User login
Six factors predicted poor surgical outcomes in toxic colitis
Older age, female sex, preoperative chronic steroid use, azotemia, respiratory insufficiency, and coagulopathy all predicted death within a month of colectomy in patients with toxic colitis in the National Surgical Quality Improvement Project database.
The study is the largest to evaluate patients undergoing colectomy for toxic colitis, according to lead investigator Dr. Anand Dayama of the University of California, Davis, and his associates.
“In a case such as multiorgan failure with toxic colitis, the decision whether ... to operate can be an immensely difficult one,” Dr. Dayama and his colleagues wrote. “This study can help in making informed decisions in order to avoid the medicolegal ramifications of either performing an unnecessary procedure or withholding a lifesaving one,” they wrote in the American Journal of Surgery.
Surgical salvage remains the preferred treatment for patients with medically refractory toxic colitis. To assess outcomes in these patients, the researchers queried the National Surgical Quality Improvement Project database for relevant International Classification of Diseases, Ninth Revision codes between 2005 and 2012 (Am J Surg. 2015 Nov;210[5]:852-8).
The results underscored the severity of toxic colitis, they said. Of 189 patients, more than 26% died within 30 days after surgery, one in five developed postsurgical sepsis, about 17% had cardiovascular complications, 15% had wound complications, and 13% had renal complications. Furthermore, patients who were 70-80 years old had 3.5 times greater odds of dying, compared with younger patients (95% confidence interval, 1.0-12.8), and the increased likelihood of death rose by 22.2 when patients were older than 80 years (95% CI, 5.7-86.4).
Other baseline predictors of 30-day mortality included female sex (odds ratio, 4.1), blood urea nitrogen levels above 40 mg/dL (OR, 4.1), an international normalized ratio exceeding 2 (OR, 7.7), preoperative respiratory insufficiency (OR, 2.73), and a history of chronic steroid use (OR, 3.9), the researchers said. In addition, patients who died within 30 days after surgery were more likely than survivors to have undergone prolonged mechanical ventilation (56% vs. 27%), to have returned to the operating room (18% vs. 14%), to have acute renal failure (28% vs. 6%), or to have suffered a cardiac arrest that required cardiopulmonary resuscitation (18% vs. 7%). Survivors averaged about 2 fewer days in the hospital, compared with patients who died after surgery.
“The high morbidity and mortality of toxic colitis requires early and intensive medical management with IV [intravenous] steroids, antibiotics, decompressive maneuvers, and other resuscitative measures to treat the underlying cause,” they emphasized. “If there is no sign of improvement within 7 days or if there are any signs of deterioration, urgent surgical intervention should be considered.”
The link between female sex and mortality might reflect hormonal changes associated with menopause, but the study did not assess hormonal status or use of hormone therapy, the investigators noted. The association between chronic steroid use and postoperative death “is highly relevant” because long-term steroids are so often used in inflammatory bowel disease, they added. Clinical guidelines (Am J Gastroenterol. 2012 Feb;107:179-94) recommend that patients with acute severe ulcerative colitis proceed to second-line therapy or surgery if they do not respond to 3 days of intravenous steroids, because unnecessary delays can increase the risk of postoperative complications, they added.
The researchers reported no funding sources and had no disclosures.
Older age, female sex, preoperative chronic steroid use, azotemia, respiratory insufficiency, and coagulopathy all predicted death within a month of colectomy in patients with toxic colitis in the National Surgical Quality Improvement Project database.
The study is the largest to evaluate patients undergoing colectomy for toxic colitis, according to lead investigator Dr. Anand Dayama of the University of California, Davis, and his associates.
“In a case such as multiorgan failure with toxic colitis, the decision whether ... to operate can be an immensely difficult one,” Dr. Dayama and his colleagues wrote. “This study can help in making informed decisions in order to avoid the medicolegal ramifications of either performing an unnecessary procedure or withholding a lifesaving one,” they wrote in the American Journal of Surgery.
Surgical salvage remains the preferred treatment for patients with medically refractory toxic colitis. To assess outcomes in these patients, the researchers queried the National Surgical Quality Improvement Project database for relevant International Classification of Diseases, Ninth Revision codes between 2005 and 2012 (Am J Surg. 2015 Nov;210[5]:852-8).
The results underscored the severity of toxic colitis, they said. Of 189 patients, more than 26% died within 30 days after surgery, one in five developed postsurgical sepsis, about 17% had cardiovascular complications, 15% had wound complications, and 13% had renal complications. Furthermore, patients who were 70-80 years old had 3.5 times greater odds of dying, compared with younger patients (95% confidence interval, 1.0-12.8), and the increased likelihood of death rose by 22.2 when patients were older than 80 years (95% CI, 5.7-86.4).
Other baseline predictors of 30-day mortality included female sex (odds ratio, 4.1), blood urea nitrogen levels above 40 mg/dL (OR, 4.1), an international normalized ratio exceeding 2 (OR, 7.7), preoperative respiratory insufficiency (OR, 2.73), and a history of chronic steroid use (OR, 3.9), the researchers said. In addition, patients who died within 30 days after surgery were more likely than survivors to have undergone prolonged mechanical ventilation (56% vs. 27%), to have returned to the operating room (18% vs. 14%), to have acute renal failure (28% vs. 6%), or to have suffered a cardiac arrest that required cardiopulmonary resuscitation (18% vs. 7%). Survivors averaged about 2 fewer days in the hospital, compared with patients who died after surgery.
“The high morbidity and mortality of toxic colitis requires early and intensive medical management with IV [intravenous] steroids, antibiotics, decompressive maneuvers, and other resuscitative measures to treat the underlying cause,” they emphasized. “If there is no sign of improvement within 7 days or if there are any signs of deterioration, urgent surgical intervention should be considered.”
The link between female sex and mortality might reflect hormonal changes associated with menopause, but the study did not assess hormonal status or use of hormone therapy, the investigators noted. The association between chronic steroid use and postoperative death “is highly relevant” because long-term steroids are so often used in inflammatory bowel disease, they added. Clinical guidelines (Am J Gastroenterol. 2012 Feb;107:179-94) recommend that patients with acute severe ulcerative colitis proceed to second-line therapy or surgery if they do not respond to 3 days of intravenous steroids, because unnecessary delays can increase the risk of postoperative complications, they added.
The researchers reported no funding sources and had no disclosures.
Older age, female sex, preoperative chronic steroid use, azotemia, respiratory insufficiency, and coagulopathy all predicted death within a month of colectomy in patients with toxic colitis in the National Surgical Quality Improvement Project database.
The study is the largest to evaluate patients undergoing colectomy for toxic colitis, according to lead investigator Dr. Anand Dayama of the University of California, Davis, and his associates.
“In a case such as multiorgan failure with toxic colitis, the decision whether ... to operate can be an immensely difficult one,” Dr. Dayama and his colleagues wrote. “This study can help in making informed decisions in order to avoid the medicolegal ramifications of either performing an unnecessary procedure or withholding a lifesaving one,” they wrote in the American Journal of Surgery.
Surgical salvage remains the preferred treatment for patients with medically refractory toxic colitis. To assess outcomes in these patients, the researchers queried the National Surgical Quality Improvement Project database for relevant International Classification of Diseases, Ninth Revision codes between 2005 and 2012 (Am J Surg. 2015 Nov;210[5]:852-8).
The results underscored the severity of toxic colitis, they said. Of 189 patients, more than 26% died within 30 days after surgery, one in five developed postsurgical sepsis, about 17% had cardiovascular complications, 15% had wound complications, and 13% had renal complications. Furthermore, patients who were 70-80 years old had 3.5 times greater odds of dying, compared with younger patients (95% confidence interval, 1.0-12.8), and the increased likelihood of death rose by 22.2 when patients were older than 80 years (95% CI, 5.7-86.4).
Other baseline predictors of 30-day mortality included female sex (odds ratio, 4.1), blood urea nitrogen levels above 40 mg/dL (OR, 4.1), an international normalized ratio exceeding 2 (OR, 7.7), preoperative respiratory insufficiency (OR, 2.73), and a history of chronic steroid use (OR, 3.9), the researchers said. In addition, patients who died within 30 days after surgery were more likely than survivors to have undergone prolonged mechanical ventilation (56% vs. 27%), to have returned to the operating room (18% vs. 14%), to have acute renal failure (28% vs. 6%), or to have suffered a cardiac arrest that required cardiopulmonary resuscitation (18% vs. 7%). Survivors averaged about 2 fewer days in the hospital, compared with patients who died after surgery.
“The high morbidity and mortality of toxic colitis requires early and intensive medical management with IV [intravenous] steroids, antibiotics, decompressive maneuvers, and other resuscitative measures to treat the underlying cause,” they emphasized. “If there is no sign of improvement within 7 days or if there are any signs of deterioration, urgent surgical intervention should be considered.”
The link between female sex and mortality might reflect hormonal changes associated with menopause, but the study did not assess hormonal status or use of hormone therapy, the investigators noted. The association between chronic steroid use and postoperative death “is highly relevant” because long-term steroids are so often used in inflammatory bowel disease, they added. Clinical guidelines (Am J Gastroenterol. 2012 Feb;107:179-94) recommend that patients with acute severe ulcerative colitis proceed to second-line therapy or surgery if they do not respond to 3 days of intravenous steroids, because unnecessary delays can increase the risk of postoperative complications, they added.
The researchers reported no funding sources and had no disclosures.
FROM THE AMERICAN JOURNAL OF SURGERY
Key clinical point: Older age, female sex, preoperative azotemia, chronic steroid use, preoperative respiratory failure, and coagulopathy predicted adverse surgical outcomes in patients with toxic colitis.
Major finding: Odds ratios for these factors in the multivariate model ranged from 2.7 (preoperative respiratory failure) to 22.2 (age older than 80 years).
Data source: A multicenter prospective analysis of data from the National Surgical Quality Improvement Project.
Disclosures: The investigators reported no funding sources and had no disclosures.
ACS: Watchful waiting for some rectal cancers almost ready for ‘prime time’
CHICAGO – Watchful waiting with careful surveillance may become an option for the majority of locally advanced rectal cancer patients who have a complete clinical response to neoadjuvant therapy, according to a review of 442 rectal cancer patients at Memorial Sloan Kettering Cancer Center in New York.
Seventy-three of those patients had a complete clinical response to neoadjuvant therapy and opted for watchful waiting instead of surgery after weighing the risks and benefits – including about a 25% chance of local recurrence – with their doctors.
At 4 years’ follow-up, 54 (74%) remained cancer free. Nineteen patients had local tumor recurrence, generally within 13 months. Two of those patients had successful local excisions, and the remaining 17 had salvage total mesorectal excisions (TME).
There were no statistically significant differences in 4-year disease-specific and overall survival among the 73 patients and 72 other patients who opted for TME after neoadjuvant chemotherapy and were found to have had pathologic complete responses.
“In our cohort, watch and wait was safe. It’s an effective treatment strategy achieving a high rate of rectal preservation in tumors that respond to neoadjuvant therapy. I don’t think the rectum needs to come out in everybody,” said investigator Dr. J. Joshua Smith, a surgical oncologist at Sloan Kettering.
Several studies have reported similar results similar to the Sloan Kettering study, but other investigations have been retrospective, so optimal patient selection, assessment of response, surveillance protocols, and other matters remain uncertain. Sloan Kettering and about 20 other cancer centers in United States – all members of the Rectal Cancer Consortium – recently launched a randomized clinical trial to get a better handle on those issues.
Locally advanced rectal cancer patients will be randomized to either chemoradiation for 5.5 weeks followed by folinic acid, fluorouracil, and oxaliplatin (FOLFOX) or capecitabine and oxaliplatin (CapeOX) over about 16 weeks, or FOLFOX/CapeOX first and chemoradiation second. Those who have a significant clinical response will then undergo watchful waiting; those who do not will have TME.
About 50 patients have enrolled in the phase II trial so far; the investigators are looking for more than 200.
“I think ‘prime time for watchful waiting’ is around the corner, but not yet here. It must be preceded by a prospective trial.” Meanwhile, “how we define complete clinical response is important” when considering watchful waiting, Dr. Smith said at the annual clinical congress of the American College of Surgeons..
At Sloan Kettering, where watchful waiting has become more popular in recent years, complete clinical response means no tumor or lymph nodes on imaging, and, on digital rectal exam (DRE) and proctoscopy, normal flat mucosa, smooth induration, no mass, no nodules, no ulcerations, and no luminal narrowing; a pale scar and telangiectasias are okay.
In the first year, surveillance includes DRE and endoscopy every 3 months and imaging every 6 months. In the second year, DRE and endoscopy come every 4 months, and imaging again every 6 months. From years 3 to 5, DRE and endoscopy are done every 6 months, and imaging every 6-12 months. After 5 years, surveillance is by yearly DRE and endoscopy.
When discussing the option with patients, they need to know – besides the risk of recurrence – that watchful waiting is currently not standard medical management; surveillance must be frequent; they are at risk for a more extensive salvage TME than they might have had otherwise; and the approach might compromise the chance of a cure, Dr. Smith said.
Dr. Smith said he has no relevant disclosures.
CHICAGO – Watchful waiting with careful surveillance may become an option for the majority of locally advanced rectal cancer patients who have a complete clinical response to neoadjuvant therapy, according to a review of 442 rectal cancer patients at Memorial Sloan Kettering Cancer Center in New York.
Seventy-three of those patients had a complete clinical response to neoadjuvant therapy and opted for watchful waiting instead of surgery after weighing the risks and benefits – including about a 25% chance of local recurrence – with their doctors.
At 4 years’ follow-up, 54 (74%) remained cancer free. Nineteen patients had local tumor recurrence, generally within 13 months. Two of those patients had successful local excisions, and the remaining 17 had salvage total mesorectal excisions (TME).
There were no statistically significant differences in 4-year disease-specific and overall survival among the 73 patients and 72 other patients who opted for TME after neoadjuvant chemotherapy and were found to have had pathologic complete responses.
“In our cohort, watch and wait was safe. It’s an effective treatment strategy achieving a high rate of rectal preservation in tumors that respond to neoadjuvant therapy. I don’t think the rectum needs to come out in everybody,” said investigator Dr. J. Joshua Smith, a surgical oncologist at Sloan Kettering.
Several studies have reported similar results similar to the Sloan Kettering study, but other investigations have been retrospective, so optimal patient selection, assessment of response, surveillance protocols, and other matters remain uncertain. Sloan Kettering and about 20 other cancer centers in United States – all members of the Rectal Cancer Consortium – recently launched a randomized clinical trial to get a better handle on those issues.
Locally advanced rectal cancer patients will be randomized to either chemoradiation for 5.5 weeks followed by folinic acid, fluorouracil, and oxaliplatin (FOLFOX) or capecitabine and oxaliplatin (CapeOX) over about 16 weeks, or FOLFOX/CapeOX first and chemoradiation second. Those who have a significant clinical response will then undergo watchful waiting; those who do not will have TME.
About 50 patients have enrolled in the phase II trial so far; the investigators are looking for more than 200.
“I think ‘prime time for watchful waiting’ is around the corner, but not yet here. It must be preceded by a prospective trial.” Meanwhile, “how we define complete clinical response is important” when considering watchful waiting, Dr. Smith said at the annual clinical congress of the American College of Surgeons..
At Sloan Kettering, where watchful waiting has become more popular in recent years, complete clinical response means no tumor or lymph nodes on imaging, and, on digital rectal exam (DRE) and proctoscopy, normal flat mucosa, smooth induration, no mass, no nodules, no ulcerations, and no luminal narrowing; a pale scar and telangiectasias are okay.
In the first year, surveillance includes DRE and endoscopy every 3 months and imaging every 6 months. In the second year, DRE and endoscopy come every 4 months, and imaging again every 6 months. From years 3 to 5, DRE and endoscopy are done every 6 months, and imaging every 6-12 months. After 5 years, surveillance is by yearly DRE and endoscopy.
When discussing the option with patients, they need to know – besides the risk of recurrence – that watchful waiting is currently not standard medical management; surveillance must be frequent; they are at risk for a more extensive salvage TME than they might have had otherwise; and the approach might compromise the chance of a cure, Dr. Smith said.
Dr. Smith said he has no relevant disclosures.
CHICAGO – Watchful waiting with careful surveillance may become an option for the majority of locally advanced rectal cancer patients who have a complete clinical response to neoadjuvant therapy, according to a review of 442 rectal cancer patients at Memorial Sloan Kettering Cancer Center in New York.
Seventy-three of those patients had a complete clinical response to neoadjuvant therapy and opted for watchful waiting instead of surgery after weighing the risks and benefits – including about a 25% chance of local recurrence – with their doctors.
At 4 years’ follow-up, 54 (74%) remained cancer free. Nineteen patients had local tumor recurrence, generally within 13 months. Two of those patients had successful local excisions, and the remaining 17 had salvage total mesorectal excisions (TME).
There were no statistically significant differences in 4-year disease-specific and overall survival among the 73 patients and 72 other patients who opted for TME after neoadjuvant chemotherapy and were found to have had pathologic complete responses.
“In our cohort, watch and wait was safe. It’s an effective treatment strategy achieving a high rate of rectal preservation in tumors that respond to neoadjuvant therapy. I don’t think the rectum needs to come out in everybody,” said investigator Dr. J. Joshua Smith, a surgical oncologist at Sloan Kettering.
Several studies have reported similar results similar to the Sloan Kettering study, but other investigations have been retrospective, so optimal patient selection, assessment of response, surveillance protocols, and other matters remain uncertain. Sloan Kettering and about 20 other cancer centers in United States – all members of the Rectal Cancer Consortium – recently launched a randomized clinical trial to get a better handle on those issues.
Locally advanced rectal cancer patients will be randomized to either chemoradiation for 5.5 weeks followed by folinic acid, fluorouracil, and oxaliplatin (FOLFOX) or capecitabine and oxaliplatin (CapeOX) over about 16 weeks, or FOLFOX/CapeOX first and chemoradiation second. Those who have a significant clinical response will then undergo watchful waiting; those who do not will have TME.
About 50 patients have enrolled in the phase II trial so far; the investigators are looking for more than 200.
“I think ‘prime time for watchful waiting’ is around the corner, but not yet here. It must be preceded by a prospective trial.” Meanwhile, “how we define complete clinical response is important” when considering watchful waiting, Dr. Smith said at the annual clinical congress of the American College of Surgeons..
At Sloan Kettering, where watchful waiting has become more popular in recent years, complete clinical response means no tumor or lymph nodes on imaging, and, on digital rectal exam (DRE) and proctoscopy, normal flat mucosa, smooth induration, no mass, no nodules, no ulcerations, and no luminal narrowing; a pale scar and telangiectasias are okay.
In the first year, surveillance includes DRE and endoscopy every 3 months and imaging every 6 months. In the second year, DRE and endoscopy come every 4 months, and imaging again every 6 months. From years 3 to 5, DRE and endoscopy are done every 6 months, and imaging every 6-12 months. After 5 years, surveillance is by yearly DRE and endoscopy.
When discussing the option with patients, they need to know – besides the risk of recurrence – that watchful waiting is currently not standard medical management; surveillance must be frequent; they are at risk for a more extensive salvage TME than they might have had otherwise; and the approach might compromise the chance of a cure, Dr. Smith said.
Dr. Smith said he has no relevant disclosures.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Organ preservation seems to be a valid option when locally advanced rectal cancers respond completely to neoadjuvant therapy.
Major finding: Almost three-quarters of 73 patients who opted for watchful waiting after complete clinical responses to neodjuvant therapy remained cancer free at 4 years.
Data source: Review of 442 patients at Memorial Sloan Kettering Cancer Center.
Disclosures: The presenting investigator has no relevant financial disclosures.
ACS: No clear answers to black patients’ worse rectal cancer outcomes
CHICAGO – Access to equal care decreases but does not eliminate the survival disparities between black and white patients with rectal cancer, according to investigators from the University of Cincinnati, Ohio.
After rigorous propensity score matching of thousands of black and white patients for patient, disease, and treatment characteristics, median survival was 109.6 months among white patients and 85.8 months among black patients (J Am Coll Surg. 2015 Nov [doi: 10.1016/j.jamcollsurg.2015.07.056]).
“Blacks have worse outcomes, but we don’t have a clear explanation,” explained investigator and surgery resident Dr. Meghan Nolan. For now, the findings suggest that it might be a good idea to start screening black patients before age 50 years, perhaps even as early as age 40 years.
“We are urging people to screen at a lower age in black patients,” Dr. Nolan said at the annual clinical congress of the American College of Surgeons.
Racial disparities in rectal cancer are well known. The investigators wanted to see if they simply are because of unequal access to care, so they analyzed 178,414 white and 18,385 black patients in the National Cancer Data Base from 1998 to 2006.
Mean 5-year survival for blacks was 50.7%, compared with 56.2% for whites, and black patients were more likely to present with stage IV disease. Such findings aren’t new, the investigators noted.
To account for the difference in late-stage presentation, the investigators limited their analysis to patients with stage I-III rectal cancer. But even then, 5-year survival was 66.7% among whites and 58.7% among blacks.
That might have had something to do with the fact 85% of white patients, but only 78% of black patients, had surgery for those potentially curable lower-stage tumors. Among those who didn’t undergo surgery, patient refusal was slightly more common among black patients than white patients, which suggests that “cultural factors may be playing a role” in the surgery disparity, Dr. Nolan said.
The investigators controlled for the different surgery rates by limiting their analysis to stage I-III patients who had appropriate operations. The survival gap narrowed but did not disappear: 65.8% of white patients were alive at 5 years, compared with 61% of black patients. Blacks were also more likely to have positive margins on pathology. “I’m not sure why. That was a surprise,” Dr. Nolan said.
The propensity score matching led the team to conclude that there’s more at work than differences in access to care. A total of 7,569 pairs of black and white patients were matched for age at diagnosis, gender, insurance coverage, income, education, facility type, tumor stage, Charlson-Deyo score, surgical management, margin status, and other potential confounders.
Every matched patient completed their recommended therapy, and there was no statistical difference between matched black and white patients who received appropriate, stage-specific chemoradiation. Still, the survival differences persisted.
Dr. Nolan had no relevant disclosures.
CHICAGO – Access to equal care decreases but does not eliminate the survival disparities between black and white patients with rectal cancer, according to investigators from the University of Cincinnati, Ohio.
After rigorous propensity score matching of thousands of black and white patients for patient, disease, and treatment characteristics, median survival was 109.6 months among white patients and 85.8 months among black patients (J Am Coll Surg. 2015 Nov [doi: 10.1016/j.jamcollsurg.2015.07.056]).
“Blacks have worse outcomes, but we don’t have a clear explanation,” explained investigator and surgery resident Dr. Meghan Nolan. For now, the findings suggest that it might be a good idea to start screening black patients before age 50 years, perhaps even as early as age 40 years.
“We are urging people to screen at a lower age in black patients,” Dr. Nolan said at the annual clinical congress of the American College of Surgeons.
Racial disparities in rectal cancer are well known. The investigators wanted to see if they simply are because of unequal access to care, so they analyzed 178,414 white and 18,385 black patients in the National Cancer Data Base from 1998 to 2006.
Mean 5-year survival for blacks was 50.7%, compared with 56.2% for whites, and black patients were more likely to present with stage IV disease. Such findings aren’t new, the investigators noted.
To account for the difference in late-stage presentation, the investigators limited their analysis to patients with stage I-III rectal cancer. But even then, 5-year survival was 66.7% among whites and 58.7% among blacks.
That might have had something to do with the fact 85% of white patients, but only 78% of black patients, had surgery for those potentially curable lower-stage tumors. Among those who didn’t undergo surgery, patient refusal was slightly more common among black patients than white patients, which suggests that “cultural factors may be playing a role” in the surgery disparity, Dr. Nolan said.
The investigators controlled for the different surgery rates by limiting their analysis to stage I-III patients who had appropriate operations. The survival gap narrowed but did not disappear: 65.8% of white patients were alive at 5 years, compared with 61% of black patients. Blacks were also more likely to have positive margins on pathology. “I’m not sure why. That was a surprise,” Dr. Nolan said.
The propensity score matching led the team to conclude that there’s more at work than differences in access to care. A total of 7,569 pairs of black and white patients were matched for age at diagnosis, gender, insurance coverage, income, education, facility type, tumor stage, Charlson-Deyo score, surgical management, margin status, and other potential confounders.
Every matched patient completed their recommended therapy, and there was no statistical difference between matched black and white patients who received appropriate, stage-specific chemoradiation. Still, the survival differences persisted.
Dr. Nolan had no relevant disclosures.
CHICAGO – Access to equal care decreases but does not eliminate the survival disparities between black and white patients with rectal cancer, according to investigators from the University of Cincinnati, Ohio.
After rigorous propensity score matching of thousands of black and white patients for patient, disease, and treatment characteristics, median survival was 109.6 months among white patients and 85.8 months among black patients (J Am Coll Surg. 2015 Nov [doi: 10.1016/j.jamcollsurg.2015.07.056]).
“Blacks have worse outcomes, but we don’t have a clear explanation,” explained investigator and surgery resident Dr. Meghan Nolan. For now, the findings suggest that it might be a good idea to start screening black patients before age 50 years, perhaps even as early as age 40 years.
“We are urging people to screen at a lower age in black patients,” Dr. Nolan said at the annual clinical congress of the American College of Surgeons.
Racial disparities in rectal cancer are well known. The investigators wanted to see if they simply are because of unequal access to care, so they analyzed 178,414 white and 18,385 black patients in the National Cancer Data Base from 1998 to 2006.
Mean 5-year survival for blacks was 50.7%, compared with 56.2% for whites, and black patients were more likely to present with stage IV disease. Such findings aren’t new, the investigators noted.
To account for the difference in late-stage presentation, the investigators limited their analysis to patients with stage I-III rectal cancer. But even then, 5-year survival was 66.7% among whites and 58.7% among blacks.
That might have had something to do with the fact 85% of white patients, but only 78% of black patients, had surgery for those potentially curable lower-stage tumors. Among those who didn’t undergo surgery, patient refusal was slightly more common among black patients than white patients, which suggests that “cultural factors may be playing a role” in the surgery disparity, Dr. Nolan said.
The investigators controlled for the different surgery rates by limiting their analysis to stage I-III patients who had appropriate operations. The survival gap narrowed but did not disappear: 65.8% of white patients were alive at 5 years, compared with 61% of black patients. Blacks were also more likely to have positive margins on pathology. “I’m not sure why. That was a surprise,” Dr. Nolan said.
The propensity score matching led the team to conclude that there’s more at work than differences in access to care. A total of 7,569 pairs of black and white patients were matched for age at diagnosis, gender, insurance coverage, income, education, facility type, tumor stage, Charlson-Deyo score, surgical management, margin status, and other potential confounders.
Every matched patient completed their recommended therapy, and there was no statistical difference between matched black and white patients who received appropriate, stage-specific chemoradiation. Still, the survival differences persisted.
Dr. Nolan had no relevant disclosures.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Screen black patients for rectal cancer before the age of 50.
Major finding: Even with rigorous propensity score matching, median survival was 109.6 months among white patients and 85.8 months among black patients with rectal cancer.
Data source: Review of almost 200,000 rectal cancer patients in the National Cancer Data Base.
Disclosures: Dr. Nolan had no relevant disclosures.
ACS: Loop ileostomy may give IBD colitis patients an alternative to urgent colectomy
CHICAGO – Diverting loop ileostomy may be a better option than urgent colectomy as the first surgical step for medically refractory severe ulcerative colitis and Crohn’s disease.
Investigators from the University of California, Los Angeles, have found that ileostomy gives patients a chance to recover from their acute illness – and their colons a chance to heal – so they’re in better shape for definitive surgery further down the road, if it’s even needed (J Am Coll Surg. 2015 Oct;221[4]:S37-S38).
“Urgent colectomy is standard practice for medically refractory severe ulcerative and Crohn’s colitis. However, immunosuppression and malnutrition can result in significant morbidity. This change in management strategy does not eliminate the potential need for definitive surgery, but it does allow for the more extensive procedure to be performed in an elective setting under optimized conditions, thereby improving clinical outcomes,” said the investigators, led by Dr. Amy Lightner, formerly of UCLA but now a colorectal surgery fellow at the Mayo Clinic in Rochester, Minn.
There were just eight patients in the series, so the results are tentative. Six had ulcerative colitis (UC) and two had Crohn’s disease (CD). On presentation, the patients were tachycardic, febrile, malnourished, and anemic, with severe mucosal disease confirmed by endoscopy. Steroids, immunomodulators, and biologics no longer helped. Overall, the patients were too sick to go home, but not quite sick enough for the ICU. Their average age was 29 years.
They underwent a single-incision, laparoscopic diverting loop ileostomy, which took about 45 minutes. The technique, and perhaps the thinking behind it, are similar to one gaining popularity for Clostridium difficile colitis, but without the colonic lavage.
Within 24-48 hours postop, tachycardia and fevers resolved, and patients tolerated oral intake. Narcotic use dropped, and bloody stools became less frequent, and then ceased in all but one patient. Within a month, the average hemoglobin level had climbed from a baseline of 9 g/dL to 11.5 g/dL, and average albumin from 2.5 g/dL to 4 g/dL. Within 2 months, patients’ bowels looked pink and healthy on repeat endoscopy.
“It was a remarkable turnaround. Within 48 hours, they looked markedly different. We are having very good results with this, and it’s much better for patients” than is colectomy during acute illness. “It’s a good change in management,” Dr. Lightner said.
After months of follow-up, two patients, one with UC and one with CD, haven’t needed a colectomy and are maintained on biologics. The other UC patients have had ileal pouch-anal anastomosis. The other CD patient had a subsequent ileorectal anastomosis. Patients were able to undergo those procedures laparoscopically and “have done really well,” Dr. Lightner said.
It’s unclear why loop ileostomy seems so helpful. Perhaps it has something to do with shifts in bacterial populations or decompression of the colon. Maybe it’s just about giving the colon a rest, she said.
The investigators will continue to study the approach. Since the initial report, 8 more patients have joined the series, for a current total of 16. “We are still seeing good results,” Dr. Lightner said.
Dr. Lightner has no disclosures, and there was no outside funding for the work.
These patients are challenging. Often, they are on multiple immunomodulators and are malnourished and anemic, with systemic manifestations of inflammatory disease. The abdomen may be hostile. None of these are favorable factors for doing a total abdominal colectomy, but that remains the standard even today.
This is truly a feasibility or pilot study, and as such, it’s difficult to draw definitive conclusions. Cost-effectiveness is unclear, and some patients are maintained on biologics when, in fact, they may have had a curative procedure with surgery. The follow-up isn’t long enough to look at recurrence of colitis. Nevertheless, it certainly is an intriguing and perhaps revolutionary approach to treating these patients.
Dr. Sean C. Glasgow is a colorectal surgeon and assistant professor of surgery at Washington University in St. Louis. He was not involved with the study.
These patients are challenging. Often, they are on multiple immunomodulators and are malnourished and anemic, with systemic manifestations of inflammatory disease. The abdomen may be hostile. None of these are favorable factors for doing a total abdominal colectomy, but that remains the standard even today.
This is truly a feasibility or pilot study, and as such, it’s difficult to draw definitive conclusions. Cost-effectiveness is unclear, and some patients are maintained on biologics when, in fact, they may have had a curative procedure with surgery. The follow-up isn’t long enough to look at recurrence of colitis. Nevertheless, it certainly is an intriguing and perhaps revolutionary approach to treating these patients.
Dr. Sean C. Glasgow is a colorectal surgeon and assistant professor of surgery at Washington University in St. Louis. He was not involved with the study.
These patients are challenging. Often, they are on multiple immunomodulators and are malnourished and anemic, with systemic manifestations of inflammatory disease. The abdomen may be hostile. None of these are favorable factors for doing a total abdominal colectomy, but that remains the standard even today.
This is truly a feasibility or pilot study, and as such, it’s difficult to draw definitive conclusions. Cost-effectiveness is unclear, and some patients are maintained on biologics when, in fact, they may have had a curative procedure with surgery. The follow-up isn’t long enough to look at recurrence of colitis. Nevertheless, it certainly is an intriguing and perhaps revolutionary approach to treating these patients.
Dr. Sean C. Glasgow is a colorectal surgeon and assistant professor of surgery at Washington University in St. Louis. He was not involved with the study.
CHICAGO – Diverting loop ileostomy may be a better option than urgent colectomy as the first surgical step for medically refractory severe ulcerative colitis and Crohn’s disease.
Investigators from the University of California, Los Angeles, have found that ileostomy gives patients a chance to recover from their acute illness – and their colons a chance to heal – so they’re in better shape for definitive surgery further down the road, if it’s even needed (J Am Coll Surg. 2015 Oct;221[4]:S37-S38).
“Urgent colectomy is standard practice for medically refractory severe ulcerative and Crohn’s colitis. However, immunosuppression and malnutrition can result in significant morbidity. This change in management strategy does not eliminate the potential need for definitive surgery, but it does allow for the more extensive procedure to be performed in an elective setting under optimized conditions, thereby improving clinical outcomes,” said the investigators, led by Dr. Amy Lightner, formerly of UCLA but now a colorectal surgery fellow at the Mayo Clinic in Rochester, Minn.
There were just eight patients in the series, so the results are tentative. Six had ulcerative colitis (UC) and two had Crohn’s disease (CD). On presentation, the patients were tachycardic, febrile, malnourished, and anemic, with severe mucosal disease confirmed by endoscopy. Steroids, immunomodulators, and biologics no longer helped. Overall, the patients were too sick to go home, but not quite sick enough for the ICU. Their average age was 29 years.
They underwent a single-incision, laparoscopic diverting loop ileostomy, which took about 45 minutes. The technique, and perhaps the thinking behind it, are similar to one gaining popularity for Clostridium difficile colitis, but without the colonic lavage.
Within 24-48 hours postop, tachycardia and fevers resolved, and patients tolerated oral intake. Narcotic use dropped, and bloody stools became less frequent, and then ceased in all but one patient. Within a month, the average hemoglobin level had climbed from a baseline of 9 g/dL to 11.5 g/dL, and average albumin from 2.5 g/dL to 4 g/dL. Within 2 months, patients’ bowels looked pink and healthy on repeat endoscopy.
“It was a remarkable turnaround. Within 48 hours, they looked markedly different. We are having very good results with this, and it’s much better for patients” than is colectomy during acute illness. “It’s a good change in management,” Dr. Lightner said.
After months of follow-up, two patients, one with UC and one with CD, haven’t needed a colectomy and are maintained on biologics. The other UC patients have had ileal pouch-anal anastomosis. The other CD patient had a subsequent ileorectal anastomosis. Patients were able to undergo those procedures laparoscopically and “have done really well,” Dr. Lightner said.
It’s unclear why loop ileostomy seems so helpful. Perhaps it has something to do with shifts in bacterial populations or decompression of the colon. Maybe it’s just about giving the colon a rest, she said.
The investigators will continue to study the approach. Since the initial report, 8 more patients have joined the series, for a current total of 16. “We are still seeing good results,” Dr. Lightner said.
Dr. Lightner has no disclosures, and there was no outside funding for the work.
CHICAGO – Diverting loop ileostomy may be a better option than urgent colectomy as the first surgical step for medically refractory severe ulcerative colitis and Crohn’s disease.
Investigators from the University of California, Los Angeles, have found that ileostomy gives patients a chance to recover from their acute illness – and their colons a chance to heal – so they’re in better shape for definitive surgery further down the road, if it’s even needed (J Am Coll Surg. 2015 Oct;221[4]:S37-S38).
“Urgent colectomy is standard practice for medically refractory severe ulcerative and Crohn’s colitis. However, immunosuppression and malnutrition can result in significant morbidity. This change in management strategy does not eliminate the potential need for definitive surgery, but it does allow for the more extensive procedure to be performed in an elective setting under optimized conditions, thereby improving clinical outcomes,” said the investigators, led by Dr. Amy Lightner, formerly of UCLA but now a colorectal surgery fellow at the Mayo Clinic in Rochester, Minn.
There were just eight patients in the series, so the results are tentative. Six had ulcerative colitis (UC) and two had Crohn’s disease (CD). On presentation, the patients were tachycardic, febrile, malnourished, and anemic, with severe mucosal disease confirmed by endoscopy. Steroids, immunomodulators, and biologics no longer helped. Overall, the patients were too sick to go home, but not quite sick enough for the ICU. Their average age was 29 years.
They underwent a single-incision, laparoscopic diverting loop ileostomy, which took about 45 minutes. The technique, and perhaps the thinking behind it, are similar to one gaining popularity for Clostridium difficile colitis, but without the colonic lavage.
Within 24-48 hours postop, tachycardia and fevers resolved, and patients tolerated oral intake. Narcotic use dropped, and bloody stools became less frequent, and then ceased in all but one patient. Within a month, the average hemoglobin level had climbed from a baseline of 9 g/dL to 11.5 g/dL, and average albumin from 2.5 g/dL to 4 g/dL. Within 2 months, patients’ bowels looked pink and healthy on repeat endoscopy.
“It was a remarkable turnaround. Within 48 hours, they looked markedly different. We are having very good results with this, and it’s much better for patients” than is colectomy during acute illness. “It’s a good change in management,” Dr. Lightner said.
After months of follow-up, two patients, one with UC and one with CD, haven’t needed a colectomy and are maintained on biologics. The other UC patients have had ileal pouch-anal anastomosis. The other CD patient had a subsequent ileorectal anastomosis. Patients were able to undergo those procedures laparoscopically and “have done really well,” Dr. Lightner said.
It’s unclear why loop ileostomy seems so helpful. Perhaps it has something to do with shifts in bacterial populations or decompression of the colon. Maybe it’s just about giving the colon a rest, she said.
The investigators will continue to study the approach. Since the initial report, 8 more patients have joined the series, for a current total of 16. “We are still seeing good results,” Dr. Lightner said.
Dr. Lightner has no disclosures, and there was no outside funding for the work.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Patients with refractory inflammatory bowel disease may benefit from loop ileostomy in lieu of urgent colectomy as a first surgical step.
Major finding: Within 24-48 hours after diverting loop ileostomy, tachycardia and fevers resolved, and patients tolerated oral intake. Narcotic use dropped, and bloody stools became less frequent, then ceased.
Data source: Pilot study in eight patients with refractory inflammatory bowel disease
Disclosures: The lead investigator has no disclosures, and there was no outside funding for the work.
VIDEO: A better option for C. difficile toxic megacolon
CHICAGO – Last-minute colectomy isn’t the way to go for Clostridium difficile–induced toxic megacolon; outcomes are better with a timely loop ileostomy and colonic lavage.
University of Pittsburgh surgery professor Dr. Brian Zuckerbraun, a pioneer of the technique, explained the procedure and its benefits in an interview at the annual Clinical Congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Last-minute colectomy isn’t the way to go for Clostridium difficile–induced toxic megacolon; outcomes are better with a timely loop ileostomy and colonic lavage.
University of Pittsburgh surgery professor Dr. Brian Zuckerbraun, a pioneer of the technique, explained the procedure and its benefits in an interview at the annual Clinical Congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Last-minute colectomy isn’t the way to go for Clostridium difficile–induced toxic megacolon; outcomes are better with a timely loop ileostomy and colonic lavage.
University of Pittsburgh surgery professor Dr. Brian Zuckerbraun, a pioneer of the technique, explained the procedure and its benefits in an interview at the annual Clinical Congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE ACS CLINICAL CONGRESS
VIDEO: Dialysis-dependent patients face rocky road after colorectal surgery
CHICAGO – The odds of emergency surgery were sevenfold higher in dialysis-dependent patients undergoing colorectal surgery than patients with renal insufficiency not on dialysis or those with normal renal function.
Dialysis patients were also far less likely to undergo laparoscopic surgery and to be rescued from death if they experienced a complication.
These are just some of the results of a retrospective study involving 156,645 elective colorectal surgery cases selected as a poster of exceptional merit here at the annual clinical congress of the American College of Surgeons.
Dialysis patients are known to be at high risk for postoperative complications, but few studies have evaluated outcomes after colorectal surgery in these patients or distinguished them from patients with non–dialysis dependent renal insufficiency (NDDRI) or normal renal function (NRF), observed study author Dr. Isibor Arhuidese of Johns Hopkins University in Baltimore.
Indeed, when the researchers compared these three groups, perioperative mortality and morbidity after elective colorectal surgery was the worst in dialysis patients.
Absolute perioperative mortality was highest for dialysis patients vs. NDDRI and NRF patients after open (13.4% vs. 4.8% vs. 2%; P less than .001) and laparoscopic (8% vs. 2% vs. 0.6%; P less than .001) surgery.
Three complications were significantly associated with death in dialysis patients: myocardial infarction (adjusted odds ratio, 48.6; P = .027), bleeding (aOR, 14.5; P = .025), and sepsis or septic shock (aOR, 8.7; P = .001).
It is not enough to simply identify dialysis dependence as a predictor of poor outcomes, but one must identify targets for improvement in surgical care, Dr. Arhuidese stressed.
Dr. Arhuidese reported having no relevant conflicts of interest.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @pwendl
CHICAGO – The odds of emergency surgery were sevenfold higher in dialysis-dependent patients undergoing colorectal surgery than patients with renal insufficiency not on dialysis or those with normal renal function.
Dialysis patients were also far less likely to undergo laparoscopic surgery and to be rescued from death if they experienced a complication.
These are just some of the results of a retrospective study involving 156,645 elective colorectal surgery cases selected as a poster of exceptional merit here at the annual clinical congress of the American College of Surgeons.
Dialysis patients are known to be at high risk for postoperative complications, but few studies have evaluated outcomes after colorectal surgery in these patients or distinguished them from patients with non–dialysis dependent renal insufficiency (NDDRI) or normal renal function (NRF), observed study author Dr. Isibor Arhuidese of Johns Hopkins University in Baltimore.
Indeed, when the researchers compared these three groups, perioperative mortality and morbidity after elective colorectal surgery was the worst in dialysis patients.
Absolute perioperative mortality was highest for dialysis patients vs. NDDRI and NRF patients after open (13.4% vs. 4.8% vs. 2%; P less than .001) and laparoscopic (8% vs. 2% vs. 0.6%; P less than .001) surgery.
Three complications were significantly associated with death in dialysis patients: myocardial infarction (adjusted odds ratio, 48.6; P = .027), bleeding (aOR, 14.5; P = .025), and sepsis or septic shock (aOR, 8.7; P = .001).
It is not enough to simply identify dialysis dependence as a predictor of poor outcomes, but one must identify targets for improvement in surgical care, Dr. Arhuidese stressed.
Dr. Arhuidese reported having no relevant conflicts of interest.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @pwendl
CHICAGO – The odds of emergency surgery were sevenfold higher in dialysis-dependent patients undergoing colorectal surgery than patients with renal insufficiency not on dialysis or those with normal renal function.
Dialysis patients were also far less likely to undergo laparoscopic surgery and to be rescued from death if they experienced a complication.
These are just some of the results of a retrospective study involving 156,645 elective colorectal surgery cases selected as a poster of exceptional merit here at the annual clinical congress of the American College of Surgeons.
Dialysis patients are known to be at high risk for postoperative complications, but few studies have evaluated outcomes after colorectal surgery in these patients or distinguished them from patients with non–dialysis dependent renal insufficiency (NDDRI) or normal renal function (NRF), observed study author Dr. Isibor Arhuidese of Johns Hopkins University in Baltimore.
Indeed, when the researchers compared these three groups, perioperative mortality and morbidity after elective colorectal surgery was the worst in dialysis patients.
Absolute perioperative mortality was highest for dialysis patients vs. NDDRI and NRF patients after open (13.4% vs. 4.8% vs. 2%; P less than .001) and laparoscopic (8% vs. 2% vs. 0.6%; P less than .001) surgery.
Three complications were significantly associated with death in dialysis patients: myocardial infarction (adjusted odds ratio, 48.6; P = .027), bleeding (aOR, 14.5; P = .025), and sepsis or septic shock (aOR, 8.7; P = .001).
It is not enough to simply identify dialysis dependence as a predictor of poor outcomes, but one must identify targets for improvement in surgical care, Dr. Arhuidese stressed.
Dr. Arhuidese reported having no relevant conflicts of interest.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @pwendl
AT THE ACS CLINICAL CONGRESS
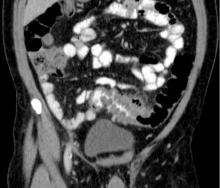
Lavage does not reduce severe complications in perforated diverticulitis
Patients needing emergency surgery for perforated diverticulitis saw no decrease in serious complications when treated with laparoscopic lavage, a minimally invasive procedure, than with primary resection of the colon, according to results from a randomized multicenter trial in Scandinavia.
Likelihood of reoperation also was significantly higher among patients undergoing laparoscopic lavage, and more sigmoid carcinomas were missed.
For their research, published Oct. 6 in JAMA (2015;314:1364-75), a group led by Dr. Johannes Kurt Schultz of the Akershus University Hospital in Lørenskog, Norway, and the University of Oslo sought to eliminate the selection bias that may have contributed to more favorable outcomes associated with laparoscopic lavage in observational studies.
Dr. Schultz and colleagues randomized patients with suspected perforated diverticulitis from 21 centers in Sweden and Norway to laparoscopic peritoneal lavage (n = 101) or colon resection (n = 98), with the choice of open or laparoscopic approach used for resection, as well as the option of colorectal anastomosis, left to the surgeon.
The study did not use laparoscopic Hinchey staging to classify the severity of the perforation prior to treatment assignment as a way of reducing the selection bias that may have occurred in observational studies.
The preoperative randomization resulted in both groups having similar rates of feculent peritonitis and incorrect preoperative diagnoses. Patients assigned to laparoscopic lavage were treated instead with resection if they were found to have fecal peritonitis. Also, patients in both groups whose pathology required additional treatment were treated at surgeon discretion. This left 74 patients randomized to lavage who received it as assigned and 70 patients undergoing resection per assigned protocol. In the intention-to-treat analysis, 31% of patients in the lavage group and 26% of patients in the resection group saw severe postoperative complications within 90 days, a difference of 4.7% that did not reach statistical significance (95% confidence interval, −7.9% to 17%; P = .53). Severe postoperative complications were defined as any complications resulting in a reintervention requiring general anesthesia, a life-threatening organ dysfunction, or death.
Of the patients treated as assigned with lavage, about 20% (n = 15) required reoperation, compared with 6% (n = 4) in the resection arm, a difference of about 14.6% (95% CI, 3.5% to 25.6%; P =.01).
The main reasons for reoperation were secondary peritonitis in the lavage group and wound rupture in the resection group. Intra-abdominal infections were more frequent in the laparoscopic lavage group, Dr. Schultz and colleagues found.
Also in the lavage group, four carcinomas were missed, compared with two in the resection group. “Because of the relatively high rate of missed colon carcinomas in the lavage group, it was essential to perform a colonoscopy after a patient recovered from the perforation,” the researchers wrote in their analysis.
Although patients in the laparoscopic lavage group had significantly shorter operating times, less blood loss, and lower incidence of stoma at 3 months, the researchers concluded that, based on these results, laparoscopic lavage could not be supported in perforated diverticulitis.
Dr. Schultz and colleagues had planned to enroll about half of eligible patients at the study sites. They noted as a limitation of their study that those not enrolled had more severe disease and worse postoperative outcomes, raising the possibility that the results “may not pertain to patients with perforated diverticulitis who are very ill.”
The study was funded by the South-Eastern Norway Regional Health Authority and Akershus University Hospital. None of its authors reported conflicts of interest.
Dr. Schultz and associates detail findings from a randomized, multicenter clinical trial conducted in Scandinavia designed to assess the superiority of laparoscopic lavage plus drainage, compared with laparoscopic or open resection with or without anastomosis for diverticulitis (Hinchey grades I-III) requiring urgent surgery.
The primary outcome was the incidence of severe complications (Clavien-Dindo classification IIIb-V). Of 144 patients, 74 were randomized to receive laparoscopic lavage and 70 to resection. The two groups were similar in characteristics, although significantly fewer of the lavage procedures were performed by a specialty-trained surgeon. Severe complications occurred in 25.7% of patients in the lavage group and 14.3% in the resection group (difference, 11.4%; 95% CI, −1.8 to 24.1), and significantly more patients in the lavage group developed secondary peritonitis (12% vs. 0%) or returned to the operating room (20% vs. 6%). The hospital mortality rates and follow-up quality-of-life scores were comparable between the groups (3% vs. 4% and 0.75 vs. 0.73, respectively). Somewhat worrisome is that four colon cancers were initially missed in patients treated by laparoscopic lavage alone.
Performing laparoscopic lavage is more difficult than merely irrigating the abdomen and placing drains within the pelvis. Surgeons vary in their attitudes related to concomitant adhesiolysis or debridement, and consensus about these procedures is lacking. Furthermore, subjective signs and objective criteria that identify patients at risk for secondary peritonitis or reoperation must be studied, and risk models should be validated to determine which patients are best suited for this less invasive approach. The utility of less intrusive strategies and minimally invasive approaches will undoubtedly expand as technologies evolve, but they must be responsibly incorporated into surgical practice based on evidence rather than subjective reasons.
Dr. Scott A. Strong and Dr. Nathaniel J. Soper are with Northwestern University, Chicago. These comments were taken from an accompanying editorial (JAMA 2015;314[13]:1343-5). They declared no conflicts of interest.
Dr. Schultz and associates detail findings from a randomized, multicenter clinical trial conducted in Scandinavia designed to assess the superiority of laparoscopic lavage plus drainage, compared with laparoscopic or open resection with or without anastomosis for diverticulitis (Hinchey grades I-III) requiring urgent surgery.
The primary outcome was the incidence of severe complications (Clavien-Dindo classification IIIb-V). Of 144 patients, 74 were randomized to receive laparoscopic lavage and 70 to resection. The two groups were similar in characteristics, although significantly fewer of the lavage procedures were performed by a specialty-trained surgeon. Severe complications occurred in 25.7% of patients in the lavage group and 14.3% in the resection group (difference, 11.4%; 95% CI, −1.8 to 24.1), and significantly more patients in the lavage group developed secondary peritonitis (12% vs. 0%) or returned to the operating room (20% vs. 6%). The hospital mortality rates and follow-up quality-of-life scores were comparable between the groups (3% vs. 4% and 0.75 vs. 0.73, respectively). Somewhat worrisome is that four colon cancers were initially missed in patients treated by laparoscopic lavage alone.
Performing laparoscopic lavage is more difficult than merely irrigating the abdomen and placing drains within the pelvis. Surgeons vary in their attitudes related to concomitant adhesiolysis or debridement, and consensus about these procedures is lacking. Furthermore, subjective signs and objective criteria that identify patients at risk for secondary peritonitis or reoperation must be studied, and risk models should be validated to determine which patients are best suited for this less invasive approach. The utility of less intrusive strategies and minimally invasive approaches will undoubtedly expand as technologies evolve, but they must be responsibly incorporated into surgical practice based on evidence rather than subjective reasons.
Dr. Scott A. Strong and Dr. Nathaniel J. Soper are with Northwestern University, Chicago. These comments were taken from an accompanying editorial (JAMA 2015;314[13]:1343-5). They declared no conflicts of interest.
Dr. Schultz and associates detail findings from a randomized, multicenter clinical trial conducted in Scandinavia designed to assess the superiority of laparoscopic lavage plus drainage, compared with laparoscopic or open resection with or without anastomosis for diverticulitis (Hinchey grades I-III) requiring urgent surgery.
The primary outcome was the incidence of severe complications (Clavien-Dindo classification IIIb-V). Of 144 patients, 74 were randomized to receive laparoscopic lavage and 70 to resection. The two groups were similar in characteristics, although significantly fewer of the lavage procedures were performed by a specialty-trained surgeon. Severe complications occurred in 25.7% of patients in the lavage group and 14.3% in the resection group (difference, 11.4%; 95% CI, −1.8 to 24.1), and significantly more patients in the lavage group developed secondary peritonitis (12% vs. 0%) or returned to the operating room (20% vs. 6%). The hospital mortality rates and follow-up quality-of-life scores were comparable between the groups (3% vs. 4% and 0.75 vs. 0.73, respectively). Somewhat worrisome is that four colon cancers were initially missed in patients treated by laparoscopic lavage alone.
Performing laparoscopic lavage is more difficult than merely irrigating the abdomen and placing drains within the pelvis. Surgeons vary in their attitudes related to concomitant adhesiolysis or debridement, and consensus about these procedures is lacking. Furthermore, subjective signs and objective criteria that identify patients at risk for secondary peritonitis or reoperation must be studied, and risk models should be validated to determine which patients are best suited for this less invasive approach. The utility of less intrusive strategies and minimally invasive approaches will undoubtedly expand as technologies evolve, but they must be responsibly incorporated into surgical practice based on evidence rather than subjective reasons.
Dr. Scott A. Strong and Dr. Nathaniel J. Soper are with Northwestern University, Chicago. These comments were taken from an accompanying editorial (JAMA 2015;314[13]:1343-5). They declared no conflicts of interest.
Patients needing emergency surgery for perforated diverticulitis saw no decrease in serious complications when treated with laparoscopic lavage, a minimally invasive procedure, than with primary resection of the colon, according to results from a randomized multicenter trial in Scandinavia.
Likelihood of reoperation also was significantly higher among patients undergoing laparoscopic lavage, and more sigmoid carcinomas were missed.
For their research, published Oct. 6 in JAMA (2015;314:1364-75), a group led by Dr. Johannes Kurt Schultz of the Akershus University Hospital in Lørenskog, Norway, and the University of Oslo sought to eliminate the selection bias that may have contributed to more favorable outcomes associated with laparoscopic lavage in observational studies.
Dr. Schultz and colleagues randomized patients with suspected perforated diverticulitis from 21 centers in Sweden and Norway to laparoscopic peritoneal lavage (n = 101) or colon resection (n = 98), with the choice of open or laparoscopic approach used for resection, as well as the option of colorectal anastomosis, left to the surgeon.
The study did not use laparoscopic Hinchey staging to classify the severity of the perforation prior to treatment assignment as a way of reducing the selection bias that may have occurred in observational studies.
The preoperative randomization resulted in both groups having similar rates of feculent peritonitis and incorrect preoperative diagnoses. Patients assigned to laparoscopic lavage were treated instead with resection if they were found to have fecal peritonitis. Also, patients in both groups whose pathology required additional treatment were treated at surgeon discretion. This left 74 patients randomized to lavage who received it as assigned and 70 patients undergoing resection per assigned protocol. In the intention-to-treat analysis, 31% of patients in the lavage group and 26% of patients in the resection group saw severe postoperative complications within 90 days, a difference of 4.7% that did not reach statistical significance (95% confidence interval, −7.9% to 17%; P = .53). Severe postoperative complications were defined as any complications resulting in a reintervention requiring general anesthesia, a life-threatening organ dysfunction, or death.
Of the patients treated as assigned with lavage, about 20% (n = 15) required reoperation, compared with 6% (n = 4) in the resection arm, a difference of about 14.6% (95% CI, 3.5% to 25.6%; P =.01).
The main reasons for reoperation were secondary peritonitis in the lavage group and wound rupture in the resection group. Intra-abdominal infections were more frequent in the laparoscopic lavage group, Dr. Schultz and colleagues found.
Also in the lavage group, four carcinomas were missed, compared with two in the resection group. “Because of the relatively high rate of missed colon carcinomas in the lavage group, it was essential to perform a colonoscopy after a patient recovered from the perforation,” the researchers wrote in their analysis.
Although patients in the laparoscopic lavage group had significantly shorter operating times, less blood loss, and lower incidence of stoma at 3 months, the researchers concluded that, based on these results, laparoscopic lavage could not be supported in perforated diverticulitis.
Dr. Schultz and colleagues had planned to enroll about half of eligible patients at the study sites. They noted as a limitation of their study that those not enrolled had more severe disease and worse postoperative outcomes, raising the possibility that the results “may not pertain to patients with perforated diverticulitis who are very ill.”
The study was funded by the South-Eastern Norway Regional Health Authority and Akershus University Hospital. None of its authors reported conflicts of interest.
Patients needing emergency surgery for perforated diverticulitis saw no decrease in serious complications when treated with laparoscopic lavage, a minimally invasive procedure, than with primary resection of the colon, according to results from a randomized multicenter trial in Scandinavia.
Likelihood of reoperation also was significantly higher among patients undergoing laparoscopic lavage, and more sigmoid carcinomas were missed.
For their research, published Oct. 6 in JAMA (2015;314:1364-75), a group led by Dr. Johannes Kurt Schultz of the Akershus University Hospital in Lørenskog, Norway, and the University of Oslo sought to eliminate the selection bias that may have contributed to more favorable outcomes associated with laparoscopic lavage in observational studies.
Dr. Schultz and colleagues randomized patients with suspected perforated diverticulitis from 21 centers in Sweden and Norway to laparoscopic peritoneal lavage (n = 101) or colon resection (n = 98), with the choice of open or laparoscopic approach used for resection, as well as the option of colorectal anastomosis, left to the surgeon.
The study did not use laparoscopic Hinchey staging to classify the severity of the perforation prior to treatment assignment as a way of reducing the selection bias that may have occurred in observational studies.
The preoperative randomization resulted in both groups having similar rates of feculent peritonitis and incorrect preoperative diagnoses. Patients assigned to laparoscopic lavage were treated instead with resection if they were found to have fecal peritonitis. Also, patients in both groups whose pathology required additional treatment were treated at surgeon discretion. This left 74 patients randomized to lavage who received it as assigned and 70 patients undergoing resection per assigned protocol. In the intention-to-treat analysis, 31% of patients in the lavage group and 26% of patients in the resection group saw severe postoperative complications within 90 days, a difference of 4.7% that did not reach statistical significance (95% confidence interval, −7.9% to 17%; P = .53). Severe postoperative complications were defined as any complications resulting in a reintervention requiring general anesthesia, a life-threatening organ dysfunction, or death.
Of the patients treated as assigned with lavage, about 20% (n = 15) required reoperation, compared with 6% (n = 4) in the resection arm, a difference of about 14.6% (95% CI, 3.5% to 25.6%; P =.01).
The main reasons for reoperation were secondary peritonitis in the lavage group and wound rupture in the resection group. Intra-abdominal infections were more frequent in the laparoscopic lavage group, Dr. Schultz and colleagues found.
Also in the lavage group, four carcinomas were missed, compared with two in the resection group. “Because of the relatively high rate of missed colon carcinomas in the lavage group, it was essential to perform a colonoscopy after a patient recovered from the perforation,” the researchers wrote in their analysis.
Although patients in the laparoscopic lavage group had significantly shorter operating times, less blood loss, and lower incidence of stoma at 3 months, the researchers concluded that, based on these results, laparoscopic lavage could not be supported in perforated diverticulitis.
Dr. Schultz and colleagues had planned to enroll about half of eligible patients at the study sites. They noted as a limitation of their study that those not enrolled had more severe disease and worse postoperative outcomes, raising the possibility that the results “may not pertain to patients with perforated diverticulitis who are very ill.”
The study was funded by the South-Eastern Norway Regional Health Authority and Akershus University Hospital. None of its authors reported conflicts of interest.
FROM JAMA
Key clinical point: Laparoscopic lavage carries risks of severe postoperative complications similar to colon resection in people presenting with suspected perforated diverticulitis requiring emergency surgery.
Major finding: Mortality and severe complications did not differ significantly at 90 days postoperation between intention-to-treat groups, while reoperation was significantly higher among patients treated with lavage (5.7% for resection vs. 20.3% for lavage, P < .01).
Data source: A multicenter, open-label randomized trial in which patients presenting with likely perforated diverticulitis were randomized to lavage (n = 74) or resection (n = 70).
Disclosures: The study was sponsored by investigator institutions and Norwegian regional government grants. No conflicts of interest were reported.
High death rates for IBD patients who underwent emergency resections
Patients with inflammatory bowel disease (IBD) were about five to eight times more likely to die after emergency intestinal resection as opposed to elective surgery, a large meta-analysis found.
Overall mortality rates after emergency intestinal resection were 5.3% for patients with ulcerative colitis (UC) and 3.6% for patients with Crohn’s disease (CD), said Dr. Sunny Singh and his associates at the University of Calgary in Alberta, Canada. In contrast, only 0.6%-0.7% of patients died after elective resection, the researchers reported in the October issue of Gastroenterology (2015 Jun 5. doi: 10.1053/j.gastro.2015.06.001).
Source: American Gastroenterological AssociationClinicians should optimize medical management to avoid emergency resection, seek ways to reduce associated mortality, and use the data when counseling patients and weighing medical and surgical management options, they added.
Intestinal resection is less common among patients with IBD than in decades past, but almost half of CD patients undergo the surgery within 10 years of diagnosis, as do 16% of UC patients, according to another meta-analysis (Gastroenterology 2013;145:996-1006). Past studies have reported divergent rates of death after these surgeries, the researchers noted. To better understand mortality rates and relevant risk factors, they reviewed 18 original research articles and three abstracts published between 1990 and 2015, all of which were indexed in Medline, EMBASE, or PubMed. The studies included 67,057 UC patients and 75,971 CD patients from 15 countries.
Rates of mortality after elective resection were significantly lower than after emergency resection, whether patients had CD (elective, 0.6%; 95% confidence interval, 0.2%-1.7%; emergency, 3.6%; 1.8%-6.9%) or UC (elective, 0.7%; 0.6%-0.9%; emergency, 5.3%; 3.8%-7.3%), the researchers found. Death rates did not significantly differ based on disease type. Postoperative mortality dropped significantly after the 1990s among CD patients only, perhaps because emergency surgery has become less common in Calgary since 1997, the researchers said. However, they were unable to compare changes in death rates over time by surgery type, they said.
Several factors could explain the high fatality rates after emergency intestinal resection, the researchers said. Patients tended to have worse disease activity and higher rates of intestinal obstruction, intra-abdominal abscess, toxic megacolon, preoperative clostridial diarrhea, venous thromboembolism, malnourishment, or prolonged treatment with intravenous corticosteroids, they said. General surgeons are more likely to perform emergency resections than elective cases, which are typically handled by more experienced colorectal surgeons, they added. Emergency resections also are less likely to be performed laparoscopically than are elective resections, they noted. “The low risk of death associated with elective intestinal resections for CD and UC could be used as a quality assurance benchmark to compare outcomes between hospitals and surgeons,” they added.
The research was funded by the Canadian Institute of Health Research, Alberta-Innovates Health-Solutions, the Alberta IBD Consortium. Dr. Singh reported no conflicts of interest. Senior author Dr. Gilaad Kaplan and four coauthors disclosed speaker, advisory board, and funding relationships with a number of pharmaceutical companies.
Patients with inflammatory bowel disease (IBD) were about five to eight times more likely to die after emergency intestinal resection as opposed to elective surgery, a large meta-analysis found.
Overall mortality rates after emergency intestinal resection were 5.3% for patients with ulcerative colitis (UC) and 3.6% for patients with Crohn’s disease (CD), said Dr. Sunny Singh and his associates at the University of Calgary in Alberta, Canada. In contrast, only 0.6%-0.7% of patients died after elective resection, the researchers reported in the October issue of Gastroenterology (2015 Jun 5. doi: 10.1053/j.gastro.2015.06.001).
Source: American Gastroenterological AssociationClinicians should optimize medical management to avoid emergency resection, seek ways to reduce associated mortality, and use the data when counseling patients and weighing medical and surgical management options, they added.
Intestinal resection is less common among patients with IBD than in decades past, but almost half of CD patients undergo the surgery within 10 years of diagnosis, as do 16% of UC patients, according to another meta-analysis (Gastroenterology 2013;145:996-1006). Past studies have reported divergent rates of death after these surgeries, the researchers noted. To better understand mortality rates and relevant risk factors, they reviewed 18 original research articles and three abstracts published between 1990 and 2015, all of which were indexed in Medline, EMBASE, or PubMed. The studies included 67,057 UC patients and 75,971 CD patients from 15 countries.
Rates of mortality after elective resection were significantly lower than after emergency resection, whether patients had CD (elective, 0.6%; 95% confidence interval, 0.2%-1.7%; emergency, 3.6%; 1.8%-6.9%) or UC (elective, 0.7%; 0.6%-0.9%; emergency, 5.3%; 3.8%-7.3%), the researchers found. Death rates did not significantly differ based on disease type. Postoperative mortality dropped significantly after the 1990s among CD patients only, perhaps because emergency surgery has become less common in Calgary since 1997, the researchers said. However, they were unable to compare changes in death rates over time by surgery type, they said.
Several factors could explain the high fatality rates after emergency intestinal resection, the researchers said. Patients tended to have worse disease activity and higher rates of intestinal obstruction, intra-abdominal abscess, toxic megacolon, preoperative clostridial diarrhea, venous thromboembolism, malnourishment, or prolonged treatment with intravenous corticosteroids, they said. General surgeons are more likely to perform emergency resections than elective cases, which are typically handled by more experienced colorectal surgeons, they added. Emergency resections also are less likely to be performed laparoscopically than are elective resections, they noted. “The low risk of death associated with elective intestinal resections for CD and UC could be used as a quality assurance benchmark to compare outcomes between hospitals and surgeons,” they added.
The research was funded by the Canadian Institute of Health Research, Alberta-Innovates Health-Solutions, the Alberta IBD Consortium. Dr. Singh reported no conflicts of interest. Senior author Dr. Gilaad Kaplan and four coauthors disclosed speaker, advisory board, and funding relationships with a number of pharmaceutical companies.
Patients with inflammatory bowel disease (IBD) were about five to eight times more likely to die after emergency intestinal resection as opposed to elective surgery, a large meta-analysis found.
Overall mortality rates after emergency intestinal resection were 5.3% for patients with ulcerative colitis (UC) and 3.6% for patients with Crohn’s disease (CD), said Dr. Sunny Singh and his associates at the University of Calgary in Alberta, Canada. In contrast, only 0.6%-0.7% of patients died after elective resection, the researchers reported in the October issue of Gastroenterology (2015 Jun 5. doi: 10.1053/j.gastro.2015.06.001).
Source: American Gastroenterological AssociationClinicians should optimize medical management to avoid emergency resection, seek ways to reduce associated mortality, and use the data when counseling patients and weighing medical and surgical management options, they added.
Intestinal resection is less common among patients with IBD than in decades past, but almost half of CD patients undergo the surgery within 10 years of diagnosis, as do 16% of UC patients, according to another meta-analysis (Gastroenterology 2013;145:996-1006). Past studies have reported divergent rates of death after these surgeries, the researchers noted. To better understand mortality rates and relevant risk factors, they reviewed 18 original research articles and three abstracts published between 1990 and 2015, all of which were indexed in Medline, EMBASE, or PubMed. The studies included 67,057 UC patients and 75,971 CD patients from 15 countries.
Rates of mortality after elective resection were significantly lower than after emergency resection, whether patients had CD (elective, 0.6%; 95% confidence interval, 0.2%-1.7%; emergency, 3.6%; 1.8%-6.9%) or UC (elective, 0.7%; 0.6%-0.9%; emergency, 5.3%; 3.8%-7.3%), the researchers found. Death rates did not significantly differ based on disease type. Postoperative mortality dropped significantly after the 1990s among CD patients only, perhaps because emergency surgery has become less common in Calgary since 1997, the researchers said. However, they were unable to compare changes in death rates over time by surgery type, they said.
Several factors could explain the high fatality rates after emergency intestinal resection, the researchers said. Patients tended to have worse disease activity and higher rates of intestinal obstruction, intra-abdominal abscess, toxic megacolon, preoperative clostridial diarrhea, venous thromboembolism, malnourishment, or prolonged treatment with intravenous corticosteroids, they said. General surgeons are more likely to perform emergency resections than elective cases, which are typically handled by more experienced colorectal surgeons, they added. Emergency resections also are less likely to be performed laparoscopically than are elective resections, they noted. “The low risk of death associated with elective intestinal resections for CD and UC could be used as a quality assurance benchmark to compare outcomes between hospitals and surgeons,” they added.
The research was funded by the Canadian Institute of Health Research, Alberta-Innovates Health-Solutions, the Alberta IBD Consortium. Dr. Singh reported no conflicts of interest. Senior author Dr. Gilaad Kaplan and four coauthors disclosed speaker, advisory board, and funding relationships with a number of pharmaceutical companies.
FROM GASTROENTEROLOGY
Key clinical point: Patients with IBD were about five to eight times more likely to die after emergency intestinal resection as opposed to elective surgery.
Major finding: Overall mortality rates after emergency intestinal resection were 5.3% for patients with ulcerative colitis and 3.6% for Crohn’s disease; mortality rates after elective surgery were 0.7% and 0.6%, respectively.
Data source: Meta-analysis of 18 original research studies and three abstracts published between 1990 and 2015.
Disclosures: The research was funded by the Canadian Institute of Health Research, Alberta-Innovates Health-Solutions, the Alberta IBD Consortium. Dr. Singh reported no conflicts of interest. Senior author Dr. Gilaad Kaplan and four coauthors disclosed speaker, advisory board, and funding relationships with a number of pharmaceutical companies.
Patterns in the Use of Neoadjuvant and Adjuvant Therapy in Stage II/III Rectal Cancer and Associated Survival
Background: A 2004 German study found preoperative chemoradiotherapy followed by postoperative chemotherapy provided increased local control and reduced toxicity over postoperative chemoradiotherapy in stage II/III rectal cancer, though a statistically significant advantage in overall survival was not observed. We examined similar survival differences and the utilization of appropriate therapy on a larger scale.
Methods: This study retrospectively examined patients diagnosed with stage II/III rectal cancer from 2006 to 2011 using a participant user file from the National Cancer Database, a data registry jointly sponsored by the American College of Surgeons and the American Cancer Society capturing approximately 70% of newly diagnosed cancer cases nationwide. Overall survival differences between treatment modalities were assessed using life tables and pairwise comparisons, and changes in the utilization of these treatments were examined.
Results: Of 40,546 patients diagnosed with stage II/III rectal cancer, 27,014 (66.6%) received therapy consisting of surgery, chemotherapy, and radiation. Those administered preoperative chemoradiotherapy followed by postoperative chemotherapy had the highest 5-year survival rate (stage II 81.4%, stage III 71.2%), but the difference was not significant against postoperative chemoradiotherapy in stage III disease (69.9%) after the Bonferroni correction was applied. Five-year survival was higher in postoperative (stage II 76.0%, stage III 69.9%) than that in preoperative (stage II 72.5%, stage III: 65.8%) chemoradiotherapy in both stages. Preoperative chemoradiotherapy remains the most commonly administered (60.6% in stage II and 46.0% in stage III), but preoperative chemoradio-therapy followed by postoperative chemotherapy has been steadily rising (2006: 12.2% in stage II, 16.5% in stage III vs 2011: 22.8% in stage II, 28.0% in stage III).
Conclusions: A survival benefit of preoperative chemoradiotherapy followed by postoperative chemotherapy in stage II disease was observed, along with a nonsignificant advantage in stage III disease. The utilization of preoperative chemoradiotherapy followed by postoperative chemotherapy increased, but preoperative chemoradiotherapy remained most prevalent despite its lesser overall survival. Cox regression will be performed prior to the AVAHO annual meeting to evaluate the impact of other characteristics such as age, insurance, income, and comorbidities on survival.
Background: A 2004 German study found preoperative chemoradiotherapy followed by postoperative chemotherapy provided increased local control and reduced toxicity over postoperative chemoradiotherapy in stage II/III rectal cancer, though a statistically significant advantage in overall survival was not observed. We examined similar survival differences and the utilization of appropriate therapy on a larger scale.
Methods: This study retrospectively examined patients diagnosed with stage II/III rectal cancer from 2006 to 2011 using a participant user file from the National Cancer Database, a data registry jointly sponsored by the American College of Surgeons and the American Cancer Society capturing approximately 70% of newly diagnosed cancer cases nationwide. Overall survival differences between treatment modalities were assessed using life tables and pairwise comparisons, and changes in the utilization of these treatments were examined.
Results: Of 40,546 patients diagnosed with stage II/III rectal cancer, 27,014 (66.6%) received therapy consisting of surgery, chemotherapy, and radiation. Those administered preoperative chemoradiotherapy followed by postoperative chemotherapy had the highest 5-year survival rate (stage II 81.4%, stage III 71.2%), but the difference was not significant against postoperative chemoradiotherapy in stage III disease (69.9%) after the Bonferroni correction was applied. Five-year survival was higher in postoperative (stage II 76.0%, stage III 69.9%) than that in preoperative (stage II 72.5%, stage III: 65.8%) chemoradiotherapy in both stages. Preoperative chemoradiotherapy remains the most commonly administered (60.6% in stage II and 46.0% in stage III), but preoperative chemoradio-therapy followed by postoperative chemotherapy has been steadily rising (2006: 12.2% in stage II, 16.5% in stage III vs 2011: 22.8% in stage II, 28.0% in stage III).
Conclusions: A survival benefit of preoperative chemoradiotherapy followed by postoperative chemotherapy in stage II disease was observed, along with a nonsignificant advantage in stage III disease. The utilization of preoperative chemoradiotherapy followed by postoperative chemotherapy increased, but preoperative chemoradiotherapy remained most prevalent despite its lesser overall survival. Cox regression will be performed prior to the AVAHO annual meeting to evaluate the impact of other characteristics such as age, insurance, income, and comorbidities on survival.
Background: A 2004 German study found preoperative chemoradiotherapy followed by postoperative chemotherapy provided increased local control and reduced toxicity over postoperative chemoradiotherapy in stage II/III rectal cancer, though a statistically significant advantage in overall survival was not observed. We examined similar survival differences and the utilization of appropriate therapy on a larger scale.
Methods: This study retrospectively examined patients diagnosed with stage II/III rectal cancer from 2006 to 2011 using a participant user file from the National Cancer Database, a data registry jointly sponsored by the American College of Surgeons and the American Cancer Society capturing approximately 70% of newly diagnosed cancer cases nationwide. Overall survival differences between treatment modalities were assessed using life tables and pairwise comparisons, and changes in the utilization of these treatments were examined.
Results: Of 40,546 patients diagnosed with stage II/III rectal cancer, 27,014 (66.6%) received therapy consisting of surgery, chemotherapy, and radiation. Those administered preoperative chemoradiotherapy followed by postoperative chemotherapy had the highest 5-year survival rate (stage II 81.4%, stage III 71.2%), but the difference was not significant against postoperative chemoradiotherapy in stage III disease (69.9%) after the Bonferroni correction was applied. Five-year survival was higher in postoperative (stage II 76.0%, stage III 69.9%) than that in preoperative (stage II 72.5%, stage III: 65.8%) chemoradiotherapy in both stages. Preoperative chemoradiotherapy remains the most commonly administered (60.6% in stage II and 46.0% in stage III), but preoperative chemoradio-therapy followed by postoperative chemotherapy has been steadily rising (2006: 12.2% in stage II, 16.5% in stage III vs 2011: 22.8% in stage II, 28.0% in stage III).
Conclusions: A survival benefit of preoperative chemoradiotherapy followed by postoperative chemotherapy in stage II disease was observed, along with a nonsignificant advantage in stage III disease. The utilization of preoperative chemoradiotherapy followed by postoperative chemotherapy increased, but preoperative chemoradiotherapy remained most prevalent despite its lesser overall survival. Cox regression will be performed prior to the AVAHO annual meeting to evaluate the impact of other characteristics such as age, insurance, income, and comorbidities on survival.
Stage IV Rectal Cancer Trends by Year: A Review of the National Cancer Database, 1998 to 2009
Background: The arrival of novel surgical techniques and chemotherapeutic agents has changed the range of available treatments and improved outcomes for stage IV rectal cancers. This is the largest study on stage IV rectal cancer to evaluate the change in treatment strategy and corresponding mortality from 1998 to 2009.
Methods: A population-based study was conducted using the National Cancer Database (1998-2009), which contains 70% of all cancer diagnoses in the U.S. After exclusion criteria were met, 25,046 stage IV rectal cancer patients were analyzed. Treatment modalities were compared by year of diagnosis between 1998 and 2009. Life tables were used to determine mortality by year. All statistics were run on SPSS Version 22 (IBM, Armonk, NY).
Results: Overall survival in stage IV rectal cancer has increased from 1998 to 2009 for 1-year survival (50% vs 61%) and 5-year survival (7% vs 12%). Analysis by treatment revealed that chemotherapy with radiation was most prevalent (20.6%) in 1998, but chemotherapy alone became the predominant treatment (25%) in 2009. Surgery as a planned first course of treatment decreased from 51.5% in 1998 to 27.2% in 2009, with a concordant increase in chemotherapy from 8.4% to 25% in that time frame. The largest 5-year survival increase across these years included surgery only (6% to 15%), surgery and chemotherapy (8% to 23%), and trimodal therapy (15% to 27%).
Conclusions: The outcomes for stage IV rectal cancer have meaningfully improved from 1998 to 2009, as evidenced by the significant improvement in 1- and 5-year survival. There has been a general trend to treat with chemotherapy and avoid surgery as a planned first course of treatment, despite improvement in mortality for both. Survival rates remain highest with trimodal therapy, but 5-year survival for surgery with chemotherapy and surgery only has also significantly improved from 1998 to 2009. Prior to the AVAHO annual meeting, we will conduct a multivariate analysis to evaluate other influences on survival such as age, comorbidities, insurance, education, and income.
Background: The arrival of novel surgical techniques and chemotherapeutic agents has changed the range of available treatments and improved outcomes for stage IV rectal cancers. This is the largest study on stage IV rectal cancer to evaluate the change in treatment strategy and corresponding mortality from 1998 to 2009.
Methods: A population-based study was conducted using the National Cancer Database (1998-2009), which contains 70% of all cancer diagnoses in the U.S. After exclusion criteria were met, 25,046 stage IV rectal cancer patients were analyzed. Treatment modalities were compared by year of diagnosis between 1998 and 2009. Life tables were used to determine mortality by year. All statistics were run on SPSS Version 22 (IBM, Armonk, NY).
Results: Overall survival in stage IV rectal cancer has increased from 1998 to 2009 for 1-year survival (50% vs 61%) and 5-year survival (7% vs 12%). Analysis by treatment revealed that chemotherapy with radiation was most prevalent (20.6%) in 1998, but chemotherapy alone became the predominant treatment (25%) in 2009. Surgery as a planned first course of treatment decreased from 51.5% in 1998 to 27.2% in 2009, with a concordant increase in chemotherapy from 8.4% to 25% in that time frame. The largest 5-year survival increase across these years included surgery only (6% to 15%), surgery and chemotherapy (8% to 23%), and trimodal therapy (15% to 27%).
Conclusions: The outcomes for stage IV rectal cancer have meaningfully improved from 1998 to 2009, as evidenced by the significant improvement in 1- and 5-year survival. There has been a general trend to treat with chemotherapy and avoid surgery as a planned first course of treatment, despite improvement in mortality for both. Survival rates remain highest with trimodal therapy, but 5-year survival for surgery with chemotherapy and surgery only has also significantly improved from 1998 to 2009. Prior to the AVAHO annual meeting, we will conduct a multivariate analysis to evaluate other influences on survival such as age, comorbidities, insurance, education, and income.
Background: The arrival of novel surgical techniques and chemotherapeutic agents has changed the range of available treatments and improved outcomes for stage IV rectal cancers. This is the largest study on stage IV rectal cancer to evaluate the change in treatment strategy and corresponding mortality from 1998 to 2009.
Methods: A population-based study was conducted using the National Cancer Database (1998-2009), which contains 70% of all cancer diagnoses in the U.S. After exclusion criteria were met, 25,046 stage IV rectal cancer patients were analyzed. Treatment modalities were compared by year of diagnosis between 1998 and 2009. Life tables were used to determine mortality by year. All statistics were run on SPSS Version 22 (IBM, Armonk, NY).
Results: Overall survival in stage IV rectal cancer has increased from 1998 to 2009 for 1-year survival (50% vs 61%) and 5-year survival (7% vs 12%). Analysis by treatment revealed that chemotherapy with radiation was most prevalent (20.6%) in 1998, but chemotherapy alone became the predominant treatment (25%) in 2009. Surgery as a planned first course of treatment decreased from 51.5% in 1998 to 27.2% in 2009, with a concordant increase in chemotherapy from 8.4% to 25% in that time frame. The largest 5-year survival increase across these years included surgery only (6% to 15%), surgery and chemotherapy (8% to 23%), and trimodal therapy (15% to 27%).
Conclusions: The outcomes for stage IV rectal cancer have meaningfully improved from 1998 to 2009, as evidenced by the significant improvement in 1- and 5-year survival. There has been a general trend to treat with chemotherapy and avoid surgery as a planned first course of treatment, despite improvement in mortality for both. Survival rates remain highest with trimodal therapy, but 5-year survival for surgery with chemotherapy and surgery only has also significantly improved from 1998 to 2009. Prior to the AVAHO annual meeting, we will conduct a multivariate analysis to evaluate other influences on survival such as age, comorbidities, insurance, education, and income.