User login
CDC: Opioid prescribing and use rates down since 2010
Trends in opioid prescribing and use from 2010 to 2016 offer some encouragement, but opioid-attributable deaths continued to increase over that period, according to the Centers for Disease Control and Prevention.
Prescribing rates dropped during that period, as did daily opioid dosage rates and the percentage of patients with high daily opioid dosages, Gail K. Strickler, PhD, of the Institute for Behavioral Health at Brandeis University in Waltham, Mass., and associates wrote in MMWR Surveillance Summaries.
Their analysis involved 11 of the 12 states (Washington was unable to provide data for the analysis) participating in the CDC’s Prescription Behavior Surveillance System, which uses data from the states’ prescription drug monitoring programs. The 11 states represented about 38% of the U.S. population in 2016.
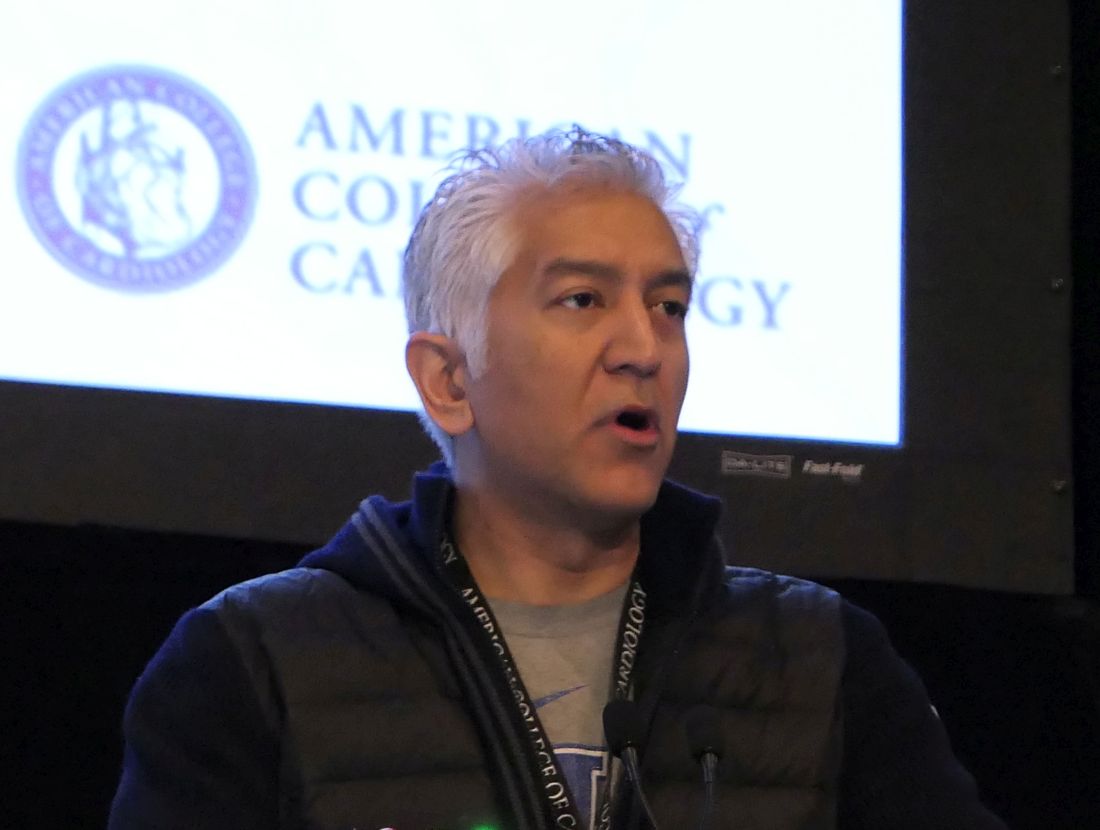
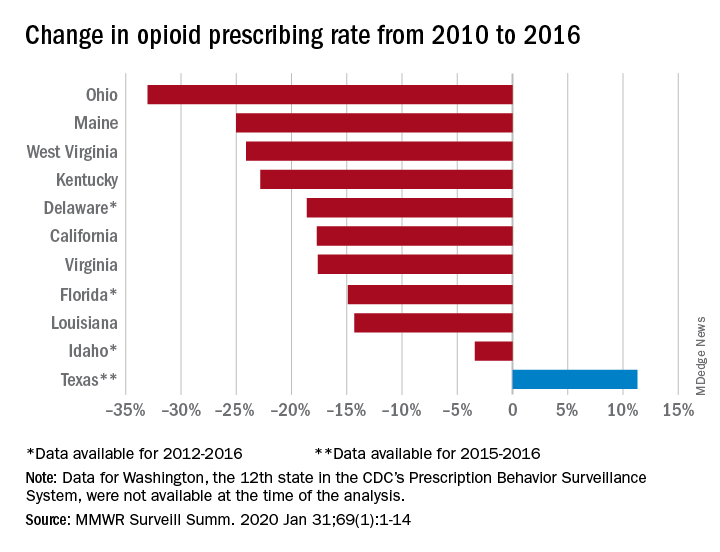
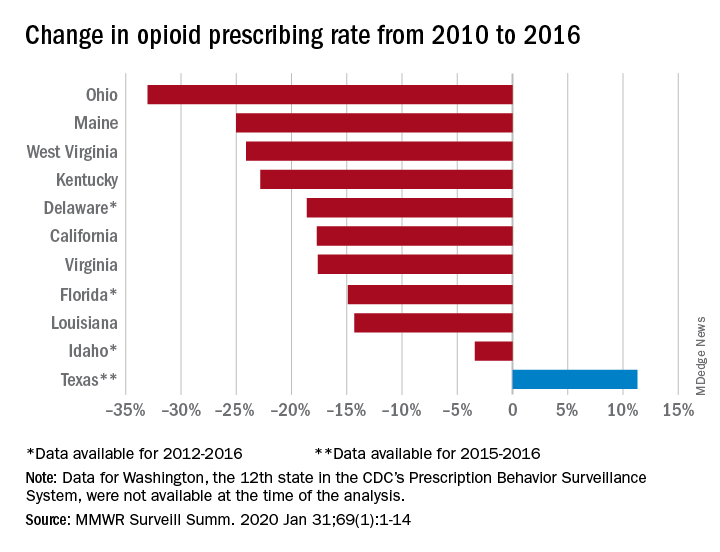
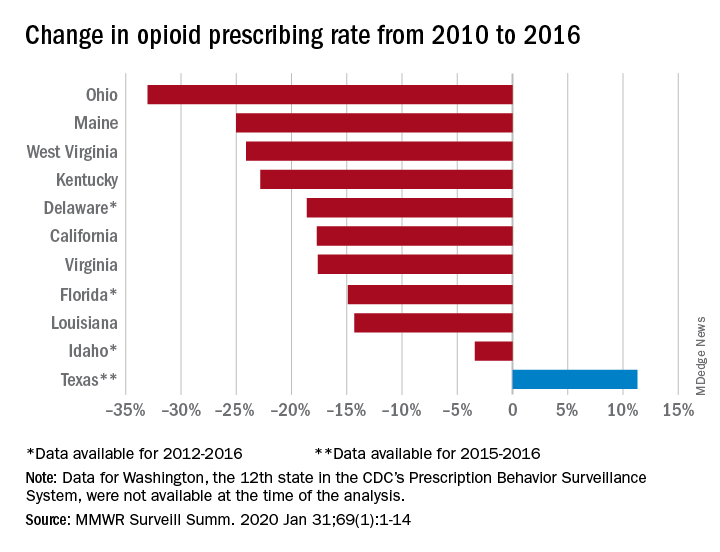
The opioid prescribing rate fell in 10 of those 11 states, with declines varying from 3.4% in Idaho to 33.0% in Ohio. Prescribing went up in Texas by 11.3%, but the state only had data available for 2015 and 2016. Three other states – Delaware, Florida, and Idaho – were limited to data from 2012 to 2016, the investigators noted.
As for the other measures, all states showed declines for the mean daily opioid dosage. Texas had the smallest drop at 2.9% and Florida saw the largest, at 27.4%. All states also had reductions in the percentage of patients with high daily opioid dosage, with decreases varying from 5.7% in Idaho to 43.9% in Louisiana, Dr. Strickler and associates reported. A high daily dosage was defined as at least 90 morphine milligram equivalents for all class II-V opioid drugs.
“Despite these favorable trends ... opioid overdose deaths attributable to the most commonly prescribed opioids, the natural and semisynthetics (e.g., morphine and oxycodone), increased during 2010-2016,” they said.
It is possible that a change in mortality is lagging “behind changes in prescribing behaviors” or that “the trend in deaths related to these types of opioids has been driven by factors other than prescription opioid misuse rates, such as increasing mortality from heroin, which is frequently classified as morphine or found concomitantly with morphine postmortem, and a spike in deaths involving illicitly manufactured fentanyl combined with heroin and prescribed opioids since 2013,” the investigators suggested.
SOURCE: Strickler GK et al. MMWR Surveill Summ. 2020 Jan 31;69(1):1-14.
Trends in opioid prescribing and use from 2010 to 2016 offer some encouragement, but opioid-attributable deaths continued to increase over that period, according to the Centers for Disease Control and Prevention.
Prescribing rates dropped during that period, as did daily opioid dosage rates and the percentage of patients with high daily opioid dosages, Gail K. Strickler, PhD, of the Institute for Behavioral Health at Brandeis University in Waltham, Mass., and associates wrote in MMWR Surveillance Summaries.
Their analysis involved 11 of the 12 states (Washington was unable to provide data for the analysis) participating in the CDC’s Prescription Behavior Surveillance System, which uses data from the states’ prescription drug monitoring programs. The 11 states represented about 38% of the U.S. population in 2016.
The opioid prescribing rate fell in 10 of those 11 states, with declines varying from 3.4% in Idaho to 33.0% in Ohio. Prescribing went up in Texas by 11.3%, but the state only had data available for 2015 and 2016. Three other states – Delaware, Florida, and Idaho – were limited to data from 2012 to 2016, the investigators noted.
As for the other measures, all states showed declines for the mean daily opioid dosage. Texas had the smallest drop at 2.9% and Florida saw the largest, at 27.4%. All states also had reductions in the percentage of patients with high daily opioid dosage, with decreases varying from 5.7% in Idaho to 43.9% in Louisiana, Dr. Strickler and associates reported. A high daily dosage was defined as at least 90 morphine milligram equivalents for all class II-V opioid drugs.
“Despite these favorable trends ... opioid overdose deaths attributable to the most commonly prescribed opioids, the natural and semisynthetics (e.g., morphine and oxycodone), increased during 2010-2016,” they said.
It is possible that a change in mortality is lagging “behind changes in prescribing behaviors” or that “the trend in deaths related to these types of opioids has been driven by factors other than prescription opioid misuse rates, such as increasing mortality from heroin, which is frequently classified as morphine or found concomitantly with morphine postmortem, and a spike in deaths involving illicitly manufactured fentanyl combined with heroin and prescribed opioids since 2013,” the investigators suggested.
SOURCE: Strickler GK et al. MMWR Surveill Summ. 2020 Jan 31;69(1):1-14.
Trends in opioid prescribing and use from 2010 to 2016 offer some encouragement, but opioid-attributable deaths continued to increase over that period, according to the Centers for Disease Control and Prevention.
Prescribing rates dropped during that period, as did daily opioid dosage rates and the percentage of patients with high daily opioid dosages, Gail K. Strickler, PhD, of the Institute for Behavioral Health at Brandeis University in Waltham, Mass., and associates wrote in MMWR Surveillance Summaries.
Their analysis involved 11 of the 12 states (Washington was unable to provide data for the analysis) participating in the CDC’s Prescription Behavior Surveillance System, which uses data from the states’ prescription drug monitoring programs. The 11 states represented about 38% of the U.S. population in 2016.
The opioid prescribing rate fell in 10 of those 11 states, with declines varying from 3.4% in Idaho to 33.0% in Ohio. Prescribing went up in Texas by 11.3%, but the state only had data available for 2015 and 2016. Three other states – Delaware, Florida, and Idaho – were limited to data from 2012 to 2016, the investigators noted.
As for the other measures, all states showed declines for the mean daily opioid dosage. Texas had the smallest drop at 2.9% and Florida saw the largest, at 27.4%. All states also had reductions in the percentage of patients with high daily opioid dosage, with decreases varying from 5.7% in Idaho to 43.9% in Louisiana, Dr. Strickler and associates reported. A high daily dosage was defined as at least 90 morphine milligram equivalents for all class II-V opioid drugs.
“Despite these favorable trends ... opioid overdose deaths attributable to the most commonly prescribed opioids, the natural and semisynthetics (e.g., morphine and oxycodone), increased during 2010-2016,” they said.
It is possible that a change in mortality is lagging “behind changes in prescribing behaviors” or that “the trend in deaths related to these types of opioids has been driven by factors other than prescription opioid misuse rates, such as increasing mortality from heroin, which is frequently classified as morphine or found concomitantly with morphine postmortem, and a spike in deaths involving illicitly manufactured fentanyl combined with heroin and prescribed opioids since 2013,” the investigators suggested.
SOURCE: Strickler GK et al. MMWR Surveill Summ. 2020 Jan 31;69(1):1-14.
FROM MMWR SURVEILLANCE SUMMARIES
Rural treatment of opioid use disorder increasingly driven by nonphysician workforce
Nurse practitioners and physician assistants, rather than physicians, are the clinicians who have boosted capacity for buprenorphine prescribing in rural America, according to a study in a rural health–focused issue of the journal Health Affairs.
In the face of an ongoing crisis of opioid use disorder, and associated overdoses and deaths that have spared no sector of the U.S. population, the federal government expanded its waiver program for buprenorphine prescribing in 2017. The waiver expansion allows nurse practitioners (NPs) and physician assistants (PAs) – along with clinical nurse specialists, certified registered nurse anesthetists, and certified nurse-midwives – to use the drug for medication-assisted treatment (MAT) for opioid use disorder after completing 24 hours of mandated training; physicians are required to complete 8 hours of training to receive their waiver.
From 2016 to 2019, capacity for MAT in rural areas increased, with the number of clinicians with buprenorphine waivers more than doubling. Of the newly waivered prescribers accounting for this 111% increase, more than half were NPs and PAs.
In many areas, NPs and PAs led the way forward, wrote the study’s lead author Michael L. Barnett, MD, and coauthors, noting in the abstract accompanying the paper that “NPs and PAs accounted for more than half of this increase and were the first waivered clinicians in 285 rural counties with 5.7 million residents.” Overall, the proportion of people living in a county without a waivered clinician has decreased by 36% since NPs and PAs were permitted to obtain waivers.
SAMHSA data identifies trends
In an in-depth interview, Dr. Barnett, an internal medicine physician and health services researcher at the Harvard School of Public Health, Boston, said the issue today is “not so much continuing to dissect the risks and benefits of opioids as a treatment for pain, but more trying to address the current overdose crisis, and the fact that our patient treatment infrastructure is woefully inadequate for the magnitude of the problem that we face.”
Dr. Barnett’s chief intention for this study, he said, was to generate information that will drive policy to implement effective opioid treatment. He’d always been interested in models of care delivery that move beyond seeing just the physician-patient dyad.
“There are a whole range of nonphysician providers that are probably better at providing many different types of care – things that physicians aren’t necessarily that well trained to do,” he said.
Expansion of buprenorphine waivers to NPs and PAs, said Dr. Barnett, presented “a very interesting opportunity to see: How does a nonphysician workforce respond to a new practice opportunity, to really be engaged in areas that many physicians really were neglecting?”
The researchers used information drawn from what Dr. Barnett characterized as a “gold-standard” dataset maintained by the federal Substance Abuse and Mental Health Services Administration. They found that, by March 2019, 52% of U.S. rural residents lived in counties with at least one NP or PA holding a buprenorphine waiver, though there was wide geographic variation: Every county in Maine and New Hampshire had waivered NPs or PAs, but in Tennessee, just 3 of 95 counties had an NP or PA with a waiver.
Scope-of-practice regulations matter
The scope of practice permitted NPs and PAs varies by state, and Dr. Barnett and coauthors also looked to see whether broader scope of practice meant that more advanced practice clinicians were getting buprenorphine waivers. This did appear to be the case: In an analysis that dichotomized scope of practice into “broad” and “restricted,” states with broader practice scope saw twice as many waivered NPs per 100,000 rural residents as those with restrictive practice scope. This association was not seen for PAs, but Dr. Barnett pointed out that PAs are less likely overall to work in primary care.
This, he added, is where scope of practice starts to matter. “A lot of states are still bickering about scope of practice. We show in our paper the clear relationship between scope of practice and the degree to which providers are able to take up these waivers. We can’t prove causality, but I think it’s not a big stretch to think that these policies are playing a big role. I hope we’re working to try to advance that conversation.”
Helping address the unmet need for evidence-based treatment of opioid use disorder, he said, “is one of the more important examples, because doctors have been leaving rural areas in droves. We are lucky that there is a workforce of NPs that still seem to recognize the market opportunity; rural areas still need providers, and they have been willing to fill the gap.”
Waivered NPs or PAs can apply for an expanded waiver, permitting expansion of the buprenorphine panel from 30 to 100 patients after 1 year of holding their initial waiver. Physicians may apply for a waiver to treat up to 275 patients.
Effect on quality of care
The evidence doesn’t support big worries about quality of care, he said. “We don’t have any data on this in the clinical context of addiction, but all of the data that are out there in terms of evaluating the quality of care and level of care being offered by NPs and PAs versus primary care doctors – the types of things that we think of as within the scope of NP and PA practice typically – have shown that they are the same.” Dr. Barnett acknowledged that “there are a little bit of mixed results here and there in one direction or another, but largely, the care being delivered is much more the same than different.”
In addressing the opioid crisis as in the rest of medicine, it’s a mistake not to include this sector of the health care workforce when policies are being crafted, said Dr. Barnett. “People who are making policy and aren’t familiar with the workforce in rural areas could miss the boat. ... NPs aren’t just an asterisk to the workforce – they are an essential part of delivering medicine, just as much as physicians are.”
Dr. Barnett said that, in his estimation, “a lot of protectionist myths get physicians worked up around increased scope of practice for NPs.” However, “The truth is that there’s enough health care spending to go around for everybody and there’s plenty of work to go around.”
Dr. Barnett acknowledged that the current study captured only prescribing capacity, and not actual prescription volume. But, based on some preliminary data, “my sense is that NPs and PAs who acquire waivers are more likely to be prescribing to a larger number of patients proportionately than MDs.” He wasn’t surprised to see this, since the many more hours of training required for NPs and PAs to acquire a waiver means they’re likely to be committed to using the waiver in practice.
Stepping back to look at the bigger picture, Dr. Barnett remarked that, “taking a look at the waiver requirement, a part of me feels that it’s a bit of an anachronistic regulation, anyway – it’s really hard to justify clinically or ethically versus other things that we do.” The waiver program he said, is “a regulation barrier whose time should be limited. ... I’m hoping that the waiver disappears soon.”
Prescribing issues will linger beyond any future abolition of the waiver program, since many clinicians will still not be comfortable prescribing medication for MAT of opioid use disorder, said Dr. Barnett. “It’ll be a lot of the same stigma and structural barriers that were in place prior to the waiver.”
Dr. Barnett reported that he has been retained as an expert witness for plaintiffs in lawsuits against opioid manufacturers. The study was partly funded by the National Institutes of Health.
SOURCE: Barnett ML et al. Health Aff. 2019 Jan;38(12):2048-56.
Nurse practitioners and physician assistants, rather than physicians, are the clinicians who have boosted capacity for buprenorphine prescribing in rural America, according to a study in a rural health–focused issue of the journal Health Affairs.
In the face of an ongoing crisis of opioid use disorder, and associated overdoses and deaths that have spared no sector of the U.S. population, the federal government expanded its waiver program for buprenorphine prescribing in 2017. The waiver expansion allows nurse practitioners (NPs) and physician assistants (PAs) – along with clinical nurse specialists, certified registered nurse anesthetists, and certified nurse-midwives – to use the drug for medication-assisted treatment (MAT) for opioid use disorder after completing 24 hours of mandated training; physicians are required to complete 8 hours of training to receive their waiver.
From 2016 to 2019, capacity for MAT in rural areas increased, with the number of clinicians with buprenorphine waivers more than doubling. Of the newly waivered prescribers accounting for this 111% increase, more than half were NPs and PAs.
In many areas, NPs and PAs led the way forward, wrote the study’s lead author Michael L. Barnett, MD, and coauthors, noting in the abstract accompanying the paper that “NPs and PAs accounted for more than half of this increase and were the first waivered clinicians in 285 rural counties with 5.7 million residents.” Overall, the proportion of people living in a county without a waivered clinician has decreased by 36% since NPs and PAs were permitted to obtain waivers.
SAMHSA data identifies trends
In an in-depth interview, Dr. Barnett, an internal medicine physician and health services researcher at the Harvard School of Public Health, Boston, said the issue today is “not so much continuing to dissect the risks and benefits of opioids as a treatment for pain, but more trying to address the current overdose crisis, and the fact that our patient treatment infrastructure is woefully inadequate for the magnitude of the problem that we face.”
Dr. Barnett’s chief intention for this study, he said, was to generate information that will drive policy to implement effective opioid treatment. He’d always been interested in models of care delivery that move beyond seeing just the physician-patient dyad.
“There are a whole range of nonphysician providers that are probably better at providing many different types of care – things that physicians aren’t necessarily that well trained to do,” he said.
Expansion of buprenorphine waivers to NPs and PAs, said Dr. Barnett, presented “a very interesting opportunity to see: How does a nonphysician workforce respond to a new practice opportunity, to really be engaged in areas that many physicians really were neglecting?”
The researchers used information drawn from what Dr. Barnett characterized as a “gold-standard” dataset maintained by the federal Substance Abuse and Mental Health Services Administration. They found that, by March 2019, 52% of U.S. rural residents lived in counties with at least one NP or PA holding a buprenorphine waiver, though there was wide geographic variation: Every county in Maine and New Hampshire had waivered NPs or PAs, but in Tennessee, just 3 of 95 counties had an NP or PA with a waiver.
Scope-of-practice regulations matter
The scope of practice permitted NPs and PAs varies by state, and Dr. Barnett and coauthors also looked to see whether broader scope of practice meant that more advanced practice clinicians were getting buprenorphine waivers. This did appear to be the case: In an analysis that dichotomized scope of practice into “broad” and “restricted,” states with broader practice scope saw twice as many waivered NPs per 100,000 rural residents as those with restrictive practice scope. This association was not seen for PAs, but Dr. Barnett pointed out that PAs are less likely overall to work in primary care.
This, he added, is where scope of practice starts to matter. “A lot of states are still bickering about scope of practice. We show in our paper the clear relationship between scope of practice and the degree to which providers are able to take up these waivers. We can’t prove causality, but I think it’s not a big stretch to think that these policies are playing a big role. I hope we’re working to try to advance that conversation.”
Helping address the unmet need for evidence-based treatment of opioid use disorder, he said, “is one of the more important examples, because doctors have been leaving rural areas in droves. We are lucky that there is a workforce of NPs that still seem to recognize the market opportunity; rural areas still need providers, and they have been willing to fill the gap.”
Waivered NPs or PAs can apply for an expanded waiver, permitting expansion of the buprenorphine panel from 30 to 100 patients after 1 year of holding their initial waiver. Physicians may apply for a waiver to treat up to 275 patients.
Effect on quality of care
The evidence doesn’t support big worries about quality of care, he said. “We don’t have any data on this in the clinical context of addiction, but all of the data that are out there in terms of evaluating the quality of care and level of care being offered by NPs and PAs versus primary care doctors – the types of things that we think of as within the scope of NP and PA practice typically – have shown that they are the same.” Dr. Barnett acknowledged that “there are a little bit of mixed results here and there in one direction or another, but largely, the care being delivered is much more the same than different.”
In addressing the opioid crisis as in the rest of medicine, it’s a mistake not to include this sector of the health care workforce when policies are being crafted, said Dr. Barnett. “People who are making policy and aren’t familiar with the workforce in rural areas could miss the boat. ... NPs aren’t just an asterisk to the workforce – they are an essential part of delivering medicine, just as much as physicians are.”
Dr. Barnett said that, in his estimation, “a lot of protectionist myths get physicians worked up around increased scope of practice for NPs.” However, “The truth is that there’s enough health care spending to go around for everybody and there’s plenty of work to go around.”
Dr. Barnett acknowledged that the current study captured only prescribing capacity, and not actual prescription volume. But, based on some preliminary data, “my sense is that NPs and PAs who acquire waivers are more likely to be prescribing to a larger number of patients proportionately than MDs.” He wasn’t surprised to see this, since the many more hours of training required for NPs and PAs to acquire a waiver means they’re likely to be committed to using the waiver in practice.
Stepping back to look at the bigger picture, Dr. Barnett remarked that, “taking a look at the waiver requirement, a part of me feels that it’s a bit of an anachronistic regulation, anyway – it’s really hard to justify clinically or ethically versus other things that we do.” The waiver program he said, is “a regulation barrier whose time should be limited. ... I’m hoping that the waiver disappears soon.”
Prescribing issues will linger beyond any future abolition of the waiver program, since many clinicians will still not be comfortable prescribing medication for MAT of opioid use disorder, said Dr. Barnett. “It’ll be a lot of the same stigma and structural barriers that were in place prior to the waiver.”
Dr. Barnett reported that he has been retained as an expert witness for plaintiffs in lawsuits against opioid manufacturers. The study was partly funded by the National Institutes of Health.
SOURCE: Barnett ML et al. Health Aff. 2019 Jan;38(12):2048-56.
Nurse practitioners and physician assistants, rather than physicians, are the clinicians who have boosted capacity for buprenorphine prescribing in rural America, according to a study in a rural health–focused issue of the journal Health Affairs.
In the face of an ongoing crisis of opioid use disorder, and associated overdoses and deaths that have spared no sector of the U.S. population, the federal government expanded its waiver program for buprenorphine prescribing in 2017. The waiver expansion allows nurse practitioners (NPs) and physician assistants (PAs) – along with clinical nurse specialists, certified registered nurse anesthetists, and certified nurse-midwives – to use the drug for medication-assisted treatment (MAT) for opioid use disorder after completing 24 hours of mandated training; physicians are required to complete 8 hours of training to receive their waiver.
From 2016 to 2019, capacity for MAT in rural areas increased, with the number of clinicians with buprenorphine waivers more than doubling. Of the newly waivered prescribers accounting for this 111% increase, more than half were NPs and PAs.
In many areas, NPs and PAs led the way forward, wrote the study’s lead author Michael L. Barnett, MD, and coauthors, noting in the abstract accompanying the paper that “NPs and PAs accounted for more than half of this increase and were the first waivered clinicians in 285 rural counties with 5.7 million residents.” Overall, the proportion of people living in a county without a waivered clinician has decreased by 36% since NPs and PAs were permitted to obtain waivers.
SAMHSA data identifies trends
In an in-depth interview, Dr. Barnett, an internal medicine physician and health services researcher at the Harvard School of Public Health, Boston, said the issue today is “not so much continuing to dissect the risks and benefits of opioids as a treatment for pain, but more trying to address the current overdose crisis, and the fact that our patient treatment infrastructure is woefully inadequate for the magnitude of the problem that we face.”
Dr. Barnett’s chief intention for this study, he said, was to generate information that will drive policy to implement effective opioid treatment. He’d always been interested in models of care delivery that move beyond seeing just the physician-patient dyad.
“There are a whole range of nonphysician providers that are probably better at providing many different types of care – things that physicians aren’t necessarily that well trained to do,” he said.
Expansion of buprenorphine waivers to NPs and PAs, said Dr. Barnett, presented “a very interesting opportunity to see: How does a nonphysician workforce respond to a new practice opportunity, to really be engaged in areas that many physicians really were neglecting?”
The researchers used information drawn from what Dr. Barnett characterized as a “gold-standard” dataset maintained by the federal Substance Abuse and Mental Health Services Administration. They found that, by March 2019, 52% of U.S. rural residents lived in counties with at least one NP or PA holding a buprenorphine waiver, though there was wide geographic variation: Every county in Maine and New Hampshire had waivered NPs or PAs, but in Tennessee, just 3 of 95 counties had an NP or PA with a waiver.
Scope-of-practice regulations matter
The scope of practice permitted NPs and PAs varies by state, and Dr. Barnett and coauthors also looked to see whether broader scope of practice meant that more advanced practice clinicians were getting buprenorphine waivers. This did appear to be the case: In an analysis that dichotomized scope of practice into “broad” and “restricted,” states with broader practice scope saw twice as many waivered NPs per 100,000 rural residents as those with restrictive practice scope. This association was not seen for PAs, but Dr. Barnett pointed out that PAs are less likely overall to work in primary care.
This, he added, is where scope of practice starts to matter. “A lot of states are still bickering about scope of practice. We show in our paper the clear relationship between scope of practice and the degree to which providers are able to take up these waivers. We can’t prove causality, but I think it’s not a big stretch to think that these policies are playing a big role. I hope we’re working to try to advance that conversation.”
Helping address the unmet need for evidence-based treatment of opioid use disorder, he said, “is one of the more important examples, because doctors have been leaving rural areas in droves. We are lucky that there is a workforce of NPs that still seem to recognize the market opportunity; rural areas still need providers, and they have been willing to fill the gap.”
Waivered NPs or PAs can apply for an expanded waiver, permitting expansion of the buprenorphine panel from 30 to 100 patients after 1 year of holding their initial waiver. Physicians may apply for a waiver to treat up to 275 patients.
Effect on quality of care
The evidence doesn’t support big worries about quality of care, he said. “We don’t have any data on this in the clinical context of addiction, but all of the data that are out there in terms of evaluating the quality of care and level of care being offered by NPs and PAs versus primary care doctors – the types of things that we think of as within the scope of NP and PA practice typically – have shown that they are the same.” Dr. Barnett acknowledged that “there are a little bit of mixed results here and there in one direction or another, but largely, the care being delivered is much more the same than different.”
In addressing the opioid crisis as in the rest of medicine, it’s a mistake not to include this sector of the health care workforce when policies are being crafted, said Dr. Barnett. “People who are making policy and aren’t familiar with the workforce in rural areas could miss the boat. ... NPs aren’t just an asterisk to the workforce – they are an essential part of delivering medicine, just as much as physicians are.”
Dr. Barnett said that, in his estimation, “a lot of protectionist myths get physicians worked up around increased scope of practice for NPs.” However, “The truth is that there’s enough health care spending to go around for everybody and there’s plenty of work to go around.”
Dr. Barnett acknowledged that the current study captured only prescribing capacity, and not actual prescription volume. But, based on some preliminary data, “my sense is that NPs and PAs who acquire waivers are more likely to be prescribing to a larger number of patients proportionately than MDs.” He wasn’t surprised to see this, since the many more hours of training required for NPs and PAs to acquire a waiver means they’re likely to be committed to using the waiver in practice.
Stepping back to look at the bigger picture, Dr. Barnett remarked that, “taking a look at the waiver requirement, a part of me feels that it’s a bit of an anachronistic regulation, anyway – it’s really hard to justify clinically or ethically versus other things that we do.” The waiver program he said, is “a regulation barrier whose time should be limited. ... I’m hoping that the waiver disappears soon.”
Prescribing issues will linger beyond any future abolition of the waiver program, since many clinicians will still not be comfortable prescribing medication for MAT of opioid use disorder, said Dr. Barnett. “It’ll be a lot of the same stigma and structural barriers that were in place prior to the waiver.”
Dr. Barnett reported that he has been retained as an expert witness for plaintiffs in lawsuits against opioid manufacturers. The study was partly funded by the National Institutes of Health.
SOURCE: Barnett ML et al. Health Aff. 2019 Jan;38(12):2048-56.
FROM HEALTH AFFAIRS
Opioid deaths boost donor heart supply
SNOWMASS, COLO. – The tragic opioid epidemic has “one small bright spot”: an expanding pool of eligible donor hearts for transplantation, Akshay S. Desai, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
For decades, the annual volume of heart transplantations performed in the U.S. was static because of the huge mismatch between donor organ supply and demand. But heart transplant volume has increased steadily in the last few years – a result of the opioid epidemic.
Data from the U.S. Organ Procurement and Transplantation Network show that the proportion of donor hearts obtained from individuals who died from drug intoxication climbed from a mere 1.5% in 1999 to 17.6% in 2017, the most recent year for which data are available. Meanwhile, the size of the heart transplant waiting list, which rose year after year in 2009-2015, has since declined (N Engl J Med. 2019 Feb 7;380[6]:597-9).
“What’s amazing is that, even though these patients might have historically been considered high risk in general, the organs recovered from these patients – and particularly the hearts – don’t seem to be any worse in terms of allograft survival than the organs recovered from patients who died from other causes, which are the traditional sources, like blunt head trauma, gunshot wounds, or stroke, that lead to brain death. In general, these organs are useful and do quite well,” according to Dr. Desai, medical director of the cardiomyopathy and heart failure program at Brigham and Women’s Hospital, Boston.
He highlighted several other recent developments in the field of cardiac transplantation that promise to further expand the donor heart pool, including acceptance of hepatitis C–infected donors and organ donation after circulatory rather than brain death. Dr. Desai also drew attention to the unintended perverse consequences of a recent redesign of the U.S. donor heart allocation system and discussed the impressive improvement in clinical outcomes with mechanical circulatory support. He noted that, while relatively few cardiologists practice in the highly specialized centers where heart transplants take place, virtually all cardiologists are affected by advances in heart transplantation since hundreds of thousands of the estimated 7 million Americans with heart failure have advanced disease.
Heart transplantation, he emphasized, is becoming increasingly complex. Recipients are on average older, sicker, and have more comorbidities than in times past. As a result, there is greater need for dual organ transplants: heart/lung, heart/liver, or heart/kidney. Plus, more patients come to transplantation after prior cardiac surgery for implantation of a ventricular assist device, so sensitization to blood products is a growing issue. And, of course, the pool of transplant candidates has expanded.
“We’re now forced to take patients previously considered to have contraindications to transplant; for example, diabetes was a contraindication to transplant in the early years, but now it’s the rule in 35%-40% of our patients who present with advanced heart failure,” the cardiologist noted.
Transplants from HCV-infected donors to uninfected recipients
Hearts and lungs from donors with hepatitis C viremia were traditionally deemed unsuitable for transplant. That’s all changed in the current era of highly effective direct-acting antiviral agents for the treatment of HCV infection.
In the DONATE HCV trial, Dr. Desai’s colleagues at Brigham and Women’s Hospital showed that giving HCV-uninfected recipients of hearts or lungs from HCV-viremic donors a shortened 4-week course of treatment with sofosbuvir-velpatasvir (Epclusa) beginning within a few hours after transplantation uniformly blocked viral replication. Six months after transplantation, none of the study participants had a detectable HCV viral load, and all had excellent graft function (N Engl J Med. 2019 Apr 25;380[17]:1606-17).
“This is effective prevention of HCV infection by aggressive upfront therapy,” Dr. Desai explained. “We can now take organs from HCV-viremic patients and use them in solid organ transplantation. This has led to a skyrocketing increase in donors with HCV infection, and those donations have helped us clear the waiting list.”
Donation after circulatory death
Australian transplant physicians have pioneered the use of donor hearts obtained after circulatory death in individuals with devastating neurologic injury who didn’t quite meet the criteria for brain death, which is the traditional prerequisite. In the new scenario, withdrawal of life-supporting therapy is followed by circulatory death, then the donor heart is procured and preserved via extracorporeal perfusion until transplantation.
The Australians report excellent outcomes, with rates of overall survival and rejection episodes similar to outcomes from brain-dead donors (J Am Coll Cardiol. 2019 Apr 2;73[12]:1447-59). The first U.S. heart transplant involving donation after circulatory death took place at Duke University in Durham, North Carolina. A multicenter U.S. clinical trial of this practice is underway.
If the results are positive and the practice of donation after circulatory death becomes widely implemented, the U.S. heart donor pool could increase by 30%.
Recent overhaul of donor heart allocation system may have backfired
The U.S. donor heart allocation system was redesigned in the fall of 2018 in an effort to reduce waiting times. One of the biggest changes involved breaking down the category with the highest urgency status into three new subcategories based upon sickness. Now, the highest-urgency category is for patients in cardiogenic shock who are supported by extracorporeal membrane oxygenation (ECMO) or other temporary mechanical circulatory support devices.
But an analysis of United Network for Organ Sharing (UNOS) data suggests this change has unintended adverse consequences for clinical outcomes.
Indeed, the investigators reported that the use of ECMO support is fourfold greater in the new system, the use of durable left ventricular assist devices (LVADs) as a bridge to transplant is down, and outcomes are worse. The 180-day rate of freedom from death or retransplantation was 77.9%, down significantly from 93.4% in the former system. In a multivariate analysis, patients transplanted in the new system had an adjusted 2.1-fold increased risk of death or retransplantation (J Heart Lung Transplant. 2020 Jan;39[1]:1-4).
“When you create a new listing system, you create new incentives, and people start to manage patients differently,” Dr. Desai observed. “Increasingly now, the path direct to transplant is through temporary mechanical circulatory support rather than durable mechanical circulatory support. Is that a good idea? We don’t know, but if you look at the best data, those on ECMO or percutaneous VADs have the worst outcomes. So the question of whether we should take the sickest of sick patients directly to transplant as a standard strategy has come under scrutiny.”
Improved durable LVAD technology brings impressive clinical outcomes
Results of the landmark MOMENTUM 3 randomized trial showed that 2-year clinical outcomes with the magnetically levitated centrifugal-flow HeartMate 3 LVAD now rival those of percutaneous mitral valve repair using the MitraClip device. Two-year all-cause mortality in the LVAD recipients was 22% versus 29.1% with the MitraClip in the COAPT trial and 34.9% in the MITRA-FR trial. The HeartMate 3 reduces the hemocompatibility issues that plagued earlier-generation durable LVADs, with resultant lower rates of pump thrombosis, stroke, and GI bleeding. Indeed, the outcomes in MOMENTUM 3 were so good – and so similar – with the HeartMate 3, regardless of whether the intended treatment goal was as a bridge to transplant or as lifelong destination therapy, that the investigators have recently proposed doing away with those distinctions.
“It is possible that use of arbitrary categorizations based on current or future transplant eligibility should be clinically abandoned in favor of a single preimplant strategy: to extend the survival and improve the quality of life of patients with medically refractory heart failure,” according to the investigators (JAMA Cardiol. 2020 Jan 15. doi: 10.1001/jamacardio.2019.5323).
The next step forward in LVAD technology is already on the horizon: a fully implantable device that eliminates the transcutaneous drive-line for the power supply, which is prone to infection and diminishes overall quality of life. This investigational device utilizes wireless coplanar energy transfer, with a coil ring placed around the lung and fixed to the chest wall. The implanted battery provides more than 6 hours of power without a recharge (J Heart Lung Transplant. 2019 Apr;38[4]:339-43).
“The first LVAD patient has gone swimming in Kazakhstan,” according to Dr. Desai.
Myocardial recovery in LVAD recipients remains elusive
The initial hope for LVADs was that they would not only be able to serve as a bridge to transplantation or as lifetime therapy, but that the prolonged unloading of the ventricle would enable potent medical therapy to rescue myocardial function so that the device could eventually be explanted. That does happen, but only rarely. In a large registry study, myocardial recovery occurred in only about 1% of patients on mechanical circulatory support. Attempts to enhance the process by add-on stem cell therapy have thus far been ineffective.
“For the moment, recovery is still a hope, not a reality,” the cardiologist said.
He reported serving as a consultant to more than a dozen pharmaceutical or medical device companies and receiving research grants from Alnylam, AstraZeneca, Bayer Healthcare, MyoKardia, and Novartis.
SNOWMASS, COLO. – The tragic opioid epidemic has “one small bright spot”: an expanding pool of eligible donor hearts for transplantation, Akshay S. Desai, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
For decades, the annual volume of heart transplantations performed in the U.S. was static because of the huge mismatch between donor organ supply and demand. But heart transplant volume has increased steadily in the last few years – a result of the opioid epidemic.
Data from the U.S. Organ Procurement and Transplantation Network show that the proportion of donor hearts obtained from individuals who died from drug intoxication climbed from a mere 1.5% in 1999 to 17.6% in 2017, the most recent year for which data are available. Meanwhile, the size of the heart transplant waiting list, which rose year after year in 2009-2015, has since declined (N Engl J Med. 2019 Feb 7;380[6]:597-9).
“What’s amazing is that, even though these patients might have historically been considered high risk in general, the organs recovered from these patients – and particularly the hearts – don’t seem to be any worse in terms of allograft survival than the organs recovered from patients who died from other causes, which are the traditional sources, like blunt head trauma, gunshot wounds, or stroke, that lead to brain death. In general, these organs are useful and do quite well,” according to Dr. Desai, medical director of the cardiomyopathy and heart failure program at Brigham and Women’s Hospital, Boston.
He highlighted several other recent developments in the field of cardiac transplantation that promise to further expand the donor heart pool, including acceptance of hepatitis C–infected donors and organ donation after circulatory rather than brain death. Dr. Desai also drew attention to the unintended perverse consequences of a recent redesign of the U.S. donor heart allocation system and discussed the impressive improvement in clinical outcomes with mechanical circulatory support. He noted that, while relatively few cardiologists practice in the highly specialized centers where heart transplants take place, virtually all cardiologists are affected by advances in heart transplantation since hundreds of thousands of the estimated 7 million Americans with heart failure have advanced disease.
Heart transplantation, he emphasized, is becoming increasingly complex. Recipients are on average older, sicker, and have more comorbidities than in times past. As a result, there is greater need for dual organ transplants: heart/lung, heart/liver, or heart/kidney. Plus, more patients come to transplantation after prior cardiac surgery for implantation of a ventricular assist device, so sensitization to blood products is a growing issue. And, of course, the pool of transplant candidates has expanded.
“We’re now forced to take patients previously considered to have contraindications to transplant; for example, diabetes was a contraindication to transplant in the early years, but now it’s the rule in 35%-40% of our patients who present with advanced heart failure,” the cardiologist noted.
Transplants from HCV-infected donors to uninfected recipients
Hearts and lungs from donors with hepatitis C viremia were traditionally deemed unsuitable for transplant. That’s all changed in the current era of highly effective direct-acting antiviral agents for the treatment of HCV infection.
In the DONATE HCV trial, Dr. Desai’s colleagues at Brigham and Women’s Hospital showed that giving HCV-uninfected recipients of hearts or lungs from HCV-viremic donors a shortened 4-week course of treatment with sofosbuvir-velpatasvir (Epclusa) beginning within a few hours after transplantation uniformly blocked viral replication. Six months after transplantation, none of the study participants had a detectable HCV viral load, and all had excellent graft function (N Engl J Med. 2019 Apr 25;380[17]:1606-17).
“This is effective prevention of HCV infection by aggressive upfront therapy,” Dr. Desai explained. “We can now take organs from HCV-viremic patients and use them in solid organ transplantation. This has led to a skyrocketing increase in donors with HCV infection, and those donations have helped us clear the waiting list.”
Donation after circulatory death
Australian transplant physicians have pioneered the use of donor hearts obtained after circulatory death in individuals with devastating neurologic injury who didn’t quite meet the criteria for brain death, which is the traditional prerequisite. In the new scenario, withdrawal of life-supporting therapy is followed by circulatory death, then the donor heart is procured and preserved via extracorporeal perfusion until transplantation.
The Australians report excellent outcomes, with rates of overall survival and rejection episodes similar to outcomes from brain-dead donors (J Am Coll Cardiol. 2019 Apr 2;73[12]:1447-59). The first U.S. heart transplant involving donation after circulatory death took place at Duke University in Durham, North Carolina. A multicenter U.S. clinical trial of this practice is underway.
If the results are positive and the practice of donation after circulatory death becomes widely implemented, the U.S. heart donor pool could increase by 30%.
Recent overhaul of donor heart allocation system may have backfired
The U.S. donor heart allocation system was redesigned in the fall of 2018 in an effort to reduce waiting times. One of the biggest changes involved breaking down the category with the highest urgency status into three new subcategories based upon sickness. Now, the highest-urgency category is for patients in cardiogenic shock who are supported by extracorporeal membrane oxygenation (ECMO) or other temporary mechanical circulatory support devices.
But an analysis of United Network for Organ Sharing (UNOS) data suggests this change has unintended adverse consequences for clinical outcomes.
Indeed, the investigators reported that the use of ECMO support is fourfold greater in the new system, the use of durable left ventricular assist devices (LVADs) as a bridge to transplant is down, and outcomes are worse. The 180-day rate of freedom from death or retransplantation was 77.9%, down significantly from 93.4% in the former system. In a multivariate analysis, patients transplanted in the new system had an adjusted 2.1-fold increased risk of death or retransplantation (J Heart Lung Transplant. 2020 Jan;39[1]:1-4).
“When you create a new listing system, you create new incentives, and people start to manage patients differently,” Dr. Desai observed. “Increasingly now, the path direct to transplant is through temporary mechanical circulatory support rather than durable mechanical circulatory support. Is that a good idea? We don’t know, but if you look at the best data, those on ECMO or percutaneous VADs have the worst outcomes. So the question of whether we should take the sickest of sick patients directly to transplant as a standard strategy has come under scrutiny.”
Improved durable LVAD technology brings impressive clinical outcomes
Results of the landmark MOMENTUM 3 randomized trial showed that 2-year clinical outcomes with the magnetically levitated centrifugal-flow HeartMate 3 LVAD now rival those of percutaneous mitral valve repair using the MitraClip device. Two-year all-cause mortality in the LVAD recipients was 22% versus 29.1% with the MitraClip in the COAPT trial and 34.9% in the MITRA-FR trial. The HeartMate 3 reduces the hemocompatibility issues that plagued earlier-generation durable LVADs, with resultant lower rates of pump thrombosis, stroke, and GI bleeding. Indeed, the outcomes in MOMENTUM 3 were so good – and so similar – with the HeartMate 3, regardless of whether the intended treatment goal was as a bridge to transplant or as lifelong destination therapy, that the investigators have recently proposed doing away with those distinctions.
“It is possible that use of arbitrary categorizations based on current or future transplant eligibility should be clinically abandoned in favor of a single preimplant strategy: to extend the survival and improve the quality of life of patients with medically refractory heart failure,” according to the investigators (JAMA Cardiol. 2020 Jan 15. doi: 10.1001/jamacardio.2019.5323).
The next step forward in LVAD technology is already on the horizon: a fully implantable device that eliminates the transcutaneous drive-line for the power supply, which is prone to infection and diminishes overall quality of life. This investigational device utilizes wireless coplanar energy transfer, with a coil ring placed around the lung and fixed to the chest wall. The implanted battery provides more than 6 hours of power without a recharge (J Heart Lung Transplant. 2019 Apr;38[4]:339-43).
“The first LVAD patient has gone swimming in Kazakhstan,” according to Dr. Desai.
Myocardial recovery in LVAD recipients remains elusive
The initial hope for LVADs was that they would not only be able to serve as a bridge to transplantation or as lifetime therapy, but that the prolonged unloading of the ventricle would enable potent medical therapy to rescue myocardial function so that the device could eventually be explanted. That does happen, but only rarely. In a large registry study, myocardial recovery occurred in only about 1% of patients on mechanical circulatory support. Attempts to enhance the process by add-on stem cell therapy have thus far been ineffective.
“For the moment, recovery is still a hope, not a reality,” the cardiologist said.
He reported serving as a consultant to more than a dozen pharmaceutical or medical device companies and receiving research grants from Alnylam, AstraZeneca, Bayer Healthcare, MyoKardia, and Novartis.
SNOWMASS, COLO. – The tragic opioid epidemic has “one small bright spot”: an expanding pool of eligible donor hearts for transplantation, Akshay S. Desai, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
For decades, the annual volume of heart transplantations performed in the U.S. was static because of the huge mismatch between donor organ supply and demand. But heart transplant volume has increased steadily in the last few years – a result of the opioid epidemic.
Data from the U.S. Organ Procurement and Transplantation Network show that the proportion of donor hearts obtained from individuals who died from drug intoxication climbed from a mere 1.5% in 1999 to 17.6% in 2017, the most recent year for which data are available. Meanwhile, the size of the heart transplant waiting list, which rose year after year in 2009-2015, has since declined (N Engl J Med. 2019 Feb 7;380[6]:597-9).
“What’s amazing is that, even though these patients might have historically been considered high risk in general, the organs recovered from these patients – and particularly the hearts – don’t seem to be any worse in terms of allograft survival than the organs recovered from patients who died from other causes, which are the traditional sources, like blunt head trauma, gunshot wounds, or stroke, that lead to brain death. In general, these organs are useful and do quite well,” according to Dr. Desai, medical director of the cardiomyopathy and heart failure program at Brigham and Women’s Hospital, Boston.
He highlighted several other recent developments in the field of cardiac transplantation that promise to further expand the donor heart pool, including acceptance of hepatitis C–infected donors and organ donation after circulatory rather than brain death. Dr. Desai also drew attention to the unintended perverse consequences of a recent redesign of the U.S. donor heart allocation system and discussed the impressive improvement in clinical outcomes with mechanical circulatory support. He noted that, while relatively few cardiologists practice in the highly specialized centers where heart transplants take place, virtually all cardiologists are affected by advances in heart transplantation since hundreds of thousands of the estimated 7 million Americans with heart failure have advanced disease.
Heart transplantation, he emphasized, is becoming increasingly complex. Recipients are on average older, sicker, and have more comorbidities than in times past. As a result, there is greater need for dual organ transplants: heart/lung, heart/liver, or heart/kidney. Plus, more patients come to transplantation after prior cardiac surgery for implantation of a ventricular assist device, so sensitization to blood products is a growing issue. And, of course, the pool of transplant candidates has expanded.
“We’re now forced to take patients previously considered to have contraindications to transplant; for example, diabetes was a contraindication to transplant in the early years, but now it’s the rule in 35%-40% of our patients who present with advanced heart failure,” the cardiologist noted.
Transplants from HCV-infected donors to uninfected recipients
Hearts and lungs from donors with hepatitis C viremia were traditionally deemed unsuitable for transplant. That’s all changed in the current era of highly effective direct-acting antiviral agents for the treatment of HCV infection.
In the DONATE HCV trial, Dr. Desai’s colleagues at Brigham and Women’s Hospital showed that giving HCV-uninfected recipients of hearts or lungs from HCV-viremic donors a shortened 4-week course of treatment with sofosbuvir-velpatasvir (Epclusa) beginning within a few hours after transplantation uniformly blocked viral replication. Six months after transplantation, none of the study participants had a detectable HCV viral load, and all had excellent graft function (N Engl J Med. 2019 Apr 25;380[17]:1606-17).
“This is effective prevention of HCV infection by aggressive upfront therapy,” Dr. Desai explained. “We can now take organs from HCV-viremic patients and use them in solid organ transplantation. This has led to a skyrocketing increase in donors with HCV infection, and those donations have helped us clear the waiting list.”
Donation after circulatory death
Australian transplant physicians have pioneered the use of donor hearts obtained after circulatory death in individuals with devastating neurologic injury who didn’t quite meet the criteria for brain death, which is the traditional prerequisite. In the new scenario, withdrawal of life-supporting therapy is followed by circulatory death, then the donor heart is procured and preserved via extracorporeal perfusion until transplantation.
The Australians report excellent outcomes, with rates of overall survival and rejection episodes similar to outcomes from brain-dead donors (J Am Coll Cardiol. 2019 Apr 2;73[12]:1447-59). The first U.S. heart transplant involving donation after circulatory death took place at Duke University in Durham, North Carolina. A multicenter U.S. clinical trial of this practice is underway.
If the results are positive and the practice of donation after circulatory death becomes widely implemented, the U.S. heart donor pool could increase by 30%.
Recent overhaul of donor heart allocation system may have backfired
The U.S. donor heart allocation system was redesigned in the fall of 2018 in an effort to reduce waiting times. One of the biggest changes involved breaking down the category with the highest urgency status into three new subcategories based upon sickness. Now, the highest-urgency category is for patients in cardiogenic shock who are supported by extracorporeal membrane oxygenation (ECMO) or other temporary mechanical circulatory support devices.
But an analysis of United Network for Organ Sharing (UNOS) data suggests this change has unintended adverse consequences for clinical outcomes.
Indeed, the investigators reported that the use of ECMO support is fourfold greater in the new system, the use of durable left ventricular assist devices (LVADs) as a bridge to transplant is down, and outcomes are worse. The 180-day rate of freedom from death or retransplantation was 77.9%, down significantly from 93.4% in the former system. In a multivariate analysis, patients transplanted in the new system had an adjusted 2.1-fold increased risk of death or retransplantation (J Heart Lung Transplant. 2020 Jan;39[1]:1-4).
“When you create a new listing system, you create new incentives, and people start to manage patients differently,” Dr. Desai observed. “Increasingly now, the path direct to transplant is through temporary mechanical circulatory support rather than durable mechanical circulatory support. Is that a good idea? We don’t know, but if you look at the best data, those on ECMO or percutaneous VADs have the worst outcomes. So the question of whether we should take the sickest of sick patients directly to transplant as a standard strategy has come under scrutiny.”
Improved durable LVAD technology brings impressive clinical outcomes
Results of the landmark MOMENTUM 3 randomized trial showed that 2-year clinical outcomes with the magnetically levitated centrifugal-flow HeartMate 3 LVAD now rival those of percutaneous mitral valve repair using the MitraClip device. Two-year all-cause mortality in the LVAD recipients was 22% versus 29.1% with the MitraClip in the COAPT trial and 34.9% in the MITRA-FR trial. The HeartMate 3 reduces the hemocompatibility issues that plagued earlier-generation durable LVADs, with resultant lower rates of pump thrombosis, stroke, and GI bleeding. Indeed, the outcomes in MOMENTUM 3 were so good – and so similar – with the HeartMate 3, regardless of whether the intended treatment goal was as a bridge to transplant or as lifelong destination therapy, that the investigators have recently proposed doing away with those distinctions.
“It is possible that use of arbitrary categorizations based on current or future transplant eligibility should be clinically abandoned in favor of a single preimplant strategy: to extend the survival and improve the quality of life of patients with medically refractory heart failure,” according to the investigators (JAMA Cardiol. 2020 Jan 15. doi: 10.1001/jamacardio.2019.5323).
The next step forward in LVAD technology is already on the horizon: a fully implantable device that eliminates the transcutaneous drive-line for the power supply, which is prone to infection and diminishes overall quality of life. This investigational device utilizes wireless coplanar energy transfer, with a coil ring placed around the lung and fixed to the chest wall. The implanted battery provides more than 6 hours of power without a recharge (J Heart Lung Transplant. 2019 Apr;38[4]:339-43).
“The first LVAD patient has gone swimming in Kazakhstan,” according to Dr. Desai.
Myocardial recovery in LVAD recipients remains elusive
The initial hope for LVADs was that they would not only be able to serve as a bridge to transplantation or as lifetime therapy, but that the prolonged unloading of the ventricle would enable potent medical therapy to rescue myocardial function so that the device could eventually be explanted. That does happen, but only rarely. In a large registry study, myocardial recovery occurred in only about 1% of patients on mechanical circulatory support. Attempts to enhance the process by add-on stem cell therapy have thus far been ineffective.
“For the moment, recovery is still a hope, not a reality,” the cardiologist said.
He reported serving as a consultant to more than a dozen pharmaceutical or medical device companies and receiving research grants from Alnylam, AstraZeneca, Bayer Healthcare, MyoKardia, and Novartis.
EXPERT ANALYSIS FROM ACC SNOWMASS 2020
Cannabis use in pregnancy and lactation: A changing landscape
National survey data from 2007-2012 of more than 93,000 pregnant women suggest that around 7% of pregnant respondents reported any cannabis use in the last 2-12 months; of those, 16% reported daily or almost daily use. Among pregnant past-year users in the same survey, 70% perceived slight or no risk of harm from cannabis use 1-2 times a week in pregnancy.1
Data from the Kaiser Northern California health plan involving more than 279,000 pregnancies followed during 2009-2016 suggest that there has been a significant upward trend in use of cannabis during pregnancy, from 4% to 7%, as reported by the mother and/or identified by routine urine screening. The highest prevalence in that study was seen among 18- to 24-year-old pregnant women, increasing from 13% to 22% over the 7-year study period. Importantly, more than 50% of cannabis users in the sample were identified by toxicology screening alone.2,3 Common reasons given for use of cannabis in pregnancy include anxiety, pain, and nausea and vomiting of pregnancy.4
With respect to adverse perinatal outcomes, several case-control studies have examined risks for major birth defects with maternal self-report of cannabis use. Some have noted very modest increased risks for selected major birth defects (odds ratios less than 2); however, data still are very limited.5,6
A number of prospective studies have addressed risks of preterm birth and growth restriction, accounting for mother’s concomitant tobacco use.7-11 Some of these studies have suggested about a twofold to threefold increased risk for preterm delivery and an increased risk for reduced birth weight – particularly with heavier or regular cannabis use – but study findings have not been entirely consistent.
Given its psychoactive properties, there has been high interest in understanding whether there are any short- or long-term neurodevelopmental effects on children prenatally exposed to cannabis. These outcomes have been studied in two small older cohorts in the United States and Canada and one more recent cohort in the Netherlands.12-15 Deficits in several measures of cognition and behavior were noted in follow-up of those children from birth to adulthood. However, it is unclear to what extent these findings may have been influenced by heredity, environment, or other factors.
There have been limitations in almost all studies published to date, including small sample sizes, no biomarker validation of maternal report of dose and gestational timing of cannabis use, and lack of detailed data on common coexposures, such as alcohol, tobacco, and other drugs. In addition, newer studies of pregnancy outcomes in women who use currently available cannabis products are needed, given the substantial increase in the potency of cannabis used today, compared with that of 20 years ago. For example, the tetrahydrocannabinol (THC) concentration in commonly cultivated marijuana plants has increased threefold from 4% to 12% between 1995 and 2014.16
There are very limited data on the presence of cannabis in breast milk and the potential effects of exposure to THC and other metabolites for breastfed infants. However, two recent studies have demonstrated there are low but measurable levels of some cannabis metabolites in breast milk.17-18 Further work is needed to determine if these metabolites accumulate in milk and if at a given dose and age of the breastfed infant, there are any growth, neurodevelopmental, or other clinically important adverse effects.
Related questions, such as potential differences in the effects of exposure during pregnancy or lactation based on the route of administration (edible vs. inhaled) and the use of cannabidiol (CBD) products, have not been studied.
At the present time, the American College of Obstetricians and Gynecologists recommends that women who are pregnant or contemplating pregnancy be encouraged to discontinue marijuana use. With respect to lactation and breastfeeding, ACOG concludes there are insufficient data to evaluate the effects on infants, and in the absence of such data, marijuana use is discouraged. Similarly, the American Academy of Pediatrics recommends women of childbearing age abstain from marijuana use while pregnant or breastfeeding because of potential adverse consequences to the fetus, infant, or child.
In August 2019, the U.S. Surgeon General issued an advisory regarding potential harm to developing brains from the use of marijuana during pregnancy and lactation. The Food and Drug Administration issued a similar statement in October 2019 strongly advising against the use of CBD, THC, and marijuana in any form during pregnancy or while breastfeeding.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is also director of MotherToBaby California, president of the Organization of Teratology Information Specialists, and past president of the Teratology Society.
References
1. Am J Obstet Gynecol. 2015 Aug;213(2):201.e1-10.
2. JAMA. 2017 Dec 26;318(24):2490-1.
3. JAMA. 2017 Jan 10;317(2):207-9.
4. Complement Ther Clin Pract. 2009 Nov;15(4)242-6.
5. Paediatr Perinat Epidemiol. 2014 Sep; 28(5): 424-33.
6. J Toxicol Environ Health A. 2007 Jan;70(1):7-18.
7. Am J Obstet Gynecol. 1983 Aug 15;146(8):992-4.
8. Clin Perinatol. 1991 Mar;18(1):77-91.
9. Am J Epidemiol. 1986 Dec;124(6):986-93.
10. Pediatr Res. 2012 Feb;71(2):215-9.
11. Reprod Toxicol. 2016;62:77-86.
12. Neurotoxicol Teratol. 1987 Jan-Feb;9(1):1-7.
13. Neurotoxicol Teratol. 1994 Mar-Apr;16(2):169-75.
14. Biol Psychiatry. 2016 Jun 15;79(12):971-9.
15. Pharmacol Ther. 2018 Feb;182:133-51.
16. Biol Psychiatry. 2016 Apr 1;79(7):613-9.
17. Obstet Gynecol. 2018 May;131(5):783-8.
18. Pediatrics. 2018 Sep;142(3):e20181076.
National survey data from 2007-2012 of more than 93,000 pregnant women suggest that around 7% of pregnant respondents reported any cannabis use in the last 2-12 months; of those, 16% reported daily or almost daily use. Among pregnant past-year users in the same survey, 70% perceived slight or no risk of harm from cannabis use 1-2 times a week in pregnancy.1
Data from the Kaiser Northern California health plan involving more than 279,000 pregnancies followed during 2009-2016 suggest that there has been a significant upward trend in use of cannabis during pregnancy, from 4% to 7%, as reported by the mother and/or identified by routine urine screening. The highest prevalence in that study was seen among 18- to 24-year-old pregnant women, increasing from 13% to 22% over the 7-year study period. Importantly, more than 50% of cannabis users in the sample were identified by toxicology screening alone.2,3 Common reasons given for use of cannabis in pregnancy include anxiety, pain, and nausea and vomiting of pregnancy.4
With respect to adverse perinatal outcomes, several case-control studies have examined risks for major birth defects with maternal self-report of cannabis use. Some have noted very modest increased risks for selected major birth defects (odds ratios less than 2); however, data still are very limited.5,6
A number of prospective studies have addressed risks of preterm birth and growth restriction, accounting for mother’s concomitant tobacco use.7-11 Some of these studies have suggested about a twofold to threefold increased risk for preterm delivery and an increased risk for reduced birth weight – particularly with heavier or regular cannabis use – but study findings have not been entirely consistent.
Given its psychoactive properties, there has been high interest in understanding whether there are any short- or long-term neurodevelopmental effects on children prenatally exposed to cannabis. These outcomes have been studied in two small older cohorts in the United States and Canada and one more recent cohort in the Netherlands.12-15 Deficits in several measures of cognition and behavior were noted in follow-up of those children from birth to adulthood. However, it is unclear to what extent these findings may have been influenced by heredity, environment, or other factors.
There have been limitations in almost all studies published to date, including small sample sizes, no biomarker validation of maternal report of dose and gestational timing of cannabis use, and lack of detailed data on common coexposures, such as alcohol, tobacco, and other drugs. In addition, newer studies of pregnancy outcomes in women who use currently available cannabis products are needed, given the substantial increase in the potency of cannabis used today, compared with that of 20 years ago. For example, the tetrahydrocannabinol (THC) concentration in commonly cultivated marijuana plants has increased threefold from 4% to 12% between 1995 and 2014.16
There are very limited data on the presence of cannabis in breast milk and the potential effects of exposure to THC and other metabolites for breastfed infants. However, two recent studies have demonstrated there are low but measurable levels of some cannabis metabolites in breast milk.17-18 Further work is needed to determine if these metabolites accumulate in milk and if at a given dose and age of the breastfed infant, there are any growth, neurodevelopmental, or other clinically important adverse effects.
Related questions, such as potential differences in the effects of exposure during pregnancy or lactation based on the route of administration (edible vs. inhaled) and the use of cannabidiol (CBD) products, have not been studied.
At the present time, the American College of Obstetricians and Gynecologists recommends that women who are pregnant or contemplating pregnancy be encouraged to discontinue marijuana use. With respect to lactation and breastfeeding, ACOG concludes there are insufficient data to evaluate the effects on infants, and in the absence of such data, marijuana use is discouraged. Similarly, the American Academy of Pediatrics recommends women of childbearing age abstain from marijuana use while pregnant or breastfeeding because of potential adverse consequences to the fetus, infant, or child.
In August 2019, the U.S. Surgeon General issued an advisory regarding potential harm to developing brains from the use of marijuana during pregnancy and lactation. The Food and Drug Administration issued a similar statement in October 2019 strongly advising against the use of CBD, THC, and marijuana in any form during pregnancy or while breastfeeding.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is also director of MotherToBaby California, president of the Organization of Teratology Information Specialists, and past president of the Teratology Society.
References
1. Am J Obstet Gynecol. 2015 Aug;213(2):201.e1-10.
2. JAMA. 2017 Dec 26;318(24):2490-1.
3. JAMA. 2017 Jan 10;317(2):207-9.
4. Complement Ther Clin Pract. 2009 Nov;15(4)242-6.
5. Paediatr Perinat Epidemiol. 2014 Sep; 28(5): 424-33.
6. J Toxicol Environ Health A. 2007 Jan;70(1):7-18.
7. Am J Obstet Gynecol. 1983 Aug 15;146(8):992-4.
8. Clin Perinatol. 1991 Mar;18(1):77-91.
9. Am J Epidemiol. 1986 Dec;124(6):986-93.
10. Pediatr Res. 2012 Feb;71(2):215-9.
11. Reprod Toxicol. 2016;62:77-86.
12. Neurotoxicol Teratol. 1987 Jan-Feb;9(1):1-7.
13. Neurotoxicol Teratol. 1994 Mar-Apr;16(2):169-75.
14. Biol Psychiatry. 2016 Jun 15;79(12):971-9.
15. Pharmacol Ther. 2018 Feb;182:133-51.
16. Biol Psychiatry. 2016 Apr 1;79(7):613-9.
17. Obstet Gynecol. 2018 May;131(5):783-8.
18. Pediatrics. 2018 Sep;142(3):e20181076.
National survey data from 2007-2012 of more than 93,000 pregnant women suggest that around 7% of pregnant respondents reported any cannabis use in the last 2-12 months; of those, 16% reported daily or almost daily use. Among pregnant past-year users in the same survey, 70% perceived slight or no risk of harm from cannabis use 1-2 times a week in pregnancy.1
Data from the Kaiser Northern California health plan involving more than 279,000 pregnancies followed during 2009-2016 suggest that there has been a significant upward trend in use of cannabis during pregnancy, from 4% to 7%, as reported by the mother and/or identified by routine urine screening. The highest prevalence in that study was seen among 18- to 24-year-old pregnant women, increasing from 13% to 22% over the 7-year study period. Importantly, more than 50% of cannabis users in the sample were identified by toxicology screening alone.2,3 Common reasons given for use of cannabis in pregnancy include anxiety, pain, and nausea and vomiting of pregnancy.4
With respect to adverse perinatal outcomes, several case-control studies have examined risks for major birth defects with maternal self-report of cannabis use. Some have noted very modest increased risks for selected major birth defects (odds ratios less than 2); however, data still are very limited.5,6
A number of prospective studies have addressed risks of preterm birth and growth restriction, accounting for mother’s concomitant tobacco use.7-11 Some of these studies have suggested about a twofold to threefold increased risk for preterm delivery and an increased risk for reduced birth weight – particularly with heavier or regular cannabis use – but study findings have not been entirely consistent.
Given its psychoactive properties, there has been high interest in understanding whether there are any short- or long-term neurodevelopmental effects on children prenatally exposed to cannabis. These outcomes have been studied in two small older cohorts in the United States and Canada and one more recent cohort in the Netherlands.12-15 Deficits in several measures of cognition and behavior were noted in follow-up of those children from birth to adulthood. However, it is unclear to what extent these findings may have been influenced by heredity, environment, or other factors.
There have been limitations in almost all studies published to date, including small sample sizes, no biomarker validation of maternal report of dose and gestational timing of cannabis use, and lack of detailed data on common coexposures, such as alcohol, tobacco, and other drugs. In addition, newer studies of pregnancy outcomes in women who use currently available cannabis products are needed, given the substantial increase in the potency of cannabis used today, compared with that of 20 years ago. For example, the tetrahydrocannabinol (THC) concentration in commonly cultivated marijuana plants has increased threefold from 4% to 12% between 1995 and 2014.16
There are very limited data on the presence of cannabis in breast milk and the potential effects of exposure to THC and other metabolites for breastfed infants. However, two recent studies have demonstrated there are low but measurable levels of some cannabis metabolites in breast milk.17-18 Further work is needed to determine if these metabolites accumulate in milk and if at a given dose and age of the breastfed infant, there are any growth, neurodevelopmental, or other clinically important adverse effects.
Related questions, such as potential differences in the effects of exposure during pregnancy or lactation based on the route of administration (edible vs. inhaled) and the use of cannabidiol (CBD) products, have not been studied.
At the present time, the American College of Obstetricians and Gynecologists recommends that women who are pregnant or contemplating pregnancy be encouraged to discontinue marijuana use. With respect to lactation and breastfeeding, ACOG concludes there are insufficient data to evaluate the effects on infants, and in the absence of such data, marijuana use is discouraged. Similarly, the American Academy of Pediatrics recommends women of childbearing age abstain from marijuana use while pregnant or breastfeeding because of potential adverse consequences to the fetus, infant, or child.
In August 2019, the U.S. Surgeon General issued an advisory regarding potential harm to developing brains from the use of marijuana during pregnancy and lactation. The Food and Drug Administration issued a similar statement in October 2019 strongly advising against the use of CBD, THC, and marijuana in any form during pregnancy or while breastfeeding.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is also director of MotherToBaby California, president of the Organization of Teratology Information Specialists, and past president of the Teratology Society.
References
1. Am J Obstet Gynecol. 2015 Aug;213(2):201.e1-10.
2. JAMA. 2017 Dec 26;318(24):2490-1.
3. JAMA. 2017 Jan 10;317(2):207-9.
4. Complement Ther Clin Pract. 2009 Nov;15(4)242-6.
5. Paediatr Perinat Epidemiol. 2014 Sep; 28(5): 424-33.
6. J Toxicol Environ Health A. 2007 Jan;70(1):7-18.
7. Am J Obstet Gynecol. 1983 Aug 15;146(8):992-4.
8. Clin Perinatol. 1991 Mar;18(1):77-91.
9. Am J Epidemiol. 1986 Dec;124(6):986-93.
10. Pediatr Res. 2012 Feb;71(2):215-9.
11. Reprod Toxicol. 2016;62:77-86.
12. Neurotoxicol Teratol. 1987 Jan-Feb;9(1):1-7.
13. Neurotoxicol Teratol. 1994 Mar-Apr;16(2):169-75.
14. Biol Psychiatry. 2016 Jun 15;79(12):971-9.
15. Pharmacol Ther. 2018 Feb;182:133-51.
16. Biol Psychiatry. 2016 Apr 1;79(7):613-9.
17. Obstet Gynecol. 2018 May;131(5):783-8.
18. Pediatrics. 2018 Sep;142(3):e20181076.
EVALI update warns of chemicals in vaping products
A report issued by the Centers for Disease Control and Prevention confirms that 82% of patients presenting with e-cigarette– or vaping product use–associated lung injury (EVALI) used products containing tetrahydrocannabinol (THC).
Another report published in the CDC’s Morbidity and Mortality Weekly Report assessed cases in which the patients reported using only nicotine-containing vaping products.
“As of Jan. 14, 2020, a total of 2,668 hospitalized EVALI cases had been reported to CDC,” based on data from the National Syndromic Surveillance Program (NSSP), wrote Vikram P. Krishnasamy, MD, of the National Center for Injury Prevention and Control at the CDC, Atlanta, and colleagues. Cases have occurred in all 50 states, the District of Columbia, the U.S. Virgin Islands, and Puerto Rico. The age of the patients ranged from 13 to 85 years, with an average age of 24 years; 66% were male, and 73% were non-Hispanic white.
In addition, 57% of the patients reported using any nicotine-containing product, and 14% of these reported use of nicotine products exclusively.
Previous studies have shown that vitamin E acetate is associated with the EVALI outbreak, which peaked during the week of Sept. 15, 2019, with 215 reported hospital admissions, Dr. Krishnasamy and associates noted. “However, evidence is not sufficient to rule out the contribution of other chemicals of concern, including chemicals in either THC- or non-THC–containing products, in some reported EVALI cases,” they said.
The study findings were limited by several factors, including incomplete data on product use, increased reporting of vaping product use at emergency department visits after increased public awareness of risk, and inconsistency in the health care facilities contributing data via the NSSP, the researchers wrote.
The decline in EVALI cases since September 2019 may be related to factors including the rapid public health response to increase awareness of the risks of vaping, and the possible removal of vitamin E acetate as a diluent in THC-containing products, but clinicians and public health professionals should remain on alert for new EVALI cases and continue to discourage the use of THC-containing e-cigarette or vaping products, Dr. Krishnasamy and associates concluded.
Nicotine-only vaping products
In a second report published in MMWR, Isaac Ghinai, MBBS, of the Illinois Department of Public Health and CDC researchers examined characteristics of EVALI patients in Illinois who reported using only nicotine-containing vaping products.
A total of 9 of 121 (7%) EVALI patients surveyed in Illinois reported no indication of THC use. These patients were more likely than those who reported any use of THC-containing products to be female (78% vs. 25%) and aged 45 years and older (33% vs. 2%); P less than .01 in both cases.
In addition, EVALI patients with no indication of THC-containing product use were less likely than THC product users to present with constitutional symptoms (56% vs. 96%) or initial leukocytosis (38% vs. 91%), or to have previously visited an outpatient provider or ED before being hospitalized (25% vs. 80%).
Other presenting characteristics including initial vital signs and lab results, as well as the frequency of severe outcomes such as death or respiratory failure, were not significantly different between users and nonusers of THC-containing vaping products.
The study findings were limited by factors including the use of self-reports, the small sample size, and lack of initial and follow-up interviews for all EVALI patients, the researchers noted. However, the results support the CDC’s recommendation that “persons should not use THC-containing e-cigarette, or vaping, products, particularly those obtained from informal sources such as friends, family members, or from in-person or online dealers,” and should not add vitamin E acetate or other substances to these products, they said.
In addition, users of nicotine-containing e-cigarette or vaping products as an alternative to cigarettes should not return to cigarettes, but should explore other options to help them quit, Dr. Ghinai, and associates said.
The studies were supported by the CDC. The researchers in both studies had no financial conflicts to disclose.
SOURCES: Krishnasamy VP et al. MMWR Morb Mortal Wkly Rep. 17 Jan 2020. doi: 10.15585/mmwr.mm6903e2; Ghinai I et al. MMWR Morb Mortal Wkly Rep. 17 Jan 2020. doi: 10.15585/mmwr.mm6903e1.
A report issued by the Centers for Disease Control and Prevention confirms that 82% of patients presenting with e-cigarette– or vaping product use–associated lung injury (EVALI) used products containing tetrahydrocannabinol (THC).
Another report published in the CDC’s Morbidity and Mortality Weekly Report assessed cases in which the patients reported using only nicotine-containing vaping products.
“As of Jan. 14, 2020, a total of 2,668 hospitalized EVALI cases had been reported to CDC,” based on data from the National Syndromic Surveillance Program (NSSP), wrote Vikram P. Krishnasamy, MD, of the National Center for Injury Prevention and Control at the CDC, Atlanta, and colleagues. Cases have occurred in all 50 states, the District of Columbia, the U.S. Virgin Islands, and Puerto Rico. The age of the patients ranged from 13 to 85 years, with an average age of 24 years; 66% were male, and 73% were non-Hispanic white.
In addition, 57% of the patients reported using any nicotine-containing product, and 14% of these reported use of nicotine products exclusively.
Previous studies have shown that vitamin E acetate is associated with the EVALI outbreak, which peaked during the week of Sept. 15, 2019, with 215 reported hospital admissions, Dr. Krishnasamy and associates noted. “However, evidence is not sufficient to rule out the contribution of other chemicals of concern, including chemicals in either THC- or non-THC–containing products, in some reported EVALI cases,” they said.
The study findings were limited by several factors, including incomplete data on product use, increased reporting of vaping product use at emergency department visits after increased public awareness of risk, and inconsistency in the health care facilities contributing data via the NSSP, the researchers wrote.
The decline in EVALI cases since September 2019 may be related to factors including the rapid public health response to increase awareness of the risks of vaping, and the possible removal of vitamin E acetate as a diluent in THC-containing products, but clinicians and public health professionals should remain on alert for new EVALI cases and continue to discourage the use of THC-containing e-cigarette or vaping products, Dr. Krishnasamy and associates concluded.
Nicotine-only vaping products
In a second report published in MMWR, Isaac Ghinai, MBBS, of the Illinois Department of Public Health and CDC researchers examined characteristics of EVALI patients in Illinois who reported using only nicotine-containing vaping products.
A total of 9 of 121 (7%) EVALI patients surveyed in Illinois reported no indication of THC use. These patients were more likely than those who reported any use of THC-containing products to be female (78% vs. 25%) and aged 45 years and older (33% vs. 2%); P less than .01 in both cases.
In addition, EVALI patients with no indication of THC-containing product use were less likely than THC product users to present with constitutional symptoms (56% vs. 96%) or initial leukocytosis (38% vs. 91%), or to have previously visited an outpatient provider or ED before being hospitalized (25% vs. 80%).
Other presenting characteristics including initial vital signs and lab results, as well as the frequency of severe outcomes such as death or respiratory failure, were not significantly different between users and nonusers of THC-containing vaping products.
The study findings were limited by factors including the use of self-reports, the small sample size, and lack of initial and follow-up interviews for all EVALI patients, the researchers noted. However, the results support the CDC’s recommendation that “persons should not use THC-containing e-cigarette, or vaping, products, particularly those obtained from informal sources such as friends, family members, or from in-person or online dealers,” and should not add vitamin E acetate or other substances to these products, they said.
In addition, users of nicotine-containing e-cigarette or vaping products as an alternative to cigarettes should not return to cigarettes, but should explore other options to help them quit, Dr. Ghinai, and associates said.
The studies were supported by the CDC. The researchers in both studies had no financial conflicts to disclose.
SOURCES: Krishnasamy VP et al. MMWR Morb Mortal Wkly Rep. 17 Jan 2020. doi: 10.15585/mmwr.mm6903e2; Ghinai I et al. MMWR Morb Mortal Wkly Rep. 17 Jan 2020. doi: 10.15585/mmwr.mm6903e1.
A report issued by the Centers for Disease Control and Prevention confirms that 82% of patients presenting with e-cigarette– or vaping product use–associated lung injury (EVALI) used products containing tetrahydrocannabinol (THC).
Another report published in the CDC’s Morbidity and Mortality Weekly Report assessed cases in which the patients reported using only nicotine-containing vaping products.
“As of Jan. 14, 2020, a total of 2,668 hospitalized EVALI cases had been reported to CDC,” based on data from the National Syndromic Surveillance Program (NSSP), wrote Vikram P. Krishnasamy, MD, of the National Center for Injury Prevention and Control at the CDC, Atlanta, and colleagues. Cases have occurred in all 50 states, the District of Columbia, the U.S. Virgin Islands, and Puerto Rico. The age of the patients ranged from 13 to 85 years, with an average age of 24 years; 66% were male, and 73% were non-Hispanic white.
In addition, 57% of the patients reported using any nicotine-containing product, and 14% of these reported use of nicotine products exclusively.
Previous studies have shown that vitamin E acetate is associated with the EVALI outbreak, which peaked during the week of Sept. 15, 2019, with 215 reported hospital admissions, Dr. Krishnasamy and associates noted. “However, evidence is not sufficient to rule out the contribution of other chemicals of concern, including chemicals in either THC- or non-THC–containing products, in some reported EVALI cases,” they said.
The study findings were limited by several factors, including incomplete data on product use, increased reporting of vaping product use at emergency department visits after increased public awareness of risk, and inconsistency in the health care facilities contributing data via the NSSP, the researchers wrote.
The decline in EVALI cases since September 2019 may be related to factors including the rapid public health response to increase awareness of the risks of vaping, and the possible removal of vitamin E acetate as a diluent in THC-containing products, but clinicians and public health professionals should remain on alert for new EVALI cases and continue to discourage the use of THC-containing e-cigarette or vaping products, Dr. Krishnasamy and associates concluded.
Nicotine-only vaping products
In a second report published in MMWR, Isaac Ghinai, MBBS, of the Illinois Department of Public Health and CDC researchers examined characteristics of EVALI patients in Illinois who reported using only nicotine-containing vaping products.
A total of 9 of 121 (7%) EVALI patients surveyed in Illinois reported no indication of THC use. These patients were more likely than those who reported any use of THC-containing products to be female (78% vs. 25%) and aged 45 years and older (33% vs. 2%); P less than .01 in both cases.
In addition, EVALI patients with no indication of THC-containing product use were less likely than THC product users to present with constitutional symptoms (56% vs. 96%) or initial leukocytosis (38% vs. 91%), or to have previously visited an outpatient provider or ED before being hospitalized (25% vs. 80%).
Other presenting characteristics including initial vital signs and lab results, as well as the frequency of severe outcomes such as death or respiratory failure, were not significantly different between users and nonusers of THC-containing vaping products.
The study findings were limited by factors including the use of self-reports, the small sample size, and lack of initial and follow-up interviews for all EVALI patients, the researchers noted. However, the results support the CDC’s recommendation that “persons should not use THC-containing e-cigarette, or vaping, products, particularly those obtained from informal sources such as friends, family members, or from in-person or online dealers,” and should not add vitamin E acetate or other substances to these products, they said.
In addition, users of nicotine-containing e-cigarette or vaping products as an alternative to cigarettes should not return to cigarettes, but should explore other options to help them quit, Dr. Ghinai, and associates said.
The studies were supported by the CDC. The researchers in both studies had no financial conflicts to disclose.
SOURCES: Krishnasamy VP et al. MMWR Morb Mortal Wkly Rep. 17 Jan 2020. doi: 10.15585/mmwr.mm6903e2; Ghinai I et al. MMWR Morb Mortal Wkly Rep. 17 Jan 2020. doi: 10.15585/mmwr.mm6903e1.
FROM MMWR
Surgeon General scolds docs for failing to help patients quit smoking
The U.S. Surgeon General is calling on all physicians to help patients stop smoking, noting that two-thirds of adult smokers say they want to quit, but only 40% report that their doctor has advised them to stop.
“I’ve got to own this as the nation’s doctor, and our health providers in this room and in this country need to own this stat,” said Surgeon General Jerome Adams, MD, at a press briefing releasing a new report on smoking cessation.
“Smoking is the No. 1 preventable cause of death, disease, and disability in the United States,” he said. “So why are 40% of our health providers out there not advising smokers to quit when they come in?”
In the first U.S. Surgeon General report on smoking cessation in 30 years, the 700-page report suggests smoking cessation-related quality measures that include physician reimbursement would increase treatment.
The evidence also suggests that using electronic health records to prompt clinicians to inquire about smoking would increase cessation treatment.
EHRs could be used to “empower and enable” physicians to advise people to quit, said Dr. Adams. Physicians also need “the education and the confidence to be able to have that conversation, because too many of them look at someone and say: ‘Nope, too hard, too much effort, no, that’s not what they’re here for today,’ ” he said.
However, “simply asking, advising, and referring can be enough to get someone on the pathway to quitting,” Dr. Adams said.
34 million still smoke
The new report is the first on the topic released since 1990, and the 34th on tobacco control since the first one was issued in 1964, said Dr. Adams. Since that first report, adult smoking has declined 70%, but some 34 million Americans (14%) still smoke, he said.
In addition, Dr. Adams said that many subpopulations have been left behind, noting: “Cigarette smoking remains highest among LGBTQ adults, people with disabilities or limitations, American Indians and Alaska Natives, and people with mental health conditions or substance use disorders.”
He also noted that 40% of cigarettes are consumed by those with a mental illness or a substance use disorder.
Quitting is beneficial at any age and can add as much as a decade to life expectancy, the report notes. Quitting also reduces the risk of 12 cancers, cuts the risk of chronic obstructive pulmonary disease, and reduces cardiovascular and stroke morbidity and mortality.
Pregnant women who quit also reduce their own morbidity and mortality risk and that of unborn children and infants, the report says.
“We know more about the science of quitting than ever before. We can, and must, do more to ensure that evidence-based cessation treatments are reaching the people that need them,” said Dr. Adams.
Less than one-third of those who have quit have used Food and Drug Administration–approved cessation medications or behavioral counseling, Dr. Adams said.
Barriers to care
Despite the existence of five nicotine replacement therapies and two nonnicotine oral medications, and more widespread availability of proven counseling methods – including web- or text-based programs – barriers to access remain.
These include a lack of insurance coverage for comprehensive, evidence-based smoking cessation treatment, which, when offered, increases availability and use.
“These are cost-effective interventions,” said Dr. Adams. “It’s penny wise and pound foolish to not give someone access to what we know works,” he said.
Because of the diversity of e-cigarette products and the variety of ways they are used, coupled with little research, it’s not currently possible to determine whether they are, or are not, useful smoking cessation tools, the report notes.
However, experts who compiled the report found some evidence to suggest that e-cigarettes containing nicotine may be “associated with increased smoking cessation compared with the use of e-cigarettes not containing nicotine.”
Asked whether the report’s conclusions might be interpreted as supportive of e-cigarettes, Dr. Adams said the report focused on smoking cessation, not initiation.
“I’m terribly concerned about the clear data that shows youth are initiating tobacco product use with e-cigarettes,” he said.
The Trump administration’s current proposal to partially restrict sales of some flavored e-cigarettes “reflects the science,” and “a balance between a desire to really make sure that people aren’t initiating with these products, but also a desire to again try to maintain a pathway for adults who want to use these products to quit to use them,” Dr. Adams said.
The focus, said Dr. Adams, should not be on e-cigarettes and whether they do, or do not, work.
“People want to quit,” he said. “We know what works. Not enough of them are getting it, and there are terrible disparities in who is and who is not getting access to effective and evidence-based treatment – that’s the story here.”
This article first appeared on Medscape.com.
The U.S. Surgeon General is calling on all physicians to help patients stop smoking, noting that two-thirds of adult smokers say they want to quit, but only 40% report that their doctor has advised them to stop.
“I’ve got to own this as the nation’s doctor, and our health providers in this room and in this country need to own this stat,” said Surgeon General Jerome Adams, MD, at a press briefing releasing a new report on smoking cessation.
“Smoking is the No. 1 preventable cause of death, disease, and disability in the United States,” he said. “So why are 40% of our health providers out there not advising smokers to quit when they come in?”
In the first U.S. Surgeon General report on smoking cessation in 30 years, the 700-page report suggests smoking cessation-related quality measures that include physician reimbursement would increase treatment.
The evidence also suggests that using electronic health records to prompt clinicians to inquire about smoking would increase cessation treatment.
EHRs could be used to “empower and enable” physicians to advise people to quit, said Dr. Adams. Physicians also need “the education and the confidence to be able to have that conversation, because too many of them look at someone and say: ‘Nope, too hard, too much effort, no, that’s not what they’re here for today,’ ” he said.
However, “simply asking, advising, and referring can be enough to get someone on the pathway to quitting,” Dr. Adams said.
34 million still smoke
The new report is the first on the topic released since 1990, and the 34th on tobacco control since the first one was issued in 1964, said Dr. Adams. Since that first report, adult smoking has declined 70%, but some 34 million Americans (14%) still smoke, he said.
In addition, Dr. Adams said that many subpopulations have been left behind, noting: “Cigarette smoking remains highest among LGBTQ adults, people with disabilities or limitations, American Indians and Alaska Natives, and people with mental health conditions or substance use disorders.”
He also noted that 40% of cigarettes are consumed by those with a mental illness or a substance use disorder.
Quitting is beneficial at any age and can add as much as a decade to life expectancy, the report notes. Quitting also reduces the risk of 12 cancers, cuts the risk of chronic obstructive pulmonary disease, and reduces cardiovascular and stroke morbidity and mortality.
Pregnant women who quit also reduce their own morbidity and mortality risk and that of unborn children and infants, the report says.
“We know more about the science of quitting than ever before. We can, and must, do more to ensure that evidence-based cessation treatments are reaching the people that need them,” said Dr. Adams.
Less than one-third of those who have quit have used Food and Drug Administration–approved cessation medications or behavioral counseling, Dr. Adams said.
Barriers to care
Despite the existence of five nicotine replacement therapies and two nonnicotine oral medications, and more widespread availability of proven counseling methods – including web- or text-based programs – barriers to access remain.
These include a lack of insurance coverage for comprehensive, evidence-based smoking cessation treatment, which, when offered, increases availability and use.
“These are cost-effective interventions,” said Dr. Adams. “It’s penny wise and pound foolish to not give someone access to what we know works,” he said.
Because of the diversity of e-cigarette products and the variety of ways they are used, coupled with little research, it’s not currently possible to determine whether they are, or are not, useful smoking cessation tools, the report notes.
However, experts who compiled the report found some evidence to suggest that e-cigarettes containing nicotine may be “associated with increased smoking cessation compared with the use of e-cigarettes not containing nicotine.”
Asked whether the report’s conclusions might be interpreted as supportive of e-cigarettes, Dr. Adams said the report focused on smoking cessation, not initiation.
“I’m terribly concerned about the clear data that shows youth are initiating tobacco product use with e-cigarettes,” he said.
The Trump administration’s current proposal to partially restrict sales of some flavored e-cigarettes “reflects the science,” and “a balance between a desire to really make sure that people aren’t initiating with these products, but also a desire to again try to maintain a pathway for adults who want to use these products to quit to use them,” Dr. Adams said.
The focus, said Dr. Adams, should not be on e-cigarettes and whether they do, or do not, work.
“People want to quit,” he said. “We know what works. Not enough of them are getting it, and there are terrible disparities in who is and who is not getting access to effective and evidence-based treatment – that’s the story here.”
This article first appeared on Medscape.com.
The U.S. Surgeon General is calling on all physicians to help patients stop smoking, noting that two-thirds of adult smokers say they want to quit, but only 40% report that their doctor has advised them to stop.
“I’ve got to own this as the nation’s doctor, and our health providers in this room and in this country need to own this stat,” said Surgeon General Jerome Adams, MD, at a press briefing releasing a new report on smoking cessation.
“Smoking is the No. 1 preventable cause of death, disease, and disability in the United States,” he said. “So why are 40% of our health providers out there not advising smokers to quit when they come in?”
In the first U.S. Surgeon General report on smoking cessation in 30 years, the 700-page report suggests smoking cessation-related quality measures that include physician reimbursement would increase treatment.
The evidence also suggests that using electronic health records to prompt clinicians to inquire about smoking would increase cessation treatment.
EHRs could be used to “empower and enable” physicians to advise people to quit, said Dr. Adams. Physicians also need “the education and the confidence to be able to have that conversation, because too many of them look at someone and say: ‘Nope, too hard, too much effort, no, that’s not what they’re here for today,’ ” he said.
However, “simply asking, advising, and referring can be enough to get someone on the pathway to quitting,” Dr. Adams said.
34 million still smoke
The new report is the first on the topic released since 1990, and the 34th on tobacco control since the first one was issued in 1964, said Dr. Adams. Since that first report, adult smoking has declined 70%, but some 34 million Americans (14%) still smoke, he said.
In addition, Dr. Adams said that many subpopulations have been left behind, noting: “Cigarette smoking remains highest among LGBTQ adults, people with disabilities or limitations, American Indians and Alaska Natives, and people with mental health conditions or substance use disorders.”
He also noted that 40% of cigarettes are consumed by those with a mental illness or a substance use disorder.
Quitting is beneficial at any age and can add as much as a decade to life expectancy, the report notes. Quitting also reduces the risk of 12 cancers, cuts the risk of chronic obstructive pulmonary disease, and reduces cardiovascular and stroke morbidity and mortality.
Pregnant women who quit also reduce their own morbidity and mortality risk and that of unborn children and infants, the report says.
“We know more about the science of quitting than ever before. We can, and must, do more to ensure that evidence-based cessation treatments are reaching the people that need them,” said Dr. Adams.
Less than one-third of those who have quit have used Food and Drug Administration–approved cessation medications or behavioral counseling, Dr. Adams said.
Barriers to care
Despite the existence of five nicotine replacement therapies and two nonnicotine oral medications, and more widespread availability of proven counseling methods – including web- or text-based programs – barriers to access remain.
These include a lack of insurance coverage for comprehensive, evidence-based smoking cessation treatment, which, when offered, increases availability and use.
“These are cost-effective interventions,” said Dr. Adams. “It’s penny wise and pound foolish to not give someone access to what we know works,” he said.
Because of the diversity of e-cigarette products and the variety of ways they are used, coupled with little research, it’s not currently possible to determine whether they are, or are not, useful smoking cessation tools, the report notes.
However, experts who compiled the report found some evidence to suggest that e-cigarettes containing nicotine may be “associated with increased smoking cessation compared with the use of e-cigarettes not containing nicotine.”
Asked whether the report’s conclusions might be interpreted as supportive of e-cigarettes, Dr. Adams said the report focused on smoking cessation, not initiation.
“I’m terribly concerned about the clear data that shows youth are initiating tobacco product use with e-cigarettes,” he said.
The Trump administration’s current proposal to partially restrict sales of some flavored e-cigarettes “reflects the science,” and “a balance between a desire to really make sure that people aren’t initiating with these products, but also a desire to again try to maintain a pathway for adults who want to use these products to quit to use them,” Dr. Adams said.
The focus, said Dr. Adams, should not be on e-cigarettes and whether they do, or do not, work.
“People want to quit,” he said. “We know what works. Not enough of them are getting it, and there are terrible disparities in who is and who is not getting access to effective and evidence-based treatment – that’s the story here.”
This article first appeared on Medscape.com.
The suicide wars
Topic of suicide prevention causing divisions within psychiatry
At every swipe through my social media feeds, I’m greeted with another topic that has advocates clustered at the extremes. People align, and they align quickly in our strangely polarized world in which anyone who might sit in the middle lies low.
It seems we’re divided: On the left you are a CNN fan or you’re one of those soulless monsters who tunes in to Fox News. You’re pro-life or you’re a baby killer, advocating for late-term abortions or even the execution of live infants. When it comes to firearm regulation, one side says you’re a threat to the Constitution, while the other says that those opposed are responsible for the death of every person who was ever the victim of a discharged firearm. And those who feel strongly about a given topic often justify their attacks on those who disagree. Psychiatry is no stranger to this thinking, and we are the only medical specialty with organized “antipsychiatry” groups who oppose our work. I have been a bit surprised, however, that the topic of suicide prevention is one that has us divided within our own specialty.
Amy Barnhorst, MD, is a psychiatrist at the University of California, Davis, and the author of “The empty promise of suicide prevention: Many of the problems that lead people to kill themselves cannot be fixed with a little serotonin,” an op-ed piece that appeared in the New York Times on April 26, 2019. Dr. Barnhorst began her essay with the story of a patient who was hospitalized after a relative realized she was planning her suicide. That story had an ending that psychiatrists relish: A person with previously unrecognized and untreated bipolar disorder received care, including medication, and got better. This suicide was preventable, a life was saved, and this story followed a model we all hope is being replicated over and over.
Dr. Barnhorst went on to say that this was an outlier in her career, that most of the suicidal patients she sees are impoverished, homeless, addicted, and she wrote about how little the treatment setting has to offer: The idea that a pill would fix these problems is almost laughable. She suggests that there is more to suicide prevention than identifying prospective patients and getting them acute psychiatric care.
The decision to stop living is one that people arrive at by different paths, some over months, but many in a matter of minutes. Those people won’t be intercepted by the mental health system. We certainly need more psychiatric services and more research into better, faster-acting treatments for severe depression and suicidal thoughts, but that will never be enough.
We need to address the root causes of our nation’s suicide problem – poverty, homelessness, and the accompanying exposure to trauma, crime, and drugs. That means better alcohol and drug treatment, family counseling, low-income housing resources, job training, and individual therapy. And for those at risk who still slip past all the checkpoints, we need to make sure they don’t have access to guns and lethal medications.
Psychological autopsies done after suicides have indicated that more than 90% of people who die from suicide suffered from a mental illness, yet 54% of those who ended their own lives had never received a psychiatric diagnosis. There is a hopefulness that, if only we had more – more services, more therapy, more medication – then we could prevent suicide. Unfortunately, this line of thinking, with a “Zero Suicide” initiative, points a finger at those who survive: Suicide is preventable, so someone is to blame, if not a family member for missing the warning signs then the clinician who offered treatment that wasn’t good enough.
Along this line, the New York Times printed another opinion piece on Jan. 6 by Richard A. Friedman, MD, titled, “Why are young Americans killing themselves?” Dr. Friedman’s conclusion was more along the psychiatrist party line: “The good news is that we don’t have to wait for all the answers to know what to do. We know that various psychotherapies and medication are highly effective in treating depression. We just need to do a better job of identifying, reaching out to and providing resources for at-risk youths.”
Dr. Friedman goes on to propose universal screening at school, among other measures to identify those at risk. It is no surprise that Dr. Friedman’s article had more than 1,700 comments before commenting was closed by the Times. I have written about the pros and cons of screening adolescents for depression in a primary care setting, so putting the responsibility of identifying suicidal teenagers on school teachers seems like an ominous responsibility to add to a teacher’s obligations.
I did not read Dr. Barnhorst’s earlier op-ed piece as a condemnation of psychiatric care, but rather as a call to action and a reality check on the idea that psychiatry is the only answer to our suicide epidemic. More people than ever get treatment – from psychiatrists, from primary care doctors, from nonphysician prescribing clinicians, and from so many varieties of psychotherapists, and yet our suicide rates continue to rise.
In a post on the Psychology Today website, Sara Gorman, PhD, and Jack M. Gorman, MD, discussed Dr. Barnhorst’s article. “In the process of making her point, Barnhorst also manages to seriously trivialize the role of antidepressant medication in the treatment of depression and to imply that, given societal woes, there isn’t much we can do to try to prevent suicides – aside from limiting access to lethal means,” they wrote.
The Gormans were not alone in their objections; the day after the op-ed appeared in the New York Times, a well-respected psychiatry department chairman took on not just the content of the op-ed, but also the author, in his Twitter feed. He wrote, “@amybarnhorst doesn’t read scientific literature or skipped training. this article is wrong. #suicide is largely preventable, if proper measures taken n Rx provided. @nytimes please vet authors better @APAPsychiatric.” Dr. Barnhorst, also a voice on Twitter, added the wry response, “I skipped training.” When Twitter users responded that initial Twitter comment conveyed a lack of civility toward a colleague, the original Tweeter – I’m withholding his name with the hope that even writing about these interactions won’t put me on anyone’s enemy list – like many others sitting on the poles of these contentious topics, responded with the following, “All for civility except in the case of misinformation that puts lives at risk, especially when purveyed by a professional who wears the patina of credibility.”
If it’s not yet obvious, I don’t believe there is a simple answer to our suicide problem, nor do I think it puts lives at risk to point out that, so far, our treatments have not lowered suicide rates. The issue is complex and we have no perfect explanation as to why countries differ so greatly with regard to suicide. There are impoverished, war-torn countries with remarkably lower suicide rates, and nations with much stricter gun laws that have higher statistics. Honduras, deemed “the murder capital of the world,” has an enviable suicide rate of only 2.9 per 100,000.
If the solution were as simple as making medications more accessible, the answer might be an easy one (or at least worth trying) – make antidepressants available over-the-counter, a move that would both increase access and decrease stigma.
Some people are determined to end their own lives. They aren’t looking to see psychiatrists or to call hotlines, and they may well resort to an alternate method if any given one is not readily available. For these individuals, suicide may not be preventable, and we may be left to say that this tragic phenomena with its diverse causes should also lead us to explore the root causes of human misery and our cultural features that lead some people to end their own lives while others endure.
Clearly, there are those who have untreated psychiatric illnesses and who make impulsive and lethal decisions – access to care and means restrictions certainly save some lives. And while it is obvious to us as psychiatrists that anyone who is depressed or is having suicidal thoughts is deserving of a psychiatric evaluation and intervention, the truth remains that access to treatment in this country is limited by finances, by the availability of mental health professionals, and by stigma and shame. In the end, The one thing I am certain of is that our efforts to prevent suicide should unite, and not fracture, our profession.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Topic of suicide prevention causing divisions within psychiatry
Topic of suicide prevention causing divisions within psychiatry
At every swipe through my social media feeds, I’m greeted with another topic that has advocates clustered at the extremes. People align, and they align quickly in our strangely polarized world in which anyone who might sit in the middle lies low.
It seems we’re divided: On the left you are a CNN fan or you’re one of those soulless monsters who tunes in to Fox News. You’re pro-life or you’re a baby killer, advocating for late-term abortions or even the execution of live infants. When it comes to firearm regulation, one side says you’re a threat to the Constitution, while the other says that those opposed are responsible for the death of every person who was ever the victim of a discharged firearm. And those who feel strongly about a given topic often justify their attacks on those who disagree. Psychiatry is no stranger to this thinking, and we are the only medical specialty with organized “antipsychiatry” groups who oppose our work. I have been a bit surprised, however, that the topic of suicide prevention is one that has us divided within our own specialty.
Amy Barnhorst, MD, is a psychiatrist at the University of California, Davis, and the author of “The empty promise of suicide prevention: Many of the problems that lead people to kill themselves cannot be fixed with a little serotonin,” an op-ed piece that appeared in the New York Times on April 26, 2019. Dr. Barnhorst began her essay with the story of a patient who was hospitalized after a relative realized she was planning her suicide. That story had an ending that psychiatrists relish: A person with previously unrecognized and untreated bipolar disorder received care, including medication, and got better. This suicide was preventable, a life was saved, and this story followed a model we all hope is being replicated over and over.
Dr. Barnhorst went on to say that this was an outlier in her career, that most of the suicidal patients she sees are impoverished, homeless, addicted, and she wrote about how little the treatment setting has to offer: The idea that a pill would fix these problems is almost laughable. She suggests that there is more to suicide prevention than identifying prospective patients and getting them acute psychiatric care.
The decision to stop living is one that people arrive at by different paths, some over months, but many in a matter of minutes. Those people won’t be intercepted by the mental health system. We certainly need more psychiatric services and more research into better, faster-acting treatments for severe depression and suicidal thoughts, but that will never be enough.
We need to address the root causes of our nation’s suicide problem – poverty, homelessness, and the accompanying exposure to trauma, crime, and drugs. That means better alcohol and drug treatment, family counseling, low-income housing resources, job training, and individual therapy. And for those at risk who still slip past all the checkpoints, we need to make sure they don’t have access to guns and lethal medications.
Psychological autopsies done after suicides have indicated that more than 90% of people who die from suicide suffered from a mental illness, yet 54% of those who ended their own lives had never received a psychiatric diagnosis. There is a hopefulness that, if only we had more – more services, more therapy, more medication – then we could prevent suicide. Unfortunately, this line of thinking, with a “Zero Suicide” initiative, points a finger at those who survive: Suicide is preventable, so someone is to blame, if not a family member for missing the warning signs then the clinician who offered treatment that wasn’t good enough.
Along this line, the New York Times printed another opinion piece on Jan. 6 by Richard A. Friedman, MD, titled, “Why are young Americans killing themselves?” Dr. Friedman’s conclusion was more along the psychiatrist party line: “The good news is that we don’t have to wait for all the answers to know what to do. We know that various psychotherapies and medication are highly effective in treating depression. We just need to do a better job of identifying, reaching out to and providing resources for at-risk youths.”
Dr. Friedman goes on to propose universal screening at school, among other measures to identify those at risk. It is no surprise that Dr. Friedman’s article had more than 1,700 comments before commenting was closed by the Times. I have written about the pros and cons of screening adolescents for depression in a primary care setting, so putting the responsibility of identifying suicidal teenagers on school teachers seems like an ominous responsibility to add to a teacher’s obligations.
I did not read Dr. Barnhorst’s earlier op-ed piece as a condemnation of psychiatric care, but rather as a call to action and a reality check on the idea that psychiatry is the only answer to our suicide epidemic. More people than ever get treatment – from psychiatrists, from primary care doctors, from nonphysician prescribing clinicians, and from so many varieties of psychotherapists, and yet our suicide rates continue to rise.
In a post on the Psychology Today website, Sara Gorman, PhD, and Jack M. Gorman, MD, discussed Dr. Barnhorst’s article. “In the process of making her point, Barnhorst also manages to seriously trivialize the role of antidepressant medication in the treatment of depression and to imply that, given societal woes, there isn’t much we can do to try to prevent suicides – aside from limiting access to lethal means,” they wrote.
The Gormans were not alone in their objections; the day after the op-ed appeared in the New York Times, a well-respected psychiatry department chairman took on not just the content of the op-ed, but also the author, in his Twitter feed. He wrote, “@amybarnhorst doesn’t read scientific literature or skipped training. this article is wrong. #suicide is largely preventable, if proper measures taken n Rx provided. @nytimes please vet authors better @APAPsychiatric.” Dr. Barnhorst, also a voice on Twitter, added the wry response, “I skipped training.” When Twitter users responded that initial Twitter comment conveyed a lack of civility toward a colleague, the original Tweeter – I’m withholding his name with the hope that even writing about these interactions won’t put me on anyone’s enemy list – like many others sitting on the poles of these contentious topics, responded with the following, “All for civility except in the case of misinformation that puts lives at risk, especially when purveyed by a professional who wears the patina of credibility.”
If it’s not yet obvious, I don’t believe there is a simple answer to our suicide problem, nor do I think it puts lives at risk to point out that, so far, our treatments have not lowered suicide rates. The issue is complex and we have no perfect explanation as to why countries differ so greatly with regard to suicide. There are impoverished, war-torn countries with remarkably lower suicide rates, and nations with much stricter gun laws that have higher statistics. Honduras, deemed “the murder capital of the world,” has an enviable suicide rate of only 2.9 per 100,000.
If the solution were as simple as making medications more accessible, the answer might be an easy one (or at least worth trying) – make antidepressants available over-the-counter, a move that would both increase access and decrease stigma.
Some people are determined to end their own lives. They aren’t looking to see psychiatrists or to call hotlines, and they may well resort to an alternate method if any given one is not readily available. For these individuals, suicide may not be preventable, and we may be left to say that this tragic phenomena with its diverse causes should also lead us to explore the root causes of human misery and our cultural features that lead some people to end their own lives while others endure.
Clearly, there are those who have untreated psychiatric illnesses and who make impulsive and lethal decisions – access to care and means restrictions certainly save some lives. And while it is obvious to us as psychiatrists that anyone who is depressed or is having suicidal thoughts is deserving of a psychiatric evaluation and intervention, the truth remains that access to treatment in this country is limited by finances, by the availability of mental health professionals, and by stigma and shame. In the end, The one thing I am certain of is that our efforts to prevent suicide should unite, and not fracture, our profession.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
At every swipe through my social media feeds, I’m greeted with another topic that has advocates clustered at the extremes. People align, and they align quickly in our strangely polarized world in which anyone who might sit in the middle lies low.
It seems we’re divided: On the left you are a CNN fan or you’re one of those soulless monsters who tunes in to Fox News. You’re pro-life or you’re a baby killer, advocating for late-term abortions or even the execution of live infants. When it comes to firearm regulation, one side says you’re a threat to the Constitution, while the other says that those opposed are responsible for the death of every person who was ever the victim of a discharged firearm. And those who feel strongly about a given topic often justify their attacks on those who disagree. Psychiatry is no stranger to this thinking, and we are the only medical specialty with organized “antipsychiatry” groups who oppose our work. I have been a bit surprised, however, that the topic of suicide prevention is one that has us divided within our own specialty.
Amy Barnhorst, MD, is a psychiatrist at the University of California, Davis, and the author of “The empty promise of suicide prevention: Many of the problems that lead people to kill themselves cannot be fixed with a little serotonin,” an op-ed piece that appeared in the New York Times on April 26, 2019. Dr. Barnhorst began her essay with the story of a patient who was hospitalized after a relative realized she was planning her suicide. That story had an ending that psychiatrists relish: A person with previously unrecognized and untreated bipolar disorder received care, including medication, and got better. This suicide was preventable, a life was saved, and this story followed a model we all hope is being replicated over and over.
Dr. Barnhorst went on to say that this was an outlier in her career, that most of the suicidal patients she sees are impoverished, homeless, addicted, and she wrote about how little the treatment setting has to offer: The idea that a pill would fix these problems is almost laughable. She suggests that there is more to suicide prevention than identifying prospective patients and getting them acute psychiatric care.
The decision to stop living is one that people arrive at by different paths, some over months, but many in a matter of minutes. Those people won’t be intercepted by the mental health system. We certainly need more psychiatric services and more research into better, faster-acting treatments for severe depression and suicidal thoughts, but that will never be enough.
We need to address the root causes of our nation’s suicide problem – poverty, homelessness, and the accompanying exposure to trauma, crime, and drugs. That means better alcohol and drug treatment, family counseling, low-income housing resources, job training, and individual therapy. And for those at risk who still slip past all the checkpoints, we need to make sure they don’t have access to guns and lethal medications.
Psychological autopsies done after suicides have indicated that more than 90% of people who die from suicide suffered from a mental illness, yet 54% of those who ended their own lives had never received a psychiatric diagnosis. There is a hopefulness that, if only we had more – more services, more therapy, more medication – then we could prevent suicide. Unfortunately, this line of thinking, with a “Zero Suicide” initiative, points a finger at those who survive: Suicide is preventable, so someone is to blame, if not a family member for missing the warning signs then the clinician who offered treatment that wasn’t good enough.
Along this line, the New York Times printed another opinion piece on Jan. 6 by Richard A. Friedman, MD, titled, “Why are young Americans killing themselves?” Dr. Friedman’s conclusion was more along the psychiatrist party line: “The good news is that we don’t have to wait for all the answers to know what to do. We know that various psychotherapies and medication are highly effective in treating depression. We just need to do a better job of identifying, reaching out to and providing resources for at-risk youths.”
Dr. Friedman goes on to propose universal screening at school, among other measures to identify those at risk. It is no surprise that Dr. Friedman’s article had more than 1,700 comments before commenting was closed by the Times. I have written about the pros and cons of screening adolescents for depression in a primary care setting, so putting the responsibility of identifying suicidal teenagers on school teachers seems like an ominous responsibility to add to a teacher’s obligations.
I did not read Dr. Barnhorst’s earlier op-ed piece as a condemnation of psychiatric care, but rather as a call to action and a reality check on the idea that psychiatry is the only answer to our suicide epidemic. More people than ever get treatment – from psychiatrists, from primary care doctors, from nonphysician prescribing clinicians, and from so many varieties of psychotherapists, and yet our suicide rates continue to rise.
In a post on the Psychology Today website, Sara Gorman, PhD, and Jack M. Gorman, MD, discussed Dr. Barnhorst’s article. “In the process of making her point, Barnhorst also manages to seriously trivialize the role of antidepressant medication in the treatment of depression and to imply that, given societal woes, there isn’t much we can do to try to prevent suicides – aside from limiting access to lethal means,” they wrote.
The Gormans were not alone in their objections; the day after the op-ed appeared in the New York Times, a well-respected psychiatry department chairman took on not just the content of the op-ed, but also the author, in his Twitter feed. He wrote, “@amybarnhorst doesn’t read scientific literature or skipped training. this article is wrong. #suicide is largely preventable, if proper measures taken n Rx provided. @nytimes please vet authors better @APAPsychiatric.” Dr. Barnhorst, also a voice on Twitter, added the wry response, “I skipped training.” When Twitter users responded that initial Twitter comment conveyed a lack of civility toward a colleague, the original Tweeter – I’m withholding his name with the hope that even writing about these interactions won’t put me on anyone’s enemy list – like many others sitting on the poles of these contentious topics, responded with the following, “All for civility except in the case of misinformation that puts lives at risk, especially when purveyed by a professional who wears the patina of credibility.”
If it’s not yet obvious, I don’t believe there is a simple answer to our suicide problem, nor do I think it puts lives at risk to point out that, so far, our treatments have not lowered suicide rates. The issue is complex and we have no perfect explanation as to why countries differ so greatly with regard to suicide. There are impoverished, war-torn countries with remarkably lower suicide rates, and nations with much stricter gun laws that have higher statistics. Honduras, deemed “the murder capital of the world,” has an enviable suicide rate of only 2.9 per 100,000.
If the solution were as simple as making medications more accessible, the answer might be an easy one (or at least worth trying) – make antidepressants available over-the-counter, a move that would both increase access and decrease stigma.
Some people are determined to end their own lives. They aren’t looking to see psychiatrists or to call hotlines, and they may well resort to an alternate method if any given one is not readily available. For these individuals, suicide may not be preventable, and we may be left to say that this tragic phenomena with its diverse causes should also lead us to explore the root causes of human misery and our cultural features that lead some people to end their own lives while others endure.
Clearly, there are those who have untreated psychiatric illnesses and who make impulsive and lethal decisions – access to care and means restrictions certainly save some lives. And while it is obvious to us as psychiatrists that anyone who is depressed or is having suicidal thoughts is deserving of a psychiatric evaluation and intervention, the truth remains that access to treatment in this country is limited by finances, by the availability of mental health professionals, and by stigma and shame. In the end, The one thing I am certain of is that our efforts to prevent suicide should unite, and not fracture, our profession.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
FDA advisers set high bar for new opioids
During an opioid-addiction epidemic, can any new opioid pain drug meet prevailing safety demands to gain regulatory approval?
On Jan. 14 and 15, a Food and Drug Administration advisory committee voted virtually unanimously against two new opioid formulations and evenly split for and against a third; the 2 days of data and discussion showed how high a bar new opioids face these days for getting onto the U.S. market.
The bar’s height is very understandable given how many Americans have become addicted to opioids over the past decade, more often than not by accident while using pain medications as they believed they had been directed, said experts during the sessions held on the FDA’s campus in White Oak, Md.
Among the many upshots of the opioid crisis, the meetings held to discuss these three contender opioids highlighted the bitter irony confronting attempts to bring new, safer opioids to the U.S. market: While less abusable pain-relief medications that still harness the potent analgesic power of mu opioid receptor agonists are desperately desired, new agents in this space now receive withering scrutiny over their safeguards against misuse and abuse, and over whether they add anything meaningfully new to what’s already available. While these demands seem reasonable, perhaps even essential, it’s unclear whether any new opioid-based pain drugs will ever fully meet the safety that researchers, clinicians, and the public now seek.
A special FDA advisory committee that combined the Anesthetic and Analgesic Drug Products Advisory Committee with members of the Drug Safety and Risk Management Advisory Committee considered the application for three different opioid drugs from three separate companies. None received a clear endorsement. Oxycodegol, a new type of orally delivered opioid molecule engineered to slow brain entry and thereby delay an abuser’s high, got voted down without any votes in favor and 27 votes against agency approval. Aximris XR, an extended-release oxycodone formulation that successfully deterred intravenous abuse but had no deterrence efficacy for intranasal or oral abuse failed by a 2-24 vote against. The third agent, CTC, a novel formulation of the schedule IV opioid tramadol with the NSAID celecoxib designed to be analgesic but with limited opioid-abuse appeal, came the closest to meaningful support with a tied 13-13 vote from advisory committee members for and against agency approval. FDA staff takes advisory committee opinions and votes into account when making their final decisions about drug marketing approvals.
In each case, the committee members, mostly the same roster assembled for each of the three agents, identified specific concerns with the data purported to show each drug’s safety and efficacy. But the gathered experts and consumer representatives also consistently cited holistic challenges to approving new opioids and the stiffer criteria these agents face amid a continuing wave of opioid misuse and abuse.
“In the context of the public health issues, we don’t want to be perceived in any way of taking shortcuts,” said Linda S. Tyler, PharmD,, an advisory committee member and professor of pharmacy and chief pharmacy officer at the University of Utah in Salt Lake City. “There is no question that for a new product to come to market in this space it needs to add to what’s on the market, meet a high bar, and provide advantages compared with what’s already on the market,” she said.
Tramadol plus celecoxib gains some support
The proposed combined formulation of tramadol and celecoxib came closest to meeting that bar, as far as the advisory committee was concerned, coming away with 13 votes favoring approval to match 13 votes against. The premise behind this agent, know as CTC (cocrystal of tramadol and celecoxib), was that it combined a modest dose (44 mg) of the schedule IV opioid tramadol with a 56-mg dose of celecoxib in a twice-daily pill. Eugene R. Viscusi, MD, professor of anesthesiology and director of acute pain management at Thomas Jefferson University in Philadelphia and a speaker at the session on behalf of the applicant company, spelled out the rationale behind CTC: “We are caught in a dilemma. We need to reduce opioid use, but we also need to treat pain. We have an urgent need to have pain treatment options that are effective but have low potential for abuse and dependence. We are looking at multimodal analgesia, that uses combination of agents, recognizing that postoperative pain is a mixed pain syndrome. Multimodal pain treatments are now considered standard care. We want to minimize opioids to the lowest dose possible to produce safe analgesia. Tramadol is the least-preferred opioid for abuse,” and is rated as schedule IV, the U.S. designation for drugs considered to have a low level of potential for causing abuse or dependence. “Opioids used as stand-alone agents have contributed to the current opioid crisis,” Dr. Viscusi told the committee.
In contrast to tramadol’s schedule IV status, the mainstays of recent opioid pain therapy have been hydrocodone and oxycodone, schedule II opioids rated as having a “high potential for abuse.”
Several advisory committee members agreed that CTC minimized patient exposure to an opioid. “This drug isn’t even tramadol; it’s tramadol light. It has about as low a dose [of an opioid] as you can have and still have a drug,” said member Lee A. Hoffer, PhD, a medical anthropologist at Case Western Reserve University, Cleveland, who studies substance use disorders. “All opioids are dangerous, even at a low dose, but there is a linear relationship based on potency, so if we want to have an opioid for acute pain, I’d like it to have the lowest morphine milligram equivalent possible. The ideal is no opioids, but that is not what happens,” he said. The CTC formulation delivers 17.6 morphine milligram equivalents (MME) per pill, the manufacturer’s representatives said. The Centers for Disease Control and Prevention defines a “relatively low” daily opioid dose as 20-50 MME.
Some committee members hailed the CTC formulation as a meaningful step toward cutting opioid consumption.
“We may be very nervous about abuse of scheduled opioids, but a schedule IV opioid in an opioid-sparing formulation is as good as it gets in 2020,” said committee member Kevin L. Zacharoff, MD, a pain medicine specialist at the State University of New York at Stony Brook. “Any opioid has potential for abuse, but this is a safer alternative to the schedule II drugs. There is less public health risk with this,” said committee member Sherif Zaafran, MD, a Houston anesthesiologist. “This represents an incremental but important approach to addressing the opioid crisis, especially if used to replace schedule II opioids,” said Brandon D.L. Marshall, PhD, an epidemiologist and substance abuse researcher at Brown University in Providence, R.I.
But despite agreement that CTC represented a new low in the MME of an opioid given to patients, several committee members still saw the formulation as problematic by introducing any opioid, no matter how small the dose.
“The landscape of tramadol use and prescribing is evolving. There’s been an exponential upturn in tramadol prescribing. It’s perceived [as] safer, but it’s not completely safe. Will this change tramadol abuse and open the door to abuse of other opioids? This is what got us into trouble with opioids in the first place. Patients start with a prescription opioid that they perceive is safe. Patients don’t start with oxycodone or heroin. They start with drugs that are believed to be safe. I feel this combination has less risk for abuse, but I’m worried that it would produce a false sense of security for tolerability and safety,” said committee member Maryann E. Amirshahi, MD, a medical toxicologist at Georgetown University and MedStar Health in Washington.
Several other committee members returned to this point throughout the 2 days of discussions: The majority of Americans who have become hooked on opioids reached that point by taking an opioid pain medication for a legitimate medical reason and using the drug the way they had understood they should.
“I’m most concerned about unintentional misuse leading to addiction and abuse. Most people with an opioid addiction got it inadvertently, misusing it by mistake,” said committee member Suzanne B. Robotti, a consumer representative and executive director of DES Action USA. “I’m concerned about approving an opioid, even an opioid with a low abuse history, without a clearer picture of the human abuse potential data and what would happen if this drug were abused,” she added, referring to the proposed CTC formulation.
“All the patients I work with started [their opioid addiction] as pain patients,” Dr. Hoffer said.
“The most common use and abuse of opioids is orally. We need to avoid having patients who use the drug as prescribed and still end up addicted,” said committee member Friedhelm Sandbrink, MD, a neurologist and director of pain management at the Veterans Affairs (VA) Medical Center in Washington.
What this means, said several panelists, is functionally clamping down a class-wide lid on new opioids. “The way to reduce deaths from abuse is to reduce addiction, and to have an impact you need to reduce opioid exposure.” said committee member Sonia Hernandez-Diaz, MD, professor of epidemiology at the Harvard School of Public Health in Boston.
“In this opioid crisis, we ask for data that we wouldn’t ordinarily ask for. I feel there are unanswered questions about the abuse potential [of CTC]. We have seen a recent reduction in oxycodone use, which is great, but also an increase in tramadol use. We should not be fooled. Tramadol is an opioid, even if it’s schedule IV,” Dr. Tyler said.
Two other opioids faced greater opposition
The other two agents that the committee considered received much less support and sharper skepticism. The application for Aximris XR, an extended release form of oxycodone with a purported abuse-deterrent formulation (ADF) that relies on being difficult to extract for intravenous use as well as possibly having effective deterrence mechanisms for other forms of abuse. But FDA staffers reported that the only effective deterrence they could document was against manipulation for intravenous use, making Aximris XR the first opioid seeking ADF labeling based on deterrence to a single delivery route. This led several committee members, as well as the FDA, to comment on the clinical meaningfulness of ADF for one route. So far, the FDA approved ADF labeling for seven opioids, most notably OxyContin, an extended-release oxycodone with the biggest share of the U.S. market for opioids with ADF labeling.
“For ADF, we label based on what we expect from the premarket data. We don’t really know how that translates into what happens once the drug is on the market. Every company with an ADF in their label is required to do postmarketing studies on the abuse routes that are supposed to be deterred. We see shifts to other routes. Assessment of ADF is incredibly challenging, both scientifically and logistically, because there has not been a lot of uptake of these products, for a variety of reasons,” said Judy Staffa, PhD, associate director for Public Health Initiatives in the Office of Surveillance & Epidemiology in the FDA’s Center for Drug Evaluation and Research. The company that markets OxyContin has been the first to submit to the FDA all of its required postmarketing data on ADF efficacy, and the agency is now reviewing this filing, Dr. Staffa said.
The data presented for Aximris XR appeared to generally fail to convince committee members that it provided a meaningful addition to the range of opioids with ADF designations already available, which meant that their decision mostly came down to whether they felt it made sense to bring a me-too opioid to the U.S. market. Their answer was mostly no.
“In the end, it’s another opioid, and I’m not sure we need another opioid,” said committee member Lonnie K. Zeltzer, MD, professor of pediatrics, anesthesiology, psychiatry, and biobehavioral sciences and director of pediatric pain at the University of California, Los Angeles “There are so many options for patients and for people who abuse these drug. I don’t see this formulation as having a profound impact, but I’m very concerned about adding more prescription opioids,” said Martin Garcia-Bunuel, MD, deputy chief of staff for the VA Maryland Health Care System in Baltimore. Another concern of some committee members was that ADF remains a designation with an uncertain meaning, pending the FDA’s analysis of the OxyContin data.
“At the end of the day, we don’t know whether any of the [ADF] stuff makes a difference,” noted Steve B. Meisel, PharmD, system director of medication safety for M Health Fairview in Minneapolis and a committee member,
The third agent, oxycodegol, a molecule designed to pass more slowly across the blood-brain barrier because of an attached polyethylene glycol chain that’s supposed to prevent a rapid high after ingestion and hence cut abuse potential. It received unanimous committee rejection, primarily because its safety and efficacy evidence had so many holes, but the shadow of opioid abuse permeated the committee’s discussion.
“One dogma in the abuse world is that slowing entry into the brain reduces abuse potential, but the opioid crisis showed that this is not the only factor. Some people have become addicted to slow-acting drugs. The abuse potential of this drug, oxycodegol, needs to be considered given where we’ve been with the opioid crisis,” said Jane B. Acri, PhD, chief of the Medications Discovery and Toxicology Branch of the National Institute on Drug Abuse.
“During the opioid epidemic, do we want to approve more opioids? If the [pain] efficacy is about the same as oxycodone, is better safety or abuse potential a reason to approve it? We need guidance [from the FDA] about what is ‘better enough.’ No opioid will ever be perfect; there will always be abuse and misuse. But what is good enough to justify bringing another opioid onto the market? What is a good enough improvement? I don’t have an answer,” Dr. Hernandez-Diaz said.
Adviser comments showed that the continued threat of widespread opioid addiction has cooled prospects for new opioid approvals by making FDA advisers skittish over how to properly score the incremental value of a new opioid.
“Do we need to go back to the drawing board on how we make decisions on exposing the American public to these kinds of agents?” Dr. Garcia-Bunuel asked. “I don’t think we have the tools to make these decisions.”
During an opioid-addiction epidemic, can any new opioid pain drug meet prevailing safety demands to gain regulatory approval?
On Jan. 14 and 15, a Food and Drug Administration advisory committee voted virtually unanimously against two new opioid formulations and evenly split for and against a third; the 2 days of data and discussion showed how high a bar new opioids face these days for getting onto the U.S. market.
The bar’s height is very understandable given how many Americans have become addicted to opioids over the past decade, more often than not by accident while using pain medications as they believed they had been directed, said experts during the sessions held on the FDA’s campus in White Oak, Md.
Among the many upshots of the opioid crisis, the meetings held to discuss these three contender opioids highlighted the bitter irony confronting attempts to bring new, safer opioids to the U.S. market: While less abusable pain-relief medications that still harness the potent analgesic power of mu opioid receptor agonists are desperately desired, new agents in this space now receive withering scrutiny over their safeguards against misuse and abuse, and over whether they add anything meaningfully new to what’s already available. While these demands seem reasonable, perhaps even essential, it’s unclear whether any new opioid-based pain drugs will ever fully meet the safety that researchers, clinicians, and the public now seek.
A special FDA advisory committee that combined the Anesthetic and Analgesic Drug Products Advisory Committee with members of the Drug Safety and Risk Management Advisory Committee considered the application for three different opioid drugs from three separate companies. None received a clear endorsement. Oxycodegol, a new type of orally delivered opioid molecule engineered to slow brain entry and thereby delay an abuser’s high, got voted down without any votes in favor and 27 votes against agency approval. Aximris XR, an extended-release oxycodone formulation that successfully deterred intravenous abuse but had no deterrence efficacy for intranasal or oral abuse failed by a 2-24 vote against. The third agent, CTC, a novel formulation of the schedule IV opioid tramadol with the NSAID celecoxib designed to be analgesic but with limited opioid-abuse appeal, came the closest to meaningful support with a tied 13-13 vote from advisory committee members for and against agency approval. FDA staff takes advisory committee opinions and votes into account when making their final decisions about drug marketing approvals.
In each case, the committee members, mostly the same roster assembled for each of the three agents, identified specific concerns with the data purported to show each drug’s safety and efficacy. But the gathered experts and consumer representatives also consistently cited holistic challenges to approving new opioids and the stiffer criteria these agents face amid a continuing wave of opioid misuse and abuse.
“In the context of the public health issues, we don’t want to be perceived in any way of taking shortcuts,” said Linda S. Tyler, PharmD,, an advisory committee member and professor of pharmacy and chief pharmacy officer at the University of Utah in Salt Lake City. “There is no question that for a new product to come to market in this space it needs to add to what’s on the market, meet a high bar, and provide advantages compared with what’s already on the market,” she said.
Tramadol plus celecoxib gains some support
The proposed combined formulation of tramadol and celecoxib came closest to meeting that bar, as far as the advisory committee was concerned, coming away with 13 votes favoring approval to match 13 votes against. The premise behind this agent, know as CTC (cocrystal of tramadol and celecoxib), was that it combined a modest dose (44 mg) of the schedule IV opioid tramadol with a 56-mg dose of celecoxib in a twice-daily pill. Eugene R. Viscusi, MD, professor of anesthesiology and director of acute pain management at Thomas Jefferson University in Philadelphia and a speaker at the session on behalf of the applicant company, spelled out the rationale behind CTC: “We are caught in a dilemma. We need to reduce opioid use, but we also need to treat pain. We have an urgent need to have pain treatment options that are effective but have low potential for abuse and dependence. We are looking at multimodal analgesia, that uses combination of agents, recognizing that postoperative pain is a mixed pain syndrome. Multimodal pain treatments are now considered standard care. We want to minimize opioids to the lowest dose possible to produce safe analgesia. Tramadol is the least-preferred opioid for abuse,” and is rated as schedule IV, the U.S. designation for drugs considered to have a low level of potential for causing abuse or dependence. “Opioids used as stand-alone agents have contributed to the current opioid crisis,” Dr. Viscusi told the committee.
In contrast to tramadol’s schedule IV status, the mainstays of recent opioid pain therapy have been hydrocodone and oxycodone, schedule II opioids rated as having a “high potential for abuse.”
Several advisory committee members agreed that CTC minimized patient exposure to an opioid. “This drug isn’t even tramadol; it’s tramadol light. It has about as low a dose [of an opioid] as you can have and still have a drug,” said member Lee A. Hoffer, PhD, a medical anthropologist at Case Western Reserve University, Cleveland, who studies substance use disorders. “All opioids are dangerous, even at a low dose, but there is a linear relationship based on potency, so if we want to have an opioid for acute pain, I’d like it to have the lowest morphine milligram equivalent possible. The ideal is no opioids, but that is not what happens,” he said. The CTC formulation delivers 17.6 morphine milligram equivalents (MME) per pill, the manufacturer’s representatives said. The Centers for Disease Control and Prevention defines a “relatively low” daily opioid dose as 20-50 MME.
Some committee members hailed the CTC formulation as a meaningful step toward cutting opioid consumption.
“We may be very nervous about abuse of scheduled opioids, but a schedule IV opioid in an opioid-sparing formulation is as good as it gets in 2020,” said committee member Kevin L. Zacharoff, MD, a pain medicine specialist at the State University of New York at Stony Brook. “Any opioid has potential for abuse, but this is a safer alternative to the schedule II drugs. There is less public health risk with this,” said committee member Sherif Zaafran, MD, a Houston anesthesiologist. “This represents an incremental but important approach to addressing the opioid crisis, especially if used to replace schedule II opioids,” said Brandon D.L. Marshall, PhD, an epidemiologist and substance abuse researcher at Brown University in Providence, R.I.
But despite agreement that CTC represented a new low in the MME of an opioid given to patients, several committee members still saw the formulation as problematic by introducing any opioid, no matter how small the dose.
“The landscape of tramadol use and prescribing is evolving. There’s been an exponential upturn in tramadol prescribing. It’s perceived [as] safer, but it’s not completely safe. Will this change tramadol abuse and open the door to abuse of other opioids? This is what got us into trouble with opioids in the first place. Patients start with a prescription opioid that they perceive is safe. Patients don’t start with oxycodone or heroin. They start with drugs that are believed to be safe. I feel this combination has less risk for abuse, but I’m worried that it would produce a false sense of security for tolerability and safety,” said committee member Maryann E. Amirshahi, MD, a medical toxicologist at Georgetown University and MedStar Health in Washington.
Several other committee members returned to this point throughout the 2 days of discussions: The majority of Americans who have become hooked on opioids reached that point by taking an opioid pain medication for a legitimate medical reason and using the drug the way they had understood they should.
“I’m most concerned about unintentional misuse leading to addiction and abuse. Most people with an opioid addiction got it inadvertently, misusing it by mistake,” said committee member Suzanne B. Robotti, a consumer representative and executive director of DES Action USA. “I’m concerned about approving an opioid, even an opioid with a low abuse history, without a clearer picture of the human abuse potential data and what would happen if this drug were abused,” she added, referring to the proposed CTC formulation.
“All the patients I work with started [their opioid addiction] as pain patients,” Dr. Hoffer said.
“The most common use and abuse of opioids is orally. We need to avoid having patients who use the drug as prescribed and still end up addicted,” said committee member Friedhelm Sandbrink, MD, a neurologist and director of pain management at the Veterans Affairs (VA) Medical Center in Washington.
What this means, said several panelists, is functionally clamping down a class-wide lid on new opioids. “The way to reduce deaths from abuse is to reduce addiction, and to have an impact you need to reduce opioid exposure.” said committee member Sonia Hernandez-Diaz, MD, professor of epidemiology at the Harvard School of Public Health in Boston.
“In this opioid crisis, we ask for data that we wouldn’t ordinarily ask for. I feel there are unanswered questions about the abuse potential [of CTC]. We have seen a recent reduction in oxycodone use, which is great, but also an increase in tramadol use. We should not be fooled. Tramadol is an opioid, even if it’s schedule IV,” Dr. Tyler said.
Two other opioids faced greater opposition
The other two agents that the committee considered received much less support and sharper skepticism. The application for Aximris XR, an extended release form of oxycodone with a purported abuse-deterrent formulation (ADF) that relies on being difficult to extract for intravenous use as well as possibly having effective deterrence mechanisms for other forms of abuse. But FDA staffers reported that the only effective deterrence they could document was against manipulation for intravenous use, making Aximris XR the first opioid seeking ADF labeling based on deterrence to a single delivery route. This led several committee members, as well as the FDA, to comment on the clinical meaningfulness of ADF for one route. So far, the FDA approved ADF labeling for seven opioids, most notably OxyContin, an extended-release oxycodone with the biggest share of the U.S. market for opioids with ADF labeling.
“For ADF, we label based on what we expect from the premarket data. We don’t really know how that translates into what happens once the drug is on the market. Every company with an ADF in their label is required to do postmarketing studies on the abuse routes that are supposed to be deterred. We see shifts to other routes. Assessment of ADF is incredibly challenging, both scientifically and logistically, because there has not been a lot of uptake of these products, for a variety of reasons,” said Judy Staffa, PhD, associate director for Public Health Initiatives in the Office of Surveillance & Epidemiology in the FDA’s Center for Drug Evaluation and Research. The company that markets OxyContin has been the first to submit to the FDA all of its required postmarketing data on ADF efficacy, and the agency is now reviewing this filing, Dr. Staffa said.
The data presented for Aximris XR appeared to generally fail to convince committee members that it provided a meaningful addition to the range of opioids with ADF designations already available, which meant that their decision mostly came down to whether they felt it made sense to bring a me-too opioid to the U.S. market. Their answer was mostly no.
“In the end, it’s another opioid, and I’m not sure we need another opioid,” said committee member Lonnie K. Zeltzer, MD, professor of pediatrics, anesthesiology, psychiatry, and biobehavioral sciences and director of pediatric pain at the University of California, Los Angeles “There are so many options for patients and for people who abuse these drug. I don’t see this formulation as having a profound impact, but I’m very concerned about adding more prescription opioids,” said Martin Garcia-Bunuel, MD, deputy chief of staff for the VA Maryland Health Care System in Baltimore. Another concern of some committee members was that ADF remains a designation with an uncertain meaning, pending the FDA’s analysis of the OxyContin data.
“At the end of the day, we don’t know whether any of the [ADF] stuff makes a difference,” noted Steve B. Meisel, PharmD, system director of medication safety for M Health Fairview in Minneapolis and a committee member,
The third agent, oxycodegol, a molecule designed to pass more slowly across the blood-brain barrier because of an attached polyethylene glycol chain that’s supposed to prevent a rapid high after ingestion and hence cut abuse potential. It received unanimous committee rejection, primarily because its safety and efficacy evidence had so many holes, but the shadow of opioid abuse permeated the committee’s discussion.
“One dogma in the abuse world is that slowing entry into the brain reduces abuse potential, but the opioid crisis showed that this is not the only factor. Some people have become addicted to slow-acting drugs. The abuse potential of this drug, oxycodegol, needs to be considered given where we’ve been with the opioid crisis,” said Jane B. Acri, PhD, chief of the Medications Discovery and Toxicology Branch of the National Institute on Drug Abuse.
“During the opioid epidemic, do we want to approve more opioids? If the [pain] efficacy is about the same as oxycodone, is better safety or abuse potential a reason to approve it? We need guidance [from the FDA] about what is ‘better enough.’ No opioid will ever be perfect; there will always be abuse and misuse. But what is good enough to justify bringing another opioid onto the market? What is a good enough improvement? I don’t have an answer,” Dr. Hernandez-Diaz said.
Adviser comments showed that the continued threat of widespread opioid addiction has cooled prospects for new opioid approvals by making FDA advisers skittish over how to properly score the incremental value of a new opioid.
“Do we need to go back to the drawing board on how we make decisions on exposing the American public to these kinds of agents?” Dr. Garcia-Bunuel asked. “I don’t think we have the tools to make these decisions.”
During an opioid-addiction epidemic, can any new opioid pain drug meet prevailing safety demands to gain regulatory approval?
On Jan. 14 and 15, a Food and Drug Administration advisory committee voted virtually unanimously against two new opioid formulations and evenly split for and against a third; the 2 days of data and discussion showed how high a bar new opioids face these days for getting onto the U.S. market.
The bar’s height is very understandable given how many Americans have become addicted to opioids over the past decade, more often than not by accident while using pain medications as they believed they had been directed, said experts during the sessions held on the FDA’s campus in White Oak, Md.
Among the many upshots of the opioid crisis, the meetings held to discuss these three contender opioids highlighted the bitter irony confronting attempts to bring new, safer opioids to the U.S. market: While less abusable pain-relief medications that still harness the potent analgesic power of mu opioid receptor agonists are desperately desired, new agents in this space now receive withering scrutiny over their safeguards against misuse and abuse, and over whether they add anything meaningfully new to what’s already available. While these demands seem reasonable, perhaps even essential, it’s unclear whether any new opioid-based pain drugs will ever fully meet the safety that researchers, clinicians, and the public now seek.
A special FDA advisory committee that combined the Anesthetic and Analgesic Drug Products Advisory Committee with members of the Drug Safety and Risk Management Advisory Committee considered the application for three different opioid drugs from three separate companies. None received a clear endorsement. Oxycodegol, a new type of orally delivered opioid molecule engineered to slow brain entry and thereby delay an abuser’s high, got voted down without any votes in favor and 27 votes against agency approval. Aximris XR, an extended-release oxycodone formulation that successfully deterred intravenous abuse but had no deterrence efficacy for intranasal or oral abuse failed by a 2-24 vote against. The third agent, CTC, a novel formulation of the schedule IV opioid tramadol with the NSAID celecoxib designed to be analgesic but with limited opioid-abuse appeal, came the closest to meaningful support with a tied 13-13 vote from advisory committee members for and against agency approval. FDA staff takes advisory committee opinions and votes into account when making their final decisions about drug marketing approvals.
In each case, the committee members, mostly the same roster assembled for each of the three agents, identified specific concerns with the data purported to show each drug’s safety and efficacy. But the gathered experts and consumer representatives also consistently cited holistic challenges to approving new opioids and the stiffer criteria these agents face amid a continuing wave of opioid misuse and abuse.
“In the context of the public health issues, we don’t want to be perceived in any way of taking shortcuts,” said Linda S. Tyler, PharmD,, an advisory committee member and professor of pharmacy and chief pharmacy officer at the University of Utah in Salt Lake City. “There is no question that for a new product to come to market in this space it needs to add to what’s on the market, meet a high bar, and provide advantages compared with what’s already on the market,” she said.
Tramadol plus celecoxib gains some support
The proposed combined formulation of tramadol and celecoxib came closest to meeting that bar, as far as the advisory committee was concerned, coming away with 13 votes favoring approval to match 13 votes against. The premise behind this agent, know as CTC (cocrystal of tramadol and celecoxib), was that it combined a modest dose (44 mg) of the schedule IV opioid tramadol with a 56-mg dose of celecoxib in a twice-daily pill. Eugene R. Viscusi, MD, professor of anesthesiology and director of acute pain management at Thomas Jefferson University in Philadelphia and a speaker at the session on behalf of the applicant company, spelled out the rationale behind CTC: “We are caught in a dilemma. We need to reduce opioid use, but we also need to treat pain. We have an urgent need to have pain treatment options that are effective but have low potential for abuse and dependence. We are looking at multimodal analgesia, that uses combination of agents, recognizing that postoperative pain is a mixed pain syndrome. Multimodal pain treatments are now considered standard care. We want to minimize opioids to the lowest dose possible to produce safe analgesia. Tramadol is the least-preferred opioid for abuse,” and is rated as schedule IV, the U.S. designation for drugs considered to have a low level of potential for causing abuse or dependence. “Opioids used as stand-alone agents have contributed to the current opioid crisis,” Dr. Viscusi told the committee.
In contrast to tramadol’s schedule IV status, the mainstays of recent opioid pain therapy have been hydrocodone and oxycodone, schedule II opioids rated as having a “high potential for abuse.”
Several advisory committee members agreed that CTC minimized patient exposure to an opioid. “This drug isn’t even tramadol; it’s tramadol light. It has about as low a dose [of an opioid] as you can have and still have a drug,” said member Lee A. Hoffer, PhD, a medical anthropologist at Case Western Reserve University, Cleveland, who studies substance use disorders. “All opioids are dangerous, even at a low dose, but there is a linear relationship based on potency, so if we want to have an opioid for acute pain, I’d like it to have the lowest morphine milligram equivalent possible. The ideal is no opioids, but that is not what happens,” he said. The CTC formulation delivers 17.6 morphine milligram equivalents (MME) per pill, the manufacturer’s representatives said. The Centers for Disease Control and Prevention defines a “relatively low” daily opioid dose as 20-50 MME.
Some committee members hailed the CTC formulation as a meaningful step toward cutting opioid consumption.
“We may be very nervous about abuse of scheduled opioids, but a schedule IV opioid in an opioid-sparing formulation is as good as it gets in 2020,” said committee member Kevin L. Zacharoff, MD, a pain medicine specialist at the State University of New York at Stony Brook. “Any opioid has potential for abuse, but this is a safer alternative to the schedule II drugs. There is less public health risk with this,” said committee member Sherif Zaafran, MD, a Houston anesthesiologist. “This represents an incremental but important approach to addressing the opioid crisis, especially if used to replace schedule II opioids,” said Brandon D.L. Marshall, PhD, an epidemiologist and substance abuse researcher at Brown University in Providence, R.I.
But despite agreement that CTC represented a new low in the MME of an opioid given to patients, several committee members still saw the formulation as problematic by introducing any opioid, no matter how small the dose.
“The landscape of tramadol use and prescribing is evolving. There’s been an exponential upturn in tramadol prescribing. It’s perceived [as] safer, but it’s not completely safe. Will this change tramadol abuse and open the door to abuse of other opioids? This is what got us into trouble with opioids in the first place. Patients start with a prescription opioid that they perceive is safe. Patients don’t start with oxycodone or heroin. They start with drugs that are believed to be safe. I feel this combination has less risk for abuse, but I’m worried that it would produce a false sense of security for tolerability and safety,” said committee member Maryann E. Amirshahi, MD, a medical toxicologist at Georgetown University and MedStar Health in Washington.
Several other committee members returned to this point throughout the 2 days of discussions: The majority of Americans who have become hooked on opioids reached that point by taking an opioid pain medication for a legitimate medical reason and using the drug the way they had understood they should.
“I’m most concerned about unintentional misuse leading to addiction and abuse. Most people with an opioid addiction got it inadvertently, misusing it by mistake,” said committee member Suzanne B. Robotti, a consumer representative and executive director of DES Action USA. “I’m concerned about approving an opioid, even an opioid with a low abuse history, without a clearer picture of the human abuse potential data and what would happen if this drug were abused,” she added, referring to the proposed CTC formulation.
“All the patients I work with started [their opioid addiction] as pain patients,” Dr. Hoffer said.
“The most common use and abuse of opioids is orally. We need to avoid having patients who use the drug as prescribed and still end up addicted,” said committee member Friedhelm Sandbrink, MD, a neurologist and director of pain management at the Veterans Affairs (VA) Medical Center in Washington.
What this means, said several panelists, is functionally clamping down a class-wide lid on new opioids. “The way to reduce deaths from abuse is to reduce addiction, and to have an impact you need to reduce opioid exposure.” said committee member Sonia Hernandez-Diaz, MD, professor of epidemiology at the Harvard School of Public Health in Boston.
“In this opioid crisis, we ask for data that we wouldn’t ordinarily ask for. I feel there are unanswered questions about the abuse potential [of CTC]. We have seen a recent reduction in oxycodone use, which is great, but also an increase in tramadol use. We should not be fooled. Tramadol is an opioid, even if it’s schedule IV,” Dr. Tyler said.
Two other opioids faced greater opposition
The other two agents that the committee considered received much less support and sharper skepticism. The application for Aximris XR, an extended release form of oxycodone with a purported abuse-deterrent formulation (ADF) that relies on being difficult to extract for intravenous use as well as possibly having effective deterrence mechanisms for other forms of abuse. But FDA staffers reported that the only effective deterrence they could document was against manipulation for intravenous use, making Aximris XR the first opioid seeking ADF labeling based on deterrence to a single delivery route. This led several committee members, as well as the FDA, to comment on the clinical meaningfulness of ADF for one route. So far, the FDA approved ADF labeling for seven opioids, most notably OxyContin, an extended-release oxycodone with the biggest share of the U.S. market for opioids with ADF labeling.
“For ADF, we label based on what we expect from the premarket data. We don’t really know how that translates into what happens once the drug is on the market. Every company with an ADF in their label is required to do postmarketing studies on the abuse routes that are supposed to be deterred. We see shifts to other routes. Assessment of ADF is incredibly challenging, both scientifically and logistically, because there has not been a lot of uptake of these products, for a variety of reasons,” said Judy Staffa, PhD, associate director for Public Health Initiatives in the Office of Surveillance & Epidemiology in the FDA’s Center for Drug Evaluation and Research. The company that markets OxyContin has been the first to submit to the FDA all of its required postmarketing data on ADF efficacy, and the agency is now reviewing this filing, Dr. Staffa said.
The data presented for Aximris XR appeared to generally fail to convince committee members that it provided a meaningful addition to the range of opioids with ADF designations already available, which meant that their decision mostly came down to whether they felt it made sense to bring a me-too opioid to the U.S. market. Their answer was mostly no.
“In the end, it’s another opioid, and I’m not sure we need another opioid,” said committee member Lonnie K. Zeltzer, MD, professor of pediatrics, anesthesiology, psychiatry, and biobehavioral sciences and director of pediatric pain at the University of California, Los Angeles “There are so many options for patients and for people who abuse these drug. I don’t see this formulation as having a profound impact, but I’m very concerned about adding more prescription opioids,” said Martin Garcia-Bunuel, MD, deputy chief of staff for the VA Maryland Health Care System in Baltimore. Another concern of some committee members was that ADF remains a designation with an uncertain meaning, pending the FDA’s analysis of the OxyContin data.
“At the end of the day, we don’t know whether any of the [ADF] stuff makes a difference,” noted Steve B. Meisel, PharmD, system director of medication safety for M Health Fairview in Minneapolis and a committee member,
The third agent, oxycodegol, a molecule designed to pass more slowly across the blood-brain barrier because of an attached polyethylene glycol chain that’s supposed to prevent a rapid high after ingestion and hence cut abuse potential. It received unanimous committee rejection, primarily because its safety and efficacy evidence had so many holes, but the shadow of opioid abuse permeated the committee’s discussion.
“One dogma in the abuse world is that slowing entry into the brain reduces abuse potential, but the opioid crisis showed that this is not the only factor. Some people have become addicted to slow-acting drugs. The abuse potential of this drug, oxycodegol, needs to be considered given where we’ve been with the opioid crisis,” said Jane B. Acri, PhD, chief of the Medications Discovery and Toxicology Branch of the National Institute on Drug Abuse.
“During the opioid epidemic, do we want to approve more opioids? If the [pain] efficacy is about the same as oxycodone, is better safety or abuse potential a reason to approve it? We need guidance [from the FDA] about what is ‘better enough.’ No opioid will ever be perfect; there will always be abuse and misuse. But what is good enough to justify bringing another opioid onto the market? What is a good enough improvement? I don’t have an answer,” Dr. Hernandez-Diaz said.
Adviser comments showed that the continued threat of widespread opioid addiction has cooled prospects for new opioid approvals by making FDA advisers skittish over how to properly score the incremental value of a new opioid.
“Do we need to go back to the drawing board on how we make decisions on exposing the American public to these kinds of agents?” Dr. Garcia-Bunuel asked. “I don’t think we have the tools to make these decisions.”
IHS and AAP Issue Recommendations on Prenatal Exposure to Opioids
The opioid crisis has hit the American Indian and Alaska Native (AI/AN) communities particularly hard, and “[i]nfants born withdrawing from opioids represent one of the most heartbreaking aspects,” says US Department of Health and Human Services Secretary Alex Azar.
Intrauterine exposure to opioids can induce symptoms that may result in spontaneous abortion, placental injury, and reduced nutrients for the fetus. Moreover, as many as 55% to 94% of infants prenatally exposed to opioids develop neonatal opioid withdrawal syndrome (NOWS), which can vary in severity from mild to life-threatening.
AI/AN women face significant barriers to obtaining appropriate care for substance use disorders, which may delay early interventions for the newborn’s health, said Shaquita Bell, MD, FAAP, chair of the American Academy of Pediatrics (AAP) Committee on Native American Child Health. The Indian Health Service (IHS) and the AAP have recently released clinical recommendations on NOWS for IHS, tribal, and urban Indian organization health care facilities.
The recommendations describe supportive, culturally appropriate standards of care for screening, diagnosing, and treating pregnant mothers and infants affected by prenatal opioid exposure. Management of NOWS begins with identifying women at risk, says the multidisciplinary panel responsible for the recommendations. Among other things, the experts advise screening a pregnant woman at the initial presentation for risk of substance use disorder, as well as for prescription opioid use for treatment of pain, and other risk factors for NOWS.
The panel notes that early application of nonpharmacologic treatment and support can reduce the need for pharmacologic treatment and transfer. Patient education should be a “key component of every prenatal care visit,” the panel says, provided in a nonjudgmental, culturally competent way to increase engagement, involving the partner and other family members if possible. Discussion topics may include the physical effects of continued substance use on both the woman and her infant, but also may include social and legal consequences of continued use.
The recommendations are also a companion guide to clinical recommendations for improving care of AI/AN pregnant women and women of childbearing age with opioid use disorder, which were announced by IHS and the American College of Obstetricians and Gynecologists in March 2019.
The opioid crisis has hit the American Indian and Alaska Native (AI/AN) communities particularly hard, and “[i]nfants born withdrawing from opioids represent one of the most heartbreaking aspects,” says US Department of Health and Human Services Secretary Alex Azar.
Intrauterine exposure to opioids can induce symptoms that may result in spontaneous abortion, placental injury, and reduced nutrients for the fetus. Moreover, as many as 55% to 94% of infants prenatally exposed to opioids develop neonatal opioid withdrawal syndrome (NOWS), which can vary in severity from mild to life-threatening.
AI/AN women face significant barriers to obtaining appropriate care for substance use disorders, which may delay early interventions for the newborn’s health, said Shaquita Bell, MD, FAAP, chair of the American Academy of Pediatrics (AAP) Committee on Native American Child Health. The Indian Health Service (IHS) and the AAP have recently released clinical recommendations on NOWS for IHS, tribal, and urban Indian organization health care facilities.
The recommendations describe supportive, culturally appropriate standards of care for screening, diagnosing, and treating pregnant mothers and infants affected by prenatal opioid exposure. Management of NOWS begins with identifying women at risk, says the multidisciplinary panel responsible for the recommendations. Among other things, the experts advise screening a pregnant woman at the initial presentation for risk of substance use disorder, as well as for prescription opioid use for treatment of pain, and other risk factors for NOWS.
The panel notes that early application of nonpharmacologic treatment and support can reduce the need for pharmacologic treatment and transfer. Patient education should be a “key component of every prenatal care visit,” the panel says, provided in a nonjudgmental, culturally competent way to increase engagement, involving the partner and other family members if possible. Discussion topics may include the physical effects of continued substance use on both the woman and her infant, but also may include social and legal consequences of continued use.
The recommendations are also a companion guide to clinical recommendations for improving care of AI/AN pregnant women and women of childbearing age with opioid use disorder, which were announced by IHS and the American College of Obstetricians and Gynecologists in March 2019.
The opioid crisis has hit the American Indian and Alaska Native (AI/AN) communities particularly hard, and “[i]nfants born withdrawing from opioids represent one of the most heartbreaking aspects,” says US Department of Health and Human Services Secretary Alex Azar.
Intrauterine exposure to opioids can induce symptoms that may result in spontaneous abortion, placental injury, and reduced nutrients for the fetus. Moreover, as many as 55% to 94% of infants prenatally exposed to opioids develop neonatal opioid withdrawal syndrome (NOWS), which can vary in severity from mild to life-threatening.
AI/AN women face significant barriers to obtaining appropriate care for substance use disorders, which may delay early interventions for the newborn’s health, said Shaquita Bell, MD, FAAP, chair of the American Academy of Pediatrics (AAP) Committee on Native American Child Health. The Indian Health Service (IHS) and the AAP have recently released clinical recommendations on NOWS for IHS, tribal, and urban Indian organization health care facilities.
The recommendations describe supportive, culturally appropriate standards of care for screening, diagnosing, and treating pregnant mothers and infants affected by prenatal opioid exposure. Management of NOWS begins with identifying women at risk, says the multidisciplinary panel responsible for the recommendations. Among other things, the experts advise screening a pregnant woman at the initial presentation for risk of substance use disorder, as well as for prescription opioid use for treatment of pain, and other risk factors for NOWS.
The panel notes that early application of nonpharmacologic treatment and support can reduce the need for pharmacologic treatment and transfer. Patient education should be a “key component of every prenatal care visit,” the panel says, provided in a nonjudgmental, culturally competent way to increase engagement, involving the partner and other family members if possible. Discussion topics may include the physical effects of continued substance use on both the woman and her infant, but also may include social and legal consequences of continued use.
The recommendations are also a companion guide to clinical recommendations for improving care of AI/AN pregnant women and women of childbearing age with opioid use disorder, which were announced by IHS and the American College of Obstetricians and Gynecologists in March 2019.
Cannabis users struggle to quit cigarettes
a large national survey has found.
“Over the past decade, there has been an increase in the use of cannabis among cigarette smokers and prevalence of cigarettes and cannabis co-use, suggesting that the negative consequences of cigarette–cannabis co-use may also become more prevalent over time,” wrote Andrea H. Weinberger, PhD, of Yeshiva University, New York, and colleagues. They noted that the prevalence of cigarette smoking is nearly three times higher among persons who use cannabis and have cannabis use disorders relative to those who do not.
The 2019 National Survey of Drug Use and Health estimated that 15.9% of Americans aged 12 years or older used cannabis in the past year. This number has been rising throughout the 2000s.
In that same report, cannabis use disorder (or marijuana use disorder) was defined as when an individual experiences clinically significant impairment caused by the recurrent use of marijuana, including health problems, persistent or increasing use, and failure to meet major responsibilities at work, school, or home. The report stated that approximately 1.6% of Americans aged 12 or older in 2018 had marijuana use disorder.
In the study published in Tobacco Control, the researchers used the National Survey on Drug Use and Health data to analyze cigarette smoking quit ratios among U.S. adults with and without cannabis use and cannabis use disorders. “Quit ratio was calculated as the proportion of former smokers among lifetime smokers and is considered a measure of total cessation in a population,” the researchers said.
In 2016, the quit ratios for adults with a history of cannabis use or cannabis use disorders were 23% and 15%, respectively, compared with 51% and 48%, respectively, in those with no cannabis use or cannabis use disorders.
Overall, quit ratios did not change significantly from 2002 to 2016 for individuals with cannabis use disorders after controlling for multiple demographic factors and other substance use disorders. However, during the same time period, quit ratios showed a nonlinear increase in cannabis users, nonusers, and individuals without cannabis use disorders.
The study findings were limited by several factors including the inability to generalize results to youth or individuals living outside the United States, the use of DSM-IV criteria to identify cannabis use disorder, the use of self-reports, and the inability to examine the timing of cannabis use as related to attempts to quit smoking, the researchers noted. However, the results highlight the need to consider offering smoking cessation treatment to individuals being treated for cannabis use disorders, and to include cannabis users in smoking cessation programs, the researchers noted.
“Based on our results, both public health and clinical efforts to improve cigarette quit outcomes may benefit from including those with any cannabis use,” they said. More research is needed to determine whether trends in the quit ratio change over time for cannabis users or those with cannabis use disorder, they added.
The study was funded by the National Institute on Drug Abuse. The researchers had no financial conflicts to disclose.
SOURCE: Weinberger AH et al. Tob Control. 2020;29(1):74-80. doi: 10.1136/tobaccocontrol-2018-054590.
a large national survey has found.
“Over the past decade, there has been an increase in the use of cannabis among cigarette smokers and prevalence of cigarettes and cannabis co-use, suggesting that the negative consequences of cigarette–cannabis co-use may also become more prevalent over time,” wrote Andrea H. Weinberger, PhD, of Yeshiva University, New York, and colleagues. They noted that the prevalence of cigarette smoking is nearly three times higher among persons who use cannabis and have cannabis use disorders relative to those who do not.
The 2019 National Survey of Drug Use and Health estimated that 15.9% of Americans aged 12 years or older used cannabis in the past year. This number has been rising throughout the 2000s.
In that same report, cannabis use disorder (or marijuana use disorder) was defined as when an individual experiences clinically significant impairment caused by the recurrent use of marijuana, including health problems, persistent or increasing use, and failure to meet major responsibilities at work, school, or home. The report stated that approximately 1.6% of Americans aged 12 or older in 2018 had marijuana use disorder.
In the study published in Tobacco Control, the researchers used the National Survey on Drug Use and Health data to analyze cigarette smoking quit ratios among U.S. adults with and without cannabis use and cannabis use disorders. “Quit ratio was calculated as the proportion of former smokers among lifetime smokers and is considered a measure of total cessation in a population,” the researchers said.
In 2016, the quit ratios for adults with a history of cannabis use or cannabis use disorders were 23% and 15%, respectively, compared with 51% and 48%, respectively, in those with no cannabis use or cannabis use disorders.
Overall, quit ratios did not change significantly from 2002 to 2016 for individuals with cannabis use disorders after controlling for multiple demographic factors and other substance use disorders. However, during the same time period, quit ratios showed a nonlinear increase in cannabis users, nonusers, and individuals without cannabis use disorders.
The study findings were limited by several factors including the inability to generalize results to youth or individuals living outside the United States, the use of DSM-IV criteria to identify cannabis use disorder, the use of self-reports, and the inability to examine the timing of cannabis use as related to attempts to quit smoking, the researchers noted. However, the results highlight the need to consider offering smoking cessation treatment to individuals being treated for cannabis use disorders, and to include cannabis users in smoking cessation programs, the researchers noted.
“Based on our results, both public health and clinical efforts to improve cigarette quit outcomes may benefit from including those with any cannabis use,” they said. More research is needed to determine whether trends in the quit ratio change over time for cannabis users or those with cannabis use disorder, they added.
The study was funded by the National Institute on Drug Abuse. The researchers had no financial conflicts to disclose.
SOURCE: Weinberger AH et al. Tob Control. 2020;29(1):74-80. doi: 10.1136/tobaccocontrol-2018-054590.
a large national survey has found.
“Over the past decade, there has been an increase in the use of cannabis among cigarette smokers and prevalence of cigarettes and cannabis co-use, suggesting that the negative consequences of cigarette–cannabis co-use may also become more prevalent over time,” wrote Andrea H. Weinberger, PhD, of Yeshiva University, New York, and colleagues. They noted that the prevalence of cigarette smoking is nearly three times higher among persons who use cannabis and have cannabis use disorders relative to those who do not.
The 2019 National Survey of Drug Use and Health estimated that 15.9% of Americans aged 12 years or older used cannabis in the past year. This number has been rising throughout the 2000s.
In that same report, cannabis use disorder (or marijuana use disorder) was defined as when an individual experiences clinically significant impairment caused by the recurrent use of marijuana, including health problems, persistent or increasing use, and failure to meet major responsibilities at work, school, or home. The report stated that approximately 1.6% of Americans aged 12 or older in 2018 had marijuana use disorder.
In the study published in Tobacco Control, the researchers used the National Survey on Drug Use and Health data to analyze cigarette smoking quit ratios among U.S. adults with and without cannabis use and cannabis use disorders. “Quit ratio was calculated as the proportion of former smokers among lifetime smokers and is considered a measure of total cessation in a population,” the researchers said.
In 2016, the quit ratios for adults with a history of cannabis use or cannabis use disorders were 23% and 15%, respectively, compared with 51% and 48%, respectively, in those with no cannabis use or cannabis use disorders.
Overall, quit ratios did not change significantly from 2002 to 2016 for individuals with cannabis use disorders after controlling for multiple demographic factors and other substance use disorders. However, during the same time period, quit ratios showed a nonlinear increase in cannabis users, nonusers, and individuals without cannabis use disorders.
The study findings were limited by several factors including the inability to generalize results to youth or individuals living outside the United States, the use of DSM-IV criteria to identify cannabis use disorder, the use of self-reports, and the inability to examine the timing of cannabis use as related to attempts to quit smoking, the researchers noted. However, the results highlight the need to consider offering smoking cessation treatment to individuals being treated for cannabis use disorders, and to include cannabis users in smoking cessation programs, the researchers noted.
“Based on our results, both public health and clinical efforts to improve cigarette quit outcomes may benefit from including those with any cannabis use,” they said. More research is needed to determine whether trends in the quit ratio change over time for cannabis users or those with cannabis use disorder, they added.
The study was funded by the National Institute on Drug Abuse. The researchers had no financial conflicts to disclose.
SOURCE: Weinberger AH et al. Tob Control. 2020;29(1):74-80. doi: 10.1136/tobaccocontrol-2018-054590.
FROM TOBACCO CONTROL