User login
Plant-based foods could keep type 2 diabetes at bay
according to a new systematic review and meta-analysis of nine observational studies.
The findings aren’t conclusive, but the study authors wrote in JAMA Internal Medicine that they suggest that “plant-based dietary patterns were associated with lower risk of type 2 diabetes, even after adjustment for [body mass index].”
According to 2015 figures provided by the American Diabetes Association, about 29 million people in the United States have type 2 diabetes. Overall, diabetes contributes to hundreds of thousands of deaths each year, which makes it the seventh-leading cause of death in the nation.
For the new analysis, researchers led by Frank Qian, MPH, of Harvard T.H. Chan School of Public Health included nine studies that examined diet and type 2 diabetes. In all, the studies included 307,099 participants, and there were 23,544 cases of incident type 2 diabetes. They were conducted in five countries, including the United States, and tracked participants for 2-28 years; the studies were all published within the last 11 years. The mean ages of participants ranged from 36-65 years.
The meta-analysis linked higher consumption of plant-based foods to a 23% reduced risk of type 2 diabetes, compared with lower consumption (relative risk, 0.77; 95% confidence interval, 0.71-0.84; P = .07 for heterogeneity). The risk dipped even further (down to 30%) when the researchers analyzed four studies that focused on healthy plant-based foods, such as fruits and vegetables, instead of foods such as refined grains, starches, and sugars (RR, 0.70; 95% CI, 0.62-0.79).
The researchers suggested that plant-based diets may lower the risk of diabetes type 2 by limiting weight gain. They also noted various limitations to their analysis, such as the reliance on self-reports and the observational nature of the studies.
Still, “in general populations that do not practice strict vegetarian or vegan diets, replacing animal products with healthful plant-based foods is likely to exert a significant reduction in the risk of diabetes,” the authors wrote.
The study was funded by the National Institutes of Health, and one author received support from the National Institute of Diabetes and Digestive and Kidney Diseases. The remaining authors reported no conflicts of interest withing the scope of this study.
SOURCE: Qian F et al. JAMA Internal Medicine. 2019 Jul 22. doi: 10.1001/jamainternmed.2019.2195.
according to a new systematic review and meta-analysis of nine observational studies.
The findings aren’t conclusive, but the study authors wrote in JAMA Internal Medicine that they suggest that “plant-based dietary patterns were associated with lower risk of type 2 diabetes, even after adjustment for [body mass index].”
According to 2015 figures provided by the American Diabetes Association, about 29 million people in the United States have type 2 diabetes. Overall, diabetes contributes to hundreds of thousands of deaths each year, which makes it the seventh-leading cause of death in the nation.
For the new analysis, researchers led by Frank Qian, MPH, of Harvard T.H. Chan School of Public Health included nine studies that examined diet and type 2 diabetes. In all, the studies included 307,099 participants, and there were 23,544 cases of incident type 2 diabetes. They were conducted in five countries, including the United States, and tracked participants for 2-28 years; the studies were all published within the last 11 years. The mean ages of participants ranged from 36-65 years.
The meta-analysis linked higher consumption of plant-based foods to a 23% reduced risk of type 2 diabetes, compared with lower consumption (relative risk, 0.77; 95% confidence interval, 0.71-0.84; P = .07 for heterogeneity). The risk dipped even further (down to 30%) when the researchers analyzed four studies that focused on healthy plant-based foods, such as fruits and vegetables, instead of foods such as refined grains, starches, and sugars (RR, 0.70; 95% CI, 0.62-0.79).
The researchers suggested that plant-based diets may lower the risk of diabetes type 2 by limiting weight gain. They also noted various limitations to their analysis, such as the reliance on self-reports and the observational nature of the studies.
Still, “in general populations that do not practice strict vegetarian or vegan diets, replacing animal products with healthful plant-based foods is likely to exert a significant reduction in the risk of diabetes,” the authors wrote.
The study was funded by the National Institutes of Health, and one author received support from the National Institute of Diabetes and Digestive and Kidney Diseases. The remaining authors reported no conflicts of interest withing the scope of this study.
SOURCE: Qian F et al. JAMA Internal Medicine. 2019 Jul 22. doi: 10.1001/jamainternmed.2019.2195.
according to a new systematic review and meta-analysis of nine observational studies.
The findings aren’t conclusive, but the study authors wrote in JAMA Internal Medicine that they suggest that “plant-based dietary patterns were associated with lower risk of type 2 diabetes, even after adjustment for [body mass index].”
According to 2015 figures provided by the American Diabetes Association, about 29 million people in the United States have type 2 diabetes. Overall, diabetes contributes to hundreds of thousands of deaths each year, which makes it the seventh-leading cause of death in the nation.
For the new analysis, researchers led by Frank Qian, MPH, of Harvard T.H. Chan School of Public Health included nine studies that examined diet and type 2 diabetes. In all, the studies included 307,099 participants, and there were 23,544 cases of incident type 2 diabetes. They were conducted in five countries, including the United States, and tracked participants for 2-28 years; the studies were all published within the last 11 years. The mean ages of participants ranged from 36-65 years.
The meta-analysis linked higher consumption of plant-based foods to a 23% reduced risk of type 2 diabetes, compared with lower consumption (relative risk, 0.77; 95% confidence interval, 0.71-0.84; P = .07 for heterogeneity). The risk dipped even further (down to 30%) when the researchers analyzed four studies that focused on healthy plant-based foods, such as fruits and vegetables, instead of foods such as refined grains, starches, and sugars (RR, 0.70; 95% CI, 0.62-0.79).
The researchers suggested that plant-based diets may lower the risk of diabetes type 2 by limiting weight gain. They also noted various limitations to their analysis, such as the reliance on self-reports and the observational nature of the studies.
Still, “in general populations that do not practice strict vegetarian or vegan diets, replacing animal products with healthful plant-based foods is likely to exert a significant reduction in the risk of diabetes,” the authors wrote.
The study was funded by the National Institutes of Health, and one author received support from the National Institute of Diabetes and Digestive and Kidney Diseases. The remaining authors reported no conflicts of interest withing the scope of this study.
SOURCE: Qian F et al. JAMA Internal Medicine. 2019 Jul 22. doi: 10.1001/jamainternmed.2019.2195.
FROM JAMA INTERNAL MEDICINE
FDA declines dapagliflozin indication as adjunct for type 1 diabetes
The Food and Drug Administration has rejected AstraZeneca’s supplemental New Drug Application for the sodium-glucose cotransporter 2 inhibitor dapagliflozin (Farxiga) as an adjunct treatment to insulin in adult patients with type 1 diabetes.
The company said in a press statement that the FDA had issued a complete response letter regarding the application. No reason was given for the decision, but the company said it would work with the agency to discuss the next steps.
The once-daily therapy has been approved as both a monotherapy and combination therapy, as an adjunct to diet and exercise, for improving glycemic control in adults with type 2 diabetes who cannot achieve control with insulin alone. It also has additional demonstrated benefits of weight loss and reduction in blood pressure.
On March 25, 2019, the drug received its first approval for treatment of patients with type 1 diabetes when the European Commission gave it the green light for use in patients with a body mass index of 27 kg/m2 or more when insulin alone does not provide adequate glycemic control. Japan followed a few days later with its approval of the sodium-glucose cotransporter 2 inhibitor, also for type 1 disease in adults.
The approvals for type 1 diabetes in the European Union and Japan were based on data from the phase 3 DEPICT (Dapagliflozin Evaluation in Patients With Inadequately Controlled Type 1 Diabetes) trial program (DEPICT-1 and DEPICT-2), which showed that 5 mg dapagliflozin, taken daily as an oral adjunct to insulin in patients with hard-to-control type 1 disease, reduced blood glucose levels from baseline (the primary endpoint). Secondary endpoints – reductions in weight and total daily insulin use – were also achieved.
Dapagliflozin’s safety profile in the trials in patients with type 1 diabetes was consistent with that established in patients with type 2 disease. However, there was a higher number of cases of diabetic ketoacidosis events in patients who received dapagliflozin. Diabetic ketoacidosis is a known complication for adults with type 1 diabetes and is more prevalent in patients with type 1 disease than in those with type 2.
The Food and Drug Administration has rejected AstraZeneca’s supplemental New Drug Application for the sodium-glucose cotransporter 2 inhibitor dapagliflozin (Farxiga) as an adjunct treatment to insulin in adult patients with type 1 diabetes.
The company said in a press statement that the FDA had issued a complete response letter regarding the application. No reason was given for the decision, but the company said it would work with the agency to discuss the next steps.
The once-daily therapy has been approved as both a monotherapy and combination therapy, as an adjunct to diet and exercise, for improving glycemic control in adults with type 2 diabetes who cannot achieve control with insulin alone. It also has additional demonstrated benefits of weight loss and reduction in blood pressure.
On March 25, 2019, the drug received its first approval for treatment of patients with type 1 diabetes when the European Commission gave it the green light for use in patients with a body mass index of 27 kg/m2 or more when insulin alone does not provide adequate glycemic control. Japan followed a few days later with its approval of the sodium-glucose cotransporter 2 inhibitor, also for type 1 disease in adults.
The approvals for type 1 diabetes in the European Union and Japan were based on data from the phase 3 DEPICT (Dapagliflozin Evaluation in Patients With Inadequately Controlled Type 1 Diabetes) trial program (DEPICT-1 and DEPICT-2), which showed that 5 mg dapagliflozin, taken daily as an oral adjunct to insulin in patients with hard-to-control type 1 disease, reduced blood glucose levels from baseline (the primary endpoint). Secondary endpoints – reductions in weight and total daily insulin use – were also achieved.
Dapagliflozin’s safety profile in the trials in patients with type 1 diabetes was consistent with that established in patients with type 2 disease. However, there was a higher number of cases of diabetic ketoacidosis events in patients who received dapagliflozin. Diabetic ketoacidosis is a known complication for adults with type 1 diabetes and is more prevalent in patients with type 1 disease than in those with type 2.
The Food and Drug Administration has rejected AstraZeneca’s supplemental New Drug Application for the sodium-glucose cotransporter 2 inhibitor dapagliflozin (Farxiga) as an adjunct treatment to insulin in adult patients with type 1 diabetes.
The company said in a press statement that the FDA had issued a complete response letter regarding the application. No reason was given for the decision, but the company said it would work with the agency to discuss the next steps.
The once-daily therapy has been approved as both a monotherapy and combination therapy, as an adjunct to diet and exercise, for improving glycemic control in adults with type 2 diabetes who cannot achieve control with insulin alone. It also has additional demonstrated benefits of weight loss and reduction in blood pressure.
On March 25, 2019, the drug received its first approval for treatment of patients with type 1 diabetes when the European Commission gave it the green light for use in patients with a body mass index of 27 kg/m2 or more when insulin alone does not provide adequate glycemic control. Japan followed a few days later with its approval of the sodium-glucose cotransporter 2 inhibitor, also for type 1 disease in adults.
The approvals for type 1 diabetes in the European Union and Japan were based on data from the phase 3 DEPICT (Dapagliflozin Evaluation in Patients With Inadequately Controlled Type 1 Diabetes) trial program (DEPICT-1 and DEPICT-2), which showed that 5 mg dapagliflozin, taken daily as an oral adjunct to insulin in patients with hard-to-control type 1 disease, reduced blood glucose levels from baseline (the primary endpoint). Secondary endpoints – reductions in weight and total daily insulin use – were also achieved.
Dapagliflozin’s safety profile in the trials in patients with type 1 diabetes was consistent with that established in patients with type 2 disease. However, there was a higher number of cases of diabetic ketoacidosis events in patients who received dapagliflozin. Diabetic ketoacidosis is a known complication for adults with type 1 diabetes and is more prevalent in patients with type 1 disease than in those with type 2.
CARMELINA confirms linagliptin’s renal, CV safety, but it’s still third-line for type 2 diabetes
SAN FRANCISCO – The dipeptidyl peptidase-4 inhibitor linagliptin (Tradjenta) is safe on the kidneys, the cardiovascular system, and in older people with type 2 diabetes, according to findings presented at the annual scientific sessions of the American Diabetes Association.
Investigators in the international Cardiovascular and Renal Microvascular Outcome Study with Linagliptin (CARMELINA) randomized 6,979 patients with type 2 diabetes who also had cardiovascular and/or kidney disease 1:1 to daily oral linagliptin 5 mg or placebo on top of standard of care, and they followed them for a median of 2.2 years. The mean age was 65.9 years, baseline hemoglobin A1c was 8.0%, and disease duration was about 15 years. Almost 63% of the patients were men, and about a quarter had a history of heart failure at baseline (JAMA. 2019;321[1]:69-79).
The study was unusual among other DPP-4 trials in that almost 60% of the patients were older than 65 years and 62.3% had impaired renal function with an estimated glomerular filtration rate (eGFR) of less than 60 ml/min per 1.73 m2.
There was no increased risk with linagliptin, compared with placebo, in the primary composite outcome of cardiovascular death, nonfatal stroke, or nonfatal myocardial infarction (12.4% vs. 12.1%, respectively; hazard ratio, 1.02; P = .74), and there was no difference between the individual components even when broken down by age (younger than 65, 65-75, or older than 75 years) or by renal function (eGFR 60 or more, 45 to less than 60, 30 to less than 45, or less than 30 ml/min per 1.73 m2), according to investigator Mark Cooper, MBBS, PhD, of the department of diabetes at Monash University, Melbourne, who presented the findings.
There was no increase in the number of hospitalizations for heart failure with linagliptin, compared with placebo (6% vs. 6.5%, respectively; HR, 0.90; P = .26) – a concern with some DPP-4 inhibitors – and no increase in hypoglycemia (just over a quarter in both groups), even when broken down by age and renal function.
A decrease in albuminuria with linagliptin held across all renal subgroups. It is not known if that was because of glucose lowering or some other effect, but Dr. Cooper said he believed there was “a modest renal protective effect, [although] not at the level one would expect to translate into hard renal outcomes.”
Robert Eckel, MD, a professor of medicine at the University of Colorado at Denver, Aurora, who moderated the session, said the results were reassuring. “Ultimately, linagliptin seems safe,” even in older people with reduced eGFR. “It does not improve cardiovascular outcomes, but based on many DPP-4 trials, we didn’t expect it to,” he said.
“I don’t think DPP-4s are going to fall into any different place in the [treatment] algorithm” based on these results, he added. The class is currently third-line after metformin or insulin, followed by sodium-glucose cotransporter 2 inhibitors or glucagonlike peptide–1 receptor agonists for cardiovascular protection.
“When we look at [cardiovascular outcomes], ultimately, the SGLT2 inhibitors and the GLP-1 receptor agonists win,” he said. In addition, the blood glucose effects of linagliptin are “pretty modest, so if lowering hemoglobin A1c is the focus, this drug would be lower down on the list.”
Overall, linagliptin “falls into a lesser class, but a safe class for certain circumstances,” said Dr. Eckel, who gave the example of a woman in her late 70s with moderate to severe kidney function, an HbA1c level of 7.9%, and no cardiovascular disease. Her HbA1c might get down to 7.6% or so with linagliptin, he said, “but I’m not sure we have absolute proof of the benefit” of such a modest decline.
Boehringer Ingelheim, the maker of linagliptin, funded the study. The presenter disclosed honoraria, speaking fees, and grants from the company. A number of the investigators were employees of the company.
SAN FRANCISCO – The dipeptidyl peptidase-4 inhibitor linagliptin (Tradjenta) is safe on the kidneys, the cardiovascular system, and in older people with type 2 diabetes, according to findings presented at the annual scientific sessions of the American Diabetes Association.
Investigators in the international Cardiovascular and Renal Microvascular Outcome Study with Linagliptin (CARMELINA) randomized 6,979 patients with type 2 diabetes who also had cardiovascular and/or kidney disease 1:1 to daily oral linagliptin 5 mg or placebo on top of standard of care, and they followed them for a median of 2.2 years. The mean age was 65.9 years, baseline hemoglobin A1c was 8.0%, and disease duration was about 15 years. Almost 63% of the patients were men, and about a quarter had a history of heart failure at baseline (JAMA. 2019;321[1]:69-79).
The study was unusual among other DPP-4 trials in that almost 60% of the patients were older than 65 years and 62.3% had impaired renal function with an estimated glomerular filtration rate (eGFR) of less than 60 ml/min per 1.73 m2.
There was no increased risk with linagliptin, compared with placebo, in the primary composite outcome of cardiovascular death, nonfatal stroke, or nonfatal myocardial infarction (12.4% vs. 12.1%, respectively; hazard ratio, 1.02; P = .74), and there was no difference between the individual components even when broken down by age (younger than 65, 65-75, or older than 75 years) or by renal function (eGFR 60 or more, 45 to less than 60, 30 to less than 45, or less than 30 ml/min per 1.73 m2), according to investigator Mark Cooper, MBBS, PhD, of the department of diabetes at Monash University, Melbourne, who presented the findings.
There was no increase in the number of hospitalizations for heart failure with linagliptin, compared with placebo (6% vs. 6.5%, respectively; HR, 0.90; P = .26) – a concern with some DPP-4 inhibitors – and no increase in hypoglycemia (just over a quarter in both groups), even when broken down by age and renal function.
A decrease in albuminuria with linagliptin held across all renal subgroups. It is not known if that was because of glucose lowering or some other effect, but Dr. Cooper said he believed there was “a modest renal protective effect, [although] not at the level one would expect to translate into hard renal outcomes.”
Robert Eckel, MD, a professor of medicine at the University of Colorado at Denver, Aurora, who moderated the session, said the results were reassuring. “Ultimately, linagliptin seems safe,” even in older people with reduced eGFR. “It does not improve cardiovascular outcomes, but based on many DPP-4 trials, we didn’t expect it to,” he said.
“I don’t think DPP-4s are going to fall into any different place in the [treatment] algorithm” based on these results, he added. The class is currently third-line after metformin or insulin, followed by sodium-glucose cotransporter 2 inhibitors or glucagonlike peptide–1 receptor agonists for cardiovascular protection.
“When we look at [cardiovascular outcomes], ultimately, the SGLT2 inhibitors and the GLP-1 receptor agonists win,” he said. In addition, the blood glucose effects of linagliptin are “pretty modest, so if lowering hemoglobin A1c is the focus, this drug would be lower down on the list.”
Overall, linagliptin “falls into a lesser class, but a safe class for certain circumstances,” said Dr. Eckel, who gave the example of a woman in her late 70s with moderate to severe kidney function, an HbA1c level of 7.9%, and no cardiovascular disease. Her HbA1c might get down to 7.6% or so with linagliptin, he said, “but I’m not sure we have absolute proof of the benefit” of such a modest decline.
Boehringer Ingelheim, the maker of linagliptin, funded the study. The presenter disclosed honoraria, speaking fees, and grants from the company. A number of the investigators were employees of the company.
SAN FRANCISCO – The dipeptidyl peptidase-4 inhibitor linagliptin (Tradjenta) is safe on the kidneys, the cardiovascular system, and in older people with type 2 diabetes, according to findings presented at the annual scientific sessions of the American Diabetes Association.
Investigators in the international Cardiovascular and Renal Microvascular Outcome Study with Linagliptin (CARMELINA) randomized 6,979 patients with type 2 diabetes who also had cardiovascular and/or kidney disease 1:1 to daily oral linagliptin 5 mg or placebo on top of standard of care, and they followed them for a median of 2.2 years. The mean age was 65.9 years, baseline hemoglobin A1c was 8.0%, and disease duration was about 15 years. Almost 63% of the patients were men, and about a quarter had a history of heart failure at baseline (JAMA. 2019;321[1]:69-79).
The study was unusual among other DPP-4 trials in that almost 60% of the patients were older than 65 years and 62.3% had impaired renal function with an estimated glomerular filtration rate (eGFR) of less than 60 ml/min per 1.73 m2.
There was no increased risk with linagliptin, compared with placebo, in the primary composite outcome of cardiovascular death, nonfatal stroke, or nonfatal myocardial infarction (12.4% vs. 12.1%, respectively; hazard ratio, 1.02; P = .74), and there was no difference between the individual components even when broken down by age (younger than 65, 65-75, or older than 75 years) or by renal function (eGFR 60 or more, 45 to less than 60, 30 to less than 45, or less than 30 ml/min per 1.73 m2), according to investigator Mark Cooper, MBBS, PhD, of the department of diabetes at Monash University, Melbourne, who presented the findings.
There was no increase in the number of hospitalizations for heart failure with linagliptin, compared with placebo (6% vs. 6.5%, respectively; HR, 0.90; P = .26) – a concern with some DPP-4 inhibitors – and no increase in hypoglycemia (just over a quarter in both groups), even when broken down by age and renal function.
A decrease in albuminuria with linagliptin held across all renal subgroups. It is not known if that was because of glucose lowering or some other effect, but Dr. Cooper said he believed there was “a modest renal protective effect, [although] not at the level one would expect to translate into hard renal outcomes.”
Robert Eckel, MD, a professor of medicine at the University of Colorado at Denver, Aurora, who moderated the session, said the results were reassuring. “Ultimately, linagliptin seems safe,” even in older people with reduced eGFR. “It does not improve cardiovascular outcomes, but based on many DPP-4 trials, we didn’t expect it to,” he said.
“I don’t think DPP-4s are going to fall into any different place in the [treatment] algorithm” based on these results, he added. The class is currently third-line after metformin or insulin, followed by sodium-glucose cotransporter 2 inhibitors or glucagonlike peptide–1 receptor agonists for cardiovascular protection.
“When we look at [cardiovascular outcomes], ultimately, the SGLT2 inhibitors and the GLP-1 receptor agonists win,” he said. In addition, the blood glucose effects of linagliptin are “pretty modest, so if lowering hemoglobin A1c is the focus, this drug would be lower down on the list.”
Overall, linagliptin “falls into a lesser class, but a safe class for certain circumstances,” said Dr. Eckel, who gave the example of a woman in her late 70s with moderate to severe kidney function, an HbA1c level of 7.9%, and no cardiovascular disease. Her HbA1c might get down to 7.6% or so with linagliptin, he said, “but I’m not sure we have absolute proof of the benefit” of such a modest decline.
Boehringer Ingelheim, the maker of linagliptin, funded the study. The presenter disclosed honoraria, speaking fees, and grants from the company. A number of the investigators were employees of the company.
REPORTING FROM ADA 2019
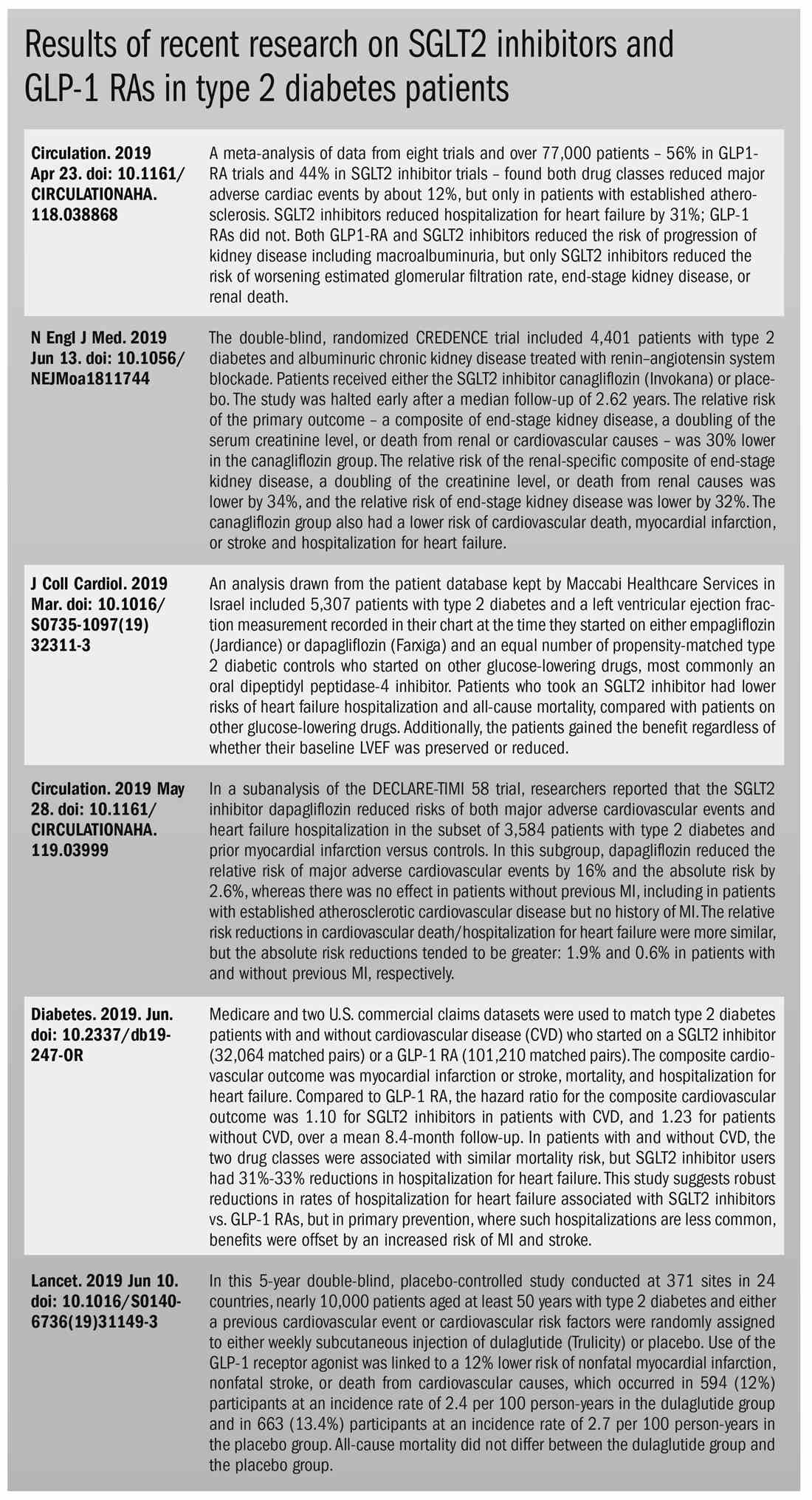
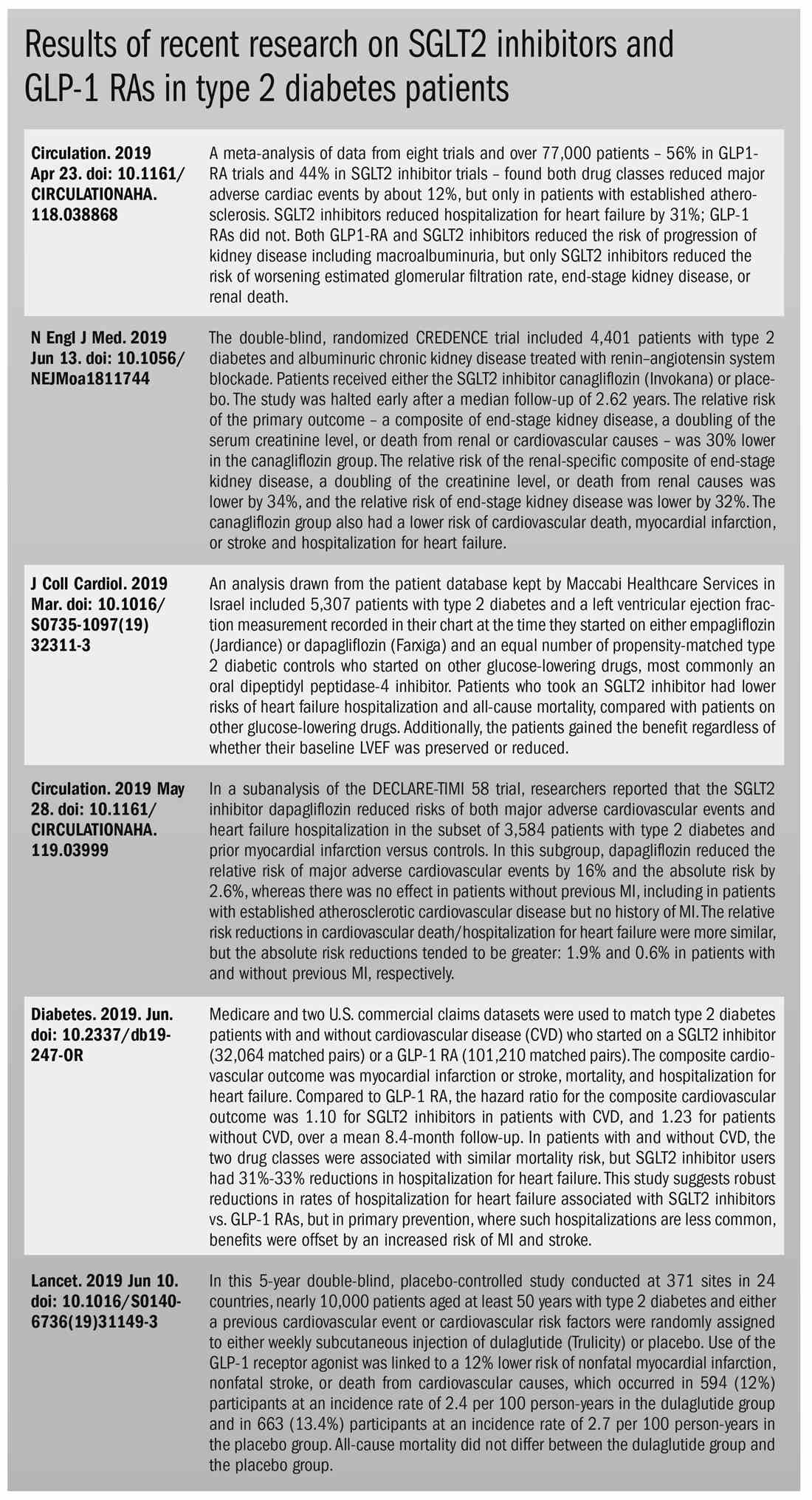
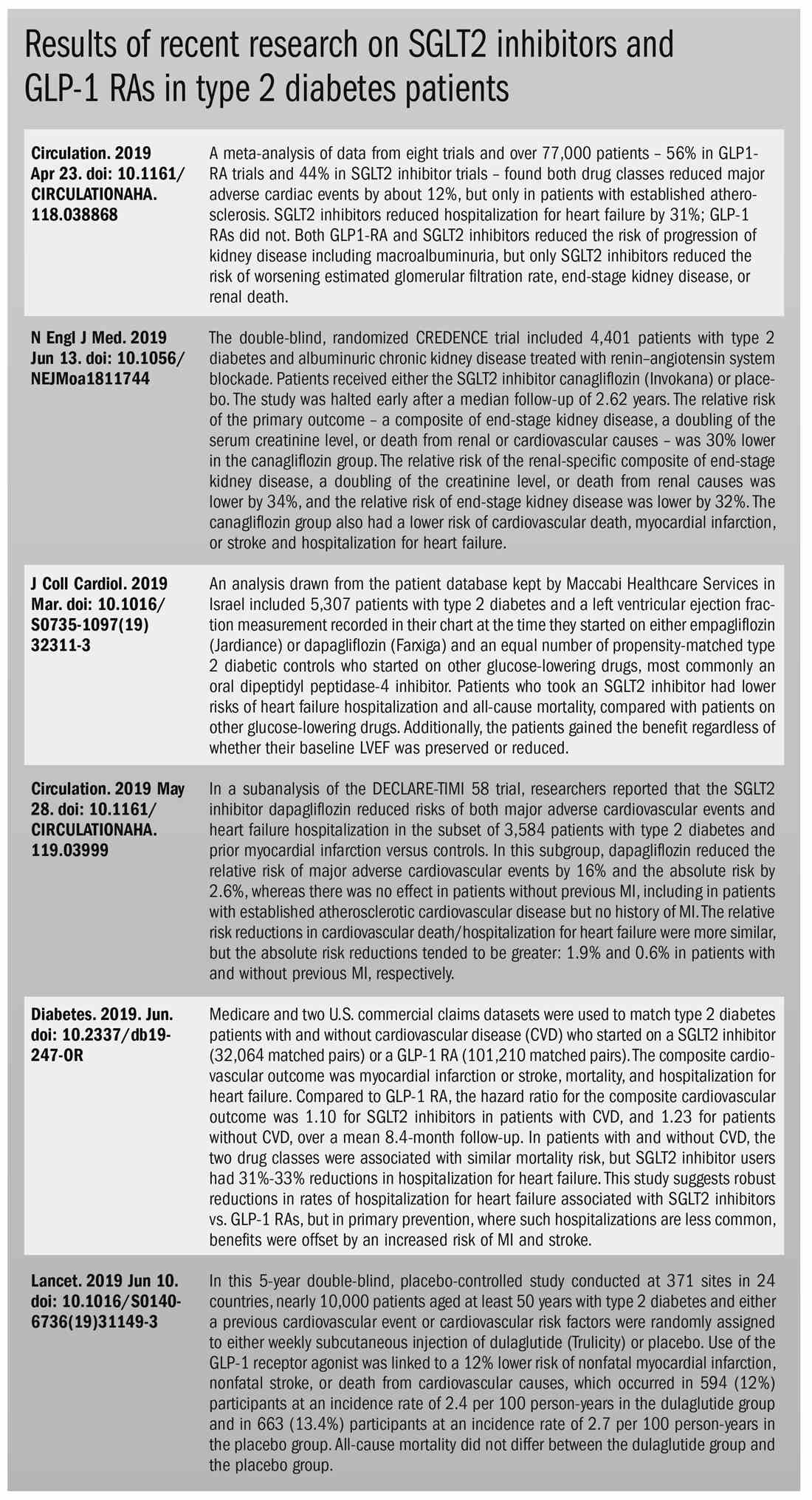
The costs and benefits of SGLT2 inhibitors & GLP-1 RAs
The options for treating type 2 diabetes without insulin have grown beyond metformin to include a long list of sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagonlike peptide–1 (GLP-1) receptor agonists that can be taken with or without metformin. These new drugs have cardiovascular and kidney benefits and help with weight loss, but they also carry risks and, according to some experts, their costs can be prohibitively expensive.
Given the medical community’s long-term experience with treating patients with metformin, and metformin’s lower cost, most of the physicians interviewed for this article advise using SGLT2 inhibitors and GLP-1 receptor agonists as second-line treatments. Others said that they would prefer to use the newer drugs as first-line therapies in select high-risk patients, but prior authorization hurdles created by insurance companies make that approach too burdensome.
“The economics of U.S. health care is stacked against many of our patients with diabetes in the current era,” Robert H. Hopkins Jr., MD, said in an interview.
Even when their insurance approves the drugs, patients still may not be able to afford the copay, explained Dr. Hopkins, professor of internal medicine and pediatrics and director of the division of general internal medicine at the University of Arkansas for Medical Sciences, Little Rock. “Sometimes patients can purchase drugs at a lower cost than the copay to purchase with the ‘drug coverage’ in their insurance plan – unfortunately, this is not the case with the newer diabetes medications we are discussing here.”
“SGLT2 inhibitors and GLP-1 agonists can cost several hundred dollars a month, and insurers often balk at paying for them. They’ll say, ‘Have you tried metformin?’ ” explained endocrinologist Victor Lawrence Roberts, MD, in a interview. “We have to work with insurance companies the best we can in a stepwise fashion.”
According to Dr. Roberts, 80% of his patients with diabetes struggle with the cost of medicine in general. “They’re either underinsured or not insured or their formulary is limited.
Douglas S. Paauw, MD, agreed in an interview that the newer drugs can be problematic on the insurance front.
“For some patients they aren’t affordable, especially for the uninsured if you can’t get them on an assistance program,” said Dr. Paauw, who is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the university.
Dr. Hopkins, who is on the Internal Medicine News board, noted that “unfortunately, the treatment of type 2 diabetes in patients who cannot achieve control with metformin, diet, weight control, and exercise is a story of the ‘haves’ and the ‘have nots.’ The ‘haves’ are those who have pharmacy benefits which make access to newer agents like SGLT2 inhibitors and GLP-1 agonists a possibility.”
“I have had very few of the ‘have nots’ who have been able to even consider these newer agents, which carry price tags of $600-$1,300 a month even with the availability of discounting coupons in the marketplace,” he added. “Most of these patients end up requiring a sulfonylurea or TZD [thiazolidinedione] as a second agent to achieve glycemic control. This makes it very difficult to achieve sufficient weight and metabolic control to avoid an eventual switch to insulin.”
Fatima Z. Syed, MD, an endocrine-trained general internist at DukeHealth in Durham, N.C., said she prescribes SGLT2 inhibitors and GLP-1 receptor agonists in combination with metformin. “I prescribe them frequently, but they are not first-line treatments,” she explained.
“Nothing replaces diet and exercise” as therapy for patients with type 2 diabetes, she added.
Neil S. Skolnik, MD, said that insurance companies were not preventing patients from using these drugs in his experience. He also provided an optimistic take on the accessibility of these drugs in the near future.
“Most insurance companies are now covering select SGLT2 inhibitors and GLP-1 receptor agonists for appropriate patients and those companies that currently do not will soon have to,” said Dr. Skolnik, who is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
“The outcomes [associated with use of the new drugs] are robust, the benefits are large, and are well worth the cost,” he added.
The side effects
While others praised these drugs for their beneficial effects, they also noted that the side effects of these drugs are serious and must be discussed with patients.
GLP-1 receptor agonists are linked to gastrointestinal symptoms, especially nausea, while SGLT2 inhibitors have been linked to kidney failure, ketoacidosis, and more. The Food and Drug Administration warned in 2018 that the SGLT2 inhibitors can cause a rare serious infection known as Fournier’s gangrene – necrotizing fasciitis of the perineum.
“We have to tell our patients to let us know right away if they get pain or swelling in the genital area,” Dr. Paauw, who is on the Internal Medicine News board, noted. “The chance that an infection could explode quickly is higher in those who take these drugs.”
Amputation risks also are associated with taking the SGLT2 inhibitor canagliflozin (Invokana). The FDA requires the manufacturer of this drug to include a black-box warning about the risk of “lower-limb amputations, most frequently of the toe and midfoot,” but also the leg. In approval trials, the risk doubled versus placebo.
These amputation risks “put a damper on some of the enthusiasm on behalf of physicians and patients ... for taking this drug,” noted Dr. Roberts, who is a professor of internal medicine at the University of Central Florida, Orlando.
While a manufacturer-funded study released last year found no link to amputations, the results weren’t powerful enough to rule out a moderately increased risk.
“[If] you are at high risk for having an amputation, we really have to take this risk very seriously,” said John B. Buse, MD, chief of the division of endocrinology at the University of North Carolina at Chapel Hill, in a presentation about the study at the 2018 annual scientific sessions of the American Diabetes Association.
The benefits
Despite these risks of adverse events, most interviewed agreed that the many benefits observed in those taking SGLT2 inhibitors or GLP-1 receptor agonists make them worth prescribing, at least to those who are able to afford them.
Both SGLT2 inhibitors and GLP-1 receptor agonists appear to have significant cardiovascular benefits. A 2019 meta-analysis and systematic review found that both drugs reduced major adverse cardiac events by about 12% (Circulation. 2019 Apr 23;139[17]:2022-31).
“They don’t cause hypoglycemia, they lower blood pressure, they don’t cause weight gain, and they might promote weight loss,” noted Dr. Paauw.
SGLT2 inhibitors also have shown signs of kidney benefits. The CREDENCE trial linked canagliflozin to a lowering of kidney disorders versus placebo (N Engl J Med. 2019 Jun 13;380[24]:2295-306). “The relative risk of the renal-specific composite of end-stage kidney disease, a doubling of the creatinine level, or death from renal causes was lower by 34% (hazard ratio, 0.66; 95% confidence interval, 0.53-0.81; P less than .001), and the relative risk of end-stage kidney disease was lower by 32% (HR, 0.68; 95% CI, 0.54-0.86; P = .002),” the trial investigators wrote.
“They showed very nicely that the drug improved the kidney function of those patients and reduced the kidney deterioration,” said Yehuda Handelsman, MD, an endocrinologist in Tarzana, Calif., who chaired the 2011 and 2015 American Association of Clinical Endocrinologists’ Comprehensive Diabetes Guidelines. The study was especially impressive, he added, because it included patients with low kidney function.
SGLT2 inhibitors’ “diuretic mechanism explains why there is a substantial reduction in heart failure hospitalizations in patients who take these drugs,” said cardiologist Marc E. Goldschmidt, MD, director of the Heart Success Program at Atlantic Health System’s Morristown (N.J.) Medical Center, in an interview. “Both the EMPA-REG Outcome and the CREDENCE trials demonstrated substantial benefit of this class of medications by showing a lower risk of cardiovascular death as well as death from any cause and a lower risk of hospitalization for heart failure."
Overall, the SGLT2 trial data have been very consistent with a benefit for cardiovascular risk reduction, particularly in regard to heart failure hospitalizations and even in potentially preventing heart failure in diabetics,” he added.
Dr. Skolnik, a columnist for Family Practice News, cited SGLT2 inhibitors and GLP-1 receptor agonists’ ability to slow renal disease progression, promote weight loss, and prevent poor cardiac outcomes.“These drugs should be used, in addition to metformin, in all patients with diabetes and vascular disease. These proven outcomes are far better than we ever were able to achieve previously and the strength of the evidence at this point is very strong,” said Dr. Skolnik. “In addition to the benefits of decreasing the development of cardiovascular disease, serious heart failure, and slowing progression of renal disease, these two classes of medication have additional benefits. Both classes help patients lose weight, which is very different from what was found with either sulfonylureas or insulin, which cause patients to gain weight. Also both the SGLT2 inhibitors and the GLP-1 RAs [receptor agonists] have a low incidence of hypoglycemia. For all these reasons, these have become important medications for us to use in primary care.”
Other recent trials offer “very powerful data” about SGLT2 inhibitors, Dr. Roberts said. That’s good news, since “our approach needs to be toward cardiovascular protection and preservation as well as managing blood sugar.”An Israeli trial, whose results were released in May 2019 at the annual meeting of the American College of Cardiology, found that, compared with other glucose-lowering drugs, taking an SGLT2 inhibitor was associated with lower risks of heart failure hospitalization and all-cause mortality (HR, 0.54; 95% CI, 0.44-0.65; P less than .001). This trial also offered a new detail: The patients gained the benefit regardless of whether their baseline left ventricular ejection fraction was preserved or reduced (J Coll Cardiol. 2019 Mar;73[9]:suppl 1). The SGLT2 inhibitors used in this trial included dapagliflozin (Farxiga) and empagliflozin (Jardiance).
In another study released this year, a subanalysis of the DECLARE-TIMI 58 trial, researchers reported that the SGLT2 inhibitor dapagliflozin reduced risks of both major adverse cardiovascular events and heart failure hospitalization in the subset of patients with type 2 diabetes and prior myocardial infarction versus controls (Circulation. 2019 May 28;139[22]:2516-27). The absolute risk reduction for major adverse cardiovascular events was 1.9% (HR, 0.81; 95% CI, 0.65-1.00; P = .046), while it was 0.6% for heart failure hospitalization (HR, 0.85; 95% CI, 0.72-1.00; P = .055).
These and other studies “speak volumes about the efficacy of managing blood sugar and addressing our biggest nemesis, which is cardiovascular disease,” Dr. Roberts said. “It’s irrefutable. The data [are] very good.”
Dr. Paauw said an SGLT2 inhibitor or GLP-1 receptor agonist is best reserved for use in select patients with cardiovascular risks and type 2 diabetes that need management beyond metformin.
For example, they might fit a 70-year-old with persistent hypertension who’s already taking a couple of blood pressure medications. “If they have another cardiovascular risk factor, the cardiovascular protection piece will be a bigger deal,” he said. Also, “it will probably help lower their blood pressure so they can avoid taking another blood pressure medicine.”
Trials of both GLP-1 receptor agonists and SGLT2 inhibitors have shown benefits “in improving [major adverse cardiac events], with the SGLT2 class showing substantial benefit in improving both heart failure and renal outcomes as well,” noted Dr. Skolnik. “It is in this context that one must address the question of whether the price of the medications are worthwhile. With such substantial benefit, there is no question in my mind that – for patients who have underlying cardiovascular illness, which includes patients with existent coronary disease, history of stroke, transient ischemic attack, or peripheral vascular disease – it is far and away worth it to prescribe these classes of medications.”
Indeed, the American Diabetes Association and the European Association for the Study of Diabetes’ most recent guidelines now call for a GLP-1 receptor agonist – instead of insulin – to be the first injectable used to treat type 2 diabetes (Diabetes Care 2018 Dec; 41[12]:2669-701).
“For the relatively small number of my patients who have been able to access and use these medications for months or longer, more have tolerated the GLP-1 agonists than SGLT2 inhibitors primarily due to urinary issues,” noted Dr. Hopkins.
Dipeptidyl peptidase–4 inhibitors are another option in patients with type 2 diabetes, but research suggests they may not be a top option for patients with cardiovascular risk. A 2018 review noted that cardiovascular outcome trials for alogliptin (Nesina), saxagliptin (Onglyza), and sitagliptin (Januvia) showed noninferiority but failed to demonstrate any superiority, compared with placebo in patients with type 2 diabetes mellitus and high cardiovascular risk (Circ Res. 2018 May 11;122[10]:1439-59).
The combination therapies
Many of the newer drugs are available as combinations with other types of diabetes drugs. In some cases, physicians create their own form of combination therapy by separately prescribing two or more diabetes drugs. Earlier this year, a study suggested the benefits of this kind of add-on therapy: Diabetes outcomes improved in patients who took the GLP-1 receptor agonist semaglutide and an SGLT2 inhibitor (Lancet Diabetes Endocrinol. 2019 Mar 1. doi: 10.1016/S2213-8587[19]30066-X).
Dr. Roberts suggested caution, however, when prescribing combination therapies. “My recommendation is always to begin with the individual medications to see if the patient tolerates the drugs and then decide which component needs to be titrated. It’s hard to titrate a combination drug, and it doesn’t leave a lot of flexibility. You never know which drug is doing what.
Dr. Handelsman said some patients may need to take three medications such as metformin, an SGLT2 inhibitor, and a GLP-1 receptor agonist.
“I don’t recommend using the combinations if you’re not familiar with the drugs ... These are relatively new pharmaceuticals, and most of us are on a learning curve as to how they fit into the armamentarium. If a drug is tolerated with a good response, you can certainly consider going to the combination tablets,” he added.
There is at least one drug that combines these three classes: The newly FDA-approved Qternmet XR, which combines dapagliflozin (an SGLT2 inhibitor), saxagliptin (a GLP-1 receptor agonist), and metformin. As of mid-June 2019, it was not yet available in the United States. Its sister drug Qtern, which combines dapagliflozin and saxagliptin, costs more than $500 a month with a free coupon, according to goodrx.com. In contrast, metformin is extremely inexpensive, costing just a few dollars a month for a common starting dose.
What about adding insulin?
“Both [SGLT2 inhibitors and GLP-1 receptor agonists] work very well with insulin,” Dr. Handelsman said. “There is a nice additive effect on the reduction of [hemoglobin] A1c. The only caution is that, although neither SGLT2 inhibitors nor GLP-1 receptor agonists cause hypoglycemia, in combination with insulin they do increase the risk of hypoglycemia. You may have to adjust the dose of insulin.”
Dr. Hopkins warned that cost becomes an even bigger issue when you add insulin into the mix.
“When insulin comes into the discussion, we are again stuck with astronomical costs which many struggle to afford,” he explained.
Indeed, the price tag on these drugs seems to be the biggest problem physicians have with them.
“The challenges in managing patients with diabetes aren’t the risks associated with the drugs. It’s dealing with their insurers,” noted Dr. Roberts.
Dr. Hopkins, Dr. Paauw, Dr. Roberts, and Dr. Syed reported no disclosures. Dr. Buse is an investigator for Johnson and Johnson. Dr. Goldschmidt is paid to speak by Novartis. Dr. Handelsman reported research grants, consulting work, and speaker honoraria from Amgen, Gilead, Lilly, Merck, Novo Nordisk, and others. Dr Skolnik reported nonfinancial support from AstraZeneca, Boehringer Ingelheim, Sanofi, and GlaxoSmithKline and personal fees from AstraZeneca, Boehringer Ingelheim, and Eli Lilly. He also serves on the advisory boards of AstraZeneca, Boehringer Ingelheim, Teva Pharmaceutical, Eli Lilly, Sanofi, Janssen Pharmaceuticals, Intarcia, Mylan, and GlaxoSmithKline.
Dr. Paauw and Dr. Skolnik are columnists for Family Practice News and Internal Medicine News.
M. Alexander Otto contributed to this report.
The options for treating type 2 diabetes without insulin have grown beyond metformin to include a long list of sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagonlike peptide–1 (GLP-1) receptor agonists that can be taken with or without metformin. These new drugs have cardiovascular and kidney benefits and help with weight loss, but they also carry risks and, according to some experts, their costs can be prohibitively expensive.
Given the medical community’s long-term experience with treating patients with metformin, and metformin’s lower cost, most of the physicians interviewed for this article advise using SGLT2 inhibitors and GLP-1 receptor agonists as second-line treatments. Others said that they would prefer to use the newer drugs as first-line therapies in select high-risk patients, but prior authorization hurdles created by insurance companies make that approach too burdensome.
“The economics of U.S. health care is stacked against many of our patients with diabetes in the current era,” Robert H. Hopkins Jr., MD, said in an interview.
Even when their insurance approves the drugs, patients still may not be able to afford the copay, explained Dr. Hopkins, professor of internal medicine and pediatrics and director of the division of general internal medicine at the University of Arkansas for Medical Sciences, Little Rock. “Sometimes patients can purchase drugs at a lower cost than the copay to purchase with the ‘drug coverage’ in their insurance plan – unfortunately, this is not the case with the newer diabetes medications we are discussing here.”
“SGLT2 inhibitors and GLP-1 agonists can cost several hundred dollars a month, and insurers often balk at paying for them. They’ll say, ‘Have you tried metformin?’ ” explained endocrinologist Victor Lawrence Roberts, MD, in a interview. “We have to work with insurance companies the best we can in a stepwise fashion.”
According to Dr. Roberts, 80% of his patients with diabetes struggle with the cost of medicine in general. “They’re either underinsured or not insured or their formulary is limited.
Douglas S. Paauw, MD, agreed in an interview that the newer drugs can be problematic on the insurance front.
“For some patients they aren’t affordable, especially for the uninsured if you can’t get them on an assistance program,” said Dr. Paauw, who is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the university.
Dr. Hopkins, who is on the Internal Medicine News board, noted that “unfortunately, the treatment of type 2 diabetes in patients who cannot achieve control with metformin, diet, weight control, and exercise is a story of the ‘haves’ and the ‘have nots.’ The ‘haves’ are those who have pharmacy benefits which make access to newer agents like SGLT2 inhibitors and GLP-1 agonists a possibility.”
“I have had very few of the ‘have nots’ who have been able to even consider these newer agents, which carry price tags of $600-$1,300 a month even with the availability of discounting coupons in the marketplace,” he added. “Most of these patients end up requiring a sulfonylurea or TZD [thiazolidinedione] as a second agent to achieve glycemic control. This makes it very difficult to achieve sufficient weight and metabolic control to avoid an eventual switch to insulin.”
Fatima Z. Syed, MD, an endocrine-trained general internist at DukeHealth in Durham, N.C., said she prescribes SGLT2 inhibitors and GLP-1 receptor agonists in combination with metformin. “I prescribe them frequently, but they are not first-line treatments,” she explained.
“Nothing replaces diet and exercise” as therapy for patients with type 2 diabetes, she added.
Neil S. Skolnik, MD, said that insurance companies were not preventing patients from using these drugs in his experience. He also provided an optimistic take on the accessibility of these drugs in the near future.
“Most insurance companies are now covering select SGLT2 inhibitors and GLP-1 receptor agonists for appropriate patients and those companies that currently do not will soon have to,” said Dr. Skolnik, who is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
“The outcomes [associated with use of the new drugs] are robust, the benefits are large, and are well worth the cost,” he added.
The side effects
While others praised these drugs for their beneficial effects, they also noted that the side effects of these drugs are serious and must be discussed with patients.
GLP-1 receptor agonists are linked to gastrointestinal symptoms, especially nausea, while SGLT2 inhibitors have been linked to kidney failure, ketoacidosis, and more. The Food and Drug Administration warned in 2018 that the SGLT2 inhibitors can cause a rare serious infection known as Fournier’s gangrene – necrotizing fasciitis of the perineum.
“We have to tell our patients to let us know right away if they get pain or swelling in the genital area,” Dr. Paauw, who is on the Internal Medicine News board, noted. “The chance that an infection could explode quickly is higher in those who take these drugs.”
Amputation risks also are associated with taking the SGLT2 inhibitor canagliflozin (Invokana). The FDA requires the manufacturer of this drug to include a black-box warning about the risk of “lower-limb amputations, most frequently of the toe and midfoot,” but also the leg. In approval trials, the risk doubled versus placebo.
These amputation risks “put a damper on some of the enthusiasm on behalf of physicians and patients ... for taking this drug,” noted Dr. Roberts, who is a professor of internal medicine at the University of Central Florida, Orlando.
While a manufacturer-funded study released last year found no link to amputations, the results weren’t powerful enough to rule out a moderately increased risk.
“[If] you are at high risk for having an amputation, we really have to take this risk very seriously,” said John B. Buse, MD, chief of the division of endocrinology at the University of North Carolina at Chapel Hill, in a presentation about the study at the 2018 annual scientific sessions of the American Diabetes Association.
The benefits
Despite these risks of adverse events, most interviewed agreed that the many benefits observed in those taking SGLT2 inhibitors or GLP-1 receptor agonists make them worth prescribing, at least to those who are able to afford them.
Both SGLT2 inhibitors and GLP-1 receptor agonists appear to have significant cardiovascular benefits. A 2019 meta-analysis and systematic review found that both drugs reduced major adverse cardiac events by about 12% (Circulation. 2019 Apr 23;139[17]:2022-31).
“They don’t cause hypoglycemia, they lower blood pressure, they don’t cause weight gain, and they might promote weight loss,” noted Dr. Paauw.
SGLT2 inhibitors also have shown signs of kidney benefits. The CREDENCE trial linked canagliflozin to a lowering of kidney disorders versus placebo (N Engl J Med. 2019 Jun 13;380[24]:2295-306). “The relative risk of the renal-specific composite of end-stage kidney disease, a doubling of the creatinine level, or death from renal causes was lower by 34% (hazard ratio, 0.66; 95% confidence interval, 0.53-0.81; P less than .001), and the relative risk of end-stage kidney disease was lower by 32% (HR, 0.68; 95% CI, 0.54-0.86; P = .002),” the trial investigators wrote.
“They showed very nicely that the drug improved the kidney function of those patients and reduced the kidney deterioration,” said Yehuda Handelsman, MD, an endocrinologist in Tarzana, Calif., who chaired the 2011 and 2015 American Association of Clinical Endocrinologists’ Comprehensive Diabetes Guidelines. The study was especially impressive, he added, because it included patients with low kidney function.
SGLT2 inhibitors’ “diuretic mechanism explains why there is a substantial reduction in heart failure hospitalizations in patients who take these drugs,” said cardiologist Marc E. Goldschmidt, MD, director of the Heart Success Program at Atlantic Health System’s Morristown (N.J.) Medical Center, in an interview. “Both the EMPA-REG Outcome and the CREDENCE trials demonstrated substantial benefit of this class of medications by showing a lower risk of cardiovascular death as well as death from any cause and a lower risk of hospitalization for heart failure."
Overall, the SGLT2 trial data have been very consistent with a benefit for cardiovascular risk reduction, particularly in regard to heart failure hospitalizations and even in potentially preventing heart failure in diabetics,” he added.
Dr. Skolnik, a columnist for Family Practice News, cited SGLT2 inhibitors and GLP-1 receptor agonists’ ability to slow renal disease progression, promote weight loss, and prevent poor cardiac outcomes.“These drugs should be used, in addition to metformin, in all patients with diabetes and vascular disease. These proven outcomes are far better than we ever were able to achieve previously and the strength of the evidence at this point is very strong,” said Dr. Skolnik. “In addition to the benefits of decreasing the development of cardiovascular disease, serious heart failure, and slowing progression of renal disease, these two classes of medication have additional benefits. Both classes help patients lose weight, which is very different from what was found with either sulfonylureas or insulin, which cause patients to gain weight. Also both the SGLT2 inhibitors and the GLP-1 RAs [receptor agonists] have a low incidence of hypoglycemia. For all these reasons, these have become important medications for us to use in primary care.”
Other recent trials offer “very powerful data” about SGLT2 inhibitors, Dr. Roberts said. That’s good news, since “our approach needs to be toward cardiovascular protection and preservation as well as managing blood sugar.”An Israeli trial, whose results were released in May 2019 at the annual meeting of the American College of Cardiology, found that, compared with other glucose-lowering drugs, taking an SGLT2 inhibitor was associated with lower risks of heart failure hospitalization and all-cause mortality (HR, 0.54; 95% CI, 0.44-0.65; P less than .001). This trial also offered a new detail: The patients gained the benefit regardless of whether their baseline left ventricular ejection fraction was preserved or reduced (J Coll Cardiol. 2019 Mar;73[9]:suppl 1). The SGLT2 inhibitors used in this trial included dapagliflozin (Farxiga) and empagliflozin (Jardiance).
In another study released this year, a subanalysis of the DECLARE-TIMI 58 trial, researchers reported that the SGLT2 inhibitor dapagliflozin reduced risks of both major adverse cardiovascular events and heart failure hospitalization in the subset of patients with type 2 diabetes and prior myocardial infarction versus controls (Circulation. 2019 May 28;139[22]:2516-27). The absolute risk reduction for major adverse cardiovascular events was 1.9% (HR, 0.81; 95% CI, 0.65-1.00; P = .046), while it was 0.6% for heart failure hospitalization (HR, 0.85; 95% CI, 0.72-1.00; P = .055).
These and other studies “speak volumes about the efficacy of managing blood sugar and addressing our biggest nemesis, which is cardiovascular disease,” Dr. Roberts said. “It’s irrefutable. The data [are] very good.”
Dr. Paauw said an SGLT2 inhibitor or GLP-1 receptor agonist is best reserved for use in select patients with cardiovascular risks and type 2 diabetes that need management beyond metformin.
For example, they might fit a 70-year-old with persistent hypertension who’s already taking a couple of blood pressure medications. “If they have another cardiovascular risk factor, the cardiovascular protection piece will be a bigger deal,” he said. Also, “it will probably help lower their blood pressure so they can avoid taking another blood pressure medicine.”
Trials of both GLP-1 receptor agonists and SGLT2 inhibitors have shown benefits “in improving [major adverse cardiac events], with the SGLT2 class showing substantial benefit in improving both heart failure and renal outcomes as well,” noted Dr. Skolnik. “It is in this context that one must address the question of whether the price of the medications are worthwhile. With such substantial benefit, there is no question in my mind that – for patients who have underlying cardiovascular illness, which includes patients with existent coronary disease, history of stroke, transient ischemic attack, or peripheral vascular disease – it is far and away worth it to prescribe these classes of medications.”
Indeed, the American Diabetes Association and the European Association for the Study of Diabetes’ most recent guidelines now call for a GLP-1 receptor agonist – instead of insulin – to be the first injectable used to treat type 2 diabetes (Diabetes Care 2018 Dec; 41[12]:2669-701).
“For the relatively small number of my patients who have been able to access and use these medications for months or longer, more have tolerated the GLP-1 agonists than SGLT2 inhibitors primarily due to urinary issues,” noted Dr. Hopkins.
Dipeptidyl peptidase–4 inhibitors are another option in patients with type 2 diabetes, but research suggests they may not be a top option for patients with cardiovascular risk. A 2018 review noted that cardiovascular outcome trials for alogliptin (Nesina), saxagliptin (Onglyza), and sitagliptin (Januvia) showed noninferiority but failed to demonstrate any superiority, compared with placebo in patients with type 2 diabetes mellitus and high cardiovascular risk (Circ Res. 2018 May 11;122[10]:1439-59).
The combination therapies
Many of the newer drugs are available as combinations with other types of diabetes drugs. In some cases, physicians create their own form of combination therapy by separately prescribing two or more diabetes drugs. Earlier this year, a study suggested the benefits of this kind of add-on therapy: Diabetes outcomes improved in patients who took the GLP-1 receptor agonist semaglutide and an SGLT2 inhibitor (Lancet Diabetes Endocrinol. 2019 Mar 1. doi: 10.1016/S2213-8587[19]30066-X).
Dr. Roberts suggested caution, however, when prescribing combination therapies. “My recommendation is always to begin with the individual medications to see if the patient tolerates the drugs and then decide which component needs to be titrated. It’s hard to titrate a combination drug, and it doesn’t leave a lot of flexibility. You never know which drug is doing what.
Dr. Handelsman said some patients may need to take three medications such as metformin, an SGLT2 inhibitor, and a GLP-1 receptor agonist.
“I don’t recommend using the combinations if you’re not familiar with the drugs ... These are relatively new pharmaceuticals, and most of us are on a learning curve as to how they fit into the armamentarium. If a drug is tolerated with a good response, you can certainly consider going to the combination tablets,” he added.
There is at least one drug that combines these three classes: The newly FDA-approved Qternmet XR, which combines dapagliflozin (an SGLT2 inhibitor), saxagliptin (a GLP-1 receptor agonist), and metformin. As of mid-June 2019, it was not yet available in the United States. Its sister drug Qtern, which combines dapagliflozin and saxagliptin, costs more than $500 a month with a free coupon, according to goodrx.com. In contrast, metformin is extremely inexpensive, costing just a few dollars a month for a common starting dose.
What about adding insulin?
“Both [SGLT2 inhibitors and GLP-1 receptor agonists] work very well with insulin,” Dr. Handelsman said. “There is a nice additive effect on the reduction of [hemoglobin] A1c. The only caution is that, although neither SGLT2 inhibitors nor GLP-1 receptor agonists cause hypoglycemia, in combination with insulin they do increase the risk of hypoglycemia. You may have to adjust the dose of insulin.”
Dr. Hopkins warned that cost becomes an even bigger issue when you add insulin into the mix.
“When insulin comes into the discussion, we are again stuck with astronomical costs which many struggle to afford,” he explained.
Indeed, the price tag on these drugs seems to be the biggest problem physicians have with them.
“The challenges in managing patients with diabetes aren’t the risks associated with the drugs. It’s dealing with their insurers,” noted Dr. Roberts.
Dr. Hopkins, Dr. Paauw, Dr. Roberts, and Dr. Syed reported no disclosures. Dr. Buse is an investigator for Johnson and Johnson. Dr. Goldschmidt is paid to speak by Novartis. Dr. Handelsman reported research grants, consulting work, and speaker honoraria from Amgen, Gilead, Lilly, Merck, Novo Nordisk, and others. Dr Skolnik reported nonfinancial support from AstraZeneca, Boehringer Ingelheim, Sanofi, and GlaxoSmithKline and personal fees from AstraZeneca, Boehringer Ingelheim, and Eli Lilly. He also serves on the advisory boards of AstraZeneca, Boehringer Ingelheim, Teva Pharmaceutical, Eli Lilly, Sanofi, Janssen Pharmaceuticals, Intarcia, Mylan, and GlaxoSmithKline.
Dr. Paauw and Dr. Skolnik are columnists for Family Practice News and Internal Medicine News.
M. Alexander Otto contributed to this report.
The options for treating type 2 diabetes without insulin have grown beyond metformin to include a long list of sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagonlike peptide–1 (GLP-1) receptor agonists that can be taken with or without metformin. These new drugs have cardiovascular and kidney benefits and help with weight loss, but they also carry risks and, according to some experts, their costs can be prohibitively expensive.
Given the medical community’s long-term experience with treating patients with metformin, and metformin’s lower cost, most of the physicians interviewed for this article advise using SGLT2 inhibitors and GLP-1 receptor agonists as second-line treatments. Others said that they would prefer to use the newer drugs as first-line therapies in select high-risk patients, but prior authorization hurdles created by insurance companies make that approach too burdensome.
“The economics of U.S. health care is stacked against many of our patients with diabetes in the current era,” Robert H. Hopkins Jr., MD, said in an interview.
Even when their insurance approves the drugs, patients still may not be able to afford the copay, explained Dr. Hopkins, professor of internal medicine and pediatrics and director of the division of general internal medicine at the University of Arkansas for Medical Sciences, Little Rock. “Sometimes patients can purchase drugs at a lower cost than the copay to purchase with the ‘drug coverage’ in their insurance plan – unfortunately, this is not the case with the newer diabetes medications we are discussing here.”
“SGLT2 inhibitors and GLP-1 agonists can cost several hundred dollars a month, and insurers often balk at paying for them. They’ll say, ‘Have you tried metformin?’ ” explained endocrinologist Victor Lawrence Roberts, MD, in a interview. “We have to work with insurance companies the best we can in a stepwise fashion.”
According to Dr. Roberts, 80% of his patients with diabetes struggle with the cost of medicine in general. “They’re either underinsured or not insured or their formulary is limited.
Douglas S. Paauw, MD, agreed in an interview that the newer drugs can be problematic on the insurance front.
“For some patients they aren’t affordable, especially for the uninsured if you can’t get them on an assistance program,” said Dr. Paauw, who is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the university.
Dr. Hopkins, who is on the Internal Medicine News board, noted that “unfortunately, the treatment of type 2 diabetes in patients who cannot achieve control with metformin, diet, weight control, and exercise is a story of the ‘haves’ and the ‘have nots.’ The ‘haves’ are those who have pharmacy benefits which make access to newer agents like SGLT2 inhibitors and GLP-1 agonists a possibility.”
“I have had very few of the ‘have nots’ who have been able to even consider these newer agents, which carry price tags of $600-$1,300 a month even with the availability of discounting coupons in the marketplace,” he added. “Most of these patients end up requiring a sulfonylurea or TZD [thiazolidinedione] as a second agent to achieve glycemic control. This makes it very difficult to achieve sufficient weight and metabolic control to avoid an eventual switch to insulin.”
Fatima Z. Syed, MD, an endocrine-trained general internist at DukeHealth in Durham, N.C., said she prescribes SGLT2 inhibitors and GLP-1 receptor agonists in combination with metformin. “I prescribe them frequently, but they are not first-line treatments,” she explained.
“Nothing replaces diet and exercise” as therapy for patients with type 2 diabetes, she added.
Neil S. Skolnik, MD, said that insurance companies were not preventing patients from using these drugs in his experience. He also provided an optimistic take on the accessibility of these drugs in the near future.
“Most insurance companies are now covering select SGLT2 inhibitors and GLP-1 receptor agonists for appropriate patients and those companies that currently do not will soon have to,” said Dr. Skolnik, who is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
“The outcomes [associated with use of the new drugs] are robust, the benefits are large, and are well worth the cost,” he added.
The side effects
While others praised these drugs for their beneficial effects, they also noted that the side effects of these drugs are serious and must be discussed with patients.
GLP-1 receptor agonists are linked to gastrointestinal symptoms, especially nausea, while SGLT2 inhibitors have been linked to kidney failure, ketoacidosis, and more. The Food and Drug Administration warned in 2018 that the SGLT2 inhibitors can cause a rare serious infection known as Fournier’s gangrene – necrotizing fasciitis of the perineum.
“We have to tell our patients to let us know right away if they get pain or swelling in the genital area,” Dr. Paauw, who is on the Internal Medicine News board, noted. “The chance that an infection could explode quickly is higher in those who take these drugs.”
Amputation risks also are associated with taking the SGLT2 inhibitor canagliflozin (Invokana). The FDA requires the manufacturer of this drug to include a black-box warning about the risk of “lower-limb amputations, most frequently of the toe and midfoot,” but also the leg. In approval trials, the risk doubled versus placebo.
These amputation risks “put a damper on some of the enthusiasm on behalf of physicians and patients ... for taking this drug,” noted Dr. Roberts, who is a professor of internal medicine at the University of Central Florida, Orlando.
While a manufacturer-funded study released last year found no link to amputations, the results weren’t powerful enough to rule out a moderately increased risk.
“[If] you are at high risk for having an amputation, we really have to take this risk very seriously,” said John B. Buse, MD, chief of the division of endocrinology at the University of North Carolina at Chapel Hill, in a presentation about the study at the 2018 annual scientific sessions of the American Diabetes Association.
The benefits
Despite these risks of adverse events, most interviewed agreed that the many benefits observed in those taking SGLT2 inhibitors or GLP-1 receptor agonists make them worth prescribing, at least to those who are able to afford them.
Both SGLT2 inhibitors and GLP-1 receptor agonists appear to have significant cardiovascular benefits. A 2019 meta-analysis and systematic review found that both drugs reduced major adverse cardiac events by about 12% (Circulation. 2019 Apr 23;139[17]:2022-31).
“They don’t cause hypoglycemia, they lower blood pressure, they don’t cause weight gain, and they might promote weight loss,” noted Dr. Paauw.
SGLT2 inhibitors also have shown signs of kidney benefits. The CREDENCE trial linked canagliflozin to a lowering of kidney disorders versus placebo (N Engl J Med. 2019 Jun 13;380[24]:2295-306). “The relative risk of the renal-specific composite of end-stage kidney disease, a doubling of the creatinine level, or death from renal causes was lower by 34% (hazard ratio, 0.66; 95% confidence interval, 0.53-0.81; P less than .001), and the relative risk of end-stage kidney disease was lower by 32% (HR, 0.68; 95% CI, 0.54-0.86; P = .002),” the trial investigators wrote.
“They showed very nicely that the drug improved the kidney function of those patients and reduced the kidney deterioration,” said Yehuda Handelsman, MD, an endocrinologist in Tarzana, Calif., who chaired the 2011 and 2015 American Association of Clinical Endocrinologists’ Comprehensive Diabetes Guidelines. The study was especially impressive, he added, because it included patients with low kidney function.
SGLT2 inhibitors’ “diuretic mechanism explains why there is a substantial reduction in heart failure hospitalizations in patients who take these drugs,” said cardiologist Marc E. Goldschmidt, MD, director of the Heart Success Program at Atlantic Health System’s Morristown (N.J.) Medical Center, in an interview. “Both the EMPA-REG Outcome and the CREDENCE trials demonstrated substantial benefit of this class of medications by showing a lower risk of cardiovascular death as well as death from any cause and a lower risk of hospitalization for heart failure."
Overall, the SGLT2 trial data have been very consistent with a benefit for cardiovascular risk reduction, particularly in regard to heart failure hospitalizations and even in potentially preventing heart failure in diabetics,” he added.
Dr. Skolnik, a columnist for Family Practice News, cited SGLT2 inhibitors and GLP-1 receptor agonists’ ability to slow renal disease progression, promote weight loss, and prevent poor cardiac outcomes.“These drugs should be used, in addition to metformin, in all patients with diabetes and vascular disease. These proven outcomes are far better than we ever were able to achieve previously and the strength of the evidence at this point is very strong,” said Dr. Skolnik. “In addition to the benefits of decreasing the development of cardiovascular disease, serious heart failure, and slowing progression of renal disease, these two classes of medication have additional benefits. Both classes help patients lose weight, which is very different from what was found with either sulfonylureas or insulin, which cause patients to gain weight. Also both the SGLT2 inhibitors and the GLP-1 RAs [receptor agonists] have a low incidence of hypoglycemia. For all these reasons, these have become important medications for us to use in primary care.”
Other recent trials offer “very powerful data” about SGLT2 inhibitors, Dr. Roberts said. That’s good news, since “our approach needs to be toward cardiovascular protection and preservation as well as managing blood sugar.”An Israeli trial, whose results were released in May 2019 at the annual meeting of the American College of Cardiology, found that, compared with other glucose-lowering drugs, taking an SGLT2 inhibitor was associated with lower risks of heart failure hospitalization and all-cause mortality (HR, 0.54; 95% CI, 0.44-0.65; P less than .001). This trial also offered a new detail: The patients gained the benefit regardless of whether their baseline left ventricular ejection fraction was preserved or reduced (J Coll Cardiol. 2019 Mar;73[9]:suppl 1). The SGLT2 inhibitors used in this trial included dapagliflozin (Farxiga) and empagliflozin (Jardiance).
In another study released this year, a subanalysis of the DECLARE-TIMI 58 trial, researchers reported that the SGLT2 inhibitor dapagliflozin reduced risks of both major adverse cardiovascular events and heart failure hospitalization in the subset of patients with type 2 diabetes and prior myocardial infarction versus controls (Circulation. 2019 May 28;139[22]:2516-27). The absolute risk reduction for major adverse cardiovascular events was 1.9% (HR, 0.81; 95% CI, 0.65-1.00; P = .046), while it was 0.6% for heart failure hospitalization (HR, 0.85; 95% CI, 0.72-1.00; P = .055).
These and other studies “speak volumes about the efficacy of managing blood sugar and addressing our biggest nemesis, which is cardiovascular disease,” Dr. Roberts said. “It’s irrefutable. The data [are] very good.”
Dr. Paauw said an SGLT2 inhibitor or GLP-1 receptor agonist is best reserved for use in select patients with cardiovascular risks and type 2 diabetes that need management beyond metformin.
For example, they might fit a 70-year-old with persistent hypertension who’s already taking a couple of blood pressure medications. “If they have another cardiovascular risk factor, the cardiovascular protection piece will be a bigger deal,” he said. Also, “it will probably help lower their blood pressure so they can avoid taking another blood pressure medicine.”
Trials of both GLP-1 receptor agonists and SGLT2 inhibitors have shown benefits “in improving [major adverse cardiac events], with the SGLT2 class showing substantial benefit in improving both heart failure and renal outcomes as well,” noted Dr. Skolnik. “It is in this context that one must address the question of whether the price of the medications are worthwhile. With such substantial benefit, there is no question in my mind that – for patients who have underlying cardiovascular illness, which includes patients with existent coronary disease, history of stroke, transient ischemic attack, or peripheral vascular disease – it is far and away worth it to prescribe these classes of medications.”
Indeed, the American Diabetes Association and the European Association for the Study of Diabetes’ most recent guidelines now call for a GLP-1 receptor agonist – instead of insulin – to be the first injectable used to treat type 2 diabetes (Diabetes Care 2018 Dec; 41[12]:2669-701).
“For the relatively small number of my patients who have been able to access and use these medications for months or longer, more have tolerated the GLP-1 agonists than SGLT2 inhibitors primarily due to urinary issues,” noted Dr. Hopkins.
Dipeptidyl peptidase–4 inhibitors are another option in patients with type 2 diabetes, but research suggests they may not be a top option for patients with cardiovascular risk. A 2018 review noted that cardiovascular outcome trials for alogliptin (Nesina), saxagliptin (Onglyza), and sitagliptin (Januvia) showed noninferiority but failed to demonstrate any superiority, compared with placebo in patients with type 2 diabetes mellitus and high cardiovascular risk (Circ Res. 2018 May 11;122[10]:1439-59).
The combination therapies
Many of the newer drugs are available as combinations with other types of diabetes drugs. In some cases, physicians create their own form of combination therapy by separately prescribing two or more diabetes drugs. Earlier this year, a study suggested the benefits of this kind of add-on therapy: Diabetes outcomes improved in patients who took the GLP-1 receptor agonist semaglutide and an SGLT2 inhibitor (Lancet Diabetes Endocrinol. 2019 Mar 1. doi: 10.1016/S2213-8587[19]30066-X).
Dr. Roberts suggested caution, however, when prescribing combination therapies. “My recommendation is always to begin with the individual medications to see if the patient tolerates the drugs and then decide which component needs to be titrated. It’s hard to titrate a combination drug, and it doesn’t leave a lot of flexibility. You never know which drug is doing what.
Dr. Handelsman said some patients may need to take three medications such as metformin, an SGLT2 inhibitor, and a GLP-1 receptor agonist.
“I don’t recommend using the combinations if you’re not familiar with the drugs ... These are relatively new pharmaceuticals, and most of us are on a learning curve as to how they fit into the armamentarium. If a drug is tolerated with a good response, you can certainly consider going to the combination tablets,” he added.
There is at least one drug that combines these three classes: The newly FDA-approved Qternmet XR, which combines dapagliflozin (an SGLT2 inhibitor), saxagliptin (a GLP-1 receptor agonist), and metformin. As of mid-June 2019, it was not yet available in the United States. Its sister drug Qtern, which combines dapagliflozin and saxagliptin, costs more than $500 a month with a free coupon, according to goodrx.com. In contrast, metformin is extremely inexpensive, costing just a few dollars a month for a common starting dose.
What about adding insulin?
“Both [SGLT2 inhibitors and GLP-1 receptor agonists] work very well with insulin,” Dr. Handelsman said. “There is a nice additive effect on the reduction of [hemoglobin] A1c. The only caution is that, although neither SGLT2 inhibitors nor GLP-1 receptor agonists cause hypoglycemia, in combination with insulin they do increase the risk of hypoglycemia. You may have to adjust the dose of insulin.”
Dr. Hopkins warned that cost becomes an even bigger issue when you add insulin into the mix.
“When insulin comes into the discussion, we are again stuck with astronomical costs which many struggle to afford,” he explained.
Indeed, the price tag on these drugs seems to be the biggest problem physicians have with them.
“The challenges in managing patients with diabetes aren’t the risks associated with the drugs. It’s dealing with their insurers,” noted Dr. Roberts.
Dr. Hopkins, Dr. Paauw, Dr. Roberts, and Dr. Syed reported no disclosures. Dr. Buse is an investigator for Johnson and Johnson. Dr. Goldschmidt is paid to speak by Novartis. Dr. Handelsman reported research grants, consulting work, and speaker honoraria from Amgen, Gilead, Lilly, Merck, Novo Nordisk, and others. Dr Skolnik reported nonfinancial support from AstraZeneca, Boehringer Ingelheim, Sanofi, and GlaxoSmithKline and personal fees from AstraZeneca, Boehringer Ingelheim, and Eli Lilly. He also serves on the advisory boards of AstraZeneca, Boehringer Ingelheim, Teva Pharmaceutical, Eli Lilly, Sanofi, Janssen Pharmaceuticals, Intarcia, Mylan, and GlaxoSmithKline.
Dr. Paauw and Dr. Skolnik are columnists for Family Practice News and Internal Medicine News.
M. Alexander Otto contributed to this report.
BMI screening trigger for type 2 diabetes is unreliable for at-risk black, Hispanic adults
SAN FRANCISCO – according to findings presented at the annual scientific sessions of the American Diabetes Association.
The conclusions come from a review of 5,656 participants aged 45-84 years in the Multi-Ethnic Study of Atherosclerosis (MESA), an ongoing prospective cohort study. The participants had no signs of cardiovascular disease at enrollment.
The goal of the study reported at the meeting was to see if current ADA screening guidelines are appropriate across racial groups in an increasingly diverse United States. The guidelines recommend body mass index (BMI) as a trigger for screening for type 2 diabetes. The current advice is to screen any adult who has a BMI at or above 25 kg/m2 (23 kg/m2 for Asian Americans) and at least one risk factor for type 2 diabetes, such as hypertension, dyslipidemia, or physical inactivity.
Being black, Asian American, Hispanic, Pacific Islander, or American Indian is itself a risk factor, so “someone from a minority group just needs to meet the BMI criteria,” said lead investigator Luis Rodriguez, a PhD candidate in epidemiology at the University of California, San Francisco.
He and his colleagues focused on 2,383 white, 653 Chinese American, 1,459 black, and 1,161 Hispanic participants in MESA who did not have type 2 diabetes at baseline. Participants were in their early 60s at baseline, on average, and just more than half of them were women. They had five medical exams between 2000 and 2012. The investigators calculated the BMI at which each group hit a 10% risk of developing diabetes within the next 10 years.
In general, the lines crossed at a BMI of about 23 kg/m2 for Chinese Americans; 25 kg/m2 for black and Hispanic participants; and 27 kg/m2 for white participants, which is consistent with ADA advice. The guideline cut points are “appropriate for population-based screening where you may not know if the person in front of you has any diabetes risk factors,” Mr. Rodriguez said.
With known risk factors, however, BMI didn’t hold up. Black participants with one or more risk factor hit the 10% mark at a BMI of 24.7 kg/m2, Hispanics at 23.8 kg/m2, and Chinese Americans at 21.7 kg/m2, all of which are below the recommended cut-points.
“Almost 80%-90% of participants” in minority groups “who had one or more risk factors were above the 10% threshold, so if they have at least one factor, they should pretty much be screened for diabetes, regardless of BMI,” he said.
The 25-kg/m2 threshold worked for white participants; the investigators found that with one or more risk factors, white participants crossed the 10% line at a BMI of 26.2 kg/m2. In addition, white participants with no diabetes risk factors crossed the 10% mark at around a BMI of 30 kg/m2, which the investigators suggested as an appropriate screening trigger.
Participants were in their early 60s at baseline, on average, and just more than half of them were women. In all, 696 cases of type 2 diabetes were diagnosed over a median follow-up of about 9 years, which translated to an incidence rate of 11 cases per 1,000 person-years in white participants, 16 cases for Chinese Americans, 21 for black participants, and 22 for Hispanic participants. Well over half of the participants were overweight or obese at baseline, including about 80% of black and Hispanic participants.
The sample size reported in the abstract was smaller than that in the final presentation because the investigators did not adjust for diet in the final presentation, Mr. Rodriguez explained. Because some study participants did not report diet, by excluding diet from the model adjustment, the number of participants increased, as reflected in this text. Adjusting for diet did not alter the findings.
The National Heart, Lung, and Blood Institute sponsors MESA. Mr. Rodriguez was supported by a grant from the National Institutes of Health/National Institute of Diabetes and Kidney Disease. The other investigators reported having no disclosures.
SOURCE: Rodriguez L et al. ADA 2019, Abstract 115-OR.
SAN FRANCISCO – according to findings presented at the annual scientific sessions of the American Diabetes Association.
The conclusions come from a review of 5,656 participants aged 45-84 years in the Multi-Ethnic Study of Atherosclerosis (MESA), an ongoing prospective cohort study. The participants had no signs of cardiovascular disease at enrollment.
The goal of the study reported at the meeting was to see if current ADA screening guidelines are appropriate across racial groups in an increasingly diverse United States. The guidelines recommend body mass index (BMI) as a trigger for screening for type 2 diabetes. The current advice is to screen any adult who has a BMI at or above 25 kg/m2 (23 kg/m2 for Asian Americans) and at least one risk factor for type 2 diabetes, such as hypertension, dyslipidemia, or physical inactivity.
Being black, Asian American, Hispanic, Pacific Islander, or American Indian is itself a risk factor, so “someone from a minority group just needs to meet the BMI criteria,” said lead investigator Luis Rodriguez, a PhD candidate in epidemiology at the University of California, San Francisco.
He and his colleagues focused on 2,383 white, 653 Chinese American, 1,459 black, and 1,161 Hispanic participants in MESA who did not have type 2 diabetes at baseline. Participants were in their early 60s at baseline, on average, and just more than half of them were women. They had five medical exams between 2000 and 2012. The investigators calculated the BMI at which each group hit a 10% risk of developing diabetes within the next 10 years.
In general, the lines crossed at a BMI of about 23 kg/m2 for Chinese Americans; 25 kg/m2 for black and Hispanic participants; and 27 kg/m2 for white participants, which is consistent with ADA advice. The guideline cut points are “appropriate for population-based screening where you may not know if the person in front of you has any diabetes risk factors,” Mr. Rodriguez said.
With known risk factors, however, BMI didn’t hold up. Black participants with one or more risk factor hit the 10% mark at a BMI of 24.7 kg/m2, Hispanics at 23.8 kg/m2, and Chinese Americans at 21.7 kg/m2, all of which are below the recommended cut-points.
“Almost 80%-90% of participants” in minority groups “who had one or more risk factors were above the 10% threshold, so if they have at least one factor, they should pretty much be screened for diabetes, regardless of BMI,” he said.
The 25-kg/m2 threshold worked for white participants; the investigators found that with one or more risk factors, white participants crossed the 10% line at a BMI of 26.2 kg/m2. In addition, white participants with no diabetes risk factors crossed the 10% mark at around a BMI of 30 kg/m2, which the investigators suggested as an appropriate screening trigger.
Participants were in their early 60s at baseline, on average, and just more than half of them were women. In all, 696 cases of type 2 diabetes were diagnosed over a median follow-up of about 9 years, which translated to an incidence rate of 11 cases per 1,000 person-years in white participants, 16 cases for Chinese Americans, 21 for black participants, and 22 for Hispanic participants. Well over half of the participants were overweight or obese at baseline, including about 80% of black and Hispanic participants.
The sample size reported in the abstract was smaller than that in the final presentation because the investigators did not adjust for diet in the final presentation, Mr. Rodriguez explained. Because some study participants did not report diet, by excluding diet from the model adjustment, the number of participants increased, as reflected in this text. Adjusting for diet did not alter the findings.
The National Heart, Lung, and Blood Institute sponsors MESA. Mr. Rodriguez was supported by a grant from the National Institutes of Health/National Institute of Diabetes and Kidney Disease. The other investigators reported having no disclosures.
SOURCE: Rodriguez L et al. ADA 2019, Abstract 115-OR.
SAN FRANCISCO – according to findings presented at the annual scientific sessions of the American Diabetes Association.
The conclusions come from a review of 5,656 participants aged 45-84 years in the Multi-Ethnic Study of Atherosclerosis (MESA), an ongoing prospective cohort study. The participants had no signs of cardiovascular disease at enrollment.
The goal of the study reported at the meeting was to see if current ADA screening guidelines are appropriate across racial groups in an increasingly diverse United States. The guidelines recommend body mass index (BMI) as a trigger for screening for type 2 diabetes. The current advice is to screen any adult who has a BMI at or above 25 kg/m2 (23 kg/m2 for Asian Americans) and at least one risk factor for type 2 diabetes, such as hypertension, dyslipidemia, or physical inactivity.
Being black, Asian American, Hispanic, Pacific Islander, or American Indian is itself a risk factor, so “someone from a minority group just needs to meet the BMI criteria,” said lead investigator Luis Rodriguez, a PhD candidate in epidemiology at the University of California, San Francisco.
He and his colleagues focused on 2,383 white, 653 Chinese American, 1,459 black, and 1,161 Hispanic participants in MESA who did not have type 2 diabetes at baseline. Participants were in their early 60s at baseline, on average, and just more than half of them were women. They had five medical exams between 2000 and 2012. The investigators calculated the BMI at which each group hit a 10% risk of developing diabetes within the next 10 years.
In general, the lines crossed at a BMI of about 23 kg/m2 for Chinese Americans; 25 kg/m2 for black and Hispanic participants; and 27 kg/m2 for white participants, which is consistent with ADA advice. The guideline cut points are “appropriate for population-based screening where you may not know if the person in front of you has any diabetes risk factors,” Mr. Rodriguez said.
With known risk factors, however, BMI didn’t hold up. Black participants with one or more risk factor hit the 10% mark at a BMI of 24.7 kg/m2, Hispanics at 23.8 kg/m2, and Chinese Americans at 21.7 kg/m2, all of which are below the recommended cut-points.
“Almost 80%-90% of participants” in minority groups “who had one or more risk factors were above the 10% threshold, so if they have at least one factor, they should pretty much be screened for diabetes, regardless of BMI,” he said.
The 25-kg/m2 threshold worked for white participants; the investigators found that with one or more risk factors, white participants crossed the 10% line at a BMI of 26.2 kg/m2. In addition, white participants with no diabetes risk factors crossed the 10% mark at around a BMI of 30 kg/m2, which the investigators suggested as an appropriate screening trigger.
Participants were in their early 60s at baseline, on average, and just more than half of them were women. In all, 696 cases of type 2 diabetes were diagnosed over a median follow-up of about 9 years, which translated to an incidence rate of 11 cases per 1,000 person-years in white participants, 16 cases for Chinese Americans, 21 for black participants, and 22 for Hispanic participants. Well over half of the participants were overweight or obese at baseline, including about 80% of black and Hispanic participants.
The sample size reported in the abstract was smaller than that in the final presentation because the investigators did not adjust for diet in the final presentation, Mr. Rodriguez explained. Because some study participants did not report diet, by excluding diet from the model adjustment, the number of participants increased, as reflected in this text. Adjusting for diet did not alter the findings.
The National Heart, Lung, and Blood Institute sponsors MESA. Mr. Rodriguez was supported by a grant from the National Institutes of Health/National Institute of Diabetes and Kidney Disease. The other investigators reported having no disclosures.
SOURCE: Rodriguez L et al. ADA 2019, Abstract 115-OR.
REPORTING FROM ADA 2019
Key clinical point:
Major finding: Black participants with one or more risk factors had a 10% or greater risk of type 2 diabetes at a BMI of 24.7 kg/m2; Hispanic participants had the same risk at 23.8 kg/m2; and Chinese Americans at 21.7 kg/mg2, all of which are below the BMI cut points recommended by the ADA.
Study details: Review of 5,656 participants in the Multi-Ethnic Study of Atherosclerosis .
Disclosures: The National Heart, Lung, and Blood Institute sponsors MESA. Mr. Rodriguez was supported by grant from the National Institutes of Health/National Institute of Diabetes and Kidney Disease. The other investigators reported having no disclosures.
Source: Rodriguez L et al. ADA 2019, Abstract 115-OR.
Low-fat dairy associated with decreased risk of type 2 diabetes
SAN FRANCISCO – in a review of almost 200,000 participants presented at the annual scientific sessions at the American Diabetes Association.
Increasing yogurt consumption was also independently associated with a moderately lower risk of type 2 diabetes, and increasing cheese consumption with a moderately higher risk.
It might have been that yogurt and low-fat milk were simply indicators of healthier living and that cheese consumption – in the study, most commonly on pizza or as processed slices on cheeseburgers – indicated a less healthy way of life, but “we tried our best to control for confounders,” said study lead Jean-Philippe Drouin-Chartier, PhD, of the Harvard School of Public Health, Boston.
And it is possible, he said, that lactic acid bacteria in yogurt could have some effect on the gut microbiome that protects against type 2 disease.
Total dairy consumption has not changed much over the past few decades, but people are drinking less milk and eating more cheese and yogurt. Dr. Drouin-Chartier and colleagues wondered how that affected the risk of type 2 diabetes.
The investigators correlated changes in dairy consumption during 4-year intervals with the incidence of type 2 diabetes in subsequent 4-year intervals using three large, prospective cohort studies that all started about 30 years ago: the Health Professionals Follow-Up Study, Nurses’ Health Study I, and Nurses’ Health Study II.
There were almost 200,000 participants in the pooled analysis, with 2.9 million person-years of follow-up and 12,007 new cases of type 2 diabetes. Participants completed food-frequency questionnaires every 4 years. About 82% of the participants were women. At baseline, they reported consuming about one to four servings of dairy a day.
After adjustment for race, body mass index, calorie intake, family history, physical activity, and other factors associated with type 2 diabetes, the investigators found that increasing yogurt intake by one 4-ounce serving a day while decreasing cheese intake by one 1-ounce serving a day was associated with a 16% (95% confidence interval, 10%-22%) reduction in subsequent risk of type 2 disease. There was an 11% (95% CI, 7%-15%) reduction in risk when a cheese serving was subbed out for a daily 8-ounce serving of reduced-fat milk.
An extra 2 ounces of yogurt a day was associated with a 13% (95% CI, 6%-19%) lower risk of type 2 diabetes, compared with stable consumption, while an extra half ounce of cheese was associated with an 8% (95% CI, 2%-16%) increase in risk.
Overall, substitution of low-fat products (such as 0%-2% milk and low-fat cheese, yogurt, or sherbet) for high-fat products (such as whole milk, ice cream, and high-fat cheese) was associated with a 4% decrease in risk (hazard ratio, 0.96; 95% CI, 0.93-0.99).
However, substitution of reduced-fat milk for whole milk or low-fat cheese for high-fat cheese did not influence the risk, possibly because there is actually not much difference in fat content, Dr. Drouin-Chartier said.
The National Institutes of Health funded the study. Dr. Drouin-Chartier has served as a speaker and consultant for Dairy Farmers of Canada, one other author has advised the group, another has advised the U.S. Department of Agriculture, and the remaining authors had no disclosures.
SOURCE: Drouin-Chartier J et al. ADA 2019, Abstract 159-OR.
SAN FRANCISCO – in a review of almost 200,000 participants presented at the annual scientific sessions at the American Diabetes Association.
Increasing yogurt consumption was also independently associated with a moderately lower risk of type 2 diabetes, and increasing cheese consumption with a moderately higher risk.
It might have been that yogurt and low-fat milk were simply indicators of healthier living and that cheese consumption – in the study, most commonly on pizza or as processed slices on cheeseburgers – indicated a less healthy way of life, but “we tried our best to control for confounders,” said study lead Jean-Philippe Drouin-Chartier, PhD, of the Harvard School of Public Health, Boston.
And it is possible, he said, that lactic acid bacteria in yogurt could have some effect on the gut microbiome that protects against type 2 disease.
Total dairy consumption has not changed much over the past few decades, but people are drinking less milk and eating more cheese and yogurt. Dr. Drouin-Chartier and colleagues wondered how that affected the risk of type 2 diabetes.
The investigators correlated changes in dairy consumption during 4-year intervals with the incidence of type 2 diabetes in subsequent 4-year intervals using three large, prospective cohort studies that all started about 30 years ago: the Health Professionals Follow-Up Study, Nurses’ Health Study I, and Nurses’ Health Study II.
There were almost 200,000 participants in the pooled analysis, with 2.9 million person-years of follow-up and 12,007 new cases of type 2 diabetes. Participants completed food-frequency questionnaires every 4 years. About 82% of the participants were women. At baseline, they reported consuming about one to four servings of dairy a day.
After adjustment for race, body mass index, calorie intake, family history, physical activity, and other factors associated with type 2 diabetes, the investigators found that increasing yogurt intake by one 4-ounce serving a day while decreasing cheese intake by one 1-ounce serving a day was associated with a 16% (95% confidence interval, 10%-22%) reduction in subsequent risk of type 2 disease. There was an 11% (95% CI, 7%-15%) reduction in risk when a cheese serving was subbed out for a daily 8-ounce serving of reduced-fat milk.
An extra 2 ounces of yogurt a day was associated with a 13% (95% CI, 6%-19%) lower risk of type 2 diabetes, compared with stable consumption, while an extra half ounce of cheese was associated with an 8% (95% CI, 2%-16%) increase in risk.
Overall, substitution of low-fat products (such as 0%-2% milk and low-fat cheese, yogurt, or sherbet) for high-fat products (such as whole milk, ice cream, and high-fat cheese) was associated with a 4% decrease in risk (hazard ratio, 0.96; 95% CI, 0.93-0.99).
However, substitution of reduced-fat milk for whole milk or low-fat cheese for high-fat cheese did not influence the risk, possibly because there is actually not much difference in fat content, Dr. Drouin-Chartier said.
The National Institutes of Health funded the study. Dr. Drouin-Chartier has served as a speaker and consultant for Dairy Farmers of Canada, one other author has advised the group, another has advised the U.S. Department of Agriculture, and the remaining authors had no disclosures.
SOURCE: Drouin-Chartier J et al. ADA 2019, Abstract 159-OR.
SAN FRANCISCO – in a review of almost 200,000 participants presented at the annual scientific sessions at the American Diabetes Association.
Increasing yogurt consumption was also independently associated with a moderately lower risk of type 2 diabetes, and increasing cheese consumption with a moderately higher risk.
It might have been that yogurt and low-fat milk were simply indicators of healthier living and that cheese consumption – in the study, most commonly on pizza or as processed slices on cheeseburgers – indicated a less healthy way of life, but “we tried our best to control for confounders,” said study lead Jean-Philippe Drouin-Chartier, PhD, of the Harvard School of Public Health, Boston.
And it is possible, he said, that lactic acid bacteria in yogurt could have some effect on the gut microbiome that protects against type 2 disease.
Total dairy consumption has not changed much over the past few decades, but people are drinking less milk and eating more cheese and yogurt. Dr. Drouin-Chartier and colleagues wondered how that affected the risk of type 2 diabetes.
The investigators correlated changes in dairy consumption during 4-year intervals with the incidence of type 2 diabetes in subsequent 4-year intervals using three large, prospective cohort studies that all started about 30 years ago: the Health Professionals Follow-Up Study, Nurses’ Health Study I, and Nurses’ Health Study II.
There were almost 200,000 participants in the pooled analysis, with 2.9 million person-years of follow-up and 12,007 new cases of type 2 diabetes. Participants completed food-frequency questionnaires every 4 years. About 82% of the participants were women. At baseline, they reported consuming about one to four servings of dairy a day.
After adjustment for race, body mass index, calorie intake, family history, physical activity, and other factors associated with type 2 diabetes, the investigators found that increasing yogurt intake by one 4-ounce serving a day while decreasing cheese intake by one 1-ounce serving a day was associated with a 16% (95% confidence interval, 10%-22%) reduction in subsequent risk of type 2 disease. There was an 11% (95% CI, 7%-15%) reduction in risk when a cheese serving was subbed out for a daily 8-ounce serving of reduced-fat milk.
An extra 2 ounces of yogurt a day was associated with a 13% (95% CI, 6%-19%) lower risk of type 2 diabetes, compared with stable consumption, while an extra half ounce of cheese was associated with an 8% (95% CI, 2%-16%) increase in risk.
Overall, substitution of low-fat products (such as 0%-2% milk and low-fat cheese, yogurt, or sherbet) for high-fat products (such as whole milk, ice cream, and high-fat cheese) was associated with a 4% decrease in risk (hazard ratio, 0.96; 95% CI, 0.93-0.99).
However, substitution of reduced-fat milk for whole milk or low-fat cheese for high-fat cheese did not influence the risk, possibly because there is actually not much difference in fat content, Dr. Drouin-Chartier said.
The National Institutes of Health funded the study. Dr. Drouin-Chartier has served as a speaker and consultant for Dairy Farmers of Canada, one other author has advised the group, another has advised the U.S. Department of Agriculture, and the remaining authors had no disclosures.
SOURCE: Drouin-Chartier J et al. ADA 2019, Abstract 159-OR.
REPORTING FROM ADA 2019
Using Obamacare authority, Trump aims to shift dialysis care to patients’ homes
President Trump on July 10 announced a bold plan to improve care to patients with kidney disease, which he claimed would save thousands of lives each year and billions of dollars for taxpayers.
“It could be higher if it works the way we anticipate,” Mr. Trump boasted in a 25-minute speech to dozens of kidney patients, their families, and kidney care providers in Washington.
Ten Americans die each day because of the shortage of organs, Mr. Trump said.
Kidney disease is the ninth-leading cause of death in the United States and accounts for 20% of annual Medicare spending, or about $110 billion, administration officials said.
Mr. Trump’s strategy centers on changing how Medicare pays doctors and dialysis centers to boost their incentives to help patients get dialysis at home and keep them healthy enough to be eligible for transplantation. This would be a far cry from the current system, which focuses on in-patient dialysis center treatment.
Mark E. Rosenberg, MD, president of the American Society of Nephrology, said he was pleased that some of the new payment models offered by the Centers for Medicare & Medicaid Services have only “upside” potential for doctors. He said doctors now get paid more to see their patients at the dialysis center than at home. As a result, there is little incentive to promote home dialysis options.
“I have been a kidney doctor for 35 years, and this is the most game-changing thing ever to happen,” he said.
The authority to make such major changes without congressional approval comes from the Centers for Medicare and Medicaid Innovation (CMMI), which was created by the 2010 Affordable Care Act.
On Tuesday, the Trump administration was in a federal appeals court in New Orleans arguing the entire health law should be declared unconstitutional.
“If the law is invalidated, the Innovation Center, and all its authorities, would be eliminated,” said Nicholas Bagley, a University of Michigan law professor.
In touting the new effort, Health and Human Services Secretary Alex M. Azar II and CMMI Director Adam Boehler spoke about how kidney disease has affected their families. Mr. Azar noted his father was on dialysis for several years before receiving a kidney transplant. Mr. Boehler said an aunt died while on dialysis.
Since 1973, all Americans with end-stage kidney disease have been entitled to coverage through Medicare.
The administration said it would expand the number of kidneys available for transplant by increasing public awareness about the need for living donors and help those who donate a kidney. Currently, their medical costs are covered, but the president’s plan would provide financial assistance to cover day care and time missed from work. Mr. Trump said the initiative would also hold organ procurement organizations more accountable so that fewer usable organs are discarded.
Trump said his plan would help 17,000 additional Americans get a kidney transplant each year by 2030. The policy would also help 11,000 more Americans get hearts, lungs, and livers annually.
Kidney transplants cost less than having patients spend years on dialysis, according to government figures. Dialysis treatment runs on average about $89,000 a year, while a kidney transplant surgery averages about $32,000 and postsurgery care runs about $25,000 per year. Mr. Trump estimated his plan would save families and taxpayers $4.2 billion a year. “This is a dramatic and long overdue reform,” he said.
In the United States, only about 12% of patients get dialysis at home, far lower than in other countries, Mr. Trump said. The plan calls for increasing that share to 80% by 2025.
Nichole Jefferson, 47 years, of Dallas, who is awaiting a second transplant to replace a transplanted kidney that is failing, said getting the treatment at home is much less taxing. She had home dialysis for 4 years before her initial transplant in 2008.
“It’s great to be at home where I was more comfortable and more relaxed and the care was in my hands,” she said in an interview at the Trump event. By getting dialysis at night while she slept, she was able to work during the day and take part in family events.
She had to go to a center for the dialysis when the home dialysis stopped working. “I was depressed to be in the center tied to a chair for 4 hours next to people I did not know,” she said. Patients often have dialysis several days a week.
Other patient advocates applauded Mr. Trump’s plan.
“The administration’s commitment to charting a new course for kidney health will help revolutionize transplantation and dialysis and advance new innovations, therapies and treatments, which patients everywhere have been waiting on for far too long,” said Kevin Longino, CEO of the National Kidney Foundation and a kidney transplant patient.
DaVita, the Denver-based company that is the largest provider of home dialysis in the country, offered a more muted response, saying it looked forward to working with the administration. The company’s stock, which fell in recent days ahead of the announcement, rose about 5% Wednesday.
Administration officials said many aspects of their plan would begin next year. Health providers in half the country will be required to participate in one of the new payment models in which they will face some financial risk for caring for patients. Doctors and health systems will have options to take on more financial risk, which means they could make more money or lose more money based on the health of their kidney patients.
Patients, however, will continue to be able to choose their doctors and dialysis providers.
Joe Grogan, head of the White House Domestic Policy Council, said the kidney disease issue “fits in the wheelhouse of items the president likes to confront. ... The current quality of outcomes are pathetic in this area.”
About half of patients on dialysis die within 5 years, Mr. Azar said.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
President Trump on July 10 announced a bold plan to improve care to patients with kidney disease, which he claimed would save thousands of lives each year and billions of dollars for taxpayers.
“It could be higher if it works the way we anticipate,” Mr. Trump boasted in a 25-minute speech to dozens of kidney patients, their families, and kidney care providers in Washington.
Ten Americans die each day because of the shortage of organs, Mr. Trump said.
Kidney disease is the ninth-leading cause of death in the United States and accounts for 20% of annual Medicare spending, or about $110 billion, administration officials said.
Mr. Trump’s strategy centers on changing how Medicare pays doctors and dialysis centers to boost their incentives to help patients get dialysis at home and keep them healthy enough to be eligible for transplantation. This would be a far cry from the current system, which focuses on in-patient dialysis center treatment.
Mark E. Rosenberg, MD, president of the American Society of Nephrology, said he was pleased that some of the new payment models offered by the Centers for Medicare & Medicaid Services have only “upside” potential for doctors. He said doctors now get paid more to see their patients at the dialysis center than at home. As a result, there is little incentive to promote home dialysis options.
“I have been a kidney doctor for 35 years, and this is the most game-changing thing ever to happen,” he said.
The authority to make such major changes without congressional approval comes from the Centers for Medicare and Medicaid Innovation (CMMI), which was created by the 2010 Affordable Care Act.
On Tuesday, the Trump administration was in a federal appeals court in New Orleans arguing the entire health law should be declared unconstitutional.
“If the law is invalidated, the Innovation Center, and all its authorities, would be eliminated,” said Nicholas Bagley, a University of Michigan law professor.
In touting the new effort, Health and Human Services Secretary Alex M. Azar II and CMMI Director Adam Boehler spoke about how kidney disease has affected their families. Mr. Azar noted his father was on dialysis for several years before receiving a kidney transplant. Mr. Boehler said an aunt died while on dialysis.
Since 1973, all Americans with end-stage kidney disease have been entitled to coverage through Medicare.
The administration said it would expand the number of kidneys available for transplant by increasing public awareness about the need for living donors and help those who donate a kidney. Currently, their medical costs are covered, but the president’s plan would provide financial assistance to cover day care and time missed from work. Mr. Trump said the initiative would also hold organ procurement organizations more accountable so that fewer usable organs are discarded.
Trump said his plan would help 17,000 additional Americans get a kidney transplant each year by 2030. The policy would also help 11,000 more Americans get hearts, lungs, and livers annually.
Kidney transplants cost less than having patients spend years on dialysis, according to government figures. Dialysis treatment runs on average about $89,000 a year, while a kidney transplant surgery averages about $32,000 and postsurgery care runs about $25,000 per year. Mr. Trump estimated his plan would save families and taxpayers $4.2 billion a year. “This is a dramatic and long overdue reform,” he said.
In the United States, only about 12% of patients get dialysis at home, far lower than in other countries, Mr. Trump said. The plan calls for increasing that share to 80% by 2025.
Nichole Jefferson, 47 years, of Dallas, who is awaiting a second transplant to replace a transplanted kidney that is failing, said getting the treatment at home is much less taxing. She had home dialysis for 4 years before her initial transplant in 2008.
“It’s great to be at home where I was more comfortable and more relaxed and the care was in my hands,” she said in an interview at the Trump event. By getting dialysis at night while she slept, she was able to work during the day and take part in family events.
She had to go to a center for the dialysis when the home dialysis stopped working. “I was depressed to be in the center tied to a chair for 4 hours next to people I did not know,” she said. Patients often have dialysis several days a week.
Other patient advocates applauded Mr. Trump’s plan.
“The administration’s commitment to charting a new course for kidney health will help revolutionize transplantation and dialysis and advance new innovations, therapies and treatments, which patients everywhere have been waiting on for far too long,” said Kevin Longino, CEO of the National Kidney Foundation and a kidney transplant patient.
DaVita, the Denver-based company that is the largest provider of home dialysis in the country, offered a more muted response, saying it looked forward to working with the administration. The company’s stock, which fell in recent days ahead of the announcement, rose about 5% Wednesday.
Administration officials said many aspects of their plan would begin next year. Health providers in half the country will be required to participate in one of the new payment models in which they will face some financial risk for caring for patients. Doctors and health systems will have options to take on more financial risk, which means they could make more money or lose more money based on the health of their kidney patients.
Patients, however, will continue to be able to choose their doctors and dialysis providers.
Joe Grogan, head of the White House Domestic Policy Council, said the kidney disease issue “fits in the wheelhouse of items the president likes to confront. ... The current quality of outcomes are pathetic in this area.”
About half of patients on dialysis die within 5 years, Mr. Azar said.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
President Trump on July 10 announced a bold plan to improve care to patients with kidney disease, which he claimed would save thousands of lives each year and billions of dollars for taxpayers.
“It could be higher if it works the way we anticipate,” Mr. Trump boasted in a 25-minute speech to dozens of kidney patients, their families, and kidney care providers in Washington.
Ten Americans die each day because of the shortage of organs, Mr. Trump said.
Kidney disease is the ninth-leading cause of death in the United States and accounts for 20% of annual Medicare spending, or about $110 billion, administration officials said.
Mr. Trump’s strategy centers on changing how Medicare pays doctors and dialysis centers to boost their incentives to help patients get dialysis at home and keep them healthy enough to be eligible for transplantation. This would be a far cry from the current system, which focuses on in-patient dialysis center treatment.
Mark E. Rosenberg, MD, president of the American Society of Nephrology, said he was pleased that some of the new payment models offered by the Centers for Medicare & Medicaid Services have only “upside” potential for doctors. He said doctors now get paid more to see their patients at the dialysis center than at home. As a result, there is little incentive to promote home dialysis options.
“I have been a kidney doctor for 35 years, and this is the most game-changing thing ever to happen,” he said.
The authority to make such major changes without congressional approval comes from the Centers for Medicare and Medicaid Innovation (CMMI), which was created by the 2010 Affordable Care Act.
On Tuesday, the Trump administration was in a federal appeals court in New Orleans arguing the entire health law should be declared unconstitutional.
“If the law is invalidated, the Innovation Center, and all its authorities, would be eliminated,” said Nicholas Bagley, a University of Michigan law professor.
In touting the new effort, Health and Human Services Secretary Alex M. Azar II and CMMI Director Adam Boehler spoke about how kidney disease has affected their families. Mr. Azar noted his father was on dialysis for several years before receiving a kidney transplant. Mr. Boehler said an aunt died while on dialysis.
Since 1973, all Americans with end-stage kidney disease have been entitled to coverage through Medicare.
The administration said it would expand the number of kidneys available for transplant by increasing public awareness about the need for living donors and help those who donate a kidney. Currently, their medical costs are covered, but the president’s plan would provide financial assistance to cover day care and time missed from work. Mr. Trump said the initiative would also hold organ procurement organizations more accountable so that fewer usable organs are discarded.
Trump said his plan would help 17,000 additional Americans get a kidney transplant each year by 2030. The policy would also help 11,000 more Americans get hearts, lungs, and livers annually.
Kidney transplants cost less than having patients spend years on dialysis, according to government figures. Dialysis treatment runs on average about $89,000 a year, while a kidney transplant surgery averages about $32,000 and postsurgery care runs about $25,000 per year. Mr. Trump estimated his plan would save families and taxpayers $4.2 billion a year. “This is a dramatic and long overdue reform,” he said.
In the United States, only about 12% of patients get dialysis at home, far lower than in other countries, Mr. Trump said. The plan calls for increasing that share to 80% by 2025.
Nichole Jefferson, 47 years, of Dallas, who is awaiting a second transplant to replace a transplanted kidney that is failing, said getting the treatment at home is much less taxing. She had home dialysis for 4 years before her initial transplant in 2008.
“It’s great to be at home where I was more comfortable and more relaxed and the care was in my hands,” she said in an interview at the Trump event. By getting dialysis at night while she slept, she was able to work during the day and take part in family events.
She had to go to a center for the dialysis when the home dialysis stopped working. “I was depressed to be in the center tied to a chair for 4 hours next to people I did not know,” she said. Patients often have dialysis several days a week.
Other patient advocates applauded Mr. Trump’s plan.
“The administration’s commitment to charting a new course for kidney health will help revolutionize transplantation and dialysis and advance new innovations, therapies and treatments, which patients everywhere have been waiting on for far too long,” said Kevin Longino, CEO of the National Kidney Foundation and a kidney transplant patient.
DaVita, the Denver-based company that is the largest provider of home dialysis in the country, offered a more muted response, saying it looked forward to working with the administration. The company’s stock, which fell in recent days ahead of the announcement, rose about 5% Wednesday.
Administration officials said many aspects of their plan would begin next year. Health providers in half the country will be required to participate in one of the new payment models in which they will face some financial risk for caring for patients. Doctors and health systems will have options to take on more financial risk, which means they could make more money or lose more money based on the health of their kidney patients.
Patients, however, will continue to be able to choose their doctors and dialysis providers.
Joe Grogan, head of the White House Domestic Policy Council, said the kidney disease issue “fits in the wheelhouse of items the president likes to confront. ... The current quality of outcomes are pathetic in this area.”
About half of patients on dialysis die within 5 years, Mr. Azar said.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Type 2 diabetes is particularly devastating in adolescents
SAN FRANCISCO – and by the time those with youth-onset diabetes reach their early 20s, they are beset with disease-related complications usually seen in older populations, findings from the RISE and TODAY2 studies have demonstrated.
“Additional research is urgently needed to better understand the reasons for this more serious trajectory,” Philip Zeitler, MD, PhD, of Children’s Hospital Colorado, Aurora, said at the annual scientific sessions of the American Diabetes Association. The hope is to identify at-risk children and prevent the disease, but at this point “we don’t know the answer.”
In the meantime, “we are getting more aggressive with bariatric surgery at our center, because nothing else is working as well. It would be nice to move away from that, but these kids are going to die,” he added.
Steven Kahn, MD, of the diabetes Research Center at the University of Washington, Seattle, presented the findings from a comparison of outcomes from the Restoring Insulin Secretion (RISE) studies in adolescents aged 10-19 years and in adults. The RISE Pediatric Medication Study (Diabetes Care. 2018; 41[8]:1717-25) and RISE Adult Medication Study were parallel investigations treatments to preserve or improve beta-cell function.
“This is the first-ever true comparison of outcomes in youth versus adults,” he said. Both arms had the same design and lab measurements, but the differences in outcomes were “very scary,” he added. “The disease is much more aggressive in youth than in adults.”
Among other things, the RISE youth-versus-adult study compared the outcomes after 3 months of insulin glargine followed by 9 months of metformin, or 12 months of metformin in 132 obese adults and 91 obese adolescents with impaired glucose tolerance or recently diagnosed type 2 diabetes. The treatments were stopped after 12 months, and the participants were reevaluated at 15 months. Hyperglycemic clamps were conducted at baseline, 12 months, and 3 months after treatment cessation (Diabetes. 2019 Jun 9. doi: 10.2337/db19-0299).
In adults, treatment improved insulin sensitivity and beta-cell response, but after treatment cessation, they reverted to baseline by the 15-month evaluation. However, there was no improvement in insulin sensitivity and beta-cell response in adolescents, either during treatment or after cessation, and in fact, they were worse off at 15 months than they had been at baseline, with lower insulin secretion and higher hemoglobin A1c.
Those stark differences in outcomes between the adolescents and adults were indicative of a more aggressive disease trajectory for younger patients.
Compliance was not the issue, with more than 80% of both adults and children taking more than 80% of their medications, Dr. Kahn said.
He suggested that adolescents might have a different underlying pathology that makes it worse to develop diabetes during puberty, which is already an insulin-resistant state. But, whatever the case, there is an “urgent need” to better understand the differences between adolescents and adults and to find better treatments for younger patients with diabetes, he said.
In regard to using weight loss as a means of treatment or prevention, Dr. Zeitler emphasized that type 2 diabetes in younger patients “occurs in a context of very low socioeconomic status, family dysfunction, and a great deal of stress and [family] illness. It’s often a complex situation and it’s difficult to accomplish effective lifestyle change when families are struggling to have afford quality food, facing challenges of family and neighborhood violence, and working multiple jobs.”
The RISE findings of a more aggressive deterioration in beta-cell function for younger patients were reflected in outcomes in the TODAY2 study, which found that adolescents who are diagnosed with type 2 diabetes face severe renal, cardiovascular, eye, and nerve complications by the time they reach their early 20s.
TODAY2 was an 8-year follow-up to the Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) trial published in 2012 (N Engl J Med. 2012;366:2247-56). Data from the original study of patients aged 10-17 years with type 2 diabetes showed that after a roughly 4-year follow-up, almost half of all participants had experienced loss of glycemic control on their original treatment assignment, a rate much higher than that reported in adults. Metformin plus rosiglitazone was superior to metformin alone in maintaining durable glycemic control and metformin plus an intensive lifestyle intervention was intermediate to the other groups, but not significantly different from them. In addition, metformin alone was found to be least effective in non-Hispanic black patients, metformin and rosiglitazone was most effective in girls.
Overall, 517 participants of the original study’s 669 participants are still being followed as part of the TODAY2 trial. They are managed in community practices now and are in their early 20s, on average.
But, less than 10 years down the road from TODAY, the young adults “have problems you’d expect in your grandparents. Target-organ damage is already evident, and serious cardiovascular events are occurring,” Dr. Zeitler said.
Cardiovascular complications
The cardiovascular event rate in TODAY 2 was about the same as is seen in older adults with type 1 diabetes. Overall, there were 38 cardiovascular events in 19 patients for an event rate of 6.4/1,000 patients per year. Those events included heart failure, arrhythmia, coronary artery disease or myocardial infarction, deep venous thrombosis, stroke or transient ischemic attack, and vascular insufficiency.
Over that time, the cumulative incidence of elevated LDL cholesterol increased from 3% in the TODAY report to 26% for TODAY2, and for triglycerides, it went from 18% to 35%. The cumulative incidence of hypertension increased from 19% to 55%.
Decline renal function
In regard to renal complications, the cumulative incident curve for microalbuminuria went from 8% at baseline to 40% at 12 years, while macroalbuminuria prevalence increased from 1.5% to 11% during the same time. The cumulative incidence of hyperfiltration increased from 12% to 48%. Risk factors for hyperfiltration included female sex, Hispanic ethnicity, loss of glycemic control, and hypertension, although body mass index was actually associated with lower risk.
So far, there have been four renal events in two patients, who both had chronic kidney disease and end-stage renal failure, for an event rate of 0.7/1,000 patients per year.
Pregnancy outcomes
Women in the cohort – about two-thirds of the study population – have had high rates of maternal complications, and their offspring also face complications after birth.
There were 306 pregnancies reported, of which there are known outcomes for 53 (TODAY) and 236 (TODAY2). In all, 5% of the total cohort had voluntary elective termination; 9% and 12% of patients, respectively, suffered a miscarriage before 20 weeks; and 4% of pregnancies in the total cohort ended in stillbirth.
Preterm live births more than doubled from 11% to 24%, and full-term deliveries decreased from 62% to 46% in the TODAY2 patients.
In regard to offspring characteristics, average birth weight in the total cohort was just over 4.5 pounds (national average, 7.3 pounds), and the prevalence of very low birth weight more than doubled from 8% to 16% at the 12-year mark. The prevalence of macrosomia was 19% for the cohort, more than double the national average of 8%. In all, 5% and 7% of offspring were small for gestational age, whereas 22% and 26% of offspring were large for gestational age.
Among other complications, respiratory distress occurred in 8% and 14% of offspring, and cardiac anomalies occurred in 10% and 9%, which, although they held steady across the cohorts, were significantly higher than the national average of 1%. Similarly, neonatal hypoglycemia occurred in 17% and 29% of offspring, again, notably higher than the national average of 2%. Offspring outcomes were worse in mothers with loss of glycemic control.
In regard to maternal pregnancy complications, the rate of hospitalization before delivery increased from 25% to 36%; hypertension increased in prevalence from 19% to 36%; and while macroalbuminuria held steady at 9.4%, microalbuminuria increased from 6% to 8%. Thirty-three percent of the TODAY2 cohort had a hemoglobin A1c level of more than 8%.
Retinopathy
Serious eye problems were common, with notable progression seen in diabetic retinopathy in patients who had fundus photos taken in 2011 (TODAY) and 2018 (TODAY2). Among the patients, 86% and 51%, respectively, of 371 patients had no definitive diabetic retinopathy; 14% and 22% of patients had very mild nonproliferative diabetic retinopathy (NPDR); and 0% and 16% of patients had mild NPDR. None of the TODAY patients had early or high-risk proliferative diabetic retinopathy, compared with 3% and 1%, respectively, in TODAY2. Risk factors included loss of glycemic control (hazard ratio, 19.23; 95% confidence interval, 4.62-80.07).
None of the TODAY patients had macular edema, whereas it occurred in 4% of TODAY2 patients. In all, there were 142 adjudicated eye-related events reported for 92 patients, for an event rate of 15.5/1,000 patients per year. The events included NPDR, proliferative diabetic retinopathy, macular edema, cataracts, glaucoma, and vitreous hemorrhage).
Neuropathy
The prevalence of diabetic neuropathy also increased over the duration of follow-up, rising to 28%-33% based on Michigan Neuropathy Screening Instrument scores. There were 14 adjudicated events reported for 12 patients (2.4 events/1,000 patients per year), including peripheral diabetic neuropathy, autonomic neuropathy, and diabetic mononeuropathy.
“We’ve had a number of amputations; quite a number of toes are now missing in this group of kids,” Dr. Zeitler said.
There have been five deaths so far: one heart attack, one renal failure, one overwhelming sepsis, one postop cardiac arrest, and a drug overdose.
Dr. Zeitler was the senior author on 2018 updated ADA guidelines for managing youth-onset type 2 diabetes. The recommendations where extensively shaped by the TODAY findings and were more aggressive than those previously put forward, suggesting, among other things, hemoglobin A1c targets of 6.5%-7%; earlier treatment with insulin; and stricter management of hypertension, dyslipidemia, and proteinuria (Diabetes Care. 2018;41[12]:2648-68).
The National Institute of Diabetes & Kidney disease funded the studies. The presenters reported no relevant disclosures or conflicts of interest.
This article was updated 7/22/19.
SAN FRANCISCO – and by the time those with youth-onset diabetes reach their early 20s, they are beset with disease-related complications usually seen in older populations, findings from the RISE and TODAY2 studies have demonstrated.
“Additional research is urgently needed to better understand the reasons for this more serious trajectory,” Philip Zeitler, MD, PhD, of Children’s Hospital Colorado, Aurora, said at the annual scientific sessions of the American Diabetes Association. The hope is to identify at-risk children and prevent the disease, but at this point “we don’t know the answer.”
In the meantime, “we are getting more aggressive with bariatric surgery at our center, because nothing else is working as well. It would be nice to move away from that, but these kids are going to die,” he added.
Steven Kahn, MD, of the diabetes Research Center at the University of Washington, Seattle, presented the findings from a comparison of outcomes from the Restoring Insulin Secretion (RISE) studies in adolescents aged 10-19 years and in adults. The RISE Pediatric Medication Study (Diabetes Care. 2018; 41[8]:1717-25) and RISE Adult Medication Study were parallel investigations treatments to preserve or improve beta-cell function.
“This is the first-ever true comparison of outcomes in youth versus adults,” he said. Both arms had the same design and lab measurements, but the differences in outcomes were “very scary,” he added. “The disease is much more aggressive in youth than in adults.”
Among other things, the RISE youth-versus-adult study compared the outcomes after 3 months of insulin glargine followed by 9 months of metformin, or 12 months of metformin in 132 obese adults and 91 obese adolescents with impaired glucose tolerance or recently diagnosed type 2 diabetes. The treatments were stopped after 12 months, and the participants were reevaluated at 15 months. Hyperglycemic clamps were conducted at baseline, 12 months, and 3 months after treatment cessation (Diabetes. 2019 Jun 9. doi: 10.2337/db19-0299).
In adults, treatment improved insulin sensitivity and beta-cell response, but after treatment cessation, they reverted to baseline by the 15-month evaluation. However, there was no improvement in insulin sensitivity and beta-cell response in adolescents, either during treatment or after cessation, and in fact, they were worse off at 15 months than they had been at baseline, with lower insulin secretion and higher hemoglobin A1c.
Those stark differences in outcomes between the adolescents and adults were indicative of a more aggressive disease trajectory for younger patients.
Compliance was not the issue, with more than 80% of both adults and children taking more than 80% of their medications, Dr. Kahn said.
He suggested that adolescents might have a different underlying pathology that makes it worse to develop diabetes during puberty, which is already an insulin-resistant state. But, whatever the case, there is an “urgent need” to better understand the differences between adolescents and adults and to find better treatments for younger patients with diabetes, he said.
In regard to using weight loss as a means of treatment or prevention, Dr. Zeitler emphasized that type 2 diabetes in younger patients “occurs in a context of very low socioeconomic status, family dysfunction, and a great deal of stress and [family] illness. It’s often a complex situation and it’s difficult to accomplish effective lifestyle change when families are struggling to have afford quality food, facing challenges of family and neighborhood violence, and working multiple jobs.”
The RISE findings of a more aggressive deterioration in beta-cell function for younger patients were reflected in outcomes in the TODAY2 study, which found that adolescents who are diagnosed with type 2 diabetes face severe renal, cardiovascular, eye, and nerve complications by the time they reach their early 20s.
TODAY2 was an 8-year follow-up to the Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) trial published in 2012 (N Engl J Med. 2012;366:2247-56). Data from the original study of patients aged 10-17 years with type 2 diabetes showed that after a roughly 4-year follow-up, almost half of all participants had experienced loss of glycemic control on their original treatment assignment, a rate much higher than that reported in adults. Metformin plus rosiglitazone was superior to metformin alone in maintaining durable glycemic control and metformin plus an intensive lifestyle intervention was intermediate to the other groups, but not significantly different from them. In addition, metformin alone was found to be least effective in non-Hispanic black patients, metformin and rosiglitazone was most effective in girls.
Overall, 517 participants of the original study’s 669 participants are still being followed as part of the TODAY2 trial. They are managed in community practices now and are in their early 20s, on average.
But, less than 10 years down the road from TODAY, the young adults “have problems you’d expect in your grandparents. Target-organ damage is already evident, and serious cardiovascular events are occurring,” Dr. Zeitler said.
Cardiovascular complications
The cardiovascular event rate in TODAY 2 was about the same as is seen in older adults with type 1 diabetes. Overall, there were 38 cardiovascular events in 19 patients for an event rate of 6.4/1,000 patients per year. Those events included heart failure, arrhythmia, coronary artery disease or myocardial infarction, deep venous thrombosis, stroke or transient ischemic attack, and vascular insufficiency.
Over that time, the cumulative incidence of elevated LDL cholesterol increased from 3% in the TODAY report to 26% for TODAY2, and for triglycerides, it went from 18% to 35%. The cumulative incidence of hypertension increased from 19% to 55%.
Decline renal function
In regard to renal complications, the cumulative incident curve for microalbuminuria went from 8% at baseline to 40% at 12 years, while macroalbuminuria prevalence increased from 1.5% to 11% during the same time. The cumulative incidence of hyperfiltration increased from 12% to 48%. Risk factors for hyperfiltration included female sex, Hispanic ethnicity, loss of glycemic control, and hypertension, although body mass index was actually associated with lower risk.
So far, there have been four renal events in two patients, who both had chronic kidney disease and end-stage renal failure, for an event rate of 0.7/1,000 patients per year.
Pregnancy outcomes
Women in the cohort – about two-thirds of the study population – have had high rates of maternal complications, and their offspring also face complications after birth.
There were 306 pregnancies reported, of which there are known outcomes for 53 (TODAY) and 236 (TODAY2). In all, 5% of the total cohort had voluntary elective termination; 9% and 12% of patients, respectively, suffered a miscarriage before 20 weeks; and 4% of pregnancies in the total cohort ended in stillbirth.
Preterm live births more than doubled from 11% to 24%, and full-term deliveries decreased from 62% to 46% in the TODAY2 patients.
In regard to offspring characteristics, average birth weight in the total cohort was just over 4.5 pounds (national average, 7.3 pounds), and the prevalence of very low birth weight more than doubled from 8% to 16% at the 12-year mark. The prevalence of macrosomia was 19% for the cohort, more than double the national average of 8%. In all, 5% and 7% of offspring were small for gestational age, whereas 22% and 26% of offspring were large for gestational age.
Among other complications, respiratory distress occurred in 8% and 14% of offspring, and cardiac anomalies occurred in 10% and 9%, which, although they held steady across the cohorts, were significantly higher than the national average of 1%. Similarly, neonatal hypoglycemia occurred in 17% and 29% of offspring, again, notably higher than the national average of 2%. Offspring outcomes were worse in mothers with loss of glycemic control.
In regard to maternal pregnancy complications, the rate of hospitalization before delivery increased from 25% to 36%; hypertension increased in prevalence from 19% to 36%; and while macroalbuminuria held steady at 9.4%, microalbuminuria increased from 6% to 8%. Thirty-three percent of the TODAY2 cohort had a hemoglobin A1c level of more than 8%.
Retinopathy
Serious eye problems were common, with notable progression seen in diabetic retinopathy in patients who had fundus photos taken in 2011 (TODAY) and 2018 (TODAY2). Among the patients, 86% and 51%, respectively, of 371 patients had no definitive diabetic retinopathy; 14% and 22% of patients had very mild nonproliferative diabetic retinopathy (NPDR); and 0% and 16% of patients had mild NPDR. None of the TODAY patients had early or high-risk proliferative diabetic retinopathy, compared with 3% and 1%, respectively, in TODAY2. Risk factors included loss of glycemic control (hazard ratio, 19.23; 95% confidence interval, 4.62-80.07).
None of the TODAY patients had macular edema, whereas it occurred in 4% of TODAY2 patients. In all, there were 142 adjudicated eye-related events reported for 92 patients, for an event rate of 15.5/1,000 patients per year. The events included NPDR, proliferative diabetic retinopathy, macular edema, cataracts, glaucoma, and vitreous hemorrhage).
Neuropathy
The prevalence of diabetic neuropathy also increased over the duration of follow-up, rising to 28%-33% based on Michigan Neuropathy Screening Instrument scores. There were 14 adjudicated events reported for 12 patients (2.4 events/1,000 patients per year), including peripheral diabetic neuropathy, autonomic neuropathy, and diabetic mononeuropathy.
“We’ve had a number of amputations; quite a number of toes are now missing in this group of kids,” Dr. Zeitler said.
There have been five deaths so far: one heart attack, one renal failure, one overwhelming sepsis, one postop cardiac arrest, and a drug overdose.
Dr. Zeitler was the senior author on 2018 updated ADA guidelines for managing youth-onset type 2 diabetes. The recommendations where extensively shaped by the TODAY findings and were more aggressive than those previously put forward, suggesting, among other things, hemoglobin A1c targets of 6.5%-7%; earlier treatment with insulin; and stricter management of hypertension, dyslipidemia, and proteinuria (Diabetes Care. 2018;41[12]:2648-68).
The National Institute of Diabetes & Kidney disease funded the studies. The presenters reported no relevant disclosures or conflicts of interest.
This article was updated 7/22/19.
SAN FRANCISCO – and by the time those with youth-onset diabetes reach their early 20s, they are beset with disease-related complications usually seen in older populations, findings from the RISE and TODAY2 studies have demonstrated.
“Additional research is urgently needed to better understand the reasons for this more serious trajectory,” Philip Zeitler, MD, PhD, of Children’s Hospital Colorado, Aurora, said at the annual scientific sessions of the American Diabetes Association. The hope is to identify at-risk children and prevent the disease, but at this point “we don’t know the answer.”
In the meantime, “we are getting more aggressive with bariatric surgery at our center, because nothing else is working as well. It would be nice to move away from that, but these kids are going to die,” he added.
Steven Kahn, MD, of the diabetes Research Center at the University of Washington, Seattle, presented the findings from a comparison of outcomes from the Restoring Insulin Secretion (RISE) studies in adolescents aged 10-19 years and in adults. The RISE Pediatric Medication Study (Diabetes Care. 2018; 41[8]:1717-25) and RISE Adult Medication Study were parallel investigations treatments to preserve or improve beta-cell function.
“This is the first-ever true comparison of outcomes in youth versus adults,” he said. Both arms had the same design and lab measurements, but the differences in outcomes were “very scary,” he added. “The disease is much more aggressive in youth than in adults.”
Among other things, the RISE youth-versus-adult study compared the outcomes after 3 months of insulin glargine followed by 9 months of metformin, or 12 months of metformin in 132 obese adults and 91 obese adolescents with impaired glucose tolerance or recently diagnosed type 2 diabetes. The treatments were stopped after 12 months, and the participants were reevaluated at 15 months. Hyperglycemic clamps were conducted at baseline, 12 months, and 3 months after treatment cessation (Diabetes. 2019 Jun 9. doi: 10.2337/db19-0299).
In adults, treatment improved insulin sensitivity and beta-cell response, but after treatment cessation, they reverted to baseline by the 15-month evaluation. However, there was no improvement in insulin sensitivity and beta-cell response in adolescents, either during treatment or after cessation, and in fact, they were worse off at 15 months than they had been at baseline, with lower insulin secretion and higher hemoglobin A1c.
Those stark differences in outcomes between the adolescents and adults were indicative of a more aggressive disease trajectory for younger patients.
Compliance was not the issue, with more than 80% of both adults and children taking more than 80% of their medications, Dr. Kahn said.
He suggested that adolescents might have a different underlying pathology that makes it worse to develop diabetes during puberty, which is already an insulin-resistant state. But, whatever the case, there is an “urgent need” to better understand the differences between adolescents and adults and to find better treatments for younger patients with diabetes, he said.
In regard to using weight loss as a means of treatment or prevention, Dr. Zeitler emphasized that type 2 diabetes in younger patients “occurs in a context of very low socioeconomic status, family dysfunction, and a great deal of stress and [family] illness. It’s often a complex situation and it’s difficult to accomplish effective lifestyle change when families are struggling to have afford quality food, facing challenges of family and neighborhood violence, and working multiple jobs.”
The RISE findings of a more aggressive deterioration in beta-cell function for younger patients were reflected in outcomes in the TODAY2 study, which found that adolescents who are diagnosed with type 2 diabetes face severe renal, cardiovascular, eye, and nerve complications by the time they reach their early 20s.
TODAY2 was an 8-year follow-up to the Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) trial published in 2012 (N Engl J Med. 2012;366:2247-56). Data from the original study of patients aged 10-17 years with type 2 diabetes showed that after a roughly 4-year follow-up, almost half of all participants had experienced loss of glycemic control on their original treatment assignment, a rate much higher than that reported in adults. Metformin plus rosiglitazone was superior to metformin alone in maintaining durable glycemic control and metformin plus an intensive lifestyle intervention was intermediate to the other groups, but not significantly different from them. In addition, metformin alone was found to be least effective in non-Hispanic black patients, metformin and rosiglitazone was most effective in girls.
Overall, 517 participants of the original study’s 669 participants are still being followed as part of the TODAY2 trial. They are managed in community practices now and are in their early 20s, on average.
But, less than 10 years down the road from TODAY, the young adults “have problems you’d expect in your grandparents. Target-organ damage is already evident, and serious cardiovascular events are occurring,” Dr. Zeitler said.
Cardiovascular complications
The cardiovascular event rate in TODAY 2 was about the same as is seen in older adults with type 1 diabetes. Overall, there were 38 cardiovascular events in 19 patients for an event rate of 6.4/1,000 patients per year. Those events included heart failure, arrhythmia, coronary artery disease or myocardial infarction, deep venous thrombosis, stroke or transient ischemic attack, and vascular insufficiency.
Over that time, the cumulative incidence of elevated LDL cholesterol increased from 3% in the TODAY report to 26% for TODAY2, and for triglycerides, it went from 18% to 35%. The cumulative incidence of hypertension increased from 19% to 55%.
Decline renal function
In regard to renal complications, the cumulative incident curve for microalbuminuria went from 8% at baseline to 40% at 12 years, while macroalbuminuria prevalence increased from 1.5% to 11% during the same time. The cumulative incidence of hyperfiltration increased from 12% to 48%. Risk factors for hyperfiltration included female sex, Hispanic ethnicity, loss of glycemic control, and hypertension, although body mass index was actually associated with lower risk.
So far, there have been four renal events in two patients, who both had chronic kidney disease and end-stage renal failure, for an event rate of 0.7/1,000 patients per year.
Pregnancy outcomes
Women in the cohort – about two-thirds of the study population – have had high rates of maternal complications, and their offspring also face complications after birth.
There were 306 pregnancies reported, of which there are known outcomes for 53 (TODAY) and 236 (TODAY2). In all, 5% of the total cohort had voluntary elective termination; 9% and 12% of patients, respectively, suffered a miscarriage before 20 weeks; and 4% of pregnancies in the total cohort ended in stillbirth.
Preterm live births more than doubled from 11% to 24%, and full-term deliveries decreased from 62% to 46% in the TODAY2 patients.
In regard to offspring characteristics, average birth weight in the total cohort was just over 4.5 pounds (national average, 7.3 pounds), and the prevalence of very low birth weight more than doubled from 8% to 16% at the 12-year mark. The prevalence of macrosomia was 19% for the cohort, more than double the national average of 8%. In all, 5% and 7% of offspring were small for gestational age, whereas 22% and 26% of offspring were large for gestational age.
Among other complications, respiratory distress occurred in 8% and 14% of offspring, and cardiac anomalies occurred in 10% and 9%, which, although they held steady across the cohorts, were significantly higher than the national average of 1%. Similarly, neonatal hypoglycemia occurred in 17% and 29% of offspring, again, notably higher than the national average of 2%. Offspring outcomes were worse in mothers with loss of glycemic control.
In regard to maternal pregnancy complications, the rate of hospitalization before delivery increased from 25% to 36%; hypertension increased in prevalence from 19% to 36%; and while macroalbuminuria held steady at 9.4%, microalbuminuria increased from 6% to 8%. Thirty-three percent of the TODAY2 cohort had a hemoglobin A1c level of more than 8%.
Retinopathy
Serious eye problems were common, with notable progression seen in diabetic retinopathy in patients who had fundus photos taken in 2011 (TODAY) and 2018 (TODAY2). Among the patients, 86% and 51%, respectively, of 371 patients had no definitive diabetic retinopathy; 14% and 22% of patients had very mild nonproliferative diabetic retinopathy (NPDR); and 0% and 16% of patients had mild NPDR. None of the TODAY patients had early or high-risk proliferative diabetic retinopathy, compared with 3% and 1%, respectively, in TODAY2. Risk factors included loss of glycemic control (hazard ratio, 19.23; 95% confidence interval, 4.62-80.07).
None of the TODAY patients had macular edema, whereas it occurred in 4% of TODAY2 patients. In all, there were 142 adjudicated eye-related events reported for 92 patients, for an event rate of 15.5/1,000 patients per year. The events included NPDR, proliferative diabetic retinopathy, macular edema, cataracts, glaucoma, and vitreous hemorrhage).
Neuropathy
The prevalence of diabetic neuropathy also increased over the duration of follow-up, rising to 28%-33% based on Michigan Neuropathy Screening Instrument scores. There were 14 adjudicated events reported for 12 patients (2.4 events/1,000 patients per year), including peripheral diabetic neuropathy, autonomic neuropathy, and diabetic mononeuropathy.
“We’ve had a number of amputations; quite a number of toes are now missing in this group of kids,” Dr. Zeitler said.
There have been five deaths so far: one heart attack, one renal failure, one overwhelming sepsis, one postop cardiac arrest, and a drug overdose.
Dr. Zeitler was the senior author on 2018 updated ADA guidelines for managing youth-onset type 2 diabetes. The recommendations where extensively shaped by the TODAY findings and were more aggressive than those previously put forward, suggesting, among other things, hemoglobin A1c targets of 6.5%-7%; earlier treatment with insulin; and stricter management of hypertension, dyslipidemia, and proteinuria (Diabetes Care. 2018;41[12]:2648-68).
The National Institute of Diabetes & Kidney disease funded the studies. The presenters reported no relevant disclosures or conflicts of interest.
This article was updated 7/22/19.
EXPERT ANALYSIS FROM ADA 2019
SGLT2 inhibitors, GLP-1 RAs are effective, but costly in T2D
Metformin linked to lower dementia risk in black patients
Black individuals who develop type 2 diabetes are more likely than their white counterparts to develop dementia. Now, findings from a new study point to a possible preventive strategy: Putting older patients on metformin when they are diagnosed could reduce their risk for dementia by as much as 40%, whereas sulfonylureas do not seem to have such an effect.
The researchers did not examine cause and effect, so their findings are not conclusive, and very few women were included in the study. Still, the authors said that their data showing a 29% lower risk of dementia associated with metformin use in black patients aged 65-74 years, and a 40% lower risk in those aged 50-64 years, suggested that “this inexpensive, widely available treatment could be broadly prescribed to substantially reduce the risk of dementia in younger [black] patients with [type 2 diabetes]” (Ann Fam Med. 2019;17:352-62).
Previous findings have suggested that black patients with type 2 diabetes face a 10%-18% higher risk of dementia, compared with white patients (Diabetes Care. 2014; 37[4]:1009-15). Another study linked type 2 diabetes in middle-aged black patients to a 41% decrease in cognition per test results over 14 years. There was no such decrease in white patients (Neuroepidemiology. 2014;43[3-4]: 220-7).
For the new study, researchers led by Jeffrey F. Scherrer, PhD, of Saint Louis University tracked 73,761 patients aged 50 years or older from 2000-2001 (when they were free of dementia and not taking diabetes) to 2015. Among the patients, 86% were white and 14% were black. In the white and black groups, 97% and 95% were men, respectively, and 61% and 55% were obese, respectively.
All participants began metformin (76%) or sulfonylurea (24%) monotherapy after the baseline period. Guidelines recommend metformin as a first-line treatment for type 2 diabetes, whereas sulfonylureas are considered second-line drugs that should be added to metformin.
After adjustment for confounders such as socioeconomic status and other medical conditions, the researchers found a significantly lower risk of dementia in black patients who took metformin, compared with those taking a sulfonylurea (hazard ratio, 0.73; 95% confidence interval, 0.6-0.89). There was no difference between the drugs among white patients (HR, 0.96; 95% CI, 0.9-1.03, both P = .008)
The results were not statistically significant among age groups, but there were trends. In black patients, the dementia-lowering benefit was largest among those aged 50-64 years (HR, 0.6; 95% CI, 0.45-0.81), followed by those aged 65-74 years (HR, 0.71; 95% CI, 0.53-0.94), and there was no benefit among those aged at least 75 (HR, 1.17; 95% CI, 0.73-1.85) all P = .055. There was a slight benefit among white patients in one of the age groups – 65-74 years (HR, 0.9; 95% CI, 0.82-0.99; P = .315).
The authors suggested that the findings could have been the result of an effect of metformin to reduce vascular disease and chronic inflammation in black patients.
They also noted that further research is needed to identify the demographic and clinical subgroups in which metformin is most strongly associated with a reduction in the risk of dementia. In addition, they emphasized that clinical trials are needed to confirm the study findings.
The National Institutes of Health funded the study. The authors report no relevant disclosures.
SOURCE: Scherrer JF et al. Ann Fam Med. 2019;17:352-62.
Black individuals who develop type 2 diabetes are more likely than their white counterparts to develop dementia. Now, findings from a new study point to a possible preventive strategy: Putting older patients on metformin when they are diagnosed could reduce their risk for dementia by as much as 40%, whereas sulfonylureas do not seem to have such an effect.
The researchers did not examine cause and effect, so their findings are not conclusive, and very few women were included in the study. Still, the authors said that their data showing a 29% lower risk of dementia associated with metformin use in black patients aged 65-74 years, and a 40% lower risk in those aged 50-64 years, suggested that “this inexpensive, widely available treatment could be broadly prescribed to substantially reduce the risk of dementia in younger [black] patients with [type 2 diabetes]” (Ann Fam Med. 2019;17:352-62).
Previous findings have suggested that black patients with type 2 diabetes face a 10%-18% higher risk of dementia, compared with white patients (Diabetes Care. 2014; 37[4]:1009-15). Another study linked type 2 diabetes in middle-aged black patients to a 41% decrease in cognition per test results over 14 years. There was no such decrease in white patients (Neuroepidemiology. 2014;43[3-4]: 220-7).
For the new study, researchers led by Jeffrey F. Scherrer, PhD, of Saint Louis University tracked 73,761 patients aged 50 years or older from 2000-2001 (when they were free of dementia and not taking diabetes) to 2015. Among the patients, 86% were white and 14% were black. In the white and black groups, 97% and 95% were men, respectively, and 61% and 55% were obese, respectively.
All participants began metformin (76%) or sulfonylurea (24%) monotherapy after the baseline period. Guidelines recommend metformin as a first-line treatment for type 2 diabetes, whereas sulfonylureas are considered second-line drugs that should be added to metformin.
After adjustment for confounders such as socioeconomic status and other medical conditions, the researchers found a significantly lower risk of dementia in black patients who took metformin, compared with those taking a sulfonylurea (hazard ratio, 0.73; 95% confidence interval, 0.6-0.89). There was no difference between the drugs among white patients (HR, 0.96; 95% CI, 0.9-1.03, both P = .008)
The results were not statistically significant among age groups, but there were trends. In black patients, the dementia-lowering benefit was largest among those aged 50-64 years (HR, 0.6; 95% CI, 0.45-0.81), followed by those aged 65-74 years (HR, 0.71; 95% CI, 0.53-0.94), and there was no benefit among those aged at least 75 (HR, 1.17; 95% CI, 0.73-1.85) all P = .055. There was a slight benefit among white patients in one of the age groups – 65-74 years (HR, 0.9; 95% CI, 0.82-0.99; P = .315).
The authors suggested that the findings could have been the result of an effect of metformin to reduce vascular disease and chronic inflammation in black patients.
They also noted that further research is needed to identify the demographic and clinical subgroups in which metformin is most strongly associated with a reduction in the risk of dementia. In addition, they emphasized that clinical trials are needed to confirm the study findings.
The National Institutes of Health funded the study. The authors report no relevant disclosures.
SOURCE: Scherrer JF et al. Ann Fam Med. 2019;17:352-62.
Black individuals who develop type 2 diabetes are more likely than their white counterparts to develop dementia. Now, findings from a new study point to a possible preventive strategy: Putting older patients on metformin when they are diagnosed could reduce their risk for dementia by as much as 40%, whereas sulfonylureas do not seem to have such an effect.
The researchers did not examine cause and effect, so their findings are not conclusive, and very few women were included in the study. Still, the authors said that their data showing a 29% lower risk of dementia associated with metformin use in black patients aged 65-74 years, and a 40% lower risk in those aged 50-64 years, suggested that “this inexpensive, widely available treatment could be broadly prescribed to substantially reduce the risk of dementia in younger [black] patients with [type 2 diabetes]” (Ann Fam Med. 2019;17:352-62).
Previous findings have suggested that black patients with type 2 diabetes face a 10%-18% higher risk of dementia, compared with white patients (Diabetes Care. 2014; 37[4]:1009-15). Another study linked type 2 diabetes in middle-aged black patients to a 41% decrease in cognition per test results over 14 years. There was no such decrease in white patients (Neuroepidemiology. 2014;43[3-4]: 220-7).
For the new study, researchers led by Jeffrey F. Scherrer, PhD, of Saint Louis University tracked 73,761 patients aged 50 years or older from 2000-2001 (when they were free of dementia and not taking diabetes) to 2015. Among the patients, 86% were white and 14% were black. In the white and black groups, 97% and 95% were men, respectively, and 61% and 55% were obese, respectively.
All participants began metformin (76%) or sulfonylurea (24%) monotherapy after the baseline period. Guidelines recommend metformin as a first-line treatment for type 2 diabetes, whereas sulfonylureas are considered second-line drugs that should be added to metformin.
After adjustment for confounders such as socioeconomic status and other medical conditions, the researchers found a significantly lower risk of dementia in black patients who took metformin, compared with those taking a sulfonylurea (hazard ratio, 0.73; 95% confidence interval, 0.6-0.89). There was no difference between the drugs among white patients (HR, 0.96; 95% CI, 0.9-1.03, both P = .008)
The results were not statistically significant among age groups, but there were trends. In black patients, the dementia-lowering benefit was largest among those aged 50-64 years (HR, 0.6; 95% CI, 0.45-0.81), followed by those aged 65-74 years (HR, 0.71; 95% CI, 0.53-0.94), and there was no benefit among those aged at least 75 (HR, 1.17; 95% CI, 0.73-1.85) all P = .055. There was a slight benefit among white patients in one of the age groups – 65-74 years (HR, 0.9; 95% CI, 0.82-0.99; P = .315).
The authors suggested that the findings could have been the result of an effect of metformin to reduce vascular disease and chronic inflammation in black patients.
They also noted that further research is needed to identify the demographic and clinical subgroups in which metformin is most strongly associated with a reduction in the risk of dementia. In addition, they emphasized that clinical trials are needed to confirm the study findings.
The National Institutes of Health funded the study. The authors report no relevant disclosures.
SOURCE: Scherrer JF et al. Ann Fam Med. 2019;17:352-62.
FROM ANNALS OF FAMILY MEDICINE
Key clinical point:
Major finding: Metformin monotherapy, compared with sulfonylurea monotherapy, was linked to a significantly lower risk for dementia in black patients (HR, 0.73; 95% CI, 0.6-0.89), but not in white patients (HR, 0.96; 95% CI, 0.9-1.03; P = .008).
Study details: Retrospective analysis of 73,761 patients aged 50 years or older in the Veterans Health Administration system who were tracked from 2000-2001 to 2015 and began metformin or sulfonylurea monotherapy after baseline.
Disclosures: The National Institutes of Health funded the study. The authors report no relevant disclosures.
Source: Scherrer JF et al. Ann Fam Med. 2019;17:352-62.