User login
What Patients Want to Know After Colorectal Surgery
Patients who have just had surgery for colorectal cancer may not be getting enough information at discharge, say researchers from Lund University in Sweden.
The researchers conducted 31 interviews with 16 patients during their first 7 weeks at home after surgery. A theme emerged from the interviews: trying to regain control in life by using information. That had several subthemes, such as needing more information on how to manage symptoms and self-care.
Related: Do Age and Gender Matter in Colorectal Cancer?
Patients lacked information on how long recovery would take, how to improve physical fitness, what to eat and drink, how bowel function and weight would be affected, and how to remove the sutures and care for the wound. Some patients were concerned about how to take medications and painkillers, and some received incorrect prescriptions.
Related: Colonoscopy Bowel Preparation Instructions
Researchers also found that patients wanted to take part in planning and preparation. Some patients compared the discharge process unfavorably with the preoperative preparation, which they described as being calmer, with easier-to-follow information. Patients also wanted straightforward information given as part of a mutual meeting, which was important in part because they closely observed health care practitioners’ facial expressions and intonation to determine whether anything was being withheld.
Lack of information added to patient worry about treatment and about their future. And having to wait without being told anything worsened worry for some patients. Even things like not having a promised appointment take place on time added to the anxiety and insecurity.
Related: Oxaliplatin-Induced Lhermitte Sign
The researchers acknowledge that not all patients want information, or they want it later in the trajectory of the disease and recovery stages. But when patients do seek information, they may choose untrustworthy sources. The onus is on the health care professionals, the researchers say, to provide person-centered care with easily accessible information for all patients, even those who might wish to avoid it.
Source
Lithner M, Klefsgard R, Johannson J, Andersson E. BMC Nurse. 2015;14:36.
doi: 10.1186/s12912-015-0086-6.
Patients who have just had surgery for colorectal cancer may not be getting enough information at discharge, say researchers from Lund University in Sweden.
The researchers conducted 31 interviews with 16 patients during their first 7 weeks at home after surgery. A theme emerged from the interviews: trying to regain control in life by using information. That had several subthemes, such as needing more information on how to manage symptoms and self-care.
Related: Do Age and Gender Matter in Colorectal Cancer?
Patients lacked information on how long recovery would take, how to improve physical fitness, what to eat and drink, how bowel function and weight would be affected, and how to remove the sutures and care for the wound. Some patients were concerned about how to take medications and painkillers, and some received incorrect prescriptions.
Related: Colonoscopy Bowel Preparation Instructions
Researchers also found that patients wanted to take part in planning and preparation. Some patients compared the discharge process unfavorably with the preoperative preparation, which they described as being calmer, with easier-to-follow information. Patients also wanted straightforward information given as part of a mutual meeting, which was important in part because they closely observed health care practitioners’ facial expressions and intonation to determine whether anything was being withheld.
Lack of information added to patient worry about treatment and about their future. And having to wait without being told anything worsened worry for some patients. Even things like not having a promised appointment take place on time added to the anxiety and insecurity.
Related: Oxaliplatin-Induced Lhermitte Sign
The researchers acknowledge that not all patients want information, or they want it later in the trajectory of the disease and recovery stages. But when patients do seek information, they may choose untrustworthy sources. The onus is on the health care professionals, the researchers say, to provide person-centered care with easily accessible information for all patients, even those who might wish to avoid it.
Source
Lithner M, Klefsgard R, Johannson J, Andersson E. BMC Nurse. 2015;14:36.
doi: 10.1186/s12912-015-0086-6.
Patients who have just had surgery for colorectal cancer may not be getting enough information at discharge, say researchers from Lund University in Sweden.
The researchers conducted 31 interviews with 16 patients during their first 7 weeks at home after surgery. A theme emerged from the interviews: trying to regain control in life by using information. That had several subthemes, such as needing more information on how to manage symptoms and self-care.
Related: Do Age and Gender Matter in Colorectal Cancer?
Patients lacked information on how long recovery would take, how to improve physical fitness, what to eat and drink, how bowel function and weight would be affected, and how to remove the sutures and care for the wound. Some patients were concerned about how to take medications and painkillers, and some received incorrect prescriptions.
Related: Colonoscopy Bowel Preparation Instructions
Researchers also found that patients wanted to take part in planning and preparation. Some patients compared the discharge process unfavorably with the preoperative preparation, which they described as being calmer, with easier-to-follow information. Patients also wanted straightforward information given as part of a mutual meeting, which was important in part because they closely observed health care practitioners’ facial expressions and intonation to determine whether anything was being withheld.
Lack of information added to patient worry about treatment and about their future. And having to wait without being told anything worsened worry for some patients. Even things like not having a promised appointment take place on time added to the anxiety and insecurity.
Related: Oxaliplatin-Induced Lhermitte Sign
The researchers acknowledge that not all patients want information, or they want it later in the trajectory of the disease and recovery stages. But when patients do seek information, they may choose untrustworthy sources. The onus is on the health care professionals, the researchers say, to provide person-centered care with easily accessible information for all patients, even those who might wish to avoid it.
Source
Lithner M, Klefsgard R, Johannson J, Andersson E. BMC Nurse. 2015;14:36.
doi: 10.1186/s12912-015-0086-6.
Managing Malignant Bowel Obstruction
There are several relevant strategies for patients with cancer who have malignant bowel obstruction. According to Jocelyn White, MD, strategies for management must be based on patient characteristics, current cancer treatment, and care goals.
“For hospice and palliative patients, we start by treating the reversible causes,” Dr. White said. “The first thing you do when you suspect obstruction is to try to treat for pseudo-obstruction. I can’t tell you how many times we have gotten patients referred to us for complete malignant bowel obstruction who actually are constipated or obstipated.”
There are several relevant strategies for patients with cancer who have malignant bowel obstruction. According to Jocelyn White, MD, strategies for management must be based on patient characteristics, current cancer treatment, and care goals.
“For hospice and palliative patients, we start by treating the reversible causes,” Dr. White said. “The first thing you do when you suspect obstruction is to try to treat for pseudo-obstruction. I can’t tell you how many times we have gotten patients referred to us for complete malignant bowel obstruction who actually are constipated or obstipated.”
There are several relevant strategies for patients with cancer who have malignant bowel obstruction. According to Jocelyn White, MD, strategies for management must be based on patient characteristics, current cancer treatment, and care goals.
“For hospice and palliative patients, we start by treating the reversible causes,” Dr. White said. “The first thing you do when you suspect obstruction is to try to treat for pseudo-obstruction. I can’t tell you how many times we have gotten patients referred to us for complete malignant bowel obstruction who actually are constipated or obstipated.”
Elective colectomy topped medical therapy for advanced ulcerative colitis
For adults with advanced ulcerative colitis (UC) older than 50 years of age, elective colectomy offered a significantly higher survival rate than did medical therapy, according to a retrospective study of 8,371 patients.
Dr. Meenakshi Bewtra of the University of Pennsylvania, Philadelphia, and her coinvestigators matched 830 UC patients seeking elective colectomy for treatment with 7,541 UC patients opting for more traditional medical therapy, all recruited using data from Medicaid and Medicare from 2000 to 2011 (Ann. Intern. Med. July 14, 2015 [doi:10.7326/M14-0960]).
In total, 63 patients who received elective colectomy died, compared with 783 patients in the medical therapy cohort. Mortality rates per cohort were 34 and 54 per 1,000 person-years, respectively. Furthermore, patients were more likely to respond more favorably to elective colectomy than to medical therapy, with an adjusted hazard ratio of 0.67. Additional post hoc analysis revealed higher survival odds with colectomy for patients age 50 years or older (HR, 0.60; P = .032). “These findings warrant discussion with patients when one is weighing the risks and benefits of different medical therapies and total colectomy,” the investigators said.
The authors noted that the study had several limitations, such as potential residual confounding and the possibility of reduced statistical power in subsequent analyses because several databases were used to cull data.
The study was funded by grants from the National Institutes of Health and the Agency for Healthcare Research and Quality. Dr. Bewtra disclosed receiving a grant from NIH and accepting speaking engagements for Imedex and the Crohn’s & Colitis Foundation of America/Robert Michael Educational Institute outside the submitted work.
For adults with advanced ulcerative colitis (UC) older than 50 years of age, elective colectomy offered a significantly higher survival rate than did medical therapy, according to a retrospective study of 8,371 patients.
Dr. Meenakshi Bewtra of the University of Pennsylvania, Philadelphia, and her coinvestigators matched 830 UC patients seeking elective colectomy for treatment with 7,541 UC patients opting for more traditional medical therapy, all recruited using data from Medicaid and Medicare from 2000 to 2011 (Ann. Intern. Med. July 14, 2015 [doi:10.7326/M14-0960]).
In total, 63 patients who received elective colectomy died, compared with 783 patients in the medical therapy cohort. Mortality rates per cohort were 34 and 54 per 1,000 person-years, respectively. Furthermore, patients were more likely to respond more favorably to elective colectomy than to medical therapy, with an adjusted hazard ratio of 0.67. Additional post hoc analysis revealed higher survival odds with colectomy for patients age 50 years or older (HR, 0.60; P = .032). “These findings warrant discussion with patients when one is weighing the risks and benefits of different medical therapies and total colectomy,” the investigators said.
The authors noted that the study had several limitations, such as potential residual confounding and the possibility of reduced statistical power in subsequent analyses because several databases were used to cull data.
The study was funded by grants from the National Institutes of Health and the Agency for Healthcare Research and Quality. Dr. Bewtra disclosed receiving a grant from NIH and accepting speaking engagements for Imedex and the Crohn’s & Colitis Foundation of America/Robert Michael Educational Institute outside the submitted work.
For adults with advanced ulcerative colitis (UC) older than 50 years of age, elective colectomy offered a significantly higher survival rate than did medical therapy, according to a retrospective study of 8,371 patients.
Dr. Meenakshi Bewtra of the University of Pennsylvania, Philadelphia, and her coinvestigators matched 830 UC patients seeking elective colectomy for treatment with 7,541 UC patients opting for more traditional medical therapy, all recruited using data from Medicaid and Medicare from 2000 to 2011 (Ann. Intern. Med. July 14, 2015 [doi:10.7326/M14-0960]).
In total, 63 patients who received elective colectomy died, compared with 783 patients in the medical therapy cohort. Mortality rates per cohort were 34 and 54 per 1,000 person-years, respectively. Furthermore, patients were more likely to respond more favorably to elective colectomy than to medical therapy, with an adjusted hazard ratio of 0.67. Additional post hoc analysis revealed higher survival odds with colectomy for patients age 50 years or older (HR, 0.60; P = .032). “These findings warrant discussion with patients when one is weighing the risks and benefits of different medical therapies and total colectomy,” the investigators said.
The authors noted that the study had several limitations, such as potential residual confounding and the possibility of reduced statistical power in subsequent analyses because several databases were used to cull data.
The study was funded by grants from the National Institutes of Health and the Agency for Healthcare Research and Quality. Dr. Bewtra disclosed receiving a grant from NIH and accepting speaking engagements for Imedex and the Crohn’s & Colitis Foundation of America/Robert Michael Educational Institute outside the submitted work.
FROM THE ANNALS OF INTERNAL MEDICINE
Resection margin correlates with survival in CRC liver metastases
SAN DIEGO – Clear resection margins, no matter how narrow, are associated with increased survival when surgeons excise liver tumors from metastatic colorectal cancer (MCRC).
When colorectal cancer metastasizes to the liver, tumor resection can be a safe intervention that improves long-term survival and contributes to cure. Previous studies have shown that any amount of negative margin had a positive impact on overall survival, but these smaller studies were hampered by lack of uniformity in definitions and in surgical technique. Additionally, new developments in chemotherapy have changed the treatment course and overall survival for those with MCRC and need to be taken into account.
Dr. Michael D’Angelica and his colleagues at Memorial Sloan Kettering Cancer Center, New York, presented findings from a large, single-center cohort of patients with MCRC at the annual meeting of the American Surgical Association. The aims of the study, he said, were to analyze the association between margin width of tumor resection and survival in an updated cohort receiving modern therapies, and to account for potentially confounding factors.
The study included 2,368 patients who had hepatic resection for MCRC from 1992 to 2012; patients had the same liver transection method and had high-resolution microscopic pathologic measurement of tumor margins, which allowed submillimeter assessment of margin width. Dr. D’Angelica said that the study captured clinical and patient characteristics, including the number and size of tumors, clinical risk scores, and the presence of any extrahepatic disease.
About half of all patients (n = 1,191) had tumor margins between 1 and 9 mm; one-third (n = 765) had tumor margins of 10 mm or more. One in 10 patients (n = 245) had positive tumor margins, while the remaining 7% (n = 160) had negative tumor margins of 0.9 mm or less.
The study cohort was followed for a median 55 months; a significant relationship between margin width and survival emerged, with all negative margins widths being associated with significantly longer overall survival than the survival curve for those with positive margins (P < .01). This was true even for the narrowest margin widths. Factors associated with submillimeter tumor margins included tumor ablation, having more than three tumors, or tumor size over 5 cm.
Survival differences seen with submillimeter differences in tumor margin are likely attributable to currently unknown tumor growth properties, rather than actual margin width, Dr. D’Angelica said. In response to a question from Dr. Jean-Nicolas Vauthey of MD Anderson Cancer Center, Houston, Dr. D’Angelica speculated that the future of treating MCRC may rely on microscopic determination of tumor growth patterns, as well as better understanding of underlying gene patterns.
“Negative histologic margins, at all widths, including submillimeter margins, are independently associated with improved overall survival,” said Dr. D’Angelica. A significant difference was seen between patients with positive margins and any negative margin width, and between patients with submillimeter vs. 1 mm or greater margins. Beyond 1 mm, however, increasing margins widths were not associated with increased survival benefit.
Dr. D’Angelica noted that surgeons should not fear that a surgery with anticipated close margins would not benefit the patient, since any amount of clear margin confers a survival benefit. Wide margins, however, should be attempted when the approach is safe and feasible because it is the best-known technical approach to ensure a negative tumor margin. Very narrow margins, he noted, are probably a marker for an unknown biological factor rather than a true reflection of surgical technique.
The authors reported no disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – Clear resection margins, no matter how narrow, are associated with increased survival when surgeons excise liver tumors from metastatic colorectal cancer (MCRC).
When colorectal cancer metastasizes to the liver, tumor resection can be a safe intervention that improves long-term survival and contributes to cure. Previous studies have shown that any amount of negative margin had a positive impact on overall survival, but these smaller studies were hampered by lack of uniformity in definitions and in surgical technique. Additionally, new developments in chemotherapy have changed the treatment course and overall survival for those with MCRC and need to be taken into account.
Dr. Michael D’Angelica and his colleagues at Memorial Sloan Kettering Cancer Center, New York, presented findings from a large, single-center cohort of patients with MCRC at the annual meeting of the American Surgical Association. The aims of the study, he said, were to analyze the association between margin width of tumor resection and survival in an updated cohort receiving modern therapies, and to account for potentially confounding factors.
The study included 2,368 patients who had hepatic resection for MCRC from 1992 to 2012; patients had the same liver transection method and had high-resolution microscopic pathologic measurement of tumor margins, which allowed submillimeter assessment of margin width. Dr. D’Angelica said that the study captured clinical and patient characteristics, including the number and size of tumors, clinical risk scores, and the presence of any extrahepatic disease.
About half of all patients (n = 1,191) had tumor margins between 1 and 9 mm; one-third (n = 765) had tumor margins of 10 mm or more. One in 10 patients (n = 245) had positive tumor margins, while the remaining 7% (n = 160) had negative tumor margins of 0.9 mm or less.
The study cohort was followed for a median 55 months; a significant relationship between margin width and survival emerged, with all negative margins widths being associated with significantly longer overall survival than the survival curve for those with positive margins (P < .01). This was true even for the narrowest margin widths. Factors associated with submillimeter tumor margins included tumor ablation, having more than three tumors, or tumor size over 5 cm.
Survival differences seen with submillimeter differences in tumor margin are likely attributable to currently unknown tumor growth properties, rather than actual margin width, Dr. D’Angelica said. In response to a question from Dr. Jean-Nicolas Vauthey of MD Anderson Cancer Center, Houston, Dr. D’Angelica speculated that the future of treating MCRC may rely on microscopic determination of tumor growth patterns, as well as better understanding of underlying gene patterns.
“Negative histologic margins, at all widths, including submillimeter margins, are independently associated with improved overall survival,” said Dr. D’Angelica. A significant difference was seen between patients with positive margins and any negative margin width, and between patients with submillimeter vs. 1 mm or greater margins. Beyond 1 mm, however, increasing margins widths were not associated with increased survival benefit.
Dr. D’Angelica noted that surgeons should not fear that a surgery with anticipated close margins would not benefit the patient, since any amount of clear margin confers a survival benefit. Wide margins, however, should be attempted when the approach is safe and feasible because it is the best-known technical approach to ensure a negative tumor margin. Very narrow margins, he noted, are probably a marker for an unknown biological factor rather than a true reflection of surgical technique.
The authors reported no disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – Clear resection margins, no matter how narrow, are associated with increased survival when surgeons excise liver tumors from metastatic colorectal cancer (MCRC).
When colorectal cancer metastasizes to the liver, tumor resection can be a safe intervention that improves long-term survival and contributes to cure. Previous studies have shown that any amount of negative margin had a positive impact on overall survival, but these smaller studies were hampered by lack of uniformity in definitions and in surgical technique. Additionally, new developments in chemotherapy have changed the treatment course and overall survival for those with MCRC and need to be taken into account.
Dr. Michael D’Angelica and his colleagues at Memorial Sloan Kettering Cancer Center, New York, presented findings from a large, single-center cohort of patients with MCRC at the annual meeting of the American Surgical Association. The aims of the study, he said, were to analyze the association between margin width of tumor resection and survival in an updated cohort receiving modern therapies, and to account for potentially confounding factors.
The study included 2,368 patients who had hepatic resection for MCRC from 1992 to 2012; patients had the same liver transection method and had high-resolution microscopic pathologic measurement of tumor margins, which allowed submillimeter assessment of margin width. Dr. D’Angelica said that the study captured clinical and patient characteristics, including the number and size of tumors, clinical risk scores, and the presence of any extrahepatic disease.
About half of all patients (n = 1,191) had tumor margins between 1 and 9 mm; one-third (n = 765) had tumor margins of 10 mm or more. One in 10 patients (n = 245) had positive tumor margins, while the remaining 7% (n = 160) had negative tumor margins of 0.9 mm or less.
The study cohort was followed for a median 55 months; a significant relationship between margin width and survival emerged, with all negative margins widths being associated with significantly longer overall survival than the survival curve for those with positive margins (P < .01). This was true even for the narrowest margin widths. Factors associated with submillimeter tumor margins included tumor ablation, having more than three tumors, or tumor size over 5 cm.
Survival differences seen with submillimeter differences in tumor margin are likely attributable to currently unknown tumor growth properties, rather than actual margin width, Dr. D’Angelica said. In response to a question from Dr. Jean-Nicolas Vauthey of MD Anderson Cancer Center, Houston, Dr. D’Angelica speculated that the future of treating MCRC may rely on microscopic determination of tumor growth patterns, as well as better understanding of underlying gene patterns.
“Negative histologic margins, at all widths, including submillimeter margins, are independently associated with improved overall survival,” said Dr. D’Angelica. A significant difference was seen between patients with positive margins and any negative margin width, and between patients with submillimeter vs. 1 mm or greater margins. Beyond 1 mm, however, increasing margins widths were not associated with increased survival benefit.
Dr. D’Angelica noted that surgeons should not fear that a surgery with anticipated close margins would not benefit the patient, since any amount of clear margin confers a survival benefit. Wide margins, however, should be attempted when the approach is safe and feasible because it is the best-known technical approach to ensure a negative tumor margin. Very narrow margins, he noted, are probably a marker for an unknown biological factor rather than a true reflection of surgical technique.
The authors reported no disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: Negative margins of any size improve overall survival in liver metastases from colorectal cancer.
Major findings: Overall survival for individuals with liver metastases from colorectal cancer was correlated with tumor resection margins, with improved survival seen for all groups, compared with those who had tumor cells at the resection margin (P < .001).
Data source: Single-institution, prospectively collected database of patients (n = 2,368) undergoing resection for colorectal liver metastases.
Disclosures: The authors reported no disclosures.
ASA: Bowel prep, oral antibiotics cut postop colorectal complications
SAN DIEGO – A combination of bowel cleansing and oral antibiotics nearly halved the risk of common and troublesome complications in colorectal surgery. Infections, leaks, and postsurgical ileus were all significantly less likely with the combined regime, according to a study reported at the annual meeting of the American Surgical Association.
Patients preparing for colorectal surgery routinely received mechanical bowel preparation in combination with oral antibiotics in the 1970s. However, since then, the availability of IV antibiotics combined with concerns about complications from bowel preparation have contributed to a decline in use of the regime. Consensus is lacking about best practices for preparation for colorectal surgery.
Dr. P. Ravi Kiran, chief and program director of Columbia University Medical Center’s division of colorectal surgery, presented findings from a large retrospective study that addressed whether oral antibiotics and mechanical bowel preparation reduced the risk of complications from colorectal surgery. Drawing from targeted colectomy data, available from 2012 onward through the large American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database, Dr. Kiran and associates compared three groups of patients undergoing elective colectomy. Of the total 8,644 patients, 2,498 (28.9%) received no preparation, 3,822 (44.2%) received mechanical bowel preparation alone, and 2,324 (26.9%) received both oral antibiotics and mechanical bowel preparation.
Primary outcome measures included the presence of anastomotic leak from the surgery, surgical site infections, ileus, and all-cause mortality. The patients were well matched by age and gender, and surgery type; case complexity and degree of resident physician involvement in the surgical procedures were also similar between arms.
On multivariable analysis, patients who received mechanical bowel preparation and oral antibiotics were significantly less likely to have surgical site infections (odds ratio, 0.43), to sustain ileus (OR, 0.71), or to have anastomotic leak (OR, 0.56). Postoperatively, those who had received no bowel preparation were also significantly more likely to have pneumonia, to require reintubation, and to fail to wean from the ventilator. They also were more likely to have deep vein thrombosis and sepsis. All-cause 30-day mortality was also significantly less likely in the group receiving both bowel preparation and oral antibiotics.
Dr. Kiran noted that investigators were not able to determine the type of mechanical bowel preparation patients received, and likely could not control for all confounders.
Discussant Dr. Heidi Nelson of the Mayo Clinic, Rochester, Minn., noted that despite the study’s strengths, including its large size and the real-world nature of the investigation, she doubts that the study will be considered definitive. Limitations that critics might point out, she noted, are the retrospective nature of the study and the possibility that the three groups studied were not really comparable because of subtle selection biases on the part of the treating surgeons. Dr. Kiran conceded that though multivariable analysis attempted to account and control for as many between-group differences as they could identify, differences probably did persist.
Dr. Hiram Polk of the University of Louisville (Ky.) commented that studies such as these using massive databases, though they may show what is true, may not always point to what is clinically relevant. Overall, it’s been shown that about one in four patients given systemic antibiotics are given the wrong drug, he said; further, “the only place you can truly sterilize a colon is in an autoclave.” Dr. Kiran did note that the combined oral preparation regime was successful in reducing the incidence of the most common complications by about 50%.
Following with more real-world observations, Dr. Mary Otterson of the Medical College of Wisconsin, Milwaukee, commented that the effective dose of preoperative erythromycin is very close to doses that cause significant nausea and vomiting. In her experience, “If we went any higher, they vomited. We also had unplanned admits with electrolyte abnormalities.” The best-tolerated and most effective regime, she said, should be identified by a prospective, randomized, controlled trial.
The authors reported no conflicts of interest.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – A combination of bowel cleansing and oral antibiotics nearly halved the risk of common and troublesome complications in colorectal surgery. Infections, leaks, and postsurgical ileus were all significantly less likely with the combined regime, according to a study reported at the annual meeting of the American Surgical Association.
Patients preparing for colorectal surgery routinely received mechanical bowel preparation in combination with oral antibiotics in the 1970s. However, since then, the availability of IV antibiotics combined with concerns about complications from bowel preparation have contributed to a decline in use of the regime. Consensus is lacking about best practices for preparation for colorectal surgery.
Dr. P. Ravi Kiran, chief and program director of Columbia University Medical Center’s division of colorectal surgery, presented findings from a large retrospective study that addressed whether oral antibiotics and mechanical bowel preparation reduced the risk of complications from colorectal surgery. Drawing from targeted colectomy data, available from 2012 onward through the large American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database, Dr. Kiran and associates compared three groups of patients undergoing elective colectomy. Of the total 8,644 patients, 2,498 (28.9%) received no preparation, 3,822 (44.2%) received mechanical bowel preparation alone, and 2,324 (26.9%) received both oral antibiotics and mechanical bowel preparation.
Primary outcome measures included the presence of anastomotic leak from the surgery, surgical site infections, ileus, and all-cause mortality. The patients were well matched by age and gender, and surgery type; case complexity and degree of resident physician involvement in the surgical procedures were also similar between arms.
On multivariable analysis, patients who received mechanical bowel preparation and oral antibiotics were significantly less likely to have surgical site infections (odds ratio, 0.43), to sustain ileus (OR, 0.71), or to have anastomotic leak (OR, 0.56). Postoperatively, those who had received no bowel preparation were also significantly more likely to have pneumonia, to require reintubation, and to fail to wean from the ventilator. They also were more likely to have deep vein thrombosis and sepsis. All-cause 30-day mortality was also significantly less likely in the group receiving both bowel preparation and oral antibiotics.
Dr. Kiran noted that investigators were not able to determine the type of mechanical bowel preparation patients received, and likely could not control for all confounders.
Discussant Dr. Heidi Nelson of the Mayo Clinic, Rochester, Minn., noted that despite the study’s strengths, including its large size and the real-world nature of the investigation, she doubts that the study will be considered definitive. Limitations that critics might point out, she noted, are the retrospective nature of the study and the possibility that the three groups studied were not really comparable because of subtle selection biases on the part of the treating surgeons. Dr. Kiran conceded that though multivariable analysis attempted to account and control for as many between-group differences as they could identify, differences probably did persist.
Dr. Hiram Polk of the University of Louisville (Ky.) commented that studies such as these using massive databases, though they may show what is true, may not always point to what is clinically relevant. Overall, it’s been shown that about one in four patients given systemic antibiotics are given the wrong drug, he said; further, “the only place you can truly sterilize a colon is in an autoclave.” Dr. Kiran did note that the combined oral preparation regime was successful in reducing the incidence of the most common complications by about 50%.
Following with more real-world observations, Dr. Mary Otterson of the Medical College of Wisconsin, Milwaukee, commented that the effective dose of preoperative erythromycin is very close to doses that cause significant nausea and vomiting. In her experience, “If we went any higher, they vomited. We also had unplanned admits with electrolyte abnormalities.” The best-tolerated and most effective regime, she said, should be identified by a prospective, randomized, controlled trial.
The authors reported no conflicts of interest.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – A combination of bowel cleansing and oral antibiotics nearly halved the risk of common and troublesome complications in colorectal surgery. Infections, leaks, and postsurgical ileus were all significantly less likely with the combined regime, according to a study reported at the annual meeting of the American Surgical Association.
Patients preparing for colorectal surgery routinely received mechanical bowel preparation in combination with oral antibiotics in the 1970s. However, since then, the availability of IV antibiotics combined with concerns about complications from bowel preparation have contributed to a decline in use of the regime. Consensus is lacking about best practices for preparation for colorectal surgery.
Dr. P. Ravi Kiran, chief and program director of Columbia University Medical Center’s division of colorectal surgery, presented findings from a large retrospective study that addressed whether oral antibiotics and mechanical bowel preparation reduced the risk of complications from colorectal surgery. Drawing from targeted colectomy data, available from 2012 onward through the large American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database, Dr. Kiran and associates compared three groups of patients undergoing elective colectomy. Of the total 8,644 patients, 2,498 (28.9%) received no preparation, 3,822 (44.2%) received mechanical bowel preparation alone, and 2,324 (26.9%) received both oral antibiotics and mechanical bowel preparation.
Primary outcome measures included the presence of anastomotic leak from the surgery, surgical site infections, ileus, and all-cause mortality. The patients were well matched by age and gender, and surgery type; case complexity and degree of resident physician involvement in the surgical procedures were also similar between arms.
On multivariable analysis, patients who received mechanical bowel preparation and oral antibiotics were significantly less likely to have surgical site infections (odds ratio, 0.43), to sustain ileus (OR, 0.71), or to have anastomotic leak (OR, 0.56). Postoperatively, those who had received no bowel preparation were also significantly more likely to have pneumonia, to require reintubation, and to fail to wean from the ventilator. They also were more likely to have deep vein thrombosis and sepsis. All-cause 30-day mortality was also significantly less likely in the group receiving both bowel preparation and oral antibiotics.
Dr. Kiran noted that investigators were not able to determine the type of mechanical bowel preparation patients received, and likely could not control for all confounders.
Discussant Dr. Heidi Nelson of the Mayo Clinic, Rochester, Minn., noted that despite the study’s strengths, including its large size and the real-world nature of the investigation, she doubts that the study will be considered definitive. Limitations that critics might point out, she noted, are the retrospective nature of the study and the possibility that the three groups studied were not really comparable because of subtle selection biases on the part of the treating surgeons. Dr. Kiran conceded that though multivariable analysis attempted to account and control for as many between-group differences as they could identify, differences probably did persist.
Dr. Hiram Polk of the University of Louisville (Ky.) commented that studies such as these using massive databases, though they may show what is true, may not always point to what is clinically relevant. Overall, it’s been shown that about one in four patients given systemic antibiotics are given the wrong drug, he said; further, “the only place you can truly sterilize a colon is in an autoclave.” Dr. Kiran did note that the combined oral preparation regime was successful in reducing the incidence of the most common complications by about 50%.
Following with more real-world observations, Dr. Mary Otterson of the Medical College of Wisconsin, Milwaukee, commented that the effective dose of preoperative erythromycin is very close to doses that cause significant nausea and vomiting. In her experience, “If we went any higher, they vomited. We also had unplanned admits with electrolyte abnormalities.” The best-tolerated and most effective regime, she said, should be identified by a prospective, randomized, controlled trial.
The authors reported no conflicts of interest.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: A combination of mechanical cleansing and oral antibiotics reduced major colorectal surgery complications by nearly one-half.
Major findings: Mechanical bowel preparation combined with oral antibiotics resulted in reduced colorectal surgery complications, with odds ratios of 0.43 for surgical site infections, 0.71 for ileus, and 0.56 for anastomotic leak; overall mortality was also reduced.
Data source: Retrospective multivariable analysis of data for 8,644 surgical patients undergoing elective colorectal resection in 2012; targeted colectomy data drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database.
Disclosures: The authors reported no conflicts of interest.
Ileal pouch re-dos successful in most patients
SAN DIEGO – Patients hoping to avoid a permanent stoma by having a salvage surgery to repair or replace a failing ileal pouch–anal anastomosis (IPAA) achieved good functional outcomes and quality of life in one institution’s long-term experience.
A large case series drawn from IPAA re-dos at the Cleveland Clinic over a 20-year span showed that the procedure was successful for four in five patients, and more than 90% were satisfied with their quality of life, despite some functional limitations. Dr. Feza Remzi, chairman of the department of colorectal surgery at the Cleveland Clinic, presented findings from 500 patients undergoing IPAA re-dos via the transabdominal approach. In this group, 80% (401) of transabdominally revised IPAAs were successful.
IPAA is a procedure indicated for patients with Crohn’s disease, ulcerative or indeterminate colitis, or familial adenomatous polyposis. The surgery preserves the capacity for anal defecation with intestinal continuity after proctocolectomy by fashioning a reservoir for stool from the small intestine. However, up to 15% of patients will have pouch failure, necessitating a permanent stoma unless the pouch is surgically revised, he said at the annual meeting of the American Surgical Association.
To determine outcomes for patients having a re-do of a failed IPAA, Dr. Remzi and colleagues assessed 502 IPAA re-do patients (215, male; median age, 38 years) who received their procedure at the Cleveland Clinic from 1983 to 2014. Crohn’s disease was the primary diagnosis for 419 patients (84%); just over half (n = 263) had anastomotic leak or fistula as the cause of first pouch failure, followed by pouch-vaginal fistula in 85 women (17%) and obstruction in 116 patients (23%).
The primary endpoints of the study were surgery morbidity, how many patients had a functioning pouch after re-do, pouch function, and quality of life.
Surgeon discretion dictated whether the pouch was revised, as it was in 295 patients (59%), or whether a new pouch was created. Overall, just over half of patients (n = 270) had postoperative complications, though there were no short-term deaths. Ileus and pelvic sepsis were the most common short-term complications, occurring in 81 (16%) and 50 (10%) patients, respectively. All of the other complications occurred in less than 10% of patients. Patients stayed in the hospital a median of 7 days, and 63 (13%) were readmitted.
Over the duration of the study, 101 patients (20%) had failure of their redone IPAA pouches, and pelvis sepsis and anastomotic stricture each occurred in more than 10% of patients. Short-term postoperative morbidity and occurrence of pelvic sepsis at any point after re-do surgery were associated with failure of the redone IPAA based on a Cox regression model (P = .035 and P < .0001, respectively).
Patients were overall very satisfied with their quality of life after IPAA re-do surgery; 92% of the 261 respondents said they would undergo the surgery again, and 93% would recommend the surgery. This was true although patients reported a mean of six daytime bowel movements, about half of patients reported having stool seepage or requiring pad use, and a third of patients reported dietary restrictions related to their bowel function.
Study limitations included the lack of information regarding patients in whom the re-do attempt was abandoned, or for those referred for surgery who did not have an IPAA re-do. Another limitation was the relatively low number of patients who completed all items on the function and quality of life questionnaires; investigators decided that the most robust analysis would flow from including only data for those who had completed all forms.
Discussion focused on the real-world and technical aspects of lessons learned from this large single-institution data set. Dr. David Rothenberger, Jay Phillips Professor and Chair of the department of surgery at the University of Minnesota, Minneapolis, asked whether patients had been carefully selected for this salvage procedure. In his experience, he said, obese patients or those with a heavily muscled pelvis, as well as those with a significant history of prior pelvic infections, would not necessarily be good candidates for a re-do. He suggested that an intention-to-treat analysis might give a truer denominator, and might even change the conclusion that the salvage surgery has a high likelihood of success. Dr. Remzi agreed that obesity or a high body mass index in a patient “is a very good reason not to do the surgery.”
Dr. Neil Hyman, codirector of the digestive diseases center at the University of Chicago Medicine, asked whether Dr. Remzi preferred to do an S pouch rather than a J pouch. In response, Dr. Remzi said, “We have to think about what the patient will give us. Throughout the years, I’ve learned that I like to divert the patient for 6 months before surgery. This gets them and their family engaged in the process. … It also elongates the mesentery to give you that reach. But I don’t necessarily do an intentional S pouch if the J pouch gives me what I need for the health of that patient.”
The authors reported no relevant financial disclosures.
SAN DIEGO – Patients hoping to avoid a permanent stoma by having a salvage surgery to repair or replace a failing ileal pouch–anal anastomosis (IPAA) achieved good functional outcomes and quality of life in one institution’s long-term experience.
A large case series drawn from IPAA re-dos at the Cleveland Clinic over a 20-year span showed that the procedure was successful for four in five patients, and more than 90% were satisfied with their quality of life, despite some functional limitations. Dr. Feza Remzi, chairman of the department of colorectal surgery at the Cleveland Clinic, presented findings from 500 patients undergoing IPAA re-dos via the transabdominal approach. In this group, 80% (401) of transabdominally revised IPAAs were successful.
IPAA is a procedure indicated for patients with Crohn’s disease, ulcerative or indeterminate colitis, or familial adenomatous polyposis. The surgery preserves the capacity for anal defecation with intestinal continuity after proctocolectomy by fashioning a reservoir for stool from the small intestine. However, up to 15% of patients will have pouch failure, necessitating a permanent stoma unless the pouch is surgically revised, he said at the annual meeting of the American Surgical Association.
To determine outcomes for patients having a re-do of a failed IPAA, Dr. Remzi and colleagues assessed 502 IPAA re-do patients (215, male; median age, 38 years) who received their procedure at the Cleveland Clinic from 1983 to 2014. Crohn’s disease was the primary diagnosis for 419 patients (84%); just over half (n = 263) had anastomotic leak or fistula as the cause of first pouch failure, followed by pouch-vaginal fistula in 85 women (17%) and obstruction in 116 patients (23%).
The primary endpoints of the study were surgery morbidity, how many patients had a functioning pouch after re-do, pouch function, and quality of life.
Surgeon discretion dictated whether the pouch was revised, as it was in 295 patients (59%), or whether a new pouch was created. Overall, just over half of patients (n = 270) had postoperative complications, though there were no short-term deaths. Ileus and pelvic sepsis were the most common short-term complications, occurring in 81 (16%) and 50 (10%) patients, respectively. All of the other complications occurred in less than 10% of patients. Patients stayed in the hospital a median of 7 days, and 63 (13%) were readmitted.
Over the duration of the study, 101 patients (20%) had failure of their redone IPAA pouches, and pelvis sepsis and anastomotic stricture each occurred in more than 10% of patients. Short-term postoperative morbidity and occurrence of pelvic sepsis at any point after re-do surgery were associated with failure of the redone IPAA based on a Cox regression model (P = .035 and P < .0001, respectively).
Patients were overall very satisfied with their quality of life after IPAA re-do surgery; 92% of the 261 respondents said they would undergo the surgery again, and 93% would recommend the surgery. This was true although patients reported a mean of six daytime bowel movements, about half of patients reported having stool seepage or requiring pad use, and a third of patients reported dietary restrictions related to their bowel function.
Study limitations included the lack of information regarding patients in whom the re-do attempt was abandoned, or for those referred for surgery who did not have an IPAA re-do. Another limitation was the relatively low number of patients who completed all items on the function and quality of life questionnaires; investigators decided that the most robust analysis would flow from including only data for those who had completed all forms.
Discussion focused on the real-world and technical aspects of lessons learned from this large single-institution data set. Dr. David Rothenberger, Jay Phillips Professor and Chair of the department of surgery at the University of Minnesota, Minneapolis, asked whether patients had been carefully selected for this salvage procedure. In his experience, he said, obese patients or those with a heavily muscled pelvis, as well as those with a significant history of prior pelvic infections, would not necessarily be good candidates for a re-do. He suggested that an intention-to-treat analysis might give a truer denominator, and might even change the conclusion that the salvage surgery has a high likelihood of success. Dr. Remzi agreed that obesity or a high body mass index in a patient “is a very good reason not to do the surgery.”
Dr. Neil Hyman, codirector of the digestive diseases center at the University of Chicago Medicine, asked whether Dr. Remzi preferred to do an S pouch rather than a J pouch. In response, Dr. Remzi said, “We have to think about what the patient will give us. Throughout the years, I’ve learned that I like to divert the patient for 6 months before surgery. This gets them and their family engaged in the process. … It also elongates the mesentery to give you that reach. But I don’t necessarily do an intentional S pouch if the J pouch gives me what I need for the health of that patient.”
The authors reported no relevant financial disclosures.
SAN DIEGO – Patients hoping to avoid a permanent stoma by having a salvage surgery to repair or replace a failing ileal pouch–anal anastomosis (IPAA) achieved good functional outcomes and quality of life in one institution’s long-term experience.
A large case series drawn from IPAA re-dos at the Cleveland Clinic over a 20-year span showed that the procedure was successful for four in five patients, and more than 90% were satisfied with their quality of life, despite some functional limitations. Dr. Feza Remzi, chairman of the department of colorectal surgery at the Cleveland Clinic, presented findings from 500 patients undergoing IPAA re-dos via the transabdominal approach. In this group, 80% (401) of transabdominally revised IPAAs were successful.
IPAA is a procedure indicated for patients with Crohn’s disease, ulcerative or indeterminate colitis, or familial adenomatous polyposis. The surgery preserves the capacity for anal defecation with intestinal continuity after proctocolectomy by fashioning a reservoir for stool from the small intestine. However, up to 15% of patients will have pouch failure, necessitating a permanent stoma unless the pouch is surgically revised, he said at the annual meeting of the American Surgical Association.
To determine outcomes for patients having a re-do of a failed IPAA, Dr. Remzi and colleagues assessed 502 IPAA re-do patients (215, male; median age, 38 years) who received their procedure at the Cleveland Clinic from 1983 to 2014. Crohn’s disease was the primary diagnosis for 419 patients (84%); just over half (n = 263) had anastomotic leak or fistula as the cause of first pouch failure, followed by pouch-vaginal fistula in 85 women (17%) and obstruction in 116 patients (23%).
The primary endpoints of the study were surgery morbidity, how many patients had a functioning pouch after re-do, pouch function, and quality of life.
Surgeon discretion dictated whether the pouch was revised, as it was in 295 patients (59%), or whether a new pouch was created. Overall, just over half of patients (n = 270) had postoperative complications, though there were no short-term deaths. Ileus and pelvic sepsis were the most common short-term complications, occurring in 81 (16%) and 50 (10%) patients, respectively. All of the other complications occurred in less than 10% of patients. Patients stayed in the hospital a median of 7 days, and 63 (13%) were readmitted.
Over the duration of the study, 101 patients (20%) had failure of their redone IPAA pouches, and pelvis sepsis and anastomotic stricture each occurred in more than 10% of patients. Short-term postoperative morbidity and occurrence of pelvic sepsis at any point after re-do surgery were associated with failure of the redone IPAA based on a Cox regression model (P = .035 and P < .0001, respectively).
Patients were overall very satisfied with their quality of life after IPAA re-do surgery; 92% of the 261 respondents said they would undergo the surgery again, and 93% would recommend the surgery. This was true although patients reported a mean of six daytime bowel movements, about half of patients reported having stool seepage or requiring pad use, and a third of patients reported dietary restrictions related to their bowel function.
Study limitations included the lack of information regarding patients in whom the re-do attempt was abandoned, or for those referred for surgery who did not have an IPAA re-do. Another limitation was the relatively low number of patients who completed all items on the function and quality of life questionnaires; investigators decided that the most robust analysis would flow from including only data for those who had completed all forms.
Discussion focused on the real-world and technical aspects of lessons learned from this large single-institution data set. Dr. David Rothenberger, Jay Phillips Professor and Chair of the department of surgery at the University of Minnesota, Minneapolis, asked whether patients had been carefully selected for this salvage procedure. In his experience, he said, obese patients or those with a heavily muscled pelvis, as well as those with a significant history of prior pelvic infections, would not necessarily be good candidates for a re-do. He suggested that an intention-to-treat analysis might give a truer denominator, and might even change the conclusion that the salvage surgery has a high likelihood of success. Dr. Remzi agreed that obesity or a high body mass index in a patient “is a very good reason not to do the surgery.”
Dr. Neil Hyman, codirector of the digestive diseases center at the University of Chicago Medicine, asked whether Dr. Remzi preferred to do an S pouch rather than a J pouch. In response, Dr. Remzi said, “We have to think about what the patient will give us. Throughout the years, I’ve learned that I like to divert the patient for 6 months before surgery. This gets them and their family engaged in the process. … It also elongates the mesentery to give you that reach. But I don’t necessarily do an intentional S pouch if the J pouch gives me what I need for the health of that patient.”
The authors reported no relevant financial disclosures.
AT THE ASA ANNUAL MEETING
Key clinical point: Eighty percent of transabdominal revisions of failed ileal pouch–anal anastomosis surgeries were successful; patients were overall content with the results.
Major findings: 80% (401) of transabdominally revised IPAAs were successful, and patients were overall satisfied with their quality of life, with 92% affirming that they would undergo the procedure again and 93% recommending the procedure to similarly situated patients.
Data source: A retrospective analysis of a prospectively enrolled single-center registry of patients having transabdominal re-do surgeries for failed ileal pouch–anal anastomosis between 1983 and 2014.
Disclosures: The authors reported no relevant financial disclosures.
SSIs a factor in postop colon cancer survival
HOUSTON – Surgical-site infections occurring in patients who underwent curative resection for localized colon cancer were associated with worse overall survival in a large retrospective study.
Among nearly 10,000 patients with nonmetastatic colon cancer who underwent surgery with curative intent, surgical-site infections (SSIs) were associated with both worse overall survival and a reduced likelihood of receiving adjuvant chemotherapy, reported Dr. Gala Markia Barden, a surgical resident at Baylor College of Medicine, Houston.
Both SSIs and failure to receive adjuvant chemotherapy are independently associated with worse overall survival, she said at the annual Society of Surgical Oncology Cancer Symposium.
“Future studies and practice guidelines should focus on target areas for improving these potentially preventable problems, including active surveillance for and early recognition of surgical-site infections, as well as vigilant follow-up to ensure treatment completion and to improve the transition between the surgical and medical oncology teams to mitigate losses to follow-up,” she said.
Tapping into the merged Veterans Affairs Surgical Quality Improvement Program and VA Central Cancer Registry (VASQIP-VA) databases, the authors identified 9,946 patients aged 18 years and older who underwent radical resection for colon cancer from 1999 through 2009. Patients with rectal cancers or early postoperative deaths (within 90 days of surgery) were excluded.
The investigators examined the relationships between SSIs and both 5-year overall survival and receipt of adjuvant chemotherapy, which has been documented to improve survival in patients with stage III colon cancer. Delivery of adjuvant chemotherapy in these patients is considered to be a measure of the quality of cancer care, Dr. Barden noted.
Of the 9,946 patients included in the study, 1,340 (13.5%) developed SSIs. These patients were slightly but significantly younger (P < .001), had worse functional status (P = .002), and had higher American Society of Anesthesiologists (ASA) physical status scores (P < .001).
In univariate analysis, the investigators found that, in the entire cohort, SSIs were associated with worse overall survival (OS); in multivariate analysis controlling for sex, nutrition, functional status, ASA score, and number of lymph nodes resected, they saw that SSI was associated with a hazard ratio (HR) for worse overall survival of 1.35 (P < .0001).
When they looked at the association of SSI and OS stratified by cancer stage, however, they found that it was significant only for stage III disease. Patients with stage III who developed an SSI had a median OS of 29 months, compared with 33 months for those with no site infections (P< .001).
Dr. Barden and her associates also found that 42% of patients with infections did not receive adjuvant chemotherapy, compared with 34% of patients without SSIs (P = .002).
To see whether the worse survival among patients with SSI was primarily driven by the failure to deliver chemotherapy, they created a model adjusted for cancer risk factors, which showed that patients with stage III disease who developed an SSI and did not undergo adjuvant chemotherapy had an HR of worse overall survival of 1.59 (P < .0001).
They then added into the model those patients with SSIs who did receive adjuvant therapy but, contrary to their expectations, saw that the HR was only slightly reduced (1.56) and remained significant (P < .0001). The model also confirmed that failure to deliver chemotherapy was associated with worse survival (HR 1.52, P <.0001)
Dr. Barden acknowledged that the study was limited by the retrospective design, predominantly male VA cohort, and the lack of information in the databases about why patients did not receive adjuvant therapy.
The study was internally supported. Dr. Barden reported having no conflicts of interest.
HOUSTON – Surgical-site infections occurring in patients who underwent curative resection for localized colon cancer were associated with worse overall survival in a large retrospective study.
Among nearly 10,000 patients with nonmetastatic colon cancer who underwent surgery with curative intent, surgical-site infections (SSIs) were associated with both worse overall survival and a reduced likelihood of receiving adjuvant chemotherapy, reported Dr. Gala Markia Barden, a surgical resident at Baylor College of Medicine, Houston.
Both SSIs and failure to receive adjuvant chemotherapy are independently associated with worse overall survival, she said at the annual Society of Surgical Oncology Cancer Symposium.
“Future studies and practice guidelines should focus on target areas for improving these potentially preventable problems, including active surveillance for and early recognition of surgical-site infections, as well as vigilant follow-up to ensure treatment completion and to improve the transition between the surgical and medical oncology teams to mitigate losses to follow-up,” she said.
Tapping into the merged Veterans Affairs Surgical Quality Improvement Program and VA Central Cancer Registry (VASQIP-VA) databases, the authors identified 9,946 patients aged 18 years and older who underwent radical resection for colon cancer from 1999 through 2009. Patients with rectal cancers or early postoperative deaths (within 90 days of surgery) were excluded.
The investigators examined the relationships between SSIs and both 5-year overall survival and receipt of adjuvant chemotherapy, which has been documented to improve survival in patients with stage III colon cancer. Delivery of adjuvant chemotherapy in these patients is considered to be a measure of the quality of cancer care, Dr. Barden noted.
Of the 9,946 patients included in the study, 1,340 (13.5%) developed SSIs. These patients were slightly but significantly younger (P < .001), had worse functional status (P = .002), and had higher American Society of Anesthesiologists (ASA) physical status scores (P < .001).
In univariate analysis, the investigators found that, in the entire cohort, SSIs were associated with worse overall survival (OS); in multivariate analysis controlling for sex, nutrition, functional status, ASA score, and number of lymph nodes resected, they saw that SSI was associated with a hazard ratio (HR) for worse overall survival of 1.35 (P < .0001).
When they looked at the association of SSI and OS stratified by cancer stage, however, they found that it was significant only for stage III disease. Patients with stage III who developed an SSI had a median OS of 29 months, compared with 33 months for those with no site infections (P< .001).
Dr. Barden and her associates also found that 42% of patients with infections did not receive adjuvant chemotherapy, compared with 34% of patients without SSIs (P = .002).
To see whether the worse survival among patients with SSI was primarily driven by the failure to deliver chemotherapy, they created a model adjusted for cancer risk factors, which showed that patients with stage III disease who developed an SSI and did not undergo adjuvant chemotherapy had an HR of worse overall survival of 1.59 (P < .0001).
They then added into the model those patients with SSIs who did receive adjuvant therapy but, contrary to their expectations, saw that the HR was only slightly reduced (1.56) and remained significant (P < .0001). The model also confirmed that failure to deliver chemotherapy was associated with worse survival (HR 1.52, P <.0001)
Dr. Barden acknowledged that the study was limited by the retrospective design, predominantly male VA cohort, and the lack of information in the databases about why patients did not receive adjuvant therapy.
The study was internally supported. Dr. Barden reported having no conflicts of interest.
HOUSTON – Surgical-site infections occurring in patients who underwent curative resection for localized colon cancer were associated with worse overall survival in a large retrospective study.
Among nearly 10,000 patients with nonmetastatic colon cancer who underwent surgery with curative intent, surgical-site infections (SSIs) were associated with both worse overall survival and a reduced likelihood of receiving adjuvant chemotherapy, reported Dr. Gala Markia Barden, a surgical resident at Baylor College of Medicine, Houston.
Both SSIs and failure to receive adjuvant chemotherapy are independently associated with worse overall survival, she said at the annual Society of Surgical Oncology Cancer Symposium.
“Future studies and practice guidelines should focus on target areas for improving these potentially preventable problems, including active surveillance for and early recognition of surgical-site infections, as well as vigilant follow-up to ensure treatment completion and to improve the transition between the surgical and medical oncology teams to mitigate losses to follow-up,” she said.
Tapping into the merged Veterans Affairs Surgical Quality Improvement Program and VA Central Cancer Registry (VASQIP-VA) databases, the authors identified 9,946 patients aged 18 years and older who underwent radical resection for colon cancer from 1999 through 2009. Patients with rectal cancers or early postoperative deaths (within 90 days of surgery) were excluded.
The investigators examined the relationships between SSIs and both 5-year overall survival and receipt of adjuvant chemotherapy, which has been documented to improve survival in patients with stage III colon cancer. Delivery of adjuvant chemotherapy in these patients is considered to be a measure of the quality of cancer care, Dr. Barden noted.
Of the 9,946 patients included in the study, 1,340 (13.5%) developed SSIs. These patients were slightly but significantly younger (P < .001), had worse functional status (P = .002), and had higher American Society of Anesthesiologists (ASA) physical status scores (P < .001).
In univariate analysis, the investigators found that, in the entire cohort, SSIs were associated with worse overall survival (OS); in multivariate analysis controlling for sex, nutrition, functional status, ASA score, and number of lymph nodes resected, they saw that SSI was associated with a hazard ratio (HR) for worse overall survival of 1.35 (P < .0001).
When they looked at the association of SSI and OS stratified by cancer stage, however, they found that it was significant only for stage III disease. Patients with stage III who developed an SSI had a median OS of 29 months, compared with 33 months for those with no site infections (P< .001).
Dr. Barden and her associates also found that 42% of patients with infections did not receive adjuvant chemotherapy, compared with 34% of patients without SSIs (P = .002).
To see whether the worse survival among patients with SSI was primarily driven by the failure to deliver chemotherapy, they created a model adjusted for cancer risk factors, which showed that patients with stage III disease who developed an SSI and did not undergo adjuvant chemotherapy had an HR of worse overall survival of 1.59 (P < .0001).
They then added into the model those patients with SSIs who did receive adjuvant therapy but, contrary to their expectations, saw that the HR was only slightly reduced (1.56) and remained significant (P < .0001). The model also confirmed that failure to deliver chemotherapy was associated with worse survival (HR 1.52, P <.0001)
Dr. Barden acknowledged that the study was limited by the retrospective design, predominantly male VA cohort, and the lack of information in the databases about why patients did not receive adjuvant therapy.
The study was internally supported. Dr. Barden reported having no conflicts of interest.
AT SSO 2015
Key clinical point: Surgical site infections in patients with colon cancer are associated with both worse overall survival and lower chance of receiving adjuvant chemotherapy.
Major finding: Median overall survival for stage III patients with SSIs was 29 months, vs. 33 for no SSIs.
Data source: Retrospective cohort study of 9,946 patients who underwent radical colon cancer resection with curative intent.
Disclosures: The study was internally supported. Dr. Barden reported having no conflicts of interest.
Rectal preservation feasible after cancer clinical remission
HOUSTON – Patients who achieve complete clinical responses after neoadjuvant therapy for locally advanced rectal cancer may, in many cases, be safely spared the trauma and morbidity of total mesorectal excision.
That’s the opinion of investigators at Memorial Sloan Kettering Cancer Center, New York, who found that nearly two-thirds of patients followed with nonoperative management (NOM) had durable complete clinical remissions (cCR) for at least 4 years.
Disease-specific survival and overall survival rates among patients who had nonoperative management were similar to those seen in patients with pathologic complete responses (pCR), defined as no viable tumor cells in the resected specimen.
“We know that there is a very good overall and disease-free survival associated with a [pCR]. Clinical complete response is also associated with pathologic complete response. In that regard, this brings up the question: Is an operation always necessary in these patients?” Dr. Jesse Joshua Smith of the cancer center said at the annual Society of Surgical Oncology Cancer Symposium.
Dr. Smith and colleagues conducted a review of their center’s experience to date with NOM for patients with locally advanced rectal cancer, asking whether the data support the approach as oncologically safe and effective for organ preservation.
They identified 442 patients with rectal cancer treated with neoadjuvant chemotherapy from 2006 through 2014 and compared results for 73 who achieved a cCR and were followed with nonoperative management with those of 72 patients who had a pCR following total mesorectal excision.
Demographic and clinical characteristics between the groups were generally similar, although patients in the pCR group were significantly younger (58 years vs. 65 years, P = .01), had a greater tumor distance from the anal verge (median of 6 cm vs. 5.25 cm, P = .02), and higher proportions of clinical stage II (32% vs. 24%) and III (66% vs. 62%, P = .02).
Among the 73 patients managed with NOM, 54 had durable cCR at 4 years. Of the remaining 19 with local tumor regrowth, 2 had local excisions with no further recurrence and 17 went on to have rectal resections. The total number of patients with rectal preservation in this group was 56 (77%).
Of the 19 patients in the conservatively managed group who had local regrowths, all but three of the recurrences were detected within 13 months.
As noted before, neither disease-specific survival nor overall survival were significantly different between patients managed with NOM or with total mesorectal excision.
There were numerically more distant recurrences at both 1 and 4 years among patients treated with NOM compared with total mesorectal excision (7% vs. 2%, and 17% vs. 9%, respectively), but the differences were not statistically significant, the authors found.
Dr. Smith noted that patients who are offered the option of NOM have a discussion with the surgeon emphasizing that the practice is nonstandard management, carries about a 25% risk of local regrowth, and requires increased endoscopic and radiographic surveillance. Patients also are informed about the risks of salvage abdominoperineal resection or extended resections, and about the potential risk of compromising cure.
The study was supported in part by the Berezuk Colorectal Cancer Fund. Dr. Smith reported having no disclosures.
HOUSTON – Patients who achieve complete clinical responses after neoadjuvant therapy for locally advanced rectal cancer may, in many cases, be safely spared the trauma and morbidity of total mesorectal excision.
That’s the opinion of investigators at Memorial Sloan Kettering Cancer Center, New York, who found that nearly two-thirds of patients followed with nonoperative management (NOM) had durable complete clinical remissions (cCR) for at least 4 years.
Disease-specific survival and overall survival rates among patients who had nonoperative management were similar to those seen in patients with pathologic complete responses (pCR), defined as no viable tumor cells in the resected specimen.
“We know that there is a very good overall and disease-free survival associated with a [pCR]. Clinical complete response is also associated with pathologic complete response. In that regard, this brings up the question: Is an operation always necessary in these patients?” Dr. Jesse Joshua Smith of the cancer center said at the annual Society of Surgical Oncology Cancer Symposium.
Dr. Smith and colleagues conducted a review of their center’s experience to date with NOM for patients with locally advanced rectal cancer, asking whether the data support the approach as oncologically safe and effective for organ preservation.
They identified 442 patients with rectal cancer treated with neoadjuvant chemotherapy from 2006 through 2014 and compared results for 73 who achieved a cCR and were followed with nonoperative management with those of 72 patients who had a pCR following total mesorectal excision.
Demographic and clinical characteristics between the groups were generally similar, although patients in the pCR group were significantly younger (58 years vs. 65 years, P = .01), had a greater tumor distance from the anal verge (median of 6 cm vs. 5.25 cm, P = .02), and higher proportions of clinical stage II (32% vs. 24%) and III (66% vs. 62%, P = .02).
Among the 73 patients managed with NOM, 54 had durable cCR at 4 years. Of the remaining 19 with local tumor regrowth, 2 had local excisions with no further recurrence and 17 went on to have rectal resections. The total number of patients with rectal preservation in this group was 56 (77%).
Of the 19 patients in the conservatively managed group who had local regrowths, all but three of the recurrences were detected within 13 months.
As noted before, neither disease-specific survival nor overall survival were significantly different between patients managed with NOM or with total mesorectal excision.
There were numerically more distant recurrences at both 1 and 4 years among patients treated with NOM compared with total mesorectal excision (7% vs. 2%, and 17% vs. 9%, respectively), but the differences were not statistically significant, the authors found.
Dr. Smith noted that patients who are offered the option of NOM have a discussion with the surgeon emphasizing that the practice is nonstandard management, carries about a 25% risk of local regrowth, and requires increased endoscopic and radiographic surveillance. Patients also are informed about the risks of salvage abdominoperineal resection or extended resections, and about the potential risk of compromising cure.
The study was supported in part by the Berezuk Colorectal Cancer Fund. Dr. Smith reported having no disclosures.
HOUSTON – Patients who achieve complete clinical responses after neoadjuvant therapy for locally advanced rectal cancer may, in many cases, be safely spared the trauma and morbidity of total mesorectal excision.
That’s the opinion of investigators at Memorial Sloan Kettering Cancer Center, New York, who found that nearly two-thirds of patients followed with nonoperative management (NOM) had durable complete clinical remissions (cCR) for at least 4 years.
Disease-specific survival and overall survival rates among patients who had nonoperative management were similar to those seen in patients with pathologic complete responses (pCR), defined as no viable tumor cells in the resected specimen.
“We know that there is a very good overall and disease-free survival associated with a [pCR]. Clinical complete response is also associated with pathologic complete response. In that regard, this brings up the question: Is an operation always necessary in these patients?” Dr. Jesse Joshua Smith of the cancer center said at the annual Society of Surgical Oncology Cancer Symposium.
Dr. Smith and colleagues conducted a review of their center’s experience to date with NOM for patients with locally advanced rectal cancer, asking whether the data support the approach as oncologically safe and effective for organ preservation.
They identified 442 patients with rectal cancer treated with neoadjuvant chemotherapy from 2006 through 2014 and compared results for 73 who achieved a cCR and were followed with nonoperative management with those of 72 patients who had a pCR following total mesorectal excision.
Demographic and clinical characteristics between the groups were generally similar, although patients in the pCR group were significantly younger (58 years vs. 65 years, P = .01), had a greater tumor distance from the anal verge (median of 6 cm vs. 5.25 cm, P = .02), and higher proportions of clinical stage II (32% vs. 24%) and III (66% vs. 62%, P = .02).
Among the 73 patients managed with NOM, 54 had durable cCR at 4 years. Of the remaining 19 with local tumor regrowth, 2 had local excisions with no further recurrence and 17 went on to have rectal resections. The total number of patients with rectal preservation in this group was 56 (77%).
Of the 19 patients in the conservatively managed group who had local regrowths, all but three of the recurrences were detected within 13 months.
As noted before, neither disease-specific survival nor overall survival were significantly different between patients managed with NOM or with total mesorectal excision.
There were numerically more distant recurrences at both 1 and 4 years among patients treated with NOM compared with total mesorectal excision (7% vs. 2%, and 17% vs. 9%, respectively), but the differences were not statistically significant, the authors found.
Dr. Smith noted that patients who are offered the option of NOM have a discussion with the surgeon emphasizing that the practice is nonstandard management, carries about a 25% risk of local regrowth, and requires increased endoscopic and radiographic surveillance. Patients also are informed about the risks of salvage abdominoperineal resection or extended resections, and about the potential risk of compromising cure.
The study was supported in part by the Berezuk Colorectal Cancer Fund. Dr. Smith reported having no disclosures.
Key clinical point: Patients with complete clinical response after neoadjuvant chemotherapy for rectal cancer may be able to be safely followed with nonoperative management.
Major finding: There were no significant differences at 4 years in either disease-specific or overall survival among patients with rectal cancer managed conservatively or with total mesorectal excision.
Data source: Review of prospectively collected data on 145 patients with locally advanced rectal cancer.
Disclosures: The study was supported in part by the Berezuk Colorectal Cancer Fund. Dr. Smith reported having no disclosures.
Risk scale predicts mortality after gastric cancer surgery
HOUSTON – A simple preoperative scale can accurately predict a patient’s risk for near-term death following surgery for gastric cancer, investigators say.
The scale accounts for both patient and hospital factors, and is useful as a clinical tool for preoperative counseling of patients, reported Dr. Cristina Harnsberger of the University of California San Diego.
“Male gender, increasing age, and comorbid disease increase risk of in-hospital mortality for patients who undergo gastric resection for malignancy. Additionally, low hospital volume was an independent risk factor,” she said at the annual Society of Surgical Oncology Cancer Symposium.
The scale was able to accurately classify patients as being at low or high risk, and the observed and expected mortality rates for each risk score were well correlated, she said.
Weighing risks
Perioperative mortality rates following resection for gastric malignancies range from 0.6% to 15%. Risk scales and nomograms are intended to help clinicians predict risks for individual patients, but most incorporate postoperative data rather than preoperative or hospital data, Dr. Harnsberger said.
She and her colleagues conducted a study to determine whether a simple preoperative scale based on patient and hospital factors could accurately predict risk for death following gastric resection for malignancy.
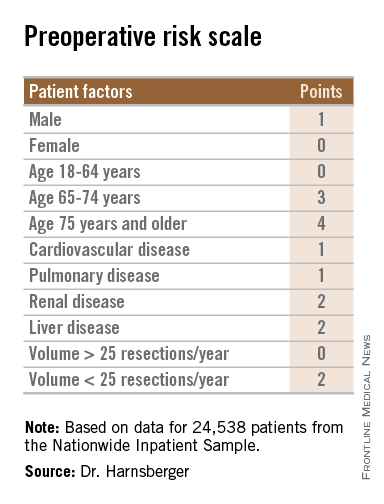
They drew on data from the Nationwide Inpatient Sample database to identify adult patients with a diagnosis of gastric cancer who underwent potentially curative partial or total gastrectomy from 1998 through 2011.
They identified a total 24,538 patients, based on International Classification of Diseases, Revision 9 (ICD-9) diagnosis and procedure codes.
They then created multivariate logistic regression models to identify independent predictors of mortality, create a predictive model, and construct a risk scale. The models controlled for sex, age, race, comorbidities, insurance status, hospital volume (less than 25 vs. 25 or more gastric resections for malignancy per year), laparoscopic vs. open approach, poverty level, alcohol abuse, tobacco use, diabetes mellitus, and year of procedure.
The mean length of stay for the patient sample was 11 days. The overall in-hospital mortality was 5.5%.
The models identified three patient-related factors and one hospital-related factor that were predictive of mortality and when combined in a risk scale proved to be accurate.
The patient factors were male sex, age 65 and older, and comorbid disease, specifically cardiovascular, pulmonary, renal, and/or hepatic.
The hospital factor, expressed as protective, was 25 or more gastric resections for cancer per year.
The maximum possible score is 13. Patients with scores lower than 6 are at low risk for perioperative mortality, while those with scores 6 and higher are at high risk. Among patients with a score of 0-5, the perioperative death rate ranged from 1.3% to 4.5%. In contrast, patients with higher scores had death rates ranging from 6.0% to 23.1%.
Clinical applications for the bedside risk scale include perioperative patient counseling, aiding in informed consent discussions, and as an adjunct to postoperative risk calculators, Dr. Harnsberger said.The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
HOUSTON – A simple preoperative scale can accurately predict a patient’s risk for near-term death following surgery for gastric cancer, investigators say.
The scale accounts for both patient and hospital factors, and is useful as a clinical tool for preoperative counseling of patients, reported Dr. Cristina Harnsberger of the University of California San Diego.
“Male gender, increasing age, and comorbid disease increase risk of in-hospital mortality for patients who undergo gastric resection for malignancy. Additionally, low hospital volume was an independent risk factor,” she said at the annual Society of Surgical Oncology Cancer Symposium.
The scale was able to accurately classify patients as being at low or high risk, and the observed and expected mortality rates for each risk score were well correlated, she said.
Weighing risks
Perioperative mortality rates following resection for gastric malignancies range from 0.6% to 15%. Risk scales and nomograms are intended to help clinicians predict risks for individual patients, but most incorporate postoperative data rather than preoperative or hospital data, Dr. Harnsberger said.
She and her colleagues conducted a study to determine whether a simple preoperative scale based on patient and hospital factors could accurately predict risk for death following gastric resection for malignancy.
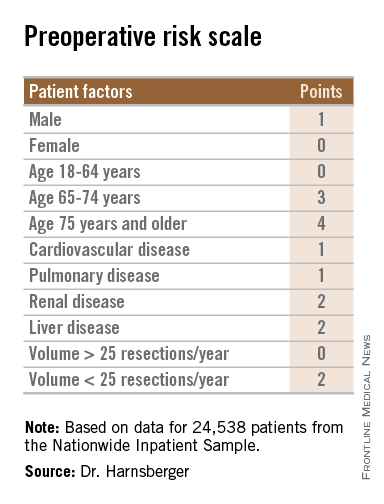
They drew on data from the Nationwide Inpatient Sample database to identify adult patients with a diagnosis of gastric cancer who underwent potentially curative partial or total gastrectomy from 1998 through 2011.
They identified a total 24,538 patients, based on International Classification of Diseases, Revision 9 (ICD-9) diagnosis and procedure codes.
They then created multivariate logistic regression models to identify independent predictors of mortality, create a predictive model, and construct a risk scale. The models controlled for sex, age, race, comorbidities, insurance status, hospital volume (less than 25 vs. 25 or more gastric resections for malignancy per year), laparoscopic vs. open approach, poverty level, alcohol abuse, tobacco use, diabetes mellitus, and year of procedure.
The mean length of stay for the patient sample was 11 days. The overall in-hospital mortality was 5.5%.
The models identified three patient-related factors and one hospital-related factor that were predictive of mortality and when combined in a risk scale proved to be accurate.
The patient factors were male sex, age 65 and older, and comorbid disease, specifically cardiovascular, pulmonary, renal, and/or hepatic.
The hospital factor, expressed as protective, was 25 or more gastric resections for cancer per year.
The maximum possible score is 13. Patients with scores lower than 6 are at low risk for perioperative mortality, while those with scores 6 and higher are at high risk. Among patients with a score of 0-5, the perioperative death rate ranged from 1.3% to 4.5%. In contrast, patients with higher scores had death rates ranging from 6.0% to 23.1%.
Clinical applications for the bedside risk scale include perioperative patient counseling, aiding in informed consent discussions, and as an adjunct to postoperative risk calculators, Dr. Harnsberger said.The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
HOUSTON – A simple preoperative scale can accurately predict a patient’s risk for near-term death following surgery for gastric cancer, investigators say.
The scale accounts for both patient and hospital factors, and is useful as a clinical tool for preoperative counseling of patients, reported Dr. Cristina Harnsberger of the University of California San Diego.
“Male gender, increasing age, and comorbid disease increase risk of in-hospital mortality for patients who undergo gastric resection for malignancy. Additionally, low hospital volume was an independent risk factor,” she said at the annual Society of Surgical Oncology Cancer Symposium.
The scale was able to accurately classify patients as being at low or high risk, and the observed and expected mortality rates for each risk score were well correlated, she said.
Weighing risks
Perioperative mortality rates following resection for gastric malignancies range from 0.6% to 15%. Risk scales and nomograms are intended to help clinicians predict risks for individual patients, but most incorporate postoperative data rather than preoperative or hospital data, Dr. Harnsberger said.
She and her colleagues conducted a study to determine whether a simple preoperative scale based on patient and hospital factors could accurately predict risk for death following gastric resection for malignancy.
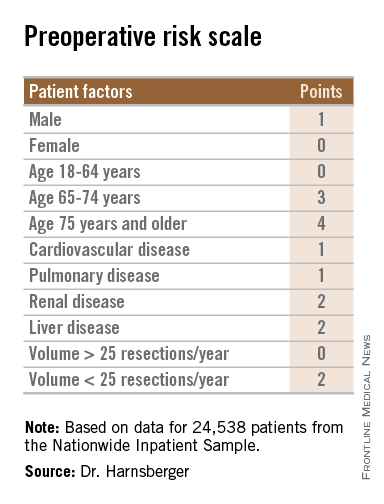
They drew on data from the Nationwide Inpatient Sample database to identify adult patients with a diagnosis of gastric cancer who underwent potentially curative partial or total gastrectomy from 1998 through 2011.
They identified a total 24,538 patients, based on International Classification of Diseases, Revision 9 (ICD-9) diagnosis and procedure codes.
They then created multivariate logistic regression models to identify independent predictors of mortality, create a predictive model, and construct a risk scale. The models controlled for sex, age, race, comorbidities, insurance status, hospital volume (less than 25 vs. 25 or more gastric resections for malignancy per year), laparoscopic vs. open approach, poverty level, alcohol abuse, tobacco use, diabetes mellitus, and year of procedure.
The mean length of stay for the patient sample was 11 days. The overall in-hospital mortality was 5.5%.
The models identified three patient-related factors and one hospital-related factor that were predictive of mortality and when combined in a risk scale proved to be accurate.
The patient factors were male sex, age 65 and older, and comorbid disease, specifically cardiovascular, pulmonary, renal, and/or hepatic.
The hospital factor, expressed as protective, was 25 or more gastric resections for cancer per year.
The maximum possible score is 13. Patients with scores lower than 6 are at low risk for perioperative mortality, while those with scores 6 and higher are at high risk. Among patients with a score of 0-5, the perioperative death rate ranged from 1.3% to 4.5%. In contrast, patients with higher scores had death rates ranging from 6.0% to 23.1%.
Clinical applications for the bedside risk scale include perioperative patient counseling, aiding in informed consent discussions, and as an adjunct to postoperative risk calculators, Dr. Harnsberger said.The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
AT SSO 2015
Key clinical point: The bedside risk scale can be used in patient counseling prior to surgery for gastric malignancies.
Major finding: Patients with scores of 0-5 had perioperative death rates of 1.3%-4.5%. Patients with higher scores had death rates ranging from 6.0% to 23.1%.
Data source: Review of retrospective data on 24,538 adults who underwent partial or total gastric resection for malignancies.
Disclosures: The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
Laparoscopic ‘noninferior’ to open approach for rectal cancer
Laparoscopic resection of rectal cancer is noninferior to open surgery in preventing locoregional recurrence and in improving overall and disease-free survival, according to a report published online April 1 in the New England Journal of Medicine.
The laparoscopic approach has increasingly replaced open surgery in recent years, primarily because it offers short-term advantages such as less pain, reduced blood loss, and a shorter recovery time. But no large randomized trials have established that long-term outcomes with laparoscopic resection, including survival, are at least noninferior to those with open surgery, said Dr. Hendrik Jaap Bonjer of VU University Medical Center, Amsterdam, and his associates.
They now report the 3-year outcomes of the Colorectal Cancer Laparoscopic or Open Resection (COLOR) II trial, an industry-sponsored noninferiority study performed at 30 medical centers in eight countries in Europe, North America, and Asia. The trial involved 1,044 patients who had solitary, noninvasive adenocarcinomas of the rectum within 15 cm of the anal verge. A total of 699 of the study participants were randomly assigned to laparoscopic and 345 to open surgery.
At 3-year follow-up, the rate of locoregional recurrence was identical between the two study groups, at 5% each. In addition, rates of disease-free survival slightly favored the laparoscopic approach (74.8%) over the open approach (70.8%), as did rates of overall survival (86.7% and 83.6%, respectively) and rates of distant metastases (19.1% and 22.1%, respectively). Patients with stage III disease appeared to benefit the most from laparoscopic surgery, with disease-free survival of 64.9% vs. 52.0%, the investigators said (N. Engl. J. Med. 2015 April 1 [doi:10.1056/NEJMoa1414882]). These findings support the idea that the reduced surgical trauma associated with laparoscopic techniques may decrease tumor recurrence, perhaps by attenuating stress responses and preserving immune function, they noted.
“In our study, laparoscopic surgery in patients with cancer in the lower third of the rectum was associated with a lower rate of involved circumferential resection margin and a lower locoregional recurrence rate than was open surgery. During laparoscopic surgery, narrow spaces such as the lower pelvis are better visualized than in open surgery, owing to the use of a laparoscope, which projects a magnified and well-illuminated image of the operative field on the monitors. A clear view is of paramount importance to accomplish a resection of the cancer with sufficient margins,” Dr. Bonjer and his associates added.
The trial was funded by Ethicon Endo-Surgery Europe, a subsidiary of Johnson & Johnson; the Swedish Cancer Society; the Health and Medical Care Committee of Region Vastra Gotaland; Sahlgrenska University Hospital; Erasmus University Medical Center; Dahousie University; and VU University Medical Center. Dr. Bonjer reported having no disclosures; two of his associates reported ties to AbbVie, Merck Sharp & Dohme, Takeda, Johnson & Johnson, Covidien, Olympus Medical, and Applied Medical.
Laparoscopic resection of rectal cancer is noninferior to open surgery in preventing locoregional recurrence and in improving overall and disease-free survival, according to a report published online April 1 in the New England Journal of Medicine.
The laparoscopic approach has increasingly replaced open surgery in recent years, primarily because it offers short-term advantages such as less pain, reduced blood loss, and a shorter recovery time. But no large randomized trials have established that long-term outcomes with laparoscopic resection, including survival, are at least noninferior to those with open surgery, said Dr. Hendrik Jaap Bonjer of VU University Medical Center, Amsterdam, and his associates.
They now report the 3-year outcomes of the Colorectal Cancer Laparoscopic or Open Resection (COLOR) II trial, an industry-sponsored noninferiority study performed at 30 medical centers in eight countries in Europe, North America, and Asia. The trial involved 1,044 patients who had solitary, noninvasive adenocarcinomas of the rectum within 15 cm of the anal verge. A total of 699 of the study participants were randomly assigned to laparoscopic and 345 to open surgery.
At 3-year follow-up, the rate of locoregional recurrence was identical between the two study groups, at 5% each. In addition, rates of disease-free survival slightly favored the laparoscopic approach (74.8%) over the open approach (70.8%), as did rates of overall survival (86.7% and 83.6%, respectively) and rates of distant metastases (19.1% and 22.1%, respectively). Patients with stage III disease appeared to benefit the most from laparoscopic surgery, with disease-free survival of 64.9% vs. 52.0%, the investigators said (N. Engl. J. Med. 2015 April 1 [doi:10.1056/NEJMoa1414882]). These findings support the idea that the reduced surgical trauma associated with laparoscopic techniques may decrease tumor recurrence, perhaps by attenuating stress responses and preserving immune function, they noted.
“In our study, laparoscopic surgery in patients with cancer in the lower third of the rectum was associated with a lower rate of involved circumferential resection margin and a lower locoregional recurrence rate than was open surgery. During laparoscopic surgery, narrow spaces such as the lower pelvis are better visualized than in open surgery, owing to the use of a laparoscope, which projects a magnified and well-illuminated image of the operative field on the monitors. A clear view is of paramount importance to accomplish a resection of the cancer with sufficient margins,” Dr. Bonjer and his associates added.
The trial was funded by Ethicon Endo-Surgery Europe, a subsidiary of Johnson & Johnson; the Swedish Cancer Society; the Health and Medical Care Committee of Region Vastra Gotaland; Sahlgrenska University Hospital; Erasmus University Medical Center; Dahousie University; and VU University Medical Center. Dr. Bonjer reported having no disclosures; two of his associates reported ties to AbbVie, Merck Sharp & Dohme, Takeda, Johnson & Johnson, Covidien, Olympus Medical, and Applied Medical.
Laparoscopic resection of rectal cancer is noninferior to open surgery in preventing locoregional recurrence and in improving overall and disease-free survival, according to a report published online April 1 in the New England Journal of Medicine.
The laparoscopic approach has increasingly replaced open surgery in recent years, primarily because it offers short-term advantages such as less pain, reduced blood loss, and a shorter recovery time. But no large randomized trials have established that long-term outcomes with laparoscopic resection, including survival, are at least noninferior to those with open surgery, said Dr. Hendrik Jaap Bonjer of VU University Medical Center, Amsterdam, and his associates.
They now report the 3-year outcomes of the Colorectal Cancer Laparoscopic or Open Resection (COLOR) II trial, an industry-sponsored noninferiority study performed at 30 medical centers in eight countries in Europe, North America, and Asia. The trial involved 1,044 patients who had solitary, noninvasive adenocarcinomas of the rectum within 15 cm of the anal verge. A total of 699 of the study participants were randomly assigned to laparoscopic and 345 to open surgery.
At 3-year follow-up, the rate of locoregional recurrence was identical between the two study groups, at 5% each. In addition, rates of disease-free survival slightly favored the laparoscopic approach (74.8%) over the open approach (70.8%), as did rates of overall survival (86.7% and 83.6%, respectively) and rates of distant metastases (19.1% and 22.1%, respectively). Patients with stage III disease appeared to benefit the most from laparoscopic surgery, with disease-free survival of 64.9% vs. 52.0%, the investigators said (N. Engl. J. Med. 2015 April 1 [doi:10.1056/NEJMoa1414882]). These findings support the idea that the reduced surgical trauma associated with laparoscopic techniques may decrease tumor recurrence, perhaps by attenuating stress responses and preserving immune function, they noted.
“In our study, laparoscopic surgery in patients with cancer in the lower third of the rectum was associated with a lower rate of involved circumferential resection margin and a lower locoregional recurrence rate than was open surgery. During laparoscopic surgery, narrow spaces such as the lower pelvis are better visualized than in open surgery, owing to the use of a laparoscope, which projects a magnified and well-illuminated image of the operative field on the monitors. A clear view is of paramount importance to accomplish a resection of the cancer with sufficient margins,” Dr. Bonjer and his associates added.
The trial was funded by Ethicon Endo-Surgery Europe, a subsidiary of Johnson & Johnson; the Swedish Cancer Society; the Health and Medical Care Committee of Region Vastra Gotaland; Sahlgrenska University Hospital; Erasmus University Medical Center; Dahousie University; and VU University Medical Center. Dr. Bonjer reported having no disclosures; two of his associates reported ties to AbbVie, Merck Sharp & Dohme, Takeda, Johnson & Johnson, Covidien, Olympus Medical, and Applied Medical.
Key clinical point: Laparoscopic resection is noninferior to open surgery in preventing locoregional recurrence of rectal cancer and improving survival.
Major finding: At 3-year follow-up, the rate of locoregional recurrence was identical between the laparoscopic- and the open-surgery groups, at 5% each.
Data source: An industry-sponsored multicenter open-label noninferiority trial comparing laparoscopic to open resection of rectal cancer in 1,044 patients followed for 3 years.
Disclosures: The trial was funded by Ethicon Endo-Surgery Europe, a subsidiary of Johnson & Johnson; the Swedish Cancer Society; the Health and Medical Care Committee of Region Vastra Gotaland; Sahlgrenska University Hospital; Erasmus University Medical Center; Dahousie University; and VU University Medical Center. Dr. Bonjer reported having no disclosures; two of his associates reported ties to AbbVie, Merck Sharp & Dohme, Takeda, Johnson & Johnson, Covidien, Olympus Medical, and Applied Medical.