User login
Bariatric surgery leads to better cardiovascular function in pregnancy
Pregnant women with a history of bariatric surgery have better cardiovascular adaptation to pregnancy compared with women who have similar early-pregnancy body mass index (BMI) but no history of weight loss surgery, new data suggest.
“Pregnant women who have had bariatric surgery demonstrate better cardiovascular adaptation through lower blood pressure, heart rate, and cardiac output, more favorable diastolic indices, and better systolic function,” reported Deesha Patel, MBBS MRCOG, specialist registrar, Chelsea and Westminster Hospital, London.
“Because the groups were matched for early pregnancy BMI, it’s unlikely that the results are due to weight loss alone but indicate that the metabolic alterations as a result of the surgery, via the enterocardiac axis, play an important role,” Dr. Patel continued.
The findings were presented at the Royal College of Obstetricians and Gynecologists 2021 Virtual World Congress.
Although obesity is known for its inflammatory and toxic effects on the cardiovascular system, it is not clear to what extent the various treatment options for obesity modify these risks in the long term, said Hutan Ashrafian, MD, clinical lecturer in surgery, Imperial College London.
“It is even less clear how anti-obesity interventions affect the cardiovascular system in pregnancy,” Dr. Ashrafian told this news organization.
“This very novel study in pregnant mothers having undergone the most successful and consistent intervention for severe obesity – bariatric or metabolic surgery – gives new clues as to the extent that bariatric procedures can alter cardiovascular risk in pregnant mothers,” continued Dr. Ashrafian, who was not involved in the study.
The results show how bariatric surgery has favorable effects on cardiac adaptation in pregnancy and in turn “might offer protection from pregnancy-related cardiovascular pathology such as preeclampsia,” explained Dr. Ashrafian. “This adds to the known effects of cardiovascular protection of bariatric surgery through the enterocardiac axis, which may explain a wider range of effects that can be translated within pregnancy and possibly following pregnancy in the postpartum era and beyond.”
A history of bariatric surgery versus no surgery
The prospective, longitudinal study compared 41 women who had a history of bariatric surgery with 41 women who had not undergone surgery. Patients’ characteristics were closely matched for age, BMI (34.5 kg/m2 and 34.3 kg/m2 in the surgery and bariatric surgery groups, respectively) and race. Hypertensive disorders in the post-surgery group were significantly less common compared with the no-surgery group (0% vs. 9.8%).
During the study, participants underwent cardiovascular assessment at 12-14 weeks, 20-24 weeks, and 30-32 weeks of gestation. The assessment included measurement of blood pressure and heart rate, transthoracic echocardiography, and 2D speckle tracking, performed offline to assess global longitudinal and circumferential strain.
Blood pressure readings across the three trimesters were consistently lower in the women who had undergone bariatric surgery compared with those in the no-surgery group, and all differences were statistically significant. Likewise, heart rate and cardiac output across the three trimesters were lower in the post-surgery cohort. However, there was no difference in stroke volume between the two groups.
As for diastolic function, there were more favorable indices in the post-surgery group with a higher E/A ratio, a marker of left ventricle filling (P < .001), and lower left atrial volume (P < .05), Dr. Patel reported.
With respect to systolic function, there was no difference in ejection fraction, but there was lower global longitudinal strain (P < .01) and global circumferential strain in the post-bariatric group (P = .02), suggesting better systolic function.
“Strain is a measure of differences in motion and velocity between regions of the myocardium through the cardiac cycle and can detect subclinical changes when ejection fraction is normal,” she added.
“This is a fascinating piece of work. The author should be congratulated on gathering so many [pregnant] women who had had bariatric surgery. The work gives a unique glimpse into metabolic syndrome,” said Philip Toozs-Hobson, MD, who moderated the session.
“We are increasingly recognizing the impact [of bariatric surgery] on metabolic syndrome, and the fact that this study demonstrates that there is more to it than just weight is important,” continued Dr. Toosz-Hobson, who is a consultant gynecologist at Birmingham Women’s Hospital NHS Foundation Trust, United Kingdom.
Cardiovascular benefits of bariatric surgery
Bariatric surgery has been associated with loss of excess body weight of up to 55% and with approximately 40% reduction in all-cause mortality in the general population. The procedure also reduces the risk for heart disease, diabetes, and cancer.
The cardiovascular benefits of bariatric surgery include reduced hypertension, remodeling of the heart with a reduction in left ventricular mass, and an improvement in diastolic and systolic function.
“Traditionally, the cardiac changes were thought to be due to weight loss and blood pressure reduction, but it is now conceivable that the metabolic components contribute to the reverse modeling via changes to the enterocardiac axis involving changes to gut hormones,” said Dr. Patel. These hormones include secretin, glucagon, and vasoactive intestinal peptide, which are known to have inotropic effects, as well as adiponectin and leptin, which are known to have cardiac effects, she added.
“Pregnancy following bariatric surgery is associated with a reduced risk of hypertensive disorders, as well as a reduced risk of gestational diabetes, large-for-gestational-age neonates, and a small increased risk of small-for-gestational-age neonates,” said Dr. Patel.
Dr. Patel and Dr. Toosz-Hobson have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women with a history of bariatric surgery have better cardiovascular adaptation to pregnancy compared with women who have similar early-pregnancy body mass index (BMI) but no history of weight loss surgery, new data suggest.
“Pregnant women who have had bariatric surgery demonstrate better cardiovascular adaptation through lower blood pressure, heart rate, and cardiac output, more favorable diastolic indices, and better systolic function,” reported Deesha Patel, MBBS MRCOG, specialist registrar, Chelsea and Westminster Hospital, London.
“Because the groups were matched for early pregnancy BMI, it’s unlikely that the results are due to weight loss alone but indicate that the metabolic alterations as a result of the surgery, via the enterocardiac axis, play an important role,” Dr. Patel continued.
The findings were presented at the Royal College of Obstetricians and Gynecologists 2021 Virtual World Congress.
Although obesity is known for its inflammatory and toxic effects on the cardiovascular system, it is not clear to what extent the various treatment options for obesity modify these risks in the long term, said Hutan Ashrafian, MD, clinical lecturer in surgery, Imperial College London.
“It is even less clear how anti-obesity interventions affect the cardiovascular system in pregnancy,” Dr. Ashrafian told this news organization.
“This very novel study in pregnant mothers having undergone the most successful and consistent intervention for severe obesity – bariatric or metabolic surgery – gives new clues as to the extent that bariatric procedures can alter cardiovascular risk in pregnant mothers,” continued Dr. Ashrafian, who was not involved in the study.
The results show how bariatric surgery has favorable effects on cardiac adaptation in pregnancy and in turn “might offer protection from pregnancy-related cardiovascular pathology such as preeclampsia,” explained Dr. Ashrafian. “This adds to the known effects of cardiovascular protection of bariatric surgery through the enterocardiac axis, which may explain a wider range of effects that can be translated within pregnancy and possibly following pregnancy in the postpartum era and beyond.”
A history of bariatric surgery versus no surgery
The prospective, longitudinal study compared 41 women who had a history of bariatric surgery with 41 women who had not undergone surgery. Patients’ characteristics were closely matched for age, BMI (34.5 kg/m2 and 34.3 kg/m2 in the surgery and bariatric surgery groups, respectively) and race. Hypertensive disorders in the post-surgery group were significantly less common compared with the no-surgery group (0% vs. 9.8%).
During the study, participants underwent cardiovascular assessment at 12-14 weeks, 20-24 weeks, and 30-32 weeks of gestation. The assessment included measurement of blood pressure and heart rate, transthoracic echocardiography, and 2D speckle tracking, performed offline to assess global longitudinal and circumferential strain.
Blood pressure readings across the three trimesters were consistently lower in the women who had undergone bariatric surgery compared with those in the no-surgery group, and all differences were statistically significant. Likewise, heart rate and cardiac output across the three trimesters were lower in the post-surgery cohort. However, there was no difference in stroke volume between the two groups.
As for diastolic function, there were more favorable indices in the post-surgery group with a higher E/A ratio, a marker of left ventricle filling (P < .001), and lower left atrial volume (P < .05), Dr. Patel reported.
With respect to systolic function, there was no difference in ejection fraction, but there was lower global longitudinal strain (P < .01) and global circumferential strain in the post-bariatric group (P = .02), suggesting better systolic function.
“Strain is a measure of differences in motion and velocity between regions of the myocardium through the cardiac cycle and can detect subclinical changes when ejection fraction is normal,” she added.
“This is a fascinating piece of work. The author should be congratulated on gathering so many [pregnant] women who had had bariatric surgery. The work gives a unique glimpse into metabolic syndrome,” said Philip Toozs-Hobson, MD, who moderated the session.
“We are increasingly recognizing the impact [of bariatric surgery] on metabolic syndrome, and the fact that this study demonstrates that there is more to it than just weight is important,” continued Dr. Toosz-Hobson, who is a consultant gynecologist at Birmingham Women’s Hospital NHS Foundation Trust, United Kingdom.
Cardiovascular benefits of bariatric surgery
Bariatric surgery has been associated with loss of excess body weight of up to 55% and with approximately 40% reduction in all-cause mortality in the general population. The procedure also reduces the risk for heart disease, diabetes, and cancer.
The cardiovascular benefits of bariatric surgery include reduced hypertension, remodeling of the heart with a reduction in left ventricular mass, and an improvement in diastolic and systolic function.
“Traditionally, the cardiac changes were thought to be due to weight loss and blood pressure reduction, but it is now conceivable that the metabolic components contribute to the reverse modeling via changes to the enterocardiac axis involving changes to gut hormones,” said Dr. Patel. These hormones include secretin, glucagon, and vasoactive intestinal peptide, which are known to have inotropic effects, as well as adiponectin and leptin, which are known to have cardiac effects, she added.
“Pregnancy following bariatric surgery is associated with a reduced risk of hypertensive disorders, as well as a reduced risk of gestational diabetes, large-for-gestational-age neonates, and a small increased risk of small-for-gestational-age neonates,” said Dr. Patel.
Dr. Patel and Dr. Toosz-Hobson have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women with a history of bariatric surgery have better cardiovascular adaptation to pregnancy compared with women who have similar early-pregnancy body mass index (BMI) but no history of weight loss surgery, new data suggest.
“Pregnant women who have had bariatric surgery demonstrate better cardiovascular adaptation through lower blood pressure, heart rate, and cardiac output, more favorable diastolic indices, and better systolic function,” reported Deesha Patel, MBBS MRCOG, specialist registrar, Chelsea and Westminster Hospital, London.
“Because the groups were matched for early pregnancy BMI, it’s unlikely that the results are due to weight loss alone but indicate that the metabolic alterations as a result of the surgery, via the enterocardiac axis, play an important role,” Dr. Patel continued.
The findings were presented at the Royal College of Obstetricians and Gynecologists 2021 Virtual World Congress.
Although obesity is known for its inflammatory and toxic effects on the cardiovascular system, it is not clear to what extent the various treatment options for obesity modify these risks in the long term, said Hutan Ashrafian, MD, clinical lecturer in surgery, Imperial College London.
“It is even less clear how anti-obesity interventions affect the cardiovascular system in pregnancy,” Dr. Ashrafian told this news organization.
“This very novel study in pregnant mothers having undergone the most successful and consistent intervention for severe obesity – bariatric or metabolic surgery – gives new clues as to the extent that bariatric procedures can alter cardiovascular risk in pregnant mothers,” continued Dr. Ashrafian, who was not involved in the study.
The results show how bariatric surgery has favorable effects on cardiac adaptation in pregnancy and in turn “might offer protection from pregnancy-related cardiovascular pathology such as preeclampsia,” explained Dr. Ashrafian. “This adds to the known effects of cardiovascular protection of bariatric surgery through the enterocardiac axis, which may explain a wider range of effects that can be translated within pregnancy and possibly following pregnancy in the postpartum era and beyond.”
A history of bariatric surgery versus no surgery
The prospective, longitudinal study compared 41 women who had a history of bariatric surgery with 41 women who had not undergone surgery. Patients’ characteristics were closely matched for age, BMI (34.5 kg/m2 and 34.3 kg/m2 in the surgery and bariatric surgery groups, respectively) and race. Hypertensive disorders in the post-surgery group were significantly less common compared with the no-surgery group (0% vs. 9.8%).
During the study, participants underwent cardiovascular assessment at 12-14 weeks, 20-24 weeks, and 30-32 weeks of gestation. The assessment included measurement of blood pressure and heart rate, transthoracic echocardiography, and 2D speckle tracking, performed offline to assess global longitudinal and circumferential strain.
Blood pressure readings across the three trimesters were consistently lower in the women who had undergone bariatric surgery compared with those in the no-surgery group, and all differences were statistically significant. Likewise, heart rate and cardiac output across the three trimesters were lower in the post-surgery cohort. However, there was no difference in stroke volume between the two groups.
As for diastolic function, there were more favorable indices in the post-surgery group with a higher E/A ratio, a marker of left ventricle filling (P < .001), and lower left atrial volume (P < .05), Dr. Patel reported.
With respect to systolic function, there was no difference in ejection fraction, but there was lower global longitudinal strain (P < .01) and global circumferential strain in the post-bariatric group (P = .02), suggesting better systolic function.
“Strain is a measure of differences in motion and velocity between regions of the myocardium through the cardiac cycle and can detect subclinical changes when ejection fraction is normal,” she added.
“This is a fascinating piece of work. The author should be congratulated on gathering so many [pregnant] women who had had bariatric surgery. The work gives a unique glimpse into metabolic syndrome,” said Philip Toozs-Hobson, MD, who moderated the session.
“We are increasingly recognizing the impact [of bariatric surgery] on metabolic syndrome, and the fact that this study demonstrates that there is more to it than just weight is important,” continued Dr. Toosz-Hobson, who is a consultant gynecologist at Birmingham Women’s Hospital NHS Foundation Trust, United Kingdom.
Cardiovascular benefits of bariatric surgery
Bariatric surgery has been associated with loss of excess body weight of up to 55% and with approximately 40% reduction in all-cause mortality in the general population. The procedure also reduces the risk for heart disease, diabetes, and cancer.
The cardiovascular benefits of bariatric surgery include reduced hypertension, remodeling of the heart with a reduction in left ventricular mass, and an improvement in diastolic and systolic function.
“Traditionally, the cardiac changes were thought to be due to weight loss and blood pressure reduction, but it is now conceivable that the metabolic components contribute to the reverse modeling via changes to the enterocardiac axis involving changes to gut hormones,” said Dr. Patel. These hormones include secretin, glucagon, and vasoactive intestinal peptide, which are known to have inotropic effects, as well as adiponectin and leptin, which are known to have cardiac effects, she added.
“Pregnancy following bariatric surgery is associated with a reduced risk of hypertensive disorders, as well as a reduced risk of gestational diabetes, large-for-gestational-age neonates, and a small increased risk of small-for-gestational-age neonates,” said Dr. Patel.
Dr. Patel and Dr. Toosz-Hobson have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Women with migraine are ‘high-risk’ patients during pregnancy
new research suggests. Although pregnancy is generally considered a “safe period” for women with migraine, “we actually found they have more diabetes, more hypertension, more blood clots, more complications during their delivery, and more postpartum complications,” said study investigator Nirit Lev, MD, PhD, head, department of neurology, Meir Medical Center, Kfar Saba Sackler Faculty of Medicine, Tel Aviv University.
The results highlight the need for clinicians “to take people with migraines seriously” and reinforce the idea that migraine is not “just a headache,” said Dr. Lev.
Pregnant women with migraine should be considered high risk and have specialized neurologic follow-up during pregnancy and the postpartum period, she added.
The findings were presented at the 2021 Congress of the European Academy of Neurology.
Prevalent, disabling
Migraine is one of the most prevalent and disabling neurologic disorders. Such disorders are major causes of death and disability.
In childhood, there’s no difference between the sexes in terms of migraine prevalence, but after puberty, migraine is about three times more common in women than men. Fluctuating levels of estrogen and progesterone likely explain these differences, said Dr. Lev.
The prevalence of migraine among females peaks during their reproductive years. Most female migraine patients report an improvement in headache symptoms during pregnancy, with some experiencing a “complete remission.” However, a minority report worsening of migraine when expecting a child, said Dr. Lev.
Some patients have their first aura during pregnancy. The most common migraine aura is visual, a problem with the visual field that can affect motor and sensory functioning, said Dr. Lev.
Managing migraine during pregnancy is “very complicated,” said Dr. Lev. She said the first-line treatment is paracetamol (acetaminophen) and stressed that taking opioids should be avoided.
Retrospective database study
For the study, the researchers retrospectively reviewed pregnancy and delivery records from a database of Clalit Medical Services, which has more than 4.5 million members and is the largest such database in Israel. They collected demographic data and information on mode of delivery, medical and obstetric complications, hospitalizations, emergency department visits, use of medications, laboratory reports, and medical consultations.
The study included 145,102 women who gave birth from 2014 to 2020.
Of these, 10,646 had migraine without aura, and 1,576 had migraine with aura. The migraine diagnoses, which were based on International Headache Society criteria and diagnostic codes, were made prior to pregnancy.
Dr. Lev noted that the number of patients with migraine is likely an underestimation because migraine is “not always diagnosed.”
Results showed that the risk for obstetric complications was higher among pregnant women with migraine, especially those with aura, in comparison with women without migraine. About 6.9% of patients with migraine without aura were admitted to high-risk hospital departments, compared with 6% of pregnant control patients who did not have migraine (P < .0001). For patients with migraine with aura, the risk for admissions was even higher (8.7%; P < .0001 vs. control patients and P < .03 vs. patients with migraine without aura) and was “very highly statistically significant,” said Dr. Lev.
Pregnant women with migraine were at significantly increased risk for gestational diabetes, hyperlipidemia, and being diagnosed with a psychiatric disorder (all P < .0001). These women were also more likely to experience preeclampsia and blood clots (P < .0001).
Unexpected finding
The finding that the risk for diabetes was higher was “unexpected,” inasmuch as older women with migraine are typically at increased risk for metabolic syndrome and higher body mass index, said Dr. Lev.
Migraine patients had significantly more consultations with family physicians, gynecologists, and neurologists (P < .0001). In addition, they were more likely to utilize emergency services; take more medications, mostly analgesics; and undergo more laboratory studies and brain imaging.
Those with aura had significantly more specialist consultations and took more medications compared with migraine patients without aura.
There was a statistically significant increase in the use of epidural anesthesia for migraine patients (40.5% of women without migraine; 45.7% of those with migraine accompanied by aura; and 47.5% of migraine patients without aura).
This was an “interesting” finding, said Dr. Lev. “We didn’t know what to expect; people with migraine are used to pain, so the question was, will they tolerate pain better or be more afraid of pain?”
Women with migraine also experienced more assisted deliveries with increased use of vacuums and forceps.
During the 3-month postpartum period, women with migraine sought more medical consultations and used more medications compared with control patients. They also underwent more lab examinations and more brain imaging during this period.
Dr. Lev noted that some of these evaluations may have been postponed because of the pregnancy.
Women with migraine also had a greater risk for postpartum depression, which Dr. Lev found “concerning.” She noted that depression is often underreported but is treatable. Women with migraine should be monitored for depression post partum, she said.
It’s unclear which factors contribute to the increased risk for pregnancy complications in women with migraine. Dr. Lev said she doesn’t believe it’s drug related.
“Although they’re taking more medications than people who don’t have migraine, we still are giving very low doses and only safe medicines, so I don’t think these increased risks are side effects,” she said.
She noted that women with migraine have more cardiovascular complications, including stroke and myocardial infarction, although these generally affect older patients.
Dr. Lev also noted that pain, especially chronic pain, can cause depression. “We know that people with migraine have more depression and anxiety, so maybe that also affects them during their pregnancy and after,” she said.
She suggested that pregnant women with migraine be considered high risk and be managed via specialized clinics.
Room for improvement
Commenting on the research, Lauren Doyle Strauss, DO, associate professor of neurology, Wake Forest University, Winston-Salem, N.C., who has written about the management of migraine during pregnancy, said studies such as this help raise awareness about pregnancy risks in migraine patients. Dr. Strauss did not attend the live presentation but is aware of the findings.
The increased use of epidurals during delivery among migraine patients in the study makes some sense, said Dr. Strauss. “It kind of shows a comfort level with medicines.”
She expressed concern that such research may be “skewed” because it includes patients with more severe migraine. If less severe cases were included in this research, “maybe there would still be higher risks, but not as high as what we have been finding in some of our studies,” she said.
Dr. Strauss said she feels the medical community should do a better job of identifying and diagnosing migraine. She said she would like to see migraine screening become a routine part of obstetric/gynecologic care. Doctors should counsel migraine patients who wish to become pregnant about potential risks, said Dr. Strauss. “We need to be up front in telling them when to seek care and when to report symptoms and not to wait for it to become super severe,” she said.
She also believes doctors should be “proactive” in helping patients develop a treatment plan before becoming pregnant, because the limited pain control options available for pregnant patients can take time to have an effect.
Also commenting on the study findings, Nina Riggins, MD, PhD, clinical associate professor of neurology at the University of California, San Francisco, said the study raises “important questions” and has “important aims.”
She believes the study reinforces the importance of collaboration between experts in primary care, obstetrics/gynecology, and neurology. However, she was surprised at some of the investigators’ assertions that there are no differences in migraine among prepubertal children and that the course of migraine for men is stable throughout their life span.
“There is literature that supports the view that the prevalence in boys is higher in prepuberty, and studies do show that migraine prevalence decreases in older adults – men and women,” she said.
There is still not enough evidence to determine that antiemetics and triptans are safe during pregnancy or that pregnant women with migraine should be taking acetylsalicylic acid, said Dr. Riggins.
The investigators, Dr. Strauss, and Dr. Riggins have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests. Although pregnancy is generally considered a “safe period” for women with migraine, “we actually found they have more diabetes, more hypertension, more blood clots, more complications during their delivery, and more postpartum complications,” said study investigator Nirit Lev, MD, PhD, head, department of neurology, Meir Medical Center, Kfar Saba Sackler Faculty of Medicine, Tel Aviv University.
The results highlight the need for clinicians “to take people with migraines seriously” and reinforce the idea that migraine is not “just a headache,” said Dr. Lev.
Pregnant women with migraine should be considered high risk and have specialized neurologic follow-up during pregnancy and the postpartum period, she added.
The findings were presented at the 2021 Congress of the European Academy of Neurology.
Prevalent, disabling
Migraine is one of the most prevalent and disabling neurologic disorders. Such disorders are major causes of death and disability.
In childhood, there’s no difference between the sexes in terms of migraine prevalence, but after puberty, migraine is about three times more common in women than men. Fluctuating levels of estrogen and progesterone likely explain these differences, said Dr. Lev.
The prevalence of migraine among females peaks during their reproductive years. Most female migraine patients report an improvement in headache symptoms during pregnancy, with some experiencing a “complete remission.” However, a minority report worsening of migraine when expecting a child, said Dr. Lev.
Some patients have their first aura during pregnancy. The most common migraine aura is visual, a problem with the visual field that can affect motor and sensory functioning, said Dr. Lev.
Managing migraine during pregnancy is “very complicated,” said Dr. Lev. She said the first-line treatment is paracetamol (acetaminophen) and stressed that taking opioids should be avoided.
Retrospective database study
For the study, the researchers retrospectively reviewed pregnancy and delivery records from a database of Clalit Medical Services, which has more than 4.5 million members and is the largest such database in Israel. They collected demographic data and information on mode of delivery, medical and obstetric complications, hospitalizations, emergency department visits, use of medications, laboratory reports, and medical consultations.
The study included 145,102 women who gave birth from 2014 to 2020.
Of these, 10,646 had migraine without aura, and 1,576 had migraine with aura. The migraine diagnoses, which were based on International Headache Society criteria and diagnostic codes, were made prior to pregnancy.
Dr. Lev noted that the number of patients with migraine is likely an underestimation because migraine is “not always diagnosed.”
Results showed that the risk for obstetric complications was higher among pregnant women with migraine, especially those with aura, in comparison with women without migraine. About 6.9% of patients with migraine without aura were admitted to high-risk hospital departments, compared with 6% of pregnant control patients who did not have migraine (P < .0001). For patients with migraine with aura, the risk for admissions was even higher (8.7%; P < .0001 vs. control patients and P < .03 vs. patients with migraine without aura) and was “very highly statistically significant,” said Dr. Lev.
Pregnant women with migraine were at significantly increased risk for gestational diabetes, hyperlipidemia, and being diagnosed with a psychiatric disorder (all P < .0001). These women were also more likely to experience preeclampsia and blood clots (P < .0001).
Unexpected finding
The finding that the risk for diabetes was higher was “unexpected,” inasmuch as older women with migraine are typically at increased risk for metabolic syndrome and higher body mass index, said Dr. Lev.
Migraine patients had significantly more consultations with family physicians, gynecologists, and neurologists (P < .0001). In addition, they were more likely to utilize emergency services; take more medications, mostly analgesics; and undergo more laboratory studies and brain imaging.
Those with aura had significantly more specialist consultations and took more medications compared with migraine patients without aura.
There was a statistically significant increase in the use of epidural anesthesia for migraine patients (40.5% of women without migraine; 45.7% of those with migraine accompanied by aura; and 47.5% of migraine patients without aura).
This was an “interesting” finding, said Dr. Lev. “We didn’t know what to expect; people with migraine are used to pain, so the question was, will they tolerate pain better or be more afraid of pain?”
Women with migraine also experienced more assisted deliveries with increased use of vacuums and forceps.
During the 3-month postpartum period, women with migraine sought more medical consultations and used more medications compared with control patients. They also underwent more lab examinations and more brain imaging during this period.
Dr. Lev noted that some of these evaluations may have been postponed because of the pregnancy.
Women with migraine also had a greater risk for postpartum depression, which Dr. Lev found “concerning.” She noted that depression is often underreported but is treatable. Women with migraine should be monitored for depression post partum, she said.
It’s unclear which factors contribute to the increased risk for pregnancy complications in women with migraine. Dr. Lev said she doesn’t believe it’s drug related.
“Although they’re taking more medications than people who don’t have migraine, we still are giving very low doses and only safe medicines, so I don’t think these increased risks are side effects,” she said.
She noted that women with migraine have more cardiovascular complications, including stroke and myocardial infarction, although these generally affect older patients.
Dr. Lev also noted that pain, especially chronic pain, can cause depression. “We know that people with migraine have more depression and anxiety, so maybe that also affects them during their pregnancy and after,” she said.
She suggested that pregnant women with migraine be considered high risk and be managed via specialized clinics.
Room for improvement
Commenting on the research, Lauren Doyle Strauss, DO, associate professor of neurology, Wake Forest University, Winston-Salem, N.C., who has written about the management of migraine during pregnancy, said studies such as this help raise awareness about pregnancy risks in migraine patients. Dr. Strauss did not attend the live presentation but is aware of the findings.
The increased use of epidurals during delivery among migraine patients in the study makes some sense, said Dr. Strauss. “It kind of shows a comfort level with medicines.”
She expressed concern that such research may be “skewed” because it includes patients with more severe migraine. If less severe cases were included in this research, “maybe there would still be higher risks, but not as high as what we have been finding in some of our studies,” she said.
Dr. Strauss said she feels the medical community should do a better job of identifying and diagnosing migraine. She said she would like to see migraine screening become a routine part of obstetric/gynecologic care. Doctors should counsel migraine patients who wish to become pregnant about potential risks, said Dr. Strauss. “We need to be up front in telling them when to seek care and when to report symptoms and not to wait for it to become super severe,” she said.
She also believes doctors should be “proactive” in helping patients develop a treatment plan before becoming pregnant, because the limited pain control options available for pregnant patients can take time to have an effect.
Also commenting on the study findings, Nina Riggins, MD, PhD, clinical associate professor of neurology at the University of California, San Francisco, said the study raises “important questions” and has “important aims.”
She believes the study reinforces the importance of collaboration between experts in primary care, obstetrics/gynecology, and neurology. However, she was surprised at some of the investigators’ assertions that there are no differences in migraine among prepubertal children and that the course of migraine for men is stable throughout their life span.
“There is literature that supports the view that the prevalence in boys is higher in prepuberty, and studies do show that migraine prevalence decreases in older adults – men and women,” she said.
There is still not enough evidence to determine that antiemetics and triptans are safe during pregnancy or that pregnant women with migraine should be taking acetylsalicylic acid, said Dr. Riggins.
The investigators, Dr. Strauss, and Dr. Riggins have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests. Although pregnancy is generally considered a “safe period” for women with migraine, “we actually found they have more diabetes, more hypertension, more blood clots, more complications during their delivery, and more postpartum complications,” said study investigator Nirit Lev, MD, PhD, head, department of neurology, Meir Medical Center, Kfar Saba Sackler Faculty of Medicine, Tel Aviv University.
The results highlight the need for clinicians “to take people with migraines seriously” and reinforce the idea that migraine is not “just a headache,” said Dr. Lev.
Pregnant women with migraine should be considered high risk and have specialized neurologic follow-up during pregnancy and the postpartum period, she added.
The findings were presented at the 2021 Congress of the European Academy of Neurology.
Prevalent, disabling
Migraine is one of the most prevalent and disabling neurologic disorders. Such disorders are major causes of death and disability.
In childhood, there’s no difference between the sexes in terms of migraine prevalence, but after puberty, migraine is about three times more common in women than men. Fluctuating levels of estrogen and progesterone likely explain these differences, said Dr. Lev.
The prevalence of migraine among females peaks during their reproductive years. Most female migraine patients report an improvement in headache symptoms during pregnancy, with some experiencing a “complete remission.” However, a minority report worsening of migraine when expecting a child, said Dr. Lev.
Some patients have their first aura during pregnancy. The most common migraine aura is visual, a problem with the visual field that can affect motor and sensory functioning, said Dr. Lev.
Managing migraine during pregnancy is “very complicated,” said Dr. Lev. She said the first-line treatment is paracetamol (acetaminophen) and stressed that taking opioids should be avoided.
Retrospective database study
For the study, the researchers retrospectively reviewed pregnancy and delivery records from a database of Clalit Medical Services, which has more than 4.5 million members and is the largest such database in Israel. They collected demographic data and information on mode of delivery, medical and obstetric complications, hospitalizations, emergency department visits, use of medications, laboratory reports, and medical consultations.
The study included 145,102 women who gave birth from 2014 to 2020.
Of these, 10,646 had migraine without aura, and 1,576 had migraine with aura. The migraine diagnoses, which were based on International Headache Society criteria and diagnostic codes, were made prior to pregnancy.
Dr. Lev noted that the number of patients with migraine is likely an underestimation because migraine is “not always diagnosed.”
Results showed that the risk for obstetric complications was higher among pregnant women with migraine, especially those with aura, in comparison with women without migraine. About 6.9% of patients with migraine without aura were admitted to high-risk hospital departments, compared with 6% of pregnant control patients who did not have migraine (P < .0001). For patients with migraine with aura, the risk for admissions was even higher (8.7%; P < .0001 vs. control patients and P < .03 vs. patients with migraine without aura) and was “very highly statistically significant,” said Dr. Lev.
Pregnant women with migraine were at significantly increased risk for gestational diabetes, hyperlipidemia, and being diagnosed with a psychiatric disorder (all P < .0001). These women were also more likely to experience preeclampsia and blood clots (P < .0001).
Unexpected finding
The finding that the risk for diabetes was higher was “unexpected,” inasmuch as older women with migraine are typically at increased risk for metabolic syndrome and higher body mass index, said Dr. Lev.
Migraine patients had significantly more consultations with family physicians, gynecologists, and neurologists (P < .0001). In addition, they were more likely to utilize emergency services; take more medications, mostly analgesics; and undergo more laboratory studies and brain imaging.
Those with aura had significantly more specialist consultations and took more medications compared with migraine patients without aura.
There was a statistically significant increase in the use of epidural anesthesia for migraine patients (40.5% of women without migraine; 45.7% of those with migraine accompanied by aura; and 47.5% of migraine patients without aura).
This was an “interesting” finding, said Dr. Lev. “We didn’t know what to expect; people with migraine are used to pain, so the question was, will they tolerate pain better or be more afraid of pain?”
Women with migraine also experienced more assisted deliveries with increased use of vacuums and forceps.
During the 3-month postpartum period, women with migraine sought more medical consultations and used more medications compared with control patients. They also underwent more lab examinations and more brain imaging during this period.
Dr. Lev noted that some of these evaluations may have been postponed because of the pregnancy.
Women with migraine also had a greater risk for postpartum depression, which Dr. Lev found “concerning.” She noted that depression is often underreported but is treatable. Women with migraine should be monitored for depression post partum, she said.
It’s unclear which factors contribute to the increased risk for pregnancy complications in women with migraine. Dr. Lev said she doesn’t believe it’s drug related.
“Although they’re taking more medications than people who don’t have migraine, we still are giving very low doses and only safe medicines, so I don’t think these increased risks are side effects,” she said.
She noted that women with migraine have more cardiovascular complications, including stroke and myocardial infarction, although these generally affect older patients.
Dr. Lev also noted that pain, especially chronic pain, can cause depression. “We know that people with migraine have more depression and anxiety, so maybe that also affects them during their pregnancy and after,” she said.
She suggested that pregnant women with migraine be considered high risk and be managed via specialized clinics.
Room for improvement
Commenting on the research, Lauren Doyle Strauss, DO, associate professor of neurology, Wake Forest University, Winston-Salem, N.C., who has written about the management of migraine during pregnancy, said studies such as this help raise awareness about pregnancy risks in migraine patients. Dr. Strauss did not attend the live presentation but is aware of the findings.
The increased use of epidurals during delivery among migraine patients in the study makes some sense, said Dr. Strauss. “It kind of shows a comfort level with medicines.”
She expressed concern that such research may be “skewed” because it includes patients with more severe migraine. If less severe cases were included in this research, “maybe there would still be higher risks, but not as high as what we have been finding in some of our studies,” she said.
Dr. Strauss said she feels the medical community should do a better job of identifying and diagnosing migraine. She said she would like to see migraine screening become a routine part of obstetric/gynecologic care. Doctors should counsel migraine patients who wish to become pregnant about potential risks, said Dr. Strauss. “We need to be up front in telling them when to seek care and when to report symptoms and not to wait for it to become super severe,” she said.
She also believes doctors should be “proactive” in helping patients develop a treatment plan before becoming pregnant, because the limited pain control options available for pregnant patients can take time to have an effect.
Also commenting on the study findings, Nina Riggins, MD, PhD, clinical associate professor of neurology at the University of California, San Francisco, said the study raises “important questions” and has “important aims.”
She believes the study reinforces the importance of collaboration between experts in primary care, obstetrics/gynecology, and neurology. However, she was surprised at some of the investigators’ assertions that there are no differences in migraine among prepubertal children and that the course of migraine for men is stable throughout their life span.
“There is literature that supports the view that the prevalence in boys is higher in prepuberty, and studies do show that migraine prevalence decreases in older adults – men and women,” she said.
There is still not enough evidence to determine that antiemetics and triptans are safe during pregnancy or that pregnant women with migraine should be taking acetylsalicylic acid, said Dr. Riggins.
The investigators, Dr. Strauss, and Dr. Riggins have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
From EAN 2021
Focus on diabetes mellitus
Diabetes mellitus affects 10% of the US population, and as many as one-third of US adults have prediabetes, according to the National Diabetes Statistics Report 2020 from the Centers for Disease Control and Prevention. While diabetes is associated with significant long-term morbidity and mortality, with early identification and interventions, lifestyle modifications can significantly improve long-term health.
As with obesity (see “Focus on obesity” in OBG Management, May 2021), it is difficult to address lifestyle modifications with patients who have diabetes. However, many apps can be leveraged to aid physicians in this effort.
Diabetes app considerations
Obstetrician-gynecologists can play a pivotal role in helping to screen women for diabetes. When applying the ACOG-recommended rubric to evaluate the quality of an app that is targeted to address screening and diagnosing diabetes, it’s important to consider the app’s timeliness, authority, usefulness, and design.
There are point-of-care apps that include a few simple questions that can quickly identify which women should be screened. Some apps combine screening questions with testing results to streamline screening and diagnosis of diabetes and prediabetes. These apps also provide clinical content to help physicians educate, initiate, and even treat diabetes if they desire.
A wealth of patient-centered apps are available to help patients address a diagnosis of diabetes. Apps that provide real-time feedback, motivational features to engage the user, and links to nutritional, fitness, and diabetic goals provide a woman with a comprehensive and personalized experience that can considerably improve health.
By incorporating apps and engaging with our patients on app technology, ObGyns can successfully partner with women to decrease morbidity with respect to diabetes mellitus and its long-term implications. ●
Diabetes mellitus affects 10% of the US population, and as many as one-third of US adults have prediabetes, according to the National Diabetes Statistics Report 2020 from the Centers for Disease Control and Prevention. While diabetes is associated with significant long-term morbidity and mortality, with early identification and interventions, lifestyle modifications can significantly improve long-term health.
As with obesity (see “Focus on obesity” in OBG Management, May 2021), it is difficult to address lifestyle modifications with patients who have diabetes. However, many apps can be leveraged to aid physicians in this effort.
Diabetes app considerations
Obstetrician-gynecologists can play a pivotal role in helping to screen women for diabetes. When applying the ACOG-recommended rubric to evaluate the quality of an app that is targeted to address screening and diagnosing diabetes, it’s important to consider the app’s timeliness, authority, usefulness, and design.
There are point-of-care apps that include a few simple questions that can quickly identify which women should be screened. Some apps combine screening questions with testing results to streamline screening and diagnosis of diabetes and prediabetes. These apps also provide clinical content to help physicians educate, initiate, and even treat diabetes if they desire.
A wealth of patient-centered apps are available to help patients address a diagnosis of diabetes. Apps that provide real-time feedback, motivational features to engage the user, and links to nutritional, fitness, and diabetic goals provide a woman with a comprehensive and personalized experience that can considerably improve health.
By incorporating apps and engaging with our patients on app technology, ObGyns can successfully partner with women to decrease morbidity with respect to diabetes mellitus and its long-term implications. ●
Diabetes mellitus affects 10% of the US population, and as many as one-third of US adults have prediabetes, according to the National Diabetes Statistics Report 2020 from the Centers for Disease Control and Prevention. While diabetes is associated with significant long-term morbidity and mortality, with early identification and interventions, lifestyle modifications can significantly improve long-term health.
As with obesity (see “Focus on obesity” in OBG Management, May 2021), it is difficult to address lifestyle modifications with patients who have diabetes. However, many apps can be leveraged to aid physicians in this effort.
Diabetes app considerations
Obstetrician-gynecologists can play a pivotal role in helping to screen women for diabetes. When applying the ACOG-recommended rubric to evaluate the quality of an app that is targeted to address screening and diagnosing diabetes, it’s important to consider the app’s timeliness, authority, usefulness, and design.
There are point-of-care apps that include a few simple questions that can quickly identify which women should be screened. Some apps combine screening questions with testing results to streamline screening and diagnosis of diabetes and prediabetes. These apps also provide clinical content to help physicians educate, initiate, and even treat diabetes if they desire.
A wealth of patient-centered apps are available to help patients address a diagnosis of diabetes. Apps that provide real-time feedback, motivational features to engage the user, and links to nutritional, fitness, and diabetic goals provide a woman with a comprehensive and personalized experience that can considerably improve health.
By incorporating apps and engaging with our patients on app technology, ObGyns can successfully partner with women to decrease morbidity with respect to diabetes mellitus and its long-term implications. ●
Adverse pregnancy outcomes and later cardiovascular disease
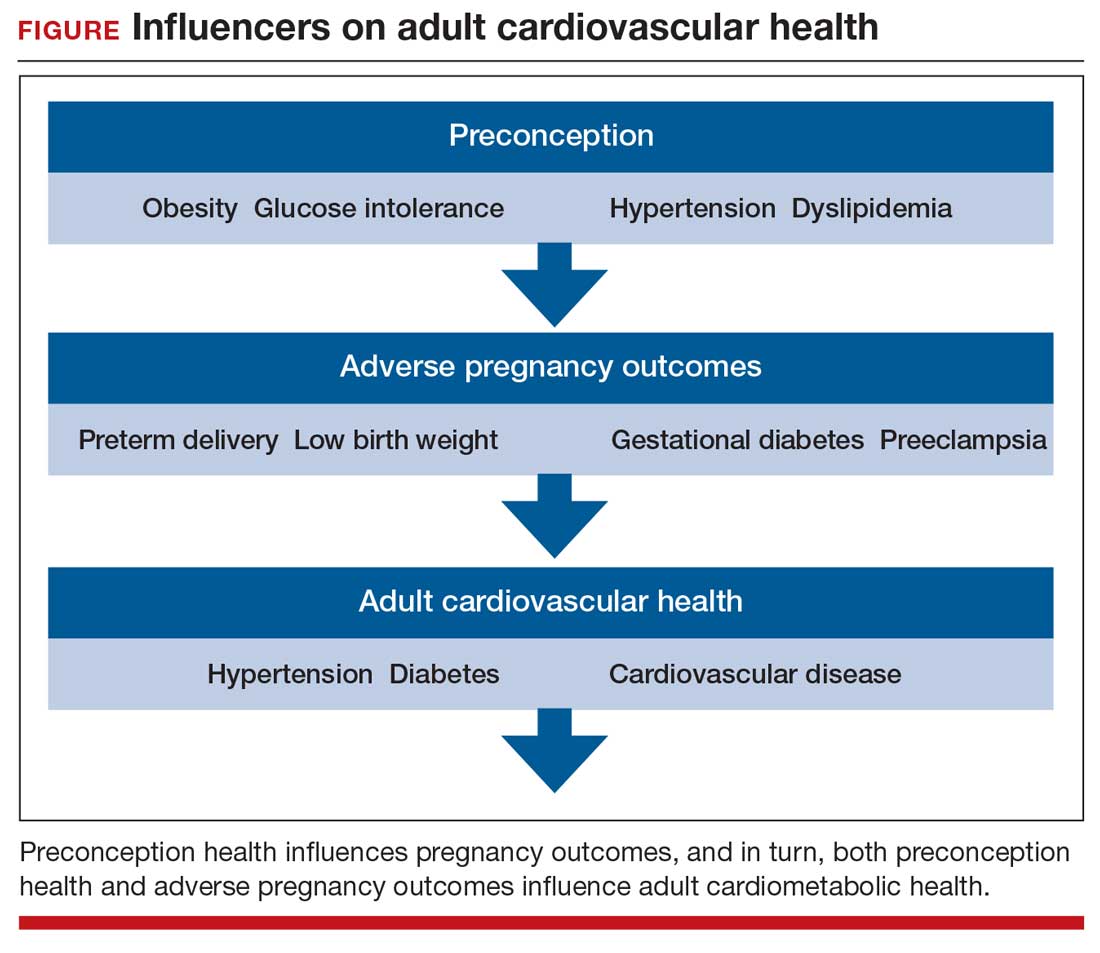
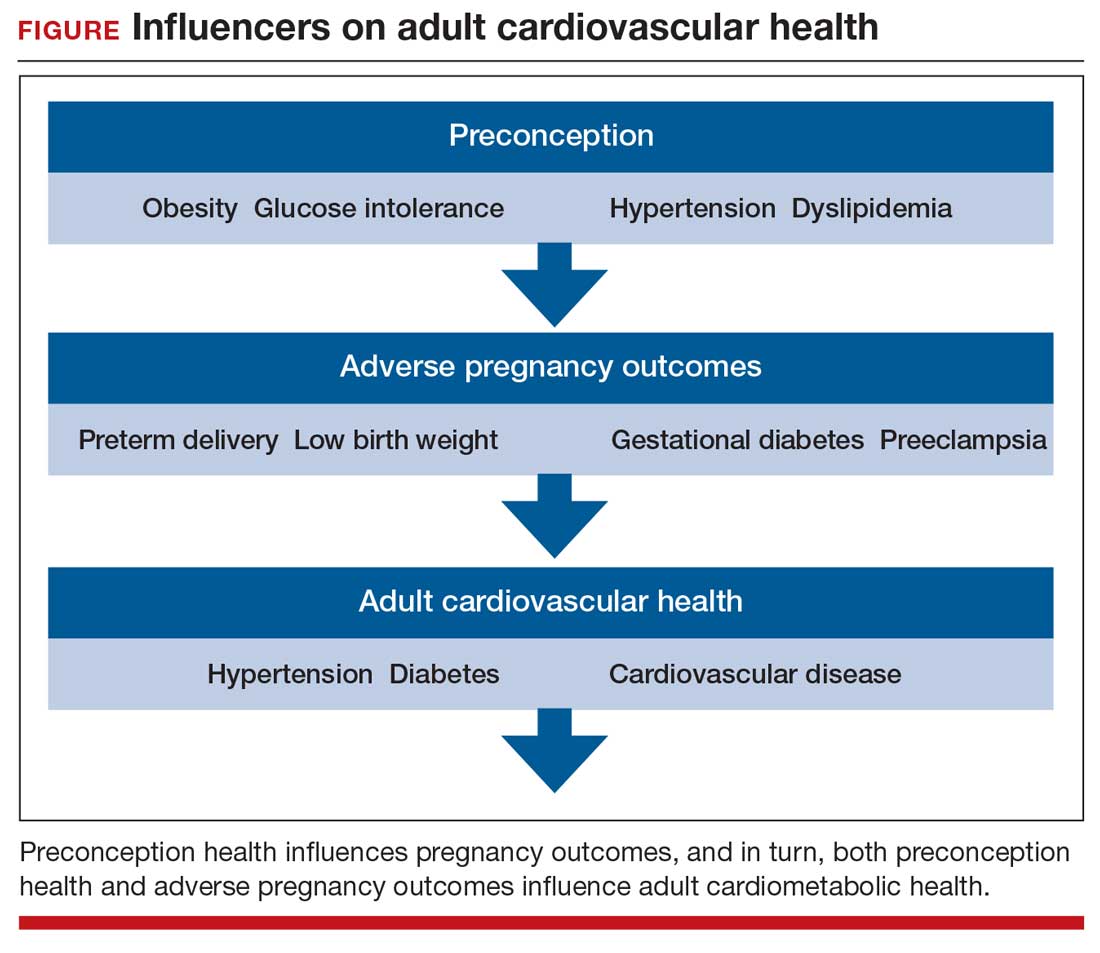
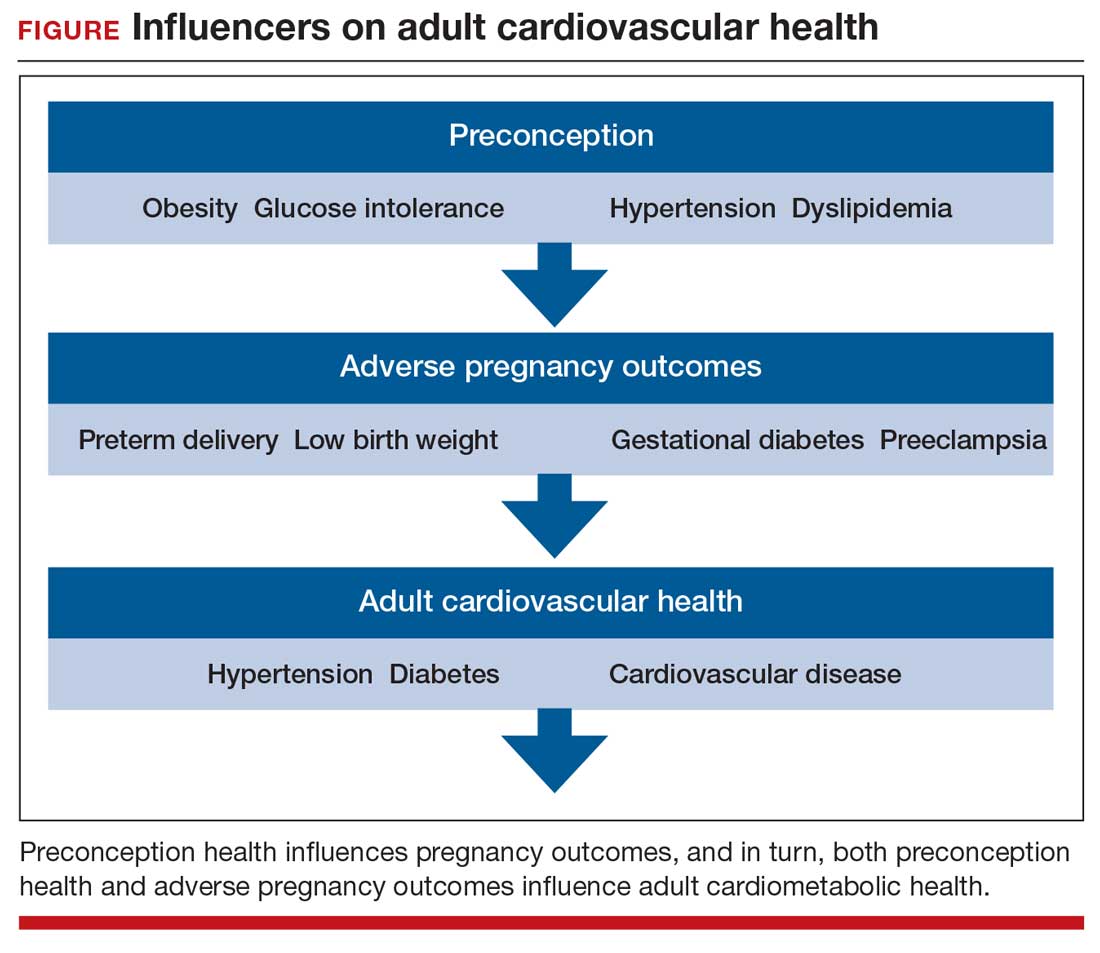
Preconception health influences pregnancy outcomes, and in turn, both preconception health and an APO influence adult cardiometabolic health (FIGURE). This editorial is focused on the link between APOs and later cardiometabolic morbidity and mortality, recognizing that preconception health greatly influences the risk of an APO and lifetime cardiometabolic disease.
Adverse pregnancy outcomes
Major APOs include miscarriage, preterm birth (birth <37 weeks’ gestation), low birth weight (birth weight ≤2,500 g; 5.5 lb), gestational diabetes (GDM), preeclampsia, and placental abruption. In the United States, among all births, reported rates of the following APOs are:1-3
- preterm birth, 10.2%
- low birth weight, 8.3%
- GDM, 6%
- preeclampsia, 5%
- placental abruption, 1%.
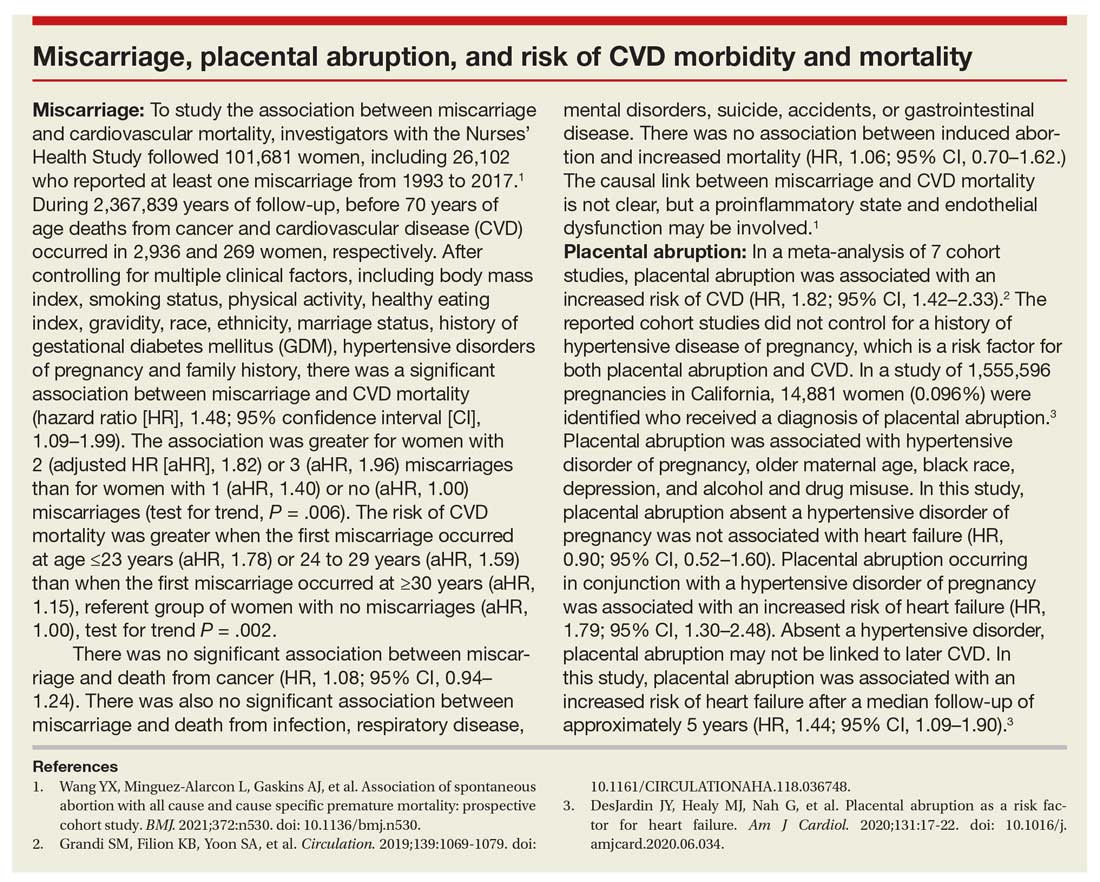
Miscarriage occurs in approximately 10% to 15% of pregnancies, influenced by both the age of the woman and the method used to diagnose pregnancy.4 Miscarriage, preterm birth, low birth weight, GDM, preeclampsia, and placental abruption have been reported to be associated with an increased risk of later cardiovascular morbidity and mortality.
APOs and cardiovascular disease
Cardiovascular disease (CVD) affects the majority of people past the age of 60 years and includes 4 major subcategories:
- coronary heart disease, including myocardial infarction, angina, and heart failure
- CVD, stroke, and transient ischemic attack
- peripheral artery disease
- atherosclerosis of the aorta leading to aortic aneurysm.
Multiple meta-analyses report that APOs are associated with CVD in later life. A comprehensive review reported that the risk of CVD was increased following a pregnancy with one of these APOs: severe preeclampsia (odds ratio [OR], 2.74), GDM (OR, 1.68), preterm birth (OR, 1.93), low birth weight (OR, 1.29), and placental abruption (OR, 1.82).5
The link between APOs and CVD may be explained in part by the association of APOs with multiple risk factors for CVD, including chronic hypertension, type 2 diabetes mellitus (T2DM), and dyslipidemia. A meta-analysis of 43 studies reported that, compared with controls, women with a history of preeclampsia have a 3.13 times greater risk of developing chronic hypertension.6 Among women with preeclampsia, approximately 20% will develop hypertension within 15 years.7 A meta-analysis of 20 studies reported that women with a history of GDM had a 9.51-times greater risk of developing T2DM than women without GDM.8 Among women with a history of GDM, over 16 years of follow-up, T2DM was diagnosed in 16.2%, compared with 1.9% of control women.8
CVD prevention—Breastfeeding: An antidote for APOs
Pregnancy stresses both the cardiovascular and metabolic systems. Breastfeeding is an antidote to the stresses imposed by pregnancy. Breastfeeding women have lower blood glucose9 and blood pressure.10
Breastfeeding reduces the risk of CVD. In a study of 100,864 parous Australian women, with a mean age of 60 years, ever breastfeeding was associated a lower risk of CVD hospitalization (adjusted hazard ratio [aHR], 0.86; 95% confidence interval [CI], 0.78–0.96; P = .005) and CVD mortality (aHR, 0.66; 95% CI, 0.49–0.89; P = .006).11
Continue to: CVD prevention—American Heart Association recommendations...
CVD prevention—American Heart Association recommendations
The American Heart Association12 recommends lifestyle interventions to reduce the risk of CVD, including:
- Eat a high-quality diet that includes vegetables, fruit, whole grains, beans, legumes, nuts, plant-based protein, lean animal protein, and fish.
- Limit intake of sugary drinks and foods, fatty or processed meats, full-fat dairy products, eggs, highly processed foods, and tropical oils.
- Exercise at least 150 minutes weekly at a moderate activity level, including muscle-strengthening activity.
- Reduce prolonged intervals of sitting.
- Live a tobacco- and nicotine-free life.
- Strive to maintain a normal body mass index.
- Consider using an activity tracker to monitor activity level.
- After 40 years of age calculate CVD risk using a validated calculator such as the American Cardiology Association risk calculator.13 This calculator uses age, gender, and lipid and blood pressure measurements to calculate the 10-year risk of atherosclerotic CVD, including coronary death, myocardial infarction, and stroke.
Medications to reduce CVD risk
Historically, ObGyns have not routinely prescribed medications to treat hypertension, dyslipidemia, or to prevent diabetes. The recent increase in the valuation of return ambulatory visits and a reduction in the valuation assigned to procedural care may provide ObGyn practices the additional resources needed to manage some chronic diseases. Physician assistants and nurse practitioners may help ObGyn practices to manage hypertension, dyslipidemia, and prediabetes.
Prior to initiating a medicine, counseling about healthy living, including smoking cessation, exercise, heart-healthy diet, and achieving an optimal body mass index is warranted.
For treatment of stage II hypertension, defined as blood pressure (BP) measurements with systolic BP ≥140 mm Hg and diastolic BP ≥90 mm Hg, therapeutic lifestyle interventions include: optimizing weight, following the DASH diet, restricting dietary sodium, physical activity, and reducing alcohol consumption. Medication treatment for essential hypertension is guided by the magnitude of BP reduction needed to achieve normotension. For women with hypertension needing antihypertensive medication and planning another pregnancy in the near future, labetalol or extended-release nifedipine may be first-line medications. For women who have completed their families or who have no immediate plans for pregnancy, an angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, calcium channel blocker, or thiazide diuretic are commonly prescribed.14
For the treatment of elevated low-density lipoprotein (LDL) cholesterol in women who have not had a cardiovascular event, statin therapy is often warranted when both the LDL cholesterol is >100 mg/dL and the woman has a calculated 10-year risk of >10% for a cardiovascular event using the American Heart Association or American College of Cardiology calculator. Most women who meet these criteria will be older than age 40 years and many will be under the care of an internal medicine or family medicine specialist, limiting the role of the ObGyn.15-17
For prevention of diabetes in women with a history of GDM, both weight loss and metformin (1,750 mg daily) have been shown in clinical trials to reduce the risk of developing T2DM.18 Among 350 women with a history of GDM who were followed for 10 years, metformin 850 mg twice daily reduced the risk of developing T2DM by 40% compared with placebo.19 In the same study, lifestyle changes without metformin, including loss of 7% of body weight plus 150 minutes of exercise weekly was associated with a 35% reduction in the risk of developing T2DM.19 Metformin is one of the least expensive prescription medications and is cost-effective for the prevention of T2DM.18
Low-dose aspirin treatment for the prevention of CVD in women who have not had a cardiovascular event must balance a modest reduction in cardiovascular events with a small increased risk of bleeding events. The US Preventive Services Task Force (USPSTF) recommends low-dose aspirin for a limited group of women, those aged 50 to 59 years of age with a 10-year risk of a cardiovascular event >10% who are willing to take aspirin for 10 years. The USPSTF concluded that there is insufficient evidence to recommend low-dose aspirin prevention of CVD in women aged <50 years.20
Continue to: Beyond the fourth trimester...
Beyond the fourth trimester
The fourth trimester is the 12-week period following birth. At the comprehensive postpartum visit, the American College of Obstetricians and Gynecologists (ACOG) recommends that women with APOs be counseled about their increased lifetime risk of maternal cardiometabolic disease.21 In addition, ACOG recommends that at this visit the clinician who will assume primary responsibility for the woman’s ongoing medical care in her primary medical home be clarified. One option is to ensure a high-quality hand-off to an internal medicine or family medicine clinician. Another option is for a clinician in the ObGyn’s office practice, including a physician assistant, nurse practitioner, or office-based ObGyn, to assume some role in the primary care of the woman.
An APO is not only a pregnancy problem
An APO reverberates across a woman’s lifetime, increasing the risk of CVD and diabetes. In the United States the mean age at first birth is 27 years.1 The mean life expectancy of US women is 81 years.22 Following a birth complicated by an APO there are 5 decades of opportunity to improve health through lifestyle changes and medication treatment of obesity, hypertension, dyslipidemia, and hyperglycemia, thereby reducing the risk of CVD.
- Martin JA, Hamilton BE, Osterman MJ, et al. Births: final data for 2019. Natl Vital Stat Rep. 2021;70:1-51.
- Deputy NP, Kim SY, Conrey EJ, et al. Prevalence and changes in preexisting diabetes and gestational diabetes among women who had a live birth—United States, 2012-2016. MMWR Morb Mortal Wkly Rep. 2018;67:1201-1207. doi: 10.15585/mmwr.mm6743a2.
- Fingar KR, Mabry-Hernandez I, Ngo-Metzger Q, et al. Delivery hospitalizations involving preeclampsia and eclampsia, 2005–2014. Statistical brief #222. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Agency for Healthcare Research and Quality: Rockville, MD; April 2017.
- Magnus MC, Wilcox AJ, Morken NH, et al. Role of maternal age and pregnancy history in risk of miscarriage: prospective register-based study. BMJ. 2019;364:869.
- Parikh NI, Gonzalez JM, Anderson CAM, et al. Adverse pregnancy outcomes and cardiovascular disease risk: unique opportunities for cardiovascular disease prevention in women. Circulation. 2021;143:e902-e916. doi: 10.1161 /CIR.0000000000000961.
- Brown MC, Best KE, Pearce MS, et al. Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur J Epidemiol. 2013;28:1-19. doi: 10.1007/s10654-013- 9762-6.
- Groenfol TK, Zoet GA, Franx A, et al; on behalf of the PREVENT Group. Trajectory of cardiovascular risk factors after hypertensive disorders of pregnancy. Hypertension. 2019;73:171-178. doi: 10.1161/HYPERTENSIONAHA.118.11726.
- Vounzoulaki E, Khunti K, Abner SC, et al. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ. 2020;369:m1361. doi: 10.1136/bmj.m1361.
- Tarrant M, Chooniedass R, Fan HSL, et al. Breastfeeding and postpartum glucose regulation among women with prior gestational diabetes: a systematic review. J Hum Lact. 2020;36:723-738. doi: 10.1177/0890334420950259.
- Park S, Choi NK. Breastfeeding and maternal hypertension. Am J Hypertens. 2018;31:615-621. doi: 10.1093/ajh/hpx219.
- Nguyen B, Gale J, Nassar N, et al. Breastfeeding and cardiovascular disease hospitalization and mortality in parous women: evidence from a large Australian cohort study. J Am Heart Assoc. 2019;8:e011056. doi: 10.1161/JAHA.118.011056.
- Eight things you can do to prevent heart disease and stroke. American Heart Association website. https://www.heart.org/en/healthy-living /healthy-lifestyle/prevent-heart-disease-andstroke. Last Reviewed March 14, 2019. Accessed May 19, 2021.
- ASCVD risk estimator plus. American College of Cardiology website. https://tools.acc.org /ascvd-risk-estimator-plus/#!/calculate /estimate/. Accessed May 19, 2021.
- Ferdinand KC, Nasser SA. Management of essential hypertension. Cardiol Clin. 2017;35:231-246. doi: 10.1016/j.ccl.2016.12.005.
- Packard CJ. LDL cholesterol: how low to go? Trends Cardiovasc Med. 2018;28:348-354. doi: 10.1016/j.tcm.2017.12.011.
- Simons L. An updated review of lipid-modifying therapy. Med J Aust. 2019;211:87-92. doi: 10.5694 /mja2.50142.
- Chou R, Dana T, Blazina I, et al. Statins for the prevention of cardiovascular disease in adults: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;316:2008. doi: 10.1001/jama.2015.15629.
- Moin T, Schmittdiel JA, Flory JH, et al. Review of metformin use for type 2 diabetes mellitus prevention. Am J Prev Med. 2018;55:565-574. doi: 10.1016/j.amepre.2018.04.038.
- Aorda VR, Christophi CA, Edelstein SL, et al, for the Diabetes Prevention Program Research Group. The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the Diabetes Prevention Program outcomes study 10-year follow-up. J Clin Endocrinol Metab. 2015;100:1646- 1653. doi: 10.1210/jc.2014-3761.
- Bibbins-Domingo K, U.S. Preventive Services Task Force. Aspirin use of the primary prevention of cardiovascular disease and colorectal cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Int Med. 2016; 164: 836-845. doi: 10.7326/M16-0577.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 736: optimizing postpartum care. Obstet Gynecol. 2018;131:e140-e150. doi: 10.1097 /AOG.0000000000002633.
- National Center for Health Statistics. Health, United States, 2017: Table 015. Hyattsville, MD; 2021. https://www.cdc.gov/nchs/data /hus/2017/015.pdf. Accessed May 18, 2021.
Preconception health influences pregnancy outcomes, and in turn, both preconception health and an APO influence adult cardiometabolic health (FIGURE). This editorial is focused on the link between APOs and later cardiometabolic morbidity and mortality, recognizing that preconception health greatly influences the risk of an APO and lifetime cardiometabolic disease.
Adverse pregnancy outcomes
Major APOs include miscarriage, preterm birth (birth <37 weeks’ gestation), low birth weight (birth weight ≤2,500 g; 5.5 lb), gestational diabetes (GDM), preeclampsia, and placental abruption. In the United States, among all births, reported rates of the following APOs are:1-3
- preterm birth, 10.2%
- low birth weight, 8.3%
- GDM, 6%
- preeclampsia, 5%
- placental abruption, 1%.
Miscarriage occurs in approximately 10% to 15% of pregnancies, influenced by both the age of the woman and the method used to diagnose pregnancy.4 Miscarriage, preterm birth, low birth weight, GDM, preeclampsia, and placental abruption have been reported to be associated with an increased risk of later cardiovascular morbidity and mortality.
APOs and cardiovascular disease
Cardiovascular disease (CVD) affects the majority of people past the age of 60 years and includes 4 major subcategories:
- coronary heart disease, including myocardial infarction, angina, and heart failure
- CVD, stroke, and transient ischemic attack
- peripheral artery disease
- atherosclerosis of the aorta leading to aortic aneurysm.
Multiple meta-analyses report that APOs are associated with CVD in later life. A comprehensive review reported that the risk of CVD was increased following a pregnancy with one of these APOs: severe preeclampsia (odds ratio [OR], 2.74), GDM (OR, 1.68), preterm birth (OR, 1.93), low birth weight (OR, 1.29), and placental abruption (OR, 1.82).5
The link between APOs and CVD may be explained in part by the association of APOs with multiple risk factors for CVD, including chronic hypertension, type 2 diabetes mellitus (T2DM), and dyslipidemia. A meta-analysis of 43 studies reported that, compared with controls, women with a history of preeclampsia have a 3.13 times greater risk of developing chronic hypertension.6 Among women with preeclampsia, approximately 20% will develop hypertension within 15 years.7 A meta-analysis of 20 studies reported that women with a history of GDM had a 9.51-times greater risk of developing T2DM than women without GDM.8 Among women with a history of GDM, over 16 years of follow-up, T2DM was diagnosed in 16.2%, compared with 1.9% of control women.8
CVD prevention—Breastfeeding: An antidote for APOs
Pregnancy stresses both the cardiovascular and metabolic systems. Breastfeeding is an antidote to the stresses imposed by pregnancy. Breastfeeding women have lower blood glucose9 and blood pressure.10
Breastfeeding reduces the risk of CVD. In a study of 100,864 parous Australian women, with a mean age of 60 years, ever breastfeeding was associated a lower risk of CVD hospitalization (adjusted hazard ratio [aHR], 0.86; 95% confidence interval [CI], 0.78–0.96; P = .005) and CVD mortality (aHR, 0.66; 95% CI, 0.49–0.89; P = .006).11
Continue to: CVD prevention—American Heart Association recommendations...
CVD prevention—American Heart Association recommendations
The American Heart Association12 recommends lifestyle interventions to reduce the risk of CVD, including:
- Eat a high-quality diet that includes vegetables, fruit, whole grains, beans, legumes, nuts, plant-based protein, lean animal protein, and fish.
- Limit intake of sugary drinks and foods, fatty or processed meats, full-fat dairy products, eggs, highly processed foods, and tropical oils.
- Exercise at least 150 minutes weekly at a moderate activity level, including muscle-strengthening activity.
- Reduce prolonged intervals of sitting.
- Live a tobacco- and nicotine-free life.
- Strive to maintain a normal body mass index.
- Consider using an activity tracker to monitor activity level.
- After 40 years of age calculate CVD risk using a validated calculator such as the American Cardiology Association risk calculator.13 This calculator uses age, gender, and lipid and blood pressure measurements to calculate the 10-year risk of atherosclerotic CVD, including coronary death, myocardial infarction, and stroke.
Medications to reduce CVD risk
Historically, ObGyns have not routinely prescribed medications to treat hypertension, dyslipidemia, or to prevent diabetes. The recent increase in the valuation of return ambulatory visits and a reduction in the valuation assigned to procedural care may provide ObGyn practices the additional resources needed to manage some chronic diseases. Physician assistants and nurse practitioners may help ObGyn practices to manage hypertension, dyslipidemia, and prediabetes.
Prior to initiating a medicine, counseling about healthy living, including smoking cessation, exercise, heart-healthy diet, and achieving an optimal body mass index is warranted.
For treatment of stage II hypertension, defined as blood pressure (BP) measurements with systolic BP ≥140 mm Hg and diastolic BP ≥90 mm Hg, therapeutic lifestyle interventions include: optimizing weight, following the DASH diet, restricting dietary sodium, physical activity, and reducing alcohol consumption. Medication treatment for essential hypertension is guided by the magnitude of BP reduction needed to achieve normotension. For women with hypertension needing antihypertensive medication and planning another pregnancy in the near future, labetalol or extended-release nifedipine may be first-line medications. For women who have completed their families or who have no immediate plans for pregnancy, an angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, calcium channel blocker, or thiazide diuretic are commonly prescribed.14
For the treatment of elevated low-density lipoprotein (LDL) cholesterol in women who have not had a cardiovascular event, statin therapy is often warranted when both the LDL cholesterol is >100 mg/dL and the woman has a calculated 10-year risk of >10% for a cardiovascular event using the American Heart Association or American College of Cardiology calculator. Most women who meet these criteria will be older than age 40 years and many will be under the care of an internal medicine or family medicine specialist, limiting the role of the ObGyn.15-17
For prevention of diabetes in women with a history of GDM, both weight loss and metformin (1,750 mg daily) have been shown in clinical trials to reduce the risk of developing T2DM.18 Among 350 women with a history of GDM who were followed for 10 years, metformin 850 mg twice daily reduced the risk of developing T2DM by 40% compared with placebo.19 In the same study, lifestyle changes without metformin, including loss of 7% of body weight plus 150 minutes of exercise weekly was associated with a 35% reduction in the risk of developing T2DM.19 Metformin is one of the least expensive prescription medications and is cost-effective for the prevention of T2DM.18
Low-dose aspirin treatment for the prevention of CVD in women who have not had a cardiovascular event must balance a modest reduction in cardiovascular events with a small increased risk of bleeding events. The US Preventive Services Task Force (USPSTF) recommends low-dose aspirin for a limited group of women, those aged 50 to 59 years of age with a 10-year risk of a cardiovascular event >10% who are willing to take aspirin for 10 years. The USPSTF concluded that there is insufficient evidence to recommend low-dose aspirin prevention of CVD in women aged <50 years.20
Continue to: Beyond the fourth trimester...
Beyond the fourth trimester
The fourth trimester is the 12-week period following birth. At the comprehensive postpartum visit, the American College of Obstetricians and Gynecologists (ACOG) recommends that women with APOs be counseled about their increased lifetime risk of maternal cardiometabolic disease.21 In addition, ACOG recommends that at this visit the clinician who will assume primary responsibility for the woman’s ongoing medical care in her primary medical home be clarified. One option is to ensure a high-quality hand-off to an internal medicine or family medicine clinician. Another option is for a clinician in the ObGyn’s office practice, including a physician assistant, nurse practitioner, or office-based ObGyn, to assume some role in the primary care of the woman.
An APO is not only a pregnancy problem
An APO reverberates across a woman’s lifetime, increasing the risk of CVD and diabetes. In the United States the mean age at first birth is 27 years.1 The mean life expectancy of US women is 81 years.22 Following a birth complicated by an APO there are 5 decades of opportunity to improve health through lifestyle changes and medication treatment of obesity, hypertension, dyslipidemia, and hyperglycemia, thereby reducing the risk of CVD.
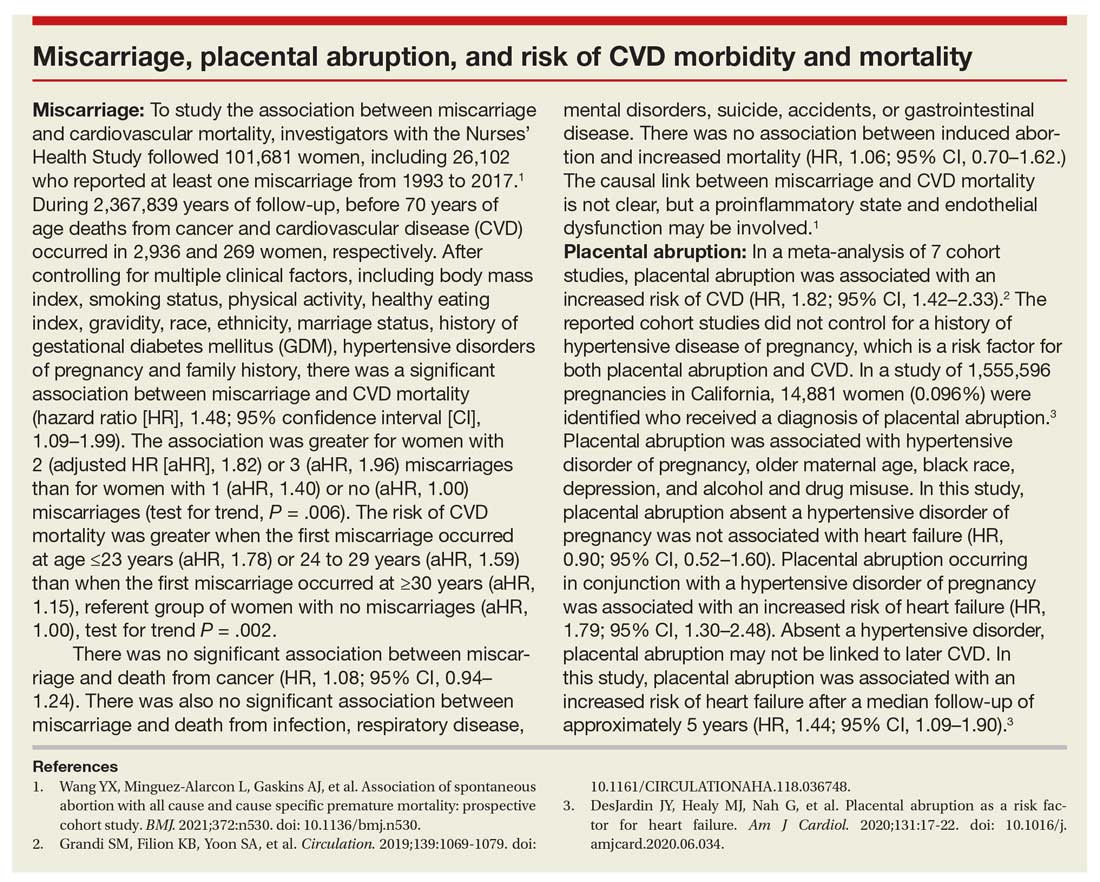
Preconception health influences pregnancy outcomes, and in turn, both preconception health and an APO influence adult cardiometabolic health (FIGURE). This editorial is focused on the link between APOs and later cardiometabolic morbidity and mortality, recognizing that preconception health greatly influences the risk of an APO and lifetime cardiometabolic disease.
Adverse pregnancy outcomes
Major APOs include miscarriage, preterm birth (birth <37 weeks’ gestation), low birth weight (birth weight ≤2,500 g; 5.5 lb), gestational diabetes (GDM), preeclampsia, and placental abruption. In the United States, among all births, reported rates of the following APOs are:1-3
- preterm birth, 10.2%
- low birth weight, 8.3%
- GDM, 6%
- preeclampsia, 5%
- placental abruption, 1%.
Miscarriage occurs in approximately 10% to 15% of pregnancies, influenced by both the age of the woman and the method used to diagnose pregnancy.4 Miscarriage, preterm birth, low birth weight, GDM, preeclampsia, and placental abruption have been reported to be associated with an increased risk of later cardiovascular morbidity and mortality.
APOs and cardiovascular disease
Cardiovascular disease (CVD) affects the majority of people past the age of 60 years and includes 4 major subcategories:
- coronary heart disease, including myocardial infarction, angina, and heart failure
- CVD, stroke, and transient ischemic attack
- peripheral artery disease
- atherosclerosis of the aorta leading to aortic aneurysm.
Multiple meta-analyses report that APOs are associated with CVD in later life. A comprehensive review reported that the risk of CVD was increased following a pregnancy with one of these APOs: severe preeclampsia (odds ratio [OR], 2.74), GDM (OR, 1.68), preterm birth (OR, 1.93), low birth weight (OR, 1.29), and placental abruption (OR, 1.82).5
The link between APOs and CVD may be explained in part by the association of APOs with multiple risk factors for CVD, including chronic hypertension, type 2 diabetes mellitus (T2DM), and dyslipidemia. A meta-analysis of 43 studies reported that, compared with controls, women with a history of preeclampsia have a 3.13 times greater risk of developing chronic hypertension.6 Among women with preeclampsia, approximately 20% will develop hypertension within 15 years.7 A meta-analysis of 20 studies reported that women with a history of GDM had a 9.51-times greater risk of developing T2DM than women without GDM.8 Among women with a history of GDM, over 16 years of follow-up, T2DM was diagnosed in 16.2%, compared with 1.9% of control women.8
CVD prevention—Breastfeeding: An antidote for APOs
Pregnancy stresses both the cardiovascular and metabolic systems. Breastfeeding is an antidote to the stresses imposed by pregnancy. Breastfeeding women have lower blood glucose9 and blood pressure.10
Breastfeeding reduces the risk of CVD. In a study of 100,864 parous Australian women, with a mean age of 60 years, ever breastfeeding was associated a lower risk of CVD hospitalization (adjusted hazard ratio [aHR], 0.86; 95% confidence interval [CI], 0.78–0.96; P = .005) and CVD mortality (aHR, 0.66; 95% CI, 0.49–0.89; P = .006).11
Continue to: CVD prevention—American Heart Association recommendations...
CVD prevention—American Heart Association recommendations
The American Heart Association12 recommends lifestyle interventions to reduce the risk of CVD, including:
- Eat a high-quality diet that includes vegetables, fruit, whole grains, beans, legumes, nuts, plant-based protein, lean animal protein, and fish.
- Limit intake of sugary drinks and foods, fatty or processed meats, full-fat dairy products, eggs, highly processed foods, and tropical oils.
- Exercise at least 150 minutes weekly at a moderate activity level, including muscle-strengthening activity.
- Reduce prolonged intervals of sitting.
- Live a tobacco- and nicotine-free life.
- Strive to maintain a normal body mass index.
- Consider using an activity tracker to monitor activity level.
- After 40 years of age calculate CVD risk using a validated calculator such as the American Cardiology Association risk calculator.13 This calculator uses age, gender, and lipid and blood pressure measurements to calculate the 10-year risk of atherosclerotic CVD, including coronary death, myocardial infarction, and stroke.
Medications to reduce CVD risk
Historically, ObGyns have not routinely prescribed medications to treat hypertension, dyslipidemia, or to prevent diabetes. The recent increase in the valuation of return ambulatory visits and a reduction in the valuation assigned to procedural care may provide ObGyn practices the additional resources needed to manage some chronic diseases. Physician assistants and nurse practitioners may help ObGyn practices to manage hypertension, dyslipidemia, and prediabetes.
Prior to initiating a medicine, counseling about healthy living, including smoking cessation, exercise, heart-healthy diet, and achieving an optimal body mass index is warranted.
For treatment of stage II hypertension, defined as blood pressure (BP) measurements with systolic BP ≥140 mm Hg and diastolic BP ≥90 mm Hg, therapeutic lifestyle interventions include: optimizing weight, following the DASH diet, restricting dietary sodium, physical activity, and reducing alcohol consumption. Medication treatment for essential hypertension is guided by the magnitude of BP reduction needed to achieve normotension. For women with hypertension needing antihypertensive medication and planning another pregnancy in the near future, labetalol or extended-release nifedipine may be first-line medications. For women who have completed their families or who have no immediate plans for pregnancy, an angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, calcium channel blocker, or thiazide diuretic are commonly prescribed.14
For the treatment of elevated low-density lipoprotein (LDL) cholesterol in women who have not had a cardiovascular event, statin therapy is often warranted when both the LDL cholesterol is >100 mg/dL and the woman has a calculated 10-year risk of >10% for a cardiovascular event using the American Heart Association or American College of Cardiology calculator. Most women who meet these criteria will be older than age 40 years and many will be under the care of an internal medicine or family medicine specialist, limiting the role of the ObGyn.15-17
For prevention of diabetes in women with a history of GDM, both weight loss and metformin (1,750 mg daily) have been shown in clinical trials to reduce the risk of developing T2DM.18 Among 350 women with a history of GDM who were followed for 10 years, metformin 850 mg twice daily reduced the risk of developing T2DM by 40% compared with placebo.19 In the same study, lifestyle changes without metformin, including loss of 7% of body weight plus 150 minutes of exercise weekly was associated with a 35% reduction in the risk of developing T2DM.19 Metformin is one of the least expensive prescription medications and is cost-effective for the prevention of T2DM.18
Low-dose aspirin treatment for the prevention of CVD in women who have not had a cardiovascular event must balance a modest reduction in cardiovascular events with a small increased risk of bleeding events. The US Preventive Services Task Force (USPSTF) recommends low-dose aspirin for a limited group of women, those aged 50 to 59 years of age with a 10-year risk of a cardiovascular event >10% who are willing to take aspirin for 10 years. The USPSTF concluded that there is insufficient evidence to recommend low-dose aspirin prevention of CVD in women aged <50 years.20
Continue to: Beyond the fourth trimester...
Beyond the fourth trimester
The fourth trimester is the 12-week period following birth. At the comprehensive postpartum visit, the American College of Obstetricians and Gynecologists (ACOG) recommends that women with APOs be counseled about their increased lifetime risk of maternal cardiometabolic disease.21 In addition, ACOG recommends that at this visit the clinician who will assume primary responsibility for the woman’s ongoing medical care in her primary medical home be clarified. One option is to ensure a high-quality hand-off to an internal medicine or family medicine clinician. Another option is for a clinician in the ObGyn’s office practice, including a physician assistant, nurse practitioner, or office-based ObGyn, to assume some role in the primary care of the woman.
An APO is not only a pregnancy problem
An APO reverberates across a woman’s lifetime, increasing the risk of CVD and diabetes. In the United States the mean age at first birth is 27 years.1 The mean life expectancy of US women is 81 years.22 Following a birth complicated by an APO there are 5 decades of opportunity to improve health through lifestyle changes and medication treatment of obesity, hypertension, dyslipidemia, and hyperglycemia, thereby reducing the risk of CVD.
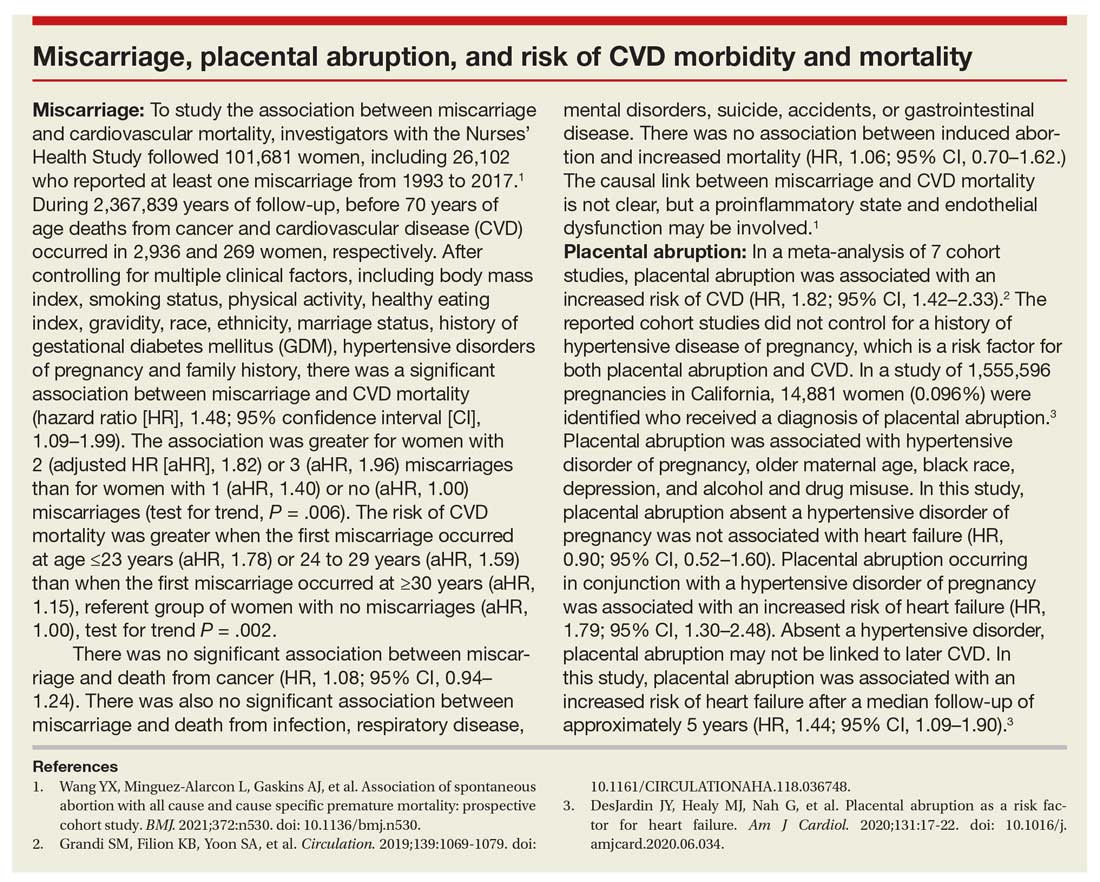
- Martin JA, Hamilton BE, Osterman MJ, et al. Births: final data for 2019. Natl Vital Stat Rep. 2021;70:1-51.
- Deputy NP, Kim SY, Conrey EJ, et al. Prevalence and changes in preexisting diabetes and gestational diabetes among women who had a live birth—United States, 2012-2016. MMWR Morb Mortal Wkly Rep. 2018;67:1201-1207. doi: 10.15585/mmwr.mm6743a2.
- Fingar KR, Mabry-Hernandez I, Ngo-Metzger Q, et al. Delivery hospitalizations involving preeclampsia and eclampsia, 2005–2014. Statistical brief #222. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Agency for Healthcare Research and Quality: Rockville, MD; April 2017.
- Magnus MC, Wilcox AJ, Morken NH, et al. Role of maternal age and pregnancy history in risk of miscarriage: prospective register-based study. BMJ. 2019;364:869.
- Parikh NI, Gonzalez JM, Anderson CAM, et al. Adverse pregnancy outcomes and cardiovascular disease risk: unique opportunities for cardiovascular disease prevention in women. Circulation. 2021;143:e902-e916. doi: 10.1161 /CIR.0000000000000961.
- Brown MC, Best KE, Pearce MS, et al. Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur J Epidemiol. 2013;28:1-19. doi: 10.1007/s10654-013- 9762-6.
- Groenfol TK, Zoet GA, Franx A, et al; on behalf of the PREVENT Group. Trajectory of cardiovascular risk factors after hypertensive disorders of pregnancy. Hypertension. 2019;73:171-178. doi: 10.1161/HYPERTENSIONAHA.118.11726.
- Vounzoulaki E, Khunti K, Abner SC, et al. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ. 2020;369:m1361. doi: 10.1136/bmj.m1361.
- Tarrant M, Chooniedass R, Fan HSL, et al. Breastfeeding and postpartum glucose regulation among women with prior gestational diabetes: a systematic review. J Hum Lact. 2020;36:723-738. doi: 10.1177/0890334420950259.
- Park S, Choi NK. Breastfeeding and maternal hypertension. Am J Hypertens. 2018;31:615-621. doi: 10.1093/ajh/hpx219.
- Nguyen B, Gale J, Nassar N, et al. Breastfeeding and cardiovascular disease hospitalization and mortality in parous women: evidence from a large Australian cohort study. J Am Heart Assoc. 2019;8:e011056. doi: 10.1161/JAHA.118.011056.
- Eight things you can do to prevent heart disease and stroke. American Heart Association website. https://www.heart.org/en/healthy-living /healthy-lifestyle/prevent-heart-disease-andstroke. Last Reviewed March 14, 2019. Accessed May 19, 2021.
- ASCVD risk estimator plus. American College of Cardiology website. https://tools.acc.org /ascvd-risk-estimator-plus/#!/calculate /estimate/. Accessed May 19, 2021.
- Ferdinand KC, Nasser SA. Management of essential hypertension. Cardiol Clin. 2017;35:231-246. doi: 10.1016/j.ccl.2016.12.005.
- Packard CJ. LDL cholesterol: how low to go? Trends Cardiovasc Med. 2018;28:348-354. doi: 10.1016/j.tcm.2017.12.011.
- Simons L. An updated review of lipid-modifying therapy. Med J Aust. 2019;211:87-92. doi: 10.5694 /mja2.50142.
- Chou R, Dana T, Blazina I, et al. Statins for the prevention of cardiovascular disease in adults: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;316:2008. doi: 10.1001/jama.2015.15629.
- Moin T, Schmittdiel JA, Flory JH, et al. Review of metformin use for type 2 diabetes mellitus prevention. Am J Prev Med. 2018;55:565-574. doi: 10.1016/j.amepre.2018.04.038.
- Aorda VR, Christophi CA, Edelstein SL, et al, for the Diabetes Prevention Program Research Group. The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the Diabetes Prevention Program outcomes study 10-year follow-up. J Clin Endocrinol Metab. 2015;100:1646- 1653. doi: 10.1210/jc.2014-3761.
- Bibbins-Domingo K, U.S. Preventive Services Task Force. Aspirin use of the primary prevention of cardiovascular disease and colorectal cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Int Med. 2016; 164: 836-845. doi: 10.7326/M16-0577.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 736: optimizing postpartum care. Obstet Gynecol. 2018;131:e140-e150. doi: 10.1097 /AOG.0000000000002633.
- National Center for Health Statistics. Health, United States, 2017: Table 015. Hyattsville, MD; 2021. https://www.cdc.gov/nchs/data /hus/2017/015.pdf. Accessed May 18, 2021.
- Martin JA, Hamilton BE, Osterman MJ, et al. Births: final data for 2019. Natl Vital Stat Rep. 2021;70:1-51.
- Deputy NP, Kim SY, Conrey EJ, et al. Prevalence and changes in preexisting diabetes and gestational diabetes among women who had a live birth—United States, 2012-2016. MMWR Morb Mortal Wkly Rep. 2018;67:1201-1207. doi: 10.15585/mmwr.mm6743a2.
- Fingar KR, Mabry-Hernandez I, Ngo-Metzger Q, et al. Delivery hospitalizations involving preeclampsia and eclampsia, 2005–2014. Statistical brief #222. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Agency for Healthcare Research and Quality: Rockville, MD; April 2017.
- Magnus MC, Wilcox AJ, Morken NH, et al. Role of maternal age and pregnancy history in risk of miscarriage: prospective register-based study. BMJ. 2019;364:869.
- Parikh NI, Gonzalez JM, Anderson CAM, et al. Adverse pregnancy outcomes and cardiovascular disease risk: unique opportunities for cardiovascular disease prevention in women. Circulation. 2021;143:e902-e916. doi: 10.1161 /CIR.0000000000000961.
- Brown MC, Best KE, Pearce MS, et al. Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur J Epidemiol. 2013;28:1-19. doi: 10.1007/s10654-013- 9762-6.
- Groenfol TK, Zoet GA, Franx A, et al; on behalf of the PREVENT Group. Trajectory of cardiovascular risk factors after hypertensive disorders of pregnancy. Hypertension. 2019;73:171-178. doi: 10.1161/HYPERTENSIONAHA.118.11726.
- Vounzoulaki E, Khunti K, Abner SC, et al. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ. 2020;369:m1361. doi: 10.1136/bmj.m1361.
- Tarrant M, Chooniedass R, Fan HSL, et al. Breastfeeding and postpartum glucose regulation among women with prior gestational diabetes: a systematic review. J Hum Lact. 2020;36:723-738. doi: 10.1177/0890334420950259.
- Park S, Choi NK. Breastfeeding and maternal hypertension. Am J Hypertens. 2018;31:615-621. doi: 10.1093/ajh/hpx219.
- Nguyen B, Gale J, Nassar N, et al. Breastfeeding and cardiovascular disease hospitalization and mortality in parous women: evidence from a large Australian cohort study. J Am Heart Assoc. 2019;8:e011056. doi: 10.1161/JAHA.118.011056.
- Eight things you can do to prevent heart disease and stroke. American Heart Association website. https://www.heart.org/en/healthy-living /healthy-lifestyle/prevent-heart-disease-andstroke. Last Reviewed March 14, 2019. Accessed May 19, 2021.
- ASCVD risk estimator plus. American College of Cardiology website. https://tools.acc.org /ascvd-risk-estimator-plus/#!/calculate /estimate/. Accessed May 19, 2021.
- Ferdinand KC, Nasser SA. Management of essential hypertension. Cardiol Clin. 2017;35:231-246. doi: 10.1016/j.ccl.2016.12.005.
- Packard CJ. LDL cholesterol: how low to go? Trends Cardiovasc Med. 2018;28:348-354. doi: 10.1016/j.tcm.2017.12.011.
- Simons L. An updated review of lipid-modifying therapy. Med J Aust. 2019;211:87-92. doi: 10.5694 /mja2.50142.
- Chou R, Dana T, Blazina I, et al. Statins for the prevention of cardiovascular disease in adults: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;316:2008. doi: 10.1001/jama.2015.15629.
- Moin T, Schmittdiel JA, Flory JH, et al. Review of metformin use for type 2 diabetes mellitus prevention. Am J Prev Med. 2018;55:565-574. doi: 10.1016/j.amepre.2018.04.038.
- Aorda VR, Christophi CA, Edelstein SL, et al, for the Diabetes Prevention Program Research Group. The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the Diabetes Prevention Program outcomes study 10-year follow-up. J Clin Endocrinol Metab. 2015;100:1646- 1653. doi: 10.1210/jc.2014-3761.
- Bibbins-Domingo K, U.S. Preventive Services Task Force. Aspirin use of the primary prevention of cardiovascular disease and colorectal cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Int Med. 2016; 164: 836-845. doi: 10.7326/M16-0577.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 736: optimizing postpartum care. Obstet Gynecol. 2018;131:e140-e150. doi: 10.1097 /AOG.0000000000002633.
- National Center for Health Statistics. Health, United States, 2017: Table 015. Hyattsville, MD; 2021. https://www.cdc.gov/nchs/data /hus/2017/015.pdf. Accessed May 18, 2021.
Intersection of trauma and race in pregnancy calls for more study
Black patients experienced more moderate to severe violent trauma during pregnancy than did non-Black patients at a single Baltimore institution, according to a small retrospective cohort study presented in a poster at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
“Trauma is the leading nonobstetric cause of death in pregnant women,” and Black communities are at a disproportionately greater risk of trauma, Rebecca H. Jessel, MD, of Icahn School of Medicine at Mount Sinai in New York, and associates wrote in their poster.
The study’s findings raise research questions that need more exploration, according to Neel Shah, MD, assistant professor of obstetrics, gynecology, and reproductive biology at Harvard Medical School, Boston, and founding director of the Delivery Decisions Initiative at Harvard’s Ariadne Labs.
“This is an interesting study that opens a line of inquiry into how trauma may impact the pregnancies of those who are Black differently,” Dr. Shah, who was not involved in the research, said in an interview. “The observed disparity is consistent with the racial inequities in outcomes we see across obstetric outcomes and requires further research into the causes and solutions.”
The researchers retrospectively reviewed all pregnant patients treated between 2015 and 2018 at the University of Maryland’s R Adams Cowley Shock Trauma Center in Baltimore. In addition to maternal demographics, details about the delivery, and perinatal outcomes, the researchers noted whether the trauma was violent, such as assault, or nonviolent, such as motor vehicle accidents. Moderate to severe trauma was defined as an injury severity score of at least 9.
Among 3,536 women aged 15-49 treated at the shock trauma center, 62 were pregnant, and 71% of these women were Black. Nineteen percent were White patients, 5% were Asian patients, and 5% were of a different race/ethnicity. Black patients were, on average, 27 years old at the time of the trauma. Non-Black patients were, on average, 25 years old. The average gestational age at the time of trauma was 25 weeks, 3 days in Black women and 23 weeks, 4 days in non-Black women.
The most common cause of trauma was a car accident, implicated in 56% of the trauma cases. Assault was the next most common cause of trauma, making up nearly a quarter (23%) of cases. The other injuries came from accidents (16%) or inhalation (5%). The average injury severity score was 4.7, with a mild injury for 76% of patients and a moderate to severe injury in 24%.
The researchers then compared the mechanisms and severity of injuries between Black and non-Black patients. The severity of trauma was similar between the two groups: Seventy-five percent of Black patients and 78% of non-Black patients had mild trauma with injury severity scores below 9. However, assault or another violent form of trauma was more likely to occur to Black patients than to non-Black patients. More than a quarter (27%) of Black patients experienced violent trauma, compared to 11% of non-Black patients.
“It is very notable that among pregnant people who experience trauma, obstetric complications leading to preterm delivery were observed much more often for those who are Black,” Dr. Shah said. “A case series to understand the underlying causes could be very valuable.”
Black patients delivered an average 59 days (8 weeks, 3 days) after the trauma compared to an average 83 days (11 weeks, 6 days) for non-Black patients, but the difference was not statistically significant. However, preterm birth was more likely in non-Black patients (83%) than in Black patients (78%). A similar proportion of deliveries were preterm in Black (57%) and non-Black (56%) patients.
Though the poster did not show the data, the researchers wrote that Black women who experienced moderate to severe trauma after 24 weeks’ gestational age either had a preterm birth or a fetal demise.
Though the study findings warrant deeper investigation, the study has substantial limitations.
“It is challenging to generalize from this study because the sample size is small and it is from a single institution,” Dr. Shah said. “It does not appear to be adequately powered to draw statistically significant conclusions. In particular, the data are not adequate to support the authors’ statement that Black people are more likely to experience the forms of described trauma generally.”
The authors and Dr. Shah reported no disclosures.
Black patients experienced more moderate to severe violent trauma during pregnancy than did non-Black patients at a single Baltimore institution, according to a small retrospective cohort study presented in a poster at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
“Trauma is the leading nonobstetric cause of death in pregnant women,” and Black communities are at a disproportionately greater risk of trauma, Rebecca H. Jessel, MD, of Icahn School of Medicine at Mount Sinai in New York, and associates wrote in their poster.
The study’s findings raise research questions that need more exploration, according to Neel Shah, MD, assistant professor of obstetrics, gynecology, and reproductive biology at Harvard Medical School, Boston, and founding director of the Delivery Decisions Initiative at Harvard’s Ariadne Labs.
“This is an interesting study that opens a line of inquiry into how trauma may impact the pregnancies of those who are Black differently,” Dr. Shah, who was not involved in the research, said in an interview. “The observed disparity is consistent with the racial inequities in outcomes we see across obstetric outcomes and requires further research into the causes and solutions.”
The researchers retrospectively reviewed all pregnant patients treated between 2015 and 2018 at the University of Maryland’s R Adams Cowley Shock Trauma Center in Baltimore. In addition to maternal demographics, details about the delivery, and perinatal outcomes, the researchers noted whether the trauma was violent, such as assault, or nonviolent, such as motor vehicle accidents. Moderate to severe trauma was defined as an injury severity score of at least 9.
Among 3,536 women aged 15-49 treated at the shock trauma center, 62 were pregnant, and 71% of these women were Black. Nineteen percent were White patients, 5% were Asian patients, and 5% were of a different race/ethnicity. Black patients were, on average, 27 years old at the time of the trauma. Non-Black patients were, on average, 25 years old. The average gestational age at the time of trauma was 25 weeks, 3 days in Black women and 23 weeks, 4 days in non-Black women.
The most common cause of trauma was a car accident, implicated in 56% of the trauma cases. Assault was the next most common cause of trauma, making up nearly a quarter (23%) of cases. The other injuries came from accidents (16%) or inhalation (5%). The average injury severity score was 4.7, with a mild injury for 76% of patients and a moderate to severe injury in 24%.
The researchers then compared the mechanisms and severity of injuries between Black and non-Black patients. The severity of trauma was similar between the two groups: Seventy-five percent of Black patients and 78% of non-Black patients had mild trauma with injury severity scores below 9. However, assault or another violent form of trauma was more likely to occur to Black patients than to non-Black patients. More than a quarter (27%) of Black patients experienced violent trauma, compared to 11% of non-Black patients.
“It is very notable that among pregnant people who experience trauma, obstetric complications leading to preterm delivery were observed much more often for those who are Black,” Dr. Shah said. “A case series to understand the underlying causes could be very valuable.”
Black patients delivered an average 59 days (8 weeks, 3 days) after the trauma compared to an average 83 days (11 weeks, 6 days) for non-Black patients, but the difference was not statistically significant. However, preterm birth was more likely in non-Black patients (83%) than in Black patients (78%). A similar proportion of deliveries were preterm in Black (57%) and non-Black (56%) patients.
Though the poster did not show the data, the researchers wrote that Black women who experienced moderate to severe trauma after 24 weeks’ gestational age either had a preterm birth or a fetal demise.
Though the study findings warrant deeper investigation, the study has substantial limitations.
“It is challenging to generalize from this study because the sample size is small and it is from a single institution,” Dr. Shah said. “It does not appear to be adequately powered to draw statistically significant conclusions. In particular, the data are not adequate to support the authors’ statement that Black people are more likely to experience the forms of described trauma generally.”
The authors and Dr. Shah reported no disclosures.
Black patients experienced more moderate to severe violent trauma during pregnancy than did non-Black patients at a single Baltimore institution, according to a small retrospective cohort study presented in a poster at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
“Trauma is the leading nonobstetric cause of death in pregnant women,” and Black communities are at a disproportionately greater risk of trauma, Rebecca H. Jessel, MD, of Icahn School of Medicine at Mount Sinai in New York, and associates wrote in their poster.
The study’s findings raise research questions that need more exploration, according to Neel Shah, MD, assistant professor of obstetrics, gynecology, and reproductive biology at Harvard Medical School, Boston, and founding director of the Delivery Decisions Initiative at Harvard’s Ariadne Labs.
“This is an interesting study that opens a line of inquiry into how trauma may impact the pregnancies of those who are Black differently,” Dr. Shah, who was not involved in the research, said in an interview. “The observed disparity is consistent with the racial inequities in outcomes we see across obstetric outcomes and requires further research into the causes and solutions.”
The researchers retrospectively reviewed all pregnant patients treated between 2015 and 2018 at the University of Maryland’s R Adams Cowley Shock Trauma Center in Baltimore. In addition to maternal demographics, details about the delivery, and perinatal outcomes, the researchers noted whether the trauma was violent, such as assault, or nonviolent, such as motor vehicle accidents. Moderate to severe trauma was defined as an injury severity score of at least 9.
Among 3,536 women aged 15-49 treated at the shock trauma center, 62 were pregnant, and 71% of these women were Black. Nineteen percent were White patients, 5% were Asian patients, and 5% were of a different race/ethnicity. Black patients were, on average, 27 years old at the time of the trauma. Non-Black patients were, on average, 25 years old. The average gestational age at the time of trauma was 25 weeks, 3 days in Black women and 23 weeks, 4 days in non-Black women.
The most common cause of trauma was a car accident, implicated in 56% of the trauma cases. Assault was the next most common cause of trauma, making up nearly a quarter (23%) of cases. The other injuries came from accidents (16%) or inhalation (5%). The average injury severity score was 4.7, with a mild injury for 76% of patients and a moderate to severe injury in 24%.
The researchers then compared the mechanisms and severity of injuries between Black and non-Black patients. The severity of trauma was similar between the two groups: Seventy-five percent of Black patients and 78% of non-Black patients had mild trauma with injury severity scores below 9. However, assault or another violent form of trauma was more likely to occur to Black patients than to non-Black patients. More than a quarter (27%) of Black patients experienced violent trauma, compared to 11% of non-Black patients.
“It is very notable that among pregnant people who experience trauma, obstetric complications leading to preterm delivery were observed much more often for those who are Black,” Dr. Shah said. “A case series to understand the underlying causes could be very valuable.”
Black patients delivered an average 59 days (8 weeks, 3 days) after the trauma compared to an average 83 days (11 weeks, 6 days) for non-Black patients, but the difference was not statistically significant. However, preterm birth was more likely in non-Black patients (83%) than in Black patients (78%). A similar proportion of deliveries were preterm in Black (57%) and non-Black (56%) patients.
Though the poster did not show the data, the researchers wrote that Black women who experienced moderate to severe trauma after 24 weeks’ gestational age either had a preterm birth or a fetal demise.
Though the study findings warrant deeper investigation, the study has substantial limitations.
“It is challenging to generalize from this study because the sample size is small and it is from a single institution,” Dr. Shah said. “It does not appear to be adequately powered to draw statistically significant conclusions. In particular, the data are not adequate to support the authors’ statement that Black people are more likely to experience the forms of described trauma generally.”
The authors and Dr. Shah reported no disclosures.
FROM ACOG 2021
Patients and providers alike support virtual prenatal care
Obstetric patients and clinicians both overwhelmingly reported that telehealth was a safer way to receive ob.gyn. care and improve health care access during the COVID-19 pandemic, according to a survey at a single institution. The findings, from the Vanderbilt University Medical Center in Nashville, Tenn., were presented in a poster at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
“The COVID-19 pandemic caused rapid and broad expansion of tele-obstetrics, warranting the need to assess patient and provider experiences and opinions about these services,” Karampreet Kaur, a 4th-year MD candidate at Vanderbilt University, and colleagues wrote in the poster. The group’s findings led them to conclude that virtual choices for prenatal care should be available independent of the pandemic.
Neel Shah, MD, assistant professor of obstetrics, gynecology, and reproductive biology at Harvard Medical School, Boston, and founding director of the Delivery Decisions Initiative at Harvard’s Ariadne Labs, agreed that the study results supported continuation of telehealth even without COVID-19. Dr. Shah was not involved with the research.
“The fact that telehealth is broadly acceptable is not surprising but the magnitudes are striking,” Dr. Shah said in an interview. “Both providers and patients overwhelmingly see telehealth as a value-added fixture of obstetrical care that should be sustained beyond the pandemic.”
The researchers conducted an online survey of both obstetrical patients who received virtual prenatal care and ob.gyn. department providers, including MDs, DOs, advanced practice providers, genetic counselors, social workers, and registered dietitians.
Just over half (53%) of the 167 patients who completed the survey between June 2020 and April 2021 were between the ages 25 and 34. The remaining patients included 13% between ages 18 and 24 and 35% between ages 35 and 44. Most of these patients (84%) were at home for their telehealth appointment, but 16% were at a clinic for the telehealth appointment.
A quarter of the patients had a telehealth visit with a genetic counselor (26%) while 44% of patients saw an ob generalist and 28% saw a maternal fetal medicine specialist. Only 1% reported a social worker visit.
The majority of patients (75%) reported that they felt personally safer using telehealth rather than an in-person visit, and 18% said they would have forgone care if telehealth were not an option. Similarly, 74% of patients said the virtual care reduced their travel time, and 46% said they saved at least $35 in transportation, child care, or missed wages. More than half the patients surveyed were satisfied with their telehealth experience and believe Tennessee should have a tele-obstetrics program.
“The fact that a significant number of patients would have forgone care, and that nearly all providers observed improvements in access, makes widespread adoption of telehealth a moral imperative,” Dr. Shah said. “Telehealth and other forms of virtual care require rethinking our standard care models,” he added. “Traditional prenatal care for example is based on a model that is nearly a century old and may not meet the needs of many people. The experimentation with new ways of providing care that the pandemic forced should be an ongoing effort to ensure every person giving birth receives the care they deserve.”
Medical doctors (MD and DO) made up 53% of the 72 providers who completed the survey between June and August 2020, and a little over a third (36%) were advanced practice providers. Nearly all the providers (more than 95%) agreed with the statement that “telehealth was safer than in-clinic appointments for themselves, colleagues, and obstetrical patients.” Similar majorities felt telehealth was an acceptable way to provide health care (94%) and that virtual care improved access to health care (96%).
Most of the providers (85%) also felt that telehealth provided an opportunity for high-quality communication with their patients. More than half the providers said they would be willing to use telehealth outside of the pandemic, and a similar proportion felt that “Vanderbilt telehealth is a positive program for the state of Tennessee.”
Though not an author of the study, another Vanderbilt ob.gyn. also believes the findings support exploring continued telehealth options for the patients and providers interested in it.
“Health care providers and patients alike can attest to the benefits of telehealth utilization, Etoi A. Garrison, MD, PhD, associate professor of maternal-fetal medicine at Vanderbilt University, said in an interview. She was particularly struck by the savings reported by patients. “These costs are difficult to quantify but can have a significant impact on patients’ day-to-day quality of life,” she said.
A limitation of the study is the lack of information on how many were invited to complete it, so it’s not possible to know if the results are representative of the majority of people who used telehealth services, Dr. Garrison added. Dr. Shah agreed but didn’t think that limitation diminished the clinical implications of the study.
“A relatively small number of patients and providers are surveyed over a long period of time in which the context of the pandemic varied significantly,” he said. “Nonetheless, the findings show strong and internally consistent beliefs among those receiving and providing care that telehealth is valuable.”
The authors and Dr. Shah reported no disclosures. Dr. Garrison reported receiving a grant from the Tennessee Maternal Mortality Review committee to create an Unconscious Bias Faculty Train-the-Trainer program.
Obstetric patients and clinicians both overwhelmingly reported that telehealth was a safer way to receive ob.gyn. care and improve health care access during the COVID-19 pandemic, according to a survey at a single institution. The findings, from the Vanderbilt University Medical Center in Nashville, Tenn., were presented in a poster at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
“The COVID-19 pandemic caused rapid and broad expansion of tele-obstetrics, warranting the need to assess patient and provider experiences and opinions about these services,” Karampreet Kaur, a 4th-year MD candidate at Vanderbilt University, and colleagues wrote in the poster. The group’s findings led them to conclude that virtual choices for prenatal care should be available independent of the pandemic.
Neel Shah, MD, assistant professor of obstetrics, gynecology, and reproductive biology at Harvard Medical School, Boston, and founding director of the Delivery Decisions Initiative at Harvard’s Ariadne Labs, agreed that the study results supported continuation of telehealth even without COVID-19. Dr. Shah was not involved with the research.
“The fact that telehealth is broadly acceptable is not surprising but the magnitudes are striking,” Dr. Shah said in an interview. “Both providers and patients overwhelmingly see telehealth as a value-added fixture of obstetrical care that should be sustained beyond the pandemic.”
The researchers conducted an online survey of both obstetrical patients who received virtual prenatal care and ob.gyn. department providers, including MDs, DOs, advanced practice providers, genetic counselors, social workers, and registered dietitians.
Just over half (53%) of the 167 patients who completed the survey between June 2020 and April 2021 were between the ages 25 and 34. The remaining patients included 13% between ages 18 and 24 and 35% between ages 35 and 44. Most of these patients (84%) were at home for their telehealth appointment, but 16% were at a clinic for the telehealth appointment.
A quarter of the patients had a telehealth visit with a genetic counselor (26%) while 44% of patients saw an ob generalist and 28% saw a maternal fetal medicine specialist. Only 1% reported a social worker visit.
The majority of patients (75%) reported that they felt personally safer using telehealth rather than an in-person visit, and 18% said they would have forgone care if telehealth were not an option. Similarly, 74% of patients said the virtual care reduced their travel time, and 46% said they saved at least $35 in transportation, child care, or missed wages. More than half the patients surveyed were satisfied with their telehealth experience and believe Tennessee should have a tele-obstetrics program.
“The fact that a significant number of patients would have forgone care, and that nearly all providers observed improvements in access, makes widespread adoption of telehealth a moral imperative,” Dr. Shah said. “Telehealth and other forms of virtual care require rethinking our standard care models,” he added. “Traditional prenatal care for example is based on a model that is nearly a century old and may not meet the needs of many people. The experimentation with new ways of providing care that the pandemic forced should be an ongoing effort to ensure every person giving birth receives the care they deserve.”
Medical doctors (MD and DO) made up 53% of the 72 providers who completed the survey between June and August 2020, and a little over a third (36%) were advanced practice providers. Nearly all the providers (more than 95%) agreed with the statement that “telehealth was safer than in-clinic appointments for themselves, colleagues, and obstetrical patients.” Similar majorities felt telehealth was an acceptable way to provide health care (94%) and that virtual care improved access to health care (96%).
Most of the providers (85%) also felt that telehealth provided an opportunity for high-quality communication with their patients. More than half the providers said they would be willing to use telehealth outside of the pandemic, and a similar proportion felt that “Vanderbilt telehealth is a positive program for the state of Tennessee.”
Though not an author of the study, another Vanderbilt ob.gyn. also believes the findings support exploring continued telehealth options for the patients and providers interested in it.
“Health care providers and patients alike can attest to the benefits of telehealth utilization, Etoi A. Garrison, MD, PhD, associate professor of maternal-fetal medicine at Vanderbilt University, said in an interview. She was particularly struck by the savings reported by patients. “These costs are difficult to quantify but can have a significant impact on patients’ day-to-day quality of life,” she said.
A limitation of the study is the lack of information on how many were invited to complete it, so it’s not possible to know if the results are representative of the majority of people who used telehealth services, Dr. Garrison added. Dr. Shah agreed but didn’t think that limitation diminished the clinical implications of the study.
“A relatively small number of patients and providers are surveyed over a long period of time in which the context of the pandemic varied significantly,” he said. “Nonetheless, the findings show strong and internally consistent beliefs among those receiving and providing care that telehealth is valuable.”
The authors and Dr. Shah reported no disclosures. Dr. Garrison reported receiving a grant from the Tennessee Maternal Mortality Review committee to create an Unconscious Bias Faculty Train-the-Trainer program.
Obstetric patients and clinicians both overwhelmingly reported that telehealth was a safer way to receive ob.gyn. care and improve health care access during the COVID-19 pandemic, according to a survey at a single institution. The findings, from the Vanderbilt University Medical Center in Nashville, Tenn., were presented in a poster at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
“The COVID-19 pandemic caused rapid and broad expansion of tele-obstetrics, warranting the need to assess patient and provider experiences and opinions about these services,” Karampreet Kaur, a 4th-year MD candidate at Vanderbilt University, and colleagues wrote in the poster. The group’s findings led them to conclude that virtual choices for prenatal care should be available independent of the pandemic.
Neel Shah, MD, assistant professor of obstetrics, gynecology, and reproductive biology at Harvard Medical School, Boston, and founding director of the Delivery Decisions Initiative at Harvard’s Ariadne Labs, agreed that the study results supported continuation of telehealth even without COVID-19. Dr. Shah was not involved with the research.
“The fact that telehealth is broadly acceptable is not surprising but the magnitudes are striking,” Dr. Shah said in an interview. “Both providers and patients overwhelmingly see telehealth as a value-added fixture of obstetrical care that should be sustained beyond the pandemic.”
The researchers conducted an online survey of both obstetrical patients who received virtual prenatal care and ob.gyn. department providers, including MDs, DOs, advanced practice providers, genetic counselors, social workers, and registered dietitians.
Just over half (53%) of the 167 patients who completed the survey between June 2020 and April 2021 were between the ages 25 and 34. The remaining patients included 13% between ages 18 and 24 and 35% between ages 35 and 44. Most of these patients (84%) were at home for their telehealth appointment, but 16% were at a clinic for the telehealth appointment.
A quarter of the patients had a telehealth visit with a genetic counselor (26%) while 44% of patients saw an ob generalist and 28% saw a maternal fetal medicine specialist. Only 1% reported a social worker visit.
The majority of patients (75%) reported that they felt personally safer using telehealth rather than an in-person visit, and 18% said they would have forgone care if telehealth were not an option. Similarly, 74% of patients said the virtual care reduced their travel time, and 46% said they saved at least $35 in transportation, child care, or missed wages. More than half the patients surveyed were satisfied with their telehealth experience and believe Tennessee should have a tele-obstetrics program.
“The fact that a significant number of patients would have forgone care, and that nearly all providers observed improvements in access, makes widespread adoption of telehealth a moral imperative,” Dr. Shah said. “Telehealth and other forms of virtual care require rethinking our standard care models,” he added. “Traditional prenatal care for example is based on a model that is nearly a century old and may not meet the needs of many people. The experimentation with new ways of providing care that the pandemic forced should be an ongoing effort to ensure every person giving birth receives the care they deserve.”
Medical doctors (MD and DO) made up 53% of the 72 providers who completed the survey between June and August 2020, and a little over a third (36%) were advanced practice providers. Nearly all the providers (more than 95%) agreed with the statement that “telehealth was safer than in-clinic appointments for themselves, colleagues, and obstetrical patients.” Similar majorities felt telehealth was an acceptable way to provide health care (94%) and that virtual care improved access to health care (96%).
Most of the providers (85%) also felt that telehealth provided an opportunity for high-quality communication with their patients. More than half the providers said they would be willing to use telehealth outside of the pandemic, and a similar proportion felt that “Vanderbilt telehealth is a positive program for the state of Tennessee.”
Though not an author of the study, another Vanderbilt ob.gyn. also believes the findings support exploring continued telehealth options for the patients and providers interested in it.
“Health care providers and patients alike can attest to the benefits of telehealth utilization, Etoi A. Garrison, MD, PhD, associate professor of maternal-fetal medicine at Vanderbilt University, said in an interview. She was particularly struck by the savings reported by patients. “These costs are difficult to quantify but can have a significant impact on patients’ day-to-day quality of life,” she said.
A limitation of the study is the lack of information on how many were invited to complete it, so it’s not possible to know if the results are representative of the majority of people who used telehealth services, Dr. Garrison added. Dr. Shah agreed but didn’t think that limitation diminished the clinical implications of the study.
“A relatively small number of patients and providers are surveyed over a long period of time in which the context of the pandemic varied significantly,” he said. “Nonetheless, the findings show strong and internally consistent beliefs among those receiving and providing care that telehealth is valuable.”
The authors and Dr. Shah reported no disclosures. Dr. Garrison reported receiving a grant from the Tennessee Maternal Mortality Review committee to create an Unconscious Bias Faculty Train-the-Trainer program.
FROM ACOG 2021
Language barrier may contribute to ob.gyn. pain management disparities
Obstetric patients whose first language is not English received fewer pain assessments and fewer doses of NSAIDs and oxycodone therapeutic equivalents (OTEs) following cesarean deliveries, according to a retrospective cohort study poster presented at the 2021 annual meeting of the American College of Obstetricians and Gynecologists.
The findings “may indicate language as a barrier for equitable pain management in the postpartum period,” concluded Alison Wiles, MD, a resident at Mount Sinai South Nassau in Oceanside, N.Y., and colleagues. They recommended “scheduled pain assessment and around the clock nonopioid medication administration” as potential ways to reduce the disparities.
“Racial and ethnic disparities in pain management have been well documented in both inpatient and outpatient settings, [and] similar disparities exist within postpartum pain management,” the researchers note in their background material. They also note that non-Hispanic White communities tend to have a higher incidence of opioid misuse.
The researchers conducted a retrospective study of 327 women who had cesarean deliveries from January to June 2018 at Mount Sinai South Nassau Hospital. They excluded women who underwent cesarean hysterectomies, received general anesthesia or patient-controlled analgesia, had a history of drug use, or had allergies to opiates. They did not note incidence of uterine fibroids, endometriosis, or other gynecologic conditions aside from delivery that could cause pain.
The population included a similar number of non-Hispanic White women (n = 111) and Hispanic women (n = 125). The remaining study participants included 32 non-Hispanic Black women and 59 women who were Asian or had another race/ethnicity. The women’s average age was 31, which was statistically similar across all four race/ethnicity groups. Average body mass index of participants was also similar, ranging from 32 to 34.6 kg/m2, across all four demographic groups.
About half of all the women (52%) had a previous cesarean delivery, but rates were significantly different between groups: 31% of non-Hispanic Black women and 58% of Hispanic women had a prior cesarean, compared to 50% of non-Hispanic White, Asian, and other women (P < .05).
Half the women in the study overall (50.5%) had public insurance, but the proportion of those with public insurance differed significantly by racial/ethnic demographics. Less than a quarter of Asian/other women (23%) had public insurance, compared with 78% of Hispanic women, 74% of non-Hispanic White women, and 59% of non-Hispanic Black women (P < .0001).
Most of the women (76%) spoke English as their primary language, which included nearly all the women in each demographic group except Hispanic, in which 58% of the women’s primary language was Spanish or another language (P < .0001).
Hispanic patients received an average of 10 pain assessments after their cesarean, compared with an average of 11 in each of the other demographic groups (P = .02). Similarly, English speakers received an average 11 pain assessments, but those who primarily spoke Spanish or another language received 10 (P = .01).
The differences between English and non-English speakers were reflected in who received pain medication even though pain scores were the same between the two groups. English speakers received an average two doses of NSAIDs in the first 24 hours post partum, compared with one dose for those who spoke a primary language other than English (P = .03). At 24-48 hours post partum, those who spoke English received an average three NSAID doses, compared with two among those whose primary language was Spanish or another language (P = .03).
There was no difference between language groups in doses of OTEs in the first 24 hours post partum, but differences did occur on the second day. Women who primarily spoke English received an average four OTE doses in the 24-48 hours post partum, compared with two doses given to women who spoke a non-English primary language (P = .03).
Differences were less consistent or not significant when looking solely at race/ethnicity. All four groups received an average of two NSAID doses in the first 24 hours post partum, but second-day rates varied. Non-Hispanic White women and Asian/other women received an average three doses from 24 to 48 hours post partum while non-Hispanic Black women received one and Hispanic women received two (P = .0009).
No statistically significant differences in OTE doses occurred across the groups in the first 24 hours, but from 24 to 48 hours, the average two doses received by Hispanic women and 3 doses received by Asian women differed significantly from the average four doses received by non-Hispanic White women and the average five doses received by non-Hispanic Black women (P =.01).
“Non-Hispanic Black patients had higher OTE doses and fewer NSAID doses in the 24- to 48-hour postpartum period despite no differences in severe pain scores,” the authors also reported.
“These findings are surprising given the standardized protocols in place designed to assess and treat pain post partum,” Etoi A. Garrison, MD, PhD, an associate professor of maternal-fetal medicine at Vanderbilt University Medical Center, Memphis, Tenn., said in an interview. ” Protocols should minimize bias and promote equitable delivery of care.”
Dr. Garrison said it’s important to find out why these discrepancies exist even when ready access to interpretation services exist in the hospital.
“An important component of health care disparity research is to hear directly from patients themselves about their experiences,” Dr. Garrison said. “Often the patient voice is an overlooked and underappreciated resource. I hope that future iterations of this work include patient perceptions about the adequacy of postpartum care and provide more information about how health care delivery can be tailored to the unique needs of this vulnerable population.”
The authors reported no disclosures. Dr Garrison reported receiving a grant from the State of Tennessee Maternal Mortality Review Committee to Create an Unconscious Bias Faculty Train-the-Trainer Program.
Obstetric patients whose first language is not English received fewer pain assessments and fewer doses of NSAIDs and oxycodone therapeutic equivalents (OTEs) following cesarean deliveries, according to a retrospective cohort study poster presented at the 2021 annual meeting of the American College of Obstetricians and Gynecologists.
The findings “may indicate language as a barrier for equitable pain management in the postpartum period,” concluded Alison Wiles, MD, a resident at Mount Sinai South Nassau in Oceanside, N.Y., and colleagues. They recommended “scheduled pain assessment and around the clock nonopioid medication administration” as potential ways to reduce the disparities.
“Racial and ethnic disparities in pain management have been well documented in both inpatient and outpatient settings, [and] similar disparities exist within postpartum pain management,” the researchers note in their background material. They also note that non-Hispanic White communities tend to have a higher incidence of opioid misuse.
The researchers conducted a retrospective study of 327 women who had cesarean deliveries from January to June 2018 at Mount Sinai South Nassau Hospital. They excluded women who underwent cesarean hysterectomies, received general anesthesia or patient-controlled analgesia, had a history of drug use, or had allergies to opiates. They did not note incidence of uterine fibroids, endometriosis, or other gynecologic conditions aside from delivery that could cause pain.
The population included a similar number of non-Hispanic White women (n = 111) and Hispanic women (n = 125). The remaining study participants included 32 non-Hispanic Black women and 59 women who were Asian or had another race/ethnicity. The women’s average age was 31, which was statistically similar across all four race/ethnicity groups. Average body mass index of participants was also similar, ranging from 32 to 34.6 kg/m2, across all four demographic groups.
About half of all the women (52%) had a previous cesarean delivery, but rates were significantly different between groups: 31% of non-Hispanic Black women and 58% of Hispanic women had a prior cesarean, compared to 50% of non-Hispanic White, Asian, and other women (P < .05).
Half the women in the study overall (50.5%) had public insurance, but the proportion of those with public insurance differed significantly by racial/ethnic demographics. Less than a quarter of Asian/other women (23%) had public insurance, compared with 78% of Hispanic women, 74% of non-Hispanic White women, and 59% of non-Hispanic Black women (P < .0001).
Most of the women (76%) spoke English as their primary language, which included nearly all the women in each demographic group except Hispanic, in which 58% of the women’s primary language was Spanish or another language (P < .0001).
Hispanic patients received an average of 10 pain assessments after their cesarean, compared with an average of 11 in each of the other demographic groups (P = .02). Similarly, English speakers received an average 11 pain assessments, but those who primarily spoke Spanish or another language received 10 (P = .01).
The differences between English and non-English speakers were reflected in who received pain medication even though pain scores were the same between the two groups. English speakers received an average two doses of NSAIDs in the first 24 hours post partum, compared with one dose for those who spoke a primary language other than English (P = .03). At 24-48 hours post partum, those who spoke English received an average three NSAID doses, compared with two among those whose primary language was Spanish or another language (P = .03).
There was no difference between language groups in doses of OTEs in the first 24 hours post partum, but differences did occur on the second day. Women who primarily spoke English received an average four OTE doses in the 24-48 hours post partum, compared with two doses given to women who spoke a non-English primary language (P = .03).
Differences were less consistent or not significant when looking solely at race/ethnicity. All four groups received an average of two NSAID doses in the first 24 hours post partum, but second-day rates varied. Non-Hispanic White women and Asian/other women received an average three doses from 24 to 48 hours post partum while non-Hispanic Black women received one and Hispanic women received two (P = .0009).
No statistically significant differences in OTE doses occurred across the groups in the first 24 hours, but from 24 to 48 hours, the average two doses received by Hispanic women and 3 doses received by Asian women differed significantly from the average four doses received by non-Hispanic White women and the average five doses received by non-Hispanic Black women (P =.01).
“Non-Hispanic Black patients had higher OTE doses and fewer NSAID doses in the 24- to 48-hour postpartum period despite no differences in severe pain scores,” the authors also reported.
“These findings are surprising given the standardized protocols in place designed to assess and treat pain post partum,” Etoi A. Garrison, MD, PhD, an associate professor of maternal-fetal medicine at Vanderbilt University Medical Center, Memphis, Tenn., said in an interview. ” Protocols should minimize bias and promote equitable delivery of care.”
Dr. Garrison said it’s important to find out why these discrepancies exist even when ready access to interpretation services exist in the hospital.
“An important component of health care disparity research is to hear directly from patients themselves about their experiences,” Dr. Garrison said. “Often the patient voice is an overlooked and underappreciated resource. I hope that future iterations of this work include patient perceptions about the adequacy of postpartum care and provide more information about how health care delivery can be tailored to the unique needs of this vulnerable population.”
The authors reported no disclosures. Dr Garrison reported receiving a grant from the State of Tennessee Maternal Mortality Review Committee to Create an Unconscious Bias Faculty Train-the-Trainer Program.
Obstetric patients whose first language is not English received fewer pain assessments and fewer doses of NSAIDs and oxycodone therapeutic equivalents (OTEs) following cesarean deliveries, according to a retrospective cohort study poster presented at the 2021 annual meeting of the American College of Obstetricians and Gynecologists.
The findings “may indicate language as a barrier for equitable pain management in the postpartum period,” concluded Alison Wiles, MD, a resident at Mount Sinai South Nassau in Oceanside, N.Y., and colleagues. They recommended “scheduled pain assessment and around the clock nonopioid medication administration” as potential ways to reduce the disparities.
“Racial and ethnic disparities in pain management have been well documented in both inpatient and outpatient settings, [and] similar disparities exist within postpartum pain management,” the researchers note in their background material. They also note that non-Hispanic White communities tend to have a higher incidence of opioid misuse.
The researchers conducted a retrospective study of 327 women who had cesarean deliveries from January to June 2018 at Mount Sinai South Nassau Hospital. They excluded women who underwent cesarean hysterectomies, received general anesthesia or patient-controlled analgesia, had a history of drug use, or had allergies to opiates. They did not note incidence of uterine fibroids, endometriosis, or other gynecologic conditions aside from delivery that could cause pain.
The population included a similar number of non-Hispanic White women (n = 111) and Hispanic women (n = 125). The remaining study participants included 32 non-Hispanic Black women and 59 women who were Asian or had another race/ethnicity. The women’s average age was 31, which was statistically similar across all four race/ethnicity groups. Average body mass index of participants was also similar, ranging from 32 to 34.6 kg/m2, across all four demographic groups.
About half of all the women (52%) had a previous cesarean delivery, but rates were significantly different between groups: 31% of non-Hispanic Black women and 58% of Hispanic women had a prior cesarean, compared to 50% of non-Hispanic White, Asian, and other women (P < .05).
Half the women in the study overall (50.5%) had public insurance, but the proportion of those with public insurance differed significantly by racial/ethnic demographics. Less than a quarter of Asian/other women (23%) had public insurance, compared with 78% of Hispanic women, 74% of non-Hispanic White women, and 59% of non-Hispanic Black women (P < .0001).
Most of the women (76%) spoke English as their primary language, which included nearly all the women in each demographic group except Hispanic, in which 58% of the women’s primary language was Spanish or another language (P < .0001).
Hispanic patients received an average of 10 pain assessments after their cesarean, compared with an average of 11 in each of the other demographic groups (P = .02). Similarly, English speakers received an average 11 pain assessments, but those who primarily spoke Spanish or another language received 10 (P = .01).
The differences between English and non-English speakers were reflected in who received pain medication even though pain scores were the same between the two groups. English speakers received an average two doses of NSAIDs in the first 24 hours post partum, compared with one dose for those who spoke a primary language other than English (P = .03). At 24-48 hours post partum, those who spoke English received an average three NSAID doses, compared with two among those whose primary language was Spanish or another language (P = .03).
There was no difference between language groups in doses of OTEs in the first 24 hours post partum, but differences did occur on the second day. Women who primarily spoke English received an average four OTE doses in the 24-48 hours post partum, compared with two doses given to women who spoke a non-English primary language (P = .03).
Differences were less consistent or not significant when looking solely at race/ethnicity. All four groups received an average of two NSAID doses in the first 24 hours post partum, but second-day rates varied. Non-Hispanic White women and Asian/other women received an average three doses from 24 to 48 hours post partum while non-Hispanic Black women received one and Hispanic women received two (P = .0009).
No statistically significant differences in OTE doses occurred across the groups in the first 24 hours, but from 24 to 48 hours, the average two doses received by Hispanic women and 3 doses received by Asian women differed significantly from the average four doses received by non-Hispanic White women and the average five doses received by non-Hispanic Black women (P =.01).
“Non-Hispanic Black patients had higher OTE doses and fewer NSAID doses in the 24- to 48-hour postpartum period despite no differences in severe pain scores,” the authors also reported.
“These findings are surprising given the standardized protocols in place designed to assess and treat pain post partum,” Etoi A. Garrison, MD, PhD, an associate professor of maternal-fetal medicine at Vanderbilt University Medical Center, Memphis, Tenn., said in an interview. ” Protocols should minimize bias and promote equitable delivery of care.”
Dr. Garrison said it’s important to find out why these discrepancies exist even when ready access to interpretation services exist in the hospital.
“An important component of health care disparity research is to hear directly from patients themselves about their experiences,” Dr. Garrison said. “Often the patient voice is an overlooked and underappreciated resource. I hope that future iterations of this work include patient perceptions about the adequacy of postpartum care and provide more information about how health care delivery can be tailored to the unique needs of this vulnerable population.”
The authors reported no disclosures. Dr Garrison reported receiving a grant from the State of Tennessee Maternal Mortality Review Committee to Create an Unconscious Bias Faculty Train-the-Trainer Program.
FROM ACOG 2021
Vaping and pregnancy: Inhaled toxins among reasons for pause
Researchers are trying to understand how e-cigarette use affects pregnancy and birth outcomes. This question may become more relevant as younger vapers, among whom the devices gained considerable popularity, start having children.
Limited emerging data from animal experiments and human epidemiologic studies suggest that vaping may have negative effects on fertility and pregnancy. “Even if these impacts are less severe than conventional smoking, we really should be thinking about alternate options that may be safer for our patients than inhalation of this aerosol,” said Blair J. Wylie, MD, MPH, a maternal-fetal medicine physician at Beth Israel Deaconess Medical Center in Boston.
Dr. Wylie reviewed what is known about vaping, including chemicals other than nicotine that have been detected in vape aerosols, and pregnancy at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
“There’s a lot we don’t know,” she said. “These products were only introduced recently, in 2003. They are marketed aggressively to our youth and have gained tremendous popularity among that population. And it’s only a matter of time, I think, before we see a lot of use in our own patient population.”
In a separate study presented at the ACOG meeting, Nicole Izhakoff, a researcher at Florida International University, Miami, and colleagues evaluated the association between e-cigarette use during pregnancy and unfavorable birth outcomes, such as preterm birth, low birth weight, or extended hospital stay for the newborn.
The investigators used 2016-2017 survey data from the Pregnancy Risk Assessment Monitoring System. In all, 71,940 women completed the survey, including 859 who reported e-cigarette use during pregnancy.
After adjusting for age, race, ethnicity, insurance, maternal education, prenatal care, abuse during pregnancy, and complications during pregnancy, the researchers estimated that the odds of an unfavorable birth outcome were 62% greater among women who used e-cigarettes during pregnancy, compared with those who did not.
The researchers lacked information about simultaneous use of alcohol, traditional tobacco, or other drugs, however.
“Physicians of all subspecialties, especially those of obstetrics-gynecology and pediatrics, need to increase the implementation of screening for past or current e-cigarette use in at-risk patients,” Ms. Izhakoff and coauthors concluded. “Further research regarding the long-term health effects of e-cigarettes is warranted.”
Dr. Wylie coauthored another study related to this topic that was published online May 24, 2021, in the Journal of Maternal-Fetal & Neonatal Medicine.
The researchers examined birth weights of children whose mothers use e-cigarettes alone, those whose mothers used both e-cigarettes and conventional cigarettes, and those whose mothers smoked conventional cigarettes only. Their estimates were imprecise, but signaled that e-cigarette use may reduce birth weight. The use of e-cigarettes alone appeared to have less of an impact on birth weight than the dual use of conventional cigarettes and e-cigarettes did.
Dr. Wylie cautioned that outcomes like birth weight are “pretty crude measures of whether an exposure is okay or not in pregnancy. Many of these toxins that we know that are in the aerosols can cause harm, but they may not be reflected in the absolute value of the birth weight.”
In addition, clinicians should avoid focusing on the wrong question when caring for patients.
“I think the wrong question is: Is vaping safer than smoking?” Dr. Wylie said in an interview. “Metals are going into your lungs. Plastics are going into your lungs. It is hard for me to think that we are going to identify that as our champion smoking cessation strategy in pregnancy.”
Rapidly changing landscape
Answering the question of which is safer is a challenge anyway because researchers likely have incomplete information about who vapes, who smokes, and who does both.
Still, the new research illustrates that “people are starting to think about this and beginning to do some analysis that is really hypothesis generating at this point,” Dr. Wylie said. Such studies may prompt clinicians to ask their patients about e-cigarette use. “Marijuana is sort of a similar thing where patients’ perception of safety, because things are legal, can lead to use during pregnancy without ... letting their care teams know,” she said. “Things are changing so rapidly in terms of what’s available to people to use that we need to stay on top of that as obstetricians and ask the right questions and try to understand what the risks are and potential benefits.”
Dr. Wylie is an obstetric consultant to the New England Pediatric Environmental Health Specialty Unit, which is where she heard pediatricians discussing widespread e-cigarette use among youth. It occurred to her that some of these teens eventually would be seeing obstetricians. She also saw parallels to prior research she conducted that focused on household air pollution or cooking from wood-burning fires in Africa.
“What is frightening, I think, about these electronic cigarettes is that you’re heating this liquid to extraordinarily high temperatures to create the vapor,” and the extreme heat vaporizes plastics and metals as well as nicotine, Dr. Wylie said.
An ACOG committee opinion discusses approaches to smoking and vaping cessation such as counseling, behavioral therapy, and medication.
The publication also lists a host of elements have been isolated from vape aerosol, including “carbonyl compounds (formaldehyde, acetaldehyde, acetone, and acrolein); volatile organic compounds (benzene and toluene); nitrosamines; particulate matter; and heavy metals such as copper, lead, zinc, and tin.”
In addition to the nicotine in e-cigarette liquids, which is harmful in itself, there is “all of this other company that it keeps,” including solvent byproducts, known carcinogens, and lung irritants, Dr. Wylie said. Fine particulate matter “can land in the small airways and cause inflammation, even translocate into the systemic circulation and cause systemic inflammation.”
The use of flavoring “likely alters perceptions of harm” and contributes to the popularity of vaping, Dr. Wylie noted. At the same time, the use of flavoring also has little regulatory oversight. Flavors usually are approved for marketing based on safety for ingestion, but that may not translate into safety for inhalation.
Parsing the health effects
People who vape have increased cough, wheezing, and phlegm production, compared with people who do not vape. Vaping also may worsen underlying lung disease like asthma. Lung function on spirometry decreases after e-cigarette use, studies have shown.
In 2019, researchers described e-cigarette or vaping product use–related acute lung injury (EVALI), which has caused more than 60 deaths in the United States. The condition may be related to vitamin E acetate, a component that had been used in some liquids used by patients with EVALI.
And the nicotine in e-cigarettes can accelerate atherogenesis and affect blood pressure, heart rate, and arterial stiffness.
Initially introduced as a smoking cessation tool, e-cigarettes now often are used on their own or in addition to cigarettes, rather than strictly for smoking cessation.
A Cochrane review suggests that e-cigarettes may be more effective than other approaches to smoking cessation. But “the effect is modest at best,” Dr. Wylie said. Among 100 people attempting to quit cigarette smoking, there might four to six more quitters with the use of e-cigarettes as a smoking cessation intervention, compared with other approaches.
Animal models provide other reasons for caution. One experiment in mice showed that exposure to e-cigarette aerosol impaired implantation and fetal health. The results suggest “that there might be some negative impacts across generations,” Dr. Wylie said.
Another study has suggested the possibility that women who currently use e-cigarettes may have slightly diminished fecundability. The results were not statistically significant, but the study “gives us pause about whether there could be some impact on early pregnancy and fertility,” Dr. Wylie said.
In mouse models, prenatal exposure to e-cigarette aerosol has decreased fetal weight and length, altered neurodevelopment and neuroregulatory gene expression, and increased proinflammatory cytokines. E-cigarette aerosol also has caused birth defects in zebrafish and facial clefting in frogs. Whether and how these data relate to human pregnancy is unclear.
While e-cigarette ads may convey a sense of style and harmlessness, clinicians have reasons to worry about the effects. “We have to be a little bit more cautious when we are talking about this with our patients,” Dr. Wylie said.
Dr. Wylie had no relevant financial disclosures. She is a Society for Maternal-Fetal Medicine board member and receives grant support related to research of household air pollution and pregnancy, prenatal pesticide exposure, preeclampsia in low income settings, and malaria during pregnancy. Ms. Izhakoff and coauthors had no disclosures.
Researchers are trying to understand how e-cigarette use affects pregnancy and birth outcomes. This question may become more relevant as younger vapers, among whom the devices gained considerable popularity, start having children.
Limited emerging data from animal experiments and human epidemiologic studies suggest that vaping may have negative effects on fertility and pregnancy. “Even if these impacts are less severe than conventional smoking, we really should be thinking about alternate options that may be safer for our patients than inhalation of this aerosol,” said Blair J. Wylie, MD, MPH, a maternal-fetal medicine physician at Beth Israel Deaconess Medical Center in Boston.
Dr. Wylie reviewed what is known about vaping, including chemicals other than nicotine that have been detected in vape aerosols, and pregnancy at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
“There’s a lot we don’t know,” she said. “These products were only introduced recently, in 2003. They are marketed aggressively to our youth and have gained tremendous popularity among that population. And it’s only a matter of time, I think, before we see a lot of use in our own patient population.”
In a separate study presented at the ACOG meeting, Nicole Izhakoff, a researcher at Florida International University, Miami, and colleagues evaluated the association between e-cigarette use during pregnancy and unfavorable birth outcomes, such as preterm birth, low birth weight, or extended hospital stay for the newborn.
The investigators used 2016-2017 survey data from the Pregnancy Risk Assessment Monitoring System. In all, 71,940 women completed the survey, including 859 who reported e-cigarette use during pregnancy.
After adjusting for age, race, ethnicity, insurance, maternal education, prenatal care, abuse during pregnancy, and complications during pregnancy, the researchers estimated that the odds of an unfavorable birth outcome were 62% greater among women who used e-cigarettes during pregnancy, compared with those who did not.
The researchers lacked information about simultaneous use of alcohol, traditional tobacco, or other drugs, however.
“Physicians of all subspecialties, especially those of obstetrics-gynecology and pediatrics, need to increase the implementation of screening for past or current e-cigarette use in at-risk patients,” Ms. Izhakoff and coauthors concluded. “Further research regarding the long-term health effects of e-cigarettes is warranted.”
Dr. Wylie coauthored another study related to this topic that was published online May 24, 2021, in the Journal of Maternal-Fetal & Neonatal Medicine.
The researchers examined birth weights of children whose mothers use e-cigarettes alone, those whose mothers used both e-cigarettes and conventional cigarettes, and those whose mothers smoked conventional cigarettes only. Their estimates were imprecise, but signaled that e-cigarette use may reduce birth weight. The use of e-cigarettes alone appeared to have less of an impact on birth weight than the dual use of conventional cigarettes and e-cigarettes did.
Dr. Wylie cautioned that outcomes like birth weight are “pretty crude measures of whether an exposure is okay or not in pregnancy. Many of these toxins that we know that are in the aerosols can cause harm, but they may not be reflected in the absolute value of the birth weight.”
In addition, clinicians should avoid focusing on the wrong question when caring for patients.
“I think the wrong question is: Is vaping safer than smoking?” Dr. Wylie said in an interview. “Metals are going into your lungs. Plastics are going into your lungs. It is hard for me to think that we are going to identify that as our champion smoking cessation strategy in pregnancy.”
Rapidly changing landscape
Answering the question of which is safer is a challenge anyway because researchers likely have incomplete information about who vapes, who smokes, and who does both.
Still, the new research illustrates that “people are starting to think about this and beginning to do some analysis that is really hypothesis generating at this point,” Dr. Wylie said. Such studies may prompt clinicians to ask their patients about e-cigarette use. “Marijuana is sort of a similar thing where patients’ perception of safety, because things are legal, can lead to use during pregnancy without ... letting their care teams know,” she said. “Things are changing so rapidly in terms of what’s available to people to use that we need to stay on top of that as obstetricians and ask the right questions and try to understand what the risks are and potential benefits.”
Dr. Wylie is an obstetric consultant to the New England Pediatric Environmental Health Specialty Unit, which is where she heard pediatricians discussing widespread e-cigarette use among youth. It occurred to her that some of these teens eventually would be seeing obstetricians. She also saw parallels to prior research she conducted that focused on household air pollution or cooking from wood-burning fires in Africa.
“What is frightening, I think, about these electronic cigarettes is that you’re heating this liquid to extraordinarily high temperatures to create the vapor,” and the extreme heat vaporizes plastics and metals as well as nicotine, Dr. Wylie said.
An ACOG committee opinion discusses approaches to smoking and vaping cessation such as counseling, behavioral therapy, and medication.
The publication also lists a host of elements have been isolated from vape aerosol, including “carbonyl compounds (formaldehyde, acetaldehyde, acetone, and acrolein); volatile organic compounds (benzene and toluene); nitrosamines; particulate matter; and heavy metals such as copper, lead, zinc, and tin.”
In addition to the nicotine in e-cigarette liquids, which is harmful in itself, there is “all of this other company that it keeps,” including solvent byproducts, known carcinogens, and lung irritants, Dr. Wylie said. Fine particulate matter “can land in the small airways and cause inflammation, even translocate into the systemic circulation and cause systemic inflammation.”
The use of flavoring “likely alters perceptions of harm” and contributes to the popularity of vaping, Dr. Wylie noted. At the same time, the use of flavoring also has little regulatory oversight. Flavors usually are approved for marketing based on safety for ingestion, but that may not translate into safety for inhalation.
Parsing the health effects
People who vape have increased cough, wheezing, and phlegm production, compared with people who do not vape. Vaping also may worsen underlying lung disease like asthma. Lung function on spirometry decreases after e-cigarette use, studies have shown.
In 2019, researchers described e-cigarette or vaping product use–related acute lung injury (EVALI), which has caused more than 60 deaths in the United States. The condition may be related to vitamin E acetate, a component that had been used in some liquids used by patients with EVALI.
And the nicotine in e-cigarettes can accelerate atherogenesis and affect blood pressure, heart rate, and arterial stiffness.
Initially introduced as a smoking cessation tool, e-cigarettes now often are used on their own or in addition to cigarettes, rather than strictly for smoking cessation.
A Cochrane review suggests that e-cigarettes may be more effective than other approaches to smoking cessation. But “the effect is modest at best,” Dr. Wylie said. Among 100 people attempting to quit cigarette smoking, there might four to six more quitters with the use of e-cigarettes as a smoking cessation intervention, compared with other approaches.
Animal models provide other reasons for caution. One experiment in mice showed that exposure to e-cigarette aerosol impaired implantation and fetal health. The results suggest “that there might be some negative impacts across generations,” Dr. Wylie said.
Another study has suggested the possibility that women who currently use e-cigarettes may have slightly diminished fecundability. The results were not statistically significant, but the study “gives us pause about whether there could be some impact on early pregnancy and fertility,” Dr. Wylie said.
In mouse models, prenatal exposure to e-cigarette aerosol has decreased fetal weight and length, altered neurodevelopment and neuroregulatory gene expression, and increased proinflammatory cytokines. E-cigarette aerosol also has caused birth defects in zebrafish and facial clefting in frogs. Whether and how these data relate to human pregnancy is unclear.
While e-cigarette ads may convey a sense of style and harmlessness, clinicians have reasons to worry about the effects. “We have to be a little bit more cautious when we are talking about this with our patients,” Dr. Wylie said.
Dr. Wylie had no relevant financial disclosures. She is a Society for Maternal-Fetal Medicine board member and receives grant support related to research of household air pollution and pregnancy, prenatal pesticide exposure, preeclampsia in low income settings, and malaria during pregnancy. Ms. Izhakoff and coauthors had no disclosures.
Researchers are trying to understand how e-cigarette use affects pregnancy and birth outcomes. This question may become more relevant as younger vapers, among whom the devices gained considerable popularity, start having children.
Limited emerging data from animal experiments and human epidemiologic studies suggest that vaping may have negative effects on fertility and pregnancy. “Even if these impacts are less severe than conventional smoking, we really should be thinking about alternate options that may be safer for our patients than inhalation of this aerosol,” said Blair J. Wylie, MD, MPH, a maternal-fetal medicine physician at Beth Israel Deaconess Medical Center in Boston.
Dr. Wylie reviewed what is known about vaping, including chemicals other than nicotine that have been detected in vape aerosols, and pregnancy at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
“There’s a lot we don’t know,” she said. “These products were only introduced recently, in 2003. They are marketed aggressively to our youth and have gained tremendous popularity among that population. And it’s only a matter of time, I think, before we see a lot of use in our own patient population.”
In a separate study presented at the ACOG meeting, Nicole Izhakoff, a researcher at Florida International University, Miami, and colleagues evaluated the association between e-cigarette use during pregnancy and unfavorable birth outcomes, such as preterm birth, low birth weight, or extended hospital stay for the newborn.
The investigators used 2016-2017 survey data from the Pregnancy Risk Assessment Monitoring System. In all, 71,940 women completed the survey, including 859 who reported e-cigarette use during pregnancy.
After adjusting for age, race, ethnicity, insurance, maternal education, prenatal care, abuse during pregnancy, and complications during pregnancy, the researchers estimated that the odds of an unfavorable birth outcome were 62% greater among women who used e-cigarettes during pregnancy, compared with those who did not.
The researchers lacked information about simultaneous use of alcohol, traditional tobacco, or other drugs, however.
“Physicians of all subspecialties, especially those of obstetrics-gynecology and pediatrics, need to increase the implementation of screening for past or current e-cigarette use in at-risk patients,” Ms. Izhakoff and coauthors concluded. “Further research regarding the long-term health effects of e-cigarettes is warranted.”
Dr. Wylie coauthored another study related to this topic that was published online May 24, 2021, in the Journal of Maternal-Fetal & Neonatal Medicine.
The researchers examined birth weights of children whose mothers use e-cigarettes alone, those whose mothers used both e-cigarettes and conventional cigarettes, and those whose mothers smoked conventional cigarettes only. Their estimates were imprecise, but signaled that e-cigarette use may reduce birth weight. The use of e-cigarettes alone appeared to have less of an impact on birth weight than the dual use of conventional cigarettes and e-cigarettes did.
Dr. Wylie cautioned that outcomes like birth weight are “pretty crude measures of whether an exposure is okay or not in pregnancy. Many of these toxins that we know that are in the aerosols can cause harm, but they may not be reflected in the absolute value of the birth weight.”
In addition, clinicians should avoid focusing on the wrong question when caring for patients.
“I think the wrong question is: Is vaping safer than smoking?” Dr. Wylie said in an interview. “Metals are going into your lungs. Plastics are going into your lungs. It is hard for me to think that we are going to identify that as our champion smoking cessation strategy in pregnancy.”
Rapidly changing landscape
Answering the question of which is safer is a challenge anyway because researchers likely have incomplete information about who vapes, who smokes, and who does both.
Still, the new research illustrates that “people are starting to think about this and beginning to do some analysis that is really hypothesis generating at this point,” Dr. Wylie said. Such studies may prompt clinicians to ask their patients about e-cigarette use. “Marijuana is sort of a similar thing where patients’ perception of safety, because things are legal, can lead to use during pregnancy without ... letting their care teams know,” she said. “Things are changing so rapidly in terms of what’s available to people to use that we need to stay on top of that as obstetricians and ask the right questions and try to understand what the risks are and potential benefits.”
Dr. Wylie is an obstetric consultant to the New England Pediatric Environmental Health Specialty Unit, which is where she heard pediatricians discussing widespread e-cigarette use among youth. It occurred to her that some of these teens eventually would be seeing obstetricians. She also saw parallels to prior research she conducted that focused on household air pollution or cooking from wood-burning fires in Africa.
“What is frightening, I think, about these electronic cigarettes is that you’re heating this liquid to extraordinarily high temperatures to create the vapor,” and the extreme heat vaporizes plastics and metals as well as nicotine, Dr. Wylie said.
An ACOG committee opinion discusses approaches to smoking and vaping cessation such as counseling, behavioral therapy, and medication.
The publication also lists a host of elements have been isolated from vape aerosol, including “carbonyl compounds (formaldehyde, acetaldehyde, acetone, and acrolein); volatile organic compounds (benzene and toluene); nitrosamines; particulate matter; and heavy metals such as copper, lead, zinc, and tin.”
In addition to the nicotine in e-cigarette liquids, which is harmful in itself, there is “all of this other company that it keeps,” including solvent byproducts, known carcinogens, and lung irritants, Dr. Wylie said. Fine particulate matter “can land in the small airways and cause inflammation, even translocate into the systemic circulation and cause systemic inflammation.”
The use of flavoring “likely alters perceptions of harm” and contributes to the popularity of vaping, Dr. Wylie noted. At the same time, the use of flavoring also has little regulatory oversight. Flavors usually are approved for marketing based on safety for ingestion, but that may not translate into safety for inhalation.
Parsing the health effects
People who vape have increased cough, wheezing, and phlegm production, compared with people who do not vape. Vaping also may worsen underlying lung disease like asthma. Lung function on spirometry decreases after e-cigarette use, studies have shown.
In 2019, researchers described e-cigarette or vaping product use–related acute lung injury (EVALI), which has caused more than 60 deaths in the United States. The condition may be related to vitamin E acetate, a component that had been used in some liquids used by patients with EVALI.
And the nicotine in e-cigarettes can accelerate atherogenesis and affect blood pressure, heart rate, and arterial stiffness.
Initially introduced as a smoking cessation tool, e-cigarettes now often are used on their own or in addition to cigarettes, rather than strictly for smoking cessation.
A Cochrane review suggests that e-cigarettes may be more effective than other approaches to smoking cessation. But “the effect is modest at best,” Dr. Wylie said. Among 100 people attempting to quit cigarette smoking, there might four to six more quitters with the use of e-cigarettes as a smoking cessation intervention, compared with other approaches.
Animal models provide other reasons for caution. One experiment in mice showed that exposure to e-cigarette aerosol impaired implantation and fetal health. The results suggest “that there might be some negative impacts across generations,” Dr. Wylie said.
Another study has suggested the possibility that women who currently use e-cigarettes may have slightly diminished fecundability. The results were not statistically significant, but the study “gives us pause about whether there could be some impact on early pregnancy and fertility,” Dr. Wylie said.
In mouse models, prenatal exposure to e-cigarette aerosol has decreased fetal weight and length, altered neurodevelopment and neuroregulatory gene expression, and increased proinflammatory cytokines. E-cigarette aerosol also has caused birth defects in zebrafish and facial clefting in frogs. Whether and how these data relate to human pregnancy is unclear.
While e-cigarette ads may convey a sense of style and harmlessness, clinicians have reasons to worry about the effects. “We have to be a little bit more cautious when we are talking about this with our patients,” Dr. Wylie said.
Dr. Wylie had no relevant financial disclosures. She is a Society for Maternal-Fetal Medicine board member and receives grant support related to research of household air pollution and pregnancy, prenatal pesticide exposure, preeclampsia in low income settings, and malaria during pregnancy. Ms. Izhakoff and coauthors had no disclosures.
FROM ACOG 2021
USPSTF recommends clinicians counsel pregnant patients to limit gestational weight gain
The U.S. Preventive Services Task Force has recommended clinicians counsel their adolescent and adult pregnant patients in primary care settings to use interventions to limit excess gestational weight gain.
Counseling pregnant persons on gestational weight gain (GWG) carries a B recommendation from the U.S. Preventive Services Task Force (USPSTF), meaning there is “moderate certainty that behavioral counseling interventions aimed at promoting healthy weight gain and preventing excess GWG in pregnancy have a moderate net benefit for pregnant persons,” the task force said in its recommendation statement, which was published in JAMA on May 25.
While the USPSTF has made other recommendations on screening for obesity in adults and gestational diabetes, this is the first recommendation from the task force on behavioral counseling interventions for pregnant persons to promote a healthy weight and limit GWG. The recommendation is important, the USPSTF said, because half of individuals entered pregnancy while either overweight (24%) or obese (24%) in 2015, with the prevalence of prepregnancy obesity higher among Alaska Native/American Indian (36.4%), Black (34.7%), and Hispanic (27.3%) women.
To define gestational weight gain, the USPSTF used National Academy of Medicine recommendations of weight change of 28-40 pounds in the underweight category (body mass index [BMI], < 18.5 kg/m2), 25-35 pounds in the normal-weight category (BMI, 18.5-24.9 kg/m2), 15-25 pounds in the overweight category (BMI, 25-29.9 kg/m2), and 11-20 pounds in the obese category (≥ 30 kg/m2).
Implementations of this recommendation include content with a focus on nutrition, physical activity, lifestyle change, or behavioral change. The counseling should be performed at the end of the first trimester or start of the second trimester and should stop shortly before delivery. “The most common types of behavioral counseling interventions included active or supervised exercise or counseling about diet and physical activity,” the USPSTF said.
The average duration of counseling sessions was between 15 and 120 minutes, varying from less than 2 contacts to more than 12 contacts involved in the intervention. Primary care clinicians can deliver these interventions themselves or refer the patient out to an intervention in another setting. “Effective behavioral counseling interventions often referred participants to various interventionists in different settings,” such as a local community fitness center, the authors wrote. “Participants were counseled on healthy diet and exercise through individual or group education sessions. Some interventions provided medically supervised group exercise classes with or without counseling.”
In their evidence report for the USPSTF recommendation, Amy G. Cantor, MD, of the Pacific Northwest Evidence-Based Practice Center, department of medical informatics and clinical epidemiology at Oregon Health & Science University in Portland, and colleagues performed a systematic review of 68 studies in the Ovid MEDLINE, Cochrane Central Register of Controlled Trials, and Cochrane Database of Systematic Reviews evaluating the effect of diet, exercise, and/or behavioral counseling interventions for 25,789 pregnant patients with GWG. The results were current up to February 2021 when the last search was performed. The mean ages of patients across all studies were 18.6 to 33.8 years, and 41% of studies contained patients from “diverse backgrounds.”
The results of the systematic review showed use of an intervention to limit GWG decreased the risk of gestational diabetes compared with a control group in 43 trials (relative risk, 0.87; 95% confidence interval, 0.79-0.95), emergency cesarean delivery in 14 trials (RR, 0.85; 95% CI, 0.74-0.96), macrosomia in 25 trials (RR, 0.77; 95% CI, 0.65-0.92), and large for gestational age infants in 26 trials (RR, 0.89; 95% CI, 0.80-0.99). There was not an association between GWG interventions and reduced gestational hypertension in 28 trials (RR, 0.87; 95% CI, 0.70-1.04), preeclampsia in 27 trials (RR, 0.98; 95% CI, 0.84-1.13), and lower risk of preterm birth in 33 trials (RR, 0.93; 95% CI, 0.81-1.07), as well as other outcomes such as respiratory distress syndrome, shoulder dystocia, neonatal intensive care unit admission, neonatal death, or infant growth during the first year.
In terms of the types of interventions used, Dr. Canton and colleagues found the greatest impact on GWG occurred when a high-intensity intervention with 12 or more sessions was used in 28 trials (−1.47 kg; 95% CI, −1.78 to −1.22) than in moderate-intensity interventions in 18 trials (−0.32 kg; 95% CI, −0.71 to −0.04) and low-intensity interventions in 9 trials (−0.64 kg; 94% CI, −1.44 to 0.02).
Implementing these interventions could be challenging
D. Yvette LaCoursiere, MD, of the department of obstetrics, gynecology, and reproductive sciences at the University of California, San Diego, in La Jolla, Calif., wrote in an accompanying editorial that the USPSTF recommendation supports the recommendation of the American College of Obstetricians and Gynecologists (ACOG) of offering nutritional and exercise-based support for patients with “excessive GWG,” but noted that leaving implementation of behavioral counseling interventions to the clinicians “is where challenges lie.”
“The USPSTF recommendations will require lengthening already time-constrained prenatal visits or relying on adjunctive professionals,” she said.
Dr. LaCoursiere highlighted the amount of time the behavioral counseling interventions took to implement, with the shortest intervention lasting 15 minutes. “With the exception of those in group prenatal care practices, clinicians conducting the standard prenatal visit will find it difficult to accommodate moderate- or high-intensity interventions. On a similar note, the topics included in many of the interventions are broad and not necessarily in the purview of clinicians who provide prenatal care,” she said.
In addition, behavioral counseling interventions may not be covered by some patients’ insurance plans, Dr. LaCoursiere explained. “While it is a federal requirement for states to provide pregnant Medicaid enrollees smoking cessation counseling and prescription drugs, there is no such mandate for nutrition or physical activity counseling. Neither is it required that states provide these services to nonpregnant enrollees,” she said. “These are not insurmountable challenges, but more groundwork is necessary to ensure an effective and efficient implementation.”
Commenting on how a clinician could fit a behavioral counseling intervention into the prenatal care model, Dr. LaCoursiere said creativity may be needed. Some researchers in the systematic review used Internet or telehealth-based programs for dietary education, exercise support, health information, and goal setting, for example, which could help with continuity of care during the COVID-19 pandemic. “These types of interventions may help overcome the obstacle of insufficient clinic time by separating the primary implementation phase from the traditional clinical setting,” she said.
While the evidence supports the implementation of these interventions, “additional work remains for clinicians and researchers to identify high-yield components and determine best practices for the delivery of GWG interventions,” she said.
“The success of this intervention will depend on improving resources for clinicians to facilitate provision of direct counseling or to refer patients to skilled professionals and explore novel alternatives. Promising innovative approaches such as the use of telehealth, technology-based delivery systems, and group prenatal care are under investigation and may expand the ability to successfully implement these recommendations and ultimately improve outcomes for pregnant persons and their infants,” Dr. LaCoursiere concluded.
This research was funded by contracts from the Agency for Healthcare Research and Quality and U.S. Department of Health and Human Services. The authors report no relevant conflict of interest.
The U.S. Preventive Services Task Force has recommended clinicians counsel their adolescent and adult pregnant patients in primary care settings to use interventions to limit excess gestational weight gain.
Counseling pregnant persons on gestational weight gain (GWG) carries a B recommendation from the U.S. Preventive Services Task Force (USPSTF), meaning there is “moderate certainty that behavioral counseling interventions aimed at promoting healthy weight gain and preventing excess GWG in pregnancy have a moderate net benefit for pregnant persons,” the task force said in its recommendation statement, which was published in JAMA on May 25.
While the USPSTF has made other recommendations on screening for obesity in adults and gestational diabetes, this is the first recommendation from the task force on behavioral counseling interventions for pregnant persons to promote a healthy weight and limit GWG. The recommendation is important, the USPSTF said, because half of individuals entered pregnancy while either overweight (24%) or obese (24%) in 2015, with the prevalence of prepregnancy obesity higher among Alaska Native/American Indian (36.4%), Black (34.7%), and Hispanic (27.3%) women.
To define gestational weight gain, the USPSTF used National Academy of Medicine recommendations of weight change of 28-40 pounds in the underweight category (body mass index [BMI], < 18.5 kg/m2), 25-35 pounds in the normal-weight category (BMI, 18.5-24.9 kg/m2), 15-25 pounds in the overweight category (BMI, 25-29.9 kg/m2), and 11-20 pounds in the obese category (≥ 30 kg/m2).
Implementations of this recommendation include content with a focus on nutrition, physical activity, lifestyle change, or behavioral change. The counseling should be performed at the end of the first trimester or start of the second trimester and should stop shortly before delivery. “The most common types of behavioral counseling interventions included active or supervised exercise or counseling about diet and physical activity,” the USPSTF said.
The average duration of counseling sessions was between 15 and 120 minutes, varying from less than 2 contacts to more than 12 contacts involved in the intervention. Primary care clinicians can deliver these interventions themselves or refer the patient out to an intervention in another setting. “Effective behavioral counseling interventions often referred participants to various interventionists in different settings,” such as a local community fitness center, the authors wrote. “Participants were counseled on healthy diet and exercise through individual or group education sessions. Some interventions provided medically supervised group exercise classes with or without counseling.”
In their evidence report for the USPSTF recommendation, Amy G. Cantor, MD, of the Pacific Northwest Evidence-Based Practice Center, department of medical informatics and clinical epidemiology at Oregon Health & Science University in Portland, and colleagues performed a systematic review of 68 studies in the Ovid MEDLINE, Cochrane Central Register of Controlled Trials, and Cochrane Database of Systematic Reviews evaluating the effect of diet, exercise, and/or behavioral counseling interventions for 25,789 pregnant patients with GWG. The results were current up to February 2021 when the last search was performed. The mean ages of patients across all studies were 18.6 to 33.8 years, and 41% of studies contained patients from “diverse backgrounds.”
The results of the systematic review showed use of an intervention to limit GWG decreased the risk of gestational diabetes compared with a control group in 43 trials (relative risk, 0.87; 95% confidence interval, 0.79-0.95), emergency cesarean delivery in 14 trials (RR, 0.85; 95% CI, 0.74-0.96), macrosomia in 25 trials (RR, 0.77; 95% CI, 0.65-0.92), and large for gestational age infants in 26 trials (RR, 0.89; 95% CI, 0.80-0.99). There was not an association between GWG interventions and reduced gestational hypertension in 28 trials (RR, 0.87; 95% CI, 0.70-1.04), preeclampsia in 27 trials (RR, 0.98; 95% CI, 0.84-1.13), and lower risk of preterm birth in 33 trials (RR, 0.93; 95% CI, 0.81-1.07), as well as other outcomes such as respiratory distress syndrome, shoulder dystocia, neonatal intensive care unit admission, neonatal death, or infant growth during the first year.
In terms of the types of interventions used, Dr. Canton and colleagues found the greatest impact on GWG occurred when a high-intensity intervention with 12 or more sessions was used in 28 trials (−1.47 kg; 95% CI, −1.78 to −1.22) than in moderate-intensity interventions in 18 trials (−0.32 kg; 95% CI, −0.71 to −0.04) and low-intensity interventions in 9 trials (−0.64 kg; 94% CI, −1.44 to 0.02).
Implementing these interventions could be challenging
D. Yvette LaCoursiere, MD, of the department of obstetrics, gynecology, and reproductive sciences at the University of California, San Diego, in La Jolla, Calif., wrote in an accompanying editorial that the USPSTF recommendation supports the recommendation of the American College of Obstetricians and Gynecologists (ACOG) of offering nutritional and exercise-based support for patients with “excessive GWG,” but noted that leaving implementation of behavioral counseling interventions to the clinicians “is where challenges lie.”
“The USPSTF recommendations will require lengthening already time-constrained prenatal visits or relying on adjunctive professionals,” she said.
Dr. LaCoursiere highlighted the amount of time the behavioral counseling interventions took to implement, with the shortest intervention lasting 15 minutes. “With the exception of those in group prenatal care practices, clinicians conducting the standard prenatal visit will find it difficult to accommodate moderate- or high-intensity interventions. On a similar note, the topics included in many of the interventions are broad and not necessarily in the purview of clinicians who provide prenatal care,” she said.
In addition, behavioral counseling interventions may not be covered by some patients’ insurance plans, Dr. LaCoursiere explained. “While it is a federal requirement for states to provide pregnant Medicaid enrollees smoking cessation counseling and prescription drugs, there is no such mandate for nutrition or physical activity counseling. Neither is it required that states provide these services to nonpregnant enrollees,” she said. “These are not insurmountable challenges, but more groundwork is necessary to ensure an effective and efficient implementation.”
Commenting on how a clinician could fit a behavioral counseling intervention into the prenatal care model, Dr. LaCoursiere said creativity may be needed. Some researchers in the systematic review used Internet or telehealth-based programs for dietary education, exercise support, health information, and goal setting, for example, which could help with continuity of care during the COVID-19 pandemic. “These types of interventions may help overcome the obstacle of insufficient clinic time by separating the primary implementation phase from the traditional clinical setting,” she said.
While the evidence supports the implementation of these interventions, “additional work remains for clinicians and researchers to identify high-yield components and determine best practices for the delivery of GWG interventions,” she said.
“The success of this intervention will depend on improving resources for clinicians to facilitate provision of direct counseling or to refer patients to skilled professionals and explore novel alternatives. Promising innovative approaches such as the use of telehealth, technology-based delivery systems, and group prenatal care are under investigation and may expand the ability to successfully implement these recommendations and ultimately improve outcomes for pregnant persons and their infants,” Dr. LaCoursiere concluded.
This research was funded by contracts from the Agency for Healthcare Research and Quality and U.S. Department of Health and Human Services. The authors report no relevant conflict of interest.
The U.S. Preventive Services Task Force has recommended clinicians counsel their adolescent and adult pregnant patients in primary care settings to use interventions to limit excess gestational weight gain.
Counseling pregnant persons on gestational weight gain (GWG) carries a B recommendation from the U.S. Preventive Services Task Force (USPSTF), meaning there is “moderate certainty that behavioral counseling interventions aimed at promoting healthy weight gain and preventing excess GWG in pregnancy have a moderate net benefit for pregnant persons,” the task force said in its recommendation statement, which was published in JAMA on May 25.
While the USPSTF has made other recommendations on screening for obesity in adults and gestational diabetes, this is the first recommendation from the task force on behavioral counseling interventions for pregnant persons to promote a healthy weight and limit GWG. The recommendation is important, the USPSTF said, because half of individuals entered pregnancy while either overweight (24%) or obese (24%) in 2015, with the prevalence of prepregnancy obesity higher among Alaska Native/American Indian (36.4%), Black (34.7%), and Hispanic (27.3%) women.
To define gestational weight gain, the USPSTF used National Academy of Medicine recommendations of weight change of 28-40 pounds in the underweight category (body mass index [BMI], < 18.5 kg/m2), 25-35 pounds in the normal-weight category (BMI, 18.5-24.9 kg/m2), 15-25 pounds in the overweight category (BMI, 25-29.9 kg/m2), and 11-20 pounds in the obese category (≥ 30 kg/m2).
Implementations of this recommendation include content with a focus on nutrition, physical activity, lifestyle change, or behavioral change. The counseling should be performed at the end of the first trimester or start of the second trimester and should stop shortly before delivery. “The most common types of behavioral counseling interventions included active or supervised exercise or counseling about diet and physical activity,” the USPSTF said.
The average duration of counseling sessions was between 15 and 120 minutes, varying from less than 2 contacts to more than 12 contacts involved in the intervention. Primary care clinicians can deliver these interventions themselves or refer the patient out to an intervention in another setting. “Effective behavioral counseling interventions often referred participants to various interventionists in different settings,” such as a local community fitness center, the authors wrote. “Participants were counseled on healthy diet and exercise through individual or group education sessions. Some interventions provided medically supervised group exercise classes with or without counseling.”
In their evidence report for the USPSTF recommendation, Amy G. Cantor, MD, of the Pacific Northwest Evidence-Based Practice Center, department of medical informatics and clinical epidemiology at Oregon Health & Science University in Portland, and colleagues performed a systematic review of 68 studies in the Ovid MEDLINE, Cochrane Central Register of Controlled Trials, and Cochrane Database of Systematic Reviews evaluating the effect of diet, exercise, and/or behavioral counseling interventions for 25,789 pregnant patients with GWG. The results were current up to February 2021 when the last search was performed. The mean ages of patients across all studies were 18.6 to 33.8 years, and 41% of studies contained patients from “diverse backgrounds.”
The results of the systematic review showed use of an intervention to limit GWG decreased the risk of gestational diabetes compared with a control group in 43 trials (relative risk, 0.87; 95% confidence interval, 0.79-0.95), emergency cesarean delivery in 14 trials (RR, 0.85; 95% CI, 0.74-0.96), macrosomia in 25 trials (RR, 0.77; 95% CI, 0.65-0.92), and large for gestational age infants in 26 trials (RR, 0.89; 95% CI, 0.80-0.99). There was not an association between GWG interventions and reduced gestational hypertension in 28 trials (RR, 0.87; 95% CI, 0.70-1.04), preeclampsia in 27 trials (RR, 0.98; 95% CI, 0.84-1.13), and lower risk of preterm birth in 33 trials (RR, 0.93; 95% CI, 0.81-1.07), as well as other outcomes such as respiratory distress syndrome, shoulder dystocia, neonatal intensive care unit admission, neonatal death, or infant growth during the first year.
In terms of the types of interventions used, Dr. Canton and colleagues found the greatest impact on GWG occurred when a high-intensity intervention with 12 or more sessions was used in 28 trials (−1.47 kg; 95% CI, −1.78 to −1.22) than in moderate-intensity interventions in 18 trials (−0.32 kg; 95% CI, −0.71 to −0.04) and low-intensity interventions in 9 trials (−0.64 kg; 94% CI, −1.44 to 0.02).
Implementing these interventions could be challenging
D. Yvette LaCoursiere, MD, of the department of obstetrics, gynecology, and reproductive sciences at the University of California, San Diego, in La Jolla, Calif., wrote in an accompanying editorial that the USPSTF recommendation supports the recommendation of the American College of Obstetricians and Gynecologists (ACOG) of offering nutritional and exercise-based support for patients with “excessive GWG,” but noted that leaving implementation of behavioral counseling interventions to the clinicians “is where challenges lie.”
“The USPSTF recommendations will require lengthening already time-constrained prenatal visits or relying on adjunctive professionals,” she said.
Dr. LaCoursiere highlighted the amount of time the behavioral counseling interventions took to implement, with the shortest intervention lasting 15 minutes. “With the exception of those in group prenatal care practices, clinicians conducting the standard prenatal visit will find it difficult to accommodate moderate- or high-intensity interventions. On a similar note, the topics included in many of the interventions are broad and not necessarily in the purview of clinicians who provide prenatal care,” she said.
In addition, behavioral counseling interventions may not be covered by some patients’ insurance plans, Dr. LaCoursiere explained. “While it is a federal requirement for states to provide pregnant Medicaid enrollees smoking cessation counseling and prescription drugs, there is no such mandate for nutrition or physical activity counseling. Neither is it required that states provide these services to nonpregnant enrollees,” she said. “These are not insurmountable challenges, but more groundwork is necessary to ensure an effective and efficient implementation.”
Commenting on how a clinician could fit a behavioral counseling intervention into the prenatal care model, Dr. LaCoursiere said creativity may be needed. Some researchers in the systematic review used Internet or telehealth-based programs for dietary education, exercise support, health information, and goal setting, for example, which could help with continuity of care during the COVID-19 pandemic. “These types of interventions may help overcome the obstacle of insufficient clinic time by separating the primary implementation phase from the traditional clinical setting,” she said.
While the evidence supports the implementation of these interventions, “additional work remains for clinicians and researchers to identify high-yield components and determine best practices for the delivery of GWG interventions,” she said.
“The success of this intervention will depend on improving resources for clinicians to facilitate provision of direct counseling or to refer patients to skilled professionals and explore novel alternatives. Promising innovative approaches such as the use of telehealth, technology-based delivery systems, and group prenatal care are under investigation and may expand the ability to successfully implement these recommendations and ultimately improve outcomes for pregnant persons and their infants,” Dr. LaCoursiere concluded.
This research was funded by contracts from the Agency for Healthcare Research and Quality and U.S. Department of Health and Human Services. The authors report no relevant conflict of interest.
FROM JAMA
Novel drug approvals of 2020
In 2020, the Food and Drug Administration approved 53 new drugs for humans. One of these agents, Annovera (segesterone and ethinyl estradiol), is a vaginal ring to prevent pregnancy and is not relevant in this article. A second drug, Asparlas (calaspargase pegol), indicated to treat acute lymphoblastic leukemia, has not yet been released by its manufacturer. Orgovyx (relugolix) is used for prostate cancer and Lampit (nifurtimox) is drug used in children – neither of these two agents will be covered. The remaining 49 are covered below. The agents with molecular weights less than 1,000 probably cross the placenta in the first half of pregnancy, but nearly all, regardless of MW, will cross in the second half of pregnancy.
No human pregnancy data for these agents has been found, but there are five drugs included in pregnancy registries. It will take some time before the outcomes of these drugs are published. The routine absence of pregnancy data for most drugs was pointed out in an article that I coauthored, “Should pregnant women be included in phase 4 clinical drug trials?”. The article makes a strong argument for including some pregnant women in these trials.
Anti-infectives
Artesunate (384)
The drug appears low risk when used in the second and third trimesters. There is inadequate information regarding its use in the first trimester, so the safest course for the embryo appears to be avoiding its use during this period. A single intravenous dose given to rats early in gestation resulted in embryolethality.
Ebanga (ansuvimab) (147,000)
Studies on its use in pregnant animals have not been conducted.
Inmazeb (atoltivimab, maftivimab, odesivimab) (144,000-146,000)
Inmazeb is a combination of the three agents. Studies on its use in pregnant animals have not been conducted.
Veklury (remdesivir) (603)
Veklury is indicated for the treatment of pregnant women hospitalized with COVID-19 who are at risk for serious morbidity and mortality. The drug should be used during pregnancy only if the potential benefit justifies the potential risk for the mother and the fetus.
Antineoplastics
Ayvakit (avapritinib) (499)
The drug may cause fetal harm. The drug was teratogenic in animals.
Blenrep (belantamab mafodotin-blmf) (152,000)
A B-cell maturation antigen, it is indicated for the treatment of multiple myeloma. No human or animal pregnancy data have been located.
Danyelza (naxitamab-gqgk) (144,000)
This agent is used for the treatment of neuroblastoma. Based on its mechanism of action it may cause fetal harm if used in pregnancy.
Gavreto (pralsetinib) (534)
Gavreto is indicated for the treatment of small cell lung cancer. It may cause embryo-fetal harm if used in pregnancy.
Inqovi (cedazuridine + decitabine) (268,228)
The drug combination can cause fetal harm in human pregnancy. It is toxic in pregnant animals.
Margenza (margetuximab-cmkb) (149,000)
Although there are no data on the use of this drug in human pregnancy, the findings in animals and mechanism of action suggest that it will cause fetal harm.
Monjuvi (tafasitamab-cxix) (150,000)
This drug is a cytolytic antibody that is indicated in combination with lenalidomide. The combination may cause fetal harm.
Pemazyre (pemigatinib) (488)
It is indicated for the treatment of cholangiocarcinoma. In an animal study, the drug caused fetal defects, fetal growth retardation, and embryo-fetal death at maternal exposures lower than the human exposure.
Qinlock (ripretinib) (510)
This drug is used for the treatment of patients with advanced gastrointestinal stromal tumor. The drug was teratogenic in pregnant animals.
Retevmo (selpercatinib) (526)
This is a kinase inhibitor used for the treatment of small cell lung cancer. The drug is teratogenic in animals.
Sarclisa (isatuximab-irfc) (148,000)This drug is used in combination with pomalidomide and dexamethasone. The combination would probably cause major toxicity in an embryo or fetus.
Tabrecta (capmatinib) (412 – free base)Capmatinib is a kinase inhibitor used for the treatment of metastatic non–small cell lung cancer. It is teratogenic in animals.
Tazverik (tazemetostat) (654)Tazemetostat is indicated for the treatment of epithelioid sarcoma and follicular lymphoma, The drug is teratogenic in animals.
Trodelvy (sacituzumab govitecan-hziy) (1,602)This agent is used for the treatment of breast cancer. The drug has not been tested in pregnant animals. However, according to the manufacturer, there is a high possibility of human teratogenicity if it is given to a pregnant woman.
Tukysa (tucatinib) (481)
Tukysa is a tyrosine kinase inhibitor that is used in combination with trastuzumab and capecitabine for the treatment of breast cancer. The drug is teratogenic in animals.
Zeposia (ozanimod) (441)
Zeposia is indicated for the treatment of multiple sclerosis. The drug takes about 3 months to eliminate from the body. The drug is teratogenic in animals.
Zepzelca (lurbinectedin) (785)
This agent is used for the treatment of metastatic small cell lung cancer. The drug is teratogenic in animals.
Antiemetics
Barhemsys (amisulpride) (369)
This agent is Indicated to prevent nausea and vomiting. Animal data suggest low risk of embryo/fetal birth defects.
Antimigraine
Nurtec (rimegepant) (611)
Nurtec is indicated for acute treatment of migraine. Development toxicity was not observed in animals given doses similar to those used in humans.
Vyepti (eptinezumab-jjmr) (143,000)
A humanized monoclonal antibody that is given every 3 months to prevent migraine. There was no embryo-fetal harm in animals given the drug.
CNS
Byfavo (remimazolam) (493 – free base)
This drug is indicated for procedural sedation in adults undergoing procedures lasting 30 minutes or less. No defects were observed in animals.
Diagnostics
Cerianna (fluoroestradiol F 18) (289)
It is indicated for use with PET for characterization of estrogen receptor status in patients with ER-positive breast cancer. It has the potential to cause fetal harm depending on the fetal stage of development and the magnitude of radiation dose. There are no data on its use in pregnant women or animals.
Detectnet (copper CU-64 dotatate) (1,497)
All radiopharmaceuticals have the potential to cause fetal harm depending on the fetal stage of development and the magnitude of the radiation dose. There are no pregnancy data in humans or animals
Miscellaneous
Dojolvi (triheptanoin) (429)
This agent is indicated as a source of calories and fatty acids for the treatment of pediatric and adult patients with molecularly confirmed long-chain fatty acid oxidation disorders. Advise patients that there is a pregnancy safety study that collects pregnancy outcome data in women taking Dojolvi during pregnancy. Pregnant patients can enroll in the study by calling 1-888-756-8657.
Enspryng (satralizumab-mwge) (143,000)
It is indicated for the treatment of neuromyelitis optica spectrum disorder in adult patients who are anti–aquaporin-4 (AQP4) antibody positive. No information is available on the risks, if any, in pregnancy. No adverse effects on maternal or fetal development were observed in pregnant monkeys and their offspring.
Evrysdi (risdiplam) (401)
This is a prescription medicine used to treat spinal muscular atrophy in adults and children aged 2 months and older. In pregnant animals the drug caused adverse effects on fetal development.
Gemtesa (vibegron) (445)
Gemtesa is used in adults to treat the symptoms of overactive bladder. The drug had no adverse effects on pregnant animals.
Imcivree (setmelanotide) (1,117)
This drug is indicated for chronic weight management in adult and pediatric patients aged 6 years and older with obesity because of proopiomelanocortin, proprotein convertase subtilisin/kexin type 1, or leptin receptor deficiency. The drug was not embryo toxic in animals.
Isturisa (osilodrostat) (325)
Isturisa is a cortisol synthesis inhibitor indicated for the treatment of adult patients with Cushing’s disease. No adverse fetal effects were observed in pregnant animals.
Klisyri (tirbanibulin) (431)
Tirbanibulin ointment is a microtubule inhibitor that is used to treat actinic keratosis. Information on its effects in pregnancy is not available.
Koselugo (selumetinib) (556)
This is a kinase inhibitor indicated for the treatment of pediatric patients aged 2 years and older. The drug is toxic in pregnant animals but its effects in human pregnancy are not known.
Nexletol (bempedoic acid) (344)
Nexletol is indicated as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia or established atherosclerotic cardiovascular disease who require additional lowering of LDL cholesterol. The drug was not teratogenic in animals. Discontinue Nexletol when pregnancy is recognized unless the benefits of therapy outweigh the potential risks to the fetus.
Olinvyk (oliceridine) (503)
Olinvyk injection is indicated in adults for the management of acute pain severe enough to require an intravenous opioid analgesic. Prolonged use of Olinvyk during pregnancy can result in neonatal opioid withdrawal syndrome. The drug was not teratogenic in animals.
Ongentys (opicapone) (413)
Ongentys is indicated as adjunctive treatment to levodopa/carbidopa in patients with Parkinson’s disease experiencing “off” episodes. The drug was teratogenic in rabbits but not in rats.
Orladeyo (berotralstat) (635)
This drug is a plasma kallikrein inhibitor indicated for prophylaxis to prevent attacks of hereditary angioedema. It was not teratogenic in animals.
Oxlumo (lumasiran) (17,286)
Oxlumo is a HAO1-directed small interfering ribonucleic acid indicated for the treatment of primary hyperoxaluria type 1 to lower urinary oxalate levels. No adverse effects on pregnancy or embryo-fetal development related to the drug were observed in animals.
Pizensy (lactitol) (344)
Lactitol is minimally absorbed systemically following oral administration. It is unknown whether maternal use will result in fetal exposure to the drug. No effects on embryo-fetal development were observed in animals at doses much higher than the maximum recommended human dosage.
Rukobia (fostemsavir) (705; 584 for free acid)
This drug is an HIV-1–directed attachment inhibitor, in combination with other antiretrovirals. There is a pregnancy exposure registry that monitors pregnancy outcomes in individuals exposed to the drug during pregnancy. Health care providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry at 1-800-258-4263.
Sogroya (somapacitan-beco) (23,305)
This is a human growth hormone analog indicated for replacement of endogenous growth hormone in adults with growth hormone deficiency. The drug was not teratogenic in animals.
Tepezza (teprotumumab-trbw) (148,000)
Drug is indicated for the treatment of thyroid eye disease. The drug was teratogenic in cynomolgus monkeys. The manufacturer states that because of the risk, the drug should not be used in pregnancy.
Tauvid (flortaucipir F-18) (262)
This drug is indicated for use with PET imaging of the brain to evaluate for Alzheimer’s disease. It is a radioactive drug and should not be used in pregnant women.
Uplizna (inebilizumab-cdon) (149,000)
Uplizna is indicated for the treatment of neuromyelitis optica spectrum disorder in adult patients who are anti-AQP4 antibody positive. It is a humanized IgG1 monoclonal antibody and immunoglobulins are known to cross the placental barrier. Based on animal data, the drug can cause fetal harm because of B-cell lymphopenia and reduce antibody response in offspring exposed to the drug. Women of childbearing potential should use contraception while receiving Uplizna and for 6 months after the last dose.
Winlevi (clascoterone) (403)
This cream is an androgen receptor inhibitor that is indicated for the topical treatment of acne vulgaris in patients aged 12 years and older. Subcutaneous use in animals was associated with fetal defects.
Xeglyze (abametapir) (1,840)
Xeglyze is indicated for the topical treatment of head lice infestation in patients aged 6 months and older. The drug was not teratogenic in animals.
Zokinvy (lonafarnib) (639)
Zokinvy is indicated in patients 12 months or older to reduce the risk of mortality in several conditions. Animal studies have found embryo-fetal harm.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
In 2020, the Food and Drug Administration approved 53 new drugs for humans. One of these agents, Annovera (segesterone and ethinyl estradiol), is a vaginal ring to prevent pregnancy and is not relevant in this article. A second drug, Asparlas (calaspargase pegol), indicated to treat acute lymphoblastic leukemia, has not yet been released by its manufacturer. Orgovyx (relugolix) is used for prostate cancer and Lampit (nifurtimox) is drug used in children – neither of these two agents will be covered. The remaining 49 are covered below. The agents with molecular weights less than 1,000 probably cross the placenta in the first half of pregnancy, but nearly all, regardless of MW, will cross in the second half of pregnancy.
No human pregnancy data for these agents has been found, but there are five drugs included in pregnancy registries. It will take some time before the outcomes of these drugs are published. The routine absence of pregnancy data for most drugs was pointed out in an article that I coauthored, “Should pregnant women be included in phase 4 clinical drug trials?”. The article makes a strong argument for including some pregnant women in these trials.
Anti-infectives
Artesunate (384)
The drug appears low risk when used in the second and third trimesters. There is inadequate information regarding its use in the first trimester, so the safest course for the embryo appears to be avoiding its use during this period. A single intravenous dose given to rats early in gestation resulted in embryolethality.
Ebanga (ansuvimab) (147,000)
Studies on its use in pregnant animals have not been conducted.
Inmazeb (atoltivimab, maftivimab, odesivimab) (144,000-146,000)
Inmazeb is a combination of the three agents. Studies on its use in pregnant animals have not been conducted.
Veklury (remdesivir) (603)
Veklury is indicated for the treatment of pregnant women hospitalized with COVID-19 who are at risk for serious morbidity and mortality. The drug should be used during pregnancy only if the potential benefit justifies the potential risk for the mother and the fetus.
Antineoplastics
Ayvakit (avapritinib) (499)
The drug may cause fetal harm. The drug was teratogenic in animals.
Blenrep (belantamab mafodotin-blmf) (152,000)
A B-cell maturation antigen, it is indicated for the treatment of multiple myeloma. No human or animal pregnancy data have been located.
Danyelza (naxitamab-gqgk) (144,000)
This agent is used for the treatment of neuroblastoma. Based on its mechanism of action it may cause fetal harm if used in pregnancy.
Gavreto (pralsetinib) (534)
Gavreto is indicated for the treatment of small cell lung cancer. It may cause embryo-fetal harm if used in pregnancy.
Inqovi (cedazuridine + decitabine) (268,228)
The drug combination can cause fetal harm in human pregnancy. It is toxic in pregnant animals.
Margenza (margetuximab-cmkb) (149,000)
Although there are no data on the use of this drug in human pregnancy, the findings in animals and mechanism of action suggest that it will cause fetal harm.
Monjuvi (tafasitamab-cxix) (150,000)
This drug is a cytolytic antibody that is indicated in combination with lenalidomide. The combination may cause fetal harm.
Pemazyre (pemigatinib) (488)
It is indicated for the treatment of cholangiocarcinoma. In an animal study, the drug caused fetal defects, fetal growth retardation, and embryo-fetal death at maternal exposures lower than the human exposure.
Qinlock (ripretinib) (510)
This drug is used for the treatment of patients with advanced gastrointestinal stromal tumor. The drug was teratogenic in pregnant animals.
Retevmo (selpercatinib) (526)
This is a kinase inhibitor used for the treatment of small cell lung cancer. The drug is teratogenic in animals.
Sarclisa (isatuximab-irfc) (148,000)This drug is used in combination with pomalidomide and dexamethasone. The combination would probably cause major toxicity in an embryo or fetus.
Tabrecta (capmatinib) (412 – free base)Capmatinib is a kinase inhibitor used for the treatment of metastatic non–small cell lung cancer. It is teratogenic in animals.
Tazverik (tazemetostat) (654)Tazemetostat is indicated for the treatment of epithelioid sarcoma and follicular lymphoma, The drug is teratogenic in animals.
Trodelvy (sacituzumab govitecan-hziy) (1,602)This agent is used for the treatment of breast cancer. The drug has not been tested in pregnant animals. However, according to the manufacturer, there is a high possibility of human teratogenicity if it is given to a pregnant woman.
Tukysa (tucatinib) (481)
Tukysa is a tyrosine kinase inhibitor that is used in combination with trastuzumab and capecitabine for the treatment of breast cancer. The drug is teratogenic in animals.
Zeposia (ozanimod) (441)
Zeposia is indicated for the treatment of multiple sclerosis. The drug takes about 3 months to eliminate from the body. The drug is teratogenic in animals.
Zepzelca (lurbinectedin) (785)
This agent is used for the treatment of metastatic small cell lung cancer. The drug is teratogenic in animals.
Antiemetics
Barhemsys (amisulpride) (369)
This agent is Indicated to prevent nausea and vomiting. Animal data suggest low risk of embryo/fetal birth defects.
Antimigraine
Nurtec (rimegepant) (611)
Nurtec is indicated for acute treatment of migraine. Development toxicity was not observed in animals given doses similar to those used in humans.
Vyepti (eptinezumab-jjmr) (143,000)
A humanized monoclonal antibody that is given every 3 months to prevent migraine. There was no embryo-fetal harm in animals given the drug.
CNS
Byfavo (remimazolam) (493 – free base)
This drug is indicated for procedural sedation in adults undergoing procedures lasting 30 minutes or less. No defects were observed in animals.
Diagnostics
Cerianna (fluoroestradiol F 18) (289)
It is indicated for use with PET for characterization of estrogen receptor status in patients with ER-positive breast cancer. It has the potential to cause fetal harm depending on the fetal stage of development and the magnitude of radiation dose. There are no data on its use in pregnant women or animals.
Detectnet (copper CU-64 dotatate) (1,497)
All radiopharmaceuticals have the potential to cause fetal harm depending on the fetal stage of development and the magnitude of the radiation dose. There are no pregnancy data in humans or animals
Miscellaneous
Dojolvi (triheptanoin) (429)
This agent is indicated as a source of calories and fatty acids for the treatment of pediatric and adult patients with molecularly confirmed long-chain fatty acid oxidation disorders. Advise patients that there is a pregnancy safety study that collects pregnancy outcome data in women taking Dojolvi during pregnancy. Pregnant patients can enroll in the study by calling 1-888-756-8657.
Enspryng (satralizumab-mwge) (143,000)
It is indicated for the treatment of neuromyelitis optica spectrum disorder in adult patients who are anti–aquaporin-4 (AQP4) antibody positive. No information is available on the risks, if any, in pregnancy. No adverse effects on maternal or fetal development were observed in pregnant monkeys and their offspring.
Evrysdi (risdiplam) (401)
This is a prescription medicine used to treat spinal muscular atrophy in adults and children aged 2 months and older. In pregnant animals the drug caused adverse effects on fetal development.
Gemtesa (vibegron) (445)
Gemtesa is used in adults to treat the symptoms of overactive bladder. The drug had no adverse effects on pregnant animals.
Imcivree (setmelanotide) (1,117)
This drug is indicated for chronic weight management in adult and pediatric patients aged 6 years and older with obesity because of proopiomelanocortin, proprotein convertase subtilisin/kexin type 1, or leptin receptor deficiency. The drug was not embryo toxic in animals.
Isturisa (osilodrostat) (325)
Isturisa is a cortisol synthesis inhibitor indicated for the treatment of adult patients with Cushing’s disease. No adverse fetal effects were observed in pregnant animals.
Klisyri (tirbanibulin) (431)
Tirbanibulin ointment is a microtubule inhibitor that is used to treat actinic keratosis. Information on its effects in pregnancy is not available.
Koselugo (selumetinib) (556)
This is a kinase inhibitor indicated for the treatment of pediatric patients aged 2 years and older. The drug is toxic in pregnant animals but its effects in human pregnancy are not known.
Nexletol (bempedoic acid) (344)
Nexletol is indicated as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia or established atherosclerotic cardiovascular disease who require additional lowering of LDL cholesterol. The drug was not teratogenic in animals. Discontinue Nexletol when pregnancy is recognized unless the benefits of therapy outweigh the potential risks to the fetus.
Olinvyk (oliceridine) (503)
Olinvyk injection is indicated in adults for the management of acute pain severe enough to require an intravenous opioid analgesic. Prolonged use of Olinvyk during pregnancy can result in neonatal opioid withdrawal syndrome. The drug was not teratogenic in animals.
Ongentys (opicapone) (413)
Ongentys is indicated as adjunctive treatment to levodopa/carbidopa in patients with Parkinson’s disease experiencing “off” episodes. The drug was teratogenic in rabbits but not in rats.
Orladeyo (berotralstat) (635)
This drug is a plasma kallikrein inhibitor indicated for prophylaxis to prevent attacks of hereditary angioedema. It was not teratogenic in animals.
Oxlumo (lumasiran) (17,286)
Oxlumo is a HAO1-directed small interfering ribonucleic acid indicated for the treatment of primary hyperoxaluria type 1 to lower urinary oxalate levels. No adverse effects on pregnancy or embryo-fetal development related to the drug were observed in animals.
Pizensy (lactitol) (344)
Lactitol is minimally absorbed systemically following oral administration. It is unknown whether maternal use will result in fetal exposure to the drug. No effects on embryo-fetal development were observed in animals at doses much higher than the maximum recommended human dosage.
Rukobia (fostemsavir) (705; 584 for free acid)
This drug is an HIV-1–directed attachment inhibitor, in combination with other antiretrovirals. There is a pregnancy exposure registry that monitors pregnancy outcomes in individuals exposed to the drug during pregnancy. Health care providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry at 1-800-258-4263.
Sogroya (somapacitan-beco) (23,305)
This is a human growth hormone analog indicated for replacement of endogenous growth hormone in adults with growth hormone deficiency. The drug was not teratogenic in animals.
Tepezza (teprotumumab-trbw) (148,000)
Drug is indicated for the treatment of thyroid eye disease. The drug was teratogenic in cynomolgus monkeys. The manufacturer states that because of the risk, the drug should not be used in pregnancy.
Tauvid (flortaucipir F-18) (262)
This drug is indicated for use with PET imaging of the brain to evaluate for Alzheimer’s disease. It is a radioactive drug and should not be used in pregnant women.
Uplizna (inebilizumab-cdon) (149,000)
Uplizna is indicated for the treatment of neuromyelitis optica spectrum disorder in adult patients who are anti-AQP4 antibody positive. It is a humanized IgG1 monoclonal antibody and immunoglobulins are known to cross the placental barrier. Based on animal data, the drug can cause fetal harm because of B-cell lymphopenia and reduce antibody response in offspring exposed to the drug. Women of childbearing potential should use contraception while receiving Uplizna and for 6 months after the last dose.
Winlevi (clascoterone) (403)
This cream is an androgen receptor inhibitor that is indicated for the topical treatment of acne vulgaris in patients aged 12 years and older. Subcutaneous use in animals was associated with fetal defects.
Xeglyze (abametapir) (1,840)
Xeglyze is indicated for the topical treatment of head lice infestation in patients aged 6 months and older. The drug was not teratogenic in animals.
Zokinvy (lonafarnib) (639)
Zokinvy is indicated in patients 12 months or older to reduce the risk of mortality in several conditions. Animal studies have found embryo-fetal harm.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
In 2020, the Food and Drug Administration approved 53 new drugs for humans. One of these agents, Annovera (segesterone and ethinyl estradiol), is a vaginal ring to prevent pregnancy and is not relevant in this article. A second drug, Asparlas (calaspargase pegol), indicated to treat acute lymphoblastic leukemia, has not yet been released by its manufacturer. Orgovyx (relugolix) is used for prostate cancer and Lampit (nifurtimox) is drug used in children – neither of these two agents will be covered. The remaining 49 are covered below. The agents with molecular weights less than 1,000 probably cross the placenta in the first half of pregnancy, but nearly all, regardless of MW, will cross in the second half of pregnancy.
No human pregnancy data for these agents has been found, but there are five drugs included in pregnancy registries. It will take some time before the outcomes of these drugs are published. The routine absence of pregnancy data for most drugs was pointed out in an article that I coauthored, “Should pregnant women be included in phase 4 clinical drug trials?”. The article makes a strong argument for including some pregnant women in these trials.
Anti-infectives
Artesunate (384)
The drug appears low risk when used in the second and third trimesters. There is inadequate information regarding its use in the first trimester, so the safest course for the embryo appears to be avoiding its use during this period. A single intravenous dose given to rats early in gestation resulted in embryolethality.
Ebanga (ansuvimab) (147,000)
Studies on its use in pregnant animals have not been conducted.
Inmazeb (atoltivimab, maftivimab, odesivimab) (144,000-146,000)
Inmazeb is a combination of the three agents. Studies on its use in pregnant animals have not been conducted.
Veklury (remdesivir) (603)
Veklury is indicated for the treatment of pregnant women hospitalized with COVID-19 who are at risk for serious morbidity and mortality. The drug should be used during pregnancy only if the potential benefit justifies the potential risk for the mother and the fetus.
Antineoplastics
Ayvakit (avapritinib) (499)
The drug may cause fetal harm. The drug was teratogenic in animals.
Blenrep (belantamab mafodotin-blmf) (152,000)
A B-cell maturation antigen, it is indicated for the treatment of multiple myeloma. No human or animal pregnancy data have been located.
Danyelza (naxitamab-gqgk) (144,000)
This agent is used for the treatment of neuroblastoma. Based on its mechanism of action it may cause fetal harm if used in pregnancy.
Gavreto (pralsetinib) (534)
Gavreto is indicated for the treatment of small cell lung cancer. It may cause embryo-fetal harm if used in pregnancy.
Inqovi (cedazuridine + decitabine) (268,228)
The drug combination can cause fetal harm in human pregnancy. It is toxic in pregnant animals.
Margenza (margetuximab-cmkb) (149,000)
Although there are no data on the use of this drug in human pregnancy, the findings in animals and mechanism of action suggest that it will cause fetal harm.
Monjuvi (tafasitamab-cxix) (150,000)
This drug is a cytolytic antibody that is indicated in combination with lenalidomide. The combination may cause fetal harm.
Pemazyre (pemigatinib) (488)
It is indicated for the treatment of cholangiocarcinoma. In an animal study, the drug caused fetal defects, fetal growth retardation, and embryo-fetal death at maternal exposures lower than the human exposure.
Qinlock (ripretinib) (510)
This drug is used for the treatment of patients with advanced gastrointestinal stromal tumor. The drug was teratogenic in pregnant animals.
Retevmo (selpercatinib) (526)
This is a kinase inhibitor used for the treatment of small cell lung cancer. The drug is teratogenic in animals.
Sarclisa (isatuximab-irfc) (148,000)This drug is used in combination with pomalidomide and dexamethasone. The combination would probably cause major toxicity in an embryo or fetus.
Tabrecta (capmatinib) (412 – free base)Capmatinib is a kinase inhibitor used for the treatment of metastatic non–small cell lung cancer. It is teratogenic in animals.
Tazverik (tazemetostat) (654)Tazemetostat is indicated for the treatment of epithelioid sarcoma and follicular lymphoma, The drug is teratogenic in animals.
Trodelvy (sacituzumab govitecan-hziy) (1,602)This agent is used for the treatment of breast cancer. The drug has not been tested in pregnant animals. However, according to the manufacturer, there is a high possibility of human teratogenicity if it is given to a pregnant woman.
Tukysa (tucatinib) (481)
Tukysa is a tyrosine kinase inhibitor that is used in combination with trastuzumab and capecitabine for the treatment of breast cancer. The drug is teratogenic in animals.
Zeposia (ozanimod) (441)
Zeposia is indicated for the treatment of multiple sclerosis. The drug takes about 3 months to eliminate from the body. The drug is teratogenic in animals.
Zepzelca (lurbinectedin) (785)
This agent is used for the treatment of metastatic small cell lung cancer. The drug is teratogenic in animals.
Antiemetics
Barhemsys (amisulpride) (369)
This agent is Indicated to prevent nausea and vomiting. Animal data suggest low risk of embryo/fetal birth defects.
Antimigraine
Nurtec (rimegepant) (611)
Nurtec is indicated for acute treatment of migraine. Development toxicity was not observed in animals given doses similar to those used in humans.
Vyepti (eptinezumab-jjmr) (143,000)
A humanized monoclonal antibody that is given every 3 months to prevent migraine. There was no embryo-fetal harm in animals given the drug.
CNS
Byfavo (remimazolam) (493 – free base)
This drug is indicated for procedural sedation in adults undergoing procedures lasting 30 minutes or less. No defects were observed in animals.
Diagnostics
Cerianna (fluoroestradiol F 18) (289)
It is indicated for use with PET for characterization of estrogen receptor status in patients with ER-positive breast cancer. It has the potential to cause fetal harm depending on the fetal stage of development and the magnitude of radiation dose. There are no data on its use in pregnant women or animals.
Detectnet (copper CU-64 dotatate) (1,497)
All radiopharmaceuticals have the potential to cause fetal harm depending on the fetal stage of development and the magnitude of the radiation dose. There are no pregnancy data in humans or animals
Miscellaneous
Dojolvi (triheptanoin) (429)
This agent is indicated as a source of calories and fatty acids for the treatment of pediatric and adult patients with molecularly confirmed long-chain fatty acid oxidation disorders. Advise patients that there is a pregnancy safety study that collects pregnancy outcome data in women taking Dojolvi during pregnancy. Pregnant patients can enroll in the study by calling 1-888-756-8657.
Enspryng (satralizumab-mwge) (143,000)
It is indicated for the treatment of neuromyelitis optica spectrum disorder in adult patients who are anti–aquaporin-4 (AQP4) antibody positive. No information is available on the risks, if any, in pregnancy. No adverse effects on maternal or fetal development were observed in pregnant monkeys and their offspring.
Evrysdi (risdiplam) (401)
This is a prescription medicine used to treat spinal muscular atrophy in adults and children aged 2 months and older. In pregnant animals the drug caused adverse effects on fetal development.
Gemtesa (vibegron) (445)
Gemtesa is used in adults to treat the symptoms of overactive bladder. The drug had no adverse effects on pregnant animals.
Imcivree (setmelanotide) (1,117)
This drug is indicated for chronic weight management in adult and pediatric patients aged 6 years and older with obesity because of proopiomelanocortin, proprotein convertase subtilisin/kexin type 1, or leptin receptor deficiency. The drug was not embryo toxic in animals.
Isturisa (osilodrostat) (325)
Isturisa is a cortisol synthesis inhibitor indicated for the treatment of adult patients with Cushing’s disease. No adverse fetal effects were observed in pregnant animals.
Klisyri (tirbanibulin) (431)
Tirbanibulin ointment is a microtubule inhibitor that is used to treat actinic keratosis. Information on its effects in pregnancy is not available.
Koselugo (selumetinib) (556)
This is a kinase inhibitor indicated for the treatment of pediatric patients aged 2 years and older. The drug is toxic in pregnant animals but its effects in human pregnancy are not known.
Nexletol (bempedoic acid) (344)
Nexletol is indicated as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia or established atherosclerotic cardiovascular disease who require additional lowering of LDL cholesterol. The drug was not teratogenic in animals. Discontinue Nexletol when pregnancy is recognized unless the benefits of therapy outweigh the potential risks to the fetus.
Olinvyk (oliceridine) (503)
Olinvyk injection is indicated in adults for the management of acute pain severe enough to require an intravenous opioid analgesic. Prolonged use of Olinvyk during pregnancy can result in neonatal opioid withdrawal syndrome. The drug was not teratogenic in animals.
Ongentys (opicapone) (413)
Ongentys is indicated as adjunctive treatment to levodopa/carbidopa in patients with Parkinson’s disease experiencing “off” episodes. The drug was teratogenic in rabbits but not in rats.
Orladeyo (berotralstat) (635)
This drug is a plasma kallikrein inhibitor indicated for prophylaxis to prevent attacks of hereditary angioedema. It was not teratogenic in animals.
Oxlumo (lumasiran) (17,286)
Oxlumo is a HAO1-directed small interfering ribonucleic acid indicated for the treatment of primary hyperoxaluria type 1 to lower urinary oxalate levels. No adverse effects on pregnancy or embryo-fetal development related to the drug were observed in animals.
Pizensy (lactitol) (344)
Lactitol is minimally absorbed systemically following oral administration. It is unknown whether maternal use will result in fetal exposure to the drug. No effects on embryo-fetal development were observed in animals at doses much higher than the maximum recommended human dosage.
Rukobia (fostemsavir) (705; 584 for free acid)
This drug is an HIV-1–directed attachment inhibitor, in combination with other antiretrovirals. There is a pregnancy exposure registry that monitors pregnancy outcomes in individuals exposed to the drug during pregnancy. Health care providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry at 1-800-258-4263.
Sogroya (somapacitan-beco) (23,305)
This is a human growth hormone analog indicated for replacement of endogenous growth hormone in adults with growth hormone deficiency. The drug was not teratogenic in animals.
Tepezza (teprotumumab-trbw) (148,000)
Drug is indicated for the treatment of thyroid eye disease. The drug was teratogenic in cynomolgus monkeys. The manufacturer states that because of the risk, the drug should not be used in pregnancy.
Tauvid (flortaucipir F-18) (262)
This drug is indicated for use with PET imaging of the brain to evaluate for Alzheimer’s disease. It is a radioactive drug and should not be used in pregnant women.
Uplizna (inebilizumab-cdon) (149,000)
Uplizna is indicated for the treatment of neuromyelitis optica spectrum disorder in adult patients who are anti-AQP4 antibody positive. It is a humanized IgG1 monoclonal antibody and immunoglobulins are known to cross the placental barrier. Based on animal data, the drug can cause fetal harm because of B-cell lymphopenia and reduce antibody response in offspring exposed to the drug. Women of childbearing potential should use contraception while receiving Uplizna and for 6 months after the last dose.
Winlevi (clascoterone) (403)
This cream is an androgen receptor inhibitor that is indicated for the topical treatment of acne vulgaris in patients aged 12 years and older. Subcutaneous use in animals was associated with fetal defects.
Xeglyze (abametapir) (1,840)
Xeglyze is indicated for the topical treatment of head lice infestation in patients aged 6 months and older. The drug was not teratogenic in animals.
Zokinvy (lonafarnib) (639)
Zokinvy is indicated in patients 12 months or older to reduce the risk of mortality in several conditions. Animal studies have found embryo-fetal harm.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].