User login
Mental health assessment for gender-diverse patients
Over the past several years, the number of patients seeking gender-affirming services has exponentially increased.1 Unfortunately, the number of patients presenting for treatment has exceeded evidence-based guidelines, research, and the number of providers familiar with gender-affirming care. Many institutions and associations such as the American College of Obstetricians and Gynecologists and the World Professional Association for Transgender Health (WPATH) advocate for training of providers; however, many patients will be seen by providers who are not qualified in diagnosing gender dysphoria. As a result, many practitioners rely on the mental health evaluation of gender-diverse individuals prior to prescribing hormonal therapy or before planning surgery.
Practitioners qualified to provide mental health services can include persons within in the field of psychology, psychiatry, social work, licensed professional counseling, nursing, or family medicine (with specific training in mental health).2 WPATH also defines specific criteria as part of the mental health assessment. For example, providers should have a master’s degree or higher in clinical behavioral science, competence in using the DSM/ICD, the ability to recognize and diagnose coexisting mental health concerns, and undergo continuing education in the treatment of gender dysphoria.2 Unfortunately, the demand for gender-competent mental health professionals exceeds the number available, and many patients are seen by therapists lacking experience within this field.3 This discrepancy can present an additional barrier to the health needs of transgender patients and sometimes inhibit access to hormone therapy, or even more catastrophically, compromise their presurgical assessment and surgical outcome.
For patients seeking chest surgery (mastectomy or breast augmentation), one letter from a mental health provider is necessary. If a patient is interested in pursuing genital surgery or the removal or reproductive organs, two letters from two separate mental health providers are required. Typically, one letter is from the patient’s primary therapist, and the other is often a second opinion. These letters must include a patient’s general characteristics, psychosocial assessment results, duration of the mental health professional’s relationship with the client, an explanation that the criteria for surgery have been met, a statement supporting the patient’s request for surgery and that informed consent was obtained, and a statement that the mental health professional is available for coordination of care.2 It is crucial to delineate that while a mental health evaluation is mandated, psychotherapy is not.
A therapist’s letter is not essential prior to initiating hormones; however, it is recommended if practitioners are unfamiliar with gender-diverse patients and current standards of care. If a provider such as a family physician, endocrinologist, or obstetrician/gynecologist is knowledgeable about the diagnostic criteria for gender dysphoria, they can prescribe hormones without a therapist’s letter. Additional considerations include establishing whether a patient has persistent gender dysphoria, has the capacity to give informed consent, and has “reasonably well-controlled” mental illness.3 The prevalence of both depression and anxiety is exceptionally high in this population, whereas rates of bipolar disorder and schizophrenia mirror that of the general population.3 Mental illness is not a contraindication to hormone therapy because there is sufficient evidence to support the benefits of gender-affirming hormones in reducing both anxiety and depression.
In contrast, concurrent severe psychiatric illness (i.e., bipolar disorder, schizophrenia, borderline personality disorder) that is not well controlled could prohibit patients from undergoing gender-affirming surgeries. Even the most well-educated patients do not truly understand the process of surgery and the rigorous postoperative care required, particularly after genital surgery. Many patients underestimate the need for a support system in the postoperative period and cannot predict their emotional response after undergoing such complex procedures. During a surgical consultation, the surgeon can help identify any mental, physical, monetary, or social constraints patients may have and work closely with other providers, including a well-trained mental health professional, to optimize a patient’s surgical recovery. Ideally, patients undergoing surgery are seen at multidisciplinary centers with the capabilities of addressing these concerns.
The patient’s perspective on the need for a therapist is often mixed. Historically, therapist letters have been viewed by patients as a form of “gatekeeping” and an additional barrier they are forced to overcome to receive treatment. However, the role of a mental health provider who specializes in gender-affirming care cannot be overstated. In the context of surgery, I often try to reframe the role the therapist as an integral part of the multidisciplinary team. Mental health assessments preoperatively can better prepare patients for their upcoming surgery. More importantly, this multidisciplinary approach can help identify potential issues with coping strategies or exacerbations of other mental health conditions that may arise in the immediate postoperative period.
There is no question that exceptional gender-affirming care requires a multidisciplinary approach. Establishing strong relationships between hormone prescribers, surgeons, and behavioral health specialists in an essential step toward providing competent patient-centered care.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Ettner R. Mental health evaluation for gender confirmation surgery. Clin Plastic Surg. 2018;45(3):307-11.
2. Karasic D. Mental health care for the adult transgender patient. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia: Elsevier; 2020:8-11.
3. World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people. 7th ed. Minneapolis: WPATH; 2012.
Over the past several years, the number of patients seeking gender-affirming services has exponentially increased.1 Unfortunately, the number of patients presenting for treatment has exceeded evidence-based guidelines, research, and the number of providers familiar with gender-affirming care. Many institutions and associations such as the American College of Obstetricians and Gynecologists and the World Professional Association for Transgender Health (WPATH) advocate for training of providers; however, many patients will be seen by providers who are not qualified in diagnosing gender dysphoria. As a result, many practitioners rely on the mental health evaluation of gender-diverse individuals prior to prescribing hormonal therapy or before planning surgery.
Practitioners qualified to provide mental health services can include persons within in the field of psychology, psychiatry, social work, licensed professional counseling, nursing, or family medicine (with specific training in mental health).2 WPATH also defines specific criteria as part of the mental health assessment. For example, providers should have a master’s degree or higher in clinical behavioral science, competence in using the DSM/ICD, the ability to recognize and diagnose coexisting mental health concerns, and undergo continuing education in the treatment of gender dysphoria.2 Unfortunately, the demand for gender-competent mental health professionals exceeds the number available, and many patients are seen by therapists lacking experience within this field.3 This discrepancy can present an additional barrier to the health needs of transgender patients and sometimes inhibit access to hormone therapy, or even more catastrophically, compromise their presurgical assessment and surgical outcome.
For patients seeking chest surgery (mastectomy or breast augmentation), one letter from a mental health provider is necessary. If a patient is interested in pursuing genital surgery or the removal or reproductive organs, two letters from two separate mental health providers are required. Typically, one letter is from the patient’s primary therapist, and the other is often a second opinion. These letters must include a patient’s general characteristics, psychosocial assessment results, duration of the mental health professional’s relationship with the client, an explanation that the criteria for surgery have been met, a statement supporting the patient’s request for surgery and that informed consent was obtained, and a statement that the mental health professional is available for coordination of care.2 It is crucial to delineate that while a mental health evaluation is mandated, psychotherapy is not.
A therapist’s letter is not essential prior to initiating hormones; however, it is recommended if practitioners are unfamiliar with gender-diverse patients and current standards of care. If a provider such as a family physician, endocrinologist, or obstetrician/gynecologist is knowledgeable about the diagnostic criteria for gender dysphoria, they can prescribe hormones without a therapist’s letter. Additional considerations include establishing whether a patient has persistent gender dysphoria, has the capacity to give informed consent, and has “reasonably well-controlled” mental illness.3 The prevalence of both depression and anxiety is exceptionally high in this population, whereas rates of bipolar disorder and schizophrenia mirror that of the general population.3 Mental illness is not a contraindication to hormone therapy because there is sufficient evidence to support the benefits of gender-affirming hormones in reducing both anxiety and depression.
In contrast, concurrent severe psychiatric illness (i.e., bipolar disorder, schizophrenia, borderline personality disorder) that is not well controlled could prohibit patients from undergoing gender-affirming surgeries. Even the most well-educated patients do not truly understand the process of surgery and the rigorous postoperative care required, particularly after genital surgery. Many patients underestimate the need for a support system in the postoperative period and cannot predict their emotional response after undergoing such complex procedures. During a surgical consultation, the surgeon can help identify any mental, physical, monetary, or social constraints patients may have and work closely with other providers, including a well-trained mental health professional, to optimize a patient’s surgical recovery. Ideally, patients undergoing surgery are seen at multidisciplinary centers with the capabilities of addressing these concerns.
The patient’s perspective on the need for a therapist is often mixed. Historically, therapist letters have been viewed by patients as a form of “gatekeeping” and an additional barrier they are forced to overcome to receive treatment. However, the role of a mental health provider who specializes in gender-affirming care cannot be overstated. In the context of surgery, I often try to reframe the role the therapist as an integral part of the multidisciplinary team. Mental health assessments preoperatively can better prepare patients for their upcoming surgery. More importantly, this multidisciplinary approach can help identify potential issues with coping strategies or exacerbations of other mental health conditions that may arise in the immediate postoperative period.
There is no question that exceptional gender-affirming care requires a multidisciplinary approach. Establishing strong relationships between hormone prescribers, surgeons, and behavioral health specialists in an essential step toward providing competent patient-centered care.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Ettner R. Mental health evaluation for gender confirmation surgery. Clin Plastic Surg. 2018;45(3):307-11.
2. Karasic D. Mental health care for the adult transgender patient. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia: Elsevier; 2020:8-11.
3. World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people. 7th ed. Minneapolis: WPATH; 2012.
Over the past several years, the number of patients seeking gender-affirming services has exponentially increased.1 Unfortunately, the number of patients presenting for treatment has exceeded evidence-based guidelines, research, and the number of providers familiar with gender-affirming care. Many institutions and associations such as the American College of Obstetricians and Gynecologists and the World Professional Association for Transgender Health (WPATH) advocate for training of providers; however, many patients will be seen by providers who are not qualified in diagnosing gender dysphoria. As a result, many practitioners rely on the mental health evaluation of gender-diverse individuals prior to prescribing hormonal therapy or before planning surgery.
Practitioners qualified to provide mental health services can include persons within in the field of psychology, psychiatry, social work, licensed professional counseling, nursing, or family medicine (with specific training in mental health).2 WPATH also defines specific criteria as part of the mental health assessment. For example, providers should have a master’s degree or higher in clinical behavioral science, competence in using the DSM/ICD, the ability to recognize and diagnose coexisting mental health concerns, and undergo continuing education in the treatment of gender dysphoria.2 Unfortunately, the demand for gender-competent mental health professionals exceeds the number available, and many patients are seen by therapists lacking experience within this field.3 This discrepancy can present an additional barrier to the health needs of transgender patients and sometimes inhibit access to hormone therapy, or even more catastrophically, compromise their presurgical assessment and surgical outcome.
For patients seeking chest surgery (mastectomy or breast augmentation), one letter from a mental health provider is necessary. If a patient is interested in pursuing genital surgery or the removal or reproductive organs, two letters from two separate mental health providers are required. Typically, one letter is from the patient’s primary therapist, and the other is often a second opinion. These letters must include a patient’s general characteristics, psychosocial assessment results, duration of the mental health professional’s relationship with the client, an explanation that the criteria for surgery have been met, a statement supporting the patient’s request for surgery and that informed consent was obtained, and a statement that the mental health professional is available for coordination of care.2 It is crucial to delineate that while a mental health evaluation is mandated, psychotherapy is not.
A therapist’s letter is not essential prior to initiating hormones; however, it is recommended if practitioners are unfamiliar with gender-diverse patients and current standards of care. If a provider such as a family physician, endocrinologist, or obstetrician/gynecologist is knowledgeable about the diagnostic criteria for gender dysphoria, they can prescribe hormones without a therapist’s letter. Additional considerations include establishing whether a patient has persistent gender dysphoria, has the capacity to give informed consent, and has “reasonably well-controlled” mental illness.3 The prevalence of both depression and anxiety is exceptionally high in this population, whereas rates of bipolar disorder and schizophrenia mirror that of the general population.3 Mental illness is not a contraindication to hormone therapy because there is sufficient evidence to support the benefits of gender-affirming hormones in reducing both anxiety and depression.
In contrast, concurrent severe psychiatric illness (i.e., bipolar disorder, schizophrenia, borderline personality disorder) that is not well controlled could prohibit patients from undergoing gender-affirming surgeries. Even the most well-educated patients do not truly understand the process of surgery and the rigorous postoperative care required, particularly after genital surgery. Many patients underestimate the need for a support system in the postoperative period and cannot predict their emotional response after undergoing such complex procedures. During a surgical consultation, the surgeon can help identify any mental, physical, monetary, or social constraints patients may have and work closely with other providers, including a well-trained mental health professional, to optimize a patient’s surgical recovery. Ideally, patients undergoing surgery are seen at multidisciplinary centers with the capabilities of addressing these concerns.
The patient’s perspective on the need for a therapist is often mixed. Historically, therapist letters have been viewed by patients as a form of “gatekeeping” and an additional barrier they are forced to overcome to receive treatment. However, the role of a mental health provider who specializes in gender-affirming care cannot be overstated. In the context of surgery, I often try to reframe the role the therapist as an integral part of the multidisciplinary team. Mental health assessments preoperatively can better prepare patients for their upcoming surgery. More importantly, this multidisciplinary approach can help identify potential issues with coping strategies or exacerbations of other mental health conditions that may arise in the immediate postoperative period.
There is no question that exceptional gender-affirming care requires a multidisciplinary approach. Establishing strong relationships between hormone prescribers, surgeons, and behavioral health specialists in an essential step toward providing competent patient-centered care.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Ettner R. Mental health evaluation for gender confirmation surgery. Clin Plastic Surg. 2018;45(3):307-11.
2. Karasic D. Mental health care for the adult transgender patient. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia: Elsevier; 2020:8-11.
3. World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people. 7th ed. Minneapolis: WPATH; 2012.
Clinical characteristics of recurrent RIME elucidated in chart review
INDIANAPOLIS – , in a single-center retrospective study. In addition, 71% of patients with recurrent disease experienced 1-2 recurrences – episodes that were generally milder and occurred at variable intervals.
Those are among key findings from the study of 50 patients with RIME, presented by Catherina X. Pan at the annual meeting of the Society for Pediatric Dermatology.
Reactive infectious mucocutaneous eruption (RIME) is a novel term encompassing an array of rare, parainfectious mucositis diseases, noted Ms. Pan, a fourth-year medical student at Harvard Medical School, Boston. Previously known as Mycoplasma pneumoniae-induced rash and mucositis (MIRM), common clinical characteristics of RIME include less than 10% body surface area involvement of polymorphic skin lesions (vesiculobullous or targetoid macules/papules); erosive oral, genital, and/or ocular mucositis involving more than two sites, and evidence of prior infection including but not limited to upper respiratory infection, fever, and cough.
In addition to M. pneumoniae, other pathogens have been implicated, she said. “While the underlying etiology of the disease is not entirely clear, it’s become increasingly known that RIME tends to recur in a subset of patients.”
A cohort study of 13 patients with RIME found that Black race, male sex, and older age were predominant among the five patients who developed recurrent disease.
The estimated recurrence rate is between 8% and 38%, but the clinical characteristics of patients who develop recurrent RIME tend to be poorly understood, Ms. Pan said.
Along with her mentor, Sadaf Hussain, MD, of the department of dermatology at Boston Children’s Hospital, Ms. Pan conducted a retrospective chart review to characterize the clinical history and course of disease in patients diagnosed with recurrent RIME. They extracted data between January of 2000 and March of 2022 using ICD-10 codes used by board-certified dermatologists at Boston Children’s Hospital, as well as a text search for RIME or MIRM in the dermatology notes. Patients were included if they had a RIME/MIRM diagnosis by a board-certified dermatologist and/or infection on PCR/serology and mucositis involvement with limited skin involvement.
The study population included 50 patients: 24 with recurrent RIME and 26 with isolated RIME. The majority (66%) were male, and the mean age of RIME onset was between 11 and 12 years old, which is up to two years younger than previously reported in the case series of 13 patients. Most of the study participants (79%) were White, but there were no significant differences in patients who had recurrent RIME and those who had isolated RIME in terms of age, sex, or race.
Isolated vs. recurrent RIME
However, compared with patients who had isolated RIME, a greater proportion of those with recurrent RIME had a history of atopic disease (46% vs. 23%, respectively; P = .136), as well as a history of tonsillectomy and adenoidectomy (25% vs. 4%; P = .045). “This has not been previously observed, but it may generate a hypothesis that patients with a history of frequent infection as well as amplified immune responses may be associated with disease recurrence,” Ms. Pan said.
The average number of episodes among patients with recurrent RIME was 3.5 and the interval between episodes was variable, at a mean of 10.2 months. Ms. Pan reported that 71% of recurrent RIME patients experienced 1-2 episodes, although one patient experienced 9 episodes.
Clinically, episodes among all patients with RIME were characterized by infectious prodromal symptoms (69%), oral lesions (95%), ocular lesions (60%), genital lesions (41%) and cutaneous lesions (40%). However, RIME recurrences were less severe and more atypical, with 49% involving only one mucosal surface and 29% involving two mucosal surfaces. Also, except for oral lesions, rates of infectious prodromal symptoms and other lesions significantly decreased among recurrences compared with initial RIME.
“Notably, we found that M. pneumoniae was the most common known cause of RIME, particularly among the initial episodes,” Ms. Pan said. “However, 61% of recurrent RIME episodes did not have a known cause in terms of infectious etiology. And, concordant with prior studies, we also found decreased severity [of RIME recurrences] as indicated by decreased rates of emergency department presentation, hospitalization, and duration of hospitalization.”
In other findings, psychiatric complications such as anxiety and depression followed the onset of RIME in 33% of those with recurrent disease and 22% of those with isolated disease. In addition, the three most common treatments among all 50 patients were systemic steroids, topical steroids, and M. pneumoniae-specific antibiotics.
“While RIME is considered as typically milder than Stevens-Johnson syndrome and toxic epidermal necrolysis with low mortality rates, it can lead to severe complications including conjunctival shrinkage, corneal ulceration and scarring, blindness, and oral, ocular, urogenital synechiae,” Ms. Pan noted. “Increased use of corticosteroids and steroid-sparing agents such as IVIG have also been observed. Multidisciplinary care with ophthalmology, urology, and mental health services is critical.”
She acknowledged certain limitations of the study, including its retrospective, single-center design, and the possibility that milder cases may have been excluded due to a lack of accurate diagnosis or referral.
Carrie C. Coughlin, MD, who was asked to comment on the study results, pointed out that nearly half (24) of patients in the cohort experienced recurrent RIME. “This is a high proportion, suggesting counseling about the possibility of recurrence is more important than previously thought,” said Dr. Coughlin, director of the section of pediatric dermatology Washington University/St. Louis Children’s Hospital.
“Fortunately, recurrent cases tended to be less severe. However, many patients had more than one recurrence, making this challenging for affected patients.”
The researchers reported having no financial disclosures. Dr. Coughlin is on the board of the Pediatric Dermatology Research Alliance (PeDRA) and the International Immunosuppression and Transplant Skin Cancer Collaborative.
INDIANAPOLIS – , in a single-center retrospective study. In addition, 71% of patients with recurrent disease experienced 1-2 recurrences – episodes that were generally milder and occurred at variable intervals.
Those are among key findings from the study of 50 patients with RIME, presented by Catherina X. Pan at the annual meeting of the Society for Pediatric Dermatology.
Reactive infectious mucocutaneous eruption (RIME) is a novel term encompassing an array of rare, parainfectious mucositis diseases, noted Ms. Pan, a fourth-year medical student at Harvard Medical School, Boston. Previously known as Mycoplasma pneumoniae-induced rash and mucositis (MIRM), common clinical characteristics of RIME include less than 10% body surface area involvement of polymorphic skin lesions (vesiculobullous or targetoid macules/papules); erosive oral, genital, and/or ocular mucositis involving more than two sites, and evidence of prior infection including but not limited to upper respiratory infection, fever, and cough.
In addition to M. pneumoniae, other pathogens have been implicated, she said. “While the underlying etiology of the disease is not entirely clear, it’s become increasingly known that RIME tends to recur in a subset of patients.”
A cohort study of 13 patients with RIME found that Black race, male sex, and older age were predominant among the five patients who developed recurrent disease.
The estimated recurrence rate is between 8% and 38%, but the clinical characteristics of patients who develop recurrent RIME tend to be poorly understood, Ms. Pan said.
Along with her mentor, Sadaf Hussain, MD, of the department of dermatology at Boston Children’s Hospital, Ms. Pan conducted a retrospective chart review to characterize the clinical history and course of disease in patients diagnosed with recurrent RIME. They extracted data between January of 2000 and March of 2022 using ICD-10 codes used by board-certified dermatologists at Boston Children’s Hospital, as well as a text search for RIME or MIRM in the dermatology notes. Patients were included if they had a RIME/MIRM diagnosis by a board-certified dermatologist and/or infection on PCR/serology and mucositis involvement with limited skin involvement.
The study population included 50 patients: 24 with recurrent RIME and 26 with isolated RIME. The majority (66%) were male, and the mean age of RIME onset was between 11 and 12 years old, which is up to two years younger than previously reported in the case series of 13 patients. Most of the study participants (79%) were White, but there were no significant differences in patients who had recurrent RIME and those who had isolated RIME in terms of age, sex, or race.
Isolated vs. recurrent RIME
However, compared with patients who had isolated RIME, a greater proportion of those with recurrent RIME had a history of atopic disease (46% vs. 23%, respectively; P = .136), as well as a history of tonsillectomy and adenoidectomy (25% vs. 4%; P = .045). “This has not been previously observed, but it may generate a hypothesis that patients with a history of frequent infection as well as amplified immune responses may be associated with disease recurrence,” Ms. Pan said.
The average number of episodes among patients with recurrent RIME was 3.5 and the interval between episodes was variable, at a mean of 10.2 months. Ms. Pan reported that 71% of recurrent RIME patients experienced 1-2 episodes, although one patient experienced 9 episodes.
Clinically, episodes among all patients with RIME were characterized by infectious prodromal symptoms (69%), oral lesions (95%), ocular lesions (60%), genital lesions (41%) and cutaneous lesions (40%). However, RIME recurrences were less severe and more atypical, with 49% involving only one mucosal surface and 29% involving two mucosal surfaces. Also, except for oral lesions, rates of infectious prodromal symptoms and other lesions significantly decreased among recurrences compared with initial RIME.
“Notably, we found that M. pneumoniae was the most common known cause of RIME, particularly among the initial episodes,” Ms. Pan said. “However, 61% of recurrent RIME episodes did not have a known cause in terms of infectious etiology. And, concordant with prior studies, we also found decreased severity [of RIME recurrences] as indicated by decreased rates of emergency department presentation, hospitalization, and duration of hospitalization.”
In other findings, psychiatric complications such as anxiety and depression followed the onset of RIME in 33% of those with recurrent disease and 22% of those with isolated disease. In addition, the three most common treatments among all 50 patients were systemic steroids, topical steroids, and M. pneumoniae-specific antibiotics.
“While RIME is considered as typically milder than Stevens-Johnson syndrome and toxic epidermal necrolysis with low mortality rates, it can lead to severe complications including conjunctival shrinkage, corneal ulceration and scarring, blindness, and oral, ocular, urogenital synechiae,” Ms. Pan noted. “Increased use of corticosteroids and steroid-sparing agents such as IVIG have also been observed. Multidisciplinary care with ophthalmology, urology, and mental health services is critical.”
She acknowledged certain limitations of the study, including its retrospective, single-center design, and the possibility that milder cases may have been excluded due to a lack of accurate diagnosis or referral.
Carrie C. Coughlin, MD, who was asked to comment on the study results, pointed out that nearly half (24) of patients in the cohort experienced recurrent RIME. “This is a high proportion, suggesting counseling about the possibility of recurrence is more important than previously thought,” said Dr. Coughlin, director of the section of pediatric dermatology Washington University/St. Louis Children’s Hospital.
“Fortunately, recurrent cases tended to be less severe. However, many patients had more than one recurrence, making this challenging for affected patients.”
The researchers reported having no financial disclosures. Dr. Coughlin is on the board of the Pediatric Dermatology Research Alliance (PeDRA) and the International Immunosuppression and Transplant Skin Cancer Collaborative.
INDIANAPOLIS – , in a single-center retrospective study. In addition, 71% of patients with recurrent disease experienced 1-2 recurrences – episodes that were generally milder and occurred at variable intervals.
Those are among key findings from the study of 50 patients with RIME, presented by Catherina X. Pan at the annual meeting of the Society for Pediatric Dermatology.
Reactive infectious mucocutaneous eruption (RIME) is a novel term encompassing an array of rare, parainfectious mucositis diseases, noted Ms. Pan, a fourth-year medical student at Harvard Medical School, Boston. Previously known as Mycoplasma pneumoniae-induced rash and mucositis (MIRM), common clinical characteristics of RIME include less than 10% body surface area involvement of polymorphic skin lesions (vesiculobullous or targetoid macules/papules); erosive oral, genital, and/or ocular mucositis involving more than two sites, and evidence of prior infection including but not limited to upper respiratory infection, fever, and cough.
In addition to M. pneumoniae, other pathogens have been implicated, she said. “While the underlying etiology of the disease is not entirely clear, it’s become increasingly known that RIME tends to recur in a subset of patients.”
A cohort study of 13 patients with RIME found that Black race, male sex, and older age were predominant among the five patients who developed recurrent disease.
The estimated recurrence rate is between 8% and 38%, but the clinical characteristics of patients who develop recurrent RIME tend to be poorly understood, Ms. Pan said.
Along with her mentor, Sadaf Hussain, MD, of the department of dermatology at Boston Children’s Hospital, Ms. Pan conducted a retrospective chart review to characterize the clinical history and course of disease in patients diagnosed with recurrent RIME. They extracted data between January of 2000 and March of 2022 using ICD-10 codes used by board-certified dermatologists at Boston Children’s Hospital, as well as a text search for RIME or MIRM in the dermatology notes. Patients were included if they had a RIME/MIRM diagnosis by a board-certified dermatologist and/or infection on PCR/serology and mucositis involvement with limited skin involvement.
The study population included 50 patients: 24 with recurrent RIME and 26 with isolated RIME. The majority (66%) were male, and the mean age of RIME onset was between 11 and 12 years old, which is up to two years younger than previously reported in the case series of 13 patients. Most of the study participants (79%) were White, but there were no significant differences in patients who had recurrent RIME and those who had isolated RIME in terms of age, sex, or race.
Isolated vs. recurrent RIME
However, compared with patients who had isolated RIME, a greater proportion of those with recurrent RIME had a history of atopic disease (46% vs. 23%, respectively; P = .136), as well as a history of tonsillectomy and adenoidectomy (25% vs. 4%; P = .045). “This has not been previously observed, but it may generate a hypothesis that patients with a history of frequent infection as well as amplified immune responses may be associated with disease recurrence,” Ms. Pan said.
The average number of episodes among patients with recurrent RIME was 3.5 and the interval between episodes was variable, at a mean of 10.2 months. Ms. Pan reported that 71% of recurrent RIME patients experienced 1-2 episodes, although one patient experienced 9 episodes.
Clinically, episodes among all patients with RIME were characterized by infectious prodromal symptoms (69%), oral lesions (95%), ocular lesions (60%), genital lesions (41%) and cutaneous lesions (40%). However, RIME recurrences were less severe and more atypical, with 49% involving only one mucosal surface and 29% involving two mucosal surfaces. Also, except for oral lesions, rates of infectious prodromal symptoms and other lesions significantly decreased among recurrences compared with initial RIME.
“Notably, we found that M. pneumoniae was the most common known cause of RIME, particularly among the initial episodes,” Ms. Pan said. “However, 61% of recurrent RIME episodes did not have a known cause in terms of infectious etiology. And, concordant with prior studies, we also found decreased severity [of RIME recurrences] as indicated by decreased rates of emergency department presentation, hospitalization, and duration of hospitalization.”
In other findings, psychiatric complications such as anxiety and depression followed the onset of RIME in 33% of those with recurrent disease and 22% of those with isolated disease. In addition, the three most common treatments among all 50 patients were systemic steroids, topical steroids, and M. pneumoniae-specific antibiotics.
“While RIME is considered as typically milder than Stevens-Johnson syndrome and toxic epidermal necrolysis with low mortality rates, it can lead to severe complications including conjunctival shrinkage, corneal ulceration and scarring, blindness, and oral, ocular, urogenital synechiae,” Ms. Pan noted. “Increased use of corticosteroids and steroid-sparing agents such as IVIG have also been observed. Multidisciplinary care with ophthalmology, urology, and mental health services is critical.”
She acknowledged certain limitations of the study, including its retrospective, single-center design, and the possibility that milder cases may have been excluded due to a lack of accurate diagnosis or referral.
Carrie C. Coughlin, MD, who was asked to comment on the study results, pointed out that nearly half (24) of patients in the cohort experienced recurrent RIME. “This is a high proportion, suggesting counseling about the possibility of recurrence is more important than previously thought,” said Dr. Coughlin, director of the section of pediatric dermatology Washington University/St. Louis Children’s Hospital.
“Fortunately, recurrent cases tended to be less severe. However, many patients had more than one recurrence, making this challenging for affected patients.”
The researchers reported having no financial disclosures. Dr. Coughlin is on the board of the Pediatric Dermatology Research Alliance (PeDRA) and the International Immunosuppression and Transplant Skin Cancer Collaborative.
AT SPD 2022
‘Ecotrauma’: The effects of climate change on mental health
In June of this year, the World Health Organization launched a policy report to confront the increasingly strong and lasting impacts that climate change is having directly and indirectly on people’s mental health and psychosocial well-being.
In addition to the increasingly high incidence of mental disorders (for instance, emotional distress, stress, depression, and suicidal behavior) affecting people worldwide This term refers to anxiety in the face of the apocalyptic scenario predicted to result from the transformation of ecosystems by anthropogenic activity.
Two weeks after the release of the policy report, which integrates key policies for countries to address one of the biggest challenges, the WHO published its largest review of global mental health since the turn of the century. The work provides a model for governments, academics, health professionals, and civil society to become key players when dealing with the mental health problems that our society is going through.
As the document highlights, almost 1 billion people, including 14% of the world’s adolescents, were living with a mental health disorder in 2019. Suicide accounted for more than 1 in 100 deaths, and 58% of cases occurred before age 50 years. Mental health disorders are already the leading cause of disability in the world, and people with serious but preventable diseases die on average 10-20 years earlier than the general population.
The COVID-19 crisis has significantly aggravated mental health disorders, especially in populations such as minors. Consequently, many experts refer to this public health phenomenon as the new major pandemic. “I’m not sure it’s correct to call a set of mental health problems a pandemic, but the reality is that many countries are ignoring or largely forgetting this crisis,” Sarah Sheppard, WHO communications officer, told this news organization. According to Ms. Sheppard, “stigma and lack of understanding are key drivers of these problems and have been one of the reasons for the lack of mental health funding for decades. Mental health receives less than 1% of international health aid.” We recently interviewed Ms. Sheppard about these challenges.
Univadis: As the data provided in the recently released Mental Health and Climate Change Policy Brief indicate, there are large gaps in many countries between mental health needs and the services and systems available to address them. Where can we start to change this reality?
Ms. Sheppard: The simplest answer to improve the situation we face begins with a change in people’s priorities when it comes to valuing mental health. This would lead to greater investment in human and financial resources for mental health services and systems. However, the challenge lies in the complexity of the problem. In the report we just published, we provide comprehensive recommendations on how to transform mental health systems for all, such as trying to integrate climate change considerations into policies and programs for mental health or building on existing global commitments, including the Sustainable Development Goals (SDGs) or the Paris Agreement.
Univadis: Is there evidence that mental illnesses and disorders affect some populations more than others, such as women, for example?
Ms. Sheppard: The prevalence of mental disorders varies according to conditions and according to sex and age. In general, I don’t think we can say that mental health conditions or disorders affect women more than men. There are groups at risk, but vulnerability depends on the context and varies a lot. Of course, social determinants such as poverty, unstable housing, and exposure to adversity can significantly increase risk.
Univadis: According to the statistics recently provided by the WHO, changes in the environment are directly and indirectly affecting people’s mental health and psychosocial well-being. The new report highlights the gap between countries when it comes to addressing this complex problem. Is there any country that is carrying out political or innovative initiatives in this regard?
Ms. Sheppard: Yes, there are many case studies in the policy brief that highlight important work in the area. There are strong examples that are highlighted in the summary. One of them is India and its resilient cities program. Focused on the reduction of disaster risk, climate resilience, and mental health and psychosocial support at city level, this project resulted from a collaboration between the United Nations Development Program and the Indian National Institute of Mental Health and Neurosciences, which began in 2017.
Univadis: In addition to its effects on mental health, we are seeing how climate change is causing the appearance and resurgence of zoonoses, such as the pandemic caused by coronavirus and now monkeypox.
Ms. Sheppard: Mike Ryan, head of emergency situations at WHO, stated at the beginning of June that the increase in zoonoses raises the risk of new pandemics. Infections transmitted from animals to humans, such as Ebola, COVID-19, or monkeypox, have multiplied in recent years. Climate change alters the conditions for pathogens and zoonotic disease vectors and their distribution. The intensification of travel, for example, allows them to spread more quickly and in a more uncontrolled way.
Human health, including mental health, is connected to animal health. As various materials available to us from our World Health Day 2022 campaign examine, the links between planetary health and human health are inextricable.
Univadis: How is it possible that while scientific progress advances and more powerful and efficient technologies are developed, we become increasingly vulnerable to environmental phenomena?
Ms. Sheppard: Scientific advancement improves our understanding of the quality and scale of the health impacts of climate change, including the identification of the most vulnerable groups, as well as the adaptation and mitigation measures that would work to reduce the consequences on health. At the same time, climate change is widespread, rapid, and intensifying. Technological advances have a role to play in mitigation, particularly those tools that reduce our dependence on burning fossil fuels, as well as adaptation to climate change. For example, early warning systems for extreme weather events could reduce those vulnerabilities your question mentioned.
On the other hand, the measures proposed by the latest report on mental health and climate change have multiple effects. Some are particularly powerful and are not overly dependent on new technology. These include changing our mode of transport to low-emission, physically active ways to get around (walking, cycling), the benefits of which are already more than proven for both the environment and human health.
This article was translated from Univadis Spain.
A version of this article first appeared on Medscape.com.
In June of this year, the World Health Organization launched a policy report to confront the increasingly strong and lasting impacts that climate change is having directly and indirectly on people’s mental health and psychosocial well-being.
In addition to the increasingly high incidence of mental disorders (for instance, emotional distress, stress, depression, and suicidal behavior) affecting people worldwide This term refers to anxiety in the face of the apocalyptic scenario predicted to result from the transformation of ecosystems by anthropogenic activity.
Two weeks after the release of the policy report, which integrates key policies for countries to address one of the biggest challenges, the WHO published its largest review of global mental health since the turn of the century. The work provides a model for governments, academics, health professionals, and civil society to become key players when dealing with the mental health problems that our society is going through.
As the document highlights, almost 1 billion people, including 14% of the world’s adolescents, were living with a mental health disorder in 2019. Suicide accounted for more than 1 in 100 deaths, and 58% of cases occurred before age 50 years. Mental health disorders are already the leading cause of disability in the world, and people with serious but preventable diseases die on average 10-20 years earlier than the general population.
The COVID-19 crisis has significantly aggravated mental health disorders, especially in populations such as minors. Consequently, many experts refer to this public health phenomenon as the new major pandemic. “I’m not sure it’s correct to call a set of mental health problems a pandemic, but the reality is that many countries are ignoring or largely forgetting this crisis,” Sarah Sheppard, WHO communications officer, told this news organization. According to Ms. Sheppard, “stigma and lack of understanding are key drivers of these problems and have been one of the reasons for the lack of mental health funding for decades. Mental health receives less than 1% of international health aid.” We recently interviewed Ms. Sheppard about these challenges.
Univadis: As the data provided in the recently released Mental Health and Climate Change Policy Brief indicate, there are large gaps in many countries between mental health needs and the services and systems available to address them. Where can we start to change this reality?
Ms. Sheppard: The simplest answer to improve the situation we face begins with a change in people’s priorities when it comes to valuing mental health. This would lead to greater investment in human and financial resources for mental health services and systems. However, the challenge lies in the complexity of the problem. In the report we just published, we provide comprehensive recommendations on how to transform mental health systems for all, such as trying to integrate climate change considerations into policies and programs for mental health or building on existing global commitments, including the Sustainable Development Goals (SDGs) or the Paris Agreement.
Univadis: Is there evidence that mental illnesses and disorders affect some populations more than others, such as women, for example?
Ms. Sheppard: The prevalence of mental disorders varies according to conditions and according to sex and age. In general, I don’t think we can say that mental health conditions or disorders affect women more than men. There are groups at risk, but vulnerability depends on the context and varies a lot. Of course, social determinants such as poverty, unstable housing, and exposure to adversity can significantly increase risk.
Univadis: According to the statistics recently provided by the WHO, changes in the environment are directly and indirectly affecting people’s mental health and psychosocial well-being. The new report highlights the gap between countries when it comes to addressing this complex problem. Is there any country that is carrying out political or innovative initiatives in this regard?
Ms. Sheppard: Yes, there are many case studies in the policy brief that highlight important work in the area. There are strong examples that are highlighted in the summary. One of them is India and its resilient cities program. Focused on the reduction of disaster risk, climate resilience, and mental health and psychosocial support at city level, this project resulted from a collaboration between the United Nations Development Program and the Indian National Institute of Mental Health and Neurosciences, which began in 2017.
Univadis: In addition to its effects on mental health, we are seeing how climate change is causing the appearance and resurgence of zoonoses, such as the pandemic caused by coronavirus and now monkeypox.
Ms. Sheppard: Mike Ryan, head of emergency situations at WHO, stated at the beginning of June that the increase in zoonoses raises the risk of new pandemics. Infections transmitted from animals to humans, such as Ebola, COVID-19, or monkeypox, have multiplied in recent years. Climate change alters the conditions for pathogens and zoonotic disease vectors and their distribution. The intensification of travel, for example, allows them to spread more quickly and in a more uncontrolled way.
Human health, including mental health, is connected to animal health. As various materials available to us from our World Health Day 2022 campaign examine, the links between planetary health and human health are inextricable.
Univadis: How is it possible that while scientific progress advances and more powerful and efficient technologies are developed, we become increasingly vulnerable to environmental phenomena?
Ms. Sheppard: Scientific advancement improves our understanding of the quality and scale of the health impacts of climate change, including the identification of the most vulnerable groups, as well as the adaptation and mitigation measures that would work to reduce the consequences on health. At the same time, climate change is widespread, rapid, and intensifying. Technological advances have a role to play in mitigation, particularly those tools that reduce our dependence on burning fossil fuels, as well as adaptation to climate change. For example, early warning systems for extreme weather events could reduce those vulnerabilities your question mentioned.
On the other hand, the measures proposed by the latest report on mental health and climate change have multiple effects. Some are particularly powerful and are not overly dependent on new technology. These include changing our mode of transport to low-emission, physically active ways to get around (walking, cycling), the benefits of which are already more than proven for both the environment and human health.
This article was translated from Univadis Spain.
A version of this article first appeared on Medscape.com.
In June of this year, the World Health Organization launched a policy report to confront the increasingly strong and lasting impacts that climate change is having directly and indirectly on people’s mental health and psychosocial well-being.
In addition to the increasingly high incidence of mental disorders (for instance, emotional distress, stress, depression, and suicidal behavior) affecting people worldwide This term refers to anxiety in the face of the apocalyptic scenario predicted to result from the transformation of ecosystems by anthropogenic activity.
Two weeks after the release of the policy report, which integrates key policies for countries to address one of the biggest challenges, the WHO published its largest review of global mental health since the turn of the century. The work provides a model for governments, academics, health professionals, and civil society to become key players when dealing with the mental health problems that our society is going through.
As the document highlights, almost 1 billion people, including 14% of the world’s adolescents, were living with a mental health disorder in 2019. Suicide accounted for more than 1 in 100 deaths, and 58% of cases occurred before age 50 years. Mental health disorders are already the leading cause of disability in the world, and people with serious but preventable diseases die on average 10-20 years earlier than the general population.
The COVID-19 crisis has significantly aggravated mental health disorders, especially in populations such as minors. Consequently, many experts refer to this public health phenomenon as the new major pandemic. “I’m not sure it’s correct to call a set of mental health problems a pandemic, but the reality is that many countries are ignoring or largely forgetting this crisis,” Sarah Sheppard, WHO communications officer, told this news organization. According to Ms. Sheppard, “stigma and lack of understanding are key drivers of these problems and have been one of the reasons for the lack of mental health funding for decades. Mental health receives less than 1% of international health aid.” We recently interviewed Ms. Sheppard about these challenges.
Univadis: As the data provided in the recently released Mental Health and Climate Change Policy Brief indicate, there are large gaps in many countries between mental health needs and the services and systems available to address them. Where can we start to change this reality?
Ms. Sheppard: The simplest answer to improve the situation we face begins with a change in people’s priorities when it comes to valuing mental health. This would lead to greater investment in human and financial resources for mental health services and systems. However, the challenge lies in the complexity of the problem. In the report we just published, we provide comprehensive recommendations on how to transform mental health systems for all, such as trying to integrate climate change considerations into policies and programs for mental health or building on existing global commitments, including the Sustainable Development Goals (SDGs) or the Paris Agreement.
Univadis: Is there evidence that mental illnesses and disorders affect some populations more than others, such as women, for example?
Ms. Sheppard: The prevalence of mental disorders varies according to conditions and according to sex and age. In general, I don’t think we can say that mental health conditions or disorders affect women more than men. There are groups at risk, but vulnerability depends on the context and varies a lot. Of course, social determinants such as poverty, unstable housing, and exposure to adversity can significantly increase risk.
Univadis: According to the statistics recently provided by the WHO, changes in the environment are directly and indirectly affecting people’s mental health and psychosocial well-being. The new report highlights the gap between countries when it comes to addressing this complex problem. Is there any country that is carrying out political or innovative initiatives in this regard?
Ms. Sheppard: Yes, there are many case studies in the policy brief that highlight important work in the area. There are strong examples that are highlighted in the summary. One of them is India and its resilient cities program. Focused on the reduction of disaster risk, climate resilience, and mental health and psychosocial support at city level, this project resulted from a collaboration between the United Nations Development Program and the Indian National Institute of Mental Health and Neurosciences, which began in 2017.
Univadis: In addition to its effects on mental health, we are seeing how climate change is causing the appearance and resurgence of zoonoses, such as the pandemic caused by coronavirus and now monkeypox.
Ms. Sheppard: Mike Ryan, head of emergency situations at WHO, stated at the beginning of June that the increase in zoonoses raises the risk of new pandemics. Infections transmitted from animals to humans, such as Ebola, COVID-19, or monkeypox, have multiplied in recent years. Climate change alters the conditions for pathogens and zoonotic disease vectors and their distribution. The intensification of travel, for example, allows them to spread more quickly and in a more uncontrolled way.
Human health, including mental health, is connected to animal health. As various materials available to us from our World Health Day 2022 campaign examine, the links between planetary health and human health are inextricable.
Univadis: How is it possible that while scientific progress advances and more powerful and efficient technologies are developed, we become increasingly vulnerable to environmental phenomena?
Ms. Sheppard: Scientific advancement improves our understanding of the quality and scale of the health impacts of climate change, including the identification of the most vulnerable groups, as well as the adaptation and mitigation measures that would work to reduce the consequences on health. At the same time, climate change is widespread, rapid, and intensifying. Technological advances have a role to play in mitigation, particularly those tools that reduce our dependence on burning fossil fuels, as well as adaptation to climate change. For example, early warning systems for extreme weather events could reduce those vulnerabilities your question mentioned.
On the other hand, the measures proposed by the latest report on mental health and climate change have multiple effects. Some are particularly powerful and are not overly dependent on new technology. These include changing our mode of transport to low-emission, physically active ways to get around (walking, cycling), the benefits of which are already more than proven for both the environment and human health.
This article was translated from Univadis Spain.
A version of this article first appeared on Medscape.com.
Growing evidence gardening cultivates mental health
The results of the small pilot study add to the growing body of evidence supporting the therapeutic value of gardening, study investigator Charles Guy, PhD, professor emeritus, University of Florida Institute of Food and Agricultural Sciences, Gainesville, told this news organization.
“If we can see therapeutic benefits among healthy individuals in a rigorously designed study, where variability was as controlled as you will see in this field, then now is the time to invest in some large-scale multi-institutional studies,” Dr. Guy added.
The study was published online in PLOS ONE.
Horticulture as therapy
Horticulture therapy involves engaging in gardening and plant-based activities facilitated by a trained therapist. Previous studies found that this intervention reduces apathy and improves cognitive function in some populations.
The current study included healthy, nonsmoking, and non–drug-using women, whose average age was about 32.5 years and whose body mass index was less than 32. The participants had no chronic conditions and were not allergic to pollen or plants.
Virtually all previous studies of therapeutic gardening included participants who had been diagnosed with conditions such as depression, chronic pain, or PTSD. “If we can see a therapeutic benefit with perfectly healthy people, then this is likely to have a therapeutic effect with whatever clinical population you might be interested in looking at,” said Dr. Guy.
In addition, including only women reduced variability, which is important in a small study, he said.
The researchers randomly assigned 20 participants to the gardening intervention and 20 to an art intervention. Each intervention consisted of twice-weekly 60-minute sessions for 4 weeks and a single follow-up session.
The art group was asked not to visit art galleries, museums, arts and crafts events, or art-related websites. Those in the gardening group were told not to visit parks or botanical gardens, not to engage in gardening activities, and not to visit gardening websites.
Activities in both groups involved a similar level of physical, cognitive, and social engagement. Gardeners were taught how to plant seeds and transplant and harvest edible crops, such as tomatoes, beans, and basil. Those in the art group learned papermaking and storytelling through drawing, printmaking, and mixed media collage.
At the beginning and end of the study, participants completed six questionnaires: the Profile of Mood States 2-A (POMS) short form, the Perceived Stress Scale (PSS), the Beck Depression Inventory II (BDI-II), the State-Trait Anxiety Inventory for Adults, the Satisfaction With Participation in Discretionary Social Activities, and the 36-item Short-Form Survey.
Participants wore wrist cuff blood pressure and heart rate monitors.
The analysis included 15 persons in the gardening group and 17 in the art group.
Participants in both interventions improved on several scales. For example, the mean preintervention POMS TMD (T score) for gardeners was 53.1, which was reduced to a mean of 46.9 post intervention (P = .018). In the art group, the means score was 53.5 before the intervention and 47.0 after the intervention (P = .009).
For the PSS, mean scores went from 14.9 to 9.4 (P = .002) for gardening and from 15.8 to 10.0 (P = .001) for artmaking.
For the BDI-II, mean scores dropped from 8.2 to 2.8 (P = .001) for gardening and from 9.0 to 5.1 (P = .009) for art.
However, gardening was associated with less trait anxiety than artmaking. “We concluded that both interventions were roughly equally therapeutic, with one glaring exception, and that was with trait anxiety, where the gardening resulted in statistical separation from the art group,” said Dr. Guy.
There appeared to be dose responses for total mood disturbance, perceived stress, and depression symptomatology for both gardening and artmaking.
Neither intervention affected heart rate or blood pressure. A larger sample might be needed to detect treatment differences in healthy women, the investigators noted.
The therapeutic benefit of gardening may lie in the role of plants in human evolution, during which “we relied on plants for shelter; we relied on them for protection; we relied on them obviously for nutrition,” said Dr. Guy.
The study results support carrying out large, well-designed, rigorously designed trials “that will definitively and conclusively demonstrate treatment effects with quantitative descriptions of those treatment effects with respect to dosage,” he said.
Good for the mind
Commenting on the study, Sir Richard Thompson, MD, past president, Royal College of Physicians, London, who has written about the health benefits of gardening, said this new study provides “more evidence that both gardening and art therapy are good for the mind” with mostly equal benefits for the two interventions.
“A much larger study would be needed to strengthen their case, but it fits in with much of the literature,” said Dr. Thompson.
However, he acknowledged the difficulty of carrying out scientifically robust studies in the field of alternative medicine, which “tends to be frowned upon” by some scientists.
Dr. Thompson identified some drawbacks of the study. In trying to measure so many parameters, the authors “may have had to resort to complex statistical analyses,” which may have led to some outcome changes being statistically positive by chance.
He noted that the study was small and that the gardening arm was “artificial” in that it was carried out in a greenhouse. “Maybe being outside would have been more beneficial; it would be interesting to test that hypothesis.”
As well, he pointed out initial differences between the two groups, including income and initial blood pressure, but he doubts these were significant.
He agreed that changes in cardiovascular parameters wouldn’t be expected in healthy young women, “as there’s little room for improvement.
“I wonder whether more improvement might have been seen in participants who were already suffering from anxiety, depression, etc.”
The study was supported by the Horticulture Research Institute, the Gene and Barbara Batson Endowed Nursery Fund, Florida Nursery Growers and Landscape Association, the Institute of Food and Agricultural Sciences, Wilmot Botanical Gardens, the Center for Arts in Medicine, Health Shands Arts in Medicine, and the department of environmental horticulture at the University of Florida. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The results of the small pilot study add to the growing body of evidence supporting the therapeutic value of gardening, study investigator Charles Guy, PhD, professor emeritus, University of Florida Institute of Food and Agricultural Sciences, Gainesville, told this news organization.
“If we can see therapeutic benefits among healthy individuals in a rigorously designed study, where variability was as controlled as you will see in this field, then now is the time to invest in some large-scale multi-institutional studies,” Dr. Guy added.
The study was published online in PLOS ONE.
Horticulture as therapy
Horticulture therapy involves engaging in gardening and plant-based activities facilitated by a trained therapist. Previous studies found that this intervention reduces apathy and improves cognitive function in some populations.
The current study included healthy, nonsmoking, and non–drug-using women, whose average age was about 32.5 years and whose body mass index was less than 32. The participants had no chronic conditions and were not allergic to pollen or plants.
Virtually all previous studies of therapeutic gardening included participants who had been diagnosed with conditions such as depression, chronic pain, or PTSD. “If we can see a therapeutic benefit with perfectly healthy people, then this is likely to have a therapeutic effect with whatever clinical population you might be interested in looking at,” said Dr. Guy.
In addition, including only women reduced variability, which is important in a small study, he said.
The researchers randomly assigned 20 participants to the gardening intervention and 20 to an art intervention. Each intervention consisted of twice-weekly 60-minute sessions for 4 weeks and a single follow-up session.
The art group was asked not to visit art galleries, museums, arts and crafts events, or art-related websites. Those in the gardening group were told not to visit parks or botanical gardens, not to engage in gardening activities, and not to visit gardening websites.
Activities in both groups involved a similar level of physical, cognitive, and social engagement. Gardeners were taught how to plant seeds and transplant and harvest edible crops, such as tomatoes, beans, and basil. Those in the art group learned papermaking and storytelling through drawing, printmaking, and mixed media collage.
At the beginning and end of the study, participants completed six questionnaires: the Profile of Mood States 2-A (POMS) short form, the Perceived Stress Scale (PSS), the Beck Depression Inventory II (BDI-II), the State-Trait Anxiety Inventory for Adults, the Satisfaction With Participation in Discretionary Social Activities, and the 36-item Short-Form Survey.
Participants wore wrist cuff blood pressure and heart rate monitors.
The analysis included 15 persons in the gardening group and 17 in the art group.
Participants in both interventions improved on several scales. For example, the mean preintervention POMS TMD (T score) for gardeners was 53.1, which was reduced to a mean of 46.9 post intervention (P = .018). In the art group, the means score was 53.5 before the intervention and 47.0 after the intervention (P = .009).
For the PSS, mean scores went from 14.9 to 9.4 (P = .002) for gardening and from 15.8 to 10.0 (P = .001) for artmaking.
For the BDI-II, mean scores dropped from 8.2 to 2.8 (P = .001) for gardening and from 9.0 to 5.1 (P = .009) for art.
However, gardening was associated with less trait anxiety than artmaking. “We concluded that both interventions were roughly equally therapeutic, with one glaring exception, and that was with trait anxiety, where the gardening resulted in statistical separation from the art group,” said Dr. Guy.
There appeared to be dose responses for total mood disturbance, perceived stress, and depression symptomatology for both gardening and artmaking.
Neither intervention affected heart rate or blood pressure. A larger sample might be needed to detect treatment differences in healthy women, the investigators noted.
The therapeutic benefit of gardening may lie in the role of plants in human evolution, during which “we relied on plants for shelter; we relied on them for protection; we relied on them obviously for nutrition,” said Dr. Guy.
The study results support carrying out large, well-designed, rigorously designed trials “that will definitively and conclusively demonstrate treatment effects with quantitative descriptions of those treatment effects with respect to dosage,” he said.
Good for the mind
Commenting on the study, Sir Richard Thompson, MD, past president, Royal College of Physicians, London, who has written about the health benefits of gardening, said this new study provides “more evidence that both gardening and art therapy are good for the mind” with mostly equal benefits for the two interventions.
“A much larger study would be needed to strengthen their case, but it fits in with much of the literature,” said Dr. Thompson.
However, he acknowledged the difficulty of carrying out scientifically robust studies in the field of alternative medicine, which “tends to be frowned upon” by some scientists.
Dr. Thompson identified some drawbacks of the study. In trying to measure so many parameters, the authors “may have had to resort to complex statistical analyses,” which may have led to some outcome changes being statistically positive by chance.
He noted that the study was small and that the gardening arm was “artificial” in that it was carried out in a greenhouse. “Maybe being outside would have been more beneficial; it would be interesting to test that hypothesis.”
As well, he pointed out initial differences between the two groups, including income and initial blood pressure, but he doubts these were significant.
He agreed that changes in cardiovascular parameters wouldn’t be expected in healthy young women, “as there’s little room for improvement.
“I wonder whether more improvement might have been seen in participants who were already suffering from anxiety, depression, etc.”
The study was supported by the Horticulture Research Institute, the Gene and Barbara Batson Endowed Nursery Fund, Florida Nursery Growers and Landscape Association, the Institute of Food and Agricultural Sciences, Wilmot Botanical Gardens, the Center for Arts in Medicine, Health Shands Arts in Medicine, and the department of environmental horticulture at the University of Florida. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The results of the small pilot study add to the growing body of evidence supporting the therapeutic value of gardening, study investigator Charles Guy, PhD, professor emeritus, University of Florida Institute of Food and Agricultural Sciences, Gainesville, told this news organization.
“If we can see therapeutic benefits among healthy individuals in a rigorously designed study, where variability was as controlled as you will see in this field, then now is the time to invest in some large-scale multi-institutional studies,” Dr. Guy added.
The study was published online in PLOS ONE.
Horticulture as therapy
Horticulture therapy involves engaging in gardening and plant-based activities facilitated by a trained therapist. Previous studies found that this intervention reduces apathy and improves cognitive function in some populations.
The current study included healthy, nonsmoking, and non–drug-using women, whose average age was about 32.5 years and whose body mass index was less than 32. The participants had no chronic conditions and were not allergic to pollen or plants.
Virtually all previous studies of therapeutic gardening included participants who had been diagnosed with conditions such as depression, chronic pain, or PTSD. “If we can see a therapeutic benefit with perfectly healthy people, then this is likely to have a therapeutic effect with whatever clinical population you might be interested in looking at,” said Dr. Guy.
In addition, including only women reduced variability, which is important in a small study, he said.
The researchers randomly assigned 20 participants to the gardening intervention and 20 to an art intervention. Each intervention consisted of twice-weekly 60-minute sessions for 4 weeks and a single follow-up session.
The art group was asked not to visit art galleries, museums, arts and crafts events, or art-related websites. Those in the gardening group were told not to visit parks or botanical gardens, not to engage in gardening activities, and not to visit gardening websites.
Activities in both groups involved a similar level of physical, cognitive, and social engagement. Gardeners were taught how to plant seeds and transplant and harvest edible crops, such as tomatoes, beans, and basil. Those in the art group learned papermaking and storytelling through drawing, printmaking, and mixed media collage.
At the beginning and end of the study, participants completed six questionnaires: the Profile of Mood States 2-A (POMS) short form, the Perceived Stress Scale (PSS), the Beck Depression Inventory II (BDI-II), the State-Trait Anxiety Inventory for Adults, the Satisfaction With Participation in Discretionary Social Activities, and the 36-item Short-Form Survey.
Participants wore wrist cuff blood pressure and heart rate monitors.
The analysis included 15 persons in the gardening group and 17 in the art group.
Participants in both interventions improved on several scales. For example, the mean preintervention POMS TMD (T score) for gardeners was 53.1, which was reduced to a mean of 46.9 post intervention (P = .018). In the art group, the means score was 53.5 before the intervention and 47.0 after the intervention (P = .009).
For the PSS, mean scores went from 14.9 to 9.4 (P = .002) for gardening and from 15.8 to 10.0 (P = .001) for artmaking.
For the BDI-II, mean scores dropped from 8.2 to 2.8 (P = .001) for gardening and from 9.0 to 5.1 (P = .009) for art.
However, gardening was associated with less trait anxiety than artmaking. “We concluded that both interventions were roughly equally therapeutic, with one glaring exception, and that was with trait anxiety, where the gardening resulted in statistical separation from the art group,” said Dr. Guy.
There appeared to be dose responses for total mood disturbance, perceived stress, and depression symptomatology for both gardening and artmaking.
Neither intervention affected heart rate or blood pressure. A larger sample might be needed to detect treatment differences in healthy women, the investigators noted.
The therapeutic benefit of gardening may lie in the role of plants in human evolution, during which “we relied on plants for shelter; we relied on them for protection; we relied on them obviously for nutrition,” said Dr. Guy.
The study results support carrying out large, well-designed, rigorously designed trials “that will definitively and conclusively demonstrate treatment effects with quantitative descriptions of those treatment effects with respect to dosage,” he said.
Good for the mind
Commenting on the study, Sir Richard Thompson, MD, past president, Royal College of Physicians, London, who has written about the health benefits of gardening, said this new study provides “more evidence that both gardening and art therapy are good for the mind” with mostly equal benefits for the two interventions.
“A much larger study would be needed to strengthen their case, but it fits in with much of the literature,” said Dr. Thompson.
However, he acknowledged the difficulty of carrying out scientifically robust studies in the field of alternative medicine, which “tends to be frowned upon” by some scientists.
Dr. Thompson identified some drawbacks of the study. In trying to measure so many parameters, the authors “may have had to resort to complex statistical analyses,” which may have led to some outcome changes being statistically positive by chance.
He noted that the study was small and that the gardening arm was “artificial” in that it was carried out in a greenhouse. “Maybe being outside would have been more beneficial; it would be interesting to test that hypothesis.”
As well, he pointed out initial differences between the two groups, including income and initial blood pressure, but he doubts these were significant.
He agreed that changes in cardiovascular parameters wouldn’t be expected in healthy young women, “as there’s little room for improvement.
“I wonder whether more improvement might have been seen in participants who were already suffering from anxiety, depression, etc.”
The study was supported by the Horticulture Research Institute, the Gene and Barbara Batson Endowed Nursery Fund, Florida Nursery Growers and Landscape Association, the Institute of Food and Agricultural Sciences, Wilmot Botanical Gardens, the Center for Arts in Medicine, Health Shands Arts in Medicine, and the department of environmental horticulture at the University of Florida. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PLOS ONE
No increase in overdose deaths with take-home methadone
new research shows.
Overdose deaths both with and without methadone rose sharply in March 2020, when the policy was announced. Of note, methadone-related deaths decreased in the following months, whereas deaths not involving methadone continued to increase.
“Coupled with research demonstrating improved patient satisfaction, treatment access, and engagement from these policies, these findings can inform decisions about permanently expanding take-home methadone,” the investigators wrote.
The study was published online in JAMA Psychiatry.
An essential tool
Before the pandemic, patients seeking methadone treatment for OUD in the United States had to visit a federally certified opioid treatment clinic every day to receive the medication.
In response to the pandemic, the Substance Abuse and Mental Health Services Administration instituted a new policy that allowed states to request exceptions to provide take-home methadone for up to 4 weeks for stable patients and up to 2 weeks for those who were less stable.
To determine the effect of this policy change on overdose death rates, researchers analyzed data on overdose deaths from January 2019 to August 2021.
Overall, the percentage of deaths involving methadone decreased from 4.5% in 2019 to 3.2% in 2021.
The investigators found a sharp increase in all overdose deaths in March 2020. Deaths that did not involve methadone increased by an average of 78.12 more each month before March 2020, increased by an average of 1,078.27 during March 2020, and then continued to increase by an average of 69.07 more each month after March 2020.
Overdose deaths involving methadone increased by a similar amount in March 2020, stabilized, and then decreased 0.05% per month.
Researchers attributed the increase in methadone-related deaths in March 2020 with the rise in overall drug overdose deaths driven by illicitly made fentanyl in the early months of the COVID-19 pandemic.
A study published in JAMA Network Open in March 2022 showed that methadone and other medications to treat OUD are widely underutilized.
That research cited concern over misuse as a key reason for clinicians’ reluctance to prescribe the drugs. The researchers of the current study hope that these new findings lay some of these fears to rest.
“Treatment is an essential tool to stop the addiction and overdose crises, but it is vastly underused,” Nora Volkow, MD, coinvestigator, and director of the National Institute on Drug Abuse, said in a press release. “This evidence adds significant weight to the argument that effective treatment for substance use disorders should be offered in an accessible and practical way that works for people who need it.”
The study was funded by the Centers for Disease Control and Prevention and the National Institutes of Health. The authors reported no relevant disclosures related to the study.
A version of this article first appeared on Medscape.com.
new research shows.
Overdose deaths both with and without methadone rose sharply in March 2020, when the policy was announced. Of note, methadone-related deaths decreased in the following months, whereas deaths not involving methadone continued to increase.
“Coupled with research demonstrating improved patient satisfaction, treatment access, and engagement from these policies, these findings can inform decisions about permanently expanding take-home methadone,” the investigators wrote.
The study was published online in JAMA Psychiatry.
An essential tool
Before the pandemic, patients seeking methadone treatment for OUD in the United States had to visit a federally certified opioid treatment clinic every day to receive the medication.
In response to the pandemic, the Substance Abuse and Mental Health Services Administration instituted a new policy that allowed states to request exceptions to provide take-home methadone for up to 4 weeks for stable patients and up to 2 weeks for those who were less stable.
To determine the effect of this policy change on overdose death rates, researchers analyzed data on overdose deaths from January 2019 to August 2021.
Overall, the percentage of deaths involving methadone decreased from 4.5% in 2019 to 3.2% in 2021.
The investigators found a sharp increase in all overdose deaths in March 2020. Deaths that did not involve methadone increased by an average of 78.12 more each month before March 2020, increased by an average of 1,078.27 during March 2020, and then continued to increase by an average of 69.07 more each month after March 2020.
Overdose deaths involving methadone increased by a similar amount in March 2020, stabilized, and then decreased 0.05% per month.
Researchers attributed the increase in methadone-related deaths in March 2020 with the rise in overall drug overdose deaths driven by illicitly made fentanyl in the early months of the COVID-19 pandemic.
A study published in JAMA Network Open in March 2022 showed that methadone and other medications to treat OUD are widely underutilized.
That research cited concern over misuse as a key reason for clinicians’ reluctance to prescribe the drugs. The researchers of the current study hope that these new findings lay some of these fears to rest.
“Treatment is an essential tool to stop the addiction and overdose crises, but it is vastly underused,” Nora Volkow, MD, coinvestigator, and director of the National Institute on Drug Abuse, said in a press release. “This evidence adds significant weight to the argument that effective treatment for substance use disorders should be offered in an accessible and practical way that works for people who need it.”
The study was funded by the Centers for Disease Control and Prevention and the National Institutes of Health. The authors reported no relevant disclosures related to the study.
A version of this article first appeared on Medscape.com.
new research shows.
Overdose deaths both with and without methadone rose sharply in March 2020, when the policy was announced. Of note, methadone-related deaths decreased in the following months, whereas deaths not involving methadone continued to increase.
“Coupled with research demonstrating improved patient satisfaction, treatment access, and engagement from these policies, these findings can inform decisions about permanently expanding take-home methadone,” the investigators wrote.
The study was published online in JAMA Psychiatry.
An essential tool
Before the pandemic, patients seeking methadone treatment for OUD in the United States had to visit a federally certified opioid treatment clinic every day to receive the medication.
In response to the pandemic, the Substance Abuse and Mental Health Services Administration instituted a new policy that allowed states to request exceptions to provide take-home methadone for up to 4 weeks for stable patients and up to 2 weeks for those who were less stable.
To determine the effect of this policy change on overdose death rates, researchers analyzed data on overdose deaths from January 2019 to August 2021.
Overall, the percentage of deaths involving methadone decreased from 4.5% in 2019 to 3.2% in 2021.
The investigators found a sharp increase in all overdose deaths in March 2020. Deaths that did not involve methadone increased by an average of 78.12 more each month before March 2020, increased by an average of 1,078.27 during March 2020, and then continued to increase by an average of 69.07 more each month after March 2020.
Overdose deaths involving methadone increased by a similar amount in March 2020, stabilized, and then decreased 0.05% per month.
Researchers attributed the increase in methadone-related deaths in March 2020 with the rise in overall drug overdose deaths driven by illicitly made fentanyl in the early months of the COVID-19 pandemic.
A study published in JAMA Network Open in March 2022 showed that methadone and other medications to treat OUD are widely underutilized.
That research cited concern over misuse as a key reason for clinicians’ reluctance to prescribe the drugs. The researchers of the current study hope that these new findings lay some of these fears to rest.
“Treatment is an essential tool to stop the addiction and overdose crises, but it is vastly underused,” Nora Volkow, MD, coinvestigator, and director of the National Institute on Drug Abuse, said in a press release. “This evidence adds significant weight to the argument that effective treatment for substance use disorders should be offered in an accessible and practical way that works for people who need it.”
The study was funded by the Centers for Disease Control and Prevention and the National Institutes of Health. The authors reported no relevant disclosures related to the study.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Our role in preventing postpartum depression
Tragic, embarrassing, criminal ... Choose your own adjective. The maternal mortality rate in this country is the worst of any developed nation in the world. And the numbers are getting worse with an increase of 14% over the previous year. One-third of these deaths occur weeks or months after the delivery.
In a recent issue of Harvard Public Health, researchers at the T.H. Chan School of Public Health discuss some of the possible remedies for what they describe as a crisis. While some of the solutions they list will require major restructuring of how we deliver health care to mothers, others could take advantage of our current systems by employing a slight shift in emphasis. And here is where those of us on the frontline of care delivery can make a difference.
The researchers point out that “More than 90% of maternal deaths could be prevented if women had access to quality care.” They also observe that most mothers have a single postpartum check with the ob.gyn. facility that delivered the baby and then are often left to navigate the health system because transfer to their primary care and/or mental health professional is haphazard or lacking in follow-up.
As I read through the article it struck me that as pediatricians we could and should be playing a larger role in this critical postpartum period when so many women seem to be falling through the cracks in our health care nonsystem. This is not a great “Ah-ha” moment for which I deserve any credit. In 2010 the American Academy of Pediatrics recommended that mothers be screened for depression at the 1-, 2-, and 4-month visits using either a validated 10-question screening instrument or a more direct 2-question tool (Pediatrics 2010;126[5]:1032-9). However, a periodic survey of AAP members 3 years later revealed that less than a third of the respondents were screening regularly for postpartum depression. In 2019 the academy reemphasized the important role that pediatric primary care givers can play in the detection and early management of the condition.
The reasons for the disappointing response include the list of usual suspects of inadequate training, workload demands, reimbursement, liability concerns, and the difficulty in finding and establishing effective referral networks. Unfortunately, these factors continue to exist, and many cases have multiplied in the wake of the pandemic.
In some states, educational outreach, funding, and changes in the reimbursement structure have resulted in improved outcomes. Not all of us are fortunate enough to live in a state that has made postpartum depression detection and management a priority. However, simply making it our own professional priority can save lives, ease suffering, and improve postpartum outcomes. Here I am talking about first caring and then inquiring about a mother’s mental health. Asking how much sleep she is getting. And then spending the time to give personalized advice on feeding and sleep schedules. Even, if this means ignoring half of the topics on the recommended health maintenance. It doesn’t take but a few minutes to convince yourself that the baby is healthy, and you know that 90% of them are.
However, a new mother who is sleep deprived and already has one foot on the spiral staircase down into postpartum depression represents an emergency. And, you should have the skills to turn it around. But, you have to care about the problem and make it your own priority – high enough on the list to make a follow-up appointment or call in a week instead of waiting a month or 2 until the next visit.
Unfortunately, even with your best efforts there are some families who need services beyond the scope of your practice. Making the necessary referrals can be frustrating and time consuming but not dropping ball until it lands in the appropriate place may save a life.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Tragic, embarrassing, criminal ... Choose your own adjective. The maternal mortality rate in this country is the worst of any developed nation in the world. And the numbers are getting worse with an increase of 14% over the previous year. One-third of these deaths occur weeks or months after the delivery.
In a recent issue of Harvard Public Health, researchers at the T.H. Chan School of Public Health discuss some of the possible remedies for what they describe as a crisis. While some of the solutions they list will require major restructuring of how we deliver health care to mothers, others could take advantage of our current systems by employing a slight shift in emphasis. And here is where those of us on the frontline of care delivery can make a difference.
The researchers point out that “More than 90% of maternal deaths could be prevented if women had access to quality care.” They also observe that most mothers have a single postpartum check with the ob.gyn. facility that delivered the baby and then are often left to navigate the health system because transfer to their primary care and/or mental health professional is haphazard or lacking in follow-up.
As I read through the article it struck me that as pediatricians we could and should be playing a larger role in this critical postpartum period when so many women seem to be falling through the cracks in our health care nonsystem. This is not a great “Ah-ha” moment for which I deserve any credit. In 2010 the American Academy of Pediatrics recommended that mothers be screened for depression at the 1-, 2-, and 4-month visits using either a validated 10-question screening instrument or a more direct 2-question tool (Pediatrics 2010;126[5]:1032-9). However, a periodic survey of AAP members 3 years later revealed that less than a third of the respondents were screening regularly for postpartum depression. In 2019 the academy reemphasized the important role that pediatric primary care givers can play in the detection and early management of the condition.
The reasons for the disappointing response include the list of usual suspects of inadequate training, workload demands, reimbursement, liability concerns, and the difficulty in finding and establishing effective referral networks. Unfortunately, these factors continue to exist, and many cases have multiplied in the wake of the pandemic.
In some states, educational outreach, funding, and changes in the reimbursement structure have resulted in improved outcomes. Not all of us are fortunate enough to live in a state that has made postpartum depression detection and management a priority. However, simply making it our own professional priority can save lives, ease suffering, and improve postpartum outcomes. Here I am talking about first caring and then inquiring about a mother’s mental health. Asking how much sleep she is getting. And then spending the time to give personalized advice on feeding and sleep schedules. Even, if this means ignoring half of the topics on the recommended health maintenance. It doesn’t take but a few minutes to convince yourself that the baby is healthy, and you know that 90% of them are.
However, a new mother who is sleep deprived and already has one foot on the spiral staircase down into postpartum depression represents an emergency. And, you should have the skills to turn it around. But, you have to care about the problem and make it your own priority – high enough on the list to make a follow-up appointment or call in a week instead of waiting a month or 2 until the next visit.
Unfortunately, even with your best efforts there are some families who need services beyond the scope of your practice. Making the necessary referrals can be frustrating and time consuming but not dropping ball until it lands in the appropriate place may save a life.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Tragic, embarrassing, criminal ... Choose your own adjective. The maternal mortality rate in this country is the worst of any developed nation in the world. And the numbers are getting worse with an increase of 14% over the previous year. One-third of these deaths occur weeks or months after the delivery.
In a recent issue of Harvard Public Health, researchers at the T.H. Chan School of Public Health discuss some of the possible remedies for what they describe as a crisis. While some of the solutions they list will require major restructuring of how we deliver health care to mothers, others could take advantage of our current systems by employing a slight shift in emphasis. And here is where those of us on the frontline of care delivery can make a difference.
The researchers point out that “More than 90% of maternal deaths could be prevented if women had access to quality care.” They also observe that most mothers have a single postpartum check with the ob.gyn. facility that delivered the baby and then are often left to navigate the health system because transfer to their primary care and/or mental health professional is haphazard or lacking in follow-up.
As I read through the article it struck me that as pediatricians we could and should be playing a larger role in this critical postpartum period when so many women seem to be falling through the cracks in our health care nonsystem. This is not a great “Ah-ha” moment for which I deserve any credit. In 2010 the American Academy of Pediatrics recommended that mothers be screened for depression at the 1-, 2-, and 4-month visits using either a validated 10-question screening instrument or a more direct 2-question tool (Pediatrics 2010;126[5]:1032-9). However, a periodic survey of AAP members 3 years later revealed that less than a third of the respondents were screening regularly for postpartum depression. In 2019 the academy reemphasized the important role that pediatric primary care givers can play in the detection and early management of the condition.
The reasons for the disappointing response include the list of usual suspects of inadequate training, workload demands, reimbursement, liability concerns, and the difficulty in finding and establishing effective referral networks. Unfortunately, these factors continue to exist, and many cases have multiplied in the wake of the pandemic.
In some states, educational outreach, funding, and changes in the reimbursement structure have resulted in improved outcomes. Not all of us are fortunate enough to live in a state that has made postpartum depression detection and management a priority. However, simply making it our own professional priority can save lives, ease suffering, and improve postpartum outcomes. Here I am talking about first caring and then inquiring about a mother’s mental health. Asking how much sleep she is getting. And then spending the time to give personalized advice on feeding and sleep schedules. Even, if this means ignoring half of the topics on the recommended health maintenance. It doesn’t take but a few minutes to convince yourself that the baby is healthy, and you know that 90% of them are.
However, a new mother who is sleep deprived and already has one foot on the spiral staircase down into postpartum depression represents an emergency. And, you should have the skills to turn it around. But, you have to care about the problem and make it your own priority – high enough on the list to make a follow-up appointment or call in a week instead of waiting a month or 2 until the next visit.
Unfortunately, even with your best efforts there are some families who need services beyond the scope of your practice. Making the necessary referrals can be frustrating and time consuming but not dropping ball until it lands in the appropriate place may save a life.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Electroacupuncture promising for depression-related insomnia
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).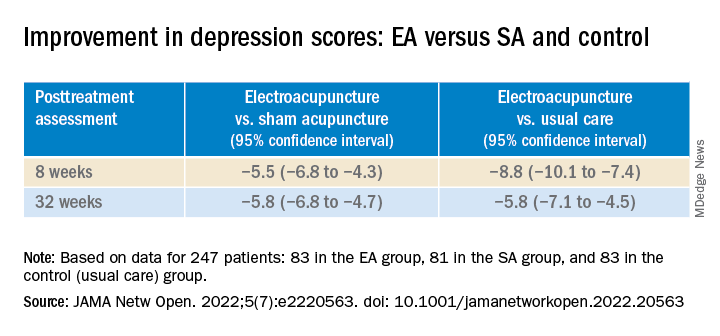
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).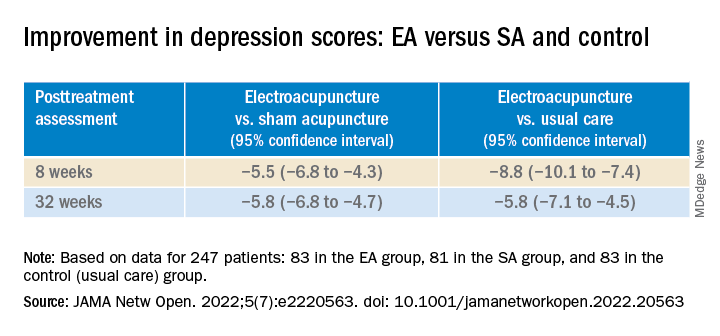
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).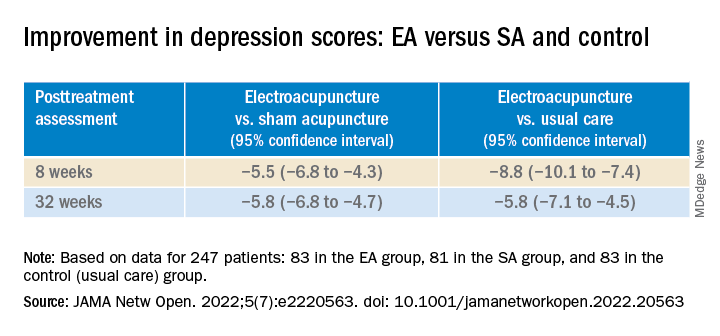
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Anxiety spreads from mother to daughter, father to son
The new findings suggest that children learn anxious behavior from their parents, study investigator Barbara Pavlova, PhD, clinical psychologist with Nova Scotia Health Authority, told this news organization.
“This means that transmission of anxiety from parents to children may be preventable,” said Dr. Pavlova, assistant professor, department of psychiatry, Dalhousie University, Halifax, Canada.
“Treating parents’ anxiety is not just important for their own health but also for the health of their children. This may be especially true if the child and the parent are the same sex,” Dr. Pavlova added.
The study was published online in JAMA Network Open.
Parental anxiety a disruptor
Anxiety disorders run in families. Both genes and environment are thought to be at play, but there are few data on sex-specific transmission from parent to child.
To investigate, the researchers conducted a cross-sectional study of 203 girls and 195 boys and their parents. The average age of the children was 11 years, and they had a familial risk for mood disorders.
Anxiety disorder in a same-sex parent was significantly associated with anxiety disorder in offspring (odds ratio, 2.85; 95% confidence interval, 1.52-5.34; P = .001) but not in an opposite-sex parent (OR, 1.51; 95% CI, 0.81-2.81; P = .20).
Living with a same-sex parent without anxiety was associated with lower rates of offspring anxiety (OR, 0.38; 95% CI, 0.22-0.67; P = .001).
Among all 398 children, 108 (27%) had been diagnosed with one or more anxiety disorders, including generalized anxiety disorder (7.8%), social anxiety disorder (6.3%), separation anxiety disorder (8.6%), specific phobia (8%), and anxiety disorder not otherwise specified (5%).
Rates of anxiety disorders in children increased with age, from 14% in those younger than 9 years to 52% in those older than 15 years. Anxiety disorders were similarly common among boys (24%) and girls (30%).
Rates of anxiety disorders were lowest (24%) in children of two parents without anxiety disorders and highest (41%) in cases in which both parents had anxiety disorders.
The findings point to the possible role of environmental factors, “such as modeling and vicarious learning,” in the transmission of anxiety from parents to their children, the researchers note.
“A child receives [a] similar amount of genetic information from each biological parent. A strong same-sex parent effect suggests children learn resilience by modeling the behavior of their same-sex parent. A parent’s anxiety disorder may disrupt this protective learning,” said Dr. Pavlova.
Early diagnosis, treatment essential
Reached for comment, Jill Emanuele, PhD, vice president of clinical training for the Child MIND Institute, New York, said that when it comes to anxiety, it’s important to assess and treat both the parent and the child.
“We know that both environment and genetics play a role in anxiety disorders. From a clinical perspective, if we see a parent with an anxiety disorder, we know that there is a chance that that is also going to affect the child – whether or not the child has an anxiety disorder,” Dr. Emanuele said in an interview.
“Anxiety disorders are the most common psychiatric disorders diagnosed. We also know that anxiety disorders emerge earlier than mood disorders and certainly can emerge in childhood. It’s important to address anxiety early because those same problems can continue into adulthood if left untreated,” Dr. Emanuele added.
The study was supported by the Canada Research Chairs Program, the Canadian Institutes of Health Research, the Brain & Behavior Research Foundation, the Nova Scotia Health Research Foundation, and the Dalhousie Medical Research Foundation. The authors have disclosed no relevant financial relationships. Dr. Emanuele is a board member with the Anxiety and Depression Association of America.
A version of this article first appeared on Medscape.com.
The new findings suggest that children learn anxious behavior from their parents, study investigator Barbara Pavlova, PhD, clinical psychologist with Nova Scotia Health Authority, told this news organization.
“This means that transmission of anxiety from parents to children may be preventable,” said Dr. Pavlova, assistant professor, department of psychiatry, Dalhousie University, Halifax, Canada.
“Treating parents’ anxiety is not just important for their own health but also for the health of their children. This may be especially true if the child and the parent are the same sex,” Dr. Pavlova added.
The study was published online in JAMA Network Open.
Parental anxiety a disruptor
Anxiety disorders run in families. Both genes and environment are thought to be at play, but there are few data on sex-specific transmission from parent to child.
To investigate, the researchers conducted a cross-sectional study of 203 girls and 195 boys and their parents. The average age of the children was 11 years, and they had a familial risk for mood disorders.
Anxiety disorder in a same-sex parent was significantly associated with anxiety disorder in offspring (odds ratio, 2.85; 95% confidence interval, 1.52-5.34; P = .001) but not in an opposite-sex parent (OR, 1.51; 95% CI, 0.81-2.81; P = .20).
Living with a same-sex parent without anxiety was associated with lower rates of offspring anxiety (OR, 0.38; 95% CI, 0.22-0.67; P = .001).
Among all 398 children, 108 (27%) had been diagnosed with one or more anxiety disorders, including generalized anxiety disorder (7.8%), social anxiety disorder (6.3%), separation anxiety disorder (8.6%), specific phobia (8%), and anxiety disorder not otherwise specified (5%).
Rates of anxiety disorders in children increased with age, from 14% in those younger than 9 years to 52% in those older than 15 years. Anxiety disorders were similarly common among boys (24%) and girls (30%).
Rates of anxiety disorders were lowest (24%) in children of two parents without anxiety disorders and highest (41%) in cases in which both parents had anxiety disorders.
The findings point to the possible role of environmental factors, “such as modeling and vicarious learning,” in the transmission of anxiety from parents to their children, the researchers note.
“A child receives [a] similar amount of genetic information from each biological parent. A strong same-sex parent effect suggests children learn resilience by modeling the behavior of their same-sex parent. A parent’s anxiety disorder may disrupt this protective learning,” said Dr. Pavlova.
Early diagnosis, treatment essential
Reached for comment, Jill Emanuele, PhD, vice president of clinical training for the Child MIND Institute, New York, said that when it comes to anxiety, it’s important to assess and treat both the parent and the child.
“We know that both environment and genetics play a role in anxiety disorders. From a clinical perspective, if we see a parent with an anxiety disorder, we know that there is a chance that that is also going to affect the child – whether or not the child has an anxiety disorder,” Dr. Emanuele said in an interview.
“Anxiety disorders are the most common psychiatric disorders diagnosed. We also know that anxiety disorders emerge earlier than mood disorders and certainly can emerge in childhood. It’s important to address anxiety early because those same problems can continue into adulthood if left untreated,” Dr. Emanuele added.
The study was supported by the Canada Research Chairs Program, the Canadian Institutes of Health Research, the Brain & Behavior Research Foundation, the Nova Scotia Health Research Foundation, and the Dalhousie Medical Research Foundation. The authors have disclosed no relevant financial relationships. Dr. Emanuele is a board member with the Anxiety and Depression Association of America.
A version of this article first appeared on Medscape.com.
The new findings suggest that children learn anxious behavior from their parents, study investigator Barbara Pavlova, PhD, clinical psychologist with Nova Scotia Health Authority, told this news organization.
“This means that transmission of anxiety from parents to children may be preventable,” said Dr. Pavlova, assistant professor, department of psychiatry, Dalhousie University, Halifax, Canada.
“Treating parents’ anxiety is not just important for their own health but also for the health of their children. This may be especially true if the child and the parent are the same sex,” Dr. Pavlova added.
The study was published online in JAMA Network Open.
Parental anxiety a disruptor
Anxiety disorders run in families. Both genes and environment are thought to be at play, but there are few data on sex-specific transmission from parent to child.
To investigate, the researchers conducted a cross-sectional study of 203 girls and 195 boys and their parents. The average age of the children was 11 years, and they had a familial risk for mood disorders.
Anxiety disorder in a same-sex parent was significantly associated with anxiety disorder in offspring (odds ratio, 2.85; 95% confidence interval, 1.52-5.34; P = .001) but not in an opposite-sex parent (OR, 1.51; 95% CI, 0.81-2.81; P = .20).
Living with a same-sex parent without anxiety was associated with lower rates of offspring anxiety (OR, 0.38; 95% CI, 0.22-0.67; P = .001).
Among all 398 children, 108 (27%) had been diagnosed with one or more anxiety disorders, including generalized anxiety disorder (7.8%), social anxiety disorder (6.3%), separation anxiety disorder (8.6%), specific phobia (8%), and anxiety disorder not otherwise specified (5%).
Rates of anxiety disorders in children increased with age, from 14% in those younger than 9 years to 52% in those older than 15 years. Anxiety disorders were similarly common among boys (24%) and girls (30%).
Rates of anxiety disorders were lowest (24%) in children of two parents without anxiety disorders and highest (41%) in cases in which both parents had anxiety disorders.
The findings point to the possible role of environmental factors, “such as modeling and vicarious learning,” in the transmission of anxiety from parents to their children, the researchers note.
“A child receives [a] similar amount of genetic information from each biological parent. A strong same-sex parent effect suggests children learn resilience by modeling the behavior of their same-sex parent. A parent’s anxiety disorder may disrupt this protective learning,” said Dr. Pavlova.
Early diagnosis, treatment essential
Reached for comment, Jill Emanuele, PhD, vice president of clinical training for the Child MIND Institute, New York, said that when it comes to anxiety, it’s important to assess and treat both the parent and the child.
“We know that both environment and genetics play a role in anxiety disorders. From a clinical perspective, if we see a parent with an anxiety disorder, we know that there is a chance that that is also going to affect the child – whether or not the child has an anxiety disorder,” Dr. Emanuele said in an interview.
“Anxiety disorders are the most common psychiatric disorders diagnosed. We also know that anxiety disorders emerge earlier than mood disorders and certainly can emerge in childhood. It’s important to address anxiety early because those same problems can continue into adulthood if left untreated,” Dr. Emanuele added.
The study was supported by the Canada Research Chairs Program, the Canadian Institutes of Health Research, the Brain & Behavior Research Foundation, the Nova Scotia Health Research Foundation, and the Dalhousie Medical Research Foundation. The authors have disclosed no relevant financial relationships. Dr. Emanuele is a board member with the Anxiety and Depression Association of America.
A version of this article first appeared on Medscape.com.
Americans’ biggest source of anxiety? Hint: It’s not COVID-19
, results from a new national report from the American Psychiatric Association show.
“The economy seems to have supplanted COVID as a major factor in Americans’ day-to-day anxiety,” APA President Rebecca W. Brendel, MD, JD, said in a news release.
“Knowing that so many Americans are concerned about finances is important because it can prepare clinicians to be ready to approach the subject, which is one that people are often reluctant or ashamed to raise on their own,” Dr. Brendel told this news organization.
What’s the best way to bring up the sensitive topic of money?
“In general, it’s best to start with open-ended questions to allow individuals in therapy to share what is on their minds, explore their concerns, and develop strategies to address these issues. Once a patient raises a concern, that is a good time to ask more about the issues they’ve raised and to explore other potential sources of anxiety or stress,” said Dr. Brendel.
The latest APA poll was conducted by Morning Consult, June 18-20, 2022, among a nationally representative sample of 2,210 adults.
In addition to an uptick in worry about inflation, the poll shows that more than half (51%) of adults are worried about a potential loss of income.
Hispanic adults (66%), mothers (65%), millennials (63%), and genZers (62%) are among the groups most likely to be concerned about income loss.
“Stress is not good for health, mental or physical. So, while it’s a reality that Americans are faced with finding ways of making ends meet, it’s more important than ever to make sure that we are all accessing the care that we need,” said Dr. Brendel.
“People should be aware that there may be low- or no-cost options such as community mental health centers or employer-sponsored resources to address mental health concerns,” she added.
Coping with traumatic events
The latest poll also shows that about one-third of adults are worried about gun violence (35% overall, 47% among genZers) or a natural disaster (29%) personally affecting them.
Climate change anxiety is also up slightly in June, compared with May (+4%).
The same goes for mid-term election-related anxiety (+3%) – particularly among Democrats (54% vs. 59%) compared with Republicans (48% vs. 48%).
The latest poll provides insight how Americans would cope after a traumatic event. More adults report they will turn to family and friends for support (60%) than practice self-care (42%), speak openly about their feelings (37%), or seek help from a professional (31%). Nearly one-third (30%) say they will move on from it and not dwell on their feelings.
GenZers are the least likely to say they will speak openly about their feelings (29%) and are less likely than millennials to say they would speak to a health professional (28% vs. 38%).
“While many people show resilience, it’s troubling that most Americans wouldn’t speak openly about their feelings after a traumatic event,” APA CEO and Medical Director Saul Levin, MD, said in the news release.
“In many ways, naming feelings is the most important step toward healing, and this reluctance to air our thoughts may indicate that mental health stigma is still a powerful force in our society,” Dr. Levin said.
After a traumatic current event, 41% of Americans say they consume more news and 30% say they take in more social media, but the majority say this does not impact their mental health, the poll shows.
Two in five adults (43%) say the news of a traumatic event makes them feel more informed, 32% say it makes them feel more anxious, and about one-quarter say it makes them feel overwhelmed (27%) or discouraged (24%).
Dr. Brendel noted that, after a traumatic event, “it’s expected that people may experience anxiety or other symptoms for brief periods of time. However, no two people experience things the same way. If symptoms don’t go away, are overwhelming, or get worse over time, for example, it’s critical to seek help right away.”
The June poll shows that 50% of Americans are anxious about the future of reproductive rights but the poll was conducted before the Dobbs ruling.
Anxiety around COVID-19 continues to ease, with about 47% of Americans saying they are concerned about the pandemic, down 2% among all Americans and 16% among Black Americans since May.
The APA’s Healthy Minds Monthly tracks timely mental health issues throughout the year. The APA also releases its annual Healthy Minds Poll each May in conjunction with Mental Health Awareness Month.
A version of this article first appeared on Medscape.com.
, results from a new national report from the American Psychiatric Association show.
“The economy seems to have supplanted COVID as a major factor in Americans’ day-to-day anxiety,” APA President Rebecca W. Brendel, MD, JD, said in a news release.
“Knowing that so many Americans are concerned about finances is important because it can prepare clinicians to be ready to approach the subject, which is one that people are often reluctant or ashamed to raise on their own,” Dr. Brendel told this news organization.
What’s the best way to bring up the sensitive topic of money?
“In general, it’s best to start with open-ended questions to allow individuals in therapy to share what is on their minds, explore their concerns, and develop strategies to address these issues. Once a patient raises a concern, that is a good time to ask more about the issues they’ve raised and to explore other potential sources of anxiety or stress,” said Dr. Brendel.
The latest APA poll was conducted by Morning Consult, June 18-20, 2022, among a nationally representative sample of 2,210 adults.
In addition to an uptick in worry about inflation, the poll shows that more than half (51%) of adults are worried about a potential loss of income.
Hispanic adults (66%), mothers (65%), millennials (63%), and genZers (62%) are among the groups most likely to be concerned about income loss.
“Stress is not good for health, mental or physical. So, while it’s a reality that Americans are faced with finding ways of making ends meet, it’s more important than ever to make sure that we are all accessing the care that we need,” said Dr. Brendel.
“People should be aware that there may be low- or no-cost options such as community mental health centers or employer-sponsored resources to address mental health concerns,” she added.
Coping with traumatic events
The latest poll also shows that about one-third of adults are worried about gun violence (35% overall, 47% among genZers) or a natural disaster (29%) personally affecting them.
Climate change anxiety is also up slightly in June, compared with May (+4%).
The same goes for mid-term election-related anxiety (+3%) – particularly among Democrats (54% vs. 59%) compared with Republicans (48% vs. 48%).
The latest poll provides insight how Americans would cope after a traumatic event. More adults report they will turn to family and friends for support (60%) than practice self-care (42%), speak openly about their feelings (37%), or seek help from a professional (31%). Nearly one-third (30%) say they will move on from it and not dwell on their feelings.
GenZers are the least likely to say they will speak openly about their feelings (29%) and are less likely than millennials to say they would speak to a health professional (28% vs. 38%).
“While many people show resilience, it’s troubling that most Americans wouldn’t speak openly about their feelings after a traumatic event,” APA CEO and Medical Director Saul Levin, MD, said in the news release.
“In many ways, naming feelings is the most important step toward healing, and this reluctance to air our thoughts may indicate that mental health stigma is still a powerful force in our society,” Dr. Levin said.
After a traumatic current event, 41% of Americans say they consume more news and 30% say they take in more social media, but the majority say this does not impact their mental health, the poll shows.
Two in five adults (43%) say the news of a traumatic event makes them feel more informed, 32% say it makes them feel more anxious, and about one-quarter say it makes them feel overwhelmed (27%) or discouraged (24%).
Dr. Brendel noted that, after a traumatic event, “it’s expected that people may experience anxiety or other symptoms for brief periods of time. However, no two people experience things the same way. If symptoms don’t go away, are overwhelming, or get worse over time, for example, it’s critical to seek help right away.”
The June poll shows that 50% of Americans are anxious about the future of reproductive rights but the poll was conducted before the Dobbs ruling.
Anxiety around COVID-19 continues to ease, with about 47% of Americans saying they are concerned about the pandemic, down 2% among all Americans and 16% among Black Americans since May.
The APA’s Healthy Minds Monthly tracks timely mental health issues throughout the year. The APA also releases its annual Healthy Minds Poll each May in conjunction with Mental Health Awareness Month.
A version of this article first appeared on Medscape.com.
, results from a new national report from the American Psychiatric Association show.
“The economy seems to have supplanted COVID as a major factor in Americans’ day-to-day anxiety,” APA President Rebecca W. Brendel, MD, JD, said in a news release.
“Knowing that so many Americans are concerned about finances is important because it can prepare clinicians to be ready to approach the subject, which is one that people are often reluctant or ashamed to raise on their own,” Dr. Brendel told this news organization.
What’s the best way to bring up the sensitive topic of money?
“In general, it’s best to start with open-ended questions to allow individuals in therapy to share what is on their minds, explore their concerns, and develop strategies to address these issues. Once a patient raises a concern, that is a good time to ask more about the issues they’ve raised and to explore other potential sources of anxiety or stress,” said Dr. Brendel.
The latest APA poll was conducted by Morning Consult, June 18-20, 2022, among a nationally representative sample of 2,210 adults.
In addition to an uptick in worry about inflation, the poll shows that more than half (51%) of adults are worried about a potential loss of income.
Hispanic adults (66%), mothers (65%), millennials (63%), and genZers (62%) are among the groups most likely to be concerned about income loss.
“Stress is not good for health, mental or physical. So, while it’s a reality that Americans are faced with finding ways of making ends meet, it’s more important than ever to make sure that we are all accessing the care that we need,” said Dr. Brendel.
“People should be aware that there may be low- or no-cost options such as community mental health centers or employer-sponsored resources to address mental health concerns,” she added.
Coping with traumatic events
The latest poll also shows that about one-third of adults are worried about gun violence (35% overall, 47% among genZers) or a natural disaster (29%) personally affecting them.
Climate change anxiety is also up slightly in June, compared with May (+4%).
The same goes for mid-term election-related anxiety (+3%) – particularly among Democrats (54% vs. 59%) compared with Republicans (48% vs. 48%).
The latest poll provides insight how Americans would cope after a traumatic event. More adults report they will turn to family and friends for support (60%) than practice self-care (42%), speak openly about their feelings (37%), or seek help from a professional (31%). Nearly one-third (30%) say they will move on from it and not dwell on their feelings.
GenZers are the least likely to say they will speak openly about their feelings (29%) and are less likely than millennials to say they would speak to a health professional (28% vs. 38%).
“While many people show resilience, it’s troubling that most Americans wouldn’t speak openly about their feelings after a traumatic event,” APA CEO and Medical Director Saul Levin, MD, said in the news release.
“In many ways, naming feelings is the most important step toward healing, and this reluctance to air our thoughts may indicate that mental health stigma is still a powerful force in our society,” Dr. Levin said.
After a traumatic current event, 41% of Americans say they consume more news and 30% say they take in more social media, but the majority say this does not impact their mental health, the poll shows.
Two in five adults (43%) say the news of a traumatic event makes them feel more informed, 32% say it makes them feel more anxious, and about one-quarter say it makes them feel overwhelmed (27%) or discouraged (24%).
Dr. Brendel noted that, after a traumatic event, “it’s expected that people may experience anxiety or other symptoms for brief periods of time. However, no two people experience things the same way. If symptoms don’t go away, are overwhelming, or get worse over time, for example, it’s critical to seek help right away.”
The June poll shows that 50% of Americans are anxious about the future of reproductive rights but the poll was conducted before the Dobbs ruling.
Anxiety around COVID-19 continues to ease, with about 47% of Americans saying they are concerned about the pandemic, down 2% among all Americans and 16% among Black Americans since May.
The APA’s Healthy Minds Monthly tracks timely mental health issues throughout the year. The APA also releases its annual Healthy Minds Poll each May in conjunction with Mental Health Awareness Month.
A version of this article first appeared on Medscape.com.
Antidepressants may curb opioid overdose
Investigators analyzed insurance claims for more than 200,000 adults with a history of depression. Of these, 8,200 experienced adverse events (AEs) during the year after initiation of opioid therapy.
However, the risk for an AE such as overdose and other forms of self-harm was reduced among patients who had been treated with antidepressants for at least 6 weeks.
The take-home message is that clinicians and health systems need to be more aware that individuals in pain are more likely to be depressed and at higher risk for AEs – so the depression should be treated “more liberally,” corresponding author Bradley Stein, MD, PhD, a practicing psychiatrist in Pittsburgh and director of the Rand Corporation Opioid Policy Center, told this news organization.
“If you are treating someone with pain, particularly chronic pain, it’s critically important to better assess their depression and not to attribute depressive symptoms only to pain,” Dr. Stein said.
The findings were published online in Psychiatric Services.
Promising approach?
Opioid treatment for pain “complicates the interactions among pain, depression, and self-harm,” the investigators write. Individuals with depression receiving long-term opioid therapy are two to three times more likely to misuse opioids, compared with individuals who do not have depression.
Although comorbid depression “substantially increases overdose and suicide risk, it remains underdiagnosed and undertreated among individuals with chronic pain,” the researchers note. They add that increasing access to depression treatment may be a “potentially promising approach to preventing overdoses and suicide” in these patients.
“We know that individuals using opioids who have a history of depression are more likely to have negative outcomes, such as overdoses and self-harm events,” Dr. Stein said. “We wanted to see whether antidepressants, which would treat depression in these individuals, would help with that.”
The researchers assessed a database of commercial insurance claims of adults with a history of depression who received opioids between 2007 and 2017 (n = 283,374). The data included 336,599 opioid treatment episodes.
To be included in the study, patients had to have been diagnosed with depression before they filled their first opioid prescription.
The “outcome of interest” was time from the beginning of an opioid episode until an adverse event, such as opioid poisoning, overdose of nonopioid controlled or illicit substances, or self-harm unrelated to overdose.
Participants were followed from the onset of the opioid episode until an AE occurred, loss to follow-up, or week 52, whichever came first.
The “key independent variable” was filling an antidepressant prescription. The patient’s sex and age were considered to be independent variables as well.
Teasing out antidepressant effect
Of participants with a history of depression treatment, 8,203 experienced at least one AE during the 12 months after treatment initiation (n = 47,486 AEs). Approximately half (50.8%) filled an antidepressant prescription at least once during the 12 months after the opioid episode began.
AEs were more likely among men than among women. The highest risk was in patients aged 18-24 years.
After adjusting for age and sex, participants who had received antidepressants had a greater risk for all adverse outcomes during the first 6 weeks of antidepressant treatment. However, those who had received antidepressants for 6 weeks or longer were at reduced risk for all adverse outcomes.

“We took advantage of the fact that, for most people, antidepressants take a while to work and aren’t immediately effective, so we were able to use that difference in our research,” Dr. Stein said.
“We wouldn’t expect to see an immediate effect of antidepressants, so the difference between what we saw immediately after the person had started treatment and the time it took for the antidepressant to be effective enabled us to tease out the effect of the antidepressant,” he added.
Consider CBT?
Andrew Saxon, MD, professor, department of psychiatry and behavioral sciences, University of Washington School of Medicine, Seattle, said clinicians “tend to think categorically and give people diagnoses that are clear-cut.” But neurobiologically, “it may be hard to distinguish where chronic pain ends and depression begins, or whether there’s some commonality.”
For patients with chronic pain and those taking opioids, “we need to be very attuned to the possibility or likelihood that they have major depression and other psychiatric diagnoses, like PTSD and anxiety disorders, which are very common,” said Dr. Saxon, who is also the director of the Center of Excellence in Substance Abuse Treatment and Education at the VA Puget Sound Health Care System. He was not involved with the current research.
He noted that treating those disorders “is a very important component of managing chronic pain.” However, “patients just starting antidepressants need to be carefully monitored when they’re getting stabilized on their antidepressants because they can have side effects, particularly early on, that can destabilize them.”
Dr. Saxon added that beyond pharmacotherapy, cognitive-behavioral therapy (CBT) for pain might be an even better intervention for addressing both pain and depression.
Also commenting for this article, Brian Hurley, MD, an addiction medicine specialist and the medical director of the Division of Substance Abuse Prevention and Control for the Los Angeles County Department of Public Health, said: “In the context of the largest wave of overdose mortality in U.S. history, we know comparatively little about the impact of mental health interventions that mitigate overdose risks.”
This study “contributes important new information that treating depression with antidepressant medications reduces overdose and self-harm risks for people who are prescribed opioids,” said Dr. Hurley, who is also the president-elect of the American Society of Addiction Medicine.
It also “underscores the general importance of integrated mental health and substance use disorder treatment in both primary care and in mental health settings,” added Dr. Hurley, who was not involved with the study.
The study was funded by the National Institute on Drug Abuse. The investigators and commenters reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed insurance claims for more than 200,000 adults with a history of depression. Of these, 8,200 experienced adverse events (AEs) during the year after initiation of opioid therapy.
However, the risk for an AE such as overdose and other forms of self-harm was reduced among patients who had been treated with antidepressants for at least 6 weeks.
The take-home message is that clinicians and health systems need to be more aware that individuals in pain are more likely to be depressed and at higher risk for AEs – so the depression should be treated “more liberally,” corresponding author Bradley Stein, MD, PhD, a practicing psychiatrist in Pittsburgh and director of the Rand Corporation Opioid Policy Center, told this news organization.
“If you are treating someone with pain, particularly chronic pain, it’s critically important to better assess their depression and not to attribute depressive symptoms only to pain,” Dr. Stein said.
The findings were published online in Psychiatric Services.
Promising approach?
Opioid treatment for pain “complicates the interactions among pain, depression, and self-harm,” the investigators write. Individuals with depression receiving long-term opioid therapy are two to three times more likely to misuse opioids, compared with individuals who do not have depression.
Although comorbid depression “substantially increases overdose and suicide risk, it remains underdiagnosed and undertreated among individuals with chronic pain,” the researchers note. They add that increasing access to depression treatment may be a “potentially promising approach to preventing overdoses and suicide” in these patients.
“We know that individuals using opioids who have a history of depression are more likely to have negative outcomes, such as overdoses and self-harm events,” Dr. Stein said. “We wanted to see whether antidepressants, which would treat depression in these individuals, would help with that.”
The researchers assessed a database of commercial insurance claims of adults with a history of depression who received opioids between 2007 and 2017 (n = 283,374). The data included 336,599 opioid treatment episodes.
To be included in the study, patients had to have been diagnosed with depression before they filled their first opioid prescription.
The “outcome of interest” was time from the beginning of an opioid episode until an adverse event, such as opioid poisoning, overdose of nonopioid controlled or illicit substances, or self-harm unrelated to overdose.
Participants were followed from the onset of the opioid episode until an AE occurred, loss to follow-up, or week 52, whichever came first.
The “key independent variable” was filling an antidepressant prescription. The patient’s sex and age were considered to be independent variables as well.
Teasing out antidepressant effect
Of participants with a history of depression treatment, 8,203 experienced at least one AE during the 12 months after treatment initiation (n = 47,486 AEs). Approximately half (50.8%) filled an antidepressant prescription at least once during the 12 months after the opioid episode began.
AEs were more likely among men than among women. The highest risk was in patients aged 18-24 years.
After adjusting for age and sex, participants who had received antidepressants had a greater risk for all adverse outcomes during the first 6 weeks of antidepressant treatment. However, those who had received antidepressants for 6 weeks or longer were at reduced risk for all adverse outcomes.

“We took advantage of the fact that, for most people, antidepressants take a while to work and aren’t immediately effective, so we were able to use that difference in our research,” Dr. Stein said.
“We wouldn’t expect to see an immediate effect of antidepressants, so the difference between what we saw immediately after the person had started treatment and the time it took for the antidepressant to be effective enabled us to tease out the effect of the antidepressant,” he added.
Consider CBT?
Andrew Saxon, MD, professor, department of psychiatry and behavioral sciences, University of Washington School of Medicine, Seattle, said clinicians “tend to think categorically and give people diagnoses that are clear-cut.” But neurobiologically, “it may be hard to distinguish where chronic pain ends and depression begins, or whether there’s some commonality.”
For patients with chronic pain and those taking opioids, “we need to be very attuned to the possibility or likelihood that they have major depression and other psychiatric diagnoses, like PTSD and anxiety disorders, which are very common,” said Dr. Saxon, who is also the director of the Center of Excellence in Substance Abuse Treatment and Education at the VA Puget Sound Health Care System. He was not involved with the current research.
He noted that treating those disorders “is a very important component of managing chronic pain.” However, “patients just starting antidepressants need to be carefully monitored when they’re getting stabilized on their antidepressants because they can have side effects, particularly early on, that can destabilize them.”
Dr. Saxon added that beyond pharmacotherapy, cognitive-behavioral therapy (CBT) for pain might be an even better intervention for addressing both pain and depression.
Also commenting for this article, Brian Hurley, MD, an addiction medicine specialist and the medical director of the Division of Substance Abuse Prevention and Control for the Los Angeles County Department of Public Health, said: “In the context of the largest wave of overdose mortality in U.S. history, we know comparatively little about the impact of mental health interventions that mitigate overdose risks.”
This study “contributes important new information that treating depression with antidepressant medications reduces overdose and self-harm risks for people who are prescribed opioids,” said Dr. Hurley, who is also the president-elect of the American Society of Addiction Medicine.
It also “underscores the general importance of integrated mental health and substance use disorder treatment in both primary care and in mental health settings,” added Dr. Hurley, who was not involved with the study.
The study was funded by the National Institute on Drug Abuse. The investigators and commenters reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed insurance claims for more than 200,000 adults with a history of depression. Of these, 8,200 experienced adverse events (AEs) during the year after initiation of opioid therapy.
However, the risk for an AE such as overdose and other forms of self-harm was reduced among patients who had been treated with antidepressants for at least 6 weeks.
The take-home message is that clinicians and health systems need to be more aware that individuals in pain are more likely to be depressed and at higher risk for AEs – so the depression should be treated “more liberally,” corresponding author Bradley Stein, MD, PhD, a practicing psychiatrist in Pittsburgh and director of the Rand Corporation Opioid Policy Center, told this news organization.
“If you are treating someone with pain, particularly chronic pain, it’s critically important to better assess their depression and not to attribute depressive symptoms only to pain,” Dr. Stein said.
The findings were published online in Psychiatric Services.
Promising approach?
Opioid treatment for pain “complicates the interactions among pain, depression, and self-harm,” the investigators write. Individuals with depression receiving long-term opioid therapy are two to three times more likely to misuse opioids, compared with individuals who do not have depression.
Although comorbid depression “substantially increases overdose and suicide risk, it remains underdiagnosed and undertreated among individuals with chronic pain,” the researchers note. They add that increasing access to depression treatment may be a “potentially promising approach to preventing overdoses and suicide” in these patients.
“We know that individuals using opioids who have a history of depression are more likely to have negative outcomes, such as overdoses and self-harm events,” Dr. Stein said. “We wanted to see whether antidepressants, which would treat depression in these individuals, would help with that.”
The researchers assessed a database of commercial insurance claims of adults with a history of depression who received opioids between 2007 and 2017 (n = 283,374). The data included 336,599 opioid treatment episodes.
To be included in the study, patients had to have been diagnosed with depression before they filled their first opioid prescription.
The “outcome of interest” was time from the beginning of an opioid episode until an adverse event, such as opioid poisoning, overdose of nonopioid controlled or illicit substances, or self-harm unrelated to overdose.
Participants were followed from the onset of the opioid episode until an AE occurred, loss to follow-up, or week 52, whichever came first.
The “key independent variable” was filling an antidepressant prescription. The patient’s sex and age were considered to be independent variables as well.
Teasing out antidepressant effect
Of participants with a history of depression treatment, 8,203 experienced at least one AE during the 12 months after treatment initiation (n = 47,486 AEs). Approximately half (50.8%) filled an antidepressant prescription at least once during the 12 months after the opioid episode began.
AEs were more likely among men than among women. The highest risk was in patients aged 18-24 years.
After adjusting for age and sex, participants who had received antidepressants had a greater risk for all adverse outcomes during the first 6 weeks of antidepressant treatment. However, those who had received antidepressants for 6 weeks or longer were at reduced risk for all adverse outcomes.

“We took advantage of the fact that, for most people, antidepressants take a while to work and aren’t immediately effective, so we were able to use that difference in our research,” Dr. Stein said.
“We wouldn’t expect to see an immediate effect of antidepressants, so the difference between what we saw immediately after the person had started treatment and the time it took for the antidepressant to be effective enabled us to tease out the effect of the antidepressant,” he added.
Consider CBT?
Andrew Saxon, MD, professor, department of psychiatry and behavioral sciences, University of Washington School of Medicine, Seattle, said clinicians “tend to think categorically and give people diagnoses that are clear-cut.” But neurobiologically, “it may be hard to distinguish where chronic pain ends and depression begins, or whether there’s some commonality.”
For patients with chronic pain and those taking opioids, “we need to be very attuned to the possibility or likelihood that they have major depression and other psychiatric diagnoses, like PTSD and anxiety disorders, which are very common,” said Dr. Saxon, who is also the director of the Center of Excellence in Substance Abuse Treatment and Education at the VA Puget Sound Health Care System. He was not involved with the current research.
He noted that treating those disorders “is a very important component of managing chronic pain.” However, “patients just starting antidepressants need to be carefully monitored when they’re getting stabilized on their antidepressants because they can have side effects, particularly early on, that can destabilize them.”
Dr. Saxon added that beyond pharmacotherapy, cognitive-behavioral therapy (CBT) for pain might be an even better intervention for addressing both pain and depression.
Also commenting for this article, Brian Hurley, MD, an addiction medicine specialist and the medical director of the Division of Substance Abuse Prevention and Control for the Los Angeles County Department of Public Health, said: “In the context of the largest wave of overdose mortality in U.S. history, we know comparatively little about the impact of mental health interventions that mitigate overdose risks.”
This study “contributes important new information that treating depression with antidepressant medications reduces overdose and self-harm risks for people who are prescribed opioids,” said Dr. Hurley, who is also the president-elect of the American Society of Addiction Medicine.
It also “underscores the general importance of integrated mental health and substance use disorder treatment in both primary care and in mental health settings,” added Dr. Hurley, who was not involved with the study.
The study was funded by the National Institute on Drug Abuse. The investigators and commenters reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PSYCHIATRIC SERVICES














