User login
New cancer cases to reach nearly 2.4 million in 2035 – AACR
There will be nearly 2.4 million new cases of cancer in the U.S. by 2035, according to an estimate from the American Association for Cancer Research.
In its Cancer Progress Report 2015, AACR notes that new cases in the current year are estimated at nearly 1.7 million.
“Given that cancer is primarily a disease of aging and that the portion of the U.S. population age 65 and older is expected to double in size by 2060, it is anticipated that the number of new cancer cases diagnosed each year in the United States will increase dramatically,” the report states.
“Also contributing to the projected increase are the continual use of cigarettes by 18% of U.S. adults, and high rates of obesity and physical inactivity, both of which are linked to an increased risk for several types of cancer.”
The spike in new cases comes as death rates are trending downward. From 2002 to 2011, overall cancer death rates declined per year by 1.8% for U.S. men, 1.4% for U.S. women, and 2.1% for 0- to 19-year-olds, though the overall number of cancer deaths is expected to rise. Nearly 600,000 people living in the United States are expected to die from cancer in 2015.
The new diagnoses are expected to drive up the cost of cancer.
“In the United States alone, it is estimated that the direct medical costs of cancer care will rise to $156 billion in 2020, from nearly $125 billion in 2010,” AACR says in the report. “When these costs are compared to the total NCI budget for fiscal year 2015, which is just $5 billion, it is clear that research that spurs lifesaving progress against cancer is a wise national investment.”
To that end, AACR is calling on Congress and the White House to boost funding for both the National Institutes of Health and the National Cancer Institute by at least 7%, which would result in funding levels in fiscal year 2020 for NIH and NCI of $42.5 billion and $7 billion, respectively. AACR is also calling for a similar 7% increase the Food and Drug Administration’s budget to help drive private biomedical research.
There will be nearly 2.4 million new cases of cancer in the U.S. by 2035, according to an estimate from the American Association for Cancer Research.
In its Cancer Progress Report 2015, AACR notes that new cases in the current year are estimated at nearly 1.7 million.
“Given that cancer is primarily a disease of aging and that the portion of the U.S. population age 65 and older is expected to double in size by 2060, it is anticipated that the number of new cancer cases diagnosed each year in the United States will increase dramatically,” the report states.
“Also contributing to the projected increase are the continual use of cigarettes by 18% of U.S. adults, and high rates of obesity and physical inactivity, both of which are linked to an increased risk for several types of cancer.”
The spike in new cases comes as death rates are trending downward. From 2002 to 2011, overall cancer death rates declined per year by 1.8% for U.S. men, 1.4% for U.S. women, and 2.1% for 0- to 19-year-olds, though the overall number of cancer deaths is expected to rise. Nearly 600,000 people living in the United States are expected to die from cancer in 2015.
The new diagnoses are expected to drive up the cost of cancer.
“In the United States alone, it is estimated that the direct medical costs of cancer care will rise to $156 billion in 2020, from nearly $125 billion in 2010,” AACR says in the report. “When these costs are compared to the total NCI budget for fiscal year 2015, which is just $5 billion, it is clear that research that spurs lifesaving progress against cancer is a wise national investment.”
To that end, AACR is calling on Congress and the White House to boost funding for both the National Institutes of Health and the National Cancer Institute by at least 7%, which would result in funding levels in fiscal year 2020 for NIH and NCI of $42.5 billion and $7 billion, respectively. AACR is also calling for a similar 7% increase the Food and Drug Administration’s budget to help drive private biomedical research.
There will be nearly 2.4 million new cases of cancer in the U.S. by 2035, according to an estimate from the American Association for Cancer Research.
In its Cancer Progress Report 2015, AACR notes that new cases in the current year are estimated at nearly 1.7 million.
“Given that cancer is primarily a disease of aging and that the portion of the U.S. population age 65 and older is expected to double in size by 2060, it is anticipated that the number of new cancer cases diagnosed each year in the United States will increase dramatically,” the report states.
“Also contributing to the projected increase are the continual use of cigarettes by 18% of U.S. adults, and high rates of obesity and physical inactivity, both of which are linked to an increased risk for several types of cancer.”
The spike in new cases comes as death rates are trending downward. From 2002 to 2011, overall cancer death rates declined per year by 1.8% for U.S. men, 1.4% for U.S. women, and 2.1% for 0- to 19-year-olds, though the overall number of cancer deaths is expected to rise. Nearly 600,000 people living in the United States are expected to die from cancer in 2015.
The new diagnoses are expected to drive up the cost of cancer.
“In the United States alone, it is estimated that the direct medical costs of cancer care will rise to $156 billion in 2020, from nearly $125 billion in 2010,” AACR says in the report. “When these costs are compared to the total NCI budget for fiscal year 2015, which is just $5 billion, it is clear that research that spurs lifesaving progress against cancer is a wise national investment.”
To that end, AACR is calling on Congress and the White House to boost funding for both the National Institutes of Health and the National Cancer Institute by at least 7%, which would result in funding levels in fiscal year 2020 for NIH and NCI of $42.5 billion and $7 billion, respectively. AACR is also calling for a similar 7% increase the Food and Drug Administration’s budget to help drive private biomedical research.
FROM AACR CANCER PROGRESS REPORT 2015
Share of lung cancer patients who never smoked is rising
DENVER – An increasing share of patients with lung cancer report that they have never smoked, according to a pair of retrospective cohort studies reported at a world conference on lung cancer.
At three U.S. institutions serving geographically and racially diverse populations, the proportion of never-smokers rose from 9% to 15% over a 24-year period among patients with non–small-cell lung cancer (NSCLC), but did not change among those with small-cell lung cancer (SCLC). At a U.K. tertiary care institution, the proportion of never-smokers rose from 13% to 27% over a 7-year period among patients undergoing surgery for lung cancer.
Data further suggested that these trends were due at least in part to an increase in the absolute number of never-smokers with lung cancer, and not simply to a decline in the proportion of smokers with lung cancer, or to earlier, incidental detection of tumors resulting from better imaging technology.
More research will be needed to determine the specific factors driving this increase, according to Dr. Everett E. Vokes, cochair of the conference, moderator of a related press conference, and the John E. Ultmann Professor and Chair, department of medicine, University of Chicago.
“What is causing this, for me, would be very, very speculative,” he said. “Secondhand smoke is still there, and radon is mentioned. That shouldn’t necessarily justify an increase, because those are either constant or also decreasing [like smoking]. And of course it could be pollution and factors that have to do with small particles and carcinogens in the air.”
In the first study, investigators led by Dr. Lorraine Pelosof of UT Southwestern Medical Center in Dallas used registries at three institutions – UT Southwestern Medical Center, Parkland Hospital in Dallas, and Vanderbilt University in Nashville, Tenn. – to identify patients who were diagnosed with lung cancer between 1990 and 2013.
Analyses were based on 10,593 patients with NSCLC and 1,510 patients with SCLC. The latter serve as an internal control given that cancer’s tight link with smoking, Dr. Pelosof noted.
In adjusted analyses, the proportion in the NSCLC group who reported never smoking increased from 9% to 15% during the study period (P less than .0001). In contrast, the proportion in the SCLC group held steady at roughly 2%.
Among patients with NSCLC, never-smokers were on average younger and more likely to be female compared with smokers, Dr. Pelosof reported at the conference, which was sponsored by the International Association for the Study of Lung Cancer.
In teasing out the cause for the rise in never-smokers with NSCLC, analyses showed that the absolute numbers of patients with NSCLC increased during the study period.
Preliminary data suggested that earlier, incidental detection did not explain the trend, as rates of stage I, II, and III disease in never-smokers were stable or decreased, while the rate of stage IV disease increased.
In addition, the trend did not appear to be explained by an influx to the institutions of patients with mutations seeking targeted therapies on clinical trials, as the trend persisted after adjustment for race/ethnicity, which was used as a surrogate for mutational status.
The investigators plan several avenues of additional research to sort this out, Dr. Pelosof said.
“We want to look at possibly other institutions that are geographically and demographically diverse. Additional institutions would be helpful,” she said. “And then to get at some of the mechanisms, [looking at] mutational status and biology I think would be very important.”
In the second study, Dr. Eric Lim, a consultant thoracic surgeon at Royal Brompton Hospital, and a senior lecturer and reader in thoracic surgery at the National Heart and Lung Institute, Imperial College, London, and colleagues assessed smoking status among 2,170 patients who underwent surgery for lung cancer at the hospital between 2008 and 2014.
Overall, 20% of the patients in the cohort were never-smokers. Their mean age at presentation was 60 years, and two-thirds were women. The predominant tumor types were adenocarcinoma, seen in 54%, and carcinoid, seen in 27%.
The proportion who were never-smokers more than doubled during the study period, from 13% to 27%. The absolute annual number of such patients also rose, from about 60 to nearly 100.
Fully 52% of the never-smokers presented with only nonspecific symptoms of cough or chest infection, while 11% had hemoptysis. In the remaining 36%, the cancer was identified as an incidental finding on imaging done for other reasons.
“Nonsmoking lung cancer is increasing and now a significant proportion of the workload for surgeons across the United Kingdom,” concluded Dr. Lim. “Early detection in this group is challenging because they have no clear-cut symptoms, and serious symptoms were only present in a minority,” he said.
“Clearly it’s not going to be cost-effective to screen the entire population of nonsmokers for lung cancer,” he added. Since these patients “do not have established risk factors, research into early detection, ideally by noninvasive or molecular screening, is urgently required to identify early lung cancer in nonsmokers.”
Dr. Pelosof and Dr. Lim reported having no conflicts of interest.
DENVER – An increasing share of patients with lung cancer report that they have never smoked, according to a pair of retrospective cohort studies reported at a world conference on lung cancer.
At three U.S. institutions serving geographically and racially diverse populations, the proportion of never-smokers rose from 9% to 15% over a 24-year period among patients with non–small-cell lung cancer (NSCLC), but did not change among those with small-cell lung cancer (SCLC). At a U.K. tertiary care institution, the proportion of never-smokers rose from 13% to 27% over a 7-year period among patients undergoing surgery for lung cancer.
Data further suggested that these trends were due at least in part to an increase in the absolute number of never-smokers with lung cancer, and not simply to a decline in the proportion of smokers with lung cancer, or to earlier, incidental detection of tumors resulting from better imaging technology.
More research will be needed to determine the specific factors driving this increase, according to Dr. Everett E. Vokes, cochair of the conference, moderator of a related press conference, and the John E. Ultmann Professor and Chair, department of medicine, University of Chicago.
“What is causing this, for me, would be very, very speculative,” he said. “Secondhand smoke is still there, and radon is mentioned. That shouldn’t necessarily justify an increase, because those are either constant or also decreasing [like smoking]. And of course it could be pollution and factors that have to do with small particles and carcinogens in the air.”
In the first study, investigators led by Dr. Lorraine Pelosof of UT Southwestern Medical Center in Dallas used registries at three institutions – UT Southwestern Medical Center, Parkland Hospital in Dallas, and Vanderbilt University in Nashville, Tenn. – to identify patients who were diagnosed with lung cancer between 1990 and 2013.
Analyses were based on 10,593 patients with NSCLC and 1,510 patients with SCLC. The latter serve as an internal control given that cancer’s tight link with smoking, Dr. Pelosof noted.
In adjusted analyses, the proportion in the NSCLC group who reported never smoking increased from 9% to 15% during the study period (P less than .0001). In contrast, the proportion in the SCLC group held steady at roughly 2%.
Among patients with NSCLC, never-smokers were on average younger and more likely to be female compared with smokers, Dr. Pelosof reported at the conference, which was sponsored by the International Association for the Study of Lung Cancer.
In teasing out the cause for the rise in never-smokers with NSCLC, analyses showed that the absolute numbers of patients with NSCLC increased during the study period.
Preliminary data suggested that earlier, incidental detection did not explain the trend, as rates of stage I, II, and III disease in never-smokers were stable or decreased, while the rate of stage IV disease increased.
In addition, the trend did not appear to be explained by an influx to the institutions of patients with mutations seeking targeted therapies on clinical trials, as the trend persisted after adjustment for race/ethnicity, which was used as a surrogate for mutational status.
The investigators plan several avenues of additional research to sort this out, Dr. Pelosof said.
“We want to look at possibly other institutions that are geographically and demographically diverse. Additional institutions would be helpful,” she said. “And then to get at some of the mechanisms, [looking at] mutational status and biology I think would be very important.”
In the second study, Dr. Eric Lim, a consultant thoracic surgeon at Royal Brompton Hospital, and a senior lecturer and reader in thoracic surgery at the National Heart and Lung Institute, Imperial College, London, and colleagues assessed smoking status among 2,170 patients who underwent surgery for lung cancer at the hospital between 2008 and 2014.
Overall, 20% of the patients in the cohort were never-smokers. Their mean age at presentation was 60 years, and two-thirds were women. The predominant tumor types were adenocarcinoma, seen in 54%, and carcinoid, seen in 27%.
The proportion who were never-smokers more than doubled during the study period, from 13% to 27%. The absolute annual number of such patients also rose, from about 60 to nearly 100.
Fully 52% of the never-smokers presented with only nonspecific symptoms of cough or chest infection, while 11% had hemoptysis. In the remaining 36%, the cancer was identified as an incidental finding on imaging done for other reasons.
“Nonsmoking lung cancer is increasing and now a significant proportion of the workload for surgeons across the United Kingdom,” concluded Dr. Lim. “Early detection in this group is challenging because they have no clear-cut symptoms, and serious symptoms were only present in a minority,” he said.
“Clearly it’s not going to be cost-effective to screen the entire population of nonsmokers for lung cancer,” he added. Since these patients “do not have established risk factors, research into early detection, ideally by noninvasive or molecular screening, is urgently required to identify early lung cancer in nonsmokers.”
Dr. Pelosof and Dr. Lim reported having no conflicts of interest.
DENVER – An increasing share of patients with lung cancer report that they have never smoked, according to a pair of retrospective cohort studies reported at a world conference on lung cancer.
At three U.S. institutions serving geographically and racially diverse populations, the proportion of never-smokers rose from 9% to 15% over a 24-year period among patients with non–small-cell lung cancer (NSCLC), but did not change among those with small-cell lung cancer (SCLC). At a U.K. tertiary care institution, the proportion of never-smokers rose from 13% to 27% over a 7-year period among patients undergoing surgery for lung cancer.
Data further suggested that these trends were due at least in part to an increase in the absolute number of never-smokers with lung cancer, and not simply to a decline in the proportion of smokers with lung cancer, or to earlier, incidental detection of tumors resulting from better imaging technology.
More research will be needed to determine the specific factors driving this increase, according to Dr. Everett E. Vokes, cochair of the conference, moderator of a related press conference, and the John E. Ultmann Professor and Chair, department of medicine, University of Chicago.
“What is causing this, for me, would be very, very speculative,” he said. “Secondhand smoke is still there, and radon is mentioned. That shouldn’t necessarily justify an increase, because those are either constant or also decreasing [like smoking]. And of course it could be pollution and factors that have to do with small particles and carcinogens in the air.”
In the first study, investigators led by Dr. Lorraine Pelosof of UT Southwestern Medical Center in Dallas used registries at three institutions – UT Southwestern Medical Center, Parkland Hospital in Dallas, and Vanderbilt University in Nashville, Tenn. – to identify patients who were diagnosed with lung cancer between 1990 and 2013.
Analyses were based on 10,593 patients with NSCLC and 1,510 patients with SCLC. The latter serve as an internal control given that cancer’s tight link with smoking, Dr. Pelosof noted.
In adjusted analyses, the proportion in the NSCLC group who reported never smoking increased from 9% to 15% during the study period (P less than .0001). In contrast, the proportion in the SCLC group held steady at roughly 2%.
Among patients with NSCLC, never-smokers were on average younger and more likely to be female compared with smokers, Dr. Pelosof reported at the conference, which was sponsored by the International Association for the Study of Lung Cancer.
In teasing out the cause for the rise in never-smokers with NSCLC, analyses showed that the absolute numbers of patients with NSCLC increased during the study period.
Preliminary data suggested that earlier, incidental detection did not explain the trend, as rates of stage I, II, and III disease in never-smokers were stable or decreased, while the rate of stage IV disease increased.
In addition, the trend did not appear to be explained by an influx to the institutions of patients with mutations seeking targeted therapies on clinical trials, as the trend persisted after adjustment for race/ethnicity, which was used as a surrogate for mutational status.
The investigators plan several avenues of additional research to sort this out, Dr. Pelosof said.
“We want to look at possibly other institutions that are geographically and demographically diverse. Additional institutions would be helpful,” she said. “And then to get at some of the mechanisms, [looking at] mutational status and biology I think would be very important.”
In the second study, Dr. Eric Lim, a consultant thoracic surgeon at Royal Brompton Hospital, and a senior lecturer and reader in thoracic surgery at the National Heart and Lung Institute, Imperial College, London, and colleagues assessed smoking status among 2,170 patients who underwent surgery for lung cancer at the hospital between 2008 and 2014.
Overall, 20% of the patients in the cohort were never-smokers. Their mean age at presentation was 60 years, and two-thirds were women. The predominant tumor types were adenocarcinoma, seen in 54%, and carcinoid, seen in 27%.
The proportion who were never-smokers more than doubled during the study period, from 13% to 27%. The absolute annual number of such patients also rose, from about 60 to nearly 100.
Fully 52% of the never-smokers presented with only nonspecific symptoms of cough or chest infection, while 11% had hemoptysis. In the remaining 36%, the cancer was identified as an incidental finding on imaging done for other reasons.
“Nonsmoking lung cancer is increasing and now a significant proportion of the workload for surgeons across the United Kingdom,” concluded Dr. Lim. “Early detection in this group is challenging because they have no clear-cut symptoms, and serious symptoms were only present in a minority,” he said.
“Clearly it’s not going to be cost-effective to screen the entire population of nonsmokers for lung cancer,” he added. Since these patients “do not have established risk factors, research into early detection, ideally by noninvasive or molecular screening, is urgently required to identify early lung cancer in nonsmokers.”
Dr. Pelosof and Dr. Lim reported having no conflicts of interest.
AT THE IASLC WORLD CONFERENCE
Key clinical point: The proportion of patients with lung cancer who have never smoked has risen in recent decades.
Major finding: Between 1990 and 2013 in the United States, the proportion with NSCLC who never smoked rose from 9% to 15%. Between 2008 and 2014 in the United Kingdom, the proportion undergoing surgery for lung cancer who never smoked rose from 13% to 27%.
Data source: A pair of retrospective cohort studies of 12,103 U.S. patients and 2,170 U.K. patients with lung cancer.
Disclosures: Dr. Pelosof and Dr. Lim reported having no conflicts of interest.
VIDEO: High-value care: The OCCAM’s initiative
What is high-value care and how can it be achieved? Overuse of clinical tests and diagnostic procedures, largely driven by concerns about missing unusual but potentially significant diagnoses, drives health care costs and can result in worrisome incidental findings.
Dr. Hyung “Harry” Cho, a hospitalist and assistant professor of medicine at the Mt. Sinai School of Medicine in New York, has launched the Overuse Clinical Case Morbidity and Mortality (OCCAM’s) Conference to attack the problem of clinical overuse from a new perspective. Dr. Cho and his colleagues have turned the traditional morbidity and mortality conference on its head by addressing overuse as a medical error and using the conference as a forum to discuss which practical steps should be taken to improve quality of care while avoiding overuse of tests.
In this video interview, Dr. Cho – along with other key members of the OCCAM’s team – discuss the initiative’s inception, the importance of workgroups in implementing quality improvement initiatives from the ground up, and how to advance the conversation to define high-value care.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
What is high-value care and how can it be achieved? Overuse of clinical tests and diagnostic procedures, largely driven by concerns about missing unusual but potentially significant diagnoses, drives health care costs and can result in worrisome incidental findings.
Dr. Hyung “Harry” Cho, a hospitalist and assistant professor of medicine at the Mt. Sinai School of Medicine in New York, has launched the Overuse Clinical Case Morbidity and Mortality (OCCAM’s) Conference to attack the problem of clinical overuse from a new perspective. Dr. Cho and his colleagues have turned the traditional morbidity and mortality conference on its head by addressing overuse as a medical error and using the conference as a forum to discuss which practical steps should be taken to improve quality of care while avoiding overuse of tests.
In this video interview, Dr. Cho – along with other key members of the OCCAM’s team – discuss the initiative’s inception, the importance of workgroups in implementing quality improvement initiatives from the ground up, and how to advance the conversation to define high-value care.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
What is high-value care and how can it be achieved? Overuse of clinical tests and diagnostic procedures, largely driven by concerns about missing unusual but potentially significant diagnoses, drives health care costs and can result in worrisome incidental findings.
Dr. Hyung “Harry” Cho, a hospitalist and assistant professor of medicine at the Mt. Sinai School of Medicine in New York, has launched the Overuse Clinical Case Morbidity and Mortality (OCCAM’s) Conference to attack the problem of clinical overuse from a new perspective. Dr. Cho and his colleagues have turned the traditional morbidity and mortality conference on its head by addressing overuse as a medical error and using the conference as a forum to discuss which practical steps should be taken to improve quality of care while avoiding overuse of tests.
In this video interview, Dr. Cho – along with other key members of the OCCAM’s team – discuss the initiative’s inception, the importance of workgroups in implementing quality improvement initiatives from the ground up, and how to advance the conversation to define high-value care.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
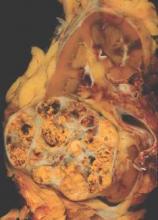
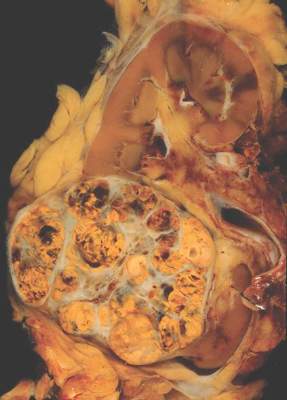
Individualized approach improves surveillance after renal cell carcinoma resection
A novel approach to oncologic surveillance after surgical resection for renal cell carcinoma (RCC) that incorporates patient age, Charlson comorbidity index, pathologic tumor stage, and relapse location–specific data, may provide better recommendations for surveillance duration than current guidelines, researchers reported.
“By providing more individualized recommendations and by eliminating oversimplified time thresholds for surveillance, this strategy, we believe, represents an improvement over current guidelines,” wrote Dr. Suzanne Stewart-Merrill of the department of urology, Mayo Clinic, Rochester, Minn., and colleagues (J Clin Oncol. 2015 Sep 7. doi: 10.1200/JCO.2015.61.8009).
Guidelines suggest surveillance durations based on cumulative incidence of recurrences, but do not account for individual patient risk factors. Adherence to the guidelines could miss up to one-third of all recurrences, the authors noted. The longest surveillance duration advocated by the National Comprehensive Cancer Network or the American Urological Association is 5 years.
Researchers used Weibull models for risk of recurrence, stratified by stage and relapse location, combined with risk estimates for non-RCC death, to estimate the optimum surveillance duration. For example, for patients aged 50-59 years with pT1Nx-0 disease and a Charlson comorbidity index of less than or equal to 1, risk of non-RCC death exceeded the risk of abdominal recurrence at 7 years, marking the recommended surveillance duration for that subgroup. The recommended surveillance duration for patients with similar characteristics aged 60-69 years is 2.5 years, and for patients aged 70-79 years it is 1.5 years.
When taking into account individual risk factors, the method produced a wide range of surveillance durations. For patients under 50 years old with pT1Nx-0 disease and a Charlson comorbidity index less than or equal to 1, the risk of non-RCC death did not exceed the risk of abdominal recurrence for more than 20 years. By contrast, patients with pT1Nx-0 disease and Charlson comorbidity index greater than or equal to 2, had a higher risk of non-RCC death than risk of abdominal recurrence at 30 days after surgery.
The retrospective study of 2,511 patients who underwent surgical resection for M0 sporadic RCC between 1990 and 2008 had a median follow up of 9.0 years (interquartile range 6.4-12.7 years).
The researchers noted that recurrences beyond 5 years are fairly common, with up to 15% of patients, by one study’s estimate, experiencing recurrence during the decade following surgery. Cumulative incidence of recurrence does not capture how a patient’s risk of recurrence changes with time or how comorbid conditions influence risk.
The proposed surveillance method results in shorter surveillance durations for some patients and longer surveillance durations than currently recommended for others. This diversity in stopping points “better reflects the range of disease courses appreciated in patients with RCC on the basis of the interplay that occurs between the risk of recurrence and other competing health factors,” Dr. Stewart-Merrill and associates explained.
Dr. Stewart-Merrill reported having no disclosures.
A novel approach to oncologic surveillance after surgical resection for renal cell carcinoma (RCC) that incorporates patient age, Charlson comorbidity index, pathologic tumor stage, and relapse location–specific data, may provide better recommendations for surveillance duration than current guidelines, researchers reported.
“By providing more individualized recommendations and by eliminating oversimplified time thresholds for surveillance, this strategy, we believe, represents an improvement over current guidelines,” wrote Dr. Suzanne Stewart-Merrill of the department of urology, Mayo Clinic, Rochester, Minn., and colleagues (J Clin Oncol. 2015 Sep 7. doi: 10.1200/JCO.2015.61.8009).
Guidelines suggest surveillance durations based on cumulative incidence of recurrences, but do not account for individual patient risk factors. Adherence to the guidelines could miss up to one-third of all recurrences, the authors noted. The longest surveillance duration advocated by the National Comprehensive Cancer Network or the American Urological Association is 5 years.
Researchers used Weibull models for risk of recurrence, stratified by stage and relapse location, combined with risk estimates for non-RCC death, to estimate the optimum surveillance duration. For example, for patients aged 50-59 years with pT1Nx-0 disease and a Charlson comorbidity index of less than or equal to 1, risk of non-RCC death exceeded the risk of abdominal recurrence at 7 years, marking the recommended surveillance duration for that subgroup. The recommended surveillance duration for patients with similar characteristics aged 60-69 years is 2.5 years, and for patients aged 70-79 years it is 1.5 years.
When taking into account individual risk factors, the method produced a wide range of surveillance durations. For patients under 50 years old with pT1Nx-0 disease and a Charlson comorbidity index less than or equal to 1, the risk of non-RCC death did not exceed the risk of abdominal recurrence for more than 20 years. By contrast, patients with pT1Nx-0 disease and Charlson comorbidity index greater than or equal to 2, had a higher risk of non-RCC death than risk of abdominal recurrence at 30 days after surgery.
The retrospective study of 2,511 patients who underwent surgical resection for M0 sporadic RCC between 1990 and 2008 had a median follow up of 9.0 years (interquartile range 6.4-12.7 years).
The researchers noted that recurrences beyond 5 years are fairly common, with up to 15% of patients, by one study’s estimate, experiencing recurrence during the decade following surgery. Cumulative incidence of recurrence does not capture how a patient’s risk of recurrence changes with time or how comorbid conditions influence risk.
The proposed surveillance method results in shorter surveillance durations for some patients and longer surveillance durations than currently recommended for others. This diversity in stopping points “better reflects the range of disease courses appreciated in patients with RCC on the basis of the interplay that occurs between the risk of recurrence and other competing health factors,” Dr. Stewart-Merrill and associates explained.
Dr. Stewart-Merrill reported having no disclosures.
A novel approach to oncologic surveillance after surgical resection for renal cell carcinoma (RCC) that incorporates patient age, Charlson comorbidity index, pathologic tumor stage, and relapse location–specific data, may provide better recommendations for surveillance duration than current guidelines, researchers reported.
“By providing more individualized recommendations and by eliminating oversimplified time thresholds for surveillance, this strategy, we believe, represents an improvement over current guidelines,” wrote Dr. Suzanne Stewart-Merrill of the department of urology, Mayo Clinic, Rochester, Minn., and colleagues (J Clin Oncol. 2015 Sep 7. doi: 10.1200/JCO.2015.61.8009).
Guidelines suggest surveillance durations based on cumulative incidence of recurrences, but do not account for individual patient risk factors. Adherence to the guidelines could miss up to one-third of all recurrences, the authors noted. The longest surveillance duration advocated by the National Comprehensive Cancer Network or the American Urological Association is 5 years.
Researchers used Weibull models for risk of recurrence, stratified by stage and relapse location, combined with risk estimates for non-RCC death, to estimate the optimum surveillance duration. For example, for patients aged 50-59 years with pT1Nx-0 disease and a Charlson comorbidity index of less than or equal to 1, risk of non-RCC death exceeded the risk of abdominal recurrence at 7 years, marking the recommended surveillance duration for that subgroup. The recommended surveillance duration for patients with similar characteristics aged 60-69 years is 2.5 years, and for patients aged 70-79 years it is 1.5 years.
When taking into account individual risk factors, the method produced a wide range of surveillance durations. For patients under 50 years old with pT1Nx-0 disease and a Charlson comorbidity index less than or equal to 1, the risk of non-RCC death did not exceed the risk of abdominal recurrence for more than 20 years. By contrast, patients with pT1Nx-0 disease and Charlson comorbidity index greater than or equal to 2, had a higher risk of non-RCC death than risk of abdominal recurrence at 30 days after surgery.
The retrospective study of 2,511 patients who underwent surgical resection for M0 sporadic RCC between 1990 and 2008 had a median follow up of 9.0 years (interquartile range 6.4-12.7 years).
The researchers noted that recurrences beyond 5 years are fairly common, with up to 15% of patients, by one study’s estimate, experiencing recurrence during the decade following surgery. Cumulative incidence of recurrence does not capture how a patient’s risk of recurrence changes with time or how comorbid conditions influence risk.
The proposed surveillance method results in shorter surveillance durations for some patients and longer surveillance durations than currently recommended for others. This diversity in stopping points “better reflects the range of disease courses appreciated in patients with RCC on the basis of the interplay that occurs between the risk of recurrence and other competing health factors,” Dr. Stewart-Merrill and associates explained.
Dr. Stewart-Merrill reported having no disclosures.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: An individualized approach to surveillance after surgical resection in patients with renal cell carcinoma may provide better patient benefit and resource allocation.
Major finding: Weibull models for risk of recurrence, stratified by stage and relapse location, combined with risk estimates for non-RCC death, provided the basis for recommendations on surveillance duration.
Data source: Retrospective study of 2,511 patients who underwent surgical resection for M0 sporadic RCC between 1990 and 2008, with a median follow up of 9.0 years (interquartile range 6.4-12.7 years).
Disclosures: Dr. Stewart-Merrill reported having no disclosures.
Circulating tumor DNA marked progressive liver cancer
A personalized PCR test for circulating tumor DNA identified cases of progressive hepatocellular carcinoma, investigators reported in the September issue of Cellular and Molecular Gastroenterology and Hepatology.
Patients with liver cancer who underwent resection or transplantation and were positive for ctDNA had significantly higher rates of recurrence (P <.0102) and metastasis (P <.0386), reported Dr. Atsushi Ono of Hiroshima (Japan) University and the RIKEN Center for Integrative Medical Sciences and associates. The study also found that transcatheter arterial chemoembolization [TACE] increased levels of ctDNA, compared with total cell-free DNA, making the marker easier to detect.
“Analyzing cell-free DNA after TACE in unresectable and recurrent cases as a liquid biopsy to establish cancer genome profiles might … guide selection of an individualized therapeutic regimen without requiring percutaneous biopsy,” they added.
Assays for ctDNA have shown promise for diagnosing other cancers and targeting their treatments, but HCC diagnosis relies primarily on imaging, and HCC ctDNA has not been well characterized, noted the investigators. They performed massively parallel whole-genome sequencing of DNA extracted from resected HCCs from 46 patients. They serially measured plasma ctDNA levels before and after surgery using personalized quantitative PCR assays that targeted somatic rearrangements. They also used chemiluminescent immunoassays to test for two conventional tumor markers, alpha-fetoprotein and des-gamma-carboxy prothrombin (Cell Mol Gastroenterol Hepatol. 2015 Jul 2 [doi: 10.1016/j.jcmgh.2015.06.009]).
In all, 25 somatic mutations were present in both primary tumor tissue and in cell-free DNA samples, and 83% of mutations in the primary tumor were detectable in cell-free DNA. Among seven patients who tested positive for ctDNA before surgery, six developed recurrent disease and four developed extrahepatic metastases, Dr. Ono and associates said.
Levels of ctDNA increased as disease progressed and dropped in response to treatment, and one case remained positive for ctDNA even after alpha-fetoprotein and des-gamma-carboxy prothrombin became negative or dropped below threshold after resection. “This suggests that, in some patients, ctDNA might be a better and more sensitive biomarker for HCC than the conventional tumor markers,” they said.
The assay analyzed plasma instead of serum because serum was likely to have more normal cell-free nucleic acids, which would make it harder to detect mutant alleles, the investigators noted. Testing for ctDNA could help address the problem of tumor heterogeneity because ctDNA contains the entire tumor genome, including variants from independent tumors, but the assay will need further validation, especially because its lower limits varied by primer sets, which reduced its sensitivity and meant that some cases went undetected, they added.
The study was funded by the government of Japan, the RIKEN President’s Fund, the Princess Takamatsu Cancer Research Fund, and the Takeda Science Foundation. The investigators declared no competing interests.
As the oncology field advances toward implementation of personalized medicine programs, molecular and genomic analysis of circulating tumor DNA (ctDNA) represents a promising approach for diagnosis, prognosis, therapy selection, and minimal residual disease monitoring of a wide array of malignancies.

|
| Dr. Larissa Furtado |
With the purpose of assessing the utility of extracellular tumor DNA as a potential biomarker for hepatocellular carcinoma (HCC), Dr. Ono and colleagues analyzed serum ctDNA from 46 HCC patients using quantitative PCR assays for somatic rearrangements uncovered by whole-genome sequencing of their primary tumors.
For the seven patients with detectable ctDNA in preoperative serum, the incidence of recurrence and extrahepatic metastasis within 2 years following hepatectomy were significantly worse than in the ctDNA-negative group, although no significant difference in the cumulative survival rate was observed between these patients. The ctDNA positivity also was found to be an independent predictor of microscopic vascular invasion of the portal vein, and it correlated with larger tumor size and higher alpha-fetoprotein and des-gamma-carboxy prothrombin levels.
In addition, the investigators demonstrated that transcatheter arterial chemoembolization (TACE) enriched ctDNA levels in cell-free DNA in blood, and that serum ctDNA levels were increased with disease progression and reflected response to treatments.

|
| Dr. Jeremy Segal |
The diagnosis of HCC is currently based on imaging and/or biopsies. Even though there are no well-established biomarkers for early detection and monitoring of HCC at present, the data presented here indicate the potential utility of personalized ctDNA testing for individualized management of hepatocellular carcinoma patients.
Dr. Larissa V. Furtado and Dr. Jeremy P. Segal are both assistant professors and assistant directors of the division of genomic and molecular pathology in the department of pathology at the University of Chicago Medical Center. Neither has conflicts of interest.
As the oncology field advances toward implementation of personalized medicine programs, molecular and genomic analysis of circulating tumor DNA (ctDNA) represents a promising approach for diagnosis, prognosis, therapy selection, and minimal residual disease monitoring of a wide array of malignancies.

|
| Dr. Larissa Furtado |
With the purpose of assessing the utility of extracellular tumor DNA as a potential biomarker for hepatocellular carcinoma (HCC), Dr. Ono and colleagues analyzed serum ctDNA from 46 HCC patients using quantitative PCR assays for somatic rearrangements uncovered by whole-genome sequencing of their primary tumors.
For the seven patients with detectable ctDNA in preoperative serum, the incidence of recurrence and extrahepatic metastasis within 2 years following hepatectomy were significantly worse than in the ctDNA-negative group, although no significant difference in the cumulative survival rate was observed between these patients. The ctDNA positivity also was found to be an independent predictor of microscopic vascular invasion of the portal vein, and it correlated with larger tumor size and higher alpha-fetoprotein and des-gamma-carboxy prothrombin levels.
In addition, the investigators demonstrated that transcatheter arterial chemoembolization (TACE) enriched ctDNA levels in cell-free DNA in blood, and that serum ctDNA levels were increased with disease progression and reflected response to treatments.

|
| Dr. Jeremy Segal |
The diagnosis of HCC is currently based on imaging and/or biopsies. Even though there are no well-established biomarkers for early detection and monitoring of HCC at present, the data presented here indicate the potential utility of personalized ctDNA testing for individualized management of hepatocellular carcinoma patients.
Dr. Larissa V. Furtado and Dr. Jeremy P. Segal are both assistant professors and assistant directors of the division of genomic and molecular pathology in the department of pathology at the University of Chicago Medical Center. Neither has conflicts of interest.
As the oncology field advances toward implementation of personalized medicine programs, molecular and genomic analysis of circulating tumor DNA (ctDNA) represents a promising approach for diagnosis, prognosis, therapy selection, and minimal residual disease monitoring of a wide array of malignancies.

|
| Dr. Larissa Furtado |
With the purpose of assessing the utility of extracellular tumor DNA as a potential biomarker for hepatocellular carcinoma (HCC), Dr. Ono and colleagues analyzed serum ctDNA from 46 HCC patients using quantitative PCR assays for somatic rearrangements uncovered by whole-genome sequencing of their primary tumors.
For the seven patients with detectable ctDNA in preoperative serum, the incidence of recurrence and extrahepatic metastasis within 2 years following hepatectomy were significantly worse than in the ctDNA-negative group, although no significant difference in the cumulative survival rate was observed between these patients. The ctDNA positivity also was found to be an independent predictor of microscopic vascular invasion of the portal vein, and it correlated with larger tumor size and higher alpha-fetoprotein and des-gamma-carboxy prothrombin levels.
In addition, the investigators demonstrated that transcatheter arterial chemoembolization (TACE) enriched ctDNA levels in cell-free DNA in blood, and that serum ctDNA levels were increased with disease progression and reflected response to treatments.

|
| Dr. Jeremy Segal |
The diagnosis of HCC is currently based on imaging and/or biopsies. Even though there are no well-established biomarkers for early detection and monitoring of HCC at present, the data presented here indicate the potential utility of personalized ctDNA testing for individualized management of hepatocellular carcinoma patients.
Dr. Larissa V. Furtado and Dr. Jeremy P. Segal are both assistant professors and assistant directors of the division of genomic and molecular pathology in the department of pathology at the University of Chicago Medical Center. Neither has conflicts of interest.
A personalized PCR test for circulating tumor DNA identified cases of progressive hepatocellular carcinoma, investigators reported in the September issue of Cellular and Molecular Gastroenterology and Hepatology.
Patients with liver cancer who underwent resection or transplantation and were positive for ctDNA had significantly higher rates of recurrence (P <.0102) and metastasis (P <.0386), reported Dr. Atsushi Ono of Hiroshima (Japan) University and the RIKEN Center for Integrative Medical Sciences and associates. The study also found that transcatheter arterial chemoembolization [TACE] increased levels of ctDNA, compared with total cell-free DNA, making the marker easier to detect.
“Analyzing cell-free DNA after TACE in unresectable and recurrent cases as a liquid biopsy to establish cancer genome profiles might … guide selection of an individualized therapeutic regimen without requiring percutaneous biopsy,” they added.
Assays for ctDNA have shown promise for diagnosing other cancers and targeting their treatments, but HCC diagnosis relies primarily on imaging, and HCC ctDNA has not been well characterized, noted the investigators. They performed massively parallel whole-genome sequencing of DNA extracted from resected HCCs from 46 patients. They serially measured plasma ctDNA levels before and after surgery using personalized quantitative PCR assays that targeted somatic rearrangements. They also used chemiluminescent immunoassays to test for two conventional tumor markers, alpha-fetoprotein and des-gamma-carboxy prothrombin (Cell Mol Gastroenterol Hepatol. 2015 Jul 2 [doi: 10.1016/j.jcmgh.2015.06.009]).
In all, 25 somatic mutations were present in both primary tumor tissue and in cell-free DNA samples, and 83% of mutations in the primary tumor were detectable in cell-free DNA. Among seven patients who tested positive for ctDNA before surgery, six developed recurrent disease and four developed extrahepatic metastases, Dr. Ono and associates said.
Levels of ctDNA increased as disease progressed and dropped in response to treatment, and one case remained positive for ctDNA even after alpha-fetoprotein and des-gamma-carboxy prothrombin became negative or dropped below threshold after resection. “This suggests that, in some patients, ctDNA might be a better and more sensitive biomarker for HCC than the conventional tumor markers,” they said.
The assay analyzed plasma instead of serum because serum was likely to have more normal cell-free nucleic acids, which would make it harder to detect mutant alleles, the investigators noted. Testing for ctDNA could help address the problem of tumor heterogeneity because ctDNA contains the entire tumor genome, including variants from independent tumors, but the assay will need further validation, especially because its lower limits varied by primer sets, which reduced its sensitivity and meant that some cases went undetected, they added.
The study was funded by the government of Japan, the RIKEN President’s Fund, the Princess Takamatsu Cancer Research Fund, and the Takeda Science Foundation. The investigators declared no competing interests.
A personalized PCR test for circulating tumor DNA identified cases of progressive hepatocellular carcinoma, investigators reported in the September issue of Cellular and Molecular Gastroenterology and Hepatology.
Patients with liver cancer who underwent resection or transplantation and were positive for ctDNA had significantly higher rates of recurrence (P <.0102) and metastasis (P <.0386), reported Dr. Atsushi Ono of Hiroshima (Japan) University and the RIKEN Center for Integrative Medical Sciences and associates. The study also found that transcatheter arterial chemoembolization [TACE] increased levels of ctDNA, compared with total cell-free DNA, making the marker easier to detect.
“Analyzing cell-free DNA after TACE in unresectable and recurrent cases as a liquid biopsy to establish cancer genome profiles might … guide selection of an individualized therapeutic regimen without requiring percutaneous biopsy,” they added.
Assays for ctDNA have shown promise for diagnosing other cancers and targeting their treatments, but HCC diagnosis relies primarily on imaging, and HCC ctDNA has not been well characterized, noted the investigators. They performed massively parallel whole-genome sequencing of DNA extracted from resected HCCs from 46 patients. They serially measured plasma ctDNA levels before and after surgery using personalized quantitative PCR assays that targeted somatic rearrangements. They also used chemiluminescent immunoassays to test for two conventional tumor markers, alpha-fetoprotein and des-gamma-carboxy prothrombin (Cell Mol Gastroenterol Hepatol. 2015 Jul 2 [doi: 10.1016/j.jcmgh.2015.06.009]).
In all, 25 somatic mutations were present in both primary tumor tissue and in cell-free DNA samples, and 83% of mutations in the primary tumor were detectable in cell-free DNA. Among seven patients who tested positive for ctDNA before surgery, six developed recurrent disease and four developed extrahepatic metastases, Dr. Ono and associates said.
Levels of ctDNA increased as disease progressed and dropped in response to treatment, and one case remained positive for ctDNA even after alpha-fetoprotein and des-gamma-carboxy prothrombin became negative or dropped below threshold after resection. “This suggests that, in some patients, ctDNA might be a better and more sensitive biomarker for HCC than the conventional tumor markers,” they said.
The assay analyzed plasma instead of serum because serum was likely to have more normal cell-free nucleic acids, which would make it harder to detect mutant alleles, the investigators noted. Testing for ctDNA could help address the problem of tumor heterogeneity because ctDNA contains the entire tumor genome, including variants from independent tumors, but the assay will need further validation, especially because its lower limits varied by primer sets, which reduced its sensitivity and meant that some cases went undetected, they added.
The study was funded by the government of Japan, the RIKEN President’s Fund, the Princess Takamatsu Cancer Research Fund, and the Takeda Science Foundation. The investigators declared no competing interests.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: The presence of circulating tumor (ct) DNA indicated progression of hepatocellular carcinoma.
Major finding: Among seven patients who tested positive for ctDNA before undergoing surgical resection, six developed recurrent HCC and four developed extrahepatic metastases.
Data source: Real-time quantitative PCR analysis of serum samples from 46 patients with HCC who underwent hepatectomy or liver transplantation.
Disclosures: The study was funded by the government of Japan, the RIKEN President’s Fund, the Princess Takamatsu Cancer Research Fund, and the Takeda Science Foundation. The investigators declared no competing interests.
Evidence-based practices can cut breast cancer costs
HOUSTON – There are at least three evidence-based practices for reducing the costs of locoregional therapy for early breast cancer without compromising the quality of care, according to Dr. Rachel Adams Greenup of the department of surgery at Duke University Medical Center, in Durham, North Carolina.
Management of axilla per the ACOSOG Z0011 study, adherence to joint Society of Surgical Oncology/American Society of Radiation Oncology (SSO/ASTRO) margin guidelines, and alternative radiation regimens following lumpectomy can all cut costs without compromsing quality of care, she said at the annual Society of Surgical Oncology Symposium.
The results of ACOSOG Z0011, published in 2010, were universally acknowledged to be practice changing. They showed that for women undergoing lumpectomy and radiation therapy for T1-2 invasive breast cancer and positive sentinel lymph node biopsy, completion axiallary dissection did not improve either disease-free or overall survival (DFS/OS). There were low rates of locoregional recurrence regardless of whether patients received axillary node dissection.
The potential savings from eliminating the routine practice of axillary dissection were estimated to be a 64% reduction in inpatient days, and an 18% decrease in perioperative costs.
The SSO/ASTRO margin guidelines, published in 2014, were developed by a multidisciplinary panel based on a meta-analysis of 33 studies involving more than 28,000 patients. The guidelines note that positive surgical margins are associated with a 2-fold increase in ipsilateral breast tumor recurrence, with “no ink on tumor” sufficient for a negative margin. The guidelines say that further margin width resections do not decrease same-breast recurrences.
In a related analysis of the cost implications, Dr. Greenup and colleagues noted that there are wide variations in clinical practice, and that 20% of women with close but negative margins were re-excised needlessly. Eliminating 25,000 unnecessary re-excisions annually would save $31 million dollars. These savings do not include cost reductions from an estimated 8% to 12% reduction in conversions to mastectomy that would be avoided, the authors calculated.
The costs of radiation following lumpectomy correlate directly with the number of delivered radiation fractions or treatment sessions, and also with the technique. Alternatives to standard radiation schedules include the following:
Per-patient costs for each of these options in 2011 ranged from $0 for no radiation, as in CALGB 9343, to $5342 for APBI, $9122 for HF-WBI, and $13m358 for conventionally fractionated WBI.
Dr Greenup and colleagues looked at data on 43,247 women in the National Cancer Data Base with T1-T2, NO invasive breast cancers treated with lumpectomy, and compared the actual costs of treatment with the evidence-based alternative. They found that 26% of patients were treated with the least cost-effective radiation, while nearly all of the remaining patients received more expensive radiation than necessary. If every patient were treated with the most cost-effective approach, there would be an estimated 39% reduction in costs, translating into a saving of $164 million over a single year, they reported in an abstract presented at the 2014 San Antonio Breast Cancer Symposium.
“We can’t make decisions based on cost alone, and value is certainly more important, but clinical trials, moving forward, should incorporate cost information. There is an opportunity to have small changes in clinical practice have the potential to make dramatic reductions in health care spending, and there are lots of opportunities in early stage breast cancer to practice evidence-based care while reducing health care spending,” Dr. Greenup concluded.
Dr. Greenup reported having no relevant financial disclosures.
HOUSTON – There are at least three evidence-based practices for reducing the costs of locoregional therapy for early breast cancer without compromising the quality of care, according to Dr. Rachel Adams Greenup of the department of surgery at Duke University Medical Center, in Durham, North Carolina.
Management of axilla per the ACOSOG Z0011 study, adherence to joint Society of Surgical Oncology/American Society of Radiation Oncology (SSO/ASTRO) margin guidelines, and alternative radiation regimens following lumpectomy can all cut costs without compromsing quality of care, she said at the annual Society of Surgical Oncology Symposium.
The results of ACOSOG Z0011, published in 2010, were universally acknowledged to be practice changing. They showed that for women undergoing lumpectomy and radiation therapy for T1-2 invasive breast cancer and positive sentinel lymph node biopsy, completion axiallary dissection did not improve either disease-free or overall survival (DFS/OS). There were low rates of locoregional recurrence regardless of whether patients received axillary node dissection.
The potential savings from eliminating the routine practice of axillary dissection were estimated to be a 64% reduction in inpatient days, and an 18% decrease in perioperative costs.
The SSO/ASTRO margin guidelines, published in 2014, were developed by a multidisciplinary panel based on a meta-analysis of 33 studies involving more than 28,000 patients. The guidelines note that positive surgical margins are associated with a 2-fold increase in ipsilateral breast tumor recurrence, with “no ink on tumor” sufficient for a negative margin. The guidelines say that further margin width resections do not decrease same-breast recurrences.
In a related analysis of the cost implications, Dr. Greenup and colleagues noted that there are wide variations in clinical practice, and that 20% of women with close but negative margins were re-excised needlessly. Eliminating 25,000 unnecessary re-excisions annually would save $31 million dollars. These savings do not include cost reductions from an estimated 8% to 12% reduction in conversions to mastectomy that would be avoided, the authors calculated.
The costs of radiation following lumpectomy correlate directly with the number of delivered radiation fractions or treatment sessions, and also with the technique. Alternatives to standard radiation schedules include the following:
Per-patient costs for each of these options in 2011 ranged from $0 for no radiation, as in CALGB 9343, to $5342 for APBI, $9122 for HF-WBI, and $13m358 for conventionally fractionated WBI.
Dr Greenup and colleagues looked at data on 43,247 women in the National Cancer Data Base with T1-T2, NO invasive breast cancers treated with lumpectomy, and compared the actual costs of treatment with the evidence-based alternative. They found that 26% of patients were treated with the least cost-effective radiation, while nearly all of the remaining patients received more expensive radiation than necessary. If every patient were treated with the most cost-effective approach, there would be an estimated 39% reduction in costs, translating into a saving of $164 million over a single year, they reported in an abstract presented at the 2014 San Antonio Breast Cancer Symposium.
“We can’t make decisions based on cost alone, and value is certainly more important, but clinical trials, moving forward, should incorporate cost information. There is an opportunity to have small changes in clinical practice have the potential to make dramatic reductions in health care spending, and there are lots of opportunities in early stage breast cancer to practice evidence-based care while reducing health care spending,” Dr. Greenup concluded.
Dr. Greenup reported having no relevant financial disclosures.
HOUSTON – There are at least three evidence-based practices for reducing the costs of locoregional therapy for early breast cancer without compromising the quality of care, according to Dr. Rachel Adams Greenup of the department of surgery at Duke University Medical Center, in Durham, North Carolina.
Management of axilla per the ACOSOG Z0011 study, adherence to joint Society of Surgical Oncology/American Society of Radiation Oncology (SSO/ASTRO) margin guidelines, and alternative radiation regimens following lumpectomy can all cut costs without compromsing quality of care, she said at the annual Society of Surgical Oncology Symposium.
The results of ACOSOG Z0011, published in 2010, were universally acknowledged to be practice changing. They showed that for women undergoing lumpectomy and radiation therapy for T1-2 invasive breast cancer and positive sentinel lymph node biopsy, completion axiallary dissection did not improve either disease-free or overall survival (DFS/OS). There were low rates of locoregional recurrence regardless of whether patients received axillary node dissection.
The potential savings from eliminating the routine practice of axillary dissection were estimated to be a 64% reduction in inpatient days, and an 18% decrease in perioperative costs.
The SSO/ASTRO margin guidelines, published in 2014, were developed by a multidisciplinary panel based on a meta-analysis of 33 studies involving more than 28,000 patients. The guidelines note that positive surgical margins are associated with a 2-fold increase in ipsilateral breast tumor recurrence, with “no ink on tumor” sufficient for a negative margin. The guidelines say that further margin width resections do not decrease same-breast recurrences.
In a related analysis of the cost implications, Dr. Greenup and colleagues noted that there are wide variations in clinical practice, and that 20% of women with close but negative margins were re-excised needlessly. Eliminating 25,000 unnecessary re-excisions annually would save $31 million dollars. These savings do not include cost reductions from an estimated 8% to 12% reduction in conversions to mastectomy that would be avoided, the authors calculated.
The costs of radiation following lumpectomy correlate directly with the number of delivered radiation fractions or treatment sessions, and also with the technique. Alternatives to standard radiation schedules include the following:
Per-patient costs for each of these options in 2011 ranged from $0 for no radiation, as in CALGB 9343, to $5342 for APBI, $9122 for HF-WBI, and $13m358 for conventionally fractionated WBI.
Dr Greenup and colleagues looked at data on 43,247 women in the National Cancer Data Base with T1-T2, NO invasive breast cancers treated with lumpectomy, and compared the actual costs of treatment with the evidence-based alternative. They found that 26% of patients were treated with the least cost-effective radiation, while nearly all of the remaining patients received more expensive radiation than necessary. If every patient were treated with the most cost-effective approach, there would be an estimated 39% reduction in costs, translating into a saving of $164 million over a single year, they reported in an abstract presented at the 2014 San Antonio Breast Cancer Symposium.
“We can’t make decisions based on cost alone, and value is certainly more important, but clinical trials, moving forward, should incorporate cost information. There is an opportunity to have small changes in clinical practice have the potential to make dramatic reductions in health care spending, and there are lots of opportunities in early stage breast cancer to practice evidence-based care while reducing health care spending,” Dr. Greenup concluded.
Dr. Greenup reported having no relevant financial disclosures.
EXPERT ANALYSIS AT SSO 2015
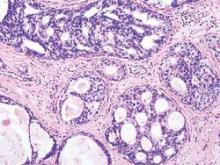
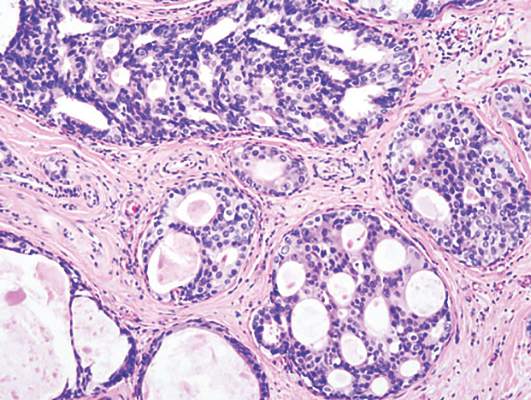
Reduced invasive recurrence after DCIS does not reduce mortality
Radiotherapy after breast-conserving surgery for ductal carcinoma in situ reduces the risk of ipsilateral invasive recurrence but does not reduce breast cancer mortality, new research shows.
Analysis of data from 108,196 women diagnosed with ductal carcinoma in situ (DCIS), who were included in the Surveillance, Epidemiology, and End Results (SEER) 18 registries database, showed radiotherapy significantly reduced the risk of ipsilateral invasive recurrence at 10 years (adjusted hazard, 0.47; 95% confidence interval, 0.42-0.53; P less than .001) but only achieved a nonsignificant reduction in breast cancer mortality (adjusted HR, 0.81; 95% CI, 0.63-1.04; P = .10).
“The finding of greatest clinical importance was that prevention of ipsilateral invasive recurrence did not prevent death from breast cancer,” wrote Dr. Steven A. Narod and his colleagues from the Women’s College Hospital and the University of Toronto.
Though it is often stated that DCIS is a preinvasive neoplastic lesion that is not lethal in itself, these results suggest that this interpretation should be revisited, they said in the report, published online August 20 in JAMA Oncology.
“Some cases of DCIS have an inherent potential for distant metastatic spread. It is therefore appropriate to consider these as de facto breast cancers and not as preinvasive markers predictive of a subsequent invasive cancer,” they said.
The mean age at diagnosis of DCIS for the women in the database was 53.8 (range, 15-69) years, and the mean duration of follow-up was 7.5 (range, 0-23.9) years. Overall, the 20-year breast cancer–specific mortality rate following a diagnosis of DCIS was 3.3% (95% CI, 3.0%-3.6%).
Just over 1% of the 42,250 women treated with lumpectomy and radiotherapy developed an ipsilateral invasive recurrence in the follow-up period and 163 women (0.4%) died of breast cancer. Of the 19,762 women who were treated with lumpectomy without radiotherapy, 595 women (3%) developed an ipsilateral invasive recurrence and 102 women (0.5%) died of breast cancer, Dr. Narod and his associates reported (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2510).
Among the 956 women who died of breast cancer in the follow-up period, over half (517) did not experience an in-breast invasive recurrence prior to death. Of the 163 women who were treated with lumpectomy and radiotherapy and then died of breast cancer, 57.7% (94) did not experience an in-breast invasive recurrence prior to death. Among the 102 women treated with lumpectomy without radiotherapy who died of breast cancer, 51 did not experience an in-breast invasive recurrence prior to death (50.0%). Among the 154 women treated with a mastectomy (unilateral or bilateral) who died of breast cancer, 112 did not experience an in-breast invasive recurrence prior to death (72.7%), the investigators reported.
They found that young age at diagnosis and black ethnicity were predictors of breast cancer mortality. Young women diagnosed with ductal carcinoma in situ before the age of 35 years had a more than twofold greater risk of dying from breast cancer than older women (7.8% vs. 3.2%; HR 2.58, 95% CI, 1.85-3.60; P less than .001). Black women also had a much greater risk of dying from breast cancer than non-Hispanic whites (7.0% vs. 3.0%; HR, 2.55, 95% CI, 2.17-3.01; P less than .001).
“If DCIS were truly a (noninvasive) precursor of breast cancer, then a woman with DCIS should not die of breast cancer without first experiencing an invasive breast cancer (ipsilateral or contralateral), and the prevention of an invasive recurrence should prevent her death from breast cancer. Surprisingly, the majority of women with DCIS in the cohort who died of breast cancer did not experience an invasive in-breast recurrence (ipsilateral or contralateral) prior to death (54.1%),” the investigators said.
“The outcome of breast cancer mortality for DCIS patients is of importance in itself and potential treatments that affect mortality are deserving of study,” they concluded.
No relevant conflicts of interest were declared.
The analysis by Dr. Narod and his associates fuels a growing concern that we should rethink our strategy for the detection and treatment of DCIS. Given the low breast cancer mortality risk, we should stop telling women that DCIS is an emergency and that they should schedule definitive surgery within 2 weeks of diagnosis. For the lowest-risk lesions, observation and prevention interventions alone should be tested. High-risk lesions (such as HER2 positive, those in patients aged less than 40 years, hormone-receptor negative, large size) should still be aggressively treated, but this analysis suggests that our current approach of surgical removal and radiation therapy may not suffice for the rare cases that lead to breast cancer mortality, so new approaches are needed.
We should continue to better understand the biological characteristics of the highest-risk DCIS and test targeted approaches to reduce death from breast cancer.
Dr. Laura Esserman and Christina Yau, Ph.D., are with the department of surgery at the University of California, San Francisco. These comments were taken from an accompanying editorial (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2607). No conflicts of interest were declared.
The analysis by Dr. Narod and his associates fuels a growing concern that we should rethink our strategy for the detection and treatment of DCIS. Given the low breast cancer mortality risk, we should stop telling women that DCIS is an emergency and that they should schedule definitive surgery within 2 weeks of diagnosis. For the lowest-risk lesions, observation and prevention interventions alone should be tested. High-risk lesions (such as HER2 positive, those in patients aged less than 40 years, hormone-receptor negative, large size) should still be aggressively treated, but this analysis suggests that our current approach of surgical removal and radiation therapy may not suffice for the rare cases that lead to breast cancer mortality, so new approaches are needed.
We should continue to better understand the biological characteristics of the highest-risk DCIS and test targeted approaches to reduce death from breast cancer.
Dr. Laura Esserman and Christina Yau, Ph.D., are with the department of surgery at the University of California, San Francisco. These comments were taken from an accompanying editorial (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2607). No conflicts of interest were declared.
The analysis by Dr. Narod and his associates fuels a growing concern that we should rethink our strategy for the detection and treatment of DCIS. Given the low breast cancer mortality risk, we should stop telling women that DCIS is an emergency and that they should schedule definitive surgery within 2 weeks of diagnosis. For the lowest-risk lesions, observation and prevention interventions alone should be tested. High-risk lesions (such as HER2 positive, those in patients aged less than 40 years, hormone-receptor negative, large size) should still be aggressively treated, but this analysis suggests that our current approach of surgical removal and radiation therapy may not suffice for the rare cases that lead to breast cancer mortality, so new approaches are needed.
We should continue to better understand the biological characteristics of the highest-risk DCIS and test targeted approaches to reduce death from breast cancer.
Dr. Laura Esserman and Christina Yau, Ph.D., are with the department of surgery at the University of California, San Francisco. These comments were taken from an accompanying editorial (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2607). No conflicts of interest were declared.
Radiotherapy after breast-conserving surgery for ductal carcinoma in situ reduces the risk of ipsilateral invasive recurrence but does not reduce breast cancer mortality, new research shows.
Analysis of data from 108,196 women diagnosed with ductal carcinoma in situ (DCIS), who were included in the Surveillance, Epidemiology, and End Results (SEER) 18 registries database, showed radiotherapy significantly reduced the risk of ipsilateral invasive recurrence at 10 years (adjusted hazard, 0.47; 95% confidence interval, 0.42-0.53; P less than .001) but only achieved a nonsignificant reduction in breast cancer mortality (adjusted HR, 0.81; 95% CI, 0.63-1.04; P = .10).
“The finding of greatest clinical importance was that prevention of ipsilateral invasive recurrence did not prevent death from breast cancer,” wrote Dr. Steven A. Narod and his colleagues from the Women’s College Hospital and the University of Toronto.
Though it is often stated that DCIS is a preinvasive neoplastic lesion that is not lethal in itself, these results suggest that this interpretation should be revisited, they said in the report, published online August 20 in JAMA Oncology.
“Some cases of DCIS have an inherent potential for distant metastatic spread. It is therefore appropriate to consider these as de facto breast cancers and not as preinvasive markers predictive of a subsequent invasive cancer,” they said.
The mean age at diagnosis of DCIS for the women in the database was 53.8 (range, 15-69) years, and the mean duration of follow-up was 7.5 (range, 0-23.9) years. Overall, the 20-year breast cancer–specific mortality rate following a diagnosis of DCIS was 3.3% (95% CI, 3.0%-3.6%).
Just over 1% of the 42,250 women treated with lumpectomy and radiotherapy developed an ipsilateral invasive recurrence in the follow-up period and 163 women (0.4%) died of breast cancer. Of the 19,762 women who were treated with lumpectomy without radiotherapy, 595 women (3%) developed an ipsilateral invasive recurrence and 102 women (0.5%) died of breast cancer, Dr. Narod and his associates reported (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2510).
Among the 956 women who died of breast cancer in the follow-up period, over half (517) did not experience an in-breast invasive recurrence prior to death. Of the 163 women who were treated with lumpectomy and radiotherapy and then died of breast cancer, 57.7% (94) did not experience an in-breast invasive recurrence prior to death. Among the 102 women treated with lumpectomy without radiotherapy who died of breast cancer, 51 did not experience an in-breast invasive recurrence prior to death (50.0%). Among the 154 women treated with a mastectomy (unilateral or bilateral) who died of breast cancer, 112 did not experience an in-breast invasive recurrence prior to death (72.7%), the investigators reported.
They found that young age at diagnosis and black ethnicity were predictors of breast cancer mortality. Young women diagnosed with ductal carcinoma in situ before the age of 35 years had a more than twofold greater risk of dying from breast cancer than older women (7.8% vs. 3.2%; HR 2.58, 95% CI, 1.85-3.60; P less than .001). Black women also had a much greater risk of dying from breast cancer than non-Hispanic whites (7.0% vs. 3.0%; HR, 2.55, 95% CI, 2.17-3.01; P less than .001).
“If DCIS were truly a (noninvasive) precursor of breast cancer, then a woman with DCIS should not die of breast cancer without first experiencing an invasive breast cancer (ipsilateral or contralateral), and the prevention of an invasive recurrence should prevent her death from breast cancer. Surprisingly, the majority of women with DCIS in the cohort who died of breast cancer did not experience an invasive in-breast recurrence (ipsilateral or contralateral) prior to death (54.1%),” the investigators said.
“The outcome of breast cancer mortality for DCIS patients is of importance in itself and potential treatments that affect mortality are deserving of study,” they concluded.
No relevant conflicts of interest were declared.
Radiotherapy after breast-conserving surgery for ductal carcinoma in situ reduces the risk of ipsilateral invasive recurrence but does not reduce breast cancer mortality, new research shows.
Analysis of data from 108,196 women diagnosed with ductal carcinoma in situ (DCIS), who were included in the Surveillance, Epidemiology, and End Results (SEER) 18 registries database, showed radiotherapy significantly reduced the risk of ipsilateral invasive recurrence at 10 years (adjusted hazard, 0.47; 95% confidence interval, 0.42-0.53; P less than .001) but only achieved a nonsignificant reduction in breast cancer mortality (adjusted HR, 0.81; 95% CI, 0.63-1.04; P = .10).
“The finding of greatest clinical importance was that prevention of ipsilateral invasive recurrence did not prevent death from breast cancer,” wrote Dr. Steven A. Narod and his colleagues from the Women’s College Hospital and the University of Toronto.
Though it is often stated that DCIS is a preinvasive neoplastic lesion that is not lethal in itself, these results suggest that this interpretation should be revisited, they said in the report, published online August 20 in JAMA Oncology.
“Some cases of DCIS have an inherent potential for distant metastatic spread. It is therefore appropriate to consider these as de facto breast cancers and not as preinvasive markers predictive of a subsequent invasive cancer,” they said.
The mean age at diagnosis of DCIS for the women in the database was 53.8 (range, 15-69) years, and the mean duration of follow-up was 7.5 (range, 0-23.9) years. Overall, the 20-year breast cancer–specific mortality rate following a diagnosis of DCIS was 3.3% (95% CI, 3.0%-3.6%).
Just over 1% of the 42,250 women treated with lumpectomy and radiotherapy developed an ipsilateral invasive recurrence in the follow-up period and 163 women (0.4%) died of breast cancer. Of the 19,762 women who were treated with lumpectomy without radiotherapy, 595 women (3%) developed an ipsilateral invasive recurrence and 102 women (0.5%) died of breast cancer, Dr. Narod and his associates reported (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2510).
Among the 956 women who died of breast cancer in the follow-up period, over half (517) did not experience an in-breast invasive recurrence prior to death. Of the 163 women who were treated with lumpectomy and radiotherapy and then died of breast cancer, 57.7% (94) did not experience an in-breast invasive recurrence prior to death. Among the 102 women treated with lumpectomy without radiotherapy who died of breast cancer, 51 did not experience an in-breast invasive recurrence prior to death (50.0%). Among the 154 women treated with a mastectomy (unilateral or bilateral) who died of breast cancer, 112 did not experience an in-breast invasive recurrence prior to death (72.7%), the investigators reported.
They found that young age at diagnosis and black ethnicity were predictors of breast cancer mortality. Young women diagnosed with ductal carcinoma in situ before the age of 35 years had a more than twofold greater risk of dying from breast cancer than older women (7.8% vs. 3.2%; HR 2.58, 95% CI, 1.85-3.60; P less than .001). Black women also had a much greater risk of dying from breast cancer than non-Hispanic whites (7.0% vs. 3.0%; HR, 2.55, 95% CI, 2.17-3.01; P less than .001).
“If DCIS were truly a (noninvasive) precursor of breast cancer, then a woman with DCIS should not die of breast cancer without first experiencing an invasive breast cancer (ipsilateral or contralateral), and the prevention of an invasive recurrence should prevent her death from breast cancer. Surprisingly, the majority of women with DCIS in the cohort who died of breast cancer did not experience an invasive in-breast recurrence (ipsilateral or contralateral) prior to death (54.1%),” the investigators said.
“The outcome of breast cancer mortality for DCIS patients is of importance in itself and potential treatments that affect mortality are deserving of study,” they concluded.
No relevant conflicts of interest were declared.
FROM JAMA ONCOLOGY
Key clinical point: Radiotherapy after ductal carcinoma in situ reduces the risk of ipsilateral invasive recurrence but does not reduce breast cancer mortality.
Major finding: Radiotherapy after DCIS halves the risk of recurrence but does not significantly impact the risk of death from breast cancer.
Data source: Observational study of data from 108,196 women diagnosed with ductal carcinoma in situ in the SEER18 registries.
Disclosures: No conflicts of interest were declared.
Solid histology predicts poor survival in resected lung adenocarcinoma
For patients with lung adenocarcinoma, a predominantly solid tumor subtype was associated with earlier recurrence and shorter postrecurrence survival (PRS). These patients were more likely to have more extrathoracic and multisite recurrences, according to a single-center retrospective record review of stage I lung adenocarcinoma patients who received surgical resection.
“Despite curative-intent surgical resection, tumor recurrence and spread remain the primary causes of cancer-related death among patients with early-stage lung cancer,” Dr. Hideki Ujiie of Memorial Sloan Kettering Cancer Center (New York), wrote in a study published online in Journal of Clinical Oncology.
To identify which tumor subtypes place patients at higher risk for recurrence after surgery, Dr. Ujiie and his colleagues reviewed records of 1,120 patients undergoing complete surgical resection for stage I lung adenocarcinoma from 1999 to 2009 at Memorial-Sloan Kettering Cancer Center.
The 2-year PRS in the patients studied was 45%, with median PRS of just over 26 months; median follow-up was 60 months. On multivariable analysis, Dr. Ujiie and coauthors found that predominantly solid tumor type was the variable most strongly associated with worse PRS (HR 1.76, 95% CI 1.11-2.77, P = .016).
“The risk of recurrence for tumors with solid predominant histologic subtype peaked within 12 months and ... these tumors were associated with a higher incidence of extrathoracic, multiple-site recurrences in patients with stage I lung adenocarcinoma,” the investigators said (J Clin Oncol. 2015 Aug 10. doi:10.1200/JCO2015.60.9818).
The study was prompted, in part, by the new International Association for the Study of Lung Cancer, American Thoracic Society, and European Respiratory Society lung cancer classification system. The new classification schema recognizes the histologic heterogeneity of lung adenocarcinoma subtypes. Dr. Ujiie and his coauthors sought to use these characterizations to develop prognostic factors for recurrence risk and PRS. Their findings have clinical implications: “[R]egular surveillance is even more important when tumors of aggressive predominant subtypes (e.g., solid predominant histologic pattern) are present,” said Dr. Ujiie and his coauthors.
The National Institutes of Health and the U.S. Department of Defense supported the study. Dr. Chaft reported ties with DAVA Oncology, Myriad Genetics, Biodesix, Otsuka, and Eli Lilly. Dr. Sima is employed by Genentech/Roche. Dr. Huang received funding from Bristol-Myers Squibb. Dr. Rudin reported ties with AbbVia, Aveo Pharmaceuticals, Boehringer Ingelheim, GlaxoSmithKlin, Merck, Celgene, and BioMarin Pharmaceutical. Dr. Adusumilli received funding from Myriad Genetics. The other authors reported no disclosures.
On Twitter: @karioakes
For patients with lung adenocarcinoma, a predominantly solid tumor subtype was associated with earlier recurrence and shorter postrecurrence survival (PRS). These patients were more likely to have more extrathoracic and multisite recurrences, according to a single-center retrospective record review of stage I lung adenocarcinoma patients who received surgical resection.
“Despite curative-intent surgical resection, tumor recurrence and spread remain the primary causes of cancer-related death among patients with early-stage lung cancer,” Dr. Hideki Ujiie of Memorial Sloan Kettering Cancer Center (New York), wrote in a study published online in Journal of Clinical Oncology.
To identify which tumor subtypes place patients at higher risk for recurrence after surgery, Dr. Ujiie and his colleagues reviewed records of 1,120 patients undergoing complete surgical resection for stage I lung adenocarcinoma from 1999 to 2009 at Memorial-Sloan Kettering Cancer Center.
The 2-year PRS in the patients studied was 45%, with median PRS of just over 26 months; median follow-up was 60 months. On multivariable analysis, Dr. Ujiie and coauthors found that predominantly solid tumor type was the variable most strongly associated with worse PRS (HR 1.76, 95% CI 1.11-2.77, P = .016).
“The risk of recurrence for tumors with solid predominant histologic subtype peaked within 12 months and ... these tumors were associated with a higher incidence of extrathoracic, multiple-site recurrences in patients with stage I lung adenocarcinoma,” the investigators said (J Clin Oncol. 2015 Aug 10. doi:10.1200/JCO2015.60.9818).
The study was prompted, in part, by the new International Association for the Study of Lung Cancer, American Thoracic Society, and European Respiratory Society lung cancer classification system. The new classification schema recognizes the histologic heterogeneity of lung adenocarcinoma subtypes. Dr. Ujiie and his coauthors sought to use these characterizations to develop prognostic factors for recurrence risk and PRS. Their findings have clinical implications: “[R]egular surveillance is even more important when tumors of aggressive predominant subtypes (e.g., solid predominant histologic pattern) are present,” said Dr. Ujiie and his coauthors.
The National Institutes of Health and the U.S. Department of Defense supported the study. Dr. Chaft reported ties with DAVA Oncology, Myriad Genetics, Biodesix, Otsuka, and Eli Lilly. Dr. Sima is employed by Genentech/Roche. Dr. Huang received funding from Bristol-Myers Squibb. Dr. Rudin reported ties with AbbVia, Aveo Pharmaceuticals, Boehringer Ingelheim, GlaxoSmithKlin, Merck, Celgene, and BioMarin Pharmaceutical. Dr. Adusumilli received funding from Myriad Genetics. The other authors reported no disclosures.
On Twitter: @karioakes
For patients with lung adenocarcinoma, a predominantly solid tumor subtype was associated with earlier recurrence and shorter postrecurrence survival (PRS). These patients were more likely to have more extrathoracic and multisite recurrences, according to a single-center retrospective record review of stage I lung adenocarcinoma patients who received surgical resection.
“Despite curative-intent surgical resection, tumor recurrence and spread remain the primary causes of cancer-related death among patients with early-stage lung cancer,” Dr. Hideki Ujiie of Memorial Sloan Kettering Cancer Center (New York), wrote in a study published online in Journal of Clinical Oncology.
To identify which tumor subtypes place patients at higher risk for recurrence after surgery, Dr. Ujiie and his colleagues reviewed records of 1,120 patients undergoing complete surgical resection for stage I lung adenocarcinoma from 1999 to 2009 at Memorial-Sloan Kettering Cancer Center.
The 2-year PRS in the patients studied was 45%, with median PRS of just over 26 months; median follow-up was 60 months. On multivariable analysis, Dr. Ujiie and coauthors found that predominantly solid tumor type was the variable most strongly associated with worse PRS (HR 1.76, 95% CI 1.11-2.77, P = .016).
“The risk of recurrence for tumors with solid predominant histologic subtype peaked within 12 months and ... these tumors were associated with a higher incidence of extrathoracic, multiple-site recurrences in patients with stage I lung adenocarcinoma,” the investigators said (J Clin Oncol. 2015 Aug 10. doi:10.1200/JCO2015.60.9818).
The study was prompted, in part, by the new International Association for the Study of Lung Cancer, American Thoracic Society, and European Respiratory Society lung cancer classification system. The new classification schema recognizes the histologic heterogeneity of lung adenocarcinoma subtypes. Dr. Ujiie and his coauthors sought to use these characterizations to develop prognostic factors for recurrence risk and PRS. Their findings have clinical implications: “[R]egular surveillance is even more important when tumors of aggressive predominant subtypes (e.g., solid predominant histologic pattern) are present,” said Dr. Ujiie and his coauthors.
The National Institutes of Health and the U.S. Department of Defense supported the study. Dr. Chaft reported ties with DAVA Oncology, Myriad Genetics, Biodesix, Otsuka, and Eli Lilly. Dr. Sima is employed by Genentech/Roche. Dr. Huang received funding from Bristol-Myers Squibb. Dr. Rudin reported ties with AbbVia, Aveo Pharmaceuticals, Boehringer Ingelheim, GlaxoSmithKlin, Merck, Celgene, and BioMarin Pharmaceutical. Dr. Adusumilli received funding from Myriad Genetics. The other authors reported no disclosures.
On Twitter: @karioakes
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Predominantly solid tumor histology predicted earlier recurrence and poorer postrecurrence survival (PRS) in surgically resected stage I lung adenocarcinoma.
Major finding: Lung adenocarcinoma patients with predominantly solid tumor subtype had worse PRS than did those with other subtypes after surgical resection (HR, 1.76, P = .016).
Data source: Retrospective, single-site medical record review of 1,120 patients undergoing complete resection for stage I lung adenocarcinoma from 1999 to 2009.
Disclosures: The National Institutes of Health and the U.S. Department of Defense supported the study. Dr. Chaft reported ties with DAVA Oncology, Myriad Genetics, Biodesix, Otsuka, and Eli Lilly. Dr. Sima is employed by Genentech/Roche. Dr. Huang received funding from Bristol-Myers Squibb. Dr. Rudin reported ties with AbbVia, Aveo Pharmaceuticals, Boehringer Ingelheim, GlaxoSmithKlin, Merck, Celgene, and BioMarin Pharmaceutical. Dr. Adusumilli received funding from Myriad Genetics. The other authors reported no disclosures.
Limited resection inferior for elderly with early NSCLC
Limited resection is inferior to lobectomy for older patients with early-stage invasive NSCLC, yielding lower overall survival and cancer-specific survival, according to a study published online Aug. 3 in Journal of Clinical Oncology.
Limited resection – wedge resection or segmentectomy – is increasingly chosen over lobectomy for patients older than 65 because it is thought to yield equivalent survival among patients who are already near the end of their lives and to cut down on perioperative and postoperative complications. Moreover, the number of these surgeries is expected to increase substantially when the recently released U.S. Preventive Services Task Force recommendations for lung cancer screening are fully implemented, said Dr. Rajwanth R. Veluswamy of the division of hematology and medical oncology, Mount Sinai University, New York, and his associates.
However, the evidence supporting the equivalency of limited resection to lobectomy is scant and not of high quality. To examine the issue more closely, the investigators analyzed survival outcomes for 3,147 patients aged 65 and older who were included in the nationally representative population-based Surveillance, Epidemiology, and End Results (SEER) database. These patients had stage 1A NSCLC of 2 cm or less in diameter and were treated surgically in 1998 through 2009.
Limited resection was found to be inferior to lobectomy regarding overall survival (HR, 1.21) and lung cancer–specific survival (HR, 1.66) among patients with invasive adenocarcinoma. Limited resection also was inferior to lobectomy regarding overall survival (HR, 1.21) and lung cancer–specific survival (HR, 1.41) among patients with squamous cell carcinoma, Dr. Veluswamy and his associates said (J Clin Oncol. 2015 Aug. 3. doi:10.1200/JCO.2014.60.6624).
“Our findings should help decide the best treatment for older patients by balancing the potential short- and long-term risks of limited resection versus lobectomy,” they said.
The investigators added that they focused on patients older than age 65 because that is the age group most frequently affected by invasive NSCLC and most likely to be considered for limited resection. These results cannot be extrapolated to younger patients because they have longer life expectancies and thus higher risk of recurrence after “limited” treatment.
The U.S. Agency for Healthcare Research and Quality supported the study. Dr. Veluswamy had no disclosures; his associates reported ties to Pfizer, Otsuka, Teva Neuroscience, EHE International, United BioSource, Ethicon, Covidien, Genentech, IMS Health, Merck, Bristol-Myers Squibb, Quintiles, and Sanofi.
Limited resection is inferior to lobectomy for older patients with early-stage invasive NSCLC, yielding lower overall survival and cancer-specific survival, according to a study published online Aug. 3 in Journal of Clinical Oncology.
Limited resection – wedge resection or segmentectomy – is increasingly chosen over lobectomy for patients older than 65 because it is thought to yield equivalent survival among patients who are already near the end of their lives and to cut down on perioperative and postoperative complications. Moreover, the number of these surgeries is expected to increase substantially when the recently released U.S. Preventive Services Task Force recommendations for lung cancer screening are fully implemented, said Dr. Rajwanth R. Veluswamy of the division of hematology and medical oncology, Mount Sinai University, New York, and his associates.
However, the evidence supporting the equivalency of limited resection to lobectomy is scant and not of high quality. To examine the issue more closely, the investigators analyzed survival outcomes for 3,147 patients aged 65 and older who were included in the nationally representative population-based Surveillance, Epidemiology, and End Results (SEER) database. These patients had stage 1A NSCLC of 2 cm or less in diameter and were treated surgically in 1998 through 2009.
Limited resection was found to be inferior to lobectomy regarding overall survival (HR, 1.21) and lung cancer–specific survival (HR, 1.66) among patients with invasive adenocarcinoma. Limited resection also was inferior to lobectomy regarding overall survival (HR, 1.21) and lung cancer–specific survival (HR, 1.41) among patients with squamous cell carcinoma, Dr. Veluswamy and his associates said (J Clin Oncol. 2015 Aug. 3. doi:10.1200/JCO.2014.60.6624).
“Our findings should help decide the best treatment for older patients by balancing the potential short- and long-term risks of limited resection versus lobectomy,” they said.
The investigators added that they focused on patients older than age 65 because that is the age group most frequently affected by invasive NSCLC and most likely to be considered for limited resection. These results cannot be extrapolated to younger patients because they have longer life expectancies and thus higher risk of recurrence after “limited” treatment.
The U.S. Agency for Healthcare Research and Quality supported the study. Dr. Veluswamy had no disclosures; his associates reported ties to Pfizer, Otsuka, Teva Neuroscience, EHE International, United BioSource, Ethicon, Covidien, Genentech, IMS Health, Merck, Bristol-Myers Squibb, Quintiles, and Sanofi.
Limited resection is inferior to lobectomy for older patients with early-stage invasive NSCLC, yielding lower overall survival and cancer-specific survival, according to a study published online Aug. 3 in Journal of Clinical Oncology.
Limited resection – wedge resection or segmentectomy – is increasingly chosen over lobectomy for patients older than 65 because it is thought to yield equivalent survival among patients who are already near the end of their lives and to cut down on perioperative and postoperative complications. Moreover, the number of these surgeries is expected to increase substantially when the recently released U.S. Preventive Services Task Force recommendations for lung cancer screening are fully implemented, said Dr. Rajwanth R. Veluswamy of the division of hematology and medical oncology, Mount Sinai University, New York, and his associates.
However, the evidence supporting the equivalency of limited resection to lobectomy is scant and not of high quality. To examine the issue more closely, the investigators analyzed survival outcomes for 3,147 patients aged 65 and older who were included in the nationally representative population-based Surveillance, Epidemiology, and End Results (SEER) database. These patients had stage 1A NSCLC of 2 cm or less in diameter and were treated surgically in 1998 through 2009.
Limited resection was found to be inferior to lobectomy regarding overall survival (HR, 1.21) and lung cancer–specific survival (HR, 1.66) among patients with invasive adenocarcinoma. Limited resection also was inferior to lobectomy regarding overall survival (HR, 1.21) and lung cancer–specific survival (HR, 1.41) among patients with squamous cell carcinoma, Dr. Veluswamy and his associates said (J Clin Oncol. 2015 Aug. 3. doi:10.1200/JCO.2014.60.6624).
“Our findings should help decide the best treatment for older patients by balancing the potential short- and long-term risks of limited resection versus lobectomy,” they said.
The investigators added that they focused on patients older than age 65 because that is the age group most frequently affected by invasive NSCLC and most likely to be considered for limited resection. These results cannot be extrapolated to younger patients because they have longer life expectancies and thus higher risk of recurrence after “limited” treatment.
The U.S. Agency for Healthcare Research and Quality supported the study. Dr. Veluswamy had no disclosures; his associates reported ties to Pfizer, Otsuka, Teva Neuroscience, EHE International, United BioSource, Ethicon, Covidien, Genentech, IMS Health, Merck, Bristol-Myers Squibb, Quintiles, and Sanofi.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Limited resection is inferior to lobectomy for older patients with early-stage invasive NSCLC.
Major finding: Limited resection was found to be inferior to lobectomy regarding overall survival (HR, 1.21) and lung cancer–specific survival (HR, 1.66) among patients with invasive adenocarcinoma. Limited resection also was inferior to lobectomy regarding overall survival (HR, 1.21) and lung cancer–specific survival (HR, 1.41) among patients with squamous cell carcinoma, .
Data source: An analysis of population-based data of survival outcomes in 3,147 older patients with early-stage invasive NSCLC treated surgically in 1998-2009.
Disclosures: The U.S. Agency for Healthcare Research and Quality supported the study. Dr. Veluswamy had no disclosures; his associates reported ties to Pfizer, Otsuka, Teva Neuroscience, EHE International, United BioSource, Ethicon, Covidien, Genentech, IMS Health, Merck, Bristol-Myers Squibb, Quintiles, and Sanofi.
Similar outcomes for salvage vs. planned surgery after chemoradiotherapy in esophageal cancer
For patients with esophageal cancer, salvage surgery after definitive chemoradiotherapy had similar mortality and morbidity rates, and similar survival outcomes, to the combination of neoadjuvant chemoradiation and planned surgery, according to a study published online in the Journal of Clinical Oncology.
Definitive chemoradiotherapy (dCRT) is an alternative to highly invasive surgical resection, which carries a significant rate of morbidity and mortality; however, recent data indicate that 50% of patients with complete response to dCRT experience tumor recurrence.
“Our study demonstrated a similar survival and recurrence pattern for the SALV [salvage surgery after definitive chemoradiotherapy] and NCRS [neoadjuvant chemoradiation and planned surgery] groups, potentially validating an approach of dCRT with reserved SALV for persistent or recurrent disease. Importantly, there were no differences in oncologic safety of surgery, including extent of nodal dissection, between the SALV and NCRS groups,” wrote Dr. Sheraz Markar, a clinical research fellow from Imperial College, London, and colleagues (Journ. Clin. Onc. 2015 July 20 [doi:10.1200/JCO.2014.59.9092]).
The retrospective study compared 308 patients with esophageal cancer who underwent SALV with 540 patients who received NCRS at European centers from 2000 to 2010. After a median follow up of 54 months, the SALV and NCRS groups had similar rates of 3-year overall survival (43.3% vs. 40.1% ) and disease-free survival (39.2% vs. 32.8%). The two groups also had similar rates tumor recurrence: overall (46.8% vs. 47.9%), locoregional (18.8% vs. 15.9%), distant (24.3% vs. 28.1%) and mixed (13.0% vs. 13.5%).
The SALV and NCRS groups had similar rates of in-hospital mortality (8.4% vs. 9.3%) and morbidity (63.6% vs. 58.9%), but SALV patients had significantly more complications from anastomotic leak (17.2% vs. 10.7%) and surgical site infection (18.5% vs. 12.2%).
Subset analysis of the SALV group showed that patients who received a total radiation dose ≥ 55 Gy (compared with SALV patients who received a lower dose) had significantly increased in-hospital mortality (27.8% vs. 4.3%; P < .001), overall morbidity (75.9% vs. 61%; P = .039), anastomotic leak (27.8% vs. 15%; P = .023), surgical site infection (29.6% vs. 16.1%; P = .02), and pulmonary complications (55.6% vs. 40.2%; P = .038).
“Currently, there is no evidence in terms of locoregional control or survival benefit to support a high total radiation dose (> 50 Gy) in patients receiving dCRT,” according to the researchers, who noted that the findings suggest, “an upper threshold of 50 Gy should be used in these patients to optimize the benefits of dCRT without compromising the safety of SALV, if required.”
Patients who underwent SALV at high-volume centers had significantly lower rates of in-hospital mortality (6.3% vs. 16.2%; P = .009) and overall morbidity (58.8% vs. 80.9%; P = .001) compared with procedures done at low-volume centers.
Compared with recurrent disease, patients with persistent disease after dCRT had poorer long-term prognoses, suggesting a more aggressive tumor biology. Early identification of CRT-resistant tumors to allow early surgical treatment is an important area for future investigation, the investigators said.
For patients with esophageal cancer, salvage surgery after definitive chemoradiotherapy had similar mortality and morbidity rates, and similar survival outcomes, to the combination of neoadjuvant chemoradiation and planned surgery, according to a study published online in the Journal of Clinical Oncology.
Definitive chemoradiotherapy (dCRT) is an alternative to highly invasive surgical resection, which carries a significant rate of morbidity and mortality; however, recent data indicate that 50% of patients with complete response to dCRT experience tumor recurrence.
“Our study demonstrated a similar survival and recurrence pattern for the SALV [salvage surgery after definitive chemoradiotherapy] and NCRS [neoadjuvant chemoradiation and planned surgery] groups, potentially validating an approach of dCRT with reserved SALV for persistent or recurrent disease. Importantly, there were no differences in oncologic safety of surgery, including extent of nodal dissection, between the SALV and NCRS groups,” wrote Dr. Sheraz Markar, a clinical research fellow from Imperial College, London, and colleagues (Journ. Clin. Onc. 2015 July 20 [doi:10.1200/JCO.2014.59.9092]).
The retrospective study compared 308 patients with esophageal cancer who underwent SALV with 540 patients who received NCRS at European centers from 2000 to 2010. After a median follow up of 54 months, the SALV and NCRS groups had similar rates of 3-year overall survival (43.3% vs. 40.1% ) and disease-free survival (39.2% vs. 32.8%). The two groups also had similar rates tumor recurrence: overall (46.8% vs. 47.9%), locoregional (18.8% vs. 15.9%), distant (24.3% vs. 28.1%) and mixed (13.0% vs. 13.5%).
The SALV and NCRS groups had similar rates of in-hospital mortality (8.4% vs. 9.3%) and morbidity (63.6% vs. 58.9%), but SALV patients had significantly more complications from anastomotic leak (17.2% vs. 10.7%) and surgical site infection (18.5% vs. 12.2%).
Subset analysis of the SALV group showed that patients who received a total radiation dose ≥ 55 Gy (compared with SALV patients who received a lower dose) had significantly increased in-hospital mortality (27.8% vs. 4.3%; P < .001), overall morbidity (75.9% vs. 61%; P = .039), anastomotic leak (27.8% vs. 15%; P = .023), surgical site infection (29.6% vs. 16.1%; P = .02), and pulmonary complications (55.6% vs. 40.2%; P = .038).
“Currently, there is no evidence in terms of locoregional control or survival benefit to support a high total radiation dose (> 50 Gy) in patients receiving dCRT,” according to the researchers, who noted that the findings suggest, “an upper threshold of 50 Gy should be used in these patients to optimize the benefits of dCRT without compromising the safety of SALV, if required.”
Patients who underwent SALV at high-volume centers had significantly lower rates of in-hospital mortality (6.3% vs. 16.2%; P = .009) and overall morbidity (58.8% vs. 80.9%; P = .001) compared with procedures done at low-volume centers.
Compared with recurrent disease, patients with persistent disease after dCRT had poorer long-term prognoses, suggesting a more aggressive tumor biology. Early identification of CRT-resistant tumors to allow early surgical treatment is an important area for future investigation, the investigators said.
For patients with esophageal cancer, salvage surgery after definitive chemoradiotherapy had similar mortality and morbidity rates, and similar survival outcomes, to the combination of neoadjuvant chemoradiation and planned surgery, according to a study published online in the Journal of Clinical Oncology.
Definitive chemoradiotherapy (dCRT) is an alternative to highly invasive surgical resection, which carries a significant rate of morbidity and mortality; however, recent data indicate that 50% of patients with complete response to dCRT experience tumor recurrence.
“Our study demonstrated a similar survival and recurrence pattern for the SALV [salvage surgery after definitive chemoradiotherapy] and NCRS [neoadjuvant chemoradiation and planned surgery] groups, potentially validating an approach of dCRT with reserved SALV for persistent or recurrent disease. Importantly, there were no differences in oncologic safety of surgery, including extent of nodal dissection, between the SALV and NCRS groups,” wrote Dr. Sheraz Markar, a clinical research fellow from Imperial College, London, and colleagues (Journ. Clin. Onc. 2015 July 20 [doi:10.1200/JCO.2014.59.9092]).
The retrospective study compared 308 patients with esophageal cancer who underwent SALV with 540 patients who received NCRS at European centers from 2000 to 2010. After a median follow up of 54 months, the SALV and NCRS groups had similar rates of 3-year overall survival (43.3% vs. 40.1% ) and disease-free survival (39.2% vs. 32.8%). The two groups also had similar rates tumor recurrence: overall (46.8% vs. 47.9%), locoregional (18.8% vs. 15.9%), distant (24.3% vs. 28.1%) and mixed (13.0% vs. 13.5%).
The SALV and NCRS groups had similar rates of in-hospital mortality (8.4% vs. 9.3%) and morbidity (63.6% vs. 58.9%), but SALV patients had significantly more complications from anastomotic leak (17.2% vs. 10.7%) and surgical site infection (18.5% vs. 12.2%).
Subset analysis of the SALV group showed that patients who received a total radiation dose ≥ 55 Gy (compared with SALV patients who received a lower dose) had significantly increased in-hospital mortality (27.8% vs. 4.3%; P < .001), overall morbidity (75.9% vs. 61%; P = .039), anastomotic leak (27.8% vs. 15%; P = .023), surgical site infection (29.6% vs. 16.1%; P = .02), and pulmonary complications (55.6% vs. 40.2%; P = .038).
“Currently, there is no evidence in terms of locoregional control or survival benefit to support a high total radiation dose (> 50 Gy) in patients receiving dCRT,” according to the researchers, who noted that the findings suggest, “an upper threshold of 50 Gy should be used in these patients to optimize the benefits of dCRT without compromising the safety of SALV, if required.”
Patients who underwent SALV at high-volume centers had significantly lower rates of in-hospital mortality (6.3% vs. 16.2%; P = .009) and overall morbidity (58.8% vs. 80.9%; P = .001) compared with procedures done at low-volume centers.
Compared with recurrent disease, patients with persistent disease after dCRT had poorer long-term prognoses, suggesting a more aggressive tumor biology. Early identification of CRT-resistant tumors to allow early surgical treatment is an important area for future investigation, the investigators said.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: As management for esophageal cancer, salvage esophagectomy after definitive chemoradiotherapy (SALV) produced similar outcomes to the combination of neoadjuvant chemoradiation and planned surgery (NCRS).
Major finding: The SALV and NCRS groups had similar rates of 3-year overall survival (43.3% vs. 40.1% ) and disease-free survival (39.2% vs. 32.8%), tumor recurrence (46.8% vs. 47.9%), and in-hospital mortality (8.4% vs. 9.3%) and morbidity (63.6% vs. 58.9%).
Data source: Retrospective analysis of 848 patients (308 SALV, 540 NCRS) who underwent surgical resection for esophageal cancer in French-speaking European centers from 2000 to 2010.
Disclosures: Dr. Markar reported having no disclosures. Two of his coauthors reported ties to industry.