User login
Increased risk of death even in lower-risk PPI users
Proton pump inhibitors (PPIs) are associated with a significantly higher risk of death than are H2 receptor antagonists, according to a 5-year longitudinal cohort study.
The study, published online in BMJ Open, found that increased risk of death was evident even in people without gastrointestinal conditions, and it increased with longer duration of use.
Yan Xie, PhD, of the VA Saint Louis Health Care System and coauthors, wrote that PPIs are linked to a range of serious adverse outcomes – such as acute interstitial nephritis, chronic kidney disease, incident dementia, and Clostridium difficile infection – each of which is associated with higher risk of mortality.
“Whether PPI use is associated with excess risk of death is not known and has not been examined in large epidemiological studies spanning a sufficiently long duration of follow-up.”
In this study, a cohort of 349,312 veterans initiated on acid-suppression therapy was followed for a mean duration of 5.71 years (BMJ Open 2017. July 4;7:e015735. doi: 10.1136/bmjopen-2016-015735).
Researchers saw a 25% higher risk of death in the 275,977 participants treated with PPIs, compared with that in those who were treated with H2 receptor antagonists (95% confidence interval, 1.23-1.28), after adjusting for factors such as estimated glomerular filtration rate, age, hospitalizations, and a range of comorbidities, including gastrointestinal disorders.
When PPI use was compared with no PPI use, there was a 15% increase in the risk of death (95% CI, 1.14-1.15). When compared with no known exposure to any acid suppression therapy, the increased risk of death was 23% (95% CI, 1.22-1.24).
In an attempt to look at the risk of death in a lower-risk cohort, the researchers analyzed a subgroup of participants who did not have the conditions for which PPIs are normally prescribed, such as gastroesophageal reflux disease, upper gastrointestinal tract bleeding, ulcer disease, Helicobacter pylori infection, and Barrett’s esophagus.
However, even in this lower-risk cohort, the study still showed a 24% increase in the risk of death with PPIs, compared with that in H2 receptor antagonists (95% CI, 1.21-1.27); a 19% increase with PPIs, compared with no PPIs; and a 22% increase with PPIs, compared with no acid suppression.
Duration of exposure to PPIs was also associated with increasing risk of death. Participants who had taken PPIs for fewer than 90 days in total only had a 5% increase in risk, while those taking them for 361-720 days had a 51% increased risk of death.
“Although our results should not deter prescription and use of PPIs where medically indicated, they may be used to encourage and promote pharmacovigilance and emphasize the need to exercise judicious use of PPIs and limit use and duration of therapy to instances where there is a clear medical indication and where benefit outweighs potential risk,” the authors wrote.
“Standardized guidelines for initiating PPI prescription may lead to reduced overuse [and] regular review of prescription and over-the-counter medications, and deprescription, where a medical indication for PPI treatment ceases to exist, may be a meritorious approach.”
Examining possible physiologic mechanisms to explain the increased risk of death, the authors noted that animal studies suggested PPIs may limit the liver’s capacity to regenerate.
PPIs are also associated with increased activity of the heme oxygenase-1 enzyme in gastric and endothelial cells and impairment of lysosomal acidification and proteostasis and may alter gene expression in the cellular retinol metabolism pathway and the complement and coagulation cascades pathway.
However, the clinical mediator of the heightened risk of death was likely one of the adverse events linked to PPI use, they said.
No conflicts of interest were declared.
Proton pump inhibitors (PPIs) are associated with a significantly higher risk of death than are H2 receptor antagonists, according to a 5-year longitudinal cohort study.
The study, published online in BMJ Open, found that increased risk of death was evident even in people without gastrointestinal conditions, and it increased with longer duration of use.
Yan Xie, PhD, of the VA Saint Louis Health Care System and coauthors, wrote that PPIs are linked to a range of serious adverse outcomes – such as acute interstitial nephritis, chronic kidney disease, incident dementia, and Clostridium difficile infection – each of which is associated with higher risk of mortality.
“Whether PPI use is associated with excess risk of death is not known and has not been examined in large epidemiological studies spanning a sufficiently long duration of follow-up.”
In this study, a cohort of 349,312 veterans initiated on acid-suppression therapy was followed for a mean duration of 5.71 years (BMJ Open 2017. July 4;7:e015735. doi: 10.1136/bmjopen-2016-015735).
Researchers saw a 25% higher risk of death in the 275,977 participants treated with PPIs, compared with that in those who were treated with H2 receptor antagonists (95% confidence interval, 1.23-1.28), after adjusting for factors such as estimated glomerular filtration rate, age, hospitalizations, and a range of comorbidities, including gastrointestinal disorders.
When PPI use was compared with no PPI use, there was a 15% increase in the risk of death (95% CI, 1.14-1.15). When compared with no known exposure to any acid suppression therapy, the increased risk of death was 23% (95% CI, 1.22-1.24).
In an attempt to look at the risk of death in a lower-risk cohort, the researchers analyzed a subgroup of participants who did not have the conditions for which PPIs are normally prescribed, such as gastroesophageal reflux disease, upper gastrointestinal tract bleeding, ulcer disease, Helicobacter pylori infection, and Barrett’s esophagus.
However, even in this lower-risk cohort, the study still showed a 24% increase in the risk of death with PPIs, compared with that in H2 receptor antagonists (95% CI, 1.21-1.27); a 19% increase with PPIs, compared with no PPIs; and a 22% increase with PPIs, compared with no acid suppression.
Duration of exposure to PPIs was also associated with increasing risk of death. Participants who had taken PPIs for fewer than 90 days in total only had a 5% increase in risk, while those taking them for 361-720 days had a 51% increased risk of death.
“Although our results should not deter prescription and use of PPIs where medically indicated, they may be used to encourage and promote pharmacovigilance and emphasize the need to exercise judicious use of PPIs and limit use and duration of therapy to instances where there is a clear medical indication and where benefit outweighs potential risk,” the authors wrote.
“Standardized guidelines for initiating PPI prescription may lead to reduced overuse [and] regular review of prescription and over-the-counter medications, and deprescription, where a medical indication for PPI treatment ceases to exist, may be a meritorious approach.”
Examining possible physiologic mechanisms to explain the increased risk of death, the authors noted that animal studies suggested PPIs may limit the liver’s capacity to regenerate.
PPIs are also associated with increased activity of the heme oxygenase-1 enzyme in gastric and endothelial cells and impairment of lysosomal acidification and proteostasis and may alter gene expression in the cellular retinol metabolism pathway and the complement and coagulation cascades pathway.
However, the clinical mediator of the heightened risk of death was likely one of the adverse events linked to PPI use, they said.
No conflicts of interest were declared.
Proton pump inhibitors (PPIs) are associated with a significantly higher risk of death than are H2 receptor antagonists, according to a 5-year longitudinal cohort study.
The study, published online in BMJ Open, found that increased risk of death was evident even in people without gastrointestinal conditions, and it increased with longer duration of use.
Yan Xie, PhD, of the VA Saint Louis Health Care System and coauthors, wrote that PPIs are linked to a range of serious adverse outcomes – such as acute interstitial nephritis, chronic kidney disease, incident dementia, and Clostridium difficile infection – each of which is associated with higher risk of mortality.
“Whether PPI use is associated with excess risk of death is not known and has not been examined in large epidemiological studies spanning a sufficiently long duration of follow-up.”
In this study, a cohort of 349,312 veterans initiated on acid-suppression therapy was followed for a mean duration of 5.71 years (BMJ Open 2017. July 4;7:e015735. doi: 10.1136/bmjopen-2016-015735).
Researchers saw a 25% higher risk of death in the 275,977 participants treated with PPIs, compared with that in those who were treated with H2 receptor antagonists (95% confidence interval, 1.23-1.28), after adjusting for factors such as estimated glomerular filtration rate, age, hospitalizations, and a range of comorbidities, including gastrointestinal disorders.
When PPI use was compared with no PPI use, there was a 15% increase in the risk of death (95% CI, 1.14-1.15). When compared with no known exposure to any acid suppression therapy, the increased risk of death was 23% (95% CI, 1.22-1.24).
In an attempt to look at the risk of death in a lower-risk cohort, the researchers analyzed a subgroup of participants who did not have the conditions for which PPIs are normally prescribed, such as gastroesophageal reflux disease, upper gastrointestinal tract bleeding, ulcer disease, Helicobacter pylori infection, and Barrett’s esophagus.
However, even in this lower-risk cohort, the study still showed a 24% increase in the risk of death with PPIs, compared with that in H2 receptor antagonists (95% CI, 1.21-1.27); a 19% increase with PPIs, compared with no PPIs; and a 22% increase with PPIs, compared with no acid suppression.
Duration of exposure to PPIs was also associated with increasing risk of death. Participants who had taken PPIs for fewer than 90 days in total only had a 5% increase in risk, while those taking them for 361-720 days had a 51% increased risk of death.
“Although our results should not deter prescription and use of PPIs where medically indicated, they may be used to encourage and promote pharmacovigilance and emphasize the need to exercise judicious use of PPIs and limit use and duration of therapy to instances where there is a clear medical indication and where benefit outweighs potential risk,” the authors wrote.
“Standardized guidelines for initiating PPI prescription may lead to reduced overuse [and] regular review of prescription and over-the-counter medications, and deprescription, where a medical indication for PPI treatment ceases to exist, may be a meritorious approach.”
Examining possible physiologic mechanisms to explain the increased risk of death, the authors noted that animal studies suggested PPIs may limit the liver’s capacity to regenerate.
PPIs are also associated with increased activity of the heme oxygenase-1 enzyme in gastric and endothelial cells and impairment of lysosomal acidification and proteostasis and may alter gene expression in the cellular retinol metabolism pathway and the complement and coagulation cascades pathway.
However, the clinical mediator of the heightened risk of death was likely one of the adverse events linked to PPI use, they said.
No conflicts of interest were declared.
FROM BMJ OPEN
Key clinical point: Proton pump inhibitors are associated with a significantly higher risk of death, even among people without the gastrointestinal conditions for which the drugs are normally prescribed.
Major finding: People taking PPIs have a 25% higher risk of death, compared with those taking H2 receptor antagonists.
Data source: A longitudinal cohort study in 349,312 veterans.
Disclosures: No conflicts of interest were declared.
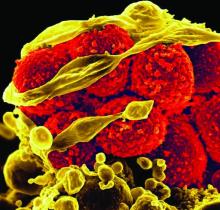
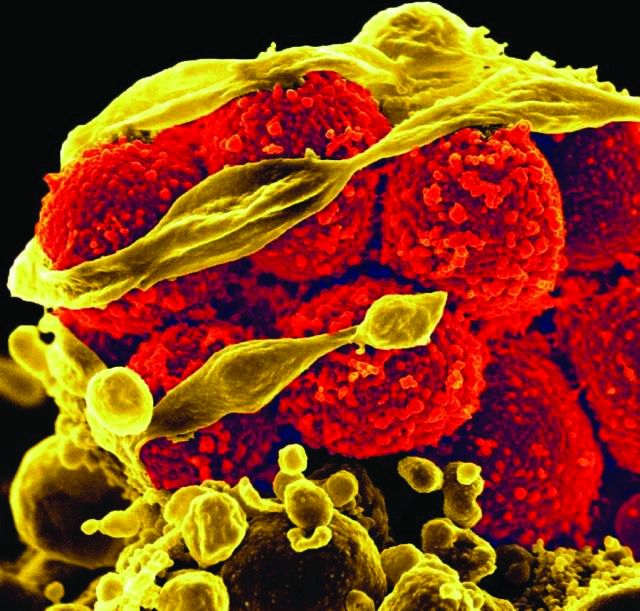
Ceftaroline shortens duration of MRSA bacteremia
NEW ORLEANS – Ceftaroline fosamil reduced the median duration of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia by 2 days in Veterans Administration patients, a retrospective study showed.
Investigators identified 219 patients with MRSA within the Veterans Affairs (VA) medical system nationwide from 2011 to 2015. All patients received at least 48 hours of ceftaroline fosamil (Teflaro) therapy to treat MRSA bacteremia. “We know it has good activity against MRSA in vitro. We use it in bacteremia, but we don’t have a lot of clinical data to support or refute its use,” said Nicholas S. Britt, PharmD, a PGY2 infectious diseases resident at Barnes-Jewish Hospital in St. Louis.
“Ceftaroline was primarily used as second-line or salvage therapy … which is basically what we expected, based on how it’s used in clinical practice,” Dr. Britt said.
Treatment failures
A total of 88 of the 219 (40%) patients experienced treatment failure. This rate “seems kind of high, but, if you look at some of the other MRSA agents for bacteremia (vancomycin, for example), it usually has a treatment failure rate around 60%,” Dr. Britt said. “The outcomes were not as poor as I would expect with [patients] using it for second- and third-line therapy.”
Hospital-acquired infection (odds ratio, 2.11; P = .013), ICU admission (OR, 3.95; P less than .001) and infective endocarditis (OR, 4.77; P = .002) were significantly associated with treatment failure in a univariate analysis. “Admissions to the ICU and endocarditis were the big ones, factors you would associate with failure for most antibiotics,” Dr. Britt said. In a multivariate analysis, only ICU admission remained significantly associated with treatment failure (adjusted OR, 2.24; P = .028).
The investigators also looked at treatment failure with ceftaroline monotherapy, compared with its use in combination. There is in vitro data showing synergy when you add ceftaroline to daptomycin, vancomycin, or some of these other agents,” Dr. Britt said. However, he added, “We didn’t find any significant difference in outcomes when you added another agent.” Treatment failure with monotherapy was 35%, versus 46%, with combination treatment (P = .107).
“This could be because the sicker patients are the ones getting combination therapy.”
No observed differences by dosing
Dr. Britt and his colleagues also looked for any differences by dosing interval, “which hasn’t been evaluated extensively.”
The Food and Drug Administration labeled it for use every 12 hours, but treatment of MRSA bacteremia is an off-label use, Dr. Britt explained. Dosing every 8 hours instead improves the achievement of pharmacokinetic and pharmacodynamic parameters in in vitro studies. “Clinically, we’re almost always using it q8. They’re sick patients, so you don’t want to under-dose them. And ceftaroline is pretty well tolerated overall.”
“But, we didn’t really see any difference between the q8 and the q12” in terms of treatment failure. The rates were 36% and 42%, respectively, and not significantly different (P = .440). “Granted, patients who are sicker are probably going to get treated more aggressively,” Dr. Britt added.
The current research only focused on outcomes associated with ceftaroline. Going forward, Dr. Britt said, “We’re hoping to use this data to compare ceftaroline to other agents as well, probably as second-line therapy, since that’s how it’s used most often.”
Dr. Britt had no relevant financial disclosures.
NEW ORLEANS – Ceftaroline fosamil reduced the median duration of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia by 2 days in Veterans Administration patients, a retrospective study showed.
Investigators identified 219 patients with MRSA within the Veterans Affairs (VA) medical system nationwide from 2011 to 2015. All patients received at least 48 hours of ceftaroline fosamil (Teflaro) therapy to treat MRSA bacteremia. “We know it has good activity against MRSA in vitro. We use it in bacteremia, but we don’t have a lot of clinical data to support or refute its use,” said Nicholas S. Britt, PharmD, a PGY2 infectious diseases resident at Barnes-Jewish Hospital in St. Louis.
“Ceftaroline was primarily used as second-line or salvage therapy … which is basically what we expected, based on how it’s used in clinical practice,” Dr. Britt said.
Treatment failures
A total of 88 of the 219 (40%) patients experienced treatment failure. This rate “seems kind of high, but, if you look at some of the other MRSA agents for bacteremia (vancomycin, for example), it usually has a treatment failure rate around 60%,” Dr. Britt said. “The outcomes were not as poor as I would expect with [patients] using it for second- and third-line therapy.”
Hospital-acquired infection (odds ratio, 2.11; P = .013), ICU admission (OR, 3.95; P less than .001) and infective endocarditis (OR, 4.77; P = .002) were significantly associated with treatment failure in a univariate analysis. “Admissions to the ICU and endocarditis were the big ones, factors you would associate with failure for most antibiotics,” Dr. Britt said. In a multivariate analysis, only ICU admission remained significantly associated with treatment failure (adjusted OR, 2.24; P = .028).
The investigators also looked at treatment failure with ceftaroline monotherapy, compared with its use in combination. There is in vitro data showing synergy when you add ceftaroline to daptomycin, vancomycin, or some of these other agents,” Dr. Britt said. However, he added, “We didn’t find any significant difference in outcomes when you added another agent.” Treatment failure with monotherapy was 35%, versus 46%, with combination treatment (P = .107).
“This could be because the sicker patients are the ones getting combination therapy.”
No observed differences by dosing
Dr. Britt and his colleagues also looked for any differences by dosing interval, “which hasn’t been evaluated extensively.”
The Food and Drug Administration labeled it for use every 12 hours, but treatment of MRSA bacteremia is an off-label use, Dr. Britt explained. Dosing every 8 hours instead improves the achievement of pharmacokinetic and pharmacodynamic parameters in in vitro studies. “Clinically, we’re almost always using it q8. They’re sick patients, so you don’t want to under-dose them. And ceftaroline is pretty well tolerated overall.”
“But, we didn’t really see any difference between the q8 and the q12” in terms of treatment failure. The rates were 36% and 42%, respectively, and not significantly different (P = .440). “Granted, patients who are sicker are probably going to get treated more aggressively,” Dr. Britt added.
The current research only focused on outcomes associated with ceftaroline. Going forward, Dr. Britt said, “We’re hoping to use this data to compare ceftaroline to other agents as well, probably as second-line therapy, since that’s how it’s used most often.”
Dr. Britt had no relevant financial disclosures.
NEW ORLEANS – Ceftaroline fosamil reduced the median duration of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia by 2 days in Veterans Administration patients, a retrospective study showed.
Investigators identified 219 patients with MRSA within the Veterans Affairs (VA) medical system nationwide from 2011 to 2015. All patients received at least 48 hours of ceftaroline fosamil (Teflaro) therapy to treat MRSA bacteremia. “We know it has good activity against MRSA in vitro. We use it in bacteremia, but we don’t have a lot of clinical data to support or refute its use,” said Nicholas S. Britt, PharmD, a PGY2 infectious diseases resident at Barnes-Jewish Hospital in St. Louis.
“Ceftaroline was primarily used as second-line or salvage therapy … which is basically what we expected, based on how it’s used in clinical practice,” Dr. Britt said.
Treatment failures
A total of 88 of the 219 (40%) patients experienced treatment failure. This rate “seems kind of high, but, if you look at some of the other MRSA agents for bacteremia (vancomycin, for example), it usually has a treatment failure rate around 60%,” Dr. Britt said. “The outcomes were not as poor as I would expect with [patients] using it for second- and third-line therapy.”
Hospital-acquired infection (odds ratio, 2.11; P = .013), ICU admission (OR, 3.95; P less than .001) and infective endocarditis (OR, 4.77; P = .002) were significantly associated with treatment failure in a univariate analysis. “Admissions to the ICU and endocarditis were the big ones, factors you would associate with failure for most antibiotics,” Dr. Britt said. In a multivariate analysis, only ICU admission remained significantly associated with treatment failure (adjusted OR, 2.24; P = .028).
The investigators also looked at treatment failure with ceftaroline monotherapy, compared with its use in combination. There is in vitro data showing synergy when you add ceftaroline to daptomycin, vancomycin, or some of these other agents,” Dr. Britt said. However, he added, “We didn’t find any significant difference in outcomes when you added another agent.” Treatment failure with monotherapy was 35%, versus 46%, with combination treatment (P = .107).
“This could be because the sicker patients are the ones getting combination therapy.”
No observed differences by dosing
Dr. Britt and his colleagues also looked for any differences by dosing interval, “which hasn’t been evaluated extensively.”
The Food and Drug Administration labeled it for use every 12 hours, but treatment of MRSA bacteremia is an off-label use, Dr. Britt explained. Dosing every 8 hours instead improves the achievement of pharmacokinetic and pharmacodynamic parameters in in vitro studies. “Clinically, we’re almost always using it q8. They’re sick patients, so you don’t want to under-dose them. And ceftaroline is pretty well tolerated overall.”
“But, we didn’t really see any difference between the q8 and the q12” in terms of treatment failure. The rates were 36% and 42%, respectively, and not significantly different (P = .440). “Granted, patients who are sicker are probably going to get treated more aggressively,” Dr. Britt added.
The current research only focused on outcomes associated with ceftaroline. Going forward, Dr. Britt said, “We’re hoping to use this data to compare ceftaroline to other agents as well, probably as second-line therapy, since that’s how it’s used most often.”
Dr. Britt had no relevant financial disclosures.
AT ASM MICROBE 2017
Key clinical point:
Major finding: Median duration of MRSA bacteremia dropped from 2.79 days before to 1.18 days after initiation of ceftaroline (P less than .001).
Data source: A retrospective study of 219 hospitalized VA patients initiating ceftaroline for MRSA bacteremia.
Disclosures: Dr. Britt had no relevant financial disclosures.
Carbapenem-resistant sepsis risk factors vary significantly
NEW ORLEANS – Investigators discovered significant differences in risk factors when comparing 603 people hospitalized with carbapenem-resistant Gram-negative sepsis with either Enterobacteriaceae-caused or non-Enterobacteriaceae–caused infection.
“We know some of the virulence factors and the resistance mechanisms can differ between those two groups. We really wanted to see if that would influence outcomes,” said Nicholas S. Britt, PharmD, a PGY2 infectious disease resident at Barnes-Jewish Hospital in St. Louis. Mortality rates, however, did not differ significantly.
“Patients who had Enterobacteriaceae infections were more likely to have urinary tract infections, to be older patients, and to have higher APACHE (Acute Physiologic Assessment and Chronic Health Evaluation) II scores,” Dr. Britt said at the annual meeting of the American Society for Microbiology. These differences all were statistically significant, compared with those of the CRNE group (P less than .05).
In contrast, the non-Enterobacteriaceae patients tended to have more respiratory infections and more frequent central venous catheter use. This group also was more likely to have a history of carbapenem use and more frequent antimicrobial exposures overall and to present after solid organ transplantation. “The cystic fibrosis patients were more likely to get non-Enterobacteriaceae infections as well,” Dr. Britt added. These differences also were statistically significant (all P less than .05).
“I think the biggest takeaway from this study, honestly, is the number of patients infected with CRE, versus CRNE,” Dr. Britt said. “We know CRE are a serious public health threat, one of the biggest threats out there, but, if you look at the burden on carbapenem-resistant disease, it’s primarily the non-Enterobacteriaceae.”
In fact, more than three-quarters of the patient studied (78%) had CRNE infections, and Pseudomonas was a major driver, he added. “Carbapenem resistance in this group of patients is something we should be focusing on – not only the CRE – because we’re seeing more of the non-CRE clinically.”
Patient age, presence of bloodstream infection, and use of mechanical ventilation, vasopressors, and immunosuppression was associated with hospital mortality in the study. After adjusting for potential confounders, however, CRNE infection was not associated with increased hospital mortality, compared with CRE cases (adjusted odds ratio, 0.97; P = .917).
“Our mortality rate was 16%, which is comparable to [that of] other studies,” Dr. Britt said. “There doesn’t seem to be any difference in this outcome between the two groups.” Mortality was 16.4% in the CRE cohort, versus 16.5% in the CRNE cohort (P = 0.965).
NEW ORLEANS – Investigators discovered significant differences in risk factors when comparing 603 people hospitalized with carbapenem-resistant Gram-negative sepsis with either Enterobacteriaceae-caused or non-Enterobacteriaceae–caused infection.
“We know some of the virulence factors and the resistance mechanisms can differ between those two groups. We really wanted to see if that would influence outcomes,” said Nicholas S. Britt, PharmD, a PGY2 infectious disease resident at Barnes-Jewish Hospital in St. Louis. Mortality rates, however, did not differ significantly.
“Patients who had Enterobacteriaceae infections were more likely to have urinary tract infections, to be older patients, and to have higher APACHE (Acute Physiologic Assessment and Chronic Health Evaluation) II scores,” Dr. Britt said at the annual meeting of the American Society for Microbiology. These differences all were statistically significant, compared with those of the CRNE group (P less than .05).
In contrast, the non-Enterobacteriaceae patients tended to have more respiratory infections and more frequent central venous catheter use. This group also was more likely to have a history of carbapenem use and more frequent antimicrobial exposures overall and to present after solid organ transplantation. “The cystic fibrosis patients were more likely to get non-Enterobacteriaceae infections as well,” Dr. Britt added. These differences also were statistically significant (all P less than .05).
“I think the biggest takeaway from this study, honestly, is the number of patients infected with CRE, versus CRNE,” Dr. Britt said. “We know CRE are a serious public health threat, one of the biggest threats out there, but, if you look at the burden on carbapenem-resistant disease, it’s primarily the non-Enterobacteriaceae.”
In fact, more than three-quarters of the patient studied (78%) had CRNE infections, and Pseudomonas was a major driver, he added. “Carbapenem resistance in this group of patients is something we should be focusing on – not only the CRE – because we’re seeing more of the non-CRE clinically.”
Patient age, presence of bloodstream infection, and use of mechanical ventilation, vasopressors, and immunosuppression was associated with hospital mortality in the study. After adjusting for potential confounders, however, CRNE infection was not associated with increased hospital mortality, compared with CRE cases (adjusted odds ratio, 0.97; P = .917).
“Our mortality rate was 16%, which is comparable to [that of] other studies,” Dr. Britt said. “There doesn’t seem to be any difference in this outcome between the two groups.” Mortality was 16.4% in the CRE cohort, versus 16.5% in the CRNE cohort (P = 0.965).
NEW ORLEANS – Investigators discovered significant differences in risk factors when comparing 603 people hospitalized with carbapenem-resistant Gram-negative sepsis with either Enterobacteriaceae-caused or non-Enterobacteriaceae–caused infection.
“We know some of the virulence factors and the resistance mechanisms can differ between those two groups. We really wanted to see if that would influence outcomes,” said Nicholas S. Britt, PharmD, a PGY2 infectious disease resident at Barnes-Jewish Hospital in St. Louis. Mortality rates, however, did not differ significantly.
“Patients who had Enterobacteriaceae infections were more likely to have urinary tract infections, to be older patients, and to have higher APACHE (Acute Physiologic Assessment and Chronic Health Evaluation) II scores,” Dr. Britt said at the annual meeting of the American Society for Microbiology. These differences all were statistically significant, compared with those of the CRNE group (P less than .05).
In contrast, the non-Enterobacteriaceae patients tended to have more respiratory infections and more frequent central venous catheter use. This group also was more likely to have a history of carbapenem use and more frequent antimicrobial exposures overall and to present after solid organ transplantation. “The cystic fibrosis patients were more likely to get non-Enterobacteriaceae infections as well,” Dr. Britt added. These differences also were statistically significant (all P less than .05).
“I think the biggest takeaway from this study, honestly, is the number of patients infected with CRE, versus CRNE,” Dr. Britt said. “We know CRE are a serious public health threat, one of the biggest threats out there, but, if you look at the burden on carbapenem-resistant disease, it’s primarily the non-Enterobacteriaceae.”
In fact, more than three-quarters of the patient studied (78%) had CRNE infections, and Pseudomonas was a major driver, he added. “Carbapenem resistance in this group of patients is something we should be focusing on – not only the CRE – because we’re seeing more of the non-CRE clinically.”
Patient age, presence of bloodstream infection, and use of mechanical ventilation, vasopressors, and immunosuppression was associated with hospital mortality in the study. After adjusting for potential confounders, however, CRNE infection was not associated with increased hospital mortality, compared with CRE cases (adjusted odds ratio, 0.97; P = .917).
“Our mortality rate was 16%, which is comparable to [that of] other studies,” Dr. Britt said. “There doesn’t seem to be any difference in this outcome between the two groups.” Mortality was 16.4% in the CRE cohort, versus 16.5% in the CRNE cohort (P = 0.965).
AT ASM MICROBE 2017
Key clinical point:
Major finding: Hospital mortality was 16% overall and did not differ significantly between Enterobacteriaceae and non-Enterobacteriaceae infections (16.5% vs. 16.4%; P = 0.965).
Data source: A retrospective cohort study of 603 patients with Gram-negative sepsis at a tertiary academic medical center from 2012 to 2016.
Disclosures: Dr. Britt did not have any relevant financial disclosures.
New drug choices emerging to battle antibiotic resistance
SAN FRANCISCO – When the Infectious Diseases Society of America released the “Bad Bugs, No Drugs” report in 2004, its authors warned that effective antibiotics may not be available to treat seriously ill patients in the near future.
It also proposed legislative, regulatory, and funding solutions with a goal of developing and licensing 10 new antibiotics by the year 2020.
One such advancement was the Generating Antibiotics Incentives Now Act, which was signed into law in 2012 and created a designation for new antibiotics that are used to treat serious and/or life-threatening diseases due to certain pathogens. It also extends the patent life of these antibiotics and allows for fast-track Food and Drug Administration approval.
According to Dr. Erlich, chief of staff and medical director of infection control and antibiotic stewardship at Mills Peninsula Medical Center, Burlingame, Calif., increasingly common antibiotic-resistant pathogens besides MRSA and VRE include penicillin-resistant Streptococcus pneumoniae, extended-spectrum beta-lactamase–producing gram-negative rods, carbapenem-resistant Enterobacteriaceae (CRE), multidrug-resistant Mycobacterium tuberculosis, Salmonella enterica serotype Typhimurium DT 104, and drug-resistant Candida species.
Since 2010, several new antibiotics have been introduced to the market, including three second-generation lipoglycopeptide antibiotics with gram-positive coverage that are approved primarily for skin and soft tissue infections: dalbavancin (Dalvance), telavancin (Vibativ), and oritavancin (Orbactiv).
Compared with vancomycin, these new agents have more convenient dosing and a longer half life, “but they’re also more expensive,” said Dr. Erlich. Dalbavancin can be dosed once a week intravenously, telavancin can be dosed once daily intravenously, and oritavancin requires just one dose.
Another new agent is tedizolid phosphate (Sivextro), a second-generation oxazolidinone that is in the same drug class as linezolid (Zyvox). Tedizolid phosphate has gram-positive coverage including MRSA, but it is not approved for VRE. “It’s FDA approved for skin and soft-tissue infections (SSTI) but can be used for other locations as well,” Dr. Erlich said. “It features once-daily dosing IV or PO.”
Ceftaroline fosamil (Teflaro), ceftolozane/tazobactam (Zerbaxa), and ceftazidime/avibactam (Avycaz) are broad-spectrum cephalosporins with or without beta-lactamase inhibitors resulting in extended gram-negative coverage. FDA-approved indications include complicated urinary tract infections, complicated abdominal infections, SSTI, and pneumonia.
The primary advantage of these drugs, compared with other agents, is for multidrug-resistant gram-negative bacteria such as extended-spectrum beta-lactamase producers and CRE. “We’re not using a lot of these drugs in clinical practice, but they are available for patients with multidrug-resistant gram-negative rods who have no other options,” Dr. Erlich said.
Practical ways that clinicians can prevent antibiotic resistance include prescribing antibiotics only when necessary. “Be aware of local resistance patterns, avoid antibiotics for probable viral infections, use narrow-spectrum choices when possible, use shorter durations when appropriate, and consult published guidelines for optimal empiric antibiotic therapy,” Dr. Erlich advised.
In addition, “advocate infection control measures to keep patients from developing infections, including proper wound care, hand washing, respiratory etiquette, vaccinations, and social isolation for symptomatic individuals,” he noted.
Dr. Erlich reported having no relevant financial disclosures.
SAN FRANCISCO – When the Infectious Diseases Society of America released the “Bad Bugs, No Drugs” report in 2004, its authors warned that effective antibiotics may not be available to treat seriously ill patients in the near future.
It also proposed legislative, regulatory, and funding solutions with a goal of developing and licensing 10 new antibiotics by the year 2020.
One such advancement was the Generating Antibiotics Incentives Now Act, which was signed into law in 2012 and created a designation for new antibiotics that are used to treat serious and/or life-threatening diseases due to certain pathogens. It also extends the patent life of these antibiotics and allows for fast-track Food and Drug Administration approval.
According to Dr. Erlich, chief of staff and medical director of infection control and antibiotic stewardship at Mills Peninsula Medical Center, Burlingame, Calif., increasingly common antibiotic-resistant pathogens besides MRSA and VRE include penicillin-resistant Streptococcus pneumoniae, extended-spectrum beta-lactamase–producing gram-negative rods, carbapenem-resistant Enterobacteriaceae (CRE), multidrug-resistant Mycobacterium tuberculosis, Salmonella enterica serotype Typhimurium DT 104, and drug-resistant Candida species.
Since 2010, several new antibiotics have been introduced to the market, including three second-generation lipoglycopeptide antibiotics with gram-positive coverage that are approved primarily for skin and soft tissue infections: dalbavancin (Dalvance), telavancin (Vibativ), and oritavancin (Orbactiv).
Compared with vancomycin, these new agents have more convenient dosing and a longer half life, “but they’re also more expensive,” said Dr. Erlich. Dalbavancin can be dosed once a week intravenously, telavancin can be dosed once daily intravenously, and oritavancin requires just one dose.
Another new agent is tedizolid phosphate (Sivextro), a second-generation oxazolidinone that is in the same drug class as linezolid (Zyvox). Tedizolid phosphate has gram-positive coverage including MRSA, but it is not approved for VRE. “It’s FDA approved for skin and soft-tissue infections (SSTI) but can be used for other locations as well,” Dr. Erlich said. “It features once-daily dosing IV or PO.”
Ceftaroline fosamil (Teflaro), ceftolozane/tazobactam (Zerbaxa), and ceftazidime/avibactam (Avycaz) are broad-spectrum cephalosporins with or without beta-lactamase inhibitors resulting in extended gram-negative coverage. FDA-approved indications include complicated urinary tract infections, complicated abdominal infections, SSTI, and pneumonia.
The primary advantage of these drugs, compared with other agents, is for multidrug-resistant gram-negative bacteria such as extended-spectrum beta-lactamase producers and CRE. “We’re not using a lot of these drugs in clinical practice, but they are available for patients with multidrug-resistant gram-negative rods who have no other options,” Dr. Erlich said.
Practical ways that clinicians can prevent antibiotic resistance include prescribing antibiotics only when necessary. “Be aware of local resistance patterns, avoid antibiotics for probable viral infections, use narrow-spectrum choices when possible, use shorter durations when appropriate, and consult published guidelines for optimal empiric antibiotic therapy,” Dr. Erlich advised.
In addition, “advocate infection control measures to keep patients from developing infections, including proper wound care, hand washing, respiratory etiquette, vaccinations, and social isolation for symptomatic individuals,” he noted.
Dr. Erlich reported having no relevant financial disclosures.
SAN FRANCISCO – When the Infectious Diseases Society of America released the “Bad Bugs, No Drugs” report in 2004, its authors warned that effective antibiotics may not be available to treat seriously ill patients in the near future.
It also proposed legislative, regulatory, and funding solutions with a goal of developing and licensing 10 new antibiotics by the year 2020.
One such advancement was the Generating Antibiotics Incentives Now Act, which was signed into law in 2012 and created a designation for new antibiotics that are used to treat serious and/or life-threatening diseases due to certain pathogens. It also extends the patent life of these antibiotics and allows for fast-track Food and Drug Administration approval.
According to Dr. Erlich, chief of staff and medical director of infection control and antibiotic stewardship at Mills Peninsula Medical Center, Burlingame, Calif., increasingly common antibiotic-resistant pathogens besides MRSA and VRE include penicillin-resistant Streptococcus pneumoniae, extended-spectrum beta-lactamase–producing gram-negative rods, carbapenem-resistant Enterobacteriaceae (CRE), multidrug-resistant Mycobacterium tuberculosis, Salmonella enterica serotype Typhimurium DT 104, and drug-resistant Candida species.
Since 2010, several new antibiotics have been introduced to the market, including three second-generation lipoglycopeptide antibiotics with gram-positive coverage that are approved primarily for skin and soft tissue infections: dalbavancin (Dalvance), telavancin (Vibativ), and oritavancin (Orbactiv).
Compared with vancomycin, these new agents have more convenient dosing and a longer half life, “but they’re also more expensive,” said Dr. Erlich. Dalbavancin can be dosed once a week intravenously, telavancin can be dosed once daily intravenously, and oritavancin requires just one dose.
Another new agent is tedizolid phosphate (Sivextro), a second-generation oxazolidinone that is in the same drug class as linezolid (Zyvox). Tedizolid phosphate has gram-positive coverage including MRSA, but it is not approved for VRE. “It’s FDA approved for skin and soft-tissue infections (SSTI) but can be used for other locations as well,” Dr. Erlich said. “It features once-daily dosing IV or PO.”
Ceftaroline fosamil (Teflaro), ceftolozane/tazobactam (Zerbaxa), and ceftazidime/avibactam (Avycaz) are broad-spectrum cephalosporins with or without beta-lactamase inhibitors resulting in extended gram-negative coverage. FDA-approved indications include complicated urinary tract infections, complicated abdominal infections, SSTI, and pneumonia.
The primary advantage of these drugs, compared with other agents, is for multidrug-resistant gram-negative bacteria such as extended-spectrum beta-lactamase producers and CRE. “We’re not using a lot of these drugs in clinical practice, but they are available for patients with multidrug-resistant gram-negative rods who have no other options,” Dr. Erlich said.
Practical ways that clinicians can prevent antibiotic resistance include prescribing antibiotics only when necessary. “Be aware of local resistance patterns, avoid antibiotics for probable viral infections, use narrow-spectrum choices when possible, use shorter durations when appropriate, and consult published guidelines for optimal empiric antibiotic therapy,” Dr. Erlich advised.
In addition, “advocate infection control measures to keep patients from developing infections, including proper wound care, hand washing, respiratory etiquette, vaccinations, and social isolation for symptomatic individuals,” he noted.
Dr. Erlich reported having no relevant financial disclosures.
AT THE ANNUAL ADVANCES IN INTERNAL MEDICINE
Hospital antibiograms may not apply to emergency department patients
NEW ORLEANS – Patients seen in the emergency department present with a wider range of risk for resistant infections than do hospitalized patients overall, and as a result, hospital-wide antibiograms that dictate empiric therapy may not translate well to the ED setting, a study showed.
Instead, investigators suggested that clinicians choose empiric antimicrobial therapy in the emergency department based on factors associated with differences in susceptibility.
The study researchers compared common antibiotics to treat Escherichia coli between adults treated at their institution overall versus the emergency department, and by sex, patient age, and whether people came to the ED from home versus a long-term care setting. They found some significant differences that could guide empiric treatment in the ED setting.
“Our ED pharmacist observed a lot of broad-spectrum antibiotic prescribing for UTIs,” lead investigator Sarah Jorgensen, PharmD, said at the annual meeting of the American Society for Microbiology. “Also, we’ve had a culture follow-up program in place for the last 5 years, and they had to intervene on a lot of postdischarge antibiotic mismatches.”
E. coli was the most common urinary pathogen detected in this study of 500 randomly selected ED patients with ICD-9/ICD-10 diagnostic codes for urinary tract infection. Investigators found E. coli in 64% of the 226 culture-positive patients presenting to the ED at Huntington Hospital in Pasadena, Calif., between July 2015 and June 2016.
“What was surprising for us, because our enrollment was based on ICD codes for a UTI, is that only about 50% had a positive urine culture,” said Dr. Jorgensen, a pharmacy resident at the University of Southern California in Los Angeles. “Urinalysis was positive in about 99% of the population.”
Dr. Jorgensen and her colleagues found overall low susceptibilities of 71% for ciprofloxacin, 66% for trimethoprim/sulfamethoxazole, and 67% for cefazolin susceptibilities in the ED. They also found that 8% of isolates were positive for extended-spectrum beta-lactamase isolates, as were 1% of E. coli isolates.
The 67% cefazolin susceptibility was significantly lower in the ED, compared with the 86% susceptibility in the institutional antibiogram (P less than .001).
The investigators found E. coli susceptibility to ciprofloxacin was lower in men, at 55%, compared with 74% among women, but the difference was not statistically significant (P = .14). A similar pattern emerged with cefazolin – 55% susceptibility among men and 69% among women (P = .26). In contrast, trimethoprim/sulfamethoxazole susceptibility trended higher in men, at 73%, vs. 64% among women in the ED (P = .63).
When they divided patients by age 50 years and younger versus those older than 50, the investigators found ampicillin susceptibilities were lower in the younger group, at 30%, compared with 51% among those in the older cohort (P = .03). Similarly, gentamicin susceptibilities were 80% in the younger group, compared with 92% in the older group (P = .04).
Ciprofloxacin susceptibility was significantly lower among people coming to the ED from a long-term care facility than among those coming from home – 35% vs. 77% (P less than .001). Differences in ciprofloxacin susceptibility between admitted and discharged patients was less striking – 63% vs. 78% (P = .04).
Nitrofurantoin was the only oral agent with susceptibility greater than 80% in all patient groups, with susceptibility ranging from 88% to 100%.
Because it typically takes 2-3 days to get the susceptibility results back at Huntington Hospital, many patients are discharged on empiric therapy, noted Mira Zurayk, PharmD, a resident at Huntington Hospital. That can present multiple challenges, particularly with homeless patients who are difficult to find and provide follow-up for, Dr. Jorgensen added.
Based partly on the study findings, the investigators developed a clinical algorithm specifically to address UTI antimicrobial prescriptions in the ED. The algorithm incorporates different recommendations for different groups of patients because of their different resistance trends.
“I think that is a good way to tailor empiric therapy when you don’t have culture results up front,” Dr. Jorgensen said. “We just implemented the algorithm, and I’m now analyzing the outcomes.”
Having more data on outcomes will help the clinicians target lowering the rate of “drug-bug mismatches,” as well as UTI-related revisits to the ED. In addition, the work could help expand the antibiotic stewardship program in the hospital to the ED for the first time, Dr. Jorgensen said.
Dr. Jorgensen and Dr. Zurayk had no relevant financial disclosures. One of the study coauthors, Annie Wong-Beringer, PharmD, receives grant funding from Merck.
NEW ORLEANS – Patients seen in the emergency department present with a wider range of risk for resistant infections than do hospitalized patients overall, and as a result, hospital-wide antibiograms that dictate empiric therapy may not translate well to the ED setting, a study showed.
Instead, investigators suggested that clinicians choose empiric antimicrobial therapy in the emergency department based on factors associated with differences in susceptibility.
The study researchers compared common antibiotics to treat Escherichia coli between adults treated at their institution overall versus the emergency department, and by sex, patient age, and whether people came to the ED from home versus a long-term care setting. They found some significant differences that could guide empiric treatment in the ED setting.
“Our ED pharmacist observed a lot of broad-spectrum antibiotic prescribing for UTIs,” lead investigator Sarah Jorgensen, PharmD, said at the annual meeting of the American Society for Microbiology. “Also, we’ve had a culture follow-up program in place for the last 5 years, and they had to intervene on a lot of postdischarge antibiotic mismatches.”
E. coli was the most common urinary pathogen detected in this study of 500 randomly selected ED patients with ICD-9/ICD-10 diagnostic codes for urinary tract infection. Investigators found E. coli in 64% of the 226 culture-positive patients presenting to the ED at Huntington Hospital in Pasadena, Calif., between July 2015 and June 2016.
“What was surprising for us, because our enrollment was based on ICD codes for a UTI, is that only about 50% had a positive urine culture,” said Dr. Jorgensen, a pharmacy resident at the University of Southern California in Los Angeles. “Urinalysis was positive in about 99% of the population.”
Dr. Jorgensen and her colleagues found overall low susceptibilities of 71% for ciprofloxacin, 66% for trimethoprim/sulfamethoxazole, and 67% for cefazolin susceptibilities in the ED. They also found that 8% of isolates were positive for extended-spectrum beta-lactamase isolates, as were 1% of E. coli isolates.
The 67% cefazolin susceptibility was significantly lower in the ED, compared with the 86% susceptibility in the institutional antibiogram (P less than .001).
The investigators found E. coli susceptibility to ciprofloxacin was lower in men, at 55%, compared with 74% among women, but the difference was not statistically significant (P = .14). A similar pattern emerged with cefazolin – 55% susceptibility among men and 69% among women (P = .26). In contrast, trimethoprim/sulfamethoxazole susceptibility trended higher in men, at 73%, vs. 64% among women in the ED (P = .63).
When they divided patients by age 50 years and younger versus those older than 50, the investigators found ampicillin susceptibilities were lower in the younger group, at 30%, compared with 51% among those in the older cohort (P = .03). Similarly, gentamicin susceptibilities were 80% in the younger group, compared with 92% in the older group (P = .04).
Ciprofloxacin susceptibility was significantly lower among people coming to the ED from a long-term care facility than among those coming from home – 35% vs. 77% (P less than .001). Differences in ciprofloxacin susceptibility between admitted and discharged patients was less striking – 63% vs. 78% (P = .04).
Nitrofurantoin was the only oral agent with susceptibility greater than 80% in all patient groups, with susceptibility ranging from 88% to 100%.
Because it typically takes 2-3 days to get the susceptibility results back at Huntington Hospital, many patients are discharged on empiric therapy, noted Mira Zurayk, PharmD, a resident at Huntington Hospital. That can present multiple challenges, particularly with homeless patients who are difficult to find and provide follow-up for, Dr. Jorgensen added.
Based partly on the study findings, the investigators developed a clinical algorithm specifically to address UTI antimicrobial prescriptions in the ED. The algorithm incorporates different recommendations for different groups of patients because of their different resistance trends.
“I think that is a good way to tailor empiric therapy when you don’t have culture results up front,” Dr. Jorgensen said. “We just implemented the algorithm, and I’m now analyzing the outcomes.”
Having more data on outcomes will help the clinicians target lowering the rate of “drug-bug mismatches,” as well as UTI-related revisits to the ED. In addition, the work could help expand the antibiotic stewardship program in the hospital to the ED for the first time, Dr. Jorgensen said.
Dr. Jorgensen and Dr. Zurayk had no relevant financial disclosures. One of the study coauthors, Annie Wong-Beringer, PharmD, receives grant funding from Merck.
NEW ORLEANS – Patients seen in the emergency department present with a wider range of risk for resistant infections than do hospitalized patients overall, and as a result, hospital-wide antibiograms that dictate empiric therapy may not translate well to the ED setting, a study showed.
Instead, investigators suggested that clinicians choose empiric antimicrobial therapy in the emergency department based on factors associated with differences in susceptibility.
The study researchers compared common antibiotics to treat Escherichia coli between adults treated at their institution overall versus the emergency department, and by sex, patient age, and whether people came to the ED from home versus a long-term care setting. They found some significant differences that could guide empiric treatment in the ED setting.
“Our ED pharmacist observed a lot of broad-spectrum antibiotic prescribing for UTIs,” lead investigator Sarah Jorgensen, PharmD, said at the annual meeting of the American Society for Microbiology. “Also, we’ve had a culture follow-up program in place for the last 5 years, and they had to intervene on a lot of postdischarge antibiotic mismatches.”
E. coli was the most common urinary pathogen detected in this study of 500 randomly selected ED patients with ICD-9/ICD-10 diagnostic codes for urinary tract infection. Investigators found E. coli in 64% of the 226 culture-positive patients presenting to the ED at Huntington Hospital in Pasadena, Calif., between July 2015 and June 2016.
“What was surprising for us, because our enrollment was based on ICD codes for a UTI, is that only about 50% had a positive urine culture,” said Dr. Jorgensen, a pharmacy resident at the University of Southern California in Los Angeles. “Urinalysis was positive in about 99% of the population.”
Dr. Jorgensen and her colleagues found overall low susceptibilities of 71% for ciprofloxacin, 66% for trimethoprim/sulfamethoxazole, and 67% for cefazolin susceptibilities in the ED. They also found that 8% of isolates were positive for extended-spectrum beta-lactamase isolates, as were 1% of E. coli isolates.
The 67% cefazolin susceptibility was significantly lower in the ED, compared with the 86% susceptibility in the institutional antibiogram (P less than .001).
The investigators found E. coli susceptibility to ciprofloxacin was lower in men, at 55%, compared with 74% among women, but the difference was not statistically significant (P = .14). A similar pattern emerged with cefazolin – 55% susceptibility among men and 69% among women (P = .26). In contrast, trimethoprim/sulfamethoxazole susceptibility trended higher in men, at 73%, vs. 64% among women in the ED (P = .63).
When they divided patients by age 50 years and younger versus those older than 50, the investigators found ampicillin susceptibilities were lower in the younger group, at 30%, compared with 51% among those in the older cohort (P = .03). Similarly, gentamicin susceptibilities were 80% in the younger group, compared with 92% in the older group (P = .04).
Ciprofloxacin susceptibility was significantly lower among people coming to the ED from a long-term care facility than among those coming from home – 35% vs. 77% (P less than .001). Differences in ciprofloxacin susceptibility between admitted and discharged patients was less striking – 63% vs. 78% (P = .04).
Nitrofurantoin was the only oral agent with susceptibility greater than 80% in all patient groups, with susceptibility ranging from 88% to 100%.
Because it typically takes 2-3 days to get the susceptibility results back at Huntington Hospital, many patients are discharged on empiric therapy, noted Mira Zurayk, PharmD, a resident at Huntington Hospital. That can present multiple challenges, particularly with homeless patients who are difficult to find and provide follow-up for, Dr. Jorgensen added.
Based partly on the study findings, the investigators developed a clinical algorithm specifically to address UTI antimicrobial prescriptions in the ED. The algorithm incorporates different recommendations for different groups of patients because of their different resistance trends.
“I think that is a good way to tailor empiric therapy when you don’t have culture results up front,” Dr. Jorgensen said. “We just implemented the algorithm, and I’m now analyzing the outcomes.”
Having more data on outcomes will help the clinicians target lowering the rate of “drug-bug mismatches,” as well as UTI-related revisits to the ED. In addition, the work could help expand the antibiotic stewardship program in the hospital to the ED for the first time, Dr. Jorgensen said.
Dr. Jorgensen and Dr. Zurayk had no relevant financial disclosures. One of the study coauthors, Annie Wong-Beringer, PharmD, receives grant funding from Merck.
AT ASM MICROBE 2017
Key clinical point: Escherichia coli susceptibility to common antibiotics in the emergency department varies by age, sex, and admitted versus discharge status.
Major finding: The only oral antimicrobial with greater than 80% susceptibility across all groups was nitrofurantoin.
Data source: A study of 500 randomly selected adults who presented to the ED with a urinary tract infection, based on ICD-9 or ICD-10 codes.
Disclosures: Dr. Jorgensen and Dr. Zurayk had no relevant financial disclosures. One study coauthor, Annie Wong-Beringer, PharmD, receives grant funding from Merck.
Study shows that 20% of inpatients given antibiotics develop adverse reactions
Twenty percent of hospitalized adults given antibiotics develop adverse drug events, including GI, nephrotoxic, hematologic, cardiac, and neurotoxic effects, according to a report in JAMA Internal Medicine.
This high frequency of adverse reactions “may not be recognized by clinicians because [these events] have varied manifestations, clinicians may be unaware of the risks associated with specific antibiotic agents, or because they occur after patients are discharged from the hospital,” said Pranita D. Tamma, MD, of the division of pediatric infectious diseases, Johns Hopkins University, Baltimore, and her associates.
They assessed antibiotic-associated adverse drug events in all 1,488 adults admitted to four general medicine services at a single medical center during a 9-month period and given at least 24 hours of any antibiotic therapy. The most common indications for antibiotics were urinary tract infections (12%), skin and soft-tissue infections (8%), and community-acquired pneumonia (7%).
Perhaps as important, the researchers noted, 19% of these adverse drug events were attributed to unnecessary antibiotics – drugs given for conditions for which they were not clinically indicated according to the hospital’s own antibiotic guidelines. These included asymptomatic bacteriuria, aspiration pneumonitis, and heart failure (JAMA Intern. Med. 2017 June 12. doi: 10.1001/jamainternmed.2017.1938).
The most common adverse reactions that developed within 30 days were GI, renal, and hematologic abnormalities. Neurotoxic effects included encephalopathy and seizures; cardiotoxic effects included QTc prolongation. Less frequent adverse events included anaphylaxis, daptomycin-associated myositis, trimethoprim/sulfamethoxazole-associated pancreatitis, linezolid-associated neuropathy, and ciprofloxacin-related tendinitis. The most common adverse reactions that developed within 90 days were C. difficile infections and infections involving multidrug-resistant organisms.
“Our findings underscore the importance of avoiding unnecessary antibiotic prescribing to reduce the harm that can result from antibiotic-associated adverse drug events,” Dr. Tamma and her associates said.
Twenty percent of hospitalized adults given antibiotics develop adverse drug events, including GI, nephrotoxic, hematologic, cardiac, and neurotoxic effects, according to a report in JAMA Internal Medicine.
This high frequency of adverse reactions “may not be recognized by clinicians because [these events] have varied manifestations, clinicians may be unaware of the risks associated with specific antibiotic agents, or because they occur after patients are discharged from the hospital,” said Pranita D. Tamma, MD, of the division of pediatric infectious diseases, Johns Hopkins University, Baltimore, and her associates.
They assessed antibiotic-associated adverse drug events in all 1,488 adults admitted to four general medicine services at a single medical center during a 9-month period and given at least 24 hours of any antibiotic therapy. The most common indications for antibiotics were urinary tract infections (12%), skin and soft-tissue infections (8%), and community-acquired pneumonia (7%).
Perhaps as important, the researchers noted, 19% of these adverse drug events were attributed to unnecessary antibiotics – drugs given for conditions for which they were not clinically indicated according to the hospital’s own antibiotic guidelines. These included asymptomatic bacteriuria, aspiration pneumonitis, and heart failure (JAMA Intern. Med. 2017 June 12. doi: 10.1001/jamainternmed.2017.1938).
The most common adverse reactions that developed within 30 days were GI, renal, and hematologic abnormalities. Neurotoxic effects included encephalopathy and seizures; cardiotoxic effects included QTc prolongation. Less frequent adverse events included anaphylaxis, daptomycin-associated myositis, trimethoprim/sulfamethoxazole-associated pancreatitis, linezolid-associated neuropathy, and ciprofloxacin-related tendinitis. The most common adverse reactions that developed within 90 days were C. difficile infections and infections involving multidrug-resistant organisms.
“Our findings underscore the importance of avoiding unnecessary antibiotic prescribing to reduce the harm that can result from antibiotic-associated adverse drug events,” Dr. Tamma and her associates said.
Twenty percent of hospitalized adults given antibiotics develop adverse drug events, including GI, nephrotoxic, hematologic, cardiac, and neurotoxic effects, according to a report in JAMA Internal Medicine.
This high frequency of adverse reactions “may not be recognized by clinicians because [these events] have varied manifestations, clinicians may be unaware of the risks associated with specific antibiotic agents, or because they occur after patients are discharged from the hospital,” said Pranita D. Tamma, MD, of the division of pediatric infectious diseases, Johns Hopkins University, Baltimore, and her associates.
They assessed antibiotic-associated adverse drug events in all 1,488 adults admitted to four general medicine services at a single medical center during a 9-month period and given at least 24 hours of any antibiotic therapy. The most common indications for antibiotics were urinary tract infections (12%), skin and soft-tissue infections (8%), and community-acquired pneumonia (7%).
Perhaps as important, the researchers noted, 19% of these adverse drug events were attributed to unnecessary antibiotics – drugs given for conditions for which they were not clinically indicated according to the hospital’s own antibiotic guidelines. These included asymptomatic bacteriuria, aspiration pneumonitis, and heart failure (JAMA Intern. Med. 2017 June 12. doi: 10.1001/jamainternmed.2017.1938).
The most common adverse reactions that developed within 30 days were GI, renal, and hematologic abnormalities. Neurotoxic effects included encephalopathy and seizures; cardiotoxic effects included QTc prolongation. Less frequent adverse events included anaphylaxis, daptomycin-associated myositis, trimethoprim/sulfamethoxazole-associated pancreatitis, linezolid-associated neuropathy, and ciprofloxacin-related tendinitis. The most common adverse reactions that developed within 90 days were C. difficile infections and infections involving multidrug-resistant organisms.
“Our findings underscore the importance of avoiding unnecessary antibiotic prescribing to reduce the harm that can result from antibiotic-associated adverse drug events,” Dr. Tamma and her associates said.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Among hospitalized adults given antibiotics, 20% develop adverse reactions, including GI, nephrotoxic, hematologic, cardiac, and neurotoxic effects.
Major finding: Among 1,488 patients, 298 (20%) developed 324 adverse reactions to antibiotics – 73% during hospitalization and 27% after discharge – requiring prolonged hospitalization; a subsequent hospitalization; an ED visit; or additional lab tests, ECGs, or imaging studies.
Data source: A single-center retrospective cohort study involving all 1,488 general medicine inpatients admitted during a 9-month period who received any antibiotic for at least 24 hours.
Disclosures: This study was supported by Pfizer Independent Grants for Learning and Change and the Joint Commission. Dr. Tamma and her associates reported having no relevant financial disclosures.
FDA approves new fluoroquinolone for skin, skin structure infections
The Food and Drug Administration has approved delafloxacin, a fluoroquinolone, for the treatment of acute bacterial skin and skin structure infections, according to an agency announcement June 19.
Delafloxacin, which will be marketed by Melinta Therapeutics as Baxdela, was designated a qualified infectious disease product (QIDP) and granted fast-track and priority review. These classifications are designed to speed approval of antibacterial products to treat serious or life-threatening infections, according to an FDA statement.
Common adverse events seen with use of delafloxacin included nausea, diarrhea, headache, elevated liver enzymes, and vomiting.
The approval requires Melinta Therapeutics to conduct a 5-year postmarketing surveillance study to look for resistance to delafloxacin; the final report on that study must be submitted by the end of 2022.
The drug was not subject to FDA advisory committee review because its new drug application “did not raise significant safety or efficacy issues that were unexpected” for a drug in its class, according to FDA officials.
For more information see the Drugs@FDA listing for Baxdela.
[email protected]
On Twitter @denisefulton
The Food and Drug Administration has approved delafloxacin, a fluoroquinolone, for the treatment of acute bacterial skin and skin structure infections, according to an agency announcement June 19.
Delafloxacin, which will be marketed by Melinta Therapeutics as Baxdela, was designated a qualified infectious disease product (QIDP) and granted fast-track and priority review. These classifications are designed to speed approval of antibacterial products to treat serious or life-threatening infections, according to an FDA statement.
Common adverse events seen with use of delafloxacin included nausea, diarrhea, headache, elevated liver enzymes, and vomiting.
The approval requires Melinta Therapeutics to conduct a 5-year postmarketing surveillance study to look for resistance to delafloxacin; the final report on that study must be submitted by the end of 2022.
The drug was not subject to FDA advisory committee review because its new drug application “did not raise significant safety or efficacy issues that were unexpected” for a drug in its class, according to FDA officials.
For more information see the Drugs@FDA listing for Baxdela.
[email protected]
On Twitter @denisefulton
The Food and Drug Administration has approved delafloxacin, a fluoroquinolone, for the treatment of acute bacterial skin and skin structure infections, according to an agency announcement June 19.
Delafloxacin, which will be marketed by Melinta Therapeutics as Baxdela, was designated a qualified infectious disease product (QIDP) and granted fast-track and priority review. These classifications are designed to speed approval of antibacterial products to treat serious or life-threatening infections, according to an FDA statement.
Common adverse events seen with use of delafloxacin included nausea, diarrhea, headache, elevated liver enzymes, and vomiting.
The approval requires Melinta Therapeutics to conduct a 5-year postmarketing surveillance study to look for resistance to delafloxacin; the final report on that study must be submitted by the end of 2022.
The drug was not subject to FDA advisory committee review because its new drug application “did not raise significant safety or efficacy issues that were unexpected” for a drug in its class, according to FDA officials.
For more information see the Drugs@FDA listing for Baxdela.
[email protected]
On Twitter @denisefulton
Cancer, heart disease increase MRSA mortality
Cancer, heart, and neurologic disease are associated with significantly higher 30-day mortality from methicillin-resistant Staphylococcus aureus (MRSA), according to a study that also showed mortality rates have changed little in 9 years.
A retrospective study of 1,168 patients, who were admitted to four Michigan hospitals with MRSA over a period of 9 years, showed an overall 30-day mortality of 16% (Int J Infect Dis. 2017 May 19. doi: 10.1016/j.ijid.2017.05.010).
“Notably, with time, we found no improvement in overall mortality over time despite advancement in antimicrobial treatment,” wrote Pedro Ayau, MD, of the Universidad Francisco Marroquin in Guatemala City and his coauthors. “Thus far, the role of different antimicrobial agents against MRSA infection in clinical settings is uncertain.”
Patients with cancer showed the highest 30-day mortality risk from MRSA infection (odds ratio, 2.29; P = .001). Heart disease increased the mortality risk by 78%, neurologic disease by 65%, and nursing home residence by 66%. A Charlson index score greater than 3 was associated with an 88% increase in 30-day mortality.
Age was also an independent risk factor, with each additional year of age associated with a 2.9% increase in the odds of 30-day mortality, even after accounting for other variables.
The authors found evidence of a protective effect associated with diabetes and peripheral vascular disease, with a decrease in 30-day mortality of 40% and 47%, respectively. Although this was an unexpected finding, it was likely related to the source of the infection, they said.
“Patients with [peripheral vascular disease] and diabetes are usually less acutely ill and present with skin/wound infections, which are more easily managed, and started earlier on appropriate antibiotic treatment,” the investigators wrote.
Patients who were readmitted had an 88% lower risk of 30-day mortality. The authors suggested this may be because these patients would likely have received earlier and better management of the infection.
There was also a relationship between the source of infection and mortality. Patients infected from an indwelling central venous catheter had a 61% lower 30-day mortality. Those with skin or wound infections had a 52% lower mortality, and those with genitourinary infection had a 60% lower mortality.
In contrast to other studies, the researchers did not see any significant increase in 30-day mortality with persistent bacteremia.
Two authors declared research grants from the pharmaceutical industries.
Cancer, heart, and neurologic disease are associated with significantly higher 30-day mortality from methicillin-resistant Staphylococcus aureus (MRSA), according to a study that also showed mortality rates have changed little in 9 years.
A retrospective study of 1,168 patients, who were admitted to four Michigan hospitals with MRSA over a period of 9 years, showed an overall 30-day mortality of 16% (Int J Infect Dis. 2017 May 19. doi: 10.1016/j.ijid.2017.05.010).
“Notably, with time, we found no improvement in overall mortality over time despite advancement in antimicrobial treatment,” wrote Pedro Ayau, MD, of the Universidad Francisco Marroquin in Guatemala City and his coauthors. “Thus far, the role of different antimicrobial agents against MRSA infection in clinical settings is uncertain.”
Patients with cancer showed the highest 30-day mortality risk from MRSA infection (odds ratio, 2.29; P = .001). Heart disease increased the mortality risk by 78%, neurologic disease by 65%, and nursing home residence by 66%. A Charlson index score greater than 3 was associated with an 88% increase in 30-day mortality.
Age was also an independent risk factor, with each additional year of age associated with a 2.9% increase in the odds of 30-day mortality, even after accounting for other variables.
The authors found evidence of a protective effect associated with diabetes and peripheral vascular disease, with a decrease in 30-day mortality of 40% and 47%, respectively. Although this was an unexpected finding, it was likely related to the source of the infection, they said.
“Patients with [peripheral vascular disease] and diabetes are usually less acutely ill and present with skin/wound infections, which are more easily managed, and started earlier on appropriate antibiotic treatment,” the investigators wrote.
Patients who were readmitted had an 88% lower risk of 30-day mortality. The authors suggested this may be because these patients would likely have received earlier and better management of the infection.
There was also a relationship between the source of infection and mortality. Patients infected from an indwelling central venous catheter had a 61% lower 30-day mortality. Those with skin or wound infections had a 52% lower mortality, and those with genitourinary infection had a 60% lower mortality.
In contrast to other studies, the researchers did not see any significant increase in 30-day mortality with persistent bacteremia.
Two authors declared research grants from the pharmaceutical industries.
Cancer, heart, and neurologic disease are associated with significantly higher 30-day mortality from methicillin-resistant Staphylococcus aureus (MRSA), according to a study that also showed mortality rates have changed little in 9 years.
A retrospective study of 1,168 patients, who were admitted to four Michigan hospitals with MRSA over a period of 9 years, showed an overall 30-day mortality of 16% (Int J Infect Dis. 2017 May 19. doi: 10.1016/j.ijid.2017.05.010).
“Notably, with time, we found no improvement in overall mortality over time despite advancement in antimicrobial treatment,” wrote Pedro Ayau, MD, of the Universidad Francisco Marroquin in Guatemala City and his coauthors. “Thus far, the role of different antimicrobial agents against MRSA infection in clinical settings is uncertain.”
Patients with cancer showed the highest 30-day mortality risk from MRSA infection (odds ratio, 2.29; P = .001). Heart disease increased the mortality risk by 78%, neurologic disease by 65%, and nursing home residence by 66%. A Charlson index score greater than 3 was associated with an 88% increase in 30-day mortality.
Age was also an independent risk factor, with each additional year of age associated with a 2.9% increase in the odds of 30-day mortality, even after accounting for other variables.
The authors found evidence of a protective effect associated with diabetes and peripheral vascular disease, with a decrease in 30-day mortality of 40% and 47%, respectively. Although this was an unexpected finding, it was likely related to the source of the infection, they said.
“Patients with [peripheral vascular disease] and diabetes are usually less acutely ill and present with skin/wound infections, which are more easily managed, and started earlier on appropriate antibiotic treatment,” the investigators wrote.
Patients who were readmitted had an 88% lower risk of 30-day mortality. The authors suggested this may be because these patients would likely have received earlier and better management of the infection.
There was also a relationship between the source of infection and mortality. Patients infected from an indwelling central venous catheter had a 61% lower 30-day mortality. Those with skin or wound infections had a 52% lower mortality, and those with genitourinary infection had a 60% lower mortality.
In contrast to other studies, the researchers did not see any significant increase in 30-day mortality with persistent bacteremia.
Two authors declared research grants from the pharmaceutical industries.
FROM INTERNATIONAL JOURNAL OF INFECTIOUS DISEASES
Key clinical point:
Major finding: Cancer is associated with a more than twofold increase in 30-day mortality from MRSA.
Data source: A 9-year retrospective study of 1,168 patients with MRSA infection.
Disclosures: Two authors declared research grants from the pharmaceutical industry.
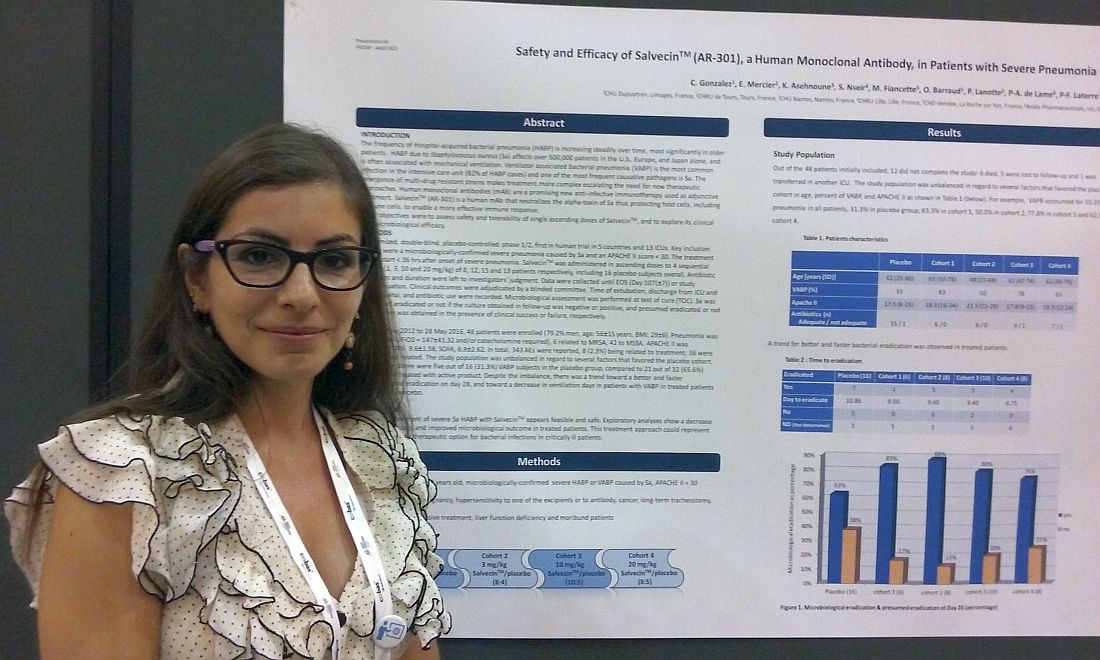
Monoclonal antibody holds promise for S. aureus pneumonia
NEW ORLEANS – Monoclonal antibody therapies have already upended treatment strategies in cancer, dermatology, and multiple inflammatory diseases, and infectious disease may be next.
That’s because , according to a new study. The monoclonal antibody attacks the alpha-toxin secreted by S. aureus, thereby helping to protect immune cells.
“We know S. aureus pneumonia is a big problem. There is a lot of antibiotic resistance, and that is why we need new treatments,” Celine Gonzalez, MD, of the Dupuytren Central University Hospital in Limoges, France, said in an interview.
“Animal studies have shown the monoclonal antibody seems to be useful. This is the first in-human study to use a monoclonal antibody to treat hospital-acquired pneumonia due to Staphylococcus aureus,” Dr. Gonzalez said in a late-breaking poster presentation at the annual meeting of the American Society for Microbiology.
Treatment started within 36 hours of onset of severe pneumonia. Severity was based on a mean PaO2/FiO2 of 147 and/or a need for catecholamine. Six cases of pneumonia were related to MRSA and the remaining 42 to methicillin-susceptible S. aureus. The mean APACHE II score was 18.7, the mean Clinical Pulmonary Infection Score was 9.6, and the mean Sequential Organ Failure Assessment score was 6.9.
Participants were recruited from 13 ICUs in four countries. About 80% of participants were men. Their mean age was 56 years, and mean body mass index was 29 kg/m2. Concurrent antibiotic treatment choice and duration were at the investigator’s discretion.
S. aureus infection was considered eradicated if a follow-up culture was negative, a result achieved by 63% of the 16 placebo patients and 75%-88% of the AR-301-dosage groups. Eradication was also based on observed clinical success in the absence of a confirmatory culture. This was achieved by 38% in the placebo group and 13%-25% of the monoclonal antibody cohorts. A total of seven placebo patients and 15 AR-301 patients met eradication by these criteria.
Side effects were primarily minor and transient, Dr. Gonzalez said. Of the 343 total adverse events reported, only 8 (2.3%) were considered treatment related, she added.
“In infectious disease, it’s the beginning” for monoclonal antibody therapy, Dr. Gonzalez said. “But, it appears to be the future because … it is a more specific treatment, and there is no resistance.”
The study suggests adjunctive treatment with AR-301 appears safe for treatment of hospital-acquired bacterial pneumonia, she noted. The next step will be to confirm the findings in a larger, follow-up study that includes more efficacy outcomes, Dr. Gonzalez added.
Dr. Gonzalez reported having no relevant disclosures. The study’s principle investigator is a scientific advisor for Aridis Pharmaceuticals, which is developing AR-301.
NEW ORLEANS – Monoclonal antibody therapies have already upended treatment strategies in cancer, dermatology, and multiple inflammatory diseases, and infectious disease may be next.
That’s because , according to a new study. The monoclonal antibody attacks the alpha-toxin secreted by S. aureus, thereby helping to protect immune cells.
“We know S. aureus pneumonia is a big problem. There is a lot of antibiotic resistance, and that is why we need new treatments,” Celine Gonzalez, MD, of the Dupuytren Central University Hospital in Limoges, France, said in an interview.
“Animal studies have shown the monoclonal antibody seems to be useful. This is the first in-human study to use a monoclonal antibody to treat hospital-acquired pneumonia due to Staphylococcus aureus,” Dr. Gonzalez said in a late-breaking poster presentation at the annual meeting of the American Society for Microbiology.
Treatment started within 36 hours of onset of severe pneumonia. Severity was based on a mean PaO2/FiO2 of 147 and/or a need for catecholamine. Six cases of pneumonia were related to MRSA and the remaining 42 to methicillin-susceptible S. aureus. The mean APACHE II score was 18.7, the mean Clinical Pulmonary Infection Score was 9.6, and the mean Sequential Organ Failure Assessment score was 6.9.
Participants were recruited from 13 ICUs in four countries. About 80% of participants were men. Their mean age was 56 years, and mean body mass index was 29 kg/m2. Concurrent antibiotic treatment choice and duration were at the investigator’s discretion.
S. aureus infection was considered eradicated if a follow-up culture was negative, a result achieved by 63% of the 16 placebo patients and 75%-88% of the AR-301-dosage groups. Eradication was also based on observed clinical success in the absence of a confirmatory culture. This was achieved by 38% in the placebo group and 13%-25% of the monoclonal antibody cohorts. A total of seven placebo patients and 15 AR-301 patients met eradication by these criteria.
Side effects were primarily minor and transient, Dr. Gonzalez said. Of the 343 total adverse events reported, only 8 (2.3%) were considered treatment related, she added.
“In infectious disease, it’s the beginning” for monoclonal antibody therapy, Dr. Gonzalez said. “But, it appears to be the future because … it is a more specific treatment, and there is no resistance.”
The study suggests adjunctive treatment with AR-301 appears safe for treatment of hospital-acquired bacterial pneumonia, she noted. The next step will be to confirm the findings in a larger, follow-up study that includes more efficacy outcomes, Dr. Gonzalez added.
Dr. Gonzalez reported having no relevant disclosures. The study’s principle investigator is a scientific advisor for Aridis Pharmaceuticals, which is developing AR-301.
NEW ORLEANS – Monoclonal antibody therapies have already upended treatment strategies in cancer, dermatology, and multiple inflammatory diseases, and infectious disease may be next.
That’s because , according to a new study. The monoclonal antibody attacks the alpha-toxin secreted by S. aureus, thereby helping to protect immune cells.
“We know S. aureus pneumonia is a big problem. There is a lot of antibiotic resistance, and that is why we need new treatments,” Celine Gonzalez, MD, of the Dupuytren Central University Hospital in Limoges, France, said in an interview.
“Animal studies have shown the monoclonal antibody seems to be useful. This is the first in-human study to use a monoclonal antibody to treat hospital-acquired pneumonia due to Staphylococcus aureus,” Dr. Gonzalez said in a late-breaking poster presentation at the annual meeting of the American Society for Microbiology.
Treatment started within 36 hours of onset of severe pneumonia. Severity was based on a mean PaO2/FiO2 of 147 and/or a need for catecholamine. Six cases of pneumonia were related to MRSA and the remaining 42 to methicillin-susceptible S. aureus. The mean APACHE II score was 18.7, the mean Clinical Pulmonary Infection Score was 9.6, and the mean Sequential Organ Failure Assessment score was 6.9.
Participants were recruited from 13 ICUs in four countries. About 80% of participants were men. Their mean age was 56 years, and mean body mass index was 29 kg/m2. Concurrent antibiotic treatment choice and duration were at the investigator’s discretion.
S. aureus infection was considered eradicated if a follow-up culture was negative, a result achieved by 63% of the 16 placebo patients and 75%-88% of the AR-301-dosage groups. Eradication was also based on observed clinical success in the absence of a confirmatory culture. This was achieved by 38% in the placebo group and 13%-25% of the monoclonal antibody cohorts. A total of seven placebo patients and 15 AR-301 patients met eradication by these criteria.
Side effects were primarily minor and transient, Dr. Gonzalez said. Of the 343 total adverse events reported, only 8 (2.3%) were considered treatment related, she added.
“In infectious disease, it’s the beginning” for monoclonal antibody therapy, Dr. Gonzalez said. “But, it appears to be the future because … it is a more specific treatment, and there is no resistance.”
The study suggests adjunctive treatment with AR-301 appears safe for treatment of hospital-acquired bacterial pneumonia, she noted. The next step will be to confirm the findings in a larger, follow-up study that includes more efficacy outcomes, Dr. Gonzalez added.
Dr. Gonzalez reported having no relevant disclosures. The study’s principle investigator is a scientific advisor for Aridis Pharmaceuticals, which is developing AR-301.
AT ASM MICROBE 2017
Key clinical point: A monoclonal antibody that neutralizes the alpha-toxin secreted by S. aureus appeared safe and effective in an early trial.
Major finding: AR-301 appeared safe, with 8 of 343 adverse events, or 2.3%, considered treatment related.
Data source: Randomized, double-blind, placebo-controlled, international study in 48 patients from 13 ICUs.
Disclosures: Dr. Gonzalez reported having no relevant disclosures. The study’s principle investigator is a scientific advisor for Aridis Pharmaceuticals, which is developing AR-301.
Rapid culture, stewardship improve S. aureus bacteremia outcomes
NEW ORLEANS – Community hospitals could see positive outcomes using a Staphylococcus aureus bacteremia strategy that combines rapid blood cultures to speed diagnosis with antibiotic stewardship to guide treatment.
Many academic medical centers report improved outcomes with this approach. Now a study of 66 patients at a medium-sized hospital in rural North Dakota suggests this strategy translates well to the community hospital setting and can reduce mortality and 30-day readmission rates, and increase cost-effectiveness overall.
“I was pleased to see we were able to replicate the positive outcomes observed in studies from large tertiary care centers with our small cohort,” Marijo Roiko, PhD, microbiology program director for pathology and laboratory services at Altru Health System in Grand Forks, N.D., said in an interview.
Dr. Roiko and colleagues compared 33 patients diagnosed and treated prior to the strategy with 33 others following its implementation. A total of 13 patients, or 39% of each cohort, developed potentially fatal methicillin-resistant S. aureus (MRSA) bacteremia. Patients’ average age ranged from 60 to 64 years, and about two-thirds of each group were men.
The investigators reported that 30-day all-cause mortality decreased from 15.6% to 13.3% after the protocol. In addition, 30-day readmission rates decreased from 25% to 11% of the group diagnosed and managed with the new strategy. Dr. Roiko presented these and other findings from the chart review at the annual meeting of the American Society for Microbiology.
Overall, the average length of stay decreased from 13 days to 10 days among the patients with S. aureus bacteremia. Among the subgroup of patients with MRSA, the length of stay dropped from 15 to 12 days. Among those with methicillin-susceptible S. aureus infections, 11 days decreased to 9 days after institution of the protocol.
The researchers also looked at time to antibiotic deescalation, and the average time decreased from 3 days to 1 day with the new strategy.
“These results demonstrate the utility of rapid testing from positive blood cultures and antibiotic stewardship for patients with Staph. aureus bacteremia,” Dr. Roiko said.
In terms of return on investment, the estimated cost savings associated with the 3-day reduction in length of hospital stay was sufficient to cover the increased capital expenditures and reagent costs, the researchers found. They estimated these increased costs as $78,960, excluding ICU and ancillary charges. The approximate $4,290 saved per day multiplied by 33 patients means the new protocol saved a total of $141,570.
Traditionally, patients with a positive blood culture of S. aureus had a gram stain, followed by provider notification when positive. Targeted antibiotic therapy was either administered at this point or held for culture-based identification and susceptibility testing. In the new protocol, a rapid culture identification panel (FilmArray BCID) is added at the time of gram staining. Positive results are reported to both the provider and pharmacist. Targeted therapy is then either administered or held based on culture-based susceptibility testing (species identification is determined as needed).
The current study findings add to a literature already supporting use of rapid blood cultures and/or stewardship guidance to address S. aureus bacteremia in academic and tertiary care centers (J Clin Microbiol. 2016;54:2455-63; Clin Microbiol Infect. 2015;21:313-22, and Clin. Infect. Dis. 2015;61:1071-80.
Dr. Roiko had no relevant financial disclosures.
NEW ORLEANS – Community hospitals could see positive outcomes using a Staphylococcus aureus bacteremia strategy that combines rapid blood cultures to speed diagnosis with antibiotic stewardship to guide treatment.
Many academic medical centers report improved outcomes with this approach. Now a study of 66 patients at a medium-sized hospital in rural North Dakota suggests this strategy translates well to the community hospital setting and can reduce mortality and 30-day readmission rates, and increase cost-effectiveness overall.
“I was pleased to see we were able to replicate the positive outcomes observed in studies from large tertiary care centers with our small cohort,” Marijo Roiko, PhD, microbiology program director for pathology and laboratory services at Altru Health System in Grand Forks, N.D., said in an interview.
Dr. Roiko and colleagues compared 33 patients diagnosed and treated prior to the strategy with 33 others following its implementation. A total of 13 patients, or 39% of each cohort, developed potentially fatal methicillin-resistant S. aureus (MRSA) bacteremia. Patients’ average age ranged from 60 to 64 years, and about two-thirds of each group were men.
The investigators reported that 30-day all-cause mortality decreased from 15.6% to 13.3% after the protocol. In addition, 30-day readmission rates decreased from 25% to 11% of the group diagnosed and managed with the new strategy. Dr. Roiko presented these and other findings from the chart review at the annual meeting of the American Society for Microbiology.
Overall, the average length of stay decreased from 13 days to 10 days among the patients with S. aureus bacteremia. Among the subgroup of patients with MRSA, the length of stay dropped from 15 to 12 days. Among those with methicillin-susceptible S. aureus infections, 11 days decreased to 9 days after institution of the protocol.
The researchers also looked at time to antibiotic deescalation, and the average time decreased from 3 days to 1 day with the new strategy.
“These results demonstrate the utility of rapid testing from positive blood cultures and antibiotic stewardship for patients with Staph. aureus bacteremia,” Dr. Roiko said.
In terms of return on investment, the estimated cost savings associated with the 3-day reduction in length of hospital stay was sufficient to cover the increased capital expenditures and reagent costs, the researchers found. They estimated these increased costs as $78,960, excluding ICU and ancillary charges. The approximate $4,290 saved per day multiplied by 33 patients means the new protocol saved a total of $141,570.
Traditionally, patients with a positive blood culture of S. aureus had a gram stain, followed by provider notification when positive. Targeted antibiotic therapy was either administered at this point or held for culture-based identification and susceptibility testing. In the new protocol, a rapid culture identification panel (FilmArray BCID) is added at the time of gram staining. Positive results are reported to both the provider and pharmacist. Targeted therapy is then either administered or held based on culture-based susceptibility testing (species identification is determined as needed).
The current study findings add to a literature already supporting use of rapid blood cultures and/or stewardship guidance to address S. aureus bacteremia in academic and tertiary care centers (J Clin Microbiol. 2016;54:2455-63; Clin Microbiol Infect. 2015;21:313-22, and Clin. Infect. Dis. 2015;61:1071-80.
Dr. Roiko had no relevant financial disclosures.
NEW ORLEANS – Community hospitals could see positive outcomes using a Staphylococcus aureus bacteremia strategy that combines rapid blood cultures to speed diagnosis with antibiotic stewardship to guide treatment.
Many academic medical centers report improved outcomes with this approach. Now a study of 66 patients at a medium-sized hospital in rural North Dakota suggests this strategy translates well to the community hospital setting and can reduce mortality and 30-day readmission rates, and increase cost-effectiveness overall.
“I was pleased to see we were able to replicate the positive outcomes observed in studies from large tertiary care centers with our small cohort,” Marijo Roiko, PhD, microbiology program director for pathology and laboratory services at Altru Health System in Grand Forks, N.D., said in an interview.
Dr. Roiko and colleagues compared 33 patients diagnosed and treated prior to the strategy with 33 others following its implementation. A total of 13 patients, or 39% of each cohort, developed potentially fatal methicillin-resistant S. aureus (MRSA) bacteremia. Patients’ average age ranged from 60 to 64 years, and about two-thirds of each group were men.
The investigators reported that 30-day all-cause mortality decreased from 15.6% to 13.3% after the protocol. In addition, 30-day readmission rates decreased from 25% to 11% of the group diagnosed and managed with the new strategy. Dr. Roiko presented these and other findings from the chart review at the annual meeting of the American Society for Microbiology.
Overall, the average length of stay decreased from 13 days to 10 days among the patients with S. aureus bacteremia. Among the subgroup of patients with MRSA, the length of stay dropped from 15 to 12 days. Among those with methicillin-susceptible S. aureus infections, 11 days decreased to 9 days after institution of the protocol.
The researchers also looked at time to antibiotic deescalation, and the average time decreased from 3 days to 1 day with the new strategy.
“These results demonstrate the utility of rapid testing from positive blood cultures and antibiotic stewardship for patients with Staph. aureus bacteremia,” Dr. Roiko said.
In terms of return on investment, the estimated cost savings associated with the 3-day reduction in length of hospital stay was sufficient to cover the increased capital expenditures and reagent costs, the researchers found. They estimated these increased costs as $78,960, excluding ICU and ancillary charges. The approximate $4,290 saved per day multiplied by 33 patients means the new protocol saved a total of $141,570.
Traditionally, patients with a positive blood culture of S. aureus had a gram stain, followed by provider notification when positive. Targeted antibiotic therapy was either administered at this point or held for culture-based identification and susceptibility testing. In the new protocol, a rapid culture identification panel (FilmArray BCID) is added at the time of gram staining. Positive results are reported to both the provider and pharmacist. Targeted therapy is then either administered or held based on culture-based susceptibility testing (species identification is determined as needed).
The current study findings add to a literature already supporting use of rapid blood cultures and/or stewardship guidance to address S. aureus bacteremia in academic and tertiary care centers (J Clin Microbiol. 2016;54:2455-63; Clin Microbiol Infect. 2015;21:313-22, and Clin. Infect. Dis. 2015;61:1071-80.
Dr. Roiko had no relevant financial disclosures.
AT ASM MICROBE 2017
Key clinical point:
Major finding: 30-day mortality dropped from 15.6% prior to the protocol to 13.3% after implementation.
Data source: A retrospective comparison of 33 patients receiving traditional diagnosis and management versus 33 others with a new rapid blood culture and stewardship program approach.
Disclosures: Dr. Roiko had no relevant financial disclosures.