User login
QUIZ: What Is Next Step for Diagnosing Cavitary Lesion with No Improvement after Serial Chest X-Rays, Antibiotics?
[WpProQuiz 9]
[WpProQuiz_toplist 9]
[WpProQuiz 9]
[WpProQuiz_toplist 9]
[WpProQuiz 9]
[WpProQuiz_toplist 9]
Case of colistin-resistant E. coli identified in the United States
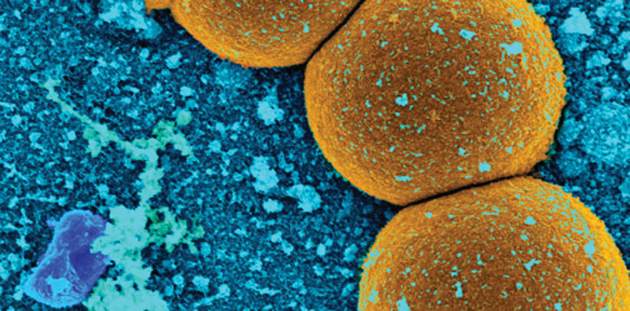
In what is believed to be the first case of its kind in the United States, researchers identified a female patient with colistin-resistant Escherichia coli. The patient harbored mcr-1, a gene resistant to colistin, an antibiotic used as a last resort for infections that are resistant to carbapenems.
The finding comes at a time when a search for colistin-resistant bacteria by officials from the U.S. Department of Agriculture and the U.S. Department of Health and Human Services revealed colistin-resistant E. coli in a single sample from a pig intestine. Combined, “these discoveries are of concern because colistin is used as a last-resort drug to treat patients with multidrug resistant infections,” according to a communication from the HHS dated May 26. “Finding colistin-resistant bacteria in the United States is important, as it was only last November that scientists in China first reported that the mcr-1 gene in bacteria confers colistin resistance.”
Researchers led by Patrick McGann, Ph.D., who reported the human case in an article published online May 26 in Antimicrobial Agents and Chemotherapy, wrote that the recent discovery of a plasmid-borne colistin resistance gene, mcr-1, “heralds the emergence of truly pan-drug resistant bacteria. The gene has been found primarily in Escherichia coli, but has also been identified in other members of the Enterobacteriaceae from human, animal, food and environmental samples on every continent” (Antimicrob Agents Chemother. 2016 May 26. doi: 10.1128/AAC.01103-16).
As a result of this threat, in May, Dr. McGann, of the Department of Defense’s Multidrug-resistant Organism Repository and Surveillance Network at Walter Reed Army Institute of Research, Silver Spring, Md., and his associates began analyzing all extended-spectrum beta-lactamase (ESBL)–producing E. coli clinical isolates submitted to Walter Reed National Military Medical Center for analysis for resistance to colistin by E-test.
The case of interest was the presence of mcr-1 in an E. coli isolate cultured from a 49-year-old woman who presented to a military clinic in Pennsylvania with symptoms suggestive of a urinary tract infection, and who reported no travel history within the prior 5 months. Susceptibility testing at Walter Reed indicated an ESBL phenotype.
“The isolate was included in the first 6 ESBL-producing E. coli selected for colistin susceptibility testing, and it was the only isolate to have a MIC of colistin of 4 mcg/mL [all others had MICs of 0.25 mcg/mL or less]. Colistin MIC was confirmed by microbroth dilution and mcr-1 detected by real-time PCR.”
Since mcr-1 testing at Walter Reed has been underway for a short time, “it remains unclear what the true prevalence of mcr-1 is in the population,” the researchers noted. “The association between mcr-1 and IncF plasmids is concerning as these plasmids are vehicles for the dissemination of antibiotic resistance and virulence genes against Enterobacteriaceae. Continued surveillance to determine the true frequency for this gene in the USA is critical.”
The researchers reported having no financial disclosures.
In what is believed to be the first case of its kind in the United States, researchers identified a female patient with colistin-resistant Escherichia coli. The patient harbored mcr-1, a gene resistant to colistin, an antibiotic used as a last resort for infections that are resistant to carbapenems.
The finding comes at a time when a search for colistin-resistant bacteria by officials from the U.S. Department of Agriculture and the U.S. Department of Health and Human Services revealed colistin-resistant E. coli in a single sample from a pig intestine. Combined, “these discoveries are of concern because colistin is used as a last-resort drug to treat patients with multidrug resistant infections,” according to a communication from the HHS dated May 26. “Finding colistin-resistant bacteria in the United States is important, as it was only last November that scientists in China first reported that the mcr-1 gene in bacteria confers colistin resistance.”
Researchers led by Patrick McGann, Ph.D., who reported the human case in an article published online May 26 in Antimicrobial Agents and Chemotherapy, wrote that the recent discovery of a plasmid-borne colistin resistance gene, mcr-1, “heralds the emergence of truly pan-drug resistant bacteria. The gene has been found primarily in Escherichia coli, but has also been identified in other members of the Enterobacteriaceae from human, animal, food and environmental samples on every continent” (Antimicrob Agents Chemother. 2016 May 26. doi: 10.1128/AAC.01103-16).
As a result of this threat, in May, Dr. McGann, of the Department of Defense’s Multidrug-resistant Organism Repository and Surveillance Network at Walter Reed Army Institute of Research, Silver Spring, Md., and his associates began analyzing all extended-spectrum beta-lactamase (ESBL)–producing E. coli clinical isolates submitted to Walter Reed National Military Medical Center for analysis for resistance to colistin by E-test.
The case of interest was the presence of mcr-1 in an E. coli isolate cultured from a 49-year-old woman who presented to a military clinic in Pennsylvania with symptoms suggestive of a urinary tract infection, and who reported no travel history within the prior 5 months. Susceptibility testing at Walter Reed indicated an ESBL phenotype.
“The isolate was included in the first 6 ESBL-producing E. coli selected for colistin susceptibility testing, and it was the only isolate to have a MIC of colistin of 4 mcg/mL [all others had MICs of 0.25 mcg/mL or less]. Colistin MIC was confirmed by microbroth dilution and mcr-1 detected by real-time PCR.”
Since mcr-1 testing at Walter Reed has been underway for a short time, “it remains unclear what the true prevalence of mcr-1 is in the population,” the researchers noted. “The association between mcr-1 and IncF plasmids is concerning as these plasmids are vehicles for the dissemination of antibiotic resistance and virulence genes against Enterobacteriaceae. Continued surveillance to determine the true frequency for this gene in the USA is critical.”
The researchers reported having no financial disclosures.
In what is believed to be the first case of its kind in the United States, researchers identified a female patient with colistin-resistant Escherichia coli. The patient harbored mcr-1, a gene resistant to colistin, an antibiotic used as a last resort for infections that are resistant to carbapenems.
The finding comes at a time when a search for colistin-resistant bacteria by officials from the U.S. Department of Agriculture and the U.S. Department of Health and Human Services revealed colistin-resistant E. coli in a single sample from a pig intestine. Combined, “these discoveries are of concern because colistin is used as a last-resort drug to treat patients with multidrug resistant infections,” according to a communication from the HHS dated May 26. “Finding colistin-resistant bacteria in the United States is important, as it was only last November that scientists in China first reported that the mcr-1 gene in bacteria confers colistin resistance.”
Researchers led by Patrick McGann, Ph.D., who reported the human case in an article published online May 26 in Antimicrobial Agents and Chemotherapy, wrote that the recent discovery of a plasmid-borne colistin resistance gene, mcr-1, “heralds the emergence of truly pan-drug resistant bacteria. The gene has been found primarily in Escherichia coli, but has also been identified in other members of the Enterobacteriaceae from human, animal, food and environmental samples on every continent” (Antimicrob Agents Chemother. 2016 May 26. doi: 10.1128/AAC.01103-16).
As a result of this threat, in May, Dr. McGann, of the Department of Defense’s Multidrug-resistant Organism Repository and Surveillance Network at Walter Reed Army Institute of Research, Silver Spring, Md., and his associates began analyzing all extended-spectrum beta-lactamase (ESBL)–producing E. coli clinical isolates submitted to Walter Reed National Military Medical Center for analysis for resistance to colistin by E-test.
The case of interest was the presence of mcr-1 in an E. coli isolate cultured from a 49-year-old woman who presented to a military clinic in Pennsylvania with symptoms suggestive of a urinary tract infection, and who reported no travel history within the prior 5 months. Susceptibility testing at Walter Reed indicated an ESBL phenotype.
“The isolate was included in the first 6 ESBL-producing E. coli selected for colistin susceptibility testing, and it was the only isolate to have a MIC of colistin of 4 mcg/mL [all others had MICs of 0.25 mcg/mL or less]. Colistin MIC was confirmed by microbroth dilution and mcr-1 detected by real-time PCR.”
Since mcr-1 testing at Walter Reed has been underway for a short time, “it remains unclear what the true prevalence of mcr-1 is in the population,” the researchers noted. “The association between mcr-1 and IncF plasmids is concerning as these plasmids are vehicles for the dissemination of antibiotic resistance and virulence genes against Enterobacteriaceae. Continued surveillance to determine the true frequency for this gene in the USA is critical.”
The researchers reported having no financial disclosures.
FROM ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Key clinical point: Researchers have identified the first case of colistin-resistant E. coli in the United States.
Major finding: Mcr-1 was present in an E. coli sampled from a patient with a urinary tract infection in the United States.
Data source: A case report of a 49-year-old woman who presented to a military clinic in Pennsylvania with symptoms suggestive of a urinary tract infection.
Disclosures: The researchers reported having no financial disclosures.
Risk Factors for Pseudomonas, MRSA in Healthcare-Associated Pneumonia
Clinical question: What risk factors could predict the likelihood of Pseudomonas and methicillin-resistant Staphylococcus aureus (MRSA) in patients hospitalized with healthcare-associated pneumonia (HCAP)?
Background: Patients identified with HCAP have an increased risk for multi-drug-resistant pathogens, such as gram-negative (GNR) organisms and MRSA. Meeting criteria for HCAP does not discriminate between the different infections, which require different antibiotic classes for treatment. Risk factors need to be identified to determine the most likely infectious organism to help guide initial empiric antibiotic therapy.
Study design: Retrospective cohort study.
Setting: Veterans Affairs hospitals.
Synopsis: Of 61,651 veterans with HCAP diagnosis, 1,156 (1.9%) had a discharge diagnosis of Pseudomonas pneumonia and were found to be younger and more likely to be immunocompromised; have hemiplegia; have a history of chronic obstructive pulmonary disease; have had corticosteroid exposure; and have been exposed to a fluoroquinolone, β-lactam, cephalosporin, or carbapenem antiobiotic within 90 days prior to admission. Pseudomonas pneumonia was negatively associated with age >84, drug abuse, diabetes, and higher socioeconomic status. A discharge diagnosis of MRSA pneumonia was found in 641 patients (1.0%), who also were positively associated with the male gender, age >74, recent nursing home stay, and recent exposure to fluoroquinolone antibiotics within 90 days prior to admission.
MRSA pneumonia was negatively associated with complicated diabetes. Neither diagnosis was present in 59,854 patients (97.1%).
This study was limited due to its predominantly male veteran population, low incidence of Pseudomonas and MRSA pneumonia being identified, and Pseudomonas as the only GNR organism analyzed.
Bottom line: Risk factors identified for Pseudomonas and MRSA pneumonia can help guide targeted antibiotics for HCAP patients.
Citation: Metersky ML, Frei CR, Mortenson EM. Predictors of Pseudomonas and methicillin-resistant Staphylococcus aureus in hospitalized patients with healthcare-associated pneumonia. Respirology. 2016;21(1):157-163.
Short Take
Hematuria as Marker of Urologic Cancer
Narrative literature review did not demonstrate beneficial role of screening urinalysis for cancer detection in asymptomatic patients, but it did suggest including gross hematuria as part of routine review of systems.
Citation: Nielsen M, Qaseem A, High Value Care Task Force of the American College of Physicians. Hematuria as a marker of occult urinary tract cancer: advice for high-value care from the American College of Physicians. Ann Intern Med. 2016;164(7):488-497. doi:10.7326/M15-1496.
Clinical question: What risk factors could predict the likelihood of Pseudomonas and methicillin-resistant Staphylococcus aureus (MRSA) in patients hospitalized with healthcare-associated pneumonia (HCAP)?
Background: Patients identified with HCAP have an increased risk for multi-drug-resistant pathogens, such as gram-negative (GNR) organisms and MRSA. Meeting criteria for HCAP does not discriminate between the different infections, which require different antibiotic classes for treatment. Risk factors need to be identified to determine the most likely infectious organism to help guide initial empiric antibiotic therapy.
Study design: Retrospective cohort study.
Setting: Veterans Affairs hospitals.
Synopsis: Of 61,651 veterans with HCAP diagnosis, 1,156 (1.9%) had a discharge diagnosis of Pseudomonas pneumonia and were found to be younger and more likely to be immunocompromised; have hemiplegia; have a history of chronic obstructive pulmonary disease; have had corticosteroid exposure; and have been exposed to a fluoroquinolone, β-lactam, cephalosporin, or carbapenem antiobiotic within 90 days prior to admission. Pseudomonas pneumonia was negatively associated with age >84, drug abuse, diabetes, and higher socioeconomic status. A discharge diagnosis of MRSA pneumonia was found in 641 patients (1.0%), who also were positively associated with the male gender, age >74, recent nursing home stay, and recent exposure to fluoroquinolone antibiotics within 90 days prior to admission.
MRSA pneumonia was negatively associated with complicated diabetes. Neither diagnosis was present in 59,854 patients (97.1%).
This study was limited due to its predominantly male veteran population, low incidence of Pseudomonas and MRSA pneumonia being identified, and Pseudomonas as the only GNR organism analyzed.
Bottom line: Risk factors identified for Pseudomonas and MRSA pneumonia can help guide targeted antibiotics for HCAP patients.
Citation: Metersky ML, Frei CR, Mortenson EM. Predictors of Pseudomonas and methicillin-resistant Staphylococcus aureus in hospitalized patients with healthcare-associated pneumonia. Respirology. 2016;21(1):157-163.
Short Take
Hematuria as Marker of Urologic Cancer
Narrative literature review did not demonstrate beneficial role of screening urinalysis for cancer detection in asymptomatic patients, but it did suggest including gross hematuria as part of routine review of systems.
Citation: Nielsen M, Qaseem A, High Value Care Task Force of the American College of Physicians. Hematuria as a marker of occult urinary tract cancer: advice for high-value care from the American College of Physicians. Ann Intern Med. 2016;164(7):488-497. doi:10.7326/M15-1496.
Clinical question: What risk factors could predict the likelihood of Pseudomonas and methicillin-resistant Staphylococcus aureus (MRSA) in patients hospitalized with healthcare-associated pneumonia (HCAP)?
Background: Patients identified with HCAP have an increased risk for multi-drug-resistant pathogens, such as gram-negative (GNR) organisms and MRSA. Meeting criteria for HCAP does not discriminate between the different infections, which require different antibiotic classes for treatment. Risk factors need to be identified to determine the most likely infectious organism to help guide initial empiric antibiotic therapy.
Study design: Retrospective cohort study.
Setting: Veterans Affairs hospitals.
Synopsis: Of 61,651 veterans with HCAP diagnosis, 1,156 (1.9%) had a discharge diagnosis of Pseudomonas pneumonia and were found to be younger and more likely to be immunocompromised; have hemiplegia; have a history of chronic obstructive pulmonary disease; have had corticosteroid exposure; and have been exposed to a fluoroquinolone, β-lactam, cephalosporin, or carbapenem antiobiotic within 90 days prior to admission. Pseudomonas pneumonia was negatively associated with age >84, drug abuse, diabetes, and higher socioeconomic status. A discharge diagnosis of MRSA pneumonia was found in 641 patients (1.0%), who also were positively associated with the male gender, age >74, recent nursing home stay, and recent exposure to fluoroquinolone antibiotics within 90 days prior to admission.
MRSA pneumonia was negatively associated with complicated diabetes. Neither diagnosis was present in 59,854 patients (97.1%).
This study was limited due to its predominantly male veteran population, low incidence of Pseudomonas and MRSA pneumonia being identified, and Pseudomonas as the only GNR organism analyzed.
Bottom line: Risk factors identified for Pseudomonas and MRSA pneumonia can help guide targeted antibiotics for HCAP patients.
Citation: Metersky ML, Frei CR, Mortenson EM. Predictors of Pseudomonas and methicillin-resistant Staphylococcus aureus in hospitalized patients with healthcare-associated pneumonia. Respirology. 2016;21(1):157-163.
Short Take
Hematuria as Marker of Urologic Cancer
Narrative literature review did not demonstrate beneficial role of screening urinalysis for cancer detection in asymptomatic patients, but it did suggest including gross hematuria as part of routine review of systems.
Citation: Nielsen M, Qaseem A, High Value Care Task Force of the American College of Physicians. Hematuria as a marker of occult urinary tract cancer: advice for high-value care from the American College of Physicians. Ann Intern Med. 2016;164(7):488-497. doi:10.7326/M15-1496.
Bile salts may be biomarker for recurrent C. difficile infection
SAN DIEGO – Bile acid salts in the stool may be a potential biomarker for recurrent episodes of Clostridium difficile infection, a preliminary study suggests.
Although the finding needs to be validated in a prospective study, it could have therapeutic implications, the study investigators said.
“If our results are validated, we could take bile salt profiles of patients who come in with their first episode of C. difficile infection and, using this biomarker, adjust therapy accordingly,” said study lead author Dr. Jessica Allegretti, who presented the findings at the annual Digestive Disease Week. “A patient at high risk of recurrence could get fecal transplant earlier. Right now, fecal transplant is used for recurrent infection.”
C. difficile represents a major public health threat, and recurrent disease complicates 20%-30% of cases.
The disease is communicated by spores that are resistant to heat and antibiotics, and they germinate in the gastrointestinal tract. Bile acids are part of that process. Bile acids assist in the digestion of fat, and a small proportion pass into the colon where primary bile acids undergo transformation into secondary bile acids such as deoxycholate and lithocholate.
In vitro, primary acids can stimulate C. difficile, explained Dr. Allegretti of Brigham and Women’s Hospital, Cambridge, Mass. “Antibiotic therapy may ablate critical members of the microbiota. We aimed to assess bile acid profiles in patients with C. difficile infection, compared with controls, to understand their role in pathogenesis and hopefully identify a biomarker for recurrence.”
The cross-sectional study collected serum and a single stool sample from three groups of 60 patients: patients with a first episode of C. difficile (fCDI) prior to antibiotics (20 patients), patients with a recurrent episode (rCDI) on treatment with chronic vancomycin at the time of sampling (19), and healthy controls who were fecal transplant donors (21).
The researchers sequenced stool microbial components and conducted bile salt metabolomic profiling. Significant differences were revealed in microbial analysis of the stool samples: Primary bile salts (which induce germination) were significantly elevated in rCDI, compared with fCDI and controls – while secondary bile salts in the stool (which are protective) such as deoxycholate and lithocholate were significantly elevated in controls, compared with fCDI and rCDI (P = .0002 and P = .0007, respectively).
“The same trends were seen in the plasma samples, but were less dramatic than in the stool,” Dr. Allegretti noted.
The median predicted bile salt hydrolase (BSH) gene abundance in rCDI was 20% of the median value in controls (P = .001), and it also was significantly lower than fCDI (P = .001). No significant difference was seen between predicted BSH gene abundance between controls and the fCDI groups.
“An association with reduced predicted bacterial bile salt hydrolase gene abundance may be associated with a diminished capacity to metabolize bile acids,” she said.
The difference in BSH gene abundance between controls and rCDI was largely due to changes in the abundance of 10 bacterial taxa, Dr. Allegretti said.
“This study reinforces the importance of bile salts in CDI and demonstrates for the first time in humans that this shift can be appreciated as early as the first episode of CDI in patients who are antibiotic naive,” Dr Allegretti said.
She noted that rCDI samples were collected in patients on chronic antibiotic therapy, and that may explain some of the decrease in biological microdiversity seen in the study.
In search of a biomarker, “secondary bile acids clearly seem to be the winner, and for now, stool seems to make more sense than blood for samples,” she stated.
Dr. Allegretti and her colleagues are conducting a prospective validation study.
The American College of Gastroenterology funded the study.
SAN DIEGO – Bile acid salts in the stool may be a potential biomarker for recurrent episodes of Clostridium difficile infection, a preliminary study suggests.
Although the finding needs to be validated in a prospective study, it could have therapeutic implications, the study investigators said.
“If our results are validated, we could take bile salt profiles of patients who come in with their first episode of C. difficile infection and, using this biomarker, adjust therapy accordingly,” said study lead author Dr. Jessica Allegretti, who presented the findings at the annual Digestive Disease Week. “A patient at high risk of recurrence could get fecal transplant earlier. Right now, fecal transplant is used for recurrent infection.”
C. difficile represents a major public health threat, and recurrent disease complicates 20%-30% of cases.
The disease is communicated by spores that are resistant to heat and antibiotics, and they germinate in the gastrointestinal tract. Bile acids are part of that process. Bile acids assist in the digestion of fat, and a small proportion pass into the colon where primary bile acids undergo transformation into secondary bile acids such as deoxycholate and lithocholate.
In vitro, primary acids can stimulate C. difficile, explained Dr. Allegretti of Brigham and Women’s Hospital, Cambridge, Mass. “Antibiotic therapy may ablate critical members of the microbiota. We aimed to assess bile acid profiles in patients with C. difficile infection, compared with controls, to understand their role in pathogenesis and hopefully identify a biomarker for recurrence.”
The cross-sectional study collected serum and a single stool sample from three groups of 60 patients: patients with a first episode of C. difficile (fCDI) prior to antibiotics (20 patients), patients with a recurrent episode (rCDI) on treatment with chronic vancomycin at the time of sampling (19), and healthy controls who were fecal transplant donors (21).
The researchers sequenced stool microbial components and conducted bile salt metabolomic profiling. Significant differences were revealed in microbial analysis of the stool samples: Primary bile salts (which induce germination) were significantly elevated in rCDI, compared with fCDI and controls – while secondary bile salts in the stool (which are protective) such as deoxycholate and lithocholate were significantly elevated in controls, compared with fCDI and rCDI (P = .0002 and P = .0007, respectively).
“The same trends were seen in the plasma samples, but were less dramatic than in the stool,” Dr. Allegretti noted.
The median predicted bile salt hydrolase (BSH) gene abundance in rCDI was 20% of the median value in controls (P = .001), and it also was significantly lower than fCDI (P = .001). No significant difference was seen between predicted BSH gene abundance between controls and the fCDI groups.
“An association with reduced predicted bacterial bile salt hydrolase gene abundance may be associated with a diminished capacity to metabolize bile acids,” she said.
The difference in BSH gene abundance between controls and rCDI was largely due to changes in the abundance of 10 bacterial taxa, Dr. Allegretti said.
“This study reinforces the importance of bile salts in CDI and demonstrates for the first time in humans that this shift can be appreciated as early as the first episode of CDI in patients who are antibiotic naive,” Dr Allegretti said.
She noted that rCDI samples were collected in patients on chronic antibiotic therapy, and that may explain some of the decrease in biological microdiversity seen in the study.
In search of a biomarker, “secondary bile acids clearly seem to be the winner, and for now, stool seems to make more sense than blood for samples,” she stated.
Dr. Allegretti and her colleagues are conducting a prospective validation study.
The American College of Gastroenterology funded the study.
SAN DIEGO – Bile acid salts in the stool may be a potential biomarker for recurrent episodes of Clostridium difficile infection, a preliminary study suggests.
Although the finding needs to be validated in a prospective study, it could have therapeutic implications, the study investigators said.
“If our results are validated, we could take bile salt profiles of patients who come in with their first episode of C. difficile infection and, using this biomarker, adjust therapy accordingly,” said study lead author Dr. Jessica Allegretti, who presented the findings at the annual Digestive Disease Week. “A patient at high risk of recurrence could get fecal transplant earlier. Right now, fecal transplant is used for recurrent infection.”
C. difficile represents a major public health threat, and recurrent disease complicates 20%-30% of cases.
The disease is communicated by spores that are resistant to heat and antibiotics, and they germinate in the gastrointestinal tract. Bile acids are part of that process. Bile acids assist in the digestion of fat, and a small proportion pass into the colon where primary bile acids undergo transformation into secondary bile acids such as deoxycholate and lithocholate.
In vitro, primary acids can stimulate C. difficile, explained Dr. Allegretti of Brigham and Women’s Hospital, Cambridge, Mass. “Antibiotic therapy may ablate critical members of the microbiota. We aimed to assess bile acid profiles in patients with C. difficile infection, compared with controls, to understand their role in pathogenesis and hopefully identify a biomarker for recurrence.”
The cross-sectional study collected serum and a single stool sample from three groups of 60 patients: patients with a first episode of C. difficile (fCDI) prior to antibiotics (20 patients), patients with a recurrent episode (rCDI) on treatment with chronic vancomycin at the time of sampling (19), and healthy controls who were fecal transplant donors (21).
The researchers sequenced stool microbial components and conducted bile salt metabolomic profiling. Significant differences were revealed in microbial analysis of the stool samples: Primary bile salts (which induce germination) were significantly elevated in rCDI, compared with fCDI and controls – while secondary bile salts in the stool (which are protective) such as deoxycholate and lithocholate were significantly elevated in controls, compared with fCDI and rCDI (P = .0002 and P = .0007, respectively).
“The same trends were seen in the plasma samples, but were less dramatic than in the stool,” Dr. Allegretti noted.
The median predicted bile salt hydrolase (BSH) gene abundance in rCDI was 20% of the median value in controls (P = .001), and it also was significantly lower than fCDI (P = .001). No significant difference was seen between predicted BSH gene abundance between controls and the fCDI groups.
“An association with reduced predicted bacterial bile salt hydrolase gene abundance may be associated with a diminished capacity to metabolize bile acids,” she said.
The difference in BSH gene abundance between controls and rCDI was largely due to changes in the abundance of 10 bacterial taxa, Dr. Allegretti said.
“This study reinforces the importance of bile salts in CDI and demonstrates for the first time in humans that this shift can be appreciated as early as the first episode of CDI in patients who are antibiotic naive,” Dr Allegretti said.
She noted that rCDI samples were collected in patients on chronic antibiotic therapy, and that may explain some of the decrease in biological microdiversity seen in the study.
In search of a biomarker, “secondary bile acids clearly seem to be the winner, and for now, stool seems to make more sense than blood for samples,” she stated.
Dr. Allegretti and her colleagues are conducting a prospective validation study.
The American College of Gastroenterology funded the study.
AT DDW® 2016
Key clinical point: Bile salt acids may identify patients at risk of recurrent Clostridium difficile infection who require more aggressive first-line therapy.
Major finding: Secondary bile acids in stool can distinguish between first-episode patients, recurrent-episode patients, and healthy controls.
Data source: A prospective cross-sectional study of 60 participants.
Disclosures: The American College of Gastroenterology funded the study.
Study: Number of MRSA cases in Japan may be underestimated
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
Key clinical point: Sentinel surveillance systems may substantially underestimate the number of methicillin-resistant Staphylococcus aureus cases in Japan.
Major finding: Direct notification to the Japan Nosocomial Infections Surveillance system regarding methicillin-resistant Staphylococcus aureus patients was not affected by patients’ age, and information from health insurance claims was useful for evaluation of the sentinel infection surveillance system.
Data sources: The Japan Nosocomial Infections Surveillance system and the National Health Insurance Organization.
Disclosures: Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
FDA warns against routine fluoroquinolone use
The U.S. Food and Drug Administration has issued a warning to health care providers against the routine prescribing of fluoroquinolone antibiotics to those patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options.
After conducting a safety review of the drugs, the FDA concluded that fluoroquinolone should be reserved for those patients who do not have alternative treatment options, in light of the findings that the antibiotics – when used systemically in either tablet, capsule, or injectable form – are associated with “disabling and potentially permanent serious side effects” that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system, according to the agency.
The FDA says health care providers should stop systemic fluoroquinolone treatment immediately in patients reporting serious side effects and switch to a non-fluoroquinolone antibacterial drug to complete the patient’s treatment course. The drug labels and medication guides for all fluoroquinolone antibiotics will be updated to reflect the new safety information.
The FDA had previously communicated safety information associated with systemic fluoroquinolone antibacterial drugs in August 2013 and July 2008, and the safety issues described in the current warning were discussed at an FDA Advisory Committee meeting in November 2015.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued a warning to health care providers against the routine prescribing of fluoroquinolone antibiotics to those patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options.
After conducting a safety review of the drugs, the FDA concluded that fluoroquinolone should be reserved for those patients who do not have alternative treatment options, in light of the findings that the antibiotics – when used systemically in either tablet, capsule, or injectable form – are associated with “disabling and potentially permanent serious side effects” that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system, according to the agency.
The FDA says health care providers should stop systemic fluoroquinolone treatment immediately in patients reporting serious side effects and switch to a non-fluoroquinolone antibacterial drug to complete the patient’s treatment course. The drug labels and medication guides for all fluoroquinolone antibiotics will be updated to reflect the new safety information.
The FDA had previously communicated safety information associated with systemic fluoroquinolone antibacterial drugs in August 2013 and July 2008, and the safety issues described in the current warning were discussed at an FDA Advisory Committee meeting in November 2015.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued a warning to health care providers against the routine prescribing of fluoroquinolone antibiotics to those patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options.
After conducting a safety review of the drugs, the FDA concluded that fluoroquinolone should be reserved for those patients who do not have alternative treatment options, in light of the findings that the antibiotics – when used systemically in either tablet, capsule, or injectable form – are associated with “disabling and potentially permanent serious side effects” that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system, according to the agency.
The FDA says health care providers should stop systemic fluoroquinolone treatment immediately in patients reporting serious side effects and switch to a non-fluoroquinolone antibacterial drug to complete the patient’s treatment course. The drug labels and medication guides for all fluoroquinolone antibiotics will be updated to reflect the new safety information.
The FDA had previously communicated safety information associated with systemic fluoroquinolone antibacterial drugs in August 2013 and July 2008, and the safety issues described in the current warning were discussed at an FDA Advisory Committee meeting in November 2015.
On Twitter @richpizzi
Daptomycin beats infective endocarditis caused by several pathogens
AT ECCMID 2016
AMSTERDAM – Daptomycin successfully treated infective endocarditis in 90% of patients who developed it after undergoing heart valve replacement, according to a report presented at the annual congress of the European Society of Clinical Microbiology and Infectious Diseases.
Dr. Achyut Guleri, clinical director of laboratory medicine at Blackpool Victoria Hospital, Lancashire, England, said the lipopeptide antibiotic was equally effective against methicillin- and penicillin-resistant Staphylococcus aureus, coagulase-negative staphylococcus, and enterococci.
“This is particularly good to know because sometimes in real life, on the shop floor, you don’t always have a very clear insight into what you’re trying to treat,” said Dr. Guleri. “It’s reassuring to see that the success rate is similar in all these infections.”
He presented a subgroup analysis of patients enrolled in European Cubicin Outcomes Registry and Experience (EUCORE), a retrospective, noninterventional, postmarketing registry. The 4-year study reported real-world clinical experience of daptomycin use for the treatment of Gram-positive infections in patients with infective endocarditis who had undergone heart valve replacement.
Typically, Dr. Guleri said, vancomycin, either alone or with rifampicin, is recommended for the infection. “However, with increasing antibiotic resistance, vancomycin doesn’t inspire much confidence, especially for MRSA infections,” he noted.
Daptomycin is increasingly employed as an alternative treatment. It exhibits rapid bactericidal activity against a wide range of Gram-positive pathogens, including MRSA. It’s approved for the treatment of right-sided infective endocarditis due to S. aureus, at a dose of 6 mg/kg per day. However, higher doses are now recommended by several international guidelines and are often used for hard-to-treat infections, Dr. Guleri said.
EUCORE comprised 6,075 patients from 18 countries who were enrolled from 2006 to 2012. Patients were followed until 2014. Of this group, 610 had infective endocarditis and 198 underwent valve replacement. Most were male (70%); mean age was 58 years. Medical comorbidities were common and included renal disease, sepsis, diabetes, pulmonary disease, gastrointestinal disease, cerebrovascular disease and inflammatory diseases.
Culture results were available for 87%. Of these, 68% were positive. The most common pathogen was S. aureus (37%). Half of these isolates were penicillin resistant and 35% were methicillin resistant. Enterococci were responsible for 14% of the infections, and coagulase-negative staph for 32%. The rest were caused by other pathogens.
Before trying daptomycin, most patients (83%) had already been treated with an antibiotic, which was employed in conjunction with another antibiotic in 77% of cases. The concomitant medications included rifampicin (31%), aminoglycosides (29%) and carbapenems (18%).
The overall clinical cure rate at 2 years was 90%. Daptomycin was equally effective in left- and right-sided disease, and was more effective in penicillin-resistant staph (95%) than methicillin-resistant staph (80%). The cure rate was also good in coagulase-negative staph (81%) and enterococci (75%).
High doses were more effective than low doses. At 4 mg/kg per day, the cure rate was 61%. At 6 mg/kg per day, it was 86%, and at more than 6 mg/kg per day, it was 90%.
Adverse events were rare (3%). Three patients developed increased creatine phosphokinase levels; one patient developed rhabdomyolysis and one developed cholestasis. Agranulocytosis developed in three patients and eosinophilic pneumonia in three. One patient developed a rash. No one discontinued the drug due to a side effect.
Dr. Guleri had no financial disclosures.
On Twitter @Alz_Gal
AT ECCMID 2016
AMSTERDAM – Daptomycin successfully treated infective endocarditis in 90% of patients who developed it after undergoing heart valve replacement, according to a report presented at the annual congress of the European Society of Clinical Microbiology and Infectious Diseases.
Dr. Achyut Guleri, clinical director of laboratory medicine at Blackpool Victoria Hospital, Lancashire, England, said the lipopeptide antibiotic was equally effective against methicillin- and penicillin-resistant Staphylococcus aureus, coagulase-negative staphylococcus, and enterococci.
“This is particularly good to know because sometimes in real life, on the shop floor, you don’t always have a very clear insight into what you’re trying to treat,” said Dr. Guleri. “It’s reassuring to see that the success rate is similar in all these infections.”
He presented a subgroup analysis of patients enrolled in European Cubicin Outcomes Registry and Experience (EUCORE), a retrospective, noninterventional, postmarketing registry. The 4-year study reported real-world clinical experience of daptomycin use for the treatment of Gram-positive infections in patients with infective endocarditis who had undergone heart valve replacement.
Typically, Dr. Guleri said, vancomycin, either alone or with rifampicin, is recommended for the infection. “However, with increasing antibiotic resistance, vancomycin doesn’t inspire much confidence, especially for MRSA infections,” he noted.
Daptomycin is increasingly employed as an alternative treatment. It exhibits rapid bactericidal activity against a wide range of Gram-positive pathogens, including MRSA. It’s approved for the treatment of right-sided infective endocarditis due to S. aureus, at a dose of 6 mg/kg per day. However, higher doses are now recommended by several international guidelines and are often used for hard-to-treat infections, Dr. Guleri said.
EUCORE comprised 6,075 patients from 18 countries who were enrolled from 2006 to 2012. Patients were followed until 2014. Of this group, 610 had infective endocarditis and 198 underwent valve replacement. Most were male (70%); mean age was 58 years. Medical comorbidities were common and included renal disease, sepsis, diabetes, pulmonary disease, gastrointestinal disease, cerebrovascular disease and inflammatory diseases.
Culture results were available for 87%. Of these, 68% were positive. The most common pathogen was S. aureus (37%). Half of these isolates were penicillin resistant and 35% were methicillin resistant. Enterococci were responsible for 14% of the infections, and coagulase-negative staph for 32%. The rest were caused by other pathogens.
Before trying daptomycin, most patients (83%) had already been treated with an antibiotic, which was employed in conjunction with another antibiotic in 77% of cases. The concomitant medications included rifampicin (31%), aminoglycosides (29%) and carbapenems (18%).
The overall clinical cure rate at 2 years was 90%. Daptomycin was equally effective in left- and right-sided disease, and was more effective in penicillin-resistant staph (95%) than methicillin-resistant staph (80%). The cure rate was also good in coagulase-negative staph (81%) and enterococci (75%).
High doses were more effective than low doses. At 4 mg/kg per day, the cure rate was 61%. At 6 mg/kg per day, it was 86%, and at more than 6 mg/kg per day, it was 90%.
Adverse events were rare (3%). Three patients developed increased creatine phosphokinase levels; one patient developed rhabdomyolysis and one developed cholestasis. Agranulocytosis developed in three patients and eosinophilic pneumonia in three. One patient developed a rash. No one discontinued the drug due to a side effect.
Dr. Guleri had no financial disclosures.
On Twitter @Alz_Gal
AT ECCMID 2016
AMSTERDAM – Daptomycin successfully treated infective endocarditis in 90% of patients who developed it after undergoing heart valve replacement, according to a report presented at the annual congress of the European Society of Clinical Microbiology and Infectious Diseases.
Dr. Achyut Guleri, clinical director of laboratory medicine at Blackpool Victoria Hospital, Lancashire, England, said the lipopeptide antibiotic was equally effective against methicillin- and penicillin-resistant Staphylococcus aureus, coagulase-negative staphylococcus, and enterococci.
“This is particularly good to know because sometimes in real life, on the shop floor, you don’t always have a very clear insight into what you’re trying to treat,” said Dr. Guleri. “It’s reassuring to see that the success rate is similar in all these infections.”
He presented a subgroup analysis of patients enrolled in European Cubicin Outcomes Registry and Experience (EUCORE), a retrospective, noninterventional, postmarketing registry. The 4-year study reported real-world clinical experience of daptomycin use for the treatment of Gram-positive infections in patients with infective endocarditis who had undergone heart valve replacement.
Typically, Dr. Guleri said, vancomycin, either alone or with rifampicin, is recommended for the infection. “However, with increasing antibiotic resistance, vancomycin doesn’t inspire much confidence, especially for MRSA infections,” he noted.
Daptomycin is increasingly employed as an alternative treatment. It exhibits rapid bactericidal activity against a wide range of Gram-positive pathogens, including MRSA. It’s approved for the treatment of right-sided infective endocarditis due to S. aureus, at a dose of 6 mg/kg per day. However, higher doses are now recommended by several international guidelines and are often used for hard-to-treat infections, Dr. Guleri said.
EUCORE comprised 6,075 patients from 18 countries who were enrolled from 2006 to 2012. Patients were followed until 2014. Of this group, 610 had infective endocarditis and 198 underwent valve replacement. Most were male (70%); mean age was 58 years. Medical comorbidities were common and included renal disease, sepsis, diabetes, pulmonary disease, gastrointestinal disease, cerebrovascular disease and inflammatory diseases.
Culture results were available for 87%. Of these, 68% were positive. The most common pathogen was S. aureus (37%). Half of these isolates were penicillin resistant and 35% were methicillin resistant. Enterococci were responsible for 14% of the infections, and coagulase-negative staph for 32%. The rest were caused by other pathogens.
Before trying daptomycin, most patients (83%) had already been treated with an antibiotic, which was employed in conjunction with another antibiotic in 77% of cases. The concomitant medications included rifampicin (31%), aminoglycosides (29%) and carbapenems (18%).
The overall clinical cure rate at 2 years was 90%. Daptomycin was equally effective in left- and right-sided disease, and was more effective in penicillin-resistant staph (95%) than methicillin-resistant staph (80%). The cure rate was also good in coagulase-negative staph (81%) and enterococci (75%).
High doses were more effective than low doses. At 4 mg/kg per day, the cure rate was 61%. At 6 mg/kg per day, it was 86%, and at more than 6 mg/kg per day, it was 90%.
Adverse events were rare (3%). Three patients developed increased creatine phosphokinase levels; one patient developed rhabdomyolysis and one developed cholestasis. Agranulocytosis developed in three patients and eosinophilic pneumonia in three. One patient developed a rash. No one discontinued the drug due to a side effect.
Dr. Guleri had no financial disclosures.
On Twitter @Alz_Gal
Key clinical point: Daptomycin had a high cure rate for infective endocarditis caused by MRSA, MSSA, coagulase-negative staph, and enterococci.
Major finding: The 2-year clinical cure rate was 90% for S. aureus infections.
Data source: Retrospective analysis of EUCORE, which comprised 198 patients.
Disclosures: Dr. Guleri had no financial disclosures.
MRSA prevalence in asymptomatic athletes comparable to dialysis, HIV patients
The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is more than three times higher than the rate reported for the community population overall, a systematic review and meta-analysis showed.
Investigators searched PubMed and EMBASE looking for studies on MRSA colonization among the athletic community. They did not include studies involving individuals who previously were infected or had active MRSA infections. The database search yielded 382 studies, and of those, 15 were included in the meta-analysis, reported Dr. Styliani Karanika of Rhode Island Hospital’s infectious diseases division at Brown University, Providence, R.I. (Clin Infect Dis. 2016 April 18. doi: 10.1093/cid/ciw240).
By conducting a statistical analysis among 1,495 screened asymptomatic athletic team members (athletes and staff), Dr. Karanika and colleagues were able to see how the prevalence of MRSA colonization differed among athletes by level of playing experience and sport. The investigators found that the 6% prevalence of MRSA colonization among asymptomatic athletes was comparable to the prevalence among patients on dialysis (6%) and those with HIV (6.9%). Among college athletes, the 13% prevalence of MRSA was almost twice the rate found among patients in intensive care units (7%).
When it came to individual sports, the highest prevalence was found in wrestling (22%), followed by football (8%) and basketball (8%). The risk for subsequent MRSA skin and soft tissue infection among colonized athletes was more than seven times higher than the risk of MRSA skin and soft tissue infection among noncolonized athletes within a 3-month follow-up period upon documented MRSA colonization. Decolonization treatment was effective in reducing the risk of infection in colonized individuals.
“Our findings highlight the importance of controlling the spread of MRSA in the athletic setting, particularly among collegiate athletes,” Dr. Karanika said in an interview.
Dr. Karanika noted that athletes are more susceptible to MRSA because of the frequency of skin abrasions, close contact, shared equipment and training facilities, and poor hygiene practices that can result from the intense demands and time restrictions. Because the prevalence of MRSA colonization is high among this group, coaches, athletes, and athletic trainers should be aware of the early symptoms of a MRSA skin and soft tissue infection, and they should be educated about proper hygiene and prevention and control protocols to halt the spread of MRSA.
Though researchers found decolonization to be effective at reducing the risk of subsequent infection, they believe more research is needed to determine the durability and feasibility of decolonization regimens. Until these protocols are established, they said, strategies including implementing MRSA surveillance in athletes, environmental surveys, and regularly occurring physical examinations of athletes over the course of the season might help break the cycle of MRSA colonization-infection-transmission in athletic settings.
The investigators declared no conflicts of interest.
The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is more than three times higher than the rate reported for the community population overall, a systematic review and meta-analysis showed.
Investigators searched PubMed and EMBASE looking for studies on MRSA colonization among the athletic community. They did not include studies involving individuals who previously were infected or had active MRSA infections. The database search yielded 382 studies, and of those, 15 were included in the meta-analysis, reported Dr. Styliani Karanika of Rhode Island Hospital’s infectious diseases division at Brown University, Providence, R.I. (Clin Infect Dis. 2016 April 18. doi: 10.1093/cid/ciw240).
By conducting a statistical analysis among 1,495 screened asymptomatic athletic team members (athletes and staff), Dr. Karanika and colleagues were able to see how the prevalence of MRSA colonization differed among athletes by level of playing experience and sport. The investigators found that the 6% prevalence of MRSA colonization among asymptomatic athletes was comparable to the prevalence among patients on dialysis (6%) and those with HIV (6.9%). Among college athletes, the 13% prevalence of MRSA was almost twice the rate found among patients in intensive care units (7%).
When it came to individual sports, the highest prevalence was found in wrestling (22%), followed by football (8%) and basketball (8%). The risk for subsequent MRSA skin and soft tissue infection among colonized athletes was more than seven times higher than the risk of MRSA skin and soft tissue infection among noncolonized athletes within a 3-month follow-up period upon documented MRSA colonization. Decolonization treatment was effective in reducing the risk of infection in colonized individuals.
“Our findings highlight the importance of controlling the spread of MRSA in the athletic setting, particularly among collegiate athletes,” Dr. Karanika said in an interview.
Dr. Karanika noted that athletes are more susceptible to MRSA because of the frequency of skin abrasions, close contact, shared equipment and training facilities, and poor hygiene practices that can result from the intense demands and time restrictions. Because the prevalence of MRSA colonization is high among this group, coaches, athletes, and athletic trainers should be aware of the early symptoms of a MRSA skin and soft tissue infection, and they should be educated about proper hygiene and prevention and control protocols to halt the spread of MRSA.
Though researchers found decolonization to be effective at reducing the risk of subsequent infection, they believe more research is needed to determine the durability and feasibility of decolonization regimens. Until these protocols are established, they said, strategies including implementing MRSA surveillance in athletes, environmental surveys, and regularly occurring physical examinations of athletes over the course of the season might help break the cycle of MRSA colonization-infection-transmission in athletic settings.
The investigators declared no conflicts of interest.
The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is more than three times higher than the rate reported for the community population overall, a systematic review and meta-analysis showed.
Investigators searched PubMed and EMBASE looking for studies on MRSA colonization among the athletic community. They did not include studies involving individuals who previously were infected or had active MRSA infections. The database search yielded 382 studies, and of those, 15 were included in the meta-analysis, reported Dr. Styliani Karanika of Rhode Island Hospital’s infectious diseases division at Brown University, Providence, R.I. (Clin Infect Dis. 2016 April 18. doi: 10.1093/cid/ciw240).
By conducting a statistical analysis among 1,495 screened asymptomatic athletic team members (athletes and staff), Dr. Karanika and colleagues were able to see how the prevalence of MRSA colonization differed among athletes by level of playing experience and sport. The investigators found that the 6% prevalence of MRSA colonization among asymptomatic athletes was comparable to the prevalence among patients on dialysis (6%) and those with HIV (6.9%). Among college athletes, the 13% prevalence of MRSA was almost twice the rate found among patients in intensive care units (7%).
When it came to individual sports, the highest prevalence was found in wrestling (22%), followed by football (8%) and basketball (8%). The risk for subsequent MRSA skin and soft tissue infection among colonized athletes was more than seven times higher than the risk of MRSA skin and soft tissue infection among noncolonized athletes within a 3-month follow-up period upon documented MRSA colonization. Decolonization treatment was effective in reducing the risk of infection in colonized individuals.
“Our findings highlight the importance of controlling the spread of MRSA in the athletic setting, particularly among collegiate athletes,” Dr. Karanika said in an interview.
Dr. Karanika noted that athletes are more susceptible to MRSA because of the frequency of skin abrasions, close contact, shared equipment and training facilities, and poor hygiene practices that can result from the intense demands and time restrictions. Because the prevalence of MRSA colonization is high among this group, coaches, athletes, and athletic trainers should be aware of the early symptoms of a MRSA skin and soft tissue infection, and they should be educated about proper hygiene and prevention and control protocols to halt the spread of MRSA.
Though researchers found decolonization to be effective at reducing the risk of subsequent infection, they believe more research is needed to determine the durability and feasibility of decolonization regimens. Until these protocols are established, they said, strategies including implementing MRSA surveillance in athletes, environmental surveys, and regularly occurring physical examinations of athletes over the course of the season might help break the cycle of MRSA colonization-infection-transmission in athletic settings.
The investigators declared no conflicts of interest.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: The prevalence of methicillin-resistant Staphylococcus aureus colonization among asymptomatic athletes is comparable to that among individuals with chronic illnesses.
Major finding: The prevalence of MRSA colonization was 8% among U.S. athletes and 13% among U.S. collegiate athletes. The prevalence of MRSA in the total athletic population was comparable to MRSA in patients with illnesses such as kidney disease and HIV.
Data source: A PubMed and EMBASE search yielded 382 studies and was narrowed to 15 analyses.
Disclosures: The investigators declared no conflicts of interest.
USDA to release more funds for antibiotic resistance research
The U.S. Department of Agriculture has made $6 million available through its Agriculture and Food Research Initiative to fund research on antimicrobial resistance.
“The research projects funded through this announcement will help us succeed in our efforts to preserve the effectiveness of antibiotics and protect public health,” said U.S. Agriculture Secretary Tom Vilsack in a statement.
The funding is authorized by the 2014 Farm Bill and administered by the USDA’s National Institute of Food and Agriculture. Secretary Vilsack said it is one of many ways that the USDA supports the Combating Antimicrobial Resistant Bacteria (CARB) National Action Plan and work of the Task Force for Combating Antibiotic Resistance, which the USDA cochairs. The program priority is to promote the development of sustainable and integrated food safety strategies that reduce public health risks along the entire food chain.
According to the USDA announcement, applications for funding must address one or more of the following:
• Develop novel systems approaches to investigate the ecology of microbial resistance microbes and gene reservoirs in the environment in animals, crops, food products, or farm-raised aquaculture products.
• Develop, evaluate, and implement effective and sustainable resources and strategies, to include alternative practices, techniques, technologies, or tools that mitigate emergence, spread, or persistence of antimicrobial-resistant pathogens within the agricultural ecosystem, in animals, crops, and food.
• Identify critical control points for mitigating antimicrobial resistance in the pre- and postharvest food production environment.
• Design innovative training, education, and outreach resources (including Web-based resources) that can be adapted by users across the food chain, including policy makers, producers, processors, retailers, and consumers.
• Design and conduct studies that evaluate the impact and efficacy of proposed research, education, and extension/outreach interventions on antimicrobial resistance across the food chain, from primary producers to primary consumers.
Since 2009, more than $82 million in food safety research and extension grants has been awarded through the Agriculture and Food Research Initiative, including $3.4 million in fiscal year 2015 for antimicrobial resistance. Previously funded projects include a State University of New York project evaluating critical control points in dairy farm operations and a Texas A&M University project to develop science-based decision aids related to antibiotic stewardship.
Applications are due Aug. 3, 2016. See the request for applications for more information.
On Twitter @richpizzi
The U.S. Department of Agriculture has made $6 million available through its Agriculture and Food Research Initiative to fund research on antimicrobial resistance.
“The research projects funded through this announcement will help us succeed in our efforts to preserve the effectiveness of antibiotics and protect public health,” said U.S. Agriculture Secretary Tom Vilsack in a statement.
The funding is authorized by the 2014 Farm Bill and administered by the USDA’s National Institute of Food and Agriculture. Secretary Vilsack said it is one of many ways that the USDA supports the Combating Antimicrobial Resistant Bacteria (CARB) National Action Plan and work of the Task Force for Combating Antibiotic Resistance, which the USDA cochairs. The program priority is to promote the development of sustainable and integrated food safety strategies that reduce public health risks along the entire food chain.
According to the USDA announcement, applications for funding must address one or more of the following:
• Develop novel systems approaches to investigate the ecology of microbial resistance microbes and gene reservoirs in the environment in animals, crops, food products, or farm-raised aquaculture products.
• Develop, evaluate, and implement effective and sustainable resources and strategies, to include alternative practices, techniques, technologies, or tools that mitigate emergence, spread, or persistence of antimicrobial-resistant pathogens within the agricultural ecosystem, in animals, crops, and food.
• Identify critical control points for mitigating antimicrobial resistance in the pre- and postharvest food production environment.
• Design innovative training, education, and outreach resources (including Web-based resources) that can be adapted by users across the food chain, including policy makers, producers, processors, retailers, and consumers.
• Design and conduct studies that evaluate the impact and efficacy of proposed research, education, and extension/outreach interventions on antimicrobial resistance across the food chain, from primary producers to primary consumers.
Since 2009, more than $82 million in food safety research and extension grants has been awarded through the Agriculture and Food Research Initiative, including $3.4 million in fiscal year 2015 for antimicrobial resistance. Previously funded projects include a State University of New York project evaluating critical control points in dairy farm operations and a Texas A&M University project to develop science-based decision aids related to antibiotic stewardship.
Applications are due Aug. 3, 2016. See the request for applications for more information.
On Twitter @richpizzi
The U.S. Department of Agriculture has made $6 million available through its Agriculture and Food Research Initiative to fund research on antimicrobial resistance.
“The research projects funded through this announcement will help us succeed in our efforts to preserve the effectiveness of antibiotics and protect public health,” said U.S. Agriculture Secretary Tom Vilsack in a statement.
The funding is authorized by the 2014 Farm Bill and administered by the USDA’s National Institute of Food and Agriculture. Secretary Vilsack said it is one of many ways that the USDA supports the Combating Antimicrobial Resistant Bacteria (CARB) National Action Plan and work of the Task Force for Combating Antibiotic Resistance, which the USDA cochairs. The program priority is to promote the development of sustainable and integrated food safety strategies that reduce public health risks along the entire food chain.
According to the USDA announcement, applications for funding must address one or more of the following:
• Develop novel systems approaches to investigate the ecology of microbial resistance microbes and gene reservoirs in the environment in animals, crops, food products, or farm-raised aquaculture products.
• Develop, evaluate, and implement effective and sustainable resources and strategies, to include alternative practices, techniques, technologies, or tools that mitigate emergence, spread, or persistence of antimicrobial-resistant pathogens within the agricultural ecosystem, in animals, crops, and food.
• Identify critical control points for mitigating antimicrobial resistance in the pre- and postharvest food production environment.
• Design innovative training, education, and outreach resources (including Web-based resources) that can be adapted by users across the food chain, including policy makers, producers, processors, retailers, and consumers.
• Design and conduct studies that evaluate the impact and efficacy of proposed research, education, and extension/outreach interventions on antimicrobial resistance across the food chain, from primary producers to primary consumers.
Since 2009, more than $82 million in food safety research and extension grants has been awarded through the Agriculture and Food Research Initiative, including $3.4 million in fiscal year 2015 for antimicrobial resistance. Previously funded projects include a State University of New York project evaluating critical control points in dairy farm operations and a Texas A&M University project to develop science-based decision aids related to antibiotic stewardship.
Applications are due Aug. 3, 2016. See the request for applications for more information.
On Twitter @richpizzi
Mixing, cycling of antibiotics fails to reduce antibiotic resistance
AMSTERDAM – Neither cycling through a regular schedule of antibiotics on a unit-wide basis, nor randomly mixing them on a patient-level basis reduced the prevalence of antibiotic resistance in eight European intensive care units, a randomized study has determined.
Lead investigator Dr. Pleun Joppe van Duijn of University Medical Center Utrecht (the Netherlands), said he and his colleagues did, however, discover a few common sense findings that seemed to positively affect antibiotic resistance, including compliance with hand hygiene, shorter lengths of stay, staff ratio, and unit occupancy rate. He reported the results of his research at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
Many ICUs in Europe have one preferred empirical treatment strategy which, Dr. van Duijn said, may create selective pressure for a single resistance type. “An alternative to this is a program of antibiotic rotation,” he noted. “By constantly changing the preferred first-line treatment, selective pressure is constantly changing, which may reduce selection of antibiotic resistance.”
Dr. van Duijn and his colleagues examined this idea in a randomized crossover trial that compared antibiotic cycling and mixing. The protocols employed three antibiotic classes: third- and fourth-generation cephalosporins, piperacillin/tazobactam, and carbapenems. The trial was conducted in eight ICUs in Belgium, Germany, France, Slovenia, and Portugal.
The sites were randomized to two 9-month interventions of cycling or mixing antibiotics, with a 1-month washout period between the two interventions. In cycling protocol, the preferred empiric antibiotic was changed every 6 weeks. In the mixing protocol, every consecutive patient received a different antibiotic. However, treating physicians were allowed to deviate from any protocol for patient safety or to optimize treatment.
The primary endpoint was the monthly prevalence of perineal and/or respiratory carriage of two classes of bacteria:
• Enterobacteriaceae species that were piperacillin/tazobactam–resistant or that showed extended spectrum beta-lactamase production.
• Pseudomonas aeruginosa and Acinetobacter species that were either piperacillin/tazobactam– or carbapenem-resistant.
In all, 8,945 patients were involved, with 4,238 exposed to cycling and 4,707 to mixing. Patients were a mean of 62 years old, with a mean 7-day length of stay. About 4.5% were already colonized with resistant bacteria upon admission. A quarter were on contact isolation; 2% were on both droplet and respiratory isolation.
The overall mortality rate was 11% and did not differ between the cycling and mixing groups (10.9% vs. 11.6%). Antibiotic resistance developed in 22.6% of the cycling group and 21.5% of the mixing group – not a significant difference. Neither protocol significantly reduced over time the amount of antibiotic resistance that was observed in the baseline period.
A multivariate analysis did, however, find a few things associated with resistance prevalence. Women were about 58% less likely to develop a resistant bacterial strain than men. Patients who stayed less than 48 hours had a 38% decreased risk of developing a resistant strain. Good staff compliance with hand hygiene reduced the risk by 12%, and having one-on-one nursing reduced it by 53%.
The study was funded by the European Community’s Seventh Framework Programme. Dr. van Duijn had no financial declarations.
AMSTERDAM – Neither cycling through a regular schedule of antibiotics on a unit-wide basis, nor randomly mixing them on a patient-level basis reduced the prevalence of antibiotic resistance in eight European intensive care units, a randomized study has determined.
Lead investigator Dr. Pleun Joppe van Duijn of University Medical Center Utrecht (the Netherlands), said he and his colleagues did, however, discover a few common sense findings that seemed to positively affect antibiotic resistance, including compliance with hand hygiene, shorter lengths of stay, staff ratio, and unit occupancy rate. He reported the results of his research at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
Many ICUs in Europe have one preferred empirical treatment strategy which, Dr. van Duijn said, may create selective pressure for a single resistance type. “An alternative to this is a program of antibiotic rotation,” he noted. “By constantly changing the preferred first-line treatment, selective pressure is constantly changing, which may reduce selection of antibiotic resistance.”
Dr. van Duijn and his colleagues examined this idea in a randomized crossover trial that compared antibiotic cycling and mixing. The protocols employed three antibiotic classes: third- and fourth-generation cephalosporins, piperacillin/tazobactam, and carbapenems. The trial was conducted in eight ICUs in Belgium, Germany, France, Slovenia, and Portugal.
The sites were randomized to two 9-month interventions of cycling or mixing antibiotics, with a 1-month washout period between the two interventions. In cycling protocol, the preferred empiric antibiotic was changed every 6 weeks. In the mixing protocol, every consecutive patient received a different antibiotic. However, treating physicians were allowed to deviate from any protocol for patient safety or to optimize treatment.
The primary endpoint was the monthly prevalence of perineal and/or respiratory carriage of two classes of bacteria:
• Enterobacteriaceae species that were piperacillin/tazobactam–resistant or that showed extended spectrum beta-lactamase production.
• Pseudomonas aeruginosa and Acinetobacter species that were either piperacillin/tazobactam– or carbapenem-resistant.
In all, 8,945 patients were involved, with 4,238 exposed to cycling and 4,707 to mixing. Patients were a mean of 62 years old, with a mean 7-day length of stay. About 4.5% were already colonized with resistant bacteria upon admission. A quarter were on contact isolation; 2% were on both droplet and respiratory isolation.
The overall mortality rate was 11% and did not differ between the cycling and mixing groups (10.9% vs. 11.6%). Antibiotic resistance developed in 22.6% of the cycling group and 21.5% of the mixing group – not a significant difference. Neither protocol significantly reduced over time the amount of antibiotic resistance that was observed in the baseline period.
A multivariate analysis did, however, find a few things associated with resistance prevalence. Women were about 58% less likely to develop a resistant bacterial strain than men. Patients who stayed less than 48 hours had a 38% decreased risk of developing a resistant strain. Good staff compliance with hand hygiene reduced the risk by 12%, and having one-on-one nursing reduced it by 53%.
The study was funded by the European Community’s Seventh Framework Programme. Dr. van Duijn had no financial declarations.
AMSTERDAM – Neither cycling through a regular schedule of antibiotics on a unit-wide basis, nor randomly mixing them on a patient-level basis reduced the prevalence of antibiotic resistance in eight European intensive care units, a randomized study has determined.
Lead investigator Dr. Pleun Joppe van Duijn of University Medical Center Utrecht (the Netherlands), said he and his colleagues did, however, discover a few common sense findings that seemed to positively affect antibiotic resistance, including compliance with hand hygiene, shorter lengths of stay, staff ratio, and unit occupancy rate. He reported the results of his research at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
Many ICUs in Europe have one preferred empirical treatment strategy which, Dr. van Duijn said, may create selective pressure for a single resistance type. “An alternative to this is a program of antibiotic rotation,” he noted. “By constantly changing the preferred first-line treatment, selective pressure is constantly changing, which may reduce selection of antibiotic resistance.”
Dr. van Duijn and his colleagues examined this idea in a randomized crossover trial that compared antibiotic cycling and mixing. The protocols employed three antibiotic classes: third- and fourth-generation cephalosporins, piperacillin/tazobactam, and carbapenems. The trial was conducted in eight ICUs in Belgium, Germany, France, Slovenia, and Portugal.
The sites were randomized to two 9-month interventions of cycling or mixing antibiotics, with a 1-month washout period between the two interventions. In cycling protocol, the preferred empiric antibiotic was changed every 6 weeks. In the mixing protocol, every consecutive patient received a different antibiotic. However, treating physicians were allowed to deviate from any protocol for patient safety or to optimize treatment.
The primary endpoint was the monthly prevalence of perineal and/or respiratory carriage of two classes of bacteria:
• Enterobacteriaceae species that were piperacillin/tazobactam–resistant or that showed extended spectrum beta-lactamase production.
• Pseudomonas aeruginosa and Acinetobacter species that were either piperacillin/tazobactam– or carbapenem-resistant.
In all, 8,945 patients were involved, with 4,238 exposed to cycling and 4,707 to mixing. Patients were a mean of 62 years old, with a mean 7-day length of stay. About 4.5% were already colonized with resistant bacteria upon admission. A quarter were on contact isolation; 2% were on both droplet and respiratory isolation.
The overall mortality rate was 11% and did not differ between the cycling and mixing groups (10.9% vs. 11.6%). Antibiotic resistance developed in 22.6% of the cycling group and 21.5% of the mixing group – not a significant difference. Neither protocol significantly reduced over time the amount of antibiotic resistance that was observed in the baseline period.
A multivariate analysis did, however, find a few things associated with resistance prevalence. Women were about 58% less likely to develop a resistant bacterial strain than men. Patients who stayed less than 48 hours had a 38% decreased risk of developing a resistant strain. Good staff compliance with hand hygiene reduced the risk by 12%, and having one-on-one nursing reduced it by 53%.
The study was funded by the European Community’s Seventh Framework Programme. Dr. van Duijn had no financial declarations.
AT ECCMID 2016
Key clinical point: Neither cycling nor mixing antibiotics reduced the prevalence of resistant bacteria in intensive care units.
Major finding: Antibiotic resistance developed in 22.6% of the cycling group and 21.5% of the mixing group – not a significant difference.
Data source: The randomized crossover trial comprised 8,945 patients in eight ICUs.
Disclosures: The study was funded by the European Community’s Seventh Framework Programme. Dr. van Duijn had no financial declarations.