User login
Black women have higher state-level rates of TNBC
New national data on the occurrence of triple-negative breast cancer (TNBC) among different racial groups confirms that the disease is more common among Black women nationwide. A state-by-state analysis in the study, published online in JAMA Oncology, shows that these trends persist at the state level.
The analysis revealed that incidence rate ratios of TNBC were significantly higher among Black women, compared with White women, in all states with data on this population. Rates ranged from a low of 1.38 in Colorado to a high of 2.32 in Delaware.
The state-level disparities highlight gaps in physicians’ understanding of how social factors contribute to disparities in TNBC risk and the need “to develop effective preventative measures,” the study authors explain.
“We’ve realized for a long time that Black women have a higher incidence of TNBC. This is related to the genetic signature of the cancer. So that is not at all surprising,” said Arnold M. Baskies, MD, past chairman of the national board of directors of the American Cancer Society, Atlanta, who was not involved in the research. However, “the variance of TNBC among women from state to state is somewhat surprising.”
Existing research shows that TNBC is diagnosed more frequently among non-Hispanic Black women than among other populations in the United States, but it’s unclear whether these racial and ethnic disparities differ at the state level.
The authors identified 133,579 women with TNBC from the U.S. Cancer Statistics Public Use Research Database whose conditions were diagnosed from January 2015 through the end of December 2019. Most patients (64.5%) were White, 21.5% were Black, nearly 10% were Hispanic, 3.7% were Asian or Pacific Islander, and 0.6% were American Indian or Alaska Native. States with fewer than 30 cases were excluded, as was Nevada, owing to concerns regarding data quality. That left eight states for American Indian or Alaska Natives, 22 for Asian or Pacific Islanders, 35 for Hispanic women, 38 for Black women, and 50 for White women.
Overall, the incidence ratios of TNBC were highest among Black women (IR, 25.2 per 100,000), followed by White women (IR, 12.9 per 100,000), American Indian or Alaska Native women (IR, 11.2 per 100,000), Hispanic women (IR, 11.1 per 100,000 women), and Asian or Pacific Islander (IR, 9.0 per 100,000) women.
The authors also uncovered significant state-by-state variations in TNBC incidence by racial and ethnic groups. The lowest IR rates occurred among Asian or Pacific Islander women in Oregon and Pennsylvania – fewer than 7 per 100,000 women – and the highest occurred among Black women in Delaware, Missouri, Louisiana, and Mississippi – more than 29 per 100,000 women.
In the 38 states for which data on Black women were available, IR rates were significantly higher among Black women in all 38, compared with White women. The IR rates ranged from a low of 1.38 (IR, 17.4 per 100 000 women) in Colorado to a high of 2.32 (IR, 32.0 per 100 000 women) in Delaware.
While genetics play a role in TNBC risk, “the substantial geographic variation we found within each racial and ethnic group is highly suggestive that there are structural, environmental, and social factors at play in determining women’s risk of TNBC,” said lead study author Hyuna Sung, PhD, senior principal scientist and cancer epidemiologist at the American Cancer Society, Atlanta.
Existing evidence indicates that Black and White women living in socioeconomically disadvantaged neighborhoods are at higher risk of developing more aggressive subtypes of breast cancer, Dr. Sung said. Another factor, Dr. Sung and co-authors note, is breastfeeding. Across races, women who breastfeed have lower rates of TNBC.
Getting more definitive answers as to what causes differences in TNBC rates across states and what strategies can help reduce these disparities will be difficult and requires more research. “We really need to do a better job at researching and treating TNBC to improve health care equality for all women,” Dr. Baskies said. “The mortality rates from this cancer are high, and we rely heavily on surgery and toxic chemotherapy to treat it.”
Dr. Sung agreed, noting that “the observed state variation in TNBC rates merits further studies with risk factor data at multiple levels to better understand the associations of social exposures with the risk of TNBC.”
In states such as Louisiana and Mississippi, which are known to have a disproportionately higher burden of many types of cancers, “addressing barriers to access to preventive care and empowering public health efforts to promote a healthy living environment are the best policy prescription that could be deduced from our results,” Dr. Sung concluded.
Dr. Baskies is on the board of directors of Anixa Biosciences, which is currently conducting a clinical trial of a TNBC vaccine at the Cleveland Clinic. Dr. Sung has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New national data on the occurrence of triple-negative breast cancer (TNBC) among different racial groups confirms that the disease is more common among Black women nationwide. A state-by-state analysis in the study, published online in JAMA Oncology, shows that these trends persist at the state level.
The analysis revealed that incidence rate ratios of TNBC were significantly higher among Black women, compared with White women, in all states with data on this population. Rates ranged from a low of 1.38 in Colorado to a high of 2.32 in Delaware.
The state-level disparities highlight gaps in physicians’ understanding of how social factors contribute to disparities in TNBC risk and the need “to develop effective preventative measures,” the study authors explain.
“We’ve realized for a long time that Black women have a higher incidence of TNBC. This is related to the genetic signature of the cancer. So that is not at all surprising,” said Arnold M. Baskies, MD, past chairman of the national board of directors of the American Cancer Society, Atlanta, who was not involved in the research. However, “the variance of TNBC among women from state to state is somewhat surprising.”
Existing research shows that TNBC is diagnosed more frequently among non-Hispanic Black women than among other populations in the United States, but it’s unclear whether these racial and ethnic disparities differ at the state level.
The authors identified 133,579 women with TNBC from the U.S. Cancer Statistics Public Use Research Database whose conditions were diagnosed from January 2015 through the end of December 2019. Most patients (64.5%) were White, 21.5% were Black, nearly 10% were Hispanic, 3.7% were Asian or Pacific Islander, and 0.6% were American Indian or Alaska Native. States with fewer than 30 cases were excluded, as was Nevada, owing to concerns regarding data quality. That left eight states for American Indian or Alaska Natives, 22 for Asian or Pacific Islanders, 35 for Hispanic women, 38 for Black women, and 50 for White women.
Overall, the incidence ratios of TNBC were highest among Black women (IR, 25.2 per 100,000), followed by White women (IR, 12.9 per 100,000), American Indian or Alaska Native women (IR, 11.2 per 100,000), Hispanic women (IR, 11.1 per 100,000 women), and Asian or Pacific Islander (IR, 9.0 per 100,000) women.
The authors also uncovered significant state-by-state variations in TNBC incidence by racial and ethnic groups. The lowest IR rates occurred among Asian or Pacific Islander women in Oregon and Pennsylvania – fewer than 7 per 100,000 women – and the highest occurred among Black women in Delaware, Missouri, Louisiana, and Mississippi – more than 29 per 100,000 women.
In the 38 states for which data on Black women were available, IR rates were significantly higher among Black women in all 38, compared with White women. The IR rates ranged from a low of 1.38 (IR, 17.4 per 100 000 women) in Colorado to a high of 2.32 (IR, 32.0 per 100 000 women) in Delaware.
While genetics play a role in TNBC risk, “the substantial geographic variation we found within each racial and ethnic group is highly suggestive that there are structural, environmental, and social factors at play in determining women’s risk of TNBC,” said lead study author Hyuna Sung, PhD, senior principal scientist and cancer epidemiologist at the American Cancer Society, Atlanta.
Existing evidence indicates that Black and White women living in socioeconomically disadvantaged neighborhoods are at higher risk of developing more aggressive subtypes of breast cancer, Dr. Sung said. Another factor, Dr. Sung and co-authors note, is breastfeeding. Across races, women who breastfeed have lower rates of TNBC.
Getting more definitive answers as to what causes differences in TNBC rates across states and what strategies can help reduce these disparities will be difficult and requires more research. “We really need to do a better job at researching and treating TNBC to improve health care equality for all women,” Dr. Baskies said. “The mortality rates from this cancer are high, and we rely heavily on surgery and toxic chemotherapy to treat it.”
Dr. Sung agreed, noting that “the observed state variation in TNBC rates merits further studies with risk factor data at multiple levels to better understand the associations of social exposures with the risk of TNBC.”
In states such as Louisiana and Mississippi, which are known to have a disproportionately higher burden of many types of cancers, “addressing barriers to access to preventive care and empowering public health efforts to promote a healthy living environment are the best policy prescription that could be deduced from our results,” Dr. Sung concluded.
Dr. Baskies is on the board of directors of Anixa Biosciences, which is currently conducting a clinical trial of a TNBC vaccine at the Cleveland Clinic. Dr. Sung has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New national data on the occurrence of triple-negative breast cancer (TNBC) among different racial groups confirms that the disease is more common among Black women nationwide. A state-by-state analysis in the study, published online in JAMA Oncology, shows that these trends persist at the state level.
The analysis revealed that incidence rate ratios of TNBC were significantly higher among Black women, compared with White women, in all states with data on this population. Rates ranged from a low of 1.38 in Colorado to a high of 2.32 in Delaware.
The state-level disparities highlight gaps in physicians’ understanding of how social factors contribute to disparities in TNBC risk and the need “to develop effective preventative measures,” the study authors explain.
“We’ve realized for a long time that Black women have a higher incidence of TNBC. This is related to the genetic signature of the cancer. So that is not at all surprising,” said Arnold M. Baskies, MD, past chairman of the national board of directors of the American Cancer Society, Atlanta, who was not involved in the research. However, “the variance of TNBC among women from state to state is somewhat surprising.”
Existing research shows that TNBC is diagnosed more frequently among non-Hispanic Black women than among other populations in the United States, but it’s unclear whether these racial and ethnic disparities differ at the state level.
The authors identified 133,579 women with TNBC from the U.S. Cancer Statistics Public Use Research Database whose conditions were diagnosed from January 2015 through the end of December 2019. Most patients (64.5%) were White, 21.5% were Black, nearly 10% were Hispanic, 3.7% were Asian or Pacific Islander, and 0.6% were American Indian or Alaska Native. States with fewer than 30 cases were excluded, as was Nevada, owing to concerns regarding data quality. That left eight states for American Indian or Alaska Natives, 22 for Asian or Pacific Islanders, 35 for Hispanic women, 38 for Black women, and 50 for White women.
Overall, the incidence ratios of TNBC were highest among Black women (IR, 25.2 per 100,000), followed by White women (IR, 12.9 per 100,000), American Indian or Alaska Native women (IR, 11.2 per 100,000), Hispanic women (IR, 11.1 per 100,000 women), and Asian or Pacific Islander (IR, 9.0 per 100,000) women.
The authors also uncovered significant state-by-state variations in TNBC incidence by racial and ethnic groups. The lowest IR rates occurred among Asian or Pacific Islander women in Oregon and Pennsylvania – fewer than 7 per 100,000 women – and the highest occurred among Black women in Delaware, Missouri, Louisiana, and Mississippi – more than 29 per 100,000 women.
In the 38 states for which data on Black women were available, IR rates were significantly higher among Black women in all 38, compared with White women. The IR rates ranged from a low of 1.38 (IR, 17.4 per 100 000 women) in Colorado to a high of 2.32 (IR, 32.0 per 100 000 women) in Delaware.
While genetics play a role in TNBC risk, “the substantial geographic variation we found within each racial and ethnic group is highly suggestive that there are structural, environmental, and social factors at play in determining women’s risk of TNBC,” said lead study author Hyuna Sung, PhD, senior principal scientist and cancer epidemiologist at the American Cancer Society, Atlanta.
Existing evidence indicates that Black and White women living in socioeconomically disadvantaged neighborhoods are at higher risk of developing more aggressive subtypes of breast cancer, Dr. Sung said. Another factor, Dr. Sung and co-authors note, is breastfeeding. Across races, women who breastfeed have lower rates of TNBC.
Getting more definitive answers as to what causes differences in TNBC rates across states and what strategies can help reduce these disparities will be difficult and requires more research. “We really need to do a better job at researching and treating TNBC to improve health care equality for all women,” Dr. Baskies said. “The mortality rates from this cancer are high, and we rely heavily on surgery and toxic chemotherapy to treat it.”
Dr. Sung agreed, noting that “the observed state variation in TNBC rates merits further studies with risk factor data at multiple levels to better understand the associations of social exposures with the risk of TNBC.”
In states such as Louisiana and Mississippi, which are known to have a disproportionately higher burden of many types of cancers, “addressing barriers to access to preventive care and empowering public health efforts to promote a healthy living environment are the best policy prescription that could be deduced from our results,” Dr. Sung concluded.
Dr. Baskies is on the board of directors of Anixa Biosciences, which is currently conducting a clinical trial of a TNBC vaccine at the Cleveland Clinic. Dr. Sung has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Black people are less likely to receive dementia meds
, preliminary data from a retrospective study show.
“There have been disparities regarding the use of cognition-enhancing medications in the treatment of dementia described in the literature, and disparities in the use of adjunctive treatments for other neuropsychiatric symptoms of dementia described in hospital and nursing home settings,” said study investigator Alice Hawkins, MD, with the department of neurology, Icahn School of Medicine at Mount Sinai, New York. “However, less is known about use of dementia medications that people take at home. Our study found disparities in this area as well,” Dr. Hawkins said.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
More research needed
The researchers analyzed data on 3,655 Black and 12,885 White patients with a diagnosis of dementia who were seen at Mount Sinai. They evaluated utilization of five medication classes:
- cholinesterase inhibitors.
- N-methyl D-aspartate (NMDA) receptor antagonists.
- selective serotonin reuptake inhibitors (SSRIs).
- antipsychotics.
- benzodiazepines.
They found that Black patients with dementia received cognitive enhancers less often than White patients with dementia (20% vs. 30% for cholinesterase inhibitors; 10% vs. 17% for NMDA antagonists).
Black patients with dementia were also less likely to receive medications for behavioral and psychological symptom management, compared with White peers (24% vs. 40% for SSRIs; 18% vs. 22% for antipsychotics; and 18% vs. 37% for benzodiazepines).
These disparities remained even after controlling for factors such as demographics and insurance coverage.
“Larger systemic forces such as systemic racism, quality of care, and provider bias are harder to pin down, particularly in the medical record, though they all may be playing a role in perpetuating these inequities. More research will be needed to pinpoint all the factors that are contributing to these disparities,” said Dr. Hawkins.
The researchers found Black patients who were referred to a neurologist received cholinesterase inhibitors and NMDA antagonists at rates comparable with White patients. “Therefore, referrals to specialists such as neurologists may decrease the disparities for these prescriptions,” Dr. Hawkins said.
Crucial research
Commenting on the findings, Carl V. Hill, PhD, MPH, Alzheimer’s Association chief diversity, equity, and inclusion officer, said the study “adds to previous research that points to inequities in the administering of medications for dementia symptoms, and highlights the inequities we know exist in dementia care.”
“Cognitive enhancers and other behavioral/psychological management drugs, while they don’t stop, slow, or cure dementia, can offer relief for some of the challenging symptoms associated with diseases caused by dementia. If people aren’t being appropriately prescribed medications that may offer symptom relief from this challenging disease, it could lead to poorer health outcomes,” said Dr. Hill.
“These data underscore the importance of health disparities research that is crucial in uncovering inequities in dementia treatment, care, and research for Black individuals, as well as all underrepresented populations.
“We must create a society in which the underserved, disproportionately affected, and underrepresented are safe, cared for, and valued. This can be done through enhancing cultural competence in health care settings, improving representation within the health care system, and engaging and building trust with diverse communities,” Dr. Hill said.
The Alzheimer’s Association has partnered with more than 500 diverse community-based groups on disease education programs to ensure families have information and resources to navigate this devastating disease.
The study was supported by the American Academy of Neurology Resident Research Scholarship. Dr. Hawkins and Dr. Hill reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, preliminary data from a retrospective study show.
“There have been disparities regarding the use of cognition-enhancing medications in the treatment of dementia described in the literature, and disparities in the use of adjunctive treatments for other neuropsychiatric symptoms of dementia described in hospital and nursing home settings,” said study investigator Alice Hawkins, MD, with the department of neurology, Icahn School of Medicine at Mount Sinai, New York. “However, less is known about use of dementia medications that people take at home. Our study found disparities in this area as well,” Dr. Hawkins said.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
More research needed
The researchers analyzed data on 3,655 Black and 12,885 White patients with a diagnosis of dementia who were seen at Mount Sinai. They evaluated utilization of five medication classes:
- cholinesterase inhibitors.
- N-methyl D-aspartate (NMDA) receptor antagonists.
- selective serotonin reuptake inhibitors (SSRIs).
- antipsychotics.
- benzodiazepines.
They found that Black patients with dementia received cognitive enhancers less often than White patients with dementia (20% vs. 30% for cholinesterase inhibitors; 10% vs. 17% for NMDA antagonists).
Black patients with dementia were also less likely to receive medications for behavioral and psychological symptom management, compared with White peers (24% vs. 40% for SSRIs; 18% vs. 22% for antipsychotics; and 18% vs. 37% for benzodiazepines).
These disparities remained even after controlling for factors such as demographics and insurance coverage.
“Larger systemic forces such as systemic racism, quality of care, and provider bias are harder to pin down, particularly in the medical record, though they all may be playing a role in perpetuating these inequities. More research will be needed to pinpoint all the factors that are contributing to these disparities,” said Dr. Hawkins.
The researchers found Black patients who were referred to a neurologist received cholinesterase inhibitors and NMDA antagonists at rates comparable with White patients. “Therefore, referrals to specialists such as neurologists may decrease the disparities for these prescriptions,” Dr. Hawkins said.
Crucial research
Commenting on the findings, Carl V. Hill, PhD, MPH, Alzheimer’s Association chief diversity, equity, and inclusion officer, said the study “adds to previous research that points to inequities in the administering of medications for dementia symptoms, and highlights the inequities we know exist in dementia care.”
“Cognitive enhancers and other behavioral/psychological management drugs, while they don’t stop, slow, or cure dementia, can offer relief for some of the challenging symptoms associated with diseases caused by dementia. If people aren’t being appropriately prescribed medications that may offer symptom relief from this challenging disease, it could lead to poorer health outcomes,” said Dr. Hill.
“These data underscore the importance of health disparities research that is crucial in uncovering inequities in dementia treatment, care, and research for Black individuals, as well as all underrepresented populations.
“We must create a society in which the underserved, disproportionately affected, and underrepresented are safe, cared for, and valued. This can be done through enhancing cultural competence in health care settings, improving representation within the health care system, and engaging and building trust with diverse communities,” Dr. Hill said.
The Alzheimer’s Association has partnered with more than 500 diverse community-based groups on disease education programs to ensure families have information and resources to navigate this devastating disease.
The study was supported by the American Academy of Neurology Resident Research Scholarship. Dr. Hawkins and Dr. Hill reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, preliminary data from a retrospective study show.
“There have been disparities regarding the use of cognition-enhancing medications in the treatment of dementia described in the literature, and disparities in the use of adjunctive treatments for other neuropsychiatric symptoms of dementia described in hospital and nursing home settings,” said study investigator Alice Hawkins, MD, with the department of neurology, Icahn School of Medicine at Mount Sinai, New York. “However, less is known about use of dementia medications that people take at home. Our study found disparities in this area as well,” Dr. Hawkins said.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
More research needed
The researchers analyzed data on 3,655 Black and 12,885 White patients with a diagnosis of dementia who were seen at Mount Sinai. They evaluated utilization of five medication classes:
- cholinesterase inhibitors.
- N-methyl D-aspartate (NMDA) receptor antagonists.
- selective serotonin reuptake inhibitors (SSRIs).
- antipsychotics.
- benzodiazepines.
They found that Black patients with dementia received cognitive enhancers less often than White patients with dementia (20% vs. 30% for cholinesterase inhibitors; 10% vs. 17% for NMDA antagonists).
Black patients with dementia were also less likely to receive medications for behavioral and psychological symptom management, compared with White peers (24% vs. 40% for SSRIs; 18% vs. 22% for antipsychotics; and 18% vs. 37% for benzodiazepines).
These disparities remained even after controlling for factors such as demographics and insurance coverage.
“Larger systemic forces such as systemic racism, quality of care, and provider bias are harder to pin down, particularly in the medical record, though they all may be playing a role in perpetuating these inequities. More research will be needed to pinpoint all the factors that are contributing to these disparities,” said Dr. Hawkins.
The researchers found Black patients who were referred to a neurologist received cholinesterase inhibitors and NMDA antagonists at rates comparable with White patients. “Therefore, referrals to specialists such as neurologists may decrease the disparities for these prescriptions,” Dr. Hawkins said.
Crucial research
Commenting on the findings, Carl V. Hill, PhD, MPH, Alzheimer’s Association chief diversity, equity, and inclusion officer, said the study “adds to previous research that points to inequities in the administering of medications for dementia symptoms, and highlights the inequities we know exist in dementia care.”
“Cognitive enhancers and other behavioral/psychological management drugs, while they don’t stop, slow, or cure dementia, can offer relief for some of the challenging symptoms associated with diseases caused by dementia. If people aren’t being appropriately prescribed medications that may offer symptom relief from this challenging disease, it could lead to poorer health outcomes,” said Dr. Hill.
“These data underscore the importance of health disparities research that is crucial in uncovering inequities in dementia treatment, care, and research for Black individuals, as well as all underrepresented populations.
“We must create a society in which the underserved, disproportionately affected, and underrepresented are safe, cared for, and valued. This can be done through enhancing cultural competence in health care settings, improving representation within the health care system, and engaging and building trust with diverse communities,” Dr. Hill said.
The Alzheimer’s Association has partnered with more than 500 diverse community-based groups on disease education programs to ensure families have information and resources to navigate this devastating disease.
The study was supported by the American Academy of Neurology Resident Research Scholarship. Dr. Hawkins and Dr. Hill reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term BP reductions with renal denervation not race specific
WASHINGTON – On the heels the recently published final report from the SYMPLICITY HTN-3 renal denervation trial, a new analysis showed that Black patients, like non-Blacks, had sustained blood pressure control.
Contrary to a signal from earlier results, “there is nothing race specific about renal denervation,” said presenter Deepak L. Bhatt, MD, at the Cardiovascular Research Technologies conference, sponsored by MedStar Heart & Vascular Institute.
Black patients are well represented among patients with treatment-resistant hypertension and considered an important subgroup to target, according to Dr. Bhatt, director of Mount Sinai Heart, New York. This is the reason that they were not only a prespecified subgroup in SYMPLICITY HTN-3, but race was one of two stratification factors at enrollment. At the time of the study design, there was an expectation that Black patients would benefit more than non-Blacks.
This did not prove to be the case during the 6-month controlled phase of the trial. When patients randomized to renal denervation or the sham procedure were stratified by race, the primary endpoint of reduction in office systolic blood pressure (SBP) reached significance in the experimental arm among non-Black patients (–6.63 mm Hg; P = .01), but not among Black patients (–2.25 mm Hg; P = .09).
Blacks comprised 26% of SYMPLICITY HTN-3 trial
In the initial controlled analysis, published in the New England Journal of Medicine, the lack of benefit in the substantial Black enrollment – representing 26% of the study total – weighed against the ability of the trial to demonstrate a benefit, but Dr. Bhatt pointed out that BP reductions were unexpectedly high in the sham group regardless of race. Patients randomized to the sham group were encouraged to adhere to antihypertensive therapy, and based on response, this was particularly effective in the Black sham subgroup.
In SYMPLICITY HTN-3, patients with treatment-resistant hypertension were randomized to renal denervation or a sham procedure in a 2:1 ratio. While the controlled phase lasted just 6 months, the follow-up after the study was unblinded has continued out to 3 years. Safety and efficacy were assessed at 12, 24, and 36 months.
Unlike the disappointing results at 6 months, renal denervation has been consistently associated with significantly lower BP over long-term follow-up, even though those randomized to the sham procedure were permitted to cross over. About two-thirds of the sham group did so.
In the recently published final report of SYMPLICITY, the overall median change in office SBP at 3 years regardless of race was –26.4 mm Hg in the group initially randomized to renal denervation versus –5.7 mm Hg (P < .0001) among those randomized to the sham procedure.
In the subgroup analysis presented by Dr. Bhatt, the relative control of office SBP, as well as other measures of blood pressure, were similarly and significantly reduced in both Black and non-Black patients. In general, the relative control offered by being randomized initially to renal denervation increased over time in both groups.
For example, the relative reduction in office SBP favoring renal denervation climbed from –12.0 mm Hg at 12 months (P = .0066) to –21.0 at 18 months (P = .0002) and then to –24.9 mm Hg (P < .0001) at 36 months in the Black subgroup. In non-Blacks, the same type of relative reductions were seen at each time point, climbing from –13.5 (P < .0001) to –20.5 (P < .0001) and then to –21.0 (P < .0001).
The comparisons for other measures of BP control, including office diastolic BP, 24-hour SBP, and BP control during morning, day, and night periods were also statistically and similarly improved for those initially randomized to renal denervation rather than a sham procedure among both Blacks and non-Blacks.
Renal denervation safe in Black and non-Black patients
Renal denervation was well tolerated in both Black and non-Black participants with no signal of long-term risks over 36 months in either group. Among Blacks, rates of death at 36 months (3% vs. 11%) and stroke (7% vs. 11%) were lower among those randomized to renal denervation relative to sham patients who never crossed over, but Dr. Bhatt said the numbers are too small to draw any conclusions about outcomes.
While this subgroup analysis, along with the final SYMPLICITY report, supports the efficacy of renal denervation over the long term, these data are also consistent with the recently published analysis of SPYRAL ON-MED . Together, these data have led many experts, including Dr. Bhatt, to conclude that renal denervation is effective and deserves regulatory approval.
“In out-of-control blood pressure, when patients have maxed out on medications and lifestyle, I think renal denervation is efficacious, and it is equally efficacious in Blacks and non-Blacks,” Dr. Bhatt said.
This subgroup analysis is important because of the need for options in treatment-resistant hypertension among Black as well as non-Black patients, pointed out Sripal Bangalore, MBBS, director of complex coronary intervention at New York University.
“I am glad that we did not conclude too soon that it does not work in Blacks,” Dr. Bangalore said. If renal denervation is approved, he expects this procedure to be a valuable tool in this racial group.
Dr. Bhatt reported financial relationship with more than 20 pharmaceutical and device companies, including Medtronic, which provided funding for the SYMPLICITY HTN-3 trial. Dr. Bangalore has financial relationships with Abbott Vascular, Amgen, Biotronik, Inari, Pfizer, Reata, and Truvic.
WASHINGTON – On the heels the recently published final report from the SYMPLICITY HTN-3 renal denervation trial, a new analysis showed that Black patients, like non-Blacks, had sustained blood pressure control.
Contrary to a signal from earlier results, “there is nothing race specific about renal denervation,” said presenter Deepak L. Bhatt, MD, at the Cardiovascular Research Technologies conference, sponsored by MedStar Heart & Vascular Institute.
Black patients are well represented among patients with treatment-resistant hypertension and considered an important subgroup to target, according to Dr. Bhatt, director of Mount Sinai Heart, New York. This is the reason that they were not only a prespecified subgroup in SYMPLICITY HTN-3, but race was one of two stratification factors at enrollment. At the time of the study design, there was an expectation that Black patients would benefit more than non-Blacks.
This did not prove to be the case during the 6-month controlled phase of the trial. When patients randomized to renal denervation or the sham procedure were stratified by race, the primary endpoint of reduction in office systolic blood pressure (SBP) reached significance in the experimental arm among non-Black patients (–6.63 mm Hg; P = .01), but not among Black patients (–2.25 mm Hg; P = .09).
Blacks comprised 26% of SYMPLICITY HTN-3 trial
In the initial controlled analysis, published in the New England Journal of Medicine, the lack of benefit in the substantial Black enrollment – representing 26% of the study total – weighed against the ability of the trial to demonstrate a benefit, but Dr. Bhatt pointed out that BP reductions were unexpectedly high in the sham group regardless of race. Patients randomized to the sham group were encouraged to adhere to antihypertensive therapy, and based on response, this was particularly effective in the Black sham subgroup.
In SYMPLICITY HTN-3, patients with treatment-resistant hypertension were randomized to renal denervation or a sham procedure in a 2:1 ratio. While the controlled phase lasted just 6 months, the follow-up after the study was unblinded has continued out to 3 years. Safety and efficacy were assessed at 12, 24, and 36 months.
Unlike the disappointing results at 6 months, renal denervation has been consistently associated with significantly lower BP over long-term follow-up, even though those randomized to the sham procedure were permitted to cross over. About two-thirds of the sham group did so.
In the recently published final report of SYMPLICITY, the overall median change in office SBP at 3 years regardless of race was –26.4 mm Hg in the group initially randomized to renal denervation versus –5.7 mm Hg (P < .0001) among those randomized to the sham procedure.
In the subgroup analysis presented by Dr. Bhatt, the relative control of office SBP, as well as other measures of blood pressure, were similarly and significantly reduced in both Black and non-Black patients. In general, the relative control offered by being randomized initially to renal denervation increased over time in both groups.
For example, the relative reduction in office SBP favoring renal denervation climbed from –12.0 mm Hg at 12 months (P = .0066) to –21.0 at 18 months (P = .0002) and then to –24.9 mm Hg (P < .0001) at 36 months in the Black subgroup. In non-Blacks, the same type of relative reductions were seen at each time point, climbing from –13.5 (P < .0001) to –20.5 (P < .0001) and then to –21.0 (P < .0001).
The comparisons for other measures of BP control, including office diastolic BP, 24-hour SBP, and BP control during morning, day, and night periods were also statistically and similarly improved for those initially randomized to renal denervation rather than a sham procedure among both Blacks and non-Blacks.
Renal denervation safe in Black and non-Black patients
Renal denervation was well tolerated in both Black and non-Black participants with no signal of long-term risks over 36 months in either group. Among Blacks, rates of death at 36 months (3% vs. 11%) and stroke (7% vs. 11%) were lower among those randomized to renal denervation relative to sham patients who never crossed over, but Dr. Bhatt said the numbers are too small to draw any conclusions about outcomes.
While this subgroup analysis, along with the final SYMPLICITY report, supports the efficacy of renal denervation over the long term, these data are also consistent with the recently published analysis of SPYRAL ON-MED . Together, these data have led many experts, including Dr. Bhatt, to conclude that renal denervation is effective and deserves regulatory approval.
“In out-of-control blood pressure, when patients have maxed out on medications and lifestyle, I think renal denervation is efficacious, and it is equally efficacious in Blacks and non-Blacks,” Dr. Bhatt said.
This subgroup analysis is important because of the need for options in treatment-resistant hypertension among Black as well as non-Black patients, pointed out Sripal Bangalore, MBBS, director of complex coronary intervention at New York University.
“I am glad that we did not conclude too soon that it does not work in Blacks,” Dr. Bangalore said. If renal denervation is approved, he expects this procedure to be a valuable tool in this racial group.
Dr. Bhatt reported financial relationship with more than 20 pharmaceutical and device companies, including Medtronic, which provided funding for the SYMPLICITY HTN-3 trial. Dr. Bangalore has financial relationships with Abbott Vascular, Amgen, Biotronik, Inari, Pfizer, Reata, and Truvic.
WASHINGTON – On the heels the recently published final report from the SYMPLICITY HTN-3 renal denervation trial, a new analysis showed that Black patients, like non-Blacks, had sustained blood pressure control.
Contrary to a signal from earlier results, “there is nothing race specific about renal denervation,” said presenter Deepak L. Bhatt, MD, at the Cardiovascular Research Technologies conference, sponsored by MedStar Heart & Vascular Institute.
Black patients are well represented among patients with treatment-resistant hypertension and considered an important subgroup to target, according to Dr. Bhatt, director of Mount Sinai Heart, New York. This is the reason that they were not only a prespecified subgroup in SYMPLICITY HTN-3, but race was one of two stratification factors at enrollment. At the time of the study design, there was an expectation that Black patients would benefit more than non-Blacks.
This did not prove to be the case during the 6-month controlled phase of the trial. When patients randomized to renal denervation or the sham procedure were stratified by race, the primary endpoint of reduction in office systolic blood pressure (SBP) reached significance in the experimental arm among non-Black patients (–6.63 mm Hg; P = .01), but not among Black patients (–2.25 mm Hg; P = .09).
Blacks comprised 26% of SYMPLICITY HTN-3 trial
In the initial controlled analysis, published in the New England Journal of Medicine, the lack of benefit in the substantial Black enrollment – representing 26% of the study total – weighed against the ability of the trial to demonstrate a benefit, but Dr. Bhatt pointed out that BP reductions were unexpectedly high in the sham group regardless of race. Patients randomized to the sham group were encouraged to adhere to antihypertensive therapy, and based on response, this was particularly effective in the Black sham subgroup.
In SYMPLICITY HTN-3, patients with treatment-resistant hypertension were randomized to renal denervation or a sham procedure in a 2:1 ratio. While the controlled phase lasted just 6 months, the follow-up after the study was unblinded has continued out to 3 years. Safety and efficacy were assessed at 12, 24, and 36 months.
Unlike the disappointing results at 6 months, renal denervation has been consistently associated with significantly lower BP over long-term follow-up, even though those randomized to the sham procedure were permitted to cross over. About two-thirds of the sham group did so.
In the recently published final report of SYMPLICITY, the overall median change in office SBP at 3 years regardless of race was –26.4 mm Hg in the group initially randomized to renal denervation versus –5.7 mm Hg (P < .0001) among those randomized to the sham procedure.
In the subgroup analysis presented by Dr. Bhatt, the relative control of office SBP, as well as other measures of blood pressure, were similarly and significantly reduced in both Black and non-Black patients. In general, the relative control offered by being randomized initially to renal denervation increased over time in both groups.
For example, the relative reduction in office SBP favoring renal denervation climbed from –12.0 mm Hg at 12 months (P = .0066) to –21.0 at 18 months (P = .0002) and then to –24.9 mm Hg (P < .0001) at 36 months in the Black subgroup. In non-Blacks, the same type of relative reductions were seen at each time point, climbing from –13.5 (P < .0001) to –20.5 (P < .0001) and then to –21.0 (P < .0001).
The comparisons for other measures of BP control, including office diastolic BP, 24-hour SBP, and BP control during morning, day, and night periods were also statistically and similarly improved for those initially randomized to renal denervation rather than a sham procedure among both Blacks and non-Blacks.
Renal denervation safe in Black and non-Black patients
Renal denervation was well tolerated in both Black and non-Black participants with no signal of long-term risks over 36 months in either group. Among Blacks, rates of death at 36 months (3% vs. 11%) and stroke (7% vs. 11%) were lower among those randomized to renal denervation relative to sham patients who never crossed over, but Dr. Bhatt said the numbers are too small to draw any conclusions about outcomes.
While this subgroup analysis, along with the final SYMPLICITY report, supports the efficacy of renal denervation over the long term, these data are also consistent with the recently published analysis of SPYRAL ON-MED . Together, these data have led many experts, including Dr. Bhatt, to conclude that renal denervation is effective and deserves regulatory approval.
“In out-of-control blood pressure, when patients have maxed out on medications and lifestyle, I think renal denervation is efficacious, and it is equally efficacious in Blacks and non-Blacks,” Dr. Bhatt said.
This subgroup analysis is important because of the need for options in treatment-resistant hypertension among Black as well as non-Black patients, pointed out Sripal Bangalore, MBBS, director of complex coronary intervention at New York University.
“I am glad that we did not conclude too soon that it does not work in Blacks,” Dr. Bangalore said. If renal denervation is approved, he expects this procedure to be a valuable tool in this racial group.
Dr. Bhatt reported financial relationship with more than 20 pharmaceutical and device companies, including Medtronic, which provided funding for the SYMPLICITY HTN-3 trial. Dr. Bangalore has financial relationships with Abbott Vascular, Amgen, Biotronik, Inari, Pfizer, Reata, and Truvic.
AT CRT 2023
Inequity, Bias, Racism, and Physician Burnout: Staying Connected to Purpose and Identity as an Antidote
“Where are you really from?”
When I tell patients I am from Casper, Wyoming—wh ere I have lived the majority of my life—it’smet with disbelief. The subtext: YOU can’t be from THERE.
I didn’t used to think much of comments like this, but as I have continued to hear them, I find myself feeling tired—tired of explaining myself, tired of being treated differently than my colleagues, and tired of justifying myself. My experiences as a woman of color sadly are not uncommon in medicine.
Sara Martinez-Garcia, BA
Racial bias and racism are steeped in the culture of medicine—from the medical school admissions process1,2 to the medical training itself.3 More than half of medical students who identify as underrepresented in medicine (UIM) experience microaggressions.4 Experiencing racism and sexism in the learning environment can lead to burnout, and microaggressions promote feelings of self-doubt and isolation. Medical students who experience microaggressions are more likely to report feelings of burnout and impaired learning.4 These experiences can leave one feeling as if “You do not belong” and “You are unworthy of being in this position.”
Addressing physician burnout already is complex, and addressing burnout caused by inequity, bias, and racism is even more so. In an ideal world, we would eliminate inequity, bias, and racism in medicine through institutional and individual actions. There has been movement to do so. For example, the Accreditation Council for Graduate Medical Education (ACGME), which oversees standards for US resident and fellow training, launched ACGME Equity Matters (https://www.acgme.org/what-we-do/diversity-equity-and-inclusion/ACGME-Equity-Matters/), an initiative aimed to improve diversity, equity, and antiracism practices within graduate medical eduation. However, we know that education alone isn’t enough to fix this monumental problem. Traditional diversity training as we have known it has never been demonstrated to contribute to lasting changes in behavior; it takes much more extensive and complex interventions to meaningfully reduce bias.5 In the meantime, we need action. As a medical community, we need to be better about not turning the other way when we see these things happening in our classrooms and in our hospitals. As individuals, we must self-reflect on the role that we each play in contributing to or combatting injustices and seek out bystander training to empower us to speak out against acts of bias such as sexism or racism. Whether it is supporting a fellow colleague or speaking out against an inappropriate interaction, we can all do our part. A very brief list of actions and resources to support our UIM students and colleagues are listed in the Table; those interested in more in-depth resources are encouraged to explore the Association of American Medical Colleges Diversity and Inclusion Toolkit (https://www.aamc.org/professional-development/affinity-groups/cfas/diversity-inclusion-toolkit/resources).

We can’t change the culture of medicine quickly or even in our lifetime. In the meantime, those who are UIM will continue to experience these events that erode our well-being. They will continue to need support. Discussing mental health has long been stigmatized, and physicians are no exception. Many physicians are hesitant to discuss mental health issues out of fear of judgement and perceived or even real repercussions on their careers.10 However, times are changing and evolving with the current generation of medical students. It’s no secret that medicine is stressful. Most medical schools provide free counseling services, which lowers the barrier for discussions of mental health from the beginning. Making talk about mental health just as normal as talking about other aspects of health takes away the fear that “something is wrong with me” if someone seeks out counseling and mental health services. Faculty should actively check in and maintain open lines of communication, which can be invaluable for UIM students and their training experience. Creating an environment where trainees can be real and honest about the struggles they face in and out of the classroom can make everyone feel like they are not alone.
Addressing burnout in medicine is going to require an all-hands-on-deck approach. At an institutional level, there is a lot of room for improvement—improving systems for physicians so they are able to operate at their highest level (eg, addressing the burdens of prior authorizations and the electronic medical record), setting reasonable expectations around productivity, and creating work structures that respect work-life balance.11 But what can we do for ourselves? We believe that one of the most important ways to protect ourselves from burnout is to remember why. As a medical student, there is enormous pressure—pressure to learn an enormous volume of information, pass examinations, get involved in extracurricular activities, make connections, and seek research opportunities, while also cooking healthy food, grocery shopping, maintaining relationships with loved ones, and generally taking care of oneself. At times it can feel as if our lives outside of medical school are not important enough or valuable enough to make time for, but the pieces of our identity outside of medicine are what shape us into who we are today and are the roots of our purpose in medicine. Sometimes you can feel the most motivated, valued, and supported when you make time to have dinner with friends, call a family member, or simply spend time alone in the outdoors. Who you are and how you got to this point in your life are your identity. Reminding yourself of that can help when experiencing microaggressions or when that voice tries to tell you that you are not worthy. As you progress further in your career, maintaining that relationship with who you are outside of medicine can be your armor against burnout.
- Capers Q IV, Clinchot D, McDougle L, et al. Implicit racial bias in medical school admissions. Acad Med. 2017;92:365-369.
- Lucey CR, Saguil A. The consequences of structural racism on MCAT scores and medical school admissions: the past is prologue. Acad Med. 2020;95:351-356.
- Nguemeni Tiako MJ, South EC, Ray V. Medical schools as racialized organizations: a primer. Ann Intern Med. 2021;174:1143-1144.
- Chisholm LP, Jackson KR, Davidson HA, et al. Evaluation of racial microaggressions experienced during medical school training and the effect on medical student education and burnout: a validation study. J Natl Med Assoc. 2021;113:310-314.
- Dobbin F, Kalev A. Why doesn’t diversity training work? the challenge for industry and academia. Anthropology Now. 2018;10:48-55.
- Okoye GA. Supporting underrepresented minority women in academic dermatology. Int J Womens Dermatol. 2020;6:57-60.
- Hackworth JM, Kotagal M, Bignall ONR, et al. Microaggressions: privileged observers’ duty to act and what they can do [published online December 1, 2021]. Pediatrics. doi:10.1542/peds.2021-052758.
- Wheeler DJ, Zapata J, Davis D, et al. Twelve tips for responding to microaggressions and overt discrimination: when the patient offends the learner. Med Teach. 2019;41:1112-1117.
- Scott K. Just Work: How to Root Out Bias, Prejudice, and Bullying to Build a Kick-Ass Culture of Inclusivity. St. Martin’s Press; 2021.
- Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003;289:3161-3166.
- West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283:516-529.
“Where are you really from?”
When I tell patients I am from Casper, Wyoming—wh ere I have lived the majority of my life—it’smet with disbelief. The subtext: YOU can’t be from THERE.
I didn’t used to think much of comments like this, but as I have continued to hear them, I find myself feeling tired—tired of explaining myself, tired of being treated differently than my colleagues, and tired of justifying myself. My experiences as a woman of color sadly are not uncommon in medicine.
Sara Martinez-Garcia, BA
Racial bias and racism are steeped in the culture of medicine—from the medical school admissions process1,2 to the medical training itself.3 More than half of medical students who identify as underrepresented in medicine (UIM) experience microaggressions.4 Experiencing racism and sexism in the learning environment can lead to burnout, and microaggressions promote feelings of self-doubt and isolation. Medical students who experience microaggressions are more likely to report feelings of burnout and impaired learning.4 These experiences can leave one feeling as if “You do not belong” and “You are unworthy of being in this position.”
Addressing physician burnout already is complex, and addressing burnout caused by inequity, bias, and racism is even more so. In an ideal world, we would eliminate inequity, bias, and racism in medicine through institutional and individual actions. There has been movement to do so. For example, the Accreditation Council for Graduate Medical Education (ACGME), which oversees standards for US resident and fellow training, launched ACGME Equity Matters (https://www.acgme.org/what-we-do/diversity-equity-and-inclusion/ACGME-Equity-Matters/), an initiative aimed to improve diversity, equity, and antiracism practices within graduate medical eduation. However, we know that education alone isn’t enough to fix this monumental problem. Traditional diversity training as we have known it has never been demonstrated to contribute to lasting changes in behavior; it takes much more extensive and complex interventions to meaningfully reduce bias.5 In the meantime, we need action. As a medical community, we need to be better about not turning the other way when we see these things happening in our classrooms and in our hospitals. As individuals, we must self-reflect on the role that we each play in contributing to or combatting injustices and seek out bystander training to empower us to speak out against acts of bias such as sexism or racism. Whether it is supporting a fellow colleague or speaking out against an inappropriate interaction, we can all do our part. A very brief list of actions and resources to support our UIM students and colleagues are listed in the Table; those interested in more in-depth resources are encouraged to explore the Association of American Medical Colleges Diversity and Inclusion Toolkit (https://www.aamc.org/professional-development/affinity-groups/cfas/diversity-inclusion-toolkit/resources).

We can’t change the culture of medicine quickly or even in our lifetime. In the meantime, those who are UIM will continue to experience these events that erode our well-being. They will continue to need support. Discussing mental health has long been stigmatized, and physicians are no exception. Many physicians are hesitant to discuss mental health issues out of fear of judgement and perceived or even real repercussions on their careers.10 However, times are changing and evolving with the current generation of medical students. It’s no secret that medicine is stressful. Most medical schools provide free counseling services, which lowers the barrier for discussions of mental health from the beginning. Making talk about mental health just as normal as talking about other aspects of health takes away the fear that “something is wrong with me” if someone seeks out counseling and mental health services. Faculty should actively check in and maintain open lines of communication, which can be invaluable for UIM students and their training experience. Creating an environment where trainees can be real and honest about the struggles they face in and out of the classroom can make everyone feel like they are not alone.
Addressing burnout in medicine is going to require an all-hands-on-deck approach. At an institutional level, there is a lot of room for improvement—improving systems for physicians so they are able to operate at their highest level (eg, addressing the burdens of prior authorizations and the electronic medical record), setting reasonable expectations around productivity, and creating work structures that respect work-life balance.11 But what can we do for ourselves? We believe that one of the most important ways to protect ourselves from burnout is to remember why. As a medical student, there is enormous pressure—pressure to learn an enormous volume of information, pass examinations, get involved in extracurricular activities, make connections, and seek research opportunities, while also cooking healthy food, grocery shopping, maintaining relationships with loved ones, and generally taking care of oneself. At times it can feel as if our lives outside of medical school are not important enough or valuable enough to make time for, but the pieces of our identity outside of medicine are what shape us into who we are today and are the roots of our purpose in medicine. Sometimes you can feel the most motivated, valued, and supported when you make time to have dinner with friends, call a family member, or simply spend time alone in the outdoors. Who you are and how you got to this point in your life are your identity. Reminding yourself of that can help when experiencing microaggressions or when that voice tries to tell you that you are not worthy. As you progress further in your career, maintaining that relationship with who you are outside of medicine can be your armor against burnout.
“Where are you really from?”
When I tell patients I am from Casper, Wyoming—wh ere I have lived the majority of my life—it’smet with disbelief. The subtext: YOU can’t be from THERE.
I didn’t used to think much of comments like this, but as I have continued to hear them, I find myself feeling tired—tired of explaining myself, tired of being treated differently than my colleagues, and tired of justifying myself. My experiences as a woman of color sadly are not uncommon in medicine.
Sara Martinez-Garcia, BA
Racial bias and racism are steeped in the culture of medicine—from the medical school admissions process1,2 to the medical training itself.3 More than half of medical students who identify as underrepresented in medicine (UIM) experience microaggressions.4 Experiencing racism and sexism in the learning environment can lead to burnout, and microaggressions promote feelings of self-doubt and isolation. Medical students who experience microaggressions are more likely to report feelings of burnout and impaired learning.4 These experiences can leave one feeling as if “You do not belong” and “You are unworthy of being in this position.”
Addressing physician burnout already is complex, and addressing burnout caused by inequity, bias, and racism is even more so. In an ideal world, we would eliminate inequity, bias, and racism in medicine through institutional and individual actions. There has been movement to do so. For example, the Accreditation Council for Graduate Medical Education (ACGME), which oversees standards for US resident and fellow training, launched ACGME Equity Matters (https://www.acgme.org/what-we-do/diversity-equity-and-inclusion/ACGME-Equity-Matters/), an initiative aimed to improve diversity, equity, and antiracism practices within graduate medical eduation. However, we know that education alone isn’t enough to fix this monumental problem. Traditional diversity training as we have known it has never been demonstrated to contribute to lasting changes in behavior; it takes much more extensive and complex interventions to meaningfully reduce bias.5 In the meantime, we need action. As a medical community, we need to be better about not turning the other way when we see these things happening in our classrooms and in our hospitals. As individuals, we must self-reflect on the role that we each play in contributing to or combatting injustices and seek out bystander training to empower us to speak out against acts of bias such as sexism or racism. Whether it is supporting a fellow colleague or speaking out against an inappropriate interaction, we can all do our part. A very brief list of actions and resources to support our UIM students and colleagues are listed in the Table; those interested in more in-depth resources are encouraged to explore the Association of American Medical Colleges Diversity and Inclusion Toolkit (https://www.aamc.org/professional-development/affinity-groups/cfas/diversity-inclusion-toolkit/resources).

We can’t change the culture of medicine quickly or even in our lifetime. In the meantime, those who are UIM will continue to experience these events that erode our well-being. They will continue to need support. Discussing mental health has long been stigmatized, and physicians are no exception. Many physicians are hesitant to discuss mental health issues out of fear of judgement and perceived or even real repercussions on their careers.10 However, times are changing and evolving with the current generation of medical students. It’s no secret that medicine is stressful. Most medical schools provide free counseling services, which lowers the barrier for discussions of mental health from the beginning. Making talk about mental health just as normal as talking about other aspects of health takes away the fear that “something is wrong with me” if someone seeks out counseling and mental health services. Faculty should actively check in and maintain open lines of communication, which can be invaluable for UIM students and their training experience. Creating an environment where trainees can be real and honest about the struggles they face in and out of the classroom can make everyone feel like they are not alone.
Addressing burnout in medicine is going to require an all-hands-on-deck approach. At an institutional level, there is a lot of room for improvement—improving systems for physicians so they are able to operate at their highest level (eg, addressing the burdens of prior authorizations and the electronic medical record), setting reasonable expectations around productivity, and creating work structures that respect work-life balance.11 But what can we do for ourselves? We believe that one of the most important ways to protect ourselves from burnout is to remember why. As a medical student, there is enormous pressure—pressure to learn an enormous volume of information, pass examinations, get involved in extracurricular activities, make connections, and seek research opportunities, while also cooking healthy food, grocery shopping, maintaining relationships with loved ones, and generally taking care of oneself. At times it can feel as if our lives outside of medical school are not important enough or valuable enough to make time for, but the pieces of our identity outside of medicine are what shape us into who we are today and are the roots of our purpose in medicine. Sometimes you can feel the most motivated, valued, and supported when you make time to have dinner with friends, call a family member, or simply spend time alone in the outdoors. Who you are and how you got to this point in your life are your identity. Reminding yourself of that can help when experiencing microaggressions or when that voice tries to tell you that you are not worthy. As you progress further in your career, maintaining that relationship with who you are outside of medicine can be your armor against burnout.
- Capers Q IV, Clinchot D, McDougle L, et al. Implicit racial bias in medical school admissions. Acad Med. 2017;92:365-369.
- Lucey CR, Saguil A. The consequences of structural racism on MCAT scores and medical school admissions: the past is prologue. Acad Med. 2020;95:351-356.
- Nguemeni Tiako MJ, South EC, Ray V. Medical schools as racialized organizations: a primer. Ann Intern Med. 2021;174:1143-1144.
- Chisholm LP, Jackson KR, Davidson HA, et al. Evaluation of racial microaggressions experienced during medical school training and the effect on medical student education and burnout: a validation study. J Natl Med Assoc. 2021;113:310-314.
- Dobbin F, Kalev A. Why doesn’t diversity training work? the challenge for industry and academia. Anthropology Now. 2018;10:48-55.
- Okoye GA. Supporting underrepresented minority women in academic dermatology. Int J Womens Dermatol. 2020;6:57-60.
- Hackworth JM, Kotagal M, Bignall ONR, et al. Microaggressions: privileged observers’ duty to act and what they can do [published online December 1, 2021]. Pediatrics. doi:10.1542/peds.2021-052758.
- Wheeler DJ, Zapata J, Davis D, et al. Twelve tips for responding to microaggressions and overt discrimination: when the patient offends the learner. Med Teach. 2019;41:1112-1117.
- Scott K. Just Work: How to Root Out Bias, Prejudice, and Bullying to Build a Kick-Ass Culture of Inclusivity. St. Martin’s Press; 2021.
- Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003;289:3161-3166.
- West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283:516-529.
- Capers Q IV, Clinchot D, McDougle L, et al. Implicit racial bias in medical school admissions. Acad Med. 2017;92:365-369.
- Lucey CR, Saguil A. The consequences of structural racism on MCAT scores and medical school admissions: the past is prologue. Acad Med. 2020;95:351-356.
- Nguemeni Tiako MJ, South EC, Ray V. Medical schools as racialized organizations: a primer. Ann Intern Med. 2021;174:1143-1144.
- Chisholm LP, Jackson KR, Davidson HA, et al. Evaluation of racial microaggressions experienced during medical school training and the effect on medical student education and burnout: a validation study. J Natl Med Assoc. 2021;113:310-314.
- Dobbin F, Kalev A. Why doesn’t diversity training work? the challenge for industry and academia. Anthropology Now. 2018;10:48-55.
- Okoye GA. Supporting underrepresented minority women in academic dermatology. Int J Womens Dermatol. 2020;6:57-60.
- Hackworth JM, Kotagal M, Bignall ONR, et al. Microaggressions: privileged observers’ duty to act and what they can do [published online December 1, 2021]. Pediatrics. doi:10.1542/peds.2021-052758.
- Wheeler DJ, Zapata J, Davis D, et al. Twelve tips for responding to microaggressions and overt discrimination: when the patient offends the learner. Med Teach. 2019;41:1112-1117.
- Scott K. Just Work: How to Root Out Bias, Prejudice, and Bullying to Build a Kick-Ass Culture of Inclusivity. St. Martin’s Press; 2021.
- Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003;289:3161-3166.
- West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283:516-529.
Bridging the Digital Divide in Teledermatology Usage: A Retrospective Review of Patient Visits
Teledermatology is an effective patient care model for the delivery of high-quality dermatologic care.1 Teledermatology can occur using synchronous, asynchronous, and hybrid models of care. In asynchronous visits (AVs), patients or health professionals submit photographs and information for dermatologists to review and provide treatment recommendations. With synchronous visits (SVs), patients have a visit with a dermatology health professional in real time via live video conferencing software. Hybrid models incorporate asynchronous strategies for patient intake forms and skin photograph submissions as well as synchronous methods for live video consultation in a single visit.1 However, remarkable inequities in internet access limit telemedicine usage among medically marginalized patient populations, including racialized, elderly, and low socioeconomic status groups.2
Synchronous visits, a relatively newer teledermatology format, allow for communication with dermatology professionals from the convenience of a patient’s selected location. The live interaction of SVs allows dermatology professionals to answer questions, provide treatment recommendations, and build therapeutic relationships with patients. Concerns for dermatologist reimbursement, malpractice/liability, and technological challenges stalled large-scale uptake of teledermatology platforms.3 The COVID-19 pandemic led to a drastic increase in teledermatology usage of approximately 587.2%, largely due to public safety measures and Medicaid reimbursement parity between SV and in-office visits (IVs).3,4
With the implementation of SVs as a patient care model, we investigated the demographics of patients who utilized SVs, AVs, or IVs, and we propose strategies to promote equity in dermatologic care access.
Methods
This study was approved by the University of Pittsburgh institutional review board (STUDY20110043). We performed a retrospective electronic medical record review of deidentified data from the University of Pittsburgh Medical Center, a tertiary care center in Allegheny County, Pennsylvania, with an established asynchronous teledermatology program. Hybrid SVs were integrated into the University of Pittsburgh Medical Center patient care visit options in March 2020. Patients were instructed to upload photographs of their skin conditions prior to SV appointments. The study included visits occurring between July and December 2020. Visit types included SVs, AVs, and IVs.
We analyzed the initial dermatology visits of 17,130 patients aged 17.5 years and older. Recorded data included diagnosis, age, sex, race, ethnicity, and insurance type for each visit type. Patients without a reported race (990 patients) or ethnicity (1712 patients) were excluded from analysis of race/ethnicity data. Patient zip codes were compared with the zip codes of Allegheny County municipalities as reported by the Allegheny County Elections Division.
Statistical Analysis—Descriptive statistics were calculated; frequency with percentage was used to report categorical variables, and the mean (SD) was used for normally distributed continuous variables. Univariate analysis was performed using the χ2 test for categorical variables. One-way analysis of variance was used to compare age among visit types. Statistical significance was defined as P<.05. IBM SPSS Statistics for Windows, Version 24 (IBM Corp) was used for all statistical analyses.
Results
In our study population, 81.2% (13,916) of patients were residents of Allegheny County, where 51.6% of residents are female and 81.4% are older than 18 years according to data from 2020.5 The racial and ethnic demographics of Allegheny County were 13.4% African American/Black, 0.2% American Indian/Alaska Native, 4.2% Asian, 2.3% Hispanic/Latino, and 79.6% White. The percentage of residents who identified as Native Hawaiian/Pacific Islander was reported to be greater than 0% but less than 0.5%.5
In our analysis, IVs were the most utilized visit type, accounting for 71.5% (12,240) of visits, followed by 15.0% (2577) for SVs and 13.5% (2313) for AVs. The mean age (SD) of IV patients was 51.0 (18.8) years compared with 39.9 (16.9) years for SV patients and 37.5 (14.3) years for AV patients (eTable). The majority of patients for all visits were female: 62.1% (7599) for IVs, 71.4% (1652) for AVs, and 72.8% (1877) for SVs. The largest racial or ethnic group for all visit types included White patients (83.8% [13,524] of all patients), followed by Black (12.4% [2007]), Hispanic/Latino (1.4% [209]), Asian (3.4% [555]), American Indian/Alaska Native (0.2% [35]), and Native Hawaiian/Other Pacific Islander patients (0.1% [19]).
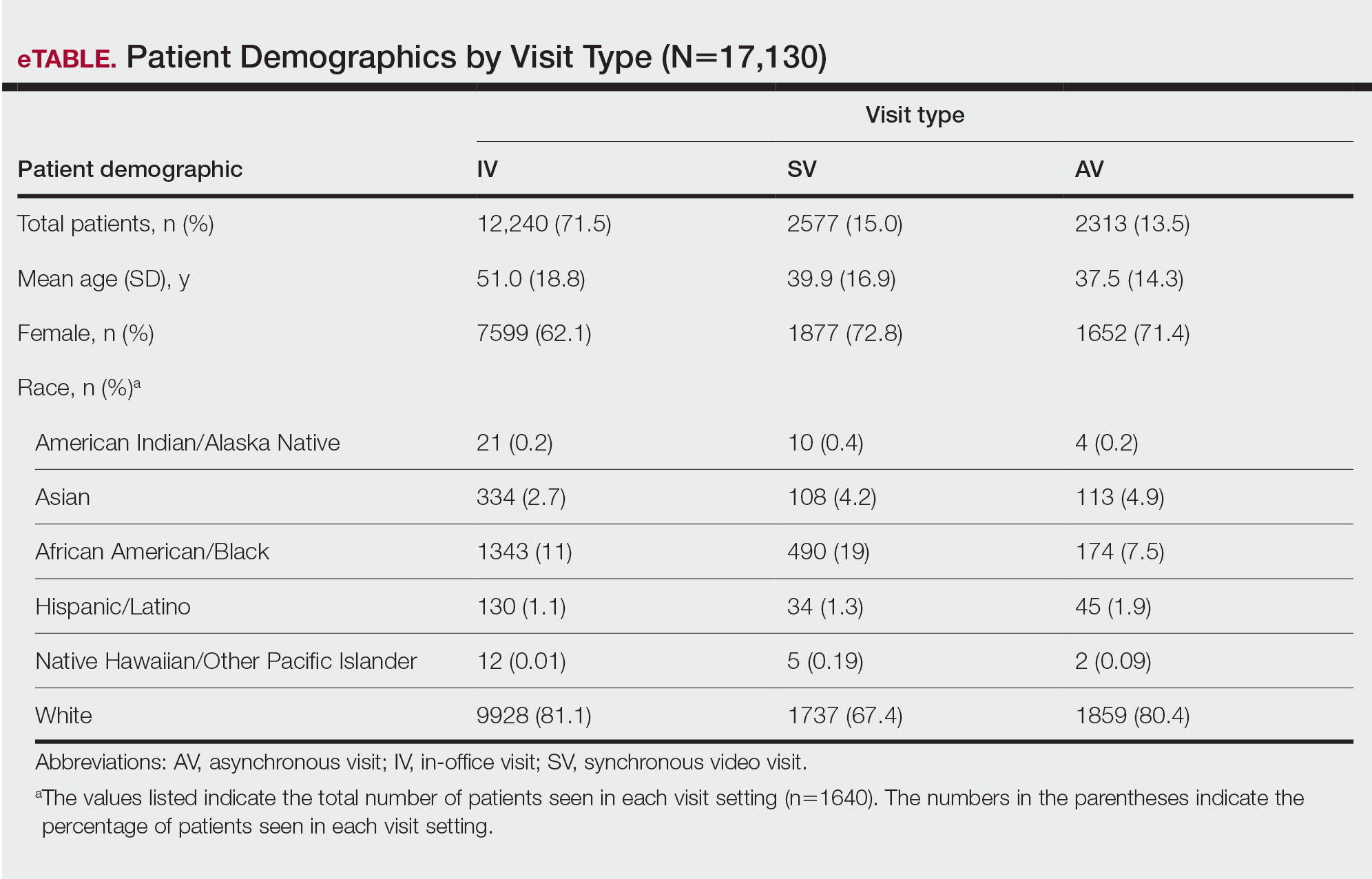
Asian patients, who comprised 4.2% of Allegheny County residents,5 accounted for 2.7% (334) of IVs, 4.9% (113) of AVs, and 4.2% (108) of SVs. Black patients, who were reported as 13.4% of the Allegheny County population,5 were more likely to utilize SVs (19% [490])compared with AVs (7.5% [174]) and IVs (11% [1343]). Hispanic/Latino patients had a disproportionally lower utilization of dermatologic care in all settings, comprising 1.4% (209) of all patients in our study compared with 2.3% of Allegheny County residents.5 White patients, who comprised 79.6% of Allegheny County residents, accounted for 81.1% (9928) of IVs, 67.4% (1737) of SVs, and 80.4% (1859) of AVs. There was no significant difference in the percentage of American Indian/Alaska Native and Native Hawaiian/Other Pacific Islander patients among visit types.
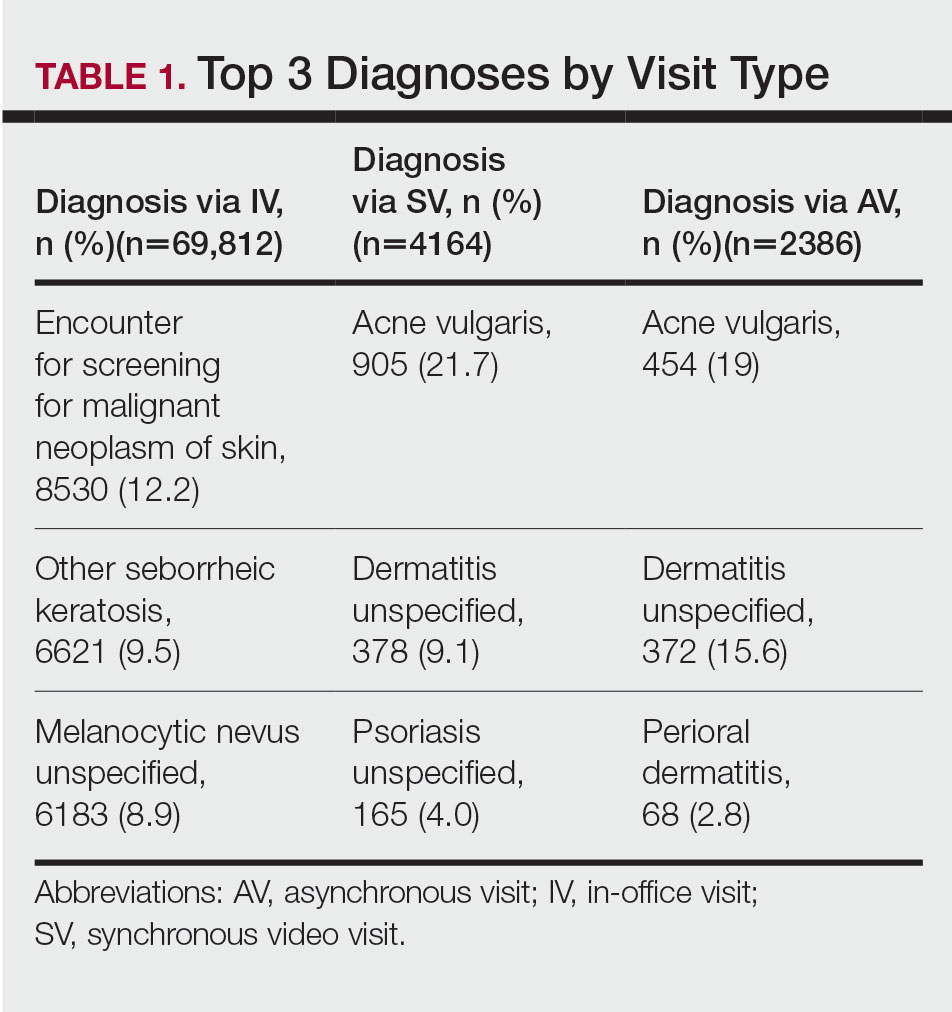
The 3 most common diagnoses for IVs were skin cancer screening, seborrheic keratosis, and melanocytic nevus (Table 1). Skin cancer screening was the most common diagnosis, accounting for 12.2% (8530) of 69,812 IVs. The 3 most common diagnoses for SVs were acne vulgaris, dermatitis, and psoriasis. The 3 most common diagnoses for AVs were acne vulgaris, dermatitis, and perioral dermatitis.
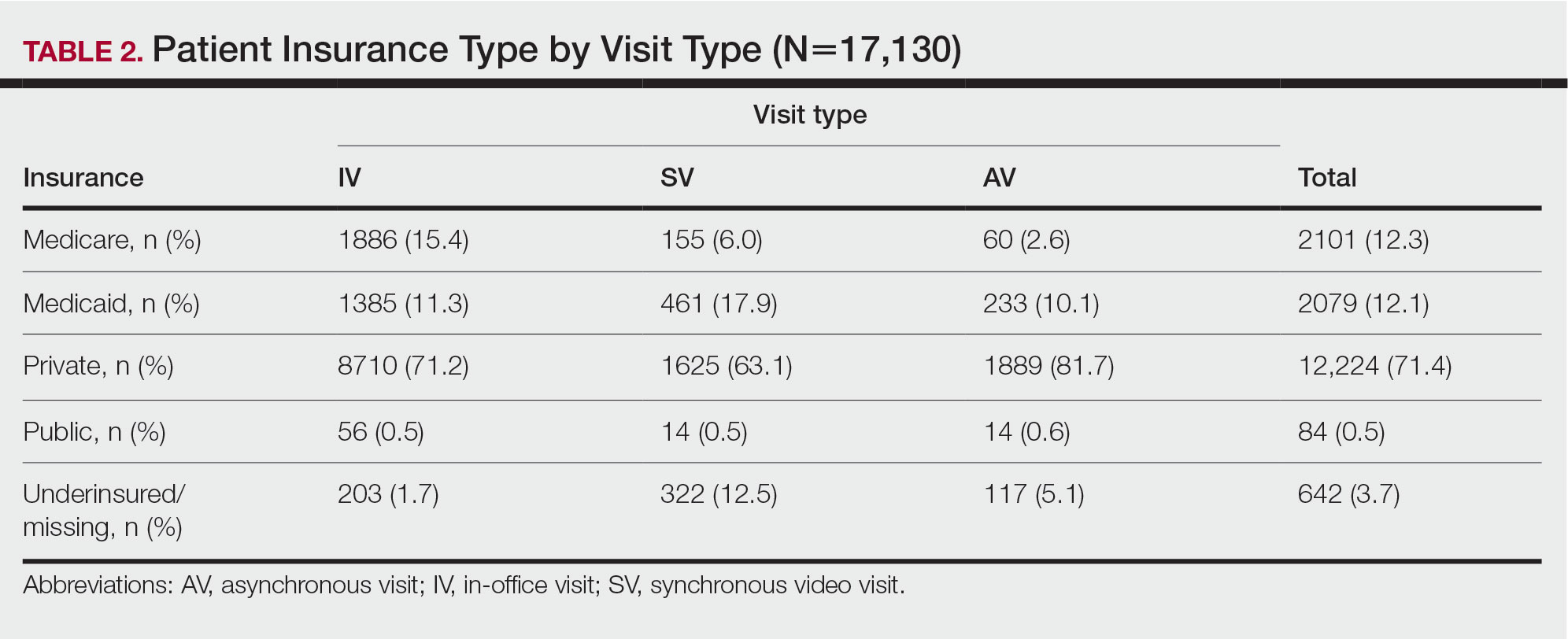
Private insurance was the most common insurance type among all patients (71.4% [12,224])(Table 2). A higher percentage of patients with Medicaid insurance (17.9% [461]) utilized SVs compared with AVs (10.1% [233]) and IVs (11.3% 1385]). Similarly, a higher percentage of patients with no insurance or no insurance listed were seen via SVs (12.5% [322]) compared with AVs (5.1% [117]) and IVs (1.7% [203]). Patients with Medicare insurance used IVs (15.4% [1886]) more than SVs (6.0% [155]) or AVs (2.6% [60]). There was no significant difference among visit type usage for patients with public insurance.
Comment
Teledermatology Benefits—In this retrospective review of medical records of patients who obtained dermatologic care after the implementation of SVs at our institution, we found a proportionally higher use of SVs among Black patients, patients with Medicaid, and patients who are underinsured. Benefits of teledermatology include decreases in patient transportation and associated costs, time away from work or home, and need for childcare.6 The SV format provides the additional advantage of direct live interaction and the development of a patient-physician or patient–physician assistant relationship. Although the prerequisite technology, internet, and broadband connectivity preclude use of teledermatology for many vulnerable patients,2 its convenience ultimately may reduce inequities in access.
Disparities in Dermatologic Care—Hispanic ethnicity and male sex are among described patient demographics associated with decreased rates of outpatient dermatologic care.7 We reported disparities in dermatologic care utilization across all visit types among Hispanic patients and males. Patients identifying as Hispanic/Latino composed only 1.4% (n=209) of our study population compared with 2.3% of Allegheny County residents.5 During our study period, most patients seen were female, accounting for 62.1% to 72.8% of visits, compared with 51.6% of Allegheny County residents.5 These disparities in dermatologic care use may have implications for increased skin-associated morbidity and provide impetus for dermatologists to increase engagement with these patient groups.
Characteristics of Patients Using Teledermatology—Patients using SVs and AVs were significantly younger (mean age [SD], 39.9 [16.9] years and 37.5 [14.3] years, respectively) compared with those using IVs (51.0 [18.8] years). This finding reflects known digital knowledge barriers among older patients.8,9 The synchronous communication format of SVs simulates the traditional visit style of IVs, which may be preferable for some patients. Continued patient education and advocacy for broadband access may increase teledermatology use among older patients and patients with limited technology resources.8
Teledermatology visits were used most frequently for acne and dermatitis, while IVs were used for skin cancer screenings and examination of concerning lesions. This usage pattern is consistent with a previously described consensus among dermatologists on the conditions most amenable to teledermatology evaluation.3
Medicaid reimbursement parity for SVs is in effect nationally until the end of the COVID-19 public health emergency declaration in the United States.10 As of February 2023, the public health emergency declaration has been renewed 12 times since January 2020, with the most recent renewal on January 11, 2023.11 As of January 2023, 21 states have enacted legislation providing permanent reimbursement parity for SV services. Six additional states have some payment parity in place, each with its own qualifying criteria, and 23 states have no payment parity.12 Only 25 Medicaid programs currently provide reimbursement for AV services.13
Study Limitations—Our study was limited by lack of data on patients who are multiracial and those who identify as nonbinary and transgender. Because of the low numbers of Hispanic patients associated with each race category and a high number of patients who did not report an ethnicity or race, race and ethnicity data were analyzed separately. For SVs, patients were instructed to upload photographs prior to their visit; however, the percentage of patients who uploaded photographs was not analyzed.
Conclusion
Expansion of teledermatology services, including SVs and AVs, patient outreach and education, advocacy for broadband access, and Medicaid payment parity, may improve dermatologic care access for medically marginalized groups. Teledermatology has the potential to serve as an effective health care option for patients who are racially minoritized, older, and underinsured. To further assess the effectiveness of teledermatology, we plan to analyze the number of SVs and AVs that were referred to IVs. Future studies also will investigate the impact of implementing patient education and patient-reported outcomes of teledermatology visits.
- Lee JJ, English JC. Teledermatology: a review and update. Am J Clin Dermatol. 2018;19:253-260.
- Bakhtiar M, Elbuluk N, Lipoff JB. The digital divide: how COVID-19’s telemedicine expansion could exacerbate disparities. J Am Acad Dermatol. 2020;83:E345-E346.
- Kennedy J, Arey S, Hopkins Z, et al. dermatologist perceptions of teledermatology implementation and future use after COVID-19: demographics, barriers, and insights. JAMA Dermatol. 2021;157:595-597.
- Centers for Disease Control and Prevention. Using telehealth to expand access to essential health services during the COVID-19 pandemic. Updated June 10, 2020. Accessed February 10, 2023. https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html
- United States Census Bureau. QuickFacts: Allegheny County, Pennsylvania. Accessed August 12, 2021. https://www.census.gov/quickfacts/alleghenycountypennsylvania
- Moore HW. Teledermatology—access to specialized care via a different model. Dermatology Advisor. November 12, 2019. Accessed February 10, 2023. https://www.dermatologyadvisor.com/home/topics/practice-management/teledermatology-access-to-specialized-care-via-a-different-model/
- Tripathi R, Knusel KD, Ezaldein HH, et al. Association of demographic and socioeconomic characteristics with differences in use of outpatient dermatology services in the United States. JAMA Dermatol. 2018;154:1286-1291.
- Nouri S, Khoong EC, Lyles CR, et al. Addressing equity in telemedicine for chronic disease management during the COVID-19 pandemic [published online May 4, 2020]. NEJM Catal Innov Care Deliv. doi:10.1056/CAT.20.0123
- Swenson K, Ghertner R. People in low-income households have less access to internet services—2019 update. Office of the Assistant Secretary for Planning and Evaluation; US Department of Health and Human Services. March 2021. Accessed February 10, 2023. https://aspe.hhs.gov/sites/default/files/private/pdf/263601/internet-access-among-low-income-2019.pdf
- Centers for Medicare and Medicaid Services. COVID-19 frequently asked questions (FAQs) on Medicare fee-for-service (FFS) billing. Updated August 16, 2022. Accessed February 10, 2023. https://www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf
- US Department of Health and Human Services. Renewal of determination that a public health emergency exists. Updated February 9, 2023. Accessed February 20, 2023. https://aspr.hhs.gov/legal/PHE/Pages/COVID19-9Feb2023.aspx?
- Augenstein J, Smith JM. Executive summary: tracking telehealth changes state-by-state in response to COVID-19. Updated January 27, 2023. Accessed February 10, 2023. https://www.manatt.com/insights/newsletters/covid-19-update/executive-summary-tracking-telehealth-changes-stat
- Center for Connected Health Policy. Policy trend maps: store and forward Medicaid reimbursement. Accessed June 23, 2022. https://www.cchpca.org/policy-trends/
Teledermatology is an effective patient care model for the delivery of high-quality dermatologic care.1 Teledermatology can occur using synchronous, asynchronous, and hybrid models of care. In asynchronous visits (AVs), patients or health professionals submit photographs and information for dermatologists to review and provide treatment recommendations. With synchronous visits (SVs), patients have a visit with a dermatology health professional in real time via live video conferencing software. Hybrid models incorporate asynchronous strategies for patient intake forms and skin photograph submissions as well as synchronous methods for live video consultation in a single visit.1 However, remarkable inequities in internet access limit telemedicine usage among medically marginalized patient populations, including racialized, elderly, and low socioeconomic status groups.2
Synchronous visits, a relatively newer teledermatology format, allow for communication with dermatology professionals from the convenience of a patient’s selected location. The live interaction of SVs allows dermatology professionals to answer questions, provide treatment recommendations, and build therapeutic relationships with patients. Concerns for dermatologist reimbursement, malpractice/liability, and technological challenges stalled large-scale uptake of teledermatology platforms.3 The COVID-19 pandemic led to a drastic increase in teledermatology usage of approximately 587.2%, largely due to public safety measures and Medicaid reimbursement parity between SV and in-office visits (IVs).3,4
With the implementation of SVs as a patient care model, we investigated the demographics of patients who utilized SVs, AVs, or IVs, and we propose strategies to promote equity in dermatologic care access.
Methods
This study was approved by the University of Pittsburgh institutional review board (STUDY20110043). We performed a retrospective electronic medical record review of deidentified data from the University of Pittsburgh Medical Center, a tertiary care center in Allegheny County, Pennsylvania, with an established asynchronous teledermatology program. Hybrid SVs were integrated into the University of Pittsburgh Medical Center patient care visit options in March 2020. Patients were instructed to upload photographs of their skin conditions prior to SV appointments. The study included visits occurring between July and December 2020. Visit types included SVs, AVs, and IVs.
We analyzed the initial dermatology visits of 17,130 patients aged 17.5 years and older. Recorded data included diagnosis, age, sex, race, ethnicity, and insurance type for each visit type. Patients without a reported race (990 patients) or ethnicity (1712 patients) were excluded from analysis of race/ethnicity data. Patient zip codes were compared with the zip codes of Allegheny County municipalities as reported by the Allegheny County Elections Division.
Statistical Analysis—Descriptive statistics were calculated; frequency with percentage was used to report categorical variables, and the mean (SD) was used for normally distributed continuous variables. Univariate analysis was performed using the χ2 test for categorical variables. One-way analysis of variance was used to compare age among visit types. Statistical significance was defined as P<.05. IBM SPSS Statistics for Windows, Version 24 (IBM Corp) was used for all statistical analyses.
Results
In our study population, 81.2% (13,916) of patients were residents of Allegheny County, where 51.6% of residents are female and 81.4% are older than 18 years according to data from 2020.5 The racial and ethnic demographics of Allegheny County were 13.4% African American/Black, 0.2% American Indian/Alaska Native, 4.2% Asian, 2.3% Hispanic/Latino, and 79.6% White. The percentage of residents who identified as Native Hawaiian/Pacific Islander was reported to be greater than 0% but less than 0.5%.5
In our analysis, IVs were the most utilized visit type, accounting for 71.5% (12,240) of visits, followed by 15.0% (2577) for SVs and 13.5% (2313) for AVs. The mean age (SD) of IV patients was 51.0 (18.8) years compared with 39.9 (16.9) years for SV patients and 37.5 (14.3) years for AV patients (eTable). The majority of patients for all visits were female: 62.1% (7599) for IVs, 71.4% (1652) for AVs, and 72.8% (1877) for SVs. The largest racial or ethnic group for all visit types included White patients (83.8% [13,524] of all patients), followed by Black (12.4% [2007]), Hispanic/Latino (1.4% [209]), Asian (3.4% [555]), American Indian/Alaska Native (0.2% [35]), and Native Hawaiian/Other Pacific Islander patients (0.1% [19]).
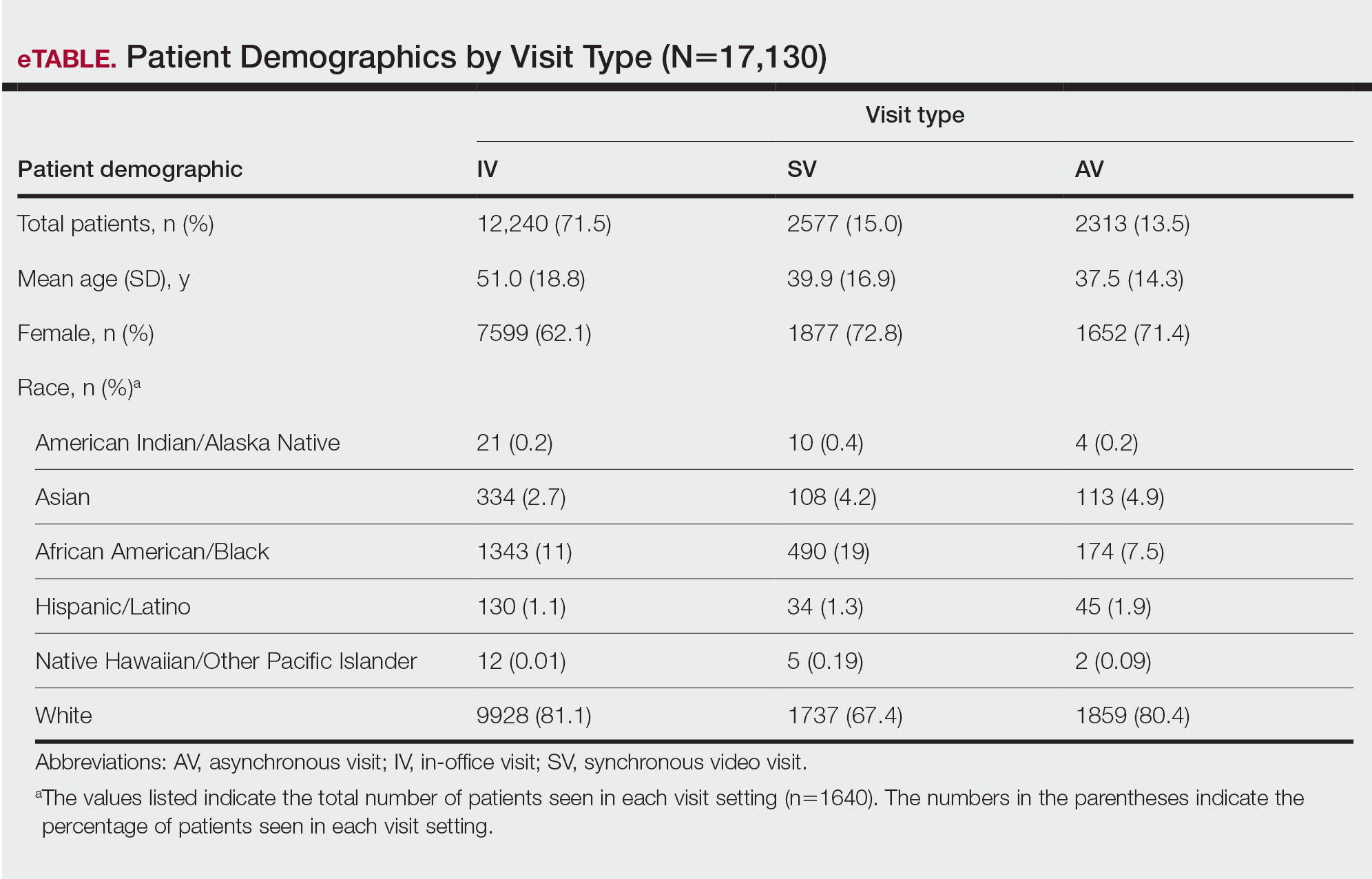
Asian patients, who comprised 4.2% of Allegheny County residents,5 accounted for 2.7% (334) of IVs, 4.9% (113) of AVs, and 4.2% (108) of SVs. Black patients, who were reported as 13.4% of the Allegheny County population,5 were more likely to utilize SVs (19% [490])compared with AVs (7.5% [174]) and IVs (11% [1343]). Hispanic/Latino patients had a disproportionally lower utilization of dermatologic care in all settings, comprising 1.4% (209) of all patients in our study compared with 2.3% of Allegheny County residents.5 White patients, who comprised 79.6% of Allegheny County residents, accounted for 81.1% (9928) of IVs, 67.4% (1737) of SVs, and 80.4% (1859) of AVs. There was no significant difference in the percentage of American Indian/Alaska Native and Native Hawaiian/Other Pacific Islander patients among visit types.
The 3 most common diagnoses for IVs were skin cancer screening, seborrheic keratosis, and melanocytic nevus (Table 1). Skin cancer screening was the most common diagnosis, accounting for 12.2% (8530) of 69,812 IVs. The 3 most common diagnoses for SVs were acne vulgaris, dermatitis, and psoriasis. The 3 most common diagnoses for AVs were acne vulgaris, dermatitis, and perioral dermatitis.
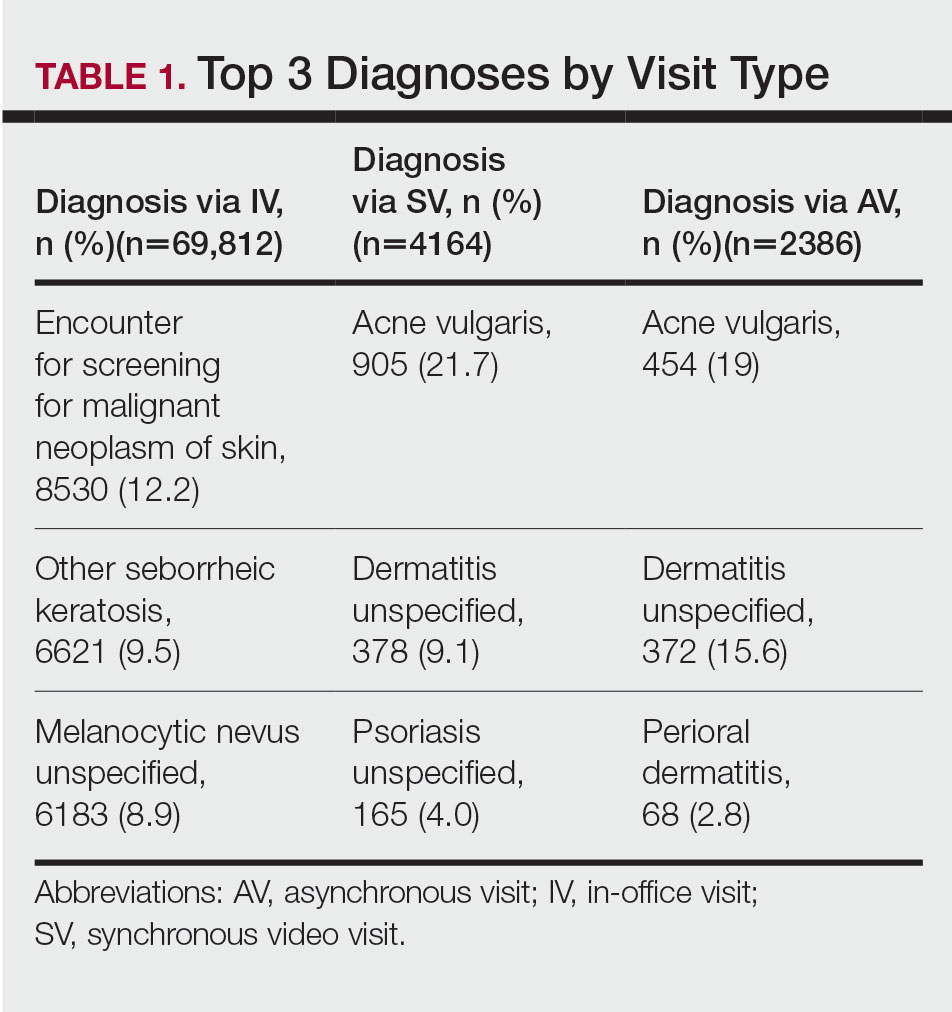
Private insurance was the most common insurance type among all patients (71.4% [12,224])(Table 2). A higher percentage of patients with Medicaid insurance (17.9% [461]) utilized SVs compared with AVs (10.1% [233]) and IVs (11.3% 1385]). Similarly, a higher percentage of patients with no insurance or no insurance listed were seen via SVs (12.5% [322]) compared with AVs (5.1% [117]) and IVs (1.7% [203]). Patients with Medicare insurance used IVs (15.4% [1886]) more than SVs (6.0% [155]) or AVs (2.6% [60]). There was no significant difference among visit type usage for patients with public insurance.
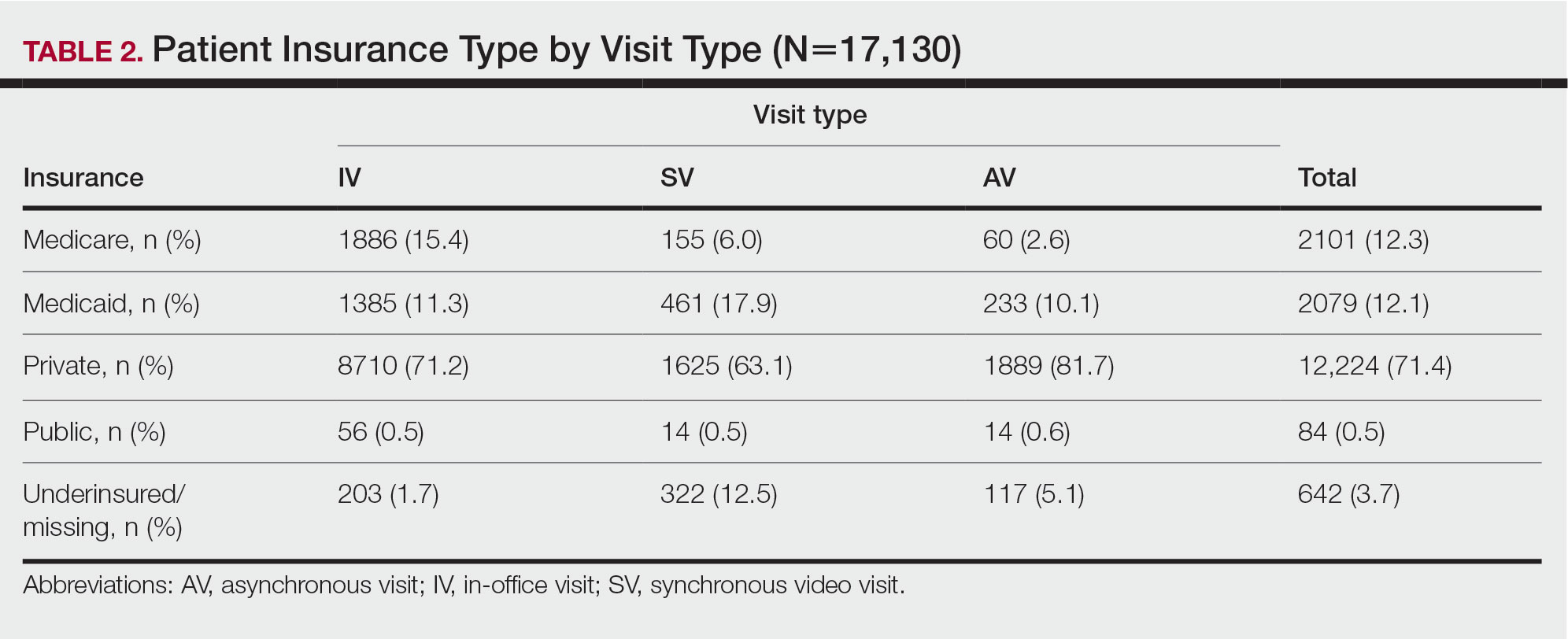
Comment
Teledermatology Benefits—In this retrospective review of medical records of patients who obtained dermatologic care after the implementation of SVs at our institution, we found a proportionally higher use of SVs among Black patients, patients with Medicaid, and patients who are underinsured. Benefits of teledermatology include decreases in patient transportation and associated costs, time away from work or home, and need for childcare.6 The SV format provides the additional advantage of direct live interaction and the development of a patient-physician or patient–physician assistant relationship. Although the prerequisite technology, internet, and broadband connectivity preclude use of teledermatology for many vulnerable patients,2 its convenience ultimately may reduce inequities in access.
Disparities in Dermatologic Care—Hispanic ethnicity and male sex are among described patient demographics associated with decreased rates of outpatient dermatologic care.7 We reported disparities in dermatologic care utilization across all visit types among Hispanic patients and males. Patients identifying as Hispanic/Latino composed only 1.4% (n=209) of our study population compared with 2.3% of Allegheny County residents.5 During our study period, most patients seen were female, accounting for 62.1% to 72.8% of visits, compared with 51.6% of Allegheny County residents.5 These disparities in dermatologic care use may have implications for increased skin-associated morbidity and provide impetus for dermatologists to increase engagement with these patient groups.
Characteristics of Patients Using Teledermatology—Patients using SVs and AVs were significantly younger (mean age [SD], 39.9 [16.9] years and 37.5 [14.3] years, respectively) compared with those using IVs (51.0 [18.8] years). This finding reflects known digital knowledge barriers among older patients.8,9 The synchronous communication format of SVs simulates the traditional visit style of IVs, which may be preferable for some patients. Continued patient education and advocacy for broadband access may increase teledermatology use among older patients and patients with limited technology resources.8
Teledermatology visits were used most frequently for acne and dermatitis, while IVs were used for skin cancer screenings and examination of concerning lesions. This usage pattern is consistent with a previously described consensus among dermatologists on the conditions most amenable to teledermatology evaluation.3
Medicaid reimbursement parity for SVs is in effect nationally until the end of the COVID-19 public health emergency declaration in the United States.10 As of February 2023, the public health emergency declaration has been renewed 12 times since January 2020, with the most recent renewal on January 11, 2023.11 As of January 2023, 21 states have enacted legislation providing permanent reimbursement parity for SV services. Six additional states have some payment parity in place, each with its own qualifying criteria, and 23 states have no payment parity.12 Only 25 Medicaid programs currently provide reimbursement for AV services.13
Study Limitations—Our study was limited by lack of data on patients who are multiracial and those who identify as nonbinary and transgender. Because of the low numbers of Hispanic patients associated with each race category and a high number of patients who did not report an ethnicity or race, race and ethnicity data were analyzed separately. For SVs, patients were instructed to upload photographs prior to their visit; however, the percentage of patients who uploaded photographs was not analyzed.
Conclusion
Expansion of teledermatology services, including SVs and AVs, patient outreach and education, advocacy for broadband access, and Medicaid payment parity, may improve dermatologic care access for medically marginalized groups. Teledermatology has the potential to serve as an effective health care option for patients who are racially minoritized, older, and underinsured. To further assess the effectiveness of teledermatology, we plan to analyze the number of SVs and AVs that were referred to IVs. Future studies also will investigate the impact of implementing patient education and patient-reported outcomes of teledermatology visits.
Teledermatology is an effective patient care model for the delivery of high-quality dermatologic care.1 Teledermatology can occur using synchronous, asynchronous, and hybrid models of care. In asynchronous visits (AVs), patients or health professionals submit photographs and information for dermatologists to review and provide treatment recommendations. With synchronous visits (SVs), patients have a visit with a dermatology health professional in real time via live video conferencing software. Hybrid models incorporate asynchronous strategies for patient intake forms and skin photograph submissions as well as synchronous methods for live video consultation in a single visit.1 However, remarkable inequities in internet access limit telemedicine usage among medically marginalized patient populations, including racialized, elderly, and low socioeconomic status groups.2
Synchronous visits, a relatively newer teledermatology format, allow for communication with dermatology professionals from the convenience of a patient’s selected location. The live interaction of SVs allows dermatology professionals to answer questions, provide treatment recommendations, and build therapeutic relationships with patients. Concerns for dermatologist reimbursement, malpractice/liability, and technological challenges stalled large-scale uptake of teledermatology platforms.3 The COVID-19 pandemic led to a drastic increase in teledermatology usage of approximately 587.2%, largely due to public safety measures and Medicaid reimbursement parity between SV and in-office visits (IVs).3,4
With the implementation of SVs as a patient care model, we investigated the demographics of patients who utilized SVs, AVs, or IVs, and we propose strategies to promote equity in dermatologic care access.
Methods
This study was approved by the University of Pittsburgh institutional review board (STUDY20110043). We performed a retrospective electronic medical record review of deidentified data from the University of Pittsburgh Medical Center, a tertiary care center in Allegheny County, Pennsylvania, with an established asynchronous teledermatology program. Hybrid SVs were integrated into the University of Pittsburgh Medical Center patient care visit options in March 2020. Patients were instructed to upload photographs of their skin conditions prior to SV appointments. The study included visits occurring between July and December 2020. Visit types included SVs, AVs, and IVs.
We analyzed the initial dermatology visits of 17,130 patients aged 17.5 years and older. Recorded data included diagnosis, age, sex, race, ethnicity, and insurance type for each visit type. Patients without a reported race (990 patients) or ethnicity (1712 patients) were excluded from analysis of race/ethnicity data. Patient zip codes were compared with the zip codes of Allegheny County municipalities as reported by the Allegheny County Elections Division.
Statistical Analysis—Descriptive statistics were calculated; frequency with percentage was used to report categorical variables, and the mean (SD) was used for normally distributed continuous variables. Univariate analysis was performed using the χ2 test for categorical variables. One-way analysis of variance was used to compare age among visit types. Statistical significance was defined as P<.05. IBM SPSS Statistics for Windows, Version 24 (IBM Corp) was used for all statistical analyses.
Results
In our study population, 81.2% (13,916) of patients were residents of Allegheny County, where 51.6% of residents are female and 81.4% are older than 18 years according to data from 2020.5 The racial and ethnic demographics of Allegheny County were 13.4% African American/Black, 0.2% American Indian/Alaska Native, 4.2% Asian, 2.3% Hispanic/Latino, and 79.6% White. The percentage of residents who identified as Native Hawaiian/Pacific Islander was reported to be greater than 0% but less than 0.5%.5
In our analysis, IVs were the most utilized visit type, accounting for 71.5% (12,240) of visits, followed by 15.0% (2577) for SVs and 13.5% (2313) for AVs. The mean age (SD) of IV patients was 51.0 (18.8) years compared with 39.9 (16.9) years for SV patients and 37.5 (14.3) years for AV patients (eTable). The majority of patients for all visits were female: 62.1% (7599) for IVs, 71.4% (1652) for AVs, and 72.8% (1877) for SVs. The largest racial or ethnic group for all visit types included White patients (83.8% [13,524] of all patients), followed by Black (12.4% [2007]), Hispanic/Latino (1.4% [209]), Asian (3.4% [555]), American Indian/Alaska Native (0.2% [35]), and Native Hawaiian/Other Pacific Islander patients (0.1% [19]).
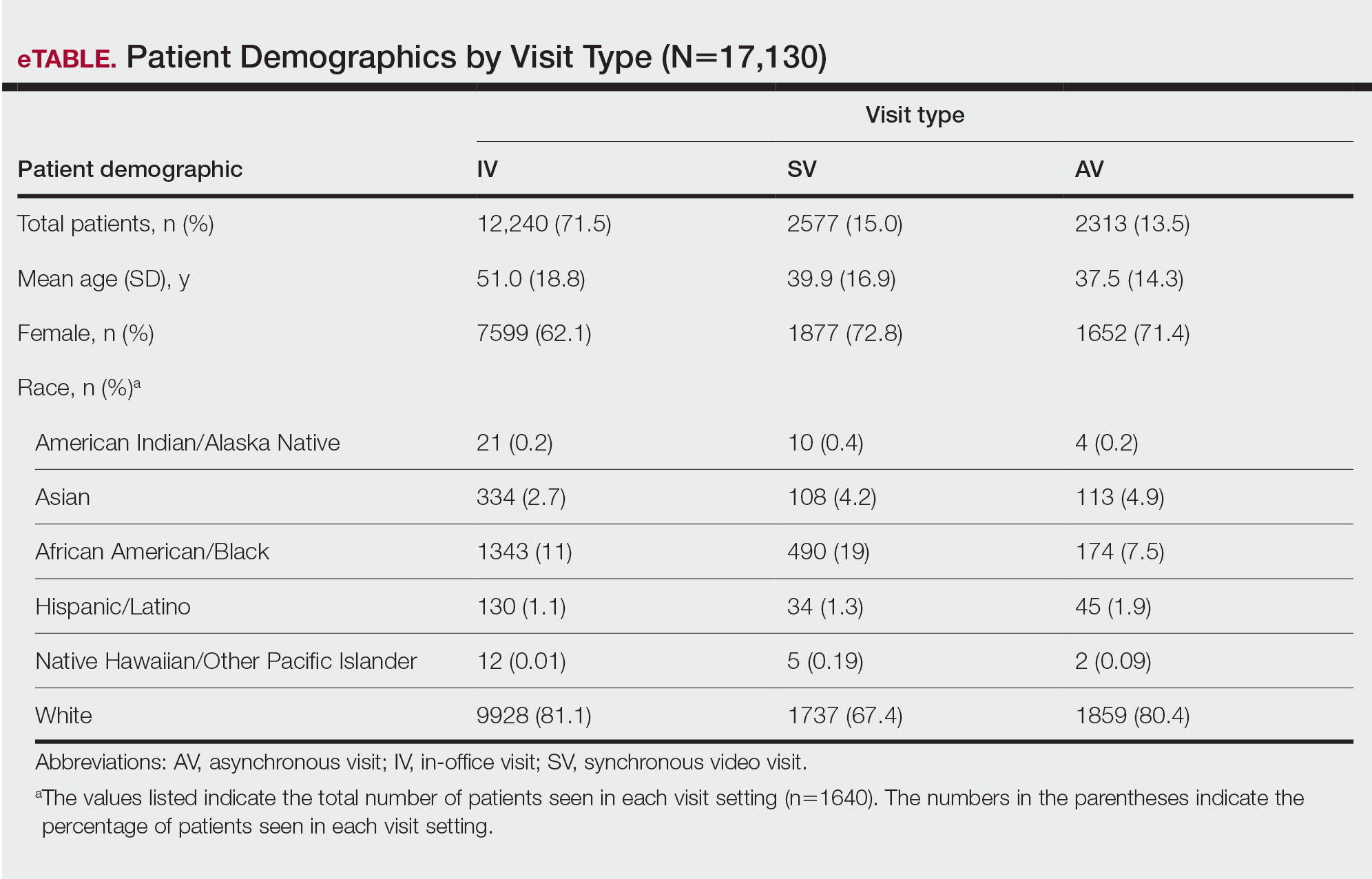
Asian patients, who comprised 4.2% of Allegheny County residents,5 accounted for 2.7% (334) of IVs, 4.9% (113) of AVs, and 4.2% (108) of SVs. Black patients, who were reported as 13.4% of the Allegheny County population,5 were more likely to utilize SVs (19% [490])compared with AVs (7.5% [174]) and IVs (11% [1343]). Hispanic/Latino patients had a disproportionally lower utilization of dermatologic care in all settings, comprising 1.4% (209) of all patients in our study compared with 2.3% of Allegheny County residents.5 White patients, who comprised 79.6% of Allegheny County residents, accounted for 81.1% (9928) of IVs, 67.4% (1737) of SVs, and 80.4% (1859) of AVs. There was no significant difference in the percentage of American Indian/Alaska Native and Native Hawaiian/Other Pacific Islander patients among visit types.
The 3 most common diagnoses for IVs were skin cancer screening, seborrheic keratosis, and melanocytic nevus (Table 1). Skin cancer screening was the most common diagnosis, accounting for 12.2% (8530) of 69,812 IVs. The 3 most common diagnoses for SVs were acne vulgaris, dermatitis, and psoriasis. The 3 most common diagnoses for AVs were acne vulgaris, dermatitis, and perioral dermatitis.
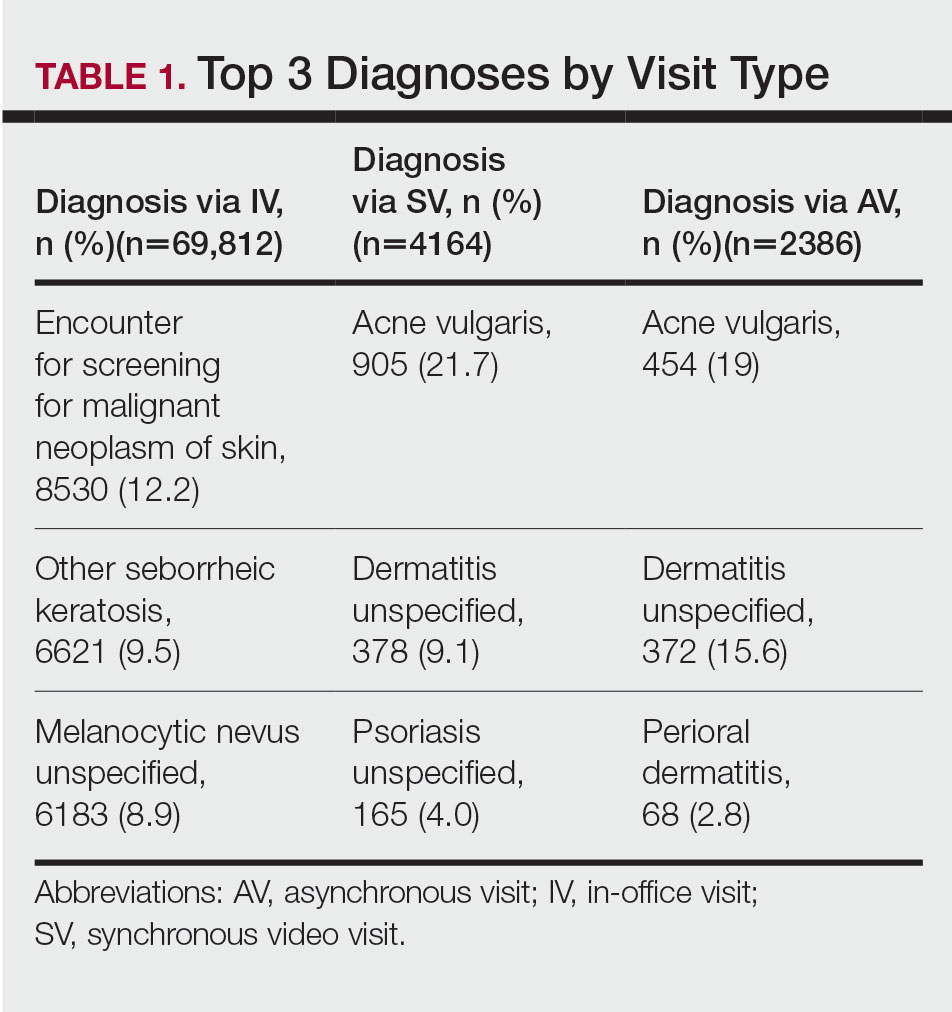
Private insurance was the most common insurance type among all patients (71.4% [12,224])(Table 2). A higher percentage of patients with Medicaid insurance (17.9% [461]) utilized SVs compared with AVs (10.1% [233]) and IVs (11.3% 1385]). Similarly, a higher percentage of patients with no insurance or no insurance listed were seen via SVs (12.5% [322]) compared with AVs (5.1% [117]) and IVs (1.7% [203]). Patients with Medicare insurance used IVs (15.4% [1886]) more than SVs (6.0% [155]) or AVs (2.6% [60]). There was no significant difference among visit type usage for patients with public insurance.
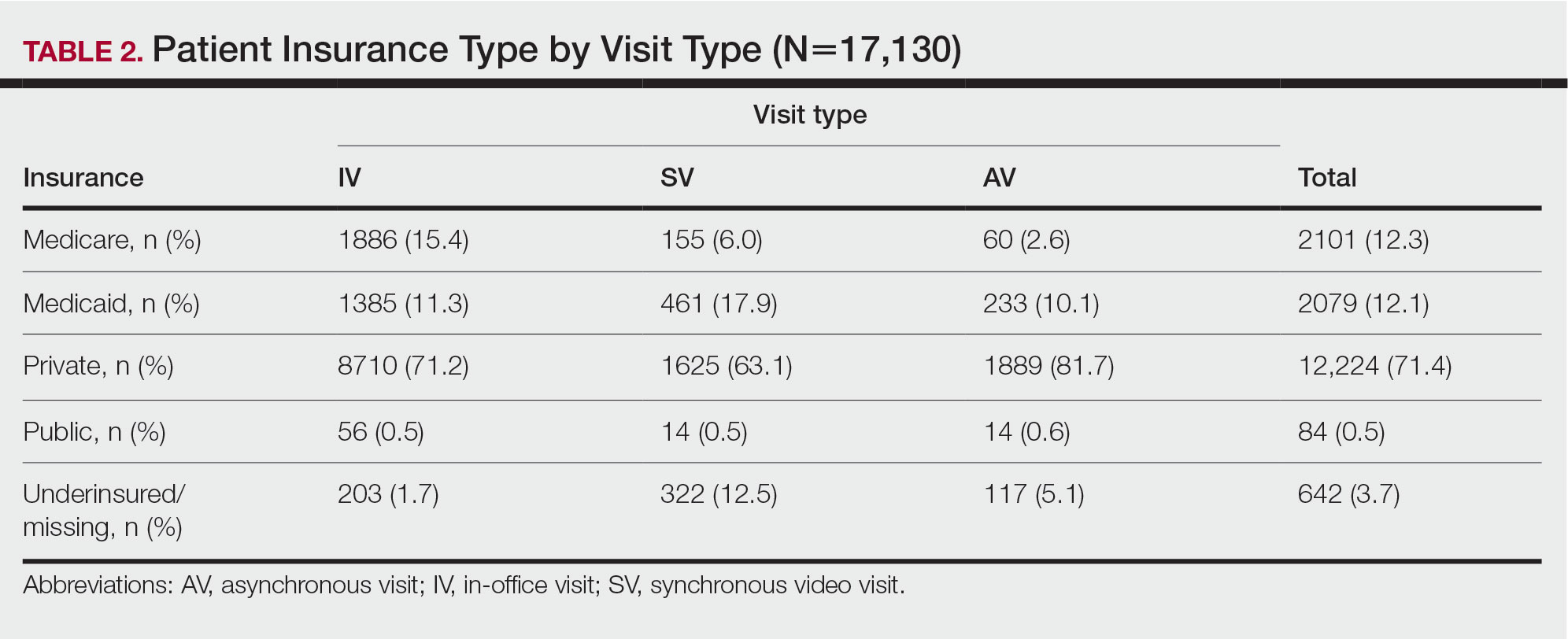
Comment
Teledermatology Benefits—In this retrospective review of medical records of patients who obtained dermatologic care after the implementation of SVs at our institution, we found a proportionally higher use of SVs among Black patients, patients with Medicaid, and patients who are underinsured. Benefits of teledermatology include decreases in patient transportation and associated costs, time away from work or home, and need for childcare.6 The SV format provides the additional advantage of direct live interaction and the development of a patient-physician or patient–physician assistant relationship. Although the prerequisite technology, internet, and broadband connectivity preclude use of teledermatology for many vulnerable patients,2 its convenience ultimately may reduce inequities in access.
Disparities in Dermatologic Care—Hispanic ethnicity and male sex are among described patient demographics associated with decreased rates of outpatient dermatologic care.7 We reported disparities in dermatologic care utilization across all visit types among Hispanic patients and males. Patients identifying as Hispanic/Latino composed only 1.4% (n=209) of our study population compared with 2.3% of Allegheny County residents.5 During our study period, most patients seen were female, accounting for 62.1% to 72.8% of visits, compared with 51.6% of Allegheny County residents.5 These disparities in dermatologic care use may have implications for increased skin-associated morbidity and provide impetus for dermatologists to increase engagement with these patient groups.
Characteristics of Patients Using Teledermatology—Patients using SVs and AVs were significantly younger (mean age [SD], 39.9 [16.9] years and 37.5 [14.3] years, respectively) compared with those using IVs (51.0 [18.8] years). This finding reflects known digital knowledge barriers among older patients.8,9 The synchronous communication format of SVs simulates the traditional visit style of IVs, which may be preferable for some patients. Continued patient education and advocacy for broadband access may increase teledermatology use among older patients and patients with limited technology resources.8
Teledermatology visits were used most frequently for acne and dermatitis, while IVs were used for skin cancer screenings and examination of concerning lesions. This usage pattern is consistent with a previously described consensus among dermatologists on the conditions most amenable to teledermatology evaluation.3
Medicaid reimbursement parity for SVs is in effect nationally until the end of the COVID-19 public health emergency declaration in the United States.10 As of February 2023, the public health emergency declaration has been renewed 12 times since January 2020, with the most recent renewal on January 11, 2023.11 As of January 2023, 21 states have enacted legislation providing permanent reimbursement parity for SV services. Six additional states have some payment parity in place, each with its own qualifying criteria, and 23 states have no payment parity.12 Only 25 Medicaid programs currently provide reimbursement for AV services.13
Study Limitations—Our study was limited by lack of data on patients who are multiracial and those who identify as nonbinary and transgender. Because of the low numbers of Hispanic patients associated with each race category and a high number of patients who did not report an ethnicity or race, race and ethnicity data were analyzed separately. For SVs, patients were instructed to upload photographs prior to their visit; however, the percentage of patients who uploaded photographs was not analyzed.
Conclusion
Expansion of teledermatology services, including SVs and AVs, patient outreach and education, advocacy for broadband access, and Medicaid payment parity, may improve dermatologic care access for medically marginalized groups. Teledermatology has the potential to serve as an effective health care option for patients who are racially minoritized, older, and underinsured. To further assess the effectiveness of teledermatology, we plan to analyze the number of SVs and AVs that were referred to IVs. Future studies also will investigate the impact of implementing patient education and patient-reported outcomes of teledermatology visits.
- Lee JJ, English JC. Teledermatology: a review and update. Am J Clin Dermatol. 2018;19:253-260.
- Bakhtiar M, Elbuluk N, Lipoff JB. The digital divide: how COVID-19’s telemedicine expansion could exacerbate disparities. J Am Acad Dermatol. 2020;83:E345-E346.
- Kennedy J, Arey S, Hopkins Z, et al. dermatologist perceptions of teledermatology implementation and future use after COVID-19: demographics, barriers, and insights. JAMA Dermatol. 2021;157:595-597.
- Centers for Disease Control and Prevention. Using telehealth to expand access to essential health services during the COVID-19 pandemic. Updated June 10, 2020. Accessed February 10, 2023. https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html
- United States Census Bureau. QuickFacts: Allegheny County, Pennsylvania. Accessed August 12, 2021. https://www.census.gov/quickfacts/alleghenycountypennsylvania
- Moore HW. Teledermatology—access to specialized care via a different model. Dermatology Advisor. November 12, 2019. Accessed February 10, 2023. https://www.dermatologyadvisor.com/home/topics/practice-management/teledermatology-access-to-specialized-care-via-a-different-model/
- Tripathi R, Knusel KD, Ezaldein HH, et al. Association of demographic and socioeconomic characteristics with differences in use of outpatient dermatology services in the United States. JAMA Dermatol. 2018;154:1286-1291.
- Nouri S, Khoong EC, Lyles CR, et al. Addressing equity in telemedicine for chronic disease management during the COVID-19 pandemic [published online May 4, 2020]. NEJM Catal Innov Care Deliv. doi:10.1056/CAT.20.0123
- Swenson K, Ghertner R. People in low-income households have less access to internet services—2019 update. Office of the Assistant Secretary for Planning and Evaluation; US Department of Health and Human Services. March 2021. Accessed February 10, 2023. https://aspe.hhs.gov/sites/default/files/private/pdf/263601/internet-access-among-low-income-2019.pdf
- Centers for Medicare and Medicaid Services. COVID-19 frequently asked questions (FAQs) on Medicare fee-for-service (FFS) billing. Updated August 16, 2022. Accessed February 10, 2023. https://www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf
- US Department of Health and Human Services. Renewal of determination that a public health emergency exists. Updated February 9, 2023. Accessed February 20, 2023. https://aspr.hhs.gov/legal/PHE/Pages/COVID19-9Feb2023.aspx?
- Augenstein J, Smith JM. Executive summary: tracking telehealth changes state-by-state in response to COVID-19. Updated January 27, 2023. Accessed February 10, 2023. https://www.manatt.com/insights/newsletters/covid-19-update/executive-summary-tracking-telehealth-changes-stat
- Center for Connected Health Policy. Policy trend maps: store and forward Medicaid reimbursement. Accessed June 23, 2022. https://www.cchpca.org/policy-trends/
- Lee JJ, English JC. Teledermatology: a review and update. Am J Clin Dermatol. 2018;19:253-260.
- Bakhtiar M, Elbuluk N, Lipoff JB. The digital divide: how COVID-19’s telemedicine expansion could exacerbate disparities. J Am Acad Dermatol. 2020;83:E345-E346.
- Kennedy J, Arey S, Hopkins Z, et al. dermatologist perceptions of teledermatology implementation and future use after COVID-19: demographics, barriers, and insights. JAMA Dermatol. 2021;157:595-597.
- Centers for Disease Control and Prevention. Using telehealth to expand access to essential health services during the COVID-19 pandemic. Updated June 10, 2020. Accessed February 10, 2023. https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html
- United States Census Bureau. QuickFacts: Allegheny County, Pennsylvania. Accessed August 12, 2021. https://www.census.gov/quickfacts/alleghenycountypennsylvania
- Moore HW. Teledermatology—access to specialized care via a different model. Dermatology Advisor. November 12, 2019. Accessed February 10, 2023. https://www.dermatologyadvisor.com/home/topics/practice-management/teledermatology-access-to-specialized-care-via-a-different-model/
- Tripathi R, Knusel KD, Ezaldein HH, et al. Association of demographic and socioeconomic characteristics with differences in use of outpatient dermatology services in the United States. JAMA Dermatol. 2018;154:1286-1291.
- Nouri S, Khoong EC, Lyles CR, et al. Addressing equity in telemedicine for chronic disease management during the COVID-19 pandemic [published online May 4, 2020]. NEJM Catal Innov Care Deliv. doi:10.1056/CAT.20.0123
- Swenson K, Ghertner R. People in low-income households have less access to internet services—2019 update. Office of the Assistant Secretary for Planning and Evaluation; US Department of Health and Human Services. March 2021. Accessed February 10, 2023. https://aspe.hhs.gov/sites/default/files/private/pdf/263601/internet-access-among-low-income-2019.pdf
- Centers for Medicare and Medicaid Services. COVID-19 frequently asked questions (FAQs) on Medicare fee-for-service (FFS) billing. Updated August 16, 2022. Accessed February 10, 2023. https://www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf
- US Department of Health and Human Services. Renewal of determination that a public health emergency exists. Updated February 9, 2023. Accessed February 20, 2023. https://aspr.hhs.gov/legal/PHE/Pages/COVID19-9Feb2023.aspx?
- Augenstein J, Smith JM. Executive summary: tracking telehealth changes state-by-state in response to COVID-19. Updated January 27, 2023. Accessed February 10, 2023. https://www.manatt.com/insights/newsletters/covid-19-update/executive-summary-tracking-telehealth-changes-stat
- Center for Connected Health Policy. Policy trend maps: store and forward Medicaid reimbursement. Accessed June 23, 2022. https://www.cchpca.org/policy-trends/
Practice Points
- There is increased use of synchronous video visits (SVs) among Black patients, patients with Medicaid, and patients who are underinsured.
- Synchronous video visits may increase dermatologic care utilization for medically marginalized groups.
- Efforts are needed to increase engagement with dermatologic care for Hispanic and male patients.
Expert dispels myths about hair care in patients with skin of color
HONOLULU –
“This is false,” Dr. Heath, director of pediatric dermatology at Temple University, Philadelphia, said at the Hawaii Dermatology Seminar provided by MedscapeLIVE! With little manipulation, length may be retained, since tightly coiled hair has a higher likelihood of breakage, she said. “But washing the scalp and hair is recommended for tightly coiled hair weekly or every other week. Exclusively co-washing – a technique where hair conditioner is used instead of shampooing – is also not advised due to scalp build-up.”
Other myths she addressed include the following:
“I have a weak spot (or stress spot) on the top of my scalp.” These terms may be used to describe hair on a spot that goes through cycles of breaking off and re-growing. This is false. “If someone were to say that, and we see short hairs on the top of a patient’s scalp, with or without tenderness, pruritus, or pain, we want to recognize that as possibly an early sign of central centrifugal cicatricial alopecia [CCCA],” she said. “We want to pick up cases of CCCA forme fruste [central hair breakage] early.”
Medicated shampoos are helpful for all patients with seborrheic dermatitis. This notion is more complicated. “In theory, medicated shampoos like ketoconazole should be helpful, but if the shampoos are too drying for the hair and they cause further hair breakage, that’s going to be a problem as well,” explained Dr. Heath, who was the senior author of an article on how to address common conditions affecting pediatric and adolescent patients with skin of color. For patients with tightly coiled hair, she recommends applying antifungal shampoos to the scalp only, waiting 5-10 minutes, rinsing, and shampooing the scalp and hair with a moisturizing shampoo and rinsing. They can then condition with a moisturizing conditioner and style their hair as desired.
Don’t touch a Black woman’s hair. That unwritten rule may apply to a woman you pass on the street, she said, but not during clinical exams in cases where clinicians and patients seeking hair loss treatment have different hair types. “Touch the hair; don’t do a lean-in exam,” emphasized Dr. Heath, who is the inaugural faculty scholar at Temple University Lewis Katz School of Medicine’s Office of Health Equity Diversity, and Inclusion. “You want to perform the scalp and hair exam with cultural humility.” Understanding the patient’s hair care goals and perspective allows dermatologists to take a more individualized approach to their concerns, especially in race-discordant patient-physician interactions.
Going natural (chemical-free) will solve scarring hair loss problems. This is false. “Genetic defects in the hair shaft have been described as the cause of some CCCA cases, so we need to stop solely blaming the patient for that condition,” she said. Dr. Heath noted that the transition point between natural hair and relaxed hair is highly prone to breakage. She suggests low or lower tension options such as knotless braids, and crochet hairstyles, and when patients have locs, they should be shoulder length or higher to reduce tension.
Dr. Heath disclosed that she has served as a consultant or adviser for Arcutis, CeraVe, Janssen Pharmaceuticals, Johnson & Johnson Pharmaceutical Research & Development, Leo, Lilly, Pfizer, and Regeneron Pharmaceuticals.
Medscape and this news organization are owned by the same parent company.
HONOLULU –
“This is false,” Dr. Heath, director of pediatric dermatology at Temple University, Philadelphia, said at the Hawaii Dermatology Seminar provided by MedscapeLIVE! With little manipulation, length may be retained, since tightly coiled hair has a higher likelihood of breakage, she said. “But washing the scalp and hair is recommended for tightly coiled hair weekly or every other week. Exclusively co-washing – a technique where hair conditioner is used instead of shampooing – is also not advised due to scalp build-up.”
Other myths she addressed include the following:
“I have a weak spot (or stress spot) on the top of my scalp.” These terms may be used to describe hair on a spot that goes through cycles of breaking off and re-growing. This is false. “If someone were to say that, and we see short hairs on the top of a patient’s scalp, with or without tenderness, pruritus, or pain, we want to recognize that as possibly an early sign of central centrifugal cicatricial alopecia [CCCA],” she said. “We want to pick up cases of CCCA forme fruste [central hair breakage] early.”
Medicated shampoos are helpful for all patients with seborrheic dermatitis. This notion is more complicated. “In theory, medicated shampoos like ketoconazole should be helpful, but if the shampoos are too drying for the hair and they cause further hair breakage, that’s going to be a problem as well,” explained Dr. Heath, who was the senior author of an article on how to address common conditions affecting pediatric and adolescent patients with skin of color. For patients with tightly coiled hair, she recommends applying antifungal shampoos to the scalp only, waiting 5-10 minutes, rinsing, and shampooing the scalp and hair with a moisturizing shampoo and rinsing. They can then condition with a moisturizing conditioner and style their hair as desired.
Don’t touch a Black woman’s hair. That unwritten rule may apply to a woman you pass on the street, she said, but not during clinical exams in cases where clinicians and patients seeking hair loss treatment have different hair types. “Touch the hair; don’t do a lean-in exam,” emphasized Dr. Heath, who is the inaugural faculty scholar at Temple University Lewis Katz School of Medicine’s Office of Health Equity Diversity, and Inclusion. “You want to perform the scalp and hair exam with cultural humility.” Understanding the patient’s hair care goals and perspective allows dermatologists to take a more individualized approach to their concerns, especially in race-discordant patient-physician interactions.
Going natural (chemical-free) will solve scarring hair loss problems. This is false. “Genetic defects in the hair shaft have been described as the cause of some CCCA cases, so we need to stop solely blaming the patient for that condition,” she said. Dr. Heath noted that the transition point between natural hair and relaxed hair is highly prone to breakage. She suggests low or lower tension options such as knotless braids, and crochet hairstyles, and when patients have locs, they should be shoulder length or higher to reduce tension.
Dr. Heath disclosed that she has served as a consultant or adviser for Arcutis, CeraVe, Janssen Pharmaceuticals, Johnson & Johnson Pharmaceutical Research & Development, Leo, Lilly, Pfizer, and Regeneron Pharmaceuticals.
Medscape and this news organization are owned by the same parent company.
HONOLULU –
“This is false,” Dr. Heath, director of pediatric dermatology at Temple University, Philadelphia, said at the Hawaii Dermatology Seminar provided by MedscapeLIVE! With little manipulation, length may be retained, since tightly coiled hair has a higher likelihood of breakage, she said. “But washing the scalp and hair is recommended for tightly coiled hair weekly or every other week. Exclusively co-washing – a technique where hair conditioner is used instead of shampooing – is also not advised due to scalp build-up.”
Other myths she addressed include the following:
“I have a weak spot (or stress spot) on the top of my scalp.” These terms may be used to describe hair on a spot that goes through cycles of breaking off and re-growing. This is false. “If someone were to say that, and we see short hairs on the top of a patient’s scalp, with or without tenderness, pruritus, or pain, we want to recognize that as possibly an early sign of central centrifugal cicatricial alopecia [CCCA],” she said. “We want to pick up cases of CCCA forme fruste [central hair breakage] early.”
Medicated shampoos are helpful for all patients with seborrheic dermatitis. This notion is more complicated. “In theory, medicated shampoos like ketoconazole should be helpful, but if the shampoos are too drying for the hair and they cause further hair breakage, that’s going to be a problem as well,” explained Dr. Heath, who was the senior author of an article on how to address common conditions affecting pediatric and adolescent patients with skin of color. For patients with tightly coiled hair, she recommends applying antifungal shampoos to the scalp only, waiting 5-10 minutes, rinsing, and shampooing the scalp and hair with a moisturizing shampoo and rinsing. They can then condition with a moisturizing conditioner and style their hair as desired.
Don’t touch a Black woman’s hair. That unwritten rule may apply to a woman you pass on the street, she said, but not during clinical exams in cases where clinicians and patients seeking hair loss treatment have different hair types. “Touch the hair; don’t do a lean-in exam,” emphasized Dr. Heath, who is the inaugural faculty scholar at Temple University Lewis Katz School of Medicine’s Office of Health Equity Diversity, and Inclusion. “You want to perform the scalp and hair exam with cultural humility.” Understanding the patient’s hair care goals and perspective allows dermatologists to take a more individualized approach to their concerns, especially in race-discordant patient-physician interactions.
Going natural (chemical-free) will solve scarring hair loss problems. This is false. “Genetic defects in the hair shaft have been described as the cause of some CCCA cases, so we need to stop solely blaming the patient for that condition,” she said. Dr. Heath noted that the transition point between natural hair and relaxed hair is highly prone to breakage. She suggests low or lower tension options such as knotless braids, and crochet hairstyles, and when patients have locs, they should be shoulder length or higher to reduce tension.
Dr. Heath disclosed that she has served as a consultant or adviser for Arcutis, CeraVe, Janssen Pharmaceuticals, Johnson & Johnson Pharmaceutical Research & Development, Leo, Lilly, Pfizer, and Regeneron Pharmaceuticals.
Medscape and this news organization are owned by the same parent company.
AT THE MEDSCAPE LIVE! HAWAII DERMATOLOGY SEMINAR
No sex bias seen in ACC 22 speaker introductions
Men making speaker introductions at the 2022 annual scientific sessions of the American College of Cardiology were similarly likely to use professional titles regardless of gender, while women making introductions were more likely to use professional titles overall, based on a review of more than 800 videos of last year’s presentations.
“Implicit sex bias in speaker introductions at major medical conferences can foster and drive sex-driven assumptions about the competency of the speaker,” corresponding author Ankur Kalra, MD, an interventional cardiologist at Franciscan Health, Lafayette, Ind., said in an interview. “This is particularly important as recent data have shown a welcome, though gradual increase in the number of women speakers at major cardiology scientific sessions.”
In a research letter published in JACC: Advances, the researchers reviewed 1,696 videos from the ACC meeting held in Washington in April 2022 compiled by ACC Anywhere, and identified the participants as either “introducers” or “speakers.”
The final analysis included 888 speaker-introducer dyads. The introducer population was 49.4% men and 50.6% women; the speaker population included 58.8% men and 41.2% women.
Overall, 77.9% of speakers were addressed professionally in the first mention, and 71.5% were addressed professionally throughout the introduction. When making introductions, full professors were significantly more likely to use nonprofessional address than associate professors, assistant professors, and trainees (28.7% vs. 18.2%, 10.8%, and 0%, respectively).
Regardless of the sex of the speaker, women making introductions were significantly more likely than men to use professional titles for the speaker on first reference and consistently (84.2% vs. 71.5% and 78.2% vs. 64.7%, respectively; P < 0.001 for both).
Men doing introductions used professional forms of address similarly for both men and women speakers on first reference and consistently (72.2% vs. 71.1% and 65.4% vs. 64.3%, respectively).
No significant difference appeared in the use of professional address by women introducing women speakers compared to women introducing men speakers on first reference and consistently (81.9% vs. 86.1% and 75.0% vs. 80.8%, respectively).
“There was no significant association of the formality of introductions with the speaker’s sex and rank,” the researchers noted.
The findings were limited by several factors, including a lack of self-identified sex data, restriction to a binary determination of sex, and a lack of race/ethnicity analysis, the authors noted. In addition, the study could not account for prior familiarity between introducers and speakers that might influence the introduction.
Findings show positive trend
Dr. Kalra was surprised by the study findings, but in a good way. “A recent study on speakers presenting at Internal Medicine grand rounds demonstrated significant sex-based differences in using professional titles for formal introductions for women speakers in comparison with men speakers,” he said in an interview. The current study researchers expected to find similar differences.
“To our pleasant surprise, there was no implicit sex bias in introductions at the ACC 22, as there was no significant difference in the use of professional forms of address by men introducers of women speakers compared with men introducers of men speakers,” he said. “Similarly, the percentage of professional forms of address by women introducers was similar for men and women speakers.”
Setting an example
“A platform like ACC 22 is a window into the world of cardiovascular disease professionals – it’s a snapshot of who we are and what ethos/principles/values we represent,” said Dr. Kalra. “How we introduce one another is a surrogate marker of the mutual respect we behold for one another; our characters are on display, and the world and our junior colleagues are watching. Modern-day cardiology departments and practices must be completely intolerant to subtle microaggressions. The important take-away for clinicians is that it could be that our surprising findings may be attributed to the increased dialogue on sex disparities in cardiology, which has made physicians more cognizant of subtle microaggressions.”
A larger sample size is needed to replicate the study findings, and Dr. Kalra and colleagues hope to include data from ACC’s 2023 meeting, held with the World Congress of Cardiology in March, for additional research in this area.
Time to close inclusion gaps
“The time is now to dive into all previous and current gaps in diversity and inclusion,” Roxana Mehran, MD, said in an interview. “We must understand what the data are, and disseminate and educate all in health care on these issues.”
Dr. Mehran said she was not surprised by the findings of the current study. “This has been my own feeling for many years, watching mostly men be given important roles, such as Grand Rounds Speaking engagements. Now we have the data, and I congratulate the authors for the hard work to dig this out.
“In all aspects, we need to look at the entire talent pool to choose leadership, speakers, and key opinion leaders, as well as principal investigators in clinical trials,” said Dr. Mehran. “This has long been given to our wonderful and talented male colleagues without any effort to look for women, and non-Whites to be given the opportunity to shine and share their talent.”
Looking ahead, “we must remain vigilant and close gaps in all aspects of medicine whether in delivering care, or in the work force; this needs intentional efforts by all.”
The study was funded by makeadent.org and the Ram and Sanjita Kalra Aavishqaar Fund. Dr. Kalra is the CEO and creative director of makeadent.org. The other authors had no financial conflicts to disclose. Dr. Mehran had no financial conflicts to disclose.
Men making speaker introductions at the 2022 annual scientific sessions of the American College of Cardiology were similarly likely to use professional titles regardless of gender, while women making introductions were more likely to use professional titles overall, based on a review of more than 800 videos of last year’s presentations.
“Implicit sex bias in speaker introductions at major medical conferences can foster and drive sex-driven assumptions about the competency of the speaker,” corresponding author Ankur Kalra, MD, an interventional cardiologist at Franciscan Health, Lafayette, Ind., said in an interview. “This is particularly important as recent data have shown a welcome, though gradual increase in the number of women speakers at major cardiology scientific sessions.”
In a research letter published in JACC: Advances, the researchers reviewed 1,696 videos from the ACC meeting held in Washington in April 2022 compiled by ACC Anywhere, and identified the participants as either “introducers” or “speakers.”
The final analysis included 888 speaker-introducer dyads. The introducer population was 49.4% men and 50.6% women; the speaker population included 58.8% men and 41.2% women.
Overall, 77.9% of speakers were addressed professionally in the first mention, and 71.5% were addressed professionally throughout the introduction. When making introductions, full professors were significantly more likely to use nonprofessional address than associate professors, assistant professors, and trainees (28.7% vs. 18.2%, 10.8%, and 0%, respectively).
Regardless of the sex of the speaker, women making introductions were significantly more likely than men to use professional titles for the speaker on first reference and consistently (84.2% vs. 71.5% and 78.2% vs. 64.7%, respectively; P < 0.001 for both).
Men doing introductions used professional forms of address similarly for both men and women speakers on first reference and consistently (72.2% vs. 71.1% and 65.4% vs. 64.3%, respectively).
No significant difference appeared in the use of professional address by women introducing women speakers compared to women introducing men speakers on first reference and consistently (81.9% vs. 86.1% and 75.0% vs. 80.8%, respectively).
“There was no significant association of the formality of introductions with the speaker’s sex and rank,” the researchers noted.
The findings were limited by several factors, including a lack of self-identified sex data, restriction to a binary determination of sex, and a lack of race/ethnicity analysis, the authors noted. In addition, the study could not account for prior familiarity between introducers and speakers that might influence the introduction.
Findings show positive trend
Dr. Kalra was surprised by the study findings, but in a good way. “A recent study on speakers presenting at Internal Medicine grand rounds demonstrated significant sex-based differences in using professional titles for formal introductions for women speakers in comparison with men speakers,” he said in an interview. The current study researchers expected to find similar differences.
“To our pleasant surprise, there was no implicit sex bias in introductions at the ACC 22, as there was no significant difference in the use of professional forms of address by men introducers of women speakers compared with men introducers of men speakers,” he said. “Similarly, the percentage of professional forms of address by women introducers was similar for men and women speakers.”
Setting an example
“A platform like ACC 22 is a window into the world of cardiovascular disease professionals – it’s a snapshot of who we are and what ethos/principles/values we represent,” said Dr. Kalra. “How we introduce one another is a surrogate marker of the mutual respect we behold for one another; our characters are on display, and the world and our junior colleagues are watching. Modern-day cardiology departments and practices must be completely intolerant to subtle microaggressions. The important take-away for clinicians is that it could be that our surprising findings may be attributed to the increased dialogue on sex disparities in cardiology, which has made physicians more cognizant of subtle microaggressions.”
A larger sample size is needed to replicate the study findings, and Dr. Kalra and colleagues hope to include data from ACC’s 2023 meeting, held with the World Congress of Cardiology in March, for additional research in this area.
Time to close inclusion gaps
“The time is now to dive into all previous and current gaps in diversity and inclusion,” Roxana Mehran, MD, said in an interview. “We must understand what the data are, and disseminate and educate all in health care on these issues.”
Dr. Mehran said she was not surprised by the findings of the current study. “This has been my own feeling for many years, watching mostly men be given important roles, such as Grand Rounds Speaking engagements. Now we have the data, and I congratulate the authors for the hard work to dig this out.
“In all aspects, we need to look at the entire talent pool to choose leadership, speakers, and key opinion leaders, as well as principal investigators in clinical trials,” said Dr. Mehran. “This has long been given to our wonderful and talented male colleagues without any effort to look for women, and non-Whites to be given the opportunity to shine and share their talent.”
Looking ahead, “we must remain vigilant and close gaps in all aspects of medicine whether in delivering care, or in the work force; this needs intentional efforts by all.”
The study was funded by makeadent.org and the Ram and Sanjita Kalra Aavishqaar Fund. Dr. Kalra is the CEO and creative director of makeadent.org. The other authors had no financial conflicts to disclose. Dr. Mehran had no financial conflicts to disclose.
Men making speaker introductions at the 2022 annual scientific sessions of the American College of Cardiology were similarly likely to use professional titles regardless of gender, while women making introductions were more likely to use professional titles overall, based on a review of more than 800 videos of last year’s presentations.
“Implicit sex bias in speaker introductions at major medical conferences can foster and drive sex-driven assumptions about the competency of the speaker,” corresponding author Ankur Kalra, MD, an interventional cardiologist at Franciscan Health, Lafayette, Ind., said in an interview. “This is particularly important as recent data have shown a welcome, though gradual increase in the number of women speakers at major cardiology scientific sessions.”
In a research letter published in JACC: Advances, the researchers reviewed 1,696 videos from the ACC meeting held in Washington in April 2022 compiled by ACC Anywhere, and identified the participants as either “introducers” or “speakers.”
The final analysis included 888 speaker-introducer dyads. The introducer population was 49.4% men and 50.6% women; the speaker population included 58.8% men and 41.2% women.
Overall, 77.9% of speakers were addressed professionally in the first mention, and 71.5% were addressed professionally throughout the introduction. When making introductions, full professors were significantly more likely to use nonprofessional address than associate professors, assistant professors, and trainees (28.7% vs. 18.2%, 10.8%, and 0%, respectively).
Regardless of the sex of the speaker, women making introductions were significantly more likely than men to use professional titles for the speaker on first reference and consistently (84.2% vs. 71.5% and 78.2% vs. 64.7%, respectively; P < 0.001 for both).
Men doing introductions used professional forms of address similarly for both men and women speakers on first reference and consistently (72.2% vs. 71.1% and 65.4% vs. 64.3%, respectively).
No significant difference appeared in the use of professional address by women introducing women speakers compared to women introducing men speakers on first reference and consistently (81.9% vs. 86.1% and 75.0% vs. 80.8%, respectively).
“There was no significant association of the formality of introductions with the speaker’s sex and rank,” the researchers noted.
The findings were limited by several factors, including a lack of self-identified sex data, restriction to a binary determination of sex, and a lack of race/ethnicity analysis, the authors noted. In addition, the study could not account for prior familiarity between introducers and speakers that might influence the introduction.
Findings show positive trend
Dr. Kalra was surprised by the study findings, but in a good way. “A recent study on speakers presenting at Internal Medicine grand rounds demonstrated significant sex-based differences in using professional titles for formal introductions for women speakers in comparison with men speakers,” he said in an interview. The current study researchers expected to find similar differences.
“To our pleasant surprise, there was no implicit sex bias in introductions at the ACC 22, as there was no significant difference in the use of professional forms of address by men introducers of women speakers compared with men introducers of men speakers,” he said. “Similarly, the percentage of professional forms of address by women introducers was similar for men and women speakers.”
Setting an example
“A platform like ACC 22 is a window into the world of cardiovascular disease professionals – it’s a snapshot of who we are and what ethos/principles/values we represent,” said Dr. Kalra. “How we introduce one another is a surrogate marker of the mutual respect we behold for one another; our characters are on display, and the world and our junior colleagues are watching. Modern-day cardiology departments and practices must be completely intolerant to subtle microaggressions. The important take-away for clinicians is that it could be that our surprising findings may be attributed to the increased dialogue on sex disparities in cardiology, which has made physicians more cognizant of subtle microaggressions.”
A larger sample size is needed to replicate the study findings, and Dr. Kalra and colleagues hope to include data from ACC’s 2023 meeting, held with the World Congress of Cardiology in March, for additional research in this area.
Time to close inclusion gaps
“The time is now to dive into all previous and current gaps in diversity and inclusion,” Roxana Mehran, MD, said in an interview. “We must understand what the data are, and disseminate and educate all in health care on these issues.”
Dr. Mehran said she was not surprised by the findings of the current study. “This has been my own feeling for many years, watching mostly men be given important roles, such as Grand Rounds Speaking engagements. Now we have the data, and I congratulate the authors for the hard work to dig this out.
“In all aspects, we need to look at the entire talent pool to choose leadership, speakers, and key opinion leaders, as well as principal investigators in clinical trials,” said Dr. Mehran. “This has long been given to our wonderful and talented male colleagues without any effort to look for women, and non-Whites to be given the opportunity to shine and share their talent.”
Looking ahead, “we must remain vigilant and close gaps in all aspects of medicine whether in delivering care, or in the work force; this needs intentional efforts by all.”
The study was funded by makeadent.org and the Ram and Sanjita Kalra Aavishqaar Fund. Dr. Kalra is the CEO and creative director of makeadent.org. The other authors had no financial conflicts to disclose. Dr. Mehran had no financial conflicts to disclose.
FROM JACC: ADVANCES
Zero tolerance for patient bias: Too harsh? Clinicians respond
If a patient refuses care from a health care practitioner because of their race or sex, should their request be accommodated?
In a recent blog on Medscape titled “No, You Can’t See a Different Doctor: We Need Zero Tolerance of Patient Bias,” Cleveland Francis Jr., MD, argued no.
Dr. Francis, who is Black, is a recently retired cardiologist who practiced for 50 years. He is currently Diversity, Equity, and Inclusion Advisor at Inova Heart and Vascular Institute in Falls Church, Va.
When Francis was a medical student and was preparing to take a patient’s history and perform a medical exam, the patient refused and requested a “White doctor,” he recounted.
“I can remember the hurt and embarrassment as if it were yesterday,” he wrote.
The blog, especially the title, drew strong reactions. Close to 500 readers weighed in.
“The title of my blog sounds harsh,” Dr. Francis said, “but in reality, a simple conversation with the patient usually resolves these issues. The difference is that in the old days, there was utter silence, and the wishes of the patient would be granted”
Health care practitioners “should expect to be treated with respect,” he concluded his blog.
Readers agreed on that point, but they debated whether being uncomfortable with a health care practitioner of a different sex or race always constituted “patient bias.”
Some noted that difficulty understanding a practitioner’s accent, for example, is a legitimate reason for asking for another clinician.
Accents and understanding
“If I am struggling to understand you because your accent is too thick or ... because hearing aids can only do so much, I need to ask for someone else,” a reader commented.
Another chimed in: “My elderly parents changed PCPs frequently during the final years of their lives, mainly due to language barriers encountered with foreign-born providers. Due to progressive hearing loss, they simply couldn’t understand them.”
“It is important to remember that there is a Patient Bill of Rights,” she noted, “the first part of which states, ‘You have the right to safe, considerate, and respectful care, provided in a manner consistent with your beliefs.’ ”
A former charge nurse added: “If a request for change was substantive (poor communication, perceived incompetence, trauma history, etc.), I would move mountains to accommodate it, but IMHO [in my humble opinion], the belief in honoring patient preference doesn’t necessarily need to include rearranging the world in order to accommodate racism, sexism, etc.”
Bias against female doctors, male nurses
Many commenters described how they gladly traded when a patient requested a practitioner of the opposite sex.
A female hospitalist related how she contacted the senior male doctor working with her to arrange a patient trade, adding, “I do agree that racial discrimination ought to be discouraged.”
Similarly, a male ICU RN commented: “Over 13 years, I have had a handful of female (usually older) patients request a female nurse. I have always strived to make this happen.”
However, an older woman related how at first she “had some bias against a male nurse touching me and also felt self-conscious,” she said. “So, I tried to relax ... and let him do his job. He was one of the most compassionate, kind, and sensitive nurses I’ve ever had.”
“I think in some cases,” she noted, “some women have had a history of some sort of abuse by a male, whether it’s sexual or psychological,” but in other cases, “it’s often just a personal preference, not a bias.”
A physician assistant (PA) who worked in a rural ED recounted how “there was only one physician and one PA on at any given evening/night shift, both usually White males.”
“Sometimes, you just have to cope as best you can with whomever is available, and in doing so,” he said, “they might just end up being pleasantly surprised.”
Don’t take it personally, move on
“If a patient doesn’t want to see me for whatever reason, then I would rather not treat them,” was a common sentiment.
Patients “should feel comfortable with their provider even if it’s with someone other than myself,” a reader wrote.
A female physician chimed in: “I frequently have older male patients refuse to see me. ... While this is irritating on several levels, I recognize that it is the patient’s choice, sigh, and move on to the next patient.”
“There are many more patients who specifically ask to see me, so I don’t waste my time and energy on being bothered by those who refuse.”
Similarly, a female mental health provider and sometimes patient wrote: “If any patient tells me that they prefer a male ... or someone of a particular race or religion or whatever, I don’t take it personally.”
A female Hispanic doctor chimed in: “Honestly, if a patient does not want to see me due to my race, I’m OK with that. Patients need to feel comfortable with me for the relationship to be therapeutic and effective,” she said.
“Forcing the patient to see me is adding injury to insult to ME! Not to mention increase[d] workload since that patient will take [so] much more time.”
Similarly, an Asian American doctor commented: “There are people who choose not to see me because of my ethnicity. However, I strongly believe that it should always be the patient’s preference. Whatever the reason, do not force the patient to see you in the name of Diversity, Equity, Inclusion, or whatever hurts your feeling. Let the patient go.”
Patient bias vs. patient preference
A physician referring to Dr. Francis’s experience suggested that “perhaps there was an opportunity to explore this misconception directly with the patient. If not, your supervising senior resident or attending should have been informed and brought into the process and conversation.”
“If/when I were rejected by a patient for whatever reason,” another physician commented, “I would gracefully accede, and hope that my colleague would tactfully point out to the patient their error.”
“Having a nurse ask the patient ... what they need style-wise (keeping race, gender, etc., out of it) might help identify whether or not the underlying issue(s) are based on style/needs mismatch match rather than bias,” a reader suggested.
A health care worker commented: “We generally assure patients that we are professionals and think nothing of situations that they might find uncomfortable, but don’t realize that our comfort does not translate to theirs.”
Maybe a different strategy is needed
“Having been the target of bias many times,” a reader said, “I understand the pain that is inflicted. Unfortunately, a patient bias policy, while a good idea, will not prevent patient bias. This is a much larger societal problem. But we can at least tell patients that it is not okay. On the other hand, I would not want to be the provider for a patient who was biased against me and held me in disdain.”
“I do not like Zero Tolerance policies ever. They are too absolute,” another reader commented. “Sometimes, there are reasons and we do have to listen to our patients for why. ... I do not think a policy of zero tolerance will fix the problem of racism.”
“Instead of trying to educate the general public about how not to be jerks,” another reader suggested, “perhaps it would be easier to provide elective classes for doctors and employees who believe themselves to be at-risk for discrimination, providing them with a ‘toolkit’ of strategies for responding to discrimination in the moment, processing it emotionally later on, and reporting the most egregious events through designated channels.”
Another commenter agreed and wrote that, “While we as doctors need and deserve protection, we are also called to act with compassion. So, rather than ask the system for ‘zero-tolerance’ in either direction, we could encourage our health systems to provide education, support, and mediation to any party who feels or fears that they are not being well served. Such a model would include support for physicians who have been the victims of bias and hurt.”
A version of this article originally appeared on Medscape.com.
If a patient refuses care from a health care practitioner because of their race or sex, should their request be accommodated?
In a recent blog on Medscape titled “No, You Can’t See a Different Doctor: We Need Zero Tolerance of Patient Bias,” Cleveland Francis Jr., MD, argued no.
Dr. Francis, who is Black, is a recently retired cardiologist who practiced for 50 years. He is currently Diversity, Equity, and Inclusion Advisor at Inova Heart and Vascular Institute in Falls Church, Va.
When Francis was a medical student and was preparing to take a patient’s history and perform a medical exam, the patient refused and requested a “White doctor,” he recounted.
“I can remember the hurt and embarrassment as if it were yesterday,” he wrote.
The blog, especially the title, drew strong reactions. Close to 500 readers weighed in.
“The title of my blog sounds harsh,” Dr. Francis said, “but in reality, a simple conversation with the patient usually resolves these issues. The difference is that in the old days, there was utter silence, and the wishes of the patient would be granted”
Health care practitioners “should expect to be treated with respect,” he concluded his blog.
Readers agreed on that point, but they debated whether being uncomfortable with a health care practitioner of a different sex or race always constituted “patient bias.”
Some noted that difficulty understanding a practitioner’s accent, for example, is a legitimate reason for asking for another clinician.
Accents and understanding
“If I am struggling to understand you because your accent is too thick or ... because hearing aids can only do so much, I need to ask for someone else,” a reader commented.
Another chimed in: “My elderly parents changed PCPs frequently during the final years of their lives, mainly due to language barriers encountered with foreign-born providers. Due to progressive hearing loss, they simply couldn’t understand them.”
“It is important to remember that there is a Patient Bill of Rights,” she noted, “the first part of which states, ‘You have the right to safe, considerate, and respectful care, provided in a manner consistent with your beliefs.’ ”
A former charge nurse added: “If a request for change was substantive (poor communication, perceived incompetence, trauma history, etc.), I would move mountains to accommodate it, but IMHO [in my humble opinion], the belief in honoring patient preference doesn’t necessarily need to include rearranging the world in order to accommodate racism, sexism, etc.”
Bias against female doctors, male nurses
Many commenters described how they gladly traded when a patient requested a practitioner of the opposite sex.
A female hospitalist related how she contacted the senior male doctor working with her to arrange a patient trade, adding, “I do agree that racial discrimination ought to be discouraged.”
Similarly, a male ICU RN commented: “Over 13 years, I have had a handful of female (usually older) patients request a female nurse. I have always strived to make this happen.”
However, an older woman related how at first she “had some bias against a male nurse touching me and also felt self-conscious,” she said. “So, I tried to relax ... and let him do his job. He was one of the most compassionate, kind, and sensitive nurses I’ve ever had.”
“I think in some cases,” she noted, “some women have had a history of some sort of abuse by a male, whether it’s sexual or psychological,” but in other cases, “it’s often just a personal preference, not a bias.”
A physician assistant (PA) who worked in a rural ED recounted how “there was only one physician and one PA on at any given evening/night shift, both usually White males.”
“Sometimes, you just have to cope as best you can with whomever is available, and in doing so,” he said, “they might just end up being pleasantly surprised.”
Don’t take it personally, move on
“If a patient doesn’t want to see me for whatever reason, then I would rather not treat them,” was a common sentiment.
Patients “should feel comfortable with their provider even if it’s with someone other than myself,” a reader wrote.
A female physician chimed in: “I frequently have older male patients refuse to see me. ... While this is irritating on several levels, I recognize that it is the patient’s choice, sigh, and move on to the next patient.”
“There are many more patients who specifically ask to see me, so I don’t waste my time and energy on being bothered by those who refuse.”
Similarly, a female mental health provider and sometimes patient wrote: “If any patient tells me that they prefer a male ... or someone of a particular race or religion or whatever, I don’t take it personally.”
A female Hispanic doctor chimed in: “Honestly, if a patient does not want to see me due to my race, I’m OK with that. Patients need to feel comfortable with me for the relationship to be therapeutic and effective,” she said.
“Forcing the patient to see me is adding injury to insult to ME! Not to mention increase[d] workload since that patient will take [so] much more time.”
Similarly, an Asian American doctor commented: “There are people who choose not to see me because of my ethnicity. However, I strongly believe that it should always be the patient’s preference. Whatever the reason, do not force the patient to see you in the name of Diversity, Equity, Inclusion, or whatever hurts your feeling. Let the patient go.”
Patient bias vs. patient preference
A physician referring to Dr. Francis’s experience suggested that “perhaps there was an opportunity to explore this misconception directly with the patient. If not, your supervising senior resident or attending should have been informed and brought into the process and conversation.”
“If/when I were rejected by a patient for whatever reason,” another physician commented, “I would gracefully accede, and hope that my colleague would tactfully point out to the patient their error.”
“Having a nurse ask the patient ... what they need style-wise (keeping race, gender, etc., out of it) might help identify whether or not the underlying issue(s) are based on style/needs mismatch match rather than bias,” a reader suggested.
A health care worker commented: “We generally assure patients that we are professionals and think nothing of situations that they might find uncomfortable, but don’t realize that our comfort does not translate to theirs.”
Maybe a different strategy is needed
“Having been the target of bias many times,” a reader said, “I understand the pain that is inflicted. Unfortunately, a patient bias policy, while a good idea, will not prevent patient bias. This is a much larger societal problem. But we can at least tell patients that it is not okay. On the other hand, I would not want to be the provider for a patient who was biased against me and held me in disdain.”
“I do not like Zero Tolerance policies ever. They are too absolute,” another reader commented. “Sometimes, there are reasons and we do have to listen to our patients for why. ... I do not think a policy of zero tolerance will fix the problem of racism.”
“Instead of trying to educate the general public about how not to be jerks,” another reader suggested, “perhaps it would be easier to provide elective classes for doctors and employees who believe themselves to be at-risk for discrimination, providing them with a ‘toolkit’ of strategies for responding to discrimination in the moment, processing it emotionally later on, and reporting the most egregious events through designated channels.”
Another commenter agreed and wrote that, “While we as doctors need and deserve protection, we are also called to act with compassion. So, rather than ask the system for ‘zero-tolerance’ in either direction, we could encourage our health systems to provide education, support, and mediation to any party who feels or fears that they are not being well served. Such a model would include support for physicians who have been the victims of bias and hurt.”
A version of this article originally appeared on Medscape.com.
If a patient refuses care from a health care practitioner because of their race or sex, should their request be accommodated?
In a recent blog on Medscape titled “No, You Can’t See a Different Doctor: We Need Zero Tolerance of Patient Bias,” Cleveland Francis Jr., MD, argued no.
Dr. Francis, who is Black, is a recently retired cardiologist who practiced for 50 years. He is currently Diversity, Equity, and Inclusion Advisor at Inova Heart and Vascular Institute in Falls Church, Va.
When Francis was a medical student and was preparing to take a patient’s history and perform a medical exam, the patient refused and requested a “White doctor,” he recounted.
“I can remember the hurt and embarrassment as if it were yesterday,” he wrote.
The blog, especially the title, drew strong reactions. Close to 500 readers weighed in.
“The title of my blog sounds harsh,” Dr. Francis said, “but in reality, a simple conversation with the patient usually resolves these issues. The difference is that in the old days, there was utter silence, and the wishes of the patient would be granted”
Health care practitioners “should expect to be treated with respect,” he concluded his blog.
Readers agreed on that point, but they debated whether being uncomfortable with a health care practitioner of a different sex or race always constituted “patient bias.”
Some noted that difficulty understanding a practitioner’s accent, for example, is a legitimate reason for asking for another clinician.
Accents and understanding
“If I am struggling to understand you because your accent is too thick or ... because hearing aids can only do so much, I need to ask for someone else,” a reader commented.
Another chimed in: “My elderly parents changed PCPs frequently during the final years of their lives, mainly due to language barriers encountered with foreign-born providers. Due to progressive hearing loss, they simply couldn’t understand them.”
“It is important to remember that there is a Patient Bill of Rights,” she noted, “the first part of which states, ‘You have the right to safe, considerate, and respectful care, provided in a manner consistent with your beliefs.’ ”
A former charge nurse added: “If a request for change was substantive (poor communication, perceived incompetence, trauma history, etc.), I would move mountains to accommodate it, but IMHO [in my humble opinion], the belief in honoring patient preference doesn’t necessarily need to include rearranging the world in order to accommodate racism, sexism, etc.”
Bias against female doctors, male nurses
Many commenters described how they gladly traded when a patient requested a practitioner of the opposite sex.
A female hospitalist related how she contacted the senior male doctor working with her to arrange a patient trade, adding, “I do agree that racial discrimination ought to be discouraged.”
Similarly, a male ICU RN commented: “Over 13 years, I have had a handful of female (usually older) patients request a female nurse. I have always strived to make this happen.”
However, an older woman related how at first she “had some bias against a male nurse touching me and also felt self-conscious,” she said. “So, I tried to relax ... and let him do his job. He was one of the most compassionate, kind, and sensitive nurses I’ve ever had.”
“I think in some cases,” she noted, “some women have had a history of some sort of abuse by a male, whether it’s sexual or psychological,” but in other cases, “it’s often just a personal preference, not a bias.”
A physician assistant (PA) who worked in a rural ED recounted how “there was only one physician and one PA on at any given evening/night shift, both usually White males.”
“Sometimes, you just have to cope as best you can with whomever is available, and in doing so,” he said, “they might just end up being pleasantly surprised.”
Don’t take it personally, move on
“If a patient doesn’t want to see me for whatever reason, then I would rather not treat them,” was a common sentiment.
Patients “should feel comfortable with their provider even if it’s with someone other than myself,” a reader wrote.
A female physician chimed in: “I frequently have older male patients refuse to see me. ... While this is irritating on several levels, I recognize that it is the patient’s choice, sigh, and move on to the next patient.”
“There are many more patients who specifically ask to see me, so I don’t waste my time and energy on being bothered by those who refuse.”
Similarly, a female mental health provider and sometimes patient wrote: “If any patient tells me that they prefer a male ... or someone of a particular race or religion or whatever, I don’t take it personally.”
A female Hispanic doctor chimed in: “Honestly, if a patient does not want to see me due to my race, I’m OK with that. Patients need to feel comfortable with me for the relationship to be therapeutic and effective,” she said.
“Forcing the patient to see me is adding injury to insult to ME! Not to mention increase[d] workload since that patient will take [so] much more time.”
Similarly, an Asian American doctor commented: “There are people who choose not to see me because of my ethnicity. However, I strongly believe that it should always be the patient’s preference. Whatever the reason, do not force the patient to see you in the name of Diversity, Equity, Inclusion, or whatever hurts your feeling. Let the patient go.”
Patient bias vs. patient preference
A physician referring to Dr. Francis’s experience suggested that “perhaps there was an opportunity to explore this misconception directly with the patient. If not, your supervising senior resident or attending should have been informed and brought into the process and conversation.”
“If/when I were rejected by a patient for whatever reason,” another physician commented, “I would gracefully accede, and hope that my colleague would tactfully point out to the patient their error.”
“Having a nurse ask the patient ... what they need style-wise (keeping race, gender, etc., out of it) might help identify whether or not the underlying issue(s) are based on style/needs mismatch match rather than bias,” a reader suggested.
A health care worker commented: “We generally assure patients that we are professionals and think nothing of situations that they might find uncomfortable, but don’t realize that our comfort does not translate to theirs.”
Maybe a different strategy is needed
“Having been the target of bias many times,” a reader said, “I understand the pain that is inflicted. Unfortunately, a patient bias policy, while a good idea, will not prevent patient bias. This is a much larger societal problem. But we can at least tell patients that it is not okay. On the other hand, I would not want to be the provider for a patient who was biased against me and held me in disdain.”
“I do not like Zero Tolerance policies ever. They are too absolute,” another reader commented. “Sometimes, there are reasons and we do have to listen to our patients for why. ... I do not think a policy of zero tolerance will fix the problem of racism.”
“Instead of trying to educate the general public about how not to be jerks,” another reader suggested, “perhaps it would be easier to provide elective classes for doctors and employees who believe themselves to be at-risk for discrimination, providing them with a ‘toolkit’ of strategies for responding to discrimination in the moment, processing it emotionally later on, and reporting the most egregious events through designated channels.”
Another commenter agreed and wrote that, “While we as doctors need and deserve protection, we are also called to act with compassion. So, rather than ask the system for ‘zero-tolerance’ in either direction, we could encourage our health systems to provide education, support, and mediation to any party who feels or fears that they are not being well served. Such a model would include support for physicians who have been the victims of bias and hurt.”
A version of this article originally appeared on Medscape.com.
Appendicitis more often missed in patients who are Black
This phenomenon, first described in children, occurs in adults as well, according to a study published in JAMA Surgery.
Some hospitals fare better than others: Those with more diverse patient populations were less likely to have missed the diagnosis, the researchers found.
“We don’t think the amount of melanin in your skin predicts how you present with appendicitis,” said Jonathan Carter, MD, professor of surgery at the University of California, San Francisco. “There’s no biological explanation,” Dr. Carter, who wrote an invited commentary on the research, said in an interview. “It’s really what’s going on in the social environment of those emergency rooms.”
For the study, Anne Stey, MD, assistant professor of surgery at Northwestern University in Chicago and her colleagues analyzed data from more than 80,000 men and women in four states – Florida, Maryland, New York, and Wisconsin – who underwent appendectomy in 2016-2017.
They identified those who had been seen for abdominal complaints at a hospital in the week before surgery but did not receive a diagnosis of appendicitis at that time, indicating a missed opportunity to intervene sooner.
Among Black patients, the proportion who had experienced this type of delay was 3.6%, whereas for White patients, it was 2.5%. For Hispanic patients, the share was 2.4%, while for Asian or Pacific Islander patients, the figure was 1.5%.
An analysis that controlled for patient and hospital variables found that among non-Hispanic Black patients, the rate of delayed diagnosis was 1.41 times higher than for non-Hispanic White patients (95% confidence interval, 1.21-1.63).
Other patient factors associated with delayed diagnosis included female sex, comorbidities, and living in a low-income zip code.
A key factor was where patients sought care. A delayed diagnosis of appendicitis was 3.51 times more likely for patients who went to hospitals where most patients are insured by Medicaid. Prior research has shown that “safety-net hospitals have fewer resources and may provide lower-quality care than hospitals with a larger private payer population,” Dr. Stey’s group writes.
On the other hand, going to a hospital with a more diverse patient population reduced the odds of a delayed diagnosis.
“Patients presenting to hospitals with a greater than 50% Black and Hispanic population were 0.73 (95% CI, 0.59-0.91) times less likely to have a delayed diagnosis, compared with patients presenting to hospitals with a less than 25% Black and Hispanic population,” the researchers report.
In the 30 days after discharge following appendectomy, Black patients returned to the hospital at a higher rate than White patients did (17.5% vs. 11.4%), indicating worse outcomes.
“Delayed diagnosis may account for some of the racial and ethnic disparities observed in outcomes after appendicitis,” according to the authors.
“It may be hospitals that are more used to serving racial-ethnic minority patients are better at diagnosing them, because they’re more culturally informed and have a better understanding of these patients,” Dr. Stey said in a news release about their findings.
Great masquerader
Diagnosing appendicitis can be challenging, Dr. Carter said. The early signs can be subtle, and the condition is sometimes called the great masquerader. It is not uncommon for patients to be diagnosed with gastroenteritis or pain associated with their menstrual period, for example, and sent home.
Scoring systems based on patients’ symptoms and liberal use of imaging have improved detection of appendicitis, but “no physician or health care system is perfect in the diagnosis,” he said.
The increased odds of delayed diagnosis for Black patients remained when the researchers focused on healthier patients who had fewer comorbidities, and it also held when they considered patients with private insurance in high-income areas, Dr. Carter noted.
“Once again, with this study we see the association of structural and systematic racism with access to health care, especially for Black patients, in emergency departments and hospitals,” he wrote. “We must redouble our efforts to become anti-racist in ourselves, our institutions, and our profession.”
‘Our health care system itself’
Elizabeth Garner, MD, MPH, a pharmaceutical executive who was not involved in the study, commented on Twitter that the study points to an underlying issue that has existed in medicine “for quite some time.”
“Minority populations are not taken as seriously as their white counterparts,” she wrote. “This needs to change.”
Measures of hospital quality need to be tied to health equity, according to Mofya Diallo, MD, MPH, of the department of anesthesiology at the Children’s Hospital Los Angeles and the University of Southern California, Los Angeles.
“Top hospitals should take pride in outcomes that do not vary based on race, income or literacy,” she tweeted in response to the study.
To better understand possible reasons for delayed diagnosis, future researchers could assess whether patients who are Black are less likely to receive a surgical consultation, imaging studies, or lab work, Dr. Carter told this news organization. He pointed to a recent analysis of patients insured by Medicare that found that Black patients were less likely than White patients to receive a surgical consultation after they were admitted with colorectal, general abdominal, hepatopancreatobiliary, intestinal obstruction, or upper gastrointestinal diagnoses.
While social determinants of health, such as income, education, housing, early childhood development, employment, and social inclusion, may account for a substantial portion of health outcomes, “Our health care system itself can be viewed as another social determinant of health,” Dr. Carter wrote. “Insurance coverage, health care professional availability, health care professional linguistic and cultural competency, and quality of care all have an effect on health outcomes.”
Dr. Stey was supported by grants from the American College of Surgeons and the National Institutes of Health.
A version of this article originally appeared on Medscape.com.
This phenomenon, first described in children, occurs in adults as well, according to a study published in JAMA Surgery.
Some hospitals fare better than others: Those with more diverse patient populations were less likely to have missed the diagnosis, the researchers found.
“We don’t think the amount of melanin in your skin predicts how you present with appendicitis,” said Jonathan Carter, MD, professor of surgery at the University of California, San Francisco. “There’s no biological explanation,” Dr. Carter, who wrote an invited commentary on the research, said in an interview. “It’s really what’s going on in the social environment of those emergency rooms.”
For the study, Anne Stey, MD, assistant professor of surgery at Northwestern University in Chicago and her colleagues analyzed data from more than 80,000 men and women in four states – Florida, Maryland, New York, and Wisconsin – who underwent appendectomy in 2016-2017.
They identified those who had been seen for abdominal complaints at a hospital in the week before surgery but did not receive a diagnosis of appendicitis at that time, indicating a missed opportunity to intervene sooner.
Among Black patients, the proportion who had experienced this type of delay was 3.6%, whereas for White patients, it was 2.5%. For Hispanic patients, the share was 2.4%, while for Asian or Pacific Islander patients, the figure was 1.5%.
An analysis that controlled for patient and hospital variables found that among non-Hispanic Black patients, the rate of delayed diagnosis was 1.41 times higher than for non-Hispanic White patients (95% confidence interval, 1.21-1.63).
Other patient factors associated with delayed diagnosis included female sex, comorbidities, and living in a low-income zip code.
A key factor was where patients sought care. A delayed diagnosis of appendicitis was 3.51 times more likely for patients who went to hospitals where most patients are insured by Medicaid. Prior research has shown that “safety-net hospitals have fewer resources and may provide lower-quality care than hospitals with a larger private payer population,” Dr. Stey’s group writes.
On the other hand, going to a hospital with a more diverse patient population reduced the odds of a delayed diagnosis.
“Patients presenting to hospitals with a greater than 50% Black and Hispanic population were 0.73 (95% CI, 0.59-0.91) times less likely to have a delayed diagnosis, compared with patients presenting to hospitals with a less than 25% Black and Hispanic population,” the researchers report.
In the 30 days after discharge following appendectomy, Black patients returned to the hospital at a higher rate than White patients did (17.5% vs. 11.4%), indicating worse outcomes.
“Delayed diagnosis may account for some of the racial and ethnic disparities observed in outcomes after appendicitis,” according to the authors.
“It may be hospitals that are more used to serving racial-ethnic minority patients are better at diagnosing them, because they’re more culturally informed and have a better understanding of these patients,” Dr. Stey said in a news release about their findings.
Great masquerader
Diagnosing appendicitis can be challenging, Dr. Carter said. The early signs can be subtle, and the condition is sometimes called the great masquerader. It is not uncommon for patients to be diagnosed with gastroenteritis or pain associated with their menstrual period, for example, and sent home.
Scoring systems based on patients’ symptoms and liberal use of imaging have improved detection of appendicitis, but “no physician or health care system is perfect in the diagnosis,” he said.
The increased odds of delayed diagnosis for Black patients remained when the researchers focused on healthier patients who had fewer comorbidities, and it also held when they considered patients with private insurance in high-income areas, Dr. Carter noted.
“Once again, with this study we see the association of structural and systematic racism with access to health care, especially for Black patients, in emergency departments and hospitals,” he wrote. “We must redouble our efforts to become anti-racist in ourselves, our institutions, and our profession.”
‘Our health care system itself’
Elizabeth Garner, MD, MPH, a pharmaceutical executive who was not involved in the study, commented on Twitter that the study points to an underlying issue that has existed in medicine “for quite some time.”
“Minority populations are not taken as seriously as their white counterparts,” she wrote. “This needs to change.”
Measures of hospital quality need to be tied to health equity, according to Mofya Diallo, MD, MPH, of the department of anesthesiology at the Children’s Hospital Los Angeles and the University of Southern California, Los Angeles.
“Top hospitals should take pride in outcomes that do not vary based on race, income or literacy,” she tweeted in response to the study.
To better understand possible reasons for delayed diagnosis, future researchers could assess whether patients who are Black are less likely to receive a surgical consultation, imaging studies, or lab work, Dr. Carter told this news organization. He pointed to a recent analysis of patients insured by Medicare that found that Black patients were less likely than White patients to receive a surgical consultation after they were admitted with colorectal, general abdominal, hepatopancreatobiliary, intestinal obstruction, or upper gastrointestinal diagnoses.
While social determinants of health, such as income, education, housing, early childhood development, employment, and social inclusion, may account for a substantial portion of health outcomes, “Our health care system itself can be viewed as another social determinant of health,” Dr. Carter wrote. “Insurance coverage, health care professional availability, health care professional linguistic and cultural competency, and quality of care all have an effect on health outcomes.”
Dr. Stey was supported by grants from the American College of Surgeons and the National Institutes of Health.
A version of this article originally appeared on Medscape.com.
This phenomenon, first described in children, occurs in adults as well, according to a study published in JAMA Surgery.
Some hospitals fare better than others: Those with more diverse patient populations were less likely to have missed the diagnosis, the researchers found.
“We don’t think the amount of melanin in your skin predicts how you present with appendicitis,” said Jonathan Carter, MD, professor of surgery at the University of California, San Francisco. “There’s no biological explanation,” Dr. Carter, who wrote an invited commentary on the research, said in an interview. “It’s really what’s going on in the social environment of those emergency rooms.”
For the study, Anne Stey, MD, assistant professor of surgery at Northwestern University in Chicago and her colleagues analyzed data from more than 80,000 men and women in four states – Florida, Maryland, New York, and Wisconsin – who underwent appendectomy in 2016-2017.
They identified those who had been seen for abdominal complaints at a hospital in the week before surgery but did not receive a diagnosis of appendicitis at that time, indicating a missed opportunity to intervene sooner.
Among Black patients, the proportion who had experienced this type of delay was 3.6%, whereas for White patients, it was 2.5%. For Hispanic patients, the share was 2.4%, while for Asian or Pacific Islander patients, the figure was 1.5%.
An analysis that controlled for patient and hospital variables found that among non-Hispanic Black patients, the rate of delayed diagnosis was 1.41 times higher than for non-Hispanic White patients (95% confidence interval, 1.21-1.63).
Other patient factors associated with delayed diagnosis included female sex, comorbidities, and living in a low-income zip code.
A key factor was where patients sought care. A delayed diagnosis of appendicitis was 3.51 times more likely for patients who went to hospitals where most patients are insured by Medicaid. Prior research has shown that “safety-net hospitals have fewer resources and may provide lower-quality care than hospitals with a larger private payer population,” Dr. Stey’s group writes.
On the other hand, going to a hospital with a more diverse patient population reduced the odds of a delayed diagnosis.
“Patients presenting to hospitals with a greater than 50% Black and Hispanic population were 0.73 (95% CI, 0.59-0.91) times less likely to have a delayed diagnosis, compared with patients presenting to hospitals with a less than 25% Black and Hispanic population,” the researchers report.
In the 30 days after discharge following appendectomy, Black patients returned to the hospital at a higher rate than White patients did (17.5% vs. 11.4%), indicating worse outcomes.
“Delayed diagnosis may account for some of the racial and ethnic disparities observed in outcomes after appendicitis,” according to the authors.
“It may be hospitals that are more used to serving racial-ethnic minority patients are better at diagnosing them, because they’re more culturally informed and have a better understanding of these patients,” Dr. Stey said in a news release about their findings.
Great masquerader
Diagnosing appendicitis can be challenging, Dr. Carter said. The early signs can be subtle, and the condition is sometimes called the great masquerader. It is not uncommon for patients to be diagnosed with gastroenteritis or pain associated with their menstrual period, for example, and sent home.
Scoring systems based on patients’ symptoms and liberal use of imaging have improved detection of appendicitis, but “no physician or health care system is perfect in the diagnosis,” he said.
The increased odds of delayed diagnosis for Black patients remained when the researchers focused on healthier patients who had fewer comorbidities, and it also held when they considered patients with private insurance in high-income areas, Dr. Carter noted.
“Once again, with this study we see the association of structural and systematic racism with access to health care, especially for Black patients, in emergency departments and hospitals,” he wrote. “We must redouble our efforts to become anti-racist in ourselves, our institutions, and our profession.”
‘Our health care system itself’
Elizabeth Garner, MD, MPH, a pharmaceutical executive who was not involved in the study, commented on Twitter that the study points to an underlying issue that has existed in medicine “for quite some time.”
“Minority populations are not taken as seriously as their white counterparts,” she wrote. “This needs to change.”
Measures of hospital quality need to be tied to health equity, according to Mofya Diallo, MD, MPH, of the department of anesthesiology at the Children’s Hospital Los Angeles and the University of Southern California, Los Angeles.
“Top hospitals should take pride in outcomes that do not vary based on race, income or literacy,” she tweeted in response to the study.
To better understand possible reasons for delayed diagnosis, future researchers could assess whether patients who are Black are less likely to receive a surgical consultation, imaging studies, or lab work, Dr. Carter told this news organization. He pointed to a recent analysis of patients insured by Medicare that found that Black patients were less likely than White patients to receive a surgical consultation after they were admitted with colorectal, general abdominal, hepatopancreatobiliary, intestinal obstruction, or upper gastrointestinal diagnoses.
While social determinants of health, such as income, education, housing, early childhood development, employment, and social inclusion, may account for a substantial portion of health outcomes, “Our health care system itself can be viewed as another social determinant of health,” Dr. Carter wrote. “Insurance coverage, health care professional availability, health care professional linguistic and cultural competency, and quality of care all have an effect on health outcomes.”
Dr. Stey was supported by grants from the American College of Surgeons and the National Institutes of Health.
A version of this article originally appeared on Medscape.com.
FROM JAMA SURGERY
New report says suicide rates rising among young Black people
Significant increases in suicide occurred among Native American, Black and Hispanic people, with a startling rise among young Black people. Meanwhile, the rate of suicide among older people declined between 2018 and 2021, the Centers for Disease Control and Prevention has reported.
In 2021, 48,183 people died by suicide in the United States, which equates to a suicide rate of 14.1 per 100,000 people. That level equals the 2018 suicide rate, which had seen a peak that was followed by declines associated with the pandemic.
Experts said rebounding suicide rates are common following times of crisis, such as the COVID-19 pandemic. Suicide declines have also occurred during times of war and natural disaster, when psychological resilience tends to increase and people work together to overcome shared adversity.
“That will wane, and then you will see rebounding in suicide rates. That is, in fact, what we feared would happen. And it has happened, at least in 2021,” Christine Moutier, MD, chief medical officer of the American Foundation for Suicide Prevention, told the New York Times.
The new CDC report found that the largest increase was among Black people aged 10-24 years, who experienced a 36.6% increase in suicide rate between 2018 and 2021. While Black people experience mental illness at the same rates as that of the general population, historically they have disproportionately limited access to mental health care, according to the American Psychiatric Association.
CDC report authors noted that some of the biggest increases in suicide rates occurred among groups most affected by the pandemic.
From 2018 to 2021, the suicide rate for people aged 25-44 increased among Native Americans by 33.7% and among Black people by 22.9%. Suicide increased among multiracial people by 20.6% and among Hispanic or Latinx people by 19.4%. Among White people of all ages, the suicide rate declined or remained steady.
“As the nation continues to respond to the short- and long-term impacts of the COVID-19 pandemic, remaining vigilant in prevention efforts is critical, especially among disproportionately affected populations where longer-term impacts might compound preexisting inequities in suicide risk,” the CDC researchers wrote.
A version of this article first appeared on WebMD.com.
Significant increases in suicide occurred among Native American, Black and Hispanic people, with a startling rise among young Black people. Meanwhile, the rate of suicide among older people declined between 2018 and 2021, the Centers for Disease Control and Prevention has reported.
In 2021, 48,183 people died by suicide in the United States, which equates to a suicide rate of 14.1 per 100,000 people. That level equals the 2018 suicide rate, which had seen a peak that was followed by declines associated with the pandemic.
Experts said rebounding suicide rates are common following times of crisis, such as the COVID-19 pandemic. Suicide declines have also occurred during times of war and natural disaster, when psychological resilience tends to increase and people work together to overcome shared adversity.
“That will wane, and then you will see rebounding in suicide rates. That is, in fact, what we feared would happen. And it has happened, at least in 2021,” Christine Moutier, MD, chief medical officer of the American Foundation for Suicide Prevention, told the New York Times.
The new CDC report found that the largest increase was among Black people aged 10-24 years, who experienced a 36.6% increase in suicide rate between 2018 and 2021. While Black people experience mental illness at the same rates as that of the general population, historically they have disproportionately limited access to mental health care, according to the American Psychiatric Association.
CDC report authors noted that some of the biggest increases in suicide rates occurred among groups most affected by the pandemic.
From 2018 to 2021, the suicide rate for people aged 25-44 increased among Native Americans by 33.7% and among Black people by 22.9%. Suicide increased among multiracial people by 20.6% and among Hispanic or Latinx people by 19.4%. Among White people of all ages, the suicide rate declined or remained steady.
“As the nation continues to respond to the short- and long-term impacts of the COVID-19 pandemic, remaining vigilant in prevention efforts is critical, especially among disproportionately affected populations where longer-term impacts might compound preexisting inequities in suicide risk,” the CDC researchers wrote.
A version of this article first appeared on WebMD.com.
Significant increases in suicide occurred among Native American, Black and Hispanic people, with a startling rise among young Black people. Meanwhile, the rate of suicide among older people declined between 2018 and 2021, the Centers for Disease Control and Prevention has reported.
In 2021, 48,183 people died by suicide in the United States, which equates to a suicide rate of 14.1 per 100,000 people. That level equals the 2018 suicide rate, which had seen a peak that was followed by declines associated with the pandemic.
Experts said rebounding suicide rates are common following times of crisis, such as the COVID-19 pandemic. Suicide declines have also occurred during times of war and natural disaster, when psychological resilience tends to increase and people work together to overcome shared adversity.
“That will wane, and then you will see rebounding in suicide rates. That is, in fact, what we feared would happen. And it has happened, at least in 2021,” Christine Moutier, MD, chief medical officer of the American Foundation for Suicide Prevention, told the New York Times.
The new CDC report found that the largest increase was among Black people aged 10-24 years, who experienced a 36.6% increase in suicide rate between 2018 and 2021. While Black people experience mental illness at the same rates as that of the general population, historically they have disproportionately limited access to mental health care, according to the American Psychiatric Association.
CDC report authors noted that some of the biggest increases in suicide rates occurred among groups most affected by the pandemic.
From 2018 to 2021, the suicide rate for people aged 25-44 increased among Native Americans by 33.7% and among Black people by 22.9%. Suicide increased among multiracial people by 20.6% and among Hispanic or Latinx people by 19.4%. Among White people of all ages, the suicide rate declined or remained steady.
“As the nation continues to respond to the short- and long-term impacts of the COVID-19 pandemic, remaining vigilant in prevention efforts is critical, especially among disproportionately affected populations where longer-term impacts might compound preexisting inequities in suicide risk,” the CDC researchers wrote.
A version of this article first appeared on WebMD.com.





