User login
Official Newspaper of the American College of Surgeons
HHS report: Record number of patients covered under ACA
About 16.4 million Americans have gained health insurance coverage since the Affordable Care Act took effect, dropping the U.S. uninsured rate by 7 percentage points, according to a new report released March 16 by the Department of Health and Human Services.
That includes 14.1 million adults who secured coverage since the beginning of open enrollment in October 2013 and 2.3 million young adults who have obtained coverage since 2010 because of the ACA’s provision allowing them to remain on a parent’s plan until age 26 years. From October 2013 to March 2015, the rate of uninsured patients fell from 20% to 13%, the report found.
Dr. Richard G. Frank, HHS assistant secretary for planning and evaluation called the reduction unprecedented.
“This is a historical drop in the uninsured, and nothing since the implementation of Medicare and Medicaid comes near to this type of change,” Dr. Frank said during a press conference. “We’re seeing gains across races and ethnicities. We’re seeing gains in all age groups, and we’re seeing notable gains in expansion states. ... Numbers and statistics are important, and the story they are telling is that the Affordable Care Act is working to drive down the number of uninsured.”
The uninsured rate has declined across all race and ethnicities since the law’s 2010 implementation, with a greater reduction among uninsured blacks and Hispanics, the report found. This includes 5-percentage point reduction in the rate of uninsured whites, a 9-percentage point reduction in the rate of uninsured blacks, and a 12-percentage point reduction in the rate of uninsured Hispanics.
Coverage gains were especially strong in states that expanded their Medicaid programs, according to the report. The baseline uninsurance rate in expansion states was 18%; by March 2015, that had dropped 7.4 percentage points. In states that have not expanded Medicaid, the average baseline uninsured rate was 23%; that rate has dropped almost 7 percentage points since the law took effect.
For young adults aged 19-25 years, the uninsured rate fell from 34% to 27% between 2010 and October 2013. In a statement, HHS Secretary Sylvia M. Burwell said the uninsured rate reduction is the largest in 4 decades.
“Because of the Affordable Care Act, young adults are able to stay on their parents’ plans until age 26, states can expand their Medicaid programs, and tax credits are available to millions of Americans in all 50 states, making health care coverage more affordable and accessible,” Ms. Burwell said in the statement. “When it comes to the key metrics of affordability, access, and quality, the evidence shows that the Affordable Care Act is working, and families, businesses and taxpayers are better off as a result.”
On Twitter @legal_med
About 16.4 million Americans have gained health insurance coverage since the Affordable Care Act took effect, dropping the U.S. uninsured rate by 7 percentage points, according to a new report released March 16 by the Department of Health and Human Services.
That includes 14.1 million adults who secured coverage since the beginning of open enrollment in October 2013 and 2.3 million young adults who have obtained coverage since 2010 because of the ACA’s provision allowing them to remain on a parent’s plan until age 26 years. From October 2013 to March 2015, the rate of uninsured patients fell from 20% to 13%, the report found.
Dr. Richard G. Frank, HHS assistant secretary for planning and evaluation called the reduction unprecedented.
“This is a historical drop in the uninsured, and nothing since the implementation of Medicare and Medicaid comes near to this type of change,” Dr. Frank said during a press conference. “We’re seeing gains across races and ethnicities. We’re seeing gains in all age groups, and we’re seeing notable gains in expansion states. ... Numbers and statistics are important, and the story they are telling is that the Affordable Care Act is working to drive down the number of uninsured.”
The uninsured rate has declined across all race and ethnicities since the law’s 2010 implementation, with a greater reduction among uninsured blacks and Hispanics, the report found. This includes 5-percentage point reduction in the rate of uninsured whites, a 9-percentage point reduction in the rate of uninsured blacks, and a 12-percentage point reduction in the rate of uninsured Hispanics.
Coverage gains were especially strong in states that expanded their Medicaid programs, according to the report. The baseline uninsurance rate in expansion states was 18%; by March 2015, that had dropped 7.4 percentage points. In states that have not expanded Medicaid, the average baseline uninsured rate was 23%; that rate has dropped almost 7 percentage points since the law took effect.
For young adults aged 19-25 years, the uninsured rate fell from 34% to 27% between 2010 and October 2013. In a statement, HHS Secretary Sylvia M. Burwell said the uninsured rate reduction is the largest in 4 decades.
“Because of the Affordable Care Act, young adults are able to stay on their parents’ plans until age 26, states can expand their Medicaid programs, and tax credits are available to millions of Americans in all 50 states, making health care coverage more affordable and accessible,” Ms. Burwell said in the statement. “When it comes to the key metrics of affordability, access, and quality, the evidence shows that the Affordable Care Act is working, and families, businesses and taxpayers are better off as a result.”
On Twitter @legal_med
About 16.4 million Americans have gained health insurance coverage since the Affordable Care Act took effect, dropping the U.S. uninsured rate by 7 percentage points, according to a new report released March 16 by the Department of Health and Human Services.
That includes 14.1 million adults who secured coverage since the beginning of open enrollment in October 2013 and 2.3 million young adults who have obtained coverage since 2010 because of the ACA’s provision allowing them to remain on a parent’s plan until age 26 years. From October 2013 to March 2015, the rate of uninsured patients fell from 20% to 13%, the report found.
Dr. Richard G. Frank, HHS assistant secretary for planning and evaluation called the reduction unprecedented.
“This is a historical drop in the uninsured, and nothing since the implementation of Medicare and Medicaid comes near to this type of change,” Dr. Frank said during a press conference. “We’re seeing gains across races and ethnicities. We’re seeing gains in all age groups, and we’re seeing notable gains in expansion states. ... Numbers and statistics are important, and the story they are telling is that the Affordable Care Act is working to drive down the number of uninsured.”
The uninsured rate has declined across all race and ethnicities since the law’s 2010 implementation, with a greater reduction among uninsured blacks and Hispanics, the report found. This includes 5-percentage point reduction in the rate of uninsured whites, a 9-percentage point reduction in the rate of uninsured blacks, and a 12-percentage point reduction in the rate of uninsured Hispanics.
Coverage gains were especially strong in states that expanded their Medicaid programs, according to the report. The baseline uninsurance rate in expansion states was 18%; by March 2015, that had dropped 7.4 percentage points. In states that have not expanded Medicaid, the average baseline uninsured rate was 23%; that rate has dropped almost 7 percentage points since the law took effect.
For young adults aged 19-25 years, the uninsured rate fell from 34% to 27% between 2010 and October 2013. In a statement, HHS Secretary Sylvia M. Burwell said the uninsured rate reduction is the largest in 4 decades.
“Because of the Affordable Care Act, young adults are able to stay on their parents’ plans until age 26, states can expand their Medicaid programs, and tax credits are available to millions of Americans in all 50 states, making health care coverage more affordable and accessible,” Ms. Burwell said in the statement. “When it comes to the key metrics of affordability, access, and quality, the evidence shows that the Affordable Care Act is working, and families, businesses and taxpayers are better off as a result.”
On Twitter @legal_med
Stem cell divisions help dictate cancer risk
The lifetime risk of many different types of cancer are correlated (0.81) with the total number of divisions of their tissue stem cells, a recent study round.
This can allow any of the most common cancer types to be differentiated into replicative (R) or deterministic (D) types, according to the results of a correlative literature review comparing cancer incidence in tissues to their known stem cell behavior. Whether a cancer is R or D has profound implications for prevention and detection, according to a report in Science (2015;347:78-81).
Extreme variation in the lifetime incidence of cancer across various tissues exist, ranging from levels such as 6.9% in the lung down to 0.00072% for laryngeal cartilage, according to Cristian Tomasetti, Ph.D., of the Johns Hopkins Bloomberg School of Public Heath and Dr. Bert Vogelstein of the Johns Hopkins Kimmel Cancer Center, both in Baltimore.
Environmental exposure to known carcinogens seems to be a factor in some, but this cannot explain why cancers of the small intestinal epithelium are three times less common than brain tumors, even though the intestinal cells are exposed to much higher levels of environmental mutagens than are the brain cells, which are protected by the blood-brain barrier. And heredity fails as a complete explanation, with only 5%-10% of cancers having a heritable component.
“If heredity and environment factors cannot fully explain the differences in organ-specific cancer risk, how else can these differences be explained?” the authors asked. They postulated that somatic cell mutation during DNA replication as the result of cell division may be a critical factor, implying that the greater level of cell division, the greater level of mutagenesis, and hence cancer. Stem cells, which both self-renew and are responsible for tissue maintenance were the obvious candidates for such mutations, and recently the technology has developed to detect and quantify them.
Via a literature search, the authors identified 31 tissue types in which stem cells had been quantitatively assessed, then plotted the total number of stem cell divisions during an average human lifetime for each of these tissues on the X axis, and the lifetime risk in the United States for the associated cancer types from sources such as the Surveillance, Epidemiology, and End Results (SEER) database. Not only was there a strikingly high positive correlation (0.81), which indicated that 65% of the differences of cancer risk among different tissues can be explained by the total number of stem cell divisions in these tissues, the correlation extended across five orders of magnitude, “thereby applying to cancers with enormous differences in incidence,” according to Dr. Tomasetti and Dr. Vogelstein.
They then proceeded to attempt to distinguish the effect of this cell-replicative component from environmental and hereditary factors that contribute to the incidence of cancer. They defined an extra risk score (ERS) as the log product of the lifetime risk of cancer and the total number of stem cell divisions. They then used unsupervised machine learning methods to classify tumors based only on this score into two groups. The result was 9 tumors with high scores and 22 tumors with low ERS scores. If the ERS was high, it meant that there were added factors, such as heredity and environment, contributing to increase the cancer incidence. These they referred to as D-tumors (deterministic). If the ERS was low, that meant that stochastic factors during cell division were the main contributors to incidence, which they called R-tumors (replicative). Upon inspection, the D-tumors were indeed those that had been previously found to have a high hereditary or environmental component. A notable D-tumor, for example, was lung cancer in smokers, while lung cancer in nonsmokers was designated an R-tumor.
“These results have could have important public health implications,” the researchers indicated.
“The maximum fraction of tumors that are preventable through primary prevention (such as vaccines against infectious agents or altered lifestyle) may be evaluated from their ERS. For nonhereditary D-tumors, this fraction is high and primary prevention may make a major impact. ... For R-tumors, primary prevention measures are not likely to be effective, and secondary prevention should be the major focus,” Dr. Tomasetti and Dr. Vogelstein concluded.
The authors reported no relevant disclosures.
This paper published in Science addresses the question of why different tissues in the body are more prone to carcinogenesis than others. The authors hypothesize that environmental factors or inherited predispositions do not explain these differences. An example given is melanocytes and basal epidermal cells in the skin. Each are exposed to the same carcinogen (UV light) at an identical dose, yet melanomas are much less common than are basal cell carcinomas. The explanation arrived at by the authors focuses on stem cells in each tissue.
Stem cells are the only cells that can self-renew and serve to maintain a tissue’s architecture and development. The authors performed a literature search and plotted the total number of stem cell divisions during the average lifetime of a human vs. the lifetime risk for cancer in that tissue type. A linear correlation was performed and found that 65% of the differences in cancer risk among different tissues were explained by total number of stem cell divisions in those tissues. In other words, the more stem cells divide in a tissue, the greater chance of mutations occurring leading to malignancy.
The simple yet elegant concept helps explain the melanoma and basal cell carcinoma differences as well as why those with familial adenomatous polyposis (APC) are 30 times more likely to develop colon carcinoma than duodenal cancer. Human colons have 150-fold more stem cell divisions than the small intestine. Amazingly, mice have more stem cell divisions in their small intestines and in the presence of APC mutation for adenomatous polyps, small intestine tumors are more common than ones in the colon. The authors’ findings suggest in cases where these tumors develop independent of environmental and hereditary factors, secondary prevention such as early detection need to be the driving focus to improve clinical outcomes.
Dr. Michael J. Liptay is the Mary and John Bent Professor and chairman of cardiovascular and thoracic surgery, director of cardiothoracic surgery, and chief of thoracic surgery at Rush University Medical Center, Chicago, and the medical editor of Thoracic Surgery News.
This paper published in Science addresses the question of why different tissues in the body are more prone to carcinogenesis than others. The authors hypothesize that environmental factors or inherited predispositions do not explain these differences. An example given is melanocytes and basal epidermal cells in the skin. Each are exposed to the same carcinogen (UV light) at an identical dose, yet melanomas are much less common than are basal cell carcinomas. The explanation arrived at by the authors focuses on stem cells in each tissue.
Stem cells are the only cells that can self-renew and serve to maintain a tissue’s architecture and development. The authors performed a literature search and plotted the total number of stem cell divisions during the average lifetime of a human vs. the lifetime risk for cancer in that tissue type. A linear correlation was performed and found that 65% of the differences in cancer risk among different tissues were explained by total number of stem cell divisions in those tissues. In other words, the more stem cells divide in a tissue, the greater chance of mutations occurring leading to malignancy.
The simple yet elegant concept helps explain the melanoma and basal cell carcinoma differences as well as why those with familial adenomatous polyposis (APC) are 30 times more likely to develop colon carcinoma than duodenal cancer. Human colons have 150-fold more stem cell divisions than the small intestine. Amazingly, mice have more stem cell divisions in their small intestines and in the presence of APC mutation for adenomatous polyps, small intestine tumors are more common than ones in the colon. The authors’ findings suggest in cases where these tumors develop independent of environmental and hereditary factors, secondary prevention such as early detection need to be the driving focus to improve clinical outcomes.
Dr. Michael J. Liptay is the Mary and John Bent Professor and chairman of cardiovascular and thoracic surgery, director of cardiothoracic surgery, and chief of thoracic surgery at Rush University Medical Center, Chicago, and the medical editor of Thoracic Surgery News.
This paper published in Science addresses the question of why different tissues in the body are more prone to carcinogenesis than others. The authors hypothesize that environmental factors or inherited predispositions do not explain these differences. An example given is melanocytes and basal epidermal cells in the skin. Each are exposed to the same carcinogen (UV light) at an identical dose, yet melanomas are much less common than are basal cell carcinomas. The explanation arrived at by the authors focuses on stem cells in each tissue.
Stem cells are the only cells that can self-renew and serve to maintain a tissue’s architecture and development. The authors performed a literature search and plotted the total number of stem cell divisions during the average lifetime of a human vs. the lifetime risk for cancer in that tissue type. A linear correlation was performed and found that 65% of the differences in cancer risk among different tissues were explained by total number of stem cell divisions in those tissues. In other words, the more stem cells divide in a tissue, the greater chance of mutations occurring leading to malignancy.
The simple yet elegant concept helps explain the melanoma and basal cell carcinoma differences as well as why those with familial adenomatous polyposis (APC) are 30 times more likely to develop colon carcinoma than duodenal cancer. Human colons have 150-fold more stem cell divisions than the small intestine. Amazingly, mice have more stem cell divisions in their small intestines and in the presence of APC mutation for adenomatous polyps, small intestine tumors are more common than ones in the colon. The authors’ findings suggest in cases where these tumors develop independent of environmental and hereditary factors, secondary prevention such as early detection need to be the driving focus to improve clinical outcomes.
Dr. Michael J. Liptay is the Mary and John Bent Professor and chairman of cardiovascular and thoracic surgery, director of cardiothoracic surgery, and chief of thoracic surgery at Rush University Medical Center, Chicago, and the medical editor of Thoracic Surgery News.
The lifetime risk of many different types of cancer are correlated (0.81) with the total number of divisions of their tissue stem cells, a recent study round.
This can allow any of the most common cancer types to be differentiated into replicative (R) or deterministic (D) types, according to the results of a correlative literature review comparing cancer incidence in tissues to their known stem cell behavior. Whether a cancer is R or D has profound implications for prevention and detection, according to a report in Science (2015;347:78-81).
Extreme variation in the lifetime incidence of cancer across various tissues exist, ranging from levels such as 6.9% in the lung down to 0.00072% for laryngeal cartilage, according to Cristian Tomasetti, Ph.D., of the Johns Hopkins Bloomberg School of Public Heath and Dr. Bert Vogelstein of the Johns Hopkins Kimmel Cancer Center, both in Baltimore.
Environmental exposure to known carcinogens seems to be a factor in some, but this cannot explain why cancers of the small intestinal epithelium are three times less common than brain tumors, even though the intestinal cells are exposed to much higher levels of environmental mutagens than are the brain cells, which are protected by the blood-brain barrier. And heredity fails as a complete explanation, with only 5%-10% of cancers having a heritable component.
“If heredity and environment factors cannot fully explain the differences in organ-specific cancer risk, how else can these differences be explained?” the authors asked. They postulated that somatic cell mutation during DNA replication as the result of cell division may be a critical factor, implying that the greater level of cell division, the greater level of mutagenesis, and hence cancer. Stem cells, which both self-renew and are responsible for tissue maintenance were the obvious candidates for such mutations, and recently the technology has developed to detect and quantify them.
Via a literature search, the authors identified 31 tissue types in which stem cells had been quantitatively assessed, then plotted the total number of stem cell divisions during an average human lifetime for each of these tissues on the X axis, and the lifetime risk in the United States for the associated cancer types from sources such as the Surveillance, Epidemiology, and End Results (SEER) database. Not only was there a strikingly high positive correlation (0.81), which indicated that 65% of the differences of cancer risk among different tissues can be explained by the total number of stem cell divisions in these tissues, the correlation extended across five orders of magnitude, “thereby applying to cancers with enormous differences in incidence,” according to Dr. Tomasetti and Dr. Vogelstein.
They then proceeded to attempt to distinguish the effect of this cell-replicative component from environmental and hereditary factors that contribute to the incidence of cancer. They defined an extra risk score (ERS) as the log product of the lifetime risk of cancer and the total number of stem cell divisions. They then used unsupervised machine learning methods to classify tumors based only on this score into two groups. The result was 9 tumors with high scores and 22 tumors with low ERS scores. If the ERS was high, it meant that there were added factors, such as heredity and environment, contributing to increase the cancer incidence. These they referred to as D-tumors (deterministic). If the ERS was low, that meant that stochastic factors during cell division were the main contributors to incidence, which they called R-tumors (replicative). Upon inspection, the D-tumors were indeed those that had been previously found to have a high hereditary or environmental component. A notable D-tumor, for example, was lung cancer in smokers, while lung cancer in nonsmokers was designated an R-tumor.
“These results have could have important public health implications,” the researchers indicated.
“The maximum fraction of tumors that are preventable through primary prevention (such as vaccines against infectious agents or altered lifestyle) may be evaluated from their ERS. For nonhereditary D-tumors, this fraction is high and primary prevention may make a major impact. ... For R-tumors, primary prevention measures are not likely to be effective, and secondary prevention should be the major focus,” Dr. Tomasetti and Dr. Vogelstein concluded.
The authors reported no relevant disclosures.
The lifetime risk of many different types of cancer are correlated (0.81) with the total number of divisions of their tissue stem cells, a recent study round.
This can allow any of the most common cancer types to be differentiated into replicative (R) or deterministic (D) types, according to the results of a correlative literature review comparing cancer incidence in tissues to their known stem cell behavior. Whether a cancer is R or D has profound implications for prevention and detection, according to a report in Science (2015;347:78-81).
Extreme variation in the lifetime incidence of cancer across various tissues exist, ranging from levels such as 6.9% in the lung down to 0.00072% for laryngeal cartilage, according to Cristian Tomasetti, Ph.D., of the Johns Hopkins Bloomberg School of Public Heath and Dr. Bert Vogelstein of the Johns Hopkins Kimmel Cancer Center, both in Baltimore.
Environmental exposure to known carcinogens seems to be a factor in some, but this cannot explain why cancers of the small intestinal epithelium are three times less common than brain tumors, even though the intestinal cells are exposed to much higher levels of environmental mutagens than are the brain cells, which are protected by the blood-brain barrier. And heredity fails as a complete explanation, with only 5%-10% of cancers having a heritable component.
“If heredity and environment factors cannot fully explain the differences in organ-specific cancer risk, how else can these differences be explained?” the authors asked. They postulated that somatic cell mutation during DNA replication as the result of cell division may be a critical factor, implying that the greater level of cell division, the greater level of mutagenesis, and hence cancer. Stem cells, which both self-renew and are responsible for tissue maintenance were the obvious candidates for such mutations, and recently the technology has developed to detect and quantify them.
Via a literature search, the authors identified 31 tissue types in which stem cells had been quantitatively assessed, then plotted the total number of stem cell divisions during an average human lifetime for each of these tissues on the X axis, and the lifetime risk in the United States for the associated cancer types from sources such as the Surveillance, Epidemiology, and End Results (SEER) database. Not only was there a strikingly high positive correlation (0.81), which indicated that 65% of the differences of cancer risk among different tissues can be explained by the total number of stem cell divisions in these tissues, the correlation extended across five orders of magnitude, “thereby applying to cancers with enormous differences in incidence,” according to Dr. Tomasetti and Dr. Vogelstein.
They then proceeded to attempt to distinguish the effect of this cell-replicative component from environmental and hereditary factors that contribute to the incidence of cancer. They defined an extra risk score (ERS) as the log product of the lifetime risk of cancer and the total number of stem cell divisions. They then used unsupervised machine learning methods to classify tumors based only on this score into two groups. The result was 9 tumors with high scores and 22 tumors with low ERS scores. If the ERS was high, it meant that there were added factors, such as heredity and environment, contributing to increase the cancer incidence. These they referred to as D-tumors (deterministic). If the ERS was low, that meant that stochastic factors during cell division were the main contributors to incidence, which they called R-tumors (replicative). Upon inspection, the D-tumors were indeed those that had been previously found to have a high hereditary or environmental component. A notable D-tumor, for example, was lung cancer in smokers, while lung cancer in nonsmokers was designated an R-tumor.
“These results have could have important public health implications,” the researchers indicated.
“The maximum fraction of tumors that are preventable through primary prevention (such as vaccines against infectious agents or altered lifestyle) may be evaluated from their ERS. For nonhereditary D-tumors, this fraction is high and primary prevention may make a major impact. ... For R-tumors, primary prevention measures are not likely to be effective, and secondary prevention should be the major focus,” Dr. Tomasetti and Dr. Vogelstein concluded.
The authors reported no relevant disclosures.
FROM SCIENCE
Key clinical point: Only a third of the variation in cancer risk among tissues is because of the environment or inheritance, and this has implications with regard to prevention and detection.
Major finding: The lifetime risk of many different types of cancer are correlated (0.81) with the total number of divisions of their tissue stem cells.
Data source: Researchers performed a literature review to correlate cancer incidence in a variety of tissues with the nature, number, and hierarchical division patterns of the tissue’s stem cells.
Disclosures: The researchers reported no relevant disclosures.
Greater surgeon experience linked to better long-term survival in NSCLC
Surgeon experience may be a factor in long-term survival of patients after lung resection for non–small cell lung cancer (NSCLC) but the correlation between the two is not straightforward.
Postfellowship surgeon experience did not influence perioperative outcomes in pathologic stage I NSCLC. However, a moderate level of experience was associated with greater utilization of video-assisted thoracic surgery, higher mediastinal lymph noted yield, and improved 5-year survival, according to the results of a single center, retrospective review of a lung cancer database.
Between January 2000 and December 2012, 800 patients underwent resection for pathologic stage I NSCLC by eight surgeons – comprising 638 lobectomies (79.8%) and 162 sublobar resections (20.2%).
Experience was based on the number of years at the time of surgery beyond the individual’s completion of a cardiothoracic surgery fellowship. The low-experience (LE) group was defined as operations conducted within the first 5 years of practice after specialty training. The moderate-experience (ME) group comprised surgeons with experience of 5-15 years. The high-experience (HE) group comprised surgeons with more than 15 years post fellowship, according to Paul J. Scheel III and colleagues in the division of cardiothoracic surgery, Washington University, St. Louis.
Over the complete time period, operations were performed by six different surgeons in the LE group, five surgeons in the ME group, and two surgeons in the HE group. By multiple criteria in previous publications, “all the operators involved in our study are specialty trained in thoracic surgery, and are high-volume surgeons,” which eliminates some potential confounders, according to the report, which was published online and in the April issue of The Journal of Thoracic and Cardiovascular Surgery. [doi:10.1016/j.jtcvs.2014.12.032].
The number of mediastinal (N2) lymph node stations sampled per operation was highest for the ME group and lowest for the HE group: LE = 2.8, ME = 3.5, and HE = 2.3, all of which were significantly different across all groups.
The risk of perioperative morbidity defined by STS criteria was not significantly different: with LE = 30.3%, ME = 22.8%, and HE = 28.9%, all similar (P = .163). There were no differences seen in length of hospital stay or perioperative mortality between the groups.
Unadjusted 5-year survival, however, was significantly higher in the ME group (76.9%) compared to the LE group (67.5%, P < .001) and the HE group (71.4%, P = .006). In addition, the ME group surgeons were significantly more likely to have used video-assisted thoracic surgery (VATS) than were the other two groups.
In their discussion, the researchers pointed out a possible reason for the difference seen in mortality: “We noted that the ME group tended to have a higher yield of lymph nodes and this also correlated with survival. It is plausible that surgeons who are in the early stage of their career may be completely focused on ‘getting the specimen out’ with less attention being paid to nodal sampling with its added operative time and perceived additional morbidity.” HE surgeons may have lower yields because “the importance of nodal sampling has been predominately realized over the last 2 decades,” they pointed out.
“Patients operated on by moderately experienced surgeons may have better long-term survival after resection for pathologic stage I lung cancer. Expanding this study to a larger patient and surgeon population would be needed to validate the results and identify the underlying causes for these differences in order to provide the best patient care,” the researchers concluded.
The authors reported having no conflicts of interest.
How do you measure surgeon experience? “What is more important, the surgeon maturity, the volume of surgeries, or a reference oncologic hospital? I believe that experience in surgery is not mathematics, but is an art that any one can be trained to do,” Dr. Daniele Cristina Cataneo wrote in her invited editorial commentary [doi: 10.1016/j.jtcvs.2014.12.073].
This is borne out by this study, she added. The authors have answered the question – surgeon experience has no impact on perioperative outcomes, but can affect long-term survival based upon N2 resection. This means that the pertinent component of experience can be trained, i.e., sampling more nodes. She concluded that with appropriate training, a surgeon could be rendered “experienced” to operate in early stage lung cancer – not only without complications, but also, by increasing N2 resection, with improved survival.
Dr. Cataneo is an associate professor of thoracic surgery at the Botucatu School of Medicine, Sao Paulo State University, Brazil.
How do you measure surgeon experience? “What is more important, the surgeon maturity, the volume of surgeries, or a reference oncologic hospital? I believe that experience in surgery is not mathematics, but is an art that any one can be trained to do,” Dr. Daniele Cristina Cataneo wrote in her invited editorial commentary [doi: 10.1016/j.jtcvs.2014.12.073].
This is borne out by this study, she added. The authors have answered the question – surgeon experience has no impact on perioperative outcomes, but can affect long-term survival based upon N2 resection. This means that the pertinent component of experience can be trained, i.e., sampling more nodes. She concluded that with appropriate training, a surgeon could be rendered “experienced” to operate in early stage lung cancer – not only without complications, but also, by increasing N2 resection, with improved survival.
Dr. Cataneo is an associate professor of thoracic surgery at the Botucatu School of Medicine, Sao Paulo State University, Brazil.
How do you measure surgeon experience? “What is more important, the surgeon maturity, the volume of surgeries, or a reference oncologic hospital? I believe that experience in surgery is not mathematics, but is an art that any one can be trained to do,” Dr. Daniele Cristina Cataneo wrote in her invited editorial commentary [doi: 10.1016/j.jtcvs.2014.12.073].
This is borne out by this study, she added. The authors have answered the question – surgeon experience has no impact on perioperative outcomes, but can affect long-term survival based upon N2 resection. This means that the pertinent component of experience can be trained, i.e., sampling more nodes. She concluded that with appropriate training, a surgeon could be rendered “experienced” to operate in early stage lung cancer – not only without complications, but also, by increasing N2 resection, with improved survival.
Dr. Cataneo is an associate professor of thoracic surgery at the Botucatu School of Medicine, Sao Paulo State University, Brazil.
Surgeon experience may be a factor in long-term survival of patients after lung resection for non–small cell lung cancer (NSCLC) but the correlation between the two is not straightforward.
Postfellowship surgeon experience did not influence perioperative outcomes in pathologic stage I NSCLC. However, a moderate level of experience was associated with greater utilization of video-assisted thoracic surgery, higher mediastinal lymph noted yield, and improved 5-year survival, according to the results of a single center, retrospective review of a lung cancer database.
Between January 2000 and December 2012, 800 patients underwent resection for pathologic stage I NSCLC by eight surgeons – comprising 638 lobectomies (79.8%) and 162 sublobar resections (20.2%).
Experience was based on the number of years at the time of surgery beyond the individual’s completion of a cardiothoracic surgery fellowship. The low-experience (LE) group was defined as operations conducted within the first 5 years of practice after specialty training. The moderate-experience (ME) group comprised surgeons with experience of 5-15 years. The high-experience (HE) group comprised surgeons with more than 15 years post fellowship, according to Paul J. Scheel III and colleagues in the division of cardiothoracic surgery, Washington University, St. Louis.
Over the complete time period, operations were performed by six different surgeons in the LE group, five surgeons in the ME group, and two surgeons in the HE group. By multiple criteria in previous publications, “all the operators involved in our study are specialty trained in thoracic surgery, and are high-volume surgeons,” which eliminates some potential confounders, according to the report, which was published online and in the April issue of The Journal of Thoracic and Cardiovascular Surgery. [doi:10.1016/j.jtcvs.2014.12.032].
The number of mediastinal (N2) lymph node stations sampled per operation was highest for the ME group and lowest for the HE group: LE = 2.8, ME = 3.5, and HE = 2.3, all of which were significantly different across all groups.
The risk of perioperative morbidity defined by STS criteria was not significantly different: with LE = 30.3%, ME = 22.8%, and HE = 28.9%, all similar (P = .163). There were no differences seen in length of hospital stay or perioperative mortality between the groups.
Unadjusted 5-year survival, however, was significantly higher in the ME group (76.9%) compared to the LE group (67.5%, P < .001) and the HE group (71.4%, P = .006). In addition, the ME group surgeons were significantly more likely to have used video-assisted thoracic surgery (VATS) than were the other two groups.
In their discussion, the researchers pointed out a possible reason for the difference seen in mortality: “We noted that the ME group tended to have a higher yield of lymph nodes and this also correlated with survival. It is plausible that surgeons who are in the early stage of their career may be completely focused on ‘getting the specimen out’ with less attention being paid to nodal sampling with its added operative time and perceived additional morbidity.” HE surgeons may have lower yields because “the importance of nodal sampling has been predominately realized over the last 2 decades,” they pointed out.
“Patients operated on by moderately experienced surgeons may have better long-term survival after resection for pathologic stage I lung cancer. Expanding this study to a larger patient and surgeon population would be needed to validate the results and identify the underlying causes for these differences in order to provide the best patient care,” the researchers concluded.
The authors reported having no conflicts of interest.
Surgeon experience may be a factor in long-term survival of patients after lung resection for non–small cell lung cancer (NSCLC) but the correlation between the two is not straightforward.
Postfellowship surgeon experience did not influence perioperative outcomes in pathologic stage I NSCLC. However, a moderate level of experience was associated with greater utilization of video-assisted thoracic surgery, higher mediastinal lymph noted yield, and improved 5-year survival, according to the results of a single center, retrospective review of a lung cancer database.
Between January 2000 and December 2012, 800 patients underwent resection for pathologic stage I NSCLC by eight surgeons – comprising 638 lobectomies (79.8%) and 162 sublobar resections (20.2%).
Experience was based on the number of years at the time of surgery beyond the individual’s completion of a cardiothoracic surgery fellowship. The low-experience (LE) group was defined as operations conducted within the first 5 years of practice after specialty training. The moderate-experience (ME) group comprised surgeons with experience of 5-15 years. The high-experience (HE) group comprised surgeons with more than 15 years post fellowship, according to Paul J. Scheel III and colleagues in the division of cardiothoracic surgery, Washington University, St. Louis.
Over the complete time period, operations were performed by six different surgeons in the LE group, five surgeons in the ME group, and two surgeons in the HE group. By multiple criteria in previous publications, “all the operators involved in our study are specialty trained in thoracic surgery, and are high-volume surgeons,” which eliminates some potential confounders, according to the report, which was published online and in the April issue of The Journal of Thoracic and Cardiovascular Surgery. [doi:10.1016/j.jtcvs.2014.12.032].
The number of mediastinal (N2) lymph node stations sampled per operation was highest for the ME group and lowest for the HE group: LE = 2.8, ME = 3.5, and HE = 2.3, all of which were significantly different across all groups.
The risk of perioperative morbidity defined by STS criteria was not significantly different: with LE = 30.3%, ME = 22.8%, and HE = 28.9%, all similar (P = .163). There were no differences seen in length of hospital stay or perioperative mortality between the groups.
Unadjusted 5-year survival, however, was significantly higher in the ME group (76.9%) compared to the LE group (67.5%, P < .001) and the HE group (71.4%, P = .006). In addition, the ME group surgeons were significantly more likely to have used video-assisted thoracic surgery (VATS) than were the other two groups.
In their discussion, the researchers pointed out a possible reason for the difference seen in mortality: “We noted that the ME group tended to have a higher yield of lymph nodes and this also correlated with survival. It is plausible that surgeons who are in the early stage of their career may be completely focused on ‘getting the specimen out’ with less attention being paid to nodal sampling with its added operative time and perceived additional morbidity.” HE surgeons may have lower yields because “the importance of nodal sampling has been predominately realized over the last 2 decades,” they pointed out.
“Patients operated on by moderately experienced surgeons may have better long-term survival after resection for pathologic stage I lung cancer. Expanding this study to a larger patient and surgeon population would be needed to validate the results and identify the underlying causes for these differences in order to provide the best patient care,” the researchers concluded.
The authors reported having no conflicts of interest.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point:Insufficient lymph-node sampling by less-experienced surgeons may be a reason why patients with stage I NSCLC had better long-term survival if operated on by moderate- and high-experience surgeons.
Major finding: Short-term outcomes in pathologic stage I NSCLC were not affected by surgeon experience, but 5-year survival was significantly lower for the low-experience compared to the moderate-experience surgeons (76.9% vs. 67.5%).
Data source: An institutional database analysis was conducted of 800 operations on stage I NSCLC patients performed from 2000 to 2012.
Disclosures: The authors reported having no conflicts of interest.
Low-volume centers using ECMO have poorest survival rates
SAN DIEGO – Lung transplantation centers that are considered low volume tend to have lower rates of survival than do those of their medium- and high-volume counterparts when patients are bridged via extracorporeal membrane oxygenation (ECMO), according to researchers.
Even so, there is a point at which survival outcomes begin to improve for low-volume centers, they added.
“Increasingly, [ECMO] is used as a bridge to lung transplantation; indeed, the use of ECMO has tripled over the past 15 years and survival has increased by the same magnitude,” Dr. Jeremiah A. Hayanga said at the annual meeting of the Society of Thoracic Surgeons.
“An entire body of literature has linked high-volume [centers] to improved outcomes in the context of complex surgical procedures. Lung transplantation [LTx] falls within the same domain, and has been considered subject to the same inverse volume-outcome paradigm,” said Dr. Hayanga of Michigan State University, Grand Rapids.
He and his coinvestigators conducted a retrospective analysis of 16,603 LTx recipients in the International Registry for Heart and Lung Transplantation (ISHLT) who underwent ECMO as their bridging strategy between 2005 and 2010. Centers were stratified into categories of low, medium, and high based on the volume of LTx procedures performed over the study interval: Low was defined as fewer than 25, medium as 25-50, and more than 50 as high volume.
Overall, 85 of the 16,603 transplant recipients in the study population were bridged via ECMO: 20 (23.5%) of them in low-volume centers, 30 (35.3%) in medium-volume centers, and 35 (41.2%) in high-volume centers. The researchers used Cox proportional hazard modeling to identify predictors of both 1- and 5-year survival rates, which were found to be significantly lower in low-volume centers – 13.61% at 5 years post LTx.
Looking at just the high-volume and low-volume centers, the researchers noted “significant differences” in both 1-year and 5-year survival rates when ECMO was used for bridging. One-year survival probability was roughly 40% in low-volume centers and roughly 70% in high-volume centers, while 5-year survival probability was well under 25% for recipients from low-volume centers and around 50% for those from high-volume centers (P = .0006). No significant differences existed for non-ECMO patients, regardless of center volume.
“No differences existed in survival in medium- and high-volume centers,” said Dr. Hayanga. “Transplanting without ECMO as a bridge showed fewer survival differences for both 1-year and 5-year survival. However, when ECMO was used as a bridge, the low-volume center [survival rates] were dramatically lower at both 1 year and 5 years.”
When Dr. Hayanga and his colleagues examined procedural volume as a continuous variable, however, a single inflection point was determined as the point at which survival outcomes steadily improve – 19 procedures. Centers that performed at least 19 LTx procedures between 2005 and 2010 experienced an uptick in survival rates, even though centers that saw 19-25 procedures were still considered low volume, the researchers noted.
“The corresponding c-statistic, however, is just under 60%,” cautioned Dr. Hayanga. “The C-statistic is a measure of the explanatory power of a variable – in this case, [center] volume – in accounting for the variability in outcome, or survival in this case. To put that number into context, a C-statistic of 50% means ‘no explanatory power’ whatsoever.”
Dr. Hayanga explained that he and his coauthors compared transplant recipient and donor characteristics using analysis of variance (ANOVA) and chi-square tests to compare variables, cumulative survival using Kaplan-Meier curves, and significance using log-rank tests.
Dr. Hayanga reported no financial conflicts of interest.
SAN DIEGO – Lung transplantation centers that are considered low volume tend to have lower rates of survival than do those of their medium- and high-volume counterparts when patients are bridged via extracorporeal membrane oxygenation (ECMO), according to researchers.
Even so, there is a point at which survival outcomes begin to improve for low-volume centers, they added.
“Increasingly, [ECMO] is used as a bridge to lung transplantation; indeed, the use of ECMO has tripled over the past 15 years and survival has increased by the same magnitude,” Dr. Jeremiah A. Hayanga said at the annual meeting of the Society of Thoracic Surgeons.
“An entire body of literature has linked high-volume [centers] to improved outcomes in the context of complex surgical procedures. Lung transplantation [LTx] falls within the same domain, and has been considered subject to the same inverse volume-outcome paradigm,” said Dr. Hayanga of Michigan State University, Grand Rapids.
He and his coinvestigators conducted a retrospective analysis of 16,603 LTx recipients in the International Registry for Heart and Lung Transplantation (ISHLT) who underwent ECMO as their bridging strategy between 2005 and 2010. Centers were stratified into categories of low, medium, and high based on the volume of LTx procedures performed over the study interval: Low was defined as fewer than 25, medium as 25-50, and more than 50 as high volume.
Overall, 85 of the 16,603 transplant recipients in the study population were bridged via ECMO: 20 (23.5%) of them in low-volume centers, 30 (35.3%) in medium-volume centers, and 35 (41.2%) in high-volume centers. The researchers used Cox proportional hazard modeling to identify predictors of both 1- and 5-year survival rates, which were found to be significantly lower in low-volume centers – 13.61% at 5 years post LTx.
Looking at just the high-volume and low-volume centers, the researchers noted “significant differences” in both 1-year and 5-year survival rates when ECMO was used for bridging. One-year survival probability was roughly 40% in low-volume centers and roughly 70% in high-volume centers, while 5-year survival probability was well under 25% for recipients from low-volume centers and around 50% for those from high-volume centers (P = .0006). No significant differences existed for non-ECMO patients, regardless of center volume.
“No differences existed in survival in medium- and high-volume centers,” said Dr. Hayanga. “Transplanting without ECMO as a bridge showed fewer survival differences for both 1-year and 5-year survival. However, when ECMO was used as a bridge, the low-volume center [survival rates] were dramatically lower at both 1 year and 5 years.”
When Dr. Hayanga and his colleagues examined procedural volume as a continuous variable, however, a single inflection point was determined as the point at which survival outcomes steadily improve – 19 procedures. Centers that performed at least 19 LTx procedures between 2005 and 2010 experienced an uptick in survival rates, even though centers that saw 19-25 procedures were still considered low volume, the researchers noted.
“The corresponding c-statistic, however, is just under 60%,” cautioned Dr. Hayanga. “The C-statistic is a measure of the explanatory power of a variable – in this case, [center] volume – in accounting for the variability in outcome, or survival in this case. To put that number into context, a C-statistic of 50% means ‘no explanatory power’ whatsoever.”
Dr. Hayanga explained that he and his coauthors compared transplant recipient and donor characteristics using analysis of variance (ANOVA) and chi-square tests to compare variables, cumulative survival using Kaplan-Meier curves, and significance using log-rank tests.
Dr. Hayanga reported no financial conflicts of interest.
SAN DIEGO – Lung transplantation centers that are considered low volume tend to have lower rates of survival than do those of their medium- and high-volume counterparts when patients are bridged via extracorporeal membrane oxygenation (ECMO), according to researchers.
Even so, there is a point at which survival outcomes begin to improve for low-volume centers, they added.
“Increasingly, [ECMO] is used as a bridge to lung transplantation; indeed, the use of ECMO has tripled over the past 15 years and survival has increased by the same magnitude,” Dr. Jeremiah A. Hayanga said at the annual meeting of the Society of Thoracic Surgeons.
“An entire body of literature has linked high-volume [centers] to improved outcomes in the context of complex surgical procedures. Lung transplantation [LTx] falls within the same domain, and has been considered subject to the same inverse volume-outcome paradigm,” said Dr. Hayanga of Michigan State University, Grand Rapids.
He and his coinvestigators conducted a retrospective analysis of 16,603 LTx recipients in the International Registry for Heart and Lung Transplantation (ISHLT) who underwent ECMO as their bridging strategy between 2005 and 2010. Centers were stratified into categories of low, medium, and high based on the volume of LTx procedures performed over the study interval: Low was defined as fewer than 25, medium as 25-50, and more than 50 as high volume.
Overall, 85 of the 16,603 transplant recipients in the study population were bridged via ECMO: 20 (23.5%) of them in low-volume centers, 30 (35.3%) in medium-volume centers, and 35 (41.2%) in high-volume centers. The researchers used Cox proportional hazard modeling to identify predictors of both 1- and 5-year survival rates, which were found to be significantly lower in low-volume centers – 13.61% at 5 years post LTx.
Looking at just the high-volume and low-volume centers, the researchers noted “significant differences” in both 1-year and 5-year survival rates when ECMO was used for bridging. One-year survival probability was roughly 40% in low-volume centers and roughly 70% in high-volume centers, while 5-year survival probability was well under 25% for recipients from low-volume centers and around 50% for those from high-volume centers (P = .0006). No significant differences existed for non-ECMO patients, regardless of center volume.
“No differences existed in survival in medium- and high-volume centers,” said Dr. Hayanga. “Transplanting without ECMO as a bridge showed fewer survival differences for both 1-year and 5-year survival. However, when ECMO was used as a bridge, the low-volume center [survival rates] were dramatically lower at both 1 year and 5 years.”
When Dr. Hayanga and his colleagues examined procedural volume as a continuous variable, however, a single inflection point was determined as the point at which survival outcomes steadily improve – 19 procedures. Centers that performed at least 19 LTx procedures between 2005 and 2010 experienced an uptick in survival rates, even though centers that saw 19-25 procedures were still considered low volume, the researchers noted.
“The corresponding c-statistic, however, is just under 60%,” cautioned Dr. Hayanga. “The C-statistic is a measure of the explanatory power of a variable – in this case, [center] volume – in accounting for the variability in outcome, or survival in this case. To put that number into context, a C-statistic of 50% means ‘no explanatory power’ whatsoever.”
Dr. Hayanga explained that he and his coauthors compared transplant recipient and donor characteristics using analysis of variance (ANOVA) and chi-square tests to compare variables, cumulative survival using Kaplan-Meier curves, and significance using log-rank tests.
Dr. Hayanga reported no financial conflicts of interest.
AT THE STS ANNUAL MEETING
Key clinical point: Low-volume lung transplantation centers in the United States typically have the poorest survival rates compared to those with higher volumes when using ECMO.
Major finding: Of 85 LTx subjects bridged via ECMO, 20 (23.5%) of these were bridged in low, 30 (35.3%) in medium, and 35 (41.2%) in high-volume centers; in the ECMO cohort, the lowest 5-year survival rate (13.61%) was observed at low-volume centers.
Data source: Retrospective analysis of 16,603 adult LTx recipients in the International Registry for Heart and Lung Transplantation during 2005-2010.
Disclosures: Dr. Hayanga reported no financial conflicts of interest.
Halting biologics before surgery tied to flares in psoriasis, psoriatic arthritis
Interrupting biologic therapy before surgery led to flares in psoriasis and psoriatic arthritis and did not appear to prevent postoperative complications in a small, retrospective cohort study.
“Our findings are in keeping with most of the existing literature on this topic,” said Dr. Waseem Bakkour and his associates at the University of Manchester (England). “However, it is important to acknowledge the deficiencies of our data, in particular the small data set and retrospective study design with numerous complexities associated with interpreting it” (J. Eur. Acad. Dermatol. Venereol. 2015 Mar. 2 [doi:10.1111/jdv.12997]).
The British Association of Dermatologists and the British Society for Rheumatology recommend stopping biologics for at least four half-lives before surgery, but the guideline is based mostly on retrospective studies of rheumatoid arthritis and inflammatory bowel disease, the researchers said. For their study, they reviewed electronic health records from 42 patients with psoriasis and psoriatic arthritis who underwent 77 major and minor surgical procedures during a 6-year period. Discontinuing biologic therapy before surgery was linked to a significant risk of flare of psoriasis or psoriatic arthritis (40% with stoppage vs. 8.7% with continuation; P = .003). For three-quarters of procedures, patients continued biologic therapy (usually etanercept, but also adalimumab and infliximab), with no apparent effect on rates of postoperative infections or delayed wound healing. About 48% of procedures required general anesthesia, and most of the rest were skin surgeries.
The findings contradict those from a larger retrospective study (Arthritis Care Res. 2006;55:333-7) that linked biologic therapy before orthopedic surgery to a fourfold rise in the odds of postoperative infections, the investigators noted. “Whilst the current evidence, not surprisingly, suggests a link between stopping treatment and disease flare, it remains equivocal regarding the question of whether continuing biologic therapy perioperatively increases the risk of postsurgical complications,” they wrote.
The authors reported no funding sources. They disclosed financial and advisory relationships with many companies that manufacture biologic therapies.
Interrupting biologic therapy before surgery led to flares in psoriasis and psoriatic arthritis and did not appear to prevent postoperative complications in a small, retrospective cohort study.
“Our findings are in keeping with most of the existing literature on this topic,” said Dr. Waseem Bakkour and his associates at the University of Manchester (England). “However, it is important to acknowledge the deficiencies of our data, in particular the small data set and retrospective study design with numerous complexities associated with interpreting it” (J. Eur. Acad. Dermatol. Venereol. 2015 Mar. 2 [doi:10.1111/jdv.12997]).
The British Association of Dermatologists and the British Society for Rheumatology recommend stopping biologics for at least four half-lives before surgery, but the guideline is based mostly on retrospective studies of rheumatoid arthritis and inflammatory bowel disease, the researchers said. For their study, they reviewed electronic health records from 42 patients with psoriasis and psoriatic arthritis who underwent 77 major and minor surgical procedures during a 6-year period. Discontinuing biologic therapy before surgery was linked to a significant risk of flare of psoriasis or psoriatic arthritis (40% with stoppage vs. 8.7% with continuation; P = .003). For three-quarters of procedures, patients continued biologic therapy (usually etanercept, but also adalimumab and infliximab), with no apparent effect on rates of postoperative infections or delayed wound healing. About 48% of procedures required general anesthesia, and most of the rest were skin surgeries.
The findings contradict those from a larger retrospective study (Arthritis Care Res. 2006;55:333-7) that linked biologic therapy before orthopedic surgery to a fourfold rise in the odds of postoperative infections, the investigators noted. “Whilst the current evidence, not surprisingly, suggests a link between stopping treatment and disease flare, it remains equivocal regarding the question of whether continuing biologic therapy perioperatively increases the risk of postsurgical complications,” they wrote.
The authors reported no funding sources. They disclosed financial and advisory relationships with many companies that manufacture biologic therapies.
Interrupting biologic therapy before surgery led to flares in psoriasis and psoriatic arthritis and did not appear to prevent postoperative complications in a small, retrospective cohort study.
“Our findings are in keeping with most of the existing literature on this topic,” said Dr. Waseem Bakkour and his associates at the University of Manchester (England). “However, it is important to acknowledge the deficiencies of our data, in particular the small data set and retrospective study design with numerous complexities associated with interpreting it” (J. Eur. Acad. Dermatol. Venereol. 2015 Mar. 2 [doi:10.1111/jdv.12997]).
The British Association of Dermatologists and the British Society for Rheumatology recommend stopping biologics for at least four half-lives before surgery, but the guideline is based mostly on retrospective studies of rheumatoid arthritis and inflammatory bowel disease, the researchers said. For their study, they reviewed electronic health records from 42 patients with psoriasis and psoriatic arthritis who underwent 77 major and minor surgical procedures during a 6-year period. Discontinuing biologic therapy before surgery was linked to a significant risk of flare of psoriasis or psoriatic arthritis (40% with stoppage vs. 8.7% with continuation; P = .003). For three-quarters of procedures, patients continued biologic therapy (usually etanercept, but also adalimumab and infliximab), with no apparent effect on rates of postoperative infections or delayed wound healing. About 48% of procedures required general anesthesia, and most of the rest were skin surgeries.
The findings contradict those from a larger retrospective study (Arthritis Care Res. 2006;55:333-7) that linked biologic therapy before orthopedic surgery to a fourfold rise in the odds of postoperative infections, the investigators noted. “Whilst the current evidence, not surprisingly, suggests a link between stopping treatment and disease flare, it remains equivocal regarding the question of whether continuing biologic therapy perioperatively increases the risk of postsurgical complications,” they wrote.
The authors reported no funding sources. They disclosed financial and advisory relationships with many companies that manufacture biologic therapies.
FROM THE JOURNAL OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Key clinical point: Interrupting biologic therapy before surgery led to flares in psoriasis and psoriatic arthritis.
Major finding: Discontinuing biologic therapy before surgery was associated with a significant risk of flare (40% with stoppage vs. 8.7% with continuation; P = .003).
Data source: A retrospective cohort study of 42 patients with psoriasis and/or psoriatic arthritis who underwent 77 surgical procedures.
Disclosures: The authors reported no funding sources. They disclosed financial and advisory relationships with many companies that manufacture biologic therapies.
Acute renal failure biggest short-term risk in I-EVAR explantation
SCOTTSDALE, ARIZ. – Acute renal failure occurred postoperatively in one-third of patients who underwent endograft explantation after endovascular abdominal aortic aneurysm repair (EVAR), according to the results of a small retrospective study.
The perioperative infected EVAR (I-EVAR) mortality across the study’s 36 patient records (83% male patients, average age 69 years), culled from four surgery centers’ data from 1997 to 2014, was 8%. The overall mortality was 25%, according to Dr. Victor J. Davila of Mayo Clinic Arizona, Phoenix, and his colleagues. Dr. Davila presented the findings at the Southern Association for Vascular Surgery annual meeting.
“These data show that I-EVAR explantation can be performed safely, with acceptable morbidity and mortality,” said Dr. Davila, who noted that while acceptable, the rates were still high, particularly for acute renal failure.
“We did not find any difference between the patients who developed renal failure and the type of graft, whether or not there was suprarenal fixation, and an incidence of postoperative acute renal failure,” Dr. Davila said, “However, because acute renal failure is multifactorial, we need to minimize aortic clamp time, as well as minimize the aortic intimal disruption around the renal arteries.”
Three deaths occurred within 30 days post operation, all from anastomotic dehiscence. Additional short-term morbidities included respiratory failure that required tracheostomy in three patients, and bleeding and sepsis in two patients each. Six patients required re-exploration because of infected hematoma, lymphatic leak, small-bowel perforation, open abdomen at initial operation, and anastomotic bleeding. Six more deaths occurred at a mean follow-up of 402 days. One death was attributable to a ruptured aneurysm, another to a progressive inflammatory illness, and four deaths were of indeterminate cause.
Only three of the explantations reviewed by Dr. Davila and his colleagues were considered emergent. The rest (92%) were either elective or urgent. Infected patients tended to present with leukocytosis (63%), pain (58%), and fever (56%), usually about 65 days prior to explantation. The average time between EVAR and presentation with infection was 589 days.
Although most underwent total graft excision, two patients underwent partial excision, including one with a distal iliac limb infection that showed no sign of infection within the main portion of the endograft. Nearly three-quarters of patients had in situ reconstruction.
While nearly a third of patients had positive preoperative blood cultures indicating infection, 81% of intraoperative cultures taken from the explanted graft, aneurysm wall, or sac contents indicated infection.
The gram-positive Staphylococcus and Streptococcus were the most common organisms found in cultures (33% and 17%, respectively), although anaerobics were found in a third of patients, gram negatives in a quarter of patients, and fungal infections in 14%. A majority (58%) of patients received long-term suppressive antibiotic therapy.
Surgeons should reserve the option to keep a graft in situ only in infected EVAR patients who likely would not survive surgical explantation and reconstruction, Dr. Davila said. “Although I believe [medical management] is an alternative, the best course of action is to remove the endograft.”
On Twitter @whitneymcknight
SCOTTSDALE, ARIZ. – Acute renal failure occurred postoperatively in one-third of patients who underwent endograft explantation after endovascular abdominal aortic aneurysm repair (EVAR), according to the results of a small retrospective study.
The perioperative infected EVAR (I-EVAR) mortality across the study’s 36 patient records (83% male patients, average age 69 years), culled from four surgery centers’ data from 1997 to 2014, was 8%. The overall mortality was 25%, according to Dr. Victor J. Davila of Mayo Clinic Arizona, Phoenix, and his colleagues. Dr. Davila presented the findings at the Southern Association for Vascular Surgery annual meeting.
“These data show that I-EVAR explantation can be performed safely, with acceptable morbidity and mortality,” said Dr. Davila, who noted that while acceptable, the rates were still high, particularly for acute renal failure.
“We did not find any difference between the patients who developed renal failure and the type of graft, whether or not there was suprarenal fixation, and an incidence of postoperative acute renal failure,” Dr. Davila said, “However, because acute renal failure is multifactorial, we need to minimize aortic clamp time, as well as minimize the aortic intimal disruption around the renal arteries.”
Three deaths occurred within 30 days post operation, all from anastomotic dehiscence. Additional short-term morbidities included respiratory failure that required tracheostomy in three patients, and bleeding and sepsis in two patients each. Six patients required re-exploration because of infected hematoma, lymphatic leak, small-bowel perforation, open abdomen at initial operation, and anastomotic bleeding. Six more deaths occurred at a mean follow-up of 402 days. One death was attributable to a ruptured aneurysm, another to a progressive inflammatory illness, and four deaths were of indeterminate cause.
Only three of the explantations reviewed by Dr. Davila and his colleagues were considered emergent. The rest (92%) were either elective or urgent. Infected patients tended to present with leukocytosis (63%), pain (58%), and fever (56%), usually about 65 days prior to explantation. The average time between EVAR and presentation with infection was 589 days.
Although most underwent total graft excision, two patients underwent partial excision, including one with a distal iliac limb infection that showed no sign of infection within the main portion of the endograft. Nearly three-quarters of patients had in situ reconstruction.
While nearly a third of patients had positive preoperative blood cultures indicating infection, 81% of intraoperative cultures taken from the explanted graft, aneurysm wall, or sac contents indicated infection.
The gram-positive Staphylococcus and Streptococcus were the most common organisms found in cultures (33% and 17%, respectively), although anaerobics were found in a third of patients, gram negatives in a quarter of patients, and fungal infections in 14%. A majority (58%) of patients received long-term suppressive antibiotic therapy.
Surgeons should reserve the option to keep a graft in situ only in infected EVAR patients who likely would not survive surgical explantation and reconstruction, Dr. Davila said. “Although I believe [medical management] is an alternative, the best course of action is to remove the endograft.”
On Twitter @whitneymcknight
SCOTTSDALE, ARIZ. – Acute renal failure occurred postoperatively in one-third of patients who underwent endograft explantation after endovascular abdominal aortic aneurysm repair (EVAR), according to the results of a small retrospective study.
The perioperative infected EVAR (I-EVAR) mortality across the study’s 36 patient records (83% male patients, average age 69 years), culled from four surgery centers’ data from 1997 to 2014, was 8%. The overall mortality was 25%, according to Dr. Victor J. Davila of Mayo Clinic Arizona, Phoenix, and his colleagues. Dr. Davila presented the findings at the Southern Association for Vascular Surgery annual meeting.
“These data show that I-EVAR explantation can be performed safely, with acceptable morbidity and mortality,” said Dr. Davila, who noted that while acceptable, the rates were still high, particularly for acute renal failure.
“We did not find any difference between the patients who developed renal failure and the type of graft, whether or not there was suprarenal fixation, and an incidence of postoperative acute renal failure,” Dr. Davila said, “However, because acute renal failure is multifactorial, we need to minimize aortic clamp time, as well as minimize the aortic intimal disruption around the renal arteries.”
Three deaths occurred within 30 days post operation, all from anastomotic dehiscence. Additional short-term morbidities included respiratory failure that required tracheostomy in three patients, and bleeding and sepsis in two patients each. Six patients required re-exploration because of infected hematoma, lymphatic leak, small-bowel perforation, open abdomen at initial operation, and anastomotic bleeding. Six more deaths occurred at a mean follow-up of 402 days. One death was attributable to a ruptured aneurysm, another to a progressive inflammatory illness, and four deaths were of indeterminate cause.
Only three of the explantations reviewed by Dr. Davila and his colleagues were considered emergent. The rest (92%) were either elective or urgent. Infected patients tended to present with leukocytosis (63%), pain (58%), and fever (56%), usually about 65 days prior to explantation. The average time between EVAR and presentation with infection was 589 days.
Although most underwent total graft excision, two patients underwent partial excision, including one with a distal iliac limb infection that showed no sign of infection within the main portion of the endograft. Nearly three-quarters of patients had in situ reconstruction.
While nearly a third of patients had positive preoperative blood cultures indicating infection, 81% of intraoperative cultures taken from the explanted graft, aneurysm wall, or sac contents indicated infection.
The gram-positive Staphylococcus and Streptococcus were the most common organisms found in cultures (33% and 17%, respectively), although anaerobics were found in a third of patients, gram negatives in a quarter of patients, and fungal infections in 14%. A majority (58%) of patients received long-term suppressive antibiotic therapy.
Surgeons should reserve the option to keep a graft in situ only in infected EVAR patients who likely would not survive surgical explantation and reconstruction, Dr. Davila said. “Although I believe [medical management] is an alternative, the best course of action is to remove the endograft.”
On Twitter @whitneymcknight
AT THE SAVS ANNUAL MEETING
Key clinical point: Minimizing cross-clamp time may reduce the rate of acute renal failure 30 days post op in infected EVAR explantation patients.
Major finding: One-third of I-EVAR patients had postoperative acute renal failure; perioperative mortality in I-EVAR was 8%, and overall mortality was 25%.
Data source: Retrospective analysis of 36 patients with infected EVAR explants performed between 1997 and 2014 across four surgical centers.
Disclosures: Dr. Davila reported he had no relevant disclosures.
mSTEADI: Better discharge-to-home rates in elderly fall patients
LAKE BUENA VISTA, FLA. – Modifying the Centers for Disease Control and Prevention’s outpatient fall prevention program STEADI for inpatient use did not prevent further falls in elderly patients hospitalized for fall injuries.
The intervention was associated, however, with a “clear reduction in median length of stay and hospital charges,” Dr. Alexander Eastman, M.P.H., said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
STEADI(Stopping Elderly Accidents, Deaths and Injuries) is a CDC–funded program. It has six core domains – fall history, medical conditions, medications, gait/balance, vision limitation, and postural hypotension – and includes standardized gait and balance assessments and a fall-prevention checklist.
Dr. Eastman and other members of a multidisciplinary team at the University of Texas Southwestern Medical Center in Dallas used the same checklist principle to create a modified version of the STEADI program (mSTEADI) for inpatient use. Their patient assessment was associated with delivery of therapeutic interventions, and the gait and posture testing and therapies were adapted for use with injured patients.
Data were then prospectively collected for 1 year from 218 patients, aged older than 65 years, who were admitted for falls at the level 1 trauma center and enrolled in the mSTEADI program. Their results were compared with data from 196 historical controls from the same period the year before mSTEADI was introduced. The two groups were well matched with respect to median age (77 years vs. 76 years); mean Injury Severity Score (12.1 vs. 11.8); and Abbreviated Injury Scale (AIS) head, face, chest, or abdomen scores. mSTEADI patients had a slightly higher mean AIS extremity score (2.7 vs. 2.5; P value = .014).
After a year, however, the mSTEADI group and the historical controls had the same in-house fall rate, 4.1%. The fall recidivism rate was 2.1% for the mSTEADI group and 2.8% for the controls, an insignificant difference, Dr. Eastman said.
The mSTEADI group, however, was discharged a day earlier (5 days vs. 6 days; P <.01), was more likely to be discharged directly home (54.5% vs. 46.8%; P <.01), and had lower overall hospital charges ($45,538 vs. $60,585; P = .02).
Limitations of the study were the use of retrospective controls and the very real possibility of selection bias in a group receiving intensive assessment and therapy, Dr. Eastman said. Discussant Dr. Stephanie Bonne of Washington University, St. Louis, asked whether the researchers were confident they captured all subsequent falls when calculating recidivism in such a large urban setting and whether the findings of shorter hospital stay and more discharges home would prompt them to recommend mSTEADI for enhancing rehabilitation protocols rather than for preventing repeated falls.
Dr. Eastman said that the combination of medical and emergency medical services records probably captured geriatric patients returning to the hospital with an injury from a fall since Southwestern is the EMS medical director for Dallas and 15 surrounding municipalities.
“As far as the decreased length of stay, I think there’s no question that increased focus on your rehabilitation efforts results in this unintended benefit of getting more patients home,” he added. “That’s a very real, tangible benefit to this program, but I’m not sure you have to incorporate all the other stuff that the mSTEADI program brings rather than breaking out just those specific portions of the program that are rehab focused and then really going out and studying in-hospital falls and fall recidivists to see what other phases are potential targets for intervention.”
Because the translation of the STEADI program to mSTEADI may have missed “some intangible associated with in-house falls,” an additional study of inpatient falls (iSTEADI) is being planned, as are home visits by Dallas paramedics to assess fall risk for every fall patient discharged from their institution, Dr. Eastman said.
LAKE BUENA VISTA, FLA. – Modifying the Centers for Disease Control and Prevention’s outpatient fall prevention program STEADI for inpatient use did not prevent further falls in elderly patients hospitalized for fall injuries.
The intervention was associated, however, with a “clear reduction in median length of stay and hospital charges,” Dr. Alexander Eastman, M.P.H., said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
STEADI(Stopping Elderly Accidents, Deaths and Injuries) is a CDC–funded program. It has six core domains – fall history, medical conditions, medications, gait/balance, vision limitation, and postural hypotension – and includes standardized gait and balance assessments and a fall-prevention checklist.
Dr. Eastman and other members of a multidisciplinary team at the University of Texas Southwestern Medical Center in Dallas used the same checklist principle to create a modified version of the STEADI program (mSTEADI) for inpatient use. Their patient assessment was associated with delivery of therapeutic interventions, and the gait and posture testing and therapies were adapted for use with injured patients.
Data were then prospectively collected for 1 year from 218 patients, aged older than 65 years, who were admitted for falls at the level 1 trauma center and enrolled in the mSTEADI program. Their results were compared with data from 196 historical controls from the same period the year before mSTEADI was introduced. The two groups were well matched with respect to median age (77 years vs. 76 years); mean Injury Severity Score (12.1 vs. 11.8); and Abbreviated Injury Scale (AIS) head, face, chest, or abdomen scores. mSTEADI patients had a slightly higher mean AIS extremity score (2.7 vs. 2.5; P value = .014).
After a year, however, the mSTEADI group and the historical controls had the same in-house fall rate, 4.1%. The fall recidivism rate was 2.1% for the mSTEADI group and 2.8% for the controls, an insignificant difference, Dr. Eastman said.
The mSTEADI group, however, was discharged a day earlier (5 days vs. 6 days; P <.01), was more likely to be discharged directly home (54.5% vs. 46.8%; P <.01), and had lower overall hospital charges ($45,538 vs. $60,585; P = .02).
Limitations of the study were the use of retrospective controls and the very real possibility of selection bias in a group receiving intensive assessment and therapy, Dr. Eastman said. Discussant Dr. Stephanie Bonne of Washington University, St. Louis, asked whether the researchers were confident they captured all subsequent falls when calculating recidivism in such a large urban setting and whether the findings of shorter hospital stay and more discharges home would prompt them to recommend mSTEADI for enhancing rehabilitation protocols rather than for preventing repeated falls.
Dr. Eastman said that the combination of medical and emergency medical services records probably captured geriatric patients returning to the hospital with an injury from a fall since Southwestern is the EMS medical director for Dallas and 15 surrounding municipalities.
“As far as the decreased length of stay, I think there’s no question that increased focus on your rehabilitation efforts results in this unintended benefit of getting more patients home,” he added. “That’s a very real, tangible benefit to this program, but I’m not sure you have to incorporate all the other stuff that the mSTEADI program brings rather than breaking out just those specific portions of the program that are rehab focused and then really going out and studying in-hospital falls and fall recidivists to see what other phases are potential targets for intervention.”
Because the translation of the STEADI program to mSTEADI may have missed “some intangible associated with in-house falls,” an additional study of inpatient falls (iSTEADI) is being planned, as are home visits by Dallas paramedics to assess fall risk for every fall patient discharged from their institution, Dr. Eastman said.
LAKE BUENA VISTA, FLA. – Modifying the Centers for Disease Control and Prevention’s outpatient fall prevention program STEADI for inpatient use did not prevent further falls in elderly patients hospitalized for fall injuries.
The intervention was associated, however, with a “clear reduction in median length of stay and hospital charges,” Dr. Alexander Eastman, M.P.H., said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
STEADI(Stopping Elderly Accidents, Deaths and Injuries) is a CDC–funded program. It has six core domains – fall history, medical conditions, medications, gait/balance, vision limitation, and postural hypotension – and includes standardized gait and balance assessments and a fall-prevention checklist.
Dr. Eastman and other members of a multidisciplinary team at the University of Texas Southwestern Medical Center in Dallas used the same checklist principle to create a modified version of the STEADI program (mSTEADI) for inpatient use. Their patient assessment was associated with delivery of therapeutic interventions, and the gait and posture testing and therapies were adapted for use with injured patients.
Data were then prospectively collected for 1 year from 218 patients, aged older than 65 years, who were admitted for falls at the level 1 trauma center and enrolled in the mSTEADI program. Their results were compared with data from 196 historical controls from the same period the year before mSTEADI was introduced. The two groups were well matched with respect to median age (77 years vs. 76 years); mean Injury Severity Score (12.1 vs. 11.8); and Abbreviated Injury Scale (AIS) head, face, chest, or abdomen scores. mSTEADI patients had a slightly higher mean AIS extremity score (2.7 vs. 2.5; P value = .014).
After a year, however, the mSTEADI group and the historical controls had the same in-house fall rate, 4.1%. The fall recidivism rate was 2.1% for the mSTEADI group and 2.8% for the controls, an insignificant difference, Dr. Eastman said.
The mSTEADI group, however, was discharged a day earlier (5 days vs. 6 days; P <.01), was more likely to be discharged directly home (54.5% vs. 46.8%; P <.01), and had lower overall hospital charges ($45,538 vs. $60,585; P = .02).
Limitations of the study were the use of retrospective controls and the very real possibility of selection bias in a group receiving intensive assessment and therapy, Dr. Eastman said. Discussant Dr. Stephanie Bonne of Washington University, St. Louis, asked whether the researchers were confident they captured all subsequent falls when calculating recidivism in such a large urban setting and whether the findings of shorter hospital stay and more discharges home would prompt them to recommend mSTEADI for enhancing rehabilitation protocols rather than for preventing repeated falls.
Dr. Eastman said that the combination of medical and emergency medical services records probably captured geriatric patients returning to the hospital with an injury from a fall since Southwestern is the EMS medical director for Dallas and 15 surrounding municipalities.
“As far as the decreased length of stay, I think there’s no question that increased focus on your rehabilitation efforts results in this unintended benefit of getting more patients home,” he added. “That’s a very real, tangible benefit to this program, but I’m not sure you have to incorporate all the other stuff that the mSTEADI program brings rather than breaking out just those specific portions of the program that are rehab focused and then really going out and studying in-hospital falls and fall recidivists to see what other phases are potential targets for intervention.”
Because the translation of the STEADI program to mSTEADI may have missed “some intangible associated with in-house falls,” an additional study of inpatient falls (iSTEADI) is being planned, as are home visits by Dallas paramedics to assess fall risk for every fall patient discharged from their institution, Dr. Eastman said.
AT THE EAST SCIENTIFIC ASSEMBLY
Key clinical point: A fall-prevention program did not prevent in-hospital falls or fall recidivism, but it was associated with lower inpatient costs, earlier discharge, and a higher likelihood of discharge to home.
Major finding: Compared with historical controls, the mSTEADI group was discharged a day earlier (5 days vs. 6 days; P <.01), was more likely to be discharged directly home (54.5% vs. 46.8%; P <.01), and had lower overall hospital charges ($45,538 vs. $60,585; P = .02).
Data source: Prospective analysis of 218 elderly fall patients and 196 historical controls.
Disclosures: Dr. Eastman and Dr. Bonne reported having no financial disclosures.
Device closure of PFO doesn’t drop combined major adverse event risk
NASHVILLE, TENN. – Device closure of a patent foramen ovale didn’t reduce the composite risk of death, stroke, or transient ischemic attack when compared against medical therapy alone in a pooled analysis of three trials.
Device intervention, did, however, reduce the individual risk of recurrent stroke, although the absolute reduction seemed modest, Dr. David M. Kent said at the International Stroke Conference, sponsored by the American Heart Association.
Overall device closure conferred about a 30% annual risk reduction of recurrent stroke upon those with patent foramen ovale (PFO) who had experienced a prior cryptogenic stroke. About 30 patients would have to be treated to prevent one stroke over 5 years, said Dr. Kent of Tufts University, Boston.
“It’s not a huge benefit – it’s not like thrombectomy. But it’s comparable to the benefit of high-dose statins seen in the SPARCL [Stroke Prevention by Aggressive Reduction in Cholesterol Levels] trial.”
Dr. Kent and his colleagues’ analysis used three trials: the CLOSURE trial, which used the STARflex device, and two trials that tested the Amplatzer device, the PC TRIAL and RESPECT.
Altogether, the pooled analysis comprised about 2,300 patients. Of these, 440 were lost to 5-year follow-up; their outcomes were imputed into an intent-to-treat analysis based on last-known clinical status.
Dr. Kent and his colleagues also conducted a subanalysis of only the two Amplatzer device trials, which comprised 1,400 patients.
The primary outcome for each analysis was a composite of recurrent stroke, transient ischemic attack (TIA), and early death. The secondary outcome was recurrent stroke alone.
The patients were a mean of 45 years old. About a third had dyslipidemia, and a third had hypertension. The PFO was considered large in 60%.
During the 5-year follow-up period, there were 58 strokes and 54 TIAs. Four patients died during the trial – two in the device arms and two in the medical therapy arms.
When all three trials were analyzed together, PFO closure was not significantly better than medical therapy in the composite endpoint (1.5% vs. 2.3%). The difference in recurrent stroke rate alone was significant (0.7% vs. 1.3%), although Dr. Kent did note that the event rate was very low in both groups.
In the two Amplatzer trials, the device also did not significantly reduce the risk of the composite endpoint. It did confer significant benefit on the stroke-only outcome (hazard ratio, 0.41; 0.4% vs. 1.1%). Again, Dr. Kent said, the event rate was very low for both intervention groups.
There was no significantly increased risk of bleeding with PFO closure in the analysis of all three trials or in the two Amplatzer device trials alone, although both did find a significantly increased risk of atrial fibrillation. In the three-trial analysis, rates of atrial fibrillation were 1.5% vs. 0.48%; in the Amplatzer-only analysis, rates were 0.87% vs. 0.47%. The investigators weren’t able to identify any factors that might predispose to a safety event.
The analyses were sponsored by the National Institutes of Health. Dr. Kent had no financial disclosures, although several coauthors had ties with multiple pharmaceutical companies, or were investigators on the original trials, which were sponsored by the device manufacturers.
On Twitter @alz_gal
NASHVILLE, TENN. – Device closure of a patent foramen ovale didn’t reduce the composite risk of death, stroke, or transient ischemic attack when compared against medical therapy alone in a pooled analysis of three trials.
Device intervention, did, however, reduce the individual risk of recurrent stroke, although the absolute reduction seemed modest, Dr. David M. Kent said at the International Stroke Conference, sponsored by the American Heart Association.
Overall device closure conferred about a 30% annual risk reduction of recurrent stroke upon those with patent foramen ovale (PFO) who had experienced a prior cryptogenic stroke. About 30 patients would have to be treated to prevent one stroke over 5 years, said Dr. Kent of Tufts University, Boston.
“It’s not a huge benefit – it’s not like thrombectomy. But it’s comparable to the benefit of high-dose statins seen in the SPARCL [Stroke Prevention by Aggressive Reduction in Cholesterol Levels] trial.”
Dr. Kent and his colleagues’ analysis used three trials: the CLOSURE trial, which used the STARflex device, and two trials that tested the Amplatzer device, the PC TRIAL and RESPECT.
Altogether, the pooled analysis comprised about 2,300 patients. Of these, 440 were lost to 5-year follow-up; their outcomes were imputed into an intent-to-treat analysis based on last-known clinical status.
Dr. Kent and his colleagues also conducted a subanalysis of only the two Amplatzer device trials, which comprised 1,400 patients.
The primary outcome for each analysis was a composite of recurrent stroke, transient ischemic attack (TIA), and early death. The secondary outcome was recurrent stroke alone.
The patients were a mean of 45 years old. About a third had dyslipidemia, and a third had hypertension. The PFO was considered large in 60%.
During the 5-year follow-up period, there were 58 strokes and 54 TIAs. Four patients died during the trial – two in the device arms and two in the medical therapy arms.
When all three trials were analyzed together, PFO closure was not significantly better than medical therapy in the composite endpoint (1.5% vs. 2.3%). The difference in recurrent stroke rate alone was significant (0.7% vs. 1.3%), although Dr. Kent did note that the event rate was very low in both groups.
In the two Amplatzer trials, the device also did not significantly reduce the risk of the composite endpoint. It did confer significant benefit on the stroke-only outcome (hazard ratio, 0.41; 0.4% vs. 1.1%). Again, Dr. Kent said, the event rate was very low for both intervention groups.
There was no significantly increased risk of bleeding with PFO closure in the analysis of all three trials or in the two Amplatzer device trials alone, although both did find a significantly increased risk of atrial fibrillation. In the three-trial analysis, rates of atrial fibrillation were 1.5% vs. 0.48%; in the Amplatzer-only analysis, rates were 0.87% vs. 0.47%. The investigators weren’t able to identify any factors that might predispose to a safety event.
The analyses were sponsored by the National Institutes of Health. Dr. Kent had no financial disclosures, although several coauthors had ties with multiple pharmaceutical companies, or were investigators on the original trials, which were sponsored by the device manufacturers.
On Twitter @alz_gal
NASHVILLE, TENN. – Device closure of a patent foramen ovale didn’t reduce the composite risk of death, stroke, or transient ischemic attack when compared against medical therapy alone in a pooled analysis of three trials.
Device intervention, did, however, reduce the individual risk of recurrent stroke, although the absolute reduction seemed modest, Dr. David M. Kent said at the International Stroke Conference, sponsored by the American Heart Association.
Overall device closure conferred about a 30% annual risk reduction of recurrent stroke upon those with patent foramen ovale (PFO) who had experienced a prior cryptogenic stroke. About 30 patients would have to be treated to prevent one stroke over 5 years, said Dr. Kent of Tufts University, Boston.
“It’s not a huge benefit – it’s not like thrombectomy. But it’s comparable to the benefit of high-dose statins seen in the SPARCL [Stroke Prevention by Aggressive Reduction in Cholesterol Levels] trial.”
Dr. Kent and his colleagues’ analysis used three trials: the CLOSURE trial, which used the STARflex device, and two trials that tested the Amplatzer device, the PC TRIAL and RESPECT.
Altogether, the pooled analysis comprised about 2,300 patients. Of these, 440 were lost to 5-year follow-up; their outcomes were imputed into an intent-to-treat analysis based on last-known clinical status.
Dr. Kent and his colleagues also conducted a subanalysis of only the two Amplatzer device trials, which comprised 1,400 patients.
The primary outcome for each analysis was a composite of recurrent stroke, transient ischemic attack (TIA), and early death. The secondary outcome was recurrent stroke alone.
The patients were a mean of 45 years old. About a third had dyslipidemia, and a third had hypertension. The PFO was considered large in 60%.
During the 5-year follow-up period, there were 58 strokes and 54 TIAs. Four patients died during the trial – two in the device arms and two in the medical therapy arms.
When all three trials were analyzed together, PFO closure was not significantly better than medical therapy in the composite endpoint (1.5% vs. 2.3%). The difference in recurrent stroke rate alone was significant (0.7% vs. 1.3%), although Dr. Kent did note that the event rate was very low in both groups.
In the two Amplatzer trials, the device also did not significantly reduce the risk of the composite endpoint. It did confer significant benefit on the stroke-only outcome (hazard ratio, 0.41; 0.4% vs. 1.1%). Again, Dr. Kent said, the event rate was very low for both intervention groups.
There was no significantly increased risk of bleeding with PFO closure in the analysis of all three trials or in the two Amplatzer device trials alone, although both did find a significantly increased risk of atrial fibrillation. In the three-trial analysis, rates of atrial fibrillation were 1.5% vs. 0.48%; in the Amplatzer-only analysis, rates were 0.87% vs. 0.47%. The investigators weren’t able to identify any factors that might predispose to a safety event.
The analyses were sponsored by the National Institutes of Health. Dr. Kent had no financial disclosures, although several coauthors had ties with multiple pharmaceutical companies, or were investigators on the original trials, which were sponsored by the device manufacturers.
On Twitter @alz_gal
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point: Device closure of a patent foramen ovale seems to reduce the risk of recurrent stroke – but not a composite of death, stroke, or TIA – better than medical therapy.
Major finding: Device closure of PFO conferred about a 30% decline in the risk of recurrent stroke over a 5-year follow-up.
Data source: The analysis pooled results for 2,300 patients who participated in three trials.
Disclosures: The analyses were sponsored by the National Institutes of Health. Dr. Kent had no financial disclosures, although several coauthors had ties with multiple pharmaceutical companies, or were investigators on the original trials, which were sponsored by the device manufacturers.
House negotiating SGR fix, repeal could come soon
Negotiations are apparently underway in the House of Representatives over the Medicare Sustainable Growth Rate (SGR) formula, and agreement on a possible repeal could be on the horizon.
The new efforts will hopefully lead to an improved, permanent payment system that ensures Medicare is on a sustainable path going forward, said Sen. Ron Wyden (D-Ore.), ranking member of the Senate Finance Committee.
“I’ve been in Congress long enough to be skeptical of rumors, but what we are hearing from the House suggests there is real movement to fully repeal and replace the flawed formula for paying Medicare providers known as SGR,” Sen. Wyden said in a statement. “If what we’re hearing is true, it’s good news and moves us closer to something I’ve been working tirelessly to achieve – a payment formula that stands on its own, doesn’t require annual and expensive ‘patches,’ and which opens the door to improving the way care is delivered.”
The current SGR patch expires March 31, after which physicians can expect a 21% pay cut.
A new analysis of last year’s repeal legislation notes the bill has strengths and weaknesses for physicians (Health Aff. 2015 doi: 10.1377/hlthaff.2014.1429). Current congressional deliberations are focused on how to pay for the SGR fix, with wide consensus that the 2014 legislation will remain the basic model for reform.
The SGR Repeal and Medicare Provider Payment Modernization Act of 2014 includes opportunities for specialists to participate in pay-for-performance programs and other alternative payment models, according to author James Reschovsky, a senior fellow at policy research firm Mathematica Policy Research. The legislation would create two new payment pathways for doctors, one for those who want to continue to receive fee-for-service payments, and another for those already participating in value-based payment models, including accountable care arrangements and bundled payment initiatives.
But the bill fails to address distortions in Medicare’s fee-for-service fee schedule, which some argue overvalues specialty care services, while undervaluing preventive care, Mr. Reschovsky and his colleagues said. Without fixing that defect, specialists may find it more lucrative to stay in Medicare’s fee-for-service program and continue to concentrate on providing high-cost services. Attempts to bring down costs through ACOs and other alternative payment methods also will be difficult as long as the fee-for-service pay rates underlying these programs are skewed.
“Correcting fee schedule valuations will be a substantial and controversial undertaking,” they wrote. “But it is one that is vitally important to the SGR fix’s prospects for success.”
The SGR Repeal and Medicare Provider Payment Modernization Act of 2014 passed the House last year, but was not taken up by the Senate
On Twitter @legal_med
Negotiations are apparently underway in the House of Representatives over the Medicare Sustainable Growth Rate (SGR) formula, and agreement on a possible repeal could be on the horizon.
The new efforts will hopefully lead to an improved, permanent payment system that ensures Medicare is on a sustainable path going forward, said Sen. Ron Wyden (D-Ore.), ranking member of the Senate Finance Committee.
“I’ve been in Congress long enough to be skeptical of rumors, but what we are hearing from the House suggests there is real movement to fully repeal and replace the flawed formula for paying Medicare providers known as SGR,” Sen. Wyden said in a statement. “If what we’re hearing is true, it’s good news and moves us closer to something I’ve been working tirelessly to achieve – a payment formula that stands on its own, doesn’t require annual and expensive ‘patches,’ and which opens the door to improving the way care is delivered.”
The current SGR patch expires March 31, after which physicians can expect a 21% pay cut.
A new analysis of last year’s repeal legislation notes the bill has strengths and weaknesses for physicians (Health Aff. 2015 doi: 10.1377/hlthaff.2014.1429). Current congressional deliberations are focused on how to pay for the SGR fix, with wide consensus that the 2014 legislation will remain the basic model for reform.
The SGR Repeal and Medicare Provider Payment Modernization Act of 2014 includes opportunities for specialists to participate in pay-for-performance programs and other alternative payment models, according to author James Reschovsky, a senior fellow at policy research firm Mathematica Policy Research. The legislation would create two new payment pathways for doctors, one for those who want to continue to receive fee-for-service payments, and another for those already participating in value-based payment models, including accountable care arrangements and bundled payment initiatives.
But the bill fails to address distortions in Medicare’s fee-for-service fee schedule, which some argue overvalues specialty care services, while undervaluing preventive care, Mr. Reschovsky and his colleagues said. Without fixing that defect, specialists may find it more lucrative to stay in Medicare’s fee-for-service program and continue to concentrate on providing high-cost services. Attempts to bring down costs through ACOs and other alternative payment methods also will be difficult as long as the fee-for-service pay rates underlying these programs are skewed.
“Correcting fee schedule valuations will be a substantial and controversial undertaking,” they wrote. “But it is one that is vitally important to the SGR fix’s prospects for success.”
The SGR Repeal and Medicare Provider Payment Modernization Act of 2014 passed the House last year, but was not taken up by the Senate
On Twitter @legal_med
Negotiations are apparently underway in the House of Representatives over the Medicare Sustainable Growth Rate (SGR) formula, and agreement on a possible repeal could be on the horizon.
The new efforts will hopefully lead to an improved, permanent payment system that ensures Medicare is on a sustainable path going forward, said Sen. Ron Wyden (D-Ore.), ranking member of the Senate Finance Committee.
“I’ve been in Congress long enough to be skeptical of rumors, but what we are hearing from the House suggests there is real movement to fully repeal and replace the flawed formula for paying Medicare providers known as SGR,” Sen. Wyden said in a statement. “If what we’re hearing is true, it’s good news and moves us closer to something I’ve been working tirelessly to achieve – a payment formula that stands on its own, doesn’t require annual and expensive ‘patches,’ and which opens the door to improving the way care is delivered.”
The current SGR patch expires March 31, after which physicians can expect a 21% pay cut.
A new analysis of last year’s repeal legislation notes the bill has strengths and weaknesses for physicians (Health Aff. 2015 doi: 10.1377/hlthaff.2014.1429). Current congressional deliberations are focused on how to pay for the SGR fix, with wide consensus that the 2014 legislation will remain the basic model for reform.
The SGR Repeal and Medicare Provider Payment Modernization Act of 2014 includes opportunities for specialists to participate in pay-for-performance programs and other alternative payment models, according to author James Reschovsky, a senior fellow at policy research firm Mathematica Policy Research. The legislation would create two new payment pathways for doctors, one for those who want to continue to receive fee-for-service payments, and another for those already participating in value-based payment models, including accountable care arrangements and bundled payment initiatives.
But the bill fails to address distortions in Medicare’s fee-for-service fee schedule, which some argue overvalues specialty care services, while undervaluing preventive care, Mr. Reschovsky and his colleagues said. Without fixing that defect, specialists may find it more lucrative to stay in Medicare’s fee-for-service program and continue to concentrate on providing high-cost services. Attempts to bring down costs through ACOs and other alternative payment methods also will be difficult as long as the fee-for-service pay rates underlying these programs are skewed.
“Correcting fee schedule valuations will be a substantial and controversial undertaking,” they wrote. “But it is one that is vitally important to the SGR fix’s prospects for success.”
The SGR Repeal and Medicare Provider Payment Modernization Act of 2014 passed the House last year, but was not taken up by the Senate
On Twitter @legal_med
Locum tenens use reached new high in 2014
Use of locum tenens physicians reached a new high for the second year in a row in 2014, according to a annual survey by Staff Care, a health care staffing company.
Last year, 91% of the 259 health care facility managers surveyed reported that they used locum tenens physicians in the 12 months before the survey, surpassing the 90% rate for 2013, which had been the previous high. The current survey is the 12th the company has conducted.
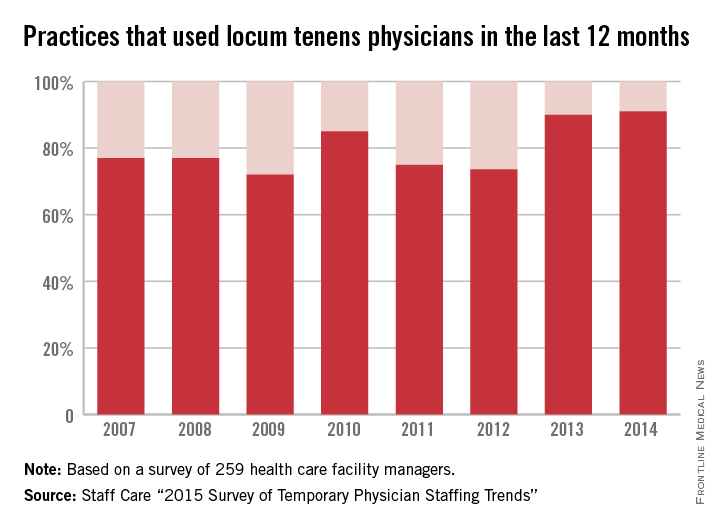
The increase appears to be driven by the shortage of physicians and by the move from independent practice to employment, the report noted.
Medical practices were most likely to be looking for primary care physicians to fill their temporary positions, followed by psychiatrists and other mental health specialists and by hospitalists, Staff Care said.
In a separate survey of 2,087 physicians who do locum tenens, Staff Care found that 21% of those physicians went directly to temporary work after completing their residencies, up from 16% in 2013 and 14.3% in 2012.
“Newly trained doctors are seeking alternatives to traditional private practice, and locum tenens offers them an avenue to explore these alternatives,” Sean Ebner, president of Staff Care, said in a written statement. “It’s a way to ‘test drive’ a practice before they buy.”
Use of locum tenens physicians reached a new high for the second year in a row in 2014, according to a annual survey by Staff Care, a health care staffing company.
Last year, 91% of the 259 health care facility managers surveyed reported that they used locum tenens physicians in the 12 months before the survey, surpassing the 90% rate for 2013, which had been the previous high. The current survey is the 12th the company has conducted.
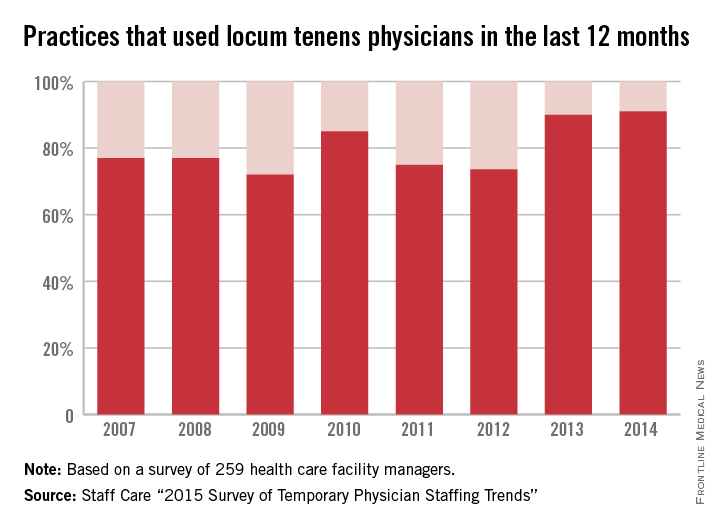
The increase appears to be driven by the shortage of physicians and by the move from independent practice to employment, the report noted.
Medical practices were most likely to be looking for primary care physicians to fill their temporary positions, followed by psychiatrists and other mental health specialists and by hospitalists, Staff Care said.
In a separate survey of 2,087 physicians who do locum tenens, Staff Care found that 21% of those physicians went directly to temporary work after completing their residencies, up from 16% in 2013 and 14.3% in 2012.
“Newly trained doctors are seeking alternatives to traditional private practice, and locum tenens offers them an avenue to explore these alternatives,” Sean Ebner, president of Staff Care, said in a written statement. “It’s a way to ‘test drive’ a practice before they buy.”
Use of locum tenens physicians reached a new high for the second year in a row in 2014, according to a annual survey by Staff Care, a health care staffing company.
Last year, 91% of the 259 health care facility managers surveyed reported that they used locum tenens physicians in the 12 months before the survey, surpassing the 90% rate for 2013, which had been the previous high. The current survey is the 12th the company has conducted.
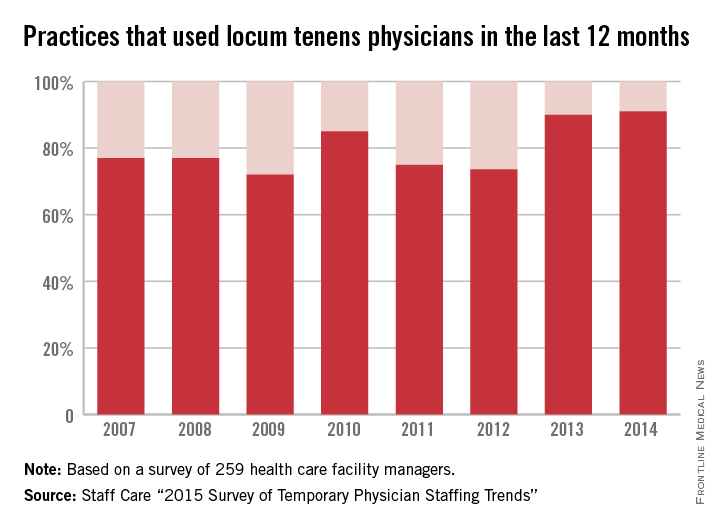
The increase appears to be driven by the shortage of physicians and by the move from independent practice to employment, the report noted.
Medical practices were most likely to be looking for primary care physicians to fill their temporary positions, followed by psychiatrists and other mental health specialists and by hospitalists, Staff Care said.
In a separate survey of 2,087 physicians who do locum tenens, Staff Care found that 21% of those physicians went directly to temporary work after completing their residencies, up from 16% in 2013 and 14.3% in 2012.
“Newly trained doctors are seeking alternatives to traditional private practice, and locum tenens offers them an avenue to explore these alternatives,” Sean Ebner, president of Staff Care, said in a written statement. “It’s a way to ‘test drive’ a practice before they buy.”