User login
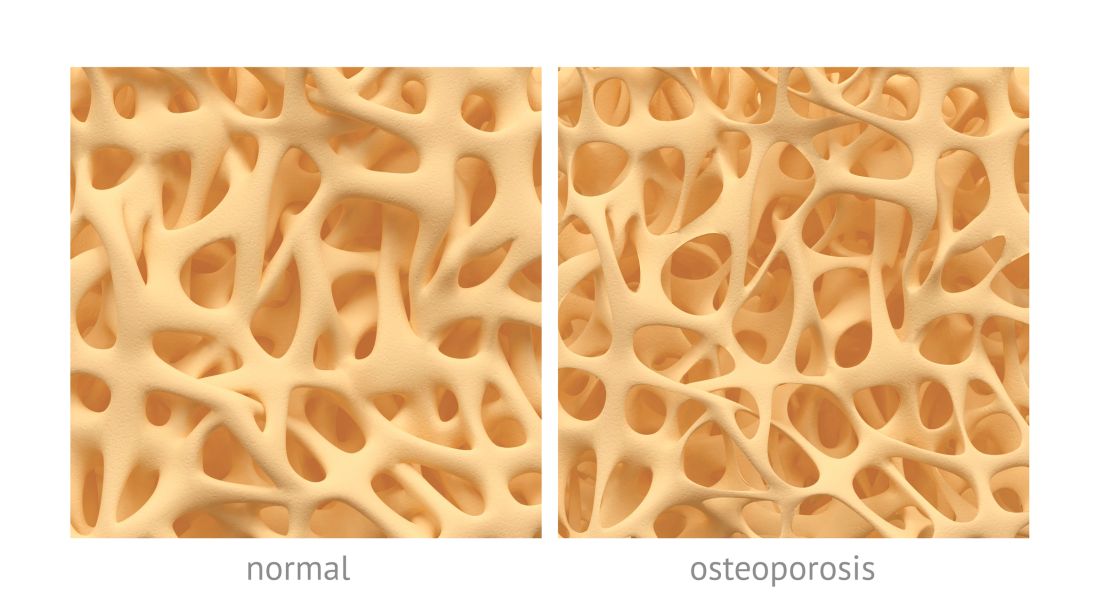
PBC linked to increased risk of bone fracture
Patients with primary biliary cholangitis (PBC) may have an increase in the risk of developing bone fracture, according to Jian Zhao, MD, and associates.
In four cross-sectional studies, 515 patients were examined to assess the prevalence of fracture in a PBC population. Of those patients, the estimated prevalence of fracture was 15.2%. In four additional studies, 1,002 patients and 8,805 controls were examined to assess the relative risk of fracture among PBC patients. Those results found a significantly increased risk of fracture in PBC patients with the pooled odds ratio of 1.93.
It is noted that multiple factors underlie the osteopenic bone disease in PBC. In addition to cholestasis, risk factors include female sex, low body mass index, advanced age, and history of fragility fracture. Steroid use may also contribute to bone loss in PBC, especially in autoimmune hepatitis–primary biliary cholangitis overlap syndrome.
“The prevalence of bone fracture among PBC patients is relatively high and PBC increases the risk of fracture,” the researchers concluded. “Calcium and vitamin D supplementation or even bisphosphonate therapy should be recommended for PBC patients with bone loss to decrease the risk of fracture.”
Read the study in Clinics and Research in Hepatology and Gastroenterology (doi: 10.1016/j.clinre.2017.05.008).
Patients with primary biliary cholangitis (PBC) may have an increase in the risk of developing bone fracture, according to Jian Zhao, MD, and associates.
In four cross-sectional studies, 515 patients were examined to assess the prevalence of fracture in a PBC population. Of those patients, the estimated prevalence of fracture was 15.2%. In four additional studies, 1,002 patients and 8,805 controls were examined to assess the relative risk of fracture among PBC patients. Those results found a significantly increased risk of fracture in PBC patients with the pooled odds ratio of 1.93.
It is noted that multiple factors underlie the osteopenic bone disease in PBC. In addition to cholestasis, risk factors include female sex, low body mass index, advanced age, and history of fragility fracture. Steroid use may also contribute to bone loss in PBC, especially in autoimmune hepatitis–primary biliary cholangitis overlap syndrome.
“The prevalence of bone fracture among PBC patients is relatively high and PBC increases the risk of fracture,” the researchers concluded. “Calcium and vitamin D supplementation or even bisphosphonate therapy should be recommended for PBC patients with bone loss to decrease the risk of fracture.”
Read the study in Clinics and Research in Hepatology and Gastroenterology (doi: 10.1016/j.clinre.2017.05.008).
Patients with primary biliary cholangitis (PBC) may have an increase in the risk of developing bone fracture, according to Jian Zhao, MD, and associates.
In four cross-sectional studies, 515 patients were examined to assess the prevalence of fracture in a PBC population. Of those patients, the estimated prevalence of fracture was 15.2%. In four additional studies, 1,002 patients and 8,805 controls were examined to assess the relative risk of fracture among PBC patients. Those results found a significantly increased risk of fracture in PBC patients with the pooled odds ratio of 1.93.
It is noted that multiple factors underlie the osteopenic bone disease in PBC. In addition to cholestasis, risk factors include female sex, low body mass index, advanced age, and history of fragility fracture. Steroid use may also contribute to bone loss in PBC, especially in autoimmune hepatitis–primary biliary cholangitis overlap syndrome.
“The prevalence of bone fracture among PBC patients is relatively high and PBC increases the risk of fracture,” the researchers concluded. “Calcium and vitamin D supplementation or even bisphosphonate therapy should be recommended for PBC patients with bone loss to decrease the risk of fracture.”
Read the study in Clinics and Research in Hepatology and Gastroenterology (doi: 10.1016/j.clinre.2017.05.008).
FROM CLINICS AND RESEARCH IN HEPATOLOGY AND GASTROENTEROLOGY
Incidental hip CT scans could serve as osteoporosis screen
DENVER – Computed tomography (CT) scans that were taken for an unrelated purpose could potentially be used to screen for osteoporosis, according to a new study. Researchers analyzed data from CT scans that produced estimates of bone mineral density (BMD) and femoral strength, and these performed similarly to dual-energy X-ray absorptiometry (DXA) in predicting fracture risk.
“The neat thing is that there’s no additional burden to the patients, because they’ve already had the CT scan. There’s no additional radiation exposure, no additional trip to the office. Another advantage to this is there are so many more men who are getting CT scans than there are who are getting DXAs for osteoporosis, so it’s an opportunity to screen more men,” Annette Adams, PhD, research scientist at Kaiser Permanente of Southern California, said in an interview at the annual meeting of the American Society for Bone and Mineral Research.
To test the potential of the CT scans, the researchers conducted a case-control cohort analysis of patients aged 65 and over who were seen at 11 Kaiser Permanente Southern California (KPSC) hospitals. The patients had undergone abdominal or pelvic CT between 2006 and 2014. They had not experienced a fragility hip fracture before the CT scan was taken, but they had to have undergone a DXA within 3 years of the scan.
A total of 1,340 women and 619 men had a first hip fracture during the study period. They were compared to randomly selected subjects without hip fractures.
The researchers found associations between hip fractures and CT-based scores, and the relationships were stronger than those seen with DXA. In women, for each decrease in one standard deviation (SD) in hip BMD T-score, the hazard ratio (HR) for hip fracture was 2.18 (95% confidence interval [CI], 1.87-2.54). In men, the HR was 3.12 (2.35-4.14). The HRs for hip fracture based on DXA hip BMD T-score values were 1.80 (95% CI, 1.53-2.13) for women and 2.74 (95% CI, 2.15-3.49) for men.
CT-derived femoral strength values also performed well. In women, each one SD decrease in femoral strength seen in the CT-based scores was associated with an HR of 2.76 (95% CI, 2.25-3.39). In men, the value was HR 2.84 (95% CI, 2.20-3.66).
In a subanalysis of subjects who had not received osteoporosis treatment, for each one SD decrease in hip BMD T-score, the HR for hip fracture was 2.72 (95% CI, 2.24-3.32) in women and 3.93 (95% CI, 2.46-6.26) in men.
In untreated patients, each increase of one SD in femoral strength was tied to an HR in women of 3.81 (95% CI, 2.90-5.01) and 3.37 (95% CI, 2.27-5.01) in men.
The addition of established thresholds for osteoporosis (BMD T-score –2.5 or less) as well as fragile bone strength (3,000 Newtons or less in women, 3,500 Newtons or less in men) increased the 5-year sensitivity for hip fracture from 0.55 to 0.67 in women, and from 0.43 to 0.54 in men.
The technique is not yet ready for large-scale implementation because the process isn’t yet completely automated – it requires human review to eliminate some glitches, and that is likely to make it cost ineffective for now, Sally Warner, PhD, said in an interview. Dr. Warner is senior director of musculoskeletal imaging at Parexel, and was not involved in the study.
But she was nevertheless enthusiastic. “CT is such a great modality to be able to look at bone and interpret the density, the volume, the quality of the bone. It’s got great potential utility,” she said.
She said she thinks it will become cost-effective in time. “As long as the acquisition is standardized, I’m sure the automation could come a little bit more readily,” Dr. Warner said.
Amgen and Merck funded the study. Dr. Adams has received research funding from both companies. Dr. Warner reported having no financial disclosures.
DENVER – Computed tomography (CT) scans that were taken for an unrelated purpose could potentially be used to screen for osteoporosis, according to a new study. Researchers analyzed data from CT scans that produced estimates of bone mineral density (BMD) and femoral strength, and these performed similarly to dual-energy X-ray absorptiometry (DXA) in predicting fracture risk.
“The neat thing is that there’s no additional burden to the patients, because they’ve already had the CT scan. There’s no additional radiation exposure, no additional trip to the office. Another advantage to this is there are so many more men who are getting CT scans than there are who are getting DXAs for osteoporosis, so it’s an opportunity to screen more men,” Annette Adams, PhD, research scientist at Kaiser Permanente of Southern California, said in an interview at the annual meeting of the American Society for Bone and Mineral Research.
To test the potential of the CT scans, the researchers conducted a case-control cohort analysis of patients aged 65 and over who were seen at 11 Kaiser Permanente Southern California (KPSC) hospitals. The patients had undergone abdominal or pelvic CT between 2006 and 2014. They had not experienced a fragility hip fracture before the CT scan was taken, but they had to have undergone a DXA within 3 years of the scan.
A total of 1,340 women and 619 men had a first hip fracture during the study period. They were compared to randomly selected subjects without hip fractures.
The researchers found associations between hip fractures and CT-based scores, and the relationships were stronger than those seen with DXA. In women, for each decrease in one standard deviation (SD) in hip BMD T-score, the hazard ratio (HR) for hip fracture was 2.18 (95% confidence interval [CI], 1.87-2.54). In men, the HR was 3.12 (2.35-4.14). The HRs for hip fracture based on DXA hip BMD T-score values were 1.80 (95% CI, 1.53-2.13) for women and 2.74 (95% CI, 2.15-3.49) for men.
CT-derived femoral strength values also performed well. In women, each one SD decrease in femoral strength seen in the CT-based scores was associated with an HR of 2.76 (95% CI, 2.25-3.39). In men, the value was HR 2.84 (95% CI, 2.20-3.66).
In a subanalysis of subjects who had not received osteoporosis treatment, for each one SD decrease in hip BMD T-score, the HR for hip fracture was 2.72 (95% CI, 2.24-3.32) in women and 3.93 (95% CI, 2.46-6.26) in men.
In untreated patients, each increase of one SD in femoral strength was tied to an HR in women of 3.81 (95% CI, 2.90-5.01) and 3.37 (95% CI, 2.27-5.01) in men.
The addition of established thresholds for osteoporosis (BMD T-score –2.5 or less) as well as fragile bone strength (3,000 Newtons or less in women, 3,500 Newtons or less in men) increased the 5-year sensitivity for hip fracture from 0.55 to 0.67 in women, and from 0.43 to 0.54 in men.
The technique is not yet ready for large-scale implementation because the process isn’t yet completely automated – it requires human review to eliminate some glitches, and that is likely to make it cost ineffective for now, Sally Warner, PhD, said in an interview. Dr. Warner is senior director of musculoskeletal imaging at Parexel, and was not involved in the study.
But she was nevertheless enthusiastic. “CT is such a great modality to be able to look at bone and interpret the density, the volume, the quality of the bone. It’s got great potential utility,” she said.
She said she thinks it will become cost-effective in time. “As long as the acquisition is standardized, I’m sure the automation could come a little bit more readily,” Dr. Warner said.
Amgen and Merck funded the study. Dr. Adams has received research funding from both companies. Dr. Warner reported having no financial disclosures.
DENVER – Computed tomography (CT) scans that were taken for an unrelated purpose could potentially be used to screen for osteoporosis, according to a new study. Researchers analyzed data from CT scans that produced estimates of bone mineral density (BMD) and femoral strength, and these performed similarly to dual-energy X-ray absorptiometry (DXA) in predicting fracture risk.
“The neat thing is that there’s no additional burden to the patients, because they’ve already had the CT scan. There’s no additional radiation exposure, no additional trip to the office. Another advantage to this is there are so many more men who are getting CT scans than there are who are getting DXAs for osteoporosis, so it’s an opportunity to screen more men,” Annette Adams, PhD, research scientist at Kaiser Permanente of Southern California, said in an interview at the annual meeting of the American Society for Bone and Mineral Research.
To test the potential of the CT scans, the researchers conducted a case-control cohort analysis of patients aged 65 and over who were seen at 11 Kaiser Permanente Southern California (KPSC) hospitals. The patients had undergone abdominal or pelvic CT between 2006 and 2014. They had not experienced a fragility hip fracture before the CT scan was taken, but they had to have undergone a DXA within 3 years of the scan.
A total of 1,340 women and 619 men had a first hip fracture during the study period. They were compared to randomly selected subjects without hip fractures.
The researchers found associations between hip fractures and CT-based scores, and the relationships were stronger than those seen with DXA. In women, for each decrease in one standard deviation (SD) in hip BMD T-score, the hazard ratio (HR) for hip fracture was 2.18 (95% confidence interval [CI], 1.87-2.54). In men, the HR was 3.12 (2.35-4.14). The HRs for hip fracture based on DXA hip BMD T-score values were 1.80 (95% CI, 1.53-2.13) for women and 2.74 (95% CI, 2.15-3.49) for men.
CT-derived femoral strength values also performed well. In women, each one SD decrease in femoral strength seen in the CT-based scores was associated with an HR of 2.76 (95% CI, 2.25-3.39). In men, the value was HR 2.84 (95% CI, 2.20-3.66).
In a subanalysis of subjects who had not received osteoporosis treatment, for each one SD decrease in hip BMD T-score, the HR for hip fracture was 2.72 (95% CI, 2.24-3.32) in women and 3.93 (95% CI, 2.46-6.26) in men.
In untreated patients, each increase of one SD in femoral strength was tied to an HR in women of 3.81 (95% CI, 2.90-5.01) and 3.37 (95% CI, 2.27-5.01) in men.
The addition of established thresholds for osteoporosis (BMD T-score –2.5 or less) as well as fragile bone strength (3,000 Newtons or less in women, 3,500 Newtons or less in men) increased the 5-year sensitivity for hip fracture from 0.55 to 0.67 in women, and from 0.43 to 0.54 in men.
The technique is not yet ready for large-scale implementation because the process isn’t yet completely automated – it requires human review to eliminate some glitches, and that is likely to make it cost ineffective for now, Sally Warner, PhD, said in an interview. Dr. Warner is senior director of musculoskeletal imaging at Parexel, and was not involved in the study.
But she was nevertheless enthusiastic. “CT is such a great modality to be able to look at bone and interpret the density, the volume, the quality of the bone. It’s got great potential utility,” she said.
She said she thinks it will become cost-effective in time. “As long as the acquisition is standardized, I’m sure the automation could come a little bit more readily,” Dr. Warner said.
Amgen and Merck funded the study. Dr. Adams has received research funding from both companies. Dr. Warner reported having no financial disclosures.
AT ASBMR
Key clinical point: Use of existing abdominal or pelvic CT scans may serve as a way to screen for osteoporosis without the need for dual-energy x-ray absorptiometry.
Major finding: For each decrease in one standard deviation in CT-derived hip BMD T-score, the hazard ratio for hip fracture was 2.18 in women and 3.12 in men.
Data source: A case-control study of 1,340 women and 619 men at 11 California centers.
Disclosures: Amgen and Merck funded the study. Dr. Adams has received research funding from both companies. Dr. Warner reported having no financial disclosures.
Reduced fracture risk maintained in abaloparatide extension study
denver – Sequential treatment with abaloparatide and alendronate was associated with reduced vertebral and non-vertebral fractures compared to placebo and alendronate among high-risk women with osteoporosis in a 3.5 year extension study of the ACTIVE trial.
The ACTIVExtend trial included 558 women in the abaloparatide group and 581 women in the placebo group of the original ACTIVE study (NCT01343004). In that double-blind trial, 2,463 postmenopausal women with osteoporosis were randomized to receive daily injections of abaloparatide (80 µg) or placebo, or open-label teriparatide (20 µg). After 18 months of treatment, patients in the placebo and abaloparatide groups were switched to alendronate 70 mg weekly for two years, Henry Bone, MD, director of the Michigan Bone and Mineral Clinic in Detroit, said at the annual meeting of the American Society for Bone and Mineral Research.
The abaloparatide-alendronate group had a 34% relative risk reduction for all clinical fractures compared to the placebo-alendronate group (P = .045). For major osteoporotic fractures, the abaloparatide-alendronate group had a 50% relative risk reduction compared to the placebo-alendronate group (P = .011).
Among women who had no new vertebral fractures during the first 18 months of the ACTIVE study, 2 women in the abaloparatide-alendronate group and 13 in the placebo-alendronate group had new vertebral fractures during ACTIVExtend.
Adverse events were similar in both arms of the study. There were no cases of atypical femur fracture or osteonecrosis of the jaw.The anabolic agent abaloparatide was approved by the Food and Drug Administration in April for the treatment of osteoporosis in women at high risk of fracture. Sequential treatment with the anti-resorptive agent alendronate aims to preserve the bone density gains from abaloparatide, as previous research has shown that improvements with anabolic agents can be lost once the drug is stopped.
denver – Sequential treatment with abaloparatide and alendronate was associated with reduced vertebral and non-vertebral fractures compared to placebo and alendronate among high-risk women with osteoporosis in a 3.5 year extension study of the ACTIVE trial.
The ACTIVExtend trial included 558 women in the abaloparatide group and 581 women in the placebo group of the original ACTIVE study (NCT01343004). In that double-blind trial, 2,463 postmenopausal women with osteoporosis were randomized to receive daily injections of abaloparatide (80 µg) or placebo, or open-label teriparatide (20 µg). After 18 months of treatment, patients in the placebo and abaloparatide groups were switched to alendronate 70 mg weekly for two years, Henry Bone, MD, director of the Michigan Bone and Mineral Clinic in Detroit, said at the annual meeting of the American Society for Bone and Mineral Research.
The abaloparatide-alendronate group had a 34% relative risk reduction for all clinical fractures compared to the placebo-alendronate group (P = .045). For major osteoporotic fractures, the abaloparatide-alendronate group had a 50% relative risk reduction compared to the placebo-alendronate group (P = .011).
Among women who had no new vertebral fractures during the first 18 months of the ACTIVE study, 2 women in the abaloparatide-alendronate group and 13 in the placebo-alendronate group had new vertebral fractures during ACTIVExtend.
Adverse events were similar in both arms of the study. There were no cases of atypical femur fracture or osteonecrosis of the jaw.The anabolic agent abaloparatide was approved by the Food and Drug Administration in April for the treatment of osteoporosis in women at high risk of fracture. Sequential treatment with the anti-resorptive agent alendronate aims to preserve the bone density gains from abaloparatide, as previous research has shown that improvements with anabolic agents can be lost once the drug is stopped.
denver – Sequential treatment with abaloparatide and alendronate was associated with reduced vertebral and non-vertebral fractures compared to placebo and alendronate among high-risk women with osteoporosis in a 3.5 year extension study of the ACTIVE trial.
The ACTIVExtend trial included 558 women in the abaloparatide group and 581 women in the placebo group of the original ACTIVE study (NCT01343004). In that double-blind trial, 2,463 postmenopausal women with osteoporosis were randomized to receive daily injections of abaloparatide (80 µg) or placebo, or open-label teriparatide (20 µg). After 18 months of treatment, patients in the placebo and abaloparatide groups were switched to alendronate 70 mg weekly for two years, Henry Bone, MD, director of the Michigan Bone and Mineral Clinic in Detroit, said at the annual meeting of the American Society for Bone and Mineral Research.
The abaloparatide-alendronate group had a 34% relative risk reduction for all clinical fractures compared to the placebo-alendronate group (P = .045). For major osteoporotic fractures, the abaloparatide-alendronate group had a 50% relative risk reduction compared to the placebo-alendronate group (P = .011).
Among women who had no new vertebral fractures during the first 18 months of the ACTIVE study, 2 women in the abaloparatide-alendronate group and 13 in the placebo-alendronate group had new vertebral fractures during ACTIVExtend.
Adverse events were similar in both arms of the study. There were no cases of atypical femur fracture or osteonecrosis of the jaw.The anabolic agent abaloparatide was approved by the Food and Drug Administration in April for the treatment of osteoporosis in women at high risk of fracture. Sequential treatment with the anti-resorptive agent alendronate aims to preserve the bone density gains from abaloparatide, as previous research has shown that improvements with anabolic agents can be lost once the drug is stopped.
REPORTING FROM ASBMR 2017
Key clinical point: The reduced fracture risk seen after 18 months of abaloparatide therapy persisted at 43 months with follow up alendronate therapy, and was superior to the results seen in women who received placebo for 18 months followed by alendronate.
Major finding: 0.9% of women who started on abaloparatide experienced at least 1 new vertebral fracture, compared to 5.6% of those who started on placebo.
Data source: The ACTIVExtend trial included 558 women in the abaloparatide group and 581 women in the placebo group.
Disclosures: The study was funded by Radius Health, the maker of abaloparatide. Dr. Bone is a consultant and investigator for Radius Health and Amgen.
Worsening osteoporosis care for RA patients shows need for action
Osteoporosis care in patients with rheumatoid arthritis is suboptimal, and the relative risk of the application of appropriate osteoporosis care in both RA and osteoarthritis patients has been declining steadily over the past decade, according to findings from a large, prospective, observational study.
The study included 11,669 RA patients and 2,829 OA patients in the National Data Bank for Rheumatic Diseases who were followed from 2003 through 2014 and showed that about half of the RA patients in whom osteoporosis treatment was indicated never received an osteoporosis medication. Further, the decline in the application of appropriate osteoporosis care was apparent even after the release of the 2010 American College of Rheumatology Guideline for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis, according to the findings, which have been accepted for publication in Arthritis Care & Research (doi: 10.1002/acr.23331).
A more recent study in the general population showed that, regardless of glucocorticoid (GC) use, there was a significant decrease in the use of oral bisphosphonates from 1996 to 2012, noted Dr. Ozen of the University of Nebraska, Omaha, and Marmara University, Istanbul, Turkey.
“The evidence from all these studies suggests that, despite a slight improvement in GIOP care, with a decline in overall OP care in the early 2000s, the OP care gap has always been suboptimal and declined over the last decade significantly,” she said, adding that this is “especially more worrisome in glucocorticoid-receiving RA patients,” in whom bone loss and fracture risk are dramatically increased.
“Additionally, considering that rheumatologists do better regarding comorbidity follow-up and management than other specialists who follow patients with rheumatic diseases, the gap for osteoporosis care might be even higher than we reported,” she said.
Indeed, among physicians caring for patients with osteoporosis, there is concern that “we’re on the precipice of further increase in fracture burden,” according to Kenneth Saag, MD, a rheumatologist and professor at the University of Alabama at Birmingham.
The conclusions of the study by Dr. Ozen and her colleagues are disturbing, but “not tremendously surprising,” said Dr. Saag, who also is president of the National Osteoporosis Foundation.
The findings are consistent with those from previous studies, he explained.
For example, Daniel H. Solomon, MD, and his associates showed that only 23% of 623 RA patients, including 236 patients who were taking glucocorticoids at an index visit in 1999, underwent bone densitometry, and only 42% were prescribed a medication (other than calcium and/or vitamin D), that reduces bone loss (Arthritis Rheum. 2002;46:3136-42). They also showed that, in 2004, despite a slight improvement vs. prior years, only 48% of 193 RA patients included in a chart review had received a bone mineral density test or medication for osteoporosis, and 64% of those taking more than 5 mg of prednisone for more than 3 months were receiving osteoporosis management (Arthritis Care Res. 2006;55:873-7).
In the current study, Dr. Ozen and her colleagues looked at both RA and OA patients and found that overall, osteoporosis treatment or screening was reported in 67.4% of study subjects over a mean of 5.5 years follow-up. Of those eligible for osteoporosis treatment based on the 2010 ACR guidelines, including 48.4% of RA patients and 17.6% of OA patients, 55% reported osteoporosis medication use. Despite their increased risk of osteoporosis, particularly in the setting of glucocorticoid use, RA patients were not more likely than OA patients to undergo screening or receive treatment (hazard ratio, 1.04).
“This suboptimal and decreasing trend for osteoporosis treatment and screening in RA patients is important as the prevalence of osteoporosis leading to fractures in RA, regardless of GC use, is still high, despite aggressive management strategies and the use of [biologic disease-modifying antirheumatic agents],” they wrote.
Factors contributing to the decline
The reasons for the decline after 2008 are not fully known, but data suggest that both patient and clinician factors play a role.
Lack of knowledge, unwillingness to take additional drugs, and cost are among patient factors that may interfere with screening and treatment, and lack of experience and time, and a focus more on disease activity and other comorbid conditions may be among clinician factors, they said.
Other factors that may have affected patient and clinician willingness to pursue care include 2007 cuts in Medicare reimbursement for dual-energy x-ray absorptiometry (DXA), a 2006 warning regarding jaw osteonecrosis with bisphosphonate use, and 2007 and 2010 publications about atrial fibrillation and atypical femoral fractures associated with long-term bisphosphonate treatment, they noted.
Dr. Saag agreed that it is difficult to pinpoint exact reasons for the decline, but said the DXA reimbursement cuts have had a significant effect.
“Declining reimbursement is likely one of the major factors, if not the major factor in the decline in testing that has been observed nationally,” he said, explaining that reimbursement was below the break-even point for many physicians in freestanding medical practices, and that slight adjustments have applied only to facilities located in hospitals. As a result, the availability of DXA screening has declined.
The National Osteoporosis Foundation and other organizations such as the International Society for Clinical Densitometry are lobbying for changes, as there is a very strong link between testing and treatment.
“If we can’t get more people tested, we’re unlikely to get more people treated,” Dr. Saag said.
The availability of new agents for the treatment of osteoporosis could also lead to improvements in screening and care, he added.
In July, Amgen submitted to the Food and Drug Administration a supplemental new Biologics License Application for Prolia (denosumab) for the treatment of patients with GIOP. The application is based on a phase 3 study evaluating the safety and efficacy of Prolia, compared with risedronate, in patients receiving glucocorticoid treatment. Denosumab was also shown in a phase 3 study presented at the 2016 ACR meeting to result in greater improvement in bone mineral density vs. bisphosphonates across multiple sites, said Dr. Saag, an investigator for the trial.
“So we’re pleased about that finding, and we’re hopeful that eventually denosumab may become another treatment option,” he said, adding that having more choices leads to more personalized care for patients.
“We hope that, if it does receive approval and is utilized, that it may partially help address the gap in treatment that has been identified,” he said, adding that abaloparatide (Tymlos), which is approved for use in postmenopausal women with osteoporosis and high fracture risk, and romosozumab, currently in late-phase development, could also eventually help bridge the gap.
Recent guideline update
There is also optimism that a recent update to the 2010 guideline, published in August in Arthritis Care & Research, will help address the problem (Arthritis Care Res. 2017;69:1095-1110).
“We hope that one the most important impacts of the new 2017 ACR GIOP guideline will be increasing the awareness of GIOP care,” Dr. Ozen said, noting that changes in the new guideline will also be helpful for guiding management of certain patients not addressed in the 2010 guideline, including adults under age 40 years and children.
The new guideline also incorporates FRAX hip fracture scores into the risk-assessment recommendations .
“Lastly, the addition of other oral bisphosphonates and denosumab to the guideline has broadened the potential therapeutic options for physicians and patients,” she said.
Efforts by the ACR to make these guidelines widely known among clinicians could also help promote improved screening and treatment, said Dr. Buckley, a professor of internal medicine and pediatrics at Yale University, New Haven, Conn.
And that awareness is what is needed most, Dr. Ozen said.
“What we need in osteoporosis care of RA or GIOP patients is more awareness and education about risk-benefit ratios of antiosteoporotic medications instead of focusing on the medication type. We hope that our paper showing the worsening osteoporosis care and the new 2017 ACR GIOP guideline provide more awareness and guidance for the physicians managing these patients,” she said, adding that overcoming obstacles in osteoporosis care requires identification and attention to all potential causes for the suboptimal management of osteoporosis from both patients’ and physicians’ perspectives.
“With the improvement in management strategies of rheumatic diseases ... we anticipate improvement in life expectancy and cardiovascular outcomes in RA and inflammatory rheumatic diseases. In this regard, with aging and decreased but ongoing clinical or subclinical chronic inflammation, it is highly likely that we might be dealing with much older patients with higher osteoporosis and fracture risks. Considering the significant contribution of fractures on cost, disability, morbidity, and mortality of these diseases, rheumatologists and other specialists should work together more vigilantly to overcome the obstacles and improve osteoporosis care,” she said.
Dr. Ozen and Dr. Buckley reported having no conflicts of interest. Dr. Saag is an investigator and consultant for Amgen, Merck, and Radius Health, and is a consultant for Lilly.
Osteoporosis care in patients with rheumatoid arthritis is suboptimal, and the relative risk of the application of appropriate osteoporosis care in both RA and osteoarthritis patients has been declining steadily over the past decade, according to findings from a large, prospective, observational study.
The study included 11,669 RA patients and 2,829 OA patients in the National Data Bank for Rheumatic Diseases who were followed from 2003 through 2014 and showed that about half of the RA patients in whom osteoporosis treatment was indicated never received an osteoporosis medication. Further, the decline in the application of appropriate osteoporosis care was apparent even after the release of the 2010 American College of Rheumatology Guideline for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis, according to the findings, which have been accepted for publication in Arthritis Care & Research (doi: 10.1002/acr.23331).
A more recent study in the general population showed that, regardless of glucocorticoid (GC) use, there was a significant decrease in the use of oral bisphosphonates from 1996 to 2012, noted Dr. Ozen of the University of Nebraska, Omaha, and Marmara University, Istanbul, Turkey.
“The evidence from all these studies suggests that, despite a slight improvement in GIOP care, with a decline in overall OP care in the early 2000s, the OP care gap has always been suboptimal and declined over the last decade significantly,” she said, adding that this is “especially more worrisome in glucocorticoid-receiving RA patients,” in whom bone loss and fracture risk are dramatically increased.
“Additionally, considering that rheumatologists do better regarding comorbidity follow-up and management than other specialists who follow patients with rheumatic diseases, the gap for osteoporosis care might be even higher than we reported,” she said.
Indeed, among physicians caring for patients with osteoporosis, there is concern that “we’re on the precipice of further increase in fracture burden,” according to Kenneth Saag, MD, a rheumatologist and professor at the University of Alabama at Birmingham.
The conclusions of the study by Dr. Ozen and her colleagues are disturbing, but “not tremendously surprising,” said Dr. Saag, who also is president of the National Osteoporosis Foundation.
The findings are consistent with those from previous studies, he explained.
For example, Daniel H. Solomon, MD, and his associates showed that only 23% of 623 RA patients, including 236 patients who were taking glucocorticoids at an index visit in 1999, underwent bone densitometry, and only 42% were prescribed a medication (other than calcium and/or vitamin D), that reduces bone loss (Arthritis Rheum. 2002;46:3136-42). They also showed that, in 2004, despite a slight improvement vs. prior years, only 48% of 193 RA patients included in a chart review had received a bone mineral density test or medication for osteoporosis, and 64% of those taking more than 5 mg of prednisone for more than 3 months were receiving osteoporosis management (Arthritis Care Res. 2006;55:873-7).
In the current study, Dr. Ozen and her colleagues looked at both RA and OA patients and found that overall, osteoporosis treatment or screening was reported in 67.4% of study subjects over a mean of 5.5 years follow-up. Of those eligible for osteoporosis treatment based on the 2010 ACR guidelines, including 48.4% of RA patients and 17.6% of OA patients, 55% reported osteoporosis medication use. Despite their increased risk of osteoporosis, particularly in the setting of glucocorticoid use, RA patients were not more likely than OA patients to undergo screening or receive treatment (hazard ratio, 1.04).
“This suboptimal and decreasing trend for osteoporosis treatment and screening in RA patients is important as the prevalence of osteoporosis leading to fractures in RA, regardless of GC use, is still high, despite aggressive management strategies and the use of [biologic disease-modifying antirheumatic agents],” they wrote.
Factors contributing to the decline
The reasons for the decline after 2008 are not fully known, but data suggest that both patient and clinician factors play a role.
Lack of knowledge, unwillingness to take additional drugs, and cost are among patient factors that may interfere with screening and treatment, and lack of experience and time, and a focus more on disease activity and other comorbid conditions may be among clinician factors, they said.
Other factors that may have affected patient and clinician willingness to pursue care include 2007 cuts in Medicare reimbursement for dual-energy x-ray absorptiometry (DXA), a 2006 warning regarding jaw osteonecrosis with bisphosphonate use, and 2007 and 2010 publications about atrial fibrillation and atypical femoral fractures associated with long-term bisphosphonate treatment, they noted.
Dr. Saag agreed that it is difficult to pinpoint exact reasons for the decline, but said the DXA reimbursement cuts have had a significant effect.
“Declining reimbursement is likely one of the major factors, if not the major factor in the decline in testing that has been observed nationally,” he said, explaining that reimbursement was below the break-even point for many physicians in freestanding medical practices, and that slight adjustments have applied only to facilities located in hospitals. As a result, the availability of DXA screening has declined.
The National Osteoporosis Foundation and other organizations such as the International Society for Clinical Densitometry are lobbying for changes, as there is a very strong link between testing and treatment.
“If we can’t get more people tested, we’re unlikely to get more people treated,” Dr. Saag said.
The availability of new agents for the treatment of osteoporosis could also lead to improvements in screening and care, he added.
In July, Amgen submitted to the Food and Drug Administration a supplemental new Biologics License Application for Prolia (denosumab) for the treatment of patients with GIOP. The application is based on a phase 3 study evaluating the safety and efficacy of Prolia, compared with risedronate, in patients receiving glucocorticoid treatment. Denosumab was also shown in a phase 3 study presented at the 2016 ACR meeting to result in greater improvement in bone mineral density vs. bisphosphonates across multiple sites, said Dr. Saag, an investigator for the trial.
“So we’re pleased about that finding, and we’re hopeful that eventually denosumab may become another treatment option,” he said, adding that having more choices leads to more personalized care for patients.
“We hope that, if it does receive approval and is utilized, that it may partially help address the gap in treatment that has been identified,” he said, adding that abaloparatide (Tymlos), which is approved for use in postmenopausal women with osteoporosis and high fracture risk, and romosozumab, currently in late-phase development, could also eventually help bridge the gap.
Recent guideline update
There is also optimism that a recent update to the 2010 guideline, published in August in Arthritis Care & Research, will help address the problem (Arthritis Care Res. 2017;69:1095-1110).
“We hope that one the most important impacts of the new 2017 ACR GIOP guideline will be increasing the awareness of GIOP care,” Dr. Ozen said, noting that changes in the new guideline will also be helpful for guiding management of certain patients not addressed in the 2010 guideline, including adults under age 40 years and children.
The new guideline also incorporates FRAX hip fracture scores into the risk-assessment recommendations .
“Lastly, the addition of other oral bisphosphonates and denosumab to the guideline has broadened the potential therapeutic options for physicians and patients,” she said.
Efforts by the ACR to make these guidelines widely known among clinicians could also help promote improved screening and treatment, said Dr. Buckley, a professor of internal medicine and pediatrics at Yale University, New Haven, Conn.
And that awareness is what is needed most, Dr. Ozen said.
“What we need in osteoporosis care of RA or GIOP patients is more awareness and education about risk-benefit ratios of antiosteoporotic medications instead of focusing on the medication type. We hope that our paper showing the worsening osteoporosis care and the new 2017 ACR GIOP guideline provide more awareness and guidance for the physicians managing these patients,” she said, adding that overcoming obstacles in osteoporosis care requires identification and attention to all potential causes for the suboptimal management of osteoporosis from both patients’ and physicians’ perspectives.
“With the improvement in management strategies of rheumatic diseases ... we anticipate improvement in life expectancy and cardiovascular outcomes in RA and inflammatory rheumatic diseases. In this regard, with aging and decreased but ongoing clinical or subclinical chronic inflammation, it is highly likely that we might be dealing with much older patients with higher osteoporosis and fracture risks. Considering the significant contribution of fractures on cost, disability, morbidity, and mortality of these diseases, rheumatologists and other specialists should work together more vigilantly to overcome the obstacles and improve osteoporosis care,” she said.
Dr. Ozen and Dr. Buckley reported having no conflicts of interest. Dr. Saag is an investigator and consultant for Amgen, Merck, and Radius Health, and is a consultant for Lilly.
Osteoporosis care in patients with rheumatoid arthritis is suboptimal, and the relative risk of the application of appropriate osteoporosis care in both RA and osteoarthritis patients has been declining steadily over the past decade, according to findings from a large, prospective, observational study.
The study included 11,669 RA patients and 2,829 OA patients in the National Data Bank for Rheumatic Diseases who were followed from 2003 through 2014 and showed that about half of the RA patients in whom osteoporosis treatment was indicated never received an osteoporosis medication. Further, the decline in the application of appropriate osteoporosis care was apparent even after the release of the 2010 American College of Rheumatology Guideline for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis, according to the findings, which have been accepted for publication in Arthritis Care & Research (doi: 10.1002/acr.23331).
A more recent study in the general population showed that, regardless of glucocorticoid (GC) use, there was a significant decrease in the use of oral bisphosphonates from 1996 to 2012, noted Dr. Ozen of the University of Nebraska, Omaha, and Marmara University, Istanbul, Turkey.
“The evidence from all these studies suggests that, despite a slight improvement in GIOP care, with a decline in overall OP care in the early 2000s, the OP care gap has always been suboptimal and declined over the last decade significantly,” she said, adding that this is “especially more worrisome in glucocorticoid-receiving RA patients,” in whom bone loss and fracture risk are dramatically increased.
“Additionally, considering that rheumatologists do better regarding comorbidity follow-up and management than other specialists who follow patients with rheumatic diseases, the gap for osteoporosis care might be even higher than we reported,” she said.
Indeed, among physicians caring for patients with osteoporosis, there is concern that “we’re on the precipice of further increase in fracture burden,” according to Kenneth Saag, MD, a rheumatologist and professor at the University of Alabama at Birmingham.
The conclusions of the study by Dr. Ozen and her colleagues are disturbing, but “not tremendously surprising,” said Dr. Saag, who also is president of the National Osteoporosis Foundation.
The findings are consistent with those from previous studies, he explained.
For example, Daniel H. Solomon, MD, and his associates showed that only 23% of 623 RA patients, including 236 patients who were taking glucocorticoids at an index visit in 1999, underwent bone densitometry, and only 42% were prescribed a medication (other than calcium and/or vitamin D), that reduces bone loss (Arthritis Rheum. 2002;46:3136-42). They also showed that, in 2004, despite a slight improvement vs. prior years, only 48% of 193 RA patients included in a chart review had received a bone mineral density test or medication for osteoporosis, and 64% of those taking more than 5 mg of prednisone for more than 3 months were receiving osteoporosis management (Arthritis Care Res. 2006;55:873-7).
In the current study, Dr. Ozen and her colleagues looked at both RA and OA patients and found that overall, osteoporosis treatment or screening was reported in 67.4% of study subjects over a mean of 5.5 years follow-up. Of those eligible for osteoporosis treatment based on the 2010 ACR guidelines, including 48.4% of RA patients and 17.6% of OA patients, 55% reported osteoporosis medication use. Despite their increased risk of osteoporosis, particularly in the setting of glucocorticoid use, RA patients were not more likely than OA patients to undergo screening or receive treatment (hazard ratio, 1.04).
“This suboptimal and decreasing trend for osteoporosis treatment and screening in RA patients is important as the prevalence of osteoporosis leading to fractures in RA, regardless of GC use, is still high, despite aggressive management strategies and the use of [biologic disease-modifying antirheumatic agents],” they wrote.
Factors contributing to the decline
The reasons for the decline after 2008 are not fully known, but data suggest that both patient and clinician factors play a role.
Lack of knowledge, unwillingness to take additional drugs, and cost are among patient factors that may interfere with screening and treatment, and lack of experience and time, and a focus more on disease activity and other comorbid conditions may be among clinician factors, they said.
Other factors that may have affected patient and clinician willingness to pursue care include 2007 cuts in Medicare reimbursement for dual-energy x-ray absorptiometry (DXA), a 2006 warning regarding jaw osteonecrosis with bisphosphonate use, and 2007 and 2010 publications about atrial fibrillation and atypical femoral fractures associated with long-term bisphosphonate treatment, they noted.
Dr. Saag agreed that it is difficult to pinpoint exact reasons for the decline, but said the DXA reimbursement cuts have had a significant effect.
“Declining reimbursement is likely one of the major factors, if not the major factor in the decline in testing that has been observed nationally,” he said, explaining that reimbursement was below the break-even point for many physicians in freestanding medical practices, and that slight adjustments have applied only to facilities located in hospitals. As a result, the availability of DXA screening has declined.
The National Osteoporosis Foundation and other organizations such as the International Society for Clinical Densitometry are lobbying for changes, as there is a very strong link between testing and treatment.
“If we can’t get more people tested, we’re unlikely to get more people treated,” Dr. Saag said.
The availability of new agents for the treatment of osteoporosis could also lead to improvements in screening and care, he added.
In July, Amgen submitted to the Food and Drug Administration a supplemental new Biologics License Application for Prolia (denosumab) for the treatment of patients with GIOP. The application is based on a phase 3 study evaluating the safety and efficacy of Prolia, compared with risedronate, in patients receiving glucocorticoid treatment. Denosumab was also shown in a phase 3 study presented at the 2016 ACR meeting to result in greater improvement in bone mineral density vs. bisphosphonates across multiple sites, said Dr. Saag, an investigator for the trial.
“So we’re pleased about that finding, and we’re hopeful that eventually denosumab may become another treatment option,” he said, adding that having more choices leads to more personalized care for patients.
“We hope that, if it does receive approval and is utilized, that it may partially help address the gap in treatment that has been identified,” he said, adding that abaloparatide (Tymlos), which is approved for use in postmenopausal women with osteoporosis and high fracture risk, and romosozumab, currently in late-phase development, could also eventually help bridge the gap.
Recent guideline update
There is also optimism that a recent update to the 2010 guideline, published in August in Arthritis Care & Research, will help address the problem (Arthritis Care Res. 2017;69:1095-1110).
“We hope that one the most important impacts of the new 2017 ACR GIOP guideline will be increasing the awareness of GIOP care,” Dr. Ozen said, noting that changes in the new guideline will also be helpful for guiding management of certain patients not addressed in the 2010 guideline, including adults under age 40 years and children.
The new guideline also incorporates FRAX hip fracture scores into the risk-assessment recommendations .
“Lastly, the addition of other oral bisphosphonates and denosumab to the guideline has broadened the potential therapeutic options for physicians and patients,” she said.
Efforts by the ACR to make these guidelines widely known among clinicians could also help promote improved screening and treatment, said Dr. Buckley, a professor of internal medicine and pediatrics at Yale University, New Haven, Conn.
And that awareness is what is needed most, Dr. Ozen said.
“What we need in osteoporosis care of RA or GIOP patients is more awareness and education about risk-benefit ratios of antiosteoporotic medications instead of focusing on the medication type. We hope that our paper showing the worsening osteoporosis care and the new 2017 ACR GIOP guideline provide more awareness and guidance for the physicians managing these patients,” she said, adding that overcoming obstacles in osteoporosis care requires identification and attention to all potential causes for the suboptimal management of osteoporosis from both patients’ and physicians’ perspectives.
“With the improvement in management strategies of rheumatic diseases ... we anticipate improvement in life expectancy and cardiovascular outcomes in RA and inflammatory rheumatic diseases. In this regard, with aging and decreased but ongoing clinical or subclinical chronic inflammation, it is highly likely that we might be dealing with much older patients with higher osteoporosis and fracture risks. Considering the significant contribution of fractures on cost, disability, morbidity, and mortality of these diseases, rheumatologists and other specialists should work together more vigilantly to overcome the obstacles and improve osteoporosis care,” she said.
Dr. Ozen and Dr. Buckley reported having no conflicts of interest. Dr. Saag is an investigator and consultant for Amgen, Merck, and Radius Health, and is a consultant for Lilly.
FROM ARTHRITIS CARE & RESEARCH
Study finds low risk for jaw osteonecrosis with denosumab for postmenopausal osteoporosis
AT ASBMR
DENVER – Osteonecrosis of the jaw (ONJ) was a rare adverse event in women taking denosumab for postmenopausal osteoporosis, with a 0.7% rate for women who reported an invasive oral procedure or event while taking the drug and a 0.05% rate for women who did not have such procedures, Nelson Watts, MD, reported at the annual meeting of the American Society of Bone and Mineral Research.
The finding comes from a new analysis of a 7-year extension study of denosumab use in 4,550 women who participated in the 3-year, double-blind, phase 3 FREEDOM trial (NCT00089791) that compared denosumab 60 mg and placebo every 6 months. Those who missed 1 dose or fewer and completed visits through year 3 of the initial study were eligible to continue in the 7-year, open-label extension study. Those who had received placebo in the initial trial were crossed over to denosumab for the extension study.
Extension study participants were instructed to chronicle invasive oral procedures and events that had occurred in the initial trial and completed an oral event questionnaire once every 6 months of the extension trial.
All surveys were completed by 3,591 (79%) of the extension study participants, and 45.1% reported at least one invasive oral procedure or event during that time. The frequency of events was similar for the crossover and long-term denosumab groups; these events included scaling or root planing (29.1% and 28.5%), tooth extraction (25.1% and 24.6%), dental implant (5.8% and 6.0%), natural tooth loss (4.2% and 4.0%), and jaw surgery (0.9% and 0.9%). ONJ occurred at a rate of 5.2 cases per 10,000 patient-years of denosumab use, said Nelson Watts, MD, director of osteoporosis and bone health services at Mercy Health Services in Cincinnati, Ohio.
Of the 12 ONJ cases identified in the study, 11 occurred in women who reported an invasive oral procedure or event. This translated to a 0.7% risk of ONJ in women who reported an invasive oral procedure or event (11 in 1,621) and a 0.05% risk in women who did not (1 in 1,970).
The most common inciting event for ONJ appeared to be dental extractions, often of two or three teeth. The next most common dental issue associated with ONJ seemed to be poorly-fitted dentures.
ONJ resolved with treatment in 10 of 12 cases; one case was ongoing at the end of the study and one had an unknown outcome because the subject had withdrawn from the study. “With effective dental therapy, healing is the most likely outcome,” said Dr. Watts.
In clinical trials, ONJ occurred at a rate between 1 and 10 per 10,000 patient-years. A report in 2003, however, described severe ONJ in 36 cancer patients who received bisphosphonates (https://www.ncbi.nlm.nih.gov/pubmed/12966493).
The denosumab doses that cancer patients receive can be 10 to 12 times higher than the typical dose given to a postmenopausal woman being treated for osteoporosis.
“I can’t tell you how many phone calls I get from patients who are worried somehow or worried in situations created by their dentists that whatever procedure they’re going to have is going to end horribly,” Dr. Watts said. “In some cases dentists are telling my patients to either stop the drug that I’m giving them or to wait to get the next dose, and there’s absolutely nothing to support that.”
The study was funded by Amgen, the maker of denosumab (Prolia). Dr. Watts has received research support from Shire and has consulted for Abbvie, Amgen, and Radius. He is on the speakers’ bureau for Amgen, Radius, and Shire.
AT ASBMR
DENVER – Osteonecrosis of the jaw (ONJ) was a rare adverse event in women taking denosumab for postmenopausal osteoporosis, with a 0.7% rate for women who reported an invasive oral procedure or event while taking the drug and a 0.05% rate for women who did not have such procedures, Nelson Watts, MD, reported at the annual meeting of the American Society of Bone and Mineral Research.
The finding comes from a new analysis of a 7-year extension study of denosumab use in 4,550 women who participated in the 3-year, double-blind, phase 3 FREEDOM trial (NCT00089791) that compared denosumab 60 mg and placebo every 6 months. Those who missed 1 dose or fewer and completed visits through year 3 of the initial study were eligible to continue in the 7-year, open-label extension study. Those who had received placebo in the initial trial were crossed over to denosumab for the extension study.
Extension study participants were instructed to chronicle invasive oral procedures and events that had occurred in the initial trial and completed an oral event questionnaire once every 6 months of the extension trial.
All surveys were completed by 3,591 (79%) of the extension study participants, and 45.1% reported at least one invasive oral procedure or event during that time. The frequency of events was similar for the crossover and long-term denosumab groups; these events included scaling or root planing (29.1% and 28.5%), tooth extraction (25.1% and 24.6%), dental implant (5.8% and 6.0%), natural tooth loss (4.2% and 4.0%), and jaw surgery (0.9% and 0.9%). ONJ occurred at a rate of 5.2 cases per 10,000 patient-years of denosumab use, said Nelson Watts, MD, director of osteoporosis and bone health services at Mercy Health Services in Cincinnati, Ohio.
Of the 12 ONJ cases identified in the study, 11 occurred in women who reported an invasive oral procedure or event. This translated to a 0.7% risk of ONJ in women who reported an invasive oral procedure or event (11 in 1,621) and a 0.05% risk in women who did not (1 in 1,970).
The most common inciting event for ONJ appeared to be dental extractions, often of two or three teeth. The next most common dental issue associated with ONJ seemed to be poorly-fitted dentures.
ONJ resolved with treatment in 10 of 12 cases; one case was ongoing at the end of the study and one had an unknown outcome because the subject had withdrawn from the study. “With effective dental therapy, healing is the most likely outcome,” said Dr. Watts.
In clinical trials, ONJ occurred at a rate between 1 and 10 per 10,000 patient-years. A report in 2003, however, described severe ONJ in 36 cancer patients who received bisphosphonates (https://www.ncbi.nlm.nih.gov/pubmed/12966493).
The denosumab doses that cancer patients receive can be 10 to 12 times higher than the typical dose given to a postmenopausal woman being treated for osteoporosis.
“I can’t tell you how many phone calls I get from patients who are worried somehow or worried in situations created by their dentists that whatever procedure they’re going to have is going to end horribly,” Dr. Watts said. “In some cases dentists are telling my patients to either stop the drug that I’m giving them or to wait to get the next dose, and there’s absolutely nothing to support that.”
The study was funded by Amgen, the maker of denosumab (Prolia). Dr. Watts has received research support from Shire and has consulted for Abbvie, Amgen, and Radius. He is on the speakers’ bureau for Amgen, Radius, and Shire.
AT ASBMR
DENVER – Osteonecrosis of the jaw (ONJ) was a rare adverse event in women taking denosumab for postmenopausal osteoporosis, with a 0.7% rate for women who reported an invasive oral procedure or event while taking the drug and a 0.05% rate for women who did not have such procedures, Nelson Watts, MD, reported at the annual meeting of the American Society of Bone and Mineral Research.
The finding comes from a new analysis of a 7-year extension study of denosumab use in 4,550 women who participated in the 3-year, double-blind, phase 3 FREEDOM trial (NCT00089791) that compared denosumab 60 mg and placebo every 6 months. Those who missed 1 dose or fewer and completed visits through year 3 of the initial study were eligible to continue in the 7-year, open-label extension study. Those who had received placebo in the initial trial were crossed over to denosumab for the extension study.
Extension study participants were instructed to chronicle invasive oral procedures and events that had occurred in the initial trial and completed an oral event questionnaire once every 6 months of the extension trial.
All surveys were completed by 3,591 (79%) of the extension study participants, and 45.1% reported at least one invasive oral procedure or event during that time. The frequency of events was similar for the crossover and long-term denosumab groups; these events included scaling or root planing (29.1% and 28.5%), tooth extraction (25.1% and 24.6%), dental implant (5.8% and 6.0%), natural tooth loss (4.2% and 4.0%), and jaw surgery (0.9% and 0.9%). ONJ occurred at a rate of 5.2 cases per 10,000 patient-years of denosumab use, said Nelson Watts, MD, director of osteoporosis and bone health services at Mercy Health Services in Cincinnati, Ohio.
Of the 12 ONJ cases identified in the study, 11 occurred in women who reported an invasive oral procedure or event. This translated to a 0.7% risk of ONJ in women who reported an invasive oral procedure or event (11 in 1,621) and a 0.05% risk in women who did not (1 in 1,970).
The most common inciting event for ONJ appeared to be dental extractions, often of two or three teeth. The next most common dental issue associated with ONJ seemed to be poorly-fitted dentures.
ONJ resolved with treatment in 10 of 12 cases; one case was ongoing at the end of the study and one had an unknown outcome because the subject had withdrawn from the study. “With effective dental therapy, healing is the most likely outcome,” said Dr. Watts.
In clinical trials, ONJ occurred at a rate between 1 and 10 per 10,000 patient-years. A report in 2003, however, described severe ONJ in 36 cancer patients who received bisphosphonates (https://www.ncbi.nlm.nih.gov/pubmed/12966493).
The denosumab doses that cancer patients receive can be 10 to 12 times higher than the typical dose given to a postmenopausal woman being treated for osteoporosis.
“I can’t tell you how many phone calls I get from patients who are worried somehow or worried in situations created by their dentists that whatever procedure they’re going to have is going to end horribly,” Dr. Watts said. “In some cases dentists are telling my patients to either stop the drug that I’m giving them or to wait to get the next dose, and there’s absolutely nothing to support that.”
The study was funded by Amgen, the maker of denosumab (Prolia). Dr. Watts has received research support from Shire and has consulted for Abbvie, Amgen, and Radius. He is on the speakers’ bureau for Amgen, Radius, and Shire.
2017 Update on female sexual dysfunction
Sexual function is a complex, multifaceted process mediated by neurologic functions, hormonal regulation, and ps
As it turns out, quite a lot. Female sexual dysfunction is a common, vastly undertreated sexual health problem that can have wide-reaching effects on a woman’s life. These effects may include impaired body image, self-confidence, and self-worth. Sexual dysfunction also can contribute to relationship dissatisfaction and leave one feeling less connected with her partner.1,2 Studies have shown women with sexual dysfunction have higher health care expenditures3 and that depression and fatigue are common comorbidities, as is frequently seen in other chronic conditions such as diabetes and back pain.4
Understanding the pathogenesis of female sexual dysfunction helps to guide our approach to its management. Indeed, increased understanding of its pathology has helped to usher in new and emerging treatment options, as well as a personalized, biopsychosocial approach to its management.
Related article:
2016 Update on female sexual dysfunction
In this Update, I discuss the interplay of physiologic and psychological factors that affect female sexual function as well as the latest options for its management. I have also assembled a panel of experts to discuss 2 cases representative of sexual dysfunction that you may encounter in your clinical practice and how prescribing decisions are made for their management.
Read about factors that impact sexual function and agents to help manage dysfunction.
Multiple transmitters in the brain can increase or decrease sexual desire and function
Neurotransmitters involved in sexual excitation include brain dopamine, melanocortin, oxytocin, vasopressin, and norepinephrine, whereas brain opioids, serotonin, prolactin, and endocannabinoids function as sexual inhibitors. Inhibitory transmitters are activated normally during sexual refractoriness but also from primary aversion or secondary avoidance disorders.1 Drugs or conditions that reduce brain dopamine levels, increase the action of brain serotonin, or enhance brain opioid pathways have been shown to inhibit sexual desire, while those that increase hypothalamic and mesolimbic dopamine or decrease serotonin release have been shown to stimulate sexual desire.1
Estradiol and progesterone can impact sexual function and desire
In addition to the neurotransmitters, hormones are important modulators of female sexual function. Decreasing levels of circulating estrogen after menopause lead to physiologic, biologic, and clinical changes in the urogenital tissues, such as decreased elastin, thinning of the epithelium, reduced vaginal blood flow, diminished lubrication, and decreased flexibility and elasticity. These changes result in the symptoms of genitourinary syndrome of menopause (GSM), which affects as many as half of all menopausal women.5,6 In clinical trials, dyspareunia and vaginal dryness are the most bothersome GSM symptoms reported.7
The role of hormonal regulation in sexual dysfunction among premenopausal women is not yet fully understood, but we do know that estradiol has been shown to improve sexual desire, progesterone tends to dampen sexual desire, and that testosterone at physiological levels has been shown in most studies to have a neutral effect on sexual desire in a well-estrogenized patient.8
Related article:
Focus on treating genital atrophy symptoms
Experience and behavior modulate or reinforce sexual dysfunction
The most common psychological factors that trigger or amplify female sexual dysfunction are depression, anxiety, distraction, negative body image, sexual abuse, and emotional neglect.9 Contextual or sociocultural factors, such as relationship discord, life-stage stressors (the empty nest syndrome or anxiety and sleep deprivation from a new baby), as well as cultural or religious values that suppress sexuality, also should be considered.9 Experience-based neuroplasticity (changes in brain pathways that become solidified by negative or positive experiences) may elucidate how a multimodal approach, utilizing medical and psychological treatment, can be beneficial for patients, particularly those with hypoactive sexual desire disorder (HSDD).1
New and emerging approaches to managing female sexual dysfunction
Three agents, one of which has been available for prescription for some time, one that is newly available, and one in the pipeline, are or may soon be in the gynecologist's armamentarium.
Flibanserin
Medications that target excitatory pathways or blunt inhibitory pathways are in development, and one, flibanserin (Addyi), has been US Food and Drug Administration (FDA)-approved for the treatment of acquired, generalized HSDD in premenopausal women.1,10 Flibanserin is a nonhormonal, centrally acting, postsynaptic serotonin 1A receptor agonist and a serotonin 2A receptor antagonist that is taken daily at bedtime (100 mg); several weeks are usually needed before any effects are noted.1 It is not approved for postmenopausal women and has a boxed warning about the risks of hypotension and syncope; its use is contraindicated in women who drink alcohol, in those who have hepatic impairment, and with the use of moderate or strong CYP3A4 inhibitors.11
Also keep in mind that flibanserin is only available through a Risk Evaluation and Mitigation Strategy program, so clinicians who wish to prescribe it must enroll in and complete training to become certified providers.9
Related article:
What you need to know (and do) to prescribe the new drug flibanserin
Prasterone
Prasterone (Intrarosa), a once-daily intravaginal dehydroepiandrosterone (DHEA) product, is a prohormone that increases local estrogen and testosterone and has the advantage of improved sexual function, desire, arousal, lubrication, orgasm, satisfaction, as well as pain at sexual activity.12 It was approved by the FDA in November 2016 to treat moderate to severe dyspareunia and has been available for prescribing since July 2017. Its cost is comparable to topical estrogen products, with a $25 copay program.
Because prasterone is not an estrogen, it does not have the boxed warning that all estrogen products are mandated by the FDA to have. This may make it more acceptable to patients, who often decline to use an estrogen product after seeing the boxed warning on the package. The Centers for Medicare and Medicaid Services (CMS) does not have prasterone on its list of potentially hazardous drugs for the elderly. However, keep in mind that because its label is for dyspareunia and not specifically for GSM, CMS considers it a drug of choice--in other words, like sildenafil (Viagra), a lifestyle choice and not for treatment of a medical condition. As such, at the present time, Medicare does not cover it.
Bremelanotide
Late-stage trials of bremelanotide, a melanocortin receptor agonist, are underway. Its mechanism of action is somewhat like that of flibanserin in that both drugs increase dopamine and norepinephrine levels. The advantage of bremelanotide is that it is used as needed. It is dosed subcutaneously (1.75 mg) and it can be used as often as a woman would like to use it. The FDA is expected to consider it for approval in about a year. Unpublished data from poster sessions at recent meetings show that, in a phase 3 study of 1,247 premenopausal women with HSDD (who had already been screened for depression and were found to have a physiologic condition), improvements in desire, arousal, lubrication, and orgasm were shown with bremelanotide. About 18% of women stopped using the drug because of adverse effects (nausea, vomiting, flushing, or headache) versus 2% for placebo. Like flibanserin, it is expected to be approved for premenopausal women only.
Read how 3 experts would manage differing GSM symptoms.
What would you prescribe for these patients?
CASE Genitourinary syndrome of menopause (GSM) in a 55-year-old woman
A 55-year-old widow is beginning a new relationship. She has not had partnered sexual activity for several years, but she recently has begun a relationship. She describes pain with attempted penetration with her new partner. Her last menstrual period was 3 years ago and she has experienced very minor menopausal symptoms, which are not bothersome. On examination, the vulva and vagina are pale, with thin epithelium and absent rugae. The tissue lacks elasticity. A virginal speculum is needed to visualize the cervix.
How would you go about deciding which of the many options for management of GSM you will recommend for this patient? What do you weigh as you consider DHEA versus estrogen and topical versus oral therapy?
JoAnn V. Pinkerton, MD: Vulvovaginal atrophy (VVA), part of GSM, is associated with postmenopausal estrogen deficiency and includes the signs and symptoms seen on this patient's physical exam: vaginal narrowing, pallor, loss of elasticity, as well as pain with intercourse.6 Estrogen therapy is the most effective treatment for vaginal atrophy.13 Since she does not have significant menopausal symptoms, low-dose vaginal estrogen preparations are effective and generally safe treatments for VVA; these include creams, tablets containing estradiol or conjugated equine estrogen (CEE), and a low-dose vaginal estradiol ring--all available at doses that result in minimal systemic absorption.
Choice is usually made based on patient desire and likely adherence. If the patient prefers nonestrogen therapies that improve VVA and have been approved for relief of dyspareunia in postmenopausal women, I would discuss with the patient the oral selective estrogen receptor modulator ospemifene,14 and the new intravaginal DHEA suppositories, prasterone.15 Ospemifene is taken daily as an oral tablet, has a small risk of blood clots, and is my choice for women who do not need systemic hormone therapy and prefer to avoid vaginal therapy.
Andrew M. Kaunitz, MD: GSM is prevalent in menopausal women and, if not treated, causes progressive vaginal dryness and sexual discomfort. When the main indication for hormonal management in a menopausal woman is GSM (as opposed to treatment of vasomotor symptoms or prevention of osteoporosis), the treatment of choice is low-dose local vaginal estrogen, ospemifene, or prasterone (DHEA). Prasterone is a vaginally administered nonestrogen steroid that was approved by the FDA to treat dyspareunia associated with GSM. DHEA is an endogenous inactive steroid that is converted locally into androgens and estrogens; one vaginal insert is placed nightly.16,17
This 55-year-old widow has not been sexually active for some time. The facts that attempted penetration was painful and only an ultrathin (virginal) speculum could be used for examination indicate that contraction of the pelvic floor muscles is likely present. Simply starting medical management may not lead to comfortable/successful penetrative sex for this woman. In addition to medical management, she would likely benefit from referral for physical therapy. Using dilators and other strategies, along with the positive impact that medical management will have on the vaginal mucosa, a woman's physical therapist can work with this patient to help the pelvic floor muscles relax and facilitate comfortable penetrative sex.
James A. Simon, MD: With only minor vasomotor symptoms, I would assess the other potential benefits of a systemic therapy. These might include cardiovascular risk reduction (systemic estrogens or estrogens/progesterone in some), breast cancer risk reduction (some data suggesting ospemifene can accomplish this), osteoporosis prevention (systemic estrogens and estrogen/androgens), etc. If there is an option for a treatment to address more than one symptom, in this case GSM, assessing the risks/benefits of each of these therapies should be estimated for this specific patient.
If there are no systemic benefits to be had, then any of the local treatments should be helpful. As there are no head-to-head comparisons available, local estrogen cream, tablets, rings, local DHEA, or systemic ospemifene each should be considered possible treatments. I also feel this patient may benefit from supplementary self-dilation and/or physical therapy.
Related article:
2017 Update on menopause
CASE Dyspareunia and vasomotor symptoms in a 42-year-old breast cancer survivor
A 42-year-old woman with a BRCA1 mutation has undergone prophylactic mastectomies as well as hysterectomy with bilateral salpingo-oophorectomy. She reports mild to moderate hot flashes and bothersome vaginal dryness and dyspareunia. Examination confirms GSM.
Would you advise systemic hormone therapy for this patient? What would your recommendation be for management of her GSM symptoms?
Dr. Simon: While one's gut reaction would be to avoid systemic estrogen therapy in a patient with a BRCA1 mutation, the scientific information confirming this fear is lacking.18 Such patients may benefit significantly from systemic estrogen therapy (reduced risk of cardiovascular disease and cognitive decline, etc.), and with both breasts and both ovaries removed, estrogen's breast cancer risks, if any in this population, are largely avoided. The patient also may benefit from additional local therapy with either estrogens or DHEA.
Dr. Kaunitz: Due to her high lifetime risk of breast and ovarian cancer, this woman has proceeded with risk-reducing breast and gynecologic surgery. As more BRCA mutation carriers are being identified and undergo risk-reducing bilateral mastectomy (usually with reconstruction) and salpingo-oophorectomy, clinicians and mutation carriers more frequently face decisions regarding use of systemic hormone therapy.
Mutation carriers who have undergone bilateral risk-reducing mastectomy experience a very low baseline future risk for breast cancer; accordingly, concerns regarding this disease should not prevent use of systemic hormone therapy. Furthermore, without hormone replacement, induced menopause in women this age is associated with an elevated risk of osteoporosis, persistent vasomotor symptoms, cardiovascular disease, stroke, mood changes, dementia, Parkinson disease, and overall mortality. Recognizing the safety of estrogen therapy in this setting, this 42-year-old BRCA1 mutation carrier can initiate estrogen therapy. Standard dose estrogen therapy refers to oral estradiol 1.0 mg, conjugated equine estrogen 0.625 mg,or transdermal estradiol 0.05 mg. In younger women like this 42-year-old with surgically induced menopause, higher than standard replacement doses of estrogen are often appropriate.17
Due to concerns the hormone therapy might further increase future risk of breast cancer, some mutation carriers may delay or avoid risk-reducing bilateral salpingo-oophorectomy, a potentially lifesaving surgery which reduces not only future risk of ovarian cancer but also future risk for breast cancer.
Among mutation carriers with intact breasts, several studies address risk of breast cancer with use of systemic hormone therapy. Although limited in numbers of participants and years of follow-up, in aggregate, these studies provide reassurance that short-term use of systemic hormone therapy does not increase breast cancer risk in women with BRCA1 or BRCA2 mutations and intact breasts.19
Dr. Pinkerton: For this woman with early surgical menopause and hysterectomy, estrogen therapy could improve her vasomotor symptoms and decrease her risk of bone loss and GSM.17 In the Women's Health Initiative trial, there were 7 fewer breast cancers per 10,000 women-years in the estrogen-onlyarm.20 Observational studies suggest that hormone therapy, when given to the average age of menopause, decreases the risks of heart disease, Parkinson disease, and dementia.21 Limited observational evidence suggests that hormone therapy use does not further increase risk of breast cancer in women following oophorectomy for BRCA1 or BRCA2 gene mutation.22
The absolute risks observed with hormone therapy tended to be small, especially in younger, healthy women. Systemic hormone therapy could treat her hot flashes and her GSM symptoms and potentially decrease health risks associated with premature estrogen deficiency. Nonestrogen therapies for hot flashes include low-dose antidepressants, gabapentin, and mind-body options, such as cognitive behavioral therapy and hypnosis, but these would not decrease her health risks or treat her GSM.
If she only requests treatment of her GSM symptoms, she would be a candidate for low-dose vaginal estrogen therapy, given as a cream, tablet, or ring depending on her choice. I would not choose ospemifene as my first choice as she is having hot flashes, and there are no data yet on the drug's health benefits in early menopause. If she prefers nonestrogen vaginal therapy, the new intravaginal DHEA might be a good choice as both estrogen and testosterone are increased locally in the vagina while hormone levels remain in the postmenopausal range. There is no boxed warning on the patient insert, although safety in women with breast cancer or in those with elevated risk of breast cancer has not been tested.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Goldstein I, Kim NN, Clayton AH, et al. Hypoactive Sexual Desire Disorder: International Society for the Study of Women’s Sexual Health (ISSWSH) Expert Consensus Panel Review. Mayo Clin Proc. 2017;92(1):114–128.
- Kingsberg SA. Attitudinal survey of women living with low sexual desire. J Womens Health (Larchmt). 2014;23(10):817–823.
- Foley K, Foley D, Johnson BH. Healthcare resource utilization and expenditures of women diagnosed with hypoactive sexual desire disorder. J Med Econ. 2010;13(4):583–590.
- Biddle AK, West SL, D’Aloisio AA, Wheeler SB, Borisov NN, Thorp J. Hypoactive sexual desire disorder in postmenopausal women: quality of life and health burden. Value Health. 2009;12(5):763–772.
- Portman DJ, Gass ML; Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21(10):1063–1068.
- Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society. Menopause. 2013;20(9):888–902.
- Ettinger B, Hait H, Reape KZ, Shu H. Measuring symptom relief in studies of vaginal and vulvar atrophy: the most bothersome symptom approach. Menopause. 2008;15(5):885–889.
- Dennerstein L, Randolph J, Taffe J, Dudley E, Burger H. Hormones, mood, sexuality, and the menopausal transition. Fertil Steril. 2002;77(suppl 4):S42–S48.
- Brotto LA, Bitzer J, Laan E, Leiblum S, Luria M. Women’s sexual desire and arousal disorders [published correction appears in J Sex Med. 2010;7(2 pt 1):856]. J Sex Med. 2010;7(1 pt 2):586–614.
- US Food and Drug Administration website. FDA approves first treatment for sexual desire disorder. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm458734.htm. Accessed August 14, 2017.
- Addyi (flibanserin) [package insert]. Bridgewater, NJ: Valeant Pharmaceuticals North America, LLC; 2016.
- Labrie F, Derogatis L, Archer DF, et al; Members of the VVA Prasterone Research Group. Effect of intravaginal prasterone on sexual dysfunction in postmenopausal women with vulvovaginal atrophy. J Sex Med. 2015;12(12):2401–2412.
- Lethaby A, Ayeleke RO, Roberts H. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst Rev. 2016;8:CD001500.
- Portman DJ, Bachmann GA, Simon JA; Ospemifene Study Group. Ospemifene, a novel selective estrogen receptor modulator for treating dyspareunia associated with postmenopausal vulvar and vaginal atrophy. Menopause. 2013;20(6):623–630.
- Labrie F, Archer DF, Koltun, W, et al; VVA Prasterone Research Group. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2016;23(3):243–256.
- Kaunitz AM. Focus on treating genital atrophy symptoms. OBG Manag. 2017;29(1):14, 16–17.
- The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2017;24(7):728–753.
- Crandall CJ, Hovey KM, Andrews CA, et al. Breast cancer, endometrial cancer, and cardiovascular events in participants who used vaginal estrogen in the Women’s Health Initiative Observational Study. Menopause. August 14, 2017. doi:10.1097/GME.0000000000000956.
- Domchek S, Kaunitz AM. Use of systemic hormone therapy in BRCA mutation carriers. Menopause. 2016;23(9):1026–1027.
- Anderson GL, Limacher M, Assaf AR, et al; Women’s Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701–1712.
- Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015;18(4):483–491.
- Gabriel CA, Tigges-Cardwell J, Stopfer J, Erlichman J, Nathanson K, Domchek SM. Use of total abdominal hysterectomy and hormone replacement therapy in BRCA1 and BRCA2 mutation carriers undergoing risk-reducing salpingo-oophorectomy. Fam Cancer. 2009;8(1):23-28.
Sexual function is a complex, multifaceted process mediated by neurologic functions, hormonal regulation, and ps
As it turns out, quite a lot. Female sexual dysfunction is a common, vastly undertreated sexual health problem that can have wide-reaching effects on a woman’s life. These effects may include impaired body image, self-confidence, and self-worth. Sexual dysfunction also can contribute to relationship dissatisfaction and leave one feeling less connected with her partner.1,2 Studies have shown women with sexual dysfunction have higher health care expenditures3 and that depression and fatigue are common comorbidities, as is frequently seen in other chronic conditions such as diabetes and back pain.4
Understanding the pathogenesis of female sexual dysfunction helps to guide our approach to its management. Indeed, increased understanding of its pathology has helped to usher in new and emerging treatment options, as well as a personalized, biopsychosocial approach to its management.
Related article:
2016 Update on female sexual dysfunction
In this Update, I discuss the interplay of physiologic and psychological factors that affect female sexual function as well as the latest options for its management. I have also assembled a panel of experts to discuss 2 cases representative of sexual dysfunction that you may encounter in your clinical practice and how prescribing decisions are made for their management.
Read about factors that impact sexual function and agents to help manage dysfunction.
Multiple transmitters in the brain can increase or decrease sexual desire and function
Neurotransmitters involved in sexual excitation include brain dopamine, melanocortin, oxytocin, vasopressin, and norepinephrine, whereas brain opioids, serotonin, prolactin, and endocannabinoids function as sexual inhibitors. Inhibitory transmitters are activated normally during sexual refractoriness but also from primary aversion or secondary avoidance disorders.1 Drugs or conditions that reduce brain dopamine levels, increase the action of brain serotonin, or enhance brain opioid pathways have been shown to inhibit sexual desire, while those that increase hypothalamic and mesolimbic dopamine or decrease serotonin release have been shown to stimulate sexual desire.1
Estradiol and progesterone can impact sexual function and desire
In addition to the neurotransmitters, hormones are important modulators of female sexual function. Decreasing levels of circulating estrogen after menopause lead to physiologic, biologic, and clinical changes in the urogenital tissues, such as decreased elastin, thinning of the epithelium, reduced vaginal blood flow, diminished lubrication, and decreased flexibility and elasticity. These changes result in the symptoms of genitourinary syndrome of menopause (GSM), which affects as many as half of all menopausal women.5,6 In clinical trials, dyspareunia and vaginal dryness are the most bothersome GSM symptoms reported.7
The role of hormonal regulation in sexual dysfunction among premenopausal women is not yet fully understood, but we do know that estradiol has been shown to improve sexual desire, progesterone tends to dampen sexual desire, and that testosterone at physiological levels has been shown in most studies to have a neutral effect on sexual desire in a well-estrogenized patient.8
Related article:
Focus on treating genital atrophy symptoms
Experience and behavior modulate or reinforce sexual dysfunction
The most common psychological factors that trigger or amplify female sexual dysfunction are depression, anxiety, distraction, negative body image, sexual abuse, and emotional neglect.9 Contextual or sociocultural factors, such as relationship discord, life-stage stressors (the empty nest syndrome or anxiety and sleep deprivation from a new baby), as well as cultural or religious values that suppress sexuality, also should be considered.9 Experience-based neuroplasticity (changes in brain pathways that become solidified by negative or positive experiences) may elucidate how a multimodal approach, utilizing medical and psychological treatment, can be beneficial for patients, particularly those with hypoactive sexual desire disorder (HSDD).1
New and emerging approaches to managing female sexual dysfunction
Three agents, one of which has been available for prescription for some time, one that is newly available, and one in the pipeline, are or may soon be in the gynecologist's armamentarium.
Flibanserin
Medications that target excitatory pathways or blunt inhibitory pathways are in development, and one, flibanserin (Addyi), has been US Food and Drug Administration (FDA)-approved for the treatment of acquired, generalized HSDD in premenopausal women.1,10 Flibanserin is a nonhormonal, centrally acting, postsynaptic serotonin 1A receptor agonist and a serotonin 2A receptor antagonist that is taken daily at bedtime (100 mg); several weeks are usually needed before any effects are noted.1 It is not approved for postmenopausal women and has a boxed warning about the risks of hypotension and syncope; its use is contraindicated in women who drink alcohol, in those who have hepatic impairment, and with the use of moderate or strong CYP3A4 inhibitors.11
Also keep in mind that flibanserin is only available through a Risk Evaluation and Mitigation Strategy program, so clinicians who wish to prescribe it must enroll in and complete training to become certified providers.9
Related article:
What you need to know (and do) to prescribe the new drug flibanserin
Prasterone
Prasterone (Intrarosa), a once-daily intravaginal dehydroepiandrosterone (DHEA) product, is a prohormone that increases local estrogen and testosterone and has the advantage of improved sexual function, desire, arousal, lubrication, orgasm, satisfaction, as well as pain at sexual activity.12 It was approved by the FDA in November 2016 to treat moderate to severe dyspareunia and has been available for prescribing since July 2017. Its cost is comparable to topical estrogen products, with a $25 copay program.
Because prasterone is not an estrogen, it does not have the boxed warning that all estrogen products are mandated by the FDA to have. This may make it more acceptable to patients, who often decline to use an estrogen product after seeing the boxed warning on the package. The Centers for Medicare and Medicaid Services (CMS) does not have prasterone on its list of potentially hazardous drugs for the elderly. However, keep in mind that because its label is for dyspareunia and not specifically for GSM, CMS considers it a drug of choice--in other words, like sildenafil (Viagra), a lifestyle choice and not for treatment of a medical condition. As such, at the present time, Medicare does not cover it.
Bremelanotide
Late-stage trials of bremelanotide, a melanocortin receptor agonist, are underway. Its mechanism of action is somewhat like that of flibanserin in that both drugs increase dopamine and norepinephrine levels. The advantage of bremelanotide is that it is used as needed. It is dosed subcutaneously (1.75 mg) and it can be used as often as a woman would like to use it. The FDA is expected to consider it for approval in about a year. Unpublished data from poster sessions at recent meetings show that, in a phase 3 study of 1,247 premenopausal women with HSDD (who had already been screened for depression and were found to have a physiologic condition), improvements in desire, arousal, lubrication, and orgasm were shown with bremelanotide. About 18% of women stopped using the drug because of adverse effects (nausea, vomiting, flushing, or headache) versus 2% for placebo. Like flibanserin, it is expected to be approved for premenopausal women only.
Read how 3 experts would manage differing GSM symptoms.
What would you prescribe for these patients?
CASE Genitourinary syndrome of menopause (GSM) in a 55-year-old woman
A 55-year-old widow is beginning a new relationship. She has not had partnered sexual activity for several years, but she recently has begun a relationship. She describes pain with attempted penetration with her new partner. Her last menstrual period was 3 years ago and she has experienced very minor menopausal symptoms, which are not bothersome. On examination, the vulva and vagina are pale, with thin epithelium and absent rugae. The tissue lacks elasticity. A virginal speculum is needed to visualize the cervix.
How would you go about deciding which of the many options for management of GSM you will recommend for this patient? What do you weigh as you consider DHEA versus estrogen and topical versus oral therapy?
JoAnn V. Pinkerton, MD: Vulvovaginal atrophy (VVA), part of GSM, is associated with postmenopausal estrogen deficiency and includes the signs and symptoms seen on this patient's physical exam: vaginal narrowing, pallor, loss of elasticity, as well as pain with intercourse.6 Estrogen therapy is the most effective treatment for vaginal atrophy.13 Since she does not have significant menopausal symptoms, low-dose vaginal estrogen preparations are effective and generally safe treatments for VVA; these include creams, tablets containing estradiol or conjugated equine estrogen (CEE), and a low-dose vaginal estradiol ring--all available at doses that result in minimal systemic absorption.
Choice is usually made based on patient desire and likely adherence. If the patient prefers nonestrogen therapies that improve VVA and have been approved for relief of dyspareunia in postmenopausal women, I would discuss with the patient the oral selective estrogen receptor modulator ospemifene,14 and the new intravaginal DHEA suppositories, prasterone.15 Ospemifene is taken daily as an oral tablet, has a small risk of blood clots, and is my choice for women who do not need systemic hormone therapy and prefer to avoid vaginal therapy.
Andrew M. Kaunitz, MD: GSM is prevalent in menopausal women and, if not treated, causes progressive vaginal dryness and sexual discomfort. When the main indication for hormonal management in a menopausal woman is GSM (as opposed to treatment of vasomotor symptoms or prevention of osteoporosis), the treatment of choice is low-dose local vaginal estrogen, ospemifene, or prasterone (DHEA). Prasterone is a vaginally administered nonestrogen steroid that was approved by the FDA to treat dyspareunia associated with GSM. DHEA is an endogenous inactive steroid that is converted locally into androgens and estrogens; one vaginal insert is placed nightly.16,17
This 55-year-old widow has not been sexually active for some time. The facts that attempted penetration was painful and only an ultrathin (virginal) speculum could be used for examination indicate that contraction of the pelvic floor muscles is likely present. Simply starting medical management may not lead to comfortable/successful penetrative sex for this woman. In addition to medical management, she would likely benefit from referral for physical therapy. Using dilators and other strategies, along with the positive impact that medical management will have on the vaginal mucosa, a woman's physical therapist can work with this patient to help the pelvic floor muscles relax and facilitate comfortable penetrative sex.
James A. Simon, MD: With only minor vasomotor symptoms, I would assess the other potential benefits of a systemic therapy. These might include cardiovascular risk reduction (systemic estrogens or estrogens/progesterone in some), breast cancer risk reduction (some data suggesting ospemifene can accomplish this), osteoporosis prevention (systemic estrogens and estrogen/androgens), etc. If there is an option for a treatment to address more than one symptom, in this case GSM, assessing the risks/benefits of each of these therapies should be estimated for this specific patient.
If there are no systemic benefits to be had, then any of the local treatments should be helpful. As there are no head-to-head comparisons available, local estrogen cream, tablets, rings, local DHEA, or systemic ospemifene each should be considered possible treatments. I also feel this patient may benefit from supplementary self-dilation and/or physical therapy.
Related article:
2017 Update on menopause
CASE Dyspareunia and vasomotor symptoms in a 42-year-old breast cancer survivor
A 42-year-old woman with a BRCA1 mutation has undergone prophylactic mastectomies as well as hysterectomy with bilateral salpingo-oophorectomy. She reports mild to moderate hot flashes and bothersome vaginal dryness and dyspareunia. Examination confirms GSM.
Would you advise systemic hormone therapy for this patient? What would your recommendation be for management of her GSM symptoms?
Dr. Simon: While one's gut reaction would be to avoid systemic estrogen therapy in a patient with a BRCA1 mutation, the scientific information confirming this fear is lacking.18 Such patients may benefit significantly from systemic estrogen therapy (reduced risk of cardiovascular disease and cognitive decline, etc.), and with both breasts and both ovaries removed, estrogen's breast cancer risks, if any in this population, are largely avoided. The patient also may benefit from additional local therapy with either estrogens or DHEA.
Dr. Kaunitz: Due to her high lifetime risk of breast and ovarian cancer, this woman has proceeded with risk-reducing breast and gynecologic surgery. As more BRCA mutation carriers are being identified and undergo risk-reducing bilateral mastectomy (usually with reconstruction) and salpingo-oophorectomy, clinicians and mutation carriers more frequently face decisions regarding use of systemic hormone therapy.
Mutation carriers who have undergone bilateral risk-reducing mastectomy experience a very low baseline future risk for breast cancer; accordingly, concerns regarding this disease should not prevent use of systemic hormone therapy. Furthermore, without hormone replacement, induced menopause in women this age is associated with an elevated risk of osteoporosis, persistent vasomotor symptoms, cardiovascular disease, stroke, mood changes, dementia, Parkinson disease, and overall mortality. Recognizing the safety of estrogen therapy in this setting, this 42-year-old BRCA1 mutation carrier can initiate estrogen therapy. Standard dose estrogen therapy refers to oral estradiol 1.0 mg, conjugated equine estrogen 0.625 mg,or transdermal estradiol 0.05 mg. In younger women like this 42-year-old with surgically induced menopause, higher than standard replacement doses of estrogen are often appropriate.17
Due to concerns the hormone therapy might further increase future risk of breast cancer, some mutation carriers may delay or avoid risk-reducing bilateral salpingo-oophorectomy, a potentially lifesaving surgery which reduces not only future risk of ovarian cancer but also future risk for breast cancer.
Among mutation carriers with intact breasts, several studies address risk of breast cancer with use of systemic hormone therapy. Although limited in numbers of participants and years of follow-up, in aggregate, these studies provide reassurance that short-term use of systemic hormone therapy does not increase breast cancer risk in women with BRCA1 or BRCA2 mutations and intact breasts.19
Dr. Pinkerton: For this woman with early surgical menopause and hysterectomy, estrogen therapy could improve her vasomotor symptoms and decrease her risk of bone loss and GSM.17 In the Women's Health Initiative trial, there were 7 fewer breast cancers per 10,000 women-years in the estrogen-onlyarm.20 Observational studies suggest that hormone therapy, when given to the average age of menopause, decreases the risks of heart disease, Parkinson disease, and dementia.21 Limited observational evidence suggests that hormone therapy use does not further increase risk of breast cancer in women following oophorectomy for BRCA1 or BRCA2 gene mutation.22
The absolute risks observed with hormone therapy tended to be small, especially in younger, healthy women. Systemic hormone therapy could treat her hot flashes and her GSM symptoms and potentially decrease health risks associated with premature estrogen deficiency. Nonestrogen therapies for hot flashes include low-dose antidepressants, gabapentin, and mind-body options, such as cognitive behavioral therapy and hypnosis, but these would not decrease her health risks or treat her GSM.
If she only requests treatment of her GSM symptoms, she would be a candidate for low-dose vaginal estrogen therapy, given as a cream, tablet, or ring depending on her choice. I would not choose ospemifene as my first choice as she is having hot flashes, and there are no data yet on the drug's health benefits in early menopause. If she prefers nonestrogen vaginal therapy, the new intravaginal DHEA might be a good choice as both estrogen and testosterone are increased locally in the vagina while hormone levels remain in the postmenopausal range. There is no boxed warning on the patient insert, although safety in women with breast cancer or in those with elevated risk of breast cancer has not been tested.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Sexual function is a complex, multifaceted process mediated by neurologic functions, hormonal regulation, and ps
As it turns out, quite a lot. Female sexual dysfunction is a common, vastly undertreated sexual health problem that can have wide-reaching effects on a woman’s life. These effects may include impaired body image, self-confidence, and self-worth. Sexual dysfunction also can contribute to relationship dissatisfaction and leave one feeling less connected with her partner.1,2 Studies have shown women with sexual dysfunction have higher health care expenditures3 and that depression and fatigue are common comorbidities, as is frequently seen in other chronic conditions such as diabetes and back pain.4
Understanding the pathogenesis of female sexual dysfunction helps to guide our approach to its management. Indeed, increased understanding of its pathology has helped to usher in new and emerging treatment options, as well as a personalized, biopsychosocial approach to its management.
Related article:
2016 Update on female sexual dysfunction
In this Update, I discuss the interplay of physiologic and psychological factors that affect female sexual function as well as the latest options for its management. I have also assembled a panel of experts to discuss 2 cases representative of sexual dysfunction that you may encounter in your clinical practice and how prescribing decisions are made for their management.
Read about factors that impact sexual function and agents to help manage dysfunction.
Multiple transmitters in the brain can increase or decrease sexual desire and function
Neurotransmitters involved in sexual excitation include brain dopamine, melanocortin, oxytocin, vasopressin, and norepinephrine, whereas brain opioids, serotonin, prolactin, and endocannabinoids function as sexual inhibitors. Inhibitory transmitters are activated normally during sexual refractoriness but also from primary aversion or secondary avoidance disorders.1 Drugs or conditions that reduce brain dopamine levels, increase the action of brain serotonin, or enhance brain opioid pathways have been shown to inhibit sexual desire, while those that increase hypothalamic and mesolimbic dopamine or decrease serotonin release have been shown to stimulate sexual desire.1
Estradiol and progesterone can impact sexual function and desire
In addition to the neurotransmitters, hormones are important modulators of female sexual function. Decreasing levels of circulating estrogen after menopause lead to physiologic, biologic, and clinical changes in the urogenital tissues, such as decreased elastin, thinning of the epithelium, reduced vaginal blood flow, diminished lubrication, and decreased flexibility and elasticity. These changes result in the symptoms of genitourinary syndrome of menopause (GSM), which affects as many as half of all menopausal women.5,6 In clinical trials, dyspareunia and vaginal dryness are the most bothersome GSM symptoms reported.7
The role of hormonal regulation in sexual dysfunction among premenopausal women is not yet fully understood, but we do know that estradiol has been shown to improve sexual desire, progesterone tends to dampen sexual desire, and that testosterone at physiological levels has been shown in most studies to have a neutral effect on sexual desire in a well-estrogenized patient.8
Related article:
Focus on treating genital atrophy symptoms
Experience and behavior modulate or reinforce sexual dysfunction
The most common psychological factors that trigger or amplify female sexual dysfunction are depression, anxiety, distraction, negative body image, sexual abuse, and emotional neglect.9 Contextual or sociocultural factors, such as relationship discord, life-stage stressors (the empty nest syndrome or anxiety and sleep deprivation from a new baby), as well as cultural or religious values that suppress sexuality, also should be considered.9 Experience-based neuroplasticity (changes in brain pathways that become solidified by negative or positive experiences) may elucidate how a multimodal approach, utilizing medical and psychological treatment, can be beneficial for patients, particularly those with hypoactive sexual desire disorder (HSDD).1
New and emerging approaches to managing female sexual dysfunction
Three agents, one of which has been available for prescription for some time, one that is newly available, and one in the pipeline, are or may soon be in the gynecologist's armamentarium.
Flibanserin
Medications that target excitatory pathways or blunt inhibitory pathways are in development, and one, flibanserin (Addyi), has been US Food and Drug Administration (FDA)-approved for the treatment of acquired, generalized HSDD in premenopausal women.1,10 Flibanserin is a nonhormonal, centrally acting, postsynaptic serotonin 1A receptor agonist and a serotonin 2A receptor antagonist that is taken daily at bedtime (100 mg); several weeks are usually needed before any effects are noted.1 It is not approved for postmenopausal women and has a boxed warning about the risks of hypotension and syncope; its use is contraindicated in women who drink alcohol, in those who have hepatic impairment, and with the use of moderate or strong CYP3A4 inhibitors.11
Also keep in mind that flibanserin is only available through a Risk Evaluation and Mitigation Strategy program, so clinicians who wish to prescribe it must enroll in and complete training to become certified providers.9
Related article:
What you need to know (and do) to prescribe the new drug flibanserin
Prasterone
Prasterone (Intrarosa), a once-daily intravaginal dehydroepiandrosterone (DHEA) product, is a prohormone that increases local estrogen and testosterone and has the advantage of improved sexual function, desire, arousal, lubrication, orgasm, satisfaction, as well as pain at sexual activity.12 It was approved by the FDA in November 2016 to treat moderate to severe dyspareunia and has been available for prescribing since July 2017. Its cost is comparable to topical estrogen products, with a $25 copay program.
Because prasterone is not an estrogen, it does not have the boxed warning that all estrogen products are mandated by the FDA to have. This may make it more acceptable to patients, who often decline to use an estrogen product after seeing the boxed warning on the package. The Centers for Medicare and Medicaid Services (CMS) does not have prasterone on its list of potentially hazardous drugs for the elderly. However, keep in mind that because its label is for dyspareunia and not specifically for GSM, CMS considers it a drug of choice--in other words, like sildenafil (Viagra), a lifestyle choice and not for treatment of a medical condition. As such, at the present time, Medicare does not cover it.
Bremelanotide
Late-stage trials of bremelanotide, a melanocortin receptor agonist, are underway. Its mechanism of action is somewhat like that of flibanserin in that both drugs increase dopamine and norepinephrine levels. The advantage of bremelanotide is that it is used as needed. It is dosed subcutaneously (1.75 mg) and it can be used as often as a woman would like to use it. The FDA is expected to consider it for approval in about a year. Unpublished data from poster sessions at recent meetings show that, in a phase 3 study of 1,247 premenopausal women with HSDD (who had already been screened for depression and were found to have a physiologic condition), improvements in desire, arousal, lubrication, and orgasm were shown with bremelanotide. About 18% of women stopped using the drug because of adverse effects (nausea, vomiting, flushing, or headache) versus 2% for placebo. Like flibanserin, it is expected to be approved for premenopausal women only.
Read how 3 experts would manage differing GSM symptoms.
What would you prescribe for these patients?
CASE Genitourinary syndrome of menopause (GSM) in a 55-year-old woman
A 55-year-old widow is beginning a new relationship. She has not had partnered sexual activity for several years, but she recently has begun a relationship. She describes pain with attempted penetration with her new partner. Her last menstrual period was 3 years ago and she has experienced very minor menopausal symptoms, which are not bothersome. On examination, the vulva and vagina are pale, with thin epithelium and absent rugae. The tissue lacks elasticity. A virginal speculum is needed to visualize the cervix.
How would you go about deciding which of the many options for management of GSM you will recommend for this patient? What do you weigh as you consider DHEA versus estrogen and topical versus oral therapy?
JoAnn V. Pinkerton, MD: Vulvovaginal atrophy (VVA), part of GSM, is associated with postmenopausal estrogen deficiency and includes the signs and symptoms seen on this patient's physical exam: vaginal narrowing, pallor, loss of elasticity, as well as pain with intercourse.6 Estrogen therapy is the most effective treatment for vaginal atrophy.13 Since she does not have significant menopausal symptoms, low-dose vaginal estrogen preparations are effective and generally safe treatments for VVA; these include creams, tablets containing estradiol or conjugated equine estrogen (CEE), and a low-dose vaginal estradiol ring--all available at doses that result in minimal systemic absorption.
Choice is usually made based on patient desire and likely adherence. If the patient prefers nonestrogen therapies that improve VVA and have been approved for relief of dyspareunia in postmenopausal women, I would discuss with the patient the oral selective estrogen receptor modulator ospemifene,14 and the new intravaginal DHEA suppositories, prasterone.15 Ospemifene is taken daily as an oral tablet, has a small risk of blood clots, and is my choice for women who do not need systemic hormone therapy and prefer to avoid vaginal therapy.
Andrew M. Kaunitz, MD: GSM is prevalent in menopausal women and, if not treated, causes progressive vaginal dryness and sexual discomfort. When the main indication for hormonal management in a menopausal woman is GSM (as opposed to treatment of vasomotor symptoms or prevention of osteoporosis), the treatment of choice is low-dose local vaginal estrogen, ospemifene, or prasterone (DHEA). Prasterone is a vaginally administered nonestrogen steroid that was approved by the FDA to treat dyspareunia associated with GSM. DHEA is an endogenous inactive steroid that is converted locally into androgens and estrogens; one vaginal insert is placed nightly.16,17
This 55-year-old widow has not been sexually active for some time. The facts that attempted penetration was painful and only an ultrathin (virginal) speculum could be used for examination indicate that contraction of the pelvic floor muscles is likely present. Simply starting medical management may not lead to comfortable/successful penetrative sex for this woman. In addition to medical management, she would likely benefit from referral for physical therapy. Using dilators and other strategies, along with the positive impact that medical management will have on the vaginal mucosa, a woman's physical therapist can work with this patient to help the pelvic floor muscles relax and facilitate comfortable penetrative sex.
James A. Simon, MD: With only minor vasomotor symptoms, I would assess the other potential benefits of a systemic therapy. These might include cardiovascular risk reduction (systemic estrogens or estrogens/progesterone in some), breast cancer risk reduction (some data suggesting ospemifene can accomplish this), osteoporosis prevention (systemic estrogens and estrogen/androgens), etc. If there is an option for a treatment to address more than one symptom, in this case GSM, assessing the risks/benefits of each of these therapies should be estimated for this specific patient.
If there are no systemic benefits to be had, then any of the local treatments should be helpful. As there are no head-to-head comparisons available, local estrogen cream, tablets, rings, local DHEA, or systemic ospemifene each should be considered possible treatments. I also feel this patient may benefit from supplementary self-dilation and/or physical therapy.
Related article:
2017 Update on menopause
CASE Dyspareunia and vasomotor symptoms in a 42-year-old breast cancer survivor
A 42-year-old woman with a BRCA1 mutation has undergone prophylactic mastectomies as well as hysterectomy with bilateral salpingo-oophorectomy. She reports mild to moderate hot flashes and bothersome vaginal dryness and dyspareunia. Examination confirms GSM.
Would you advise systemic hormone therapy for this patient? What would your recommendation be for management of her GSM symptoms?
Dr. Simon: While one's gut reaction would be to avoid systemic estrogen therapy in a patient with a BRCA1 mutation, the scientific information confirming this fear is lacking.18 Such patients may benefit significantly from systemic estrogen therapy (reduced risk of cardiovascular disease and cognitive decline, etc.), and with both breasts and both ovaries removed, estrogen's breast cancer risks, if any in this population, are largely avoided. The patient also may benefit from additional local therapy with either estrogens or DHEA.
Dr. Kaunitz: Due to her high lifetime risk of breast and ovarian cancer, this woman has proceeded with risk-reducing breast and gynecologic surgery. As more BRCA mutation carriers are being identified and undergo risk-reducing bilateral mastectomy (usually with reconstruction) and salpingo-oophorectomy, clinicians and mutation carriers more frequently face decisions regarding use of systemic hormone therapy.
Mutation carriers who have undergone bilateral risk-reducing mastectomy experience a very low baseline future risk for breast cancer; accordingly, concerns regarding this disease should not prevent use of systemic hormone therapy. Furthermore, without hormone replacement, induced menopause in women this age is associated with an elevated risk of osteoporosis, persistent vasomotor symptoms, cardiovascular disease, stroke, mood changes, dementia, Parkinson disease, and overall mortality. Recognizing the safety of estrogen therapy in this setting, this 42-year-old BRCA1 mutation carrier can initiate estrogen therapy. Standard dose estrogen therapy refers to oral estradiol 1.0 mg, conjugated equine estrogen 0.625 mg,or transdermal estradiol 0.05 mg. In younger women like this 42-year-old with surgically induced menopause, higher than standard replacement doses of estrogen are often appropriate.17
Due to concerns the hormone therapy might further increase future risk of breast cancer, some mutation carriers may delay or avoid risk-reducing bilateral salpingo-oophorectomy, a potentially lifesaving surgery which reduces not only future risk of ovarian cancer but also future risk for breast cancer.
Among mutation carriers with intact breasts, several studies address risk of breast cancer with use of systemic hormone therapy. Although limited in numbers of participants and years of follow-up, in aggregate, these studies provide reassurance that short-term use of systemic hormone therapy does not increase breast cancer risk in women with BRCA1 or BRCA2 mutations and intact breasts.19
Dr. Pinkerton: For this woman with early surgical menopause and hysterectomy, estrogen therapy could improve her vasomotor symptoms and decrease her risk of bone loss and GSM.17 In the Women's Health Initiative trial, there were 7 fewer breast cancers per 10,000 women-years in the estrogen-onlyarm.20 Observational studies suggest that hormone therapy, when given to the average age of menopause, decreases the risks of heart disease, Parkinson disease, and dementia.21 Limited observational evidence suggests that hormone therapy use does not further increase risk of breast cancer in women following oophorectomy for BRCA1 or BRCA2 gene mutation.22
The absolute risks observed with hormone therapy tended to be small, especially in younger, healthy women. Systemic hormone therapy could treat her hot flashes and her GSM symptoms and potentially decrease health risks associated with premature estrogen deficiency. Nonestrogen therapies for hot flashes include low-dose antidepressants, gabapentin, and mind-body options, such as cognitive behavioral therapy and hypnosis, but these would not decrease her health risks or treat her GSM.
If she only requests treatment of her GSM symptoms, she would be a candidate for low-dose vaginal estrogen therapy, given as a cream, tablet, or ring depending on her choice. I would not choose ospemifene as my first choice as she is having hot flashes, and there are no data yet on the drug's health benefits in early menopause. If she prefers nonestrogen vaginal therapy, the new intravaginal DHEA might be a good choice as both estrogen and testosterone are increased locally in the vagina while hormone levels remain in the postmenopausal range. There is no boxed warning on the patient insert, although safety in women with breast cancer or in those with elevated risk of breast cancer has not been tested.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Goldstein I, Kim NN, Clayton AH, et al. Hypoactive Sexual Desire Disorder: International Society for the Study of Women’s Sexual Health (ISSWSH) Expert Consensus Panel Review. Mayo Clin Proc. 2017;92(1):114–128.
- Kingsberg SA. Attitudinal survey of women living with low sexual desire. J Womens Health (Larchmt). 2014;23(10):817–823.
- Foley K, Foley D, Johnson BH. Healthcare resource utilization and expenditures of women diagnosed with hypoactive sexual desire disorder. J Med Econ. 2010;13(4):583–590.
- Biddle AK, West SL, D’Aloisio AA, Wheeler SB, Borisov NN, Thorp J. Hypoactive sexual desire disorder in postmenopausal women: quality of life and health burden. Value Health. 2009;12(5):763–772.
- Portman DJ, Gass ML; Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21(10):1063–1068.
- Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society. Menopause. 2013;20(9):888–902.
- Ettinger B, Hait H, Reape KZ, Shu H. Measuring symptom relief in studies of vaginal and vulvar atrophy: the most bothersome symptom approach. Menopause. 2008;15(5):885–889.
- Dennerstein L, Randolph J, Taffe J, Dudley E, Burger H. Hormones, mood, sexuality, and the menopausal transition. Fertil Steril. 2002;77(suppl 4):S42–S48.
- Brotto LA, Bitzer J, Laan E, Leiblum S, Luria M. Women’s sexual desire and arousal disorders [published correction appears in J Sex Med. 2010;7(2 pt 1):856]. J Sex Med. 2010;7(1 pt 2):586–614.
- US Food and Drug Administration website. FDA approves first treatment for sexual desire disorder. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm458734.htm. Accessed August 14, 2017.
- Addyi (flibanserin) [package insert]. Bridgewater, NJ: Valeant Pharmaceuticals North America, LLC; 2016.
- Labrie F, Derogatis L, Archer DF, et al; Members of the VVA Prasterone Research Group. Effect of intravaginal prasterone on sexual dysfunction in postmenopausal women with vulvovaginal atrophy. J Sex Med. 2015;12(12):2401–2412.
- Lethaby A, Ayeleke RO, Roberts H. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst Rev. 2016;8:CD001500.
- Portman DJ, Bachmann GA, Simon JA; Ospemifene Study Group. Ospemifene, a novel selective estrogen receptor modulator for treating dyspareunia associated with postmenopausal vulvar and vaginal atrophy. Menopause. 2013;20(6):623–630.
- Labrie F, Archer DF, Koltun, W, et al; VVA Prasterone Research Group. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2016;23(3):243–256.
- Kaunitz AM. Focus on treating genital atrophy symptoms. OBG Manag. 2017;29(1):14, 16–17.
- The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2017;24(7):728–753.
- Crandall CJ, Hovey KM, Andrews CA, et al. Breast cancer, endometrial cancer, and cardiovascular events in participants who used vaginal estrogen in the Women’s Health Initiative Observational Study. Menopause. August 14, 2017. doi:10.1097/GME.0000000000000956.
- Domchek S, Kaunitz AM. Use of systemic hormone therapy in BRCA mutation carriers. Menopause. 2016;23(9):1026–1027.
- Anderson GL, Limacher M, Assaf AR, et al; Women’s Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701–1712.
- Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015;18(4):483–491.
- Gabriel CA, Tigges-Cardwell J, Stopfer J, Erlichman J, Nathanson K, Domchek SM. Use of total abdominal hysterectomy and hormone replacement therapy in BRCA1 and BRCA2 mutation carriers undergoing risk-reducing salpingo-oophorectomy. Fam Cancer. 2009;8(1):23-28.
- Goldstein I, Kim NN, Clayton AH, et al. Hypoactive Sexual Desire Disorder: International Society for the Study of Women’s Sexual Health (ISSWSH) Expert Consensus Panel Review. Mayo Clin Proc. 2017;92(1):114–128.
- Kingsberg SA. Attitudinal survey of women living with low sexual desire. J Womens Health (Larchmt). 2014;23(10):817–823.
- Foley K, Foley D, Johnson BH. Healthcare resource utilization and expenditures of women diagnosed with hypoactive sexual desire disorder. J Med Econ. 2010;13(4):583–590.
- Biddle AK, West SL, D’Aloisio AA, Wheeler SB, Borisov NN, Thorp J. Hypoactive sexual desire disorder in postmenopausal women: quality of life and health burden. Value Health. 2009;12(5):763–772.
- Portman DJ, Gass ML; Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21(10):1063–1068.
- Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society. Menopause. 2013;20(9):888–902.
- Ettinger B, Hait H, Reape KZ, Shu H. Measuring symptom relief in studies of vaginal and vulvar atrophy: the most bothersome symptom approach. Menopause. 2008;15(5):885–889.
- Dennerstein L, Randolph J, Taffe J, Dudley E, Burger H. Hormones, mood, sexuality, and the menopausal transition. Fertil Steril. 2002;77(suppl 4):S42–S48.
- Brotto LA, Bitzer J, Laan E, Leiblum S, Luria M. Women’s sexual desire and arousal disorders [published correction appears in J Sex Med. 2010;7(2 pt 1):856]. J Sex Med. 2010;7(1 pt 2):586–614.
- US Food and Drug Administration website. FDA approves first treatment for sexual desire disorder. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm458734.htm. Accessed August 14, 2017.
- Addyi (flibanserin) [package insert]. Bridgewater, NJ: Valeant Pharmaceuticals North America, LLC; 2016.
- Labrie F, Derogatis L, Archer DF, et al; Members of the VVA Prasterone Research Group. Effect of intravaginal prasterone on sexual dysfunction in postmenopausal women with vulvovaginal atrophy. J Sex Med. 2015;12(12):2401–2412.
- Lethaby A, Ayeleke RO, Roberts H. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst Rev. 2016;8:CD001500.
- Portman DJ, Bachmann GA, Simon JA; Ospemifene Study Group. Ospemifene, a novel selective estrogen receptor modulator for treating dyspareunia associated with postmenopausal vulvar and vaginal atrophy. Menopause. 2013;20(6):623–630.
- Labrie F, Archer DF, Koltun, W, et al; VVA Prasterone Research Group. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2016;23(3):243–256.
- Kaunitz AM. Focus on treating genital atrophy symptoms. OBG Manag. 2017;29(1):14, 16–17.
- The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2017;24(7):728–753.
- Crandall CJ, Hovey KM, Andrews CA, et al. Breast cancer, endometrial cancer, and cardiovascular events in participants who used vaginal estrogen in the Women’s Health Initiative Observational Study. Menopause. August 14, 2017. doi:10.1097/GME.0000000000000956.
- Domchek S, Kaunitz AM. Use of systemic hormone therapy in BRCA mutation carriers. Menopause. 2016;23(9):1026–1027.
- Anderson GL, Limacher M, Assaf AR, et al; Women’s Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701–1712.
- Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015;18(4):483–491.
- Gabriel CA, Tigges-Cardwell J, Stopfer J, Erlichman J, Nathanson K, Domchek SM. Use of total abdominal hysterectomy and hormone replacement therapy in BRCA1 and BRCA2 mutation carriers undergoing risk-reducing salpingo-oophorectomy. Fam Cancer. 2009;8(1):23-28.
Fast Tracks
- Although not fully understood how, estradiol can improve sexual desire, progesterone tends to dampen sexual desire, and testosterone has a neutral effect in premenopausal women
- Newly available since July 2017, prasterone is a once-daily intravaginal agent that treats moderate to severe dyspareunia and has costs similar to topical estrogens
- Estrogen therapy may be considered in a breast cancer mutation carrier who has undergone prophylactic mastectomies and bilateral salpingo-oophorectomy
How to rule out secondary causes of osteoporosis
ESTES PARK, COLO. – Everyone diagnosed with osteoporosis deserves a laboratory assessment to rule out unsuspected secondary causes, according to Sterling West, MD. And he’s got a doozy of a workup he recommends to primary care physicians as “incredibly cost effective.”
“With this workup you’ll identify 98% of abnormalities at a mean cost of $366 per diagnosis. That’s incredibly cost effective. You’re going to get a lot of information with actually not very much outlay at all,” he said at a conference on internal medicine sponsored by the University of Colorado.
The tests he advocates that primary care physicians order in all their patients with osteoporosis include a complete blood count, a complete metabolic panel, a 24-hour urine calcium/sodium/creatinine, a serum 25-hydroxyvitamin D level, and a serum phosphorus. In addition, men with osteoporosis should have their serum testosterone measured. A thyroid-stimulating hormone level should be obtained in patients who are taking thyroxine or if they look clinically hyperthyroid.
A measurement of parathyroid hormone is warranted as part of the screen in patients with an abnormal serum calcium. If the parathyroid hormone is normal, hyperparathyroidism can be ruled out.
Ordering a serum protein electrophoresis to check for multiple myeloma is appropriate in osteoporotic patients over age 50 years with an abnormal complete blood count.
This basic laboratory workup will identify patients with the relatively common secondary causes of low bone mineral density which account for 98% of all cases. These causes include vitamin D deficiency, malabsorption, hypogonadism, hypercalciuria, and myeloma.
“Leave the other 2% to me,” the rheumatologist suggested.
Special laboratory tests Dr. Sterling recommended that are best left to bone disease specialists include bone turnover markers, a serum tryptase/urine N-methylhistamine to screen for systemic mastocytosis, antitransglutaminase antibodies for celiac disease, a 24-hour urinary free cortisol and/or overnight dexamethasone suppression test to identify patients with Cushing syndrome, and bone biopsy.
Who should be referred to a bone specialist for a more extensive workup?
“If somebody is losing bone or fracturing and they’re on appropriate therapy and you believe they’re taking their medication, that’s for sure somebody that we should see. Also, a premenopausal woman with a high Z score who has had a fracture that’s atypical. And patients with stage 4 or 5 chronic kidney disease; those are some of the toughest cases and are best referred to a bone expert,” Dr. Sterling said.
On the other hand, if an osteoporotic patient simply can’t tolerate guideline-recommended initial therapy with an oral bisphosphonate such as alendronate (Fosamax) or risedronate (Actonel), there’s no need to bring in a specialist. Simply switch the patient to denosumab (Prolia), a monoclonal antibody against receptor activator of nuclear factor kappa-B ligand, administered by subcutaneous injection once every 6 months. The cost is about $2,200 per year, but the drug is covered by Medicare Part B. Clinical trials have demonstrated that denosumab boosts bone mineral density by 6%-9%, with an absolute 5% reduction in fractures and a 40%-68% relative risk reduction, he noted.
Dr. West reported having no financial conflicts of interest regarding his presentation.
ESTES PARK, COLO. – Everyone diagnosed with osteoporosis deserves a laboratory assessment to rule out unsuspected secondary causes, according to Sterling West, MD. And he’s got a doozy of a workup he recommends to primary care physicians as “incredibly cost effective.”
“With this workup you’ll identify 98% of abnormalities at a mean cost of $366 per diagnosis. That’s incredibly cost effective. You’re going to get a lot of information with actually not very much outlay at all,” he said at a conference on internal medicine sponsored by the University of Colorado.
The tests he advocates that primary care physicians order in all their patients with osteoporosis include a complete blood count, a complete metabolic panel, a 24-hour urine calcium/sodium/creatinine, a serum 25-hydroxyvitamin D level, and a serum phosphorus. In addition, men with osteoporosis should have their serum testosterone measured. A thyroid-stimulating hormone level should be obtained in patients who are taking thyroxine or if they look clinically hyperthyroid.
A measurement of parathyroid hormone is warranted as part of the screen in patients with an abnormal serum calcium. If the parathyroid hormone is normal, hyperparathyroidism can be ruled out.
Ordering a serum protein electrophoresis to check for multiple myeloma is appropriate in osteoporotic patients over age 50 years with an abnormal complete blood count.
This basic laboratory workup will identify patients with the relatively common secondary causes of low bone mineral density which account for 98% of all cases. These causes include vitamin D deficiency, malabsorption, hypogonadism, hypercalciuria, and myeloma.
“Leave the other 2% to me,” the rheumatologist suggested.
Special laboratory tests Dr. Sterling recommended that are best left to bone disease specialists include bone turnover markers, a serum tryptase/urine N-methylhistamine to screen for systemic mastocytosis, antitransglutaminase antibodies for celiac disease, a 24-hour urinary free cortisol and/or overnight dexamethasone suppression test to identify patients with Cushing syndrome, and bone biopsy.
Who should be referred to a bone specialist for a more extensive workup?
“If somebody is losing bone or fracturing and they’re on appropriate therapy and you believe they’re taking their medication, that’s for sure somebody that we should see. Also, a premenopausal woman with a high Z score who has had a fracture that’s atypical. And patients with stage 4 or 5 chronic kidney disease; those are some of the toughest cases and are best referred to a bone expert,” Dr. Sterling said.
On the other hand, if an osteoporotic patient simply can’t tolerate guideline-recommended initial therapy with an oral bisphosphonate such as alendronate (Fosamax) or risedronate (Actonel), there’s no need to bring in a specialist. Simply switch the patient to denosumab (Prolia), a monoclonal antibody against receptor activator of nuclear factor kappa-B ligand, administered by subcutaneous injection once every 6 months. The cost is about $2,200 per year, but the drug is covered by Medicare Part B. Clinical trials have demonstrated that denosumab boosts bone mineral density by 6%-9%, with an absolute 5% reduction in fractures and a 40%-68% relative risk reduction, he noted.
Dr. West reported having no financial conflicts of interest regarding his presentation.
ESTES PARK, COLO. – Everyone diagnosed with osteoporosis deserves a laboratory assessment to rule out unsuspected secondary causes, according to Sterling West, MD. And he’s got a doozy of a workup he recommends to primary care physicians as “incredibly cost effective.”
“With this workup you’ll identify 98% of abnormalities at a mean cost of $366 per diagnosis. That’s incredibly cost effective. You’re going to get a lot of information with actually not very much outlay at all,” he said at a conference on internal medicine sponsored by the University of Colorado.
The tests he advocates that primary care physicians order in all their patients with osteoporosis include a complete blood count, a complete metabolic panel, a 24-hour urine calcium/sodium/creatinine, a serum 25-hydroxyvitamin D level, and a serum phosphorus. In addition, men with osteoporosis should have their serum testosterone measured. A thyroid-stimulating hormone level should be obtained in patients who are taking thyroxine or if they look clinically hyperthyroid.
A measurement of parathyroid hormone is warranted as part of the screen in patients with an abnormal serum calcium. If the parathyroid hormone is normal, hyperparathyroidism can be ruled out.
Ordering a serum protein electrophoresis to check for multiple myeloma is appropriate in osteoporotic patients over age 50 years with an abnormal complete blood count.
This basic laboratory workup will identify patients with the relatively common secondary causes of low bone mineral density which account for 98% of all cases. These causes include vitamin D deficiency, malabsorption, hypogonadism, hypercalciuria, and myeloma.
“Leave the other 2% to me,” the rheumatologist suggested.
Special laboratory tests Dr. Sterling recommended that are best left to bone disease specialists include bone turnover markers, a serum tryptase/urine N-methylhistamine to screen for systemic mastocytosis, antitransglutaminase antibodies for celiac disease, a 24-hour urinary free cortisol and/or overnight dexamethasone suppression test to identify patients with Cushing syndrome, and bone biopsy.
Who should be referred to a bone specialist for a more extensive workup?
“If somebody is losing bone or fracturing and they’re on appropriate therapy and you believe they’re taking their medication, that’s for sure somebody that we should see. Also, a premenopausal woman with a high Z score who has had a fracture that’s atypical. And patients with stage 4 or 5 chronic kidney disease; those are some of the toughest cases and are best referred to a bone expert,” Dr. Sterling said.
On the other hand, if an osteoporotic patient simply can’t tolerate guideline-recommended initial therapy with an oral bisphosphonate such as alendronate (Fosamax) or risedronate (Actonel), there’s no need to bring in a specialist. Simply switch the patient to denosumab (Prolia), a monoclonal antibody against receptor activator of nuclear factor kappa-B ligand, administered by subcutaneous injection once every 6 months. The cost is about $2,200 per year, but the drug is covered by Medicare Part B. Clinical trials have demonstrated that denosumab boosts bone mineral density by 6%-9%, with an absolute 5% reduction in fractures and a 40%-68% relative risk reduction, he noted.
Dr. West reported having no financial conflicts of interest regarding his presentation.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM
Anabolic agents for osteoporosis have limited role so far
SAN FRANCISCO – Parathyroid hormone and parathyroid hormone–related protein analogs show promise for treating osteoporosis, but, for now, they’re reserved for the most severe cases.
Teriparatide, a parathyroid hormone analog, is the first treatment that stimulates bone formation instead of inhibiting bone resorption, but studies to date are too small to evaluate its effect on hip fractures, Jeffrey A. Tice, MD, said at the UCSF Annual Advances in Internal Medicine meeting.
Abaloparatide, a parathyroid hormone-related protein analog approved in April 2017, requires subcutaneous dosing of 80 mcg daily for up to 2 years and has been found to increase bone density in the spine by 11% and in the hip by 4%, compared with placebo, over 18 months. In women with pre-existing vertebral fractures, the agent was found to reduce the incidence of vertebral fractures by 86% and nonvertebral fragility fractures by 43%, but data are not adequate to evaluate its effect on hip fractures. Adverse reactions include hypercalciuria, nausea, hypercalcemia, orthostatic hypotension, tachycardia, and injection site reactions.
Studies to date have shown that combining either teriparatide or abaloparatide with an antiresorptive drug is less effective than either agent alone. However, both agents must be followed by an antiresorptive agent. “These drugs are expensive,” Dr. Tice said. “Right now, they’re reserved for patients with severe osteoporosis.”
The lifetime risk for osteoporotic fractures is 50% in women and 20% in men, and they cause significant morbidity and mortality. Among U.S. hospitalizations for women 55 years and older between 2000 and 2012, Dr. Tice noted, 4.9 million were for osteoporotic fractures, 3 million were for stroke, and 2.9 million were for myocardial infarction.
“Osteoporosis is a very common condition, but it’s under-recognized, in part because it’s a silent disease,” he said. “Only 20%-30% of patients with bone mineral densities less than –2.5 are treated in this country. And, 12 months after hip fracture, only 2% had a dual-energy x-ray absorptiometry [DXA] test, and only 15% were treated with an appropriate drug. We should be asking about fracture history, note vertebral fractures, treat those patients, and we should remember to use chart reminders for DXA.”
Clinical guidelines from the American College of Physicians and other groups recommend alendronate, risedronate, zoledronic acid, or denosumab as first-line therapy for women with osteoporosis. “There are no head to head trials to indicate which agent is best,” Dr. Tice said. “They reduce the fracture risk by 30%-50%, primarily in patients with an existing vertebral fracture or a T score below –2.5.” The use of hormone therapy and raloxifene are generally not recommended.
In a review published in the New England Journal of Medicine, researchers Dennis M. Black, MD, and Clifford J. Rosen, MD, estimated the number of patients needed to treat for 3 years to prevent various fractures (N Engl J Med. 2016 Jan 21;374[3]:254-62). They found that, for nonvertebral fractures, including hip, 35 patients need to be treated for 3 years to prevent one of those fractures, 90 patients for 3 years to prevent one hip fracture, and 14 patients for 3 years to prevent one vertebral fracture.
In the FIT trial, 20% of women taking alendronate lost BMD during the first year (JAMA. 1998 Dec 23-30;280[24]:2077-82). However, those same patients had a 50% fracture reduction, and 92% regained the lost bone mineral density (BMD) by the next measurement. “Using DXA to measure BMD after 1 year of therapy does not accurately predict what will happen over time or reflect fracture reduction,” Dr. Tice said. “Effective treatment for osteoporosis should not be changed because of loss of BMD during the first year of use.”
A rare but potential harm from treatment with bisphosphonates includes osteonecrosis of the jaw, which is believed to affect only 1 in 10,000 patients who are treated for 10 years. Most of these cases (94%) were caused by IV bisphosphonates. Only 4% of cases were being treated for osteoporosis, and 60% were caused by tooth extraction. Because of this, a dental exam is recommended before starting patients on bisphosphonate therapy, but this small risk of osteonecrosis of the jaw “is not a reason to stop bisphosphonate therapy,” Dr. Tice said.
Other concerns include an increased risk for atrial fibrillation that has been observed in randomized, controlled trials of zoledronate and alendronate. “There has been no association in other trials,” Dr. Tice said. “This is likely a chance finding, likely spurious.”
Reports of an increased risk of esophageal cancer from bisphosphonate use have also been suggested, but these come from case series and from two conflicting cohorts of data. “This is most likely not a real finding but is a concern because of clinical reports of esophagitis associated with oral bisphosphonates,” he said.
Another concern from long-term bisphosphonate use is the development of atypical femoral fractures, a subtrochanteric fracture with atypical features. “These are transverse fractures of the femur and are likely a real effect of bisphosphonates,” Dr. Tice said. “They are characterized by transverse fractures, cortical thickening, and the 10-year risk is about 1:200. It’s similar to a stress fracture, and it’s often preceded by pain.”
To bring perspective on the risk of developing an atypical femoral fracture, Dr. Tice offered a comparison. If 1,000 women are treated for 3 years with zoledronic acid, it will prevent 71 vertebral fractures, 11 hip fractures, and 18 other fractures. “So, the best estimate is that you would cause 0.1 atypical femoral fractures,” he said. “That really means that, for every one atypical femoral fracture caused, you’ve prevented 110 hip fractures. So, yes, there’s a risk of harm – but there is so much more benefit.”
Dr. Tice reported having no relevant financial disclosures.
SAN FRANCISCO – Parathyroid hormone and parathyroid hormone–related protein analogs show promise for treating osteoporosis, but, for now, they’re reserved for the most severe cases.
Teriparatide, a parathyroid hormone analog, is the first treatment that stimulates bone formation instead of inhibiting bone resorption, but studies to date are too small to evaluate its effect on hip fractures, Jeffrey A. Tice, MD, said at the UCSF Annual Advances in Internal Medicine meeting.
Abaloparatide, a parathyroid hormone-related protein analog approved in April 2017, requires subcutaneous dosing of 80 mcg daily for up to 2 years and has been found to increase bone density in the spine by 11% and in the hip by 4%, compared with placebo, over 18 months. In women with pre-existing vertebral fractures, the agent was found to reduce the incidence of vertebral fractures by 86% and nonvertebral fragility fractures by 43%, but data are not adequate to evaluate its effect on hip fractures. Adverse reactions include hypercalciuria, nausea, hypercalcemia, orthostatic hypotension, tachycardia, and injection site reactions.
Studies to date have shown that combining either teriparatide or abaloparatide with an antiresorptive drug is less effective than either agent alone. However, both agents must be followed by an antiresorptive agent. “These drugs are expensive,” Dr. Tice said. “Right now, they’re reserved for patients with severe osteoporosis.”
The lifetime risk for osteoporotic fractures is 50% in women and 20% in men, and they cause significant morbidity and mortality. Among U.S. hospitalizations for women 55 years and older between 2000 and 2012, Dr. Tice noted, 4.9 million were for osteoporotic fractures, 3 million were for stroke, and 2.9 million were for myocardial infarction.
“Osteoporosis is a very common condition, but it’s under-recognized, in part because it’s a silent disease,” he said. “Only 20%-30% of patients with bone mineral densities less than –2.5 are treated in this country. And, 12 months after hip fracture, only 2% had a dual-energy x-ray absorptiometry [DXA] test, and only 15% were treated with an appropriate drug. We should be asking about fracture history, note vertebral fractures, treat those patients, and we should remember to use chart reminders for DXA.”
Clinical guidelines from the American College of Physicians and other groups recommend alendronate, risedronate, zoledronic acid, or denosumab as first-line therapy for women with osteoporosis. “There are no head to head trials to indicate which agent is best,” Dr. Tice said. “They reduce the fracture risk by 30%-50%, primarily in patients with an existing vertebral fracture or a T score below –2.5.” The use of hormone therapy and raloxifene are generally not recommended.
In a review published in the New England Journal of Medicine, researchers Dennis M. Black, MD, and Clifford J. Rosen, MD, estimated the number of patients needed to treat for 3 years to prevent various fractures (N Engl J Med. 2016 Jan 21;374[3]:254-62). They found that, for nonvertebral fractures, including hip, 35 patients need to be treated for 3 years to prevent one of those fractures, 90 patients for 3 years to prevent one hip fracture, and 14 patients for 3 years to prevent one vertebral fracture.
In the FIT trial, 20% of women taking alendronate lost BMD during the first year (JAMA. 1998 Dec 23-30;280[24]:2077-82). However, those same patients had a 50% fracture reduction, and 92% regained the lost bone mineral density (BMD) by the next measurement. “Using DXA to measure BMD after 1 year of therapy does not accurately predict what will happen over time or reflect fracture reduction,” Dr. Tice said. “Effective treatment for osteoporosis should not be changed because of loss of BMD during the first year of use.”
A rare but potential harm from treatment with bisphosphonates includes osteonecrosis of the jaw, which is believed to affect only 1 in 10,000 patients who are treated for 10 years. Most of these cases (94%) were caused by IV bisphosphonates. Only 4% of cases were being treated for osteoporosis, and 60% were caused by tooth extraction. Because of this, a dental exam is recommended before starting patients on bisphosphonate therapy, but this small risk of osteonecrosis of the jaw “is not a reason to stop bisphosphonate therapy,” Dr. Tice said.
Other concerns include an increased risk for atrial fibrillation that has been observed in randomized, controlled trials of zoledronate and alendronate. “There has been no association in other trials,” Dr. Tice said. “This is likely a chance finding, likely spurious.”
Reports of an increased risk of esophageal cancer from bisphosphonate use have also been suggested, but these come from case series and from two conflicting cohorts of data. “This is most likely not a real finding but is a concern because of clinical reports of esophagitis associated with oral bisphosphonates,” he said.
Another concern from long-term bisphosphonate use is the development of atypical femoral fractures, a subtrochanteric fracture with atypical features. “These are transverse fractures of the femur and are likely a real effect of bisphosphonates,” Dr. Tice said. “They are characterized by transverse fractures, cortical thickening, and the 10-year risk is about 1:200. It’s similar to a stress fracture, and it’s often preceded by pain.”
To bring perspective on the risk of developing an atypical femoral fracture, Dr. Tice offered a comparison. If 1,000 women are treated for 3 years with zoledronic acid, it will prevent 71 vertebral fractures, 11 hip fractures, and 18 other fractures. “So, the best estimate is that you would cause 0.1 atypical femoral fractures,” he said. “That really means that, for every one atypical femoral fracture caused, you’ve prevented 110 hip fractures. So, yes, there’s a risk of harm – but there is so much more benefit.”
Dr. Tice reported having no relevant financial disclosures.
SAN FRANCISCO – Parathyroid hormone and parathyroid hormone–related protein analogs show promise for treating osteoporosis, but, for now, they’re reserved for the most severe cases.
Teriparatide, a parathyroid hormone analog, is the first treatment that stimulates bone formation instead of inhibiting bone resorption, but studies to date are too small to evaluate its effect on hip fractures, Jeffrey A. Tice, MD, said at the UCSF Annual Advances in Internal Medicine meeting.
Abaloparatide, a parathyroid hormone-related protein analog approved in April 2017, requires subcutaneous dosing of 80 mcg daily for up to 2 years and has been found to increase bone density in the spine by 11% and in the hip by 4%, compared with placebo, over 18 months. In women with pre-existing vertebral fractures, the agent was found to reduce the incidence of vertebral fractures by 86% and nonvertebral fragility fractures by 43%, but data are not adequate to evaluate its effect on hip fractures. Adverse reactions include hypercalciuria, nausea, hypercalcemia, orthostatic hypotension, tachycardia, and injection site reactions.
Studies to date have shown that combining either teriparatide or abaloparatide with an antiresorptive drug is less effective than either agent alone. However, both agents must be followed by an antiresorptive agent. “These drugs are expensive,” Dr. Tice said. “Right now, they’re reserved for patients with severe osteoporosis.”
The lifetime risk for osteoporotic fractures is 50% in women and 20% in men, and they cause significant morbidity and mortality. Among U.S. hospitalizations for women 55 years and older between 2000 and 2012, Dr. Tice noted, 4.9 million were for osteoporotic fractures, 3 million were for stroke, and 2.9 million were for myocardial infarction.
“Osteoporosis is a very common condition, but it’s under-recognized, in part because it’s a silent disease,” he said. “Only 20%-30% of patients with bone mineral densities less than –2.5 are treated in this country. And, 12 months after hip fracture, only 2% had a dual-energy x-ray absorptiometry [DXA] test, and only 15% were treated with an appropriate drug. We should be asking about fracture history, note vertebral fractures, treat those patients, and we should remember to use chart reminders for DXA.”
Clinical guidelines from the American College of Physicians and other groups recommend alendronate, risedronate, zoledronic acid, or denosumab as first-line therapy for women with osteoporosis. “There are no head to head trials to indicate which agent is best,” Dr. Tice said. “They reduce the fracture risk by 30%-50%, primarily in patients with an existing vertebral fracture or a T score below –2.5.” The use of hormone therapy and raloxifene are generally not recommended.
In a review published in the New England Journal of Medicine, researchers Dennis M. Black, MD, and Clifford J. Rosen, MD, estimated the number of patients needed to treat for 3 years to prevent various fractures (N Engl J Med. 2016 Jan 21;374[3]:254-62). They found that, for nonvertebral fractures, including hip, 35 patients need to be treated for 3 years to prevent one of those fractures, 90 patients for 3 years to prevent one hip fracture, and 14 patients for 3 years to prevent one vertebral fracture.
In the FIT trial, 20% of women taking alendronate lost BMD during the first year (JAMA. 1998 Dec 23-30;280[24]:2077-82). However, those same patients had a 50% fracture reduction, and 92% regained the lost bone mineral density (BMD) by the next measurement. “Using DXA to measure BMD after 1 year of therapy does not accurately predict what will happen over time or reflect fracture reduction,” Dr. Tice said. “Effective treatment for osteoporosis should not be changed because of loss of BMD during the first year of use.”
A rare but potential harm from treatment with bisphosphonates includes osteonecrosis of the jaw, which is believed to affect only 1 in 10,000 patients who are treated for 10 years. Most of these cases (94%) were caused by IV bisphosphonates. Only 4% of cases were being treated for osteoporosis, and 60% were caused by tooth extraction. Because of this, a dental exam is recommended before starting patients on bisphosphonate therapy, but this small risk of osteonecrosis of the jaw “is not a reason to stop bisphosphonate therapy,” Dr. Tice said.
Other concerns include an increased risk for atrial fibrillation that has been observed in randomized, controlled trials of zoledronate and alendronate. “There has been no association in other trials,” Dr. Tice said. “This is likely a chance finding, likely spurious.”
Reports of an increased risk of esophageal cancer from bisphosphonate use have also been suggested, but these come from case series and from two conflicting cohorts of data. “This is most likely not a real finding but is a concern because of clinical reports of esophagitis associated with oral bisphosphonates,” he said.
Another concern from long-term bisphosphonate use is the development of atypical femoral fractures, a subtrochanteric fracture with atypical features. “These are transverse fractures of the femur and are likely a real effect of bisphosphonates,” Dr. Tice said. “They are characterized by transverse fractures, cortical thickening, and the 10-year risk is about 1:200. It’s similar to a stress fracture, and it’s often preceded by pain.”
To bring perspective on the risk of developing an atypical femoral fracture, Dr. Tice offered a comparison. If 1,000 women are treated for 3 years with zoledronic acid, it will prevent 71 vertebral fractures, 11 hip fractures, and 18 other fractures. “So, the best estimate is that you would cause 0.1 atypical femoral fractures,” he said. “That really means that, for every one atypical femoral fracture caused, you’ve prevented 110 hip fractures. So, yes, there’s a risk of harm – but there is so much more benefit.”
Dr. Tice reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM THE ANNUAL ADVANCES IN INTERNAL MEDICINE
Tool indicates fracture risk after HSCT
MADRID – The risk of osteoporotic fracture associated with hematopoietic stem cell transplantation (HSCT) could be assessed using the Fracture Risk Assessment Tool (FRAX), researchers from the University of Texas MD Anderson Cancer Center have found.
In a retrospective cohort study, Huifang Lu, MD, and her collaborators found that FRAX could predict the risk of fracture with reasonable accuracy. The area under the receiver operating characteristic curve was 0.66 for predicting a fracture 10 years after HSCT.
“Current guidelines recommend the evaluation of bone health at 1 year following the transplant, but we recommend that this needs to happen at a much earlier time,” Dr. Lu said at the European Congress of Rheumatology.
Determining how to assess risk earlier and prevent bone loss remains a challenge, however. FRAX is an easy and quick tool to use, but its predictive ability is modest, she said.
As the finding comes from a retrospective study, prospective evaluation of FRAX is needed in HSCT patients. If shown predictive in this setting, bone health could be assessed earlier using FRAX, ideally at or before the time of the transplant, to allow appropriate action to be taken, such as prescribing bisphosphonates to those identified to be at high risk.
There is no consensus on preventing and treating bone loss following HSCT, said Dr. Lu. In a meta-analysis performed by Dr. Lu and her associates (Bone Marrow Transplant. 2017;52[5]:663-70), less bone loss was seen in patients who received a bisphosphonate.
As the use of HSCT has expanded over the past two decades, there is an expanding population of survivors with potential long-term effects such as bone loss and a higher risk of fractures, compared with the general population, Dr. Lu explained.
The FRAX tool takes into account pre-HSCT factors such as age, smoking status, alcohol use, prior fracture, body mass index, and corticosteroid use. This can be considered in association with the fracture risk related to the various conditioning and supporting regimens that patients receive around the time of their transplants.
The study included 5,170 adult patients who had undergone HSCT at the University of Texas MD Anderson Cancer Center over a 10-year period. Patients were considered to have entered the cohort at the time of their transplants, Dr. Lu said. Their history of osteoporotic fractures up to 3.3 years later was obtained and verified by radiology and physician assessment. FRAX probabilities were then derived from baseline information.
The mean age of patients included was 52 years, 57% were male and 75% were white. One-quarter had experienced a prior fracture. Of note, 26% of the cohort underwent HSCT for multiple myeloma, 70% of whom had already had a fracture, compared with 9% of those who underwent HSCT for another reason such as leukemia or lymphoma.
Multivariate analyses were performed with and without considering death as a competing risk, and similar results were obtained. Higher FRAX scores (20 or greater) were more likely to be recorded in individuals who sustained a fracture than in those who did not. Patients who had an allogeneic HSCT were 15% more likely to have a fracture as those who received an autologous transplant. Perhaps not surprisingly, patients with multiple myeloma were more likely than those who had HSCT for other reasons to sustain a fracture by 10 years based on FRAX results (hazard ratio, 3.16).
Future research needs to look at the optimal cut offs for FRAX scores predictive of events and see if there is any association between the loss of bone and fracture risk. There also needs to be an evaluation of the use of concomitant medications and health economic analyses performed.
Dr. Lu had no conflicts of interest. The study was funded by the Rolanette and Berdon Lawrence Bone Disease Program of Texas and via Cancer Survivorship Research Seed Monday Grants from the University Cancer Foundation and Duncan Family Institute for Cancer Prevention and Risk Assessment to the University of Texas MD Anderson Cancer Center.
MADRID – The risk of osteoporotic fracture associated with hematopoietic stem cell transplantation (HSCT) could be assessed using the Fracture Risk Assessment Tool (FRAX), researchers from the University of Texas MD Anderson Cancer Center have found.
In a retrospective cohort study, Huifang Lu, MD, and her collaborators found that FRAX could predict the risk of fracture with reasonable accuracy. The area under the receiver operating characteristic curve was 0.66 for predicting a fracture 10 years after HSCT.
“Current guidelines recommend the evaluation of bone health at 1 year following the transplant, but we recommend that this needs to happen at a much earlier time,” Dr. Lu said at the European Congress of Rheumatology.
Determining how to assess risk earlier and prevent bone loss remains a challenge, however. FRAX is an easy and quick tool to use, but its predictive ability is modest, she said.
As the finding comes from a retrospective study, prospective evaluation of FRAX is needed in HSCT patients. If shown predictive in this setting, bone health could be assessed earlier using FRAX, ideally at or before the time of the transplant, to allow appropriate action to be taken, such as prescribing bisphosphonates to those identified to be at high risk.
There is no consensus on preventing and treating bone loss following HSCT, said Dr. Lu. In a meta-analysis performed by Dr. Lu and her associates (Bone Marrow Transplant. 2017;52[5]:663-70), less bone loss was seen in patients who received a bisphosphonate.
As the use of HSCT has expanded over the past two decades, there is an expanding population of survivors with potential long-term effects such as bone loss and a higher risk of fractures, compared with the general population, Dr. Lu explained.
The FRAX tool takes into account pre-HSCT factors such as age, smoking status, alcohol use, prior fracture, body mass index, and corticosteroid use. This can be considered in association with the fracture risk related to the various conditioning and supporting regimens that patients receive around the time of their transplants.
The study included 5,170 adult patients who had undergone HSCT at the University of Texas MD Anderson Cancer Center over a 10-year period. Patients were considered to have entered the cohort at the time of their transplants, Dr. Lu said. Their history of osteoporotic fractures up to 3.3 years later was obtained and verified by radiology and physician assessment. FRAX probabilities were then derived from baseline information.
The mean age of patients included was 52 years, 57% were male and 75% were white. One-quarter had experienced a prior fracture. Of note, 26% of the cohort underwent HSCT for multiple myeloma, 70% of whom had already had a fracture, compared with 9% of those who underwent HSCT for another reason such as leukemia or lymphoma.
Multivariate analyses were performed with and without considering death as a competing risk, and similar results were obtained. Higher FRAX scores (20 or greater) were more likely to be recorded in individuals who sustained a fracture than in those who did not. Patients who had an allogeneic HSCT were 15% more likely to have a fracture as those who received an autologous transplant. Perhaps not surprisingly, patients with multiple myeloma were more likely than those who had HSCT for other reasons to sustain a fracture by 10 years based on FRAX results (hazard ratio, 3.16).
Future research needs to look at the optimal cut offs for FRAX scores predictive of events and see if there is any association between the loss of bone and fracture risk. There also needs to be an evaluation of the use of concomitant medications and health economic analyses performed.
Dr. Lu had no conflicts of interest. The study was funded by the Rolanette and Berdon Lawrence Bone Disease Program of Texas and via Cancer Survivorship Research Seed Monday Grants from the University Cancer Foundation and Duncan Family Institute for Cancer Prevention and Risk Assessment to the University of Texas MD Anderson Cancer Center.
MADRID – The risk of osteoporotic fracture associated with hematopoietic stem cell transplantation (HSCT) could be assessed using the Fracture Risk Assessment Tool (FRAX), researchers from the University of Texas MD Anderson Cancer Center have found.
In a retrospective cohort study, Huifang Lu, MD, and her collaborators found that FRAX could predict the risk of fracture with reasonable accuracy. The area under the receiver operating characteristic curve was 0.66 for predicting a fracture 10 years after HSCT.
“Current guidelines recommend the evaluation of bone health at 1 year following the transplant, but we recommend that this needs to happen at a much earlier time,” Dr. Lu said at the European Congress of Rheumatology.
Determining how to assess risk earlier and prevent bone loss remains a challenge, however. FRAX is an easy and quick tool to use, but its predictive ability is modest, she said.
As the finding comes from a retrospective study, prospective evaluation of FRAX is needed in HSCT patients. If shown predictive in this setting, bone health could be assessed earlier using FRAX, ideally at or before the time of the transplant, to allow appropriate action to be taken, such as prescribing bisphosphonates to those identified to be at high risk.
There is no consensus on preventing and treating bone loss following HSCT, said Dr. Lu. In a meta-analysis performed by Dr. Lu and her associates (Bone Marrow Transplant. 2017;52[5]:663-70), less bone loss was seen in patients who received a bisphosphonate.
As the use of HSCT has expanded over the past two decades, there is an expanding population of survivors with potential long-term effects such as bone loss and a higher risk of fractures, compared with the general population, Dr. Lu explained.
The FRAX tool takes into account pre-HSCT factors such as age, smoking status, alcohol use, prior fracture, body mass index, and corticosteroid use. This can be considered in association with the fracture risk related to the various conditioning and supporting regimens that patients receive around the time of their transplants.
The study included 5,170 adult patients who had undergone HSCT at the University of Texas MD Anderson Cancer Center over a 10-year period. Patients were considered to have entered the cohort at the time of their transplants, Dr. Lu said. Their history of osteoporotic fractures up to 3.3 years later was obtained and verified by radiology and physician assessment. FRAX probabilities were then derived from baseline information.
The mean age of patients included was 52 years, 57% were male and 75% were white. One-quarter had experienced a prior fracture. Of note, 26% of the cohort underwent HSCT for multiple myeloma, 70% of whom had already had a fracture, compared with 9% of those who underwent HSCT for another reason such as leukemia or lymphoma.
Multivariate analyses were performed with and without considering death as a competing risk, and similar results were obtained. Higher FRAX scores (20 or greater) were more likely to be recorded in individuals who sustained a fracture than in those who did not. Patients who had an allogeneic HSCT were 15% more likely to have a fracture as those who received an autologous transplant. Perhaps not surprisingly, patients with multiple myeloma were more likely than those who had HSCT for other reasons to sustain a fracture by 10 years based on FRAX results (hazard ratio, 3.16).
Future research needs to look at the optimal cut offs for FRAX scores predictive of events and see if there is any association between the loss of bone and fracture risk. There also needs to be an evaluation of the use of concomitant medications and health economic analyses performed.
Dr. Lu had no conflicts of interest. The study was funded by the Rolanette and Berdon Lawrence Bone Disease Program of Texas and via Cancer Survivorship Research Seed Monday Grants from the University Cancer Foundation and Duncan Family Institute for Cancer Prevention and Risk Assessment to the University of Texas MD Anderson Cancer Center.
AT THE EULAR 2017 CONGRESS
Key clinical point: The Fracture Risk Assessment Tool (FRAX) helped in predicting osteoporotic fracture risk after hematopoietic stem cell transplantation (HSCT).
Major finding: The area under the receiver operating characteristic curve was 0.66, indicating modest predictive ability,10 years after HSCT.
Data source: A retrospective cohort study of 5,170 adult patients who received HSCT at the University of Texas MD Anderson Cancer Center between 2001 and 2010.
Disclosures: Dr. Lu had no conflicts of interest. The study was funded by the Rolanette and Berdon Lawrence Bone Disease Program of Texas and via Cancer Survivorship Research Seed Monday Grants from the University Cancer Foundation and the Duncan Family Institute for Cancer Prevention and Risk Assessment to the University of Texas MD Anderson Cancer Center.
Meta-analysis: Bisphosphonates mitigate glucocorticoid-induced bone loss
MADRID – Bisphosphonates mitigate the damaging effects of glucocorticoid on bone, boosting bone mineral density and reducing the risk of fracture by up to 33%, compared with placebo, according to a systematic review and meta-analysis.
The review of 11 randomized, controlled trials found that bisphosphonates consistently improved bone outcomes among patients taking prednisone, Anas Makhzoum, MD, said at the European Congress of Rheumatology.
The primary outcomes of these trials were mean percentage change in bone mineral density at lumbar spine and femoral neck, and fracture incidence.
The drugs examined were ibandronate, alendronate, risedronate, etidronate, and clodronate. The mean duration of these trials was 71 weeks. Patients took a mean steroid dose of 15 mg.
Dr. Makhzoum, a resident at Queen’s University, Kingston, Ont., pooled nine of these trials for the outcome of mean percentage change in lumbar spine bone mineral density. The pooled mean percentage change of lumbar spine consistently favored bisphosphonates, compared with placebo, with a mean, statistically significant difference of approximately 4%.
Six studies were pooled for the outcome of mean percentage change in femoral neck bone mineral density. The pooled mean percentage change consistently favored bisphosphonates, with a mean, statistically significant difference of 2.95% relative to placebo.
Seven studies were pooled for outcome of incident fracture and the results consistently favored bisphosphonates, with a mean, statistically significant 33% decrease in the risk of a new fracture, compared with the placebo group (relative risk, 0.66).
“Bisphosphonates remain the standard of care for prevention and treatment of bone loss in patients on chronic steroids treatment,” Dr. Makhzoum noted.
He had no financial disclosures.
[email protected]
On Twitter @alz_gal
MADRID – Bisphosphonates mitigate the damaging effects of glucocorticoid on bone, boosting bone mineral density and reducing the risk of fracture by up to 33%, compared with placebo, according to a systematic review and meta-analysis.
The review of 11 randomized, controlled trials found that bisphosphonates consistently improved bone outcomes among patients taking prednisone, Anas Makhzoum, MD, said at the European Congress of Rheumatology.
The primary outcomes of these trials were mean percentage change in bone mineral density at lumbar spine and femoral neck, and fracture incidence.
The drugs examined were ibandronate, alendronate, risedronate, etidronate, and clodronate. The mean duration of these trials was 71 weeks. Patients took a mean steroid dose of 15 mg.
Dr. Makhzoum, a resident at Queen’s University, Kingston, Ont., pooled nine of these trials for the outcome of mean percentage change in lumbar spine bone mineral density. The pooled mean percentage change of lumbar spine consistently favored bisphosphonates, compared with placebo, with a mean, statistically significant difference of approximately 4%.
Six studies were pooled for the outcome of mean percentage change in femoral neck bone mineral density. The pooled mean percentage change consistently favored bisphosphonates, with a mean, statistically significant difference of 2.95% relative to placebo.
Seven studies were pooled for outcome of incident fracture and the results consistently favored bisphosphonates, with a mean, statistically significant 33% decrease in the risk of a new fracture, compared with the placebo group (relative risk, 0.66).
“Bisphosphonates remain the standard of care for prevention and treatment of bone loss in patients on chronic steroids treatment,” Dr. Makhzoum noted.
He had no financial disclosures.
[email protected]
On Twitter @alz_gal
MADRID – Bisphosphonates mitigate the damaging effects of glucocorticoid on bone, boosting bone mineral density and reducing the risk of fracture by up to 33%, compared with placebo, according to a systematic review and meta-analysis.
The review of 11 randomized, controlled trials found that bisphosphonates consistently improved bone outcomes among patients taking prednisone, Anas Makhzoum, MD, said at the European Congress of Rheumatology.
The primary outcomes of these trials were mean percentage change in bone mineral density at lumbar spine and femoral neck, and fracture incidence.
The drugs examined were ibandronate, alendronate, risedronate, etidronate, and clodronate. The mean duration of these trials was 71 weeks. Patients took a mean steroid dose of 15 mg.
Dr. Makhzoum, a resident at Queen’s University, Kingston, Ont., pooled nine of these trials for the outcome of mean percentage change in lumbar spine bone mineral density. The pooled mean percentage change of lumbar spine consistently favored bisphosphonates, compared with placebo, with a mean, statistically significant difference of approximately 4%.
Six studies were pooled for the outcome of mean percentage change in femoral neck bone mineral density. The pooled mean percentage change consistently favored bisphosphonates, with a mean, statistically significant difference of 2.95% relative to placebo.
Seven studies were pooled for outcome of incident fracture and the results consistently favored bisphosphonates, with a mean, statistically significant 33% decrease in the risk of a new fracture, compared with the placebo group (relative risk, 0.66).
“Bisphosphonates remain the standard of care for prevention and treatment of bone loss in patients on chronic steroids treatment,” Dr. Makhzoum noted.
He had no financial disclosures.
[email protected]
On Twitter @alz_gal
AT THE EULAR 2017 CONGRESS
Key clinical point:
Major finding: Relative to placebo, bisphosphonates reduced the risk of fracture by up to 33%.
Data source: A meta-analysis comprising 11 randomized, placebo-controlled trials with more than 2,000 patients.
Disclosures: Dr. Makhzoum had no financial disclosures.