User login
Official Newspaper of the American College of Surgeons
Summit registration open
Registration is open for the American College of Surgeons (ACS) 2015 Leadership & Advocacy Summit, April 18–21, at the JW Marriott, Washington, DC. This fourth annual Summit is a dual meeting that offers volunteer leaders and advocates educational sessions focused on effective surgeon leadership, as well as interactive advocacy training with coordinated visits to congressional offices.
The 2015 Leadership Summit will commence the evening of April 18 with a Welcome Reception and continue the next morning with presentations on moving from transactional to transformational leadership, overcoming resistance to change, and conquering physician burnout. In addition, Michael Burke, JD, an attorney with Kalogredis, Sansweet, Dearden and Burke, Ltd, Wayne, PA, will discuss the key elements of a physician employment agreement. Over lunch, Summit attendees will meet in small groups by state/region to identify areas for unified efforts in the upcoming year.
The Advocacy Summit will begin the evening of Sunday, April 19, with a keynote address by General Stanley McChrystal on the tools for successful leadership. Monday, April 20, attendees will hear from speakers who will discuss the political environment in Washington, DC, and across the nation, and will provide information on the status of important health care issues. Monday’s program will include a luncheon sponsored by the ACS Professional Association’s political action committee (ACSPA-SurgeonsPAC), featuring a talk by Washington Post political reporter Chris Cillizza. Monday evening, the ACSPA-SurgeonsPAC will sponsor another event and a raffle. Tuesday morning, attendees will use what they have learned at the Summit during meetings with their senators and representative and/or congressional staff. This portion of the program provides an opportunity to rally surgery’s collective grassroots advocacy voice on such issues as physician payment, professional liability, and the physician workforce.
For more information or to register for the 2015 Leadership & Advocacy Summit, go to the ACS website at https://www.facs.org/advocacy/participate/summit. Advance registration ends April 10, and the hotel reservation deadline is March 12. Rooms are going quickly, so make your reservations now.
Registration is open for the American College of Surgeons (ACS) 2015 Leadership & Advocacy Summit, April 18–21, at the JW Marriott, Washington, DC. This fourth annual Summit is a dual meeting that offers volunteer leaders and advocates educational sessions focused on effective surgeon leadership, as well as interactive advocacy training with coordinated visits to congressional offices.
The 2015 Leadership Summit will commence the evening of April 18 with a Welcome Reception and continue the next morning with presentations on moving from transactional to transformational leadership, overcoming resistance to change, and conquering physician burnout. In addition, Michael Burke, JD, an attorney with Kalogredis, Sansweet, Dearden and Burke, Ltd, Wayne, PA, will discuss the key elements of a physician employment agreement. Over lunch, Summit attendees will meet in small groups by state/region to identify areas for unified efforts in the upcoming year.
The Advocacy Summit will begin the evening of Sunday, April 19, with a keynote address by General Stanley McChrystal on the tools for successful leadership. Monday, April 20, attendees will hear from speakers who will discuss the political environment in Washington, DC, and across the nation, and will provide information on the status of important health care issues. Monday’s program will include a luncheon sponsored by the ACS Professional Association’s political action committee (ACSPA-SurgeonsPAC), featuring a talk by Washington Post political reporter Chris Cillizza. Monday evening, the ACSPA-SurgeonsPAC will sponsor another event and a raffle. Tuesday morning, attendees will use what they have learned at the Summit during meetings with their senators and representative and/or congressional staff. This portion of the program provides an opportunity to rally surgery’s collective grassroots advocacy voice on such issues as physician payment, professional liability, and the physician workforce.
For more information or to register for the 2015 Leadership & Advocacy Summit, go to the ACS website at https://www.facs.org/advocacy/participate/summit. Advance registration ends April 10, and the hotel reservation deadline is March 12. Rooms are going quickly, so make your reservations now.
Registration is open for the American College of Surgeons (ACS) 2015 Leadership & Advocacy Summit, April 18–21, at the JW Marriott, Washington, DC. This fourth annual Summit is a dual meeting that offers volunteer leaders and advocates educational sessions focused on effective surgeon leadership, as well as interactive advocacy training with coordinated visits to congressional offices.
The 2015 Leadership Summit will commence the evening of April 18 with a Welcome Reception and continue the next morning with presentations on moving from transactional to transformational leadership, overcoming resistance to change, and conquering physician burnout. In addition, Michael Burke, JD, an attorney with Kalogredis, Sansweet, Dearden and Burke, Ltd, Wayne, PA, will discuss the key elements of a physician employment agreement. Over lunch, Summit attendees will meet in small groups by state/region to identify areas for unified efforts in the upcoming year.
The Advocacy Summit will begin the evening of Sunday, April 19, with a keynote address by General Stanley McChrystal on the tools for successful leadership. Monday, April 20, attendees will hear from speakers who will discuss the political environment in Washington, DC, and across the nation, and will provide information on the status of important health care issues. Monday’s program will include a luncheon sponsored by the ACS Professional Association’s political action committee (ACSPA-SurgeonsPAC), featuring a talk by Washington Post political reporter Chris Cillizza. Monday evening, the ACSPA-SurgeonsPAC will sponsor another event and a raffle. Tuesday morning, attendees will use what they have learned at the Summit during meetings with their senators and representative and/or congressional staff. This portion of the program provides an opportunity to rally surgery’s collective grassroots advocacy voice on such issues as physician payment, professional liability, and the physician workforce.
For more information or to register for the 2015 Leadership & Advocacy Summit, go to the ACS website at https://www.facs.org/advocacy/participate/summit. Advance registration ends April 10, and the hotel reservation deadline is March 12. Rooms are going quickly, so make your reservations now.
Surgery Oral Board Review Courses still available in 2015
Two Clinical Performance and Oral Examinations in Surgery courses will take place on the East Coast in 2015, including Amelia Island, FL, May 7–12; and Stowe, VT, September 16–21. Register online now for 2015 courses at http://www.oralboardreview.net/.
The course provides an opportunity for surgeons who have not passed the certifying examination or senior residents/fellows who anticipate difficulty with the certifying examination to receive individual feedback on their oral examination skills and knowledge base. The expanded course will begin with an evening reception on the first day and allow for more individual assessment. All participants will be videotaped in a mock certifying examination on the fifth day of the course and participate in a debriefing session on the final day. Each debriefing will include a behavioral analysis, areas of content weakness, a plan, and questions for review along with a video of the participant’s mock exam. View a full description of the course at http://www.oralboardreview.net. Direct questions about the program to Pamela Rowland, PhD, at [email protected], or [email protected], or by phone, 603-359-0824.
Two Clinical Performance and Oral Examinations in Surgery courses will take place on the East Coast in 2015, including Amelia Island, FL, May 7–12; and Stowe, VT, September 16–21. Register online now for 2015 courses at http://www.oralboardreview.net/.
The course provides an opportunity for surgeons who have not passed the certifying examination or senior residents/fellows who anticipate difficulty with the certifying examination to receive individual feedback on their oral examination skills and knowledge base. The expanded course will begin with an evening reception on the first day and allow for more individual assessment. All participants will be videotaped in a mock certifying examination on the fifth day of the course and participate in a debriefing session on the final day. Each debriefing will include a behavioral analysis, areas of content weakness, a plan, and questions for review along with a video of the participant’s mock exam. View a full description of the course at http://www.oralboardreview.net. Direct questions about the program to Pamela Rowland, PhD, at [email protected], or [email protected], or by phone, 603-359-0824.
Two Clinical Performance and Oral Examinations in Surgery courses will take place on the East Coast in 2015, including Amelia Island, FL, May 7–12; and Stowe, VT, September 16–21. Register online now for 2015 courses at http://www.oralboardreview.net/.
The course provides an opportunity for surgeons who have not passed the certifying examination or senior residents/fellows who anticipate difficulty with the certifying examination to receive individual feedback on their oral examination skills and knowledge base. The expanded course will begin with an evening reception on the first day and allow for more individual assessment. All participants will be videotaped in a mock certifying examination on the fifth day of the course and participate in a debriefing session on the final day. Each debriefing will include a behavioral analysis, areas of content weakness, a plan, and questions for review along with a video of the participant’s mock exam. View a full description of the course at http://www.oralboardreview.net. Direct questions about the program to Pamela Rowland, PhD, at [email protected], or [email protected], or by phone, 603-359-0824.
Double bubble: Concomitant hernia repair and bariatric surgery
CHICAGO – Combining hiatal hernia repair with bariatric surgery is feasible and safe, with no intraoperative complications or deaths reported in a series of 83 patients.
“Concomitant repair of hiatal hernia during these operations can be technically challenging but is a more efficient way of handling this pathology than undergoing separate procedures,” study author Dr. John Rodriguez, from the Cleveland Clinic, said at the annual meeting of the Central Surgical Association.
The presence of a hiatal hernia can play an important role when sizing a pouch or performing a dissection and can make it difficult to have consistent outcomes or gastric sleeves if the complete stomach can’t be visualized, he explained. Hernias can prevent weight gain but also prevent resolution of reflux symptoms.
Prospectively collected data from 83 patients who underwent concomitant hernia repair and bariatric surgery were retrospectively, compared with 83 historic controls who underwent bariatric surgery alone. The two groups were well-matched with regard to age (57.2 years vs. 56.2 years), weight (118.4 kg vs. 119.9 kg), and body mass index (BMI) (44.5 kg/m2vs. 44.6 kg/m2), although diabetes was significantly more common in controls (13.2% vs. 38.5%).
In the study group, hernias were classified as Type I in 47 patients, Type II in 5, Type III in 28, and Type IV in 3. Primary hernia repair was performed in all patients, using anterior reconstruction in 45, posterior reconstruction in 21, posterior reconstruction plus mesh in 7, and an unspecified approach in 10.
Operative time was slightly longer with the addition of hernia repair, but the difference did not reach statistical significance (164.4 minutes vs. 147.5 minutes; P = .07), Dr. Rodriguez said. Average hospital length of stay was nearly identical at 3.5 vs. 3.4 days (P = .09).
In all, 24 patients undergoing concomitant surgery described having early postoperative symptoms such as nausea, dysphagia, abdominal pain, reflux, and dehydration, compared with 15 controls. But, again the difference was not significant (33.7% vs. 18%; P = .09), he said.
Three study patients had late postoperative complications after 1 year requiring esophagogastroduodenoscopy caused by one each of stenosis, hernia recurrence, and marginal ulcer. Among controls, there were four late marginal ulcers and two stenoses (P = .3).
Notably, hiatal hernia was diagnosed intraoperatively in a full 61.4% of the study group. Obesity is an established risk factor for hiatal hernia, although many patients who present for bariatric surgery are asymptomatic, Dr. Rodriguez observed.
At 12 months, patients undergoing bariatric surgery with and without concomitant hernia repair had similar weight loss (80.7 kg vs. 87.4 kg; P = .1) and final BMI (30 kg/m2 vs. 32.5 kg/m2; P = .06).
Use of antireflux medication, however, was significantly higher in those without concomitant surgery (38.5% vs. 43.7%; P = .01), he said. Gastroesophageal reflux disease (GERD) symptoms were present in 84.3% of study patients and 77% of controls at baseline.
Antireflux medication use declined in 66% of patients undergoing laparoscopic Roux en-Y gastric bypass vs. 50% undergoing only laparoscopic sleeve gastrectomy. Surgical approach did not affect weight loss (59.7 kg vs. 51.8 kg) or final BMI (30.3 kg/m2 vs. 32.4 kg/m2).
“The true incidence of hiatal hernia in the obese is likely underestimated,” Dr. Rodriguez said. “Concomitant repair is safe and may prevent further symptoms.”
Limitations of the study were the small, retrospective cohort, a lack of standardized GERD symptom scoring and objective GERD testing, and no uniform hiatal hernia repair. Standardized approaches may improve outcomes during combined procedures, he said.
During a discussion of the results, Dr. Peter T. Hallowell, an audience member from the University of Virginia, Charlottesville, rose to say this is “information we urgently need in bariatric surgery.”
Dr. Rodriguez and his coauthors reported having no financial conflicts.
CHICAGO – Combining hiatal hernia repair with bariatric surgery is feasible and safe, with no intraoperative complications or deaths reported in a series of 83 patients.
“Concomitant repair of hiatal hernia during these operations can be technically challenging but is a more efficient way of handling this pathology than undergoing separate procedures,” study author Dr. John Rodriguez, from the Cleveland Clinic, said at the annual meeting of the Central Surgical Association.
The presence of a hiatal hernia can play an important role when sizing a pouch or performing a dissection and can make it difficult to have consistent outcomes or gastric sleeves if the complete stomach can’t be visualized, he explained. Hernias can prevent weight gain but also prevent resolution of reflux symptoms.
Prospectively collected data from 83 patients who underwent concomitant hernia repair and bariatric surgery were retrospectively, compared with 83 historic controls who underwent bariatric surgery alone. The two groups were well-matched with regard to age (57.2 years vs. 56.2 years), weight (118.4 kg vs. 119.9 kg), and body mass index (BMI) (44.5 kg/m2vs. 44.6 kg/m2), although diabetes was significantly more common in controls (13.2% vs. 38.5%).
In the study group, hernias were classified as Type I in 47 patients, Type II in 5, Type III in 28, and Type IV in 3. Primary hernia repair was performed in all patients, using anterior reconstruction in 45, posterior reconstruction in 21, posterior reconstruction plus mesh in 7, and an unspecified approach in 10.
Operative time was slightly longer with the addition of hernia repair, but the difference did not reach statistical significance (164.4 minutes vs. 147.5 minutes; P = .07), Dr. Rodriguez said. Average hospital length of stay was nearly identical at 3.5 vs. 3.4 days (P = .09).
In all, 24 patients undergoing concomitant surgery described having early postoperative symptoms such as nausea, dysphagia, abdominal pain, reflux, and dehydration, compared with 15 controls. But, again the difference was not significant (33.7% vs. 18%; P = .09), he said.
Three study patients had late postoperative complications after 1 year requiring esophagogastroduodenoscopy caused by one each of stenosis, hernia recurrence, and marginal ulcer. Among controls, there were four late marginal ulcers and two stenoses (P = .3).
Notably, hiatal hernia was diagnosed intraoperatively in a full 61.4% of the study group. Obesity is an established risk factor for hiatal hernia, although many patients who present for bariatric surgery are asymptomatic, Dr. Rodriguez observed.
At 12 months, patients undergoing bariatric surgery with and without concomitant hernia repair had similar weight loss (80.7 kg vs. 87.4 kg; P = .1) and final BMI (30 kg/m2 vs. 32.5 kg/m2; P = .06).
Use of antireflux medication, however, was significantly higher in those without concomitant surgery (38.5% vs. 43.7%; P = .01), he said. Gastroesophageal reflux disease (GERD) symptoms were present in 84.3% of study patients and 77% of controls at baseline.
Antireflux medication use declined in 66% of patients undergoing laparoscopic Roux en-Y gastric bypass vs. 50% undergoing only laparoscopic sleeve gastrectomy. Surgical approach did not affect weight loss (59.7 kg vs. 51.8 kg) or final BMI (30.3 kg/m2 vs. 32.4 kg/m2).
“The true incidence of hiatal hernia in the obese is likely underestimated,” Dr. Rodriguez said. “Concomitant repair is safe and may prevent further symptoms.”
Limitations of the study were the small, retrospective cohort, a lack of standardized GERD symptom scoring and objective GERD testing, and no uniform hiatal hernia repair. Standardized approaches may improve outcomes during combined procedures, he said.
During a discussion of the results, Dr. Peter T. Hallowell, an audience member from the University of Virginia, Charlottesville, rose to say this is “information we urgently need in bariatric surgery.”
Dr. Rodriguez and his coauthors reported having no financial conflicts.
CHICAGO – Combining hiatal hernia repair with bariatric surgery is feasible and safe, with no intraoperative complications or deaths reported in a series of 83 patients.
“Concomitant repair of hiatal hernia during these operations can be technically challenging but is a more efficient way of handling this pathology than undergoing separate procedures,” study author Dr. John Rodriguez, from the Cleveland Clinic, said at the annual meeting of the Central Surgical Association.
The presence of a hiatal hernia can play an important role when sizing a pouch or performing a dissection and can make it difficult to have consistent outcomes or gastric sleeves if the complete stomach can’t be visualized, he explained. Hernias can prevent weight gain but also prevent resolution of reflux symptoms.
Prospectively collected data from 83 patients who underwent concomitant hernia repair and bariatric surgery were retrospectively, compared with 83 historic controls who underwent bariatric surgery alone. The two groups were well-matched with regard to age (57.2 years vs. 56.2 years), weight (118.4 kg vs. 119.9 kg), and body mass index (BMI) (44.5 kg/m2vs. 44.6 kg/m2), although diabetes was significantly more common in controls (13.2% vs. 38.5%).
In the study group, hernias were classified as Type I in 47 patients, Type II in 5, Type III in 28, and Type IV in 3. Primary hernia repair was performed in all patients, using anterior reconstruction in 45, posterior reconstruction in 21, posterior reconstruction plus mesh in 7, and an unspecified approach in 10.
Operative time was slightly longer with the addition of hernia repair, but the difference did not reach statistical significance (164.4 minutes vs. 147.5 minutes; P = .07), Dr. Rodriguez said. Average hospital length of stay was nearly identical at 3.5 vs. 3.4 days (P = .09).
In all, 24 patients undergoing concomitant surgery described having early postoperative symptoms such as nausea, dysphagia, abdominal pain, reflux, and dehydration, compared with 15 controls. But, again the difference was not significant (33.7% vs. 18%; P = .09), he said.
Three study patients had late postoperative complications after 1 year requiring esophagogastroduodenoscopy caused by one each of stenosis, hernia recurrence, and marginal ulcer. Among controls, there were four late marginal ulcers and two stenoses (P = .3).
Notably, hiatal hernia was diagnosed intraoperatively in a full 61.4% of the study group. Obesity is an established risk factor for hiatal hernia, although many patients who present for bariatric surgery are asymptomatic, Dr. Rodriguez observed.
At 12 months, patients undergoing bariatric surgery with and without concomitant hernia repair had similar weight loss (80.7 kg vs. 87.4 kg; P = .1) and final BMI (30 kg/m2 vs. 32.5 kg/m2; P = .06).
Use of antireflux medication, however, was significantly higher in those without concomitant surgery (38.5% vs. 43.7%; P = .01), he said. Gastroesophageal reflux disease (GERD) symptoms were present in 84.3% of study patients and 77% of controls at baseline.
Antireflux medication use declined in 66% of patients undergoing laparoscopic Roux en-Y gastric bypass vs. 50% undergoing only laparoscopic sleeve gastrectomy. Surgical approach did not affect weight loss (59.7 kg vs. 51.8 kg) or final BMI (30.3 kg/m2 vs. 32.4 kg/m2).
“The true incidence of hiatal hernia in the obese is likely underestimated,” Dr. Rodriguez said. “Concomitant repair is safe and may prevent further symptoms.”
Limitations of the study were the small, retrospective cohort, a lack of standardized GERD symptom scoring and objective GERD testing, and no uniform hiatal hernia repair. Standardized approaches may improve outcomes during combined procedures, he said.
During a discussion of the results, Dr. Peter T. Hallowell, an audience member from the University of Virginia, Charlottesville, rose to say this is “information we urgently need in bariatric surgery.”
Dr. Rodriguez and his coauthors reported having no financial conflicts.
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: Hiatal hernia repair during bariatric surgery is feasible and safe.
Major finding: Concomitant hernia repair added 16.9 minutes to surgery, but did not significantly increase short- or long-term complications.
Data source: Retrospective study of 83 patients undergoing hiatal hernia repair during bariatric surgery and 83 historic controls.
Disclosures: Dr. Rodriguez and his coauthors reported having no financial conflicts.
Acute diverticulitis: Call in the surgical specialist, or maybe not?
CHICAGO – Surgical outcomes of acute, complicated diverticulitis are equivalent regardless of whether a colorectal or general surgeon wields the scalpel, a multicenter study showed.
There was no difference between the colorectal surgery (CRS) and general surgery groups for the primary outcomes of 90-day morbidity (26% vs 28%; P = .76), readmission (32% vs. 25%; P = .48), and length of stay (both median 9 days; P = .82).
Surgeon specialization was not associated with any of the outcomes in multivariate regression that accounted for patient demographics, surgeon type, and disease characteristics, study author Capt. G. Paul Wright, U.S. Army Reserve Medical Corps, reported at the annual meeting of the Central Surgical Association.
The authors tackled the controversial issue in light of recent data suggesting improved acute, complicated diverticulitis surgery outcomes in the hands of specialized surgeons. A 2014 study reported that colorectal surgeons were less likely than general surgeons to use a Hartmann’s procedure and had reduced LOS and time to stoma reversal (J. Am. Coll. Surg. 2014;218:1156-61).
The current analysis involved 115 consecutive patients with acute, complicated diverticulitis who underwent emergent surgery with either a colorectal surgeon (n = 62) or general surgeon (n = 53) at two university-affiliated hospitals from 2006 to 2013. Age, Charlson Comorbidity Index, and American Society of Anesthesiologists class were similar between groups.
The colorectal surgeon group (CRS), however, was significantly more likely to have had previous episodes of diverticulitis (58% vs. 25%; P < .001), likely representing a referral bias or preexisting relationship with their surgeon, Dr. Wright said.
The general surgeon (GS) group had a significantly higher number of Systemic Inflammatory Response Syndrome criteria (P = .009 for all groups), higher rates of Hinchey class 3 disease (59% vs. 32%: P = .02), and ICU admissions (25% vs. 7%; P = .006).
The most common procedure among general surgeons was a Hartmann’s procedure (64% vs. 34%; P < .001), whereas colorectal surgeons favored primary anastomosis with diverting ileostomy (45% vs. 0%; P < .001), Dr. Wright, from Grand Rapids Medical Education Partners and Michigan State University, both in Grand Rapids, reported.
General surgeons were more likely to close the skin (85% vs. 50%), while in the CRS group the skin was left partially or completely open in 50% of patients. Operative time at the index admission was an average of 36 minutes longer in the CRS group (mean 164 minutes vs. 128 minutes; P = .005).
The CRS group had a higher rate of stoma reversal (78% vs 65%) and shorter time to stoma reversal (4 months vs. 4.7 months), but the difference was not statistically significant. The CRS group had a significantly shorter stoma reversal OR duration (mean 106 minutes vs. 182 minutes; P = .0010) and stoma reversal length of stay (mean 4 days vs. 7 days; P < .001).
“As general surgeons will no doubt continue to care for acute diverticulitis, increased use of primary anastomosis with proximal diversion when appropriate may be warranted due to the secondary benefits seen in stoma reversal,” Dr. Wright said.
Mortality was low and similar, at just one death in the CRS and two in the GS group.
Invited discussant William Cirocco, from Ohio State University in Columbus, said the type of surgical intervention is just one aspect in the management of patients with diverticulitis.
“An additional nonoperative approach may lead to conversion of an emergent to a nonemergent single-stage dissection. These critical decisions require experience and training,” Dr. Cirocco said. “For patients who require emergent operation for diffuse peritonitis, I believe that background and experience of the individual surgeon trumps the presence or absence of specialty training.”
Dr. Wright and his coauthors reported having no financial conflicts.
CHICAGO – Surgical outcomes of acute, complicated diverticulitis are equivalent regardless of whether a colorectal or general surgeon wields the scalpel, a multicenter study showed.
There was no difference between the colorectal surgery (CRS) and general surgery groups for the primary outcomes of 90-day morbidity (26% vs 28%; P = .76), readmission (32% vs. 25%; P = .48), and length of stay (both median 9 days; P = .82).
Surgeon specialization was not associated with any of the outcomes in multivariate regression that accounted for patient demographics, surgeon type, and disease characteristics, study author Capt. G. Paul Wright, U.S. Army Reserve Medical Corps, reported at the annual meeting of the Central Surgical Association.
The authors tackled the controversial issue in light of recent data suggesting improved acute, complicated diverticulitis surgery outcomes in the hands of specialized surgeons. A 2014 study reported that colorectal surgeons were less likely than general surgeons to use a Hartmann’s procedure and had reduced LOS and time to stoma reversal (J. Am. Coll. Surg. 2014;218:1156-61).
The current analysis involved 115 consecutive patients with acute, complicated diverticulitis who underwent emergent surgery with either a colorectal surgeon (n = 62) or general surgeon (n = 53) at two university-affiliated hospitals from 2006 to 2013. Age, Charlson Comorbidity Index, and American Society of Anesthesiologists class were similar between groups.
The colorectal surgeon group (CRS), however, was significantly more likely to have had previous episodes of diverticulitis (58% vs. 25%; P < .001), likely representing a referral bias or preexisting relationship with their surgeon, Dr. Wright said.
The general surgeon (GS) group had a significantly higher number of Systemic Inflammatory Response Syndrome criteria (P = .009 for all groups), higher rates of Hinchey class 3 disease (59% vs. 32%: P = .02), and ICU admissions (25% vs. 7%; P = .006).
The most common procedure among general surgeons was a Hartmann’s procedure (64% vs. 34%; P < .001), whereas colorectal surgeons favored primary anastomosis with diverting ileostomy (45% vs. 0%; P < .001), Dr. Wright, from Grand Rapids Medical Education Partners and Michigan State University, both in Grand Rapids, reported.
General surgeons were more likely to close the skin (85% vs. 50%), while in the CRS group the skin was left partially or completely open in 50% of patients. Operative time at the index admission was an average of 36 minutes longer in the CRS group (mean 164 minutes vs. 128 minutes; P = .005).
The CRS group had a higher rate of stoma reversal (78% vs 65%) and shorter time to stoma reversal (4 months vs. 4.7 months), but the difference was not statistically significant. The CRS group had a significantly shorter stoma reversal OR duration (mean 106 minutes vs. 182 minutes; P = .0010) and stoma reversal length of stay (mean 4 days vs. 7 days; P < .001).
“As general surgeons will no doubt continue to care for acute diverticulitis, increased use of primary anastomosis with proximal diversion when appropriate may be warranted due to the secondary benefits seen in stoma reversal,” Dr. Wright said.
Mortality was low and similar, at just one death in the CRS and two in the GS group.
Invited discussant William Cirocco, from Ohio State University in Columbus, said the type of surgical intervention is just one aspect in the management of patients with diverticulitis.
“An additional nonoperative approach may lead to conversion of an emergent to a nonemergent single-stage dissection. These critical decisions require experience and training,” Dr. Cirocco said. “For patients who require emergent operation for diffuse peritonitis, I believe that background and experience of the individual surgeon trumps the presence or absence of specialty training.”
Dr. Wright and his coauthors reported having no financial conflicts.
CHICAGO – Surgical outcomes of acute, complicated diverticulitis are equivalent regardless of whether a colorectal or general surgeon wields the scalpel, a multicenter study showed.
There was no difference between the colorectal surgery (CRS) and general surgery groups for the primary outcomes of 90-day morbidity (26% vs 28%; P = .76), readmission (32% vs. 25%; P = .48), and length of stay (both median 9 days; P = .82).
Surgeon specialization was not associated with any of the outcomes in multivariate regression that accounted for patient demographics, surgeon type, and disease characteristics, study author Capt. G. Paul Wright, U.S. Army Reserve Medical Corps, reported at the annual meeting of the Central Surgical Association.
The authors tackled the controversial issue in light of recent data suggesting improved acute, complicated diverticulitis surgery outcomes in the hands of specialized surgeons. A 2014 study reported that colorectal surgeons were less likely than general surgeons to use a Hartmann’s procedure and had reduced LOS and time to stoma reversal (J. Am. Coll. Surg. 2014;218:1156-61).
The current analysis involved 115 consecutive patients with acute, complicated diverticulitis who underwent emergent surgery with either a colorectal surgeon (n = 62) or general surgeon (n = 53) at two university-affiliated hospitals from 2006 to 2013. Age, Charlson Comorbidity Index, and American Society of Anesthesiologists class were similar between groups.
The colorectal surgeon group (CRS), however, was significantly more likely to have had previous episodes of diverticulitis (58% vs. 25%; P < .001), likely representing a referral bias or preexisting relationship with their surgeon, Dr. Wright said.
The general surgeon (GS) group had a significantly higher number of Systemic Inflammatory Response Syndrome criteria (P = .009 for all groups), higher rates of Hinchey class 3 disease (59% vs. 32%: P = .02), and ICU admissions (25% vs. 7%; P = .006).
The most common procedure among general surgeons was a Hartmann’s procedure (64% vs. 34%; P < .001), whereas colorectal surgeons favored primary anastomosis with diverting ileostomy (45% vs. 0%; P < .001), Dr. Wright, from Grand Rapids Medical Education Partners and Michigan State University, both in Grand Rapids, reported.
General surgeons were more likely to close the skin (85% vs. 50%), while in the CRS group the skin was left partially or completely open in 50% of patients. Operative time at the index admission was an average of 36 minutes longer in the CRS group (mean 164 minutes vs. 128 minutes; P = .005).
The CRS group had a higher rate of stoma reversal (78% vs 65%) and shorter time to stoma reversal (4 months vs. 4.7 months), but the difference was not statistically significant. The CRS group had a significantly shorter stoma reversal OR duration (mean 106 minutes vs. 182 minutes; P = .0010) and stoma reversal length of stay (mean 4 days vs. 7 days; P < .001).
“As general surgeons will no doubt continue to care for acute diverticulitis, increased use of primary anastomosis with proximal diversion when appropriate may be warranted due to the secondary benefits seen in stoma reversal,” Dr. Wright said.
Mortality was low and similar, at just one death in the CRS and two in the GS group.
Invited discussant William Cirocco, from Ohio State University in Columbus, said the type of surgical intervention is just one aspect in the management of patients with diverticulitis.
“An additional nonoperative approach may lead to conversion of an emergent to a nonemergent single-stage dissection. These critical decisions require experience and training,” Dr. Cirocco said. “For patients who require emergent operation for diffuse peritonitis, I believe that background and experience of the individual surgeon trumps the presence or absence of specialty training.”
Dr. Wright and his coauthors reported having no financial conflicts.
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: Major outcomes of acute, complicated diverticulitis were comparable regardless of surgeon specialization.
Major finding: Patients with diverticulitis treated by colorectal and general surgeons had similar 90-day morbidity (26% vs 28%; P = .76), readmissions (32% vs. 25%; P = .48), and LOS (both median 9 days;P = .82).
Data source: Retrospective study in 115 patients with acute complicated diverticulitis.
Disclosures: Dr. Wright and his coauthors reported having no financial conflicts.
Health leaders share views at ACS Quality Forum
A panel of health care leaders and policymakers gathered January 16 for the American College of Surgeons (ACS) Surgical Health Care Quality Forum Sacramento, CA, the 21st such meeting in a series of community forums held throughout the U.S. since 2011. Participants discussed the state of health care in Northern California and highlighted ways that health leaders and government officials can collaborate to improve patient outcomes and the quality of the health care system. Forum presenters shared their views on policy recommendations, hospital and health system initiatives, physician satisfaction issues, and the role of the ACS National Surgical Quality Improvement Program in measuring and improving patient care. Panelists discussed examples of state and national quality improvement initiatives that have resulted in higher standards, reduced costs, and better outcomes.
Julie A. Freischlag, MD, FACS, vice-chancellor for human health sciences and dean of the School of Medicine, University of California (UC) Davis Health System, and Immediate Past-Chair of the ACS Board of Regents; and David H. Wisner, MD, FACS, professor of surgery, UC Davis School of Medicine, co-moderated the forum. U.S. Congressional Reps. Ami Bera, MD (D-CA), and Doris Matsui (D-CA) delivered keynote speeches. Forum panelists included:
• Ronald W. Chapman, MD, MPH, Director and State Health Officer, California Department of Public Health
• Diana L. Farmer, MD, FACS, FRCS, Pearl Stamps Stewart Professor and Chair; chair, department of surgery, UC Davis School of Medicine; surgeon-in-chief, UC Davis Children’s Hospital, UC Davis Health System; and member, ACS Board of Governors Executive Committee
• David B. Hoyt, MD, FACS, Executive Director, ACS
• Mark P. Owens, MD, FACS, vice-president of medical affairs, Mercy San Juan Medical Center, Dignity Health
• Glenn S. Tse, MD, general surgeon, Kaiser Roseville Medical Center; senior partner, The Permanente Medical Group
• Heather M. Young, PhD, RN, FAAN, associate vice-chancellor for nursing, dean and professor, Betty Irene Moore School of Nursing, UC DavisView the full program video on the ACS website [www.facs.org ].
For more information, e-mail [email protected].
A panel of health care leaders and policymakers gathered January 16 for the American College of Surgeons (ACS) Surgical Health Care Quality Forum Sacramento, CA, the 21st such meeting in a series of community forums held throughout the U.S. since 2011. Participants discussed the state of health care in Northern California and highlighted ways that health leaders and government officials can collaborate to improve patient outcomes and the quality of the health care system. Forum presenters shared their views on policy recommendations, hospital and health system initiatives, physician satisfaction issues, and the role of the ACS National Surgical Quality Improvement Program in measuring and improving patient care. Panelists discussed examples of state and national quality improvement initiatives that have resulted in higher standards, reduced costs, and better outcomes.
Julie A. Freischlag, MD, FACS, vice-chancellor for human health sciences and dean of the School of Medicine, University of California (UC) Davis Health System, and Immediate Past-Chair of the ACS Board of Regents; and David H. Wisner, MD, FACS, professor of surgery, UC Davis School of Medicine, co-moderated the forum. U.S. Congressional Reps. Ami Bera, MD (D-CA), and Doris Matsui (D-CA) delivered keynote speeches. Forum panelists included:
• Ronald W. Chapman, MD, MPH, Director and State Health Officer, California Department of Public Health
• Diana L. Farmer, MD, FACS, FRCS, Pearl Stamps Stewart Professor and Chair; chair, department of surgery, UC Davis School of Medicine; surgeon-in-chief, UC Davis Children’s Hospital, UC Davis Health System; and member, ACS Board of Governors Executive Committee
• David B. Hoyt, MD, FACS, Executive Director, ACS
• Mark P. Owens, MD, FACS, vice-president of medical affairs, Mercy San Juan Medical Center, Dignity Health
• Glenn S. Tse, MD, general surgeon, Kaiser Roseville Medical Center; senior partner, The Permanente Medical Group
• Heather M. Young, PhD, RN, FAAN, associate vice-chancellor for nursing, dean and professor, Betty Irene Moore School of Nursing, UC DavisView the full program video on the ACS website [www.facs.org ].
For more information, e-mail [email protected].
A panel of health care leaders and policymakers gathered January 16 for the American College of Surgeons (ACS) Surgical Health Care Quality Forum Sacramento, CA, the 21st such meeting in a series of community forums held throughout the U.S. since 2011. Participants discussed the state of health care in Northern California and highlighted ways that health leaders and government officials can collaborate to improve patient outcomes and the quality of the health care system. Forum presenters shared their views on policy recommendations, hospital and health system initiatives, physician satisfaction issues, and the role of the ACS National Surgical Quality Improvement Program in measuring and improving patient care. Panelists discussed examples of state and national quality improvement initiatives that have resulted in higher standards, reduced costs, and better outcomes.
Julie A. Freischlag, MD, FACS, vice-chancellor for human health sciences and dean of the School of Medicine, University of California (UC) Davis Health System, and Immediate Past-Chair of the ACS Board of Regents; and David H. Wisner, MD, FACS, professor of surgery, UC Davis School of Medicine, co-moderated the forum. U.S. Congressional Reps. Ami Bera, MD (D-CA), and Doris Matsui (D-CA) delivered keynote speeches. Forum panelists included:
• Ronald W. Chapman, MD, MPH, Director and State Health Officer, California Department of Public Health
• Diana L. Farmer, MD, FACS, FRCS, Pearl Stamps Stewart Professor and Chair; chair, department of surgery, UC Davis School of Medicine; surgeon-in-chief, UC Davis Children’s Hospital, UC Davis Health System; and member, ACS Board of Governors Executive Committee
• David B. Hoyt, MD, FACS, Executive Director, ACS
• Mark P. Owens, MD, FACS, vice-president of medical affairs, Mercy San Juan Medical Center, Dignity Health
• Glenn S. Tse, MD, general surgeon, Kaiser Roseville Medical Center; senior partner, The Permanente Medical Group
• Heather M. Young, PhD, RN, FAAN, associate vice-chancellor for nursing, dean and professor, Betty Irene Moore School of Nursing, UC DavisView the full program video on the ACS website [www.facs.org ].
For more information, e-mail [email protected].
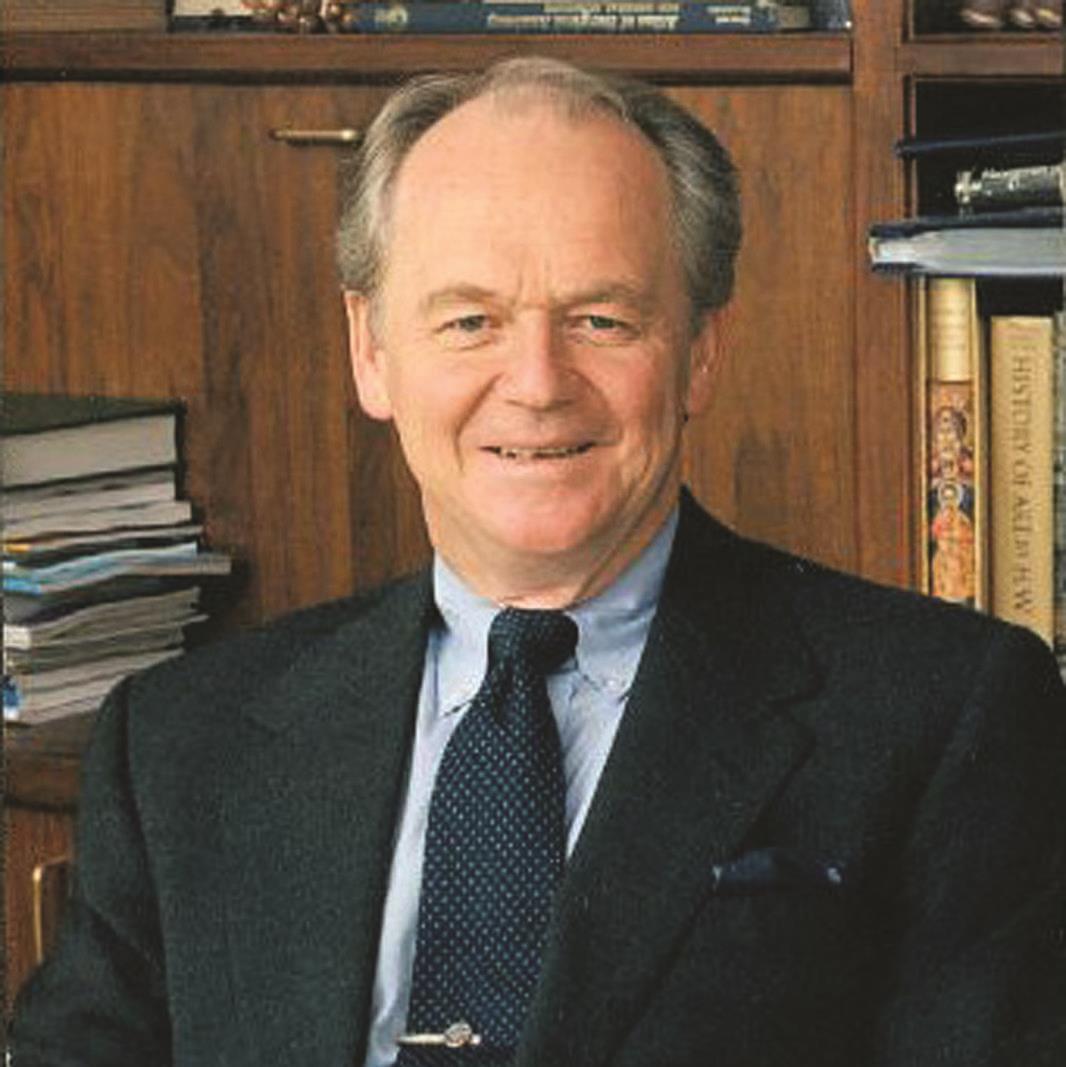
Murray F. Brennan, MD, FACS, to be knighted
Sir Murray F. Brennan, MD, FACS, was named a Knight Grand Companion of the New Zealand Order of Merit on January 1, for his service to medicine as part of the Queen’s New Year Honours. A native New Zealander, Dr. Brennan is the Benno C. Schmidt Chair in Clinical Oncology, vice-president for international programs, and director of The Bobst International Center, Memorial Sloan Kettering Cancer Center (MSKCC), New York, NY. Dr. Brennan adds knighthood to a long list of accolades that he has received throughout his distinguished career as a cancer surgeon. In 2000, he received the American College of Surgeons’ (ACS) highest honor—the Distinguished Service Award.
Crowning achievements in cancer care
Born in Auckland, Dr. Brennan received a degree in mathematics from the University of New Zealand and a medical degree from the University of Otago, Dunedin. He performed advanced laboratory and clinical work at Peter Bent Brigham Hospital, Harvard Medical School, and the Joslin Research Laboratories, Boston, MA. After residency, Dr. Brennan joined the National Cancer Institute, where he led the surgical metabolism section. He began his career at the MSKCC in 1981 as chief of gastric and mixed tumor service. From 1985 to 2006, Dr. Brennan chaired the department of surgery at MSKCC. In 1994, MSKCC established the Murray F. Brennan Chair in Surgery. Throughout his career at MSKCC, he also has served as a professor of surgery at Cornell University in New York.
Dr. Brennan is recognized around the world for his extraordinary achievements in enhancing the medical and scientific communities’ understanding of tumor biology, in evaluating the proper role of surgery and other therapies in caring for patients with cancer, and for training young surgeons and serving as a mentor to developing surgical scientists. Dr. Brennan’s clinical and research interests have centered on surgical oncology, endocrinology, metabolism, and nutrition. He has designed and conducted numerous clinical trials, which have produced significant findings in the management of patients with soft tissue sarcomas and pancreatic cancer, and played a leading role in creating the world’s largest database of more than 10,000 sarcoma patients.
Leader of surgical organizations
An ACS Fellow since 1977, Dr. Brennan has served the College in numerous capacities. He served as ACS Second Vice-President (2004–2005) and is a former Chair of the Commission on Cancer, the Surgical Forum Committee, and the International Relations Committee. In 2012, the Fellows Leadership Society of the ACS presented the Distinguished Philanthropist Award to Dr. Brennan in recognition of his philanthropic endeavors, his service to the surgical profession, and his all-encompassing support of the College. Also in 2012, the Murray F. Brennan International Scholarship was endowed through the ACS Foundation with the support of more than 100 donors.
Dr. Brennan has played an active leadership role in many other surgical organizations. He has served as director of the American Board of Surgery and president of the Society of Surgical Oncology, the James IV Association, the Society of Clinical Surgery, the International Gastric Cancer Association, and the American Surgical Association.
Dr. Brennan is an Honorary Fellow of the Royal College of Surgeons in Ireland, Edinburgh, England, and Australasia; the Brazilian and Chilean Surgical colleges; the Royal College of Physicians and Surgeons of Glasgow and Canada; a number of international surgical societies; and the Association of Surgeons of Great Britain and Ireland. He has received honorary doctorates from the Universities of Edinburgh, Otago, and Gothenburg, and the University College of London. In 1995, he was honored with membership in the Institute of Medicine of the National Academy of Sciences.The investiture ceremony for knights will take place in May. For more information, go to www.dpmc.govt.nz/node/1402, www.stuff.co.nz/national/health/64541572/highest-honour-for-surgeon-murray-brennan, and www.odt.co.nz/news/national/328643/new-year-honours-2015.
Sir Murray F. Brennan, MD, FACS, was named a Knight Grand Companion of the New Zealand Order of Merit on January 1, for his service to medicine as part of the Queen’s New Year Honours. A native New Zealander, Dr. Brennan is the Benno C. Schmidt Chair in Clinical Oncology, vice-president for international programs, and director of The Bobst International Center, Memorial Sloan Kettering Cancer Center (MSKCC), New York, NY. Dr. Brennan adds knighthood to a long list of accolades that he has received throughout his distinguished career as a cancer surgeon. In 2000, he received the American College of Surgeons’ (ACS) highest honor—the Distinguished Service Award.
Crowning achievements in cancer care
Born in Auckland, Dr. Brennan received a degree in mathematics from the University of New Zealand and a medical degree from the University of Otago, Dunedin. He performed advanced laboratory and clinical work at Peter Bent Brigham Hospital, Harvard Medical School, and the Joslin Research Laboratories, Boston, MA. After residency, Dr. Brennan joined the National Cancer Institute, where he led the surgical metabolism section. He began his career at the MSKCC in 1981 as chief of gastric and mixed tumor service. From 1985 to 2006, Dr. Brennan chaired the department of surgery at MSKCC. In 1994, MSKCC established the Murray F. Brennan Chair in Surgery. Throughout his career at MSKCC, he also has served as a professor of surgery at Cornell University in New York.
Dr. Brennan is recognized around the world for his extraordinary achievements in enhancing the medical and scientific communities’ understanding of tumor biology, in evaluating the proper role of surgery and other therapies in caring for patients with cancer, and for training young surgeons and serving as a mentor to developing surgical scientists. Dr. Brennan’s clinical and research interests have centered on surgical oncology, endocrinology, metabolism, and nutrition. He has designed and conducted numerous clinical trials, which have produced significant findings in the management of patients with soft tissue sarcomas and pancreatic cancer, and played a leading role in creating the world’s largest database of more than 10,000 sarcoma patients.
Leader of surgical organizations
An ACS Fellow since 1977, Dr. Brennan has served the College in numerous capacities. He served as ACS Second Vice-President (2004–2005) and is a former Chair of the Commission on Cancer, the Surgical Forum Committee, and the International Relations Committee. In 2012, the Fellows Leadership Society of the ACS presented the Distinguished Philanthropist Award to Dr. Brennan in recognition of his philanthropic endeavors, his service to the surgical profession, and his all-encompassing support of the College. Also in 2012, the Murray F. Brennan International Scholarship was endowed through the ACS Foundation with the support of more than 100 donors.
Dr. Brennan has played an active leadership role in many other surgical organizations. He has served as director of the American Board of Surgery and president of the Society of Surgical Oncology, the James IV Association, the Society of Clinical Surgery, the International Gastric Cancer Association, and the American Surgical Association.
Dr. Brennan is an Honorary Fellow of the Royal College of Surgeons in Ireland, Edinburgh, England, and Australasia; the Brazilian and Chilean Surgical colleges; the Royal College of Physicians and Surgeons of Glasgow and Canada; a number of international surgical societies; and the Association of Surgeons of Great Britain and Ireland. He has received honorary doctorates from the Universities of Edinburgh, Otago, and Gothenburg, and the University College of London. In 1995, he was honored with membership in the Institute of Medicine of the National Academy of Sciences.The investiture ceremony for knights will take place in May. For more information, go to www.dpmc.govt.nz/node/1402, www.stuff.co.nz/national/health/64541572/highest-honour-for-surgeon-murray-brennan, and www.odt.co.nz/news/national/328643/new-year-honours-2015.
Sir Murray F. Brennan, MD, FACS, was named a Knight Grand Companion of the New Zealand Order of Merit on January 1, for his service to medicine as part of the Queen’s New Year Honours. A native New Zealander, Dr. Brennan is the Benno C. Schmidt Chair in Clinical Oncology, vice-president for international programs, and director of The Bobst International Center, Memorial Sloan Kettering Cancer Center (MSKCC), New York, NY. Dr. Brennan adds knighthood to a long list of accolades that he has received throughout his distinguished career as a cancer surgeon. In 2000, he received the American College of Surgeons’ (ACS) highest honor—the Distinguished Service Award.
Crowning achievements in cancer care
Born in Auckland, Dr. Brennan received a degree in mathematics from the University of New Zealand and a medical degree from the University of Otago, Dunedin. He performed advanced laboratory and clinical work at Peter Bent Brigham Hospital, Harvard Medical School, and the Joslin Research Laboratories, Boston, MA. After residency, Dr. Brennan joined the National Cancer Institute, where he led the surgical metabolism section. He began his career at the MSKCC in 1981 as chief of gastric and mixed tumor service. From 1985 to 2006, Dr. Brennan chaired the department of surgery at MSKCC. In 1994, MSKCC established the Murray F. Brennan Chair in Surgery. Throughout his career at MSKCC, he also has served as a professor of surgery at Cornell University in New York.
Dr. Brennan is recognized around the world for his extraordinary achievements in enhancing the medical and scientific communities’ understanding of tumor biology, in evaluating the proper role of surgery and other therapies in caring for patients with cancer, and for training young surgeons and serving as a mentor to developing surgical scientists. Dr. Brennan’s clinical and research interests have centered on surgical oncology, endocrinology, metabolism, and nutrition. He has designed and conducted numerous clinical trials, which have produced significant findings in the management of patients with soft tissue sarcomas and pancreatic cancer, and played a leading role in creating the world’s largest database of more than 10,000 sarcoma patients.
Leader of surgical organizations
An ACS Fellow since 1977, Dr. Brennan has served the College in numerous capacities. He served as ACS Second Vice-President (2004–2005) and is a former Chair of the Commission on Cancer, the Surgical Forum Committee, and the International Relations Committee. In 2012, the Fellows Leadership Society of the ACS presented the Distinguished Philanthropist Award to Dr. Brennan in recognition of his philanthropic endeavors, his service to the surgical profession, and his all-encompassing support of the College. Also in 2012, the Murray F. Brennan International Scholarship was endowed through the ACS Foundation with the support of more than 100 donors.
Dr. Brennan has played an active leadership role in many other surgical organizations. He has served as director of the American Board of Surgery and president of the Society of Surgical Oncology, the James IV Association, the Society of Clinical Surgery, the International Gastric Cancer Association, and the American Surgical Association.
Dr. Brennan is an Honorary Fellow of the Royal College of Surgeons in Ireland, Edinburgh, England, and Australasia; the Brazilian and Chilean Surgical colleges; the Royal College of Physicians and Surgeons of Glasgow and Canada; a number of international surgical societies; and the Association of Surgeons of Great Britain and Ireland. He has received honorary doctorates from the Universities of Edinburgh, Otago, and Gothenburg, and the University College of London. In 1995, he was honored with membership in the Institute of Medicine of the National Academy of Sciences.The investiture ceremony for knights will take place in May. For more information, go to www.dpmc.govt.nz/node/1402, www.stuff.co.nz/national/health/64541572/highest-honour-for-surgeon-murray-brennan, and www.odt.co.nz/news/national/328643/new-year-honours-2015.
1913 Legacy Campaign achieves $3 million milestone
The American College of Surgeons (ACS) Foundation Chair, Amilu Stewart, MD, FACS, announced in late January that two major gifts to the 1913 Legacy Campaign have increased the total contributed to more than $3 million. One gift was designated to the ACS scholarships program, and the other will be directed for the American Joint Committee on Cancer (AJCC) Cancer Staging Manual.
Last year, the College awarded more than $1.5 million in scholarship funding to surgeons for professional development and research opportunities. The AJCC, administered by ACS Cancer Programs, provides worldwide leadership in the development, promotion, and maintenance of evidence-based systems for the classification and management of cancer in collaboration with multidisciplinary organizations dedicated to cancer surveillance and to improving care.
“We are grateful for these recent donations that will support efforts that are core to the College’s mission of optimal patient care and education. The nearly 300 donors who have each invested at least $1,913 in this special initiative are all important partners in the philanthropic work of the College. Every donation makes a meaningful impact for the surgical profession and patients,” said Dr. Stewart. Donors giving to the campaign with a legacy (bequest gift) also receive membership in the Mayne Heritage Society, the planned giving recognition program of the ACS Foundation.
The ACS Foundation Board of Directors and volunteers have led the 1913 Legacy Campaign to maintain the vital role of the College and strengthen high-impact services for its next 100 years. Philanthropic investments within three priority campaign initiatives are benefiting—the Surgeon, the Profession, and the Societal Good.
To see a complete list of 1913 Legacy Campaign donors or to make your own donation, visit the Foundation website at www.facs.org/1913Campaign.
The American College of Surgeons (ACS) Foundation Chair, Amilu Stewart, MD, FACS, announced in late January that two major gifts to the 1913 Legacy Campaign have increased the total contributed to more than $3 million. One gift was designated to the ACS scholarships program, and the other will be directed for the American Joint Committee on Cancer (AJCC) Cancer Staging Manual.
Last year, the College awarded more than $1.5 million in scholarship funding to surgeons for professional development and research opportunities. The AJCC, administered by ACS Cancer Programs, provides worldwide leadership in the development, promotion, and maintenance of evidence-based systems for the classification and management of cancer in collaboration with multidisciplinary organizations dedicated to cancer surveillance and to improving care.
“We are grateful for these recent donations that will support efforts that are core to the College’s mission of optimal patient care and education. The nearly 300 donors who have each invested at least $1,913 in this special initiative are all important partners in the philanthropic work of the College. Every donation makes a meaningful impact for the surgical profession and patients,” said Dr. Stewart. Donors giving to the campaign with a legacy (bequest gift) also receive membership in the Mayne Heritage Society, the planned giving recognition program of the ACS Foundation.
The ACS Foundation Board of Directors and volunteers have led the 1913 Legacy Campaign to maintain the vital role of the College and strengthen high-impact services for its next 100 years. Philanthropic investments within three priority campaign initiatives are benefiting—the Surgeon, the Profession, and the Societal Good.
To see a complete list of 1913 Legacy Campaign donors or to make your own donation, visit the Foundation website at www.facs.org/1913Campaign.
The American College of Surgeons (ACS) Foundation Chair, Amilu Stewart, MD, FACS, announced in late January that two major gifts to the 1913 Legacy Campaign have increased the total contributed to more than $3 million. One gift was designated to the ACS scholarships program, and the other will be directed for the American Joint Committee on Cancer (AJCC) Cancer Staging Manual.
Last year, the College awarded more than $1.5 million in scholarship funding to surgeons for professional development and research opportunities. The AJCC, administered by ACS Cancer Programs, provides worldwide leadership in the development, promotion, and maintenance of evidence-based systems for the classification and management of cancer in collaboration with multidisciplinary organizations dedicated to cancer surveillance and to improving care.
“We are grateful for these recent donations that will support efforts that are core to the College’s mission of optimal patient care and education. The nearly 300 donors who have each invested at least $1,913 in this special initiative are all important partners in the philanthropic work of the College. Every donation makes a meaningful impact for the surgical profession and patients,” said Dr. Stewart. Donors giving to the campaign with a legacy (bequest gift) also receive membership in the Mayne Heritage Society, the planned giving recognition program of the ACS Foundation.
The ACS Foundation Board of Directors and volunteers have led the 1913 Legacy Campaign to maintain the vital role of the College and strengthen high-impact services for its next 100 years. Philanthropic investments within three priority campaign initiatives are benefiting—the Surgeon, the Profession, and the Societal Good.
To see a complete list of 1913 Legacy Campaign donors or to make your own donation, visit the Foundation website at www.facs.org/1913Campaign.
ACS Members in the news
Brooke M. Buckley, MD, FACS, emergency surgeon and medical director, Anne Arundel Medical Center, Acute Care Surgeons, Annapolis, MD, was recently elected 2015–2016 president of the Maryland State Medical Society (MedChi). Dr. Buckley served as co-chair of the MedChi legislative council, 2011−2013, and has been on the board of the MedChi political action committee since 2010.
Luther F. Cobb, MD, FACS, was installed as the 147th president of the California Medical Association (CMA). Dr. Cobb has dedicated many years to the betterment of health care in California and formerly served as chair of the CMA Council on Legislation and president of the Humboldt-Del Norte County Medical Society. Over the course of the last year, he played a significant role in the successful campaign to defeat Proposition 46, with 67 percent of the California electorate voting against it. This proposal would have increased California’s $250,000 cap on noneconomic damage awards in medical liability lawsuits to $1.1 million.
Read Dr. Cobb’s president’s message in the January 14, 2015, issue of CMA News at www.cmanet.org/m/news/detail.dT/presidents-message-the-coming-year-and-beyond.
Alvin Crawford, MD, FACS, co-director of the Crawford Spine Center, Cincinnati Children’s Hospital, and professor emeritus at the University of Cincinnati College of Medicine, OH, has received a number of awards in recent months. He was among four individuals honored as 2014 Great Living Cincinnatians by the Cincinnati USA Regional Chamber. Since 1967, the Regional Chamber has honored more than 135 residents with the annual Great Living Cincinnatian Awards, based on such criteria as community service; business and civic attainment at a local, state, national, or international level; leadership; awareness of the needs of others; and distinctive accomplishments that have brought favorable attention to their community, institution, or organization. Dr. Crawford also received the Distinguished Achievement Award from the Pediatric Orthopaedic Society of North America in 2014, its highest honor. In addition, he received the Lifetime Achievement Award from the Scoliosis Research Society, the premier organization for spinal deformities. On February 12, the Cincinnati Business Courier honored Dr. Crawford with the 2015 Health Care Heroes Lifetime Achievement Award.
Brandon Snook, MD, FACS, Mike O’Callaghan Federal Medical Center, Las Vegas, NV, graduated as a categorical active duty resident in acute care surgery from the University Medical Center (UMC) of Southern Nevada, Las Vegas, the state’s only Level I trauma and burn center, in July 2013. He is part of a program called Sustained Medical and Readiness Trained, which helps medical officers stay current with the latest medical and surgical techniques used on the battlefield. In January, Lieutenant General Thomas W. Travis, MD, U.S. Air Force (USAF) Surgeon General, toured the UMC’s emergency department and formally announced the expansion of the medical center’s two-year training program, in partnership with the USAF and Nellis Air Force Base, NV. John Fildes, MD, FACS, department of surgery, University of Nevada School of Medicine, Las Vegas, and Past Medical Director of the American College of Surgeons Committee on Trauma, has been an active participant in the embedding of active duty residents into emergency medicine. As a result of this partnership, more USAF medical specialists from around the country will expand their acute care training at the UMC.
Brooke M. Buckley, MD, FACS, emergency surgeon and medical director, Anne Arundel Medical Center, Acute Care Surgeons, Annapolis, MD, was recently elected 2015–2016 president of the Maryland State Medical Society (MedChi). Dr. Buckley served as co-chair of the MedChi legislative council, 2011−2013, and has been on the board of the MedChi political action committee since 2010.
Luther F. Cobb, MD, FACS, was installed as the 147th president of the California Medical Association (CMA). Dr. Cobb has dedicated many years to the betterment of health care in California and formerly served as chair of the CMA Council on Legislation and president of the Humboldt-Del Norte County Medical Society. Over the course of the last year, he played a significant role in the successful campaign to defeat Proposition 46, with 67 percent of the California electorate voting against it. This proposal would have increased California’s $250,000 cap on noneconomic damage awards in medical liability lawsuits to $1.1 million.
Read Dr. Cobb’s president’s message in the January 14, 2015, issue of CMA News at www.cmanet.org/m/news/detail.dT/presidents-message-the-coming-year-and-beyond.
Alvin Crawford, MD, FACS, co-director of the Crawford Spine Center, Cincinnati Children’s Hospital, and professor emeritus at the University of Cincinnati College of Medicine, OH, has received a number of awards in recent months. He was among four individuals honored as 2014 Great Living Cincinnatians by the Cincinnati USA Regional Chamber. Since 1967, the Regional Chamber has honored more than 135 residents with the annual Great Living Cincinnatian Awards, based on such criteria as community service; business and civic attainment at a local, state, national, or international level; leadership; awareness of the needs of others; and distinctive accomplishments that have brought favorable attention to their community, institution, or organization. Dr. Crawford also received the Distinguished Achievement Award from the Pediatric Orthopaedic Society of North America in 2014, its highest honor. In addition, he received the Lifetime Achievement Award from the Scoliosis Research Society, the premier organization for spinal deformities. On February 12, the Cincinnati Business Courier honored Dr. Crawford with the 2015 Health Care Heroes Lifetime Achievement Award.
Brandon Snook, MD, FACS, Mike O’Callaghan Federal Medical Center, Las Vegas, NV, graduated as a categorical active duty resident in acute care surgery from the University Medical Center (UMC) of Southern Nevada, Las Vegas, the state’s only Level I trauma and burn center, in July 2013. He is part of a program called Sustained Medical and Readiness Trained, which helps medical officers stay current with the latest medical and surgical techniques used on the battlefield. In January, Lieutenant General Thomas W. Travis, MD, U.S. Air Force (USAF) Surgeon General, toured the UMC’s emergency department and formally announced the expansion of the medical center’s two-year training program, in partnership with the USAF and Nellis Air Force Base, NV. John Fildes, MD, FACS, department of surgery, University of Nevada School of Medicine, Las Vegas, and Past Medical Director of the American College of Surgeons Committee on Trauma, has been an active participant in the embedding of active duty residents into emergency medicine. As a result of this partnership, more USAF medical specialists from around the country will expand their acute care training at the UMC.
Brooke M. Buckley, MD, FACS, emergency surgeon and medical director, Anne Arundel Medical Center, Acute Care Surgeons, Annapolis, MD, was recently elected 2015–2016 president of the Maryland State Medical Society (MedChi). Dr. Buckley served as co-chair of the MedChi legislative council, 2011−2013, and has been on the board of the MedChi political action committee since 2010.
Luther F. Cobb, MD, FACS, was installed as the 147th president of the California Medical Association (CMA). Dr. Cobb has dedicated many years to the betterment of health care in California and formerly served as chair of the CMA Council on Legislation and president of the Humboldt-Del Norte County Medical Society. Over the course of the last year, he played a significant role in the successful campaign to defeat Proposition 46, with 67 percent of the California electorate voting against it. This proposal would have increased California’s $250,000 cap on noneconomic damage awards in medical liability lawsuits to $1.1 million.
Read Dr. Cobb’s president’s message in the January 14, 2015, issue of CMA News at www.cmanet.org/m/news/detail.dT/presidents-message-the-coming-year-and-beyond.
Alvin Crawford, MD, FACS, co-director of the Crawford Spine Center, Cincinnati Children’s Hospital, and professor emeritus at the University of Cincinnati College of Medicine, OH, has received a number of awards in recent months. He was among four individuals honored as 2014 Great Living Cincinnatians by the Cincinnati USA Regional Chamber. Since 1967, the Regional Chamber has honored more than 135 residents with the annual Great Living Cincinnatian Awards, based on such criteria as community service; business and civic attainment at a local, state, national, or international level; leadership; awareness of the needs of others; and distinctive accomplishments that have brought favorable attention to their community, institution, or organization. Dr. Crawford also received the Distinguished Achievement Award from the Pediatric Orthopaedic Society of North America in 2014, its highest honor. In addition, he received the Lifetime Achievement Award from the Scoliosis Research Society, the premier organization for spinal deformities. On February 12, the Cincinnati Business Courier honored Dr. Crawford with the 2015 Health Care Heroes Lifetime Achievement Award.
Brandon Snook, MD, FACS, Mike O’Callaghan Federal Medical Center, Las Vegas, NV, graduated as a categorical active duty resident in acute care surgery from the University Medical Center (UMC) of Southern Nevada, Las Vegas, the state’s only Level I trauma and burn center, in July 2013. He is part of a program called Sustained Medical and Readiness Trained, which helps medical officers stay current with the latest medical and surgical techniques used on the battlefield. In January, Lieutenant General Thomas W. Travis, MD, U.S. Air Force (USAF) Surgeon General, toured the UMC’s emergency department and formally announced the expansion of the medical center’s two-year training program, in partnership with the USAF and Nellis Air Force Base, NV. John Fildes, MD, FACS, department of surgery, University of Nevada School of Medicine, Las Vegas, and Past Medical Director of the American College of Surgeons Committee on Trauma, has been an active participant in the embedding of active duty residents into emergency medicine. As a result of this partnership, more USAF medical specialists from around the country will expand their acute care training at the UMC.
Cost comparison favors minimally invasive over conventional AVR
Outcomes were similar, but hospital costs improved with use of mini-aortic valve replacement, compared with conventional AVR, according to the results of a Society of Thoracic Surgeons (STS) database study of 1,341 patients who underwent primary AVR at 17 hospitals.
A propensity match cohort analysis was done to compare patients who had conventional (67%) vs. mini-AVR (33%) performed using either partial sternotomy or right thoracotomy.
Mortality, stroke, renal failure, atrial fibrillation, reoperation for bleeding, and respiratory insufficiency were not statistically significantly different between the two groups. There was also no significant difference in ICU or hospital length of stay between the two groups. However, mini-AVR was associated with both significantly decreased ventilator time (5 vs. 6 hours) and blood product transfusion (25% vs. 32%), according to the report, which was published online and scheduled for the April issue of the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j/jtcvs.2015.01.014).
Total hospital cost was significantly lower in the mini-AVR group ($36,348) vs. the conventional repair group ($38,239, P = .02), wrote Dr. Ravi Kiran Ghanta of the University of Virginia, Charlottesville, and his colleagues.
The authors discussed the previously raised issue of longer cross-clamp and bypass times seen in earlier studies of mini-AVR. In their current study, such was not the case, with mini-AVR appearing equivalent with conventional operations. The authors suggested that surgeons have now adopted techniques to reduce bypass and cross-clamp times with mini-AVR.
Data were limited to in-hospital costs. Other costs, such as those of rehabilitation and lost productivity, were not included in the analysis. “Including these health-care costs may have increased overall savings with mini-AVR compared to conventional AVR,” the authors noted.
“Mini-AVR is associated with decreased ventilator time, blood product utilization, early discharge, and reduced total hospital cost. In contemporary clinical practice, mini-AVR is safe and cost-effective,” the researchers concluded.
The authors reported that they had no conflicts.
“Measurement of cost and outcome, the determinant of ‘value’ in health care, is assuming increasing importance in the evaluation of all medial interventions, especially those surgical procedures done frequently and at higher cost,” wrote Dr. Verdi J. DiSesa in his invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.01.049]).
Although applauding the timeliness and importance of analyzing the costs and outcomes in propensity-matched patients undergoing aortic valve replacement via full sternotomy of mini-AVR using a partial sternotomy or limited thoracotomy incision, he questioned some of the methodology. The cost-to-charge ratio used, which provides an estimate of the cost of services, is not uniform throughout departments in a single hospital, and differs from hospital to hospital, although the latter was accounted for. He suggested that “activity-based costing” would have been a better approach, although more labor intensive. In this approach, every encounter with a caregiver is assigned a unit cost and the cost of a patient encounter is calculated by estimating the number of units of service and multiplying by the unit cost for service.
“This method is demanding of resources but has the potential to become the most accurate and therefore the preferred way to determine the costs of medical services,” he wrote. In addition, the authors included but did not separately analyze patients having AVR via minithoracotomy.
“What might be the conclusions of this research were these patients excluded or analyzed separately?” he asked.
In terms of the propensity model, the matching procedure included only three clinical factors – STS Predicted Rate of Mortality (PROM) score, the operative year, and the surgeon who performed the procedure – resulting in 35% of patients remaining unmatched, which may have biased the results.
This analysis, Dr. DiSesa concluded, is “perhaps an early version of the kind of analyses, which increasingly will be required for the evaluation of the services provided by all health care providers, not only cardiac surgeons.”
Dr. DiSesa is professor of surgery at Temple University, Philadelphia.
“Measurement of cost and outcome, the determinant of ‘value’ in health care, is assuming increasing importance in the evaluation of all medial interventions, especially those surgical procedures done frequently and at higher cost,” wrote Dr. Verdi J. DiSesa in his invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.01.049]).
Although applauding the timeliness and importance of analyzing the costs and outcomes in propensity-matched patients undergoing aortic valve replacement via full sternotomy of mini-AVR using a partial sternotomy or limited thoracotomy incision, he questioned some of the methodology. The cost-to-charge ratio used, which provides an estimate of the cost of services, is not uniform throughout departments in a single hospital, and differs from hospital to hospital, although the latter was accounted for. He suggested that “activity-based costing” would have been a better approach, although more labor intensive. In this approach, every encounter with a caregiver is assigned a unit cost and the cost of a patient encounter is calculated by estimating the number of units of service and multiplying by the unit cost for service.
“This method is demanding of resources but has the potential to become the most accurate and therefore the preferred way to determine the costs of medical services,” he wrote. In addition, the authors included but did not separately analyze patients having AVR via minithoracotomy.
“What might be the conclusions of this research were these patients excluded or analyzed separately?” he asked.
In terms of the propensity model, the matching procedure included only three clinical factors – STS Predicted Rate of Mortality (PROM) score, the operative year, and the surgeon who performed the procedure – resulting in 35% of patients remaining unmatched, which may have biased the results.
This analysis, Dr. DiSesa concluded, is “perhaps an early version of the kind of analyses, which increasingly will be required for the evaluation of the services provided by all health care providers, not only cardiac surgeons.”
Dr. DiSesa is professor of surgery at Temple University, Philadelphia.
“Measurement of cost and outcome, the determinant of ‘value’ in health care, is assuming increasing importance in the evaluation of all medial interventions, especially those surgical procedures done frequently and at higher cost,” wrote Dr. Verdi J. DiSesa in his invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.01.049]).
Although applauding the timeliness and importance of analyzing the costs and outcomes in propensity-matched patients undergoing aortic valve replacement via full sternotomy of mini-AVR using a partial sternotomy or limited thoracotomy incision, he questioned some of the methodology. The cost-to-charge ratio used, which provides an estimate of the cost of services, is not uniform throughout departments in a single hospital, and differs from hospital to hospital, although the latter was accounted for. He suggested that “activity-based costing” would have been a better approach, although more labor intensive. In this approach, every encounter with a caregiver is assigned a unit cost and the cost of a patient encounter is calculated by estimating the number of units of service and multiplying by the unit cost for service.
“This method is demanding of resources but has the potential to become the most accurate and therefore the preferred way to determine the costs of medical services,” he wrote. In addition, the authors included but did not separately analyze patients having AVR via minithoracotomy.
“What might be the conclusions of this research were these patients excluded or analyzed separately?” he asked.
In terms of the propensity model, the matching procedure included only three clinical factors – STS Predicted Rate of Mortality (PROM) score, the operative year, and the surgeon who performed the procedure – resulting in 35% of patients remaining unmatched, which may have biased the results.
This analysis, Dr. DiSesa concluded, is “perhaps an early version of the kind of analyses, which increasingly will be required for the evaluation of the services provided by all health care providers, not only cardiac surgeons.”
Dr. DiSesa is professor of surgery at Temple University, Philadelphia.
Outcomes were similar, but hospital costs improved with use of mini-aortic valve replacement, compared with conventional AVR, according to the results of a Society of Thoracic Surgeons (STS) database study of 1,341 patients who underwent primary AVR at 17 hospitals.
A propensity match cohort analysis was done to compare patients who had conventional (67%) vs. mini-AVR (33%) performed using either partial sternotomy or right thoracotomy.
Mortality, stroke, renal failure, atrial fibrillation, reoperation for bleeding, and respiratory insufficiency were not statistically significantly different between the two groups. There was also no significant difference in ICU or hospital length of stay between the two groups. However, mini-AVR was associated with both significantly decreased ventilator time (5 vs. 6 hours) and blood product transfusion (25% vs. 32%), according to the report, which was published online and scheduled for the April issue of the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j/jtcvs.2015.01.014).
Total hospital cost was significantly lower in the mini-AVR group ($36,348) vs. the conventional repair group ($38,239, P = .02), wrote Dr. Ravi Kiran Ghanta of the University of Virginia, Charlottesville, and his colleagues.
The authors discussed the previously raised issue of longer cross-clamp and bypass times seen in earlier studies of mini-AVR. In their current study, such was not the case, with mini-AVR appearing equivalent with conventional operations. The authors suggested that surgeons have now adopted techniques to reduce bypass and cross-clamp times with mini-AVR.
Data were limited to in-hospital costs. Other costs, such as those of rehabilitation and lost productivity, were not included in the analysis. “Including these health-care costs may have increased overall savings with mini-AVR compared to conventional AVR,” the authors noted.
“Mini-AVR is associated with decreased ventilator time, blood product utilization, early discharge, and reduced total hospital cost. In contemporary clinical practice, mini-AVR is safe and cost-effective,” the researchers concluded.
The authors reported that they had no conflicts.
Outcomes were similar, but hospital costs improved with use of mini-aortic valve replacement, compared with conventional AVR, according to the results of a Society of Thoracic Surgeons (STS) database study of 1,341 patients who underwent primary AVR at 17 hospitals.
A propensity match cohort analysis was done to compare patients who had conventional (67%) vs. mini-AVR (33%) performed using either partial sternotomy or right thoracotomy.
Mortality, stroke, renal failure, atrial fibrillation, reoperation for bleeding, and respiratory insufficiency were not statistically significantly different between the two groups. There was also no significant difference in ICU or hospital length of stay between the two groups. However, mini-AVR was associated with both significantly decreased ventilator time (5 vs. 6 hours) and blood product transfusion (25% vs. 32%), according to the report, which was published online and scheduled for the April issue of the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j/jtcvs.2015.01.014).
Total hospital cost was significantly lower in the mini-AVR group ($36,348) vs. the conventional repair group ($38,239, P = .02), wrote Dr. Ravi Kiran Ghanta of the University of Virginia, Charlottesville, and his colleagues.
The authors discussed the previously raised issue of longer cross-clamp and bypass times seen in earlier studies of mini-AVR. In their current study, such was not the case, with mini-AVR appearing equivalent with conventional operations. The authors suggested that surgeons have now adopted techniques to reduce bypass and cross-clamp times with mini-AVR.
Data were limited to in-hospital costs. Other costs, such as those of rehabilitation and lost productivity, were not included in the analysis. “Including these health-care costs may have increased overall savings with mini-AVR compared to conventional AVR,” the authors noted.
“Mini-AVR is associated with decreased ventilator time, blood product utilization, early discharge, and reduced total hospital cost. In contemporary clinical practice, mini-AVR is safe and cost-effective,” the researchers concluded.
The authors reported that they had no conflicts.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Mortality, stroke, renal failure, and other complications were not significantly different between mini-aortic valve replacement and conventional replacement.
Major finding: Total hospital costs were significantly lower with mini-AVR, compared with conventional replacement ($36,348 vs. $38,239).
Data source: A retrospective data analysis of patient records for isolated AVR repair, extracted from a regional, multi-institutional Society of Thoracic Surgeons database.
Disclosures: The authors reported that they had no relevant conflicts of interest.
Perioperative treatment with diuretic linked with lower lung cancer recurrence
Patients with lung cancer who underwent surgery to remove solid tumors and who were treated with atrial natriuretic peptide (ANP) had significantly lower cancer recurrence than did untreated patients, according to a report published in the Proceedings of the National Academy of Sciences.
Investigators retrospectively evaluated patients with lung cancer who underwent surgical removal of tumors; 77 patients received perioperative treatment with ANP and 390 patients did not receive ANP treatment.
ANP-treated patients had significantly greater 2-year relapse-free survival (RFS) after surgery than did those who did not receive ANP (91% vs. 75%, P = .018). Analysis of propensity-matched patients also showed significantly greater 2-year RFS in the ANP group (91% vs. 67%, P = .0013), reported Dr. Takashi Nojiri of Osaka (Japan) University Graduate School of Medicine, and his associates.
“We demonstrated that cancer recurrence after curative surgery was significantly lower in ANP-treated patients than in control patients, suggesting that ANP could potentially be used to prevent cancer recurrence after surgery,” wrote Dr. Nojiri and colleagues (Proc. Natl. Acad. Sci. USA 2015 March 16 [doi:10.1073/pnas.1417273112]).
Atrial natriuretic peptide is a vasodilating hormone from the human heart and acts as a diuretic; previous studies have shown that administration during the perioperative period reduces inflammatory responses and has a prophylactic effect on postoperative cardiopulmonary complications in lung cancer surgery.
Patients with lung cancer who underwent surgery to remove solid tumors and who were treated with atrial natriuretic peptide (ANP) had significantly lower cancer recurrence than did untreated patients, according to a report published in the Proceedings of the National Academy of Sciences.
Investigators retrospectively evaluated patients with lung cancer who underwent surgical removal of tumors; 77 patients received perioperative treatment with ANP and 390 patients did not receive ANP treatment.
ANP-treated patients had significantly greater 2-year relapse-free survival (RFS) after surgery than did those who did not receive ANP (91% vs. 75%, P = .018). Analysis of propensity-matched patients also showed significantly greater 2-year RFS in the ANP group (91% vs. 67%, P = .0013), reported Dr. Takashi Nojiri of Osaka (Japan) University Graduate School of Medicine, and his associates.
“We demonstrated that cancer recurrence after curative surgery was significantly lower in ANP-treated patients than in control patients, suggesting that ANP could potentially be used to prevent cancer recurrence after surgery,” wrote Dr. Nojiri and colleagues (Proc. Natl. Acad. Sci. USA 2015 March 16 [doi:10.1073/pnas.1417273112]).
Atrial natriuretic peptide is a vasodilating hormone from the human heart and acts as a diuretic; previous studies have shown that administration during the perioperative period reduces inflammatory responses and has a prophylactic effect on postoperative cardiopulmonary complications in lung cancer surgery.
Patients with lung cancer who underwent surgery to remove solid tumors and who were treated with atrial natriuretic peptide (ANP) had significantly lower cancer recurrence than did untreated patients, according to a report published in the Proceedings of the National Academy of Sciences.
Investigators retrospectively evaluated patients with lung cancer who underwent surgical removal of tumors; 77 patients received perioperative treatment with ANP and 390 patients did not receive ANP treatment.
ANP-treated patients had significantly greater 2-year relapse-free survival (RFS) after surgery than did those who did not receive ANP (91% vs. 75%, P = .018). Analysis of propensity-matched patients also showed significantly greater 2-year RFS in the ANP group (91% vs. 67%, P = .0013), reported Dr. Takashi Nojiri of Osaka (Japan) University Graduate School of Medicine, and his associates.
“We demonstrated that cancer recurrence after curative surgery was significantly lower in ANP-treated patients than in control patients, suggesting that ANP could potentially be used to prevent cancer recurrence after surgery,” wrote Dr. Nojiri and colleagues (Proc. Natl. Acad. Sci. USA 2015 March 16 [doi:10.1073/pnas.1417273112]).
Atrial natriuretic peptide is a vasodilating hormone from the human heart and acts as a diuretic; previous studies have shown that administration during the perioperative period reduces inflammatory responses and has a prophylactic effect on postoperative cardiopulmonary complications in lung cancer surgery.
FROM PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
Key clinical point: After surgical removal of tumors, lung cancer patients treated with atrial natriuretic peptide had a significantly lower recurrence rate than did patients who had not received atrial natriuretic peptide.
Major finding: Patients treated with atrial natriuretic peptide had significantly greater 2-year relapse-free survival than did untreated patients (91% vs. 75%, P = .018).
Data source: The retrospective study included 390 patients who were not treated with atrial natriuretic peptide and 77 patients who were.
Disclosures: Dr. Nojiri and two other authors have filed a patent related to atrial natriuretic peptide treatment for cancer metastasis with Daiichi-Sankyo Pharmaceutical Inc.