User login
For MD-IQ use only
ASTRO Pushes Return to Direct Supervision in RT: Needed or ‘Babysitting’?
Although serious errors during virtual supervision are rare, ASTRO said radiation treatments (RT) should be done with a radiation oncologist on site to ensure high-quality care. But some radiation oncologists do not agree with the proposal to move back to direct in-person supervision only.
Changes to Direct Supervision
Most radiation oncology treatments are delivered in an outpatient setting under a physician’s direction and control.
During the COVID-19 pandemic when social distancing mandates were in place, CMS temporarily changed the definition of “direct supervision” to include telehealth, specifying that a physician must be immediately available to assist and direct a procedure virtually using real-time audio and video. In other words, a physician did not need to be physically present in the room when the treatment was being performed.
CMS has extended this rule until the end of 2024 and is considering making it a permanent change. In the Calendar Year (CY) 2024 Medicare Physician Fee Schedule (PFS) Final Rule, CMS asked for comments on whether to extend the rule.
“We received input from interested parties on potential patient safety or quality concerns when direct supervision occurs virtually, which we will consider for future rulemaking,” a CMS spokesperson told this news organization. “CMS is currently considering the best approach that will protect patient access and safety as well as quality of care and program integrity concerns following CY 2024.”
CMS also noted its concerns that an abrupt transition back to requiring a physician’s physical presence could interrupt care from practitioners who have established new patterns of practice with telehealth.
What Are ASTRO’s Concerns?
Late last month, ASTRO sent CMS a letter, asking the agency to change the rules back to direct in-person supervision for all radiation services, citing that virtual supervision jeopardizes patient safety and quality of care.
Jeff Michalski, MD, MBA, chair of the ASTRO Board of Directors, said in an interview that radiation oncologists should be physically present to supervise the treatments.
“ASTRO is concerned that blanket policies of general or virtual supervision could lead to patients not having direct, in-person access to their doctors’ care,” he said. “While serious errors are rare, real-world experiences of radiation oncologists across practice settings demonstrate how an in-person radiation oncology physician is best suited to ensure high-quality care.”
What Do Radiation Oncologists Think?
According to ASTRO, most radiation oncologists would agree that in-person supervision is best for patients.
But that might not be the case.
Radiation oncologists took to X (formerly Twitter) to voice their opinions about ASTRO’s letter.
Jason Beckta, MD, PhD, of Rutland Regional’s Foley Cancer Center, Vermont, said “the February 26th ASTRO letter reads like an Onion article.”
“I’m struggling to understand the Luddite-level myopia around this topic,” he said in another tweet. “Virtual direct/outpatient general supervision has done nothing but boost my productivity and in particular, face-to-face patient contact.”
Join Y. Luh, MD, with the Providence Medical Network in Eureka, California, said he understands the challenges faced by clinicians working in more isolated rural settings. “For them, it’s either having virtual supervision or closing the center,” Dr. Luh said.
“Virtual care is definitely at my clinic and is not only an option but is critical to my patients who are 2+ snowy, mountainous hours away,” Dr. Luh wrote. “But I’m still in the clinic directly supervising treatments.”
Sidney Roberts, MD, with the CHI St. Luke’s Health-Memorial, Texas, tweeted that supervision does require some face-to-face care but contended that “babysitting trained therapists for every routine treatment is a farce.”
Another issue Dr. Luh brought up is reimbursement for virtual supervision, noting that “the elephant in the room is whether that level of service should be reimbursed at the same rate. Reimbursement has not changed — but will it stay that way?”
ASTRO has acknowledged that radiation oncologists will have varying opinions and says it is working to balance these challenges.
CMS has not reached a decision on whether the change will be implemented permanently. The organization will assess concern, patient safety, and quality of care at the end of the year.
A version of this article first appeared on Medscape.com
Although serious errors during virtual supervision are rare, ASTRO said radiation treatments (RT) should be done with a radiation oncologist on site to ensure high-quality care. But some radiation oncologists do not agree with the proposal to move back to direct in-person supervision only.
Changes to Direct Supervision
Most radiation oncology treatments are delivered in an outpatient setting under a physician’s direction and control.
During the COVID-19 pandemic when social distancing mandates were in place, CMS temporarily changed the definition of “direct supervision” to include telehealth, specifying that a physician must be immediately available to assist and direct a procedure virtually using real-time audio and video. In other words, a physician did not need to be physically present in the room when the treatment was being performed.
CMS has extended this rule until the end of 2024 and is considering making it a permanent change. In the Calendar Year (CY) 2024 Medicare Physician Fee Schedule (PFS) Final Rule, CMS asked for comments on whether to extend the rule.
“We received input from interested parties on potential patient safety or quality concerns when direct supervision occurs virtually, which we will consider for future rulemaking,” a CMS spokesperson told this news organization. “CMS is currently considering the best approach that will protect patient access and safety as well as quality of care and program integrity concerns following CY 2024.”
CMS also noted its concerns that an abrupt transition back to requiring a physician’s physical presence could interrupt care from practitioners who have established new patterns of practice with telehealth.
What Are ASTRO’s Concerns?
Late last month, ASTRO sent CMS a letter, asking the agency to change the rules back to direct in-person supervision for all radiation services, citing that virtual supervision jeopardizes patient safety and quality of care.
Jeff Michalski, MD, MBA, chair of the ASTRO Board of Directors, said in an interview that radiation oncologists should be physically present to supervise the treatments.
“ASTRO is concerned that blanket policies of general or virtual supervision could lead to patients not having direct, in-person access to their doctors’ care,” he said. “While serious errors are rare, real-world experiences of radiation oncologists across practice settings demonstrate how an in-person radiation oncology physician is best suited to ensure high-quality care.”
What Do Radiation Oncologists Think?
According to ASTRO, most radiation oncologists would agree that in-person supervision is best for patients.
But that might not be the case.
Radiation oncologists took to X (formerly Twitter) to voice their opinions about ASTRO’s letter.
Jason Beckta, MD, PhD, of Rutland Regional’s Foley Cancer Center, Vermont, said “the February 26th ASTRO letter reads like an Onion article.”
“I’m struggling to understand the Luddite-level myopia around this topic,” he said in another tweet. “Virtual direct/outpatient general supervision has done nothing but boost my productivity and in particular, face-to-face patient contact.”
Join Y. Luh, MD, with the Providence Medical Network in Eureka, California, said he understands the challenges faced by clinicians working in more isolated rural settings. “For them, it’s either having virtual supervision or closing the center,” Dr. Luh said.
“Virtual care is definitely at my clinic and is not only an option but is critical to my patients who are 2+ snowy, mountainous hours away,” Dr. Luh wrote. “But I’m still in the clinic directly supervising treatments.”
Sidney Roberts, MD, with the CHI St. Luke’s Health-Memorial, Texas, tweeted that supervision does require some face-to-face care but contended that “babysitting trained therapists for every routine treatment is a farce.”
Another issue Dr. Luh brought up is reimbursement for virtual supervision, noting that “the elephant in the room is whether that level of service should be reimbursed at the same rate. Reimbursement has not changed — but will it stay that way?”
ASTRO has acknowledged that radiation oncologists will have varying opinions and says it is working to balance these challenges.
CMS has not reached a decision on whether the change will be implemented permanently. The organization will assess concern, patient safety, and quality of care at the end of the year.
A version of this article first appeared on Medscape.com
Although serious errors during virtual supervision are rare, ASTRO said radiation treatments (RT) should be done with a radiation oncologist on site to ensure high-quality care. But some radiation oncologists do not agree with the proposal to move back to direct in-person supervision only.
Changes to Direct Supervision
Most radiation oncology treatments are delivered in an outpatient setting under a physician’s direction and control.
During the COVID-19 pandemic when social distancing mandates were in place, CMS temporarily changed the definition of “direct supervision” to include telehealth, specifying that a physician must be immediately available to assist and direct a procedure virtually using real-time audio and video. In other words, a physician did not need to be physically present in the room when the treatment was being performed.
CMS has extended this rule until the end of 2024 and is considering making it a permanent change. In the Calendar Year (CY) 2024 Medicare Physician Fee Schedule (PFS) Final Rule, CMS asked for comments on whether to extend the rule.
“We received input from interested parties on potential patient safety or quality concerns when direct supervision occurs virtually, which we will consider for future rulemaking,” a CMS spokesperson told this news organization. “CMS is currently considering the best approach that will protect patient access and safety as well as quality of care and program integrity concerns following CY 2024.”
CMS also noted its concerns that an abrupt transition back to requiring a physician’s physical presence could interrupt care from practitioners who have established new patterns of practice with telehealth.
What Are ASTRO’s Concerns?
Late last month, ASTRO sent CMS a letter, asking the agency to change the rules back to direct in-person supervision for all radiation services, citing that virtual supervision jeopardizes patient safety and quality of care.
Jeff Michalski, MD, MBA, chair of the ASTRO Board of Directors, said in an interview that radiation oncologists should be physically present to supervise the treatments.
“ASTRO is concerned that blanket policies of general or virtual supervision could lead to patients not having direct, in-person access to their doctors’ care,” he said. “While serious errors are rare, real-world experiences of radiation oncologists across practice settings demonstrate how an in-person radiation oncology physician is best suited to ensure high-quality care.”
What Do Radiation Oncologists Think?
According to ASTRO, most radiation oncologists would agree that in-person supervision is best for patients.
But that might not be the case.
Radiation oncologists took to X (formerly Twitter) to voice their opinions about ASTRO’s letter.
Jason Beckta, MD, PhD, of Rutland Regional’s Foley Cancer Center, Vermont, said “the February 26th ASTRO letter reads like an Onion article.”
“I’m struggling to understand the Luddite-level myopia around this topic,” he said in another tweet. “Virtual direct/outpatient general supervision has done nothing but boost my productivity and in particular, face-to-face patient contact.”
Join Y. Luh, MD, with the Providence Medical Network in Eureka, California, said he understands the challenges faced by clinicians working in more isolated rural settings. “For them, it’s either having virtual supervision or closing the center,” Dr. Luh said.
“Virtual care is definitely at my clinic and is not only an option but is critical to my patients who are 2+ snowy, mountainous hours away,” Dr. Luh wrote. “But I’m still in the clinic directly supervising treatments.”
Sidney Roberts, MD, with the CHI St. Luke’s Health-Memorial, Texas, tweeted that supervision does require some face-to-face care but contended that “babysitting trained therapists for every routine treatment is a farce.”
Another issue Dr. Luh brought up is reimbursement for virtual supervision, noting that “the elephant in the room is whether that level of service should be reimbursed at the same rate. Reimbursement has not changed — but will it stay that way?”
ASTRO has acknowledged that radiation oncologists will have varying opinions and says it is working to balance these challenges.
CMS has not reached a decision on whether the change will be implemented permanently. The organization will assess concern, patient safety, and quality of care at the end of the year.
A version of this article first appeared on Medscape.com
High Marks for New CAR T Toxicity Grading Tool
“Hematotoxicity after CAR T is common and clinically relevant, but it also remains poorly understood [with] a high degree of heterogeneity in terms of grading its clinical management,” said first author Kai Rejeski, MD, in presenting on the findings at the 6th European CAR T-cell Meeting, held in Spain and jointly sponsored by the European Society for Blood and Marrow Transplantation (EBMT) and the European Hematology Association (EHA).
“We hope that this novel grading system helps with this by enabling harmonized reporting using the same nomenclature and allowing the comparison of the expected incidence rates of grade 3 or higher [hematological toxicities] across several disease entities and CAR T products,” said Dr. Rejeski, of the Adult BMT (Blood Marrow Transplant) and Cellular Therapy Service, Memorial Sloan Kettering Cancer Center, New York City.
ICAHT Grading System
In a recent meta-analysis, Dr. Rejeski and his team found that infections are the cause of as many as 49% of non–relapse related deaths after CAR T-cell therapy, representing the most common cause of death and numbering significantly more than the more prominent causes of cytokine release syndrome (CRS) or immune effector cell–associated neurotoxicity (ICANS), which paradoxically have been the focus of significantly more research. In addition, the authors have reported substantial inconsistency among CAR T centers in the grading and management of the post–CAR T cytopenias that can cause those infections, underscoring the need for better guidelines.
“The narrative around CAR T toxicity has long centered on CRS and ICANS as novel and prototypical side effects with distinct management protocols,” Dr. Rejeski said in an interview. “However, it is cytopenias and the associated infections that drive nonrelapse mortality after CAR T.”
To address the need, the EHA and EBMT established the grading system for Immune Effector Cell–Associated HematoToxicity (ICAHT) that is applicable across disease types, indications, and treatment settings.
The details of the grading system were published in September 2023 in the journal Blood. The new system, which specifically focuses on neutrophil count and timing, importantly addresses the biphasic nature of ICAHT by distinguishing “early” ICAHT, occurring within 30 days of the CAR T administration, and “late” ICAHT, occurring more that 30 days following the treatment.
By contrast, conventional grading scales for CAR T–related cytopenias, such as the Common Terminology Criteria for Adverse Events (CTCAE) scale, “neither reflect the unique quality of post–CAR T neutrophil recovery, nor do they reflect the inherent risk of infections due to protracted neutropenia,” the authors report in the study.
Real-World Evaluation
To assess the ICAHT grading system’s relevance in a real-world clinical setting of CAR T-cell therapy recipients, Dr. Rejeski and colleagues conducted a multicenter observational study, published in January 2024 in Blood Advances.
The study involved 549 patients at 12 international CAR T centers treated with BCMA- or CD19- directed CAR T therapy for relapsed/refractory B-cell malignancies.
Of the patients, 112 were treated for multiple myeloma (MM), 334 for large B cell lymphoma (LBCL), and 103 for mantle cell lymphoma (MCL).
Using the grading system, grade 3 (severe) or 4 (life-threatening) ICAHT (n = 125), was found to be strongly associated with key factors including a cumulative duration of severe neutropenia (P < .0001), the presence of multilineage cytopenias, such as severe thrombocytopenia (90%, compared with 46% in nonsevere ICAHT) and severe anemia (92% vs 49%; both P < .001), as well as the use of platelet and red blood cell transfusions.
Grade 3 or higher ICAHT was more common in patients with MCL (28%), compared with LBCL (23%) and MM (15%).
Key factors at baseline that were independently associated with severe ICAHT after multivariate adjustment included the presence of bone marrow infiltration, increased serum LDH levels, elevated CAR-HEMATOTOX scores (all P < .001), and receipt of CD28z costimulatory domain products, including axi-cel or brexu-cel (P = .01).
Those with grade 3 or higher ICAHT scores had a significantly higher rate of severe infections, compared with lower ICAHT scores (49% vs 13%; P < .0001), as well as increased nonrelapse mortality (14% vs 4.5%; P < .0001), primarily attributable to fatal infections.
Survival outcomes were also worse with grade 3 or higher ICAHT, including significantly lower rates of 1-year progression-free survival (35% vs 51%) and 1-year overall survival (52% vs 73%; both P < .0001).
Grade 3 or higher ICAHT was also significantly associated with prolonged hospital stays (median 21 vs 16 days; P < .0001).
However, contrary to findings from some previous studies, the current study showed no association between ICAHT severity and the prior administration of autologous stem cell transplant.
The number of prior treatment lines was not associated with grade 3 or higher ICAHT. However, grade 3 or higher CRS was more common as a cotoxicity (15% vs 5% without severe ICAHT), as was severe ICANS (26% vs 13%; both P < .001).
Notably, ICAHT grading showed superiority in the prediction of severe infections, compared with CTCAE grading (c-index 0.73 vs 0.55, P < .0001 vs nonsignificant).
While mild to moderate toxicity after CAR T-cell therapy has been associated with more favorable outcomes, the poor survival rates associated with severe ICAHT “underscore that high-grade toxicity and inferior treatment outcomes often go hand-in-hand,” the authors write.
Conversely, “the patients with grade 1 or 2 ICAHT exhibited excellent treatment outcomes in our study,” they point out.
Recommendations in Clinical Practice
For clinical guidance, the ICAHT grading system provides best practice recommendations based on severity for diagnostic work-up and management, such as measures including use of granulocyte-colony stimulating factor (G-CSF), anti-infective prophylaxis and stem cell boosts.
The authors add that preinfusion scoring systems, including the CAR-HEMATOTOX prognostic score, may be optimized by ICAHT grading in terms of modeling for severe or life-threatening ICAHT as an important endpoint.
“We have had an absence of the standardized severity-based guidelines that we know very well for CRS and ICANS, both in terms of the diagnostic work-up and the grading but also the management,” Dr. Rejeski said at the meeting.
“We hope that the new ICAHT grading focuses future research efforts to not only understand this important side effect better, but also develop specific management strategies that mitigate the risk of infections in high-risk patients,” Dr. Rejeski added.
“The multiply validated CAR-HEMATOTOX score, assessed at time of lymphodepletion, may be helpful in this regard,” he added.
An accompanying editorial published with the guidelines underscored that “this is the first such guideline by a major organization and is a much-needed development for the management of this important CAR T-cell–associated toxicity.”
The improved standardized reporting of ICAHT “could also inform hematotoxicity management protocols,” said the editorial authors, David Qualls, MD, of the Memorial Sloan Kettering Cancer Center in New York City and Caron Jacobson, MD, of the Dana-Farber Cancer Institute, in Boston, Massachusetts.
“While providing comprehensive recommendations for ICAHT, the EHA/EBMT guidelines also highlight important gaps in our current knowledge of ICAHT, which are significant,” the editorial authors add.
Further commenting, Ulrich Jaeger, MD, a professor of hematology at the Medical University of Vienna, Vienna, Austria, agreed that the research fills an important need in post–CAR T-cell therapy management.
“Dr. Rejeski´s work is really seminal in the field and confirmed by validation cohorts in other centers,” he said in an interview. “I think the story is absolutely clear. It will be of increasing importance, with more patients surviving. [The system] will have to be adapted to novel indications as well.”
Dr. Rejeski disclosed ties with Kite/Gilead, Novartis, GMS/Celgene, and Pierre-Fabre. Jaeger reports relationships with Novartis, Gilead Sciences, Celgene/BMS, Janssen, Roche, Miltenyi Biotec, and Innovative Medicines Initiative.
“Hematotoxicity after CAR T is common and clinically relevant, but it also remains poorly understood [with] a high degree of heterogeneity in terms of grading its clinical management,” said first author Kai Rejeski, MD, in presenting on the findings at the 6th European CAR T-cell Meeting, held in Spain and jointly sponsored by the European Society for Blood and Marrow Transplantation (EBMT) and the European Hematology Association (EHA).
“We hope that this novel grading system helps with this by enabling harmonized reporting using the same nomenclature and allowing the comparison of the expected incidence rates of grade 3 or higher [hematological toxicities] across several disease entities and CAR T products,” said Dr. Rejeski, of the Adult BMT (Blood Marrow Transplant) and Cellular Therapy Service, Memorial Sloan Kettering Cancer Center, New York City.
ICAHT Grading System
In a recent meta-analysis, Dr. Rejeski and his team found that infections are the cause of as many as 49% of non–relapse related deaths after CAR T-cell therapy, representing the most common cause of death and numbering significantly more than the more prominent causes of cytokine release syndrome (CRS) or immune effector cell–associated neurotoxicity (ICANS), which paradoxically have been the focus of significantly more research. In addition, the authors have reported substantial inconsistency among CAR T centers in the grading and management of the post–CAR T cytopenias that can cause those infections, underscoring the need for better guidelines.
“The narrative around CAR T toxicity has long centered on CRS and ICANS as novel and prototypical side effects with distinct management protocols,” Dr. Rejeski said in an interview. “However, it is cytopenias and the associated infections that drive nonrelapse mortality after CAR T.”
To address the need, the EHA and EBMT established the grading system for Immune Effector Cell–Associated HematoToxicity (ICAHT) that is applicable across disease types, indications, and treatment settings.
The details of the grading system were published in September 2023 in the journal Blood. The new system, which specifically focuses on neutrophil count and timing, importantly addresses the biphasic nature of ICAHT by distinguishing “early” ICAHT, occurring within 30 days of the CAR T administration, and “late” ICAHT, occurring more that 30 days following the treatment.
By contrast, conventional grading scales for CAR T–related cytopenias, such as the Common Terminology Criteria for Adverse Events (CTCAE) scale, “neither reflect the unique quality of post–CAR T neutrophil recovery, nor do they reflect the inherent risk of infections due to protracted neutropenia,” the authors report in the study.
Real-World Evaluation
To assess the ICAHT grading system’s relevance in a real-world clinical setting of CAR T-cell therapy recipients, Dr. Rejeski and colleagues conducted a multicenter observational study, published in January 2024 in Blood Advances.
The study involved 549 patients at 12 international CAR T centers treated with BCMA- or CD19- directed CAR T therapy for relapsed/refractory B-cell malignancies.
Of the patients, 112 were treated for multiple myeloma (MM), 334 for large B cell lymphoma (LBCL), and 103 for mantle cell lymphoma (MCL).
Using the grading system, grade 3 (severe) or 4 (life-threatening) ICAHT (n = 125), was found to be strongly associated with key factors including a cumulative duration of severe neutropenia (P < .0001), the presence of multilineage cytopenias, such as severe thrombocytopenia (90%, compared with 46% in nonsevere ICAHT) and severe anemia (92% vs 49%; both P < .001), as well as the use of platelet and red blood cell transfusions.
Grade 3 or higher ICAHT was more common in patients with MCL (28%), compared with LBCL (23%) and MM (15%).
Key factors at baseline that were independently associated with severe ICAHT after multivariate adjustment included the presence of bone marrow infiltration, increased serum LDH levels, elevated CAR-HEMATOTOX scores (all P < .001), and receipt of CD28z costimulatory domain products, including axi-cel or brexu-cel (P = .01).
Those with grade 3 or higher ICAHT scores had a significantly higher rate of severe infections, compared with lower ICAHT scores (49% vs 13%; P < .0001), as well as increased nonrelapse mortality (14% vs 4.5%; P < .0001), primarily attributable to fatal infections.
Survival outcomes were also worse with grade 3 or higher ICAHT, including significantly lower rates of 1-year progression-free survival (35% vs 51%) and 1-year overall survival (52% vs 73%; both P < .0001).
Grade 3 or higher ICAHT was also significantly associated with prolonged hospital stays (median 21 vs 16 days; P < .0001).
However, contrary to findings from some previous studies, the current study showed no association between ICAHT severity and the prior administration of autologous stem cell transplant.
The number of prior treatment lines was not associated with grade 3 or higher ICAHT. However, grade 3 or higher CRS was more common as a cotoxicity (15% vs 5% without severe ICAHT), as was severe ICANS (26% vs 13%; both P < .001).
Notably, ICAHT grading showed superiority in the prediction of severe infections, compared with CTCAE grading (c-index 0.73 vs 0.55, P < .0001 vs nonsignificant).
While mild to moderate toxicity after CAR T-cell therapy has been associated with more favorable outcomes, the poor survival rates associated with severe ICAHT “underscore that high-grade toxicity and inferior treatment outcomes often go hand-in-hand,” the authors write.
Conversely, “the patients with grade 1 or 2 ICAHT exhibited excellent treatment outcomes in our study,” they point out.
Recommendations in Clinical Practice
For clinical guidance, the ICAHT grading system provides best practice recommendations based on severity for diagnostic work-up and management, such as measures including use of granulocyte-colony stimulating factor (G-CSF), anti-infective prophylaxis and stem cell boosts.
The authors add that preinfusion scoring systems, including the CAR-HEMATOTOX prognostic score, may be optimized by ICAHT grading in terms of modeling for severe or life-threatening ICAHT as an important endpoint.
“We have had an absence of the standardized severity-based guidelines that we know very well for CRS and ICANS, both in terms of the diagnostic work-up and the grading but also the management,” Dr. Rejeski said at the meeting.
“We hope that the new ICAHT grading focuses future research efforts to not only understand this important side effect better, but also develop specific management strategies that mitigate the risk of infections in high-risk patients,” Dr. Rejeski added.
“The multiply validated CAR-HEMATOTOX score, assessed at time of lymphodepletion, may be helpful in this regard,” he added.
An accompanying editorial published with the guidelines underscored that “this is the first such guideline by a major organization and is a much-needed development for the management of this important CAR T-cell–associated toxicity.”
The improved standardized reporting of ICAHT “could also inform hematotoxicity management protocols,” said the editorial authors, David Qualls, MD, of the Memorial Sloan Kettering Cancer Center in New York City and Caron Jacobson, MD, of the Dana-Farber Cancer Institute, in Boston, Massachusetts.
“While providing comprehensive recommendations for ICAHT, the EHA/EBMT guidelines also highlight important gaps in our current knowledge of ICAHT, which are significant,” the editorial authors add.
Further commenting, Ulrich Jaeger, MD, a professor of hematology at the Medical University of Vienna, Vienna, Austria, agreed that the research fills an important need in post–CAR T-cell therapy management.
“Dr. Rejeski´s work is really seminal in the field and confirmed by validation cohorts in other centers,” he said in an interview. “I think the story is absolutely clear. It will be of increasing importance, with more patients surviving. [The system] will have to be adapted to novel indications as well.”
Dr. Rejeski disclosed ties with Kite/Gilead, Novartis, GMS/Celgene, and Pierre-Fabre. Jaeger reports relationships with Novartis, Gilead Sciences, Celgene/BMS, Janssen, Roche, Miltenyi Biotec, and Innovative Medicines Initiative.
“Hematotoxicity after CAR T is common and clinically relevant, but it also remains poorly understood [with] a high degree of heterogeneity in terms of grading its clinical management,” said first author Kai Rejeski, MD, in presenting on the findings at the 6th European CAR T-cell Meeting, held in Spain and jointly sponsored by the European Society for Blood and Marrow Transplantation (EBMT) and the European Hematology Association (EHA).
“We hope that this novel grading system helps with this by enabling harmonized reporting using the same nomenclature and allowing the comparison of the expected incidence rates of grade 3 or higher [hematological toxicities] across several disease entities and CAR T products,” said Dr. Rejeski, of the Adult BMT (Blood Marrow Transplant) and Cellular Therapy Service, Memorial Sloan Kettering Cancer Center, New York City.
ICAHT Grading System
In a recent meta-analysis, Dr. Rejeski and his team found that infections are the cause of as many as 49% of non–relapse related deaths after CAR T-cell therapy, representing the most common cause of death and numbering significantly more than the more prominent causes of cytokine release syndrome (CRS) or immune effector cell–associated neurotoxicity (ICANS), which paradoxically have been the focus of significantly more research. In addition, the authors have reported substantial inconsistency among CAR T centers in the grading and management of the post–CAR T cytopenias that can cause those infections, underscoring the need for better guidelines.
“The narrative around CAR T toxicity has long centered on CRS and ICANS as novel and prototypical side effects with distinct management protocols,” Dr. Rejeski said in an interview. “However, it is cytopenias and the associated infections that drive nonrelapse mortality after CAR T.”
To address the need, the EHA and EBMT established the grading system for Immune Effector Cell–Associated HematoToxicity (ICAHT) that is applicable across disease types, indications, and treatment settings.
The details of the grading system were published in September 2023 in the journal Blood. The new system, which specifically focuses on neutrophil count and timing, importantly addresses the biphasic nature of ICAHT by distinguishing “early” ICAHT, occurring within 30 days of the CAR T administration, and “late” ICAHT, occurring more that 30 days following the treatment.
By contrast, conventional grading scales for CAR T–related cytopenias, such as the Common Terminology Criteria for Adverse Events (CTCAE) scale, “neither reflect the unique quality of post–CAR T neutrophil recovery, nor do they reflect the inherent risk of infections due to protracted neutropenia,” the authors report in the study.
Real-World Evaluation
To assess the ICAHT grading system’s relevance in a real-world clinical setting of CAR T-cell therapy recipients, Dr. Rejeski and colleagues conducted a multicenter observational study, published in January 2024 in Blood Advances.
The study involved 549 patients at 12 international CAR T centers treated with BCMA- or CD19- directed CAR T therapy for relapsed/refractory B-cell malignancies.
Of the patients, 112 were treated for multiple myeloma (MM), 334 for large B cell lymphoma (LBCL), and 103 for mantle cell lymphoma (MCL).
Using the grading system, grade 3 (severe) or 4 (life-threatening) ICAHT (n = 125), was found to be strongly associated with key factors including a cumulative duration of severe neutropenia (P < .0001), the presence of multilineage cytopenias, such as severe thrombocytopenia (90%, compared with 46% in nonsevere ICAHT) and severe anemia (92% vs 49%; both P < .001), as well as the use of platelet and red blood cell transfusions.
Grade 3 or higher ICAHT was more common in patients with MCL (28%), compared with LBCL (23%) and MM (15%).
Key factors at baseline that were independently associated with severe ICAHT after multivariate adjustment included the presence of bone marrow infiltration, increased serum LDH levels, elevated CAR-HEMATOTOX scores (all P < .001), and receipt of CD28z costimulatory domain products, including axi-cel or brexu-cel (P = .01).
Those with grade 3 or higher ICAHT scores had a significantly higher rate of severe infections, compared with lower ICAHT scores (49% vs 13%; P < .0001), as well as increased nonrelapse mortality (14% vs 4.5%; P < .0001), primarily attributable to fatal infections.
Survival outcomes were also worse with grade 3 or higher ICAHT, including significantly lower rates of 1-year progression-free survival (35% vs 51%) and 1-year overall survival (52% vs 73%; both P < .0001).
Grade 3 or higher ICAHT was also significantly associated with prolonged hospital stays (median 21 vs 16 days; P < .0001).
However, contrary to findings from some previous studies, the current study showed no association between ICAHT severity and the prior administration of autologous stem cell transplant.
The number of prior treatment lines was not associated with grade 3 or higher ICAHT. However, grade 3 or higher CRS was more common as a cotoxicity (15% vs 5% without severe ICAHT), as was severe ICANS (26% vs 13%; both P < .001).
Notably, ICAHT grading showed superiority in the prediction of severe infections, compared with CTCAE grading (c-index 0.73 vs 0.55, P < .0001 vs nonsignificant).
While mild to moderate toxicity after CAR T-cell therapy has been associated with more favorable outcomes, the poor survival rates associated with severe ICAHT “underscore that high-grade toxicity and inferior treatment outcomes often go hand-in-hand,” the authors write.
Conversely, “the patients with grade 1 or 2 ICAHT exhibited excellent treatment outcomes in our study,” they point out.
Recommendations in Clinical Practice
For clinical guidance, the ICAHT grading system provides best practice recommendations based on severity for diagnostic work-up and management, such as measures including use of granulocyte-colony stimulating factor (G-CSF), anti-infective prophylaxis and stem cell boosts.
The authors add that preinfusion scoring systems, including the CAR-HEMATOTOX prognostic score, may be optimized by ICAHT grading in terms of modeling for severe or life-threatening ICAHT as an important endpoint.
“We have had an absence of the standardized severity-based guidelines that we know very well for CRS and ICANS, both in terms of the diagnostic work-up and the grading but also the management,” Dr. Rejeski said at the meeting.
“We hope that the new ICAHT grading focuses future research efforts to not only understand this important side effect better, but also develop specific management strategies that mitigate the risk of infections in high-risk patients,” Dr. Rejeski added.
“The multiply validated CAR-HEMATOTOX score, assessed at time of lymphodepletion, may be helpful in this regard,” he added.
An accompanying editorial published with the guidelines underscored that “this is the first such guideline by a major organization and is a much-needed development for the management of this important CAR T-cell–associated toxicity.”
The improved standardized reporting of ICAHT “could also inform hematotoxicity management protocols,” said the editorial authors, David Qualls, MD, of the Memorial Sloan Kettering Cancer Center in New York City and Caron Jacobson, MD, of the Dana-Farber Cancer Institute, in Boston, Massachusetts.
“While providing comprehensive recommendations for ICAHT, the EHA/EBMT guidelines also highlight important gaps in our current knowledge of ICAHT, which are significant,” the editorial authors add.
Further commenting, Ulrich Jaeger, MD, a professor of hematology at the Medical University of Vienna, Vienna, Austria, agreed that the research fills an important need in post–CAR T-cell therapy management.
“Dr. Rejeski´s work is really seminal in the field and confirmed by validation cohorts in other centers,” he said in an interview. “I think the story is absolutely clear. It will be of increasing importance, with more patients surviving. [The system] will have to be adapted to novel indications as well.”
Dr. Rejeski disclosed ties with Kite/Gilead, Novartis, GMS/Celgene, and Pierre-Fabre. Jaeger reports relationships with Novartis, Gilead Sciences, Celgene/BMS, Janssen, Roche, Miltenyi Biotec, and Innovative Medicines Initiative.
FROM THE 6TH EUROPEAN CAR T-CELL MEETING
Does worsening metabolic syndrome increase the risk of developing cancer?
The conditions that comprise metabolic syndrome (high blood pressure, high blood sugar, increased abdominal adiposity, and high cholesterol and triglycerides) have been associated with an increased risk of diseases, including heart disease, stroke, and type 2 diabetes, wrote Li Deng, PhD, of Capital Medical University, Beijing, China, and colleagues.
A systematic review and meta-analysis published in Diabetes Care in 2012 showed an association between the presence of metabolic syndrome and an increased risk of various cancers including liver, bladder, pancreatic, breast, and colorectal.
More recently, a 2019 study published in Diabetes showed evidence of increased risk for certain cancers (pancreatic, kidney, uterine, cervical) but no increased risk for cancer overall.
However, the reasons for this association between metabolic syndrome and cancer remain unclear, and the effect of the fluctuating nature of metabolic syndrome over time on long-term cancer risk has not been explored, the researchers wrote.
What Does New Study Add to Other Research on Metabolic Syndrome and Cancer Risk?
In the new study, published in Cancer on March 11 (doi: 10.1002/cncr.35235), 44,115 adults in China were separated into four trajectories based on metabolic syndrome scores for the period from 2006 to 2010. The scores were based on clinical evidence of metabolic syndrome, defined using the International Diabetes Federation criteria of central obesity and the presence of at least two other factors including increased triglycerides, decreased HDL cholesterol, high blood pressure (or treatment for previously diagnosed hypertension), and increased fasting plasma glucose (or previous diagnosis of type 2 diabetes).
The average age of the participants was 49 years. The four trajectories of metabolic syndrome were low-stable (10.56% of participants), moderate-low (40.84%), moderate-high (41.46%), and elevated-increasing (7.14%), based on trends from the individuals’ initial physical exams on entering the study.
Over a median follow-up period of 9.4 years (from 2010 to 2021), 2,271 cancer diagnoses were reported in the study population. Those with an elevated-increasing metabolic syndrome trajectory had 1.3 times the risk of any cancer compared with those in the low-stable group. Risk for breast cancer, endometrial cancer, kidney cancer, colorectal cancer, and liver cancer in the highest trajectory group were 2.1, 3.3, 4.5, 2.5, and 1.6 times higher, respectively, compared to the lowest group. The increased risk in the elevated-trajectory group for all cancer types persisted when the low-stable, moderate-low, and moderate-high trajectory pattern groups were combined.
The researchers also examined the impact of chronic inflammation and found that individuals with persistently high metabolic syndrome scores and concurrent chronic inflammation had the highest risks of breast, endometrial, colon, and liver cancer. However, individuals with persistently high metabolic syndrome scores and no concurrent chronic inflammation had the highest risk of kidney cancer.
What Are the Limitations of This Research?
The researchers of the current study acknowledged the lack of information on other causes of cancer, including dietary habits, hepatitis C infection, and Helicobacter pylori infection. Other limitations include the focus only on individuals from a single community of mainly middle-aged men in China that may not generalize to other populations.
Also, the metabolic syndrome trajectories did not change much over time, which may be related to the short 4-year study period.
What Is the Takeaway Message for Clinical Practice?
The results suggest that monitoring and managing metabolic syndrome could help reduce cancer risk, the researchers concluded.
“This research suggests that proactive and continuous management of metabolic syndrome may serve as an essential strategy in preventing cancer,” senior author Han-Ping Shi, MD, PhD, of Capital Medical University in Beijing, said in a press release accompanying the study.
More research is needed to assess the impact of these interventions on cancer risk, he noted. However, the data from the current study can guide future research that may lead to more targeted treatments and more effective preventive strategies, he said in a statement.
The study was supported by the National Key Research and Development Program of China. The researchers had no financial conflicts to disclose.
The conditions that comprise metabolic syndrome (high blood pressure, high blood sugar, increased abdominal adiposity, and high cholesterol and triglycerides) have been associated with an increased risk of diseases, including heart disease, stroke, and type 2 diabetes, wrote Li Deng, PhD, of Capital Medical University, Beijing, China, and colleagues.
A systematic review and meta-analysis published in Diabetes Care in 2012 showed an association between the presence of metabolic syndrome and an increased risk of various cancers including liver, bladder, pancreatic, breast, and colorectal.
More recently, a 2019 study published in Diabetes showed evidence of increased risk for certain cancers (pancreatic, kidney, uterine, cervical) but no increased risk for cancer overall.
However, the reasons for this association between metabolic syndrome and cancer remain unclear, and the effect of the fluctuating nature of metabolic syndrome over time on long-term cancer risk has not been explored, the researchers wrote.
What Does New Study Add to Other Research on Metabolic Syndrome and Cancer Risk?
In the new study, published in Cancer on March 11 (doi: 10.1002/cncr.35235), 44,115 adults in China were separated into four trajectories based on metabolic syndrome scores for the period from 2006 to 2010. The scores were based on clinical evidence of metabolic syndrome, defined using the International Diabetes Federation criteria of central obesity and the presence of at least two other factors including increased triglycerides, decreased HDL cholesterol, high blood pressure (or treatment for previously diagnosed hypertension), and increased fasting plasma glucose (or previous diagnosis of type 2 diabetes).
The average age of the participants was 49 years. The four trajectories of metabolic syndrome were low-stable (10.56% of participants), moderate-low (40.84%), moderate-high (41.46%), and elevated-increasing (7.14%), based on trends from the individuals’ initial physical exams on entering the study.
Over a median follow-up period of 9.4 years (from 2010 to 2021), 2,271 cancer diagnoses were reported in the study population. Those with an elevated-increasing metabolic syndrome trajectory had 1.3 times the risk of any cancer compared with those in the low-stable group. Risk for breast cancer, endometrial cancer, kidney cancer, colorectal cancer, and liver cancer in the highest trajectory group were 2.1, 3.3, 4.5, 2.5, and 1.6 times higher, respectively, compared to the lowest group. The increased risk in the elevated-trajectory group for all cancer types persisted when the low-stable, moderate-low, and moderate-high trajectory pattern groups were combined.
The researchers also examined the impact of chronic inflammation and found that individuals with persistently high metabolic syndrome scores and concurrent chronic inflammation had the highest risks of breast, endometrial, colon, and liver cancer. However, individuals with persistently high metabolic syndrome scores and no concurrent chronic inflammation had the highest risk of kidney cancer.
What Are the Limitations of This Research?
The researchers of the current study acknowledged the lack of information on other causes of cancer, including dietary habits, hepatitis C infection, and Helicobacter pylori infection. Other limitations include the focus only on individuals from a single community of mainly middle-aged men in China that may not generalize to other populations.
Also, the metabolic syndrome trajectories did not change much over time, which may be related to the short 4-year study period.
What Is the Takeaway Message for Clinical Practice?
The results suggest that monitoring and managing metabolic syndrome could help reduce cancer risk, the researchers concluded.
“This research suggests that proactive and continuous management of metabolic syndrome may serve as an essential strategy in preventing cancer,” senior author Han-Ping Shi, MD, PhD, of Capital Medical University in Beijing, said in a press release accompanying the study.
More research is needed to assess the impact of these interventions on cancer risk, he noted. However, the data from the current study can guide future research that may lead to more targeted treatments and more effective preventive strategies, he said in a statement.
The study was supported by the National Key Research and Development Program of China. The researchers had no financial conflicts to disclose.
The conditions that comprise metabolic syndrome (high blood pressure, high blood sugar, increased abdominal adiposity, and high cholesterol and triglycerides) have been associated with an increased risk of diseases, including heart disease, stroke, and type 2 diabetes, wrote Li Deng, PhD, of Capital Medical University, Beijing, China, and colleagues.
A systematic review and meta-analysis published in Diabetes Care in 2012 showed an association between the presence of metabolic syndrome and an increased risk of various cancers including liver, bladder, pancreatic, breast, and colorectal.
More recently, a 2019 study published in Diabetes showed evidence of increased risk for certain cancers (pancreatic, kidney, uterine, cervical) but no increased risk for cancer overall.
However, the reasons for this association between metabolic syndrome and cancer remain unclear, and the effect of the fluctuating nature of metabolic syndrome over time on long-term cancer risk has not been explored, the researchers wrote.
What Does New Study Add to Other Research on Metabolic Syndrome and Cancer Risk?
In the new study, published in Cancer on March 11 (doi: 10.1002/cncr.35235), 44,115 adults in China were separated into four trajectories based on metabolic syndrome scores for the period from 2006 to 2010. The scores were based on clinical evidence of metabolic syndrome, defined using the International Diabetes Federation criteria of central obesity and the presence of at least two other factors including increased triglycerides, decreased HDL cholesterol, high blood pressure (or treatment for previously diagnosed hypertension), and increased fasting plasma glucose (or previous diagnosis of type 2 diabetes).
The average age of the participants was 49 years. The four trajectories of metabolic syndrome were low-stable (10.56% of participants), moderate-low (40.84%), moderate-high (41.46%), and elevated-increasing (7.14%), based on trends from the individuals’ initial physical exams on entering the study.
Over a median follow-up period of 9.4 years (from 2010 to 2021), 2,271 cancer diagnoses were reported in the study population. Those with an elevated-increasing metabolic syndrome trajectory had 1.3 times the risk of any cancer compared with those in the low-stable group. Risk for breast cancer, endometrial cancer, kidney cancer, colorectal cancer, and liver cancer in the highest trajectory group were 2.1, 3.3, 4.5, 2.5, and 1.6 times higher, respectively, compared to the lowest group. The increased risk in the elevated-trajectory group for all cancer types persisted when the low-stable, moderate-low, and moderate-high trajectory pattern groups were combined.
The researchers also examined the impact of chronic inflammation and found that individuals with persistently high metabolic syndrome scores and concurrent chronic inflammation had the highest risks of breast, endometrial, colon, and liver cancer. However, individuals with persistently high metabolic syndrome scores and no concurrent chronic inflammation had the highest risk of kidney cancer.
What Are the Limitations of This Research?
The researchers of the current study acknowledged the lack of information on other causes of cancer, including dietary habits, hepatitis C infection, and Helicobacter pylori infection. Other limitations include the focus only on individuals from a single community of mainly middle-aged men in China that may not generalize to other populations.
Also, the metabolic syndrome trajectories did not change much over time, which may be related to the short 4-year study period.
What Is the Takeaway Message for Clinical Practice?
The results suggest that monitoring and managing metabolic syndrome could help reduce cancer risk, the researchers concluded.
“This research suggests that proactive and continuous management of metabolic syndrome may serve as an essential strategy in preventing cancer,” senior author Han-Ping Shi, MD, PhD, of Capital Medical University in Beijing, said in a press release accompanying the study.
More research is needed to assess the impact of these interventions on cancer risk, he noted. However, the data from the current study can guide future research that may lead to more targeted treatments and more effective preventive strategies, he said in a statement.
The study was supported by the National Key Research and Development Program of China. The researchers had no financial conflicts to disclose.
FROM CANCER
Does Exercise Reduce Cancer Risk? It’s Just Not That Simple
“Exercise is medicine” has become something of a mantra, with good reason. There’s no doubt that regular physical activity has a broad range of health benefits. Exercise can improve circulation, help control weight, reduce stress, and boost mood — take your pick.
Lower cancer risk is also on the list — with exercise promoted as a risk-cutting strategy in government guidelines and in recommendations from professional groups such as the American Cancer Society.
The bulk of the data hangs on less rigorous, observational studies that have linked physical activity to lower risks for certain cancers, but plenty of questions remain.
What are the cancer types where exercise makes a difference? How significant is that impact? And what, exactly, defines a physical activity pattern powerful enough to move the needle on cancer risk?
Here’s an overview of the state of the evidence.
Exercise and Cancer Types: A Mixed Bag
When it comes to cancer prevention strategies, guidelines uniformly endorse less couch time and more movement. But a deeper look at the science reveals a complex and often poorly understood connection between exercise and cancer risk.
For certain cancer types, the benefits of exercise on cancer risk seem fairly well established.
The latest edition of the Physical Activity Guidelines for Americans, published in 2018, cites “strong evidence” that regular exercise might curb the risks for breast and colon cancers as well as bladder, endometrial, esophageal, kidney, and gastric cancers. These guidelines also point to “moderate”-strength evidence of a protective association with lung cancer.
The evidence of a protective effect, however, is strongest for breast and colon cancers, said Jennifer Ligibel, MD, senior physician in the Breast Oncology Center at Dana-Farber Cancer Institute, Boston, . “But,” she pointed out, “that may be because they’re some of the most common cancers, and it’s been easier to detect an association.”
Guidelines from the American Cancer Society, published in 2020, align with the 2018 recommendations.
“We believe there’s strong evidence to suggest at least eight different types of cancer are associated with physical activity,” said Erika Rees-Punia, PhD, MPH, senior principal scientist, epidemiology and behavioral research at the American Cancer Society.
That view is not universal, however. Current recommendations from the World Cancer Research Fund and American Institute for Cancer Research, for example, are more circumspect, citing only three cancers with good evidence of a protective effect from exercise: Breast (postmenopausal), colon, and endometrial.
“We definitely can’t say exercise reduces the risk of all cancers,” said Lee Jones, PhD, head of the Exercise Oncology Program at Memorial Sloan Kettering Cancer Center in New York City. “The data suggest it’s just not that simple.”
And it’s challenging to put all the evidence together, Dr. Jones added.
The physical activity guidelines are based on published systematic reviews, meta-analyses, and pooled analyses of data from observational studies that examined the relationship between physical activity — aerobic exercise, specifically — and cancer incidence. That means the evidence comes with all the limitations observational studies entail, such as how they collect information on participants’ exercise habits — which, Dr. Jones noted, is typically done via “monster questionnaires” that gauge physical activity in broad strokes.
Pooling all those findings into a meta-analysis is tricky, Dr. Jones added, because individual studies vary in important ways — from follow-up periods to how they quantify exercise and track cancer incidence.
In a study published in February in Cancer Cell, Dr. Jones and his colleagues attempted to address some of those issues by leveraging data from the PLCO screening trial.
The PLCO was a prospective study of over 60,000 US adults that compared the effects of annual screening vs usual care on cancer mortality. At enrollment, participants completed questionnaires that included an assessment of “vigorous” exercise. Based on that, Dr. Jones and his colleagues classified 55% as “exercisers” — meaning they reported 2 or more hours of vigorous exercise per week. The remaining 45%, who were in the 0 to 1 hour per week range, were deemed non-exercisers.
Over a median of 18 years, nearly 16,000 first-time invasive cancers were diagnosed, and some interesting differences between exercisers and non-exercisers emerged. The active group had lower risks for three cancers: Head and neck, with a 26% lower risk (hazard ratio [HR], 0.74), lung (a 20% lower risk), and breast (an 11% lower risk).
What was striking, however, was the lack of connection between exercise and many cancers cited in the guidelines, including colon, gastric, bladder, endometrial, and renal cancers.
Perhaps even more surprising — exercisers had higher risks for prostate cancer (12%) and melanoma (20%). This finding, Dr. Jones said, is in line with a previous pooled analysis of data from 12 US and European prospective cohorts. In this study, the most physically active participants (90th percentile) had higher risks for melanoma and prostate cancer, compared with the least active group (10th percentile).
The melanoma findings do make sense, Dr. Jones said, given that highly active people may spend a lot of time in the sun. “My advice,” Dr. Jones said, “is, if you’re exercising outside, wear sunscreen.” The prostate cancer findings, however, are more puzzling and warrant further research, he noted.
But the bottom line is that the relationship between exercise and cancer types is mixed and far from nailed down.
How Big Is the Effect?
Even if exercise reduces the risk for only certain cancers, that’s still important, particularly when those links appear strongest for common cancer types, such as breast and colon.
But how much of a difference can exercise make?
Based on the evidence, it may only be a modest one. A 2019 systematic review by the Physical Activity Guidelines Advisory Committee provided a rough estimate: Across hundreds of epidemiological studies, people with the highest physical activity levels had a 10%-20% lower risk for the cancers cited in the 2018 exercise guidelines compared with people who were least active.
These figures, however, are probably an underestimate, said Anne McTiernan, MD, PhD, a member of the advisory committee and professor of epidemiology, at Fred Hutchinson Cancer Center, Seattle.
“This is what we usually see when a factor is not measured very well,” said Dr. McTiernan, explaining that the individual studies differed in their categories of “highest” and “lowest” physical activity, such that one study’s “highest” could be another’s mid-range.
“In other words, the effects of physical activity are likely larger” than the review found, Dr. McTiernan said.
The next logical question is whether a bigger exercise “dose” — more time or higher intensity — would have a greater impact on cancer risk. A 2019 study published in the Journal of Clinical Oncology tried to clarify that by pooling data on over 750,000 participants from nine prospective cohorts.
Overall, people meeting government recommendations for exercise — equivalent to about 2.5-5 hours of weekly moderate activity, such as a brisk walk, or about 1.25-2.5 hours of more vigorous activities, like running — had lower risks for seven of 15 cancer types studied compared with less active people.
For cancers with positive findings, being on the higher end of the recommended 2.5- to 5-hour weekly range was better. Risk reductions for breast cancer, for instance, were 6% at 2.5 hours of physical activity per week and 10% at 5 hours per week. Similar trends emerged for other cancer types, including colon (8%-14%), endometrial (10%-18%), liver cancer (18%-27%), and non-Hodgkin lymphoma in women (11%-18%).
But there may be an exercise sweet spot that maximizes the cancer risk benefit.
Among people who surpassed the recommendations — exercising for more time or more intensely — the risk reduction benefit did not necessarily improve in a linear fashion. For certain cancer types, such as colon and endometrial, the benefits of more vigorous exercise “eroded at higher levels of activity,” the authors said.
The issue here is that most studies have not dug deeply into aerobic exercise habits. Often, studies present participants with a list of activities — walking, biking, and running — and ask them to estimate how often and for what duration they do each.
Plus, “we’ve usually lumped moderate and vigorous activities together,” Dr. Rees-Punia said, which means there’s a lack of “granular data” to say whether certain intensities or frequencies of exercise are optimal and for whom.
Why Exercise May Lower Cancer Risk
Exercise habits do not, of course, exist in a vacuum. Highly active people, Dr. Ligibel said, tend to be of higher socioeconomic status, leaner, and have generally healthier lifestyles than sedentary people.
Body weight is a big confounder as well. However, Dr. Rees-Punia noted, it’s also probably a reason that exercise is linked to lower cancer risks, particularly by preventing weight gain. Still, studies have found that the association between exercise and many cancers remains significant after adjusting for body mass index.
The why remains unclear, though some studies offer clues.
“There’s been some really interesting mechanistic research, suggesting that exercise may help inhibit tumor growth or upregulate the immune system,” Dr. Ligibel said.
That includes not only lab research but small intervention studies. While these studies have largely involved people who already have cancer, some have also focused on healthy individuals.
A 2019 study from Dr. Ligibel and her colleagues, which randomly assigned 49 women newly diagnosed with breast cancer to start either an exercise program or mind-body practices ahead of surgery, found exercisers, who had been active for about a month at the time of surgery, showed signs of immune system upregulation in their tumors, while the control group did not.
Among healthy postmenopausal women, a meta-analysis of six clinical trials from Dr. McTiernan and her colleagues found that exercise plus calorie reduction can reduce levels of breast cancer-related endogenous hormones, more so than calorie-cutting alone. And a 2023 study found that high-intensity exercise boosted the ranks of certain immune cells and reduced inflammation in the colon among people at high risk for colon and endometrial cancers due to Lynch syndrome.
Defining an Exercise ‘Prescription’
Despite the gaps and uncertainties in the research, government guidelines as well as those from the American Cancer Society and other medical groups are in lockstep in their exercise recommendations: Adults should strive for 150-300 minutes of moderate-intensity aerobic exercise (like brisk walking), 75-150 minutes of vigorous activity (like running), or some combination each week.
The guidelines also encourage strength training twice a week — advice that’s based on research tying those activity levels to lower risks for heart disease, diabetes, and other chronic conditions.
But there’s no “best” exercise prescription for lowering cancer risk specifically. Most epidemiological studies have examined only aerobic activity, Dr. Rees-Punia said, and there’s very little known about whether strength conditioning or other moderate heart rate-elevating activities, such as daily household chores, may reduce the risk for cancer.
Given the lack of nuance in the literature, it’s hard to say what intensities, types, or amounts of exercise are best for each individual.
Going forward, device-based measurements of physical activity could “help us sort out the effects of different intensities of exercise and possibly types,” Dr. Rees-Punia said.
But overall, Dr. McTiernan said, the data do show that the risks for several cancers are lower at the widely recommended activity levels.
“The bottom-line advice is still to exercise at least 150 minutes per week at a moderate-intensity level or greater,” Dr. McTiernan said.
Or put another way, moving beats being sedentary. It’s probably wise for everyone to sit less, noted Dr. Rees-Punia, for overall health and based on evidence tying sedentary time to the risks for certain cancers, including colon, endometrial, and lung.
There’s a practical element to consider in all of this: What physical activities will people actually do on the regular? In the big epidemiological studies, Dr. McTiernan noted, middle-aged and older adults most often report walking, suggesting that’s the preferred, or most accessible activity, for many.
“You can only benefit from the physical activity you’ll actually do,” Dr. Rees-Punia said.
Dr. Ligibel echoed that sentiment, saying she encourages patients to think about physical activity as a process: “You need to find things you like to do and work them into your daily life, in a sustainable way.
“People often talk about exercise being medicine,” Dr. Ligibel said. “But I think you could take that too far. If we get too prescriptive about it, that could take the joy away.”
A version of this article appeared on Medscape.com.
“Exercise is medicine” has become something of a mantra, with good reason. There’s no doubt that regular physical activity has a broad range of health benefits. Exercise can improve circulation, help control weight, reduce stress, and boost mood — take your pick.
Lower cancer risk is also on the list — with exercise promoted as a risk-cutting strategy in government guidelines and in recommendations from professional groups such as the American Cancer Society.
The bulk of the data hangs on less rigorous, observational studies that have linked physical activity to lower risks for certain cancers, but plenty of questions remain.
What are the cancer types where exercise makes a difference? How significant is that impact? And what, exactly, defines a physical activity pattern powerful enough to move the needle on cancer risk?
Here’s an overview of the state of the evidence.
Exercise and Cancer Types: A Mixed Bag
When it comes to cancer prevention strategies, guidelines uniformly endorse less couch time and more movement. But a deeper look at the science reveals a complex and often poorly understood connection between exercise and cancer risk.
For certain cancer types, the benefits of exercise on cancer risk seem fairly well established.
The latest edition of the Physical Activity Guidelines for Americans, published in 2018, cites “strong evidence” that regular exercise might curb the risks for breast and colon cancers as well as bladder, endometrial, esophageal, kidney, and gastric cancers. These guidelines also point to “moderate”-strength evidence of a protective association with lung cancer.
The evidence of a protective effect, however, is strongest for breast and colon cancers, said Jennifer Ligibel, MD, senior physician in the Breast Oncology Center at Dana-Farber Cancer Institute, Boston, . “But,” she pointed out, “that may be because they’re some of the most common cancers, and it’s been easier to detect an association.”
Guidelines from the American Cancer Society, published in 2020, align with the 2018 recommendations.
“We believe there’s strong evidence to suggest at least eight different types of cancer are associated with physical activity,” said Erika Rees-Punia, PhD, MPH, senior principal scientist, epidemiology and behavioral research at the American Cancer Society.
That view is not universal, however. Current recommendations from the World Cancer Research Fund and American Institute for Cancer Research, for example, are more circumspect, citing only three cancers with good evidence of a protective effect from exercise: Breast (postmenopausal), colon, and endometrial.
“We definitely can’t say exercise reduces the risk of all cancers,” said Lee Jones, PhD, head of the Exercise Oncology Program at Memorial Sloan Kettering Cancer Center in New York City. “The data suggest it’s just not that simple.”
And it’s challenging to put all the evidence together, Dr. Jones added.
The physical activity guidelines are based on published systematic reviews, meta-analyses, and pooled analyses of data from observational studies that examined the relationship between physical activity — aerobic exercise, specifically — and cancer incidence. That means the evidence comes with all the limitations observational studies entail, such as how they collect information on participants’ exercise habits — which, Dr. Jones noted, is typically done via “monster questionnaires” that gauge physical activity in broad strokes.
Pooling all those findings into a meta-analysis is tricky, Dr. Jones added, because individual studies vary in important ways — from follow-up periods to how they quantify exercise and track cancer incidence.
In a study published in February in Cancer Cell, Dr. Jones and his colleagues attempted to address some of those issues by leveraging data from the PLCO screening trial.
The PLCO was a prospective study of over 60,000 US adults that compared the effects of annual screening vs usual care on cancer mortality. At enrollment, participants completed questionnaires that included an assessment of “vigorous” exercise. Based on that, Dr. Jones and his colleagues classified 55% as “exercisers” — meaning they reported 2 or more hours of vigorous exercise per week. The remaining 45%, who were in the 0 to 1 hour per week range, were deemed non-exercisers.
Over a median of 18 years, nearly 16,000 first-time invasive cancers were diagnosed, and some interesting differences between exercisers and non-exercisers emerged. The active group had lower risks for three cancers: Head and neck, with a 26% lower risk (hazard ratio [HR], 0.74), lung (a 20% lower risk), and breast (an 11% lower risk).
What was striking, however, was the lack of connection between exercise and many cancers cited in the guidelines, including colon, gastric, bladder, endometrial, and renal cancers.
Perhaps even more surprising — exercisers had higher risks for prostate cancer (12%) and melanoma (20%). This finding, Dr. Jones said, is in line with a previous pooled analysis of data from 12 US and European prospective cohorts. In this study, the most physically active participants (90th percentile) had higher risks for melanoma and prostate cancer, compared with the least active group (10th percentile).
The melanoma findings do make sense, Dr. Jones said, given that highly active people may spend a lot of time in the sun. “My advice,” Dr. Jones said, “is, if you’re exercising outside, wear sunscreen.” The prostate cancer findings, however, are more puzzling and warrant further research, he noted.
But the bottom line is that the relationship between exercise and cancer types is mixed and far from nailed down.
How Big Is the Effect?
Even if exercise reduces the risk for only certain cancers, that’s still important, particularly when those links appear strongest for common cancer types, such as breast and colon.
But how much of a difference can exercise make?
Based on the evidence, it may only be a modest one. A 2019 systematic review by the Physical Activity Guidelines Advisory Committee provided a rough estimate: Across hundreds of epidemiological studies, people with the highest physical activity levels had a 10%-20% lower risk for the cancers cited in the 2018 exercise guidelines compared with people who were least active.
These figures, however, are probably an underestimate, said Anne McTiernan, MD, PhD, a member of the advisory committee and professor of epidemiology, at Fred Hutchinson Cancer Center, Seattle.
“This is what we usually see when a factor is not measured very well,” said Dr. McTiernan, explaining that the individual studies differed in their categories of “highest” and “lowest” physical activity, such that one study’s “highest” could be another’s mid-range.
“In other words, the effects of physical activity are likely larger” than the review found, Dr. McTiernan said.
The next logical question is whether a bigger exercise “dose” — more time or higher intensity — would have a greater impact on cancer risk. A 2019 study published in the Journal of Clinical Oncology tried to clarify that by pooling data on over 750,000 participants from nine prospective cohorts.
Overall, people meeting government recommendations for exercise — equivalent to about 2.5-5 hours of weekly moderate activity, such as a brisk walk, or about 1.25-2.5 hours of more vigorous activities, like running — had lower risks for seven of 15 cancer types studied compared with less active people.
For cancers with positive findings, being on the higher end of the recommended 2.5- to 5-hour weekly range was better. Risk reductions for breast cancer, for instance, were 6% at 2.5 hours of physical activity per week and 10% at 5 hours per week. Similar trends emerged for other cancer types, including colon (8%-14%), endometrial (10%-18%), liver cancer (18%-27%), and non-Hodgkin lymphoma in women (11%-18%).
But there may be an exercise sweet spot that maximizes the cancer risk benefit.
Among people who surpassed the recommendations — exercising for more time or more intensely — the risk reduction benefit did not necessarily improve in a linear fashion. For certain cancer types, such as colon and endometrial, the benefits of more vigorous exercise “eroded at higher levels of activity,” the authors said.
The issue here is that most studies have not dug deeply into aerobic exercise habits. Often, studies present participants with a list of activities — walking, biking, and running — and ask them to estimate how often and for what duration they do each.
Plus, “we’ve usually lumped moderate and vigorous activities together,” Dr. Rees-Punia said, which means there’s a lack of “granular data” to say whether certain intensities or frequencies of exercise are optimal and for whom.
Why Exercise May Lower Cancer Risk
Exercise habits do not, of course, exist in a vacuum. Highly active people, Dr. Ligibel said, tend to be of higher socioeconomic status, leaner, and have generally healthier lifestyles than sedentary people.
Body weight is a big confounder as well. However, Dr. Rees-Punia noted, it’s also probably a reason that exercise is linked to lower cancer risks, particularly by preventing weight gain. Still, studies have found that the association between exercise and many cancers remains significant after adjusting for body mass index.
The why remains unclear, though some studies offer clues.
“There’s been some really interesting mechanistic research, suggesting that exercise may help inhibit tumor growth or upregulate the immune system,” Dr. Ligibel said.
That includes not only lab research but small intervention studies. While these studies have largely involved people who already have cancer, some have also focused on healthy individuals.
A 2019 study from Dr. Ligibel and her colleagues, which randomly assigned 49 women newly diagnosed with breast cancer to start either an exercise program or mind-body practices ahead of surgery, found exercisers, who had been active for about a month at the time of surgery, showed signs of immune system upregulation in their tumors, while the control group did not.
Among healthy postmenopausal women, a meta-analysis of six clinical trials from Dr. McTiernan and her colleagues found that exercise plus calorie reduction can reduce levels of breast cancer-related endogenous hormones, more so than calorie-cutting alone. And a 2023 study found that high-intensity exercise boosted the ranks of certain immune cells and reduced inflammation in the colon among people at high risk for colon and endometrial cancers due to Lynch syndrome.
Defining an Exercise ‘Prescription’
Despite the gaps and uncertainties in the research, government guidelines as well as those from the American Cancer Society and other medical groups are in lockstep in their exercise recommendations: Adults should strive for 150-300 minutes of moderate-intensity aerobic exercise (like brisk walking), 75-150 minutes of vigorous activity (like running), or some combination each week.
The guidelines also encourage strength training twice a week — advice that’s based on research tying those activity levels to lower risks for heart disease, diabetes, and other chronic conditions.
But there’s no “best” exercise prescription for lowering cancer risk specifically. Most epidemiological studies have examined only aerobic activity, Dr. Rees-Punia said, and there’s very little known about whether strength conditioning or other moderate heart rate-elevating activities, such as daily household chores, may reduce the risk for cancer.
Given the lack of nuance in the literature, it’s hard to say what intensities, types, or amounts of exercise are best for each individual.
Going forward, device-based measurements of physical activity could “help us sort out the effects of different intensities of exercise and possibly types,” Dr. Rees-Punia said.
But overall, Dr. McTiernan said, the data do show that the risks for several cancers are lower at the widely recommended activity levels.
“The bottom-line advice is still to exercise at least 150 minutes per week at a moderate-intensity level or greater,” Dr. McTiernan said.
Or put another way, moving beats being sedentary. It’s probably wise for everyone to sit less, noted Dr. Rees-Punia, for overall health and based on evidence tying sedentary time to the risks for certain cancers, including colon, endometrial, and lung.
There’s a practical element to consider in all of this: What physical activities will people actually do on the regular? In the big epidemiological studies, Dr. McTiernan noted, middle-aged and older adults most often report walking, suggesting that’s the preferred, or most accessible activity, for many.
“You can only benefit from the physical activity you’ll actually do,” Dr. Rees-Punia said.
Dr. Ligibel echoed that sentiment, saying she encourages patients to think about physical activity as a process: “You need to find things you like to do and work them into your daily life, in a sustainable way.
“People often talk about exercise being medicine,” Dr. Ligibel said. “But I think you could take that too far. If we get too prescriptive about it, that could take the joy away.”
A version of this article appeared on Medscape.com.
“Exercise is medicine” has become something of a mantra, with good reason. There’s no doubt that regular physical activity has a broad range of health benefits. Exercise can improve circulation, help control weight, reduce stress, and boost mood — take your pick.
Lower cancer risk is also on the list — with exercise promoted as a risk-cutting strategy in government guidelines and in recommendations from professional groups such as the American Cancer Society.
The bulk of the data hangs on less rigorous, observational studies that have linked physical activity to lower risks for certain cancers, but plenty of questions remain.
What are the cancer types where exercise makes a difference? How significant is that impact? And what, exactly, defines a physical activity pattern powerful enough to move the needle on cancer risk?
Here’s an overview of the state of the evidence.
Exercise and Cancer Types: A Mixed Bag
When it comes to cancer prevention strategies, guidelines uniformly endorse less couch time and more movement. But a deeper look at the science reveals a complex and often poorly understood connection between exercise and cancer risk.
For certain cancer types, the benefits of exercise on cancer risk seem fairly well established.
The latest edition of the Physical Activity Guidelines for Americans, published in 2018, cites “strong evidence” that regular exercise might curb the risks for breast and colon cancers as well as bladder, endometrial, esophageal, kidney, and gastric cancers. These guidelines also point to “moderate”-strength evidence of a protective association with lung cancer.
The evidence of a protective effect, however, is strongest for breast and colon cancers, said Jennifer Ligibel, MD, senior physician in the Breast Oncology Center at Dana-Farber Cancer Institute, Boston, . “But,” she pointed out, “that may be because they’re some of the most common cancers, and it’s been easier to detect an association.”
Guidelines from the American Cancer Society, published in 2020, align with the 2018 recommendations.
“We believe there’s strong evidence to suggest at least eight different types of cancer are associated with physical activity,” said Erika Rees-Punia, PhD, MPH, senior principal scientist, epidemiology and behavioral research at the American Cancer Society.
That view is not universal, however. Current recommendations from the World Cancer Research Fund and American Institute for Cancer Research, for example, are more circumspect, citing only three cancers with good evidence of a protective effect from exercise: Breast (postmenopausal), colon, and endometrial.
“We definitely can’t say exercise reduces the risk of all cancers,” said Lee Jones, PhD, head of the Exercise Oncology Program at Memorial Sloan Kettering Cancer Center in New York City. “The data suggest it’s just not that simple.”
And it’s challenging to put all the evidence together, Dr. Jones added.
The physical activity guidelines are based on published systematic reviews, meta-analyses, and pooled analyses of data from observational studies that examined the relationship between physical activity — aerobic exercise, specifically — and cancer incidence. That means the evidence comes with all the limitations observational studies entail, such as how they collect information on participants’ exercise habits — which, Dr. Jones noted, is typically done via “monster questionnaires” that gauge physical activity in broad strokes.
Pooling all those findings into a meta-analysis is tricky, Dr. Jones added, because individual studies vary in important ways — from follow-up periods to how they quantify exercise and track cancer incidence.
In a study published in February in Cancer Cell, Dr. Jones and his colleagues attempted to address some of those issues by leveraging data from the PLCO screening trial.
The PLCO was a prospective study of over 60,000 US adults that compared the effects of annual screening vs usual care on cancer mortality. At enrollment, participants completed questionnaires that included an assessment of “vigorous” exercise. Based on that, Dr. Jones and his colleagues classified 55% as “exercisers” — meaning they reported 2 or more hours of vigorous exercise per week. The remaining 45%, who were in the 0 to 1 hour per week range, were deemed non-exercisers.
Over a median of 18 years, nearly 16,000 first-time invasive cancers were diagnosed, and some interesting differences between exercisers and non-exercisers emerged. The active group had lower risks for three cancers: Head and neck, with a 26% lower risk (hazard ratio [HR], 0.74), lung (a 20% lower risk), and breast (an 11% lower risk).
What was striking, however, was the lack of connection between exercise and many cancers cited in the guidelines, including colon, gastric, bladder, endometrial, and renal cancers.
Perhaps even more surprising — exercisers had higher risks for prostate cancer (12%) and melanoma (20%). This finding, Dr. Jones said, is in line with a previous pooled analysis of data from 12 US and European prospective cohorts. In this study, the most physically active participants (90th percentile) had higher risks for melanoma and prostate cancer, compared with the least active group (10th percentile).
The melanoma findings do make sense, Dr. Jones said, given that highly active people may spend a lot of time in the sun. “My advice,” Dr. Jones said, “is, if you’re exercising outside, wear sunscreen.” The prostate cancer findings, however, are more puzzling and warrant further research, he noted.
But the bottom line is that the relationship between exercise and cancer types is mixed and far from nailed down.
How Big Is the Effect?
Even if exercise reduces the risk for only certain cancers, that’s still important, particularly when those links appear strongest for common cancer types, such as breast and colon.
But how much of a difference can exercise make?
Based on the evidence, it may only be a modest one. A 2019 systematic review by the Physical Activity Guidelines Advisory Committee provided a rough estimate: Across hundreds of epidemiological studies, people with the highest physical activity levels had a 10%-20% lower risk for the cancers cited in the 2018 exercise guidelines compared with people who were least active.
These figures, however, are probably an underestimate, said Anne McTiernan, MD, PhD, a member of the advisory committee and professor of epidemiology, at Fred Hutchinson Cancer Center, Seattle.
“This is what we usually see when a factor is not measured very well,” said Dr. McTiernan, explaining that the individual studies differed in their categories of “highest” and “lowest” physical activity, such that one study’s “highest” could be another’s mid-range.
“In other words, the effects of physical activity are likely larger” than the review found, Dr. McTiernan said.
The next logical question is whether a bigger exercise “dose” — more time or higher intensity — would have a greater impact on cancer risk. A 2019 study published in the Journal of Clinical Oncology tried to clarify that by pooling data on over 750,000 participants from nine prospective cohorts.
Overall, people meeting government recommendations for exercise — equivalent to about 2.5-5 hours of weekly moderate activity, such as a brisk walk, or about 1.25-2.5 hours of more vigorous activities, like running — had lower risks for seven of 15 cancer types studied compared with less active people.
For cancers with positive findings, being on the higher end of the recommended 2.5- to 5-hour weekly range was better. Risk reductions for breast cancer, for instance, were 6% at 2.5 hours of physical activity per week and 10% at 5 hours per week. Similar trends emerged for other cancer types, including colon (8%-14%), endometrial (10%-18%), liver cancer (18%-27%), and non-Hodgkin lymphoma in women (11%-18%).
But there may be an exercise sweet spot that maximizes the cancer risk benefit.
Among people who surpassed the recommendations — exercising for more time or more intensely — the risk reduction benefit did not necessarily improve in a linear fashion. For certain cancer types, such as colon and endometrial, the benefits of more vigorous exercise “eroded at higher levels of activity,” the authors said.
The issue here is that most studies have not dug deeply into aerobic exercise habits. Often, studies present participants with a list of activities — walking, biking, and running — and ask them to estimate how often and for what duration they do each.
Plus, “we’ve usually lumped moderate and vigorous activities together,” Dr. Rees-Punia said, which means there’s a lack of “granular data” to say whether certain intensities or frequencies of exercise are optimal and for whom.
Why Exercise May Lower Cancer Risk
Exercise habits do not, of course, exist in a vacuum. Highly active people, Dr. Ligibel said, tend to be of higher socioeconomic status, leaner, and have generally healthier lifestyles than sedentary people.
Body weight is a big confounder as well. However, Dr. Rees-Punia noted, it’s also probably a reason that exercise is linked to lower cancer risks, particularly by preventing weight gain. Still, studies have found that the association between exercise and many cancers remains significant after adjusting for body mass index.
The why remains unclear, though some studies offer clues.
“There’s been some really interesting mechanistic research, suggesting that exercise may help inhibit tumor growth or upregulate the immune system,” Dr. Ligibel said.
That includes not only lab research but small intervention studies. While these studies have largely involved people who already have cancer, some have also focused on healthy individuals.
A 2019 study from Dr. Ligibel and her colleagues, which randomly assigned 49 women newly diagnosed with breast cancer to start either an exercise program or mind-body practices ahead of surgery, found exercisers, who had been active for about a month at the time of surgery, showed signs of immune system upregulation in their tumors, while the control group did not.
Among healthy postmenopausal women, a meta-analysis of six clinical trials from Dr. McTiernan and her colleagues found that exercise plus calorie reduction can reduce levels of breast cancer-related endogenous hormones, more so than calorie-cutting alone. And a 2023 study found that high-intensity exercise boosted the ranks of certain immune cells and reduced inflammation in the colon among people at high risk for colon and endometrial cancers due to Lynch syndrome.
Defining an Exercise ‘Prescription’
Despite the gaps and uncertainties in the research, government guidelines as well as those from the American Cancer Society and other medical groups are in lockstep in their exercise recommendations: Adults should strive for 150-300 minutes of moderate-intensity aerobic exercise (like brisk walking), 75-150 minutes of vigorous activity (like running), or some combination each week.
The guidelines also encourage strength training twice a week — advice that’s based on research tying those activity levels to lower risks for heart disease, diabetes, and other chronic conditions.
But there’s no “best” exercise prescription for lowering cancer risk specifically. Most epidemiological studies have examined only aerobic activity, Dr. Rees-Punia said, and there’s very little known about whether strength conditioning or other moderate heart rate-elevating activities, such as daily household chores, may reduce the risk for cancer.
Given the lack of nuance in the literature, it’s hard to say what intensities, types, or amounts of exercise are best for each individual.
Going forward, device-based measurements of physical activity could “help us sort out the effects of different intensities of exercise and possibly types,” Dr. Rees-Punia said.
But overall, Dr. McTiernan said, the data do show that the risks for several cancers are lower at the widely recommended activity levels.
“The bottom-line advice is still to exercise at least 150 minutes per week at a moderate-intensity level or greater,” Dr. McTiernan said.
Or put another way, moving beats being sedentary. It’s probably wise for everyone to sit less, noted Dr. Rees-Punia, for overall health and based on evidence tying sedentary time to the risks for certain cancers, including colon, endometrial, and lung.
There’s a practical element to consider in all of this: What physical activities will people actually do on the regular? In the big epidemiological studies, Dr. McTiernan noted, middle-aged and older adults most often report walking, suggesting that’s the preferred, or most accessible activity, for many.
“You can only benefit from the physical activity you’ll actually do,” Dr. Rees-Punia said.
Dr. Ligibel echoed that sentiment, saying she encourages patients to think about physical activity as a process: “You need to find things you like to do and work them into your daily life, in a sustainable way.
“People often talk about exercise being medicine,” Dr. Ligibel said. “But I think you could take that too far. If we get too prescriptive about it, that could take the joy away.”
A version of this article appeared on Medscape.com.
Nivolumab Wins First-Line Indication in Metastatic Urothelial Carcinoma
Approval was based on the CHECKMATE-901 trial in 608 patients randomized equally to either cisplatin and gemcitabine for ≤ six cycles or nivolumab plus cisplatin and gemcitabine for ≤ six cycles, followed by nivolumab alone for ≤ 2 years.
Median overall survival was 21.7 months with nivolumab add-on vs 18.9 months with cisplatin/gemcitabine alone (hazard ratio [HR], 0.78; P = .0171). The nivolumab group had a slightly higher median progression-free survival of 7.9 months vs 7.6 months in the cisplatin and gemcitabine group (HR, 0.72; P = .0012).
The most common adverse events, occurring in ≥ 15% of nivolumab patients, were nausea, fatigue, musculoskeletal pain, constipation, decreased appetite, rash, vomiting, peripheral neuropathy, urinary tract infection, diarrhea, edema, hypothyroidism, and pruritus.
Among numerous other oncology indications, nivolumab was previously approved for adjuvant treatment following urothelial carcinoma resection and for locally advanced or metastatic urothelial carcinoma that progresses during or following platinum-containing chemotherapy.
A version of this article appeared on Medscape.com .
Approval was based on the CHECKMATE-901 trial in 608 patients randomized equally to either cisplatin and gemcitabine for ≤ six cycles or nivolumab plus cisplatin and gemcitabine for ≤ six cycles, followed by nivolumab alone for ≤ 2 years.
Median overall survival was 21.7 months with nivolumab add-on vs 18.9 months with cisplatin/gemcitabine alone (hazard ratio [HR], 0.78; P = .0171). The nivolumab group had a slightly higher median progression-free survival of 7.9 months vs 7.6 months in the cisplatin and gemcitabine group (HR, 0.72; P = .0012).
The most common adverse events, occurring in ≥ 15% of nivolumab patients, were nausea, fatigue, musculoskeletal pain, constipation, decreased appetite, rash, vomiting, peripheral neuropathy, urinary tract infection, diarrhea, edema, hypothyroidism, and pruritus.
Among numerous other oncology indications, nivolumab was previously approved for adjuvant treatment following urothelial carcinoma resection and for locally advanced or metastatic urothelial carcinoma that progresses during or following platinum-containing chemotherapy.
A version of this article appeared on Medscape.com .
Approval was based on the CHECKMATE-901 trial in 608 patients randomized equally to either cisplatin and gemcitabine for ≤ six cycles or nivolumab plus cisplatin and gemcitabine for ≤ six cycles, followed by nivolumab alone for ≤ 2 years.
Median overall survival was 21.7 months with nivolumab add-on vs 18.9 months with cisplatin/gemcitabine alone (hazard ratio [HR], 0.78; P = .0171). The nivolumab group had a slightly higher median progression-free survival of 7.9 months vs 7.6 months in the cisplatin and gemcitabine group (HR, 0.72; P = .0012).
The most common adverse events, occurring in ≥ 15% of nivolumab patients, were nausea, fatigue, musculoskeletal pain, constipation, decreased appetite, rash, vomiting, peripheral neuropathy, urinary tract infection, diarrhea, edema, hypothyroidism, and pruritus.
Among numerous other oncology indications, nivolumab was previously approved for adjuvant treatment following urothelial carcinoma resection and for locally advanced or metastatic urothelial carcinoma that progresses during or following platinum-containing chemotherapy.
A version of this article appeared on Medscape.com .
TIL for Melanoma: What Are the Costs and Other Challenges to Getting It to Patients?
The US Food and Drug Administration (FDA) recently approved the tumor-infiltrating lymphocyte cell therapy (TIL) for use in certain adults with unresectable or metastatic melanoma. This marks the first time the FDA has allowed a cellular therapy to be marketed for a solid tumor cancer.
Lifileucel is made from a patient’s surgically removed tumor. Tissue from that tumor is then sent to a manufacturing center. Turnaround time to when the drug is ready to be sent back to the cancer center for use is approximately 34 days, according to the drug’s manufacturer, Iovance.
Insurance Adjustments
The cost of the one-time lifileucel treatment is $515,000, according to the manufacturer.
Two investigators in the clinical trials of lifileucel, Allison Betof Warner, MD, of Stanford University, Stanford, California, and Igor Puzanov, MD, of Roswell Park Comprehensive Cancer Center, Buffalo, New York, shared their expectations regarding factors that would contribute to how much a patient paid for the drug.
Given the drug’s recent approval, the logistical details are still being worked out between cancer centers and insurers regarding how much patients will pay out of pocket for lifileucel, said Dr. Betof Warner, who is assistant professor in the Department of Medicine, Division of Medical Oncology at Stanford University.
The associated costs, including the surgery that is needed to procure the TIL cells for expansion into the final drug product, will be different for each patient, she told this publication.
Patients’ costs for lifileucel will vary based on their insurance, explained Dr. Puzanov, chief of melanoma and professor of oncology at Roswell Park Comprehensive Cancer Center.
At Roswell Park, “we will work with our regionally-based payers on a case-by-case basis to seek approval for those patients we believe can most benefit from lifileucel,” he said in an interview. Preauthorization will be required, as is standard for many cancer treatments, he added.
Once payer approval is in place, Dr. Puzanov said, he did not anticipate significant delays in access for patients.
Certified centers such as the multidisciplinary team at Roswell Park are ready to treat patients now. Other centers are similarly prepared, especially those involved in the clinical trials of lifileucel, he said.
Logistics and Infrastructure
A position article and guidelines on the management of and best practices for TIL was published in the Journal for ImmunoTherapy of Cancer on February 29. The paper, of which both Dr. Betof Warner and Dr. Puzanov served as authors, noted that one of the barriers to the use of TIL cell therapy in clinical practice is the need for state-of-the art infrastructure at centers that want to offer the treatment. Scheduling, patient referrals, and surgery, as well as the production and infusion of TIL, must be organized and streamlined for successful treatment, the authors wrote.
The two supply chains involved in TIL — the transportation of the tumor tissue from the treatment center to the manufacturer and transport of the TIL infusion product back to the treatment center — must be timely and precise, they emphasized.
Docs Hope TIL Improves in Several Ways
Although the TIL technology is a breakthrough, “we hope to see even better efficacy and lower toxicity as further research looks at ways to improve on the current TIL standard,” Dr. Puzanov said.
More research and dose adjustments may impact patient costs and side effects, he noted. “I am looking to see TILs used in the front line, with or without checkpoint inhibitors.”
Research is needed to explore how to lower the chemotherapy doses and possibly the associated toxicity, he added. Finally, researchers must consider whether high-dose IL-2 therapy — given as part of the TIL cell therapy — could be replaced with other cytokines, or whether the number of doses could be lowered. Another avenue of exploration is engineering genes for cytokines into TILs, he said.
“The key is to think about TIL therapy before you need it — ideally, when the patient is still doing well on their frontline checkpoint inhibition immunotherapy,” Dr. Puzanov said in an interview. That is the time for evaluation, and specialty centers can provide an expert assessment, he said.
“We are constantly working to improve TIL therapy,” Dr. Betof Warner told this publication. More research is needed optimize the regimen to reduce side effects, which would not only make treatment easier for currently eligible patients, but might allow treatment for patients not currently eligible.
“For example, we are looking for ways to reduce the dose of preparative chemotherapy, which prepares the body for the cells to maximize their longevity and efficacy, and to reduce or eliminate the need to give IL-2 after the cell administration,” continued Dr. Betof Warner, who is also Director of Melanoma Medical Oncology, Director of Solid Tumor Cellular Therapy, and Codirector of the Pigmented Lesion and Melanoma Program at Stanford University. “We are also actively studying next-generation TIL therapies to try to increase the efficacy.”
“Lifileucel has about a 30% success rate for melanoma that has progressed after standard therapy; we are working hard to do better than that,” she noted.
In a press release, Iovance summarized the results of the trial that supported the FDA’s accelerated approval of lifileucel. In an open-label single-arm study, including multiple sites worldwide, 73 adults with unresectable or metastatic melanoma who had received at least one previous systemic therapy underwent a lymphodepleting regimen followed by treatments with fludarabine and aldesleukin. Patients then received lifileucel at a median dose of 21.1 x 109 viable cells; the recommended dose ranges from 7.5 x 109 to 72 x 109 cells.
The primary efficacy outcome was objective response rate (ORR). The ORR in the study was 31.5%, and the median time to initial lifileucel response was 1.5 months.
The clinical trials of lifileucel for which Dr. Betof Warner and Dr. Puzanov served as investigators were sponsored by Iovance.
The US Food and Drug Administration (FDA) recently approved the tumor-infiltrating lymphocyte cell therapy (TIL) for use in certain adults with unresectable or metastatic melanoma. This marks the first time the FDA has allowed a cellular therapy to be marketed for a solid tumor cancer.
Lifileucel is made from a patient’s surgically removed tumor. Tissue from that tumor is then sent to a manufacturing center. Turnaround time to when the drug is ready to be sent back to the cancer center for use is approximately 34 days, according to the drug’s manufacturer, Iovance.
Insurance Adjustments
The cost of the one-time lifileucel treatment is $515,000, according to the manufacturer.
Two investigators in the clinical trials of lifileucel, Allison Betof Warner, MD, of Stanford University, Stanford, California, and Igor Puzanov, MD, of Roswell Park Comprehensive Cancer Center, Buffalo, New York, shared their expectations regarding factors that would contribute to how much a patient paid for the drug.
Given the drug’s recent approval, the logistical details are still being worked out between cancer centers and insurers regarding how much patients will pay out of pocket for lifileucel, said Dr. Betof Warner, who is assistant professor in the Department of Medicine, Division of Medical Oncology at Stanford University.
The associated costs, including the surgery that is needed to procure the TIL cells for expansion into the final drug product, will be different for each patient, she told this publication.
Patients’ costs for lifileucel will vary based on their insurance, explained Dr. Puzanov, chief of melanoma and professor of oncology at Roswell Park Comprehensive Cancer Center.
At Roswell Park, “we will work with our regionally-based payers on a case-by-case basis to seek approval for those patients we believe can most benefit from lifileucel,” he said in an interview. Preauthorization will be required, as is standard for many cancer treatments, he added.
Once payer approval is in place, Dr. Puzanov said, he did not anticipate significant delays in access for patients.
Certified centers such as the multidisciplinary team at Roswell Park are ready to treat patients now. Other centers are similarly prepared, especially those involved in the clinical trials of lifileucel, he said.
Logistics and Infrastructure
A position article and guidelines on the management of and best practices for TIL was published in the Journal for ImmunoTherapy of Cancer on February 29. The paper, of which both Dr. Betof Warner and Dr. Puzanov served as authors, noted that one of the barriers to the use of TIL cell therapy in clinical practice is the need for state-of-the art infrastructure at centers that want to offer the treatment. Scheduling, patient referrals, and surgery, as well as the production and infusion of TIL, must be organized and streamlined for successful treatment, the authors wrote.
The two supply chains involved in TIL — the transportation of the tumor tissue from the treatment center to the manufacturer and transport of the TIL infusion product back to the treatment center — must be timely and precise, they emphasized.
Docs Hope TIL Improves in Several Ways
Although the TIL technology is a breakthrough, “we hope to see even better efficacy and lower toxicity as further research looks at ways to improve on the current TIL standard,” Dr. Puzanov said.
More research and dose adjustments may impact patient costs and side effects, he noted. “I am looking to see TILs used in the front line, with or without checkpoint inhibitors.”
Research is needed to explore how to lower the chemotherapy doses and possibly the associated toxicity, he added. Finally, researchers must consider whether high-dose IL-2 therapy — given as part of the TIL cell therapy — could be replaced with other cytokines, or whether the number of doses could be lowered. Another avenue of exploration is engineering genes for cytokines into TILs, he said.
“The key is to think about TIL therapy before you need it — ideally, when the patient is still doing well on their frontline checkpoint inhibition immunotherapy,” Dr. Puzanov said in an interview. That is the time for evaluation, and specialty centers can provide an expert assessment, he said.
“We are constantly working to improve TIL therapy,” Dr. Betof Warner told this publication. More research is needed optimize the regimen to reduce side effects, which would not only make treatment easier for currently eligible patients, but might allow treatment for patients not currently eligible.
“For example, we are looking for ways to reduce the dose of preparative chemotherapy, which prepares the body for the cells to maximize their longevity and efficacy, and to reduce or eliminate the need to give IL-2 after the cell administration,” continued Dr. Betof Warner, who is also Director of Melanoma Medical Oncology, Director of Solid Tumor Cellular Therapy, and Codirector of the Pigmented Lesion and Melanoma Program at Stanford University. “We are also actively studying next-generation TIL therapies to try to increase the efficacy.”
“Lifileucel has about a 30% success rate for melanoma that has progressed after standard therapy; we are working hard to do better than that,” she noted.
In a press release, Iovance summarized the results of the trial that supported the FDA’s accelerated approval of lifileucel. In an open-label single-arm study, including multiple sites worldwide, 73 adults with unresectable or metastatic melanoma who had received at least one previous systemic therapy underwent a lymphodepleting regimen followed by treatments with fludarabine and aldesleukin. Patients then received lifileucel at a median dose of 21.1 x 109 viable cells; the recommended dose ranges from 7.5 x 109 to 72 x 109 cells.
The primary efficacy outcome was objective response rate (ORR). The ORR in the study was 31.5%, and the median time to initial lifileucel response was 1.5 months.
The clinical trials of lifileucel for which Dr. Betof Warner and Dr. Puzanov served as investigators were sponsored by Iovance.
The US Food and Drug Administration (FDA) recently approved the tumor-infiltrating lymphocyte cell therapy (TIL) for use in certain adults with unresectable or metastatic melanoma. This marks the first time the FDA has allowed a cellular therapy to be marketed for a solid tumor cancer.
Lifileucel is made from a patient’s surgically removed tumor. Tissue from that tumor is then sent to a manufacturing center. Turnaround time to when the drug is ready to be sent back to the cancer center for use is approximately 34 days, according to the drug’s manufacturer, Iovance.
Insurance Adjustments
The cost of the one-time lifileucel treatment is $515,000, according to the manufacturer.
Two investigators in the clinical trials of lifileucel, Allison Betof Warner, MD, of Stanford University, Stanford, California, and Igor Puzanov, MD, of Roswell Park Comprehensive Cancer Center, Buffalo, New York, shared their expectations regarding factors that would contribute to how much a patient paid for the drug.
Given the drug’s recent approval, the logistical details are still being worked out between cancer centers and insurers regarding how much patients will pay out of pocket for lifileucel, said Dr. Betof Warner, who is assistant professor in the Department of Medicine, Division of Medical Oncology at Stanford University.
The associated costs, including the surgery that is needed to procure the TIL cells for expansion into the final drug product, will be different for each patient, she told this publication.
Patients’ costs for lifileucel will vary based on their insurance, explained Dr. Puzanov, chief of melanoma and professor of oncology at Roswell Park Comprehensive Cancer Center.
At Roswell Park, “we will work with our regionally-based payers on a case-by-case basis to seek approval for those patients we believe can most benefit from lifileucel,” he said in an interview. Preauthorization will be required, as is standard for many cancer treatments, he added.
Once payer approval is in place, Dr. Puzanov said, he did not anticipate significant delays in access for patients.
Certified centers such as the multidisciplinary team at Roswell Park are ready to treat patients now. Other centers are similarly prepared, especially those involved in the clinical trials of lifileucel, he said.
Logistics and Infrastructure
A position article and guidelines on the management of and best practices for TIL was published in the Journal for ImmunoTherapy of Cancer on February 29. The paper, of which both Dr. Betof Warner and Dr. Puzanov served as authors, noted that one of the barriers to the use of TIL cell therapy in clinical practice is the need for state-of-the art infrastructure at centers that want to offer the treatment. Scheduling, patient referrals, and surgery, as well as the production and infusion of TIL, must be organized and streamlined for successful treatment, the authors wrote.
The two supply chains involved in TIL — the transportation of the tumor tissue from the treatment center to the manufacturer and transport of the TIL infusion product back to the treatment center — must be timely and precise, they emphasized.
Docs Hope TIL Improves in Several Ways
Although the TIL technology is a breakthrough, “we hope to see even better efficacy and lower toxicity as further research looks at ways to improve on the current TIL standard,” Dr. Puzanov said.
More research and dose adjustments may impact patient costs and side effects, he noted. “I am looking to see TILs used in the front line, with or without checkpoint inhibitors.”
Research is needed to explore how to lower the chemotherapy doses and possibly the associated toxicity, he added. Finally, researchers must consider whether high-dose IL-2 therapy — given as part of the TIL cell therapy — could be replaced with other cytokines, or whether the number of doses could be lowered. Another avenue of exploration is engineering genes for cytokines into TILs, he said.
“The key is to think about TIL therapy before you need it — ideally, when the patient is still doing well on their frontline checkpoint inhibition immunotherapy,” Dr. Puzanov said in an interview. That is the time for evaluation, and specialty centers can provide an expert assessment, he said.
“We are constantly working to improve TIL therapy,” Dr. Betof Warner told this publication. More research is needed optimize the regimen to reduce side effects, which would not only make treatment easier for currently eligible patients, but might allow treatment for patients not currently eligible.
“For example, we are looking for ways to reduce the dose of preparative chemotherapy, which prepares the body for the cells to maximize their longevity and efficacy, and to reduce or eliminate the need to give IL-2 after the cell administration,” continued Dr. Betof Warner, who is also Director of Melanoma Medical Oncology, Director of Solid Tumor Cellular Therapy, and Codirector of the Pigmented Lesion and Melanoma Program at Stanford University. “We are also actively studying next-generation TIL therapies to try to increase the efficacy.”
“Lifileucel has about a 30% success rate for melanoma that has progressed after standard therapy; we are working hard to do better than that,” she noted.
In a press release, Iovance summarized the results of the trial that supported the FDA’s accelerated approval of lifileucel. In an open-label single-arm study, including multiple sites worldwide, 73 adults with unresectable or metastatic melanoma who had received at least one previous systemic therapy underwent a lymphodepleting regimen followed by treatments with fludarabine and aldesleukin. Patients then received lifileucel at a median dose of 21.1 x 109 viable cells; the recommended dose ranges from 7.5 x 109 to 72 x 109 cells.
The primary efficacy outcome was objective response rate (ORR). The ORR in the study was 31.5%, and the median time to initial lifileucel response was 1.5 months.
The clinical trials of lifileucel for which Dr. Betof Warner and Dr. Puzanov served as investigators were sponsored by Iovance.
Study Finds No Increased Cancer Risk With Spironolactone
TOPLINE:
than that of unexposed women.
METHODOLOGY:
- Spironolactone, used off-label for several skin conditions in women, carries a warning about an increased tumor risk associated with high doses in rat models, and its antiandrogen properties have prompted hypotheses about a possible increased risk for breast or gynecologic cancers.
- The researchers reviewed data on 420 women with a history of spironolactone use for acne, hair loss, and hirsutism and 3272 women with no spironolactone use at the authors› institution. Their mean age ranged from 42 to 63 years; the majority were White, and 38% were non-White.
- Median spironolactone doses ranged from 25 mg to 225 mg; chart reviews included 5-year follow-up data from the first spironolactone exposure to allow time for tumor development.
TAKEAWAY:
- A total of 37 of the 420 women exposed to spironolactone developed any tumors, as did 546 of the 3272 with no spironolactone exposure.
- After the researchers controlled for age and race, women exposed to spironolactone were no more likely to develop a malignant tumor than a benign tumor, compared with unexposed women (odds ratio [OR], 0.48, P = .2).
- The risk for breast or uterine cancer was not significantly different in the spironolactone and non-spironolactone groups (OR, 0.95, P > .9).
IN PRACTICE:
“Women taking spironolactone for acne, hair loss, and hirsutism and who are at low risk of breast or gynecologic cancers may be counseled to have regular gynecology follow-up, but no more frequently than the general population,” but more studies are needed to evaluate risk over longer periods of time, the researchers wrote.
SOURCE:
The lead author of the study was Rachel C. Hill, BS, a student at Weill Cornell Medical College, New York City, and Shari R. Lipner, MD, PhD, of the department of dermatology at Weill Cornell Medical College, was the corresponding author. The study was published online in The Journal of the American Academy of Dermatology.
LIMITATIONS:
The findings were limited by the retrospective design, as well as the small number of spironolactone patients analyzed, the short follow-up period, the lack of information about spironolactone courses, and the inability to control for family history of malignancy.
DISCLOSURES:
The study was supported by the National Center for Advancing Translational Sciences and a grant from the Clinical and Translational Science Center at Weill Cornell Medical College awarded to Ms. Hill. None of the authors had relevant disclosures; Dr. Lipner disclosed serving as a consultant for Ortho-Dermatologics, Eli Lilly, Moberg Pharmaceuticals, and BelleTorus Corporation.
A version of this article appeared on Medscape.com.
TOPLINE:
than that of unexposed women.
METHODOLOGY:
- Spironolactone, used off-label for several skin conditions in women, carries a warning about an increased tumor risk associated with high doses in rat models, and its antiandrogen properties have prompted hypotheses about a possible increased risk for breast or gynecologic cancers.
- The researchers reviewed data on 420 women with a history of spironolactone use for acne, hair loss, and hirsutism and 3272 women with no spironolactone use at the authors› institution. Their mean age ranged from 42 to 63 years; the majority were White, and 38% were non-White.
- Median spironolactone doses ranged from 25 mg to 225 mg; chart reviews included 5-year follow-up data from the first spironolactone exposure to allow time for tumor development.
TAKEAWAY:
- A total of 37 of the 420 women exposed to spironolactone developed any tumors, as did 546 of the 3272 with no spironolactone exposure.
- After the researchers controlled for age and race, women exposed to spironolactone were no more likely to develop a malignant tumor than a benign tumor, compared with unexposed women (odds ratio [OR], 0.48, P = .2).
- The risk for breast or uterine cancer was not significantly different in the spironolactone and non-spironolactone groups (OR, 0.95, P > .9).
IN PRACTICE:
“Women taking spironolactone for acne, hair loss, and hirsutism and who are at low risk of breast or gynecologic cancers may be counseled to have regular gynecology follow-up, but no more frequently than the general population,” but more studies are needed to evaluate risk over longer periods of time, the researchers wrote.
SOURCE:
The lead author of the study was Rachel C. Hill, BS, a student at Weill Cornell Medical College, New York City, and Shari R. Lipner, MD, PhD, of the department of dermatology at Weill Cornell Medical College, was the corresponding author. The study was published online in The Journal of the American Academy of Dermatology.
LIMITATIONS:
The findings were limited by the retrospective design, as well as the small number of spironolactone patients analyzed, the short follow-up period, the lack of information about spironolactone courses, and the inability to control for family history of malignancy.
DISCLOSURES:
The study was supported by the National Center for Advancing Translational Sciences and a grant from the Clinical and Translational Science Center at Weill Cornell Medical College awarded to Ms. Hill. None of the authors had relevant disclosures; Dr. Lipner disclosed serving as a consultant for Ortho-Dermatologics, Eli Lilly, Moberg Pharmaceuticals, and BelleTorus Corporation.
A version of this article appeared on Medscape.com.
TOPLINE:
than that of unexposed women.
METHODOLOGY:
- Spironolactone, used off-label for several skin conditions in women, carries a warning about an increased tumor risk associated with high doses in rat models, and its antiandrogen properties have prompted hypotheses about a possible increased risk for breast or gynecologic cancers.
- The researchers reviewed data on 420 women with a history of spironolactone use for acne, hair loss, and hirsutism and 3272 women with no spironolactone use at the authors› institution. Their mean age ranged from 42 to 63 years; the majority were White, and 38% were non-White.
- Median spironolactone doses ranged from 25 mg to 225 mg; chart reviews included 5-year follow-up data from the first spironolactone exposure to allow time for tumor development.
TAKEAWAY:
- A total of 37 of the 420 women exposed to spironolactone developed any tumors, as did 546 of the 3272 with no spironolactone exposure.
- After the researchers controlled for age and race, women exposed to spironolactone were no more likely to develop a malignant tumor than a benign tumor, compared with unexposed women (odds ratio [OR], 0.48, P = .2).
- The risk for breast or uterine cancer was not significantly different in the spironolactone and non-spironolactone groups (OR, 0.95, P > .9).
IN PRACTICE:
“Women taking spironolactone for acne, hair loss, and hirsutism and who are at low risk of breast or gynecologic cancers may be counseled to have regular gynecology follow-up, but no more frequently than the general population,” but more studies are needed to evaluate risk over longer periods of time, the researchers wrote.
SOURCE:
The lead author of the study was Rachel C. Hill, BS, a student at Weill Cornell Medical College, New York City, and Shari R. Lipner, MD, PhD, of the department of dermatology at Weill Cornell Medical College, was the corresponding author. The study was published online in The Journal of the American Academy of Dermatology.
LIMITATIONS:
The findings were limited by the retrospective design, as well as the small number of spironolactone patients analyzed, the short follow-up period, the lack of information about spironolactone courses, and the inability to control for family history of malignancy.
DISCLOSURES:
The study was supported by the National Center for Advancing Translational Sciences and a grant from the Clinical and Translational Science Center at Weill Cornell Medical College awarded to Ms. Hill. None of the authors had relevant disclosures; Dr. Lipner disclosed serving as a consultant for Ortho-Dermatologics, Eli Lilly, Moberg Pharmaceuticals, and BelleTorus Corporation.
A version of this article appeared on Medscape.com.
No Increase in Autoimmune Risk Seen With GLP-1 Receptor Agonists and SGLT2 Inhibitors
TOPLINE:
In patients with type 2 diabetes, there was no difference in risk of developing autoimmune disease if prescribed glucagon-like peptide 1 receptor agonists (GLP-1-RAs), sodium-glucose cotransporter-2 (SGLT2) inhibitors, or dipeptidyl peptidase-4 (DPP-4) inhibitors.
METHODOLOGY:
- The effect of GLP-1-RAs and SGLT2 inhibitors on autoimmune rheumatic disease (ARD) is understudied, though previous case reports and one study have hinted at increased risk.
- Researchers used administrative health data from 2014 to 2021 to identify 34,400 patients prescribed GLP-1-RAs and 83,500 patients prescribed SGLT2 inhibitors.
- They compared patients prescribed GLP-1-RAs or SGLT2 inhibitors with 68,400 patients prescribed DPP-4 inhibitors, which previous studies suggest do not increase ARD risk.
- Primary outcome was ARD incidence, defined by diagnostic codes.
TAKEAWAY:
- There were no significant differences in incident ARDs between the three groups.
- Mean follow-up time was 0.88-1.53 years.
- The hazard ratio (HR) for developing ARDs with GLP-1-RAs exposure was 0.93 (95% CI, 0.66-1.30) compared with DPP-4 inhibitors.
- The HR for developing ARDs with SGLT2 inhibitor exposure was 0.97 (95% CI, 0.76-1.24).
IN PRACTICE:
“Extended longitudinal data are needed to assess risk and benefit with longer-term exposure,” the authors wrote.
SOURCE:
First author Derin Karacabeyli, MD, of the University of British Columbia, Vancouver, Canada, presented the study in abstract form at the Canadian Rheumatology Association (CRA) 2024 Annual Meeting in Winnipeg on February 29.
LIMITATIONS:
The study was observational, which could have some residual or unmeasured confounding of data. The researchers relied on diagnostic codes and the average follow-up time was short.
DISCLOSURES:
The study was funded by the Canadian Institutes of Health Research. The authors had no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
In patients with type 2 diabetes, there was no difference in risk of developing autoimmune disease if prescribed glucagon-like peptide 1 receptor agonists (GLP-1-RAs), sodium-glucose cotransporter-2 (SGLT2) inhibitors, or dipeptidyl peptidase-4 (DPP-4) inhibitors.
METHODOLOGY:
- The effect of GLP-1-RAs and SGLT2 inhibitors on autoimmune rheumatic disease (ARD) is understudied, though previous case reports and one study have hinted at increased risk.
- Researchers used administrative health data from 2014 to 2021 to identify 34,400 patients prescribed GLP-1-RAs and 83,500 patients prescribed SGLT2 inhibitors.
- They compared patients prescribed GLP-1-RAs or SGLT2 inhibitors with 68,400 patients prescribed DPP-4 inhibitors, which previous studies suggest do not increase ARD risk.
- Primary outcome was ARD incidence, defined by diagnostic codes.
TAKEAWAY:
- There were no significant differences in incident ARDs between the three groups.
- Mean follow-up time was 0.88-1.53 years.
- The hazard ratio (HR) for developing ARDs with GLP-1-RAs exposure was 0.93 (95% CI, 0.66-1.30) compared with DPP-4 inhibitors.
- The HR for developing ARDs with SGLT2 inhibitor exposure was 0.97 (95% CI, 0.76-1.24).
IN PRACTICE:
“Extended longitudinal data are needed to assess risk and benefit with longer-term exposure,” the authors wrote.
SOURCE:
First author Derin Karacabeyli, MD, of the University of British Columbia, Vancouver, Canada, presented the study in abstract form at the Canadian Rheumatology Association (CRA) 2024 Annual Meeting in Winnipeg on February 29.
LIMITATIONS:
The study was observational, which could have some residual or unmeasured confounding of data. The researchers relied on diagnostic codes and the average follow-up time was short.
DISCLOSURES:
The study was funded by the Canadian Institutes of Health Research. The authors had no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
In patients with type 2 diabetes, there was no difference in risk of developing autoimmune disease if prescribed glucagon-like peptide 1 receptor agonists (GLP-1-RAs), sodium-glucose cotransporter-2 (SGLT2) inhibitors, or dipeptidyl peptidase-4 (DPP-4) inhibitors.
METHODOLOGY:
- The effect of GLP-1-RAs and SGLT2 inhibitors on autoimmune rheumatic disease (ARD) is understudied, though previous case reports and one study have hinted at increased risk.
- Researchers used administrative health data from 2014 to 2021 to identify 34,400 patients prescribed GLP-1-RAs and 83,500 patients prescribed SGLT2 inhibitors.
- They compared patients prescribed GLP-1-RAs or SGLT2 inhibitors with 68,400 patients prescribed DPP-4 inhibitors, which previous studies suggest do not increase ARD risk.
- Primary outcome was ARD incidence, defined by diagnostic codes.
TAKEAWAY:
- There were no significant differences in incident ARDs between the three groups.
- Mean follow-up time was 0.88-1.53 years.
- The hazard ratio (HR) for developing ARDs with GLP-1-RAs exposure was 0.93 (95% CI, 0.66-1.30) compared with DPP-4 inhibitors.
- The HR for developing ARDs with SGLT2 inhibitor exposure was 0.97 (95% CI, 0.76-1.24).
IN PRACTICE:
“Extended longitudinal data are needed to assess risk and benefit with longer-term exposure,” the authors wrote.
SOURCE:
First author Derin Karacabeyli, MD, of the University of British Columbia, Vancouver, Canada, presented the study in abstract form at the Canadian Rheumatology Association (CRA) 2024 Annual Meeting in Winnipeg on February 29.
LIMITATIONS:
The study was observational, which could have some residual or unmeasured confounding of data. The researchers relied on diagnostic codes and the average follow-up time was short.
DISCLOSURES:
The study was funded by the Canadian Institutes of Health Research. The authors had no disclosures.
A version of this article appeared on Medscape.com.
Vulvar Lichen Sclerosus: What’s New?
Vulvar lichen sclerosus (VLS) is an underserved area in medicine and dermatology. We discuss updates in VLS, which include the following: (1) development of core outcome domains to include in all future clinical trials, with current efforts focused on determining outcome measurements for each domain; (2) increased understanding of the impact VLS has on quality-of-life (QOL) outcomes; (3) expanded disease associations; (4) clinical and histologic variants, including vestibular sclerosis and nonsclerotic VLS; and (5) updates in management of VLS.
Core Outcomes Measures
The burden of VLS is challenging to quantify, with little agreement among experts.1 Recently there has been a focus on developing scoring scales to measure disease progression and treatment response. Simpson et al2 pioneered the development of a core outcome set to be included in all future clinical trials for genital lichen sclerosus (LS)—clinical (visible) signs, symptoms, and LS-specific QOL.
Although there is no standardized method for assessing disease severity, various scales have been proposed to measure clinical findings in VLS, such as the vulvar architecture severity scale3 as well as the clinical LS score,4 which is the only validated scale to incorporate the signs and architectural changes identified by a 2018 Delphi consensus group of the International Society for the Study of Vulvovaginal Disease.5 Work is ongoing to identify and evaluate outcome measurement instruments for each of the 3 core outcome domains.
Increased Understanding of QOL Impacts
Pain, pruritus, impairment of sexual function, genitourinary complications, architectural changes, and risk for squamous cell carcinoma (SCC) all have been well established as VLS sequelae.6,7 Recent studies have focused on the QOL impact and associations with psychiatric comorbidities. A matched case-control study found that LS was significantly associated with depression and anxiety among US women (P<.001), and individuals with LS had a more than 2-fold increased odds of receiving a diagnosis of depression or anxiety.8
A review evaluating QOL outcomes in LS found that overall QOL was impaired. Female patients reported worse QOL in the work-school domain of the dermatology life quality index compared with male counterparts.9
Finally, a study exploring the experiences of patients living with VLS highlighted the secrecy and stigma of the condition,10 which serves as a call to action to improve the general population’s knowledge about vulvar anatomy and create change in societal attitudes on vulvar conditions.
Although there are several instruments assessing vulvar-specific QOL, most are for patients with vulvar cancer and focus on sexual function. In 2020, Saunderson et al11 published the 15-item vulvar quality of life index (VQLI), which has broad implications for measuring vulvar disease burden and is an important tool for standardizing vulvar disease measurements and outcomes for clinical research.12 The VQLI, though not specific to VLS, consists of 4 domains to assess vulvar QOL including symptoms, anxiety, activities of daily living, and sexuality. Studies have evaluated this scoring system in patients with VLS, with 1 study finding that VQLI correlated with clinician-rated severity scores (P=.01) and overall patient itch/discomfort score (P<.001) in VLS.13,14
Expanded Disease Associations
Lichen sclerosus has a well-known association with vulvar SCC and other autoimmune conditions, including thyroid disease and bullous pemphigoid.15-17 Recent studies also have revealed an association between LS and psoriasis.18 A case-control study from a single center found VLS was associated with elevated body mass index, statin usage, and cholecystectomy.19 Gynecologic pain syndromes, interstitial cystitis, urinary incontinence, and some gastrointestinal tract disorders including celiac disease also have been found to be increased in patients with VLS.20 Finally, the incidence of cutaneous immune-related adverse events such as LS has increased as the use of immune checkpoint therapies as anticancer treatments has expanded.21 Clinicians should be aware of these potential disease associations when caring for patients with VLS.
The incidence of VLS is higher in lower estrogen states throughout the lifespan, and a recent case-control study evaluated the cutaneous hormonal and microbial landscapes in postmenopausal patients (6 patients with VLS; 12 controls).22 Levels of the following cutaneous hormones in the groin were found to be altered in patients with VLS compared with controls: estrone (lower; P=.006), progesterone (higher; P<.0001), and testosterone (lower; P=.02). The authors found that most hormone levels normalized following treatment with a topical steroid. Additionally, bacterial microbiome alterations were seen in patients with VLS compared with controls. Thus, cutaneous sex hormone and skin microbiome alterations may be associated with VLS.22
Updates in Clinical and Histologic Variants
Less-recognized variants of VLS have been characterized in recent years. Vestibular sclerosis is a variant of VLS with unique clinical and histopathologic features; it is characterized by involvement localized to the anterior vestibule and either an absent or sparse lymphocytic infiltrate on histopathology.23,24 Nonsclerotic VLS is a variant with clinical features consistent with VLS that does not exhibit dermal sclerosis on histopathology. Thus, a diagnosis of nonsclerotic VLS requires clinicopathologic correlation. Four nonsclerotic histopathologic subtypes are proposed: lichenoid, hypertrophic lichenoid, dermal fibrosis without acanthosis, and dermal fibrosis with acanthosis.25 Longitudinal studies that correlate duration, signs, and symptoms will be important to further understand these variants.
Management Updates
First-line treatment of VLS still consists of ultrapotent topical corticosteroids with chronic maintenance therapy (usually lifetime) to decrease the risk for SCC and architectural changes.26 However, a survey across social media platforms found steroid phobia is common in patients with VLS (N=865), with approximately 40% of respondents endorsing waiting as long as they could before using topical corticosteroids and stopping as soon as possible.27 Clinicians should be aware of possible patient perceptions in the use of chronic steroids when discussing this therapy.
Randomized controlled trials utilizing fractional CO2 devices for VLS have been performed with conflicting results and no consensus regarding outcome measurement.28,29 Additionally, long-term disease outcomes following laser use have not been investigated. Although there is evidence that both ablative and nonablative devices can improve symptoms and signs, there is no evidence that they offer a cure for a chronic inflammatory skin condition. Current evidence suggests that even for patients undergoing these procedures, maintenance therapy is still essential to prevent sequelae.30 Future studies incorporating standardized outcome measures will be important for assessing the benefits of laser therapy in VLS. Finally, the reasons why topical corticosteroids may fail in an individual patient are multifaceted and should be explored thoroughly when considering laser therapy for VLS.
Studies evaluating the role of systemic therapies for refractory cases of VLS have expanded. A systematic review of systemic therapies for both genital and extragenital LS found oral corticosteroids and methotrexate were the most-reported systemic treatment regimens.31 Use of biologics in LS has been reported, with cases utilizing adalimumab for VLS and dupilumab for extragenital LS. Use of Janus kinase inhibitors including abrocitinib and baricitinib also has been reported for LS.31 A clinical trial to evaluate the safety and efficacy of topical ruxolitinib in VLS was recently completed (ClinicalTrials.govidentifier NCT05593445). Future research studies likely will focus on the safety and efficacy of targeted and steroid-sparing therapies for patients with VLS.
Final Thoughts
Vulvar lichen sclerosus increasingly is becoming recognized as a chronic genital skin condition that impacts QOL and health outcomes, with a need to develop more effective and safe evidence-based therapies. Recent literature has focused on the importance of developing and standardizing disease outcomes; identifying disease associations including the role of cutaneous hormones and microbiome alterations; characterizing histologic and clinical variants; and staying up-to-date on management, including the need for understanding patient perceptions of chronic topical steroid therapy. Each of these are important updates for clinicians to consider when caring for patients with VLS. Future studies likely will focus on elucidating disease etiology and mechanisms to gain a better understanding of VLS pathogenesis and potential targets for therapies as well as implementation of clinical trials that incorporate standardized outcome domains to test efficacy and safety of additional therapies.
- Sheinis M, Green N, Vieira-Baptista P, et al. Adult vulvar lichen sclerosus: can experts agree on the assessment of disease severity? J Low Genit Tract Dis. 2020;24:295-298. doi:10.1097/LGT.0000000000000534
- Simpson RC, Kirtschig G, Selk A, et al. Core outcome domains for lichen sclerosus: a CORALS initiative consensus statement. Br J Dermatol. 2023;188:628-635. doi:10.1093/bjd/ljac145
- Almadori A, Zenner N, Boyle D, et al. Development and validation of a clinical grading scale to assess the vulvar region: the Vulvar Architecture Severity Scale. Aesthet Surg J. 2020;40:1319-1326. doi:10.1093/asj/sjz342
- Erni B, Navarini AA, Huang D, et al. Proposition of a severity scale for lichen sclerosus: the “Clinical Lichen Sclerosus Score.” Dermatol Ther. 2021;34:E14773. doi:10.1111/dth.14773
- Sheinis M, Selk A. Development of the Adult Vulvar Lichen Sclerosus Severity Scale—a Delphi Consensus Exercise for Item Generation. J Low Genit Tract Dis. 2018;22:66-73. doi:10.1097/LGT.0000000000000361
- Mauskar MM, Marathe K, Venkatesan A, et al. Vulvar diseases. J Am Acad Dermatol. 2020;82:1287-1298. doi:10.1016/j.jaad.2019.10.077
- Wijaya M, Lee G, Fischer G. Why do some patients with vulval lichen sclerosus on long-term topical corticosteroid treatment experience ongoing poor quality of life? Australas J Dermatol. 2022;63:463-472. doi:10.1111/ajd.13926
- Fan R, Leasure AC, Maisha FI, et al. Depression and anxiety in patients with lichen sclerosus. JAMA Dermatol. 2022;158:953-954. doi:10.1001/jamadermatol.2022.1964
- Ranum A, Pearson DR. The impact of genital lichen sclerosus and lichen planus on quality of life: a review. Int J Womens Dermatol. 2022;8:E042. doi:10.1097/JW9.0000000000000042
- Arnold S, Fernando S, Rees S. Living with vulval lichen sclerosus: a qualitative interview study. Br J Dermatol. 2022;187:909-918. doi:10.1111/bjd.21777
- Saunderson RB, Harris V, Yeh R, et al. Vulvar quality of life index (VQLI)—a simple tool to measure quality of life in patients with vulvar disease. Australas J Dermatol. 2020;61:152-157. doi:10.1111/ajd.13235
- Pyle HJ, Evans JC, Vandergriff TW, et al. Vulvar lichen sclerosus clinical severity scales and histopathologic correlation: a case series. Am J Dermatopathol. 2023;45:588-592. doi:10.1097/DAD.0000000000002471
- Wijaya M, Lee G, Fischer G. Quality of life of women with untreated vulval lichen sclerosus assessed with vulval quality of life index (VQLI) [published online January 28, 2021]. Australas J Dermatol. 2021;62:177-182. doi:10.1111/ajd.13530
- Felmingham C, Chan L, Doyle LW, et al. The Vulval Disease Quality of Life Index in women with vulval lichen sclerosus correlates with clinician and symptom scores [published online November 14, 2019]. Australas J Dermatol. 2020;61:110-118. doi:10.1111/ajd.13197
- Walsh ML, Leonard N, Shawki H, et al. Lichen sclerosus and immunobullous disease. J Low Genit Tract Dis. 2012;16:468-470. doi:10.1097/LGT.0b013e31825e9b18
- Chin S, Scurry J, Bradford J, et al. Association of topical corticosteroids with reduced vulvar squamous cell carcinoma recurrence in patients with vulvar lichen sclerosus. JAMA Dermatol. 2020;156:813. doi:10.1001/jamadermatol.2020.1074
- Fan R, Leasure AC, Maisha FI, et al. Thyroid disorders associated with lichen sclerosus: a case–control study in the All of Us Research Program. Br J Dermatol. 2022;187:797-799. doi:10.1111/bjd.21702
- Fan R, Leasure AC, Little AJ, et al. Lichen sclerosus among women with psoriasis: a cross-sectional study in the All of Us research program. J Am Acad Dermatol. 2023;88:1175-1177. doi:10.1016/j.jaad.2022.12.012
- Luu Y, Cheng AL, Reisz C. Elevated body mass index, statin use, and cholecystectomy are associated with vulvar lichen sclerosus: a retrospective, case-control study. J Am Acad Dermatol. 2023;88:1376-1378. doi:10.1016/j.jaad.2023.01.023
- Söderlund JM, Hieta NK, Kurki SH, et al. Comorbidity of urogynecological and gastrointestinal disorders in female patients with lichen sclerosus. J Low Genit Tract Dis. 2023;2:156-160. doi:10.1097/LGT.0000000000000727
- Shin L, Smith J, Shiu J, et al. Association of lichen sclerosus and morphea with immune checkpoint therapy: a systematic review. Int J Womens Dermatol. 2023;9:E070. doi:10.1097/JW9.0000000000000070
- Pyle HJ, Evans JC, Artami M, et al. Assessment of the cutaneous hormone landscapes and microbiomes in vulvar lichen sclerosus [published online February 16, 2024]. J Invest Dermatol. 2024:S0022-202X(24)00111-8. doi:10.1016/j.jid.2024.01.027
- Day T, Burston K, Dennerstein G, et al. Vestibulovaginal sclerosis versus lichen sclerosus. Int J Gynecol Pathol. 2018;37:356-363. doi:10.1097/PGP.0000000000000441
- Croker BA, Scurry JP, Petry FM, et al. Vestibular sclerosis: is this a new, distinct clinicopathological entity? J Low Genit Tract Dis. 2018;22:260-263. doi:10.1097/LGT.0000000000000404
- Day T, Selim MA, Allbritton JI, et al. Nonsclerotic lichen sclerosus: definition of a concept and pathologic description. J Low Genit Tract Dis. 2023;27:358-364. doi:10.1097/LGT.0000000000000760
- Lee A, Bradford J, Fischer G. Long-term management of adult vulvar lichen sclerosus: a prospective cohort study of 507 women. JAMA Dermatol. 2015;151:1061. doi:10.1001/jamadermatol.2015.0643
- Delpero E, Sriharan A, Selk A. Steroid phobia in patients with vulvar lichen sclerosus. J Low Genit Tract Dis. 2023;27:286-290. doi:10.1097/LGT.0000000000000753
- Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978. doi:10.1097/AOG.0000000000004332
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:979-987. doi:10.1097/AOG.0000000000004409
- Li HOY, Bailey AMJ, Tan MG, Dover JS. Lasers as an adjuvant for vulvar lichen sclerosus: a systematic review and meta-analysis. J Am Acad Dermatol. 2022;86:694-696. doi:10.1016/j.jaad.2021.02.081
- Hargis A, Ngo M, Kraus CN, et al. Systemic therapy for lichen sclerosus: a systematic review [published online November 4, 2023]. J Low Genit Tract Dis. doi:10.1097/LGT.0000000000000775
Vulvar lichen sclerosus (VLS) is an underserved area in medicine and dermatology. We discuss updates in VLS, which include the following: (1) development of core outcome domains to include in all future clinical trials, with current efforts focused on determining outcome measurements for each domain; (2) increased understanding of the impact VLS has on quality-of-life (QOL) outcomes; (3) expanded disease associations; (4) clinical and histologic variants, including vestibular sclerosis and nonsclerotic VLS; and (5) updates in management of VLS.
Core Outcomes Measures
The burden of VLS is challenging to quantify, with little agreement among experts.1 Recently there has been a focus on developing scoring scales to measure disease progression and treatment response. Simpson et al2 pioneered the development of a core outcome set to be included in all future clinical trials for genital lichen sclerosus (LS)—clinical (visible) signs, symptoms, and LS-specific QOL.
Although there is no standardized method for assessing disease severity, various scales have been proposed to measure clinical findings in VLS, such as the vulvar architecture severity scale3 as well as the clinical LS score,4 which is the only validated scale to incorporate the signs and architectural changes identified by a 2018 Delphi consensus group of the International Society for the Study of Vulvovaginal Disease.5 Work is ongoing to identify and evaluate outcome measurement instruments for each of the 3 core outcome domains.
Increased Understanding of QOL Impacts
Pain, pruritus, impairment of sexual function, genitourinary complications, architectural changes, and risk for squamous cell carcinoma (SCC) all have been well established as VLS sequelae.6,7 Recent studies have focused on the QOL impact and associations with psychiatric comorbidities. A matched case-control study found that LS was significantly associated with depression and anxiety among US women (P<.001), and individuals with LS had a more than 2-fold increased odds of receiving a diagnosis of depression or anxiety.8
A review evaluating QOL outcomes in LS found that overall QOL was impaired. Female patients reported worse QOL in the work-school domain of the dermatology life quality index compared with male counterparts.9
Finally, a study exploring the experiences of patients living with VLS highlighted the secrecy and stigma of the condition,10 which serves as a call to action to improve the general population’s knowledge about vulvar anatomy and create change in societal attitudes on vulvar conditions.
Although there are several instruments assessing vulvar-specific QOL, most are for patients with vulvar cancer and focus on sexual function. In 2020, Saunderson et al11 published the 15-item vulvar quality of life index (VQLI), which has broad implications for measuring vulvar disease burden and is an important tool for standardizing vulvar disease measurements and outcomes for clinical research.12 The VQLI, though not specific to VLS, consists of 4 domains to assess vulvar QOL including symptoms, anxiety, activities of daily living, and sexuality. Studies have evaluated this scoring system in patients with VLS, with 1 study finding that VQLI correlated with clinician-rated severity scores (P=.01) and overall patient itch/discomfort score (P<.001) in VLS.13,14
Expanded Disease Associations
Lichen sclerosus has a well-known association with vulvar SCC and other autoimmune conditions, including thyroid disease and bullous pemphigoid.15-17 Recent studies also have revealed an association between LS and psoriasis.18 A case-control study from a single center found VLS was associated with elevated body mass index, statin usage, and cholecystectomy.19 Gynecologic pain syndromes, interstitial cystitis, urinary incontinence, and some gastrointestinal tract disorders including celiac disease also have been found to be increased in patients with VLS.20 Finally, the incidence of cutaneous immune-related adverse events such as LS has increased as the use of immune checkpoint therapies as anticancer treatments has expanded.21 Clinicians should be aware of these potential disease associations when caring for patients with VLS.
The incidence of VLS is higher in lower estrogen states throughout the lifespan, and a recent case-control study evaluated the cutaneous hormonal and microbial landscapes in postmenopausal patients (6 patients with VLS; 12 controls).22 Levels of the following cutaneous hormones in the groin were found to be altered in patients with VLS compared with controls: estrone (lower; P=.006), progesterone (higher; P<.0001), and testosterone (lower; P=.02). The authors found that most hormone levels normalized following treatment with a topical steroid. Additionally, bacterial microbiome alterations were seen in patients with VLS compared with controls. Thus, cutaneous sex hormone and skin microbiome alterations may be associated with VLS.22
Updates in Clinical and Histologic Variants
Less-recognized variants of VLS have been characterized in recent years. Vestibular sclerosis is a variant of VLS with unique clinical and histopathologic features; it is characterized by involvement localized to the anterior vestibule and either an absent or sparse lymphocytic infiltrate on histopathology.23,24 Nonsclerotic VLS is a variant with clinical features consistent with VLS that does not exhibit dermal sclerosis on histopathology. Thus, a diagnosis of nonsclerotic VLS requires clinicopathologic correlation. Four nonsclerotic histopathologic subtypes are proposed: lichenoid, hypertrophic lichenoid, dermal fibrosis without acanthosis, and dermal fibrosis with acanthosis.25 Longitudinal studies that correlate duration, signs, and symptoms will be important to further understand these variants.
Management Updates
First-line treatment of VLS still consists of ultrapotent topical corticosteroids with chronic maintenance therapy (usually lifetime) to decrease the risk for SCC and architectural changes.26 However, a survey across social media platforms found steroid phobia is common in patients with VLS (N=865), with approximately 40% of respondents endorsing waiting as long as they could before using topical corticosteroids and stopping as soon as possible.27 Clinicians should be aware of possible patient perceptions in the use of chronic steroids when discussing this therapy.
Randomized controlled trials utilizing fractional CO2 devices for VLS have been performed with conflicting results and no consensus regarding outcome measurement.28,29 Additionally, long-term disease outcomes following laser use have not been investigated. Although there is evidence that both ablative and nonablative devices can improve symptoms and signs, there is no evidence that they offer a cure for a chronic inflammatory skin condition. Current evidence suggests that even for patients undergoing these procedures, maintenance therapy is still essential to prevent sequelae.30 Future studies incorporating standardized outcome measures will be important for assessing the benefits of laser therapy in VLS. Finally, the reasons why topical corticosteroids may fail in an individual patient are multifaceted and should be explored thoroughly when considering laser therapy for VLS.
Studies evaluating the role of systemic therapies for refractory cases of VLS have expanded. A systematic review of systemic therapies for both genital and extragenital LS found oral corticosteroids and methotrexate were the most-reported systemic treatment regimens.31 Use of biologics in LS has been reported, with cases utilizing adalimumab for VLS and dupilumab for extragenital LS. Use of Janus kinase inhibitors including abrocitinib and baricitinib also has been reported for LS.31 A clinical trial to evaluate the safety and efficacy of topical ruxolitinib in VLS was recently completed (ClinicalTrials.govidentifier NCT05593445). Future research studies likely will focus on the safety and efficacy of targeted and steroid-sparing therapies for patients with VLS.
Final Thoughts
Vulvar lichen sclerosus increasingly is becoming recognized as a chronic genital skin condition that impacts QOL and health outcomes, with a need to develop more effective and safe evidence-based therapies. Recent literature has focused on the importance of developing and standardizing disease outcomes; identifying disease associations including the role of cutaneous hormones and microbiome alterations; characterizing histologic and clinical variants; and staying up-to-date on management, including the need for understanding patient perceptions of chronic topical steroid therapy. Each of these are important updates for clinicians to consider when caring for patients with VLS. Future studies likely will focus on elucidating disease etiology and mechanisms to gain a better understanding of VLS pathogenesis and potential targets for therapies as well as implementation of clinical trials that incorporate standardized outcome domains to test efficacy and safety of additional therapies.
Vulvar lichen sclerosus (VLS) is an underserved area in medicine and dermatology. We discuss updates in VLS, which include the following: (1) development of core outcome domains to include in all future clinical trials, with current efforts focused on determining outcome measurements for each domain; (2) increased understanding of the impact VLS has on quality-of-life (QOL) outcomes; (3) expanded disease associations; (4) clinical and histologic variants, including vestibular sclerosis and nonsclerotic VLS; and (5) updates in management of VLS.
Core Outcomes Measures
The burden of VLS is challenging to quantify, with little agreement among experts.1 Recently there has been a focus on developing scoring scales to measure disease progression and treatment response. Simpson et al2 pioneered the development of a core outcome set to be included in all future clinical trials for genital lichen sclerosus (LS)—clinical (visible) signs, symptoms, and LS-specific QOL.
Although there is no standardized method for assessing disease severity, various scales have been proposed to measure clinical findings in VLS, such as the vulvar architecture severity scale3 as well as the clinical LS score,4 which is the only validated scale to incorporate the signs and architectural changes identified by a 2018 Delphi consensus group of the International Society for the Study of Vulvovaginal Disease.5 Work is ongoing to identify and evaluate outcome measurement instruments for each of the 3 core outcome domains.
Increased Understanding of QOL Impacts
Pain, pruritus, impairment of sexual function, genitourinary complications, architectural changes, and risk for squamous cell carcinoma (SCC) all have been well established as VLS sequelae.6,7 Recent studies have focused on the QOL impact and associations with psychiatric comorbidities. A matched case-control study found that LS was significantly associated with depression and anxiety among US women (P<.001), and individuals with LS had a more than 2-fold increased odds of receiving a diagnosis of depression or anxiety.8
A review evaluating QOL outcomes in LS found that overall QOL was impaired. Female patients reported worse QOL in the work-school domain of the dermatology life quality index compared with male counterparts.9
Finally, a study exploring the experiences of patients living with VLS highlighted the secrecy and stigma of the condition,10 which serves as a call to action to improve the general population’s knowledge about vulvar anatomy and create change in societal attitudes on vulvar conditions.
Although there are several instruments assessing vulvar-specific QOL, most are for patients with vulvar cancer and focus on sexual function. In 2020, Saunderson et al11 published the 15-item vulvar quality of life index (VQLI), which has broad implications for measuring vulvar disease burden and is an important tool for standardizing vulvar disease measurements and outcomes for clinical research.12 The VQLI, though not specific to VLS, consists of 4 domains to assess vulvar QOL including symptoms, anxiety, activities of daily living, and sexuality. Studies have evaluated this scoring system in patients with VLS, with 1 study finding that VQLI correlated with clinician-rated severity scores (P=.01) and overall patient itch/discomfort score (P<.001) in VLS.13,14
Expanded Disease Associations
Lichen sclerosus has a well-known association with vulvar SCC and other autoimmune conditions, including thyroid disease and bullous pemphigoid.15-17 Recent studies also have revealed an association between LS and psoriasis.18 A case-control study from a single center found VLS was associated with elevated body mass index, statin usage, and cholecystectomy.19 Gynecologic pain syndromes, interstitial cystitis, urinary incontinence, and some gastrointestinal tract disorders including celiac disease also have been found to be increased in patients with VLS.20 Finally, the incidence of cutaneous immune-related adverse events such as LS has increased as the use of immune checkpoint therapies as anticancer treatments has expanded.21 Clinicians should be aware of these potential disease associations when caring for patients with VLS.
The incidence of VLS is higher in lower estrogen states throughout the lifespan, and a recent case-control study evaluated the cutaneous hormonal and microbial landscapes in postmenopausal patients (6 patients with VLS; 12 controls).22 Levels of the following cutaneous hormones in the groin were found to be altered in patients with VLS compared with controls: estrone (lower; P=.006), progesterone (higher; P<.0001), and testosterone (lower; P=.02). The authors found that most hormone levels normalized following treatment with a topical steroid. Additionally, bacterial microbiome alterations were seen in patients with VLS compared with controls. Thus, cutaneous sex hormone and skin microbiome alterations may be associated with VLS.22
Updates in Clinical and Histologic Variants
Less-recognized variants of VLS have been characterized in recent years. Vestibular sclerosis is a variant of VLS with unique clinical and histopathologic features; it is characterized by involvement localized to the anterior vestibule and either an absent or sparse lymphocytic infiltrate on histopathology.23,24 Nonsclerotic VLS is a variant with clinical features consistent with VLS that does not exhibit dermal sclerosis on histopathology. Thus, a diagnosis of nonsclerotic VLS requires clinicopathologic correlation. Four nonsclerotic histopathologic subtypes are proposed: lichenoid, hypertrophic lichenoid, dermal fibrosis without acanthosis, and dermal fibrosis with acanthosis.25 Longitudinal studies that correlate duration, signs, and symptoms will be important to further understand these variants.
Management Updates
First-line treatment of VLS still consists of ultrapotent topical corticosteroids with chronic maintenance therapy (usually lifetime) to decrease the risk for SCC and architectural changes.26 However, a survey across social media platforms found steroid phobia is common in patients with VLS (N=865), with approximately 40% of respondents endorsing waiting as long as they could before using topical corticosteroids and stopping as soon as possible.27 Clinicians should be aware of possible patient perceptions in the use of chronic steroids when discussing this therapy.
Randomized controlled trials utilizing fractional CO2 devices for VLS have been performed with conflicting results and no consensus regarding outcome measurement.28,29 Additionally, long-term disease outcomes following laser use have not been investigated. Although there is evidence that both ablative and nonablative devices can improve symptoms and signs, there is no evidence that they offer a cure for a chronic inflammatory skin condition. Current evidence suggests that even for patients undergoing these procedures, maintenance therapy is still essential to prevent sequelae.30 Future studies incorporating standardized outcome measures will be important for assessing the benefits of laser therapy in VLS. Finally, the reasons why topical corticosteroids may fail in an individual patient are multifaceted and should be explored thoroughly when considering laser therapy for VLS.
Studies evaluating the role of systemic therapies for refractory cases of VLS have expanded. A systematic review of systemic therapies for both genital and extragenital LS found oral corticosteroids and methotrexate were the most-reported systemic treatment regimens.31 Use of biologics in LS has been reported, with cases utilizing adalimumab for VLS and dupilumab for extragenital LS. Use of Janus kinase inhibitors including abrocitinib and baricitinib also has been reported for LS.31 A clinical trial to evaluate the safety and efficacy of topical ruxolitinib in VLS was recently completed (ClinicalTrials.govidentifier NCT05593445). Future research studies likely will focus on the safety and efficacy of targeted and steroid-sparing therapies for patients with VLS.
Final Thoughts
Vulvar lichen sclerosus increasingly is becoming recognized as a chronic genital skin condition that impacts QOL and health outcomes, with a need to develop more effective and safe evidence-based therapies. Recent literature has focused on the importance of developing and standardizing disease outcomes; identifying disease associations including the role of cutaneous hormones and microbiome alterations; characterizing histologic and clinical variants; and staying up-to-date on management, including the need for understanding patient perceptions of chronic topical steroid therapy. Each of these are important updates for clinicians to consider when caring for patients with VLS. Future studies likely will focus on elucidating disease etiology and mechanisms to gain a better understanding of VLS pathogenesis and potential targets for therapies as well as implementation of clinical trials that incorporate standardized outcome domains to test efficacy and safety of additional therapies.
- Sheinis M, Green N, Vieira-Baptista P, et al. Adult vulvar lichen sclerosus: can experts agree on the assessment of disease severity? J Low Genit Tract Dis. 2020;24:295-298. doi:10.1097/LGT.0000000000000534
- Simpson RC, Kirtschig G, Selk A, et al. Core outcome domains for lichen sclerosus: a CORALS initiative consensus statement. Br J Dermatol. 2023;188:628-635. doi:10.1093/bjd/ljac145
- Almadori A, Zenner N, Boyle D, et al. Development and validation of a clinical grading scale to assess the vulvar region: the Vulvar Architecture Severity Scale. Aesthet Surg J. 2020;40:1319-1326. doi:10.1093/asj/sjz342
- Erni B, Navarini AA, Huang D, et al. Proposition of a severity scale for lichen sclerosus: the “Clinical Lichen Sclerosus Score.” Dermatol Ther. 2021;34:E14773. doi:10.1111/dth.14773
- Sheinis M, Selk A. Development of the Adult Vulvar Lichen Sclerosus Severity Scale—a Delphi Consensus Exercise for Item Generation. J Low Genit Tract Dis. 2018;22:66-73. doi:10.1097/LGT.0000000000000361
- Mauskar MM, Marathe K, Venkatesan A, et al. Vulvar diseases. J Am Acad Dermatol. 2020;82:1287-1298. doi:10.1016/j.jaad.2019.10.077
- Wijaya M, Lee G, Fischer G. Why do some patients with vulval lichen sclerosus on long-term topical corticosteroid treatment experience ongoing poor quality of life? Australas J Dermatol. 2022;63:463-472. doi:10.1111/ajd.13926
- Fan R, Leasure AC, Maisha FI, et al. Depression and anxiety in patients with lichen sclerosus. JAMA Dermatol. 2022;158:953-954. doi:10.1001/jamadermatol.2022.1964
- Ranum A, Pearson DR. The impact of genital lichen sclerosus and lichen planus on quality of life: a review. Int J Womens Dermatol. 2022;8:E042. doi:10.1097/JW9.0000000000000042
- Arnold S, Fernando S, Rees S. Living with vulval lichen sclerosus: a qualitative interview study. Br J Dermatol. 2022;187:909-918. doi:10.1111/bjd.21777
- Saunderson RB, Harris V, Yeh R, et al. Vulvar quality of life index (VQLI)—a simple tool to measure quality of life in patients with vulvar disease. Australas J Dermatol. 2020;61:152-157. doi:10.1111/ajd.13235
- Pyle HJ, Evans JC, Vandergriff TW, et al. Vulvar lichen sclerosus clinical severity scales and histopathologic correlation: a case series. Am J Dermatopathol. 2023;45:588-592. doi:10.1097/DAD.0000000000002471
- Wijaya M, Lee G, Fischer G. Quality of life of women with untreated vulval lichen sclerosus assessed with vulval quality of life index (VQLI) [published online January 28, 2021]. Australas J Dermatol. 2021;62:177-182. doi:10.1111/ajd.13530
- Felmingham C, Chan L, Doyle LW, et al. The Vulval Disease Quality of Life Index in women with vulval lichen sclerosus correlates with clinician and symptom scores [published online November 14, 2019]. Australas J Dermatol. 2020;61:110-118. doi:10.1111/ajd.13197
- Walsh ML, Leonard N, Shawki H, et al. Lichen sclerosus and immunobullous disease. J Low Genit Tract Dis. 2012;16:468-470. doi:10.1097/LGT.0b013e31825e9b18
- Chin S, Scurry J, Bradford J, et al. Association of topical corticosteroids with reduced vulvar squamous cell carcinoma recurrence in patients with vulvar lichen sclerosus. JAMA Dermatol. 2020;156:813. doi:10.1001/jamadermatol.2020.1074
- Fan R, Leasure AC, Maisha FI, et al. Thyroid disorders associated with lichen sclerosus: a case–control study in the All of Us Research Program. Br J Dermatol. 2022;187:797-799. doi:10.1111/bjd.21702
- Fan R, Leasure AC, Little AJ, et al. Lichen sclerosus among women with psoriasis: a cross-sectional study in the All of Us research program. J Am Acad Dermatol. 2023;88:1175-1177. doi:10.1016/j.jaad.2022.12.012
- Luu Y, Cheng AL, Reisz C. Elevated body mass index, statin use, and cholecystectomy are associated with vulvar lichen sclerosus: a retrospective, case-control study. J Am Acad Dermatol. 2023;88:1376-1378. doi:10.1016/j.jaad.2023.01.023
- Söderlund JM, Hieta NK, Kurki SH, et al. Comorbidity of urogynecological and gastrointestinal disorders in female patients with lichen sclerosus. J Low Genit Tract Dis. 2023;2:156-160. doi:10.1097/LGT.0000000000000727
- Shin L, Smith J, Shiu J, et al. Association of lichen sclerosus and morphea with immune checkpoint therapy: a systematic review. Int J Womens Dermatol. 2023;9:E070. doi:10.1097/JW9.0000000000000070
- Pyle HJ, Evans JC, Artami M, et al. Assessment of the cutaneous hormone landscapes and microbiomes in vulvar lichen sclerosus [published online February 16, 2024]. J Invest Dermatol. 2024:S0022-202X(24)00111-8. doi:10.1016/j.jid.2024.01.027
- Day T, Burston K, Dennerstein G, et al. Vestibulovaginal sclerosis versus lichen sclerosus. Int J Gynecol Pathol. 2018;37:356-363. doi:10.1097/PGP.0000000000000441
- Croker BA, Scurry JP, Petry FM, et al. Vestibular sclerosis: is this a new, distinct clinicopathological entity? J Low Genit Tract Dis. 2018;22:260-263. doi:10.1097/LGT.0000000000000404
- Day T, Selim MA, Allbritton JI, et al. Nonsclerotic lichen sclerosus: definition of a concept and pathologic description. J Low Genit Tract Dis. 2023;27:358-364. doi:10.1097/LGT.0000000000000760
- Lee A, Bradford J, Fischer G. Long-term management of adult vulvar lichen sclerosus: a prospective cohort study of 507 women. JAMA Dermatol. 2015;151:1061. doi:10.1001/jamadermatol.2015.0643
- Delpero E, Sriharan A, Selk A. Steroid phobia in patients with vulvar lichen sclerosus. J Low Genit Tract Dis. 2023;27:286-290. doi:10.1097/LGT.0000000000000753
- Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978. doi:10.1097/AOG.0000000000004332
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:979-987. doi:10.1097/AOG.0000000000004409
- Li HOY, Bailey AMJ, Tan MG, Dover JS. Lasers as an adjuvant for vulvar lichen sclerosus: a systematic review and meta-analysis. J Am Acad Dermatol. 2022;86:694-696. doi:10.1016/j.jaad.2021.02.081
- Hargis A, Ngo M, Kraus CN, et al. Systemic therapy for lichen sclerosus: a systematic review [published online November 4, 2023]. J Low Genit Tract Dis. doi:10.1097/LGT.0000000000000775
- Sheinis M, Green N, Vieira-Baptista P, et al. Adult vulvar lichen sclerosus: can experts agree on the assessment of disease severity? J Low Genit Tract Dis. 2020;24:295-298. doi:10.1097/LGT.0000000000000534
- Simpson RC, Kirtschig G, Selk A, et al. Core outcome domains for lichen sclerosus: a CORALS initiative consensus statement. Br J Dermatol. 2023;188:628-635. doi:10.1093/bjd/ljac145
- Almadori A, Zenner N, Boyle D, et al. Development and validation of a clinical grading scale to assess the vulvar region: the Vulvar Architecture Severity Scale. Aesthet Surg J. 2020;40:1319-1326. doi:10.1093/asj/sjz342
- Erni B, Navarini AA, Huang D, et al. Proposition of a severity scale for lichen sclerosus: the “Clinical Lichen Sclerosus Score.” Dermatol Ther. 2021;34:E14773. doi:10.1111/dth.14773
- Sheinis M, Selk A. Development of the Adult Vulvar Lichen Sclerosus Severity Scale—a Delphi Consensus Exercise for Item Generation. J Low Genit Tract Dis. 2018;22:66-73. doi:10.1097/LGT.0000000000000361
- Mauskar MM, Marathe K, Venkatesan A, et al. Vulvar diseases. J Am Acad Dermatol. 2020;82:1287-1298. doi:10.1016/j.jaad.2019.10.077
- Wijaya M, Lee G, Fischer G. Why do some patients with vulval lichen sclerosus on long-term topical corticosteroid treatment experience ongoing poor quality of life? Australas J Dermatol. 2022;63:463-472. doi:10.1111/ajd.13926
- Fan R, Leasure AC, Maisha FI, et al. Depression and anxiety in patients with lichen sclerosus. JAMA Dermatol. 2022;158:953-954. doi:10.1001/jamadermatol.2022.1964
- Ranum A, Pearson DR. The impact of genital lichen sclerosus and lichen planus on quality of life: a review. Int J Womens Dermatol. 2022;8:E042. doi:10.1097/JW9.0000000000000042
- Arnold S, Fernando S, Rees S. Living with vulval lichen sclerosus: a qualitative interview study. Br J Dermatol. 2022;187:909-918. doi:10.1111/bjd.21777
- Saunderson RB, Harris V, Yeh R, et al. Vulvar quality of life index (VQLI)—a simple tool to measure quality of life in patients with vulvar disease. Australas J Dermatol. 2020;61:152-157. doi:10.1111/ajd.13235
- Pyle HJ, Evans JC, Vandergriff TW, et al. Vulvar lichen sclerosus clinical severity scales and histopathologic correlation: a case series. Am J Dermatopathol. 2023;45:588-592. doi:10.1097/DAD.0000000000002471
- Wijaya M, Lee G, Fischer G. Quality of life of women with untreated vulval lichen sclerosus assessed with vulval quality of life index (VQLI) [published online January 28, 2021]. Australas J Dermatol. 2021;62:177-182. doi:10.1111/ajd.13530
- Felmingham C, Chan L, Doyle LW, et al. The Vulval Disease Quality of Life Index in women with vulval lichen sclerosus correlates with clinician and symptom scores [published online November 14, 2019]. Australas J Dermatol. 2020;61:110-118. doi:10.1111/ajd.13197
- Walsh ML, Leonard N, Shawki H, et al. Lichen sclerosus and immunobullous disease. J Low Genit Tract Dis. 2012;16:468-470. doi:10.1097/LGT.0b013e31825e9b18
- Chin S, Scurry J, Bradford J, et al. Association of topical corticosteroids with reduced vulvar squamous cell carcinoma recurrence in patients with vulvar lichen sclerosus. JAMA Dermatol. 2020;156:813. doi:10.1001/jamadermatol.2020.1074
- Fan R, Leasure AC, Maisha FI, et al. Thyroid disorders associated with lichen sclerosus: a case–control study in the All of Us Research Program. Br J Dermatol. 2022;187:797-799. doi:10.1111/bjd.21702
- Fan R, Leasure AC, Little AJ, et al. Lichen sclerosus among women with psoriasis: a cross-sectional study in the All of Us research program. J Am Acad Dermatol. 2023;88:1175-1177. doi:10.1016/j.jaad.2022.12.012
- Luu Y, Cheng AL, Reisz C. Elevated body mass index, statin use, and cholecystectomy are associated with vulvar lichen sclerosus: a retrospective, case-control study. J Am Acad Dermatol. 2023;88:1376-1378. doi:10.1016/j.jaad.2023.01.023
- Söderlund JM, Hieta NK, Kurki SH, et al. Comorbidity of urogynecological and gastrointestinal disorders in female patients with lichen sclerosus. J Low Genit Tract Dis. 2023;2:156-160. doi:10.1097/LGT.0000000000000727
- Shin L, Smith J, Shiu J, et al. Association of lichen sclerosus and morphea with immune checkpoint therapy: a systematic review. Int J Womens Dermatol. 2023;9:E070. doi:10.1097/JW9.0000000000000070
- Pyle HJ, Evans JC, Artami M, et al. Assessment of the cutaneous hormone landscapes and microbiomes in vulvar lichen sclerosus [published online February 16, 2024]. J Invest Dermatol. 2024:S0022-202X(24)00111-8. doi:10.1016/j.jid.2024.01.027
- Day T, Burston K, Dennerstein G, et al. Vestibulovaginal sclerosis versus lichen sclerosus. Int J Gynecol Pathol. 2018;37:356-363. doi:10.1097/PGP.0000000000000441
- Croker BA, Scurry JP, Petry FM, et al. Vestibular sclerosis: is this a new, distinct clinicopathological entity? J Low Genit Tract Dis. 2018;22:260-263. doi:10.1097/LGT.0000000000000404
- Day T, Selim MA, Allbritton JI, et al. Nonsclerotic lichen sclerosus: definition of a concept and pathologic description. J Low Genit Tract Dis. 2023;27:358-364. doi:10.1097/LGT.0000000000000760
- Lee A, Bradford J, Fischer G. Long-term management of adult vulvar lichen sclerosus: a prospective cohort study of 507 women. JAMA Dermatol. 2015;151:1061. doi:10.1001/jamadermatol.2015.0643
- Delpero E, Sriharan A, Selk A. Steroid phobia in patients with vulvar lichen sclerosus. J Low Genit Tract Dis. 2023;27:286-290. doi:10.1097/LGT.0000000000000753
- Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978. doi:10.1097/AOG.0000000000004332
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:979-987. doi:10.1097/AOG.0000000000004409
- Li HOY, Bailey AMJ, Tan MG, Dover JS. Lasers as an adjuvant for vulvar lichen sclerosus: a systematic review and meta-analysis. J Am Acad Dermatol. 2022;86:694-696. doi:10.1016/j.jaad.2021.02.081
- Hargis A, Ngo M, Kraus CN, et al. Systemic therapy for lichen sclerosus: a systematic review [published online November 4, 2023]. J Low Genit Tract Dis. doi:10.1097/LGT.0000000000000775
Brown Plaque in the Axilla Following Immobilization of the Arm
The Diagnosis: Granular Parakeratosis
Histopathology demonstrated diffuse parakeratosis with retention of keratohyalin granules throughout the stratum corneum consistent with a diagnosis of granular parakeratosis (Figure), a rare benign cutaneous condition that is thought to occur due to a defect in epidermal differentiation. The lesion resolved without additional treatment.
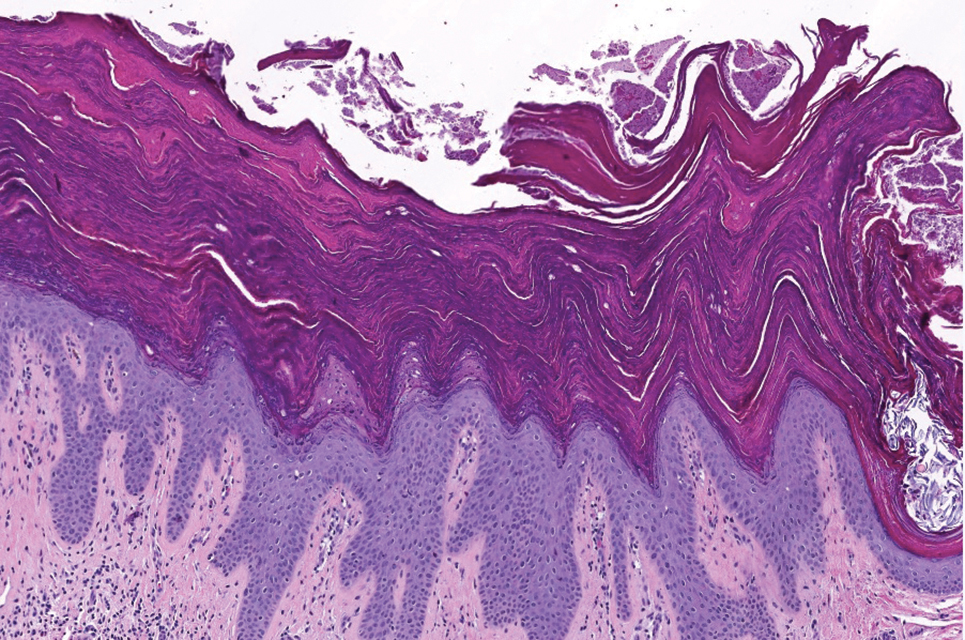
The pathogenesis of granular parakeratosis is unclear, but a reactive process in which locoregional irritation or occlusion prompts increased cell turnover and prevention of profilaggrin breakdown has been proposed.1,2 The diagnosis is linked to various precipitating agents, most commonly topical products (eg, zinc oxide, antiperspirants) and products with benzalkonium chloride (eg, laundry rinses). These agents are thought to cause retention of keratohyalin granules in the stratum corneum during epidermal differentiation.1,2
Most affected patients are middle-aged women (mean age at diagnosis, 37.8 years).2 Patients present with eruptions of erythematous, brown, hyperkeratotic patches and papules that coalesce into plaques.1,2 These lesions can be pruritic and painful or asymptomatic. They often manifest bilaterally in intertriginous sites, most commonly the axillae, groin, or inguinal folds.1,2
Treatment involves identification and removal of potential triggers including changing antiperspirants, limiting use of irritating agents (eg, topical products with strong fragrances), and reducing heat and moisture in the affected areas. If the lesion persists, stepwise treatment can be initiated with topical agents (eg, corticosteroids, vitamin D analogues, retinoids, keratolytics, calcineurin inhibitors) followed by systemic medications (eg, antibiotics, isotretinoin, antifungals, dexamethasone) and procedures (eg, botulinum toxin injections, surgery, laser, cryotherapy).1,2
Unilateral granular parakeratosis, as seen in our patient, is an uncommon manifestation. Our case supports the theory that occlusion is a precipitating factor for this condition, given persistent axillary exposure to heat, sweat, and friction in the setting of limb immobilization.3
Granular parakeratosis is a challenge to diagnose due to clinical overlap with several other cutaneous conditions; histopathologic confirmation is required. Fox- Fordyce disease is a rare condition that is thought to result from keratin buildup or occlusion of apocrine or apoeccrine sweat ducts leading to duct rupture and surrounding inflammation.4 Common triggers include laser hair removal, hormonal changes, and living conditions that promote hot and humid environments.5 It can manifest similarly to granular parakeratosis, with eruptions of multiple red-violet papules that appear bilaterally in aprocine gland–rich areas, including the axillae and less commonly the genital, periareolar, thoracic, abdominal, and facial areas.4,5 However, most patients with Fox-Fordyce disease tend to be younger females (aged 13–35 years) with severely pruritic lesions,4,5 unlike our patient. In addition, histopathology shows hyperkeratosis, hair follicle plugging, and sweat gland and duct dilation.4
Seborrheic keratoses are common benign epidermal tumors caused by an overproliferation of immature keratinocytes.6,7 Similar to granular parakeratosis, they commonly manifest in older adults as hyperpigmented, well-demarcated, verrucous plaques with a hyperkeratotic surface.6 However, they are more common on the face, neck, trunk, and extremities, and they tend to be asymptomatic, differentiating them from granular parakerosis.6 Histopathology demonstrates a papillomatous epidermal surface, large capillaries in the dermal papillae, and intraepidermal and pseudohorn epidermal cysts.7
Inverse lichen planus, a variant of lichen planus, is a rare inflammatory condition that involves the lysis of basal keratinocytes by CD8+ lymphocytes.8 Similar to granular parakeratosis, lichen planus commonly affects middle-aged women (aged 30–60 years), and this particular variant manifests with asymptomatic or mildly pruritic, hyperpigmented patches and plaques in intertriginous areas. Although it also shows hyperkeratosis on histopathology, it can be differentiated from granular parakeratosis by the additional findings of epidermal hypergranulosis, sawtooth acanthosis of rete ridges, apoptotic keratinocytes in the dermoepidermal junction, and lymphocytic infiltrate in the upper dermis.8
Hailey-Hailey disease (also known as familial benign pemphigus) is a rare condition caused by an autosomaldominant mutation affecting intracellular calcium signaling that impairs keratinocyte adhesion.9 Similar to granular parakeratosis, it is most common in middle-aged adults (aged 30–40 years) and manifests as pruritic and burning lesions in symmetric intertriginous areas that also can be triggered by heat and sweating. However, patients present with recurrent blistering and vesicular lesions that may lead to erosions and secondary infections, which reduced clinical suspicion for this diagnosis in our patient. Histopathology shows suprabasilar and intraepidermal clefts, full-thickness acantholysis, protruding dermal papillae, and a perivascular lymphocytic infiltrate in the superficial dermis.9
- Ding CY, Liu H, Khachemoune A. Granular parakeratosis: a comprehensive review and a critical reappraisal. Am J Clin Dermatol. 2015;16:495-500. doi:10.1007/s40257-015-0148-2
- Ip KH, Li A. Clinical features, histology, and treatment outcomes of granular parakeratosis: a systematic review. Int J Dermatol. 2022;61:973-978. doi:10.1111/ijd.16107
- Mehregan DA, Thomas JE, Mehregan DR. Intertriginous granular parakeratosis. J Am Acad Dermatol. 1998;39:495-496. doi:10.1016/s0190-9622(98)70333-0
- Kamada A, Saga K, Jimbow K. Apoeccrine sweat duct obstruction as a cause for Fox-Fordyce disease. J Am Acad Dermatol. 2003;48:453-455. doi:10.1067/mjd.2003.93
- Salloum A, Bouferraa Y, Bazzi N, et al. Pathophysiology, clinical findings, and management of Fox-Fordyce disease: a systematic review. J Cosmet Dermatol. 2022;21:482-500. doi:10.1111/jocd.14135
- Sun MD, Halpern AC. Advances in the etiology, detection, and clinical management of seborrheic keratoses. Dermatology. 2022;238:205-217. doi:10.1159/000517070
- Minagawa A. Dermoscopy-pathology relationship in seborrheic keratosis. J Dermatol. 2017;44:518-524. doi:10.1111/1346-8138.13657
- Weston G, Payette M. Update on lichen planus and its clinical variants [published online September 16, 2015]. Int J Womens Dermatol. 2015;1:140-149. doi:10.1016/j.ijwd.2015.04.001
- Ben Lagha I, Ashack K, Khachemoune A. Hailey-Hailey disease: an update review with a focus on treatment data. Am J Clin Dermatol. 2020;21:49-68. doi:10.1007/s40257-019-00477-z
The Diagnosis: Granular Parakeratosis
Histopathology demonstrated diffuse parakeratosis with retention of keratohyalin granules throughout the stratum corneum consistent with a diagnosis of granular parakeratosis (Figure), a rare benign cutaneous condition that is thought to occur due to a defect in epidermal differentiation. The lesion resolved without additional treatment.
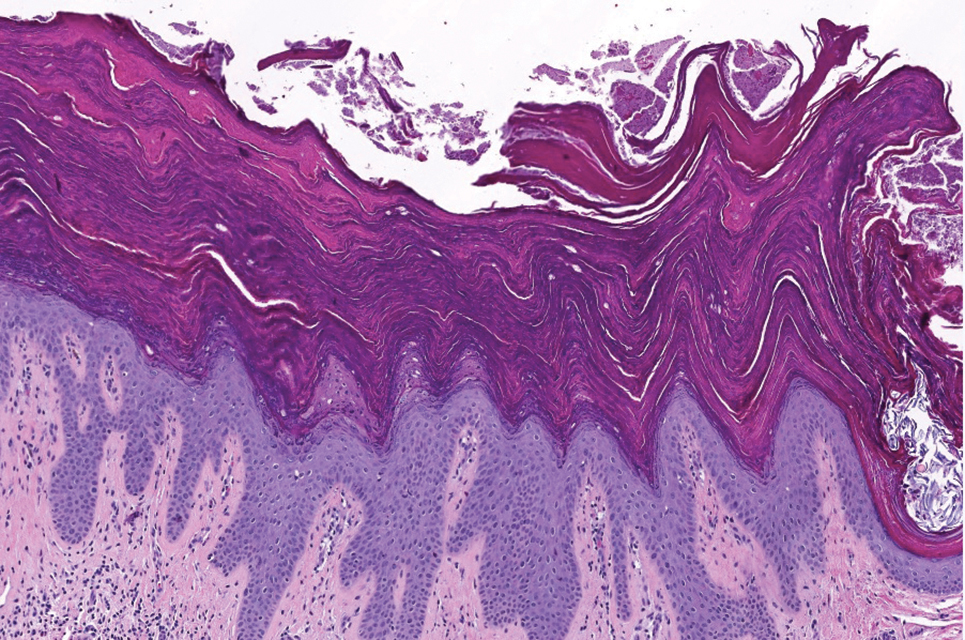
The pathogenesis of granular parakeratosis is unclear, but a reactive process in which locoregional irritation or occlusion prompts increased cell turnover and prevention of profilaggrin breakdown has been proposed.1,2 The diagnosis is linked to various precipitating agents, most commonly topical products (eg, zinc oxide, antiperspirants) and products with benzalkonium chloride (eg, laundry rinses). These agents are thought to cause retention of keratohyalin granules in the stratum corneum during epidermal differentiation.1,2
Most affected patients are middle-aged women (mean age at diagnosis, 37.8 years).2 Patients present with eruptions of erythematous, brown, hyperkeratotic patches and papules that coalesce into plaques.1,2 These lesions can be pruritic and painful or asymptomatic. They often manifest bilaterally in intertriginous sites, most commonly the axillae, groin, or inguinal folds.1,2
Treatment involves identification and removal of potential triggers including changing antiperspirants, limiting use of irritating agents (eg, topical products with strong fragrances), and reducing heat and moisture in the affected areas. If the lesion persists, stepwise treatment can be initiated with topical agents (eg, corticosteroids, vitamin D analogues, retinoids, keratolytics, calcineurin inhibitors) followed by systemic medications (eg, antibiotics, isotretinoin, antifungals, dexamethasone) and procedures (eg, botulinum toxin injections, surgery, laser, cryotherapy).1,2
Unilateral granular parakeratosis, as seen in our patient, is an uncommon manifestation. Our case supports the theory that occlusion is a precipitating factor for this condition, given persistent axillary exposure to heat, sweat, and friction in the setting of limb immobilization.3
Granular parakeratosis is a challenge to diagnose due to clinical overlap with several other cutaneous conditions; histopathologic confirmation is required. Fox- Fordyce disease is a rare condition that is thought to result from keratin buildup or occlusion of apocrine or apoeccrine sweat ducts leading to duct rupture and surrounding inflammation.4 Common triggers include laser hair removal, hormonal changes, and living conditions that promote hot and humid environments.5 It can manifest similarly to granular parakeratosis, with eruptions of multiple red-violet papules that appear bilaterally in aprocine gland–rich areas, including the axillae and less commonly the genital, periareolar, thoracic, abdominal, and facial areas.4,5 However, most patients with Fox-Fordyce disease tend to be younger females (aged 13–35 years) with severely pruritic lesions,4,5 unlike our patient. In addition, histopathology shows hyperkeratosis, hair follicle plugging, and sweat gland and duct dilation.4
Seborrheic keratoses are common benign epidermal tumors caused by an overproliferation of immature keratinocytes.6,7 Similar to granular parakeratosis, they commonly manifest in older adults as hyperpigmented, well-demarcated, verrucous plaques with a hyperkeratotic surface.6 However, they are more common on the face, neck, trunk, and extremities, and they tend to be asymptomatic, differentiating them from granular parakerosis.6 Histopathology demonstrates a papillomatous epidermal surface, large capillaries in the dermal papillae, and intraepidermal and pseudohorn epidermal cysts.7
Inverse lichen planus, a variant of lichen planus, is a rare inflammatory condition that involves the lysis of basal keratinocytes by CD8+ lymphocytes.8 Similar to granular parakeratosis, lichen planus commonly affects middle-aged women (aged 30–60 years), and this particular variant manifests with asymptomatic or mildly pruritic, hyperpigmented patches and plaques in intertriginous areas. Although it also shows hyperkeratosis on histopathology, it can be differentiated from granular parakeratosis by the additional findings of epidermal hypergranulosis, sawtooth acanthosis of rete ridges, apoptotic keratinocytes in the dermoepidermal junction, and lymphocytic infiltrate in the upper dermis.8
Hailey-Hailey disease (also known as familial benign pemphigus) is a rare condition caused by an autosomaldominant mutation affecting intracellular calcium signaling that impairs keratinocyte adhesion.9 Similar to granular parakeratosis, it is most common in middle-aged adults (aged 30–40 years) and manifests as pruritic and burning lesions in symmetric intertriginous areas that also can be triggered by heat and sweating. However, patients present with recurrent blistering and vesicular lesions that may lead to erosions and secondary infections, which reduced clinical suspicion for this diagnosis in our patient. Histopathology shows suprabasilar and intraepidermal clefts, full-thickness acantholysis, protruding dermal papillae, and a perivascular lymphocytic infiltrate in the superficial dermis.9
The Diagnosis: Granular Parakeratosis
Histopathology demonstrated diffuse parakeratosis with retention of keratohyalin granules throughout the stratum corneum consistent with a diagnosis of granular parakeratosis (Figure), a rare benign cutaneous condition that is thought to occur due to a defect in epidermal differentiation. The lesion resolved without additional treatment.
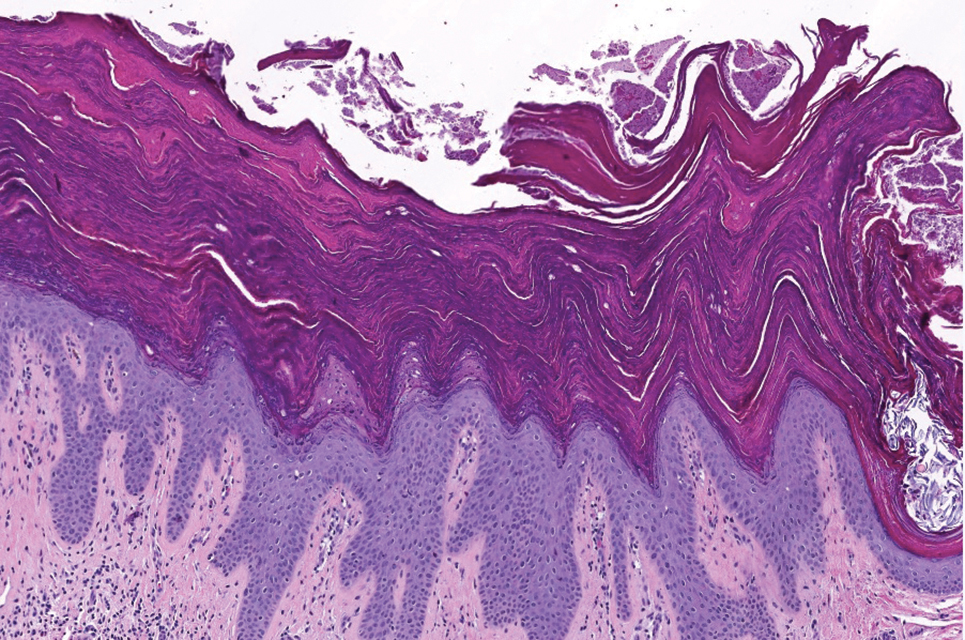
The pathogenesis of granular parakeratosis is unclear, but a reactive process in which locoregional irritation or occlusion prompts increased cell turnover and prevention of profilaggrin breakdown has been proposed.1,2 The diagnosis is linked to various precipitating agents, most commonly topical products (eg, zinc oxide, antiperspirants) and products with benzalkonium chloride (eg, laundry rinses). These agents are thought to cause retention of keratohyalin granules in the stratum corneum during epidermal differentiation.1,2
Most affected patients are middle-aged women (mean age at diagnosis, 37.8 years).2 Patients present with eruptions of erythematous, brown, hyperkeratotic patches and papules that coalesce into plaques.1,2 These lesions can be pruritic and painful or asymptomatic. They often manifest bilaterally in intertriginous sites, most commonly the axillae, groin, or inguinal folds.1,2
Treatment involves identification and removal of potential triggers including changing antiperspirants, limiting use of irritating agents (eg, topical products with strong fragrances), and reducing heat and moisture in the affected areas. If the lesion persists, stepwise treatment can be initiated with topical agents (eg, corticosteroids, vitamin D analogues, retinoids, keratolytics, calcineurin inhibitors) followed by systemic medications (eg, antibiotics, isotretinoin, antifungals, dexamethasone) and procedures (eg, botulinum toxin injections, surgery, laser, cryotherapy).1,2
Unilateral granular parakeratosis, as seen in our patient, is an uncommon manifestation. Our case supports the theory that occlusion is a precipitating factor for this condition, given persistent axillary exposure to heat, sweat, and friction in the setting of limb immobilization.3
Granular parakeratosis is a challenge to diagnose due to clinical overlap with several other cutaneous conditions; histopathologic confirmation is required. Fox- Fordyce disease is a rare condition that is thought to result from keratin buildup or occlusion of apocrine or apoeccrine sweat ducts leading to duct rupture and surrounding inflammation.4 Common triggers include laser hair removal, hormonal changes, and living conditions that promote hot and humid environments.5 It can manifest similarly to granular parakeratosis, with eruptions of multiple red-violet papules that appear bilaterally in aprocine gland–rich areas, including the axillae and less commonly the genital, periareolar, thoracic, abdominal, and facial areas.4,5 However, most patients with Fox-Fordyce disease tend to be younger females (aged 13–35 years) with severely pruritic lesions,4,5 unlike our patient. In addition, histopathology shows hyperkeratosis, hair follicle plugging, and sweat gland and duct dilation.4
Seborrheic keratoses are common benign epidermal tumors caused by an overproliferation of immature keratinocytes.6,7 Similar to granular parakeratosis, they commonly manifest in older adults as hyperpigmented, well-demarcated, verrucous plaques with a hyperkeratotic surface.6 However, they are more common on the face, neck, trunk, and extremities, and they tend to be asymptomatic, differentiating them from granular parakerosis.6 Histopathology demonstrates a papillomatous epidermal surface, large capillaries in the dermal papillae, and intraepidermal and pseudohorn epidermal cysts.7
Inverse lichen planus, a variant of lichen planus, is a rare inflammatory condition that involves the lysis of basal keratinocytes by CD8+ lymphocytes.8 Similar to granular parakeratosis, lichen planus commonly affects middle-aged women (aged 30–60 years), and this particular variant manifests with asymptomatic or mildly pruritic, hyperpigmented patches and plaques in intertriginous areas. Although it also shows hyperkeratosis on histopathology, it can be differentiated from granular parakeratosis by the additional findings of epidermal hypergranulosis, sawtooth acanthosis of rete ridges, apoptotic keratinocytes in the dermoepidermal junction, and lymphocytic infiltrate in the upper dermis.8
Hailey-Hailey disease (also known as familial benign pemphigus) is a rare condition caused by an autosomaldominant mutation affecting intracellular calcium signaling that impairs keratinocyte adhesion.9 Similar to granular parakeratosis, it is most common in middle-aged adults (aged 30–40 years) and manifests as pruritic and burning lesions in symmetric intertriginous areas that also can be triggered by heat and sweating. However, patients present with recurrent blistering and vesicular lesions that may lead to erosions and secondary infections, which reduced clinical suspicion for this diagnosis in our patient. Histopathology shows suprabasilar and intraepidermal clefts, full-thickness acantholysis, protruding dermal papillae, and a perivascular lymphocytic infiltrate in the superficial dermis.9
- Ding CY, Liu H, Khachemoune A. Granular parakeratosis: a comprehensive review and a critical reappraisal. Am J Clin Dermatol. 2015;16:495-500. doi:10.1007/s40257-015-0148-2
- Ip KH, Li A. Clinical features, histology, and treatment outcomes of granular parakeratosis: a systematic review. Int J Dermatol. 2022;61:973-978. doi:10.1111/ijd.16107
- Mehregan DA, Thomas JE, Mehregan DR. Intertriginous granular parakeratosis. J Am Acad Dermatol. 1998;39:495-496. doi:10.1016/s0190-9622(98)70333-0
- Kamada A, Saga K, Jimbow K. Apoeccrine sweat duct obstruction as a cause for Fox-Fordyce disease. J Am Acad Dermatol. 2003;48:453-455. doi:10.1067/mjd.2003.93
- Salloum A, Bouferraa Y, Bazzi N, et al. Pathophysiology, clinical findings, and management of Fox-Fordyce disease: a systematic review. J Cosmet Dermatol. 2022;21:482-500. doi:10.1111/jocd.14135
- Sun MD, Halpern AC. Advances in the etiology, detection, and clinical management of seborrheic keratoses. Dermatology. 2022;238:205-217. doi:10.1159/000517070
- Minagawa A. Dermoscopy-pathology relationship in seborrheic keratosis. J Dermatol. 2017;44:518-524. doi:10.1111/1346-8138.13657
- Weston G, Payette M. Update on lichen planus and its clinical variants [published online September 16, 2015]. Int J Womens Dermatol. 2015;1:140-149. doi:10.1016/j.ijwd.2015.04.001
- Ben Lagha I, Ashack K, Khachemoune A. Hailey-Hailey disease: an update review with a focus on treatment data. Am J Clin Dermatol. 2020;21:49-68. doi:10.1007/s40257-019-00477-z
- Ding CY, Liu H, Khachemoune A. Granular parakeratosis: a comprehensive review and a critical reappraisal. Am J Clin Dermatol. 2015;16:495-500. doi:10.1007/s40257-015-0148-2
- Ip KH, Li A. Clinical features, histology, and treatment outcomes of granular parakeratosis: a systematic review. Int J Dermatol. 2022;61:973-978. doi:10.1111/ijd.16107
- Mehregan DA, Thomas JE, Mehregan DR. Intertriginous granular parakeratosis. J Am Acad Dermatol. 1998;39:495-496. doi:10.1016/s0190-9622(98)70333-0
- Kamada A, Saga K, Jimbow K. Apoeccrine sweat duct obstruction as a cause for Fox-Fordyce disease. J Am Acad Dermatol. 2003;48:453-455. doi:10.1067/mjd.2003.93
- Salloum A, Bouferraa Y, Bazzi N, et al. Pathophysiology, clinical findings, and management of Fox-Fordyce disease: a systematic review. J Cosmet Dermatol. 2022;21:482-500. doi:10.1111/jocd.14135
- Sun MD, Halpern AC. Advances in the etiology, detection, and clinical management of seborrheic keratoses. Dermatology. 2022;238:205-217. doi:10.1159/000517070
- Minagawa A. Dermoscopy-pathology relationship in seborrheic keratosis. J Dermatol. 2017;44:518-524. doi:10.1111/1346-8138.13657
- Weston G, Payette M. Update on lichen planus and its clinical variants [published online September 16, 2015]. Int J Womens Dermatol. 2015;1:140-149. doi:10.1016/j.ijwd.2015.04.001
- Ben Lagha I, Ashack K, Khachemoune A. Hailey-Hailey disease: an update review with a focus on treatment data. Am J Clin Dermatol. 2020;21:49-68. doi:10.1007/s40257-019-00477-z
A 62-year-old woman presented to our clinic for evaluation of a brown plaque in the left axilla of 2 weeks’ duration. She had a history of a rotator cuff injury and adhesive capsulitis several months prior that required immobilization of the left arm in a shoulder orthosis for several months. After the sling was removed, she noticed the lesion and reported mild cutaneous pain. Physical examination revealed a 1.5-cm, verrucous, red-brown plaque in the left axillary vault. A shave biopsy of the plaque was performed.

