The Obama [administration] realized if they didn’t make some substantial concessions [in the form of Medicaid waivers] to various local political needs and goals, that those states would not have expanded.”
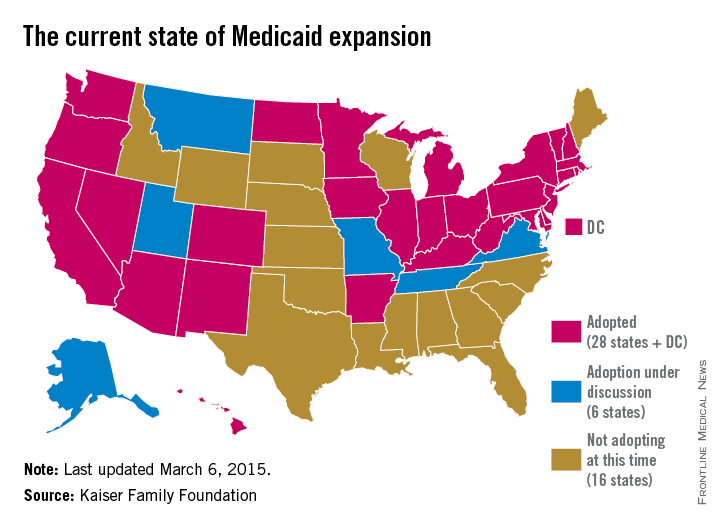
While at least 12 states chose to expand Medicaid in the 2 years immediately after ACA enactment, others held back.
Debate over the ideal expansion plan – and refusal by some states to expand – is largely based on political views, budget concerns, and resistance to federal programs, Robin Rudowitz, associate director for the Kaiser Commission on Medicaid and the Uninsured said during a webinar.
“Some of the states that have opposed have certainly [refused to expand] on ideological grounds,” she said during the presentation. “Some states have cited concerns about cost. Some states are concerned about the federal government’s commitment to maintain the high match.”
So far, six states have earned a federal waiver to create their own brand of Medicaid reform; New Hampshire is the latest. Gov. Maggie Hassan (D) announced on March 5 that the Centers for Medicare & Medicaid Services approved her state’s waiver to expand the New Hampshire Health Protection Program. New Hampshire’s plan implements mandatory qualified health plan (QHP) premium assistance for new patients to purchase coverage. QHPs refer to health plans that are certified by the federal health insurance marketplace, provide essential health benefits, follow established limits on cost-sharing, and meet other federal requirements. New Hampshire’s plan also includes the authority to waive retroactive coverage, a provision that has not been approved in other states.
Expansion waivers approved in Arkansas and Iowa follow similar QHP approaches. Arkansas’s expansion program, approved by CMS through December 2016, allows the state to implement Medicaid expansion through a premium assistance model that uses federal Medicaid funds to purchase coverage through QHPs. Iowa is using the same premium assistance model and also received approval for another option that provides Medicaid coverage through a medical home model for patients with incomes up to 100% of the federal poverty line (FPL) and for medically frail patients up to 138% of the FPL. Meanwhile, Michigan’s alternative program, called Healthy Michigan allows patients to participate in health savings accounts that can be used for required cost-sharing payments. Pennsylvania is transitioning from an approved alternative model to a traditional expansion approach. Former Pennsylvania Gov. Tom Corbett’s (R) Healthy PA program was undone when Gov. Tom Wolf (D) took office. Gov. Wolf plans to move the state to a traditional expansion by Sept. 1.
Indiana’s expansion approach is perhaps the most unique. Similar to other waivers, the state’s plan includes premium assistance and monthly contributions by patients to a personal health savings account. However, unlike other states, Indiana can prevent beneficiaries from reenrolling in coverage for 6 months if they are disenrolled for nonpayment of premiums. The plan also provides a less-generous benefit package to newly eligible beneficiaries at or below the federal poverty level who do not pay premiums. To receive the more generous benefit package, even patients with very little or no income must pay premiums of $1 per month, and medically frail patients above the federal poverty level who do not pay premiums must pay state plan copayments.
Indiana’s expansion encourages personal responsibility by patients, Gov. Mike Pence(R) said in a statement. “We have worked hard to ensure that low-income Hoosiers have access to a health care plan that empowers them to take charge of their health and prepares them to move to private insurance as they improve their lives.”
But constitutional and health law professor David Orentlicher of Indiana University, Indianapolis, said that he believes the expansion may backfire.
“When patients are expected to pay more for their health care, whether through increases in premiums, deductibles, or copayments, they are less able to afford health care,” Mr. Orentlicher said in an interview. “For low-income persons, that can mean not filling prescriptions or seeing a physician when sick. As a result, the health of poor patients may suffer.”
Indiana’s expansion could encourage more states to adopt similar approaches. “It’s important to understand what CMS has approved and what they have said they would deny because these actions set the guideposts and parameters for other states that are considering waiver approaches to implement the expansion,” Ms. Rudowitz said during the webinar.
Traditional Medicaid expansion bills are currently under consideration in Florida, Montana, and Alaska. In other states, alternative Medicaid expansions has been voted down. The Utah House on March 5 killed Gov. Gary Herbert’s (R) Healthy Utah plan in a 16-56 vote. The proposal would have covered residents earning up to 138% of the poverty line. Instead, the Utah House on Mar. 6 passed Utah Cares, an expansion plan that would use traditional Medicaid and the state’s Primary Care Network to provide limited health care to Utahans earning up to 100% of the poverty line. That bill, sponsored by House Majority Leader Jim Dunnigan (R), has been sent on to the state senate.
And in February, a Senate panel defeated Tennessee Gov. Bill Haslam’s alternative plan to expand Medicaid under the ACA. Tennessee was widely seen as the next Republican state that could expand Medicaid, with Gov. Haslam negotiating for months with the federal government for a plan that included conservative policy elements. The governor’s Insure Tennessee plan had included two coverage tracks for patients making less than 138% of the poverty level. One plan included defined contributions for beneficiaries with employer-sponsored plans to help them pay for premiums and copays. The other option would have created health savings accounts for consumers who can earn credits to pay for health care costs by engaging in healthy behaviors.
A wild card in the future of Medicaid expansions is the case of King v. Burwell before the Supreme Court, Mr. Blumstein said. Justices are weighing whether patients in states that use the federal exchange can receive federal tax credits to buy insurance or whether the credits apply only in state-run exchanges The high court heard oral arguments in the case March 4. Some states, such as North Carolina, will not consider expanding until after the court rules.
If the court rules for the plaintiffs, “there’s going to have to be a reassessment,” Mr. Blumstein said. “The Legislature and various states will have to figure out how they want to handle Medicaid expansion and whether they want to get into the business of handling an exchange. It adds a level of complexity.”
On Twitter @legal_med
State government officials are getting creative in their efforts to expand Medicaid under the Affordable Care Act.
After the 2014 election, some states sought to expand their Medicaid programs “with some kind of special arrangement in an attempt to fine tune it to their specific state needs and political objectives,” James F. Blumstein, a constitutional and health law professor at Vanderbilt University in Nashville, said in an interview. The Republican-controlled Congress is a key reason why, he said. “The Obama [administration] realized if they didn’t make some substantial concessions [in the form of Medicaid waivers] to various local political needs and goals, that those states would not have expanded.”
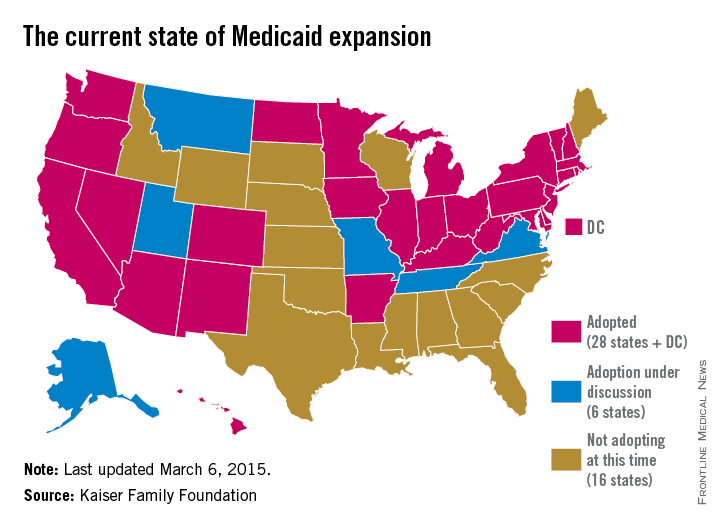
While at least 12 states chose to expand Medicaid in the 2 years immediately after ACA enactment, others held back.
Debate over the ideal expansion plan – and refusal by some states to expand – is largely based on political views, budget concerns, and resistance to federal programs, Robin Rudowitz, associate director for the Kaiser Commission on Medicaid and the Uninsured said during a webinar.
“Some of the states that have opposed have certainly [refused to expand] on ideological grounds,” she said during the presentation. “Some states have cited concerns about cost. Some states are concerned about the federal government’s commitment to maintain the high match.”
So far, six states have earned a federal waiver to create their own brand of Medicaid reform; New Hampshire is the latest. Gov. Maggie Hassan (D) announced on March 5 that the Centers for Medicare & Medicaid Services approved her state’s waiver to expand the New Hampshire Health Protection Program. New Hampshire’s plan implements mandatory qualified health plan (QHP) premium assistance for new patients to purchase coverage. QHPs refer to health plans that are certified by the federal health insurance marketplace, provide essential health benefits, follow established limits on cost-sharing, and meet other federal requirements. New Hampshire’s plan also includes the authority to waive retroactive coverage, a provision that has not been approved in other states.
Expansion waivers approved in Arkansas and Iowa follow similar QHP approaches. Arkansas’s expansion program, approved by CMS through December 2016, allows the state to implement Medicaid expansion through a premium assistance model that uses federal Medicaid funds to purchase coverage through QHPs. Iowa is using the same premium assistance model and also received approval for another option that provides Medicaid coverage through a medical home model for patients with incomes up to 100% of the federal poverty line (FPL) and for medically frail patients up to 138% of the FPL. Meanwhile, Michigan’s alternative program, called Healthy Michigan allows patients to participate in health savings accounts that can be used for required cost-sharing payments. Pennsylvania is transitioning from an approved alternative model to a traditional expansion approach. Former Pennsylvania Gov. Tom Corbett’s (R) Healthy PA program was undone when Gov. Tom Wolf (D) took office. Gov. Wolf plans to move the state to a traditional expansion by Sept. 1.
Indiana’s expansion approach is perhaps the most unique. Similar to other waivers, the state’s plan includes premium assistance and monthly contributions by patients to a personal health savings account. However, unlike other states, Indiana can prevent beneficiaries from reenrolling in coverage for 6 months if they are disenrolled for nonpayment of premiums. The plan also provides a less-generous benefit package to newly eligible beneficiaries at or below the federal poverty level who do not pay premiums. To receive the more generous benefit package, even patients with very little or no income must pay premiums of $1 per month, and medically frail patients above the federal poverty level who do not pay premiums must pay state plan copayments.
Indiana’s expansion encourages personal responsibility by patients, Gov. Mike Pence(R) said in a statement. “We have worked hard to ensure that low-income Hoosiers have access to a health care plan that empowers them to take charge of their health and prepares them to move to private insurance as they improve their lives.”
But constitutional and health law professor David Orentlicher of Indiana University, Indianapolis, said that he believes the expansion may backfire.
“When patients are expected to pay more for their health care, whether through increases in premiums, deductibles, or copayments, they are less able to afford health care,” Mr. Orentlicher said in an interview. “For low-income persons, that can mean not filling prescriptions or seeing a physician when sick. As a result, the health of poor patients may suffer.”
Indiana’s expansion could encourage more states to adopt similar approaches. “It’s important to understand what CMS has approved and what they have said they would deny because these actions set the guideposts and parameters for other states that are considering waiver approaches to implement the expansion,” Ms. Rudowitz said during the webinar.
Traditional Medicaid expansion bills are currently under consideration in Florida, Montana, and Alaska. In other states, alternative Medicaid expansions has been voted down. The Utah House on March 5 killed Gov. Gary Herbert’s (R) Healthy Utah plan in a 16-56 vote. The proposal would have covered residents earning up to 138% of the poverty line. Instead, the Utah House on Mar. 6 passed Utah Cares, an expansion plan that would use traditional Medicaid and the state’s Primary Care Network to provide limited health care to Utahans earning up to 100% of the poverty line. That bill, sponsored by House Majority Leader Jim Dunnigan (R), has been sent on to the state senate.
And in February, a Senate panel defeated Tennessee Gov. Bill Haslam’s alternative plan to expand Medicaid under the ACA. Tennessee was widely seen as the next Republican state that could expand Medicaid, with Gov. Haslam negotiating for months with the federal government for a plan that included conservative policy elements. The governor’s Insure Tennessee plan had included two coverage tracks for patients making less than 138% of the poverty level. One plan included defined contributions for beneficiaries with employer-sponsored plans to help them pay for premiums and copays. The other option would have created health savings accounts for consumers who can earn credits to pay for health care costs by engaging in healthy behaviors.
A wild card in the future of Medicaid expansions is the case of King v. Burwell before the Supreme Court, Mr. Blumstein said. Justices are weighing whether patients in states that use the federal exchange can receive federal tax credits to buy insurance or whether the credits apply only in state-run exchanges The high court heard oral arguments in the case March 4. Some states, such as North Carolina, will not consider expanding until after the court rules.
If the court rules for the plaintiffs, “there’s going to have to be a reassessment,” Mr. Blumstein said. “The Legislature and various states will have to figure out how they want to handle Medicaid expansion and whether they want to get into the business of handling an exchange. It adds a level of complexity.”
On Twitter @legal_med
Trauma bills reintroduced in the U.S. House of Representatives
The American College of Surgeons, along with a coalition of trauma advocates, succeeded in ensuring that two important trauma bills have been reintroduced in the U.S. House of Representatives. H.R. 647, the Access to Life Saving Trauma Care for All Americans Act, at http://goo.gl/w7Naq9 were reintroduced by Reps. Mike Burgess (R-TX) and Gene Green (D-TX). H.R. 647 reauthorizes language from the Public Health Service Act to fund trauma centers—funding that is set to expire this fiscal year. Meanwhile, H.R. 648 reauthorizes Trauma Care Systems Planning Grants, which support state and rural development of trauma systems, as well as pilot projects for implementing and assessing regionalized emergency care models.
The House Energy & Commerce Health Subcommittee convened a hearing on several public health bills in January and followed up with a mark-up in early February that included the trauma bills. Both bills were passed out of committee by voice vote. The full committee has scheduled a mark-up of the same public health bills, including the trauma bills, which are again expected to be passed out of the full committee by voice vote. The House is then expected to bring pieces of trauma legislation to the House floor sometime soon after. Discussions are still ongoing with the Senate at this time; however, former champions of the legislation—Sens. Mark Kirk (R-IL) and Jack Reed (D-RI)—have expressed interest in being the lead sponsors of the legislation on the Senate side.
The American College of Surgeons, along with a coalition of trauma advocates, succeeded in ensuring that two important trauma bills have been reintroduced in the U.S. House of Representatives. H.R. 647, the Access to Life Saving Trauma Care for All Americans Act, at http://goo.gl/w7Naq9 were reintroduced by Reps. Mike Burgess (R-TX) and Gene Green (D-TX). H.R. 647 reauthorizes language from the Public Health Service Act to fund trauma centers—funding that is set to expire this fiscal year. Meanwhile, H.R. 648 reauthorizes Trauma Care Systems Planning Grants, which support state and rural development of trauma systems, as well as pilot projects for implementing and assessing regionalized emergency care models.
The House Energy & Commerce Health Subcommittee convened a hearing on several public health bills in January and followed up with a mark-up in early February that included the trauma bills. Both bills were passed out of committee by voice vote. The full committee has scheduled a mark-up of the same public health bills, including the trauma bills, which are again expected to be passed out of the full committee by voice vote. The House is then expected to bring pieces of trauma legislation to the House floor sometime soon after. Discussions are still ongoing with the Senate at this time; however, former champions of the legislation—Sens. Mark Kirk (R-IL) and Jack Reed (D-RI)—have expressed interest in being the lead sponsors of the legislation on the Senate side.
The American College of Surgeons, along with a coalition of trauma advocates, succeeded in ensuring that two important trauma bills have been reintroduced in the U.S. House of Representatives. H.R. 647, the Access to Life Saving Trauma Care for All Americans Act, at http://goo.gl/w7Naq9 were reintroduced by Reps. Mike Burgess (R-TX) and Gene Green (D-TX). H.R. 647 reauthorizes language from the Public Health Service Act to fund trauma centers—funding that is set to expire this fiscal year. Meanwhile, H.R. 648 reauthorizes Trauma Care Systems Planning Grants, which support state and rural development of trauma systems, as well as pilot projects for implementing and assessing regionalized emergency care models.
The House Energy & Commerce Health Subcommittee convened a hearing on several public health bills in January and followed up with a mark-up in early February that included the trauma bills. Both bills were passed out of committee by voice vote. The full committee has scheduled a mark-up of the same public health bills, including the trauma bills, which are again expected to be passed out of the full committee by voice vote. The House is then expected to bring pieces of trauma legislation to the House floor sometime soon after. Discussions are still ongoing with the Senate at this time; however, former champions of the legislation—Sens. Mark Kirk (R-IL) and Jack Reed (D-RI)—have expressed interest in being the lead sponsors of the legislation on the Senate side.
TTP Program positions are available for 2015-2016
Several institutions participating in the American College of Surgeons (ACS) Transition to Practice (TTP) Program still have TTP Associate positions available for the 2015–2016 academic year. Interested residents and recent residency graduates are encouraged to review the program profiles on the ACS website at https://www.facs.org/education/program/ttp and submit their curriculum vitae to [email protected] with a list of institutions to which they have an interest in applying.
The ACS Division of Education launched the TTP Program in 2013 in response to the identified need for additional surgical training for general surgeons leaving residency. The program is intended to bridge the gap between residency and independent practice. TTP Associates experience increasing autonomy throughout the year in a broad-based clinical setting, build their competence and confidence in general surgery, develop practice management skills, and gain practical experience for the next phase of their careers. Working closely with experienced surgeons, TTP Associates have the ability to concentrate on specific areas within general surgery to refine operative skills based on their career goals.
Several institutions participating in the American College of Surgeons (ACS) Transition to Practice (TTP) Program still have TTP Associate positions available for the 2015–2016 academic year. Interested residents and recent residency graduates are encouraged to review the program profiles on the ACS website at https://www.facs.org/education/program/ttp and submit their curriculum vitae to [email protected] with a list of institutions to which they have an interest in applying.
The ACS Division of Education launched the TTP Program in 2013 in response to the identified need for additional surgical training for general surgeons leaving residency. The program is intended to bridge the gap between residency and independent practice. TTP Associates experience increasing autonomy throughout the year in a broad-based clinical setting, build their competence and confidence in general surgery, develop practice management skills, and gain practical experience for the next phase of their careers. Working closely with experienced surgeons, TTP Associates have the ability to concentrate on specific areas within general surgery to refine operative skills based on their career goals.
Several institutions participating in the American College of Surgeons (ACS) Transition to Practice (TTP) Program still have TTP Associate positions available for the 2015–2016 academic year. Interested residents and recent residency graduates are encouraged to review the program profiles on the ACS website at https://www.facs.org/education/program/ttp and submit their curriculum vitae to [email protected] with a list of institutions to which they have an interest in applying.
The ACS Division of Education launched the TTP Program in 2013 in response to the identified need for additional surgical training for general surgeons leaving residency. The program is intended to bridge the gap between residency and independent practice. TTP Associates experience increasing autonomy throughout the year in a broad-based clinical setting, build their competence and confidence in general surgery, develop practice management skills, and gain practical experience for the next phase of their careers. Working closely with experienced surgeons, TTP Associates have the ability to concentrate on specific areas within general surgery to refine operative skills based on their career goals.