User login
The longevity gene: Healthy mutant reverses heart aging
Everybody wants a younger heart
As more people live well past 90, scientists have been taking a closer look at how they’ve been doing it. Mostly it boiled down to genetics. You either had it or you didn’t. Well, a recent study suggests that doesn’t have to be true anymore, at least for the heart.
Scientists from the United Kingdom and Italy found an antiaging gene in some centenarians that has shown possible antiaging effects in mice and in human heart cells. A single administration of the mutant antiaging gene, they found, stopped heart function decay in middle-aged mice and even reversed the biological clock by the human equivalent of 10 years in elderly mice.
When the researchers applied the antiaging gene to samples of human heart cells from elderly people with heart problems, the cells “resumed functioning properly, proving to be more efficient in building new blood vessels,” they said in a written statement. It all kind of sounds like something out of Dr. Frankenstein’s lab.
I want to believe … in better sleep
The “X-Files” theme song plays. Mulder and Scully are sitting in a diner, breakfast laid out around them. The diner is quiet, with only a few people inside.
Mulder: I’m telling you, Scully, there’s something spooky going on here.
Scully: You mean other than the fact that this town in Georgia looks suspiciously like Vancouver?
Mulder: Not one person we spoke to yesterday has gotten a full night’s sleep since the UFO sighting last month. I’m telling you, they’re here, they’re experimenting.
Scully: Do you really want me to do this to you again?
Mulder: Do what again?
Scully: There’s nothing going on here that can’t be explained by the current research. Why, in January 2023 a study was published revealing a link between poor sleep and belief in paranormal phenomena like UFOS, demons, or ghosts. Which probably explains why you’re on your third cup of coffee for the morning.
Mulder: Scully, you’ve literally been abducted by aliens. Do we have to play this game every time?
Scully: Look, it’s simple. In a sample of nearly 9,000 people, nearly two-thirds of those who reported experiencing sleep paralysis or exploding head syndrome reported believing in UFOs and aliens walking amongst humanity, despite making up just 3% of the overall sample.
Furthermore, about 60% of those reporting sleep paralysis also reported believing near-death experiences prove the soul lingers on after death, and those with stronger insomnia symptoms were more likely to believe in the devil.
Mulder: Aha!
Scully: Aha what?
Mulder: You’re a devout Christian. You believe in the devil and the soul.
Scully: Yes, but I don’t let it interfere with a good night’s sleep, Mulder. These people saw something strange, convinced themselves it was a UFO, and now they can’t sleep. It’s a vicious cycle. The study authors even said that people experiencing strange nighttime phenomena could interpret this as evidence of aliens or other paranormal beings, thus making them even more susceptible to further sleep disruption and deepening beliefs. Look who I’m talking to.
Mulder: Always with the facts, eh?
Scully: I am a doctor, after all. And if you want more research into how paranormal belief and poor sleep quality are linked, I’d be happy to dig out the literature, because the truth is out there, Mulder.
Mulder: I hate you sometimes.
It’s ChatGPT’s world. We’re just living in it
Have you heard about ChatGPT? The artificial intelligence chatbot was just launched in November and it’s already more important to the Internet than either Vladimir Putin or “Rick and Morty.”
What’s that? You’re wondering why you should care? Well, excuuuuuse us, but we thought you might want to know that ChatGPT is in the process of taking over the world. Let’s take a quick look at what it’s been up to.
“ChatGPT bot passes law school exam”
“ChatGPT passes MBA exam given by a Wharton professor”
“A freelance writer says ChatGPT wrote a $600 article in just 30 seconds”
And here’s one that might be of interest to those of the health care persuasion: “ChatGPT can pass part of the U.S. Medical Licensing Exam.” See? It’s coming for you, too.
The artificial intelligence known as ChatGPT “performed at >50% accuracy across [the three USMLE] examinations, exceeding 60% in most analyses,” a group of researchers wrote on the preprint server medRxiv, noting that 60% is usually the pass threshold for humans taking the exam in any given year.
ChatGPT was not given any special medical training before the exam, but the investigators pointed out that another AI, PubMedGPT, which is trained exclusively on biomedical domain literature, was only 50.8% accurate on the USMLE. Its reliance on “ongoing academic discourse that tends to be inconclusive, contradictory, or highly conservative or noncommittal in its language” was its undoing, the team suggested.
To top it off, ChatGPT is listed as one of the authors at the top of the medRxiv report, with an acknowledgment at the end saying that “ChatGPT contributed to the writing of several sections of this manuscript.”
We’ve said it before, and no doubt we’ll say it again: We’re doomed.
Everybody wants a younger heart
As more people live well past 90, scientists have been taking a closer look at how they’ve been doing it. Mostly it boiled down to genetics. You either had it or you didn’t. Well, a recent study suggests that doesn’t have to be true anymore, at least for the heart.
Scientists from the United Kingdom and Italy found an antiaging gene in some centenarians that has shown possible antiaging effects in mice and in human heart cells. A single administration of the mutant antiaging gene, they found, stopped heart function decay in middle-aged mice and even reversed the biological clock by the human equivalent of 10 years in elderly mice.
When the researchers applied the antiaging gene to samples of human heart cells from elderly people with heart problems, the cells “resumed functioning properly, proving to be more efficient in building new blood vessels,” they said in a written statement. It all kind of sounds like something out of Dr. Frankenstein’s lab.
I want to believe … in better sleep
The “X-Files” theme song plays. Mulder and Scully are sitting in a diner, breakfast laid out around them. The diner is quiet, with only a few people inside.
Mulder: I’m telling you, Scully, there’s something spooky going on here.
Scully: You mean other than the fact that this town in Georgia looks suspiciously like Vancouver?
Mulder: Not one person we spoke to yesterday has gotten a full night’s sleep since the UFO sighting last month. I’m telling you, they’re here, they’re experimenting.
Scully: Do you really want me to do this to you again?
Mulder: Do what again?
Scully: There’s nothing going on here that can’t be explained by the current research. Why, in January 2023 a study was published revealing a link between poor sleep and belief in paranormal phenomena like UFOS, demons, or ghosts. Which probably explains why you’re on your third cup of coffee for the morning.
Mulder: Scully, you’ve literally been abducted by aliens. Do we have to play this game every time?
Scully: Look, it’s simple. In a sample of nearly 9,000 people, nearly two-thirds of those who reported experiencing sleep paralysis or exploding head syndrome reported believing in UFOs and aliens walking amongst humanity, despite making up just 3% of the overall sample.
Furthermore, about 60% of those reporting sleep paralysis also reported believing near-death experiences prove the soul lingers on after death, and those with stronger insomnia symptoms were more likely to believe in the devil.
Mulder: Aha!
Scully: Aha what?
Mulder: You’re a devout Christian. You believe in the devil and the soul.
Scully: Yes, but I don’t let it interfere with a good night’s sleep, Mulder. These people saw something strange, convinced themselves it was a UFO, and now they can’t sleep. It’s a vicious cycle. The study authors even said that people experiencing strange nighttime phenomena could interpret this as evidence of aliens or other paranormal beings, thus making them even more susceptible to further sleep disruption and deepening beliefs. Look who I’m talking to.
Mulder: Always with the facts, eh?
Scully: I am a doctor, after all. And if you want more research into how paranormal belief and poor sleep quality are linked, I’d be happy to dig out the literature, because the truth is out there, Mulder.
Mulder: I hate you sometimes.
It’s ChatGPT’s world. We’re just living in it
Have you heard about ChatGPT? The artificial intelligence chatbot was just launched in November and it’s already more important to the Internet than either Vladimir Putin or “Rick and Morty.”
What’s that? You’re wondering why you should care? Well, excuuuuuse us, but we thought you might want to know that ChatGPT is in the process of taking over the world. Let’s take a quick look at what it’s been up to.
“ChatGPT bot passes law school exam”
“ChatGPT passes MBA exam given by a Wharton professor”
“A freelance writer says ChatGPT wrote a $600 article in just 30 seconds”
And here’s one that might be of interest to those of the health care persuasion: “ChatGPT can pass part of the U.S. Medical Licensing Exam.” See? It’s coming for you, too.
The artificial intelligence known as ChatGPT “performed at >50% accuracy across [the three USMLE] examinations, exceeding 60% in most analyses,” a group of researchers wrote on the preprint server medRxiv, noting that 60% is usually the pass threshold for humans taking the exam in any given year.
ChatGPT was not given any special medical training before the exam, but the investigators pointed out that another AI, PubMedGPT, which is trained exclusively on biomedical domain literature, was only 50.8% accurate on the USMLE. Its reliance on “ongoing academic discourse that tends to be inconclusive, contradictory, or highly conservative or noncommittal in its language” was its undoing, the team suggested.
To top it off, ChatGPT is listed as one of the authors at the top of the medRxiv report, with an acknowledgment at the end saying that “ChatGPT contributed to the writing of several sections of this manuscript.”
We’ve said it before, and no doubt we’ll say it again: We’re doomed.
Everybody wants a younger heart
As more people live well past 90, scientists have been taking a closer look at how they’ve been doing it. Mostly it boiled down to genetics. You either had it or you didn’t. Well, a recent study suggests that doesn’t have to be true anymore, at least for the heart.
Scientists from the United Kingdom and Italy found an antiaging gene in some centenarians that has shown possible antiaging effects in mice and in human heart cells. A single administration of the mutant antiaging gene, they found, stopped heart function decay in middle-aged mice and even reversed the biological clock by the human equivalent of 10 years in elderly mice.
When the researchers applied the antiaging gene to samples of human heart cells from elderly people with heart problems, the cells “resumed functioning properly, proving to be more efficient in building new blood vessels,” they said in a written statement. It all kind of sounds like something out of Dr. Frankenstein’s lab.
I want to believe … in better sleep
The “X-Files” theme song plays. Mulder and Scully are sitting in a diner, breakfast laid out around them. The diner is quiet, with only a few people inside.
Mulder: I’m telling you, Scully, there’s something spooky going on here.
Scully: You mean other than the fact that this town in Georgia looks suspiciously like Vancouver?
Mulder: Not one person we spoke to yesterday has gotten a full night’s sleep since the UFO sighting last month. I’m telling you, they’re here, they’re experimenting.
Scully: Do you really want me to do this to you again?
Mulder: Do what again?
Scully: There’s nothing going on here that can’t be explained by the current research. Why, in January 2023 a study was published revealing a link between poor sleep and belief in paranormal phenomena like UFOS, demons, or ghosts. Which probably explains why you’re on your third cup of coffee for the morning.
Mulder: Scully, you’ve literally been abducted by aliens. Do we have to play this game every time?
Scully: Look, it’s simple. In a sample of nearly 9,000 people, nearly two-thirds of those who reported experiencing sleep paralysis or exploding head syndrome reported believing in UFOs and aliens walking amongst humanity, despite making up just 3% of the overall sample.
Furthermore, about 60% of those reporting sleep paralysis also reported believing near-death experiences prove the soul lingers on after death, and those with stronger insomnia symptoms were more likely to believe in the devil.
Mulder: Aha!
Scully: Aha what?
Mulder: You’re a devout Christian. You believe in the devil and the soul.
Scully: Yes, but I don’t let it interfere with a good night’s sleep, Mulder. These people saw something strange, convinced themselves it was a UFO, and now they can’t sleep. It’s a vicious cycle. The study authors even said that people experiencing strange nighttime phenomena could interpret this as evidence of aliens or other paranormal beings, thus making them even more susceptible to further sleep disruption and deepening beliefs. Look who I’m talking to.
Mulder: Always with the facts, eh?
Scully: I am a doctor, after all. And if you want more research into how paranormal belief and poor sleep quality are linked, I’d be happy to dig out the literature, because the truth is out there, Mulder.
Mulder: I hate you sometimes.
It’s ChatGPT’s world. We’re just living in it
Have you heard about ChatGPT? The artificial intelligence chatbot was just launched in November and it’s already more important to the Internet than either Vladimir Putin or “Rick and Morty.”
What’s that? You’re wondering why you should care? Well, excuuuuuse us, but we thought you might want to know that ChatGPT is in the process of taking over the world. Let’s take a quick look at what it’s been up to.
“ChatGPT bot passes law school exam”
“ChatGPT passes MBA exam given by a Wharton professor”
“A freelance writer says ChatGPT wrote a $600 article in just 30 seconds”
And here’s one that might be of interest to those of the health care persuasion: “ChatGPT can pass part of the U.S. Medical Licensing Exam.” See? It’s coming for you, too.
The artificial intelligence known as ChatGPT “performed at >50% accuracy across [the three USMLE] examinations, exceeding 60% in most analyses,” a group of researchers wrote on the preprint server medRxiv, noting that 60% is usually the pass threshold for humans taking the exam in any given year.
ChatGPT was not given any special medical training before the exam, but the investigators pointed out that another AI, PubMedGPT, which is trained exclusively on biomedical domain literature, was only 50.8% accurate on the USMLE. Its reliance on “ongoing academic discourse that tends to be inconclusive, contradictory, or highly conservative or noncommittal in its language” was its undoing, the team suggested.
To top it off, ChatGPT is listed as one of the authors at the top of the medRxiv report, with an acknowledgment at the end saying that “ChatGPT contributed to the writing of several sections of this manuscript.”
We’ve said it before, and no doubt we’ll say it again: We’re doomed.
Canadian guidance recommends reducing alcohol consumption
“Drinking less is better,” says the guidance, which replaces Canada’s 2011 Low-Risk Drinking Guidelines (LRDGs).
Developed in consultation with an executive committee from federal, provincial, and territorial governments; national organizations; three scientific expert panels; and an internal evidence review working group, the guidance presents the following findings:
- Consuming no drinks per week has benefits, such as better health and better sleep, and it’s the only safe option during pregnancy.
- Consuming one or two standard drinks weekly will likely not have alcohol-related consequences.
- Three to six drinks raise the risk of developing breast, colon, and other cancers.
- Seven or more increase the risk of heart disease or stroke.
- Each additional drink “radically increases” the risk of these health consequences.
“Alcohol is more harmful than was previously thought and is a key component of the health of your patients,” Adam Sherk, PhD, a scientist at the Canadian Institute for Substance Use Research at the University of Victoria (B.C.), and a member of the scientific expert panel that contributed to the guidance, said in an interview. “Display and discuss the new guidance with your patients with the main message that drinking less is better.”
Peter Butt, MD, a clinical associate professor at the University of Saskatchewan, Saskatoon, and cochair of the guidance project, said in an interview: “The World Health Organization has identified over 200 ICD-coded conditions associated with alcohol use. This creates many opportunities to inquire into quantity and frequency of alcohol use, relate it to the patient’s health and well-being, and provide advice on reduction.”
“Canada’s Guidance on Alcohol and Health: Final Report” and a related infographic were published online Jan. 17.
Continuum of risk
The impetus for the new guidance came from the fact that “our 2011 LRDGs were no longer current, and there was emerging evidence that people drinking within those levels were coming to harm,” said Dr. Butt.
That evidence indicates that alcohol causes at least seven types of cancer, mostly of the breast or colon; is a risk factor for most types of heart disease; and is a main cause of liver disease. Evidence also indicates that avoiding drinking to the point of intoxication will reduce people’s risk of perpetrating alcohol-related violence.
Responding to the need to accurately quantify the risk, the guidance defines a “standard” drink as 12 oz of beer, cooler, or cider (5% alcohol); 5 oz of wine (12% alcohol); and 1.5 oz of spirits such as whiskey, vodka, or gin (40% alcohol).
Using different mortality risk thresholds, the project’s experts developed the following continuum of risk:
- Low for individuals who consume two standard drinks or fewer per week
- Moderate for those who consume from three to six standard drinks per week
- Increasingly high for those who consume seven standard drinks or more per week
The guidance makes the following observations:
- Consuming more than two standard drinks per drinking occasion is associated with an increased risk of harms to self and others, including injuries and violence.
- When pregnant or trying to get pregnant, no amount of alcohol is safe.
- When breastfeeding, not drinking is safest.
- Above the upper limit of the moderate risk zone, health risks increase more steeply for females than males.
- Far more injuries, violence, and deaths result from men’s alcohol use, especially for per occasion drinking, than from women’s alcohol use.
- Young people should delay alcohol use for as long as possible.
- Individuals should not start to use alcohol or increase their alcohol use for health benefits.
- Any reduction in alcohol use is beneficial.
Other national guidelines
“Countries that haven’t updated their alcohol use guidelines recently should do so, as the evidence regarding alcohol and health has advanced considerably in the past 10 years,” said Dr. Sherk. He acknowledged that “any time health guidance changes substantially, it’s reasonable to expect a period of readjustment.”
“Some will be resistant,” Dr. Butt agreed. “Some professionals will need more education than others on the health effects of alcohol. Some patients will also be more invested in drinking than others. The harm-reduction, risk-zone approach should assist in the process of engaging patients and helping them reduce over time.
“Just as we benefited from the updates done in the United Kingdom, France, and especially Australia, so also researchers elsewhere will critique our work and our approach and make their own decisions on how best to communicate with their public,” Dr. Butt said. He noted that Canada’s contributions regarding the association between alcohol and violence, as well as their sex/gender approach to the evidence, “may influence the next country’s review.”
Commenting on whether the United States should consider changing its guidance, Timothy Brennan, MD, MPH, chief of clinical services for the Addiction Institute of Mount Sinai Health System in New York, said in an interview, “A lot of people will be surprised at the recommended limits on alcohol. Most think that they can have one or two glasses of alcohol per day and not have any increased risk to their health. I think the Canadians deserve credit for putting themselves out there.”
Dr. Brennan said there will “certainly be pushback by the drinking lobby, which is very strong both in the U.S. and in Canada.” In fact, the national trade group Beer Canada was recently quoted as stating that it still supports the 2011 guidelines and that the updating process lacked full transparency and expert technical peer review.
Nevertheless, Dr. Brennan said, “it’s overwhelmingly clear that alcohol affects a ton of different parts of our body, so limiting the amount of alcohol we take in is always going to be a good thing. The Canadian graphic is great because it color-codes the risk. I recommend that clinicians put it up in their offices and begin quantifying the units of alcohol that are going into a patient’s body each day.”
A version of this article originally appeared on Medscape.com.
“Drinking less is better,” says the guidance, which replaces Canada’s 2011 Low-Risk Drinking Guidelines (LRDGs).
Developed in consultation with an executive committee from federal, provincial, and territorial governments; national organizations; three scientific expert panels; and an internal evidence review working group, the guidance presents the following findings:
- Consuming no drinks per week has benefits, such as better health and better sleep, and it’s the only safe option during pregnancy.
- Consuming one or two standard drinks weekly will likely not have alcohol-related consequences.
- Three to six drinks raise the risk of developing breast, colon, and other cancers.
- Seven or more increase the risk of heart disease or stroke.
- Each additional drink “radically increases” the risk of these health consequences.
“Alcohol is more harmful than was previously thought and is a key component of the health of your patients,” Adam Sherk, PhD, a scientist at the Canadian Institute for Substance Use Research at the University of Victoria (B.C.), and a member of the scientific expert panel that contributed to the guidance, said in an interview. “Display and discuss the new guidance with your patients with the main message that drinking less is better.”
Peter Butt, MD, a clinical associate professor at the University of Saskatchewan, Saskatoon, and cochair of the guidance project, said in an interview: “The World Health Organization has identified over 200 ICD-coded conditions associated with alcohol use. This creates many opportunities to inquire into quantity and frequency of alcohol use, relate it to the patient’s health and well-being, and provide advice on reduction.”
“Canada’s Guidance on Alcohol and Health: Final Report” and a related infographic were published online Jan. 17.
Continuum of risk
The impetus for the new guidance came from the fact that “our 2011 LRDGs were no longer current, and there was emerging evidence that people drinking within those levels were coming to harm,” said Dr. Butt.
That evidence indicates that alcohol causes at least seven types of cancer, mostly of the breast or colon; is a risk factor for most types of heart disease; and is a main cause of liver disease. Evidence also indicates that avoiding drinking to the point of intoxication will reduce people’s risk of perpetrating alcohol-related violence.
Responding to the need to accurately quantify the risk, the guidance defines a “standard” drink as 12 oz of beer, cooler, or cider (5% alcohol); 5 oz of wine (12% alcohol); and 1.5 oz of spirits such as whiskey, vodka, or gin (40% alcohol).
Using different mortality risk thresholds, the project’s experts developed the following continuum of risk:
- Low for individuals who consume two standard drinks or fewer per week
- Moderate for those who consume from three to six standard drinks per week
- Increasingly high for those who consume seven standard drinks or more per week
The guidance makes the following observations:
- Consuming more than two standard drinks per drinking occasion is associated with an increased risk of harms to self and others, including injuries and violence.
- When pregnant or trying to get pregnant, no amount of alcohol is safe.
- When breastfeeding, not drinking is safest.
- Above the upper limit of the moderate risk zone, health risks increase more steeply for females than males.
- Far more injuries, violence, and deaths result from men’s alcohol use, especially for per occasion drinking, than from women’s alcohol use.
- Young people should delay alcohol use for as long as possible.
- Individuals should not start to use alcohol or increase their alcohol use for health benefits.
- Any reduction in alcohol use is beneficial.
Other national guidelines
“Countries that haven’t updated their alcohol use guidelines recently should do so, as the evidence regarding alcohol and health has advanced considerably in the past 10 years,” said Dr. Sherk. He acknowledged that “any time health guidance changes substantially, it’s reasonable to expect a period of readjustment.”
“Some will be resistant,” Dr. Butt agreed. “Some professionals will need more education than others on the health effects of alcohol. Some patients will also be more invested in drinking than others. The harm-reduction, risk-zone approach should assist in the process of engaging patients and helping them reduce over time.
“Just as we benefited from the updates done in the United Kingdom, France, and especially Australia, so also researchers elsewhere will critique our work and our approach and make their own decisions on how best to communicate with their public,” Dr. Butt said. He noted that Canada’s contributions regarding the association between alcohol and violence, as well as their sex/gender approach to the evidence, “may influence the next country’s review.”
Commenting on whether the United States should consider changing its guidance, Timothy Brennan, MD, MPH, chief of clinical services for the Addiction Institute of Mount Sinai Health System in New York, said in an interview, “A lot of people will be surprised at the recommended limits on alcohol. Most think that they can have one or two glasses of alcohol per day and not have any increased risk to their health. I think the Canadians deserve credit for putting themselves out there.”
Dr. Brennan said there will “certainly be pushback by the drinking lobby, which is very strong both in the U.S. and in Canada.” In fact, the national trade group Beer Canada was recently quoted as stating that it still supports the 2011 guidelines and that the updating process lacked full transparency and expert technical peer review.
Nevertheless, Dr. Brennan said, “it’s overwhelmingly clear that alcohol affects a ton of different parts of our body, so limiting the amount of alcohol we take in is always going to be a good thing. The Canadian graphic is great because it color-codes the risk. I recommend that clinicians put it up in their offices and begin quantifying the units of alcohol that are going into a patient’s body each day.”
A version of this article originally appeared on Medscape.com.
“Drinking less is better,” says the guidance, which replaces Canada’s 2011 Low-Risk Drinking Guidelines (LRDGs).
Developed in consultation with an executive committee from federal, provincial, and territorial governments; national organizations; three scientific expert panels; and an internal evidence review working group, the guidance presents the following findings:
- Consuming no drinks per week has benefits, such as better health and better sleep, and it’s the only safe option during pregnancy.
- Consuming one or two standard drinks weekly will likely not have alcohol-related consequences.
- Three to six drinks raise the risk of developing breast, colon, and other cancers.
- Seven or more increase the risk of heart disease or stroke.
- Each additional drink “radically increases” the risk of these health consequences.
“Alcohol is more harmful than was previously thought and is a key component of the health of your patients,” Adam Sherk, PhD, a scientist at the Canadian Institute for Substance Use Research at the University of Victoria (B.C.), and a member of the scientific expert panel that contributed to the guidance, said in an interview. “Display and discuss the new guidance with your patients with the main message that drinking less is better.”
Peter Butt, MD, a clinical associate professor at the University of Saskatchewan, Saskatoon, and cochair of the guidance project, said in an interview: “The World Health Organization has identified over 200 ICD-coded conditions associated with alcohol use. This creates many opportunities to inquire into quantity and frequency of alcohol use, relate it to the patient’s health and well-being, and provide advice on reduction.”
“Canada’s Guidance on Alcohol and Health: Final Report” and a related infographic were published online Jan. 17.
Continuum of risk
The impetus for the new guidance came from the fact that “our 2011 LRDGs were no longer current, and there was emerging evidence that people drinking within those levels were coming to harm,” said Dr. Butt.
That evidence indicates that alcohol causes at least seven types of cancer, mostly of the breast or colon; is a risk factor for most types of heart disease; and is a main cause of liver disease. Evidence also indicates that avoiding drinking to the point of intoxication will reduce people’s risk of perpetrating alcohol-related violence.
Responding to the need to accurately quantify the risk, the guidance defines a “standard” drink as 12 oz of beer, cooler, or cider (5% alcohol); 5 oz of wine (12% alcohol); and 1.5 oz of spirits such as whiskey, vodka, or gin (40% alcohol).
Using different mortality risk thresholds, the project’s experts developed the following continuum of risk:
- Low for individuals who consume two standard drinks or fewer per week
- Moderate for those who consume from three to six standard drinks per week
- Increasingly high for those who consume seven standard drinks or more per week
The guidance makes the following observations:
- Consuming more than two standard drinks per drinking occasion is associated with an increased risk of harms to self and others, including injuries and violence.
- When pregnant or trying to get pregnant, no amount of alcohol is safe.
- When breastfeeding, not drinking is safest.
- Above the upper limit of the moderate risk zone, health risks increase more steeply for females than males.
- Far more injuries, violence, and deaths result from men’s alcohol use, especially for per occasion drinking, than from women’s alcohol use.
- Young people should delay alcohol use for as long as possible.
- Individuals should not start to use alcohol or increase their alcohol use for health benefits.
- Any reduction in alcohol use is beneficial.
Other national guidelines
“Countries that haven’t updated their alcohol use guidelines recently should do so, as the evidence regarding alcohol and health has advanced considerably in the past 10 years,” said Dr. Sherk. He acknowledged that “any time health guidance changes substantially, it’s reasonable to expect a period of readjustment.”
“Some will be resistant,” Dr. Butt agreed. “Some professionals will need more education than others on the health effects of alcohol. Some patients will also be more invested in drinking than others. The harm-reduction, risk-zone approach should assist in the process of engaging patients and helping them reduce over time.
“Just as we benefited from the updates done in the United Kingdom, France, and especially Australia, so also researchers elsewhere will critique our work and our approach and make their own decisions on how best to communicate with their public,” Dr. Butt said. He noted that Canada’s contributions regarding the association between alcohol and violence, as well as their sex/gender approach to the evidence, “may influence the next country’s review.”
Commenting on whether the United States should consider changing its guidance, Timothy Brennan, MD, MPH, chief of clinical services for the Addiction Institute of Mount Sinai Health System in New York, said in an interview, “A lot of people will be surprised at the recommended limits on alcohol. Most think that they can have one or two glasses of alcohol per day and not have any increased risk to their health. I think the Canadians deserve credit for putting themselves out there.”
Dr. Brennan said there will “certainly be pushback by the drinking lobby, which is very strong both in the U.S. and in Canada.” In fact, the national trade group Beer Canada was recently quoted as stating that it still supports the 2011 guidelines and that the updating process lacked full transparency and expert technical peer review.
Nevertheless, Dr. Brennan said, “it’s overwhelmingly clear that alcohol affects a ton of different parts of our body, so limiting the amount of alcohol we take in is always going to be a good thing. The Canadian graphic is great because it color-codes the risk. I recommend that clinicians put it up in their offices and begin quantifying the units of alcohol that are going into a patient’s body each day.”
A version of this article originally appeared on Medscape.com.
Will your smartphone be the next doctor’s office?
A fingertip pressed against a phone’s camera lens can measure a heart rate. The microphone, kept by the bedside, can screen for sleep apnea. Even the speaker is being tapped, to monitor breathing using sonar technology.
In the best of this new world, the data is conveyed remotely to a medical professional for the convenience and comfort of the patient or, in some cases, to support a clinician without the need for costly hardware.
But using smartphones as diagnostic tools is a work in progress, experts say. Although doctors and their patients have found some real-world success in deploying the phone as a medical device, the overall potential remains unfulfilled and uncertain.
Smartphones come packed with sensors capable of monitoring a patient’s vital signs. They can help assess people for concussions, watch for atrial fibrillation, and conduct mental health wellness checks, to name the uses of a few nascent applications.
Companies and researchers eager to find medical applications for smartphone technology are tapping into modern phones’ built-in cameras and light sensors; microphones; accelerometers, which detect body movements; gyroscopes; and even speakers. The apps then use artificial intelligence software to analyze the collected sights and sounds to create an easy connection between patients and physicians. Earning potential and marketability are evidenced by the more than 350,000 digital health products available in app stores, according to a Grand View Research report.
“It’s very hard to put devices into the patient home or in the hospital, but everybody is just walking around with a cellphone that has a network connection,” said Dr. Andrew Gostine, CEO of the sensor network company Artisight. Most Americans own a smartphone, including more than 60% of people 65 and over, an increase from just 13% a decade ago, according the Pew Research Center. The COVID-19 pandemic has also pushed people to become more comfortable with virtual care.
Some of these products have sought FDA clearance to be marketed as a medical device. That way, if patients must pay to use the software, health insurers are more likely to cover at least part of the cost. Other products are designated as exempt from this regulatory process, placed in the same clinical classification as a Band-Aid. But how the agency handles AI and machine learning–based medical devices is still being adjusted to reflect software’s adaptive nature.
Ensuring accuracy and clinical validation is crucial to securing buy-in from health care providers. And many tools still need fine-tuning, said Eugene Yang, MD, a professor of medicine at the University of Washington, Seattle. Currently, Dr. Yang is testing contactless measurement of blood pressure, heart rate, and oxygen saturation gleaned remotely via Zoom camera footage of a patient’s face.
Judging these new technologies is difficult because they rely on algorithms built by machine learning and artificial intelligence to collect data, rather than the physical tools typically used in hospitals. So researchers cannot “compare apples to apples” with medical industry standards, Dr. Yang said. Failure to build in such assurances undermines the technology’s ultimate goals of easing costs and access because a doctor still must verify results.
“False positives and false negatives lead to more testing and more cost to the health care system,” he said.
Big tech companies like Google have heavily invested in researching this kind of technology, catering to clinicians and in-home caregivers, as well as consumers. Currently, in the Google Fit app, users can check their heart rate by placing their finger on the rear-facing camera lens or track their breathing rate using the front-facing camera.
“If you took the sensor out of the phone and out of a clinical device, they are probably the same thing,” said Shwetak Patel, director of health technologies at Google and a professor of electrical and computer engineering at the University of Washington.
Google’s research uses machine learning and computer vision, a field within AI based on information from visual inputs like videos or images. So instead of using a blood pressure cuff, for example, the algorithm can interpret slight visual changes to the body that serve as proxies and biosignals for a patient’s blood pressure, Mr. Patel said.
Google is also investigating the effectiveness of the built-in microphone for detecting heartbeats and murmurs and using the camera to preserve eyesight by screening for diabetic eye disease, according to information the company published last year.
The tech giant recently purchased Sound Life Sciences, a Seattle startup with an FDA-cleared sonar technology app. It uses a smart device’s speaker to bounce inaudible pulses off a patient’s body to identify movement and monitor breathing.
Binah.ai, based in Israel, is another company using the smartphone camera to calculate vital signs. Its software looks at the region around the eyes, where the skin is a bit thinner, and analyzes the light reflecting off blood vessels back to the lens. The company is wrapping up a U.S. clinical trial and marketing its wellness app directly to insurers and other health companies, said company spokesperson Mona Popilian-Yona.
The applications even reach into disciplines such as optometry and mental health:
- With the microphone, Canary Speech uses the same underlying technology as Amazon’s Alexa to analyze patients’ voices for mental health conditions. The software can integrate with telemedicine appointments and allow clinicians to screen for anxiety and depression using a library of vocal biomarkers and predictive analytics, said Henry O’Connell, the company’s CEO.
- Australia-based ResApp Health last year for its iPhone app that screens for moderate to severe obstructive sleep apnea by listening to breathing and snoring. SleepCheckRx, which will require a prescription, is minimally invasive compared with sleep studies currently used to diagnose sleep apnea. Those can cost thousands of dollars and require an array of tests.
- Brightlamp’s Reflex app is a clinical decision support tool for helping manage concussions and vision rehabilitation, among other things. Using an iPad’s or iPhone’s camera, the mobile app measures how a person’s pupils react to changes in light. Through machine learning analysis, the imagery gives practitioners data points for evaluating patients. Brightlamp sells directly to health care providers and is being used in more than 230 clinics. Clinicians pay a $400 standard annual fee per account, which is currently not covered by insurance. The Department of Defense has an ongoing clinical trial using Reflex.
In some cases, such as with the Reflex app, the data is processed directly on the phone – rather than in the cloud, Brightlamp CEO Kurtis Sluss said. By processing everything on the device, the app avoids running into privacy issues, as streaming data elsewhere requires patient consent.
But algorithms need to be trained and tested by collecting reams of data, and that is an ongoing process.
Researchers, for example, have found that some computer vision applications, like heart rate or blood pressure monitoring, can be less accurate for darker skin. Studies are underway to find better solutions.
Small algorithm glitches can also produce false alarms and frighten patients enough to keep widespread adoption out of reach. For example, Apple’s new car-crash detection feature, available on both the latest iPhone and Apple Watch, was set off when people were riding roller coasters and automatically dialed 911.
“We’re not there yet,” Dr. Yang said. “That’s the bottom line.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
A fingertip pressed against a phone’s camera lens can measure a heart rate. The microphone, kept by the bedside, can screen for sleep apnea. Even the speaker is being tapped, to monitor breathing using sonar technology.
In the best of this new world, the data is conveyed remotely to a medical professional for the convenience and comfort of the patient or, in some cases, to support a clinician without the need for costly hardware.
But using smartphones as diagnostic tools is a work in progress, experts say. Although doctors and their patients have found some real-world success in deploying the phone as a medical device, the overall potential remains unfulfilled and uncertain.
Smartphones come packed with sensors capable of monitoring a patient’s vital signs. They can help assess people for concussions, watch for atrial fibrillation, and conduct mental health wellness checks, to name the uses of a few nascent applications.
Companies and researchers eager to find medical applications for smartphone technology are tapping into modern phones’ built-in cameras and light sensors; microphones; accelerometers, which detect body movements; gyroscopes; and even speakers. The apps then use artificial intelligence software to analyze the collected sights and sounds to create an easy connection between patients and physicians. Earning potential and marketability are evidenced by the more than 350,000 digital health products available in app stores, according to a Grand View Research report.
“It’s very hard to put devices into the patient home or in the hospital, but everybody is just walking around with a cellphone that has a network connection,” said Dr. Andrew Gostine, CEO of the sensor network company Artisight. Most Americans own a smartphone, including more than 60% of people 65 and over, an increase from just 13% a decade ago, according the Pew Research Center. The COVID-19 pandemic has also pushed people to become more comfortable with virtual care.
Some of these products have sought FDA clearance to be marketed as a medical device. That way, if patients must pay to use the software, health insurers are more likely to cover at least part of the cost. Other products are designated as exempt from this regulatory process, placed in the same clinical classification as a Band-Aid. But how the agency handles AI and machine learning–based medical devices is still being adjusted to reflect software’s adaptive nature.
Ensuring accuracy and clinical validation is crucial to securing buy-in from health care providers. And many tools still need fine-tuning, said Eugene Yang, MD, a professor of medicine at the University of Washington, Seattle. Currently, Dr. Yang is testing contactless measurement of blood pressure, heart rate, and oxygen saturation gleaned remotely via Zoom camera footage of a patient’s face.
Judging these new technologies is difficult because they rely on algorithms built by machine learning and artificial intelligence to collect data, rather than the physical tools typically used in hospitals. So researchers cannot “compare apples to apples” with medical industry standards, Dr. Yang said. Failure to build in such assurances undermines the technology’s ultimate goals of easing costs and access because a doctor still must verify results.
“False positives and false negatives lead to more testing and more cost to the health care system,” he said.
Big tech companies like Google have heavily invested in researching this kind of technology, catering to clinicians and in-home caregivers, as well as consumers. Currently, in the Google Fit app, users can check their heart rate by placing their finger on the rear-facing camera lens or track their breathing rate using the front-facing camera.
“If you took the sensor out of the phone and out of a clinical device, they are probably the same thing,” said Shwetak Patel, director of health technologies at Google and a professor of electrical and computer engineering at the University of Washington.
Google’s research uses machine learning and computer vision, a field within AI based on information from visual inputs like videos or images. So instead of using a blood pressure cuff, for example, the algorithm can interpret slight visual changes to the body that serve as proxies and biosignals for a patient’s blood pressure, Mr. Patel said.
Google is also investigating the effectiveness of the built-in microphone for detecting heartbeats and murmurs and using the camera to preserve eyesight by screening for diabetic eye disease, according to information the company published last year.
The tech giant recently purchased Sound Life Sciences, a Seattle startup with an FDA-cleared sonar technology app. It uses a smart device’s speaker to bounce inaudible pulses off a patient’s body to identify movement and monitor breathing.
Binah.ai, based in Israel, is another company using the smartphone camera to calculate vital signs. Its software looks at the region around the eyes, where the skin is a bit thinner, and analyzes the light reflecting off blood vessels back to the lens. The company is wrapping up a U.S. clinical trial and marketing its wellness app directly to insurers and other health companies, said company spokesperson Mona Popilian-Yona.
The applications even reach into disciplines such as optometry and mental health:
- With the microphone, Canary Speech uses the same underlying technology as Amazon’s Alexa to analyze patients’ voices for mental health conditions. The software can integrate with telemedicine appointments and allow clinicians to screen for anxiety and depression using a library of vocal biomarkers and predictive analytics, said Henry O’Connell, the company’s CEO.
- Australia-based ResApp Health last year for its iPhone app that screens for moderate to severe obstructive sleep apnea by listening to breathing and snoring. SleepCheckRx, which will require a prescription, is minimally invasive compared with sleep studies currently used to diagnose sleep apnea. Those can cost thousands of dollars and require an array of tests.
- Brightlamp’s Reflex app is a clinical decision support tool for helping manage concussions and vision rehabilitation, among other things. Using an iPad’s or iPhone’s camera, the mobile app measures how a person’s pupils react to changes in light. Through machine learning analysis, the imagery gives practitioners data points for evaluating patients. Brightlamp sells directly to health care providers and is being used in more than 230 clinics. Clinicians pay a $400 standard annual fee per account, which is currently not covered by insurance. The Department of Defense has an ongoing clinical trial using Reflex.
In some cases, such as with the Reflex app, the data is processed directly on the phone – rather than in the cloud, Brightlamp CEO Kurtis Sluss said. By processing everything on the device, the app avoids running into privacy issues, as streaming data elsewhere requires patient consent.
But algorithms need to be trained and tested by collecting reams of data, and that is an ongoing process.
Researchers, for example, have found that some computer vision applications, like heart rate or blood pressure monitoring, can be less accurate for darker skin. Studies are underway to find better solutions.
Small algorithm glitches can also produce false alarms and frighten patients enough to keep widespread adoption out of reach. For example, Apple’s new car-crash detection feature, available on both the latest iPhone and Apple Watch, was set off when people were riding roller coasters and automatically dialed 911.
“We’re not there yet,” Dr. Yang said. “That’s the bottom line.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
A fingertip pressed against a phone’s camera lens can measure a heart rate. The microphone, kept by the bedside, can screen for sleep apnea. Even the speaker is being tapped, to monitor breathing using sonar technology.
In the best of this new world, the data is conveyed remotely to a medical professional for the convenience and comfort of the patient or, in some cases, to support a clinician without the need for costly hardware.
But using smartphones as diagnostic tools is a work in progress, experts say. Although doctors and their patients have found some real-world success in deploying the phone as a medical device, the overall potential remains unfulfilled and uncertain.
Smartphones come packed with sensors capable of monitoring a patient’s vital signs. They can help assess people for concussions, watch for atrial fibrillation, and conduct mental health wellness checks, to name the uses of a few nascent applications.
Companies and researchers eager to find medical applications for smartphone technology are tapping into modern phones’ built-in cameras and light sensors; microphones; accelerometers, which detect body movements; gyroscopes; and even speakers. The apps then use artificial intelligence software to analyze the collected sights and sounds to create an easy connection between patients and physicians. Earning potential and marketability are evidenced by the more than 350,000 digital health products available in app stores, according to a Grand View Research report.
“It’s very hard to put devices into the patient home or in the hospital, but everybody is just walking around with a cellphone that has a network connection,” said Dr. Andrew Gostine, CEO of the sensor network company Artisight. Most Americans own a smartphone, including more than 60% of people 65 and over, an increase from just 13% a decade ago, according the Pew Research Center. The COVID-19 pandemic has also pushed people to become more comfortable with virtual care.
Some of these products have sought FDA clearance to be marketed as a medical device. That way, if patients must pay to use the software, health insurers are more likely to cover at least part of the cost. Other products are designated as exempt from this regulatory process, placed in the same clinical classification as a Band-Aid. But how the agency handles AI and machine learning–based medical devices is still being adjusted to reflect software’s adaptive nature.
Ensuring accuracy and clinical validation is crucial to securing buy-in from health care providers. And many tools still need fine-tuning, said Eugene Yang, MD, a professor of medicine at the University of Washington, Seattle. Currently, Dr. Yang is testing contactless measurement of blood pressure, heart rate, and oxygen saturation gleaned remotely via Zoom camera footage of a patient’s face.
Judging these new technologies is difficult because they rely on algorithms built by machine learning and artificial intelligence to collect data, rather than the physical tools typically used in hospitals. So researchers cannot “compare apples to apples” with medical industry standards, Dr. Yang said. Failure to build in such assurances undermines the technology’s ultimate goals of easing costs and access because a doctor still must verify results.
“False positives and false negatives lead to more testing and more cost to the health care system,” he said.
Big tech companies like Google have heavily invested in researching this kind of technology, catering to clinicians and in-home caregivers, as well as consumers. Currently, in the Google Fit app, users can check their heart rate by placing their finger on the rear-facing camera lens or track their breathing rate using the front-facing camera.
“If you took the sensor out of the phone and out of a clinical device, they are probably the same thing,” said Shwetak Patel, director of health technologies at Google and a professor of electrical and computer engineering at the University of Washington.
Google’s research uses machine learning and computer vision, a field within AI based on information from visual inputs like videos or images. So instead of using a blood pressure cuff, for example, the algorithm can interpret slight visual changes to the body that serve as proxies and biosignals for a patient’s blood pressure, Mr. Patel said.
Google is also investigating the effectiveness of the built-in microphone for detecting heartbeats and murmurs and using the camera to preserve eyesight by screening for diabetic eye disease, according to information the company published last year.
The tech giant recently purchased Sound Life Sciences, a Seattle startup with an FDA-cleared sonar technology app. It uses a smart device’s speaker to bounce inaudible pulses off a patient’s body to identify movement and monitor breathing.
Binah.ai, based in Israel, is another company using the smartphone camera to calculate vital signs. Its software looks at the region around the eyes, where the skin is a bit thinner, and analyzes the light reflecting off blood vessels back to the lens. The company is wrapping up a U.S. clinical trial and marketing its wellness app directly to insurers and other health companies, said company spokesperson Mona Popilian-Yona.
The applications even reach into disciplines such as optometry and mental health:
- With the microphone, Canary Speech uses the same underlying technology as Amazon’s Alexa to analyze patients’ voices for mental health conditions. The software can integrate with telemedicine appointments and allow clinicians to screen for anxiety and depression using a library of vocal biomarkers and predictive analytics, said Henry O’Connell, the company’s CEO.
- Australia-based ResApp Health last year for its iPhone app that screens for moderate to severe obstructive sleep apnea by listening to breathing and snoring. SleepCheckRx, which will require a prescription, is minimally invasive compared with sleep studies currently used to diagnose sleep apnea. Those can cost thousands of dollars and require an array of tests.
- Brightlamp’s Reflex app is a clinical decision support tool for helping manage concussions and vision rehabilitation, among other things. Using an iPad’s or iPhone’s camera, the mobile app measures how a person’s pupils react to changes in light. Through machine learning analysis, the imagery gives practitioners data points for evaluating patients. Brightlamp sells directly to health care providers and is being used in more than 230 clinics. Clinicians pay a $400 standard annual fee per account, which is currently not covered by insurance. The Department of Defense has an ongoing clinical trial using Reflex.
In some cases, such as with the Reflex app, the data is processed directly on the phone – rather than in the cloud, Brightlamp CEO Kurtis Sluss said. By processing everything on the device, the app avoids running into privacy issues, as streaming data elsewhere requires patient consent.
But algorithms need to be trained and tested by collecting reams of data, and that is an ongoing process.
Researchers, for example, have found that some computer vision applications, like heart rate or blood pressure monitoring, can be less accurate for darker skin. Studies are underway to find better solutions.
Small algorithm glitches can also produce false alarms and frighten patients enough to keep widespread adoption out of reach. For example, Apple’s new car-crash detection feature, available on both the latest iPhone and Apple Watch, was set off when people were riding roller coasters and automatically dialed 911.
“We’re not there yet,” Dr. Yang said. “That’s the bottom line.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Sleep complaints in major depression flag risk for other psychiatric disorders
Investigators studied 3-year incidence rates of psychiatric disorders in almost 3,000 patients experiencing an MDE. Results showed that having a history of difficulty falling asleep, early morning awakening, and hypersomnia increased risk for incident psychiatric disorders.
“The findings of this study suggest the potential value of including insomnia and hypersomnia in clinical assessments of all psychiatric disorders,” write the investigators, led by Bénédicte Barbotin, MD, Département de Psychiatrie et d’Addictologie, Assistance Publique-Hôpitaux de Paris, Hôpital Bichat-Claude Bernard, France.
“Insomnia and hypersomnia symptoms may be prodromal transdiagnostic biomarkers and easily modifiable therapeutic targets for the prevention of psychiatric disorders,” they add.
The findings were published online recently in the Journal of Clinical Psychiatry.
Bidirectional association
The researchers note that sleep disturbance is “one of the most common symptoms” associated with major depressive disorder (MDD) and may be “both a consequence and a cause.”
Moreover, improving sleep disturbances for patients with an MDE “tends to improve depressive symptom and outcomes,” they add.
Although the possibility of a bidirectional association between MDEs and sleep disturbances “offers a new perspective that sleep complaints might be a predictive prodromal symptom,” the association of sleep complaints with the subsequent development of other psychiatric disorders in MDEs “remains poorly documented,” the investigators write.
The observation that sleep complaints are associated with psychiatric complications and adverse outcomes, such as suicidality and substance overdose, suggests that longitudinal studies “may help to better understand these relationships.”
To investigate these issues, the researchers examined three sleep complaints among patients with MDE: trouble falling asleep, early morning awakening, and hypersomnia. They adjusted for an array of variables, including antisocial personality disorders, use of sedatives or tranquilizers, sociodemographic characteristics, MDE severity, poverty, obesity, educational level, and stressful life events.
They also used a “bifactor latent variable approach” to “disentangle” a number of effects, including those shared by all psychiatric disorders; those specific to dimensions of psychopathology, such as internalizing dimension; and those specific to individual psychiatric disorders, such as dysthymia.
“To our knowledge, this is the most extensive prospective assessment [ever conducted] of associations between sleep complaints and incident psychiatric disorders,” the investigators write.
They drew on data from Waves 1 and 2 of the National Epidemiological Survey on Alcohol and Related Conditions, a large nationally representative survey conducted in 2001-2002 (Wave 1) and 2004-2005 (Wave 2) by the National Institute on Alcoholism and Alcohol Abuse.
The analysis included 2,864 participants who experienced MDE in the year prior to Wave 1 and who completed interviews at both waves.
Researchers assessed past-year DSM-IV Axis I disorders and baseline sleep complaints at Wave 1, as well as incident DSM-IV Axis I disorders between the two waves – including substance use, mood, and anxiety disorders.
Screening needed?
Results showed a wide range of incidence rates for psychiatric disorders between Wave 1 and Wave 2, ranging from 2.7% for cannabis use to 8.2% for generalized anxiety disorder.
The lifetime prevalence of sleep complaints was higher among participants who developed a psychiatric disorder between the two waves than among those who did not have sleep complaints. The range (from lowest to highest percentage) is shown in the accompanying table.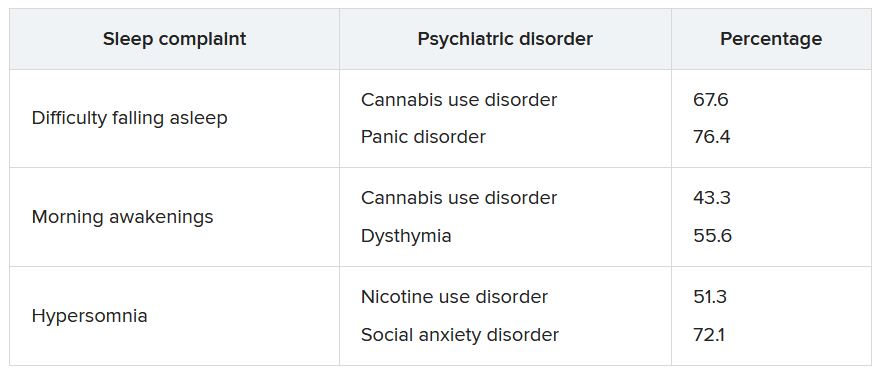
A higher number of sleep complaints was also associated with higher percentages of psychiatric disorders.
Hypersomnia, in particular, significantly increased the odds of having another psychiatric disorder. For patients with MDD who reported hypersomnia, the mean number of sleep disorders was significantly higher than for patients without hypersomnia (2.08 vs. 1.32; P < .001).
“This explains why hypersomnia appears more strongly associated with the incidence of psychiatric disorders,” the investigators write.
After adjusting for sociodemographic and clinical characteristics and antisocial personality disorder, the effects shared across all sleep complaints were “significantly associated with the incident general psychopathology factor, representing mechanisms that may lead to incidence of all psychiatric disorder in the model,” they add.
The researchers note that insomnia and hypersomnia can impair cognitive function, decision-making, problem-solving, and emotion processing networks, thereby increasing the onset of psychiatric disorders in vulnerable individuals.
Shared biological determinants, such as monoamine neurotransmitters that play a major role in depression, anxiety, substance use disorders, and the regulation of sleep stages, may also underlie both sleep disturbances and psychiatric disorders, they speculate.
“These results suggest the importance of systematically assessing insomnia and hypersomnia when evaluating psychiatric disorders and considering these symptoms as nonspecific prodromal or at-risk symptoms, also shared with suicidal behaviors,” the investigators write.
“In addition, since most individuals who developed a psychiatric disorder had at least one sleep complaint, all psychiatric disorders should be carefully screened among individuals with sleep complaints,” they add.
Transdiagnostic phenomenon
In a comment, Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto, and head of the Mood Disorders Psychopharmacology Unit, noted that the study replicates previous observations that a bidirectional relationship exists between sleep disturbances and mental disorders and that there “seems to be a relationship between sleep disturbance and suicidality that is bidirectional.”
He added that he appreciated the fact that the investigators “took this knowledge one step further; and what they are saying is that within the syndrome of depression, it is the sleep disturbance that is predicting future problems.”
Dr. McIntyre, who is also chairman and executive director of the Brain and Cognitive Discover Foundation in Toronto, was not involved with the study.
The data suggest that, “conceptually, sleep disturbance is a transdiagnostic phenomenon that may also be the nexus when multiple comorbid mental disorders occur,” he said.
“If this is the case, clinically, there is an opportunity here to prevent incident mental disorders in persons with depression and sleep disturbance, prioritizing sleep management in any patient with a mood disorder,” Dr. McIntyre added.
He noted that “the testable hypothesis” is how this is occurring mechanistically.
“I would conjecture that it could be inflammation and/or insulin resistance that is part of sleep disturbance that could predispose and portend other mental illnesses – and likely other medical conditions too, such as obesity and diabetes,” he said.
The study received no specific funding from any funding agency, commercial, or not-for-profit sectors. The investigators’ relevant financial relationships are listed in the original article. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China and the Milken Institute; has received speaker/consultation fees from Lundbeck, Janssen, Alkermes,Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, AbbVie, and Atai Life Sciences; and is a CEO of Braxia Scientific Corp.
A version of this article first appeared on Medscape.com.
Investigators studied 3-year incidence rates of psychiatric disorders in almost 3,000 patients experiencing an MDE. Results showed that having a history of difficulty falling asleep, early morning awakening, and hypersomnia increased risk for incident psychiatric disorders.
“The findings of this study suggest the potential value of including insomnia and hypersomnia in clinical assessments of all psychiatric disorders,” write the investigators, led by Bénédicte Barbotin, MD, Département de Psychiatrie et d’Addictologie, Assistance Publique-Hôpitaux de Paris, Hôpital Bichat-Claude Bernard, France.
“Insomnia and hypersomnia symptoms may be prodromal transdiagnostic biomarkers and easily modifiable therapeutic targets for the prevention of psychiatric disorders,” they add.
The findings were published online recently in the Journal of Clinical Psychiatry.
Bidirectional association
The researchers note that sleep disturbance is “one of the most common symptoms” associated with major depressive disorder (MDD) and may be “both a consequence and a cause.”
Moreover, improving sleep disturbances for patients with an MDE “tends to improve depressive symptom and outcomes,” they add.
Although the possibility of a bidirectional association between MDEs and sleep disturbances “offers a new perspective that sleep complaints might be a predictive prodromal symptom,” the association of sleep complaints with the subsequent development of other psychiatric disorders in MDEs “remains poorly documented,” the investigators write.
The observation that sleep complaints are associated with psychiatric complications and adverse outcomes, such as suicidality and substance overdose, suggests that longitudinal studies “may help to better understand these relationships.”
To investigate these issues, the researchers examined three sleep complaints among patients with MDE: trouble falling asleep, early morning awakening, and hypersomnia. They adjusted for an array of variables, including antisocial personality disorders, use of sedatives or tranquilizers, sociodemographic characteristics, MDE severity, poverty, obesity, educational level, and stressful life events.
They also used a “bifactor latent variable approach” to “disentangle” a number of effects, including those shared by all psychiatric disorders; those specific to dimensions of psychopathology, such as internalizing dimension; and those specific to individual psychiatric disorders, such as dysthymia.
“To our knowledge, this is the most extensive prospective assessment [ever conducted] of associations between sleep complaints and incident psychiatric disorders,” the investigators write.
They drew on data from Waves 1 and 2 of the National Epidemiological Survey on Alcohol and Related Conditions, a large nationally representative survey conducted in 2001-2002 (Wave 1) and 2004-2005 (Wave 2) by the National Institute on Alcoholism and Alcohol Abuse.
The analysis included 2,864 participants who experienced MDE in the year prior to Wave 1 and who completed interviews at both waves.
Researchers assessed past-year DSM-IV Axis I disorders and baseline sleep complaints at Wave 1, as well as incident DSM-IV Axis I disorders between the two waves – including substance use, mood, and anxiety disorders.
Screening needed?
Results showed a wide range of incidence rates for psychiatric disorders between Wave 1 and Wave 2, ranging from 2.7% for cannabis use to 8.2% for generalized anxiety disorder.
The lifetime prevalence of sleep complaints was higher among participants who developed a psychiatric disorder between the two waves than among those who did not have sleep complaints. The range (from lowest to highest percentage) is shown in the accompanying table.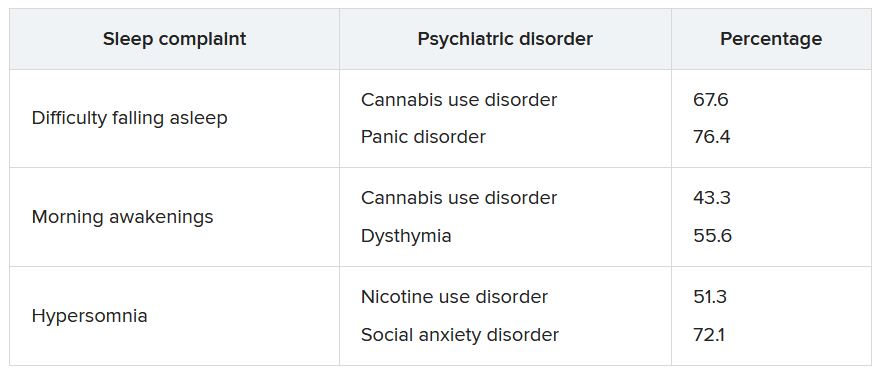
A higher number of sleep complaints was also associated with higher percentages of psychiatric disorders.
Hypersomnia, in particular, significantly increased the odds of having another psychiatric disorder. For patients with MDD who reported hypersomnia, the mean number of sleep disorders was significantly higher than for patients without hypersomnia (2.08 vs. 1.32; P < .001).
“This explains why hypersomnia appears more strongly associated with the incidence of psychiatric disorders,” the investigators write.
After adjusting for sociodemographic and clinical characteristics and antisocial personality disorder, the effects shared across all sleep complaints were “significantly associated with the incident general psychopathology factor, representing mechanisms that may lead to incidence of all psychiatric disorder in the model,” they add.
The researchers note that insomnia and hypersomnia can impair cognitive function, decision-making, problem-solving, and emotion processing networks, thereby increasing the onset of psychiatric disorders in vulnerable individuals.
Shared biological determinants, such as monoamine neurotransmitters that play a major role in depression, anxiety, substance use disorders, and the regulation of sleep stages, may also underlie both sleep disturbances and psychiatric disorders, they speculate.
“These results suggest the importance of systematically assessing insomnia and hypersomnia when evaluating psychiatric disorders and considering these symptoms as nonspecific prodromal or at-risk symptoms, also shared with suicidal behaviors,” the investigators write.
“In addition, since most individuals who developed a psychiatric disorder had at least one sleep complaint, all psychiatric disorders should be carefully screened among individuals with sleep complaints,” they add.
Transdiagnostic phenomenon
In a comment, Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto, and head of the Mood Disorders Psychopharmacology Unit, noted that the study replicates previous observations that a bidirectional relationship exists between sleep disturbances and mental disorders and that there “seems to be a relationship between sleep disturbance and suicidality that is bidirectional.”
He added that he appreciated the fact that the investigators “took this knowledge one step further; and what they are saying is that within the syndrome of depression, it is the sleep disturbance that is predicting future problems.”
Dr. McIntyre, who is also chairman and executive director of the Brain and Cognitive Discover Foundation in Toronto, was not involved with the study.
The data suggest that, “conceptually, sleep disturbance is a transdiagnostic phenomenon that may also be the nexus when multiple comorbid mental disorders occur,” he said.
“If this is the case, clinically, there is an opportunity here to prevent incident mental disorders in persons with depression and sleep disturbance, prioritizing sleep management in any patient with a mood disorder,” Dr. McIntyre added.
He noted that “the testable hypothesis” is how this is occurring mechanistically.
“I would conjecture that it could be inflammation and/or insulin resistance that is part of sleep disturbance that could predispose and portend other mental illnesses – and likely other medical conditions too, such as obesity and diabetes,” he said.
The study received no specific funding from any funding agency, commercial, or not-for-profit sectors. The investigators’ relevant financial relationships are listed in the original article. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China and the Milken Institute; has received speaker/consultation fees from Lundbeck, Janssen, Alkermes,Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, AbbVie, and Atai Life Sciences; and is a CEO of Braxia Scientific Corp.
A version of this article first appeared on Medscape.com.
Investigators studied 3-year incidence rates of psychiatric disorders in almost 3,000 patients experiencing an MDE. Results showed that having a history of difficulty falling asleep, early morning awakening, and hypersomnia increased risk for incident psychiatric disorders.
“The findings of this study suggest the potential value of including insomnia and hypersomnia in clinical assessments of all psychiatric disorders,” write the investigators, led by Bénédicte Barbotin, MD, Département de Psychiatrie et d’Addictologie, Assistance Publique-Hôpitaux de Paris, Hôpital Bichat-Claude Bernard, France.
“Insomnia and hypersomnia symptoms may be prodromal transdiagnostic biomarkers and easily modifiable therapeutic targets for the prevention of psychiatric disorders,” they add.
The findings were published online recently in the Journal of Clinical Psychiatry.
Bidirectional association
The researchers note that sleep disturbance is “one of the most common symptoms” associated with major depressive disorder (MDD) and may be “both a consequence and a cause.”
Moreover, improving sleep disturbances for patients with an MDE “tends to improve depressive symptom and outcomes,” they add.
Although the possibility of a bidirectional association between MDEs and sleep disturbances “offers a new perspective that sleep complaints might be a predictive prodromal symptom,” the association of sleep complaints with the subsequent development of other psychiatric disorders in MDEs “remains poorly documented,” the investigators write.
The observation that sleep complaints are associated with psychiatric complications and adverse outcomes, such as suicidality and substance overdose, suggests that longitudinal studies “may help to better understand these relationships.”
To investigate these issues, the researchers examined three sleep complaints among patients with MDE: trouble falling asleep, early morning awakening, and hypersomnia. They adjusted for an array of variables, including antisocial personality disorders, use of sedatives or tranquilizers, sociodemographic characteristics, MDE severity, poverty, obesity, educational level, and stressful life events.
They also used a “bifactor latent variable approach” to “disentangle” a number of effects, including those shared by all psychiatric disorders; those specific to dimensions of psychopathology, such as internalizing dimension; and those specific to individual psychiatric disorders, such as dysthymia.
“To our knowledge, this is the most extensive prospective assessment [ever conducted] of associations between sleep complaints and incident psychiatric disorders,” the investigators write.
They drew on data from Waves 1 and 2 of the National Epidemiological Survey on Alcohol and Related Conditions, a large nationally representative survey conducted in 2001-2002 (Wave 1) and 2004-2005 (Wave 2) by the National Institute on Alcoholism and Alcohol Abuse.
The analysis included 2,864 participants who experienced MDE in the year prior to Wave 1 and who completed interviews at both waves.
Researchers assessed past-year DSM-IV Axis I disorders and baseline sleep complaints at Wave 1, as well as incident DSM-IV Axis I disorders between the two waves – including substance use, mood, and anxiety disorders.
Screening needed?
Results showed a wide range of incidence rates for psychiatric disorders between Wave 1 and Wave 2, ranging from 2.7% for cannabis use to 8.2% for generalized anxiety disorder.
The lifetime prevalence of sleep complaints was higher among participants who developed a psychiatric disorder between the two waves than among those who did not have sleep complaints. The range (from lowest to highest percentage) is shown in the accompanying table.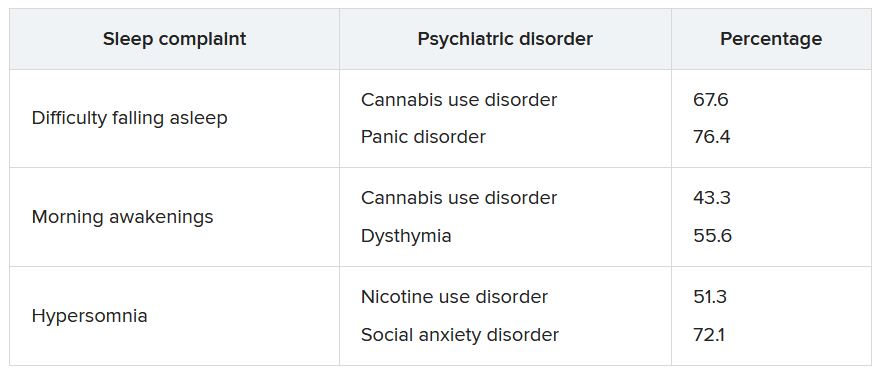
A higher number of sleep complaints was also associated with higher percentages of psychiatric disorders.
Hypersomnia, in particular, significantly increased the odds of having another psychiatric disorder. For patients with MDD who reported hypersomnia, the mean number of sleep disorders was significantly higher than for patients without hypersomnia (2.08 vs. 1.32; P < .001).
“This explains why hypersomnia appears more strongly associated with the incidence of psychiatric disorders,” the investigators write.
After adjusting for sociodemographic and clinical characteristics and antisocial personality disorder, the effects shared across all sleep complaints were “significantly associated with the incident general psychopathology factor, representing mechanisms that may lead to incidence of all psychiatric disorder in the model,” they add.
The researchers note that insomnia and hypersomnia can impair cognitive function, decision-making, problem-solving, and emotion processing networks, thereby increasing the onset of psychiatric disorders in vulnerable individuals.
Shared biological determinants, such as monoamine neurotransmitters that play a major role in depression, anxiety, substance use disorders, and the regulation of sleep stages, may also underlie both sleep disturbances and psychiatric disorders, they speculate.
“These results suggest the importance of systematically assessing insomnia and hypersomnia when evaluating psychiatric disorders and considering these symptoms as nonspecific prodromal or at-risk symptoms, also shared with suicidal behaviors,” the investigators write.
“In addition, since most individuals who developed a psychiatric disorder had at least one sleep complaint, all psychiatric disorders should be carefully screened among individuals with sleep complaints,” they add.
Transdiagnostic phenomenon
In a comment, Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto, and head of the Mood Disorders Psychopharmacology Unit, noted that the study replicates previous observations that a bidirectional relationship exists between sleep disturbances and mental disorders and that there “seems to be a relationship between sleep disturbance and suicidality that is bidirectional.”
He added that he appreciated the fact that the investigators “took this knowledge one step further; and what they are saying is that within the syndrome of depression, it is the sleep disturbance that is predicting future problems.”
Dr. McIntyre, who is also chairman and executive director of the Brain and Cognitive Discover Foundation in Toronto, was not involved with the study.
The data suggest that, “conceptually, sleep disturbance is a transdiagnostic phenomenon that may also be the nexus when multiple comorbid mental disorders occur,” he said.
“If this is the case, clinically, there is an opportunity here to prevent incident mental disorders in persons with depression and sleep disturbance, prioritizing sleep management in any patient with a mood disorder,” Dr. McIntyre added.
He noted that “the testable hypothesis” is how this is occurring mechanistically.
“I would conjecture that it could be inflammation and/or insulin resistance that is part of sleep disturbance that could predispose and portend other mental illnesses – and likely other medical conditions too, such as obesity and diabetes,” he said.
The study received no specific funding from any funding agency, commercial, or not-for-profit sectors. The investigators’ relevant financial relationships are listed in the original article. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China and the Milken Institute; has received speaker/consultation fees from Lundbeck, Janssen, Alkermes,Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, AbbVie, and Atai Life Sciences; and is a CEO of Braxia Scientific Corp.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
Serum trace metals relate to lower risk of sleep disorders
, based on data from 3,660 individuals.
Previous research has shown an association between trace metals and sleep and sleep patterns, but data on the impact of serum trace metals on sleep disorders have been limited, wrote Ming-Gang Deng, MD, of Wuhan (China) University and colleagues.
In a study published in the Journal of Affective Disorders, the researchers reviewed data from the National Health and Nutrition Examination Survey (NHANES) 2011-2016 to calculate the odds ratios of sleep disorders and serum zinc (Zn), copper (Cu), and selenium (Se). The study population included adults aged 18 years and older, with an average age of 47.6 years. Approximately half of the participants were men, and the majority was non-Hispanic white. Serum Zn, Cu, and Se were identified at the Environmental Health Sciences Laboratory of the Centers for Disease Control and Prevention National Center for Environmental Health. The lower limits of detection for Zn, Cu, and Se were 2.9 mcg/dL, 2.5 mcg/dL, and 4.5 mcg/L, respectively. Sleep disorders were assessed based on self-reports of discussions with health professionals about sleep disorders, and via the Sleep Disorder Questionnaire.
After adjusting for sociodemographic, behavioral characteristics, and health characteristics, adults in the highest tertiles of serum Zn had a 30% reduced risk of sleep disorders, compared with those in the lowest tertiles of serum Zn (odds ratio, 0.70; P = .035). In measures of trace metals ratios, serum Zn/Cu and Zn/Se also were significantly associated with reduced risk of sleep disorders for individuals in the highest tertiles, compared with those in the lowest tertiles (OR, 0.62 and OR, 0.68, respectively).
However, serum Cu, Se and Cu/Se were not associated with sleep disorder risk.
Sociodemographic factors included age, sex, race, education level, family income level; behavioral characteristics included smoking, alcohol consumption, physical activity, and caffeine intake.
The researchers also used a restricted cubic spline model to examine the dose-response relationships between serum trace metals, serum trace metals ratios, and sleep disorders. In this analysis, higher levels of serum Zn, Zn/Cu, and Zn/Se were related to reduced risk of sleep disorders, while no significant association appeared between serum Cu, Se, or Cu/Se and sleep disorders risk.
The findings showing a lack of association between Se and sleep disorders were not consistent with previous studies, the researchers wrote in their discussion. Previous research has shown that a higher Se was less likely to be associated with trouble falling asleep, and has shown a potential treatment effect of Se on obstructive sleep apnea, they said.
“Although serum Cu and Se levels were not correlated to sleep disorders in our study, the Zn/Cu and Zn/Se may provide some novel insights,” they wrote. For example, Zn/Cu has been used as a predictor of several clinical complications related to an increased risk of sleep disorders including cardiovascular disease, cancer, and major depressive disorder, they noted.
The findings were limited by several factors including the cross-sectional design, use of self-reports, and the inability to examine relationships between trace metals and specific sleep disorder symptoms, such as restless legs syndrome, insomnia, and obstructive sleep apnea, the researchers noted.
However, the results were strengthened by the large national sample, and support data from previous studies, they said.
“The inverse associations of serum Zn, and Zn/Cu, Zn/Se with sleep disorders enlightened us that increasing Zn intake may be an excellent approach to prevent sleep disorders due to its benefits from these three aspects,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
, based on data from 3,660 individuals.
Previous research has shown an association between trace metals and sleep and sleep patterns, but data on the impact of serum trace metals on sleep disorders have been limited, wrote Ming-Gang Deng, MD, of Wuhan (China) University and colleagues.
In a study published in the Journal of Affective Disorders, the researchers reviewed data from the National Health and Nutrition Examination Survey (NHANES) 2011-2016 to calculate the odds ratios of sleep disorders and serum zinc (Zn), copper (Cu), and selenium (Se). The study population included adults aged 18 years and older, with an average age of 47.6 years. Approximately half of the participants were men, and the majority was non-Hispanic white. Serum Zn, Cu, and Se were identified at the Environmental Health Sciences Laboratory of the Centers for Disease Control and Prevention National Center for Environmental Health. The lower limits of detection for Zn, Cu, and Se were 2.9 mcg/dL, 2.5 mcg/dL, and 4.5 mcg/L, respectively. Sleep disorders were assessed based on self-reports of discussions with health professionals about sleep disorders, and via the Sleep Disorder Questionnaire.
After adjusting for sociodemographic, behavioral characteristics, and health characteristics, adults in the highest tertiles of serum Zn had a 30% reduced risk of sleep disorders, compared with those in the lowest tertiles of serum Zn (odds ratio, 0.70; P = .035). In measures of trace metals ratios, serum Zn/Cu and Zn/Se also were significantly associated with reduced risk of sleep disorders for individuals in the highest tertiles, compared with those in the lowest tertiles (OR, 0.62 and OR, 0.68, respectively).
However, serum Cu, Se and Cu/Se were not associated with sleep disorder risk.
Sociodemographic factors included age, sex, race, education level, family income level; behavioral characteristics included smoking, alcohol consumption, physical activity, and caffeine intake.
The researchers also used a restricted cubic spline model to examine the dose-response relationships between serum trace metals, serum trace metals ratios, and sleep disorders. In this analysis, higher levels of serum Zn, Zn/Cu, and Zn/Se were related to reduced risk of sleep disorders, while no significant association appeared between serum Cu, Se, or Cu/Se and sleep disorders risk.
The findings showing a lack of association between Se and sleep disorders were not consistent with previous studies, the researchers wrote in their discussion. Previous research has shown that a higher Se was less likely to be associated with trouble falling asleep, and has shown a potential treatment effect of Se on obstructive sleep apnea, they said.
“Although serum Cu and Se levels were not correlated to sleep disorders in our study, the Zn/Cu and Zn/Se may provide some novel insights,” they wrote. For example, Zn/Cu has been used as a predictor of several clinical complications related to an increased risk of sleep disorders including cardiovascular disease, cancer, and major depressive disorder, they noted.
The findings were limited by several factors including the cross-sectional design, use of self-reports, and the inability to examine relationships between trace metals and specific sleep disorder symptoms, such as restless legs syndrome, insomnia, and obstructive sleep apnea, the researchers noted.
However, the results were strengthened by the large national sample, and support data from previous studies, they said.
“The inverse associations of serum Zn, and Zn/Cu, Zn/Se with sleep disorders enlightened us that increasing Zn intake may be an excellent approach to prevent sleep disorders due to its benefits from these three aspects,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
, based on data from 3,660 individuals.
Previous research has shown an association between trace metals and sleep and sleep patterns, but data on the impact of serum trace metals on sleep disorders have been limited, wrote Ming-Gang Deng, MD, of Wuhan (China) University and colleagues.
In a study published in the Journal of Affective Disorders, the researchers reviewed data from the National Health and Nutrition Examination Survey (NHANES) 2011-2016 to calculate the odds ratios of sleep disorders and serum zinc (Zn), copper (Cu), and selenium (Se). The study population included adults aged 18 years and older, with an average age of 47.6 years. Approximately half of the participants were men, and the majority was non-Hispanic white. Serum Zn, Cu, and Se were identified at the Environmental Health Sciences Laboratory of the Centers for Disease Control and Prevention National Center for Environmental Health. The lower limits of detection for Zn, Cu, and Se were 2.9 mcg/dL, 2.5 mcg/dL, and 4.5 mcg/L, respectively. Sleep disorders were assessed based on self-reports of discussions with health professionals about sleep disorders, and via the Sleep Disorder Questionnaire.
After adjusting for sociodemographic, behavioral characteristics, and health characteristics, adults in the highest tertiles of serum Zn had a 30% reduced risk of sleep disorders, compared with those in the lowest tertiles of serum Zn (odds ratio, 0.70; P = .035). In measures of trace metals ratios, serum Zn/Cu and Zn/Se also were significantly associated with reduced risk of sleep disorders for individuals in the highest tertiles, compared with those in the lowest tertiles (OR, 0.62 and OR, 0.68, respectively).
However, serum Cu, Se and Cu/Se were not associated with sleep disorder risk.
Sociodemographic factors included age, sex, race, education level, family income level; behavioral characteristics included smoking, alcohol consumption, physical activity, and caffeine intake.
The researchers also used a restricted cubic spline model to examine the dose-response relationships between serum trace metals, serum trace metals ratios, and sleep disorders. In this analysis, higher levels of serum Zn, Zn/Cu, and Zn/Se were related to reduced risk of sleep disorders, while no significant association appeared between serum Cu, Se, or Cu/Se and sleep disorders risk.
The findings showing a lack of association between Se and sleep disorders were not consistent with previous studies, the researchers wrote in their discussion. Previous research has shown that a higher Se was less likely to be associated with trouble falling asleep, and has shown a potential treatment effect of Se on obstructive sleep apnea, they said.
“Although serum Cu and Se levels were not correlated to sleep disorders in our study, the Zn/Cu and Zn/Se may provide some novel insights,” they wrote. For example, Zn/Cu has been used as a predictor of several clinical complications related to an increased risk of sleep disorders including cardiovascular disease, cancer, and major depressive disorder, they noted.
The findings were limited by several factors including the cross-sectional design, use of self-reports, and the inability to examine relationships between trace metals and specific sleep disorder symptoms, such as restless legs syndrome, insomnia, and obstructive sleep apnea, the researchers noted.
However, the results were strengthened by the large national sample, and support data from previous studies, they said.
“The inverse associations of serum Zn, and Zn/Cu, Zn/Se with sleep disorders enlightened us that increasing Zn intake may be an excellent approach to prevent sleep disorders due to its benefits from these three aspects,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Sleep-disordered breathing promotes elevated arterial stiffness and preeclampsia
, based on data from 181 individuals.
The intermittent hypoxia resulting from sleep-disordered breathing (SDB) has been linked to cardiovascular disease and hypertension, wrote Kim Phan, PhD, of McGill University, Montreal, and colleagues.
SDB has been associated with increased preeclampsia risk, and women with preeclampsia show increased arterial stiffness, but an association between SDB and arterial stiffness in pregnancy has not been explored, they said.
In a study published in the American Journal of Obstetrics & Gynecology, the researchers reviewed data from 181 women with high-risk singleton pregnancies recruited from two tertiary obstetrics clinics in Montreal. High-risk pregnancy was defined as meeting at least one of the following criteria: age 35 years and older, body mass index 25 kg/m2 or higher, chronic hypertension, preexisting diabetes mellitus, preexisting renal disease, or personal or first-degree relative with a history of preeclampsia.
Participants were assessed at each trimester via the Epworth Sleepiness Scale, Pittsburgh Sleep Quality Index, and Restless Legs Syndrome questionnaire. Sleep-disordered breathing was defined as loud snoring or witnessed sleep apneas at least three times a week. Arterial stiffness was assessed via applanation tonometry every 4 weeks from baseline throughout pregnancy.
Overall, 23% of the study population met the criteria for SDB; SDB in the first or second trimester was associated with a significantly increased risk of preeclampsia (odds ratio 3.4). The effect of SDB on preeclampsia was increased in women who reported excessive daytime sleepiness, defined as scores higher than 10 on the Epworth Sleepiness Scale. The odds ratio for preeclampsia in the first or second trimester increased to 5.7 in women with hypersomnolence in addition to SDB. The risk of preeclampsia was even higher (OR 8.2) in the third trimester.
Self-reported total sleep time decreased in the second and third trimesters compared with the first, but reports of excessive daytime sleepiness remained consistent throughout the pregnancies, the researchers noted.
The results highlight the need to screen pregnant women for SDB in all three trimesters; however, “future studies will need to assess the incremental benefit of integrating SDB into risk assessment calculators in pregnancy,” the researchers wrote in their discussion. Randomized trials are needed to determine the value of interventions such as continuous positive airway pressure to reduce arterial stiffness and the risks of hypertensive disorders of pregnancy, they said. More data also are needed to examine the role of excessive daytime sleepiness as a modifier of arterial stiffness and preeclampsia risk, they noted.
The findings were limited by the prospective design, which prevents conclusions of causality, the researchers noted. Other limitations included the focus on high-risk pregnancy, which may limit generalizability, and the use of symptoms, not sleep recordings, to identify SDB, they said.
However, the results show an independent association between SDB and arterial stiffness during pregnancy, and offer potentially useful insights into the mechanisms of SDB-associated cardiovascular conditions, they noted.
“This work may inform future studies exploring the value of using arterial stiffness, as an early noninvasive indicator of subclinical vascular dysfunction in pregnant women with SDB,” they concluded.
The study was supported by the Fonds de recherche du Quebec – Sante (FRQS), Heart and Stroke Foundation of Canada, McGill University’s academic enrichment fund, and the Canadian Foundation for Women’s Health. The researchers had no financial conflicts to disclose.
, based on data from 181 individuals.
The intermittent hypoxia resulting from sleep-disordered breathing (SDB) has been linked to cardiovascular disease and hypertension, wrote Kim Phan, PhD, of McGill University, Montreal, and colleagues.
SDB has been associated with increased preeclampsia risk, and women with preeclampsia show increased arterial stiffness, but an association between SDB and arterial stiffness in pregnancy has not been explored, they said.
In a study published in the American Journal of Obstetrics & Gynecology, the researchers reviewed data from 181 women with high-risk singleton pregnancies recruited from two tertiary obstetrics clinics in Montreal. High-risk pregnancy was defined as meeting at least one of the following criteria: age 35 years and older, body mass index 25 kg/m2 or higher, chronic hypertension, preexisting diabetes mellitus, preexisting renal disease, or personal or first-degree relative with a history of preeclampsia.
Participants were assessed at each trimester via the Epworth Sleepiness Scale, Pittsburgh Sleep Quality Index, and Restless Legs Syndrome questionnaire. Sleep-disordered breathing was defined as loud snoring or witnessed sleep apneas at least three times a week. Arterial stiffness was assessed via applanation tonometry every 4 weeks from baseline throughout pregnancy.
Overall, 23% of the study population met the criteria for SDB; SDB in the first or second trimester was associated with a significantly increased risk of preeclampsia (odds ratio 3.4). The effect of SDB on preeclampsia was increased in women who reported excessive daytime sleepiness, defined as scores higher than 10 on the Epworth Sleepiness Scale. The odds ratio for preeclampsia in the first or second trimester increased to 5.7 in women with hypersomnolence in addition to SDB. The risk of preeclampsia was even higher (OR 8.2) in the third trimester.
Self-reported total sleep time decreased in the second and third trimesters compared with the first, but reports of excessive daytime sleepiness remained consistent throughout the pregnancies, the researchers noted.
The results highlight the need to screen pregnant women for SDB in all three trimesters; however, “future studies will need to assess the incremental benefit of integrating SDB into risk assessment calculators in pregnancy,” the researchers wrote in their discussion. Randomized trials are needed to determine the value of interventions such as continuous positive airway pressure to reduce arterial stiffness and the risks of hypertensive disorders of pregnancy, they said. More data also are needed to examine the role of excessive daytime sleepiness as a modifier of arterial stiffness and preeclampsia risk, they noted.
The findings were limited by the prospective design, which prevents conclusions of causality, the researchers noted. Other limitations included the focus on high-risk pregnancy, which may limit generalizability, and the use of symptoms, not sleep recordings, to identify SDB, they said.
However, the results show an independent association between SDB and arterial stiffness during pregnancy, and offer potentially useful insights into the mechanisms of SDB-associated cardiovascular conditions, they noted.
“This work may inform future studies exploring the value of using arterial stiffness, as an early noninvasive indicator of subclinical vascular dysfunction in pregnant women with SDB,” they concluded.
The study was supported by the Fonds de recherche du Quebec – Sante (FRQS), Heart and Stroke Foundation of Canada, McGill University’s academic enrichment fund, and the Canadian Foundation for Women’s Health. The researchers had no financial conflicts to disclose.
, based on data from 181 individuals.
The intermittent hypoxia resulting from sleep-disordered breathing (SDB) has been linked to cardiovascular disease and hypertension, wrote Kim Phan, PhD, of McGill University, Montreal, and colleagues.
SDB has been associated with increased preeclampsia risk, and women with preeclampsia show increased arterial stiffness, but an association between SDB and arterial stiffness in pregnancy has not been explored, they said.
In a study published in the American Journal of Obstetrics & Gynecology, the researchers reviewed data from 181 women with high-risk singleton pregnancies recruited from two tertiary obstetrics clinics in Montreal. High-risk pregnancy was defined as meeting at least one of the following criteria: age 35 years and older, body mass index 25 kg/m2 or higher, chronic hypertension, preexisting diabetes mellitus, preexisting renal disease, or personal or first-degree relative with a history of preeclampsia.
Participants were assessed at each trimester via the Epworth Sleepiness Scale, Pittsburgh Sleep Quality Index, and Restless Legs Syndrome questionnaire. Sleep-disordered breathing was defined as loud snoring or witnessed sleep apneas at least three times a week. Arterial stiffness was assessed via applanation tonometry every 4 weeks from baseline throughout pregnancy.
Overall, 23% of the study population met the criteria for SDB; SDB in the first or second trimester was associated with a significantly increased risk of preeclampsia (odds ratio 3.4). The effect of SDB on preeclampsia was increased in women who reported excessive daytime sleepiness, defined as scores higher than 10 on the Epworth Sleepiness Scale. The odds ratio for preeclampsia in the first or second trimester increased to 5.7 in women with hypersomnolence in addition to SDB. The risk of preeclampsia was even higher (OR 8.2) in the third trimester.
Self-reported total sleep time decreased in the second and third trimesters compared with the first, but reports of excessive daytime sleepiness remained consistent throughout the pregnancies, the researchers noted.
The results highlight the need to screen pregnant women for SDB in all three trimesters; however, “future studies will need to assess the incremental benefit of integrating SDB into risk assessment calculators in pregnancy,” the researchers wrote in their discussion. Randomized trials are needed to determine the value of interventions such as continuous positive airway pressure to reduce arterial stiffness and the risks of hypertensive disorders of pregnancy, they said. More data also are needed to examine the role of excessive daytime sleepiness as a modifier of arterial stiffness and preeclampsia risk, they noted.
The findings were limited by the prospective design, which prevents conclusions of causality, the researchers noted. Other limitations included the focus on high-risk pregnancy, which may limit generalizability, and the use of symptoms, not sleep recordings, to identify SDB, they said.
However, the results show an independent association between SDB and arterial stiffness during pregnancy, and offer potentially useful insights into the mechanisms of SDB-associated cardiovascular conditions, they noted.
“This work may inform future studies exploring the value of using arterial stiffness, as an early noninvasive indicator of subclinical vascular dysfunction in pregnant women with SDB,” they concluded.
The study was supported by the Fonds de recherche du Quebec – Sante (FRQS), Heart and Stroke Foundation of Canada, McGill University’s academic enrichment fund, and the Canadian Foundation for Women’s Health. The researchers had no financial conflicts to disclose.
FROM THE AMERICAN JOURNAL OF OBSTETRICS & GYNECOLOGY
Severe OSA tied to poor prognoses in stroke patients
Patients with acute ischemic stroke had a worse prognosis if they had also experienced severe obstructive sleep apnea (OSA), based on data from 125 individuals.
OSA is on the rise, and is associated with pathophysiological changes, and data from previous studies suggest that severe OSA doubles the risk of stroke and increases risk of stroke recurrence, according to Juan Xu, PhD, of Soochow University, Suzhou, China, and colleagues.
“There is a high comorbidity between stroke and OSA,” and effective sleep is important to cerebral function recovery, the researchers wrote. Early prediction of stroke prognosis may inform treatment in stroke patients, but the value of OSA as a predictor of functional prognosis has not been explored.
In a study published in Sleep Medicine, the researchers analyzed data from 125 adults with mild to moderate ischemic stroke and OSA. The participants underwent polysomnography within a week of stroke onset between January 2015 and June 2020 and were grouped by severity according to apnea-hypopnea index (AHI) of either less than 30/h (not severe) or 30/h or higher (severe). The mean age of the patients was 58 years, and 87% were men. Approximately one-third of the participants met the criteria for severe OSA.
The researchers assessed the impact of OSA on functional prognosis in the acute phase of stroke, and reviewed quantitative electroencephalography (EEG) markers in stroke patients during sleep.
Overall, individuals with severe OSA were significantly more likely than those with less severe OSA to have comorbid hypertension (85.4% vs. 56%; P = .002) and a higher body mass index (28 vs. 24; P < .001). Other factors including blood pressure, smoking history, alcohol use, and comorbid diabetes were similar between the groups.
Quantitative EEG among patients with severe OSA showed lower relative power of high-frequency bands (alpha, beta, and sigma). The EEG also showed higher delta/alpha power ratio and slowing ratio, and higher delta relative power (delta RP) in severe OSA (P < .05 for all).
In addition, severe OSA was associated with more than triple the risk (3.6-fold increase) of poor prognosis, defined as a Modified Rankin Scale score of 3 or higher (24.4% for severe OSA vs. 8.3% for nonsevere OSA; P = .03).
the researchers wrote. “Integrating the alteration of quantitative EEG parameters may improve the accuracy of early predictions of functional prognosis in patients with stroke.”
The findings were limited by several factors including the retrospective design and the lack of a sizable non-OSA control group, the researchers noted. Other limitations included the use of an AHI of 30/h or higher to define severity and the use of data from medical histories, with the potential for information bias, and the use of only 30-second continuous polysomnography segments.
However, the results suggest that increased delta RP and TSR, and decreased alpha, beta, and sigma RP, may be independent predictors of a poor functional prognosis in stroke patients with OSA, and that the prognosis could be improved by treating the OSA, they concluded.
The study was supported by the Natural Science Foundation of China and the Discipline Construction Program of the Second Affiliated Hospital of Soochow University. The researchers reported no financial conflicts.
A version of this article first appeared on Medscape.com.
Patients with acute ischemic stroke had a worse prognosis if they had also experienced severe obstructive sleep apnea (OSA), based on data from 125 individuals.
OSA is on the rise, and is associated with pathophysiological changes, and data from previous studies suggest that severe OSA doubles the risk of stroke and increases risk of stroke recurrence, according to Juan Xu, PhD, of Soochow University, Suzhou, China, and colleagues.
“There is a high comorbidity between stroke and OSA,” and effective sleep is important to cerebral function recovery, the researchers wrote. Early prediction of stroke prognosis may inform treatment in stroke patients, but the value of OSA as a predictor of functional prognosis has not been explored.
In a study published in Sleep Medicine, the researchers analyzed data from 125 adults with mild to moderate ischemic stroke and OSA. The participants underwent polysomnography within a week of stroke onset between January 2015 and June 2020 and were grouped by severity according to apnea-hypopnea index (AHI) of either less than 30/h (not severe) or 30/h or higher (severe). The mean age of the patients was 58 years, and 87% were men. Approximately one-third of the participants met the criteria for severe OSA.
The researchers assessed the impact of OSA on functional prognosis in the acute phase of stroke, and reviewed quantitative electroencephalography (EEG) markers in stroke patients during sleep.
Overall, individuals with severe OSA were significantly more likely than those with less severe OSA to have comorbid hypertension (85.4% vs. 56%; P = .002) and a higher body mass index (28 vs. 24; P < .001). Other factors including blood pressure, smoking history, alcohol use, and comorbid diabetes were similar between the groups.
Quantitative EEG among patients with severe OSA showed lower relative power of high-frequency bands (alpha, beta, and sigma). The EEG also showed higher delta/alpha power ratio and slowing ratio, and higher delta relative power (delta RP) in severe OSA (P < .05 for all).
In addition, severe OSA was associated with more than triple the risk (3.6-fold increase) of poor prognosis, defined as a Modified Rankin Scale score of 3 or higher (24.4% for severe OSA vs. 8.3% for nonsevere OSA; P = .03).
the researchers wrote. “Integrating the alteration of quantitative EEG parameters may improve the accuracy of early predictions of functional prognosis in patients with stroke.”
The findings were limited by several factors including the retrospective design and the lack of a sizable non-OSA control group, the researchers noted. Other limitations included the use of an AHI of 30/h or higher to define severity and the use of data from medical histories, with the potential for information bias, and the use of only 30-second continuous polysomnography segments.
However, the results suggest that increased delta RP and TSR, and decreased alpha, beta, and sigma RP, may be independent predictors of a poor functional prognosis in stroke patients with OSA, and that the prognosis could be improved by treating the OSA, they concluded.
The study was supported by the Natural Science Foundation of China and the Discipline Construction Program of the Second Affiliated Hospital of Soochow University. The researchers reported no financial conflicts.
A version of this article first appeared on Medscape.com.
Patients with acute ischemic stroke had a worse prognosis if they had also experienced severe obstructive sleep apnea (OSA), based on data from 125 individuals.
OSA is on the rise, and is associated with pathophysiological changes, and data from previous studies suggest that severe OSA doubles the risk of stroke and increases risk of stroke recurrence, according to Juan Xu, PhD, of Soochow University, Suzhou, China, and colleagues.
“There is a high comorbidity between stroke and OSA,” and effective sleep is important to cerebral function recovery, the researchers wrote. Early prediction of stroke prognosis may inform treatment in stroke patients, but the value of OSA as a predictor of functional prognosis has not been explored.
In a study published in Sleep Medicine, the researchers analyzed data from 125 adults with mild to moderate ischemic stroke and OSA. The participants underwent polysomnography within a week of stroke onset between January 2015 and June 2020 and were grouped by severity according to apnea-hypopnea index (AHI) of either less than 30/h (not severe) or 30/h or higher (severe). The mean age of the patients was 58 years, and 87% were men. Approximately one-third of the participants met the criteria for severe OSA.
The researchers assessed the impact of OSA on functional prognosis in the acute phase of stroke, and reviewed quantitative electroencephalography (EEG) markers in stroke patients during sleep.
Overall, individuals with severe OSA were significantly more likely than those with less severe OSA to have comorbid hypertension (85.4% vs. 56%; P = .002) and a higher body mass index (28 vs. 24; P < .001). Other factors including blood pressure, smoking history, alcohol use, and comorbid diabetes were similar between the groups.
Quantitative EEG among patients with severe OSA showed lower relative power of high-frequency bands (alpha, beta, and sigma). The EEG also showed higher delta/alpha power ratio and slowing ratio, and higher delta relative power (delta RP) in severe OSA (P < .05 for all).
In addition, severe OSA was associated with more than triple the risk (3.6-fold increase) of poor prognosis, defined as a Modified Rankin Scale score of 3 or higher (24.4% for severe OSA vs. 8.3% for nonsevere OSA; P = .03).
the researchers wrote. “Integrating the alteration of quantitative EEG parameters may improve the accuracy of early predictions of functional prognosis in patients with stroke.”
The findings were limited by several factors including the retrospective design and the lack of a sizable non-OSA control group, the researchers noted. Other limitations included the use of an AHI of 30/h or higher to define severity and the use of data from medical histories, with the potential for information bias, and the use of only 30-second continuous polysomnography segments.
However, the results suggest that increased delta RP and TSR, and decreased alpha, beta, and sigma RP, may be independent predictors of a poor functional prognosis in stroke patients with OSA, and that the prognosis could be improved by treating the OSA, they concluded.
The study was supported by the Natural Science Foundation of China and the Discipline Construction Program of the Second Affiliated Hospital of Soochow University. The researchers reported no financial conflicts.
A version of this article first appeared on Medscape.com.
FROM SLEEP MEDICINE
Mothers’ sleep issues promote poor outcomes for infants
or insomnia, based on data from approximately 5,000 infants.
Sleep disturbance is common during pregnancy, and “sleep disorders during pregnancy can have significant consequences for both the pregnant person and their infant,” write Jennifer N. Felder, PhD, of the University of California, San Francisco, and colleagues.
However, data on the impact of maternal insomnia on specific infant outcomes are limited, they said.
In a study published recently in the journal Sleep Health, the researchers reviewed data from 3,371 pregnant women diagnosed with sleep apnea and 3,213 with insomnia. Of these, 2,357 and 2,212 were matched with controls in a propensity-score analysis. The referent controls were matched for maternal characteristics, obstetric factors, and infant factors among individuals without a sleep disorder. All were singleton pregnancies.
Adverse infant outcomes included the following:
- One- and 5-minute Apgar scores less than 7.
- Respiratory distress syndrome.
- Neonatal intensive care unit admission.
- Hypoglycemia.
- Infant death.
- Hospital stay of longer than 2 days for vaginal delivery or longer than 4 days for cesarean delivery.
- Emergency department visit before 3 months of age.
- Emergency department visit in the first year of life.
- Composite measure of adverse infant outcomes.
Compared with matched controls, the infants born to mothers with sleep apnea had a significantly increased risk for any adverse outcome (50.1% vs. 53.5%) and of the specific outcomes of low 1-minute Apgar scores (6.3% vs. 9.6%), neonatal ICU stays (6.3% vs. 8.4%), and an emergency department visit in the first year of life (33.6% vs. 36.9%).
For infants born to mothers with insomnia, the only significant difference in outcomes compared with controls was an increased likelihood of an emergency department visit (37.2% vs. 32.3%).
“Research on possible mechanisms of the relation between maternal prenatal sleep apnea and poorer birth and infant outcomes associations is small but growing, implicating systemic inflammation and late or prolonged fetal heart rate decelerations,” the researchers write in their discussion.
Research on insomnia during pregnancy and adverse infant outcomes is limited, and the largest studies have been complicated by the effects of insomnia medication; therefore, “our finding that infants born to mothers with an insomnia diagnosis were at increased risk of only emergency room visit, but no other analyzed infant outcomes, is important and novel,” they note.
The findings were limited by several factors, including the reliance on medical records, which may lack details on how routinely health care professionals assessed sleep disorders, the researchers noted. “Consequently, the findings presented here may reflect more severe cases of insomnia and sleep apnea, and may not represent the population of individuals with diagnosed sleep apnea or insomnia during pregnancy generally,” the authors say. Other limitations included a lack of information on treatment of sleep disorders and on the timing of diagnosis (before pregnancy or during pregnancy).
However, the results were strengthened by the large, population-based sample and use of codes to highlight research questions, the researchers said.
In light of the health consequences of sleep disorders in pregnancy, the data suggest that sleep apnea and insomnia in pregnant women may serve as targets for risk assessment of adverse infant outcomes, and more research is needed to determine whether addressing sleep issues reduces these outcomes, they concluded.
The study was supported by the University of California, San Francisco, Preterm Birth Initiative and by grants to lead author Dr. Felder from the National Center for Complementary and Integrative Health and to a coauthor from the National Heart, Lung, and Blood Institute. The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
or insomnia, based on data from approximately 5,000 infants.
Sleep disturbance is common during pregnancy, and “sleep disorders during pregnancy can have significant consequences for both the pregnant person and their infant,” write Jennifer N. Felder, PhD, of the University of California, San Francisco, and colleagues.
However, data on the impact of maternal insomnia on specific infant outcomes are limited, they said.
In a study published recently in the journal Sleep Health, the researchers reviewed data from 3,371 pregnant women diagnosed with sleep apnea and 3,213 with insomnia. Of these, 2,357 and 2,212 were matched with controls in a propensity-score analysis. The referent controls were matched for maternal characteristics, obstetric factors, and infant factors among individuals without a sleep disorder. All were singleton pregnancies.
Adverse infant outcomes included the following:
- One- and 5-minute Apgar scores less than 7.
- Respiratory distress syndrome.
- Neonatal intensive care unit admission.
- Hypoglycemia.
- Infant death.
- Hospital stay of longer than 2 days for vaginal delivery or longer than 4 days for cesarean delivery.
- Emergency department visit before 3 months of age.
- Emergency department visit in the first year of life.
- Composite measure of adverse infant outcomes.
Compared with matched controls, the infants born to mothers with sleep apnea had a significantly increased risk for any adverse outcome (50.1% vs. 53.5%) and of the specific outcomes of low 1-minute Apgar scores (6.3% vs. 9.6%), neonatal ICU stays (6.3% vs. 8.4%), and an emergency department visit in the first year of life (33.6% vs. 36.9%).
For infants born to mothers with insomnia, the only significant difference in outcomes compared with controls was an increased likelihood of an emergency department visit (37.2% vs. 32.3%).
“Research on possible mechanisms of the relation between maternal prenatal sleep apnea and poorer birth and infant outcomes associations is small but growing, implicating systemic inflammation and late or prolonged fetal heart rate decelerations,” the researchers write in their discussion.
Research on insomnia during pregnancy and adverse infant outcomes is limited, and the largest studies have been complicated by the effects of insomnia medication; therefore, “our finding that infants born to mothers with an insomnia diagnosis were at increased risk of only emergency room visit, but no other analyzed infant outcomes, is important and novel,” they note.
The findings were limited by several factors, including the reliance on medical records, which may lack details on how routinely health care professionals assessed sleep disorders, the researchers noted. “Consequently, the findings presented here may reflect more severe cases of insomnia and sleep apnea, and may not represent the population of individuals with diagnosed sleep apnea or insomnia during pregnancy generally,” the authors say. Other limitations included a lack of information on treatment of sleep disorders and on the timing of diagnosis (before pregnancy or during pregnancy).
However, the results were strengthened by the large, population-based sample and use of codes to highlight research questions, the researchers said.
In light of the health consequences of sleep disorders in pregnancy, the data suggest that sleep apnea and insomnia in pregnant women may serve as targets for risk assessment of adverse infant outcomes, and more research is needed to determine whether addressing sleep issues reduces these outcomes, they concluded.
The study was supported by the University of California, San Francisco, Preterm Birth Initiative and by grants to lead author Dr. Felder from the National Center for Complementary and Integrative Health and to a coauthor from the National Heart, Lung, and Blood Institute. The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
or insomnia, based on data from approximately 5,000 infants.
Sleep disturbance is common during pregnancy, and “sleep disorders during pregnancy can have significant consequences for both the pregnant person and their infant,” write Jennifer N. Felder, PhD, of the University of California, San Francisco, and colleagues.
However, data on the impact of maternal insomnia on specific infant outcomes are limited, they said.
In a study published recently in the journal Sleep Health, the researchers reviewed data from 3,371 pregnant women diagnosed with sleep apnea and 3,213 with insomnia. Of these, 2,357 and 2,212 were matched with controls in a propensity-score analysis. The referent controls were matched for maternal characteristics, obstetric factors, and infant factors among individuals without a sleep disorder. All were singleton pregnancies.
Adverse infant outcomes included the following:
- One- and 5-minute Apgar scores less than 7.
- Respiratory distress syndrome.
- Neonatal intensive care unit admission.
- Hypoglycemia.
- Infant death.
- Hospital stay of longer than 2 days for vaginal delivery or longer than 4 days for cesarean delivery.
- Emergency department visit before 3 months of age.
- Emergency department visit in the first year of life.
- Composite measure of adverse infant outcomes.
Compared with matched controls, the infants born to mothers with sleep apnea had a significantly increased risk for any adverse outcome (50.1% vs. 53.5%) and of the specific outcomes of low 1-minute Apgar scores (6.3% vs. 9.6%), neonatal ICU stays (6.3% vs. 8.4%), and an emergency department visit in the first year of life (33.6% vs. 36.9%).
For infants born to mothers with insomnia, the only significant difference in outcomes compared with controls was an increased likelihood of an emergency department visit (37.2% vs. 32.3%).
“Research on possible mechanisms of the relation between maternal prenatal sleep apnea and poorer birth and infant outcomes associations is small but growing, implicating systemic inflammation and late or prolonged fetal heart rate decelerations,” the researchers write in their discussion.
Research on insomnia during pregnancy and adverse infant outcomes is limited, and the largest studies have been complicated by the effects of insomnia medication; therefore, “our finding that infants born to mothers with an insomnia diagnosis were at increased risk of only emergency room visit, but no other analyzed infant outcomes, is important and novel,” they note.
The findings were limited by several factors, including the reliance on medical records, which may lack details on how routinely health care professionals assessed sleep disorders, the researchers noted. “Consequently, the findings presented here may reflect more severe cases of insomnia and sleep apnea, and may not represent the population of individuals with diagnosed sleep apnea or insomnia during pregnancy generally,” the authors say. Other limitations included a lack of information on treatment of sleep disorders and on the timing of diagnosis (before pregnancy or during pregnancy).
However, the results were strengthened by the large, population-based sample and use of codes to highlight research questions, the researchers said.
In light of the health consequences of sleep disorders in pregnancy, the data suggest that sleep apnea and insomnia in pregnant women may serve as targets for risk assessment of adverse infant outcomes, and more research is needed to determine whether addressing sleep issues reduces these outcomes, they concluded.
The study was supported by the University of California, San Francisco, Preterm Birth Initiative and by grants to lead author Dr. Felder from the National Center for Complementary and Integrative Health and to a coauthor from the National Heart, Lung, and Blood Institute. The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM SLEEP HEALTH
Improving sleep boosts cognition in refractory temporal lobe epilepsy
NASHVILLE, TENN. – Targeting relevant sleep problems for patients with refractory temporal lobe epilepsy (TLE) improves cognition, results of a new, double-blind, randomized controlled trial suggest.
Study findings show significant improvement in REM sleep and language scores for patients with TLE who took the cholinesterase inhibitor donepezil and better slow-wave sleep and memory scores for those who took the sleep aid zolpidem.
, study investigator Garima Shukla, MBBS, MD, DM, professor, division of neurology, department of medicine, Queens University, Kingston, Ont., told this news organization.
Daytime sleepiness could be a red flag in these patients, although it could mean they just have treatable sleep apnea, said Dr. Shukla. “But if they have very poor slow-wave sleep, we could try increasing its percentage by prescribing zolpidem.”
The findings were presented at the annual meeting of the American Epilepsy Society.
Sleep, cognitive disturbances common
Sleep disturbances and cognitive disturbances are common among patients with TLE. Executive function is affected in almost all patients with refractory epilepsy, and it’s “super common” that TLE patients have memory disturbances, said Dr. Shukla.
The study included 108 patients with refractory TLE who were awaiting surgery. The patients, who had no severe comorbidities, were randomly assigned to three groups; the final number in each group was 36.
Patients in group 1 received donepezil 10 mg in the morning and a placebo at night. (Donepezil is used to treat memory loss associated with Alzheimer’s disease.)
Those in group 2 received a placebo in the morning and zolpidem 6.25 mg at night. Group 3 patients received a placebo in the morning and again at night.
The mean age of the patients was 25.4, 27.1, and 27.6 years, and the percentage of men was 63.8%, 72.2%, and 63.8% in groups 1, 2, and 3, respectively.
In all groups, patients had been experiencing about three seizures per month. The median number of antiseizure medications was two in group 1 and three in both groups 2 and 3.
Researchers evaluated sleep using the Pittsburgh Sleep Quality Index, the Epsworth Sleepiness Scale, and video polysomnography and electroencephalography.
To assess executive function, they used the Trail A & B, Stroop, and forward and backward Digit Span tests. For memory, they used the Weschler Memory Scale, and for language, the Western Aphasia Battery. They conducted follow-up evaluations at 6 months.
The results showed significant improvement in the percentage of rapid eye movement (REM) sleep in group 1 (from 14.81 at baseline to 18.21 at 6 months). In this group, the number of patients whose REM sleep percentage was less than 15 dropped significantly from 29 (of 36) to 10.
In group 2, sleep-onset latency significantly improved, and the percentage of N3 (slow-wave) sleep stage increased significantly from 25.27 to 28.74.
Regarding cognitive outcomes, backward Digit Span was significantly improved for patients in group 1. In this group, there was also a significant reduction in the time taken for Stroop A test, and there was significant improvement in language.
In group 2, there was a significant improvement in verbal and visual memory scores. There were no significant changes in group 3.
The increase in REM sleep percentage in group 1 strongly correlated with increased language and executive function scores. Similarly, in group 2, the increase in N3 sleep percentage strongly correlated with an increase in verbal memory scores.
On the basis of these observations, giving a small dose of zolpidem to a patient with “acceptable” REM sleep but very little slow-wave sleep may boost the patient’s non-REM sleep, said Dr. Shukla. “By improving non-REM sleep percentage, we will possibly help memory consolidation.”
Dr. Shukla sees this study as “a stepping-stone” to larger, multicenter trials testing “the effect of zolpidem through its impact on improving non-REM sleep percentage consolidation and its impact on memory.”
This idea veers somewhat from the traditional idea that REM sleep plays a greater role in memory consolidation, she said. “We actually found it correlates very well with language, which we have also seen in some of our anecdotal case reports.”
Patients whose language scores are very poor are “the population I would pick to target REM sleep through donepezil,” said Dr. Shukla.
‘Encouraging’ findings
Commenting for this news organization, Daniel Goldenholz, MD, PhD, assistant professor, Harvard Beth Israel Deaconess Medical Center, Boston, praised the study design.
“It allows for comparison between different treatments, as well as a placebo control group,” said Dr. Goldenholz, who added, “There appears to be good follow-up” as well.
The fact that medication may provide some cognitive benefit for patients with TLE is “very encouraging,” he said.
He noted many patients with TLE complain of memory or language problems. “So, this is a major concern.”
However, he cautioned about side effects. “Putting all temporal lobe epilepsy patients who say that they have memory problems or language problems on these medications could have some serious consequences.”
The study was funded by a Department of Health Research grant from the government of India. Dr. Goldenholz is on the advisory board for epilepsy AI, Eyzs, and Magic Leap.
A version of this article first appeared on Medscape.com.
NASHVILLE, TENN. – Targeting relevant sleep problems for patients with refractory temporal lobe epilepsy (TLE) improves cognition, results of a new, double-blind, randomized controlled trial suggest.
Study findings show significant improvement in REM sleep and language scores for patients with TLE who took the cholinesterase inhibitor donepezil and better slow-wave sleep and memory scores for those who took the sleep aid zolpidem.
, study investigator Garima Shukla, MBBS, MD, DM, professor, division of neurology, department of medicine, Queens University, Kingston, Ont., told this news organization.
Daytime sleepiness could be a red flag in these patients, although it could mean they just have treatable sleep apnea, said Dr. Shukla. “But if they have very poor slow-wave sleep, we could try increasing its percentage by prescribing zolpidem.”
The findings were presented at the annual meeting of the American Epilepsy Society.
Sleep, cognitive disturbances common
Sleep disturbances and cognitive disturbances are common among patients with TLE. Executive function is affected in almost all patients with refractory epilepsy, and it’s “super common” that TLE patients have memory disturbances, said Dr. Shukla.
The study included 108 patients with refractory TLE who were awaiting surgery. The patients, who had no severe comorbidities, were randomly assigned to three groups; the final number in each group was 36.
Patients in group 1 received donepezil 10 mg in the morning and a placebo at night. (Donepezil is used to treat memory loss associated with Alzheimer’s disease.)
Those in group 2 received a placebo in the morning and zolpidem 6.25 mg at night. Group 3 patients received a placebo in the morning and again at night.
The mean age of the patients was 25.4, 27.1, and 27.6 years, and the percentage of men was 63.8%, 72.2%, and 63.8% in groups 1, 2, and 3, respectively.
In all groups, patients had been experiencing about three seizures per month. The median number of antiseizure medications was two in group 1 and three in both groups 2 and 3.
Researchers evaluated sleep using the Pittsburgh Sleep Quality Index, the Epsworth Sleepiness Scale, and video polysomnography and electroencephalography.
To assess executive function, they used the Trail A & B, Stroop, and forward and backward Digit Span tests. For memory, they used the Weschler Memory Scale, and for language, the Western Aphasia Battery. They conducted follow-up evaluations at 6 months.
The results showed significant improvement in the percentage of rapid eye movement (REM) sleep in group 1 (from 14.81 at baseline to 18.21 at 6 months). In this group, the number of patients whose REM sleep percentage was less than 15 dropped significantly from 29 (of 36) to 10.
In group 2, sleep-onset latency significantly improved, and the percentage of N3 (slow-wave) sleep stage increased significantly from 25.27 to 28.74.
Regarding cognitive outcomes, backward Digit Span was significantly improved for patients in group 1. In this group, there was also a significant reduction in the time taken for Stroop A test, and there was significant improvement in language.
In group 2, there was a significant improvement in verbal and visual memory scores. There were no significant changes in group 3.
The increase in REM sleep percentage in group 1 strongly correlated with increased language and executive function scores. Similarly, in group 2, the increase in N3 sleep percentage strongly correlated with an increase in verbal memory scores.
On the basis of these observations, giving a small dose of zolpidem to a patient with “acceptable” REM sleep but very little slow-wave sleep may boost the patient’s non-REM sleep, said Dr. Shukla. “By improving non-REM sleep percentage, we will possibly help memory consolidation.”
Dr. Shukla sees this study as “a stepping-stone” to larger, multicenter trials testing “the effect of zolpidem through its impact on improving non-REM sleep percentage consolidation and its impact on memory.”
This idea veers somewhat from the traditional idea that REM sleep plays a greater role in memory consolidation, she said. “We actually found it correlates very well with language, which we have also seen in some of our anecdotal case reports.”
Patients whose language scores are very poor are “the population I would pick to target REM sleep through donepezil,” said Dr. Shukla.
‘Encouraging’ findings
Commenting for this news organization, Daniel Goldenholz, MD, PhD, assistant professor, Harvard Beth Israel Deaconess Medical Center, Boston, praised the study design.
“It allows for comparison between different treatments, as well as a placebo control group,” said Dr. Goldenholz, who added, “There appears to be good follow-up” as well.
The fact that medication may provide some cognitive benefit for patients with TLE is “very encouraging,” he said.
He noted many patients with TLE complain of memory or language problems. “So, this is a major concern.”
However, he cautioned about side effects. “Putting all temporal lobe epilepsy patients who say that they have memory problems or language problems on these medications could have some serious consequences.”
The study was funded by a Department of Health Research grant from the government of India. Dr. Goldenholz is on the advisory board for epilepsy AI, Eyzs, and Magic Leap.
A version of this article first appeared on Medscape.com.
NASHVILLE, TENN. – Targeting relevant sleep problems for patients with refractory temporal lobe epilepsy (TLE) improves cognition, results of a new, double-blind, randomized controlled trial suggest.
Study findings show significant improvement in REM sleep and language scores for patients with TLE who took the cholinesterase inhibitor donepezil and better slow-wave sleep and memory scores for those who took the sleep aid zolpidem.
, study investigator Garima Shukla, MBBS, MD, DM, professor, division of neurology, department of medicine, Queens University, Kingston, Ont., told this news organization.
Daytime sleepiness could be a red flag in these patients, although it could mean they just have treatable sleep apnea, said Dr. Shukla. “But if they have very poor slow-wave sleep, we could try increasing its percentage by prescribing zolpidem.”
The findings were presented at the annual meeting of the American Epilepsy Society.
Sleep, cognitive disturbances common
Sleep disturbances and cognitive disturbances are common among patients with TLE. Executive function is affected in almost all patients with refractory epilepsy, and it’s “super common” that TLE patients have memory disturbances, said Dr. Shukla.
The study included 108 patients with refractory TLE who were awaiting surgery. The patients, who had no severe comorbidities, were randomly assigned to three groups; the final number in each group was 36.
Patients in group 1 received donepezil 10 mg in the morning and a placebo at night. (Donepezil is used to treat memory loss associated with Alzheimer’s disease.)
Those in group 2 received a placebo in the morning and zolpidem 6.25 mg at night. Group 3 patients received a placebo in the morning and again at night.
The mean age of the patients was 25.4, 27.1, and 27.6 years, and the percentage of men was 63.8%, 72.2%, and 63.8% in groups 1, 2, and 3, respectively.
In all groups, patients had been experiencing about three seizures per month. The median number of antiseizure medications was two in group 1 and three in both groups 2 and 3.
Researchers evaluated sleep using the Pittsburgh Sleep Quality Index, the Epsworth Sleepiness Scale, and video polysomnography and electroencephalography.
To assess executive function, they used the Trail A & B, Stroop, and forward and backward Digit Span tests. For memory, they used the Weschler Memory Scale, and for language, the Western Aphasia Battery. They conducted follow-up evaluations at 6 months.
The results showed significant improvement in the percentage of rapid eye movement (REM) sleep in group 1 (from 14.81 at baseline to 18.21 at 6 months). In this group, the number of patients whose REM sleep percentage was less than 15 dropped significantly from 29 (of 36) to 10.
In group 2, sleep-onset latency significantly improved, and the percentage of N3 (slow-wave) sleep stage increased significantly from 25.27 to 28.74.
Regarding cognitive outcomes, backward Digit Span was significantly improved for patients in group 1. In this group, there was also a significant reduction in the time taken for Stroop A test, and there was significant improvement in language.
In group 2, there was a significant improvement in verbal and visual memory scores. There were no significant changes in group 3.
The increase in REM sleep percentage in group 1 strongly correlated with increased language and executive function scores. Similarly, in group 2, the increase in N3 sleep percentage strongly correlated with an increase in verbal memory scores.
On the basis of these observations, giving a small dose of zolpidem to a patient with “acceptable” REM sleep but very little slow-wave sleep may boost the patient’s non-REM sleep, said Dr. Shukla. “By improving non-REM sleep percentage, we will possibly help memory consolidation.”
Dr. Shukla sees this study as “a stepping-stone” to larger, multicenter trials testing “the effect of zolpidem through its impact on improving non-REM sleep percentage consolidation and its impact on memory.”
This idea veers somewhat from the traditional idea that REM sleep plays a greater role in memory consolidation, she said. “We actually found it correlates very well with language, which we have also seen in some of our anecdotal case reports.”
Patients whose language scores are very poor are “the population I would pick to target REM sleep through donepezil,” said Dr. Shukla.
‘Encouraging’ findings
Commenting for this news organization, Daniel Goldenholz, MD, PhD, assistant professor, Harvard Beth Israel Deaconess Medical Center, Boston, praised the study design.
“It allows for comparison between different treatments, as well as a placebo control group,” said Dr. Goldenholz, who added, “There appears to be good follow-up” as well.
The fact that medication may provide some cognitive benefit for patients with TLE is “very encouraging,” he said.
He noted many patients with TLE complain of memory or language problems. “So, this is a major concern.”
However, he cautioned about side effects. “Putting all temporal lobe epilepsy patients who say that they have memory problems or language problems on these medications could have some serious consequences.”
The study was funded by a Department of Health Research grant from the government of India. Dr. Goldenholz is on the advisory board for epilepsy AI, Eyzs, and Magic Leap.
A version of this article first appeared on Medscape.com.
AT AES 2022
Chromosomal test may ID risk for sudden infant deaths
Researchers have identified pathogenic gene variations in 12% of cases of sudden unexplained death in children.
The new study, which involved 116 cases of sudden infant death syndrome or sudden unexplained deaths in children (SUDC), suggests that available methods of chromosome testing could be used to help screen for the conditions, which together account for roughly 1,800 fatalities a year in the United States.
“Even though the Back to Sleep campaign has been incredibly effective and safe sleep practices have been promoted for years, sudden unexplained death in pediatrics remains a leading cause of death for infants and children,” said Catherine Brownstein, MPH, PhD, of Boston Children’s Hospital, lead author of the new study.
The findings suggest that chromosomal microarray analysis (CMA), the method that the researchers used in the study, “should be considered in the genetic evaluation of SUDC,” Dr. Brownstein said. The approach is the first-line method of identifying conditions such as autism spectrum disorder, developmental disabilities, multiple congenital anomalies, and epilepsy, she noted.
In the study, published in Advanced Genetics, Dr. Brownstein and her colleagues used CMA to test genes from 116 deceased infants and toddlers up to age 28 months whose deaths were classified as SIDS or SUDC (the latter term applies to children older than 1 year).
The average age at the time of death was 5.7 months; 59% of the patients were boys. In 14 of the children (12%), the CMA test identified genetic variations in the form of deletions or duplications that were pathogenic (five cases) or uncertain but “favoring pathogenicity” (nine cases). Such deletions or duplications are known as copy number variants (CNVs).
CNVs are present in most people and are not necessarily associated with disease, according to the researchers. However, certain CNVs have been linked to ASD, attention-deficit/hyperactivity disorder, schizophrenia, Crohn’s disease, epilepsy, and various congenital abnormalities.
Dr. Brownstein’s group also compared pathogenicity in the SUDC group with that of a cohort of children with ASD and with healthy control persons. They found no significant difference in pathogenicity between SUDC and autism with regard to duplications. However, children in the SUDC group were significantly more likely to have higher pathogenicity scores for deletions, compared with control persons. Some of the CMVs did not appear connected to SIDS or SUDC; two cases in boys were undiagnosed cases of Klinefelter syndrome.
The study findings were limited by several factors, including the small sample size and the inability to conduct CMA analyses on parents or obtain family history, the researchers note. Other limitations were that phenotypic data were available only from autopsy material and medical records and that the study focused on younger children, the researchers add. They did not speculate about the causes of deaths in the other cases they examined.
In the current study, the other 88% of cases could involve nongenetic factors or genetic factors that aren’t measured by next-generation sequencing or chromosomal microarray, Dr. Brownstein said. “Undiagnosed disease programs looking for genetic causes for diseases in living patients identify a cause in about 1 in 4 cases,” she said. “While 12% is a modest percentage, the CNVs identified provide additional information. In the future, the goal would be to capture the full range of potential genetic changes.”
Previous research by Dr. Brownstein’s group at Robert’s Program, a clinical service for SUDC families at Boston Children’s Hospital, found genetic variants that might cause sudden death in children.
“We began this study with the simple question of whether, as a population, these children carry more copy number variation, which they do,” she said. “However, none of the CMA findings we identified are currently associated with SUDC, so much more investigation is necessary to find out if they are coincidental, risk factors, or causative.”
Looking ahead, she said, “Ideally, we would want every family affected by sudden unexplained death in pediatrics to have genetic testing, including a chromosomal microarray. Once we have more families enrolled and tested, we will be able to understand the risk factors for SIDS and SUDC much better.”
Benjamin Solomon, MD, clinical director at the National Human Genome Research Institute, Bethesda, Md., said the new research “may bring answers for individual situations as well as enable research to understand the overall biological underpinnings and causes of disease.”
The findings “help reinforce the heterogeneous nature of SUDC and related conditions,” Dr. Solomon said. “The results also highlight some of the challenges regarding how to interpret the possible clinical effects of genetic changes. That is, every person has genetic changes, and interpreting how certain genetic changes may or may not contribute to a disease or health care outcome can be challenging.”
Research is needed to understand not only the overall causes of SUDC but also how the different causes interact, Dr. Solomon said. “Eventually, better understanding of the causes could lead to knowledge that would enable interventions that could help prevent or reduce these devastating outcomes.”
The study was supported by the Robert’s Program on Sudden Unexplained Death in Pediatrics, the Jude Zayac Foundation, multiple grants from the Eunice Kennedy Shriver National Institutes of Health/National Institute of Child Health and Human Development, the Boston Children’s Hospital Intellectual and Developmental Disabilities Research Center Molecular Genetics Core Facility (supported by the NIH/NICHD), and by the NIH National Institute of Mental Health. The researchers and Dr. Solomon have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers have identified pathogenic gene variations in 12% of cases of sudden unexplained death in children.
The new study, which involved 116 cases of sudden infant death syndrome or sudden unexplained deaths in children (SUDC), suggests that available methods of chromosome testing could be used to help screen for the conditions, which together account for roughly 1,800 fatalities a year in the United States.
“Even though the Back to Sleep campaign has been incredibly effective and safe sleep practices have been promoted for years, sudden unexplained death in pediatrics remains a leading cause of death for infants and children,” said Catherine Brownstein, MPH, PhD, of Boston Children’s Hospital, lead author of the new study.
The findings suggest that chromosomal microarray analysis (CMA), the method that the researchers used in the study, “should be considered in the genetic evaluation of SUDC,” Dr. Brownstein said. The approach is the first-line method of identifying conditions such as autism spectrum disorder, developmental disabilities, multiple congenital anomalies, and epilepsy, she noted.
In the study, published in Advanced Genetics, Dr. Brownstein and her colleagues used CMA to test genes from 116 deceased infants and toddlers up to age 28 months whose deaths were classified as SIDS or SUDC (the latter term applies to children older than 1 year).
The average age at the time of death was 5.7 months; 59% of the patients were boys. In 14 of the children (12%), the CMA test identified genetic variations in the form of deletions or duplications that were pathogenic (five cases) or uncertain but “favoring pathogenicity” (nine cases). Such deletions or duplications are known as copy number variants (CNVs).
CNVs are present in most people and are not necessarily associated with disease, according to the researchers. However, certain CNVs have been linked to ASD, attention-deficit/hyperactivity disorder, schizophrenia, Crohn’s disease, epilepsy, and various congenital abnormalities.
Dr. Brownstein’s group also compared pathogenicity in the SUDC group with that of a cohort of children with ASD and with healthy control persons. They found no significant difference in pathogenicity between SUDC and autism with regard to duplications. However, children in the SUDC group were significantly more likely to have higher pathogenicity scores for deletions, compared with control persons. Some of the CMVs did not appear connected to SIDS or SUDC; two cases in boys were undiagnosed cases of Klinefelter syndrome.
The study findings were limited by several factors, including the small sample size and the inability to conduct CMA analyses on parents or obtain family history, the researchers note. Other limitations were that phenotypic data were available only from autopsy material and medical records and that the study focused on younger children, the researchers add. They did not speculate about the causes of deaths in the other cases they examined.
In the current study, the other 88% of cases could involve nongenetic factors or genetic factors that aren’t measured by next-generation sequencing or chromosomal microarray, Dr. Brownstein said. “Undiagnosed disease programs looking for genetic causes for diseases in living patients identify a cause in about 1 in 4 cases,” she said. “While 12% is a modest percentage, the CNVs identified provide additional information. In the future, the goal would be to capture the full range of potential genetic changes.”
Previous research by Dr. Brownstein’s group at Robert’s Program, a clinical service for SUDC families at Boston Children’s Hospital, found genetic variants that might cause sudden death in children.
“We began this study with the simple question of whether, as a population, these children carry more copy number variation, which they do,” she said. “However, none of the CMA findings we identified are currently associated with SUDC, so much more investigation is necessary to find out if they are coincidental, risk factors, or causative.”
Looking ahead, she said, “Ideally, we would want every family affected by sudden unexplained death in pediatrics to have genetic testing, including a chromosomal microarray. Once we have more families enrolled and tested, we will be able to understand the risk factors for SIDS and SUDC much better.”
Benjamin Solomon, MD, clinical director at the National Human Genome Research Institute, Bethesda, Md., said the new research “may bring answers for individual situations as well as enable research to understand the overall biological underpinnings and causes of disease.”
The findings “help reinforce the heterogeneous nature of SUDC and related conditions,” Dr. Solomon said. “The results also highlight some of the challenges regarding how to interpret the possible clinical effects of genetic changes. That is, every person has genetic changes, and interpreting how certain genetic changes may or may not contribute to a disease or health care outcome can be challenging.”
Research is needed to understand not only the overall causes of SUDC but also how the different causes interact, Dr. Solomon said. “Eventually, better understanding of the causes could lead to knowledge that would enable interventions that could help prevent or reduce these devastating outcomes.”
The study was supported by the Robert’s Program on Sudden Unexplained Death in Pediatrics, the Jude Zayac Foundation, multiple grants from the Eunice Kennedy Shriver National Institutes of Health/National Institute of Child Health and Human Development, the Boston Children’s Hospital Intellectual and Developmental Disabilities Research Center Molecular Genetics Core Facility (supported by the NIH/NICHD), and by the NIH National Institute of Mental Health. The researchers and Dr. Solomon have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers have identified pathogenic gene variations in 12% of cases of sudden unexplained death in children.
The new study, which involved 116 cases of sudden infant death syndrome or sudden unexplained deaths in children (SUDC), suggests that available methods of chromosome testing could be used to help screen for the conditions, which together account for roughly 1,800 fatalities a year in the United States.
“Even though the Back to Sleep campaign has been incredibly effective and safe sleep practices have been promoted for years, sudden unexplained death in pediatrics remains a leading cause of death for infants and children,” said Catherine Brownstein, MPH, PhD, of Boston Children’s Hospital, lead author of the new study.
The findings suggest that chromosomal microarray analysis (CMA), the method that the researchers used in the study, “should be considered in the genetic evaluation of SUDC,” Dr. Brownstein said. The approach is the first-line method of identifying conditions such as autism spectrum disorder, developmental disabilities, multiple congenital anomalies, and epilepsy, she noted.
In the study, published in Advanced Genetics, Dr. Brownstein and her colleagues used CMA to test genes from 116 deceased infants and toddlers up to age 28 months whose deaths were classified as SIDS or SUDC (the latter term applies to children older than 1 year).
The average age at the time of death was 5.7 months; 59% of the patients were boys. In 14 of the children (12%), the CMA test identified genetic variations in the form of deletions or duplications that were pathogenic (five cases) or uncertain but “favoring pathogenicity” (nine cases). Such deletions or duplications are known as copy number variants (CNVs).
CNVs are present in most people and are not necessarily associated with disease, according to the researchers. However, certain CNVs have been linked to ASD, attention-deficit/hyperactivity disorder, schizophrenia, Crohn’s disease, epilepsy, and various congenital abnormalities.
Dr. Brownstein’s group also compared pathogenicity in the SUDC group with that of a cohort of children with ASD and with healthy control persons. They found no significant difference in pathogenicity between SUDC and autism with regard to duplications. However, children in the SUDC group were significantly more likely to have higher pathogenicity scores for deletions, compared with control persons. Some of the CMVs did not appear connected to SIDS or SUDC; two cases in boys were undiagnosed cases of Klinefelter syndrome.
The study findings were limited by several factors, including the small sample size and the inability to conduct CMA analyses on parents or obtain family history, the researchers note. Other limitations were that phenotypic data were available only from autopsy material and medical records and that the study focused on younger children, the researchers add. They did not speculate about the causes of deaths in the other cases they examined.
In the current study, the other 88% of cases could involve nongenetic factors or genetic factors that aren’t measured by next-generation sequencing or chromosomal microarray, Dr. Brownstein said. “Undiagnosed disease programs looking for genetic causes for diseases in living patients identify a cause in about 1 in 4 cases,” she said. “While 12% is a modest percentage, the CNVs identified provide additional information. In the future, the goal would be to capture the full range of potential genetic changes.”
Previous research by Dr. Brownstein’s group at Robert’s Program, a clinical service for SUDC families at Boston Children’s Hospital, found genetic variants that might cause sudden death in children.
“We began this study with the simple question of whether, as a population, these children carry more copy number variation, which they do,” she said. “However, none of the CMA findings we identified are currently associated with SUDC, so much more investigation is necessary to find out if they are coincidental, risk factors, or causative.”
Looking ahead, she said, “Ideally, we would want every family affected by sudden unexplained death in pediatrics to have genetic testing, including a chromosomal microarray. Once we have more families enrolled and tested, we will be able to understand the risk factors for SIDS and SUDC much better.”
Benjamin Solomon, MD, clinical director at the National Human Genome Research Institute, Bethesda, Md., said the new research “may bring answers for individual situations as well as enable research to understand the overall biological underpinnings and causes of disease.”
The findings “help reinforce the heterogeneous nature of SUDC and related conditions,” Dr. Solomon said. “The results also highlight some of the challenges regarding how to interpret the possible clinical effects of genetic changes. That is, every person has genetic changes, and interpreting how certain genetic changes may or may not contribute to a disease or health care outcome can be challenging.”
Research is needed to understand not only the overall causes of SUDC but also how the different causes interact, Dr. Solomon said. “Eventually, better understanding of the causes could lead to knowledge that would enable interventions that could help prevent or reduce these devastating outcomes.”
The study was supported by the Robert’s Program on Sudden Unexplained Death in Pediatrics, the Jude Zayac Foundation, multiple grants from the Eunice Kennedy Shriver National Institutes of Health/National Institute of Child Health and Human Development, the Boston Children’s Hospital Intellectual and Developmental Disabilities Research Center Molecular Genetics Core Facility (supported by the NIH/NICHD), and by the NIH National Institute of Mental Health. The researchers and Dr. Solomon have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ADVANCED GENETICS



