User login
Follistatin, endoglin predict postallogeneic HCT NRM
ORLANDO – A composite score based on day 28 plasma levels of the angiogenic factors follistatin and endoglin predicts 1-year nonrelapse mortality in patients who have undergone myeloablative allogeneic hematopoietic cell transplantation, based on findings from the randomized Blood and Marrow Transplant Clinical Trials Network acute graft-versus-host prophylaxis study 0402 (BMT CTN 0402).
Elevations in these factors at day 28 may reflect susceptibility to regimen-related and other toxicities that adversely affect tissue repair and survival, Shernan Holtan, MD, said at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
“Without important trophic angiogenic factors, the body may not be able to heal well after injury such as graft-versus-host disease [GVHD]. We previously reported that such angiogenic factors are indeed altered at the onset of acute graft-versus-host disease based upon samples from BMT CTN 0302 and 0802,” said Dr. Holtan of the University of Minnesota, Minneapolis. “Specifically, we found that repair factors of epidermal growth factor and VEGF-A are low at the onset of acute GVHD, and that damage-associated angiogenic factors are high at the onset of acute graft-versus-host disease.”
These damage-associated factors include follistatin, endoglin, placental growth factor, and angiopoietin-2, she added.
Based on the previous results, Dr. Holtan and her colleagues hypothesized that a pattern of tissue damage as illustrated by these markers at 28 days after treatment would be associated with 1-year nonrelapse mortality.
Of 221 patients from BMT CTN 0402 with pretreatment and day 28 plasma samples available for analysis, 25 had died at 1 year of causes unrelated to relapse. In a univariate analysis, nonrelapse mortality was associated with levels of follistatin, endoglin, and angiopoietin-2. When combined to assess for an overall pattern of damage, only follistatin and endoglin were significantly associated with nonrelapse mortality.
The relative risk of death unrelated to relapse was 4.5-fold higher in patients with the highest score (score of 3) on multivariate regression analysis of follistatin and endoglin levels. Grade II-IV acute GVHD was not significantly associated with 1-year nonrelapse mortality in multivariate analyses, but age over 50 years was.
“Notably, the composite score was a better predictor than any factor alone,” Dr. Holtan said.
The composite score was also predictive of the development of acute GVHD.
“We found that a moderate score of 2 was associated with a 2.3-fold increased risk of acute GVHD prior to day 100. Interestingly, the higher score [3] was not associated with acute GVHD. There was no association of the composite score with chronic GVHD,” she said.
The risk of nonrelapse mortality was less than 10% in patients with a composite score of 1.
Among patients in the study with a score of 3, more than half of the deaths were related to organ toxicity, including liver failure and respiratory failure, which were predominantly infection-related. Those with a low composite score had very few deaths associated with organ toxicity, she noted.
While there are many unanswered questions, these findings highlight possible opportunities to improve survival after allogeneic hematopoietic cell transplantation that warrant further study, she said.
“We need to learn how to constrain this angiogenic inflammatory response with the ultimate goal of hopefully identifying novel treatment strategies to mitigate nonrelapse mortality in our patients,” she concluded.
Dr. Holtan is an investigator for Alexion and is site principal investigator on the GI GVHD clinical trial.
ORLANDO – A composite score based on day 28 plasma levels of the angiogenic factors follistatin and endoglin predicts 1-year nonrelapse mortality in patients who have undergone myeloablative allogeneic hematopoietic cell transplantation, based on findings from the randomized Blood and Marrow Transplant Clinical Trials Network acute graft-versus-host prophylaxis study 0402 (BMT CTN 0402).
Elevations in these factors at day 28 may reflect susceptibility to regimen-related and other toxicities that adversely affect tissue repair and survival, Shernan Holtan, MD, said at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
“Without important trophic angiogenic factors, the body may not be able to heal well after injury such as graft-versus-host disease [GVHD]. We previously reported that such angiogenic factors are indeed altered at the onset of acute graft-versus-host disease based upon samples from BMT CTN 0302 and 0802,” said Dr. Holtan of the University of Minnesota, Minneapolis. “Specifically, we found that repair factors of epidermal growth factor and VEGF-A are low at the onset of acute GVHD, and that damage-associated angiogenic factors are high at the onset of acute graft-versus-host disease.”
These damage-associated factors include follistatin, endoglin, placental growth factor, and angiopoietin-2, she added.
Based on the previous results, Dr. Holtan and her colleagues hypothesized that a pattern of tissue damage as illustrated by these markers at 28 days after treatment would be associated with 1-year nonrelapse mortality.
Of 221 patients from BMT CTN 0402 with pretreatment and day 28 plasma samples available for analysis, 25 had died at 1 year of causes unrelated to relapse. In a univariate analysis, nonrelapse mortality was associated with levels of follistatin, endoglin, and angiopoietin-2. When combined to assess for an overall pattern of damage, only follistatin and endoglin were significantly associated with nonrelapse mortality.
The relative risk of death unrelated to relapse was 4.5-fold higher in patients with the highest score (score of 3) on multivariate regression analysis of follistatin and endoglin levels. Grade II-IV acute GVHD was not significantly associated with 1-year nonrelapse mortality in multivariate analyses, but age over 50 years was.
“Notably, the composite score was a better predictor than any factor alone,” Dr. Holtan said.
The composite score was also predictive of the development of acute GVHD.
“We found that a moderate score of 2 was associated with a 2.3-fold increased risk of acute GVHD prior to day 100. Interestingly, the higher score [3] was not associated with acute GVHD. There was no association of the composite score with chronic GVHD,” she said.
The risk of nonrelapse mortality was less than 10% in patients with a composite score of 1.
Among patients in the study with a score of 3, more than half of the deaths were related to organ toxicity, including liver failure and respiratory failure, which were predominantly infection-related. Those with a low composite score had very few deaths associated with organ toxicity, she noted.
While there are many unanswered questions, these findings highlight possible opportunities to improve survival after allogeneic hematopoietic cell transplantation that warrant further study, she said.
“We need to learn how to constrain this angiogenic inflammatory response with the ultimate goal of hopefully identifying novel treatment strategies to mitigate nonrelapse mortality in our patients,” she concluded.
Dr. Holtan is an investigator for Alexion and is site principal investigator on the GI GVHD clinical trial.
ORLANDO – A composite score based on day 28 plasma levels of the angiogenic factors follistatin and endoglin predicts 1-year nonrelapse mortality in patients who have undergone myeloablative allogeneic hematopoietic cell transplantation, based on findings from the randomized Blood and Marrow Transplant Clinical Trials Network acute graft-versus-host prophylaxis study 0402 (BMT CTN 0402).
Elevations in these factors at day 28 may reflect susceptibility to regimen-related and other toxicities that adversely affect tissue repair and survival, Shernan Holtan, MD, said at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
“Without important trophic angiogenic factors, the body may not be able to heal well after injury such as graft-versus-host disease [GVHD]. We previously reported that such angiogenic factors are indeed altered at the onset of acute graft-versus-host disease based upon samples from BMT CTN 0302 and 0802,” said Dr. Holtan of the University of Minnesota, Minneapolis. “Specifically, we found that repair factors of epidermal growth factor and VEGF-A are low at the onset of acute GVHD, and that damage-associated angiogenic factors are high at the onset of acute graft-versus-host disease.”
These damage-associated factors include follistatin, endoglin, placental growth factor, and angiopoietin-2, she added.
Based on the previous results, Dr. Holtan and her colleagues hypothesized that a pattern of tissue damage as illustrated by these markers at 28 days after treatment would be associated with 1-year nonrelapse mortality.
Of 221 patients from BMT CTN 0402 with pretreatment and day 28 plasma samples available for analysis, 25 had died at 1 year of causes unrelated to relapse. In a univariate analysis, nonrelapse mortality was associated with levels of follistatin, endoglin, and angiopoietin-2. When combined to assess for an overall pattern of damage, only follistatin and endoglin were significantly associated with nonrelapse mortality.
The relative risk of death unrelated to relapse was 4.5-fold higher in patients with the highest score (score of 3) on multivariate regression analysis of follistatin and endoglin levels. Grade II-IV acute GVHD was not significantly associated with 1-year nonrelapse mortality in multivariate analyses, but age over 50 years was.
“Notably, the composite score was a better predictor than any factor alone,” Dr. Holtan said.
The composite score was also predictive of the development of acute GVHD.
“We found that a moderate score of 2 was associated with a 2.3-fold increased risk of acute GVHD prior to day 100. Interestingly, the higher score [3] was not associated with acute GVHD. There was no association of the composite score with chronic GVHD,” she said.
The risk of nonrelapse mortality was less than 10% in patients with a composite score of 1.
Among patients in the study with a score of 3, more than half of the deaths were related to organ toxicity, including liver failure and respiratory failure, which were predominantly infection-related. Those with a low composite score had very few deaths associated with organ toxicity, she noted.
While there are many unanswered questions, these findings highlight possible opportunities to improve survival after allogeneic hematopoietic cell transplantation that warrant further study, she said.
“We need to learn how to constrain this angiogenic inflammatory response with the ultimate goal of hopefully identifying novel treatment strategies to mitigate nonrelapse mortality in our patients,” she concluded.
Dr. Holtan is an investigator for Alexion and is site principal investigator on the GI GVHD clinical trial.
AT THE 2017 BMT TANDEM MEETINGS
Key clinical point:
Major finding: Patients with a composite score of 3 had a 4.5-fold higher relative risk of nonrelapse mortality.
Data source: The randomized BMT CTN 0402 study of 221 patients.
Disclosures: Dr. Holtan is an investigator for Alexion and is site principal investigator on the GI GVHD clinical trial.
Older AML patients benefit from frailty assessment and interventions
ORLANDO – Performing a comprehensive geriatric assessment of patients with acute myeloid leukemia (AML) does more than provide fine-tuned risk stratification; spotting areas of vulnerability and frailty can also identify targets for prehabilitation, support, and remediation as older patients face transplant.
A program at the University of Chicago termed the Transplant Optimization Program, or TOP, uses the geriatric assessment as the foundation of an interdisciplinary, customized intervention for older adults facing hematopoietic cell transplant (HCT). The team includes the transplant physician and a geriatric oncologist; however, social work, dietetics, psychology, and physical therapy professionals also are brought on board.
“High comorbidities and functional limitations influence overall survival,” Dr. Artz said. “Non-relapse mortality remains a major barrier; of course, the attendant morbidity before it is perhaps a bigger concern, and our patients’ concern.”
Dr. Artz said that he and his colleagues at the University of Chicago, where he is a professor of medicine, had adapted the geriatric assessment developed by the Cancer and Aging Group, and now administer it to all prospective transplant patients aged 50 years and older. Dr. Artz said that, at his center, they have found that 25% of patients aged 50 and older were frail according to the Fried Frailty Index. “That’s what we expect for people in the community who are aged 80 and older, so we’re painting a picture of accelerated aging for patients before they undergo allograft,” he said.
Results of the assessment are then reviewed by a multidisciplinary team, and an individualized prehabilitation and support program is developed based on those results. “Using chronologic and physiologic age in transplant can help us better risk stratify, and think about strategies to mitigate some of those risks,” Dr. Artz said.
The staging tool currently used at the University of Chicago examines seven domains and uses objective tools to deliver information in each domain. Comorbidities are assessed by the Hematopoietic Cell Transplant–Specific Comorbidity Index (HCT-CI) and the Older Americans Resources and Services (OARS) scale. “We are trying to use standardized tools such as the geriatric assessment, because our ‘eyeball test’ is quite poor,” he said.
Physical function is assessed by measuring four-meter walk speed and grip strength; by asking about falls and capacity for instrumental activities of daily living; and by administering the Karnofsky Performance Scale–MD. Patients are given the Mental Health Inventory–17 to assess psychological health.
Neurocognitive testing and the Blessed Orientation-Memory-Concentration test are used to assess cognitive function. The Medical Outcomes Study Social Activity and Social Limitations scales give an idea about social support.
Biomarkers that are tracked include C-reactive protein and ferritin, among others, Dr. Artz said. Nutritional status is assessed by measuring serum albumin as well as any weight loss.
Once the full geriatric assessment data about a patient are gathered, a plan is formulated for impairments in any given domain. For example, if significant comorbid conditions exist, the TOP team seeks subspecialty consultation for management advice in the context of transplant. “This is a consultation – not a clearance!” Dr. Artz said.
Physical and functional impairments are addressed with prehabilitation if time permits, and the home assessment is aligned with patient expectations. Sometimes, the inactivity associated with peritransplant period can worsen conditions such as osteoarthritis, so a patient who’s been functional may find themselves very stiff when going home. Caregivers can encourage early activity to help minimize this effect, Dr. Artz said.
For patients at nutritional risk, it’s vital to have a good nutrition plan for transplant and to make sure medications or social factors aren’t standing in the way of adequate nutrition, Dr. Artz said. “Don’t forget to ask about dentures,” he said, since mucositis can make dentures unbearable in the immediate posttransplant period.
It’s important to be careful when unpacking findings of cognitive impairment, Dr. Artz said, since untreated depression and anxiety can manifest as forgetfulness and perseveration. Eliminating unnecessary medication, having a good delirium protocol in place, and keeping a family member in the room with the patient can help minimize a cognitive downturn during transplant.
As patients age, it can be more common for them to have limited social support. The TOP team calls a family meeting to assess resources and appoint a “team captain” among the patient’s social circle. “We work to enlarge that circle,” by pulling in as many family members and friends as possible, Dr. Artz said. In a discussion after the talk, he said that he feels that having a family member in the hospital with the older transplant patient is important for many reasons. Not only is the patient less likely to fall, he or she may also eat better and feel better. In addition, he said he has a sense that when the caregiver has seen the patient at his or her nadir, taking that patient home isn’t as scary, since it’s easier to see that the trajectory is headed upward by the time of discharge.
Dr. Artz said that other facilities are now beginning to send patients for TOP evaluations; “the aging evaluation informs physiologic age, candidacy for transplant, and may permit optimizing outcomes,” he said. “We’re trying to ... optimize patients both before and after transplant. It’s one thing to say you’re vulnerable, but how do you take that vulnerable patient and improve their outcomes? That’s the question.” Though the proportion of older individuals receiving allogeneic transplants is growing rapidly, research is not keeping up, Dr. Artz said, calling for more prospective studies in older adults.
Dr. Artz reported that he has received research funding from Miltenyi Biotech.
[email protected]
On Twitter @karioakes
ORLANDO – Performing a comprehensive geriatric assessment of patients with acute myeloid leukemia (AML) does more than provide fine-tuned risk stratification; spotting areas of vulnerability and frailty can also identify targets for prehabilitation, support, and remediation as older patients face transplant.
A program at the University of Chicago termed the Transplant Optimization Program, or TOP, uses the geriatric assessment as the foundation of an interdisciplinary, customized intervention for older adults facing hematopoietic cell transplant (HCT). The team includes the transplant physician and a geriatric oncologist; however, social work, dietetics, psychology, and physical therapy professionals also are brought on board.
“High comorbidities and functional limitations influence overall survival,” Dr. Artz said. “Non-relapse mortality remains a major barrier; of course, the attendant morbidity before it is perhaps a bigger concern, and our patients’ concern.”
Dr. Artz said that he and his colleagues at the University of Chicago, where he is a professor of medicine, had adapted the geriatric assessment developed by the Cancer and Aging Group, and now administer it to all prospective transplant patients aged 50 years and older. Dr. Artz said that, at his center, they have found that 25% of patients aged 50 and older were frail according to the Fried Frailty Index. “That’s what we expect for people in the community who are aged 80 and older, so we’re painting a picture of accelerated aging for patients before they undergo allograft,” he said.
Results of the assessment are then reviewed by a multidisciplinary team, and an individualized prehabilitation and support program is developed based on those results. “Using chronologic and physiologic age in transplant can help us better risk stratify, and think about strategies to mitigate some of those risks,” Dr. Artz said.
The staging tool currently used at the University of Chicago examines seven domains and uses objective tools to deliver information in each domain. Comorbidities are assessed by the Hematopoietic Cell Transplant–Specific Comorbidity Index (HCT-CI) and the Older Americans Resources and Services (OARS) scale. “We are trying to use standardized tools such as the geriatric assessment, because our ‘eyeball test’ is quite poor,” he said.
Physical function is assessed by measuring four-meter walk speed and grip strength; by asking about falls and capacity for instrumental activities of daily living; and by administering the Karnofsky Performance Scale–MD. Patients are given the Mental Health Inventory–17 to assess psychological health.
Neurocognitive testing and the Blessed Orientation-Memory-Concentration test are used to assess cognitive function. The Medical Outcomes Study Social Activity and Social Limitations scales give an idea about social support.
Biomarkers that are tracked include C-reactive protein and ferritin, among others, Dr. Artz said. Nutritional status is assessed by measuring serum albumin as well as any weight loss.
Once the full geriatric assessment data about a patient are gathered, a plan is formulated for impairments in any given domain. For example, if significant comorbid conditions exist, the TOP team seeks subspecialty consultation for management advice in the context of transplant. “This is a consultation – not a clearance!” Dr. Artz said.
Physical and functional impairments are addressed with prehabilitation if time permits, and the home assessment is aligned with patient expectations. Sometimes, the inactivity associated with peritransplant period can worsen conditions such as osteoarthritis, so a patient who’s been functional may find themselves very stiff when going home. Caregivers can encourage early activity to help minimize this effect, Dr. Artz said.
For patients at nutritional risk, it’s vital to have a good nutrition plan for transplant and to make sure medications or social factors aren’t standing in the way of adequate nutrition, Dr. Artz said. “Don’t forget to ask about dentures,” he said, since mucositis can make dentures unbearable in the immediate posttransplant period.
It’s important to be careful when unpacking findings of cognitive impairment, Dr. Artz said, since untreated depression and anxiety can manifest as forgetfulness and perseveration. Eliminating unnecessary medication, having a good delirium protocol in place, and keeping a family member in the room with the patient can help minimize a cognitive downturn during transplant.
As patients age, it can be more common for them to have limited social support. The TOP team calls a family meeting to assess resources and appoint a “team captain” among the patient’s social circle. “We work to enlarge that circle,” by pulling in as many family members and friends as possible, Dr. Artz said. In a discussion after the talk, he said that he feels that having a family member in the hospital with the older transplant patient is important for many reasons. Not only is the patient less likely to fall, he or she may also eat better and feel better. In addition, he said he has a sense that when the caregiver has seen the patient at his or her nadir, taking that patient home isn’t as scary, since it’s easier to see that the trajectory is headed upward by the time of discharge.
Dr. Artz said that other facilities are now beginning to send patients for TOP evaluations; “the aging evaluation informs physiologic age, candidacy for transplant, and may permit optimizing outcomes,” he said. “We’re trying to ... optimize patients both before and after transplant. It’s one thing to say you’re vulnerable, but how do you take that vulnerable patient and improve their outcomes? That’s the question.” Though the proportion of older individuals receiving allogeneic transplants is growing rapidly, research is not keeping up, Dr. Artz said, calling for more prospective studies in older adults.
Dr. Artz reported that he has received research funding from Miltenyi Biotech.
[email protected]
On Twitter @karioakes
ORLANDO – Performing a comprehensive geriatric assessment of patients with acute myeloid leukemia (AML) does more than provide fine-tuned risk stratification; spotting areas of vulnerability and frailty can also identify targets for prehabilitation, support, and remediation as older patients face transplant.
A program at the University of Chicago termed the Transplant Optimization Program, or TOP, uses the geriatric assessment as the foundation of an interdisciplinary, customized intervention for older adults facing hematopoietic cell transplant (HCT). The team includes the transplant physician and a geriatric oncologist; however, social work, dietetics, psychology, and physical therapy professionals also are brought on board.
“High comorbidities and functional limitations influence overall survival,” Dr. Artz said. “Non-relapse mortality remains a major barrier; of course, the attendant morbidity before it is perhaps a bigger concern, and our patients’ concern.”
Dr. Artz said that he and his colleagues at the University of Chicago, where he is a professor of medicine, had adapted the geriatric assessment developed by the Cancer and Aging Group, and now administer it to all prospective transplant patients aged 50 years and older. Dr. Artz said that, at his center, they have found that 25% of patients aged 50 and older were frail according to the Fried Frailty Index. “That’s what we expect for people in the community who are aged 80 and older, so we’re painting a picture of accelerated aging for patients before they undergo allograft,” he said.
Results of the assessment are then reviewed by a multidisciplinary team, and an individualized prehabilitation and support program is developed based on those results. “Using chronologic and physiologic age in transplant can help us better risk stratify, and think about strategies to mitigate some of those risks,” Dr. Artz said.
The staging tool currently used at the University of Chicago examines seven domains and uses objective tools to deliver information in each domain. Comorbidities are assessed by the Hematopoietic Cell Transplant–Specific Comorbidity Index (HCT-CI) and the Older Americans Resources and Services (OARS) scale. “We are trying to use standardized tools such as the geriatric assessment, because our ‘eyeball test’ is quite poor,” he said.
Physical function is assessed by measuring four-meter walk speed and grip strength; by asking about falls and capacity for instrumental activities of daily living; and by administering the Karnofsky Performance Scale–MD. Patients are given the Mental Health Inventory–17 to assess psychological health.
Neurocognitive testing and the Blessed Orientation-Memory-Concentration test are used to assess cognitive function. The Medical Outcomes Study Social Activity and Social Limitations scales give an idea about social support.
Biomarkers that are tracked include C-reactive protein and ferritin, among others, Dr. Artz said. Nutritional status is assessed by measuring serum albumin as well as any weight loss.
Once the full geriatric assessment data about a patient are gathered, a plan is formulated for impairments in any given domain. For example, if significant comorbid conditions exist, the TOP team seeks subspecialty consultation for management advice in the context of transplant. “This is a consultation – not a clearance!” Dr. Artz said.
Physical and functional impairments are addressed with prehabilitation if time permits, and the home assessment is aligned with patient expectations. Sometimes, the inactivity associated with peritransplant period can worsen conditions such as osteoarthritis, so a patient who’s been functional may find themselves very stiff when going home. Caregivers can encourage early activity to help minimize this effect, Dr. Artz said.
For patients at nutritional risk, it’s vital to have a good nutrition plan for transplant and to make sure medications or social factors aren’t standing in the way of adequate nutrition, Dr. Artz said. “Don’t forget to ask about dentures,” he said, since mucositis can make dentures unbearable in the immediate posttransplant period.
It’s important to be careful when unpacking findings of cognitive impairment, Dr. Artz said, since untreated depression and anxiety can manifest as forgetfulness and perseveration. Eliminating unnecessary medication, having a good delirium protocol in place, and keeping a family member in the room with the patient can help minimize a cognitive downturn during transplant.
As patients age, it can be more common for them to have limited social support. The TOP team calls a family meeting to assess resources and appoint a “team captain” among the patient’s social circle. “We work to enlarge that circle,” by pulling in as many family members and friends as possible, Dr. Artz said. In a discussion after the talk, he said that he feels that having a family member in the hospital with the older transplant patient is important for many reasons. Not only is the patient less likely to fall, he or she may also eat better and feel better. In addition, he said he has a sense that when the caregiver has seen the patient at his or her nadir, taking that patient home isn’t as scary, since it’s easier to see that the trajectory is headed upward by the time of discharge.
Dr. Artz said that other facilities are now beginning to send patients for TOP evaluations; “the aging evaluation informs physiologic age, candidacy for transplant, and may permit optimizing outcomes,” he said. “We’re trying to ... optimize patients both before and after transplant. It’s one thing to say you’re vulnerable, but how do you take that vulnerable patient and improve their outcomes? That’s the question.” Though the proportion of older individuals receiving allogeneic transplants is growing rapidly, research is not keeping up, Dr. Artz said, calling for more prospective studies in older adults.
Dr. Artz reported that he has received research funding from Miltenyi Biotech.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM THE 2017 BMT TANDEM MEETINGS
Fewer post-transplant CMV infections with novel antiviral prophylaxis
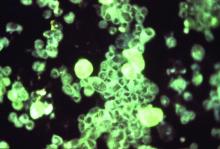
ORLANDO – A first-in-class antiviral drug was safe and effective when used to prevent clinically significant cytomegalovirus infections in adults undergoing hematopoietic cell transplantation.
At 24 weeks post-transplant, 38% (122/325) of those receiving the novel antiviral letermovir were considered treatment failures, compared with 61% (103/170) of those receiving placebo (P less than .0001). All-cause mortality was 10% (n=32/325) for patients receiving letermovir and 16%, (n=27/170) for the placebo group (log rank two-sided P = 0.0317).
The study findings show that “we [can] prevent patients from getting CMV infections from the beginning of the transplant and that [result can] confer a mortality benefit,” lead author Francisco Marty, MD, said in an interview.
Dr. Marty said that letermovir has received fast-track status both from the Food and Drug Administration and from the European Medicines Agency.
HCT recipients who are CMV-positive but who do not have clinically significant disease are not preemptively treated in current practice. “Previously, there wasn’t a primary prevention strategy in bone marrow transplantation. When myelosuppressive drugs were tried such as ganciclovir, any benefit was offset by increased myelosuppression, with resulting increases in bacterial and fungal infections,” said Dr. Marty, professor of medicine at Harvard Medical School, Boston.
Letermovir was generally well-tolerated in the clinical trial; myelotoxicity and nephrotoxicity levels were comparable in patients receiving letermovir and placebo. Letermovir targets the terminase complex, which is a viral replication process specific to CMV and not otherwise present in humans. That fact may explain, in part, letermovir’s limited toxicity, Dr. Marty said. The primary outcome measure of the phase III randomized, double-blind, placebo-controlled trial was the stratum-adjusted proportion of patients who had clinically significant CMV at post-transplant week 24, examining only the patients in the trials who had no detectable CMV DNA at the time of randomization. If patients did not complete the study, or had missing data at week 24, they were considered to have failed the trial.
Overall, 31% of patients were considered at high risk for CMV disease. Half of the patients received myeloablative conditioning, and about a third (35%) received antithymocyte globulin. Donor sources, whose characteristics were balanced between study arms, included 14% mismatched unrelated donors, 13% haploidentical donors, and 4% cord blood.
The multinational study’s 24-week results were presented at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
“This was an international study, conducted at multiple sites in multiple countries. We used two-to-one randomization, and stratified participants by their risk of CMV disease and by study sites. We wanted to make sure the groups were balanced by disease risk and by study sites, to account for regional variations in bone marrow transplant procedures and CMV treatment patterns,” said Dr. Marty.
For the study, clinically significant CMV infection was defined as either CMV disease, such as pneumonia, colitis, or hepatitis, or CMV viremia that would trigger preemptive treatment.
Letermovir, which can be administered orally or intravenously, was dosed at 480 mg per day. Because of the risk for a drug-drug interaction, patients on cyclosporine received 240 mg of letermovir per day. Having intravenous dosing as an option helped patients who were not tolerating oral intake to stay on the study drug during the post-transplant period, he said.
The study drug was begun a median of 9 days post-transplant. Some patients received letermovir or placebo as early as the day of transplant; all patients began the study drug by 28 days post-transplant. The study drug was continued through week 14, or until at least 100 days post-transplant. Overall, 37% of patients had engrafted at the time they began the study drug.
Patients had weekly serum CMV assays performed until week 14, with biweekly sampling done through week 24. If patients developed clinically significant CMV, or if their serum samples yielded CMV DNA warranting preemptive treatment, they discontinued the study drug and began treatment for CMV.
The safety analysis, which was carried through week 48, tracked adverse events from the first dose of study drug until 14 days after discontinuation. Adverse events that were more common with letermovir than placebo included vomiting (19% versus 14%), edema (15% versus 9%), atrial arrhythmias (10% versus 5%), and having alanine aspartate levels more than five times the upper limit of normal (4% versus 2%). Graft versus host disease occurred in 39% of patients in each group; diarrhea and nausea occurred in approximately one fourth of patients in each group.
In response to a question after the presentation, Dr. Marty said, “The higher the risk of CMV disease, the higher the benefit in terms of survival.” Answering another question, about who should receive letermovir. Dr. Marty replied, “Like acyclovir, we should give it during times of risk. And CMV risk is different for different populations. It’s a matter of managing risks and benefits.”
Though letermovir was safe and well-tolerated in this trial, it’s different from acyclovir in that “it’s not a one dollar a day drug,” Dr. Marty acknowledged.
Merck, which plans to market letermovir, was the sponsor of the study and plans to submit applications for approval in both the United States and in the European Union in 2017. Dr. Marty reported receiving research grants from Merck as well as Astellas, Chimerix, and Shire. Additionally, he has received honoraria from Alexion, Chimerix, LFB, Merck, Roche Molecular Diagnostics, and Shire.
This article was updated 2/27/17.
[email protected]
On Twitter @karioakes
ORLANDO – A first-in-class antiviral drug was safe and effective when used to prevent clinically significant cytomegalovirus infections in adults undergoing hematopoietic cell transplantation.
At 24 weeks post-transplant, 38% (122/325) of those receiving the novel antiviral letermovir were considered treatment failures, compared with 61% (103/170) of those receiving placebo (P less than .0001). All-cause mortality was 10% (n=32/325) for patients receiving letermovir and 16%, (n=27/170) for the placebo group (log rank two-sided P = 0.0317).
The study findings show that “we [can] prevent patients from getting CMV infections from the beginning of the transplant and that [result can] confer a mortality benefit,” lead author Francisco Marty, MD, said in an interview.
Dr. Marty said that letermovir has received fast-track status both from the Food and Drug Administration and from the European Medicines Agency.
HCT recipients who are CMV-positive but who do not have clinically significant disease are not preemptively treated in current practice. “Previously, there wasn’t a primary prevention strategy in bone marrow transplantation. When myelosuppressive drugs were tried such as ganciclovir, any benefit was offset by increased myelosuppression, with resulting increases in bacterial and fungal infections,” said Dr. Marty, professor of medicine at Harvard Medical School, Boston.
Letermovir was generally well-tolerated in the clinical trial; myelotoxicity and nephrotoxicity levels were comparable in patients receiving letermovir and placebo. Letermovir targets the terminase complex, which is a viral replication process specific to CMV and not otherwise present in humans. That fact may explain, in part, letermovir’s limited toxicity, Dr. Marty said. The primary outcome measure of the phase III randomized, double-blind, placebo-controlled trial was the stratum-adjusted proportion of patients who had clinically significant CMV at post-transplant week 24, examining only the patients in the trials who had no detectable CMV DNA at the time of randomization. If patients did not complete the study, or had missing data at week 24, they were considered to have failed the trial.
Overall, 31% of patients were considered at high risk for CMV disease. Half of the patients received myeloablative conditioning, and about a third (35%) received antithymocyte globulin. Donor sources, whose characteristics were balanced between study arms, included 14% mismatched unrelated donors, 13% haploidentical donors, and 4% cord blood.
The multinational study’s 24-week results were presented at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
“This was an international study, conducted at multiple sites in multiple countries. We used two-to-one randomization, and stratified participants by their risk of CMV disease and by study sites. We wanted to make sure the groups were balanced by disease risk and by study sites, to account for regional variations in bone marrow transplant procedures and CMV treatment patterns,” said Dr. Marty.
For the study, clinically significant CMV infection was defined as either CMV disease, such as pneumonia, colitis, or hepatitis, or CMV viremia that would trigger preemptive treatment.
Letermovir, which can be administered orally or intravenously, was dosed at 480 mg per day. Because of the risk for a drug-drug interaction, patients on cyclosporine received 240 mg of letermovir per day. Having intravenous dosing as an option helped patients who were not tolerating oral intake to stay on the study drug during the post-transplant period, he said.
The study drug was begun a median of 9 days post-transplant. Some patients received letermovir or placebo as early as the day of transplant; all patients began the study drug by 28 days post-transplant. The study drug was continued through week 14, or until at least 100 days post-transplant. Overall, 37% of patients had engrafted at the time they began the study drug.
Patients had weekly serum CMV assays performed until week 14, with biweekly sampling done through week 24. If patients developed clinically significant CMV, or if their serum samples yielded CMV DNA warranting preemptive treatment, they discontinued the study drug and began treatment for CMV.
The safety analysis, which was carried through week 48, tracked adverse events from the first dose of study drug until 14 days after discontinuation. Adverse events that were more common with letermovir than placebo included vomiting (19% versus 14%), edema (15% versus 9%), atrial arrhythmias (10% versus 5%), and having alanine aspartate levels more than five times the upper limit of normal (4% versus 2%). Graft versus host disease occurred in 39% of patients in each group; diarrhea and nausea occurred in approximately one fourth of patients in each group.
In response to a question after the presentation, Dr. Marty said, “The higher the risk of CMV disease, the higher the benefit in terms of survival.” Answering another question, about who should receive letermovir. Dr. Marty replied, “Like acyclovir, we should give it during times of risk. And CMV risk is different for different populations. It’s a matter of managing risks and benefits.”
Though letermovir was safe and well-tolerated in this trial, it’s different from acyclovir in that “it’s not a one dollar a day drug,” Dr. Marty acknowledged.
Merck, which plans to market letermovir, was the sponsor of the study and plans to submit applications for approval in both the United States and in the European Union in 2017. Dr. Marty reported receiving research grants from Merck as well as Astellas, Chimerix, and Shire. Additionally, he has received honoraria from Alexion, Chimerix, LFB, Merck, Roche Molecular Diagnostics, and Shire.
This article was updated 2/27/17.
[email protected]
On Twitter @karioakes
ORLANDO – A first-in-class antiviral drug was safe and effective when used to prevent clinically significant cytomegalovirus infections in adults undergoing hematopoietic cell transplantation.
At 24 weeks post-transplant, 38% (122/325) of those receiving the novel antiviral letermovir were considered treatment failures, compared with 61% (103/170) of those receiving placebo (P less than .0001). All-cause mortality was 10% (n=32/325) for patients receiving letermovir and 16%, (n=27/170) for the placebo group (log rank two-sided P = 0.0317).
The study findings show that “we [can] prevent patients from getting CMV infections from the beginning of the transplant and that [result can] confer a mortality benefit,” lead author Francisco Marty, MD, said in an interview.
Dr. Marty said that letermovir has received fast-track status both from the Food and Drug Administration and from the European Medicines Agency.
HCT recipients who are CMV-positive but who do not have clinically significant disease are not preemptively treated in current practice. “Previously, there wasn’t a primary prevention strategy in bone marrow transplantation. When myelosuppressive drugs were tried such as ganciclovir, any benefit was offset by increased myelosuppression, with resulting increases in bacterial and fungal infections,” said Dr. Marty, professor of medicine at Harvard Medical School, Boston.
Letermovir was generally well-tolerated in the clinical trial; myelotoxicity and nephrotoxicity levels were comparable in patients receiving letermovir and placebo. Letermovir targets the terminase complex, which is a viral replication process specific to CMV and not otherwise present in humans. That fact may explain, in part, letermovir’s limited toxicity, Dr. Marty said. The primary outcome measure of the phase III randomized, double-blind, placebo-controlled trial was the stratum-adjusted proportion of patients who had clinically significant CMV at post-transplant week 24, examining only the patients in the trials who had no detectable CMV DNA at the time of randomization. If patients did not complete the study, or had missing data at week 24, they were considered to have failed the trial.
Overall, 31% of patients were considered at high risk for CMV disease. Half of the patients received myeloablative conditioning, and about a third (35%) received antithymocyte globulin. Donor sources, whose characteristics were balanced between study arms, included 14% mismatched unrelated donors, 13% haploidentical donors, and 4% cord blood.
The multinational study’s 24-week results were presented at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
“This was an international study, conducted at multiple sites in multiple countries. We used two-to-one randomization, and stratified participants by their risk of CMV disease and by study sites. We wanted to make sure the groups were balanced by disease risk and by study sites, to account for regional variations in bone marrow transplant procedures and CMV treatment patterns,” said Dr. Marty.
For the study, clinically significant CMV infection was defined as either CMV disease, such as pneumonia, colitis, or hepatitis, or CMV viremia that would trigger preemptive treatment.
Letermovir, which can be administered orally or intravenously, was dosed at 480 mg per day. Because of the risk for a drug-drug interaction, patients on cyclosporine received 240 mg of letermovir per day. Having intravenous dosing as an option helped patients who were not tolerating oral intake to stay on the study drug during the post-transplant period, he said.
The study drug was begun a median of 9 days post-transplant. Some patients received letermovir or placebo as early as the day of transplant; all patients began the study drug by 28 days post-transplant. The study drug was continued through week 14, or until at least 100 days post-transplant. Overall, 37% of patients had engrafted at the time they began the study drug.
Patients had weekly serum CMV assays performed until week 14, with biweekly sampling done through week 24. If patients developed clinically significant CMV, or if their serum samples yielded CMV DNA warranting preemptive treatment, they discontinued the study drug and began treatment for CMV.
The safety analysis, which was carried through week 48, tracked adverse events from the first dose of study drug until 14 days after discontinuation. Adverse events that were more common with letermovir than placebo included vomiting (19% versus 14%), edema (15% versus 9%), atrial arrhythmias (10% versus 5%), and having alanine aspartate levels more than five times the upper limit of normal (4% versus 2%). Graft versus host disease occurred in 39% of patients in each group; diarrhea and nausea occurred in approximately one fourth of patients in each group.
In response to a question after the presentation, Dr. Marty said, “The higher the risk of CMV disease, the higher the benefit in terms of survival.” Answering another question, about who should receive letermovir. Dr. Marty replied, “Like acyclovir, we should give it during times of risk. And CMV risk is different for different populations. It’s a matter of managing risks and benefits.”
Though letermovir was safe and well-tolerated in this trial, it’s different from acyclovir in that “it’s not a one dollar a day drug,” Dr. Marty acknowledged.
Merck, which plans to market letermovir, was the sponsor of the study and plans to submit applications for approval in both the United States and in the European Union in 2017. Dr. Marty reported receiving research grants from Merck as well as Astellas, Chimerix, and Shire. Additionally, he has received honoraria from Alexion, Chimerix, LFB, Merck, Roche Molecular Diagnostics, and Shire.
This article was updated 2/27/17.
[email protected]
On Twitter @karioakes
AT THE 2017 BMT TANDEM MEETINGS
Key clinical point:
Major finding: Cytomegalovirus (CMV) infection or viremia occurred in 38% of patients receiving post-HCT letermovir, compared with 61% of controls.
Data source: Randomized, double-blind, placebo-controlled study of 495 patients seropositive for CMV with no detectable CMV DNA at the time of HCT.
Disclosures: Merck, which plans to market letermovir, was the sponsor of the study. Dr. Marty reported receiving research grants from Merck as well as Astellas, Chimerix, and Shire. Additionally, he has received honoraria from Alexion, Chimerix, LFB, Merck, Roche Molecular Diagnostics, and Shire.
Neuropathic pain puts cancer survivors out of work
AMSTERDAM – Five years after a cancer diagnosis, patients who report having chronic neuropathic pain are twice as likely to be out of work as patients who report having no neuropathic pain, authors of a large longitudinal study said.
“For middle-term cancer survivors, suffering from chronic neuropathic pain unfortunately predicts labor-market exit,” said Marc-Karim Bendiane, from Aix-Marseille University in Marseille, France.
Pain is still frequently underdiagnosed, poorly managed, and undertreated among cancer survivors, and there is a need for alternatives to analgesics for control of chronic neuropathic pain (CNP), Mr. Bendiane said at an annual congress sponsored by the European Cancer Organisation.
Mr. Bendiane and colleagues used data from VICAN, a longitudinal survey of issues of concern to cancer survivors 2 years and 5 years after a diagnosis. The cohort consists of patients diagnosed with cancers who comprise 88% of all cancer diagnoses in France, including cancers of the breast; colon and rectum; lip, oral cavity, and pharynx; kidney; cervix; endometrium; non-Hodgkin lymphoma; melanoma; thyroid; bladder; and prostate.
To assess CNP, the researchers used data from a seven-item questionnaire designed to identify neuropathic characteristics of pain experienced by patients in the 2 weeks prior to a comprehensive patient interview.
Of the 982 patients who were working at the time of diagnosis, 36% reported pain within the previous 2 weeks, and of this group, 79% had chronic pain of neuropathic origin. CNP was more common in women than in men (P less than .01); in college-educated people, compared with less-educated people (P less than .001); those who had undergone chemotherapy, compared with no chemotherapy (P less than .001); and those who had radiotherapy vs. no radiotherapy (P less than .001).
For each cancer site, the prevalence of CNP among 5-year cancer survivors was substantially higher than the overall prevalence in France of 7%. For example, 34% of patients with cancers of the cervix and endometrium reported CNP, as did 29.9% of patients who survived cancers of the lip, oral cavity, and pharynx, 32.1% of lung cancer survivors, and 32.7% of breast cancer survivors.
Five years after diagnosis, 22.6% of patients who had been employed in 2010 were out of work in 2015.
The presence of CNP was associated with a nearly twofold greater risk of unemployment (adjusted odds ratio, 1.96; P less than .001) in a multivariate logistic regression analysis comparing employed and unemployed patients and controlling for social and demographic characteristics, job characteristics at diagnosis, and medical factors such as tumor site, prognosis, and treatment type.
The French National Cancer Institute and INSERM, the National Institute for Research in Health and Medicine, supported the study. The investigators reported no conflicts of interest.
AMSTERDAM – Five years after a cancer diagnosis, patients who report having chronic neuropathic pain are twice as likely to be out of work as patients who report having no neuropathic pain, authors of a large longitudinal study said.
“For middle-term cancer survivors, suffering from chronic neuropathic pain unfortunately predicts labor-market exit,” said Marc-Karim Bendiane, from Aix-Marseille University in Marseille, France.
Pain is still frequently underdiagnosed, poorly managed, and undertreated among cancer survivors, and there is a need for alternatives to analgesics for control of chronic neuropathic pain (CNP), Mr. Bendiane said at an annual congress sponsored by the European Cancer Organisation.
Mr. Bendiane and colleagues used data from VICAN, a longitudinal survey of issues of concern to cancer survivors 2 years and 5 years after a diagnosis. The cohort consists of patients diagnosed with cancers who comprise 88% of all cancer diagnoses in France, including cancers of the breast; colon and rectum; lip, oral cavity, and pharynx; kidney; cervix; endometrium; non-Hodgkin lymphoma; melanoma; thyroid; bladder; and prostate.
To assess CNP, the researchers used data from a seven-item questionnaire designed to identify neuropathic characteristics of pain experienced by patients in the 2 weeks prior to a comprehensive patient interview.
Of the 982 patients who were working at the time of diagnosis, 36% reported pain within the previous 2 weeks, and of this group, 79% had chronic pain of neuropathic origin. CNP was more common in women than in men (P less than .01); in college-educated people, compared with less-educated people (P less than .001); those who had undergone chemotherapy, compared with no chemotherapy (P less than .001); and those who had radiotherapy vs. no radiotherapy (P less than .001).
For each cancer site, the prevalence of CNP among 5-year cancer survivors was substantially higher than the overall prevalence in France of 7%. For example, 34% of patients with cancers of the cervix and endometrium reported CNP, as did 29.9% of patients who survived cancers of the lip, oral cavity, and pharynx, 32.1% of lung cancer survivors, and 32.7% of breast cancer survivors.
Five years after diagnosis, 22.6% of patients who had been employed in 2010 were out of work in 2015.
The presence of CNP was associated with a nearly twofold greater risk of unemployment (adjusted odds ratio, 1.96; P less than .001) in a multivariate logistic regression analysis comparing employed and unemployed patients and controlling for social and demographic characteristics, job characteristics at diagnosis, and medical factors such as tumor site, prognosis, and treatment type.
The French National Cancer Institute and INSERM, the National Institute for Research in Health and Medicine, supported the study. The investigators reported no conflicts of interest.
AMSTERDAM – Five years after a cancer diagnosis, patients who report having chronic neuropathic pain are twice as likely to be out of work as patients who report having no neuropathic pain, authors of a large longitudinal study said.
“For middle-term cancer survivors, suffering from chronic neuropathic pain unfortunately predicts labor-market exit,” said Marc-Karim Bendiane, from Aix-Marseille University in Marseille, France.
Pain is still frequently underdiagnosed, poorly managed, and undertreated among cancer survivors, and there is a need for alternatives to analgesics for control of chronic neuropathic pain (CNP), Mr. Bendiane said at an annual congress sponsored by the European Cancer Organisation.
Mr. Bendiane and colleagues used data from VICAN, a longitudinal survey of issues of concern to cancer survivors 2 years and 5 years after a diagnosis. The cohort consists of patients diagnosed with cancers who comprise 88% of all cancer diagnoses in France, including cancers of the breast; colon and rectum; lip, oral cavity, and pharynx; kidney; cervix; endometrium; non-Hodgkin lymphoma; melanoma; thyroid; bladder; and prostate.
To assess CNP, the researchers used data from a seven-item questionnaire designed to identify neuropathic characteristics of pain experienced by patients in the 2 weeks prior to a comprehensive patient interview.
Of the 982 patients who were working at the time of diagnosis, 36% reported pain within the previous 2 weeks, and of this group, 79% had chronic pain of neuropathic origin. CNP was more common in women than in men (P less than .01); in college-educated people, compared with less-educated people (P less than .001); those who had undergone chemotherapy, compared with no chemotherapy (P less than .001); and those who had radiotherapy vs. no radiotherapy (P less than .001).
For each cancer site, the prevalence of CNP among 5-year cancer survivors was substantially higher than the overall prevalence in France of 7%. For example, 34% of patients with cancers of the cervix and endometrium reported CNP, as did 29.9% of patients who survived cancers of the lip, oral cavity, and pharynx, 32.1% of lung cancer survivors, and 32.7% of breast cancer survivors.
Five years after diagnosis, 22.6% of patients who had been employed in 2010 were out of work in 2015.
The presence of CNP was associated with a nearly twofold greater risk of unemployment (adjusted odds ratio, 1.96; P less than .001) in a multivariate logistic regression analysis comparing employed and unemployed patients and controlling for social and demographic characteristics, job characteristics at diagnosis, and medical factors such as tumor site, prognosis, and treatment type.
The French National Cancer Institute and INSERM, the National Institute for Research in Health and Medicine, supported the study. The investigators reported no conflicts of interest.
Key clinical point: Chronic neuropathic pain is a barrier to employment for many cancer survivors.
Major finding: Cancer survivors with chronic neuropathic pain were twice as likely to be unemployed 5 years after diagnosis as patients with no pain.
Data source: Longitudinal study of French cancer survivors.
Disclosures: The French National Cancer Institute and INSERM, the National Institute for Research in Health and Medicine, supported the study. The investigators reported no conflicts of interest.
FDA opens abbreviated approval pathway for interchangeable biosimilars
The Food and Drug Administration has proposed a regulatory path for biosimilar biologics that are interchangeable with the reference product, paving the way for a new generation of less-expensive versions of these unique drugs.
But bringing an interchangeable biosimilar to market won’t be easy. The bar for interchangeability will be high, requiring that manufacturers prove switching between the new and older products is safe. And clinicians, while cautiously optimistic, aren’t thrilled with the industry payoff that could come with the designation: freedom for insurance companies and pharmacies to switch products at the dispensing level without requiring a new prescription.
The draft FDA guidance for industry, “Considerations in Demonstrating Interchangeability With a Reference Product,” arises from the Biologics Price Competition and Innovation Act of 2009. That section of the Affordable Care Act provides for abbreviated approval pathways for biological products that are demonstrated to be “highly similar” (biosimilar) to or “interchangeable” with an FDA-approved biological product.
The difference between these appellations is subtle but critical to the regulatory process – and perhaps to patient safety. Regulators recognize that the structure of these large, highly complex molecules can never precisely replicate the reference product. But to be labeled a “biosimilar,” developers must prove that the new product functions essentially the same; there can be no clinically meaningful differences in terms of safety, purity, and potency. Unlike a generic medication, a biosimilar can’t be substituted for its reference product at the pharmacy level. If a physician wants the patient on that biosimilar, the script must specify it.
Interchangeables jump a higher regulatory bar
An “interchangeable biosimilar,” though, would have to jump a higher regulatory bar. Not only must it produce the same clinical result as the reference product, it also must be benignly interchangeable with it, conferring no additional risk if a patient switches from the reference to the biosimilar and back again. A pharmacist could, if permitted by state law, substitute an interchangeable product for the reference product without going through the prescriber.
Like biosimilars, interchangeable products need not be tested in every disease for which the reference drug is approved, according to the document. Once they are proved safe for one indication, those data can be extrapolated to allow approval for the other indications as well. Nor do biosimilars need to prove efficacy per se, as their molecular similarity to the reference product ensures that they bind to the same receptor and exert the same therapeutic effect.
The biosimilar/interchangeable market has been slow to take off in the United States. There are no approved interchangeable biosimilars, and only four biosimilars – three of which were approved in 2016:
• Sandoz’ filgrastim-sndz (Zarxio).
• Pfizer’s and Celltrion’s infliximab-dyyb (Inflectra).
• Sandoz’ etanercept-szzs (Erelzi).
• Amgen’s adalimumab-atto (Amjevita).
Switching studies is the key to achieving the interchangeable designation, according to the FDA document. They must include at least two full switches between the candidate product and the reference product, which must be licensed in the United States.
But because these products are so structurally diverse, the FDA isn’t imposing a one-size-fits-all process on them. Instead, the molecular complexity and immunogenicity of each product will dictate its approval requirements.
Those with relatively low structural complexity, high molecular similarity to the reference product, and a low incidence of immunogenic adverse events may only need a single switching study to achieve the “interchangeability” designation.
The bar will be higher for a product with high structural complexity that is not as similar to the reference product, or which has been associated with immunogenic adverse events. For this product, FDA might also require extensive safety postmarketing data for the product as a licensed biosimilar, as well as a switching study.
Pharmacokinetics, pharmacodynamics, immunogenicity, and safety will be the primary endpoints of a switching study. Efficacy data are not necessary but can be used as supportive endpoints. Any safety signals in a switching study would raise regulatory eyebrows whether they came from the candidate product or the reference product. Since the study replicates what could happen if the two were used sequentially, it makes little difference from which product the event might arise.
“If an apparent difference in immune response or adverse events is noticed between the switching and nonswitching arms of the study ... it would raise concerns as to whether the proposed interchangeable product is interchangeable, regardless of whether the proposed interchangeable product or the reference product or the switching of the two products actually caused the event,” the document notes.
The E.U. vs. U.S. experience
The United States is only now getting a taste of what has become common fare in the European Union, said Angus Worthing, MD, chair of the American College of Rheumatology’s Government Affairs Committee. The European Medicines Agency approved its first biosimilar in 2006. Since then, 23 such drugs have come on the market, at an average price of about 30% less than the reference drug. Prices for some drugs have dropped as much as 70% in countries in which national health care systems abandoned the reference product in favor of the competing biosimilar, Dr. Worthing said in an interview.
“But the U.S. doesn’t have a national health care system, so it won’t work like that here.” In fact, he noted, brand-new data show that Medicare actually paid 22% more for the infliximab biosimilar Inflectra than it did for Remicade in the last quarter of 2016.
It’s not immediately apparent why this is the case, but it’s probably related to company discounts and rebates on these very expensive drugs. According to the report in Inside Health Policy, Janssen Biotech may have increased its discount on the drug to compete with Inflectra’s launch price of 15% below Remicade’s wholesale cost. Prices won’t moderate as much in the United States as in the European Union until several biosimilars of the same class appear, Dr. Worthing said.
There have already been allegations that big pharma manipulates international and national pricing to reduce biosimilar competition.
In June, Russian biotech company Biocad filed a lawsuit in New York charging Roche/Genentech with price fixing. The suit alleges that the companies cut the cost of three cancer drugs (Avastin, Herceptin, and Rituxan/MabThera) in Russia, where Biocad markets biosimilars for each. At the same time, Biocad alleges, the companies raised U.S. prices on those drugs to make up for the money they were losing on the Russian market.
“I think most of the cost benefits will accrue to insurance plans and pharmacy managers, but maybe not to the patients themselves,” he said in an interview. “The most important beneficiaries may not see a single penny of benefit.”
It may be difficult to extrapolate the European economic experience into the U.S. health care market, but the safety record of its biosimilar armamentarium is solid. None of the biosimilars approved in the E.U. have ever been recalled or removed from the European market because of regulatory or safety concerns.
Nonmedical switching raises concerns
Academic medical societies and clinicians interviewed for this article view the proposed approval pathway with cautious optimism. While acknowledging the potential benefit of reducing the costs of prohibitively expensive drugs, they uniformly insist that patient safety – not economic pressure – should be the driving force here.
“I was initially skeptical, and I do believe that we need very close pharmacovigilance in monitoring these for safety,” said Gideon Smith, MD, PhD, a dermatologist at Massachusetts General Hospital, Boston. “But there has been huge uptake of these products in the E.U., and the data are so extensive that we can be reasonably confident these drugs are effective, and no good reason to believe the safety will be any different.”
He is not as comfortable with the prospect of pharmacy-level substitution of an interchangeable biosimilar with the reference product – a feeling that other clinicians echoed.
“I think this is a fundamental issue that should have been dealt with on a federal level. Physicians should always be involved in the decision,” said Dr. Smith, who spoke at an FDA advisory committee meeting last summer on behalf of the American Academy of Dermatology (AAD).
“In general, the GI field is OK with the idea of starting someone on a new prescription [of an interchangeable biosimilar], but not so much with the idea of switching around,” said Dr. Hanauer, who is the Clifford Joseph Barborka Professor of Gastroenterology at Northwestern University, Chicago. “In these biologic compounds, very small differences can be amplified” and alter therapeutic response.
The possibility of switching from the reference to the biosimilar and maybe back again worries him. He hearkened back to the approval of Remicade, when patients who had taken it during clinical trials only were finally able to obtain it on the market. Dr. Hanauer explained that, “20% of them developed serum sickness reactions after the reexposure.”
He also expressed some concern about quality control in international manufacturing plants, citing a 2005 epidemic of immune-mediated pure red cell anemia in patients who received an epoetin alfa biosimilar manufactured in Thailand. The prefilled syringes had an uncoated rubber stopper that apparently reacted with polysorbate 60 in the solution – an interaction that increased immunogenicity when the drug was administered subcutaneously.
Dr. Smith concurred. “We know that some patients produce antibodies to biologics if they come on and off, and so we discourage that. The concern is that switching may lead to an increased rate of medication failure, if you have to switch back. This is especially troubling in the case of a hard-to-control patient with severe flares. If they’re being well controlled on a medication, the last thing you want to do is change it for no good clinical reason. And we may well be forced to do that.”
Neither the AAD nor the American College of Gastroenterology has a published stand on the FDA’s proposed guidance for interchangeable biosimilars. The preliminary view of the American College of Rheumatology is a positive one, Dr. Worthing said. However, ACR feels pharmacy-level switching should be a joint, not unilateral, decision.
“Our position statement on biosimilars has been that if it’s legal for a pharmacy to make that switch then we want the doctor and the patient to know, so we can track for safety signals.”
Bringing any biosimilar to market, though, takes a lot of money and a lot of time. And while companies are growing cell lines and producing new molecules that mimic existing drugs, science marches on, said Dr. Smith.
“If we keep dragging our feet on this issue, it might end up being a moot point,” he said. Newer drugs are achieving better results, raising the bar for therapeutic success. An example is the monoclonal antibody secukinumab (Cosentyx), an inhibitor of interleukin 17A. In October 2016, late-breaking data released at the annual meeting of the European Academy of Dermatology and Venereology impressed the dermatology community. In psoriasis patients, the drug maintained 90% skin clearance for 4 years in 66% of patients, and 100% clearance for 4 years in 43%.
Not only does this kind of efficacy provide symptomatic relief, it also prevents the expensive long-term morbidity associated with psoriasis, Dr. Smith said.
“Even if these new medications are considerably more expensive upfront than a biosimilar for an older drug, they may end up being less expensive in the long run.”
Dr. Krant and Dr. Worthing had no financial disclosures. Dr. Smith has received grants from Allergan and Cipher Pharmaceuticals. Dr. Hanauer has received grants from numerous pharmaceutical companies that manufacture biologics.
*This article was updated 1/31/2017.
[email protected]
On Twitter @alz_gal
The Food and Drug Administration has proposed a regulatory path for biosimilar biologics that are interchangeable with the reference product, paving the way for a new generation of less-expensive versions of these unique drugs.
But bringing an interchangeable biosimilar to market won’t be easy. The bar for interchangeability will be high, requiring that manufacturers prove switching between the new and older products is safe. And clinicians, while cautiously optimistic, aren’t thrilled with the industry payoff that could come with the designation: freedom for insurance companies and pharmacies to switch products at the dispensing level without requiring a new prescription.
The draft FDA guidance for industry, “Considerations in Demonstrating Interchangeability With a Reference Product,” arises from the Biologics Price Competition and Innovation Act of 2009. That section of the Affordable Care Act provides for abbreviated approval pathways for biological products that are demonstrated to be “highly similar” (biosimilar) to or “interchangeable” with an FDA-approved biological product.
The difference between these appellations is subtle but critical to the regulatory process – and perhaps to patient safety. Regulators recognize that the structure of these large, highly complex molecules can never precisely replicate the reference product. But to be labeled a “biosimilar,” developers must prove that the new product functions essentially the same; there can be no clinically meaningful differences in terms of safety, purity, and potency. Unlike a generic medication, a biosimilar can’t be substituted for its reference product at the pharmacy level. If a physician wants the patient on that biosimilar, the script must specify it.
Interchangeables jump a higher regulatory bar
An “interchangeable biosimilar,” though, would have to jump a higher regulatory bar. Not only must it produce the same clinical result as the reference product, it also must be benignly interchangeable with it, conferring no additional risk if a patient switches from the reference to the biosimilar and back again. A pharmacist could, if permitted by state law, substitute an interchangeable product for the reference product without going through the prescriber.
Like biosimilars, interchangeable products need not be tested in every disease for which the reference drug is approved, according to the document. Once they are proved safe for one indication, those data can be extrapolated to allow approval for the other indications as well. Nor do biosimilars need to prove efficacy per se, as their molecular similarity to the reference product ensures that they bind to the same receptor and exert the same therapeutic effect.
The biosimilar/interchangeable market has been slow to take off in the United States. There are no approved interchangeable biosimilars, and only four biosimilars – three of which were approved in 2016:
• Sandoz’ filgrastim-sndz (Zarxio).
• Pfizer’s and Celltrion’s infliximab-dyyb (Inflectra).
• Sandoz’ etanercept-szzs (Erelzi).
• Amgen’s adalimumab-atto (Amjevita).
Switching studies is the key to achieving the interchangeable designation, according to the FDA document. They must include at least two full switches between the candidate product and the reference product, which must be licensed in the United States.
But because these products are so structurally diverse, the FDA isn’t imposing a one-size-fits-all process on them. Instead, the molecular complexity and immunogenicity of each product will dictate its approval requirements.
Those with relatively low structural complexity, high molecular similarity to the reference product, and a low incidence of immunogenic adverse events may only need a single switching study to achieve the “interchangeability” designation.
The bar will be higher for a product with high structural complexity that is not as similar to the reference product, or which has been associated with immunogenic adverse events. For this product, FDA might also require extensive safety postmarketing data for the product as a licensed biosimilar, as well as a switching study.
Pharmacokinetics, pharmacodynamics, immunogenicity, and safety will be the primary endpoints of a switching study. Efficacy data are not necessary but can be used as supportive endpoints. Any safety signals in a switching study would raise regulatory eyebrows whether they came from the candidate product or the reference product. Since the study replicates what could happen if the two were used sequentially, it makes little difference from which product the event might arise.
“If an apparent difference in immune response or adverse events is noticed between the switching and nonswitching arms of the study ... it would raise concerns as to whether the proposed interchangeable product is interchangeable, regardless of whether the proposed interchangeable product or the reference product or the switching of the two products actually caused the event,” the document notes.
The E.U. vs. U.S. experience
The United States is only now getting a taste of what has become common fare in the European Union, said Angus Worthing, MD, chair of the American College of Rheumatology’s Government Affairs Committee. The European Medicines Agency approved its first biosimilar in 2006. Since then, 23 such drugs have come on the market, at an average price of about 30% less than the reference drug. Prices for some drugs have dropped as much as 70% in countries in which national health care systems abandoned the reference product in favor of the competing biosimilar, Dr. Worthing said in an interview.
“But the U.S. doesn’t have a national health care system, so it won’t work like that here.” In fact, he noted, brand-new data show that Medicare actually paid 22% more for the infliximab biosimilar Inflectra than it did for Remicade in the last quarter of 2016.
It’s not immediately apparent why this is the case, but it’s probably related to company discounts and rebates on these very expensive drugs. According to the report in Inside Health Policy, Janssen Biotech may have increased its discount on the drug to compete with Inflectra’s launch price of 15% below Remicade’s wholesale cost. Prices won’t moderate as much in the United States as in the European Union until several biosimilars of the same class appear, Dr. Worthing said.
There have already been allegations that big pharma manipulates international and national pricing to reduce biosimilar competition.
In June, Russian biotech company Biocad filed a lawsuit in New York charging Roche/Genentech with price fixing. The suit alleges that the companies cut the cost of three cancer drugs (Avastin, Herceptin, and Rituxan/MabThera) in Russia, where Biocad markets biosimilars for each. At the same time, Biocad alleges, the companies raised U.S. prices on those drugs to make up for the money they were losing on the Russian market.
“I think most of the cost benefits will accrue to insurance plans and pharmacy managers, but maybe not to the patients themselves,” he said in an interview. “The most important beneficiaries may not see a single penny of benefit.”
It may be difficult to extrapolate the European economic experience into the U.S. health care market, but the safety record of its biosimilar armamentarium is solid. None of the biosimilars approved in the E.U. have ever been recalled or removed from the European market because of regulatory or safety concerns.
Nonmedical switching raises concerns
Academic medical societies and clinicians interviewed for this article view the proposed approval pathway with cautious optimism. While acknowledging the potential benefit of reducing the costs of prohibitively expensive drugs, they uniformly insist that patient safety – not economic pressure – should be the driving force here.
“I was initially skeptical, and I do believe that we need very close pharmacovigilance in monitoring these for safety,” said Gideon Smith, MD, PhD, a dermatologist at Massachusetts General Hospital, Boston. “But there has been huge uptake of these products in the E.U., and the data are so extensive that we can be reasonably confident these drugs are effective, and no good reason to believe the safety will be any different.”
He is not as comfortable with the prospect of pharmacy-level substitution of an interchangeable biosimilar with the reference product – a feeling that other clinicians echoed.
“I think this is a fundamental issue that should have been dealt with on a federal level. Physicians should always be involved in the decision,” said Dr. Smith, who spoke at an FDA advisory committee meeting last summer on behalf of the American Academy of Dermatology (AAD).
“In general, the GI field is OK with the idea of starting someone on a new prescription [of an interchangeable biosimilar], but not so much with the idea of switching around,” said Dr. Hanauer, who is the Clifford Joseph Barborka Professor of Gastroenterology at Northwestern University, Chicago. “In these biologic compounds, very small differences can be amplified” and alter therapeutic response.
The possibility of switching from the reference to the biosimilar and maybe back again worries him. He hearkened back to the approval of Remicade, when patients who had taken it during clinical trials only were finally able to obtain it on the market. Dr. Hanauer explained that, “20% of them developed serum sickness reactions after the reexposure.”
He also expressed some concern about quality control in international manufacturing plants, citing a 2005 epidemic of immune-mediated pure red cell anemia in patients who received an epoetin alfa biosimilar manufactured in Thailand. The prefilled syringes had an uncoated rubber stopper that apparently reacted with polysorbate 60 in the solution – an interaction that increased immunogenicity when the drug was administered subcutaneously.
Dr. Smith concurred. “We know that some patients produce antibodies to biologics if they come on and off, and so we discourage that. The concern is that switching may lead to an increased rate of medication failure, if you have to switch back. This is especially troubling in the case of a hard-to-control patient with severe flares. If they’re being well controlled on a medication, the last thing you want to do is change it for no good clinical reason. And we may well be forced to do that.”
Neither the AAD nor the American College of Gastroenterology has a published stand on the FDA’s proposed guidance for interchangeable biosimilars. The preliminary view of the American College of Rheumatology is a positive one, Dr. Worthing said. However, ACR feels pharmacy-level switching should be a joint, not unilateral, decision.
“Our position statement on biosimilars has been that if it’s legal for a pharmacy to make that switch then we want the doctor and the patient to know, so we can track for safety signals.”
Bringing any biosimilar to market, though, takes a lot of money and a lot of time. And while companies are growing cell lines and producing new molecules that mimic existing drugs, science marches on, said Dr. Smith.
“If we keep dragging our feet on this issue, it might end up being a moot point,” he said. Newer drugs are achieving better results, raising the bar for therapeutic success. An example is the monoclonal antibody secukinumab (Cosentyx), an inhibitor of interleukin 17A. In October 2016, late-breaking data released at the annual meeting of the European Academy of Dermatology and Venereology impressed the dermatology community. In psoriasis patients, the drug maintained 90% skin clearance for 4 years in 66% of patients, and 100% clearance for 4 years in 43%.
Not only does this kind of efficacy provide symptomatic relief, it also prevents the expensive long-term morbidity associated with psoriasis, Dr. Smith said.
“Even if these new medications are considerably more expensive upfront than a biosimilar for an older drug, they may end up being less expensive in the long run.”
Dr. Krant and Dr. Worthing had no financial disclosures. Dr. Smith has received grants from Allergan and Cipher Pharmaceuticals. Dr. Hanauer has received grants from numerous pharmaceutical companies that manufacture biologics.
*This article was updated 1/31/2017.
[email protected]
On Twitter @alz_gal
The Food and Drug Administration has proposed a regulatory path for biosimilar biologics that are interchangeable with the reference product, paving the way for a new generation of less-expensive versions of these unique drugs.
But bringing an interchangeable biosimilar to market won’t be easy. The bar for interchangeability will be high, requiring that manufacturers prove switching between the new and older products is safe. And clinicians, while cautiously optimistic, aren’t thrilled with the industry payoff that could come with the designation: freedom for insurance companies and pharmacies to switch products at the dispensing level without requiring a new prescription.
The draft FDA guidance for industry, “Considerations in Demonstrating Interchangeability With a Reference Product,” arises from the Biologics Price Competition and Innovation Act of 2009. That section of the Affordable Care Act provides for abbreviated approval pathways for biological products that are demonstrated to be “highly similar” (biosimilar) to or “interchangeable” with an FDA-approved biological product.
The difference between these appellations is subtle but critical to the regulatory process – and perhaps to patient safety. Regulators recognize that the structure of these large, highly complex molecules can never precisely replicate the reference product. But to be labeled a “biosimilar,” developers must prove that the new product functions essentially the same; there can be no clinically meaningful differences in terms of safety, purity, and potency. Unlike a generic medication, a biosimilar can’t be substituted for its reference product at the pharmacy level. If a physician wants the patient on that biosimilar, the script must specify it.
Interchangeables jump a higher regulatory bar
An “interchangeable biosimilar,” though, would have to jump a higher regulatory bar. Not only must it produce the same clinical result as the reference product, it also must be benignly interchangeable with it, conferring no additional risk if a patient switches from the reference to the biosimilar and back again. A pharmacist could, if permitted by state law, substitute an interchangeable product for the reference product without going through the prescriber.
Like biosimilars, interchangeable products need not be tested in every disease for which the reference drug is approved, according to the document. Once they are proved safe for one indication, those data can be extrapolated to allow approval for the other indications as well. Nor do biosimilars need to prove efficacy per se, as their molecular similarity to the reference product ensures that they bind to the same receptor and exert the same therapeutic effect.
The biosimilar/interchangeable market has been slow to take off in the United States. There are no approved interchangeable biosimilars, and only four biosimilars – three of which were approved in 2016:
• Sandoz’ filgrastim-sndz (Zarxio).
• Pfizer’s and Celltrion’s infliximab-dyyb (Inflectra).
• Sandoz’ etanercept-szzs (Erelzi).
• Amgen’s adalimumab-atto (Amjevita).
Switching studies is the key to achieving the interchangeable designation, according to the FDA document. They must include at least two full switches between the candidate product and the reference product, which must be licensed in the United States.
But because these products are so structurally diverse, the FDA isn’t imposing a one-size-fits-all process on them. Instead, the molecular complexity and immunogenicity of each product will dictate its approval requirements.
Those with relatively low structural complexity, high molecular similarity to the reference product, and a low incidence of immunogenic adverse events may only need a single switching study to achieve the “interchangeability” designation.
The bar will be higher for a product with high structural complexity that is not as similar to the reference product, or which has been associated with immunogenic adverse events. For this product, FDA might also require extensive safety postmarketing data for the product as a licensed biosimilar, as well as a switching study.
Pharmacokinetics, pharmacodynamics, immunogenicity, and safety will be the primary endpoints of a switching study. Efficacy data are not necessary but can be used as supportive endpoints. Any safety signals in a switching study would raise regulatory eyebrows whether they came from the candidate product or the reference product. Since the study replicates what could happen if the two were used sequentially, it makes little difference from which product the event might arise.
“If an apparent difference in immune response or adverse events is noticed between the switching and nonswitching arms of the study ... it would raise concerns as to whether the proposed interchangeable product is interchangeable, regardless of whether the proposed interchangeable product or the reference product or the switching of the two products actually caused the event,” the document notes.
The E.U. vs. U.S. experience
The United States is only now getting a taste of what has become common fare in the European Union, said Angus Worthing, MD, chair of the American College of Rheumatology’s Government Affairs Committee. The European Medicines Agency approved its first biosimilar in 2006. Since then, 23 such drugs have come on the market, at an average price of about 30% less than the reference drug. Prices for some drugs have dropped as much as 70% in countries in which national health care systems abandoned the reference product in favor of the competing biosimilar, Dr. Worthing said in an interview.
“But the U.S. doesn’t have a national health care system, so it won’t work like that here.” In fact, he noted, brand-new data show that Medicare actually paid 22% more for the infliximab biosimilar Inflectra than it did for Remicade in the last quarter of 2016.
It’s not immediately apparent why this is the case, but it’s probably related to company discounts and rebates on these very expensive drugs. According to the report in Inside Health Policy, Janssen Biotech may have increased its discount on the drug to compete with Inflectra’s launch price of 15% below Remicade’s wholesale cost. Prices won’t moderate as much in the United States as in the European Union until several biosimilars of the same class appear, Dr. Worthing said.
There have already been allegations that big pharma manipulates international and national pricing to reduce biosimilar competition.
In June, Russian biotech company Biocad filed a lawsuit in New York charging Roche/Genentech with price fixing. The suit alleges that the companies cut the cost of three cancer drugs (Avastin, Herceptin, and Rituxan/MabThera) in Russia, where Biocad markets biosimilars for each. At the same time, Biocad alleges, the companies raised U.S. prices on those drugs to make up for the money they were losing on the Russian market.
“I think most of the cost benefits will accrue to insurance plans and pharmacy managers, but maybe not to the patients themselves,” he said in an interview. “The most important beneficiaries may not see a single penny of benefit.”
It may be difficult to extrapolate the European economic experience into the U.S. health care market, but the safety record of its biosimilar armamentarium is solid. None of the biosimilars approved in the E.U. have ever been recalled or removed from the European market because of regulatory or safety concerns.
Nonmedical switching raises concerns
Academic medical societies and clinicians interviewed for this article view the proposed approval pathway with cautious optimism. While acknowledging the potential benefit of reducing the costs of prohibitively expensive drugs, they uniformly insist that patient safety – not economic pressure – should be the driving force here.
“I was initially skeptical, and I do believe that we need very close pharmacovigilance in monitoring these for safety,” said Gideon Smith, MD, PhD, a dermatologist at Massachusetts General Hospital, Boston. “But there has been huge uptake of these products in the E.U., and the data are so extensive that we can be reasonably confident these drugs are effective, and no good reason to believe the safety will be any different.”
He is not as comfortable with the prospect of pharmacy-level substitution of an interchangeable biosimilar with the reference product – a feeling that other clinicians echoed.
“I think this is a fundamental issue that should have been dealt with on a federal level. Physicians should always be involved in the decision,” said Dr. Smith, who spoke at an FDA advisory committee meeting last summer on behalf of the American Academy of Dermatology (AAD).
“In general, the GI field is OK with the idea of starting someone on a new prescription [of an interchangeable biosimilar], but not so much with the idea of switching around,” said Dr. Hanauer, who is the Clifford Joseph Barborka Professor of Gastroenterology at Northwestern University, Chicago. “In these biologic compounds, very small differences can be amplified” and alter therapeutic response.
The possibility of switching from the reference to the biosimilar and maybe back again worries him. He hearkened back to the approval of Remicade, when patients who had taken it during clinical trials only were finally able to obtain it on the market. Dr. Hanauer explained that, “20% of them developed serum sickness reactions after the reexposure.”
He also expressed some concern about quality control in international manufacturing plants, citing a 2005 epidemic of immune-mediated pure red cell anemia in patients who received an epoetin alfa biosimilar manufactured in Thailand. The prefilled syringes had an uncoated rubber stopper that apparently reacted with polysorbate 60 in the solution – an interaction that increased immunogenicity when the drug was administered subcutaneously.
Dr. Smith concurred. “We know that some patients produce antibodies to biologics if they come on and off, and so we discourage that. The concern is that switching may lead to an increased rate of medication failure, if you have to switch back. This is especially troubling in the case of a hard-to-control patient with severe flares. If they’re being well controlled on a medication, the last thing you want to do is change it for no good clinical reason. And we may well be forced to do that.”
Neither the AAD nor the American College of Gastroenterology has a published stand on the FDA’s proposed guidance for interchangeable biosimilars. The preliminary view of the American College of Rheumatology is a positive one, Dr. Worthing said. However, ACR feels pharmacy-level switching should be a joint, not unilateral, decision.
“Our position statement on biosimilars has been that if it’s legal for a pharmacy to make that switch then we want the doctor and the patient to know, so we can track for safety signals.”
Bringing any biosimilar to market, though, takes a lot of money and a lot of time. And while companies are growing cell lines and producing new molecules that mimic existing drugs, science marches on, said Dr. Smith.
“If we keep dragging our feet on this issue, it might end up being a moot point,” he said. Newer drugs are achieving better results, raising the bar for therapeutic success. An example is the monoclonal antibody secukinumab (Cosentyx), an inhibitor of interleukin 17A. In October 2016, late-breaking data released at the annual meeting of the European Academy of Dermatology and Venereology impressed the dermatology community. In psoriasis patients, the drug maintained 90% skin clearance for 4 years in 66% of patients, and 100% clearance for 4 years in 43%.
Not only does this kind of efficacy provide symptomatic relief, it also prevents the expensive long-term morbidity associated with psoriasis, Dr. Smith said.
“Even if these new medications are considerably more expensive upfront than a biosimilar for an older drug, they may end up being less expensive in the long run.”
Dr. Krant and Dr. Worthing had no financial disclosures. Dr. Smith has received grants from Allergan and Cipher Pharmaceuticals. Dr. Hanauer has received grants from numerous pharmaceutical companies that manufacture biologics.
*This article was updated 1/31/2017.
[email protected]
On Twitter @alz_gal
Cardiac events after NSCLC radiotherapy occur early
Cardiac events are “relatively common,” affecting 23% of patients, and occur earlier than previously thought following radiotherapy for non–small-cell lung cancer (NSCLC), according to a report in the Journal of Clinical Oncology.
Radiation-associated cardiac toxicity has long been recognized in patients treated for other thoracic cancers, but the conventional wisdom has been that it isn’t a consideration in patients with stage III NSCLC because “there are few long-term survivors to experience toxicity, given the typically long latency of radiotherapy-associated heart injury and the poor prognosis” of this cancer. However, the findings “challenge the perception that minimizing heart dose is not important in the treatment of patients with stage III NSCLC,” said Kyle Wang, MD, of University of North Carolina Hospitals, Chapel Hill, and his associates.
“Our data support minimization of heart radiation exposure whenever possible to doses lower than commonly recommended in patients with stage III NSCLC, to reduce risks of [cardiac] toxicity,” they noted.
Dr. Wang and his associates performed a retrospective post hoc analysis of data pooled from six prospective phase I and II trials that the University of North Carolina was involved in between 1996 and 2009. The studies assessed both dose-escalated radiotherapy and various chemotherapeutic regimens in 112 patients who were followed for a median of 8.8 years (range, 2.3-17.3 years). All the patients received induction chemotherapy, 90% received concurrent chemotherapy, and 25% received consolidation chemotherapy.
A total of 26 patients (23%) had at least one symptomatic cardiac event following radiotherapy: pericardial effusion (7 patients), MI (5 patients), unstable angina (3 patients), pericarditis (2 patients), significant arrhythmia (12 patients), and heart failure (1 patient). After the data were adjusted to account for competing risks of death, the 2-year rate of symptomatic cardiac toxicity was 10% and the 4-year rate was 18%. The first adverse cardiac event occurred at a median of 26 months (range, 1-84 months).
The risk of cardiac toxicities rose with increasing radiation exposure: At 2 years, the rate of cardiac events was 4% for those exposed to less than 10 Gy, 7% for those exposed to 10-20 Gy, and 21% for those exposed to greater than 20 Gy. At 4 years, those rates were 4%, 13%, and 41%, respectively. Patients whose hearts were exposed to greater than 20 Gy had a significantly higher rate of cardiac events than did those exposed to less than 10 Gy (HR, 5.47) or to 10-20 Gy (HR, 2.76).
Even though the prognosis may be poor in patients with stage III NSCLC, “they generally receive higher heart doses and may also have more comorbidities and smoking history, thus increasing risk and perhaps shortening the latency between radiotherapy and resultant heart disease,” Dr. Wang and his associates said (J Clin Oncol. 2017 Jan 23 [doi: 10.1200/JCO.2016.70.0229]).
“In our opinion, tumor coverage should rarely be compromised to meet a heart dose constraint. However, it would be reasonable to try to limit heart mean dose to less than 20 Gy (lower if possible) on the basis of the high event rate we observed in patients exceeding this dose (21% at 2 years and 41% at 4 years). Sophisticated radiation treatment planning techniques (e.g., [intensity-modulated radiation therapy]) and charged-particle therapy with protons or carbon ions may provide increased flexibility to generate more conformal treatment plans and reduce heart dose, which could potentially improve the clinical outcomes in patients with stage III NSCLC,” they added.
This is the first report to clearly associate radiation doses with clinically significant cardiac events in patients with locally advanced NSCLC treated with modern radiotherapy techniques, and it suggests that these events happen much earlier than conventionally believed.
Perhaps cardiac risk didn’t matter so much when, historically, the life expectancy of this patient population was only 2 years. But given the improvements in survival over the last 2 decades, together with the findings of Wang et al., the era of indiscriminate irradiation to the heart should end.
Charles B. Simone II, MD, is at the University of Maryland Medical Center, Baltimore. He reported having no relevant financial disclosures. Dr. Simone made these remarks in an editorial accompanying Dr. Wang’s report (J Clin Oncol. 2017 January 23 [doi: 10.1200/JCO.2016.71.5581]).
This is the first report to clearly associate radiation doses with clinically significant cardiac events in patients with locally advanced NSCLC treated with modern radiotherapy techniques, and it suggests that these events happen much earlier than conventionally believed.
Perhaps cardiac risk didn’t matter so much when, historically, the life expectancy of this patient population was only 2 years. But given the improvements in survival over the last 2 decades, together with the findings of Wang et al., the era of indiscriminate irradiation to the heart should end.
Charles B. Simone II, MD, is at the University of Maryland Medical Center, Baltimore. He reported having no relevant financial disclosures. Dr. Simone made these remarks in an editorial accompanying Dr. Wang’s report (J Clin Oncol. 2017 January 23 [doi: 10.1200/JCO.2016.71.5581]).
This is the first report to clearly associate radiation doses with clinically significant cardiac events in patients with locally advanced NSCLC treated with modern radiotherapy techniques, and it suggests that these events happen much earlier than conventionally believed.
Perhaps cardiac risk didn’t matter so much when, historically, the life expectancy of this patient population was only 2 years. But given the improvements in survival over the last 2 decades, together with the findings of Wang et al., the era of indiscriminate irradiation to the heart should end.
Charles B. Simone II, MD, is at the University of Maryland Medical Center, Baltimore. He reported having no relevant financial disclosures. Dr. Simone made these remarks in an editorial accompanying Dr. Wang’s report (J Clin Oncol. 2017 January 23 [doi: 10.1200/JCO.2016.71.5581]).
Cardiac events are “relatively common,” affecting 23% of patients, and occur earlier than previously thought following radiotherapy for non–small-cell lung cancer (NSCLC), according to a report in the Journal of Clinical Oncology.
Radiation-associated cardiac toxicity has long been recognized in patients treated for other thoracic cancers, but the conventional wisdom has been that it isn’t a consideration in patients with stage III NSCLC because “there are few long-term survivors to experience toxicity, given the typically long latency of radiotherapy-associated heart injury and the poor prognosis” of this cancer. However, the findings “challenge the perception that minimizing heart dose is not important in the treatment of patients with stage III NSCLC,” said Kyle Wang, MD, of University of North Carolina Hospitals, Chapel Hill, and his associates.
“Our data support minimization of heart radiation exposure whenever possible to doses lower than commonly recommended in patients with stage III NSCLC, to reduce risks of [cardiac] toxicity,” they noted.
Dr. Wang and his associates performed a retrospective post hoc analysis of data pooled from six prospective phase I and II trials that the University of North Carolina was involved in between 1996 and 2009. The studies assessed both dose-escalated radiotherapy and various chemotherapeutic regimens in 112 patients who were followed for a median of 8.8 years (range, 2.3-17.3 years). All the patients received induction chemotherapy, 90% received concurrent chemotherapy, and 25% received consolidation chemotherapy.
A total of 26 patients (23%) had at least one symptomatic cardiac event following radiotherapy: pericardial effusion (7 patients), MI (5 patients), unstable angina (3 patients), pericarditis (2 patients), significant arrhythmia (12 patients), and heart failure (1 patient). After the data were adjusted to account for competing risks of death, the 2-year rate of symptomatic cardiac toxicity was 10% and the 4-year rate was 18%. The first adverse cardiac event occurred at a median of 26 months (range, 1-84 months).
The risk of cardiac toxicities rose with increasing radiation exposure: At 2 years, the rate of cardiac events was 4% for those exposed to less than 10 Gy, 7% for those exposed to 10-20 Gy, and 21% for those exposed to greater than 20 Gy. At 4 years, those rates were 4%, 13%, and 41%, respectively. Patients whose hearts were exposed to greater than 20 Gy had a significantly higher rate of cardiac events than did those exposed to less than 10 Gy (HR, 5.47) or to 10-20 Gy (HR, 2.76).
Even though the prognosis may be poor in patients with stage III NSCLC, “they generally receive higher heart doses and may also have more comorbidities and smoking history, thus increasing risk and perhaps shortening the latency between radiotherapy and resultant heart disease,” Dr. Wang and his associates said (J Clin Oncol. 2017 Jan 23 [doi: 10.1200/JCO.2016.70.0229]).
“In our opinion, tumor coverage should rarely be compromised to meet a heart dose constraint. However, it would be reasonable to try to limit heart mean dose to less than 20 Gy (lower if possible) on the basis of the high event rate we observed in patients exceeding this dose (21% at 2 years and 41% at 4 years). Sophisticated radiation treatment planning techniques (e.g., [intensity-modulated radiation therapy]) and charged-particle therapy with protons or carbon ions may provide increased flexibility to generate more conformal treatment plans and reduce heart dose, which could potentially improve the clinical outcomes in patients with stage III NSCLC,” they added.
Cardiac events are “relatively common,” affecting 23% of patients, and occur earlier than previously thought following radiotherapy for non–small-cell lung cancer (NSCLC), according to a report in the Journal of Clinical Oncology.
Radiation-associated cardiac toxicity has long been recognized in patients treated for other thoracic cancers, but the conventional wisdom has been that it isn’t a consideration in patients with stage III NSCLC because “there are few long-term survivors to experience toxicity, given the typically long latency of radiotherapy-associated heart injury and the poor prognosis” of this cancer. However, the findings “challenge the perception that minimizing heart dose is not important in the treatment of patients with stage III NSCLC,” said Kyle Wang, MD, of University of North Carolina Hospitals, Chapel Hill, and his associates.
“Our data support minimization of heart radiation exposure whenever possible to doses lower than commonly recommended in patients with stage III NSCLC, to reduce risks of [cardiac] toxicity,” they noted.
Dr. Wang and his associates performed a retrospective post hoc analysis of data pooled from six prospective phase I and II trials that the University of North Carolina was involved in between 1996 and 2009. The studies assessed both dose-escalated radiotherapy and various chemotherapeutic regimens in 112 patients who were followed for a median of 8.8 years (range, 2.3-17.3 years). All the patients received induction chemotherapy, 90% received concurrent chemotherapy, and 25% received consolidation chemotherapy.
A total of 26 patients (23%) had at least one symptomatic cardiac event following radiotherapy: pericardial effusion (7 patients), MI (5 patients), unstable angina (3 patients), pericarditis (2 patients), significant arrhythmia (12 patients), and heart failure (1 patient). After the data were adjusted to account for competing risks of death, the 2-year rate of symptomatic cardiac toxicity was 10% and the 4-year rate was 18%. The first adverse cardiac event occurred at a median of 26 months (range, 1-84 months).
The risk of cardiac toxicities rose with increasing radiation exposure: At 2 years, the rate of cardiac events was 4% for those exposed to less than 10 Gy, 7% for those exposed to 10-20 Gy, and 21% for those exposed to greater than 20 Gy. At 4 years, those rates were 4%, 13%, and 41%, respectively. Patients whose hearts were exposed to greater than 20 Gy had a significantly higher rate of cardiac events than did those exposed to less than 10 Gy (HR, 5.47) or to 10-20 Gy (HR, 2.76).
Even though the prognosis may be poor in patients with stage III NSCLC, “they generally receive higher heart doses and may also have more comorbidities and smoking history, thus increasing risk and perhaps shortening the latency between radiotherapy and resultant heart disease,” Dr. Wang and his associates said (J Clin Oncol. 2017 Jan 23 [doi: 10.1200/JCO.2016.70.0229]).
“In our opinion, tumor coverage should rarely be compromised to meet a heart dose constraint. However, it would be reasonable to try to limit heart mean dose to less than 20 Gy (lower if possible) on the basis of the high event rate we observed in patients exceeding this dose (21% at 2 years and 41% at 4 years). Sophisticated radiation treatment planning techniques (e.g., [intensity-modulated radiation therapy]) and charged-particle therapy with protons or carbon ions may provide increased flexibility to generate more conformal treatment plans and reduce heart dose, which could potentially improve the clinical outcomes in patients with stage III NSCLC,” they added.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Cardiac events are “relatively common” and occur earlier than previously thought following radiotherapy for NSCLC.
Major finding: Following radiotherapy, 26 of 112 patients (23%) had at least one symptomatic cardiac event: pericardial effusion (7 patients), MI (5 patients), unstable angina (3 patients), pericarditis (2 patients), significant arrhythmia (12 patients), and heart failure (1 patient).
Data source: A retrospective post hoc analysis of data from six phase I and II trials involving 112 patients who received radiotherapy for stage-III NSCLC during 1996-2009.
Disclosures: This study was supported in part by the National Institutes of Health. Dr. Wang reported having no relevant financial disclosures; his associates disclosed ties to La Jolla Pharmaceutical, Vision RT, Medtronic, Novartis, Elekta, Morphomics, Accuray, and Varian Medical Systems.
Clonal hematopoiesis increases risk for therapy-related cancers
Small pre-leukemic clones left behind after treatment for non-myeloid malignancies appear to increase the risk for therapy-related myelodysplasia or leukemia, report investigators in two studies.
An analysis of peripheral blood samples taken from patients at the time of their primary cancer diagnosis and bone marrow samples taken at the time of a later therapy-related myeloid neoplasm diagnosis showed that 10 of 14 patients (71%) had clonal hematopoiesis before starting on cytotoxic chemotherapy. In contrast, clonal hematopoiesis was detected in pre-treatment samples of only 17 of 54 controls (31%), reported Koichi Takahashi, MD, and colleagues from the University of Texas MD Anderson Cancer Center in Houston.
“Preleukemic clonal hematopoiesis is common in patients with therapy-related myeloid neoplasms at the time of their primary cancer diagnosis and before they have been exposed to treatment. Our results suggest that clonal hematopoiesis could be used as a predictive marker to identify patients with cancer who are at risk of developing therapy-related myeloid neoplasms,” they wrote (Lancet Oncol 2017; 18: 100–11).
In a separate study, investigators from the Moffitt Cancer Center in Tampa, Florida, found in a nested case-control study that patients with therapy-related myeloid neoplasms were more likely than controls to have clonal hematopoiesis of indeterminate potential (CHIP), and that the CHIP was often present before exposure to chemotherapy.
“We recorded a significantly higher prevalence of CHIP in individuals who developed therapy-related myeloid neoplasms (cases) than in those who did not (controls); however, around 27% of individuals with CHIP did not develop therapy-related myeloid neoplasms, suggesting that this feature alone should not be used to determine a patient’s suitability for chemotherapy,” wrote Nancy K. Gillis, PharmD, and colleagues (Lancet Oncol 2017; 18:112-21).
Risk factors examined
Dr. Takahashi and colleagues noted that previous studies have identified several treatment-related risk factors as being associated with therapy-related myeloid dysplasia or leukemia, including the use of alkylating agents, topoisomerase II inhibitors, and high-dose chemotherapy with autologous stem-cell transplantation.
“By contrast, little is known about patient-specific risk factors. Older age was shown to increase the risk of therapy-related myeloid neoplasms. Several germline polymorphisms have also been associated with this risk, but none have been validated. As such, no predictive biomarkers exist for therapy-related myeloid neoplasms,” they wrote.
They performed a retrospective case-control study comparing patients treated for a primary cancer at their center from 1997 through 2015 who subsequently developed a myeloid neoplasm with controls treated during the same period. Controls were age-matched patients treated with combination chemotherapy for lymphoma who did not develop a therapy-related myeloid malignancy after at least 5 years of follow-up.
In addition, the investigators further explored the association between clonal hematopoiesis and therapy-related cancers in an external cohort of patients with lymphoma treated in a randomized trial at their center from 1999 through 2001. That trial compared the CHOP regimen (cyclophosphamide, doxorubicin, vincristine and prednisone) with and without melatonin.
To detect clonal hematopoiesis in pre-treatment peripheral blood, the investigators used molecular barcode sequencing of 32 genes. They also used targeted gene sequencing on bone marrow samples from cases to investigate clonal evolution from clonal hematopoiesis to the development of therapy-related myeloid neoplasms.
As noted before, 10 of 14 cases had evidence of pre-treatment clonal hematopoiesis, compared with 17 of 54 controls. For both cases and controls, the cumulative incidence of therapy-related myeloid cancers after 5 years was significantly higher among those with baseline clonal hematopoiesis, at 30% vs. 7% for patients without it (P = .016).
Five of 74 patients in the external cohort (7%) went on to develop therapy-related myeloid neoplasms, and of this group, four (80%) had clonal hematopoiesis at baseline. In contrast, of the 69 patients who did not develop therapy-related cancers, 11 (16%) had baseline clonal hematopoiesis.
In a multivariate model using data from the external cohort, clonal hematopoiesis was significantly associated with risk for therapy-related myeloid neoplasms, with a hazard ratio of 13.7 (P = .013).
Elderly patient study
Dr. Gillis and her colleagues conducted a nested, case-control, proof-of-concept study to compare the prevalence of CHIP between patients with cancer who later developed therapy-related myeloid neoplasms (cases) and patients who did not (controls).
The cases were identified from an internal biobank of 123,357 patients, and included all patients who were diagnosed with a primary cancer, treated with chemotherapy, and subsequently developed a therapy-related myeloid neoplasm. The patients had to be 70 or older at the time of either primary or therapy-related cancer diagnosis with peripheral blood or mononuclear samples collected before the diagnosis of the second cancer.
Controls were patients diagnosed with a primary malignancy at age 70 or older who had chemotherapy but did not develop therapy-related myeloid neoplasms. Every case was matched with at least four controls selected for sex, primary tumor type, age at diagnosis, smoking status, chemotherapy drug class, and duration of follow up.
They used sequential targeted and whole-exome sequencing to assess clonal evolution in cases for whom paired CHIP and therapy-related myeloid neoplasm samples were available.
They identified a total of 13 cases and 56 controls. Among all patients, CHIP was seen in 23 (33%). In contrast, previous studies have shown a prevalence of CHIP among older patients without cancer of about 10%, the authors note in their article.
The prevalence of CHIP was significantly higher among cases than among controls, occurring in 8 of 13 cases (62%) vs 15 of 56 controls (27%; P = .024). The odds ratio for therapy-related neoplasms with CHIP was 5.75 (P = .013).
The most commonly mutated genes were TET2 and TP53 among cases, and TET2 among controls.
“The distribution of CHIP-related gene mutations differs between individuals with therapy-related myeloid neoplasm and those without, suggesting that mutation-specific differences might exist in therapy-related myeloid neoplasm risk,” the investigators write.
Dr. Takahashi’s study was supported by the Cancer Prevention Research Institute of Texas, Red and Charline McCombs Institute for the Early Detection and Treatment of Cancer, The National Institutes of Health through MD Anderson Cancer Center Support Grant, and the MD Anderson MDS & AML Moon Shots Program. Dr. Gillis’ study was internally funded. Dr. Takahasi and colleagues reported no competing financial interests. Two of Dr. Gillis’ colleagues reported grants or fees from several drug companies.
The real importance of the work reported by Gillis and colleagues and Takahashi and colleagues will come when therapies exist that can effectively eradicate nascent clonal hematopoiesis, thereby preventing therapy-related myeloid neoplasm evolution in at-risk patients.
Although high-intensity treatments, such as anthracycline-based induction chemotherapy, can eradicate myeloid clones, their effectiveness in clearing TP53-mutant cells is limited, and it is difficult to imagine intense approaches having a favorable risk–benefit balance in patients whose clonal hematopoiesis might never become a problem. Existing lower-intensity therapies for myeloid neoplasms such as DNA hypomethylating agents are not curative and often do not result in the reduction of VAF [variant allele frequencies] even when hematopoietic improvement occurs during therapy, so such agents would not be expected to eliminate pre-therapy-related myeloid neoplasm clones (although this hypothesis might still be worth testing, given that the emergence of therapy-related myeloid neoplasm could at least be delayed – even if not entirely prevented – with azacitidine or decitabine).
More promising are strategies that change the bone marrow microenvironment or break the immune tolerance of abnormal clones, although the use of these approaches for myeloid neoplasia is still in the very early stages. Although no method yet exists to reliably eliminate the preleukemic clones that can give rise to therapy-related myeloid neoplasms, identification of higher risk patients could still affect monitoring practices, such as the frequency of clinical assessments. Molecular genetic panels are expensive at present but are becoming less so. Because VAF assessment by next-generation sequencing is quantitative and proportional to clone size, serial assessment could identify patients whose mutant clones are large and expanding and who therefore warrant closer monitoring or enrollment in so-called preventive hematology trials.
David P. Steensma, MD, is with the Dana-Farber Cancer Institute, Harvard Medical School, Boston. His remarks were excerpted from an accompanying editorial.
The real importance of the work reported by Gillis and colleagues and Takahashi and colleagues will come when therapies exist that can effectively eradicate nascent clonal hematopoiesis, thereby preventing therapy-related myeloid neoplasm evolution in at-risk patients.
Although high-intensity treatments, such as anthracycline-based induction chemotherapy, can eradicate myeloid clones, their effectiveness in clearing TP53-mutant cells is limited, and it is difficult to imagine intense approaches having a favorable risk–benefit balance in patients whose clonal hematopoiesis might never become a problem. Existing lower-intensity therapies for myeloid neoplasms such as DNA hypomethylating agents are not curative and often do not result in the reduction of VAF [variant allele frequencies] even when hematopoietic improvement occurs during therapy, so such agents would not be expected to eliminate pre-therapy-related myeloid neoplasm clones (although this hypothesis might still be worth testing, given that the emergence of therapy-related myeloid neoplasm could at least be delayed – even if not entirely prevented – with azacitidine or decitabine).
More promising are strategies that change the bone marrow microenvironment or break the immune tolerance of abnormal clones, although the use of these approaches for myeloid neoplasia is still in the very early stages. Although no method yet exists to reliably eliminate the preleukemic clones that can give rise to therapy-related myeloid neoplasms, identification of higher risk patients could still affect monitoring practices, such as the frequency of clinical assessments. Molecular genetic panels are expensive at present but are becoming less so. Because VAF assessment by next-generation sequencing is quantitative and proportional to clone size, serial assessment could identify patients whose mutant clones are large and expanding and who therefore warrant closer monitoring or enrollment in so-called preventive hematology trials.
David P. Steensma, MD, is with the Dana-Farber Cancer Institute, Harvard Medical School, Boston. His remarks were excerpted from an accompanying editorial.
The real importance of the work reported by Gillis and colleagues and Takahashi and colleagues will come when therapies exist that can effectively eradicate nascent clonal hematopoiesis, thereby preventing therapy-related myeloid neoplasm evolution in at-risk patients.
Although high-intensity treatments, such as anthracycline-based induction chemotherapy, can eradicate myeloid clones, their effectiveness in clearing TP53-mutant cells is limited, and it is difficult to imagine intense approaches having a favorable risk–benefit balance in patients whose clonal hematopoiesis might never become a problem. Existing lower-intensity therapies for myeloid neoplasms such as DNA hypomethylating agents are not curative and often do not result in the reduction of VAF [variant allele frequencies] even when hematopoietic improvement occurs during therapy, so such agents would not be expected to eliminate pre-therapy-related myeloid neoplasm clones (although this hypothesis might still be worth testing, given that the emergence of therapy-related myeloid neoplasm could at least be delayed – even if not entirely prevented – with azacitidine or decitabine).
More promising are strategies that change the bone marrow microenvironment or break the immune tolerance of abnormal clones, although the use of these approaches for myeloid neoplasia is still in the very early stages. Although no method yet exists to reliably eliminate the preleukemic clones that can give rise to therapy-related myeloid neoplasms, identification of higher risk patients could still affect monitoring practices, such as the frequency of clinical assessments. Molecular genetic panels are expensive at present but are becoming less so. Because VAF assessment by next-generation sequencing is quantitative and proportional to clone size, serial assessment could identify patients whose mutant clones are large and expanding and who therefore warrant closer monitoring or enrollment in so-called preventive hematology trials.
David P. Steensma, MD, is with the Dana-Farber Cancer Institute, Harvard Medical School, Boston. His remarks were excerpted from an accompanying editorial.
Small pre-leukemic clones left behind after treatment for non-myeloid malignancies appear to increase the risk for therapy-related myelodysplasia or leukemia, report investigators in two studies.
An analysis of peripheral blood samples taken from patients at the time of their primary cancer diagnosis and bone marrow samples taken at the time of a later therapy-related myeloid neoplasm diagnosis showed that 10 of 14 patients (71%) had clonal hematopoiesis before starting on cytotoxic chemotherapy. In contrast, clonal hematopoiesis was detected in pre-treatment samples of only 17 of 54 controls (31%), reported Koichi Takahashi, MD, and colleagues from the University of Texas MD Anderson Cancer Center in Houston.
“Preleukemic clonal hematopoiesis is common in patients with therapy-related myeloid neoplasms at the time of their primary cancer diagnosis and before they have been exposed to treatment. Our results suggest that clonal hematopoiesis could be used as a predictive marker to identify patients with cancer who are at risk of developing therapy-related myeloid neoplasms,” they wrote (Lancet Oncol 2017; 18: 100–11).
In a separate study, investigators from the Moffitt Cancer Center in Tampa, Florida, found in a nested case-control study that patients with therapy-related myeloid neoplasms were more likely than controls to have clonal hematopoiesis of indeterminate potential (CHIP), and that the CHIP was often present before exposure to chemotherapy.
“We recorded a significantly higher prevalence of CHIP in individuals who developed therapy-related myeloid neoplasms (cases) than in those who did not (controls); however, around 27% of individuals with CHIP did not develop therapy-related myeloid neoplasms, suggesting that this feature alone should not be used to determine a patient’s suitability for chemotherapy,” wrote Nancy K. Gillis, PharmD, and colleagues (Lancet Oncol 2017; 18:112-21).
Risk factors examined
Dr. Takahashi and colleagues noted that previous studies have identified several treatment-related risk factors as being associated with therapy-related myeloid dysplasia or leukemia, including the use of alkylating agents, topoisomerase II inhibitors, and high-dose chemotherapy with autologous stem-cell transplantation.
“By contrast, little is known about patient-specific risk factors. Older age was shown to increase the risk of therapy-related myeloid neoplasms. Several germline polymorphisms have also been associated with this risk, but none have been validated. As such, no predictive biomarkers exist for therapy-related myeloid neoplasms,” they wrote.
They performed a retrospective case-control study comparing patients treated for a primary cancer at their center from 1997 through 2015 who subsequently developed a myeloid neoplasm with controls treated during the same period. Controls were age-matched patients treated with combination chemotherapy for lymphoma who did not develop a therapy-related myeloid malignancy after at least 5 years of follow-up.
In addition, the investigators further explored the association between clonal hematopoiesis and therapy-related cancers in an external cohort of patients with lymphoma treated in a randomized trial at their center from 1999 through 2001. That trial compared the CHOP regimen (cyclophosphamide, doxorubicin, vincristine and prednisone) with and without melatonin.
To detect clonal hematopoiesis in pre-treatment peripheral blood, the investigators used molecular barcode sequencing of 32 genes. They also used targeted gene sequencing on bone marrow samples from cases to investigate clonal evolution from clonal hematopoiesis to the development of therapy-related myeloid neoplasms.
As noted before, 10 of 14 cases had evidence of pre-treatment clonal hematopoiesis, compared with 17 of 54 controls. For both cases and controls, the cumulative incidence of therapy-related myeloid cancers after 5 years was significantly higher among those with baseline clonal hematopoiesis, at 30% vs. 7% for patients without it (P = .016).
Five of 74 patients in the external cohort (7%) went on to develop therapy-related myeloid neoplasms, and of this group, four (80%) had clonal hematopoiesis at baseline. In contrast, of the 69 patients who did not develop therapy-related cancers, 11 (16%) had baseline clonal hematopoiesis.
In a multivariate model using data from the external cohort, clonal hematopoiesis was significantly associated with risk for therapy-related myeloid neoplasms, with a hazard ratio of 13.7 (P = .013).
Elderly patient study
Dr. Gillis and her colleagues conducted a nested, case-control, proof-of-concept study to compare the prevalence of CHIP between patients with cancer who later developed therapy-related myeloid neoplasms (cases) and patients who did not (controls).
The cases were identified from an internal biobank of 123,357 patients, and included all patients who were diagnosed with a primary cancer, treated with chemotherapy, and subsequently developed a therapy-related myeloid neoplasm. The patients had to be 70 or older at the time of either primary or therapy-related cancer diagnosis with peripheral blood or mononuclear samples collected before the diagnosis of the second cancer.
Controls were patients diagnosed with a primary malignancy at age 70 or older who had chemotherapy but did not develop therapy-related myeloid neoplasms. Every case was matched with at least four controls selected for sex, primary tumor type, age at diagnosis, smoking status, chemotherapy drug class, and duration of follow up.
They used sequential targeted and whole-exome sequencing to assess clonal evolution in cases for whom paired CHIP and therapy-related myeloid neoplasm samples were available.
They identified a total of 13 cases and 56 controls. Among all patients, CHIP was seen in 23 (33%). In contrast, previous studies have shown a prevalence of CHIP among older patients without cancer of about 10%, the authors note in their article.
The prevalence of CHIP was significantly higher among cases than among controls, occurring in 8 of 13 cases (62%) vs 15 of 56 controls (27%; P = .024). The odds ratio for therapy-related neoplasms with CHIP was 5.75 (P = .013).
The most commonly mutated genes were TET2 and TP53 among cases, and TET2 among controls.
“The distribution of CHIP-related gene mutations differs between individuals with therapy-related myeloid neoplasm and those without, suggesting that mutation-specific differences might exist in therapy-related myeloid neoplasm risk,” the investigators write.
Dr. Takahashi’s study was supported by the Cancer Prevention Research Institute of Texas, Red and Charline McCombs Institute for the Early Detection and Treatment of Cancer, The National Institutes of Health through MD Anderson Cancer Center Support Grant, and the MD Anderson MDS & AML Moon Shots Program. Dr. Gillis’ study was internally funded. Dr. Takahasi and colleagues reported no competing financial interests. Two of Dr. Gillis’ colleagues reported grants or fees from several drug companies.
Small pre-leukemic clones left behind after treatment for non-myeloid malignancies appear to increase the risk for therapy-related myelodysplasia or leukemia, report investigators in two studies.
An analysis of peripheral blood samples taken from patients at the time of their primary cancer diagnosis and bone marrow samples taken at the time of a later therapy-related myeloid neoplasm diagnosis showed that 10 of 14 patients (71%) had clonal hematopoiesis before starting on cytotoxic chemotherapy. In contrast, clonal hematopoiesis was detected in pre-treatment samples of only 17 of 54 controls (31%), reported Koichi Takahashi, MD, and colleagues from the University of Texas MD Anderson Cancer Center in Houston.
“Preleukemic clonal hematopoiesis is common in patients with therapy-related myeloid neoplasms at the time of their primary cancer diagnosis and before they have been exposed to treatment. Our results suggest that clonal hematopoiesis could be used as a predictive marker to identify patients with cancer who are at risk of developing therapy-related myeloid neoplasms,” they wrote (Lancet Oncol 2017; 18: 100–11).
In a separate study, investigators from the Moffitt Cancer Center in Tampa, Florida, found in a nested case-control study that patients with therapy-related myeloid neoplasms were more likely than controls to have clonal hematopoiesis of indeterminate potential (CHIP), and that the CHIP was often present before exposure to chemotherapy.
“We recorded a significantly higher prevalence of CHIP in individuals who developed therapy-related myeloid neoplasms (cases) than in those who did not (controls); however, around 27% of individuals with CHIP did not develop therapy-related myeloid neoplasms, suggesting that this feature alone should not be used to determine a patient’s suitability for chemotherapy,” wrote Nancy K. Gillis, PharmD, and colleagues (Lancet Oncol 2017; 18:112-21).
Risk factors examined
Dr. Takahashi and colleagues noted that previous studies have identified several treatment-related risk factors as being associated with therapy-related myeloid dysplasia or leukemia, including the use of alkylating agents, topoisomerase II inhibitors, and high-dose chemotherapy with autologous stem-cell transplantation.
“By contrast, little is known about patient-specific risk factors. Older age was shown to increase the risk of therapy-related myeloid neoplasms. Several germline polymorphisms have also been associated with this risk, but none have been validated. As such, no predictive biomarkers exist for therapy-related myeloid neoplasms,” they wrote.
They performed a retrospective case-control study comparing patients treated for a primary cancer at their center from 1997 through 2015 who subsequently developed a myeloid neoplasm with controls treated during the same period. Controls were age-matched patients treated with combination chemotherapy for lymphoma who did not develop a therapy-related myeloid malignancy after at least 5 years of follow-up.
In addition, the investigators further explored the association between clonal hematopoiesis and therapy-related cancers in an external cohort of patients with lymphoma treated in a randomized trial at their center from 1999 through 2001. That trial compared the CHOP regimen (cyclophosphamide, doxorubicin, vincristine and prednisone) with and without melatonin.
To detect clonal hematopoiesis in pre-treatment peripheral blood, the investigators used molecular barcode sequencing of 32 genes. They also used targeted gene sequencing on bone marrow samples from cases to investigate clonal evolution from clonal hematopoiesis to the development of therapy-related myeloid neoplasms.
As noted before, 10 of 14 cases had evidence of pre-treatment clonal hematopoiesis, compared with 17 of 54 controls. For both cases and controls, the cumulative incidence of therapy-related myeloid cancers after 5 years was significantly higher among those with baseline clonal hematopoiesis, at 30% vs. 7% for patients without it (P = .016).
Five of 74 patients in the external cohort (7%) went on to develop therapy-related myeloid neoplasms, and of this group, four (80%) had clonal hematopoiesis at baseline. In contrast, of the 69 patients who did not develop therapy-related cancers, 11 (16%) had baseline clonal hematopoiesis.
In a multivariate model using data from the external cohort, clonal hematopoiesis was significantly associated with risk for therapy-related myeloid neoplasms, with a hazard ratio of 13.7 (P = .013).
Elderly patient study
Dr. Gillis and her colleagues conducted a nested, case-control, proof-of-concept study to compare the prevalence of CHIP between patients with cancer who later developed therapy-related myeloid neoplasms (cases) and patients who did not (controls).
The cases were identified from an internal biobank of 123,357 patients, and included all patients who were diagnosed with a primary cancer, treated with chemotherapy, and subsequently developed a therapy-related myeloid neoplasm. The patients had to be 70 or older at the time of either primary or therapy-related cancer diagnosis with peripheral blood or mononuclear samples collected before the diagnosis of the second cancer.
Controls were patients diagnosed with a primary malignancy at age 70 or older who had chemotherapy but did not develop therapy-related myeloid neoplasms. Every case was matched with at least four controls selected for sex, primary tumor type, age at diagnosis, smoking status, chemotherapy drug class, and duration of follow up.
They used sequential targeted and whole-exome sequencing to assess clonal evolution in cases for whom paired CHIP and therapy-related myeloid neoplasm samples were available.
They identified a total of 13 cases and 56 controls. Among all patients, CHIP was seen in 23 (33%). In contrast, previous studies have shown a prevalence of CHIP among older patients without cancer of about 10%, the authors note in their article.
The prevalence of CHIP was significantly higher among cases than among controls, occurring in 8 of 13 cases (62%) vs 15 of 56 controls (27%; P = .024). The odds ratio for therapy-related neoplasms with CHIP was 5.75 (P = .013).
The most commonly mutated genes were TET2 and TP53 among cases, and TET2 among controls.
“The distribution of CHIP-related gene mutations differs between individuals with therapy-related myeloid neoplasm and those without, suggesting that mutation-specific differences might exist in therapy-related myeloid neoplasm risk,” the investigators write.
Dr. Takahashi’s study was supported by the Cancer Prevention Research Institute of Texas, Red and Charline McCombs Institute for the Early Detection and Treatment of Cancer, The National Institutes of Health through MD Anderson Cancer Center Support Grant, and the MD Anderson MDS & AML Moon Shots Program. Dr. Gillis’ study was internally funded. Dr. Takahasi and colleagues reported no competing financial interests. Two of Dr. Gillis’ colleagues reported grants or fees from several drug companies.
FROM LANCET ONCOLOGY
Key clinical point: Pre-therapy clonal hematopoiesis is associated with increased risk for therapy-related myeloid neoplasms.
Major finding: In two studies, the incidence of therapy-related myeloid neoplasms was higher among patients with clonal hematopoiesis at baseline.
Data source: Retrospective case-control studies.
Disclosures: Dr. Takahashi’s study was supported by the Cancer Prevention Research Institute of Texas, Red and Charline McCombs Institute for the Early Detection and Treatment of Cancer, The National Institutes of Health through MD Anderson Cancer Center Support Grant, and the MD Anderson MDS & AML Moon Shots Program. Dr. Gillis’ study was internally funded. Dr. Takahasi and colleagues reported no competing financial interests. Two of Dr. Gillis’ colleagues reported grants or fees from several drug companies.
New report highlights gaps in knowledge on marijuana use
A new report by the National Academies of Sciences, Engineering and Medicine shines a light on what the existing literature says about the perceived health benefits and dangers of using cannabis and cannabinoids.
“What little we know for certain about the effects of marijuana on human health — and all that we have reason to suspect — justifies serious national concern,” wrote the authors of the report, the evidence and research review of which was chaired by Marie McCormick, MD, of Harvard University in Boston. “The committee’s major recommendation called for an intensification and more comprehensive research effort into the effects of marijuana on the health of the American people.”
The authors concluded current literature shows substantial evidence stating that cannabis is effective at managing chronic pain in adults, while oral cannabinoid use is effective in mitigating nausea or vomiting induced by chemotherapy and improving patient-reported spasticity in patients with multiple sclerosis. Additionally, cannabinoids – specifically, nabiximols – are moderately effective in the short term for improving sleep disturbances brought on by obstructive sleep apnea syndrome, fibromyalgia, chronic pain, and multiple sclerosis.
However, there is limited evidence to support cannabis or cannabinoid use for reducing weight loss or inducing appetite in HIV/AIDS patients, improving clinician-measured spasicity or Tourette syndrome symptoms, reducing anxiety, improving symptoms brought on by post-traumatic stress, and improving outcomes in patients who have suffered traumatic brain injury or intracranial hemorrhage.
Additionally, there is no evidence to support the use of cannabis or cannabinoids in treating cancers or cancer-related anorexia, irritable bowel syndrome symptoms, epilepsy, spinal cord-related spasticity, symptoms of amyotrophic lateral sclerosis, Huntington’s disease, Parkinson’s disease, schizophrenia, and dystonia.
“Present data on drug use progression neither support nor refute the suggestion that medical availability would increase drug abuse,” the authors noted. “However, this question is beyond the issues normally considered for medical uses of drugs and should not be a factor in evaluating the therapeutic potential of marijuana or cannabinoids.”
From a mental health standpoint, suicidal thoughts were found to be more likely in individuals who frequently used cannabis or cannabinoids. Symptoms like depression and anxiety are also more likely in those who smoke marijuana and have bipolar disorder. There is also “limited evidence of a statistical association between sustained abstinence from cannabis use [and] impairments in the cognitive domains of learning, memory, and attention.”
Among the other significant findings of the report, children who live in states where marijuana has been legalized are significantly more likely to ingest cannabis or cannabinoids; so far, marijuana use in some form – either recreational or medical – has been approved in 28 states and Washington, DC. Furthermore, adolescents who use marijuana are more likely to experience difficulties in social and educational development. And individuals of any age who smoke marijuana and drive are more likely to be involved in a car accident.
Also noteworthy is the lack of evidence pointing to marijuana use causing cancer. While chronic marijuana smoking was found to be linked to bronchitis, it was not found to cause cancers that are most commonly associated with chronic smoking of tobacco.
“This report highlights that there are critical gaps in our understanding of the health effects of cannabis,” explained John H. Krystal, MD, of Yale University in New Haven, Connecticut.
A reviewer of the report, Dr. Krystal elaborated on the gaps that exist in the current literature, saying “One reason for these gaps has been regulatory and practical challenges facing those who attempted to conduct this research. For example, what supply of cannabis should they use? Where, in the typical hospital settings where research is conducted, should patients participating in research be permitted to smoke cannabis? What standards should the institutional review committees employ when evaluating studies that involve the administration of cannabis or other cannabinoids?”
Ultimately, Dr. Krystal stated, “what should be evident from this summary is that only a few of the many publicized clinical applications for cannabis are adequately supported by acceptable research standards for determining safety or efficacy.” Specifically, states that have approved cannabis use for managing PTSD symptoms are doing so based off “meager” evidence, and in some cases, are circumventing FDA regulatory processes in a way. This could not only compromise patient care, but muddy the waters for physicians who want to treat their patients safely while also following legal avenues.
“Physicians may face a tension between their roles as physicians [and] their wish to provide a legal path for access to cannabinoids for their patients,” Dr. Krystal said, adding that “the endorsement of particular cannabis prescription practices by the states, even for clinical indications where cannabis has not been shown to be safe and effective, may create pressure for physicians to engage in ineffective or unsafe cannabis prescription practices.”
Ultimately, the report underlines areas of need in terms of understanding and effectively using cannabis and cannabinoid in treating patients. Calling the report a “call to arms” for those in the health care – and, specifically, the public health – arena, Dr. Krystal added that he hopes the findings of the report will be used for educating “legislators, physicians, and consumers [about the] potential benefits and risks of cannabis and thereby help to guide both legislation, clinical practice, and perhaps recreational use.”
A new report by the National Academies of Sciences, Engineering and Medicine shines a light on what the existing literature says about the perceived health benefits and dangers of using cannabis and cannabinoids.
“What little we know for certain about the effects of marijuana on human health — and all that we have reason to suspect — justifies serious national concern,” wrote the authors of the report, the evidence and research review of which was chaired by Marie McCormick, MD, of Harvard University in Boston. “The committee’s major recommendation called for an intensification and more comprehensive research effort into the effects of marijuana on the health of the American people.”
The authors concluded current literature shows substantial evidence stating that cannabis is effective at managing chronic pain in adults, while oral cannabinoid use is effective in mitigating nausea or vomiting induced by chemotherapy and improving patient-reported spasticity in patients with multiple sclerosis. Additionally, cannabinoids – specifically, nabiximols – are moderately effective in the short term for improving sleep disturbances brought on by obstructive sleep apnea syndrome, fibromyalgia, chronic pain, and multiple sclerosis.
However, there is limited evidence to support cannabis or cannabinoid use for reducing weight loss or inducing appetite in HIV/AIDS patients, improving clinician-measured spasicity or Tourette syndrome symptoms, reducing anxiety, improving symptoms brought on by post-traumatic stress, and improving outcomes in patients who have suffered traumatic brain injury or intracranial hemorrhage.
Additionally, there is no evidence to support the use of cannabis or cannabinoids in treating cancers or cancer-related anorexia, irritable bowel syndrome symptoms, epilepsy, spinal cord-related spasticity, symptoms of amyotrophic lateral sclerosis, Huntington’s disease, Parkinson’s disease, schizophrenia, and dystonia.
“Present data on drug use progression neither support nor refute the suggestion that medical availability would increase drug abuse,” the authors noted. “However, this question is beyond the issues normally considered for medical uses of drugs and should not be a factor in evaluating the therapeutic potential of marijuana or cannabinoids.”
From a mental health standpoint, suicidal thoughts were found to be more likely in individuals who frequently used cannabis or cannabinoids. Symptoms like depression and anxiety are also more likely in those who smoke marijuana and have bipolar disorder. There is also “limited evidence of a statistical association between sustained abstinence from cannabis use [and] impairments in the cognitive domains of learning, memory, and attention.”
Among the other significant findings of the report, children who live in states where marijuana has been legalized are significantly more likely to ingest cannabis or cannabinoids; so far, marijuana use in some form – either recreational or medical – has been approved in 28 states and Washington, DC. Furthermore, adolescents who use marijuana are more likely to experience difficulties in social and educational development. And individuals of any age who smoke marijuana and drive are more likely to be involved in a car accident.
Also noteworthy is the lack of evidence pointing to marijuana use causing cancer. While chronic marijuana smoking was found to be linked to bronchitis, it was not found to cause cancers that are most commonly associated with chronic smoking of tobacco.
“This report highlights that there are critical gaps in our understanding of the health effects of cannabis,” explained John H. Krystal, MD, of Yale University in New Haven, Connecticut.
A reviewer of the report, Dr. Krystal elaborated on the gaps that exist in the current literature, saying “One reason for these gaps has been regulatory and practical challenges facing those who attempted to conduct this research. For example, what supply of cannabis should they use? Where, in the typical hospital settings where research is conducted, should patients participating in research be permitted to smoke cannabis? What standards should the institutional review committees employ when evaluating studies that involve the administration of cannabis or other cannabinoids?”
Ultimately, Dr. Krystal stated, “what should be evident from this summary is that only a few of the many publicized clinical applications for cannabis are adequately supported by acceptable research standards for determining safety or efficacy.” Specifically, states that have approved cannabis use for managing PTSD symptoms are doing so based off “meager” evidence, and in some cases, are circumventing FDA regulatory processes in a way. This could not only compromise patient care, but muddy the waters for physicians who want to treat their patients safely while also following legal avenues.
“Physicians may face a tension between their roles as physicians [and] their wish to provide a legal path for access to cannabinoids for their patients,” Dr. Krystal said, adding that “the endorsement of particular cannabis prescription practices by the states, even for clinical indications where cannabis has not been shown to be safe and effective, may create pressure for physicians to engage in ineffective or unsafe cannabis prescription practices.”
Ultimately, the report underlines areas of need in terms of understanding and effectively using cannabis and cannabinoid in treating patients. Calling the report a “call to arms” for those in the health care – and, specifically, the public health – arena, Dr. Krystal added that he hopes the findings of the report will be used for educating “legislators, physicians, and consumers [about the] potential benefits and risks of cannabis and thereby help to guide both legislation, clinical practice, and perhaps recreational use.”
A new report by the National Academies of Sciences, Engineering and Medicine shines a light on what the existing literature says about the perceived health benefits and dangers of using cannabis and cannabinoids.
“What little we know for certain about the effects of marijuana on human health — and all that we have reason to suspect — justifies serious national concern,” wrote the authors of the report, the evidence and research review of which was chaired by Marie McCormick, MD, of Harvard University in Boston. “The committee’s major recommendation called for an intensification and more comprehensive research effort into the effects of marijuana on the health of the American people.”
The authors concluded current literature shows substantial evidence stating that cannabis is effective at managing chronic pain in adults, while oral cannabinoid use is effective in mitigating nausea or vomiting induced by chemotherapy and improving patient-reported spasticity in patients with multiple sclerosis. Additionally, cannabinoids – specifically, nabiximols – are moderately effective in the short term for improving sleep disturbances brought on by obstructive sleep apnea syndrome, fibromyalgia, chronic pain, and multiple sclerosis.
However, there is limited evidence to support cannabis or cannabinoid use for reducing weight loss or inducing appetite in HIV/AIDS patients, improving clinician-measured spasicity or Tourette syndrome symptoms, reducing anxiety, improving symptoms brought on by post-traumatic stress, and improving outcomes in patients who have suffered traumatic brain injury or intracranial hemorrhage.
Additionally, there is no evidence to support the use of cannabis or cannabinoids in treating cancers or cancer-related anorexia, irritable bowel syndrome symptoms, epilepsy, spinal cord-related spasticity, symptoms of amyotrophic lateral sclerosis, Huntington’s disease, Parkinson’s disease, schizophrenia, and dystonia.
“Present data on drug use progression neither support nor refute the suggestion that medical availability would increase drug abuse,” the authors noted. “However, this question is beyond the issues normally considered for medical uses of drugs and should not be a factor in evaluating the therapeutic potential of marijuana or cannabinoids.”
From a mental health standpoint, suicidal thoughts were found to be more likely in individuals who frequently used cannabis or cannabinoids. Symptoms like depression and anxiety are also more likely in those who smoke marijuana and have bipolar disorder. There is also “limited evidence of a statistical association between sustained abstinence from cannabis use [and] impairments in the cognitive domains of learning, memory, and attention.”
Among the other significant findings of the report, children who live in states where marijuana has been legalized are significantly more likely to ingest cannabis or cannabinoids; so far, marijuana use in some form – either recreational or medical – has been approved in 28 states and Washington, DC. Furthermore, adolescents who use marijuana are more likely to experience difficulties in social and educational development. And individuals of any age who smoke marijuana and drive are more likely to be involved in a car accident.
Also noteworthy is the lack of evidence pointing to marijuana use causing cancer. While chronic marijuana smoking was found to be linked to bronchitis, it was not found to cause cancers that are most commonly associated with chronic smoking of tobacco.
“This report highlights that there are critical gaps in our understanding of the health effects of cannabis,” explained John H. Krystal, MD, of Yale University in New Haven, Connecticut.
A reviewer of the report, Dr. Krystal elaborated on the gaps that exist in the current literature, saying “One reason for these gaps has been regulatory and practical challenges facing those who attempted to conduct this research. For example, what supply of cannabis should they use? Where, in the typical hospital settings where research is conducted, should patients participating in research be permitted to smoke cannabis? What standards should the institutional review committees employ when evaluating studies that involve the administration of cannabis or other cannabinoids?”
Ultimately, Dr. Krystal stated, “what should be evident from this summary is that only a few of the many publicized clinical applications for cannabis are adequately supported by acceptable research standards for determining safety or efficacy.” Specifically, states that have approved cannabis use for managing PTSD symptoms are doing so based off “meager” evidence, and in some cases, are circumventing FDA regulatory processes in a way. This could not only compromise patient care, but muddy the waters for physicians who want to treat their patients safely while also following legal avenues.
“Physicians may face a tension between their roles as physicians [and] their wish to provide a legal path for access to cannabinoids for their patients,” Dr. Krystal said, adding that “the endorsement of particular cannabis prescription practices by the states, even for clinical indications where cannabis has not been shown to be safe and effective, may create pressure for physicians to engage in ineffective or unsafe cannabis prescription practices.”
Ultimately, the report underlines areas of need in terms of understanding and effectively using cannabis and cannabinoid in treating patients. Calling the report a “call to arms” for those in the health care – and, specifically, the public health – arena, Dr. Krystal added that he hopes the findings of the report will be used for educating “legislators, physicians, and consumers [about the] potential benefits and risks of cannabis and thereby help to guide both legislation, clinical practice, and perhaps recreational use.”
FROM THE NATIONAL ACADEMIES OF SCIENCES, ENGINEERING AND MEDICINE
Left ventricle dose predicts heart events after BC radiation
The risk of acute coronary events following radiotherapy for breast cancer is better predicted by the volume of the left ventricle that received 5 Gy than by the mean dose of radiation to the heart, according to a Dutch investigation of 910 women who underwent radiation treatment following breast-conserving surgery.
The finding follows up a 2013 report that found that the risk of acute coronary events (ACE) after breast cancer (BC) radiation could be predicted by the mean radiation heart dose (MHD), the presence of cardiac risk factors, and age (N Engl J Med. 2013 Mar 14;368[11]:987-98. doi: 0.1056/NEJMoa1209825).
The new study validated those findings, but also found that risk prediction was better when mean heart dose (MHD) was replaced by the volume of the left ventricle receiving 5 Gy (LV-V5); the substitution improved the c-statistic to 0.80 (95% confidence interval, 0.72-0.88). Using a weighted ACE risk score based on baseline diabetes, hypertension, and ischemic event history – instead of the risk factor yes-or-no approach from 2013 – further improved predictive power, with a c-statistic of 0.83 (95% CI, 0.75-0.91). Anything over a c-statistic of 0.8 is considered strong; 0.5 is chance, 1.0 is perfect prediction.
For instance, a 70-year-old woman with an LV-V5 of 50% and no cardiac risk factors had an excess ACE risk in the new system of 2.52% within 9 years of radiotherapy (RT). If she had a history of ischemic heart disease, the excess risk increased to 8.42%, the investigators said (J Clin Oncol. 2017 Jan 17. doi: 10.1200/JCO.2016.69.8480).
“Model performance was significantly improved by replacing MHD with LV-V5 and using the weighted ACE risk score.” However, “because we were not able to externally validate the LV-V5 model, this model” requires validation “before it can be used in routine clinical practice,” said investigators, led by Veerle van den Bogaard, MD, of the University of Groningen, the Netherlands.
The women were a median of 59 years old, and they were followed for a median of 7.6 years, with a range of 0.1-10.1 years. Radiation dose information was derived from CT planning scans. The median MHD was 2.37 Gy.
Thirty patients (3.3%) had an ACE, defined as myocardial infarction, coronary revascularization, or death due to ischemic heart disease; 17 had events in the first 5 years. The 5- and 9-year cumulative ACE incidences were 1.9% and 3.9%. Ten of the 30 women died from their cardiac complication.
The model predicted a cumulative ACE incidence at 9 years of 3.5%, which was in line with the observed rate of 3.9%. The excess cumulative risk related to RT was 1.13%. Overall, about 10 patients had an ACE that could be attributed to RT. The cumulative incidence of ACE increased by 16.5% per Gy (95% CI, 0.6-35.0; P = .042). The findings were consistent with the 2013 study.
ACE incidence was not significantly associated with the maximum dose of radiation to the heart.
LV-V5 was the most important prognostic dose-volume parameter associated with the cumulative incidence of ACE, with a hazard ratio of 1.016 (95% CI, 1.002-1.030; P = .016). “Because of this strong association, we chose to include LV-V5 in the model,” the investigators said.
There was no external funding. The lead investigator had no disclosures, but two authors reported institutional research funding from Philips, Roche, and other companies. One was an advisor and speaker for IBA.
The limitations of this study are substantial. As the authors note, their work was based on only a small number of events, and their length of follow-up prevented them from being able to examine risk in the period of 10 years and beyond.
Also, the likelihood is high that the risk of radiation-induced heart disease can be reduced below that seen in the study. Cardiac exposure in many recent studies has been lower. Techniques such as deep inspiration breath holding or treatment in the prone position often can further decrease this exposure. Several randomized trials comparing partial-breast with whole-breast irradiation have found equal local control rates with both approaches, strongly suggesting that judicious individualization of field borders and cardiac blocks are unlikely to compromise outcome for selected patients treated with partial mastectomy.
Nonetheless, at some point, compromising coverage of the breast, chest wall, or nodal target volumes because an arbitrary threshold of a cardiac dose-volume parameter has been exceeded may be dangerous. Computer programs can likely be created to perform calculations of an individual’s excess risk of cardiac events or death in relation to dose-volume and clinical parameters, although I suspect it will be some years before they provide sufficiently validated, narrow estimates of risk to be clinically useful. Perhaps by then we will also have better ways to explain such sobering decisions to patients.
Abram Recht, MD , is a professor of radiation oncology at Harvard Medical School, Boston. He is also an advisor for CareCore and US Oncology, and receives institutional research funding form Genomic Health. He made his comments in an editorial (J Clin Oncol. 2017 Jan 17. doi: 0.1200/JCO.2016.71.4113 ).
The limitations of this study are substantial. As the authors note, their work was based on only a small number of events, and their length of follow-up prevented them from being able to examine risk in the period of 10 years and beyond.
Also, the likelihood is high that the risk of radiation-induced heart disease can be reduced below that seen in the study. Cardiac exposure in many recent studies has been lower. Techniques such as deep inspiration breath holding or treatment in the prone position often can further decrease this exposure. Several randomized trials comparing partial-breast with whole-breast irradiation have found equal local control rates with both approaches, strongly suggesting that judicious individualization of field borders and cardiac blocks are unlikely to compromise outcome for selected patients treated with partial mastectomy.
Nonetheless, at some point, compromising coverage of the breast, chest wall, or nodal target volumes because an arbitrary threshold of a cardiac dose-volume parameter has been exceeded may be dangerous. Computer programs can likely be created to perform calculations of an individual’s excess risk of cardiac events or death in relation to dose-volume and clinical parameters, although I suspect it will be some years before they provide sufficiently validated, narrow estimates of risk to be clinically useful. Perhaps by then we will also have better ways to explain such sobering decisions to patients.
Abram Recht, MD , is a professor of radiation oncology at Harvard Medical School, Boston. He is also an advisor for CareCore and US Oncology, and receives institutional research funding form Genomic Health. He made his comments in an editorial (J Clin Oncol. 2017 Jan 17. doi: 0.1200/JCO.2016.71.4113 ).
The limitations of this study are substantial. As the authors note, their work was based on only a small number of events, and their length of follow-up prevented them from being able to examine risk in the period of 10 years and beyond.
Also, the likelihood is high that the risk of radiation-induced heart disease can be reduced below that seen in the study. Cardiac exposure in many recent studies has been lower. Techniques such as deep inspiration breath holding or treatment in the prone position often can further decrease this exposure. Several randomized trials comparing partial-breast with whole-breast irradiation have found equal local control rates with both approaches, strongly suggesting that judicious individualization of field borders and cardiac blocks are unlikely to compromise outcome for selected patients treated with partial mastectomy.
Nonetheless, at some point, compromising coverage of the breast, chest wall, or nodal target volumes because an arbitrary threshold of a cardiac dose-volume parameter has been exceeded may be dangerous. Computer programs can likely be created to perform calculations of an individual’s excess risk of cardiac events or death in relation to dose-volume and clinical parameters, although I suspect it will be some years before they provide sufficiently validated, narrow estimates of risk to be clinically useful. Perhaps by then we will also have better ways to explain such sobering decisions to patients.
Abram Recht, MD , is a professor of radiation oncology at Harvard Medical School, Boston. He is also an advisor for CareCore and US Oncology, and receives institutional research funding form Genomic Health. He made his comments in an editorial (J Clin Oncol. 2017 Jan 17. doi: 0.1200/JCO.2016.71.4113 ).
The risk of acute coronary events following radiotherapy for breast cancer is better predicted by the volume of the left ventricle that received 5 Gy than by the mean dose of radiation to the heart, according to a Dutch investigation of 910 women who underwent radiation treatment following breast-conserving surgery.
The finding follows up a 2013 report that found that the risk of acute coronary events (ACE) after breast cancer (BC) radiation could be predicted by the mean radiation heart dose (MHD), the presence of cardiac risk factors, and age (N Engl J Med. 2013 Mar 14;368[11]:987-98. doi: 0.1056/NEJMoa1209825).
The new study validated those findings, but also found that risk prediction was better when mean heart dose (MHD) was replaced by the volume of the left ventricle receiving 5 Gy (LV-V5); the substitution improved the c-statistic to 0.80 (95% confidence interval, 0.72-0.88). Using a weighted ACE risk score based on baseline diabetes, hypertension, and ischemic event history – instead of the risk factor yes-or-no approach from 2013 – further improved predictive power, with a c-statistic of 0.83 (95% CI, 0.75-0.91). Anything over a c-statistic of 0.8 is considered strong; 0.5 is chance, 1.0 is perfect prediction.
For instance, a 70-year-old woman with an LV-V5 of 50% and no cardiac risk factors had an excess ACE risk in the new system of 2.52% within 9 years of radiotherapy (RT). If she had a history of ischemic heart disease, the excess risk increased to 8.42%, the investigators said (J Clin Oncol. 2017 Jan 17. doi: 10.1200/JCO.2016.69.8480).
“Model performance was significantly improved by replacing MHD with LV-V5 and using the weighted ACE risk score.” However, “because we were not able to externally validate the LV-V5 model, this model” requires validation “before it can be used in routine clinical practice,” said investigators, led by Veerle van den Bogaard, MD, of the University of Groningen, the Netherlands.
The women were a median of 59 years old, and they were followed for a median of 7.6 years, with a range of 0.1-10.1 years. Radiation dose information was derived from CT planning scans. The median MHD was 2.37 Gy.
Thirty patients (3.3%) had an ACE, defined as myocardial infarction, coronary revascularization, or death due to ischemic heart disease; 17 had events in the first 5 years. The 5- and 9-year cumulative ACE incidences were 1.9% and 3.9%. Ten of the 30 women died from their cardiac complication.
The model predicted a cumulative ACE incidence at 9 years of 3.5%, which was in line with the observed rate of 3.9%. The excess cumulative risk related to RT was 1.13%. Overall, about 10 patients had an ACE that could be attributed to RT. The cumulative incidence of ACE increased by 16.5% per Gy (95% CI, 0.6-35.0; P = .042). The findings were consistent with the 2013 study.
ACE incidence was not significantly associated with the maximum dose of radiation to the heart.
LV-V5 was the most important prognostic dose-volume parameter associated with the cumulative incidence of ACE, with a hazard ratio of 1.016 (95% CI, 1.002-1.030; P = .016). “Because of this strong association, we chose to include LV-V5 in the model,” the investigators said.
There was no external funding. The lead investigator had no disclosures, but two authors reported institutional research funding from Philips, Roche, and other companies. One was an advisor and speaker for IBA.
The risk of acute coronary events following radiotherapy for breast cancer is better predicted by the volume of the left ventricle that received 5 Gy than by the mean dose of radiation to the heart, according to a Dutch investigation of 910 women who underwent radiation treatment following breast-conserving surgery.
The finding follows up a 2013 report that found that the risk of acute coronary events (ACE) after breast cancer (BC) radiation could be predicted by the mean radiation heart dose (MHD), the presence of cardiac risk factors, and age (N Engl J Med. 2013 Mar 14;368[11]:987-98. doi: 0.1056/NEJMoa1209825).
The new study validated those findings, but also found that risk prediction was better when mean heart dose (MHD) was replaced by the volume of the left ventricle receiving 5 Gy (LV-V5); the substitution improved the c-statistic to 0.80 (95% confidence interval, 0.72-0.88). Using a weighted ACE risk score based on baseline diabetes, hypertension, and ischemic event history – instead of the risk factor yes-or-no approach from 2013 – further improved predictive power, with a c-statistic of 0.83 (95% CI, 0.75-0.91). Anything over a c-statistic of 0.8 is considered strong; 0.5 is chance, 1.0 is perfect prediction.
For instance, a 70-year-old woman with an LV-V5 of 50% and no cardiac risk factors had an excess ACE risk in the new system of 2.52% within 9 years of radiotherapy (RT). If she had a history of ischemic heart disease, the excess risk increased to 8.42%, the investigators said (J Clin Oncol. 2017 Jan 17. doi: 10.1200/JCO.2016.69.8480).
“Model performance was significantly improved by replacing MHD with LV-V5 and using the weighted ACE risk score.” However, “because we were not able to externally validate the LV-V5 model, this model” requires validation “before it can be used in routine clinical practice,” said investigators, led by Veerle van den Bogaard, MD, of the University of Groningen, the Netherlands.
The women were a median of 59 years old, and they were followed for a median of 7.6 years, with a range of 0.1-10.1 years. Radiation dose information was derived from CT planning scans. The median MHD was 2.37 Gy.
Thirty patients (3.3%) had an ACE, defined as myocardial infarction, coronary revascularization, or death due to ischemic heart disease; 17 had events in the first 5 years. The 5- and 9-year cumulative ACE incidences were 1.9% and 3.9%. Ten of the 30 women died from their cardiac complication.
The model predicted a cumulative ACE incidence at 9 years of 3.5%, which was in line with the observed rate of 3.9%. The excess cumulative risk related to RT was 1.13%. Overall, about 10 patients had an ACE that could be attributed to RT. The cumulative incidence of ACE increased by 16.5% per Gy (95% CI, 0.6-35.0; P = .042). The findings were consistent with the 2013 study.
ACE incidence was not significantly associated with the maximum dose of radiation to the heart.
LV-V5 was the most important prognostic dose-volume parameter associated with the cumulative incidence of ACE, with a hazard ratio of 1.016 (95% CI, 1.002-1.030; P = .016). “Because of this strong association, we chose to include LV-V5 in the model,” the investigators said.
There was no external funding. The lead investigator had no disclosures, but two authors reported institutional research funding from Philips, Roche, and other companies. One was an advisor and speaker for IBA.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: Replacing the mean heart dose with the volume of the left ventricle receiving 5 Gy improves the predictive c-statistic to 0.80.
Data source: Investigation of 910 women who underwent radiation treatment following breast-conserving surgery.
Disclosures: There was no external funding. The lead investigator had no disclosures, but two authors reported institutional research funding from Philips, Roche, and other companies. One was an advisor and speaker for IBA.
Palliative care improves quality of life after HCT
Inpatient palliative care can help maintain quality of life (QoL) in patients undergoing hematopoietic stem cell transplantation (HCT), based on the results of a randomized clinical trial to assess the effect of inpatient palliative care on patient and caregiver-reported outcomes while hospitalized for HCT and for 3 months after transplantation.
During the 2-week period following their transplants, patients who received inpatient palliative care experienced a 14.72-point decrease in QoL, compared with a 21.54-point decrease in QoL for those assigned to standard transplant care alone. The difference was statistically significant (JAMA. 2016;316[20]:2094-2103. doi:10.1001/jama.2016.16786).
In addition to the QoL results, Areej El-Jawahri, MD, of Massachusetts General Hospital in Boston, and coauthors, noted that “exploratory secondary outcomes also showed that patients in the palliative care group benefited, with less increase in their depression symptoms, lower anxiety symptoms, and less increase in symptom burden compared with those receiving standard transplant care.
“Thus, palliative care may help to lessen the decline in QoL experienced by patients during hospitalization for HCT, which has long been perceived as a natural aspect of the transplantation process.”
The study cohort comprised 160 adults with hematologic malignancies undergoing autologous/allogeneic HCT, and 94 caregivers.
A total of 81 patients were assigned to the intervention, and were seen by palliative care clinicians at least twice a week while they were hospitalized. The palliative care intervention focused on managing both physical and psychological symptoms, and those who were assigned to the standard care arm (n = 79) could also request to be seen by the palliative care team.
Quality of life was measured based on mean FACT-BMT score. In the palliative care group, the FACT-BMT score was 110.26 at hospitalization and 95.46 at 2 weeks after transplant (mean change, −14.72). For the standard care group, FACT-BMT score was 106.83 at hospitalization and 85.42 at 2 weeks after transplant (mean change, −21.54) The −6.82 difference between the group groups was statistically significant (95% CI, −13.48 to −0.16; P = .045).
When looking at secondary outcomes, those in the intervention group had lower mean depression scores at 2 weeks based on the HADS-D measure. For the intervention group, the mean baseline score was 3.95 and the mean week 2 score was 6.39. For the control group, the baseline score was 4.94 and the week 2 score was 8.86. The difference between the groups was 1.49 (95% CI, 0.20-2.78; P = .02). Depression scores remained lower in the intervention group at 3 months.
The intervention group also reported a decrease in anxiety symptoms, but the control group reported an increase in anxiety symptoms from baseline to week 2 on the HADS-A measure. The mean difference in score between the two groups was 1.92; (95% CI, 0.83-3.01; P less than .001). However, there was no significant difference between the two groups at 3 months after transplant.
The study was supported by the National Palliative Care Research Foundation and grant K24 CA 181253 from the National Cancer Institute. Dr. El-Jawahri reported no disclosures.
Inpatient palliative care can help maintain quality of life (QoL) in patients undergoing hematopoietic stem cell transplantation (HCT), based on the results of a randomized clinical trial to assess the effect of inpatient palliative care on patient and caregiver-reported outcomes while hospitalized for HCT and for 3 months after transplantation.
During the 2-week period following their transplants, patients who received inpatient palliative care experienced a 14.72-point decrease in QoL, compared with a 21.54-point decrease in QoL for those assigned to standard transplant care alone. The difference was statistically significant (JAMA. 2016;316[20]:2094-2103. doi:10.1001/jama.2016.16786).
In addition to the QoL results, Areej El-Jawahri, MD, of Massachusetts General Hospital in Boston, and coauthors, noted that “exploratory secondary outcomes also showed that patients in the palliative care group benefited, with less increase in their depression symptoms, lower anxiety symptoms, and less increase in symptom burden compared with those receiving standard transplant care.
“Thus, palliative care may help to lessen the decline in QoL experienced by patients during hospitalization for HCT, which has long been perceived as a natural aspect of the transplantation process.”
The study cohort comprised 160 adults with hematologic malignancies undergoing autologous/allogeneic HCT, and 94 caregivers.
A total of 81 patients were assigned to the intervention, and were seen by palliative care clinicians at least twice a week while they were hospitalized. The palliative care intervention focused on managing both physical and psychological symptoms, and those who were assigned to the standard care arm (n = 79) could also request to be seen by the palliative care team.
Quality of life was measured based on mean FACT-BMT score. In the palliative care group, the FACT-BMT score was 110.26 at hospitalization and 95.46 at 2 weeks after transplant (mean change, −14.72). For the standard care group, FACT-BMT score was 106.83 at hospitalization and 85.42 at 2 weeks after transplant (mean change, −21.54) The −6.82 difference between the group groups was statistically significant (95% CI, −13.48 to −0.16; P = .045).
When looking at secondary outcomes, those in the intervention group had lower mean depression scores at 2 weeks based on the HADS-D measure. For the intervention group, the mean baseline score was 3.95 and the mean week 2 score was 6.39. For the control group, the baseline score was 4.94 and the week 2 score was 8.86. The difference between the groups was 1.49 (95% CI, 0.20-2.78; P = .02). Depression scores remained lower in the intervention group at 3 months.
The intervention group also reported a decrease in anxiety symptoms, but the control group reported an increase in anxiety symptoms from baseline to week 2 on the HADS-A measure. The mean difference in score between the two groups was 1.92; (95% CI, 0.83-3.01; P less than .001). However, there was no significant difference between the two groups at 3 months after transplant.
The study was supported by the National Palliative Care Research Foundation and grant K24 CA 181253 from the National Cancer Institute. Dr. El-Jawahri reported no disclosures.
Inpatient palliative care can help maintain quality of life (QoL) in patients undergoing hematopoietic stem cell transplantation (HCT), based on the results of a randomized clinical trial to assess the effect of inpatient palliative care on patient and caregiver-reported outcomes while hospitalized for HCT and for 3 months after transplantation.
During the 2-week period following their transplants, patients who received inpatient palliative care experienced a 14.72-point decrease in QoL, compared with a 21.54-point decrease in QoL for those assigned to standard transplant care alone. The difference was statistically significant (JAMA. 2016;316[20]:2094-2103. doi:10.1001/jama.2016.16786).
In addition to the QoL results, Areej El-Jawahri, MD, of Massachusetts General Hospital in Boston, and coauthors, noted that “exploratory secondary outcomes also showed that patients in the palliative care group benefited, with less increase in their depression symptoms, lower anxiety symptoms, and less increase in symptom burden compared with those receiving standard transplant care.
“Thus, palliative care may help to lessen the decline in QoL experienced by patients during hospitalization for HCT, which has long been perceived as a natural aspect of the transplantation process.”
The study cohort comprised 160 adults with hematologic malignancies undergoing autologous/allogeneic HCT, and 94 caregivers.
A total of 81 patients were assigned to the intervention, and were seen by palliative care clinicians at least twice a week while they were hospitalized. The palliative care intervention focused on managing both physical and psychological symptoms, and those who were assigned to the standard care arm (n = 79) could also request to be seen by the palliative care team.
Quality of life was measured based on mean FACT-BMT score. In the palliative care group, the FACT-BMT score was 110.26 at hospitalization and 95.46 at 2 weeks after transplant (mean change, −14.72). For the standard care group, FACT-BMT score was 106.83 at hospitalization and 85.42 at 2 weeks after transplant (mean change, −21.54) The −6.82 difference between the group groups was statistically significant (95% CI, −13.48 to −0.16; P = .045).
When looking at secondary outcomes, those in the intervention group had lower mean depression scores at 2 weeks based on the HADS-D measure. For the intervention group, the mean baseline score was 3.95 and the mean week 2 score was 6.39. For the control group, the baseline score was 4.94 and the week 2 score was 8.86. The difference between the groups was 1.49 (95% CI, 0.20-2.78; P = .02). Depression scores remained lower in the intervention group at 3 months.
The intervention group also reported a decrease in anxiety symptoms, but the control group reported an increase in anxiety symptoms from baseline to week 2 on the HADS-A measure. The mean difference in score between the two groups was 1.92; (95% CI, 0.83-3.01; P less than .001). However, there was no significant difference between the two groups at 3 months after transplant.
The study was supported by the National Palliative Care Research Foundation and grant K24 CA 181253 from the National Cancer Institute. Dr. El-Jawahri reported no disclosures.
FROM JAMA
Key clinical point: Inpatient palliative care can help maintain quality of life in patients undergoing hematopoietic stem cell transplantation.
Major finding: During the 2-week period following their transplants, patients who received inpatient palliative care experienced a 14.72-point decrease in QoL, compared with a 21.54-point decrease in QoL for those assigned to standard transplant care alone.
Data source: Randomized clinical trial among 160 adults with hematologic malignancies who underwent HCT, and their caregivers (n = 94).
Disclosures: The study was supported by the National Palliative Care Research Foundation and grant K24 CA 181253 from the National Cancer Institute. Dr. El-Jawahri reported no disclosures.